Antitumor Immunity and Treatment Toxicity: Unraveling the Dual Mechanisms of Cancer Immunotherapy
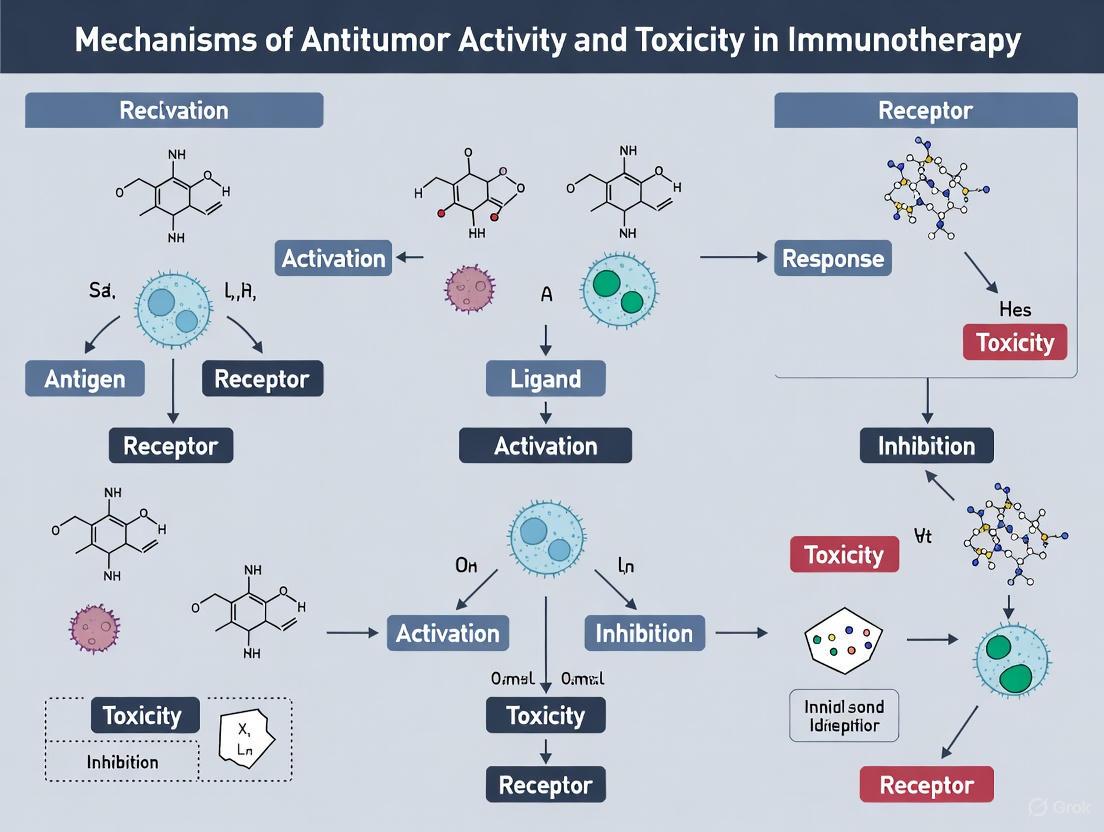
This review provides a comprehensive analysis of the molecular and cellular mechanisms that underpin both the efficacy and toxicity of cancer immunotherapy.
Antitumor Immunity and Treatment Toxicity: Unraveling the Dual Mechanisms of Cancer Immunotherapy
Abstract
This review provides a comprehensive analysis of the molecular and cellular mechanisms that underpin both the efficacy and toxicity of cancer immunotherapy. Tailored for researchers and drug development professionals, it synthesizes foundational science on immune checkpoint biology, the tumor microenvironment, and adoptive cell therapies. The article further explores the physiological basis of immune-related adverse events (irAEs), with a focus on cardiovascular, dermatological, and systemic toxicities. It critically evaluates current strategies to decouple antitumor activity from toxicity, including biomarker discovery, microbiome engineering, and combination treatments. By integrating foundational exploration with methodological applications, troubleshooting, and comparative validation, this work aims to inform the development of safer, more precise immunotherapeutic interventions.
Core Principles: Deconstructing the Immunological Mechanisms of Antitumor Activity
The cancer-immunity cycle provides a comprehensive framework for understanding the sequential events required to generate effective anti-cancer immune responses. This iterative process begins with T cell-mediated tumor cell killing, which leads to antigen presentation and T cell stimulation, creating a self-perpetuating cycle of immune activity against malignant cells [1] [2]. The cycle encompasses seven distinct yet interconnected steps that orchestrate the complex interplay between tumor cells and immune surveillance: (1) cancer cell death releases neoantigens and tumor-associated antigens; (2) antigen-presenting cells capture and process these antigens; (3) dendritic cells present antigens to prime and activate T cells in lymphoid organs; (4) activated effector T cells migrate through the bloodstream; (5) T cells infiltrate tumor sites; (6) T cells recognize cancer cells; and (7) cytotoxic T lymphocytes execute tumor cell killing, releasing additional antigens to perpetuate the cycle [3].
Understanding the cancer-immunity cycle is fundamental to advancing immunotherapy research, as any step can become rate-limiting, rendering the immune system unable to control tumor growth [2]. The remarkable progress in cancer immunotherapy over the past decade has led to a refined understanding of this cycle, including the evolving mechanism of checkpoint inhibition, the role of dendritic cells in sustaining anti-tumor immunity, and the dual nature of the tumor microenvironment in both facilitating and suppressing anti-cancer responses [2]. This whitepaper examines the core mechanisms of the cancer-immunity cycle within the broader context of antitumor activity and immunotherapy toxicity research, providing technical guidance and experimental approaches for researchers and drug development professionals.
Core Steps of the Cancer-Immunity Cycle: Mechanisms and Technical Assessment
Step 1: Antigen Release and Immunogenic Cell Death
The cancer-immunity cycle initiates with antigen release through immunogenic cell death (ICD), a critical process that transforms dying tumor cells into a therapeutic vaccine in situ. ICD involves the release of damage-associated molecular patterns (DAMPs) including calreticulin, ATP, and HMGB1 [4] [5]. These DAMPs serve as potent adjuvants that attract and activate antigen-presenting cells, particularly dendritic cells, thereby bridging innate and adaptive immunity [4].
The release of tumor-derived DNA during ICD activates the cGAS-STING pathway, a crucial mechanism of innate immune sensing within the tumor microenvironment [4] [6]. This pathway triggers type I interferon responses that enhance dendritic cell maturation and cross-priming of T cells. Recent research has also elucidated the role of extracellular vesicles, particularly exosomes, in shuttling tumor antigens to dendritic cells, expanding the scope of antigen presentation beyond traditional cellular mechanisms [4].
Table 1: Key DAMPs in Immunogenic Cell Death and Their Functions
| DAMP Molecule | Release Mechanism | Immune Function | Receptors |
|---|---|---|---|
| Calreticulin | Exposed on cell surface during ER stress | "Eat me" signal for phagocytes; enhances dendritic cell phagocytosis | LDL-receptor related protein-1 (LRP1) |
| ATP | Released from damaged mitochondria and cytoplasm | Chemoattractant for immune cells; activates NLRP3 inflammasome | P2X7, P2Y2 |
| HMGB1 | Released from nucleus during necrosis | Promotes antigen presentation; activates TLR4 pathway | TLR4, RAGE |
| Type I Interferons | Induced via cGAS-STING pathway | Dendritic cell activation; enhances cross-priming | IFNAR |
Step 2: Antigen Presentation and Dendritic Cell Maturation
Following antigen release, dendritic cells (DCs) play a pivotal role in capturing, processing, and presenting tumor antigens to T cells. Immature dendritic cells phagocytose tumor debris and undergo a complex maturation process that enables them to migrate to tumor-draining lymph nodes [4] [7]. The WDFY4 protein has been identified as critical for facilitating antigen transport to the cytosol, enabling cross-presentation of exogenous antigens on MHC class I molecules to CD8+ T cells [4].
The process of pyroptosis, a form of programmed cell death mediated by gasdermin proteins, induces potent immunogenic cell death that enhances dendritic cell maturation and establishes a positive feedback loop in the cancer-immunity cycle [4]. This creates a foundation for maximizing response rates to immune checkpoint blockade therapies. The efficiency of antigen presentation represents a crucial bottleneck in the cycle, as tumor-associated antigens alone often lack sufficient immunostimulatory potential to drive robust antitumor immunity without appropriate danger signals [5].
Step 3: T Cell Priming and Activation
In tumor-draining lymph nodes, mature dendritic cells present processed tumor antigens to naïve T cells, leading to T cell priming and activation [7]. The traditional three-signal model of T cell activation (TCR engagement, co-stimulation, and cytokine signaling) has been expanded to incorporate metabolic reprogramming as a crucial fourth signal [4]. The discovery of CD28-independent metabolic stimulation pathways, such as the ICOS-ICOSL axis, has broadened our understanding of T cell activation mechanisms [4].
Recent research has highlighted the importance of the actin cytoskeleton in T cell receptor microcluster formation and its impact on signal transduction, providing new insights into the spatial organization of T cell activation [4]. The role of innate-like T cells, particularly mucosal-associated invariant T (MAIT) cells and γδ T cells, in anti-tumor immunity has also gained recognition, although their precise functions in the cancer-immunity cycle warrant further investigation [4].
Table 2: Key Checkpoint Molecules Regulating T Cell Activation
| Checkpoint Molecule | Expression Pattern | Ligand(s) | Function in T Cell Biology | Therapeutic Inhibitors |
|---|---|---|---|---|
| CTLA-4 | Induced on activated T cells; constitutively expressed on Tregs | B7-1 (CD80), B7-2 (CD86) | Attenuates early T cell activation; mediates bystander suppression | Ipilimumab, Tremelimumab |
| PD-1 | Induced on chronically activated T cells | PD-L1, PD-L2 | Limits T cell activity in peripheral tissues; promotes exhaustion | Nivolumab, Pembrolizumab |
| LAG-3 | Activated T cells, NK cells | MHC class II, GAL-3, LSECtin | Negatively regulates cellular proliferation and effector function | Relatlimab |
| TIM-3 | IFN-γ-producing T cells | Galectin-9, HMGB1, CEACAM-1 | Regulates macrophage activation and T cell exhaustion | Cobolimab, Sabatolimab |
| TIGIT | T cells, NK cells | CD155, CD112 | Suppresses T cell responses by competing with CD226 | Tiragolumab |
Steps 4-5: T Cell Trafficking and Tumor Infiltration
Activated effector T cells must traffic through the circulatory system and infiltrate tumor tissue to execute their cytotoxic functions [3] [7]. This process involves a coordinated sequence of tethering, rolling, adhesion, and transendothelial migration mediated by specific adhesion molecules and chemokine receptors. The CXCL13-CXCR5 axis has emerged as particularly important for T cell migration and the formation of tertiary lymphoid structures, which serve as crucial hubs for anti-tumor immunity despite their lack of capsules [4].
The tumor vasculature often presents a significant barrier to T cell infiltration, with increased expression of adhesion molecules such as VCAM-1 and ICAM-1 enhancing T cell extravasation. Additionally, the chemokine landscape within tumors, particularly the expression of CXCL9, CXCL10, and CXCL11, directs T cell migration into tumor nests. Recent studies have demonstrated that CD8+ T cells producing CXCL13 can effectively predict response to immunotherapy, highlighting the importance of trafficking mechanisms in therapeutic success [4].
Steps 6-7: Cancer Cell Recognition and Cytotoxic Killing
The final steps of the cycle involve T cell recognition of cancer cells through T cell receptor engagement with peptide-MHC complexes, followed by execution of cytotoxic function [7]. Effector T cells induce tumor cell death through multiple mechanisms, including the release of perforin and granzymes, Fas-FasL interactions, and cytokine-mediated apoptosis [7]. Successful tumor cell killing releases additional tumor antigens, thereby perpetuating the cycle and potentially broadening the immune response through epitope spreading [3].
During this process, T cells progress through a differentiation continuum from progenitor exhausted T cells with stem cell-like properties to terminally exhausted T cells that have lost replicative and effector functions [4]. The immunosuppressive mechanisms within the tumor immune microenvironment drive this exhaustion process, with terminally exhausted T cells (Texterm) maintaining the ability to produce effector molecules but lacking durable anti-tumor capacity [4].
Quantitative Modeling of the Cancer-Immunity Cycle
Computational Frameworks for Cycle Analysis
Mathematical modeling provides powerful approaches for unraveling the complex interactions between tumors and the immune system. The Quantitative Cancer-Immunity Cycle (QCIC) model employs differential equations to capture the biological mechanisms underlying the cancer-immunity cycle and predicts tumor evolution dynamics under various treatment strategies through stochastic computational methods [7]. This multi-compartmental, multi-scale ODE framework includes four distinct biological compartments: tumor-draining lymph node (TDLN), peripheral blood (PB), tumor microenvironment (TME), and bone marrow and thymus (BT) [7].
The QCIC model introduces the treatment response index (TRI) to quantify disease progression in virtual clinical trials and the death probability function (DPF) to estimate overall survival [7]. Through biomarker analysis, this modeling approach has identified tumor-infiltrating CD8+ cytotoxic T lymphocytes as key predictors of disease progression and the tumor-infiltrating CD4+ Th1/Treg ratio as a significant determinant of survival outcomes in advanced metastatic colorectal cancer [7].
Table 3: Key Parameters in Quantitative Cancer-Immunity Cycle Modeling
| Parameter Category | Specific Parameters | Biological Significance | Measurement Techniques |
|---|---|---|---|
| T cell Dynamics | T cell activation rate, Proliferation rate, Exhaustion rate | Determines magnitude and duration of anti-tumor response | Flow cytometry, TCR sequencing |
| Tumor-Immune Interactions | Tumor kill rate by T cells, Immune suppression rate | Predicts efficacy of immune-mediated tumor control | Live-cell imaging, co-culture assays |
| Spatial Distribution | T cell infiltration rate, Chemokine gradients | Influences tumor penetration and contact with target cells | Multiplex IHC, spatial transcriptomics |
| Pharmacokinetic/Pharmacodynamic | Drug concentration, Target occupancy | Connects drug exposure to biological effect | Mass spectrometry, PET imaging |
Reaction-Diffusion Equations for Spatial Modeling
In addition to compartmental models, reaction-diffusion equations (RDEs) have been increasingly employed to describe molecular diffusion and intercellular interactions systematically [7]. These models excel at capturing the spatiotemporal dynamics of tumor-immune interactions, including adhesion processes and various cell migration patterns [7]. However, they typically fall short in explaining the biological mechanisms across different compartments of the organism, highlighting the complementary value of multi-compartmental approaches [7].
Experimental Methodologies for Investigating the Cancer-Immunity Cycle
Protocol 1: Assessing Immunogenic Cell Death In Vitro
Purpose: To quantify and characterize immunogenic cell death induced by therapeutic agents.
Materials:
- Tumor cell lines relevant to cancer type (e.g., MC38, B16F10, 4T1)
- Therapeutic agents (chemotherapeutics, targeted therapies, physical stressors)
- DAMP detection reagents: Anti-calreticulin antibody, ATP bioluminescence assay, HMGB1 ELISA kit
- Dendritic cells for co-culture experiments (e.g., bone marrow-derived DCs)
- Flow cytometry antibodies: CD11c, CD80, CD86, MHC class I/II
Procedure:
- Plate tumor cells in appropriate culture medium and allow to adhere overnight.
- Treat cells with ICD-inducing agents at predetermined concentrations (e.g., 1-10 μM for doxorubicin, 2-20 Gy for radiation).
- For surface calreticulin detection: Harvest cells at 12-24 hours post-treatment, stain with anti-calreticulin antibody, and analyze by flow cytometry.
- For ATP release: Collect supernatant at 4-6 hours post-treatment, measure ATP concentration using bioluminescence assay.
- For HMGB1 release: Collect supernatant at 24-48 hours post-treatment, quantify HMGB1 by ELISA.
- For functional assessment: Co-culture treated tumor cells with immature dendritic cells at 1:5 ratio (DC:tumor cell) for 24 hours, then analyze DC maturation markers by flow cytometry.
Validation: Compare DAMP release and DC maturation capacity across multiple ICD inducers and non-ICD inducing agents (e.g., UV-C irradiation) [5].
Protocol 2: T Cell Cytotoxicity and Exhaustion Assays
Purpose: To evaluate T cell-mediated killing of tumor cells and assess exhaustion markers.
Materials:
- Antigen-specific T cells (e.g., OT-I CD8+ T cells for ovalbumin model)
- Target tumor cells expressing cognate antigen
- Flow cytometry antibodies: CD3, CD8, CD44, CD62L, PD-1, TIM-3, LAG-3, TIGIT
- Cytokine detection: IFN-γ, TNF-α, IL-2 ELISA kits
- Real-time cell analysis (RTCA) system or equivalent cytotoxicity assay
Procedure:
- Isolate and activate antigen-specific T cells using cognate peptide (1 μg/mL) and IL-2 (50 IU/mL) for 3 days.
- Label target tumor cells with cell tracker dye according to manufacturer's protocol.
- Co-culture T cells with target cells at various effector:target ratios (e.g., 1:1 to 30:1) in 96-well plates.
- For real-time cytotoxicity: Use RTCA system to monitor cell impedance every 15 minutes for 48-72 hours.
- For endpoint analysis: At 4-6 hours, measure target cell death by flow cytometry using viability dyes.
- For exhaustion markers: After 5-7 days of repeated stimulation, stain T cells for exhaustion markers and analyze by flow cytometry.
- For cytokine production: Collect supernatant at 24 hours and measure IFN-γ, TNF-α, and IL-2 by ELISA.
Validation: Include controls for antigen specificity (irrelevant peptide) and baseline T cell activation (anti-CD3/CD28 beads) [4] [8].
Key Signaling Pathways in the Cancer-Immunity Cycle
PD-1/PD-L1 Signaling Axis
The PD-1/PD-L1 pathway represents one of the most clinically relevant immune checkpoints, with multiple approved therapeutic inhibitors [8] [6]. PD-1 engagement by its ligands PD-L1 or PD-L2 transmits inhibitory signals that dampen T cell receptor signaling through dephosphorylation of key signaling molecules via recruitment of SHP-2 phosphatase [8]. Tumor cells frequently upregulate PD-L1 expression in response to inflammatory cytokines (particularly IFN-γ) and oncogenic signaling pathways such as PI3K/AKT [6].
Diagram 1: PD-1/PD-L1 inhibitory signaling in T cells.
cGAS-STING Pathway in Innate Immune Sensing
The cGAS-STING pathway plays a crucial role in innate immune sensing of tumor-derived DNA, connecting immunogenic cell death to adaptive immunity [4] [6]. Cytosolic DNA sensors activate this pathway, leading to type I interferon production and enhanced dendritic cell cross-priming of T cells. This pathway has emerged as a promising target for enhancing anti-tumor immunity, particularly in immunologically "cold" tumors [6].
Diagram 2: cGAS-STING pathway in anti-tumor immunity.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Cancer-Immunity Cycle Investigation
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Immune Checkpoint Modulators | Anti-PD-1 (clone RMP1-14), Anti-CTLA-4 (clone 9D9), Anti-PD-L1 (clone 10F.9G2) | In vivo therapeutic studies, Mechanism of action research | Block inhibitory signals to enhance T cell function |
| Cytokine Detection | LEGENDplex panels, ELISA kits for IFN-γ, TNF-α, IL-2, IL-6 | Immune monitoring, T cell functionality assessment | Quantify immune activation and inflammatory responses |
| Cell Tracking Dyes | CFSE, CellTrace Violet, PKH26 | Proliferation assays, Adoptive transfer studies | Monitor cell division and migration in vivo and in vitro |
| MHC Multimers | PE- or APC-conjugated tetramers, dextramers | Antigen-specific T cell detection | Identify and isolate T cells with specific antigen specificity |
| Intracellular Staining Kits | FoxP3/Transcription Factor Staining Buffer Set | T cell differentiation and exhaustion analysis | Characterize T cell subsets and functional states |
| Animal Models | C57BL/6, BALB/c mice, MC38, B16F10, 4T1 tumor models | Preclinical efficacy studies, Tumor-immune interactions | Provide physiologically relevant systems for immunotherapy research |
The cancer-immunity cycle provides an essential framework for understanding the sequential events required for effective anti-tumor immunity and for developing strategies to overcome rate-limiting steps. Recent advances have refined our understanding of this cycle, including the evolving mechanisms of checkpoint inhibition, the role of dendritic cells in sustaining anti-tumor immunity, and the complex dynamics of the tumor microenvironment [2]. The integration of quantitative modeling approaches with experimental immunology has enabled more precise investigation of these dynamics and improved prediction of treatment outcomes [7].
Future research directions should focus on overcoming persistent challenges including tumor heterogeneity, immunosuppressive microenvironments, and acquired resistance mechanisms [3]. Novel approaches such as multi-epitope vaccines targeting conserved antigens, personalized vaccines incorporating patient-specific neoantigens, and innovative delivery systems designed to enhance lymph node targeting and antigen presentation show particular promise [3]. The convergence of artificial intelligence, systems immunology, and advanced manufacturing technologies will likely accelerate vaccine development and enable truly personalized cancer immunotherapy tailored to individual patients' immune profiles and tumor characteristics [3].
As the field advances, the cancer-immunity cycle will continue to serve as a fundamental conceptual framework for understanding and manipulating anti-tumor immune responses, guiding the development of next-generation immunotherapies with enhanced efficacy and reduced toxicity.
Immune checkpoint pathways, particularly cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and programmed death protein 1 (PD-1) and its ligand (PD-L1), constitute critical regulatory mechanisms that maintain immune homeostasis and prevent autoimmunity. In the tumor microenvironment, cancer cells exploit these pathways to evade immune surveillance, facilitating tumor progression. This technical review examines the molecular biology of CTLA-4 and PD-1/PD-L1 signaling, their distinct and complementary roles in immune regulation, and the mechanisms by which their inhibition generates antitumor immunity. We further analyze the experimental methodologies essential for investigating these pathways and summarize quantitative data on therapeutic efficacy and immune-related adverse events. Understanding these mechanisms provides the foundation for developing more effective immunotherapeutic strategies against cancer.
The adaptive immune system employs multiple checkpoint pathways to regulate the intensity and duration of immune responses, thereby maintaining self-tolerance and preventing autoimmunity. Among these, the CTLA-4 and PD-1/PD-L1 pathways represent two distinct but complementary mechanisms that negatively regulate T-cell activation and function at different stages of the immune response [9]. CTLA-4 primarily regulates the early phase of T-cell activation in lymphoid organs, while PD-1 modulates effector T-cell activity in peripheral tissues, particularly in the tumor microenvironment [9]. Malignant cells co-opt these inhibitory pathways to evade immune destruction, making them prime targets for cancer immunotherapy. Blockade of these checkpoints with monoclonal antibodies has demonstrated remarkable clinical efficacy across multiple cancer types, revolutionizing cancer treatment [10] [11]. This whitepaper provides a comprehensive technical analysis of the biology, signaling mechanisms, and therapeutic targeting of these critical immune checkpoint pathways within the broader context of antitumor immunity and treatment-related toxicity.
Molecular Biology of CTLA-4
Gene Structure and Protein Isoforms
The CTLA-4 gene is located on chromosome 2 in humans and consists of four exons [12]. Exon 1 encodes the leader peptide, exon 2 contains the ligand-binding domain, exon 3 comprises the transmembrane domain, and exon 4 encodes the cytoplasmic tail [13]. Alternative splicing generates multiple CTLA-4 isoforms:
- Full-length CTLA-4 (flCTLA-4): Contains all four exons and represents the membrane-bound form [12]
- Soluble CTLA-4 (sCTLA-4): Lacks exon 3 and is detectable in serum [13]
- Ligand-independent CTLA-4 (liCTLA-4): An murine-specific isoform containing exons 1, 3, and 4 [12]
In resting T-cells, CTLA-4 is predominantly localized in intracellular vesicles, with only minimal surface expression. Upon T-cell receptor (TCR) engagement, CTLA-4 rapidly translocates to the cell surface via exocytosis of CTLA-4-containing vesicles, a process regulated by TCR signaling strength in a graded feedback mechanism [9].
Expression and Regulation
CTLA-4 expression is primarily induced by T-cell activation, with detectable mRNA appearing within 1 hour of TCR ligation and peaking at 24-36 hours post-activation [13]. The transcription factor NF-AT plays a crucial role in CTLA-4 transcription, as inhibition of NF-AT activity significantly reduces CTLA-4 protein expression [13]. The intracellular trafficking and surface expression of CTLA-4 are tightly regulated by multiple mechanisms:
- Externalization: Mediated by TRIM (T-cell receptor interacting molecule) in the trans-Golgi network, GTPase ARF-1, phospholipase D, calcium influx, and Rab11 [13]
- Internalization: Occurs through both clathrin-dependent (via adaptor proteins CAP-1 and CAP-2) and clathrin-independent (via dynamin) pathways [13]
- Degradation: CTLA-4 binds with CAP-1 in the Golgi apparatus and is transported to lysosomal compartments for degradation [13]
Regulatory T cells (Tregs) constitutively express CTLA-4, which is essential for their suppressive function [12]. Genetic deletion of CTLA-4 in Tregs impairs their ability to suppress immune responses, leading to massive lymphoproliferation and fatal autoimmune disease [12] [9].
Signaling Mechanisms
CTLA-4 functions primarily as a competitive inhibitor of the co-stimulatory receptor CD28. Both molecules share the same ligands, CD80 (B7-1) and CD86 (B7-2), but CTLA-4 binds with significantly higher affinity and avidity [9]. The inhibitory function of CTLA-4 is mediated through several distinct mechanisms:
- Ligand Competition: CTLA-4 outcompetes CD28 for binding to CD80/CD86, thereby preventing CD28-mediated co-stimulation [9]
- Signal Inhibition: CTLA-4 engagement generates intracellular signals that actively inhibit T-cell activation by dephosphorylating key TCR signaling components, including CD3ζ and ZAP70 [13]
- Ligand Transendocytosis: CTLA-4 on Tregs physically removes CD80/CD86 from antigen-presenting cells through trans-endocytosis, thereby reducing the availability of co-stimulatory ligands for CD28 on effector T-cells [12]
- Metabolic Regulation: CTLA-4 signaling inhibits Akt phosphorylation and activation, negatively regulating cell cycle progression and T-cell proliferation [13]
The following diagram illustrates CTLA-4 signaling and its inhibitory effects on T-cell activation:
Figure 1: CTLA-4 Signaling Pathway. CTLA-4 competes with CD28 for binding to B7 molecules on antigen-presenting cells (APCs), generating inhibitory signals that counteract T-cell receptor (TCR) and CD28-mediated activation.
Molecular Biology of PD-1/PD-L1
Gene Structure and Expression
PD-1 (programmed death protein 1, CD279) is a 55-kDa transmembrane protein belonging to the CD28/CTLA-4 superfamily [14]. The PD-1 gene encodes a 288-amino acid protein consisting of an extracellular IgV-like domain, a transmembrane domain, and a cytoplasmic tail containing both an immunoreceptor tyrosine-based inhibitory motif (ITIM) and an immunoreceptor tyrosine-based switch motif (ITSM) [14] [15]. PD-1 expression is induced on T cells, B cells, natural killer (NK) cells, monocytes, and dendritic cells upon activation [14]. The transcription of PD-1 is regulated by multiple transcription factors, including NFAT, NOTCH, FOXO1, and IRF9, which bind to conserved regulatory regions in the PD-1 promoter [14].
PD-L1 (programmed death ligand 1, B7-H1, CD274) is a 33-kDa type I transmembrane glycoprotein containing 290 amino acids with Ig-like and IgC-like domains in its extracellular region [14]. PD-L1 is constitutively expressed on macrophages, dendritic cells, and some epithelial cells, and its expression can be induced by inflammatory cytokines, particularly interferon-gamma (IFN-γ), through the JAK/STAT signaling pathway [14] [10]. In the tumor microenvironment, multiple cancer types exploit this pathway by upregulating PD-L1 expression as an "adaptive immune resistance" mechanism [14].
Signaling Mechanisms
The PD-1/PD-L1 axis suppresses T-cell function through multiple intricate signaling pathways:
SHP2-Mediated Dephosphorylation: Upon PD-1 binding to PD-L1, phosphorylation of tyrosine residues in the ITSM and ITIM motifs recruits the tyrosine phosphatase SHP2 [15]. Activated SHP2 dephosphorylates key signaling molecules in the TCR pathway, including CD3ζ, ZAP70, and PKCθ, thereby attenuating TCR signal transduction [15]
PI3K/AKT Pathway Inhibition: PD-1 signaling enhances PTEN phosphatase activity by inhibiting casein kinase 2 (CK2)-mediated phosphorylation of PTEN [16]. Active PTEN dephosphorylates PIP3 to PIP2, reducing PIP3 availability and consequently inhibiting PI3K/AKT pathway activation, which is crucial for T-cell survival, metabolism, and proliferation [16]
Ras/MEK/ERK Pathway Inhibition: PD-1 suppresses the activation of the Ras/MEK/ERK pathway by inhibiting PLCγ1 activation, thereby reducing diacylglycerol (DAG) production and calcium influx, ultimately impairing T-cell proliferation and differentiation [16]
Metabolic Reprogramming: PD-1 signaling inhibits glycolysis and promotes fatty acid oxidation, shifting T-cell metabolism toward a state of energy conservation that is incompatible with robust effector function [15]
Transcriptional Regulation: Chronic PD-1 signaling induces epigenetic modifications that stabilize the exhausted T-cell phenotype, characterized by reduced production of effector cytokines (IL-2, TNF-α, IFN-γ) and impaired cytolytic function [9]
The following diagram illustrates the intracellular signaling mechanisms of the PD-1/PD-L1 pathway:
Figure 2: PD-1/PD-L1 Intracellular Signaling. PD-1 engagement recruits SHP2, which dephosphorylates key TCR signaling components. Concurrently, PD-1 signaling activates PTEN and inhibits PLCγ1, suppressing both PI3K/AKT and Ras/MEK/ERK pathways, ultimately leading to T-cell exhaustion.
Comparative Analysis of CTLA-4 and PD-1/PD-L1 Pathways
While both CTLA-4 and PD-1 function as inhibitory immune checkpoints, they regulate distinct phases of immune responses through different mechanisms. The table below summarizes the key differences between these two critical pathways:
Table 1: Comparative Analysis of CTLA-4 and PD-1/PD-L1 Pathways
| Parameter | CTLA-4 Pathway | PD-1/PD-L1 Pathway |
|---|---|---|
| Primary Function | Regulates early T-cell activation in lymphoid organs | Modulates effector T-cell function in peripheral tissues |
| Expression Pattern | Primarily on activated T cells and constitutively on Tregs | On activated T cells, B cells, NK cells, monocytes, and DCs |
| Main Ligands | CD80 (B7-1), CD86 (B7-2) | PD-L1 (B7-H1), PD-L2 (B7-DC) |
| Binding Affinity | Higher affinity for CD80/CD86 than CD28 | High affinity for both PD-L1 and PD-L2 |
| Primary Mechanism | Competes with CD28 for ligands; transendocytosis | Transduces inhibitory signals via SHP2 phosphorylation |
| Key Signaling Pathways | Inhibition of ZAP70, CD3ζ; reduced AKT activation | Inhibition of PI3K/AKT and Ras/MEK/ERK via SHP2 |
| Role in Cancer | Limits initial T-cell activation against tumor antigens | Mediates T-cell exhaustion in tumor microenvironment |
| Therapeutic Targeting | Ipilimumab (anti-CTLA-4) | Nivolumab, Pembrolizumab (anti-PD-1); Atezolizumab (anti-PD-L1) |
Therapeutic Targeting in Cancer Immunotherapy
Mechanism of Antitumor Activity
Immune checkpoint inhibitors (ICIs) function by blocking the interaction between inhibitory receptors and their ligands, thereby restoring T-cell-mediated antitumor immunity. The mechanisms of action differ between CTLA-4 and PD-1/PD-L1 blockade:
CTLA-4 Inhibition:
- Enhances priming and activation of tumor-specific T cells in lymph nodes [9]
- Increases the T-cell receptor diversity and repertoire [11]
- Reduces Treg-mediated suppression in the tumor microenvironment through Fc receptor-dependent depletion of intratumoral Tregs [11]
- Promotes clonal expansion of tumor-reactive T cells [9]
PD-1/PD-L1 Inhibition:
- Reverses T-cell exhaustion in the tumor microenvironment [15]
- Restores cytokine production (IFN-γ, TNF-α, IL-2) and cytotoxic function of tumor-infiltrating lymphocytes [14]
- Reactivates antigen-experienced T cells that have become dysfunctional [9]
- Enhances T-cell survival and metabolic fitness within tumors [15]
Dual Blockade: Combined CTLA-4 and PD-1/PD-L1 inhibition produces synergistic antitumor effects through complementary mechanisms. CTLA-4 blockade expands the T-cell repertoire during priming, while PD-1/PD-L1 blockade reverses exhaustion in the effector phase [11]. This combination has demonstrated superior efficacy in multiple cancer types, including melanoma and non-small cell lung cancer, albeit with increased immune-related adverse events [11].
Quantitative Clinical Data
Table 2: Clinical Efficacy of Immune Checkpoint Inhibitors in Selected Cancers
| Therapy | Cancer Type | Objective Response Rate (%) | Overall Survival (Months) | Grade 3-5 Adverse Events (%) |
|---|---|---|---|---|
| Ipilimumab (anti-CTLA-4) | Melanoma | 10.9-15.2 | 10.0-11.4 | 19.9-27.3 |
| Nivolumab (anti-PD-1) | Melanoma | 31.7-44 | 25.5-37.5 | 15.0-21.8 |
| Pembrolizumab (anti-PD-1) | NSCLC | 19.4-44.8 | 10.4-30.0 | 9.5-16.5 |
| Nivolumab + Ipilimumab | Melanoma | 50-58 | 36.9-Not Reached | 55.0-59.0 |
| Nivolumab + Ipilimumab | NSCLC | 35.9-43.7 | 17.1-Not Reached | 31.0-36.4 |
Table 3: Incidence of Immune-Related Adverse Events (irAEs) with Checkpoint Inhibitors
| Adverse Event | Anti-CTLA-4 (%) | Anti-PD-1/PD-L1 (%) | Combination Therapy (%) |
|---|---|---|---|
| Any Grade irAE | 72.1-88.9 | 66.1-74.1 | 89.9-95.1 |
| Colitis/Diarrhea | 8.3-36.3 | 1.5-2.9 | 9.4-13.6 |
| Hepatitis | 1.5-10.0 | 0.7-3.6 | 11.0-15.0 |
| Pneumonitis | 0.0-1.5 | 1.6-4.1 | 4.4-7.0 |
| Rash | 15.2-30.3 | 9.3-19.6 | 21.1-30.5 |
| Endocrinopathies | 4.3-10.0 | 4.1-10.6 | 7.6-13.0 |
Experimental Methodologies
Key Research Protocols
In Vitro T-cell Activation and Inhibition Assays:
- T-cell Stimulation: Isolate human PBMCs or mouse splenocytes and activate with anti-CD3/CD28 antibodies (1-5 μg/mL) for 24-72 hours [12]
- Checkpoint Blockade: Add anti-CTLA-4 (10 μg/mL) or anti-PD-1/PD-L1 (5-10 μg/mL) antibodies to cultures
- Proliferation Measurement: Assess using 3H-thymidine incorporation or CFSE dilution by flow cytometry [12]
- Cytokine Analysis: Quantify IL-2, IFN-γ, TNF-α in supernatants by ELISA or multiplex immunoassay
- Signaling Analysis: Perform Western blotting for phosphorylated AKT, ERK, ZAP70, and SHP2
Mixed Lymphocyte Reaction (MLR):
- Stimulator Cells: Irradiate (30 Gy) allogeneic PBMCs or dendritic cells
- Responder Cells: Label with CFSE and co-culture with stimulators at 1:1 to 1:10 ratios
- Checkpoint Modulation: Add blocking antibodies or recombinant checkpoint proteins
- Analysis: Measure T-cell proliferation after 5-7 days by flow cytometry and cytokine production
Transendocytosis Assay (CTLA-4 Function):
- Cell Preparation: Generate CTLA-4-expressing cells (Tregs or transfected cells) and CD80-GFP-expressing APCs
- Co-culture: Incubate cells at 37°C for 2-4 hours
- Analysis: Quantify CD80-GFP internalization by flow cytometry or confocal microscopy [12]
T-cell Exhaustion Models:
- Chronic Stimulation: Repeatedly stimulate T cells with antigen or anti-CD3 weekly for 3-5 cycles
- Exhaustion Markers: Analyze PD-1, TIM-3, LAG-3 expression by flow cytometry
- Functional Assessment: Measure cytokine production (IFN-γ, TNF-α, IL-2) and cytotoxic activity after restimulation
- Rescue Experiments: Test PD-1/PD-L1 blockade during later stimulation cycles
In Vivo Tumor Models
Syngeneic Mouse Models:
- Tumor Inoculation: Implant 5×10^5 to 1×10^6 syngeneic tumor cells (B16-F10 melanoma, MC38 colon carcinoma) subcutaneously
- Treatment Initiation: Begin checkpoint inhibitor therapy when tumors reach 50-100 mm³
- Dosing Regimen: Administer anti-CTLA-4 (100-200 μg), anti-PD-1/PD-L1 (100-200 μg), or combination intraperitoneally every 3-4 days for 3-4 doses
- Endpoint Measurements: Monitor tumor volume twice weekly and survival daily
- Immune Analysis: Harvest tumors and lymphoid organs for flow cytometry, immunohistochemistry, and cytokine analysis
Genetically Engineered Mouse Models (GEMMs):
- Model Selection: Utilize spontaneous tumor models (e.g., TRAMP for prostate cancer, KPC for pancreatic cancer)
- Treatment Schedule: Initiate therapy at defined tumor stages or ages
- Long-term Monitoring: Assess tumor development, immune infiltration, and treatment efficacy over time
The Scientist's Toolkit
Table 4: Essential Research Reagents for Immune Checkpoint Investigation
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Blocking Antibodies | Anti-CTLA-4 (clone 9D9), Anti-PD-1 (clone RMP1-14), Anti-PD-L1 (clone 10F.9G2) | In vitro and in vivo checkpoint blockade experiments |
| Recombinant Proteins | CTLA-4-Ig (Abatacept), PD-1-Fc, PD-L1-Fc | Ligand binding studies, inhibition assays |
| Reporters Systems | NFAT-luciferase, NF-κB-luciferase reporters | T-cell activation signaling measurement |
| Flow Cytometry Panels | Anti-CD3, CD4, CD8, CD25, CD44, CD62L, PD-1, CTLA-4, TIM-3, LAG-3 | Immune phenotyping and exhaustion marker analysis |
| Transgenic Models | CTLA-4 KO mice, PD-1 KO mice, huPD-1/huPD-L1 knock-in mice | Genetic function studies, humanized therapy testing |
| Signal Transduction Assays | Phospho-specific antibodies for ZAP70, AKT, ERK, SHP2 | Intracellular signaling pathway analysis |
The CTLA-4 and PD-1/PD-L1 pathways represent fundamental regulatory mechanisms that maintain immune homeostasis while serving as critical barriers to effective antitumor immunity. Understanding their distinct yet complementary biology has enabled the development of revolutionary cancer immunotherapies that have transformed treatment paradigms across multiple malignancies. Current research continues to elucidate the intricate molecular signaling events downstream of these receptors, their complex regulation at genetic, epigenetic, and post-translational levels, and their interactions with other immune modulators in the tumor microenvironment.
Future investigations should focus on several key areas: (1) identifying predictive biomarkers to optimize patient selection for monotherapy versus combination approaches; (2) developing strategies to overcome resistance to checkpoint inhibition; (3) elucidating the mechanisms underlying immune-related adverse events to improve therapeutic indices; and (4) designing novel therapeutic modalities such as bispecific antibodies that simultaneously target multiple checkpoints with reduced toxicity. As our understanding of these pathways deepens, so too will our ability to harness the immune system against cancer while maintaining the delicate balance of immune homeostasis.
The tumor microenvironment (TME) is a complex ecosystem that constitutes a major barrier to effective anti-tumor immunity and immunotherapy. This whitepaper delineates the primary mechanisms—cellular, molecular, and metabolic—through which the TME orchestrates immune evasion. We synthesize current research on stromal cell-mediated suppression, immune checkpoint dysregulation, and novel processes such as mitochondrial transfer. Furthermore, we provide a detailed experimental methodology for quantifying immunotherapy response, integrating multiparametric MRI and immunohistochemical validation. Designed for researchers and drug development professionals, this guide includes structured data, pathway visualizations, and a catalog of essential research reagents to facilitate the development of novel therapeutic strategies aimed at overcoming the immunosuppressive TME.
The tumor microenvironment (TME) is a dynamic and heterogeneous milieu composed of tumor cells, immune cells, stromal cells, vasculature, and extracellular matrix (ECM) that collectively play a decisive role in tumor initiation, progression, and resistance to therapy [17] [18]. Immune evasion within this ecosystem has emerged as a critical hallmark of cancer, enabling tumors to circumvent host immune surveillance and resist immunotherapeutic interventions [19]. The clinical significance of the TME is underscored by the limitations of current immune checkpoint inhibitors (ICIs), which, despite revolutionizing cancer care, yield durable responses only in a subset of patients [17] [20]. A comprehensive understanding of the TME's immunosuppressive mechanisms is therefore paramount for advancing precision oncology and developing effective combination therapies.
The TME fosters immunosuppression through a multifaceted network of interacting components. These include metabolic reprogramming that starves immune cells of essential nutrients; stromal cell-driven immune dysfunction; epigenetic remodeling that fosters immune tolerance; and the dysregulation of critical immune checkpoint pathways [17] [19]. Recent breakthroughs, such as the discovery of mitochondrial transfer from cancer cells to T cells, reveal previously unknown dimensions of tumor-induced immune suppression [20]. This in-depth technical guide will systematically dissect these barriers to effective immunity, providing a framework for researchers and drug development professionals to identify and target the TME's most vulnerabilities.
Cellular and Molecular Mechanisms of Immune Evasion
Stromal Cell-Mediated Immunosuppression
Stromal cells, particularly cancer-associated fibroblasts (CAFs), are the most abundant non-immune cellular components of the TME and are critical accomplices in tumor progression and immune evasion [21] [18]. CAFs originate from various sources, including resident fibroblasts, mesenchymal stem cells (MSCs), and endothelial cells, through transdifferentiation induced by tumor-derived factors such as TGF-β, PDGF, and FGF-2 [18]. They contribute to immunosuppression through several mechanisms:
- Secretion of Immunosuppressive Mediators: CAFs secrete a plethora of cytokines and chemokines, including CXCL12, which can directly exclude T cells from the tumor periphery, creating an "immune-excluded" phenotype [17] [21]. They also produce TGF-β, which drives the differentiation of regulatory T cells (Tregs) and confers CD8+ T cells with a stem-like exhausted epigenetic state [17].
- Metabolic Interference: CAFs contribute to metabolic reprogramming by expressing CD39/CD73 ectoenzymes, which catalyze the conversion of extracellular ATP to immunosuppressive adenosine, thereby blunting T cell activation [17].
- Extracellular Matrix Remodeling: CAFs deposit and cross-link ECM components, creating a physical barrier that impedes T cell infiltration and promotes a "immune desert" phenotype [17] [18]. This dense ECM also contributes to increased interstitial fluid pressure and impairs drug delivery.
The relationship between stromal cells and immune cells is complex. For instance, CAFs interact with tumor-associated macrophages (TAMs) to enhance tumorigenesis. CAF-derived factors such as IL-6, GM-CSF, and M-CSF can recruit and polarize macrophages towards an M2-like, immunosuppressive phenotype [21]. These TAMs, in turn, produce IL-10 and VEGF, further contributing to an immunosuppressive and pro-angiogenic niche [17] [21].
Immune Checkpoint Dysregulation
Immune checkpoints are crucial regulatory molecules that maintain self-tolerance and prevent autoimmunity. Tumors co-opt these pathways to suppress T cell activity and evade immune destruction [17] [22]. The programmed death-1 (PD-1) receptor on T cells and its ligand (PD-L1) on tumor and stromal cells constitute a primary axis of immune suppression in the TME.
- PD-1/PD-L1 Axis: PD-L1 is overexpressed in approximately 50% of head and neck squamous cell carcinoma (HNSCC) cases [17]. Engagement of PD-1 with PD-L1 transduces inhibitory signals that lead to T cell exhaustion, characterized by impaired effector function and proliferative capacity. Tumor cells can also release extracellular vesicles (EVs) containing PD-L1, which can systemically suppress T cell activity [17].
- CTLA-4 Pathway: Cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) is another critical checkpoint, expressed predominantly on T cells, that competes with the co-stimulatory molecule CD28 for binding to B7 molecules on antigen-presenting cells. This interaction inhibits early T cell activation in lymph nodes [22]. Antibodies blocking CTLA-4 (e.g., ipilimumab) have demonstrated clinical efficacy, particularly in combination with PD-1 inhibitors [23] [24].
- Spatial Heterogeneity: The expression of checkpoints is not uniform. Spatial proteomic analyses have revealed PD-L1 enrichment at the invasive front of tumors, particularly on cancer stem-like cells (CSCs), where they impair immune synapse formation and protect this critical cell population [17].
The following table summarizes key immune checkpoints and their roles in the TME:
Table 1: Key Immune Checkpoints in the Tumor Microenvironment
| Checkpoint Molecule | Primary Expression | Ligand(s) | Mechanism of Action in TME | Therapeutic Inhibitors |
|---|---|---|---|---|
| PD-1 | T cells | PD-L1, PD-L2 | Induces T cell exhaustion and anergy; suppresses cytokine production and cytotoxicity [17] [22]. | Pembrolizumab, Nivolumab, Cemiplimab [22] |
| PD-L1 | Tumor cells, APCs, Stromal cells | PD-1 | Binds PD-1 on T cells to inhibit anti-tumor activity; can be secreted via EVs for systemic suppression [17] [22]. | Atezolizumab, Avelumab, Durvalumab [22] |
| CTLA-4 | T cells (primarily at activation) | B7-1 (CD80), B7-2 (CD86) | Outcompetes CD28 for B7 binding, transducing inhibitory signals and dampening early T cell activation [23] [22]. | Ipilimumab, Tremelimumab [23] [22] |
| LAG-3 | T cells, NK cells | MHC Class II | Negatively regulates T cell proliferation and effector function; contributes to T cell exhaustion [22]. | Relatlimab (in combo with Nivolumab) [22] |
Metabolic Reprogramming and Nutrient Competition
The TME is often characterized by nutrient deprivation, hypoxia, and acidosis, conditions that tumor cells adapt to but which severely impair effector immune cell function [17] [19]. This metabolic reprogramming constitutes a fundamental mechanism of immune evasion.
- Glycolytic Competition and Acidosis: Tumor cells predominantly utilize glycolysis for energy, even in normoxic conditions (the Warburg effect). This high glycolytic flux consumes glucose, a critical nutrient for T cell effector functions, and results in the accumulation of lactic acid. Lactate-induced acidosis directly inhibits T cell activation, proliferation, and cytokine production, while simultaneously promoting the differentiation of immunosuppressive Tregs [17].
- Hypoxia: Hypoxic regions within tumors activate hypoxia-inducible factors (HIFs) in both tumor and stromal cells. HIF-1α activation can upregulate PD-L1 expression on tumor cells and adenosine production via CD39/CD73 on Tregs, further amplifying immune suppression [17].
- Amino Acid Depletion: Enzymes such as indoleamine 2,3-dioxygenase (IDO) and arginase 1 (ARG1) are often overexpressed in the TME by cells like MDSCs and TAMs. IDO catabolizes tryptophan, while ARG1 depletes L-arginine. The depletion of these essential amino acids impairs T cell receptor signaling and leads to T cell cell cycle arrest [17] [21].
A Novel Mechanism: Mitochondrial Transfer
A groundbreaking study published in Nature has uncovered a previously unknown mechanism of immune evasion: the transfer of mitochondria from cancer cells to T cells [20]. This process leads to metabolic sabotage and functional impairment of tumor-infiltrating lymphocytes (TILs).
Experimental Workflow and Key Findings:
- Observation: Analysis of TILs from patient samples revealed that a subset harbored mitochondrial DNA (mtDNA) mutations identical to those in the matched cancer cells, suggesting transfer [20].
- Mechanism Investigation: In vitro co-culture experiments demonstrated that mitochondria are transferred from cancer cells to T cells via two primary routes: direct cell-cell contact through tunnelling nanotubes (TNTs) and indirectly via small extracellular vesicles (EVs). The use of inhibitors like cytochalasin B (TNT inhibitor) and GW4869 (EV release inhibitor) confirmed the involvement of both pathways [20].
- Functional Consequence: The transferred mutant mitochondria, equipped with mitophagy-inhibitory molecules, evade degradation in the T cells. This leads to homoplasmic replacement of the T cell's endogenous mitochondria. The resultant mitochondrial dysfunction causes metabolic abnormalities, senescence, and defective memory formation in T cells, severely compromising their antitumor capacity [20].
- Clinical Correlation: The presence of shared mtDNA mutations in tumor tissue and TILs was associated with a poorer prognosis in patients with melanoma or non-small cell lung cancer (NSCLC) receiving immune checkpoint inhibitors, highlighting its clinical relevance [20].
This mechanism reveals a sophisticated strategy where cancer cells directly compromise the cellular energetics of attacking T cells.
Quantitative Assessment of the TME and Immunotherapy Response
Accurate assessment of the TME and early response to immunotherapy is critical for both basic research and clinical translation. Conventional anatomical imaging often fails to distinguish true progression from pseudoprogression. The following section details a multiparametric MRI (mpMRI) protocol for quantitative response assessment in a pre-clinical model, validated by ex vivo immunohistochemistry [24].
Experimental Protocol: mpMRI in a Murine Melanoma Model
Objective: To assess early response to combined anti-PD-L1 and anti-CTLA-4 immunotherapy using quantitative mpMRI features with ex vivo immunohistochemical validation [24].
Materials and Methods:
- Animal Model: Subcutaneous inoculation of B16-F10 murine melanoma cells into C57BL/6 mice (n=28). Randomization into therapy (n=14) and control (n=14) groups [24].
- Therapy Regimen: The therapy group received intraperitoneal injections of anti-PD-L1 and anti-CTLA-4 antibodies (20 µg/kg) on days 7, 9, and 11 post-inoculation. The control group received a placebo [24].
- MRI Acquisition:
- Scanner: 3-T clinical MRI scanner.
- Timepoints: Baseline (day 7) and follow-up (day 12).
- Sequences:
- T1-weighted imaging: For tumor morphology and volume.
- Diffusion-weighted imaging (DWI): To assess cellularity. Apparent Diffusion Coefficient (ADC) maps were calculated.
- Dynamic Contrast-Enhanced (DCE)-MRI: To evaluate perfusion and vascular permeability. Parameters like plasma volume (PV) and plasma flow (PF) were derived via tracer-kinetic modeling [24].
- Ex Vivo Validation: A separate cohort (n=24) was used for immunohistochemical analysis of:
- CD8+ T cells: To quantify tumor-infiltrating lymphocytes (TILs).
- Ki-67: To assess tumor cell proliferation.
- TUNEL: To measure apoptosis.
- CD31+: To determine microvascular density [24].
Key Results and Interpretation: The following table synthesizes the quantitative findings from this study, demonstrating how mpMRI parameters correlate with immunological and pathological changes in the TME post-therapy.
Table 2: Quantitative mpMRI and Immunohistochemistry Findings in Immunotherapy Response [24]
| Parameter | Group | Baseline (Day 7) | Follow-up (Day 12) | Ex Vivo Validation (IHC) | Biological Interpretation |
|---|---|---|---|---|---|
| Tumor Volume | Control | Volume V1 | Significant increase (p ≤ 0.004) | N/A | Uncontrolled tumor growth. |
| Immunotherapy | Volume V1 ~= Control | Significant increase (p ≤ 0.004); No difference vs. Control (p = 0.630) | N/A | Pseudoprogression: Initial increase not indicative of true progression. | |
| ADC (mm²/s) | Control | Value A1 | No significant change | N/A | Stable tumor cellularity. |
| Immunotherapy | Value A1 ~= Control | Significant decrease (p = 0.001) | Higher CD8+ TILs (p = 0.048) | Decreased ADC reflects increased cellularity due to robust infiltration of T cells, an early sign of efficacy. | |
| Plasma Flow / Volume | Immunotherapy | N/A | N/A | Lower microvascular density (CD31+) (p < 0.001) | Antiangiogenic effect of successful immunotherapy. |
| N/A (IHC only) | Immunotherapy | N/A | N/A | Higher TUNEL (p < 0.001); Lower Ki-67 (p < 0.001) | Increased tumor cell apoptosis and decreased proliferation confirm therapeutic efficacy. |
This integrated approach demonstrates that functional MRI parameters like ADC are more sensitive indicators of early immunological response than tumor volume alone, providing a non-invasive window into dynamic changes within the TME.
Visualizing Key Mechanisms and Workflows
The "Trinity" Network of Immune Evasion in HNSCC
This diagram illustrates the three interlinked core pathways that drive immune evasion, as proposed in recent literature [17].
Mitochondrial Transfer from Cancer Cell to T Cell
This flowchart details the novel immune evasion mechanism involving the transfer of mitochondria from cancer cells to T cells, leading to T cell dysfunction [20].
The Scientist's Toolkit: Key Research Reagents
The following table catalogs essential reagents and tools, derived from the cited experimental protocols, for investigating the TME and immune evasion mechanisms [24] [20].
Table 3: Essential Research Reagents for TME and Immune Evasion Studies
| Reagent / Tool | Category | Specific Example(s) | Research Application / Function |
|---|---|---|---|
| Immune Checkpoint Inhibitors | Biologics | Anti-PD-L1 antibody, Anti-CTLA-4 antibody [24] | In vivo intervention to study the effects of checkpoint blockade on the TME and tumor growth. |
| Pathway Inhibitors | Small Molecules | Cytochalasin B, GW4869, Y-27632 [20] | Mechanistic studies: Inhibit TNT formation (Cytochalasin B), small EV release (GW4869), or large EV release (Y-27632). |
| Cell Line | In Vitro/In Vivo Model | B16-F10 murine melanoma cells [24] | Syngeneic mouse model for studying immunotherapy and TME dynamics in vivo. |
| Fluorescent Tags | Molecular Probe | MitoDsRed, MitoTracker Green [20] | Visualize and track mitochondrial transfer and dynamics in co-culture experiments. |
| Antibodies for IHC | Research Antibodies | Anti-CD8, Anti-Ki-67, Anti-CD31, TUNEL assay kit [24] | Ex vivo validation of immune cell infiltration, proliferation, angiogenesis, and apoptosis. |
| MRI Contrast Agent | Imaging Reagent | Gadobutrol (Gadovist) [24] | Contrast agent for DCE-MRI to assess tumor perfusion and vascular permeability. |
The tumor microenvironment is a formidable barrier to effective anti-tumor immunity, employing a diverse and synergistic arsenal of cellular, molecular, and metabolic strategies to suppress and evade immune attack. From the well-established roles of stromal cells and immune checkpoints to the emerging paradigm of mitochondrial transfer, understanding these mechanisms is critical for advancing cancer immunotherapy. The integration of advanced techniques, such as multiparametric MRI and single-cell sequencing, provides researchers with the tools to dissect this complexity quantitatively. Overcoming the immunosuppressive TME will require innovative multi-targeted approaches that simultaneously disrupt these interconnected pathways. The insights and methodologies detailed in this whitepaper provide a foundation for the development of next-generation immunotherapies aimed at reprogramming the TME from a barrier into a facilitator of durable anti-tumor immunity.
While T-cells, particularly CD8+ cytotoxic T-cells, have dominated the cancer immunotherapy landscape, the immune system deploys a broader arsenal of effector cells capable of recognizing and eliminating malignant cells. Innate immune cells—including Natural Killer (NK) cells, macrophages, and dendritic cells (DCs)—are pivotal regulators of antitumor immunity, serving as both direct cytotoxic effectors and crucial orchestrators of adaptive immune responses. Within the complex ecosystem of the tumor microenvironment (TME), these cells exhibit remarkable functional plasticity, dynamically shifting between states that either suppress or promote tumor growth based on contextual signals. Understanding their molecular mechanisms, functional states, and therapeutic potential is essential for developing next-generation immunotherapies that extend beyond current T-cell-centric approaches. This review synthesizes current knowledge on NK cells, macrophages, and DCs in antitumor immunity, framing their roles within the broader mechanisms of antitumor activity and toxicity in immunotherapy research.
Natural Killer Cells: Innate Sentinels of Tumor Surveillance
Biological Characteristics and Cytotoxic Mechanisms
Natural Killer cells are innate lymphoid cells characterized by their capacity to recognize and eliminate virally infected and malignantly transformed cells without prior sensitization, functioning independently of major histocompatibility complex (MHC) restrictions [25]. Human NK cells are broadly classified into two primary subsets based on CD56 expression density: the CD56dim population, which predominates in peripheral blood and mediates potent cytotoxicity, and the CD56bright subset, which excels at cytokine production and immunoregulation [25]. NK cell activation is governed by a delicate balance between activating and inhibitory signals received through an array of surface receptors [26] [25].
Table: NK Cell Receptors and Their Functions
| Receptor Category | Example Receptors | Ligands | Primary Functions |
|---|---|---|---|
| Activating Receptors | NKG2D, NKp30, NKp44, NKp46, CD16 | Stress-induced ligands (e.g., MICA/B), viral proteins, antibody Fc regions | Recognize altered self-cells; mediate direct killing and antibody-dependent cellular cytotoxicity (ADCC) |
| Inhibitory Receptors | KIR2DL, KIR3DL, NKG2A, PD-1, TIGIT | MHC class I molecules, PD-L1, CD155 | Prevent autoimmunity by sensing "self"; often dysregulated in TME leading to NK cell dysfunction |
NK cells employ four principal mechanisms to eliminate tumor cells [25]:
- Perforin/Granzyme Pathway: Upon activation, NK cells release perforin, which forms pores in the target cell membrane, facilitating the entry of granzyme proteases that initiate apoptosis.
- Death Receptor Pathway: Expression of FAS ligand (FASL) or TNF-related apoptosis-inducing ligand (TRAIL) engages corresponding death receptors on target cells, triggering caspase-mediated apoptosis.
- Antibody-Dependent Cellular Cytotoxicity (ADCC): The CD16 (FcγRIIIa) receptor binds to the Fc portion of antibodies coating tumor cells, leading to targeted NK cell activation and killing.
- Cytokine Secretion: NK cells produce inflammatory cytokines such as IFN-γ and TNF-α, which exert direct antitumor effects and enhance adaptive immune responses.
Figure 1: Multifaceted cytotoxic mechanisms employed by NK cells against tumor targets.
NK Cell Dysfunction in the Tumor Microenvironment
Within the immunosuppressive TME, NK cells frequently exhibit functional impairment through multiple mechanisms [26]. Metabolic competition from rapidly proliferating tumor cells leads to nutrient deprivation, while inhibitory metabolites like adenosine accumulate. The TME drives metabolic reprogramming and epigenetic silencing of key NK cell effector genes, further dampening cytotoxicity [26]. Additionally, tumor cells often upregulate ligands for inhibitory receptors (e.g., PD-L1 binding to PD-1) while downregulating activating receptor ligands, tilting the balance toward inhibition [25]. These suppressive mechanisms collectively undermine NK cell surveillance and facilitate immune evasion.
NK Cell-Based Immunotherapy: Clinical Applications and Protocols
Several innovative approaches are being developed to harness NK cells for cancer therapy:
Adoptive NK Cell Transfer: This involves infusing ex vivo expanded and activated allogeneic NK cells. Clinical trials in acute myeloid leukemia (AML) have demonstrated complete response rates of 45-58% with haploidentical NK cells [25]. A standard protocol involves isolating NK cells from donor peripheral blood mononuclear cells (PBMCs) using immunomagnetic selection (e.g., CD56+), followed by 14-day ex vivo expansion with cytokines (IL-2, IL-15), and infusion into preconditioned patients.
Chimeric Antigen Receptor NK (CAR-NK) Cells: CAR-NK cells are engineered to express synthetic receptors targeting tumor-associated antigens. In a landmark trial (NCT03056339), CD19-targeting CAR-NK cells achieved a 73% objective response rate in B-cell malignancies without inducing severe cytokine release syndrome [25]. The manufacturing process typically involves lentiviral/retroviral transduction or electroporation of NK cells with CAR constructs, followed by expansion and validation of cytotoxicity.
NK Cell Engagers and Checkpoint Blockade: Bispecific engager antibodies simultaneously bind NK cell activating receptors (e.g., CD16) and tumor antigens, redirecting NK cell cytotoxicity. Combination therapy with anti-PD-1/PD-L1 antibodies reverses NK cell exhaustion and has shown synergistic efficacy in solid tumors including non-small cell lung cancer (NSCLC) and ovarian cancer [25].
Table: Clinical Outcomes of Selected NK Cell Immunotherapies
| Therapy Modality | Clinical Context | Efficacy Outcomes | Safety Profile |
|---|---|---|---|
| Haploidentical NK Cell Transfer | Relapsed/Refractory AML | 45-58% Complete Response (CR) | No graft-versus-host disease (GVHD) ≥ grade 3; manageable cytokine release syndrome (CRS) |
| CD19-CAR-NK Cells | B-cell Malignancies | 73% Objective Response Rate (ORR) | No CRS ≥ grade 3; minimal neurotoxicity |
| Cytokine-Induced Memory-like NK | Advanced AML | 50% CR in phase I trial | Transient cytopenias; no dose-limiting toxicities |
| Anti-PD-1 + NK Cell Infusion | NSCLC, Ovarian Cancer | Enhanced ORR vs. monotherapy | Well-tolerated; immune-related adverse events comparable to anti-PD-1 alone |
Tumor-Associated Macrophages: Dual Roles in Tumor Immunity
Macrophage Polarization States and Functions
Macrophages exhibit exceptional plasticity, dynamically shifting their functional phenotypes in response to local signals within the TME. The traditional classification distinguishes between M1 (pro-inflammatory, antitumor) and M2 (immunoregulatory, protumor) polarization states, though this represents a simplified spectrum rather than a fixed binary [27] [28].
M1 Macrophages: Classically activated by interferon-γ (IFN-γ) and microbial products like lipopolysaccharide (LPS), M1 macrophages express high levels of pro-inflammatory cytokines (IL-12, TNF-α), inducible nitric oxide synthase (iNOS), and major histocompatibility complex (MHC) class II molecules [28]. They mediate direct tumor cell cytotoxicity through reactive oxygen species and nitric oxide production, while also promoting Th1-type adaptive immune responses.
M2 Macrophages: Alternatively activated by IL-4, IL-13, IL-10, and transforming growth factor-beta (TGF-β), M2 macrophages upregulate scavenger receptors (CD206, CD163), produce anti-inflammatory cytokines (IL-10, TGF-β), and secrete pro-angiogenic factors like vascular endothelial growth factor (VEGF) [27]. They facilitate tumor progression through multiple mechanisms: suppressing T and NK cell function, promoting angiogenesis, enhancing tissue remodeling and metastasis, and contributing to an immunosuppressive TME.
Figure 2: Macrophage polarization states in the tumor microenvironment.
Protumor Functions and Immune Suppression
Tumor-associated macrophages (TAMs) predominantly exhibit an M2-like phenotype and contribute to multiple hallmarks of cancer progression [27]. They secrete matrix metalloproteinases (MMPs) and other proteases that remodel the extracellular matrix, facilitating tumor invasion and metastasis. Through VEGF and other angiogenic factors, TAMs promote the formation of new blood vessels to support tumor growth. Additionally, M2 TAMs suppress antitumor immunity through multiple mechanisms: expression of immune checkpoint ligands (PD-L1), secretion of immunosuppressive cytokines (IL-10, TGF-β), recruitment of regulatory T cells (Tregs) via CCL22, and metabolic disruption through arginase-1-mediated depletion of L-arginine required for T cell function [27].
Therapeutic Targeting of TAMs
Current therapeutic strategies targeting TAMs focus on three main approaches [27]:
Depletion Strategies: CSF-1R inhibitors (e.g., pexidartinib) block the colony-stimulating factor-1 receptor signaling essential for TAM survival and differentiation, reducing TAM infiltration in tumors. CCL2 inhibitors interfere with monocyte recruitment to tumors.
Repolarization Approaches: Nanoparticle-based delivery systems can be used to load M1-polarizing agents (TLR agonists, IFN-γ, or CD40 agonists) that reprogram M2 TAMs toward an M1 phenotype with antitumor capabilities.
Phagocytosis Enhancement: CD47-blocking antibodies disrupt the "don't eat me" signal employed by tumor cells, thereby enhancing macrophage-mediated phagocytosis of tumors. Clinical protocols typically involve combination therapy with tumor-opsonizing antibodies.
Table: Key Research Reagents for Macrophage Studies
| Research Reagent | Category | Primary Function | Experimental Applications |
|---|---|---|---|
| Recombinant CSF-1 | Cytokine | Promotes macrophage survival, proliferation, and differentiation | In vitro generation of bone marrow-derived macrophages; M2 polarization studies |
| Pexidartinib (PLX3397) | Small Molecule Inhibitor | Selective CSF-1R tyrosine kinase inhibitor | In vivo TAM depletion; combination therapy with chemotherapy/checkpoint inhibitors |
| Recombinant IL-4/IL-13 | Cytokines | Induce alternative M2 macrophage activation | In vitro M2 polarization models; study of protumor macrophage functions |
| Lipopolysaccharide (LPS) | TLR4 Agonist | Induces classical M1 macrophage activation | In vitro M1 polarization; study of proinflammatory macrophage responses |
| Anti-CD206 Antibody | Immunological Reagent | Binds mannose receptor (M2 marker) | Flow cytometry identification of M2 macrophages; immunohistochemistry for TAM quantification |
| Recombinant IFN-γ | Cytokine | Drives classical M1 macrophage activation | In vitro M1 polarization; macrophage-mediated tumor cell killing assays |
Dendritic Cells: Orchestrators of Antitumor Immunity
DC Subsets and Specialized Functions
Dendritic cells are professional antigen-presenting cells that bridge innate and adaptive immunity by capturing, processing, and presenting tumor antigens to T cells. The DC compartment comprises several functionally distinct subsets [29]:
Conventional DCs (cDCs): cDCs are specialized in antigen presentation and can be divided into two main subsets:
- cDC1s are defined by expression of CD141 (BDCA-3) in humans and XCR1, and depend on the transcription factor BATF3 for development. They excel at cross-presenting exogenous antigens on MHC class I to CD8+ T cells, making them essential for initiating antitumor cytotoxic T lymphocyte (CTL) responses [29] [30].
- cDC2s express CD1c (BDCA-1) in humans and specialize in presenting antigens to CD4+ T cells via MHC class II, shaping helper T cell responses through Th1, Th2, or Th17 polarization [29].
Plasmacytoid DCs (pDCs): pDCs are characterized by high CD123 expression and specialize in producing massive amounts of type I interferons (IFN-α/β) in response to viral infections. Their role in cancer is complex, as they can either promote antitumor immunity or support immunosuppression through Treg expansion in different contexts [29].
Monocyte-Derived DCs (moDCs): moDCs are generated from circulating monocytes under inflammatory conditions and have been widely utilized in clinical DC vaccination protocols due to their accessibility and expandability ex vivo [29].
DC Dysfunction and Therapeutic Engineering
In the TME, DCs often exhibit functional impairment through multiple mechanisms, including reduced antigen uptake and presentation, altered maturation, and increased expression of immunosuppressive molecules like PD-L1 and IL-10 [29]. These dysfunctional states limit their ability to initiate effective antitumor T cell responses. To overcome these limitations, several engineering strategies are being developed:
Genetic Engineering: DC progenitors (DCPs) can be engineered to express immunostimulatory cytokines (e.g., IL-12) and specialized receptors that enhance tumor antigen uptake [30]. A recent innovative approach involves engineering DCPs to express extracellular vesicle-internalizing receptors (EVIRs) that bind to "bait" molecules (e.g., GD2 disialoganglioside) on cancer cells, forcing internalization of tumor-derived EVs and promoting cross-dressing with preformed MHC-peptide complexes [30].
Ex Vivo DC Vaccines: The established protocol involves isolating monocytes from patient blood via leukapheresis, differentiating them to moDCs with GM-CSF and IL-4 over 5-7 days, loading with tumor antigens (peptides, tumor lysates, or mRNA), and maturing with cytokine cocktails (TNF-α, IL-1β, IL-6, PGE2) or TLR agonists before reinfusion [29].
Figure 3: Standardized workflow for manufacturing ex vivo dendritic cell vaccines.
Clinical Applications and Combination Strategies
DC-based immunotherapies have demonstrated clinical safety and immunogenicity across multiple cancer types. Sipuleucel-T, the first FDA-approved DC vaccine for metastatic castration-resistant prostate cancer, demonstrated improved overall survival, establishing the clinical feasibility of this approach [29]. Current research focuses on enhancing efficacy through combination strategies with immune checkpoint inhibitors (anti-PD-1/PD-L1), personalized neoantigen targeting, and in vivo DC targeting approaches that bypass complex ex vivo manufacturing [29]. Biomaterials-based delivery systems and artificial intelligence-driven epitope prediction are emerging technologies that promise to further improve DC vaccine efficacy [29].
Cross-Talk and Integrated Immune Responses
The antitumor immune response depends on sophisticated communication between innate and adaptive immune cells. DCs serve as critical integrators by capturing tumor antigens and presenting them to naïve T cells in lymph nodes, initiating antigen-specific responses [29]. NK cells contribute to this network by producing IFN-γ that enhances DC maturation and promotes Th1 differentiation, while also eliminating immunosuppressive cells and poorly immunogenic tumor variants [26] [25]. Activated T cells reciprocally enhance NK cell function through cytokine secretion and CD40L-CD40 interactions. Conversely, M2-polarized TAMs disrupt this productive cross-talk by secreting IL-10 and TGF-β that inhibit DC maturation and T cell priming, while also expressing PD-L1 that directly suppresses T and NK cell activity [27]. This complex cellular network highlights the importance of therapeutic strategies that simultaneously target multiple immune components to overcome immunosuppression and establish durable antitumor immunity.
NK cells, macrophages, and dendritic cells represent powerful effector populations whose therapeutic potential extends beyond current T-cell-centric approaches. Each cell type contributes unique mechanisms for tumor recognition and elimination, while their functional plasticity within the TME presents both challenges and opportunities for therapeutic intervention. Future progress will require strategies that overcome immunosuppressive mechanisms while enhancing the natural antitumor capabilities of these innate immune effectors. Promising directions include advanced cell engineering approaches (CAR-NK, EVIR-DC), targeted repolarization therapies (M2-to-M1 macrophage switching), and rational combination regimens that simultaneously engage multiple arms of the immune system. As our understanding of the complex interactions within the TME deepens, therapies harnessing the full spectrum of innate and adaptive immunity will likely yield more effective and durable responses against cancer.
The gut microbiome, a complex ecosystem of bacteria, fungi, viruses, and archaea, has emerged as a critical regulator of systemic immunity and a powerful modulator of cancer immunotherapy efficacy [31] [32]. Immune checkpoint inhibitors (ICIs), which block inhibitory pathways such as PD-1, PD-L1, and CTLA-4 to unleash antitumor immunity, have revolutionized oncology [33] [34]. However, only 20-40% of patients derive durable benefit, creating an urgent need to understand the factors driving treatment resistance [31] [35]. Accumulating clinical and preclinical evidence demonstrates that the composition and functional output of the gut microbiome significantly influence patient responses to ICIs and the incidence of immune-related adverse events (irAEs) [31] [36]. This review synthesizes current knowledge on the microbial species, metabolites, and mechanisms underlying this relationship, providing a technical guide for researchers and drug development professionals focused on optimizing cancer immunotherapy.
The Gut Microbiome as a Determinant of Immunotherapy Outcome
Clinical Evidence Linking Microbiome to ICI Response
The impact of the gut microbiome on ICI efficacy is observed across multiple cancer types. Clinical studies consistently show that patients responding to ICIs exhibit distinct gut microbial communities compared to non-responders [36]. A meta-analysis of 71 studies confirmed that baseline microbiota composition significantly associates with ICI efficacy, with a pooled relative risk of 1.29 for objective response rate [35]. Greater gut microbial diversity consistently correlates with improved progression-free survival (PFS) and overall survival (OS) across melanoma, non-small cell lung cancer (NSCLC), and renal cell carcinoma (RCC) [31] [32].
Table 1: Microbial Taxa Associated with Improved ICI Response Across Cancers
| Cancer Type | Associated Microbial Taxa | ICI Type | Clinical Outcome |
|---|---|---|---|
| Melanoma | Faecalibacterium prausnitzii, Bifidobacterium longum, Collinsella aerofaciens, Enterococcus faecium [31] [36] | Anti-PD-1 | Improved response [31] |
| NSCLC | Akkermansia muciniphila, Alistipes spp., Ruminococcus spp., Eubacterium spp. [31] [36] | Anti-PD-1 | Improved PFS/OS [31] |
| RCC | Akkermansia muciniphila [31] | Anti-PD-1 | Improved response [31] |
| Hepatobiliary | Alistipes [37] | Anti-PD-1/PD-L1 | Positively correlated with survival [37] |
| Multiple Cancers | Ruminococcaceae, Lachnospiraceae [31] | Anti-PD-1/CTLA-4 | Improved response [31] |
Conversely, specific microbial patterns are associated with resistance to immunotherapy. In biliary tract cancer, increased abundance of Bacilli, Lactobacillales, and the metabolite Pyrrolidine correlates with poorer survival outcomes [37]. Importantly, antibiotic exposure within 30 days of ICI initiation consistently impairs therapeutic responses across tumor types, highlighting the functional role of an intact microbial community [31] [32].
Microbiome Influence on Adoptive Cell Therapies
The gut microbiome also modulates the efficacy of adoptive cell therapies (ACTs). Early studies demonstrated that broad-spectrum antibiotics like ciprofloxacin reduce ACT effectiveness in mice, an effect reversible by bacterial lipopolysaccharide supplementation that activates Toll-like receptor 4 pathways [31]. This suggests microbial components can directly stimulate innate immunity to enhance T-cell activity. While clinical data on microbiome-ACT interactions are less extensive than for ICIs, emerging evidence indicates that gut microbial composition influences chimeric antigen receptor T-cell (CAR-T) therapy and other ACT outcomes [31].
Mechanisms of Microbiome-Mediated Immunomodulation
Microbial Metabolites as Key Immunomodulators
Microbiota-derived metabolites serve as crucial messengers between gut microbes and the host immune system, influencing anti-tumor immunity through multiple mechanisms.
Table 2: Key Microbiota-Derived Metabolites and Their Immunomodulatory Effects
| Metabolite Class | Representative Metabolites | Proposed Mechanisms in Immunotherapy | Impact on ICIs |
|---|---|---|---|
| Short-chain fatty acids (SCFAs) | Butyrate, Propionate, Acetate | Promote regulatory T-cell development; modulate dendritic cell activity; enhance CD8+ T-cell function [32] [38] | Context-dependent: Generally associated with improved response [32] |
| Bile acids | Secondary bile acids (deoxycholic acid, lithocholic acid) | Modulate Th1 and T-cell differentiation; enhance CD8+ T-cell function [31] [38] | Improved anti-tumor immunity [38] |
| Tryptophan derivatives | Indole-3-carbaldehyde, Kynurenine | Aryl hydrocarbon receptor activation; regulate immune cell function [34] [38] | Modulation of T-cell activity [38] |
| Inosine | - | Enhancement of T-cell activation and costimulation [32] | Improved anti-tumor response [32] |
| Polyamines | Spermidine, Spermine | Modulation of T-cell differentiation and function [38] | Under investigation [38] |
The immunomodulatory effects of these metabolites occur through several interconnected mechanisms: (1) direct interaction with immune cell receptors, (2) epigenetic modification of immune-related genes, and (3) alteration of cellular metabolism in both tumor and immune cells [38]. The net effect on immunotherapy outcomes depends on metabolite concentration, timing of exposure, and the local immune context.
Integrated Mechanisms of Microbiome-Mediated Antitumor Immunity
The gut microbiome influences multiple steps in the cancer-immunity cycle through diverse but interconnected mechanisms [39]. These include direct microbial stimulation of immune cells via pattern recognition receptors, metabolite-mediated epigenetic and functional reprogramming of immune cells, and molecular mimicry between microbial and tumor antigens that enhances T-cell cross-reactivity [31] [35]. The following diagram illustrates the key mechanisms through which the gut microbiome and its metabolites systemically influence antitumor immunity and response to immunotherapy.
Experimental Approaches for Microbiome-Immunotherapy Research
Standardized Workflow for Microbiome Analysis
Investigating the microbiome-ICI response relationship requires a structured pipeline from sample collection to data integration. The following workflow outlines key steps for robust microbiome analysis in immunotherapy studies.
Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for Microbiome-Immunotherapy Studies
| Category | Reagent/Method | Specific Application | Technical Considerations |
|---|---|---|---|
| Sample Collection & Preservation | Fecal collection kits with preservation buffers | Maintain microbial integrity at -80°C [39] | Immediate cryopreservation critical; standardized protocols reduce variability |
| DNA Extraction | Feces Genomic DNA Purification Kit | Metagenomic DNA extraction for sequencing [37] | Kit selection affects DNA yield and quality; mechanical lysis improves Gram-positive bacteria recovery |
| Sequencing Methods | 16S rRNA gene sequencing (V3-V4 region) | Cost-effective bacterial community profiling [39] | Limited to genus-level resolution; prone to compositionality bias |
| Shotgun metagenomic sequencing | Species/strain-level resolution; functional gene analysis [36] | Higher cost; requires more computational resources; reduces compositionality bias | |
| Metabolite Profiling | LC-MS/MS (Liquid Chromatography-Mass Spectrometry) | Quantification of SCFAs, bile acids, tryptophan derivatives [37] | Requires metabolite extraction; use of internal standards for quantification |
| Computational Tools | MetaPhlAn, HUMAnN | Taxonomic and functional profiling from metagenomic data [37] | Database-dependent; requires appropriate normalization |
| LEfSe (Linear Discriminant Analysis Effect Size) | Identify differentially abundant taxa between groups [37] | Identifies biomarkers with statistical and biological significance | |
| In Vivo Models | Germ-free (GF) mice | Establish causal relationships via FMT from patients [36] | Transfer patient response phenotypes to mice |
| Antibiotic-treated mice | Deplete microbiota to assess necessity in ICI response [36] | Timing and antibiotic spectrum critical for experimental design |
Methodological Considerations for Robust Results
Microbiome research faces reproducibility challenges that require careful methodological planning. Key considerations include:
- Absolute vs. Relative Quantification: Standard sequencing provides relative abundance data, which is compositionally constrained. Integrating quantitative PCR (qPCR), flow cytometry, or synthetic spike-in standards enables absolute quantification, providing more biologically accurate measurements [39].
- Longitudinal Sampling: Single timepoints may miss dynamic microbial changes. Collection before, during, and after ICI treatment captures temporal relationships between microbiome shifts and clinical outcomes [37].
- Multi-omics Integration: Combining metagenomics, metabolomics, and host immune profiling provides mechanistic insights beyond taxonomic associations [38] [37].
- Confounding Factors: Antibiotic use, proton pump inhibitors, diet, and invasive biliary procedures significantly alter gut microbiota and must be documented and controlled in analyses [37].
Microbiome-Targeted Therapeutic Strategies
Intervention Modalities and Clinical Evidence
Several microbiome-targeted approaches have shown promise in enhancing ICI efficacy or overcoming resistance:
Fecal Microbiota Transplantation (FMT): Transfer of processed stool from ICI responders to refractory patients can restore sensitivity to immunotherapy. In metastatic melanoma, FMT from responders combined with anti-PD-1 therapy achieved objective response rates of 20-40% in previously resistant patients [31] [32]. Phase I trials demonstrate that FMT is generally safe and can promote favorable immune changes in the tumor microenvironment, including increased CD8+ T-cell infiltration and decreased myeloid suppressor cells [31] [36].
Probiotics and Live Biotherapeutic Products: Defined bacterial consortia are being developed as pharmaceutical products. Preclinical models show that specific strains, including Bifidobacterium spp., Akkermansia muciniphila, and Faecalibacterium prausnitzii, enhance ICI efficacy [34] [36]. However, commercial probiotics have yielded mixed results in clinical studies, with some even correlating with poorer outcomes, highlighting the need for carefully selected, evidence-based formulations [32].
Dietary Interventions: Diet profoundly shapes gut microbiota composition and function. High-fiber diets increase SCFA-producing bacteria and are associated with improved ICI responses in melanoma and NSCLC patients [32]. Pilot studies of plant-forward or medically-designed diets demonstrate these interventions can modulate microbial communities and enhance CD8+ T-cell infiltration in tumors [32] [40].
Prebiotics and Postbiotics: Prebiotics (substances that selectively promote beneficial bacteria) and postbiotics (purified microbial metabolites) offer alternative modulation strategies. These approaches bypass the challenges of live bacteria engraftment and provide more controlled intervention [38].
Clinical Translation Considerations
Advancing microbiome-based interventions into clinical practice requires addressing several challenges:
- Standardization: Developing reproducible manufacturing protocols for FMT and live biotherapeutic products is essential for consistent clinical outcomes [39].
- Personalization: Microbiome composition varies significantly between individuals, suggesting that effective interventions may need tailoring to baseline microbiota [34].
- Trial Design: Future studies should incorporate larger sample sizes, standardized endpoints, and control for confounding medications like antibiotics and proton pump inhibitors [35] [32].
- Mechanistic Understanding: Deeper insights into how specific bacteria and metabolites influence immune pathways will enable more targeted therapeutic development [38] [36].
The gut microbiome represents a master regulator of systemic immunity that significantly influences response to cancer immunotherapy. Specific microbial communities and their metabolic outputs enhance antitumor immunity through multiple interconnected mechanisms, including immune cell activation, checkpoint regulation, and tumor microenvironment modification. Standardized experimental approaches and multi-omics integration are advancing our understanding of these complex interactions. While microbiome-based therapeutics like FMT and targeted probiotics show promising clinical potential, overcoming methodological challenges and developing personalized approaches will be crucial for successful clinical translation. As research in this field progresses, modulating the gut microbiome presents a promising strategy for expanding the efficacy of cancer immunotherapy to more patients.
Therapeutic Arsenal: Mechanisms of Action Across Immunotherapy Classes
The advent of immune checkpoint inhibitors (ICIs) has fundamentally reshaped the landscape of cancer therapy, representing a paradigm shift from directly targeting tumor cells to harnessing the power of the host immune system. Immune checkpoints are regulatory pathways that maintain self-tolerance and prevent excessive immune activation, but tumors exploit these mechanisms to evade immune surveillance [41]. Monoclonal antibodies targeting cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), programmed death 1 (PD-1), and its ligand PD-L1 have demonstrated remarkable clinical efficacy across numerous malignancies, providing durable responses in subsets of patients with advanced cancers that were previously considered intractable [9] [42]. This whitepaper examines the mechanisms of antitumor activity and toxicity of ICIs targeting CTLA-4, PD-1, and PD-L1, providing a comprehensive technical resource for researchers and drug development professionals working in cancer immunotherapy.
Biological Foundations of Immune Checkpoints
The Cancer-Immunity Cycle and Checkpoint Regulation
The immune-mediated destruction of cancer cells follows a coordinated sequence of events termed the "Cancer-Immunity Cycle" [11]. This process begins with neoantigen release by tumor cells and capture by dendritic cells (DCs), which then present tumor antigens to T cells in lymphoid organs. Subsequently, primed T cells traffic to tumor sites, infiltrate the tumor microenvironment (TME), and specifically recognize and kill cancer cells [11]. The cycle perpetuates as dying tumor cells release additional antigens, broadening the immune response. However, tumors disrupt this cycle at multiple points, particularly by co-opting inhibitory checkpoint pathways including CTLA-4 and PD-1 [11].
Distinct Roles of CTLA-4 and PD-1/PD-L1 Pathways
CTLA-4 functions primarily during the early phase of T cell activation in lymphoid organs [9] [43]. Expressed on activated T cells and constitutively on regulatory T cells (Tregs), CTLA-4 competitively inhibits the costimulatory receptor CD28 by binding with higher affinity to shared ligands B7-1 (CD80) and B7-2 (CD86) on antigen-presenting cells (APCs) [9] [41]. This competition attenuates T cell priming and reduces the amplitude of initial T cell activation. Additionally, CTLA-4 engagement on Tregs enhances their immunosuppressive activity, further dampening anti-tumor immunity [9].
PD-1 operates predominantly during the effector phase in peripheral tissues and the TME [9] [43]. Following chronic antigen exposure, PD-1 is upregulated on T cells and engages with its ligands PD-L1 and PD-L2, which are expressed on tumor cells, stromal cells, and immune cells [41]. This interaction recruits phosphatases SHP-1 and SHP-2, which dephosphorylate key signaling molecules in the TCR and CD28 pathways, leading to inhibited T cell proliferation, reduced cytokine production, and diminished cytolytic function [44]. The PD-1/PD-L1 axis represents a primary mechanism of adaptive immune resistance, wherein tumors upregulate PD-L1 in response to inflammatory signals like IFN-γ to evade immune attack [41].
Table 1: Comparative Biology of Key Immune Checkpoints
| Feature | CTLA-4 | PD-1 |
|---|---|---|
| Primary function | Regulates early T-cell activation in lymphoid organs | Suppresses T-cell activity in peripheral tissues and tumors |
| Expression pattern | Activated T cells, Tregs | Activated T cells, B cells, NK cells, myeloid cells |
| Ligands | B7-1 (CD80), B7-2 (CD86) | PD-L1 (B7-H1), PD-L2 (B7-DC) |
| Mechanism of inhibition | Competes with CD28 for B7 ligands; transendocytosis of B7; enhances Treg suppression | Recruits SHP-1/SHP-2 phosphatases; inhibits TCR and CD28 signaling |
| Phase of immune response | Priming phase | Effector phase |
| Mouse knockout phenotype | Lethal lymphoproliferation early in life [45] | Strain-specific autoimmunity [45] |
Mechanisms of Antitumor Activity
Monotherapy Mechanisms
CTLA-4 blockade with inhibitors such as ipilimumab primarily enhances the priming and expansion of tumor-reactive T cells in lymphoid organs [43]. By preventing CTLA-4 from engaging with B7 ligands, these inhibitors shift the balance toward productive costimulation through CD28, leading to increased T cell activation, proliferation, and diversification of the T cell repertoire [9]. Additionally, CTLA-4 blockade can reduce Treg-mediated suppression through Fc receptor-dependent depletion of intratumoral Tregs or interference with their suppressive function [11].
PD-1/PD-L1 blockade focuses on reversing T cell exhaustion within the TME [43]. Antibodies targeting PD-1 (e.g., nivolumab, pembrolizumab) or PD-L1 (e.g., atezolizumab, durvalumab) disrupt the inhibitory PD-1/PD-L1 interaction, thereby restoring TCR signaling and revitalizing the effector functions of tumor-infiltrating lymphocytes (TILs) [41]. This leads to enhanced cytokine production (IFN-γ, TNF-α, IL-2), increased T cell proliferation, and improved cytolytic activity against tumor cells [9].
Synergistic Mechanisms of Combination Therapy
Dual blockade of CTLA-4 and PD-1/PD-L1 generates synergistic antitumor activity that exceeds the additive effects of each monotherapy [11]. This synergy arises from complementary actions on distinct phases of the immune response: CTLA-4 inhibition expands the repertoire and number of tumor-reactive T cells during priming, while PD-1/PD-L1 inhibition reverses the functional exhaustion of these T cells within the TME [11] [44]. Preclinical models demonstrate that combination therapy significantly decreases the proportion of exhausted phenotype cytotoxic T cells and enhances tumor infiltration by effector T cells [11]. Additionally, combination therapy promotes the formation of immune memory, contributing to durable, long-term antitumor responses [11].
Diagram 1: CTLA-4 and PD-1/PD-L1 inhibitory pathways and mechanism of checkpoint blockade. CTLA-4 regulates early T cell activation in lymph nodes, while PD-1 suppresses T cell function in peripheral tissues. Checkpoint inhibitors block these interactions to restore anti-tumor immunity [9] [43].
Mechanisms of Toxicity
Immune-Related Adverse Events (irAEs)
The same mechanisms that underpin the antitumor efficacy of ICIs also contribute to a spectrum of inflammatory toxicities known as immune-related adverse events (irAEs) [45]. These toxicities result from the breaking of peripheral tolerance and unleashed immune responses against healthy tissues [45]. irAEs can affect nearly any organ system, with varying frequency and severity depending on the specific checkpoint target.
CTLA-4 inhibition is associated with more frequent and severe toxicities compared to PD-1/PD-L1 blockade [45]. The most common severe irAEs from CTLA-4 blockade include colitis (occurring in 10-15% of patients) and hypophysitis (6% of patients) [45]. The heightened toxicity profile of anti-CTLA-4 therapy likely stems from its fundamental role in dampening early T cell activation broadly, potentially enabling autoreactive T cell clones that would normally be suppressed.
PD-1/PD-L1 inhibition demonstrates a different toxicity profile, with higher incidence of pneumonitis, thyroiditis (8% of patients), and autoimmune diabetes compared to CTLA-4 blockade [45]. The more restricted toxicity spectrum may reflect the more tissue-specific role of the PD-1 pathway in maintaining peripheral tolerance.
Combination therapy with both CTLA-4 and PD-1/PD-L1 inhibitors increases the incidence and severity of irAEs, with toxicity that appears additive rather than synergistic [45] [44]. This enhanced toxicity underscores the non-redundant functions of these checkpoints in maintaining immune homeostasis.
Table 2: Comparative Toxicity Profiles of Immune Checkpoint Inhibitors
| Organ System | CTLA-4 Inhibitors | PD-1/PD-L1 Inhibitors | Combination Therapy |
|---|---|---|---|
| Gastrointestinal | Colitis (40%, severe 10-15%) [45] | Colitis (20%, severe 2-5%) [45] | Increased frequency and severity [44] |
| Endocrine | Hypophysitis (6%) [45] | Thyroiditis (8%) [45] | Higher endocrine dysfunction |
| Dermatologic | Common, usually mild [45] | Common, usually mild [45] | Enhanced skin toxicity |
| Hepatic | Hepatitis | Hepatitis | Increased transaminitis |
| Pulmonary | Less common | Pneumonitis | Higher pneumonitis risk |
| Other | - | Autoimmune diabetes, rare | More frequent irAEs |
Proposed Mechanisms of irAE Development
The precise mechanisms driving irAEs remain incompletely understood but several hypotheses have emerged:
- Breaking peripheral tolerance: Checkpoint inhibitors may unleash pre-existing autoreactive T cell clones that were previously restrained by CTLA-4 and PD-1 pathways [45].
- Microbiome influence: The predominance of gastrointestinal toxicity suggests that commensal microbiota may provide antigens that cross-react with host tissues or directly stimulate inflammatory responses in the context of checkpoint blockade [45].
- Tissue-specific inflammation: Endocrine toxicities may reflect the unique self-antigens expressed in specialized tissues like thyroid, pituitary, and pancreatic islets that become targets of dysregulated immunity [45].
- Cytokine-mediated damage: Enhanced T cell activation leads to increased cytokine production (e.g., IFN-γ, TNF-α, IL-6), which can directly mediate tissue inflammation and damage [45].
Clinical Applications and Efficacy Data
Approved Agents and Indications
The FDA has approved multiple ICIs targeting CTLA-4, PD-1, and PD-L1 for various cancers [44]. Ipilimumab (anti-CTLA-4) was first approved for advanced melanoma in 2011 [41]. Since then, numerous PD-1 inhibitors (nivolumab, pembrolizumab, cemiplimab, dostarlimab, toripalimab) and PD-L1 inhibitors (atezolizumab, avelumab, durvalumab) have received approval across multiple tumor types [41] [44].
Combination Therapy Efficacy
Dual checkpoint blockade has demonstrated superior efficacy over monotherapy in several malignancies:
Melanoma: The CheckMate 067 phase 3 trial established the combination of nivolumab (anti-PD-1) and ipilimumab (anti-CTLA-4) as a standard for advanced melanoma, with significantly improved median progression-free survival (11.5 months) and objective response rate (57.6%) compared to either agent alone [44]. After 6.5 years of follow-up, the combination continued to show superior progression-free and overall survival compared to monotherapy [44].
Non-Small Cell Lung Cancer (NSCLC): Combination therapy has shown improved outcomes in NSCLC, particularly in patients with high tumor mutational burden [11]. The CheckMate 227 trial demonstrated superior overall survival with nivolumab plus ipilimumab versus chemotherapy in patients with PD-L1 expression ≥1% [11].
Other Malignancies: Combination approaches have shown benefit in renal cell carcinoma, hepatocellular carcinoma, colorectal cancer with mismatch repair deficiency, and mesothelioma, leading to FDA approvals in these indications [44].
Table 3: Selected Clinical Efficacy Data for Checkpoint Inhibitors
| Therapy Regimen | Cancer Type | Trial Phase | Efficacy Outcomes | Reference |
|---|---|---|---|---|
| Nivolumab + Ipilimumab | Metastatic Melanoma | Phase 3 | ORR: 57.6%; Median PFS: 11.5 months | [44] |
| Nivolumab + Ipilimumab | NSCLC (PD-L1 ≥1%) | Phase 3 | Improved OS vs chemotherapy | [11] |
| Ipilimumab monotherapy | Metastatic Melanoma | Phase 3 | ORR: 10.9%; Median OS: 10.1 months | [44] |
| Pembrolizumab monotherapy | Metastatic Melanoma | Phase 3 | ORR: 42.9%; Median PFS: 8.4 months | [44] |
| Durvalumab + Tremelimumab | Various cancers | Multiple | Approved in HCC, NSCLC, mesothelioma | [44] |
Resistance Mechanisms
Despite impressive clinical successes, primary and acquired resistance limit the efficacy of ICIs in many patients [41] [43]. Resistance mechanisms can be categorized into tumor-intrinsic, immune cell dysfunction, and microenvironmental factors.
Tumor-Intrinsic Resistance Mechanisms
- Defects in antigen presentation: Loss or downregulation of MHC class I expression through mutations in β2-microglobulin (B2M) or other components of the antigen presentation machinery impairs T cell recognition of tumor cells [43].
- Interferon signaling defects: Mutations in IFNγ pathway components (JAK1/2, STAT1) render tumor cells insensitive to the antiproliferative and immunomodulatory effects of IFNγ signaling [43].
- Oncogenic pathway activation: Activation of oncogenic signaling pathways (e.g., WNT/β-catenin, MAPK, PI3K) can promote an immune-excluded phenotype by reducing T cell infiltration into tumors [43].
- Alternative checkpoint upregulation: Tumors may upregulate alternative immune checkpoints (e.g., TIM-3, LAG-3, TIGIT) that maintain suppression even when PD-1/CTLA-4 are blocked [43].
Immune and Microenvironmental Resistance Mechanisms
- T cell exhaustion: Chronic antigen exposure leads to a state of deep T cell exhaustion characterized by co-expression of multiple inhibitory receptors, metabolic insufficiency, and epigenetic fixation in a hypofunctional state [43].
- Suppressive cellular populations: The accumulation of regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and tumor-associated macrophages (TAMs) in the TME creates an immunosuppressive milieu that counteracts effector T cell function [11] [43].
- Metabolite-mediated suppression: Tumor and stromal cells produce immunosuppressive metabolites (e.g., kynurenine via IDO, adenosine, lactate) that inhibit T cell function and promote Treg differentiation [43].
- Abnormal vasculature: Disorganized tumor vasculature limits T cell infiltration into tumors while expressing adhesion molecules and factors that actively suppress T cell function [43].
Experimental Approaches and Research Methodologies
Preclinical Models
Murine tumor models have been instrumental in elucidating the mechanisms of action of ICIs and identifying rational combinations [11]. Syngeneic mouse models, which involve transplanting tumor cells into immunocompetent mice with matching genetic backgrounds, allow researchers to study antitumor immune responses in the context of an intact immune system [11]. Key methodologies include:
- Tumor volume measurements: Regular caliper measurements to assess growth kinetics and treatment responses.
- Immune monitoring: Flow cytometry analysis of tumor-infiltrating lymphocytes (TILs), splenocytes, and lymph node cells to characterize immune cell populations and activation states.
- Cytokine profiling: Multiplex ELISA or Luminex assays to quantify cytokine production in tumor homogenates or serum.
- Histopathological analysis: Immunohistochemistry and immunofluorescence staining of tumor sections to evaluate immune cell infiltration and spatial distribution.
Genetic knockout models have been crucial for understanding checkpoint biology. CTLA-4 knockout mice develop fatal lymphoproliferation, highlighting its critical role in immune homeostasis, while PD-1 knockout mice develop more strain-specific autoimmunity [45].
Clinical Trial Designs
Novel clinical trial designs have accelerated the development of ICI combinations:
- Phase I dose-escalation trials: Establish safety and recommended Phase 2 doses for combination therapies, with particular attention to irAEs.
- Biomarker-enriched designs: Select patients based on predictive biomarkers (e.g., PD-L1 expression, tumor mutational burden) to enhance response rates.
- Adaptive platform trials: Evaluate multiple therapeutic combinations simultaneously within a single master protocol, allowing for more efficient drug development.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Immune Checkpoint Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Anti-mouse CTLA-4 | Clone 9D9, UC10-4F10-11 | Preclinical testing in syngeneic models | Different clones may have varying functional effects |
| Anti-mouse PD-1 | Clone RMP1-14, J43 | Preclinical efficacy assessment | Can reverse T cell exhaustion in chronic infection models |
| Anti-mouse PD-L1 | Clone 10F.9G2, MIH5 | Mechanism studies | Blocks PD-1/PD-L1 interaction in mouse systems |
| Anti-human PD-1 | Nivolumab, pembrolizumab analogs | In vitro human T cell assays | Used in human PBMC or tumor culture systems |
| Flow cytometry antibodies | Anti-CD3, CD4, CD8, CD279 (PD-1), CD152 (CTLA-4) | Immune phenotyping | Intracellular staining required for CTLA-4 detection |
| Recombinant proteins | PD-1 Fc, PD-L1 Fc, CTLA-4 Fc | Binding assays, plate coating | Used in ELISA, SPR, or receptor-ligand interaction studies |
| Cell lines | MC38, CT26, B16-F10 | Syngeneic tumor models | Different lines have varying sensitivity to checkpoint blockade |
Future Directions
Several emerging approaches aim to enhance the efficacy and safety of ICIs:
- Novel checkpoint targets: Inhibitors targeting LAG-3, TIM-3, TIGIT, and VISTA are in clinical development to address resistance mediated by alternative checkpoints [46] [43].
- Biomarker development: Improved predictive biomarkers (e.g., tumor mutational burden, gene expression signatures, gut microbiome composition) are needed to better identify patients most likely to benefit from ICIs [43].
- Engineering solutions: Bispecific antibodies (e.g., cadonilimab targeting CTLA-4 and PD-1), prodrug strategies, and conditionally active biologics aim to enhance tumor specificity and reduce systemic toxicity [46] [47].
- Rational combinations: Strategic combinations with targeted therapies, chemotherapy, radiotherapy, and other immunomodulators seek to overcome resistance mechanisms and convert "cold" tumors into "hot", immunoresponsive microenvironments [43] [42].
Diagram 2: Multifactorial resistance mechanisms to PD-1/CTLA-4 blockade. Resistance arises from complex interactions between tumor-intrinsic adaptations, immune cell dysfunction, and microenvironmental suppression [43].
Immune checkpoint inhibitors targeting CTLA-4, PD-1, and PD-L1 have revolutionized cancer therapy by harnessing the native immune system against malignancies. The distinct yet complementary mechanisms of these checkpoints—with CTLA-4 regulating early T cell activation and PD-1 modulating effector responses—provide a strong rationale for combination approaches that have demonstrated synergistic efficacy in multiple cancers. However, the therapeutic benefits of ICIs are constrained by resistance mechanisms and immune-related toxicities that reflect the fundamental biological roles of these checkpoints in maintaining self-tolerance. Ongoing research focuses on understanding resistance biology, developing predictive biomarkers, and engineering next-generation immunotherapies with improved therapeutic indices. As the field advances, mechanistic insights into checkpoint biology will continue to drive innovation in cancer immunotherapy.
Adoptive cell therapy (ACT) represents a pillar of cancer immunotherapy, comprising strategies where immune cells are isolated, often engineered or selectively expanded ex vivo, and reinfused into patients to enhance anti-tumor immunity. Its development is framed within the broader study of antitumor activity and immune-related toxicity mechanisms. ACT modalities are designed to overcome central mechanisms of immune evasion—such as inadequate T cell priming, immunosuppressive checkpoints, and a hostile tumor microenvironment (TME)—that often limit endogenous immune responses and other immunotherapies [6] [48].
The two most prominent ACT approaches are Chimeric Antigen Receptor T cells (CAR-T) and Tumor-Infiltrating Lymphocytes (TILs), both showing remarkable success in specific clinical contexts. CAR-T cells are genetically engineered to recognize surface antigens with high specificity, achieving transformative outcomes in hematologic malignancies [49] [50]. In contrast, TIL therapy leverages the diverse repertoire of T cells naturally infiltrating a patient's tumor, making it particularly promising for immunogenic solid tumors [51] [52]. Understanding the engineering, mechanisms of action, and associated toxicities of these living drugs is crucial for researchers and drug development professionals aiming to expand their efficacy to a broader range of cancers.
Core Principles of ACT and Antitumor Immunity
The foundational principle of ACT is the transfer of ex vivo-manipulated immune cells to mediate a potent, targeted antitumor effector function. This process bypasses several key barriers in the cancer-immunity cycle. A critical preparatory step is lymphodepleting chemotherapy (e.g., with fludarabine and cyclophosphamide), which eradicates endogenous immunosuppressive cells and eliminates cytokine sinks, thereby enhancing the persistence and activity of the infused cells [53] [54].
The antitumor activity of T cells, the primary effectors in most ACT, is a multi-stage process. It begins with antigen presentation by dendritic cells in lymph nodes, leading to T cell priming and activation. For this "immune synapsis" to be successful, T cell receptor (TCR) recognition of antigen presented by Major Histocompatibility Complex (MHC) molecules must be accompanied by co-stimulatory signals [53]. Once activated, T cells travel to the tumor site to execute their cytotoxic function.
However, the TME is a major site of immune evasion. It is populated by immunosuppressive cells like regulatory T cells (T-regs) and myeloid-derived suppressor cells (MDSCs), and features high levels of inhibitory checkpoint molecules (e.g., PD-1/PD-L1, CTLA-4), cytokines (e.g., TGF-β, IL-10), and metabolites (e.g., lactate, ammonia) that suppress T cell function and persistence [53] [6]. ACT strategies are fundamentally designed to overcome these suppressive mechanisms by selecting highly reactive cells or genetically engineering them for enhanced potency.
CAR T-cell Therapy: Engineering Synthetic Immunity
Molecular Architecture and Engineering
CAR-T cells are generated by genetically modifying a patient's own T cells to express a synthetic Chimeric Antigen Receptor. The CAR is a fusion protein that redirects T cells to surface antigens independent of MHC presentation.
Table 1: Generations of CAR-T Cell Design and Their Components
| Generation | Extracellular Domain | Hinge/Transmembrane Domain | Intracellular Signaling Domains | Key Features |
|---|---|---|---|---|
| First | scFv (Antigen-binding) | Hinge + Transmembrane | CD3ζ | Basic activation; limited persistence |
| Second | scFv (Antigen-binding) | Hinge + Transmembrane | CD3ζ + 1 Co-stimulatory (CD28 or 4-1BB) | Enhanced persistence & cytotoxicity; basis for all FDA-approved products [50] |
| Third | scFv (Antigen-binding) | Hinge + Transmembrane | CD3ζ + 2 Co-stimulatory (e.g., CD28+4-1BB) | Potentiated signaling |
| Fourth | scFv (Antigen-binding) | Hinge + Transmembrane | CD3ζ + Co-stimulatory + Inducible Transgene (e.g., cytokine) | "TRUCK" cells; modulates TME [50] |
| Fifth | scFv (Antigen-binding) | Hinge + Transmembrane | CD3ζ + Co-stimulatory + Cytokine Receptor Domain (e.g., IL-2Rβ) | Antigen-dependent JAK/STAT activation; enhanced memory [50] |
The core components are [50] [55]:
- Single-chain variable fragment (scFv): The antigen-binding domain derived from a monoclonal antibody.
- Hinge and Transmembrane Domain: Provides flexibility and anchors the CAR to the cell membrane.
- Intracellular T-cell Signaling Domains: Typically contain a costimulatory domain (e.g., CD28 or 4-1BB) and the CD3ζ chain from the TCR complex, which initiates T cell activation upon antigen binding.
Manufacturing and Workflow
The production of autologous CAR-T cells is a multi-step process that takes approximately 3-5 weeks [49].
Diagram 1: CAR-T Cell Manufacturing and Therapeutic Workflow. This diagram outlines the key steps from patient T-cell collection to post-infusion monitoring, highlighting the ex vivo genetic modification process.
Detailed Protocol:
- Leukapheresis: T cells are collected from the patient's peripheral blood [49].
- T cell Activation and Genetic Modification: Isolated T cells are activated using anti-CD3/CD28 antibodies and transduced with a viral vector (commonly a lentivirus or gamma-retrovirus) carrying the CAR transgene [50] [55].
- Ex Vivo Expansion: Transduced T cells are cultured in bioreactors with cytokines (e.g., IL-2) to expand to a therapeutic dose (hundreds of millions to billions of cells) [49].
- Lymphodepletion: The patient undergoes chemotherapy (e.g., fludarabine/cyclophosphamide) to create a favorable immunologic environment for the CAR-T cells [53].
- Infusion and Monitoring: The CAR-T product is infused back into the patient, who is closely monitored for both efficacy and toxicities like Cytokine Release Syndrome (CRS) and ICANS [49].
Mechanisms of Efficacy and Toxicity
Antitumor Activity: Upon binding to the target antigen on tumor cells, the CAR's intracellular domains initiate a robust T cell activation signal, leading to:
- Cytolytic Killing: Release of perforin and granzymes to directly lyse target cells.
- Cytokine Production: Secretion of IFN-γ, TNF-α, and IL-2, which amplify the immune response.
- T cell Proliferation and Persistence: Clonal expansion and formation of memory T cells for durable protection [50] [55].
Toxicity Mechanisms: The potent activation of CAR-T cells is a double-edged sword, leading to unique toxicities:
- Cytokine Release Syndrome (CRS): Widespread T cell activation causes a massive release of cytokines (IFN-γ, IL-6, GM-CSF), which activate monocytes and macrophages, leading to high fevers, hypotension, and potential organ dysfunction. IL-6 is a key mediator, and the IL-6 receptor antagonist tocilizumab is a standard treatment [49] [54].
- Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS): The pathogenesis is less clear but may involve endothelial activation, disruption of the blood-brain barrier, and direct effects of cytokines or CAR-T cells in the central nervous system, causing symptoms like confusion, aphasia, and seizures [49] [54].
- On-target, off-tumor toxicity: Damage to healthy tissues that express the target antigen, such as B-cell aplasia from CD19-targeted CAR-T therapy [55].
Tumor-Infiltrating Lymphocyte (TIL) Therapy: Harnessing Endogenous Immunity
Rationale and Native Biology
TIL therapy utilizes the diverse population of T cells that have naturally trafficked to a tumor, recognizing that these cells are enriched for T cell clones with inherent reactivity against a patient's unique tumor neoantigens [53] [52]. This provides a key advantage in targeting the heterogeneous antigen landscape of solid tumors, as the TIL product is a polyclonal mixture targeting multiple antigens simultaneously, reducing the risk of antigen escape [51].
Manufacturing and Workflow
TIL manufacturing differs significantly from CAR-T therapy as it does not involve genetic engineering ex vivo (in its conventional form), but instead focuses on the selective expansion of tumor-reactive T cells.
Diagram 2: TIL Therapy Manufacturing and Therapeutic Workflow. This process begins with tumor tissue and involves a large-scale expansion of naturally occurring tumor-reactive T cells.
Detailed Protocol:
- Tumor Harvesting: A tumor lesion is surgically resected from the patient [56] [52].
- TIL Isolation and Initial Expansion: The tumor tissue is digested and fragmented, and TILs are cultured out of the tumor fragments in high-dose IL-2. This step selects for cells that have infiltrated the tumor [56].
- Rapid Expansion Protocol (REP): The initial TIL population is vastly expanded over 1-2 weeks using a REP, which involves stimulatory agents like anti-CD3 antibody and irradiated feeder cells, alongside high-dose IL-2. This can yield over 100 billion T cells [56].
- Lymphodepletion and Infusion: The patient receives lymphodepleting chemotherapy, followed by infusion of the expanded TIL product [53].
- Supportive IL-2 Administration: Patients often receive systemic IL-2 after infusion to support the in vivo survival and expansion of the TILs, which can contribute to toxicity [56] [52].
Mechanisms of Efficacy and Toxicity
Antitumor Activity: The efficacy of TILs stems from their native biology:
- Diverse Antigen Recognition: TILs contain clonotypes targeting a wide array of tumor-specific neoantigens and tumor-associated antigens, effectively attacking heterogeneous tumor cell populations [51].
- Preferential Trafficking: As TILs are derived from the tumor site, they inherently possess the ability to traffic back to tumor lesions upon reinfusion [52].
- Established TCR Specificity: The naturally selected TCRs in TILs have high affinity for tumor antigens presented by the patient's own MHC.
The landmark clinical trial for lifileucel (the first FDA-approved TIL therapy) in advanced melanoma demonstrated an objective response rate of 31.4%, including complete responses in patients refractory to anti-PD-1 therapy [56].
Toxicity Profile: The primary toxicities associated with TIL therapy are largely related to the accompanying lymphodepleting chemotherapy and the high-dose IL-2 administered post-infusion. IL-2 can cause capillary leak syndrome, hypotension, and flu-like symptoms. The risk of severe CRS and ICANS, as seen with CAR-T cells, is generally lower with TIL therapy [56] [54].
Comparative Analysis and Clinical Translation
Table 2: Comparative Analysis of CAR-T and TIL Therapies
| Feature | CAR-T Cell Therapy | TIL Therapy |
|---|---|---|
| Cell Source | Peripheral blood T cells | Tumor tissue |
| Antigen Recognition | Single, predefined surface antigen (via scFv) | Diverse, multiple intracellular/surface antigens (via native TCR) |
| MHC Restriction | No | Yes |
| Genetic Engineering | Required (CAR transduction) | Not in conventional protocol (used in next-gen) |
| Manufacturing Time | ~3-5 weeks [49] | ~4-6 weeks [56] |
| Key Approved/Advanced Indications | B-cell ALL, NHL, Multiple Myeloma [49] [50] | Advanced Melanoma [51] [56] |
| Major Efficacy Challenges in Solid Tumors | Antigen heterogeneity, on-target/off-tumor toxicity, immunosuppressive TME, poor trafficking [53] [55] | Limited to immunogenic ("hot") tumors, immunosuppressive TME, T cell exhaustion [56] [52] |
| Prominent Toxicities | CRS, ICANS, on-target/off-tumor [49] [54] | Toxicity from lymphodepletion and IL-2 (capillary leak) [56] |
Table 3: Essential Research Reagents for ACT Development
| Research Reagent / Tool | Critical Function in ACT R&D |
|---|---|
| Viral Vectors (Lentivirus, Retrovirus) | Stable delivery and genomic integration of CAR transgenes or recombinant TCRs into lymphocytes [50] [55]. |
| Cytokines (IL-2, IL-7, IL-15) | Critical for ex vivo T cell expansion and survival (IL-2), and for promoting memory and persistence phenotypes (IL-7, IL-15) in culture [56] [52]. |
| Anti-CD3/CD28 Antibodies & Beads | Polyclonal T cell activation and co-stimulation during the initial phase of cell culture, essential for initiating expansion [56]. |
| CRISPR-Cas9 Systems | Gene editing for knocking out inhibitory receptors (PD-1), alloantigens (TCR, HLA) for off-the-shelf products, or inserting CARs into specific genomic loci [51] [52]. |
| Irradiated Feeder Cells | Used in TIL REP to provide non-specific stimulation for massive T cell expansion [56]. |
| Flow Cytometry Antibodies | Characterization of cell product phenotype (e.g., memory subsets, exhaustion markers) and detection of CAR or transgenic TCR expression. |
| Cytokine & Toxicity Assays | Multiplex ELISA/MSD to quantify cytokines in culture supernatant or patient serum for potency and toxicity (CRS) assessment [54]. |
Future Directions and Next-Generation Engineering
The future of ACT lies in overcoming the current limitations, particularly for solid tumors, through sophisticated genetic engineering and combination strategies. Key research frontiers include:
- Armored CAR-T Cells: Engineering CAR-T cells to secrete immunomodulatory agents (e.g., IL-12, IL-18, BiTEs) or express dominant-negative receptors for TGF-β to resist the immunosuppressive TME [50] [52].
- Gene Editing to Combat Exhaustion: Using CRISPR-Cas9 to knock out exhaustion-associated genes (PDCD1, LAG3) or transcription factors (TOX) in both CAR-T and TIL products to enhance persistence and function [51] [52].
- Metabolic Engineering: Modifying T cells to overexpress glycolytic enzymes or transcription factors (e.g., c-Jun, FOXO1) to improve their fitness and function in the nutrient-deprived, hypoxic TME [52].
- "Off-the-Shelf" Allogeneic Products: Creating universal CAR-T/NK cells from healthy donors by knocking out the TCR and HLA molecules to avoid graft-versus-host disease and host rejection [52] [55].
These advanced strategies, informed by a deepening understanding of T cell biology and tumor immunology, are poised to expand the reach and efficacy of ACT, solidifying its role as a cornerstone of cancer treatment.
Monoclonal antibodies (mAbs) represent a cornerstone of modern immunotherapy, with over 144 FDA-approved antibody drugs on the market and 1,516 candidates in clinical development worldwide as of 2025 [57]. Their therapeutic efficacy hinges on two fundamental mechanistic pillars: target engagement through antigen-binding fragments (Fab) and effector functions mediated by the crystallizable fragment (Fc) region. The Fab region enables precise binding to specific antigens on target cells, while the Fc region facilitates immune-mediated destruction through interactions with Fc gamma receptors (FcγRs) on immune cells [58] [59]. Understanding the intricate balance between these mechanisms is crucial for optimizing the antitumor activity and managing the toxicity profiles of immunotherapeutic antibodies.
The structural composition of immunoglobulin G (IgG) antibodies, the most commonly used isotype, features two heavy and two light chains forming a characteristic Y-shape. The variable regions at the tip of the Fab arms determine antigen specificity, while the constant Fc region governs functional interactions with the immune system [59]. This review examines the core mechanisms of target engagement and effector functions within the context of antitumor activity, detailing experimental methodologies for their evaluation and highlighting emerging optimization strategies.
Mechanisms of Target Engagement
Target engagement constitutes the initial critical step in mAb therapy, enabling precise recognition of malignant cells while theoretically sparing healthy tissues. This specificity is mediated by the complementarity-determining regions (CDRs) within the Fab portion of the antibody, which form a three-dimensional structure complementary to the target antigen [60].
Antigen Recognition and Binding
Successful target engagement requires high-affinity binding to tumor-associated antigens (TAAs) or tumor-specific antigens (TSAs). The binding event can induce therapeutic effects through multiple direct mechanisms:
- Receptor Blockade: mAbs targeting growth factor receptors (e.g., EGFR, HER2) physically obstruct ligand-binding domains, disrupting downstream oncogenic signaling pathways essential for tumor proliferation and survival [61] [57].
- Receptor Internalization: Certain mAb-antigen complexes undergo rapid endocytosis, effectively depleting the target receptor from the cell surface and enhancing antigen degradation [57].
- Apoptotic Signaling: Some mAbs directly initiate programmed cell death upon binding death receptors or through induction of intracellular stress signals [61].
Affinity and Specificity Optimization
The therapeutic window of mAbs depends significantly on binding affinity and specificity. Excessively high affinity can reduce tissue penetration due to the "binding site barrier" effect, while inadequate specificity increases off-target toxicity risks [60]. Advanced optimization strategies employ both experimental and computational approaches:
Table: Antibody Affinity Optimization Strategies
| Strategy | Methodology | Applications |
|---|---|---|
| Point Mutation | Site-directed substitutions at key residues combined with phage display | SARS-CoV-2 nucleocapsid protein binders; anti-ROS1 antibody 3B20-G1K [60] |
| Saturation Mutagenesis | Systematic codon replacement generating comprehensive variant libraries | SARS-CoV-2 spike protein optimization with >1×10^7 variants [60] |
| Chain Shuffling | Recombination of VH and VL chains to create diverse pairing combinations | Anti-α-cobratoxin antibodies with improved acidic condition binding [60] |
| Computational Design | AI-guided structure prediction and molecular dynamics simulations | De novo antibody scaffold design using RoseTTAFold and RFdiffusion [57] |
Engineering broad-spectrum mAbs is particularly valuable for infectious diseases where rapid viral mutation necessitates cross-reactivity across strains. Conversely, cancer applications often prioritize high specificity for tumor-specific epitopes to minimize on-target, off-tumor effects [60].
Effector Functions Mediated by Fc Region
The Fc region of mAbs serves as the primary mediator of immune effector functions by engaging various components of the innate immune system. Following target engagement, the Fc domain interacts with Fc gamma receptors (FcγRs) on immune cells and complement proteins in the serum, initiating destructive inflammatory responses against antibody-coated target cells [58] [59].
Fc Gamma Receptor Pathways
Human FcγRs are categorized into three main classes: FcγRI (CD64), FcγRII (CD32), and FcγRIII (CD16), each with distinct cellular expression patterns, affinities, and signaling properties [58]. These receptors are expressed on various immune cells including natural killer (NK) cells, macrophages, neutrophils, and dendritic cells.
- FcγRIIIa (CD16a) on NK cells is particularly crucial for initiating antibody-dependent cellular cytotoxicity (ADCC). Upon IgG binding, FcγRIIIa triggers intracellular signaling that leads to the release of perforin and granzymes, inducing apoptosis in target cells [59].
- FcγRIIa on macrophages and neutrophils facilitates antibody-dependent cellular phagocytosis (ADCP), enabling engulfment and destruction of opsonized target cells [58].
- The high-affinity FcγRI binds monomeric IgG and enhances antigen presentation and inflammatory cytokine production [58].
The Fc glycosylation pattern, particularly core fucosylation, significantly influences FcγR binding. Afucosylated antibodies demonstrate enhanced affinity for FcγRIIIa, leading to potentiated ADCC activity [59]. This has become a critical quality attribute for therapeutic mAbs, with glycoengineering technologies being employed to optimize effector function profiles.
Complement-Dependent Cytotoxicity
The Fc region can also activate the classical complement pathway by binding the C1q complex, leading to the formation of membrane attack complexes (MAC) that lyse target cells. This process, known as complement-dependent cytotoxicity (CDC), involves sequential activation of complement proteins (C1-C9) culminating in pore formation in the target cell membrane [59].
Table: Effector Functions of Monoclonal Antibodies
| Effector Function | Mechanism | Key Receptors/Components | Primary Effector Cells |
|---|---|---|---|
| ADCC | Fc-mediated NK cell activation causing target cell lysis | FcγRIIIa (CD16) | Natural killer cells |
| ADCP | Fc-mediated engulfment of opsonized targets | FcγRIIa | Macrophages, neutrophils |
| CDC | Complement cascade activation forming membrane pores | C1q | Serum complement proteins |
Impact of Antibody Aggregation on Effector Functions
Protein aggregation presents a significant challenge in mAb formulation and manufacturing, with profound implications for effector functions. Even low levels of aggregates can substantially alter FcγR binding profiles and potentially increase immunogenicity risk [58].
FcγR Binding Enhancements with Aggregation
Recent investigations demonstrate that mAb aggregates exhibit significantly increased binding to various FcγRs, particularly FcγRIIa, in avidity-based binding formats. This enhanced binding originates from the multivalent presentation of Fc regions in aggregated forms, facilitating simultaneous engagement with multiple Fcγ receptors [58].
Forced degradation studies utilizing stressors such as pH extremes, peroxide exposure, and light stress have been employed to generate controlled aggregates for functional characterization. Size exclusion chromatography fractions enriched for aggregates demonstrated dramatically increased FcγR binding in surface plasmon resonance (SPR) assays, with FcγRIIa showing the most pronounced effects [58].
Differential Effects in Cell-Based Assays
Interestingly, the enhanced FcγR binding observed with aggregated mAbs does not consistently translate to increased activity in cell-based reporter assays. While FcγRIIa reporter assays show slight activity increases with aggregates, FcγRIIIa reporter assays often display reduced activity, potentially due to differences in Fc glycosylation patterns between aggregated and monomeric fractions [58]. This discrepancy highlights the importance of utilizing multiple assay formats when evaluating the functional consequences of mAb aggregation.
Experimental Methodologies for Evaluating Target Engagement and Effector Functions
Assessing Target Engagement
Surface Plasmon Resonance (SPR) serves as a cornerstone technology for quantifying binding kinetics and affinity. SPR instruments measure real-time binding interactions between immobilized antigens and mAbs in solution, providing precise determinations of association rate (ka), dissociation rate (kd), and equilibrium dissociation constant (KD) [58].
Experimental Protocol: Surface Plasmon Resonance Binding Analysis
- Sensor Chip Preparation: Immobilize purified antigen onto a CM5 sensor chip using standard amine-coupling chemistry to achieve approximately 100-500 response units.
- Binding Kinetics Measurements: Inject mAb samples at concentrations ranging from 0.1 nM to 100 nM in HBS-EP buffer at a flow rate of 30 μL/min.
- Association Phase Monitoring: Measure binding responses for 3-5 minutes during antibody injection.
- Dissociation Phase Monitoring: Monitor dissociation in buffer-only flow for 10-15 minutes.
- Regeneration: Remove bound antibody using 10 mM glycine-HCl, pH 2.0, for 30 seconds.
- Data Analysis: Fit sensograms to a 1:1 Langmuir binding model using BIAevaluation software to calculate kinetic parameters [58].
Flow Cytometry provides complementary data on cell-surface binding using native antigen presentation. Cells expressing the target antigen are incubated with serially diluted mAbs, followed by fluorescent anti-human IgG detection. Analysis of fluorescence intensity provides quantitative binding data and estimates of receptor density [58].
Evaluating Effector Functions
FcγR Binding Assays utilize various formats to characterize Fc interactions:
- Solution-Based Binding: Measures direct binding between mAbs and soluble FcγR extracellular domains using ELISA or AlphaScreen platforms.
- Cell-Based Reporter Assays: Employ engineered cell lines expressing individual FcγRs linked to luciferase or GFP reporters to quantify functional activation [58].
ADCC Reporter Bioassay provides a standardized system for evaluating ADCC potency:
- Effector Cells: Utilize engineered Jurkat cells stably expressing FcγRIIIa (V158 variant) and an NFAT response element driving luciferase expression.
- Target Cells: Culture antigen-positive target cells (e.g., SK-BR-3 for HER2-targeting mAbs).
- Co-culture Assay: Mix effector and target cells at optimized ratios (typically 6:1 to 12:1) with serially diluted mAbs.
- Incubation and Detection: Incubate for 6-24 hours before measuring luciferase activity as a surrogate for ADCC activation [58].
Complement C1q Binding ELISA assesses CDC potential:
- Plate Coating: Immobilize antigen or antigen-expressing cell membranes to 96-well plates.
- Antibody Binding: Incubate with serially diluted mAbs for 2 hours.
- Complement Addition: Add human C1q protein and incubate for 1 hour.
- Detection: Use anti-C1q antibodies conjugated to horseradish peroxidase for colorimetric quantification [59].
Visualization of Key Signaling Pathways
Diagram 1: mAb Mechanisms of Target Engagement and Effector Functions. This diagram illustrates the dual mechanisms of monoclonal antibody action, showing how target engagement through Fab regions and effector function via Fc regions collectively contribute to antitumor activity.
The Scientist's Toolkit: Key Research Reagents and Materials
Table: Essential Research Reagents for mAb Functional Characterization
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Fc Gamma Receptors | Recombinant human FcγRI (CD64), FcγRIIa (CD32), FcγRIIIa (CD16) | SPR binding studies, ELISA, functional characterization of Fc interactions [58] |
| Complement Components | Human C1q protein | CDC evaluation via ELISA, complement activation assays [59] |
| Engineered Cell Lines | FcγRIIIa NFAT-luciferase reporter cells (Jurkat), CHO cells expressing human FcγRs | Standardized ADCC reporter bioassays, FcγR binding and activation studies [58] |
| Surface Plasmon Resonance | CMS sensor chips, HBS-EP buffer, amine-coupling reagents | Quantitative analysis of binding kinetics (ka, kd, KD) for target engagement [58] |
| Flow Cytometry Reagents | Fluorescent anti-human IgG antibodies, antigen-expressing cell lines | Cell-surface binding studies, receptor density quantification [58] |
| Size Exclusion Chromatography | TSK-Gel G3000SWxl columns, mobile phase buffers | Aggregate quantification and fractionation for functional studies [58] |
The therapeutic efficacy of monoclonal antibodies in cancer immunotherapy derives from the integrated activities of target engagement and effector functions. Optimal antibody design requires careful balancing of Fab-mediated specificity and Fc-mediated immune recruitment, with consideration of potential aggregation effects on function and immunogenicity. Advanced engineering strategies, including Fc glycoengineering, affinity maturation, and bispecific formats, continue to enhance the precision and potency of antibody-based therapeutics. As the field progresses, comprehensive characterization using the methodologies outlined herein remains essential for developing next-generation mAbs with improved antitumor activity and reduced toxicity profiles.
Cancer immunotherapy represents a transformative approach in oncology, fundamentally shifting treatment paradigms from directly attacking tumor cells to harnessing the body's own immune system for tumor suppression. By 2025, cancer is projected to cause approximately 618,120 deaths in the United States alone, with lung cancer demonstrating the highest mortality rate [42]. The foundation of modern cancer immunotherapy can be traced back to the late 19th century with William Coley's observations of tumor regression following bacterial infections, but significant acceleration has occurred over the past decade with over 150 FDA approvals since 2011, including 17 new approvals in 2024 alone [62]. Unlike conventional treatments like chemotherapy and radiotherapy that indiscriminately target both healthy and malignant cells, immunotherapy offers greater specificity, improved biocompatibility, and the potential for long-term anticancer immunity through immune memory formation [42].
The cancer-immunity cycle describes the immune system's delicate balance between recognizing tumor cells as foreign and preventing autoimmunity [42]. However, tumors develop sophisticated evasion mechanisms, including reduced surface antigen expression to lower immunogenicity, increased expression of immune checkpoints to inhibit T-cell function, recruitment of immunosuppressive cells, and production of acidic metabolites that impair immune cell functionality within the tumor microenvironment (TME) [42]. Cancer vaccines represent a promising immunotherapeutic strategy designed to overcome these evasion mechanisms by delivering target antigens, often with adjuvants, to evoke or amplify host immune responses against malignant cells [63]. This comprehensive review examines the current landscape of cancer vaccines and immune system modulators, focusing on their mechanisms in priming and amplifying antitumor immune responses within the broader context of therapeutic efficacy and toxicity mechanisms.
Antigen Selection Strategies for Cancer Vaccines
Classification of Tumor Antigens
The development of an effective cancer vaccine begins with identifying appropriate target antigens that are highly expressed in tumor tissues and capable of eliciting robust antigen-specific T-cell responses. Tumor antigens are broadly categorized into two main classes based on their expression patterns (Table 1).
| Antigen Category | Subtypes | Characteristics | Examples | Advantages | Limitations |
|---|---|---|---|---|---|
| Tumor-Associated Antigens (TAAs) | Overexpressed proteins | Self-proteins overexpressed in cancer cells | HER2/Neu, gp100, PAP, PSA, p53, MUC-1, IDO1, survivin, PD-L1 [64] | Shared among patients; facilitates large-scale production [63] | Subject to central tolerance; limited high-affinity T cells; risk of on-target/off-tumor toxicity [64] [63] |
| Germline/testis antigens | Expressed in fetal tissues, testes, and malignant tissues | WT1, NY-ESO-1, MAGE-A3 [64] | Restricted expression pattern reduces autoimmune potential | Limited to specific cancer types; heterogeneous expression [64] | |
| Tumor-Specific Antigens (TSAs) | Neoantigens | Arise from genetic alterations; unique to tumors | Mutated proteins from SNVs, indels, gene fusions [64] [63] | High immunogenicity; not subject to central tolerance; tumor-specific [64] [63] | Highly individualized; complex identification process; costly [63] |
| Oncoviral antigens | Viral proteins driving oncogenesis | EBV LMP1/LMP2, HPV E6/E7 [64] | Not subject to self-tolerance; ideal vaccine targets | Limited to virus-associated cancers [64] | |
| Cryptic antigens | Derived from noncoding sequences | Peptides from noncanonical open reading frames [63] | Tumor-restricted expression | Challenging identification and validation [63] |
Tumor-associated antigens (TAAs) are self-proteins that are abnormally expressed in tumor cells but may also be present at lower levels in normal tissues. These include tissue-specific antigens, overexpressed proteins, and cancer-testis antigens that are normally expressed only in immune-privileged sites [64] [63]. While TAAs offer the advantage of being shared across multiple patients and cancer types, their application is limited by central thymic tolerance mechanisms that delete high-affinity T-cell receptors, potentially restricting the potency of vaccine-induced responses and carrying risks of on-target/off-tumor toxicity against normal tissues expressing these antigens [64] [63].
Tumor-specific antigens (TSAs) are unique to tumor cells and absent from normal tissues, representing ideal vaccine targets due to their high specificity and potential for strong immunogenicity without self-tolerance limitations [64] [63]. Neoantigens, a prominent class of TSAs, arise from somatic mutations including single-nucleotide variants, insertions/deletions, gene fusions, and aberrant transcriptional or translational events [63]. Viral oncoproteins from pathogens like Epstein-Barr virus (EBV) and human papillomavirus (HPV) also constitute TSAs and have been successfully targeted with prophylactic vaccines that have significantly reduced virus-associated cancer incidence [64] [63].
Neoantigen Identification Pipeline
The identification of neoantigens has been revolutionized by advances in high-throughput sequencing and bioinformatics, enabling the development of personalized cancer vaccines. The standard pipeline involves three key components (Fig. 1):
Fig. 1. Neoantigen Identification and Vaccine Development Pipeline. The process begins with sequencing of tumor and normal tissues, followed by computational prediction and prioritization of candidates, and culminates in experimental validation and vaccine production.
First, prediction of neoantigens begins with comprehensive genomic and transcriptomic profiling. Whole-exome sequencing and RNA sequencing of tumor and matched normal tissues identify tumor-specific mutations [63]. The patient's HLA genotype is determined using tools such as OptiType and Polysolver for HLA class I alleles, or HLA*PRG and HLA-HD for both class I and II alleles [63]. Based on HLA typing, computational algorithms like NetMHC, NetMHCpan, and MHCflurry predict the binding affinity of mutant peptides to specific HLA molecules [63].
Second, filtration and prioritization refine the candidate list based on multiple factors, including mutation expression level, dissimilarity to self-proteins, mutation clonality, presentation efficacy, HLA binding affinity, and peptide-HLA complex stability [63]. This process generates a ranked list of neoantigen candidates optimized for immunogenic potential.
Third, experimental validation confirms the ability of predicted neoantigens to activate T cells. Techniques include T-cell-based assays, enzyme-linked immunospot (ELISpot) assay, flow cytometry, multicolor-labeled MHC tetramers, and T-cell repertoire profiling [63]. This critical step verifies immunogenicity before vaccine formulation.
Recent advances aim to identify "shared" or "public" neoantigens arising from common mutations in oncogenes like TP53, KRAS, and PI3KCA across multiple patients [63]. Such shared neoantigens enable development of off-the-shelf vaccines that are more cost-effective and time-efficient than fully personalized approaches, particularly beneficial for patients with limited treatment windows [63].
Cancer Vaccine Platforms and Delivery Systems
Advanced Vaccine Modalities
Multiple vaccine platforms have been developed to optimize antigen delivery and immune activation (Table 2). Each platform offers distinct advantages and limitations, with selection dependent on target antigens, desired immune response characteristics, and practical considerations like manufacturing complexity.
| Vaccine Platform | Key Features | Recent Clinical Advances | Challenges |
|---|---|---|---|
| RNA-Based Vaccines | Conventional mRNA, self-amplifying RNA, circular RNA; lipid nanoparticle delivery [65] | mRNA-4157 with pembrolizumab: 44% reduction in recurrence risk in melanoma; breakthrough results in pancreatic cancer and glioblastoma [65] | Cold-chain requirements; manufacturing cost (>$100,000 per patient) [65] |
| Peptide-Based Vaccines | Synthetic tumor antigens; often combined with adjuvants | Heteroclitic WT1 peptide (Galinpepimut-S) induced T-cell responses in AML [64] | Limited to known HLA restrictions; requires adjuvant for potency [64] |
| Viral Vector Vaccines | Engineered viruses delivering antigen genes; inherent adjuvanticity | MVA virus expressing EBNA-LMP2 fusion protein increased CD4+ and CD8+ T cells [64] | Pre-existing immunity may limit efficacy; safety concerns [66] |
| Dendritic Cell Vaccines | Autologous DCs loaded with antigens ex vivo | Sipuleucel-T (FDA-approved for prostate cancer); 4-month survival benefit [64] | Complex and costly manufacturing; patient-specific [64] |
| Microbial Delivery Systems | Bacteria (e.g., Listeria, Salmonella) or oncolytic viruses with tumor tropism [66] | Engineered Salmonella colonizing hypoxic tumor cores; oncolytic viruses with tumor-selective replication [66] | Safety concerns with live vectors; requires attenuation [66] |
| Whole-Cell Vaccines | Tumor cell lines or patient-derived tumor cells | Seviprotimut-L (multivalent melanoma vaccine) improved outcomes in younger patients [64] | Complex identification of immunogenic components; potential autoimmunity [64] |
RNA-based vaccines have emerged as particularly promising platforms, with recent clinical breakthroughs establishing them as viable options across multiple cancer types [65]. Conventional mRNA vaccines encode target antigens and are packaged in lipid nanoparticles for efficient delivery. Self-amplifying RNA platforms incorporate viral replication machinery that enables intracellular amplification of tumor antigen-encoding mRNA, providing prolonged immune stimulation with lower initial doses [65]. Circular RNA vaccines offer enhanced stability characteristics crucial for prolonged tumor antigen presentation, with recent developments demonstrating retained immunogenicity after lyophilization and storage at standard refrigeration temperatures [65].
The period from 2024-2025 has witnessed unprecedented clinical advances with RNA vaccines. The mRNA-4157 (V940) in combination with pembrolizumab has demonstrated sustained clinical benefit in melanoma, with 3-year recurrence-free survival rates maintaining superiority over pembrolizumab monotherapy [65]. Revolutionary results have also emerged in pancreatic cancer, with a personalized mRNA vaccine demonstrating remarkable efficacy where vaccine-induced immune responses persisted for nearly four years after treatment [65]. Novel layered nanoparticle delivery systems have also achieved unprecedented rapid immune system activation against brain tumors, with one mRNA vaccine successfully reprogramming the immune system to attack glioblastoma within 48 hours of administration [65].
Microbial delivery systems represent another innovative approach, leveraging the natural properties of microorganisms for cancer vaccination. Bacterial vectors like Listeria monocytogenes and Salmonella typhimurium demonstrate remarkable tumor tropism, particularly for hypoxic tumor regions, and innate immunogenicity [66]. Viral platforms, including oncolytic viruses and virus-like particles, amplify antigen presentation and T-cell activation through their natural infection mechanisms [66]. These systems engage host immune responses through pathogen-associated molecular patterns that activate pattern recognition receptors such as Toll-like receptors and the cGAS-STING pathway, effectively bridging innate and adaptive immunity [66].
Nanotechnology in Vaccine Delivery
Nanotechnology has emerged as a powerful tool to enhance cancer vaccine efficacy by improving antigen delivery precision and immunogenicity. Nanoengineering strategies address critical limitations of current delivery platforms by enabling tissue-specific targeting, enhanced tumor penetration, and reduced systemic toxicity [67]. Key applications include:
- Enhanced drug delivery: Ensuring vaccine components efficiently reach tumor sites and lymphoid tissues [67]
- Tumor microenvironment reprogramming: Modifying the immunosuppressive TME to make cancers more responsive to treatment [67]
- Combination with emerging approaches: Working with mRNA vaccines and engineered immune cells to expand their therapeutic reach [67]
Engineered nano-vaccines combine traditional vaccine technology with cutting-edge nanoscience to offer superior tumor-targeting precision and long-lasting immune protection [65]. These systems address the challenge of insufficient tumor targeting and inadequate immune activation that frequently hinders conventional cancer vaccines [66].
Immune Activation Mechanisms and Signaling Pathways
Initiating Antitumor Immunity
Cancer vaccines function through a coordinated sequence of immune activation events designed to generate robust antitumor responses. The process begins with vaccine administration and culminates in the destruction of tumor cells (Fig. 2).
Fig. 2. Immune Activation Pathway Following Cancer Vaccination. The cascade begins with antigen capture and presentation, progresses through T cell priming in lymphoid organs, and culminates in effector functions at the tumor site.
Following vaccination, innate immune cells including natural killer (NK) cells, neutrophils, and macrophages use pattern recognition receptors to rapidly recognize vaccine components and initiate early immune responses [63]. Antigen-presenting cells, particularly dendritic cells (DCs), play a central role in capturing, processing, and presenting vaccine antigens to T cells. Human DCs are primarily classified into CD123+ plasmacytoid DCs and conventional DCs, with the latter further divided into CD141+ cDC1s and CD1c+ cDC2s subsets [63]. These subsets display different functional specializations, with cDC1s particularly adept at antigen cross-presentation to activate CD8+ T cells, while cDC2s are vital for initiating CD4+ T cell responses [63].
Upon activation, immature DCs undergo maturation and migrate to secondary lymphoid organs where they present processed antigens to naïve T cells via MHC molecules [42]. This interaction requires both T-cell receptor engagement with peptide-MHC complexes and costimulatory signals such as CD80/CD86 binding to CD28 on T cells [42]. Following activation, T cells differentiate into effector populations including cytotoxic T lymphocytes and T helper cells, influenced by cytokine signals in the microenvironment [42]. Activated T cells undergo clonal expansion and then exit lymphoid organs to circulate through the bloodstream and reach tumor sites where they recognize and eliminate malignant cells expressing target antigens [42].
Mechanisms of Immune System Modulators
Immune system modulators enhance vaccine-induced responses by targeting regulatory pathways in the immune system. The most clinically established modulators are immune checkpoint inhibitors (ICIs) that block inhibitory receptors on T cells, such as cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and programmed death 1 (PD-1)/programmed death-ligand 1 (PD-L1) [68]. These checkpoints normally maintain immune homeostasis by preventing excessive activation, but tumors exploit them to suppress antitumor immunity [68].
ICIs function through distinct temporal and spatial mechanisms. CTLA-4 blockade primarily acts during the early T-cell priming phase in lymphoid tissues by competing with CD28 for binding to B7 molecules on antigen-presenting cells [69]. While CD28-B7 interaction promotes T-cell activation, CTLA-4 delivers inhibitory signals that suppress T-cell proliferation [69]. Anti-CTLA-4 antibodies shift this balance toward activation, enhancing initial T-cell priming and clonal expansion [69]. In contrast, PD-1/PD-L1 blockade acts predominantly at the effector phase within peripheral tissues and tumor sites [69]. PD-L1 expressed on tumor cells engages PD-1 receptors on CD8+ T cells to inhibit their function and enable immune evasion [69]. Blocking this interaction restores T-cell cytotoxicity against tumor cells [69].
Emerging immune checkpoint targets include lymphocyte activation gene 3 (LAG-3), T cell immunoreceptor with immunoglobulin and ITIM domain (TIGIT), and T cell immunoglobulin and mucin-domain-containing-3 (TIM-3), with corresponding inhibitors under active investigation [68]. These novel targets offer opportunities for multimodal immunomodulation to address the complexity of immune resistance mechanisms.
Combination Strategies: Vaccines with Immune Modulators
Rationale for Combination Therapy
The combination of cancer vaccines with immune checkpoint inhibitors represents a particularly promising strategy to enhance therapeutic efficacy. While vaccines prime and expand tumor-specific T cells, ICIs remove inhibitory signals that otherwise constrain these T cells within the tumor microenvironment [64] [63]. This synergistic approach addresses the limitation of either therapy alone—vaccines may generate potent T-cell responses that become inhibited in the suppressive TME, while ICIs require preexisting tumor-specific T cells to unleash [63].
The combination of mRNA-4157 with pembrolizumab exemplifies this strategy's potential, demonstrating a 44% reduction in recurrence risk compared to pembrolizumab monotherapy in melanoma patients [65]. This approach effectively converts immunologically "cold" tumors with limited T-cell infiltration into "hot" tumors with vigorous immune cell infiltration, thereby enhancing response to checkpoint inhibition [65] [66].
Integration with Other Modalities
Beyond checkpoint inhibitors, cancer vaccines are being combined with various treatment modalities to create multifaceted antitumor strategies:
- Chemotherapy and radiotherapy: These conventional therapies can induce immunogenic cell death, releasing tumor antigens that may synergize with vaccine-induced immune responses [42] [66]
- Microbial vaccines with ICIs: Microbial vectors can remodel the tumor microenvironment to enhance T-cell infiltration and function, potentially overcoming resistance to ICIs in cold tumors [66]
- Adoptive cell therapies: Vaccines may be used to enhance the persistence and functionality of transferred T cells in approaches like CAR-T therapy [64]
Each combination strategy requires careful optimization of dosing schedules and sequences to maximize synergy while minimizing overlapping toxicities.
Efficacy and Toxicity Considerations
Biomarkers for Predicting Response
Identifying reliable biomarkers to predict treatment efficacy is crucial for optimizing patient selection and therapeutic outcomes. Several biomarkers have emerged as potentially informative for cancer vaccine and immunotherapy response (Table 3).
| Biomarker Category | Specific Markers | Predictive Value | Limitations |
|---|---|---|---|
| Tumor Microenvironment | PD-L1 expression | High expression (TPS ≥50%) associated with better response to anti-PD-1/PD-L1 [70] | Temporal and spatial heterogeneity; cutoff variability [70] |
| Tertiary lymphoid structures (TLS) | Presence correlates with improved ICI response; sites for immune cell activation [70] | Standardization of assessment methods needed [70] | |
| Tumor-infiltrating lymphocytes (TILs) | High CD8+ T-cell density correlates with better outcomes [70] | Heterogeneous distribution within tumors [70] | |
| Genomic Features | Tumor mutational burden (TMB) | Higher TMB generally correlates with better ICI response [64] [70] | Variable predictive power across cancer types [70] |
| Neoantigen load | Quantity and quality of neoantigens influence vaccine and ICI efficacy [64] [70] | Complex identification process [63] | |
| Circulating Biomarkers | ctDNA | Dynamic changes may reflect treatment response [70] | Standardization needed across platforms [70] |
| Circulating immune cells | Composition and phenotype may predict toxicity or efficacy [70] | Still investigational [70] | |
| Microbiome | Gut microbiota composition | Specific species correlate with ICI efficacy [70] [66] | Mechanism not fully understood [66] |
PD-L1 expression remains the most widely used biomarker in clinical practice, with expression levels ≥50% associated with significantly improved outcomes with pembrolizumab in NSCLC (objective response rate of 45.2% vs. 10.7% for PD-L1 <1%) [70]. However, limitations include temporal and spatial heterogeneity, differences between primary tumors and metastatic lesions, and ongoing debate regarding optimal cutoff values [70].
Tertiary lymphoid structures have emerged as a promising biomarker, representing organized lymphoid aggregates that develop in chronic inflammation sites including tumors [70]. These structures provide appropriate microenvironments for immune cell maturation and activation, allowing rapid initiation of immune responses near tumor tissue [70]. Their presence, composition, maturation status, and location within the TME can reflect immune characteristics and predict response to immunotherapy [70].
Immune-Related Adverse Events and Toxicity Management
Despite their therapeutic benefits, immune checkpoint inhibitors and cancer vaccines introduce a spectrum of side effects known as immune-related adverse events (irAEs), which pose significant challenges in clinical management [69]. Unlike conventional chemotherapy toxicities, irAEs resemble autoimmune conditions but follow different natural courses than traditional autoimmune diseases [69]. These adverse events can affect almost any organ system, with the skin, gastrointestinal tract, liver, and endocrine glands being most commonly involved [69].
A recent real-world cohort study of 9,193 patients receiving ICIs between 2018-2022 found that 56.2% developed irAEs within one year, including 284 hospitalized cases [69]. Multivariable analysis identified several risk factors, with younger age (18-29 years), female sex, and specific comorbidities (myocardial infarction, heart failure, renal disease) associated with increased irAE risk [69]. Patients receiving CTLA-4 + PD(L)1 combination therapy had a 35% higher risk of irAEs than those treated with PD-1 inhibitors alone [69]. Breast and hematologic cancers conferred elevated risk, whereas brain cancer was linked to reduced risk [69].
The study also revealed distinct patterns in irAE manifestations. Multi-site irAEs were most common (affecting 44.7% of irAE patients), followed by gastrointestinal irAEs (25.3%) and neurologic irAEs (7.0%) [69]. Interestingly, over 70% of patients with cardiac, renal, and respiratory irAEs were male [69]. Comorbidities played a significant role in irAE development and presentation [69].
Management of irAEs requires a paradigm shift from conventional toxicity management, emphasizing early detection and timely intervention with immunosuppressive agents like corticosteroids [69]. Failure to effectively manage irAEs can significantly compromise patients' quality of life and diminish the overall benefits of immunotherapy [69].
Experimental Protocols and Research Tools
Key Methodologies in Cancer Vaccine Research
Neoantigen Identification Protocol:
- Sample Processing: Collect tumor and matched normal tissues (fresh frozen or FFPE). Extract high-quality DNA and RNA using validated kits.
- Sequencing: Perform whole-exome sequencing (≥150x coverage for tumor, ≥60x for normal) and RNA sequencing (≥100 million reads). Include spike-in controls for quality assessment.
- Bioinformatic Analysis:
- Align sequences to reference genome (GRCh38) using BWA-MEM or STAR
- Identify somatic mutations with MuTect2, VarScan2, or similar tools
- Determine HLA genotype using OptiType (class I) and HLA-HD (class I/II)
- Predict HLA binding with NetMHCpan (version 4.1) for class I and NetMHCIIpan (version 4.0) for class II
- Prioritize candidates based on binding affinity (<50nM for strong binders, 50-500nM for weak binders), mutation clonality, and expression level
- Experimental Validation:
- Synthesize candidate peptides (≥95% purity)
- Perform IFN-γ ELISpot assays with patient PBMCs
- Use dextramer or tetramer staining to quantify antigen-specific T cells
- Conduct TCR sequencing to track clonal expansion
Vaccine Immunogenicity Assessment:
- T Cell Response Monitoring:
- Multicolor flow cytometry for T-cell phenotyping (CD3, CD4, CD8, CD45RA, CCR7, PD-1, TIM-3)
- Intracellular cytokine staining (IFN-γ, TNF-α, IL-2)
- Activation-induced marker (AIM) assay following antigen stimulation
- Functional Assays:
- Cytotoxicity assay using CFSE-labeled target cells
- Proliferation assessment with CFSE or CellTrace Violet
- Tumor Infiltration Analysis:
- Multiplex immunohistochemistry of tumor sections
- Single-cell RNA sequencing of tumor-infiltrating lymphocytes
The Scientist's Toolkit: Essential Research Reagents
| Research Tool Category | Specific Reagents/Assays | Research Application | Key Functions |
|---|---|---|---|
| Antigen Identification | NetMHCpan, NetMHCIIpan, MHCflurry | Neoantigen prediction | Computational prediction of HLA-peptide binding [63] |
| OptiType, Polysolver, HLA-HD | HLA genotyping | Determination of patient-specific HLA alleles [63] | |
| IFN-γ ELISpot, intracellular cytokine staining | Neoantigen validation | Experimental confirmation of immunogenicity [63] | |
| Immune Monitoring | MHC tetramers/dextramers | Antigen-specific T cell quantification | Direct detection and isolation of antigen-reactive T cells [63] |
| Multicolor flow cytometry panels | T cell phenotyping | Comprehensive characterization of T cell subsets and differentiation states [63] | |
| TCR sequencing | T cell repertoire analysis | Tracking clonal dynamics and persistence [63] | |
| Vaccine Delivery | Lipid nanoparticles (LNPs) | RNA vaccine delivery | Protecting and delivering nucleic acid payloads to target cells [65] |
| Bacterial vectors (Listeria, Salmonella) | Microbial vaccine platform | Tumor-targeted antigen delivery with inherent adjuvanticity [66] | |
| Viral vectors (MVA, adenovirus) | Viral vaccine platform | High-efficiency gene delivery for antigen expression [64] [66] | |
| TME Analysis | Multiplex IHC/IF | Spatial immune profiling | Visualization of immune cell distribution and tertiary lymphoid structures [70] |
| Single-cell RNA sequencing | Tumor microenvironment characterization | Comprehensive analysis of cellular heterogeneity and states [70] [68] | |
| Mass cytometry (CyTOF) | High-dimensional phenotyping | Deep immunophenotyping beyond fluorescence-based flow cytometry [70] |
The field of cancer vaccines and immune modulators continues to evolve rapidly, with several promising directions emerging. Manufacturing innovations are addressing key bottlenecks in personalized vaccine production, with automated closed-system platforms reducing production timelines from nine weeks to under four weeks for personalized vaccines, though costs remain challenging at over $100,000 per patient [65]. The integration of artificial intelligence with CRISPR technology represents a transformative advancement, enabling unprecedented precision in neoantigen selection and immune response optimization [65]. AI-driven platforms now incorporate multi-omics data analysis to identify optimal tumor-specific targets while predicting immunogenicity and potential immune escape mechanisms [65].
The regulatory landscape is also evolving, with the FDA releasing comprehensive guidance for therapeutic cancer vaccines in 2024 [65]. Experts anticipate that the first commercial mRNA cancer vaccine could receive regulatory approval by 2029, marking a significant milestone in oncology and paving the way for broader applications of mRNA technology in cancer treatment [65]. Looking ahead, the convergence of nanotechnology, synthetic biology, and immunology promises to address remaining challenges in vaccine delivery, tumor microenvironment modulation, and personalized therapy optimization.
In conclusion, cancer vaccines and immune system modulators represent a powerful therapeutic approach that primes and amplifies antitumor immune responses through sophisticated mechanisms. By selecting appropriate target antigens, employing advanced delivery platforms, strategically combining with immune modulators, and carefully managing toxicity, these therapies offer the potential to achieve durable responses across multiple cancer types. As research continues to address challenges in efficacy prediction, toxicity management, and manufacturing scalability, these modalities are positioned to become cornerstone therapeutics in precision oncology, ultimately improving outcomes for cancer patients worldwide.
Natural Killer (NK) cells are innate lymphoid cells that provide a first-line defense against malignant cells without requiring prior sensitization or major histocompatibility complex (MHC) restriction [25]. Since their discovery in 1975, NK cells have been recognized for their capacity to lyse tumor cells through sophisticated receptor systems that distinguish healthy from transformed cells [71]. The clinical significance of NK cells in cancer immunotherapy has expanded dramatically, evolving from cytokine augmentation to genetically engineered approaches that enhance their specificity and persistence [71]. Unlike chimeric antigen receptor (CAR)-T cell therapies, NK cell-based immunotheracies demonstrate superior safety profiles with minimal induction of graft-versus-host disease (GVHD) or severe cytokine release syndrome (CRS), positioning them as promising "off-the-shelf" therapeutics [72] [71].
The therapeutic landscape now includes multiple NK cell-based platforms: adoptive transfer of ex vivo-expanded allogeneic NK cells, cytokine-induced memory-like NK cells, CAR-NK constructs, bispecific/trispecific killer cell engagers (BiKEs/TriKEs), and more recently, NK cell-derived extracellular vesicles (NK-EVs) [73] [71]. These approaches leverage the inherent biological advantages of NK cells while addressing limitations of traditional immunotherapies. This technical review examines the mechanisms of antitumor activity and toxicity profiles of emerging NK cell-based therapies and extracellular vesicles, providing researchers and drug development professionals with current methodologies, quantitative comparisons, and experimental frameworks for advancing these innovative cancer treatments.
NK Cell Biology and Antitumor Mechanisms
NK Cell Development and Heterogeneity
NK cells develop from CD34+ hematopoietic stem cells in the bone marrow and secondary lymphoid tissues, undergoing a maturation process that yields functionally distinct subsets [71]. Human NK cells are primarily classified into two subsets based on CD56 and CD16 expression: CD56dimCD16+ NK cells (approximately 90% of peripheral blood NK cells) which exhibit potent cytotoxic activity, and CD56brightCD16- NK cells (approximately 10%) which specialize in cytokine production and immunoregulation [74] [25]. A third subset, CD56-CD16+ NK cells, emerges during chronic viral infections and displays impaired functionality [74]. During aging and in cancer patients, the distribution of these subsets shifts significantly, with expansions of CD57+ senescent NK populations and contractions of the CD56bright compartment, contributing to diminished immune surveillance [74].
Table 1: Human NK Cell Subsets and Characteristics
| Subset | Percentage in Peripheral Blood | Primary Function | Key Surface Markers | Changes in Cancer/Aging |
|---|---|---|---|---|
| CD56dimCD16+ | ~90% | Cytotoxicity, ADCC | CD16+, CD56dim, KIR+, CD57+ (senescent) | Expanded in aging; decreased activating receptors [74] |
| CD56brightCD16- | ~10% | Cytokine production, immunoregulation | CD16-, CD56bright, CD94/NKG2A+, IL-2R+ | Decreased in aging; impaired cytokine production [74] |
| CD56-CD16+ | Variable (in chronic infection) | Reduced cytotoxicity | CD16+, CD56-, CD57low, KIRlow | Expanded in chronic infections; considered dysfunctional [74] |
Molecular Mechanisms of Tumor Cell Recognition and Killing
NK cell activation is governed by a delicate balance between activating and inhibitory signals received through an array of surface receptors [25]. Inhibitory receptors (KIR2DL, KIR3DL, NKG2A) recognize self-MHC class I molecules, preventing autoreactivity, while activating receptors (NKG2D, NKp30, NKp46, DNAM-1) bind stress-induced ligands on transformed cells [71] [25]. The "missing-self" recognition paradigm enables NK cells to target cells with downregulated MHC class I, a common immune evasion strategy employed by tumors [71].
Upon activation, NK cells employ four primary cytotoxic mechanisms (Figure 1):
Perforin/Granzyme Pathway: Cytotoxic granules containing perforin and granzymes are released into the immune synapse. Perforin forms transmembrane pores facilitating granzyme entry into target cells, where granzymes activate caspase-dependent and independent apoptotic pathways [75] [25]. This process is regulated by cathepsins (C, H, L) which activate pro-granzymes and process perforin, while cystatin F serves as a negative regulator [75].
Death Receptor Pathway: NK cells express Fas ligand (FasL/CD178) and TRAIL which engage corresponding death receptors (Fas, TRAILR) on target cells, initiating extrinsic apoptosis through caspase-8 activation [75] [25].
Antibody-Dependent Cellular Cytotoxicity (ADCC): Through CD16 (FcγRIIIa), NK cells recognize antibody-opsonized cells, leading to potent cytolysis and cytokine production [25].
Cytokine-Mediated Antitumor Effects: NK cells secrete IFN-γ, TNF-α, and other immunomodulatory cytokines that inhibit tumor proliferation, promote macrophage activation, and enhance antigen presentation [25].
Figure 1: NK Cell Cytotoxic Mechanisms. NK cells employ four primary pathways to eliminate target tumor cells.
NK Cell Dysfunction in Cancer and Strategies for Reversal
Mechanisms of NK Cell Impairment in the Tumor Microenvironment
In cancer patients, NK cells exhibit significant functional impairment through multiple mechanisms. Quantitative and qualitative deficiencies occur in both peripheral blood and tumor-infiltrating NK populations, characterized by reduced expression of activating receptors (CD16, NKG2D, NKp30), decreased cytotoxicity, and diminished cytokine production [75] [71]. The immunosuppressive tumor microenvironment (TME) drives NK cell dysfunction through metabolic constraints (nutrient deprivation, hypoxia), inhibitory checkpoint expression (PD-1, TIGIT, NKG2A), and suppressive cytokines (TGF-β, IL-10) [71] [76]. Cancer cells further evade NK cell surveillance through proteolytic shedding of activating ligands (MICA/MICB) and upregulation of inhibitory ligands (HLA-E) [71].
Genetic and environmental factors significantly impact NK cell function during early carcinogenesis. Studies in murine models demonstrate that high-fat, high-calorie diets (HFCD) reduce NK cell numbers and cytotoxicity during the preneoplastic stage of pancreatic cancer, particularly in KRAS-mutant mice [75]. Feeder cells from these mice show decreased levels of MHC class I inhibitory ligands and RAE1-delta activating ligands essential for NK cell signaling, correlating with pancreatic intraepithelial neoplasia (PanIN) development [75]. In pancreatic ductal adenocarcinoma (PDAC), interactions between NK cells and tumors increase IL-6 secretion while decreasing IFN-γ, potentially promoting tumor growth [75].
Metabolic Adaptation and Plasticity in the TME
NK cells undergo metabolic reprogramming in the TME that compromises their antitumor functions. Tumors create nutrient-depleted niches with limited glucose, amino acids, and oxygen, forcing NK cells to adapt their metabolic pathways in ways that diminish effector capabilities [71]. Increased lipid metabolism in particular impairs NK cell function and mediates adaptation to the lymphoma environment [71]. The metabolic flexibility of NK cells ultimately determines their functional fate in the TME, with implications for persistence and cytotoxicity of adoptively transferred NK products [71].
Current NK Cell-Based Therapeutic Platforms
Adoptive NK Cell Transfer
Adoptive transfer of ex vivo-expanded allogeneic NK cells has demonstrated promising results in hematologic malignancies. In clinical trials, haploidentical NK therapy achieved 45-58% complete remission rates in acute myeloid leukemia (AML) [25]. Allogeneic NK cells with inhibitory killer immunoglobulin-like receptors (KIRs) can effectively eliminate cancer cells lacking proper MHC ligands, leveraging the "missing-self" recognition principle [75]. The production process typically involves isolation of NK cells from peripheral blood mononuclear cells (PBMCs) followed by ex vivo expansion with cytokine activation (IL-2, IL-15) over 2-3 weeks, resulting in NK cell products with >90% purity [77] [76].
Table 2: Clinical Outcomes of Selected NK Cell-Based Therapies
| Therapy Type | Clinical Setting | Efficacy Outcomes | Safety Profile | Reference |
|---|---|---|---|---|
| Haploidentical NK cells | AML | 45-58% CR | No severe GVHD; manageable CRS | [25] |
| CD19-CAR-NK cells | B-cell malignancies | 73% ORR; 91% 12-month EFS (ELIANA trial) | No CRS ≥ grade 3 | [25] |
| NKG2D CAR-NK cells | Advanced colorectal cancer | Stable disease in 1 patient; 2 patients with OS >700 days | Reversible CRS; mild GI symptoms | [72] |
| AFM13 (CD30/CD16A BiKE) + NK cells | Lymphoma | 94% ORR | Favorable safety profile | [71] |
| NK cell-derived EVs | NSCLC organoids | 40-45% decrease in viability | No major AEs in systematic review | [78] [76] |
Genetically Engineered CAR-NK Cells
Chimeric antigen receptor NK (CAR-NK) cells represent a breakthrough in cancer immunotherapy, combining the targeting specificity of CARs with the inherent safety advantages of NK cells. The CAR construct typically consists of an antigen-binding domain (often scFv), transmembrane domain, and intracellular signaling domains (CD3ζ, 4-1BB, or CD28) [72] [25]. In a phase I clinical trial of NKG2D CAR-NK cells expressing membrane-bound IL-15 for advanced colorectal cancer, the therapy demonstrated favorable safety with no treatment-related deaths or serious non-hematologic toxicities [72]. Common adverse events included reversible cytokine release syndrome (CRS) and mild gastrointestinal symptoms [72]. Notably, combination with anti-PD-1 therapy substantially increased peak CAR transgene levels compared to monotherapy (median CAR copies: 45,593 versus 1,001), suggesting potential synergistic effects [72].
Figure 2: CAR-NK Engineering Architecture. CAR-NK constructs incorporate antigen recognition, signaling, and persistence domains.
Cytokine-Induced Memory-Like NK Cells
Cytokine-induced memory-like (CIML) NK cells represent an innovative approach to enhance NK cell potency and persistence. When pre-activated with cytokines (IL-12, IL-15, and IL-18), NK cells develop enhanced functionality upon re-stimulation, characterized by improved antitumor activity and antibody-dependent cellular cytotoxicity (ADCC) [73]. These memory-like NK cells demonstrate metabolic advantages and increased longevity compared to conventional NK cells, making them promising candidates for adoptive immunotherapy [73] [71]. Clinical studies have shown that CIML NK cells can persist for extended periods and exhibit recall responses, blurring the traditional boundaries between innate and adaptive immunity [71].
NK Cell-Derived Extracellular Vesicles as Novel Therapeutics
Biogenesis, Isolation, and Characterization of NK-EVs
Extracellular vesicles derived from NK cells (NK-EVs) are nanoscale lipid bilayer structures (50-150 nm) that carry bioactive molecules from their parent cells, including cytotoxic proteins, nucleic acids, and immunomodulatory factors [73] [77]. These vesicles are formed through the endosomal pathway and released upon fusion of multivesicular bodies with the plasma membrane [73]. NK-EVs can be isolated from NK cell culture supernatants using differential ultracentrifugation, density gradient centrifugation, or size-exclusion chromatography [73] [77]. For industrial-scale production, extrusion-based methodologies have been developed to generate artificial NK-EVs (NK-aEVs) with superior yield and bioactivity compared to natural EVs (NK-nEVs) [77].
Characterization of NK-EVs requires multiple complementary techniques: transmission electron microscopy (TEM) for morphological analysis of cup-shaped structures; nanoparticle tracking analysis (NTA) for size distribution; dynamic light scattering (DLS) for dispersion uniformity; and Western blotting for protein markers (CD9, CD63, CD81, TSG101 for general EV markers; CD56, perforin for NK-specific markers) [73] [77]. Functional validation includes flow cytometry for surface antigen profiling and cytotoxicity assays (e.g., LDH release) to confirm tumor-killing efficacy [73].
Mechanisms of Antitumor Activity of NK-EVs
NK-EVs exert antitumor effects through multiple mechanisms that mirror their parent cells while offering distinct advantages. The vesicles carry a diverse cargo of cytotoxic molecules including perforin, granzymes (A, B), and FasL, which collectively induce apoptosis in target cells [73] [77]. Additionally, NK-EVs contain miRNA species (e.g., miR-186) that suppress oncogenic pathways (MYCN, AURKA) and block TGFβ signaling, countering immune evasion mechanisms [73]. In lung cancer models, NK-EVs demonstrated significant cytotoxicity, inducing 40-45% decrease in tumor organoid viability and enhancing the efficacy of standard chemotherapies [76].
Beyond direct tumor killing, NK-EVs remodel the tumor microenvironment by enhancing infiltration of CD8+ T cells and NK cells while reducing immunosuppressive populations (macrophages, myeloid-derived suppressor cells) [77]. In co-culture experiments with NSCLC organoids, NK-EV addition favorably shifted the immune population, significantly decreasing CD4+ T cells and increasing CD56+ NK cells [76]. This immunomodulatory capacity, combined with their nanoscale size, enables superior tumor penetration compared to parental NK cells, particularly across biological barriers such as the blood-brain barrier and blood-tumor barrier [73] [77].
Engineering Strategies for Enhanced NK-EV Efficacy
Unmodified NK-EVs face limitations including insufficient active components, suppression by the TME, and lack of targeting specificity [73]. Engineering approaches address these challenges through:
Drug Loading: NK-EVs serve as delivery vehicles for chemotherapeutic agents (paclitaxel), siRNAs (BCL-2 targeting), and other therapeutic payloads, enhancing tumor-specific accumulation while minimizing systemic toxicity [73].
Surface Modification: Genetic or chemical engineering of EV surfaces can improve targeting specificity through incorporation of tumor-homing peptides or antibodies [73].
Artificial EV Production: Extrusion-based generation of NK-aEVs enriches cytotoxic proteins (Granzyme B) and demonstrates superior scalability and bioactivity compared to natural EVs [77]. In murine models, intratumoral NK-aEVs suppressed Lewis lung carcinoma and MC38 tumor growth by 60% without systemic toxicity [77].
Table 3: Functional Cargo and Efficacy of NK Cell-Derived Extracellular Vesicles
| EV Cargo | Cancer Model | Administration Route | Key Findings | Reference |
|---|---|---|---|---|
| Perforin, Granzymes, FasL | Melanoma, stomach, colon cancer | In vitro and in vivo | Apoptosis induction via perforin, granzymes, Fas/FasL pathways | [73] |
| miR-186 | Neuroblastoma | In vitro | Suppressed MYCN, AURKA, TGFBR1/2; blocked TGFβ signaling | [73] |
| BCL-2 siRNA | Breast cancer | In vitro | Promoted apoptosis in cancer cells with no effect on normal cells | [73] |
| Engineered NK-aEVs with Granzyme B | Lung cancer, colon cancer | Intratumoral | 60% tumor growth suppression; enhanced CD8+ T/NK cell infiltration | [77] |
| Patient-derived NKEVs | NSCLC organoids | Co-culture | 40-45% decreased viability; lowered required cisplatin dose | [76] |
Experimental Protocols and Methodologies
NK Cell Expansion and EV Production Protocol
NK Cell Expansion from PBMCs:
- Isolate PBMCs from donor blood using Ficoll-Paque density gradient separation with SepMate tubes [77] [76].
- Cryopreserve PBMCs in 90% FBS + 10% DMSO at -80°C or in vapor phase liquid nitrogen [76].
- Thaw and pre-culture PBMCs with 200 U/mL human recombinant IL-2 in complete medium (RPMI-1640 with 10% exosome-depleted FBS) [77].
- Continuously culture for 2 weeks, maintaining cell density at 0.5-1×10^6 cells/mL with fresh IL-2 supplementation every 2-3 days [77].
- Validate NK cell purity (>90% CD56+CD3-) using flow cytometry before experimentation [77].
Natural NK-EV Isolation:
- Centrifuge NK cell culture supernatant at 300g for 10 min to remove dead cells [77].
- Centrifuge at 2,000g for 10 min to eliminate cell debris [77].
- Ultracentrifuge at 10,000g for 30 min to sediment large vesicles [77].
- Ultracentrifuge at 100,000g for 90 min to pellet NK-EVs [77].
- Resuspend EV pellets in PBS and wash 2-3 times with additional ultracentrifugation to enhance purity [77].
- Quantify EV protein concentration using BCA assay and characterize using NTA, TEM, and Western blotting [73] [77].
Artificial NK-EV Production via Extrusion:
- Collect expanded NK cells and resuspend in PBS at 1×10^6 cells/mL [77].
- Process cell suspension through a high-pressure extruder with sequential membrane filters (10μm, 5μm, 1μm, 400nm) [77].
- Collect extruded material and purify via ultracentrifugation as described above [77].
- Characterize NK-aEVs for size distribution, marker expression, and cytotoxic protein content [77].
In Vitro and In Vivo Efficacy Assessment
Cytotoxicity Assays:
- LDH Release Assay: Co-culture NK-EVs with target tumor cells at various concentrations (e.g., 0-200 μg/mL) for 24-48 hours [73] [77]. Measure lactate dehydrogenase release from damaged cells using colorimetric or fluorometric detection.
- Apoptosis Detection: Stain cells with Annexin V-FITC/PI after NK-EV treatment and analyze by flow cytometry to distinguish early/late apoptotic populations [77].
- Organoid Viability: Treat patient-derived tumor organoids with NK-EVs ± standard chemotherapies. Assess viability using Cell Counting Kit-8 (CCK-8) or similar metabolic assays [76].
In Vivo Tumor Models:
- Establish subcutaneous tumors in immunodeficient mice (e.g., NSG) by injecting 1-5×10^6 tumor cells suspended in Matrigel [77].
- When tumors reach 50-100 mm³, administer NK-EVs via intratumoral or intravenous injection [77]. Typical doses range from 100-200 μg protein equivalent, administered 2-3 times weekly [77].
- Monitor tumor dimensions 2-3 times weekly using calipers (volume = 0.5 × length × width²) [77].
- For immune profiling, harvest tumors at endpoint, process to single-cell suspensions, and analyze by flow cytometry for immune cell populations (CD45+ leukocytes, CD8+ T cells, NKp46+ NK cells, CD11b+Gr-1+ MDSCs) [77].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for NK Cell and EV Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| NK Cell Isolation | CD56 MicroBeads, CD3 Depletion Kits | Positive selection or negative enrichment of NK cells from PBMCs | Human NK cell isolation for expansion or functional studies [77] |
| Expansion Cytokines | IL-2, IL-15, IL-12, IL-18 | Promote NK cell proliferation and enhance functionality | Generation of cytokine-induced memory-like NK cells [73] [77] |
| Flow Cytometry Antibodies | Anti-CD56, CD16, CD3, CD107a, IFN-γ, perforin, granzyme B | Phenotypic characterization and functional assessment | NK cell purity validation, degranulation assays, intracellular cytokine staining [77] [76] |
| EV Characterization | Anti-CD9, CD63, CD81, TSG101, CD56, perforin | Identification of EV markers and NK-specific proteins | Western blot, flow cytometry for EV characterization [73] [77] |
| Cytotoxicity Assays | LDH Release Kit, Annexin V/PI Apoptosis Kit, CCK-8 | Quantification of tumor cell killing | In vitro assessment of NK cell or NK-EV cytotoxic potency [73] [77] |
| Animal Models | Immunodeficient mice (NSG, NOG), murine tumor cell lines (LLC, MC38) | In vivo evaluation of therapeutic efficacy | Xenograft models for assessing antitumor activity [77] |
NK cell-based therapies and extracellular vesicles represent promising approaches in cancer immunotherapy with distinct advantages in safety and "off-the-shelf" potential compared to T-cell-focused strategies. While significant progress has been made, particularly for hematological malignancies, challenges remain in achieving consistent efficacy against solid tumors and ensuring sufficient persistence of adoptively transferred cells [71] [25]. Future directions include optimizing combination strategies with immune checkpoint inhibitors, enhancing tumor homing through engineered chemokine receptors, developing improved cytokine support systems, and standardizing manufacturing processes for clinical-grade NK-EVs [72] [71] [77].
The systematic characterization of NK-EV cargo and its functional correlates will enable more rational design of next-generation vesicle-based therapeutics [76]. Similarly, advances in genetic engineering using CRISPR/Cas9 and other genome-editing technologies will further enhance the specificity and potency of CAR-NK products [25]. As these technologies mature, NK cell-based approaches are poised to transition from supportive players to central modalities in cancer immunotherapy, potentially addressing critical gaps in current treatment paradigms for both hematological and solid malignancies.
Balancing Efficacy and Safety: Overcoming Resistance and Managing Toxicity
Immune checkpoint inhibitors (ICIs) have fundamentally transformed the therapeutic landscape for a wide range of malignancies. By blocking inhibitory receptors such as cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) and programmed death 1 (PD-1) or its ligand (PD-L1), these agents reinvigorate the antitumor immune response, leading to unprecedented survival benefits in patients with advanced cancers [42]. However, the disruption of immune checkpoint pathways, which are critical for maintaining self-tolerance, inadvertently unleashes immune-mediated attacks on healthy tissues. These events are collectively termed immune-related adverse events (irAEs) [79].
irAEs represent a significant challenge in clinical oncology and immunotherapy development, characterized by their heterogeneity in onset, presentation, and organ system involvement. Their spectrum ranges from mild, self-limiting conditions to severe, life-threatening complications that necessitate treatment discontinuation [80] [69]. Understanding the precise pathophysiology and the full scope of organ-specific manifestations is therefore paramount for the safe and effective application of ICIs in cancer therapy. This whitepaper synthesizes current evidence on the mechanisms, clinical spectrum, and research methodologies pertaining to irAEs, framed within the broader context of antitumor immunity and toxicity mechanisms.
Pathophysiological Mechanisms of irAEs
The pathogenesis of irAEs is complex and multifactorial, arising from a breakdown of immune homeostasis. The core mechanism involves the non-specific activation of autoreactive T cells due to checkpoint blockade, but this is amplified by dysregulation of humoral immunity, inflammatory cytokines, and host-specific factors [79] [81].
T-Cell-Mediated Immunopathology
The predominant pathophysiological model for irAEs centers on aberrant T-cell activation. Under physiological conditions, CTLA-4 and PD-1 pathways dampen T-cell responses to prevent autoimmunity. ICIs disrupt this balance, leading to the expansion and activation of self-reactive T-cell clones [79].
- Self-Reactive T-Cell Activation: Blocking CTLA-4 enhances T-cell priming in lymphoid tissues, leading to a broader repertoire of effector T cells, including those with autoreactive potential. PD-1/PD-L1 blockade, in contrast, primarily reverses T-cell exhaustion in peripheral tissues, enabling cytotoxic CD8+ T cells and helper CD4+ T cells to attack tissues that express shared or self-antigens [6] [81]. For example, T cells specific for α-myosin have been identified in cases of ICI-induced myocarditis [79].
- Helper T-Cell Subset Polarization: ICI treatment can skew CD4+ T helper (Th) cells toward pro-inflammatory phenotypes. Shifts toward Th17 cells have been documented in patients receiving CTLA-4 blockade, while other irAEs are associated with signatures of Th2 and Th17 cells [81]. These subsets drive tissue inflammation through the production of distinct cytokine profiles (e.g., IL-17, IL-6, IL-10).
- Regulatory T-Cell (Treg) Dysfunction: Although the role of Tregs is complex, a failure of their suppressive function is implicated in irAE pathogenesis. A decreased ratio of Tregs to effector T cells can create a permissive environment for autoimmunity [79]. However, some studies suggest that CTLA-4 blockade may paradoxically inhibit Treg function within tumors, an effect that might also occur in healthy tissues [81].
- Tissue-Resident Memory T (Trm) Cells: Trm cells persist in non-lymphoid organs and accumulate in tissues affected by irAEs. Upon ICI administration, these cells exhibit a hyperactivated phenotype, producing proinflammatory cytokines and recruiting additional immune cells, thereby contributing to local tissue damage [79].
Humoral and Innate Immune Mechanisms
While T cells are central, B cells and the innate immune system also contribute significantly.
- Autoantibody Production: B cell activation and the production of autoantibodies are observed in a subset of patients experiencing irAEs. Pre-existing or newly emerging autoantibodies have been detected in patients who develop conditions such as thyroid dysfunction, myasthenia gravis, and skin toxicities [80] [81]. Their direct pathogenic role versus being a bystander phenomenon is still under investigation.
- Cytokine Release Dysregulation: A "cytokine storm" characterized by elevated levels of inflammatory mediators including TNF-α, IL-6, IL-17, and interferons is a feature of severe irAEs [80] [81]. This widespread inflammation can cause systemic symptoms and organ damage.
- Innate Immune Cell Engagement: Cells of the innate immune system, such as macrophages and myeloid-derived suppressor cells (MDSCs), contribute to the inflammatory milieu of the tumor microenvironment (TME) and, potentially, in tissues affected by irAEs. Their activation can further promote tissue infiltration and injury [6].
Host and Environmental Predisposing Factors
Several non-immune factors influence an individual's risk of developing irAEs.
- Genetic Predisposition: Certain human leukocyte antigen (HLA) haplotypes are associated with an increased risk for specific irAEs, mirroring findings in classic autoimmune diseases [80].
- Gut Microbiome: The composition of the gut microbiota has been shown to modulate the immune system and influence both ICI efficacy and the risk of toxicities, particularly colitis. A more diverse microbiome may be protective [80] [81].
- Tumor-Intrinsic and Environmental Factors: The tumor type and its associated TME can shape the irAE profile. Shared antigens between tumors and healthy tissues may predispose to organ-specific toxicity. External factors like prior infections (e.g., Hepatitis B) and lifestyle may also play a role [80] [82].
Table 1: Core Pathophysiological Mechanisms of irAEs
| Mechanistic Category | Key Effectors | Proposed Role in irAEs |
|---|---|---|
| T-Cell Dysregulation | Autoreactive CD8+ T cells, Th1/Th17 cells, Tregs, Trm cells | Direct cellular cytotoxicity, pro-inflammatory cytokine production, loss of immune suppression, localized tissue inflammation. |
| Humoral Immunity | Autoantibodies, Plasma B cells | Organ-specific opsonization and complement activation (e.g., in pemphigoid, thyroiditis). |
| Innate Immunity & Cytokines | Macrophages, MDSCs, TNF-α, IL-6, IL-17, IFN-γ | Promotion of a pro-inflammatory tissue environment, systemic inflammation, and organ damage. |
| Host Factors | HLA genotype, Gut microbiota, Preexisting autoimmunity | Genetic susceptibility, modulation of systemic immune tone, and baseline risk elevation. |
The following diagram summarizes the key pathways involved in the pathogenesis of immune-related adverse events:
Organ-Specific Clinical Manifestations and Incidence
irAEs can affect virtually any organ system, with varying frequency, timing, and severity. The onset can be acute, within weeks of treatment initiation, or delayed, occurring months after ICI cessation [80]. The profile of organ involvement is influenced by the class of ICI used.
Incidence and Severity by ICI Class
Table 2: Incidence of irAEs by ICI Class and Select Organ Systems [80] [69] [81]
| Organ System | Anti-CTLA-4 | Anti-PD-1/PD-L1 | Combination ICI (CTLA-4 + PD-1) | Common Manifestations |
|---|---|---|---|---|
| Any irAE | Up to 60-96% (G≥3: 10-30%) [79] | 5-20% (G≥3: ~10%) [80] | >50% (G≥3) [80] | - |
| Dermatologic | Very Common (Rash, Pruritus) | Common (Rash, Vitiligo) | Very Common | Maculopapular rash, pruritus, vitiligo (especially in melanoma) |
| Gastrointestinal | Very Common (Colitis) | Less Common | Very Common (Increased Severity) | Diarrhea, colitis |
| Hepatic | Common (Hepatitis) | Less Common | Common | Hepatitis, elevated transaminases |
| Endocrine | Common (Hypophysitis) | Common (Thyroiditis) | Common | Thyroid dysfunction, hypophysitis, adrenal insufficiency |
| Pulmonary | Less Common | Common (Pneumonitis) | Common | Pneumonitis |
| Musculoskeletal | Common | Common | Common | Arthralgia, myalgia, inflammatory arthritis |
| Neurological | Rare | Rare | Rare | Myasthenia gravis, neuropathy, encephalitis |
| Cardiac | Rare | Rare | Rare | Myocarditis (High Fatality) |
| Renal | Rare | Rare | Rare | Nephritis |
Characteristic Organ-Specific Pathophysiology
- Colitis (Common with CTLA-4 blockade): Driven by the proliferation of tissue-resident memory T cells and microbiota-dependent activation of CD4+ T cells. Histopathology reveals robust CD4+ and CD8+ T cell infiltrates in the colonic mucosa [79] [82].
- Pneumonitis (Common with PD-1/PD-L1 blockade): May involve the activation of T cells and B cells, with the production of autoantibodies (e.g., anti-CD74). The lung tissue shows T-cell infiltrates, and the severity can range from focal to diffuse alveolar damage [79] [82].
- Myocarditis (Rare but High Mortality): Characterized by T-cell infiltration into cardiac muscle, including clones specific for cardiac antigens like α-myosin. This is often accompanied by a cytokine-driven expansion of inflammatory macrophages [79] [82].
- Endocrinopathies (e.g., Thyroiditis, Hypophysitis): Involve T-cell infiltration into the glandular tissue (thyroid, pituitary), leading to destructive inflammation. Autoantibodies (e.g., anti-TPO, anti-ACTH) may also be present [80] [81].
- Dermatologic Toxicities: Include maculopapular rash and vitiligo, the latter associated with a favorable antitumor response in melanoma. Vitiligo results from T-cell targeting of melanocyte antigens shared by the tumor [79] [81].
Research Methodologies and Biomarker Discovery
Advancing the management of irAEs requires robust experimental models and the identification of predictive biomarkers to stratify patient risk.
Key Experimental Protocols
Research into irAE mechanisms relies on a multi-faceted approach integrating clinical data with preclinical models.
- Human Peripheral Blood Immune Profiling: Longitudinal blood collection from ICI-treated patients allows for high-dimensional analysis of immune cells using flow and mass cytometry. This protocol identifies dynamic changes in T-cell subsets (e.g., activated HLA-DR+ T cells, Tregs) and inflammatory cytokines that correlate with irAE development [79] [82].
- Protocol Summary: Collect peripheral blood mononuclear cells (PBMCs) at baseline and serial timepoints post-ICI initiation. Analyze using multi-parameter cytometry panels for activation/memory markers and multiplex cytokine assays. Correlate immune signatures with clinical irAE onset and severity.
- T-Cell Receptor (TCR) Repertoire Sequencing: TCR sequencing of peripheral blood or affected tissues assesses the clonality and diversity of the T-cell response. Reduced TCR diversity post-ICI has been linked to severe irAEs, suggesting the expansion of dominant autoreactive clones [79].
- Histopathological Analysis of Affected Tissues: Biopsy of irAE-affected organs (e.g., skin, colon, liver) remains a diagnostic gold standard. Immunohistochemistry and immunofluorescence are used to characterize infiltrating immune cells (CD4+, CD8+, Tregs, macrophages) and assess tissue architecture destruction [79].
- Preclinical Murine Models: Genetically engineered or adoptive T-cell transfer mouse models are used to study organ-specific irAEs, such as myocarditis and colitis. These models allow for controlled investigation of specific immune pathways and testing of prophylactic or therapeutic interventions [81].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents and Resources for irAE Research
| Research Tool | Primary Function / Application | Specific Examples / Targets |
|---|---|---|
| Flow Cytometry Panels | High-dimensional immunophenotyping of peripheral blood and tissue infiltrates | Antibodies against CD3, CD4, CD8, CD45RO, CCR7, HLA-DR, FoxP3, PD-1, CTLA-4 |
| Cytokine Assays | Quantification of soluble inflammatory mediators in serum/plasma | Multiplex ELISA for TNF-α, IL-6, IL-17, IL-10, IFN-γ |
| TCR Sequencing Kits | Analysis of T-cell clonality and diversity | ImmunoSEQ, SMARTer TCR profiling |
| Autoantibody Arrays | Discovery and validation of autoantibody signatures | Platforms screening for anti-TPO, anti-ACTH, anti-nuclear antibodies (ANA) |
| Multiplex Immunofluorescence | Spatial analysis of immune cells in the tissue microenvironment | Antibody panels for simultaneous detection of T cells (CD3), macrophages (CD68), and checkpoint molecules (PD-L1) |
| Animal Models | In vivo mechanistic studies and therapeutic testing | PD-1 knockout mice, humanized mouse models for ICI studies |
The following diagram illustrates a typical experimental workflow for profiling T-cell responses in irAE research:
The spectrum of immune-related adverse events is an intrinsic consequence of unleashing the immune system against cancer. The pathophysiological framework is built upon T-cell dysregulation but is significantly modulated by humoral immunity, inflammatory cytokines, and individual patient factors. The clinical manifestations are diverse, with incidence and severity profiles that are distinctly shaped by the specific immune checkpoint inhibitor class. Ongoing research efforts are critically focused on elucidating the precise molecular and cellular mechanisms that distinguish antitumor immunity from off-target autoimmunity. The development of predictive biomarkers and targeted management strategies that spare antitumor efficacy represents a paramount goal in the field. A deep understanding of irAE pathophysiology is therefore not merely a safety imperative but is also fundamental to unlocking the full therapeutic potential of cancer immunotherapy.
The advent of cancer immunotherapies, particularly Immune Checkpoint Inhibitors (ICIs) and Chimeric Antigen Receptor (CAR) T-cell therapy, has revolutionized oncology practice. While these modalities harness the immune system to achieve remarkable antitumor responses, they are accompanied by distinct and potentially severe cardiovascular toxicities. This whitepaper, framed within a broader thesis on mechanisms of antitumor activity and toxicity in immunotherapy research, provides an in-depth examination of ICI-induced myocarditis and CAR T-cell-associated Cytokine Release Syndrome (CRS). Understanding the pathophysiology, clinical presentation, and underlying mechanisms of these adverse events is paramount for researchers and drug development professionals aiming to enhance the therapeutic index of immunotherapeutic agents.
ICI-Induced Myocarditis
Pathophysiology and Mechanisms
Immune checkpoint inhibitors, including anti-CTLA-4, anti-PD-1, and anti-PD-L1 monoclonal antibodies, function by blocking inhibitory pathways to augment T-cell-mediated anti-tumor immunity. This disruption of immune homeostasis can lead to loss of self-tolerance and the development of immune-related adverse events (irAEs), with myocarditis being one of the most fatal [83] [84].
The pathogenesis of ICI-myocarditis is primarily driven by aberrant T-cell activation. The current model suggests that self-reactive cardiac T cells, which escape central tolerance due to incomplete representation of cardiac antigens in the thymus, become activated upon ICI administration [83] [84]. This process involves several key steps:
- T-Cell Activation and Clonal Expansion: In lymphoid tissues, ICIs block inhibitory signals (e.g., CTLA-4 binding to CD80/86), allowing for potent co-stimulation via CD28. This promotes the activation and proliferation of self-reactive T-cell clones, including those targeting cardiac antigens [83] [85].
- Loss of Peripheral Tolerance: In peripheral tissues, the PD-1/PD-L1 axis normally maintains tolerance by inhibiting T-cell effector functions. ICI blockade of this pathway removes this critical "brake," enabling self-reactive T cells to target myocardium [85] [86]. Furthermore, dysfunction of regulatory T cells (Tregs), which normally suppress autoimmune responses, exacerbates this loss of tolerance [83] [84].
- Myocardial Infiltration and Injury: Activated CD8+ and CD4+ T cells infiltrate the myocardium, recognizing specific antigens via T-cell receptor (TCR) engagement. Proposed mechanisms for this targeting include molecular mimicry (cross-reactivity between tumor and cardiac antigens) and direct recognition of cardiac-specific antigens like α-myosin [84] [86]. This leads to cardiomyocyte injury through direct cytolysis and cytokine release.
- Role of Macrophages and Cytokines: Activated T cells secrete cytokines, particularly IFN-γ, which induces the expansion and recruitment of pro-inflammatory macrophages (e.g., CXCL9+/CXCL10+ macrophages). These macrophages amplify the inflammatory cascade, contributing to further tissue damage [83] [86].
The following diagram illustrates the core mechanisms of ICI-induced myocarditis, showing how checkpoint inhibition leads to T-cell-mediated myocardial injury.
Clinical Presentation and Epidemiology
ICI-myocarditis presents unique clinical characteristics that distinguish it from other forms of myocarditis. Key epidemiological and clinical features are summarized in the table below.
Table 1: Clinical and Epidemiological Profile of ICI-Induced Myocarditis
| Feature | Details | References |
|---|---|---|
| Incidence | 0.06% - 1.14% of patients; higher with combination therapy (up to 1.14%) | [84] [86] [87] |
| Mortality Rate | High fatality rate, reported between 24% - 50% | [83] [84] [86] |
| Time to Onset | Median onset ~34 days (21-75 days) after initial ICI dose; majority within 3 months | [83] [86] [87] |
| Common Malignancies | Melanoma, lung cancer, renal cell carcinoma | [86] |
| Key Demographics | Male predominance; mean age 62-65 years | [86] |
| Clinical Presentation | Ranges from asymptomatic biomarker elevation to fulminant heart failure, cardiogenic shock, lethal arrhythmias | [83] [86] |
| Diagnostic Findings | Elevated troponin and NT-proBNP; LV dysfunction on echo; non-ischemic late gadolinium enhancement on cardiac MRI | [86] |
Experimental Models and Research Methodologies
Preclinical models are essential for elucidating the mechanisms of ICI-myocarditis. The following protocol outlines key methodologies used in this research.
Protocol 1: Evaluating ICI-Induced Myocarditis in a Preclinical Model
- Objective: To recapitulate and investigate the pathophysiology of ICI-induced myocarditis in a murine model.
- Materials:
- Animal Model: C57BL/6 mice or other immunocompetent strains. CTLA-4 knockout mice (which develop fatal autoimmunity) are also used for mechanistic studies [85].
- Reagents: Anti-murine CTLA-4 and/or PD-1 monoclonal antibodies (e.g., clone 9D9 for CTLA-4, clone RMP1-14 for PD-1), administered via intraperitoneal injection [83] [84].
- Adjuvants: May be co-administered with cardiac-specific antigens (e.g., α-myosin peptide) to break tolerance and enhance model robustness [84].
- Experimental Workflow:
- Treatment: Mice are treated with ICI (monotherapy or combination) or an isotype control antibody at specified doses and schedules.
- Functional & Terminal Assessment: Mice are monitored for signs of distress. Functional cardiac assessment via echocardiography is performed at baseline and endpoint.
- Sample Collection: At endpoint, blood and heart tissue are collected for analysis.
- Key Analytical Techniques:
- Histopathology and Immunostaining: Heart tissue is sectioned and stained with:
- Flow Cytometry: Single-cell suspensions from heart tissue are analyzed for immune cell composition (T cells, Tregs, macrophages) and activation status (e.g., PD-1, CTLA-4 expression) [83] [84].
- Cytokine/Chemokine Profiling: Serum or heart homogenates are analyzed using ELISA or multiplex assays (e.g., Luminex) for levels of IFN-γ, IL-6, TNF-α, CXCL9, CXCL10 [83].
- ELISpot Assay: To detect T cells secreting IFN-γ in response to cardiac-specific antigens, confirming antigen-specific immune responses [84].
CAR T-Cell Associated Cytokine Release Syndrome (CRS)
Pathophysiology and Mechanisms
CRS is the most common and significant toxicity associated with CAR T-cell therapy. It is a systemic inflammatory response initiated by the engagement of CAR T-cells with their target antigen on tumor cells, leading to massive T-cell activation and proliferation [88] [89].
The immunopathogenesis of CRS involves a complex cascade:
- CAR T-Cell Activation: Upon infusion, CAR T-cells recognize and engage tumor-associated antigens (e.g., CD19, BCMA), leading to their activation and proliferation.
- Cytokine Release by T-cells: Activated CAR T-cells release pro-inflammatory cytokines such as GM-CSF, IFN-γ, and IL-2, which act as upstream initiators of the cascade [88] [89].
- Recruitment and Activation of Myeloid Cells: IFN-γ and other factors activate bystander myeloid cells, particularly monocytes and macrophages. This is a critical amplification step.
- Cytokine Storm by Myeloid Cells: Activated monocytes and macrophages become the primary source of the key pathologic cytokines, most notably IL-6, as well as IL-1β, TNF-α, and NO [88] [89]. IL-6 signaling through its receptor is a central driver of CRS symptoms like fever, hypotension, and tachycardia.
- Cardiovascular Manifestations: The high levels of inflammatory cytokines cause widespread endothelial activation, leading to increased vascular permeability (capillary leak), hypotension, and reduced cardiac contractility. This can manifest as tachycardia, left ventricular dysfunction, troponin elevation, and cardiogenic shock [88] [90].
The following diagram illustrates the sequential immune cell activation and cytokine cascade in CAR T-cell-associated CRS.
Clinical Presentation and Grading
CRS presents with a spectrum of symptoms and can affect multiple organ systems. Its cardiovascular manifestations are of particular concern. The American Society for Transplantation and Cellular Therapy (ASTCT) consensus grading system is the standard for assessing CRS severity, which directly guides therapeutic intervention [88] [89].
Table 2: ASTCT Consensus Grading for CRS and Associated Cardiovascular Features
| CRS Grade | Fever | Hypotension | Hypoxia | Cardiovascular Manifestations |
|---|---|---|---|---|
| Grade 1 | Temperature ≥38°C | None | None | Sinus tachycardia may be present. |
| Grade 2 | Temperature ≥38°C | Not requiring vasopressors | Requiring low-flow nasal cannula ≤6 L/min | Tachycardia; may require intravenous fluids for hypotension. |
| Grade 3 | Temperature ≥38°C | Requiring a vasopressor (with or without vasopressin) | Requiring high-flow nasal cannula >6 L/min, facemask, non-rebreather, or Venturi mask | Tachycardia; hypotension requiring one vasopressor; signs of cardiac strain. |
| Grade 4 | Temperature ≥38°C | Requiring multiple vasopressors (excluding vasopressin) | Requiring positive pressure (CPAP, BiPAP, mechanical ventilation) | Life-threatening arrhythmias, severe left ventricular dysfunction, cardiogenic shock, cardiac arrest. |
The incidence of cardiotoxicity is strongly correlated with higher-grade CRS (Grade ≥2) [88] [90]. Reported cardiovascular events include arrhythmias (incidence 4-38%), left ventricular systolic dysfunction (reported up to 8.7% in meta-analyses), and cardiac death (0.6%) [90]. The median time to onset of CRS is typically within the first 1-2 weeks after CAR T-cell infusion [89].
Experimental Models and Research Methodologies
Research into CRS and its cardiotoxicity utilizes both in vitro and in vivo models to dissect the cytokine cascade and test mitigation strategies.
Protocol 2: Investigating CRS and Cardiotoxicity Using an In Vitro Coculture Model
- Objective: To model the initial immune cell interactions in CRS and screen for cardioprotective agents.
- Materials:
- Immune Cells: Primary human CAR T-cells (e.g., anti-CD19 or anti-BCMA).
- Target Cells: CD19+ or BCMA+ tumor cell lines (e.g., NALM-6 for ALL).
- Cardiac Cells: Human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs).
- Reagents: Cytokine measurement kits (ELISA/Luminex), neutralizing antibodies (e.g., anti-IL-6R, anti-IL-1R), candidate small-molecule inhibitors.
- Experimental Workflow:
- Setup of Coculture Systems:
- Group 1 (CRS Model): CAR T-cells + Target Tumor Cells.
- Group 2 (Cardiotoxicity Readout): (CAR T-cells + Target Tumor Cells) co-cultured with iPSC-CMs in a transwell system, or treated with conditioned media from Group 1.
- Appropriate Controls: Non-target tumor cells, untransduced T cells.
- Intervention: Addition of neutralizing antibodies or inhibitors to specific groups at the time of coculture.
- Sample Collection: Supernatants are collected at 24, 48, and 72 hours for cytokine analysis. Cells are harvested for flow cytometry or functional assays.
- Setup of Coculture Systems:
- Key Analytical Techniques:
- Cytokine Profiling: Quantification of IL-6, IFN-γ, IL-2, GM-CSF, IL-1β, TNF-α in supernatants using multiplex immunoassays [88] [89].
- Cardiomyocyte Functional Assessment: If using iPSC-CMs, analyze:
- Viability: Using assays like MTT or CellTiter-Glo.
- Contractility: Using real-time live-cell imaging or microelectrode array (MEA) to detect arrhythmic beating or changes in beat rate and force [90].
- Flow Cytometry: To assess CAR T-cell and myeloid cell activation, proliferation, and phenotype.
The Scientist's Toolkit: Key Research Reagents
The following table compiles essential reagents and tools for investigating the mechanisms of these immunotherapy-associated cardiovascular toxicities.
Table 3: Research Reagent Solutions for Investigating Immunotherapy Cardiotoxicity
| Reagent / Tool | Function / Application | Specific Examples / Targets |
|---|---|---|
| Anti-Mouse ICIs | To establish preclinical models of ICI-myocarditis by blocking immune checkpoints. | Anti-mouse CTLA-4 (clone 9D9), Anti-mouse PD-1 (clone RMP1-14), Anti-mouse PD-L1 [83] [84] |
| CAR T-cell Constructs | To study CRS mechanisms; different costimulatory domains influence toxicity profiles. | CD28-based (rapid, potent activation) vs. 4-1BB-based (persistent, potentially milder CRS) CARs [50] [89] |
| Neutralizing Antibodies & Inhibitors | To dissect cytokine pathways and test therapeutic interventions in vitro and in vivo. | Tocilizumab (anti-IL-6R), Anakinra (IL-1R antagonist), anti-IFN-γ, anti-GM-CSF, Metoprolol (inhibits IL-6 translation) [88] [89] |
| Flow Cytometry Antibodies | To characterize immune cell infiltration and activation status in heart tissue or blood. | Anti-mouse/human: CD3, CD4, CD8, CD45, FoxP3 (Tregs), F4/80/CD11b (macrophages), PD-1, CTLA-4, CXCR3, CCR5 [83] [84] |
| Cytokine Detection Assays | To quantify cytokine levels in serum, plasma, or tissue culture supernatants. | ELISA kits, Multiplex Luminex arrays for IL-6, IFN-γ, IL-1β, TNF-α, GM-CSF, CXCL9, CXCL10 [83] [88] [89] |
| iPSC-Derived Cardiomyocytes | As a human-relevant in vitro model to study direct cardiotoxic effects of cytokines or CAR T-cell products. | Used in coculture or conditioned media experiments to assess viability, contractility, and electrophysiology [90] |
ICI-induced myocarditis and CAR T-cell-associated CRS represent two distinct paradigms of cardiovascular toxicity in immuno-oncology. ICI-myocarditis is primarily a T-cell-driven autoimmune process targeting the heart, characterized by a high mortality rate. In contrast, CAR T-cell CRS is a systemic inflammatory syndrome driven by a cascade of cytokines from both T-cells and myeloid cells, with cardiovascular effects being a major consequence of the cytokine storm. Both toxicities stem from the intended mechanism of action of these powerful therapies—the potent activation of the immune system—highlighting the delicate balance between efficacy and toxicity. Future research must focus on elucidating precise cellular and molecular triggers, validating predictive biomarkers, and developing targeted mitigation strategies that preserve antitumor efficacy while protecting cardiovascular health. A deep mechanistic understanding of these toxicities is not merely a safety concern but is integral to the rational design of next-generation, safer immunotherapies.
The advent of immune checkpoint inhibitors (ICIs) has fundamentally transformed the oncology landscape, providing unprecedented survival benefits for patients with various advanced malignancies. However, the disruption of immune homeostasis required for antitumor activity invariably leads to a spectrum of inflammatory toxicities known as immune-related adverse events (irAEs) [80] [45]. These events represent a significant challenge in clinical practice, often necessitating treatment modification and potentially compromising long-term outcomes. irAEs can affect nearly any organ system, with dermatological manifestations being among the most frequently reported [80] [91]. Understanding the clinical presentation and underlying mechanisms of both dermatological and systemic irAEs is crucial for optimizing the risk-benefit ratio of cancer immunotherapy.
The pathogenesis of irAEs involves complex interactions between aberrant T-cell activation, autoantibody production, and inflammatory cytokine release [80]. These mechanisms share similarities with, yet are distinct from, spontaneous autoimmune diseases. The incidence and severity of irAEs vary considerably based on the class of ICI administered, with combination therapy portending the highest risk [80] [69]. This review systematically examines the clinical manifestations, epidemiological characteristics, and molecular mechanisms underpinning dermatological and systemic irAEs, framing these events within the broader context of antitumor immunity and toxicity in immunotherapy research.
Clinical Presentation and Epidemiology of irAEs
Dermatological irAEs
Dermatological toxicities represent the most common class of irAEs, affecting approximately 20-50% of patients receiving ICI therapy [80] [91]. The clinical spectrum ranges from mild, self-limited maculopapular rash to severe, life-threatening conditions such as toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS). Morbilliform rash typically presents within the first few weeks of treatment initiation, while immunobullous disorders and pruritus may develop later in the treatment course [80] [45]. These manifestations often serve as early indicators of immune system activation and may correlate with the development of irAEs in other organ systems.
The distribution of dermatological irAEs differs between ICI classes. PD-1/PD-L1 inhibitors are more frequently associated with lichenoid reactions and vitiligo, particularly in melanoma patients, while CTLA-4 inhibitors more commonly cause pruritus and maculopapular eruptions [91]. Combination therapy amplifies both the incidence and severity of cutaneous toxicities, with grade 3-4 events occurring in up to 15% of patients [80]. Vitiligo, while cosmetically concerning for some patients, has been associated with improved treatment response in melanoma, suggesting shared antigenicity between melanocytes and tumor cells [45].
Systemic irAEs
Systemic irAEs encompass a broad spectrum of toxicities affecting multiple organ systems. Gastrointestinal irAEs, particularly colitis, represent some of the most frequent and clinically significant toxicities, especially with CTLA-4 inhibitors [80] [45]. Endocrine toxicities including thyroid dysfunction, hypophysitis, and adrenal insufficiency often present with nonspecific symptoms but can become life-threatening if unrecognized. Pulmonary irAEs (pneumonitis), while less common, carry substantial mortality risk, particularly with PD-1/PD-L1 inhibitors [80]. Other potentially severe irAEs affect the hepatic, neurological, cardiovascular, and renal systems, with myocarditis representing one of the most fatal toxicities despite its relative rarity [80] [92].
Table 1: Incidence Patterns of Selected irAEs by ICI Class
| Organ System | PD-(L)1 Inhibitors | CTLA-4 Inhibitors | Combination Therapy |
|---|---|---|---|
| Skin | 20-40% [91] | 40-50% [91] | ~55% [80] |
| Gastrointestinal | 10-20% [45] | 30-40% [45] | ~50% [80] |
| Endocrine | 5-15% (especially thyroid) [45] | 5-10% (especially hypophysitis) [45] | 15-25% [80] |
| Hepatic | 2-10% [80] | 10-20% [80] | 25-30% [80] |
| Pulmonary | 3-5% [80] | 1-3% [80] | 7-15% [80] |
The timing of irAE onset follows distinct patterns based on the organ system involved and the class of ICI administered. Dermatologic and gastrointestinal toxicities typically present early, within weeks of treatment initiation, while endocrine and neurologic irAEs may manifest months later [80]. Notably, irAEs can occasionally present after treatment discontinuation, so-called delayed-onset irAEs, creating diagnostic challenges [80]. Recent evidence indicates that even a single dose of anti-PD-(L)1 therapy can trigger severe irAEs in approximately 2% of patients, with over 40% of these events being severe or fatal [92].
Table 2: Timing and Severity Patterns of Selected irAEs
| Organ System | Median Time to Onset | Common Grade 3+ Proportion | Fatality Rate |
|---|---|---|---|
| Dermatologic | 2-4 weeks [80] | 1-3% [80] | <0.1% [80] |
| Gastrointestinal | 5-10 weeks [80] | 5-15% [80] [45] | 0.5-1% [80] |
| Hepatic | 6-12 weeks [80] | 2-10% [80] | 0.5-1% [80] |
| Pulmonary | 2-6 months [80] | 2-5% [80] | 10-20% [80] |
| Cardiac | 1-3 months [80] | >50% [80] | 30-50% [80] [92] |
Risk factors for irAE development include patient-specific characteristics such as younger age, female sex, and pre-existing autoimmune conditions [69]. Treatment-related factors include ICI class, with combination therapy carrying the highest risk, and specific cancer types may predispose to certain irAEs, possibly reflecting shared antigen expression between tumors and healthy tissues [80]. Recent real-world evidence from the RADIOHEAD cohort demonstrates that patients who develop any irAE exhibit significantly improved real-world overall survival, suggesting overlapping mechanisms between antitumor immunity and autoimmunity [93].
Underlying Mechanisms of irAEs
Fundamental Immunological Pathways
The pathogenesis of irAEs stems from the fundamental mechanism of action of ICIs: the disruption of physiological immune checkpoints that maintain self-tolerance. CTLA-4 and PD-1, the two most extensively characterized immune checkpoints, play non-redundant roles in immune regulation [45] [91]. CTLA-4, expressed primarily on T cells, functions as a decoy receptor for the costimulatory proteins B7-1 and B7-2 on antigen-presenting cells (APCs), effectively outcompeting the activating receptor CD28 [91] [8]. This interaction occurs predominantly in lymphoid tissues during the early phase of T-cell activation. PD-1, in contrast, exerts its inhibitory effects later in the immune response and primarily in peripheral tissues, attenuating T-cell receptor (TCR) signaling upon binding to its ligands PD-L1 and PD-L2 [45] [91].
The differential expression patterns and mechanisms of CTLA-4 and PD-1 help explain their distinct irAE profiles. CTLA-4 deficiency in mice results in profound, fatal multi-organ lymphoproliferation, underscoring its critical role in maintaining early immune homeostasis [45]. PD-1 deficiency, while less dramatic, predisposes to tissue-specific inflammatory conditions, particularly in the context of other immune perturbations [45]. In humans, CTLA-4 inhibition more frequently causes colitis and hypophysitis, while PD-1/PD-L1 blockade is more associated with thyroiditis, pneumonitis, and dermatologic conditions such as vitiligo [45] [91].
Diagram 1: Immune Checkpoint Regulation Pathways. This diagram illustrates the fundamental mechanisms of CTLA-4 and PD-1/PD-L1 pathways in regulating T-cell activation and effector function. CTLA-4 competitively inhibits CD28 costimulation during T-cell priming in lymphoid organs, while PD-1 suppresses T-cell receptor signaling in peripheral tissues. ICI therapy disrupts these regulatory checkpoints, potentially leading to both antitumor immunity and irAEs.
Cellular and Molecular Mechanisms of irAEs
The pathophysiology of irAEs involves multiple interconnected mechanisms that collectively break immunological tolerance. First, aberrant activation of self-reactive T cells represents a central pathway. Pre-existing autoreactive T cells, which normally remain quiescent due to checkpoint-mediated suppression, become activated upon ICI administration [80] [45]. These cells can recognize self-antigens shared between tumors and healthy tissues, exemplified by melanocyte antigens in melanoma patients developing vitiligo [45]. Tissue-specific infiltration of activated CD8+ T cells has been documented in various irAEs, including bile duct epithelium targeting in hepatitis and cardiac myosin recognition in myocarditis [80].
Second, autoantibody-mediated damage contributes to certain irAEs. Elevated levels of autoantibodies against tissue-specific antigens (e.g., anti-thyroid peroxidase in thyroiditis, anti-ACTH in hypophysitis) and systemic autoantibodies (e.g., anti-nuclear antibodies) have been detected in patients receiving ICIs [80] [94]. However, the pathogenic role of these autoantibodies remains incompletely defined, as they may serve as biomarkers rather than direct mediators of tissue damage in some cases [94].
Third, innate immune dysregulation and inflammatory cytokine release amplify tissue injury in irAEs. Elevated levels of IL-6, IL-17, TNF-α, and type I interferons have been observed in patients with severe irAEs, creating a pro-inflammatory milieu that promotes immune cell recruitment and tissue damage [80]. These cytokines may derive from both innate immune cells and activated T cells, establishing positive feedback loops that sustain inflammation [80] [45].
Additional factors shaping irAE development include host genetics (e.g., HLA haplotypes), commensal microbiota composition, and organ-specific immune niches [80] [45]. The gut microbiome, in particular, has emerged as a key modulator of both ICI efficacy and toxicity, with specific microbial signatures associated with irAE risk [80]. Barrier organs such as the skin, gastrointestinal tract, and lungs may be particularly susceptible to irAEs due to their continuous exposure to microbial and environmental antigens normally kept in check by immune checkpoint pathways [45].
Diagram 2: Multifactorial Pathogenesis of Immune-Related Adverse Events. This diagram summarizes the key mechanisms contributing to irAE development following ICI therapy, including self-reactive T-cell activation, autoantibody production, and innate immune dysregulation, along with host and environmental factors that modify irAE risk.
Experimental Models and Research Methodologies
Preclinical Models for irAE Investigation
The study of irAE mechanisms has been hampered by the limited availability of animal models that faithfully recapitulate the human condition [45]. Conventional mouse strains typically develop minimal toxicities when treated with ICIs, unlike humans. However, several innovative approaches have emerged to bridge this translational gap. PD-1 deficient, CTLA-4 heterozygous mice develop some autoimmune manifestations, including myocarditis, though they lack the broader spectrum of irAEs seen in patients [45]. Humanized mouse models, created by engrafting human hematopoietic cells into immunodeficient mice, can develop inflammatory toxicities after ICI treatment, though these may overlap with graft-versus-host disease [45].
In vitro systems using human peripheral blood mononuclear cells (PBMCs) or tissue-specific immune cells have provided insights into T-cell reactivity patterns following checkpoint blockade. Co-culture models incorporating patient-derived tumor cells and autologous immune cells can help identify shared antigens potentially driving both antitumor responses and irAEs [45]. Organoid systems, particularly for the gastrointestinal tract, are being developed to study tissue-specific immune interactions and test potential therapeutic interventions for irAEs [45].
Analytical Approaches for irAE Research
Advanced molecular profiling techniques have enabled detailed characterization of immune responses in patients experiencing irAEs. High-dimensional flow cytometry and mass cytometry (CyTOF) allow comprehensive immunophenotyping of peripheral blood and tissue samples, revealing dynamic changes in immune cell populations associated with irAE development [94]. Single-cell RNA sequencing (scRNA-seq) can identify transcriptomic signatures predictive of irAE risk and elucidate cell-type-specific pathways activated during toxicities [94].
Multiplex immunofluorescence and spatial transcriptomics enable preservation of tissue architecture while characterizing immune cell infiltration and activation states in irAE-affected organs [94]. These approaches have revealed distinct cellular neighborhoods in tissues affected by irAEs, including specific T-cell and macrophage subsets that may drive pathology [95].
Serological profiling through autoantibody arrays and proteomic analyses has identified potential biomarkers for irAE risk and severity [94]. Longitudinal sampling in cohorts such as RADIOHEAD has facilitated the discovery of dynamic changes in cytokine profiles and immune cell populations preceding clinical irAE manifestation [93].
Table 3: Essential Research Reagents and Methodologies for irAE Investigation
| Category | Specific Reagents/Assays | Research Applications |
|---|---|---|
| Immune Profiling | Anti-human CD3, CD4, CD8, CD45RO, PD-1, CTLA-4 antibodies [95] | Flow cytometry, CyTOF, and immunohistochemistry for immune cell characterization |
| Cytokine Analysis | Multiplex cytokine panels (IL-6, IL-17, TNF-α, IFN-γ) [80] [94] | Measuring inflammatory mediators in serum and tissue samples |
| Autoantibody Detection | Autoantibody arrays, ELISA kits for specific autoantibodies [80] [94] | Identifying humoral autoimmunity associated with irAEs |
| Genetic Analysis | HLA genotyping, whole exome sequencing, TCR/BCR repertoire analysis [80] [94] | Assessing genetic predispositions and clonal immune responses |
| Microbiome Tools | 16S rRNA sequencing, metagenomic sequencing [80] [94] | Characterizing gut microbiota associations with irAE risk |
Diagram 3: Comprehensive Workflow for irAE Research. This diagram outlines an integrated approach to investigating irAE mechanisms, incorporating multi-modal sample collection, advanced analytical techniques, and validation models to identify pathogenic pathways and predictive biomarkers.
Dermatological and systemic irAEs represent significant challenges in the clinical application of cancer immunotherapy. These toxicities arise from the fundamental mechanisms of action of ICIs, which disrupt physiological immune checkpoints to unleash antitumor immunity but simultaneously compromise self-tolerance. The clinical spectrum of irAEs is broad, with distinct patterns based on the specific ICI class, treatment regimen, and patient characteristics. Understanding the complex immunological mechanisms underlying these events—including self-reactive T-cell activation, autoantibody production, and inflammatory cytokine release—provides crucial insights for developing more targeted management strategies.
Future research directions should focus on identifying robust predictive biomarkers for irAE risk, enabling better patient selection and monitoring strategies. The development of more physiologically relevant experimental models will facilitate deeper mechanistic studies and preclinical testing of novel therapeutic approaches. Furthermore, exploring the intriguing association between irAEs and treatment response may reveal fundamental insights into the shared pathways of antitumor immunity and autoimmunity. As immunotherapy continues to expand across cancer types and treatment settings, optimizing the balance between efficacy and toxicity remains a paramount concern for the field.
Mechanisms of Primary and Acquired Resistance to Immunotherapy
The advent of immune checkpoint inhibitors (ICIs) has fundamentally reshaped the therapeutic landscape for numerous malignancies, unlocking the potential for durable, long-term responses in conditions such as metastatic melanoma and unresectable hepatocellular carcinoma (uHCC) [62] [96]. Despite these successes, the efficacy of immunotherapy is frequently constrained by the development of resistance, a multifaceted phenomenon that poses a significant clinical challenge. Resistance is broadly categorized as either primary resistance (PR), where patients exhibit no initial response to treatment, or acquired resistance (AR), where disease progression occurs after an initial period of clinical benefit [97] [98]. A comprehensive understanding of the distinct and overlapping mechanisms underlying these resistance types is paramount for the development of novel strategies to overcome them and improve patient outcomes. This whitepaper delves into the core mechanisms of antitumor activity and the subsequent development of resistance, providing a technical guide for researchers and drug development professionals.
Defining Resistance and Its Clinical Impact
Clinical Definitions and Distinctions
The clinical definitions of PR and AR are operationalized through treatment response criteria. AR is formally defined as disease progression after achieving a complete response (CR), partial response (PR), or stable disease (SD) with a duration of 6 months or more. Conversely, PR is defined as progressive disease (PD) as the best response, or SD with a duration of less than 6 months [97]. Radiological progression is typically assessed using RECIST version 1.1 criteria [97].
Clinical Outcomes and Prognosis
The clinical distinction between PR and AR carries significant prognostic implications. A retrospective cohort study of patients with uHCC receiving ICI combination therapy revealed that patients with AR had superior general health, smaller tumors, less vessel invasion, and a markedly better prognosis compared to those with PR. The median overall survival (mOS) for patients with AR was 25.8 months, starkly contrasting with 8.63 months for patients with PR [97]. Furthermore, the patterns of progression differ; AR is less frequently associated with progression at multiple sites or the emergence of new lesions [97]. Notably, in patients with PR, the occurrence of new lesions is linked to decreased OS, whereas in AR, it is paradoxically associated with an increase in OS [97]. Critically, clinical evidence suggests that AR typically manifests within 2 years of initiating treatment [97].
Table 1: Clinical Characteristics of Primary vs. Acquired Resistance in uHCC (adapted from [97])
| Characteristic | Primary Resistance (PR) | Acquired Resistance (AR) |
|---|---|---|
| Definition | Progressive disease as best response, or stable disease < 6 months | Progression after CR, PR, or SD ≥ 6 months |
| Median Overall Survival | 8.63 months | 25.8 months |
| Tumor Burden | Larger tumors | Smaller tumors |
| Vessel Invasion | More frequent | Less frequent |
| Common Progression Pattern | Multiple lesions, new lesions | Less multifocal progression |
| Typical Onset | At initial treatment | Within 2 years of treatment start |
Fundamental Mechanisms of Resistance
The Cancer-Immunity (CI) Cycle provides a framework for understanding the multi-step process of antitumor immunity, wherein disruptions at any point can lead to resistance [98]. Resistance mechanisms can be classified as tumor-intrinsic (originating from the cancer cells themselves) or tumor-extrinsic (driven by the tumor microenvironment or other host factors).
Tumor-Intrinsic Resistance Mechanisms
Disrupted Antigen Presentation and Recognition
A critical tumor-intrinsic mechanism of resistance involves the disruption of antigen presentation, which renders tumor cells invisible to T-cell recognition.
- Lack of Neoantigens: Tumors with a low tumor mutational burden (TMB) and consequent low neoantigen load are poorly immunogenic and less sensitive to ICIs [98]. In AR, immune editing can select for tumor subclones that have lost immunogenic neoantigens [98].
- MHC-I Disruption: Loss-of-function mutations in genes critical to the antigen presentation machinery, such as B2M (Beta-2-microglobulin), are a common driver of resistance, preventing the surface expression of MHC-I complexes [96] [6]. Epigenetic downregulation of MHC-I expression and loss of MHC heterozygosity further contribute to this evasion strategy [96].
- Melanoma De-differentiation: In melanoma, a resistance program characterized by de-differentiation leads to the downregulation of melanocyte-specific wild-type differentiation antigens (e.g., MART-1/Melan-A, gp100). This process is often driven by tumor-intrinsic IFNγ signaling and the loss of key transcription factors like MITF and SOX10, making the tumors less visible to the immune system [96].
Dysregulated Intracellular Signaling
- Defective IFNγ Signaling: The IFNγ pathway is crucial for amplifying antitumor immunity by enhancing antigen presentation and recruiting immune cells. Loss-of-function mutations in genes within this pathway, such as JAK1 or JAK2, abrogate this signal and confer resistance to ICIs [96]. In contrast, some resistant melanomas exhibit constitutive intrinsic IFNγ signaling, which is associated with an immunosuppressive secretome and a de-differentiated state [96].
- Oncogenic Pathway Activation: Activation of signaling pathways like PI3K/AKT can lead to the upregulation of immune checkpoint molecules like PD-L1, contributing to an immunosuppressive niche [6]. Loss of the tumor suppressor PTEN is associated with immune cell exclusion and resistance, potentially through the creation of a non-T-cell-inflamed TME [96].
Tumor-Extrinsic Resistance Mechanisms
An Immunosuppressive Tumor Microenvironment (TME)
The TME plays a decisive role in fostering immune resistance through a variety of mechanisms.
- Recruitment of Immunosuppressive Cells: Tumors actively recruit regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), which inhibit effector T-cell function. Tregs suppress through the secretion of IL-10 and TGF-β and expression of CTLA-4, while MDSCs produce reactive oxygen species (ROS) and nitric oxide (NO), and deplete essential amino acids like arginine [6] [48].
- Immunosuppressive Soluble Factors: The TME is rich in cytokines such as TGF-β, IL-10, and VEGF, which directly inhibit T-cell and NK-cell activity and impede dendritic cell maturation [6].
- Metabolic Reprogramming: Tumors often undergo aerobic glycolysis, leading to an accumulation of lactic acid and the creation of an acidic TME. This low-pH environment directly inhibits the proliferation and cytotoxic function of T cells and NK cells [6]. Neutralizing the TME pH with bicarbonate or proton pump inhibitors has been shown to restore T-cell function and improve ICI efficacy in preclinical models [6]. Additionally, ammonia, a byproduct of glutaminolysis, can induce a unique form of T-cell death, further contributing to immune suppression [6].
Upregulation of Alternative Immune Checkpoints
Persistent immune pressure can lead to the adaptive overexpression of alternative immune checkpoint molecules beyond PD-1 and CTLA-4, such as LAG-3, TIM-3, and TIGIT [98] [96]. This represents a compensatory mechanism of immune inhibition that can drive resistance to first-line ICI regimens.
Table 2: Key Tumor-Intrinsic and Extrinsic Resistance Mechanisms
| Category | Specific Mechanism | Functional Consequence | Therapeutic Implications |
|---|---|---|---|
| Tumor-Intrinsic | Loss of neoantigens / Low TMB | Reduced immunogenicity; "immune desert" | Patient selection via TMB testing |
| Mutations in antigen presentation (e.g., B2M) | Failure of T-cell recognition | Restoration of MHC-I (e.g., HDAC inhibitors) | |
| De-differentiation (e.g., melanoma) | Loss of wild-type antigen targets | Combination therapies targeting de-differentiated state | |
| Defects in IFNγ signaling (JAK1/2 mutations) | Failure to amplify immune response | Stimulation of innate immunity (e.g., type I IFNs) | |
| Tumor-Extrinsic | Treg and MDSC infiltration | Direct suppression of effector T cells | Depleting Tregs; targeting MDSC recruitment |
| Acidic TME (lactic acid) | Impaired T/NK cell function and proliferation | Neutralizing pH (e.g., bicarbonate, CA-IX inhibitors) | |
| Upregulation of alternative checkpoints (LAG-3, TIM-3) | Reinhibition of T-cell activity | Combination ICI targeting multiple checkpoints | |
| Immunosuppressive cytokines (TGF-β, IL-10) | Inhibition of T-cell activation and DC function | Neutralizing antibodies; cytokine traps |
Experimental Models and Methodologies for Studying Resistance
Derivation and Analysis of Resistant Cell Lines
A powerful approach to dissect resistance mechanisms involves the generation and multi-omics profiling of short-term tumor cell lines derived from patients progressing on ICI therapy.
- Patient-Derived Cell Lines (PD1 PROGs): One study established 22 short-term melanoma cell lines ("PD1 PROGs") from 21 tumor biopsies collected from 18 patients at the time of progression on PD-1 inhibitors (alone or combined with CTLA-4 inhibition) [96].
- Functional Validation: These cell lines were subjected to genome, transcriptome, and high-dimensional flow cytometric profiling. Functional validation is critical. For instance, to confirm a hypothesized defect in IFNγ signaling, cells can be treated with recombinant IFNγ (e.g., 1000 U/ml for 24 hours) and assessed for STAT1 phosphorylation, and induction of MHC-I, MHC-II, and PD-L1 via flow cytometry. The transient reintroduction of a wild-type gene (e.g., JAK2) can be used to confirm its role in resistance [96].
Multiparametric Magnetic Resonance Imaging (mpMRI) for Response Assessment
Non-invasive imaging biomarkers are emerging as valuable tools for early response assessment and distinguishing pseudoprogression from true progression.
- Murine Melanoma Model: In a B16-F10 murine melanoma model, mpMRI was performed at baseline and five days after initiating immunotherapy with anti-PD-L1 and anti-CTLA-4 antibodies [99].
- Key Parameters: The protocol included:
- Tumor Volume: Measured from morphological sequences.
- Apparent Diffusion Coefficient (ADC): Calculated from Diffusion-Weighted Imaging (DWI), reflecting cellularity.
- Dynamic Contrast-Enhanced (DCE) MRI Metrics: Including plasma volume (PV) and plasma flow (PF), which inform on vascular permeability and perfusion [99].
- Ex Vivo Validation: A key strength of this methodology is the correlation of imaging findings with ex vivo immunohistochemistry (IHC) of the tumor validation cohort. IHC markers include:
- CD8+: For tumor-infiltrating lymphocytes (TILs).
- Ki-67: For cell proliferation.
- TUNEL: For apoptosis.
- CD31+: For microvascular density [99].
- Findings: The study found that a lower ADC value post-therapy, paired with increased CD8+ TILs on IHC, was suggestive of an early immunological response, whereas tumor volume changes alone were not discriminatory [99].
Diagram 1: Experimental Workflow for Profiling ICI Resistance
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Research Reagents for Investigating Immunotherapy Resistance
| Reagent / Assay | Primary Function / Target | Example Application in Resistance Research |
|---|---|---|
| Recombinant IFNγ | Stimulates JAK/STAT pathway; induces MHC and PD-L1 expression | Functional validation of IFNγ signaling integrity in resistant cell lines [96] |
| Phospho-STAT1 Antibody | Detects activated (phosphorylated) STAT1 | Flow cytometry or Western Blot to confirm downstream IFNγ pathway signaling [96] |
| Anti-Human MHC-I Antibody | Labels surface HLA-A/B/C complexes | Flow cytometry to assess defects in antigen presentation (e.g., B2M loss) [96] |
| CD8a Antibody | Identifies cytotoxic T lymphocytes | Immunohistochemistry to quantify tumor-infiltrating lymphocytes (TILs) [99] |
| Anti-PD-L1 Antibody | Detects programmed death-ligand 1 expression | Assessing adaptive upregulation in response to IFNγ or oncogenic signaling [96] [6] |
| TUNEL Assay Kit | Labels DNA fragments in apoptotic cells | Immunohistochemistry to measure therapy-induced cell death in tumor spheroids or tissue [99] |
| Ki-67 Antibody | Marks proliferating cells | Immunohistochemistry to assess tumor or immune cell proliferation status [99] |
| CD31 (PECAM-1) Antibody | Highlights vascular endothelium | Immunohistochemistry to quantify microvascular density as a surrogate for angiogenesis [99] |
| JAK1/JAK2 Inhibitors | Pharmacologically blocks JAK/STAT signaling | In vitro models to mimic resistance mutations and study synergistic therapies [96] |
| Lactic Acid Assay Kit | Quantifies lactate concentration in media/serum | Measuring lactate production by tumor cells to correlate with T-cell suppression in vitro [6] |
Signaling Pathways in Resistance: A Visual Synthesis
The following diagram synthesizes key signaling pathways involved in both the mechanism of action of ICIs and the development of resistance, integrating tumor-intrinsic and extrinsic factors.
Diagram 2: Key Signaling Pathways in ICI Response and Resistance
Resistance to immunotherapy, whether primary or acquired, is not a singular entity but a complex, multi-mechanistic process driven by dynamic interactions between tumor cells and their microenvironment. The field has moved beyond simplistic models to recognize distinct resistance programs—including loss of antigenicity, defects in IFNγ signaling, and metabolic suppression—that may coexist or dominate in different patients. Overcoming this challenge requires a multifaceted strategy: the continued use of sophisticated experimental models for mechanistic discovery, the development of reliable non-invasive biomarkers for early detection, and the rational design of combination therapies that simultaneously target tumor-intrinsic vulnerabilities and remodel the immunosuppressive TME. As our understanding deepens, the future of immunotherapy lies in personalizing salvage strategies based on the specific resistance mechanisms operative in each patient's tumor, thereby restoring the power of the immune system to achieve durable cancer control.
Cancer immunotherapy, particularly immune checkpoint inhibitors (ICIs), has revolutionized oncology by harnessing the immune system to fight tumors. However, these therapies frequently cause immune-related adverse events (irAEs) due to unintended immune activation against healthy tissues [8]. The gut microbiome plays a dual role in this context: it significantly influences immunotherapy efficacy by modulating immune responses, but dysbiosis (microbial imbalance) can exacerbate treatment-related toxicity [31] [100]. This creates a critical challenge for clinical practice—how to maintain antitumor immunity while minimizing collateral damage to healthy tissues. Understanding the intricate relationship between immunosuppressive mechanisms, microbiome integrity, and treatment toxicity provides a foundation for developing effective mitigation strategies. This technical guide examines current knowledge and emerging approaches for toxicity mitigation, focusing on microbiome-based interventions that preserve anticancer efficacy while reducing adverse effects.
Mechanisms of Immunotherapy-Induced Toxicity
Immune Checkpoint Biology and Off-Target Effects
Immune checkpoint inhibitors work by blocking inhibitory receptors such as cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), programmed cell death protein 1 (PD-1), and its ligand PD-L1 [8]. Under physiological conditions, these checkpoints maintain self-tolerance and prevent autoimmunity. CTLA-4, expressed on regulatory T cells (Tregs) and activated T cells, inhibits T-cell activation by outcompeting CD28 for binding to B7 molecules (B7-1 and B7-2) on antigen-presenting cells [8]. PD-1, expressed on activated T cells, interacts with PD-L1/PD-L2 to limit T-cell activity in peripheral tissues. While ICIs release these brakes to enhance antitumor immunity, they also lower thresholds for immune activation against self-antigens, leading to tissue damage and irAEs [8].
The gut microbiome modulates these effects through multiple mechanisms. Specific microbial compositions can differentiate patients who develop severe irAEs from those who do not [31]. Microbiome-derived metabolites, including short-chain fatty acids (SCFAs) and bile acids, shape both innate and adaptive immune responses, influencing the threshold for immune activation [31] [101]. For instance, SCFAs like butyrate have demonstrated dual roles—they can maintain intestinal barrier integrity and promote regulatory T-cell differentiation, yet systemic SCFAs have been shown to diminish the efficacy of anti-CTLA-4 therapy by reducing ICOS expression on CD4+ T cells and CD80/CD86 on dendritic cells [101].
Microbiome-Mediated Toxicity Pathways
Table 1: Microbial Taxa Associated with Immunotherapy Toxicity and Efficacy
| Microbial Taxa | Association | Proposed Mechanism | Cancer Type Context |
|---|---|---|---|
| Bacteroidetes | Enhanced ICI efficacy | Th1 cell activation, dendritic cell maturation | Melanoma, NSCLC [31] |
| Bifidobacterium | Improved PD-L1 response | DC maturation, CD8+ T cell activation | Melanoma, renal cell carcinoma [31] |
| Akkermansia muciniphila | Restored ICI efficacy in antibiotic-treated patients | Immune modulation | NSCLC, RCC [31] |
| Bacteroides fragilis | Reversed anti-CTLA-4 non-responsiveness | IL-12-dependent Th1 immune responses [101] | Melanoma [31] |
| Enterotoxigenic Bacteroides fragilis (ETBF) | Cancer progression, treatment resistance | Chronic inflammation, genotoxicity | Breast cancer [102] |
| Fusobacterium nucleatum | Poor prognosis, chemoresistance | Gal-GalNAc binding, immunosuppressive TME [102] | Breast, colorectal cancers [102] |
The microbiome influences irAE development through several interconnected pathways. Dysbiosis can compromise intestinal barrier function, leading to bacterial translocation and systemic inflammation that exacerbates immune activation [100]. Specific pathogenic bacteria, such as enterotoxigenic Bacteroides fragilis (ETBF) and Fusobacterium nucleatum, have been mechanistically implicated in cancer progression and treatment resistance through chronic inflammation, matrix metalloproteinase activation, and induction of immunosuppressive tumor microenvironments [102]. Additionally, microbiome composition affects drug metabolism, with dysbiosis altering the enzymatic conversion of chemotherapeutic agents like irinotecan to its toxic metabolite SN-38, worsening gastrointestinal toxicity [100].
Microbiome-Targeted Toxicity Mitigation Strategies
Untargeted Microbiome Modulation Approaches
Fecal Microbiota Transplantation (FMT) has emerged as a promising intervention for restoring microbial diversity and reducing irAEs. Clinical trials in patients with PD-1-refractory melanoma demonstrated that FMT from responding donors could restore microbiota diversity and dramatically improve safety and responsiveness to ICIs [101]. The proposed mechanism involves reestablishing a balanced microbial community that promotes intestinal barrier integrity, reduces pathogenic bacteria, and generates beneficial metabolites that support regulatory immune responses.
Probiotics, Prebiotics, and Dietary Interventions offer less invasive approaches to microbiome modulation. Specific probiotic strains, including Bifidobacterium and Lactobacillus, have shown potential in enhancing ICI efficacy while modulating immune responses to reduce toxicity [31]. Prebiotics, which are nondigestible food ingredients that selectively stimulate growth of beneficial bacteria, and dietary interventions such as ketogenic diets, are being explored for their ability to shape microbial communities toward a favorable composition [40] [101]. These approaches work by increasing microbial production of beneficial metabolites like SCFAs, which reinforce gut barrier function and promote Treg differentiation, thereby dampening excessive immune activation [101].
Targeted Engineering Approaches
Nanomaterial-Based Microbiome Modulation represents a transformative approach for precision targeting of pathogenic bacteria while preserving beneficial microbiota. Lipid-based antimicrobial nanoparticles functionalized with Gal/GalNAc can selectively target and eliminate tumor-associated Fusobacterium nucleatum, reversing chemotherapy resistance while maintaining microbial diversity [102]. Similarly, bacterial membrane-coated nanoplatforms enable precision antimicrobial delivery, with ferritin-nanocaged doxorubicin demonstrating >90% tumor growth inhibition in preclinical models while preserving microbial diversity [102].
Engineered Microbial Therapeutics utilize synthetic biology to create "smart" living therapeutics. Engineered symbiotic bacteria can be programmed with synthetic gene circuits to sense pathological signals and deliver targeted therapies [103]. For IBD-like inflammation, designs include bacteria that sense TNF-α and produce anti-inflammatory cytokines, creating closed-loop feedback systems [103]. Bacteriophages offer another targeted approach by selectively modulating dysbiotic microbiota through precise bacterial targeting [103]. These engineered systems address limitations of conventional approaches by providing spatial and temporal control over therapeutic delivery.
Table 2: Experimental Protocols for Microbiome-Targeted Interventions
| Intervention | Experimental Model | Key Methodology | Outcome Measures |
|---|---|---|---|
| Fecal Microbiota Transplantation (FMT) | Melanoma patients refractory to anti-PD-1 [101] | FMT from ICI responders + anti-PD-1 therapy | Microbiota diversity by 16S rRNA sequencing, irAE incidence, overall response rate |
| Probiotic Administration | Melanoma mouse models [31] | Oral gavage of Bifidobacterium combined with PD-L1 inhibition | Tumor growth inhibition, CD8+ T cell infiltration by flow cytometry, dendritic cell activation |
| Nanoparticle Targeting | Breast cancer models [102] | IV administration of Colistin-LipoFM nanoparticles | Fusobacterium nucleatum burden by qPCR, tumor volume, microbial diversity analysis |
| Engineered Bacteria | Murine colitis models [103] | Oral administration of E. coli Nissle 1917 engineered with TNF-α sensing circuit | Inflammation scoring, cytokine levels, bacterial localization by bioluminescence |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Microbiome-Immunotherapy Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Gnotobiotic Mouse Models | Germ-free C57BL/6, Swiss Webster | Establish causal microbiome relationships | Requires specialized facilities; allows human microbiota transplantation [31] |
| Bacterial Strain Collections | Bifidobacterium longum, Akkermansia muciniphila | Probiotic screening and mechanism studies | Culture conditions vary; anaerobic chambers often required [31] |
| Nanocarrier Systems | Gal/GalNAc-functionalized nanoparticles, bacterial membrane-coated nanoplatforms [102] | Targeted pathogen depletion studies | Characterize targeting efficiency and biodistribution [102] |
| Synthetic Biology Tools | CRISPR-Cas9, TALEN, synthetic gene circuits [103] | Engineer therapeutic microbial strains | Consider biocontainment strategies for live biotherapeutic products [103] |
| Microbiome Analysis | 16S rRNA sequencing, metagenomics, metabolomics | Microbial community profiling | Multi-omics integration provides mechanistic insights [31] |
| Immune Monitoring | Multiplex cytokine panels, spectral flow cytometry | Immune response characterization | Focus on T-cell exhaustion markers (PD-1, TIGIT, TIM-3) [8] |
Integrated Workflows and Signaling Pathways
Experimental Workflow for Microbiome-Immunotherapy Studies
Microbiome-Immune Signaling in Toxicity and Efficacy
The integration of microbiome engineering into cancer immunotherapy represents a paradigm shift in toxicity management. Future research priorities include developing standardized protocols for FMT in immunotherapy patients, optimizing synthetic biology approaches for engineered microbial therapeutics, and validating microbiome-based biomarkers for predicting irAE risk [103] [101]. The field must also address challenges in clinical translation, including safety concerns with genetically modified organisms, variability in individual microbiome responses, and the need for larger controlled trials to establish causal relationships [103].
Advanced nanomaterial platforms that enable targeted manipulation of specific bacterial populations without disrupting commensal communities offer particular promise for next-generation toxicity mitigation [102]. Similarly, the integration of multi-omics approaches (metagenomics, metatranscriptomics, metabolomics) will provide deeper insights into the molecular mechanisms linking microbiome composition to treatment toxicity [31] [101].
In conclusion, microbiome-focused strategies provide a powerful approach for uncoupling antitumor efficacy from treatment toxicity. By strategically modulating host-microbiome interactions, researchers and clinicians can potentially expand the therapeutic window of cancer immunotherapies, enabling more patients to benefit from these transformative treatments while experiencing fewer side effects. The continued integration of microbiome science into immuno-oncology represents a critical frontier in the effort to optimize cancer treatment outcomes.
Bench to Bedside: Biomarkers, Clinical Validation, and Comparative Efficacy
The advent of immune checkpoint inhibitors (ICIs) has fundamentally transformed the oncology landscape, providing durable responses and survival benefits across a growing number of malignancies. However, the clinical application of these immunotherapies reveals significant challenges: response rates vary dramatically between cancer types and individual patients, with some experiencing minimal benefit or severe immune-related adverse events (irAEs) [98]. This variability underscores the critical need for robust predictive biomarkers to guide patient selection, optimize clinical outcomes, and minimize toxicity.
The efficacy of ICIs hinges on a functional cancer-immunity cycle, a multi-step process encompassing tumor antigen presentation, T-cell activation, trafficking, and eventual tumor cell killing [98]. Disruptions at any point in this cycle—whether through tumor-intrinsic factors or features of the tumor microenvironment (TME)—can confer resistance to treatment [104]. The biomarkers discussed in this review serve as measurable indicators of these processes, providing windows into the complex tumor-immune interplay.
This technical guide examines the foundational biomarkers in cancer immunotherapy—PD-L1, microsatellite instability (MSI), and tumor mutational burden (TMB)—while exploring emerging candidates and the experimental frameworks essential for their investigation. Framed within the broader thesis of understanding antitumor activity and toxicity mechanisms, this resource provides drug development professionals and researchers with the methodologies and conceptual frameworks needed to advance the field of immuno-oncology.
Established Biomarkers: Mechanisms and Clinical Utility
Programmed Death-Ligand 1 (PD-L1)
Mechanism and Biological Rationale PD-L1, encoded by the CD274 gene on chromosome 9, is a transmembrane protein that serves as a key ligand for the programmed death-1 (PD-1) receptor on T cells [105]. Their interaction transmits an inhibitory signal that suppresses T-cell activation, induces T-cell exhaustion, and enables tumor immune escape [70]. ICIs targeting the PD-1/PD-L1 axis block this interaction, thereby reinvigorating antitumor immunity. PD-L1 expression is often induced by inflammatory signals, particularly interferon-gamma (IFN-γ), within the TME, representing an adaptive resistance mechanism [106].
Assessment Methodologies and Scoring Systems PD-L1 expression is predominantly assessed via immunohistochemistry (IHC) on formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections [107]. The specific clones of antibodies used, staining platforms, and scoring algorithms vary, leading to several established scoring systems:
- Tumor Proportion Score (TPS): Defined as the percentage of viable tumor cells exhibiting partial or complete membrane staining at any intensity. It is utilized as a predictive biomarker in non-small cell lung cancer (NSCLC) for pembrolizumab [70].
- Combined Positive Score (CPS): Calculated as the number of PD-L1 staining cells (tumor cells, lymphocytes, macrophages) divided by the total number of viable tumor cells, multiplied by 100. This score is used in cancers such as gastric and head and neck cancers [107].
Standardized experimental protocols require appropriate controls, validation of antibody specificity, and pathologist training to ensure scoring consistency. The Ventana BenchMark ULTRA automated staining platform with clones such as SP263 is an example of a clinically deployed methodology [107].
Clinical Validation and Limitations The KEYNOTE-024 trial established PD-L1 TPS ≥50% as a predictive biomarker for first-line pembrolizumab in metastatic NSCLC, demonstrating significantly improved overall survival (OS) compared to chemotherapy (median OS: 30.0 vs. 14.2 months; HR: 0.63) [106]. However, the CheckMate-026 trial, which also used nivolumab, failed to show a similar progression-free survival (PFS) advantage, highlighting the limitations of PD-L1 as a standalone biomarker [106]. These discrepancies are attributed to tumor heterogeneity, temporal and spatial variations in expression, and assay/platform variability [70]. Notably, a subset of patients with low or undetectable PD-L1 expression still derives clinical benefit, indicating that PD-L1 negativity should not universally preclude ICI therapy [105].
Microsatellite Instability (MSI) and Mismatch Repair Deficiency (dMMR)
Mechanism and Biological Rationale Microsatellites are short, repetitive DNA sequences prone to replication errors. The mismatch repair (MMR) system, involving proteins such as MLH1, MSH2, MSH6, and PMS2, corrects these errors [108]. Deficient MMR (dMMR) leads to the accumulation of insertion/deletion mutations across microsatellites, resulting in a hypermutated tumor genome and high neoantigen load [108] [106]. These neoantigens are presented on major histocompatibility complex (MHC) molecules, facilitating robust T-cell recognition and attack [98].
Assessment Methodologies MSI/MMR status can be evaluated through two primary techniques:
- IHC for MMR Proteins: Loss of nuclear expression of one or more MMR proteins (MLH1, MSH2, MSH6, PMS2) in tumor tissue indicates dMMR. This method is widely accessible but may miss rare mutations that cause non-functional protein expression.
- PCR-Based MSI Testing: This method compares the length of microsatellite loci (e.g., BAT-25, BAT-26, NR-21, NR-24, NR-27) between tumor and normal DNA. A shift in allele sizes at ≥2 loci classifies a tumor as MSI-High (MSI-H) [107]. Next-generation sequencing (NGS) panels now commonly include MSI assessment, providing a high-throughput alternative.
Clinical Validation and Limitations MSI-H/dMMR was the first biomarker to receive tissue-agnostic FDA approval for pembrolizumab based on data from KEYNOTE-016, -164, and -158, which demonstrated an objective response rate (ORR) of 39.6% in advanced, treatment-refractory MSI-H/dMMR cancers [106]. The response is notably durable, with 78% of responses ongoing at the data cutoff [106]. Despite its high predictive value, the prevalence of MSI-H/dMMR is low in most common cancers (e.g., 1% in esophageal carcinoma cohorts), limiting its widespread application [107].
Tumor Mutational Burden (TMB)
Mechanism and Biological Rationale TMB is defined as the total number of somatic non-synonymous mutations per megabase (mut/Mb) of the genome sequenced [109]. A high TMB increases the probability of generating immunogenic neoantigens that can be recognized by T cells, thereby enhancing tumor visibility to the immune system and susceptibility to ICIs [98].
Assessment Methodologies and Standardization Challenges TMB is most accurately measured by whole-exome sequencing (WES) but is often estimated in clinical settings using targeted NGS panels such as FoundationOne CDx and MSK-IMPACT [109]. Key considerations and challenges in its measurement include:
- Panel Size: The coefficient of variation of TMB estimation decreases as panel size increases. Panels covering ≥1 Mb are generally recommended for reliable estimation [109].
- Bioinformatic Pipelines: Variations exist in the types of mutations included (e.g., non-synonymous only vs. including synonymous), filters applied, and the minimum coverage depth required.
- Cut-off Definition: The FDA-approved cut-off for pembrolizumab is TMB-High (TMB-H) ≥10 mut/Mb, based on the KEYNOTE-158 trial [109] [106]. However, emerging evidence suggests the optimal predictive cut-off may vary by cancer type. For instance, in prostate cancer, a TMB ≥10 mut/Mb showed little benefit, whereas a cut-off of ≥20 mut/Mb was more predictive in other pan-cancer analyses [108].
Table 1: Comparison of Key Established Biomarkers
| Biomarker | Underlying Biology | Primary Testing Method(s) | Key Clinical Trial Evidence | Strengths | Limitations |
|---|---|---|---|---|---|
| PD-L1 | Adaptive immune resistance; inhibits T-cell function | IHC (TPS, CPS) | KEYNOTE-024 (NSCLC) | Widely available; standardized IHC assays | Intratumoral heterogeneity; dynamic expression; imperfect predictor |
| MSI/dMMR | Genomic hypermutability; high neoantigen load | IHC (MMR proteins), PCR/NGS (MSI status) | KEYNOTE-016/158 (Pan-cancer) | Tissue-agnostic approval; high predictive value | Low prevalence in common cancers (e.g., 1% in ESCC [107]) |
| TMB | High neoantigen burden | NGS (Panel, WES) | KEYNOTE-158 (Pan-cancer) | Quantitative; pan-cancer potential | Lack of assay harmonization; variable optimal cut-offs |
Emerging and Integrated Biomarkers
The Tumor Microenvironment (TME) and Tumor-Infiltrating Lymphocytes (TILs)
The TME is a complex ecosystem comprising immune cells, stromal cells, blood vessels, and extracellular matrix. Its composition profoundly influences immunotherapy response [70] [105].
- CD8+ T Cells: As the primary effector cells of antitumor immunity, the density, location (especially invasive margin vs. tumor core), and functional state of CD8+ T cells are critical. A lack of T-cell infiltration ("immune-excluded" or "desert" phenotype) is a major mechanism of primary resistance to ICIs [98] [70].
- Immunosuppressive Cells: Cells such as M2-like tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs) create an immunosuppressive TME by secreting inhibitory cytokines (e.g., IL-10, TGF-β) and expressing other co-inhibitory ligands, thereby contributing to ICI resistance [104].
Assessment Methodologies: TILs can be quantified by IHC for specific cell subsets (e.g., CD8, FOXP3) or evaluated on hematoxylin and eosin (H&E)-stained sections using standardized guidelines. Digital pathology and multiplex IHC (e.g., CODEX, Imaging Mass Cytometry) enable high-dimensional spatial analysis of the TME, revealing critical cellular interactions [70].
Circulating Biomarkers
Liquid biopsies offer a minimally invasive means to dynamically monitor disease and treatment response.
- Circulating Tumor DNA (ctDNA): Changes in ctDNA levels can predict response to ICIs earlier than radiographic imaging. A ≥50% reduction in ctDNA within 6-16 weeks of starting therapy correlates with improved PFS and OS [106]. The absence of detectable ctDNA (molecular response) is a particularly strong favorable prognostic sign.
- Peripheral Blood Immune Cells: The relative eosinophil count (REC) has been investigated as a potential biomarker for CTLA-4 inhibition, with one study in melanoma showing a median OS of 27 months for patients with REC ≥1.5% versus 5-7 months for those with lower counts [106].
Tertiary Lymphoid Structures (TLS) and Multi-Omics
- Tertiary Lymphoid Structures (TLS): TLS are ectopic lymphoid organs that develop in chronic inflammation sites, including tumors. They serve as hubs for local immune cell activation and maturation. Their presence, density, and maturity correlate with improved responses to ICIs in NSCLC and other cancers, suggesting a role in sustaining effective anti-tumor immunity [70].
- Multi-Omics Integration: Combining genomic, transcriptomic, proteomic, and epigenomic data through machine learning models has shown promise in improving the predictive accuracy for ICI response beyond single biomarkers. For example, Bourbonne et al. reported a ~15% improvement in predictive accuracy using a multi-omics approach [106].
Mechanisms of Resistance and Biomarker Implications
Resistance to ICIs is categorized as either primary (no initial response) or acquired (disease progression after an initial response) and can be driven by tumor-intrinsic and tumor-extrinsic factors [98] [104].
Tumor-Intrinsic Resistance Mechanisms:
- Lack of Neoantigens: Tumors with low TMB, such as pancreatic and prostate cancers, generate insufficient neoantigens to elicit a robust T-cell response, leading to primary resistance [110] [98].
- Defects in Antigen Presentation: Loss-of-function mutations in genes like B2M, which is essential for MHC-I assembly, prevent neoantigen presentation to CD8+ T cells, rendering the tumor "invisible" to immune effectors [98].
- Oncogenic Signaling Pathways: Aberrant activation of pathways like WNT/β-catenin and VEGF can inhibit T-cell infiltration and foster an immune-excluded TME [104].
Tumor-Extrinsic Resistance Mechanisms:
- Immunosuppressive Microenvironment: As previously noted, cells like M2-TAMs and MDSCs suppress T-cell function through multiple mechanisms, including expression of alternative immune checkpoints (e.g., LAG-3, TIM-3) and metabolic dysregulation (e.g., indoleamine 2,3-dioxygenase activity) [104].
- Gut Microbiota: The composition of the gut microbiome modulates systemic immunity and ICI efficacy. Antibiotic use, which disrupts the microbiome, has been associated with poorer outcomes in ICI-treated patients [104].
Table 2: Research Reagent Solutions for Biomarker Investigation
| Research Tool Category | Example Products/Assays | Primary Research Application |
|---|---|---|
| IHC & Antibodies | Anti-PD-L1 clones (SP263, 22C3); Anti-MMR proteins (MLH1, MSH2, etc.); Anti-CD8 | Protein expression analysis; Immune contexture characterization [107] [105] |
| NGS Panels | FoundationOne CDx; MSK-IMPACT; TruSight Oncology 500 | TMB, MSI, and specific gene mutation assessment [109] |
| Liquid Biopsy Assays | GuardantOMNI; ctDNA assays | Dynamic monitoring of tumor burden and genomic evolution [109] [106] |
| Multiplex Spatial Biology Platforms | Multiplex IHC/IF; CODEX; Imaging Mass Cytometry; GeoMx Digital Spatial Profiler | High-plex, spatial analysis of the tumor immune microenvironment [70] |
| Single-Cell & Spatial Transcriptomics | 10x Genomics Single Cell RNA-seq; Visium Spatial Gene Expression | Unbiased discovery of cell states and transcriptional programs within the TME [70] |
Visualizing Core Concepts
The Cancer-Immunity Cycle and ICI Mechanisms
This diagram illustrates the multi-step process of antitumor immunity and the points where ICIs and biomarkers interact.
Integrated Biomarker Analysis for ICI Response Prediction
This flowchart outlines a logical framework for integrating multiple biomarkers to predict patient response to immune checkpoint inhibitor therapy.
The pursuit of predictive biomarkers for immunotherapy response and toxicity remains a cornerstone of precision oncology. While PD-L1, MSI, and TMB provide a foundational clinical framework, their limitations highlight the biological complexity of tumor-immune interactions. The future lies in integrated biomarker platforms that combine genomic, proteomic, and cellular data from both tissue and liquid biopsies. This multi-omics approach, powered by advanced computational analytics, promises to more accurately stratify patients, uncover novel resistance mechanisms, and guide the development of rational combination therapies. For researchers and drug developers, focusing on standardizing assays, validating emerging biomarkers like TLS and ctDNA, and elucidating the spatial relationships within the TME will be critical to fully realizing the potential of cancer immunotherapy.
Clinical endpoints are objective measures used in trials to assess the safety and efficacy of new cancer therapies, serving as critical tools for regulatory approval and clinical decision-making [111] [112]. In the context of immunotherapy research, which aims to enhance the body's natural immune response against tumors, these endpoints quantify the delicate balance between antitumor activity and treatment-related toxicity [113] [114]. The selection of an appropriate endpoint is paramount, as it must align with the therapeutic agent's specific mechanism of action and the clinical context of its use [115].
Oncology endpoints are broadly classified as primary or surrogate. Primary endpoints, such as Overall Survival (OS), directly measure a patient's feeling, function, or survival. Surrogate endpoints, including Progression-Free Survival (PFS) or Overall Response Rate (ORR), are utilized as substitutes for primary endpoints and can provide earlier results, though they require validation for each specific cancer type and treatment [112]. As targeted therapies and immunotherapies have evolved, traditional size-based response assessments have shown limitations, necessitating a more sophisticated application of these endpoint metrics [115].
Defining Key Efficacy Endpoints
Overall Survival (OS) is defined as the time from randomization until death from any cause [111] [112]. It is considered the gold standard endpoint in oncology due to its objectivity, clinical relevance, and freedom from assessment bias [111] [112]. Its primary disadvantage is that it requires large sample sizes and lengthy follow-up times, which can be influenced by subsequent therapies and cross-over treatment effects, making it costly and time-consuming [112].
Other survival-based endpoints provide complementary information. Progression-Free Survival (PFS) measures the time from randomization until the first evidence of disease progression or death [111] [112]. It is not influenced by subsequent therapies and often provides earlier data than OS, making it a popular surrogate endpoint [112]. Time to Progression (TTP), a related metric, measures only the time to disease progression and excludes death, thereby focusing solely on the drug's direct effect on the tumor [112].
In adjuvant settings, Disease-Free Survival (DFS) measures the time from randomization until evidence of disease recurrence, effectively assessing the ability of a treatment to prevent relapse after definitive therapy like surgery [111] [112]. For neoadjuvant settings, Event-Free Survival (EFS) is preferred and is defined as the time from randomization to any event, which may include disease progression, discontinuation of treatment, or death [112].
Tumor Response-Based Endpoints
Endpoints based on radiographic tumor assessment provide direct evidence of a drug's antitumor activity. The Overall Response Rate (ORR) is the proportion of patients in a trial whose tumor is destroyed or significantly reduced by a drug, typically defined as the sum of Complete Responses (CR) and Partial Responses (PR) [111]. An improved ORR offers tangible proof that a drug is working [111].
The Duration of Response (DoR) measures the length of time that a tumor continues to respond to treatment without the cancer growing or spreading [111]. This endpoint is crucial for distinguishing transient responses from durable, clinically meaningful benefits, a particularly important consideration in immunotherapy where responses can be long-lasting [111].
Table 1: Key Efficacy Endpoints in Oncology Clinical Trials
| Endpoint | Definition | Key Advantages | Key Limitations |
|---|---|---|---|
| Overall Survival (OS) | Time from randomization to death from any cause [111] [112] | Gold standard; objective; clinically relevant [111] [112] | Long follow-up; large sample; confounded by subsequent therapies [112] |
| Progression-Free Survival (PFS) | Time from randomization to disease progression or death [111] [112] | Not influenced by subsequent therapy; earlier readout than OS [112] | Does not always correlate with OS; requires frequent imaging [112] |
| Overall Response Rate (ORR) | Proportion of patients with tumor size reduction (CR + PR) [111] | Direct measure of drug activity; tangible proof of efficacy [111] | Does not capture duration of benefit [111] |
| Duration of Response (DoR) | Time from initial response to disease progression [111] | Measures durability of response; distinguishes temporary vs. lasting benefit [111] | Only applicable to responders [111] |
| Disease-Free Survival (DFS) | Time from randomization to disease recurrence [112] | Useful in adjuvant settings; shorter follow-up than OS [112] | Definition of recurrence can be controversial [112] |
Endpoints in the Context of Immunotherapy
Unique Response Patterns and Associated Challenges
Immunotherapy, particularly immune checkpoint inhibitors (ICIs), has introduced unique response patterns that complicate traditional endpoint assessment [115]. Unlike cytotoxic chemotherapy, which typically leads to rapid tumor shrinkage, immunotherapies can produce:
- Pseudoprogression: Where tumors initially appear to increase in size or new lesions form due to immune cell infiltration, followed by subsequent tumor reduction [115].
- Durable responses: Where patients maintain long-term disease control even after treatment cessation, highlighting the importance of DoR [111] [113].
- Dissociated responses: Where some lesions shrink while others remain stable or grow [115].
These unconventional patterns necessitate modified assessment criteria and underscore the value of endpoints like PFS and DoR that capture disease stabilization and response durability, not just tumor shrinkage [115]. The timing of efficacy assessment is particularly critical in immunotherapy, as initial radiographic evaluation may occur before the full therapeutic effect has manifested [116].
The Efficacy-Toxicity Relationship in Immunotherapy
A complex relationship exists between efficacy and toxicity in immunotherapy. Immune-related adverse events (irAEs) resulting from immune checkpoint inhibition have been associated with therapeutic benefit, as both are driven by activated T-cells [116] [114]. However, unlike the toxicities of chemotherapy which typically occur early, the onset of irAEs is highly variable and often delayed [116].
Research shows that the median time to initial efficacy assessment is approximately 50 days after ICI initiation, while the median time to any irAE is 77 days, with 58% of irAEs occurring after initial efficacy assessment [116]. This reversed temporal relationship means that, in practice, efficacy and toxicity cannot reliably serve as clinical biomarkers for predicting one another [116]. This bidirectional relationship underscores the need for careful monitoring throughout and beyond the treatment course.
Methodologies for Endpoint Assessment
Standardized Radiographic Assessment Protocols
The Response Evaluation Criteria in Solid Tumors (RECIST) is the most widely used methodology for evaluating tumor response in clinical trials [115]. The RECIST 1.1 guidelines specify:
- Baseline Imaging: Identify up to five target lesions and record the sum of their longest diameters.
- Follow-up Imaging: Perform at predefined intervals (e.g., every 6-12 weeks).
- Response Categorization:
- Complete Response (CR): Disappearance of all target lesions.
- Partial Response (PR): ≥30% decrease in the sum of diameters of target lesions.
- Progressive Disease (PD): ≥20% increase in the sum of diameters or appearance of new lesions.
- Stable Disease (SD): Neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for PD [115].
For specific cancer types, modified criteria have been developed. The Response Assessment in Neuro-Oncology (RANO) criteria address challenges in glioma assessment, such as pseudoprogression and radiation necrosis, by incorporating additional MRI sequences like FLAIR to evaluate non-enhancing tumor components [115].
Advanced Quantitative Imaging Techniques
As molecularly targeted therapies have emerged, quantitative imaging methods have evolved beyond simple anatomical measurements to provide functional and biological data [115]. These techniques can detect early treatment response before changes in tumor size are apparent.
Table 2: Advanced Quantitative Imaging Methods for Response Assessment
| Imaging Modality | Quantitative Parameter | Biological Interpretation | Application in Immunotherapy |
|---|---|---|---|
| Volumetric CT | Tumor volume (mm³) | Direct measure of tumor burden | More sensitive than 1D measurements for detecting early changes |
| Diffusion-Weighted MRI (DW-MRI) | Apparent Diffusion Coefficient (ADC) | Assessment of cellular density | Can detect immune cell infiltration (pseudoprogression) |
| Dynamic Contrast-Enhanced MRI (DCE-MRI) | Vessel perfusion and permeability (min⁻¹) | Quantitative measure of tumor vascular properties | Monitors changes in tumor microenvironment |
| FDG-PET | Standardized Uptake Value (SUV) | Semi-quantitative assessment of glucose metabolism | Can differentiate hypermetabolic viable tumor from treatment-related inflammation |
Immune-Related Response Criteria
To address the unique response patterns of immunotherapy, specialized criteria have been developed:
- Immune-Related RECIST (irRECIST): Provides guidelines for handling pseudoprogression by requiring confirmation of progressive disease on subsequent scans before declaring treatment failure.
- Immune RECIST (iRECIST): An evolution of irRECIST that standardizes the assessment of new lesions and unconfirmed versus confirmed progression.
These modified criteria help prevent premature discontinuation of effective immunotherapy and provide a more accurate assessment of true clinical benefit.
Experimental Pathways in Immunotherapy Research
The diagram illustrates the core pathway of antitumor immunity activated by checkpoint inhibitors. The process begins with tumor cell antigen release, followed by antigen presentation by dendritic cells to naïve T-cells in lymph nodes [113]. Successful T-cell priming leads to activation and migration to the tumor site, where cytotoxic T-cells mediate tumor cell death [113]. Checkpoint inhibitors enhance this process by blocking inhibitory signals (CTLA-4 at the priming phase; PD-1/PD-L1 at the effector phase), thereby sustaining the immune response [113] [114]. This mechanism underlies the efficacy endpoints discussed, with durable responses resulting from sustained T-cell activity, while immune-related adverse events occur from off-target T-cell activation [116] [114].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Immunotherapy Efficacy Studies
| Reagent Category | Specific Examples | Research Function |
|---|---|---|
| Immune Checkpoint Inhibitors | Anti-PD-1 (Nivolumab), Anti-PD-L1 (Atezolizumab), Anti-CTLA-4 (Ipilimumab) [114] | Block inhibitory signals to enhance antitumor T-cell activity; foundational for mechanistic studies |
| Flow Cytometry Antibodies | Anti-CD3, Anti-CD8, Anti-CD4, Anti-PD-1, Anti-CTLA-4, Anti-CD69 (activation) [113] | Phenotype and quantify immune cell populations in tumor microenvironment and peripheral blood |
| Cytokine Detection Assays | IFN-γ ELISpot, Multiplex cytokine panels (IL-2, IL-6, TNF-α, Granzyme B) [113] | Measure functional immune responses and inflammatory mediators |
| In Vivo Modeling Systems | Syngeneic mouse models, Humanized mouse models (with human immune system) [113] | Preclinical evaluation of immunotherapy efficacy and toxicity mechanisms |
| Immunohistochemistry Reagents | Antibodies for CD8, CD4, FoxP3, PD-L1, Granzyme B [113] | Spatial analysis of immune cell infiltration and checkpoint expression in tumor tissue |
The evaluation of efficacy endpoints across cancer types represents a dynamic interface between clinical trial methodology and advancing cancer biology. As immunotherapies continue to reshape the oncology landscape, the strategic selection and interpretation of endpoints—from the gold standard OS to surrogate markers like PFS and ORR—must evolve in parallel. The unique response patterns and complex efficacy-toxicity relationships observed with these agents necessitate sophisticated assessment protocols that capture both the immediate antitumor effects and the long-term clinical benefits. Future directions will likely involve the development of novel composite endpoints, the integration of liquid biopsies and molecular biomarkers, and the refinement of radiographic assessment criteria to better capture the full therapeutic potential of cancer immunotherapies.
Cancer therapy has undergone a profound transformation, moving from non-specific cytotoxic agents toward precisely targeted and immune-modulating strategies. This evolution reflects our deepening understanding of tumor biology and the complex interactions between cancer cells and the host immune system. Traditional cytotoxic therapies like chemotherapy and radiotherapy remain foundational in oncology, but their limitations have spurred the development of more selective approaches, including targeted therapy and immunotherapy. Each modality possesses distinct mechanisms of antitumor activity and unique toxicity profiles, governed by their fundamental interactions with biological systems. For researchers and drug development professionals, a comparative understanding of these therapeutic classes is essential for designing novel treatment strategies, predicting and managing adverse events, and developing rational combination therapies that maximize efficacy while minimizing toxicity. This analysis examines the core mechanisms, applications, and research methodologies for these four pillars of cancer treatment, with particular emphasis on the mechanisms of action and toxicity that are central to advancing the field.
Fundamental Mechanisms of Action
Immunotherapy: Harnessing the Immune System
Immunotherapy does not directly target cancer cells but instead stimulates the host's immune system to recognize and eliminate malignant cells. Its efficacy relies on overcoming the sophisticated immune evasion mechanisms employed by tumors [6]. Key approaches include:
- Immune Checkpoint Inhibitors (ICIs): Monoclonal antibodies block inhibitory receptors on T cells (e.g., CTLA-4, PD-1) or their ligands on tumor cells (e.g., PD-L1). This prevents the suppression of T-cell activity, effectively "releasing the brakes" on the immune system and restoring anti-tumor cytotoxicity [8]. For instance, anti-CTLA-4 antibodies like ipilimumab inhibit T-cell suppression and stimulate cytokine production, enhancing immune responsiveness against cancers [8].
- Adoptive Cell Transfer (ACT): This involves engineering a patient's own T cells to express chimeric antigen receptors (CAR) or specific T-cell receptors (TCR), then reinfusing these cells to selectively target and destroy tumor cells [48] [117].
- Cancer Vaccines: These are designed to prime the immune system against tumor-specific or tumor-associated antigens, enabling a targeted and durable immune response [48].
A critical challenge is the immunosuppressive tumor microenvironment (TME), where factors like lactic acid and metabolites such as ammonia can inhibit T-cell function and promote immune evasion [6]. Modern immunotherapy research focuses on reprogramming this microenvironment to be more permissive to immune attack.
Chemotherapy: Cytotoxic Cell Death
Chemotherapy employs drugs that are toxic to rapidly dividing cells, a hallmark of cancer. Its mechanisms are non-specific and include:
- Interference with DNA Replication and Repair: Many chemotherapeutic agents cause DNA damage or inhibit key enzymes involved in DNA synthesis, triggering apoptosis in rapidly dividing cells [118].
- Disruption of Cell Metabolism: Some agents interfere with metabolic processes essential for cancer cell survival [118].
The primary limitation of chemotherapy is its indiscriminate nature; it affects all rapidly dividing cells, including healthy cells in the bone marrow, hair follicles, and intestinal lining, leading to characteristic side effects like myelosuppression, alopecia, and mucositis [118].
Radiotherapy: Localized DNA Damage
Radiotherapy uses high-energy radiation to kill cancer cells in a localized manner. Its mechanism is twofold:
- Direct DNA Damage: Ionizing radiation directly causes single- and double-strand breaks in cellular DNA [119].
- Indirect Cell Damage: Radiation generates free radicals that subsequently damage DNA and other cellular structures, leading to cell death [119].
Emerging research indicates that radiotherapy can also stimulate a systemic immune response, a phenomenon known as the abscopal effect. Tumor-directed radiation can reprogram migratory dendritic cells, which then travel to lymph nodes to activate anti-tumor T cells, converting immune tolerance into effective antitumor immunity, especially when sequenced with immunotherapy [119].
Targeted Therapy: Molecular Precision
Targeted therapy uses drugs designed to interfere with specific molecules that are crucial for tumor growth and survival. This approach is characterized by its precision, as it focuses on specific genetic or molecular alterations in cancer cells [120] [117].
- Small Molecule Inhibitors: These compounds typically target intracellular signaling pathways, such as kinases involved in growth and proliferation (e.g., EGFR, BRAF, ALK) [117].
- Monoclonal Antibodies: These biologics target extracellular proteins, such as cell surface receptors or ligands, to block pro-tumorigenic signaling [117].
A key advancement is the development of agents like ivonescimab, a novel bispecific antibody that simultaneously targets PD-1 (immunotherapy) and VEGF (targeted therapy), addressing both immune evasion and angiogenesis with a single molecule [119].
Table 1: Core Mechanisms of Antitumor Activity and Associated Toxicities
| Therapy Class | Primary Molecular Target | Mechanism of Antitumor Activity | Primary Driver of Toxicity |
|---|---|---|---|
| Immunotherapy | Immune checkpoints (e.g., PD-1, CTLA-4); T cells | Activates host immune system to recognize and kill tumor cells | Immune-related adverse events (irAEs) from overactive immunity attacking healthy tissues |
| Chemotherapy | DNA/metabolism of dividing cells | Directly kills rapidly dividing cells via DNA damage or metabolic disruption | Non-specific cytotoxicity against all rapidly dividing healthy cells (e.g., in bone marrow, gut) |
| Radiotherapy | Cellular DNA (direct/indirect damage) | Causes lethal DNA damage and cell death within a localized radiation field | Collateral damage to healthy tissues within the radiation field; systemic fatigue |
| Targeted Therapy | Specific oncogenic proteins/pathways (e.g., EGFR, BCR-ABL) | Inhibits specific molecules and signaling pathways critical for tumor growth | "On-target, off-tumor" effects from inhibiting the target in healthy cells; pathway resistance |
Comparative Clinical and Research Profiles
Efficacy and Response Dynamics
The effectiveness of each therapeutic class varies significantly based on cancer type, disease stage, and individual patient biomarkers.
- Immunotherapy can produce remarkably durable responses and long-term survival in a subset of patients, as seen in advanced melanoma and non-small cell lung cancer (NSCLC) [118] [120]. However, response can be slow and is not universal. Its success is often contingent on the presence of specific biomarkers, such as PD-L1 expression, and a pre-existing but suppressed immune infiltrate within the tumor [118] [119].
- Chemotherapy often leads to rapid tumor shrinkage and is effective across a wide range of cancers. It is frequently used as a first-line treatment, particularly for aggressive or advanced diseases [118]. A key limitation is the development of drug resistance.
- Radiotherapy is highly effective for local tumor control and is often used with curative intent for localized cancers. It also plays a critical role in palliating symptoms like pain from bone metastases [119].
- Targeted Therapy demonstrates high response rates in patients whose tumors harbor the specific molecular target, such as EGFR-mutated NSCLC or HER2-positive breast cancer [120]. However, resistance almost invariably develops, often through secondary mutations or activation of alternative pathways [120].
Table 2: Comparative Clinical Profile and Research Applications
| Parameter | Immunotherapy | Chemotherapy | Radiotherapy | Targeted Therapy |
|---|---|---|---|---|
| Typical Response Onset | Delayed (weeks-months) | Rapid (days-weeks) | Variable (during/after course) | Rapid (days-weeks) |
| Response Durability | Can be highly durable | Often limited by resistance | Durable for local control | Often limited by resistance |
| Key Predictive Biomarkers | PD-L1, TMB, MSI, TILs | Tumor histology, proliferation rate | Tumor type, volume, location | Specific genetic mutations (e.g., EGFR, ALK) |
| Primary Research Focus | Overcoming immune resistance; combination strategies | Novel delivery to reduce toxicity; overcoming resistance | Combining with immunotherapy (abscopal effect); precision targeting | Overcoming resistance; targeting "undruggable" targets |
| Common In Vivo Models | Syngeneic mouse models; humanized mouse models | Patient-derived xenografts (PDX); cell line-derived xenografts | Orthotopic models; image-guided small animal irradiators | Genetically engineered mouse models (GEMM); PDX models |
Toxicity and Side Effect Profiles
Understanding the mechanisms of toxicity is crucial for managing patients and designing safer therapeutic agents.
- Immunotherapy Toxicity: Arises from immune-related adverse events (irAEs), where an overactivated immune system attacks healthy organs, causing conditions like pneumonitis, colitis, hepatitis, and endocrinopathies [118] [8]. Management typically involves immunosuppression with corticosteroids [118].
- Chemotherapy Toxicity: Results from non-specific cytotoxicity. Common effects include myelosuppression (increasing infection risk), nausea, vomiting, and alopecia, which occur because the drugs damage healthy, rapidly dividing cells [118].
- Radiotherapy Toxicity: Generally localized to the treatment field, leading to side effects like skin reactions, fibrosis, and damage to nearby organs. Modern techniques like intensity-modulated radiotherapy (IMRT) aim to sculpt the radiation dose and minimize this collateral damage [119].
- Targeted Therapy Toxicity: Often caused by "on-target, off-tumor" effects, where inhibiting the target protein in healthy cells causes side effects, such as skin rash from EGFR inhibitors or hypertension from VEGF inhibitors [120]. These are generally different from the systemic toxicity of chemotherapy.
Experimental and Research Methodologies
Key Research Reagents and Solutions
Table 3: Essential Research Reagent Solutions for Therapy Investigation
| Research Reagent / Tool | Primary Function in Research | Example Application |
|---|---|---|
| Recombinant Immune Checkpoint Proteins (e.g., hPD-1/Fc) | Ligand binding studies; blocking assay development | In vitro validation of ICI binding affinity and blocking efficacy [8] |
| Anti-Human CD3/CD28 Activator | Polyclonal T-cell activation and expansion | Generating activated T cells for in vitro cytotoxicity assays or ACT protocols [48] |
| Lactate Assay Kit | Quantifying lactate concentration in cell culture media | Assessing glycolytic activity of tumor cells and its suppressive effect on T cells in the TME [6] |
| Annexin V Apoptosis Kit | Detecting phosphatidylserine externalization | Quantifying apoptosis in tumor cell lines post-chemotherapy or targeted therapy treatment [118] |
| Phospho-Specific Antibodies (e.g., p-ERK, p-AKT) | Detecting pathway activation/inhibition via Western Blot or IHC | Validating target engagement and efficacy of small molecule kinase inhibitors [117] |
| Cytokine Multiplex Assays (Luminex) | Profiling dozens of cytokines/chemokines in serum or supernatant | Monitoring systemic immune activation or cytokine release syndrome post-immunotherapy [8] |
Detailed Experimental Protocol: Assessing T-cell Cytotoxicity Post-Immunotherapy
This protocol is used to evaluate the functional impact of immune checkpoint inhibitors on the ability of T cells to kill cancer cells.
- T Cell Isolation and Activation: Isolate human peripheral blood mononuclear cells (PBMCs) from healthy donors using density gradient centrifugation (e.g., Ficoll-Paque). Isolate CD3+ T cells using negative selection magnetic bead kits. Activate T cells using plate-bound anti-CD3 and soluble anti-CD28 antibodies in culture media containing IL-2 for 3-4 days [48] [8].
- Tumor Cell Preparation: Culture adherent target tumor cells (e.g., A375 melanoma line). For the assay, detach cells and label with a fluorescent dye such as CFSE.
- Checkpoint Inhibition: Pre-incubate activated T cells with therapeutic ICIs (e.g., anti-PD-1 antibody) or an isotype control for 1-2 hours.
- Co-Culture and Cytotoxicity Measurement: Co-culture labeled tumor cells with the pre-treated T cells at various Effector:Target (E:T) ratios (e.g., 5:1, 10:1, 20:1) in a 96-well plate for 12-24 hours. Measure specific cell death using a flow cytometry-based assay, such as by staining with propidium iodide (PI) to identify dead CFSE+ tumor cells. Calculate specific cytotoxicity as:
(% PI+ in co-culture - % PI+ in tumor alone) / (100 - % PI+ in tumor alone) * 100.
Signaling Pathway Visualization
The following diagrams illustrate the core mechanisms of two major therapy classes.
Diagram 1: Immunotherapy and Radiotherapy Immune Mechanisms. Left: PD-1/PD-L1 checkpoint blockade. Right: Radiation-induced anti-tumor immunity [119] [8] [6].
Diagram 2: Targeted and Chemotherapy Mechanisms. Targeted therapy inhibits specific oncogenic signaling pathways, while chemotherapy induces DNA damage leading to cell death [118] [120] [117].
The future of oncology lies in the rational combination of therapeutic modalities. The synergy between different classes can overcome resistance and enhance efficacy. Promising strategies include:
- Immunotherapy + Targeted Therapy: Combining ICIs with targeted agents like zanzalintinib (which targets VEGFR, MET, and TAM kinases) has shown survival benefits in metastatic colorectal cancer by modulating the immunosuppressive TME [121].
- Immunotherapy + Radiotherapy: Sequencing lymphatic-sparing radiotherapy with anti-PD-1 immunotherapy can promote dendritic cell migration and activate robust, durable anti-tumor immunity [119].
- Immunotherapy + Chemotherapy: Chemotherapy can induce immunogenic cell death, exposing tumor antigens and enhancing the immune system's ability to recognize cancer, thereby improving the efficacy of subsequent immunotherapy [118].
Other frontiers include the development of novel checkpoint targets (e.g., TIGIT, TIM-3, LAG-3), personalized cancer vaccines using mRNA technology, and leveraging artificial intelligence and radiomics to non-invasively predict patient response [119] [8].
In conclusion, chemotherapy, radiotherapy, targeted therapy, and immunotherapy each occupy a distinct and vital role in the oncologist's arsenal. Their fundamental differences in mechanism of antitumor activity directly dictate their clinical efficacy and toxicity profiles. For the research and drug development community, the path forward requires a deep mechanistic understanding of these modalities to design intelligent combination strategies that effectively reprogram the tumor microenvironment, overcome therapeutic resistance, and ultimately improve outcomes for cancer patients. The integration of multi-omics data, advanced biomarker discovery, and innovative clinical trial designs will be paramount in this endeavor.
Multi-Omics Approaches for Patient Stratification and Prognosis
The profound heterogeneity of tumors represents a fundamental obstacle in clinical oncology, particularly in immunotherapy research where inter-patient variability in treatment response remains substantial [122]. Multi-omics approaches have emerged as transformative methodologies that comprehensively characterize tumor biology by integrating data across multiple molecular layers, including genomics, transcriptomics, epigenomics, proteomics, and spatial omics [123] [124]. These integrated analyses enable researchers to decipher the complex molecular mechanisms underlying antitumor activity and treatment-related toxicity, moving beyond the limitations of single-marker approaches. By capturing the full complexity of tumor ecosystems and their microenvironmental interactions, multi-omics frameworks provide unprecedented opportunities for precise patient stratification and prognostic assessment in immunotherapy trials [122] [125].
Within the context of immunotherapy research, multi-omics technologies enable the systematic investigation of resistance mechanisms and immune-related adverse events by revealing how different molecular layers interact to shape therapeutic outcomes [123]. The integration of these diverse data types through advanced computational methods has facilitated the identification of novel biomarkers, therapeutic targets, and molecular signatures that predict both efficacy and toxicity, ultimately supporting the development of safer, more effective personalized cancer immunotherapies [126] [125].
Multi-Omics Technologies and Methodologies
Core Omics Technologies and Their Applications
Table 1: Core Omics Technologies in Cancer Research
| Omics Layer | Biological Insight | Common Technologies | Clinical Applications in Immunotherapy |
|---|---|---|---|
| Genomics | Identifies DNA sequence variations, mutations, and structural changes | Whole genome/exome sequencing, targeted NGS | Detection of driver mutations, tumor mutational burden, neoantigen prediction [124] |
| Transcriptomics | Analyzes gene expression patterns and RNA regulation | RNA-seq, scRNA-seq, spatial transcriptomics | Immune cell infiltration analysis, cytokine profiling, exhaustion signatures [123] |
| Epigenomics | Maps heritable changes without DNA sequence alteration | scATAC-seq, bisulfite sequencing, CUT&Tag | Characterization of T-cell differentiation states, chromatin accessibility in tumor cells [123] |
| Proteomics | Identifies protein expression, modifications, and interactions | Mass spectrometry, multiplex immunofluorescence, cytometry | Immune checkpoint protein quantification, signaling pathway activity assessment [122] |
| Metabolomics | Profiles small molecule metabolites and metabolic pathways | Mass spectrometry, NMR spectroscopy | Assessment of metabolic competition in TME, nutrient availability for immune cells [124] |
Single-Cell and Spatial Multi-Omics Methodologies
Recent technological advances have enabled multi-omics profiling at single-cell resolution, providing unprecedented insights into cellular heterogeneity within tumors and their microenvironments [123]. Single-cell RNA sequencing (scRNA-seq) allows for the identification of rare immune cell populations and transitional cell states that may influence immunotherapy response and toxicity. For example, the 10x Genomics Chromium X and BD Rhapsody HT-Xpress platforms can profile over one million cells per run, capturing diverse immune cell types and their functional states within the tumor ecosystem [123].
Spatial omics technologies have further enhanced these capabilities by preserving the architectural context of tumor-immune interactions. Multiplex immunohistochemistry/immunofluorescence (mIHC/IF) and spatial transcriptomics enable the mapping of immune cell localization, cell-cell communication, and functional niches within the tumor microenvironment [122] [125]. These spatial approaches are particularly valuable for understanding the mechanisms of immune exclusion and identifying patterns associated with both efficacy and immune-related adverse events.
Experimental Protocol: Integrated Single-Cell and Spatial Analysis
- Tissue Processing: Collect fresh tumor tissue biopsies and generate single-cell suspensions using enzymatic digestion (collagenase IV/DNase I) with viability maintenance [123].
- Single-Cell Partitioning: Utilize microfluidic platforms (10x Genomics Chromium) for single-cell partitioning with cell barcoding [123].
- Multi-Omic Library Preparation: Simultaneously profile transcriptome (scRNA-seq) and surface protein expression (CITE-seq) using antibody-derived tags [123].
- Satial Validation: Process adjacent tissue sections for spatial transcriptomics (Visium) and multiplex IHC (CODEX/IMC) to preserve spatial context [122].
- Data Integration: Combine single-cell and spatial data using computational integration tools (Seurat, Harmony) to reconstruct spatial relationships of identified cell states [123].
Computational Integration and Machine Learning Approaches
Data Integration Strategies and Machine Learning Frameworks
The integration of multi-omics datasets requires sophisticated computational approaches to effectively combine heterogeneous data types and extract biologically meaningful insights. Several machine learning frameworks have been successfully applied to multi-omics integration for patient stratification:
Table 2: Machine Learning Approaches for Multi-Omics Integration
| Integration Strategy | Machine Learning Methods | Applications in Patient Stratification | Advantages |
|---|---|---|---|
| Early Integration | Random Forest, Support Vector Machines | Combining all omics data as input features for supervised learning | Preserves potential inter-omics interactions; simple implementation [127] |
| Intermediate Integration | Multi-Omics Factor Analysis, Joint Matrix Decomposition | Identifying shared latent factors across omics data types | Dimensionality reduction; captures coordinated variations [126] |
| Late Integration | Stacked Generalization, Ensemble Methods | Training separate models per omics type then combining predictions | Leverages omics-specific patterns; robust to missing data [127] |
| Hierarchical Integration | Graph Neural Networks, Multi-layer Autoencoders | Modeling biological hierarchy from DNA to protein/metabolite | Reflects biological flow of information; captures nonlinear relationships [122] |
A representative example of these approaches comes from gastric cancer research, where Wang et al. applied ten machine learning algorithms to multi-omics data to develop the Gastric Cancer Multi-Omics Programmed Cell Death Signature (GMPS) [126]. Their analysis integrated transcriptomic, epigenetic, and somatic mutation data using consensus clustering, followed by the application of 99 machine learning models to identify robust prognostic signatures associated with programmed cell death pathways. This signature notably correlated with patient survival rates, tumor mutational burden, and copy number variations, demonstrating substantial predictive power for immunotherapy response [126].
Visualization of Multi-Omics Integration Workflow
Multi-Omics Data Integration Workflow
Experimental Protocols for Multi-Omics Studies
Comprehensive Multi-Omics Profiling Protocol
Study Design and Sample Collection
- Patient Cohort Selection: Recruit patients scheduled for immunotherapy following institutional ethics approval. Collect comprehensive clinical data including prior treatments, performance status, and routine laboratory parameters [125].
- Baseline Sample Collection: Obtain tumor biopsies (core needle or surgical) prior to treatment initiation. Collect matched peripheral blood (PBMC) and plasma samples. Preserve tissue aliquots in multiple formats: fresh-frozen (OCT), RNAlater, formalin-fixed paraffin-embedded (FFPE) [126] [125].
- Longitudinal Sampling: For response and toxicity monitoring, collect peripheral blood at predetermined intervals (e.g., every 2-3 treatment cycles) and at time of progression or toxicity onset [125].
Multi-Omics Data Generation
- Genomic Profiling: Extract DNA from tumor tissue and matched normal (blood). Perform whole exome sequencing (150bp paired-end) at minimum 100x coverage. Identify somatic mutations, copy number variations, and neoantigens using established pipelines (GATK, Mutect2) [126] [124].
- Transcriptomic Profiling: Extract total RNA (RIN > 7). Perform bulk RNA-seq (100M reads/sample) and single-cell RNA-seq (10x Genomics) on selected samples. Quantify gene expression, alternative splicing, and immune cell deconvolution (CIBERSORTx) [123] [126].
- Epigenomic Profiling: Perform reduced-representation bisulfite sequencing (RRBS) or whole-genome bisulfite sequencing for DNA methylation analysis. Conduct scATAC-seq on fresh tumor tissue to assess chromatin accessibility in immune and tumor cells [123] [126].
- Proteomic Profiling: Utilize high-parameter mass spectrometry (LC-MS/MS) or Olink panels to quantify protein expression. Perform multiplex immunofluorescence (mIHC) on FFPE sections for spatial protein localization (Panel: CD8, CD4, CD68, PD-L1, PD-1, Pan-CK) [122] [125].
- Data Integration: Apply integration frameworks (MOVICS R package) to harmonize multi-omics data. Use graph neural networks (IntegrAO) for classification even with incomplete datasets [122] [126].
Reagent and Resource Solutions
Table 3: Essential Research Reagents for Multi-Omics Studies
| Category | Specific Reagents/Platforms | Application | Considerations |
|---|---|---|---|
| Single-Cell Isolation | Collagenase IV, DNase I, 10x Genomics Chromium, FACS antibodies | Tissue dissociation and single-cell partitioning | Maintain cell viability; minimize stress-induced artifacts [123] |
| Nucleic Acid Extraction | AllPrep DNA/RNA/miRNA kits, FFPE RNA extraction kits | Simultaneous DNA/RNA extraction from limited samples | Preserve RNA integrity; address FFPE degradation [126] |
| Library Preparation | Illumina TruSeq, SMARTer kits, 10x Barcoded reagents | Preparation of sequencing libraries | UMIs for quantification; unique dual indexes to reduce index hopping [123] |
| Spatial Profiling | CODEX/IMC antibodies, 10x Visium slides, RNAscope probes | Spatial context preservation | Antibody validation; tissue morphology preservation [122] |
| Computational Tools | MOVICS, Seurat, Scanpy, CIBERSORTx, Graph neural networks | Data integration and analysis | Reproducible workflows; containerization (Docker/Singularity) [122] [126] |
Clinical Applications in Immunotherapy
Patient Stratification for Immunotherapy Response
Multi-omics approaches have demonstrated significant utility in identifying patient subgroups most likely to benefit from immunotherapy while predicting those at risk for immune-related adverse events. In pancreatic ductal adenocarcinoma (PDAC), which typically shows limited response to immune checkpoint inhibitors, integrated analysis of transcriptomic profiles and immune cell composition via multiplex immunohistochemistry revealed distinct tumor microenvironment subtypes [125]. Specifically, patients showing partial response to combination immunochemotherapy exhibited increased intratumoral infiltration of CD8+ T cells and CD137+ CD8+ T cells, along with upregulation of HPX and RFXAP genes, while interleukin-6 (IL-6) expression was associated with poor prognosis [125].
Similar approaches in gastric cancer have identified programmed cell death (PCD) signatures that correlate with tumor mutational burden, copy number variations, and immune therapy response [126]. The GMPS signature, derived from multi-omics integration, successfully stratified patients into distinct prognostic subgroups and predicted sensitivity to various therapeutic agents, providing a framework for personalized treatment selection [126].
Mechanisms of Antitumor Activity and Toxicity
Multi-omics analyses provide unprecedented insights into the molecular mechanisms underlying both effective antitumor immunity and treatment-limiting toxicities. Single-cell multi-omics approaches have elucidated how tumor heterogeneity drives differential treatment responses by revealing distinct immune cell states and transcriptional programs associated with efficacy versus resistance [123]. For example, integrated single-cell RNA and spatial transcriptomics analyses in gastric cancer revealed B-cell subpopulations and tumor B-cell interactions as key modulators of the immune microenvironment [122].
Visualization of these complex relationships can be achieved through pathway diagrams that illustrate the molecular networks connecting multi-omics features to clinical outcomes:
Multi-Omics Determinants of Immunotherapy Outcomes
These integrative approaches enable researchers to move beyond correlative associations toward causal mechanistic understanding. For instance, multi-omics analyses have revealed how specific genomic alterations in tumor cells (e.g., PTEN loss, β-catenin activation) create immunologically "cold" microenvironments by suppressing T-cell infiltration, while distinct transcriptional programs in immune cells (e.g., chronic interferon signaling) drive T-cell exhaustion and resistance to checkpoint blockade [122] [123]. Similarly, integrated analyses have begun to unravel the molecular basis of immune-related adverse events, identifying shared autoimmune pathways that become activated during effective antitumor immunity, providing potential targets for therapeutic intervention to separate efficacy from toxicity [125].
Multi-omics approaches represent a paradigm shift in patient stratification and prognosis for cancer immunotherapy. By integrating comprehensive molecular profiles across genomic, transcriptomic, epigenomic, proteomic, and spatial dimensions, these methods provide unprecedented resolution of the complex mechanisms governing antitumor activity and treatment-related toxicity. The continued refinement of single-cell technologies, spatial profiling methods, and computational integration frameworks will further enhance our ability to identify clinically relevant patient subgroups and predictive biomarkers.
Future developments in multi-omics research will likely focus on dynamic profiling throughout treatment courses to capture evolving adaptations in both tumor and immune cells, standardized frameworks for data integration and interpretation, and the incorporation of artificial intelligence approaches to extract maximum biological insight from these complex datasets. As these technologies become more accessible and cost-effective, multi-omics profiling is poised to transition from research applications to clinical practice, ultimately enabling truly personalized immunotherapy approaches that maximize efficacy while minimizing adverse events.
Addressing Interindividual Variability and Tumor-Context Specificity
The efficacy of cancer immunotherapy is fundamentally constrained by two layers of biological complexity: interindividual variability in host responses and tumor-context specificity in therapeutic susceptibility. Despite the paradigm-shifting clinical success of immune checkpoint inhibitors (ICIs) and adoptive cell therapies, the overall clinical response rate remains limited to 20-30% of patients, with significant variation observed across cancer types and individuals [128] [6]. This variability stems from a complex interplay of host-specific factors—including gut microbiome composition, immune repertoire, and metabolic status—and tumor-intrinsic features—such as genetic alterations, tumor microenvironment (TME) composition, and immune evasion mechanisms [129] [130]. The immunosuppressive TME represents a critical barrier to effective immunotherapy, employing multiple mechanisms to inhibit antitumor immunity, including metabolic reprogramming, immune checkpoint expression, and recruitment of immunosuppressive cells [131] [6]. Understanding and addressing these sources of heterogeneity is paramount for developing personalized immunotherapeutic strategies that can overcome resistance mechanisms and benefit broader patient populations.
Table 1: Major Sources of Variability in Immunotherapy Response
| Variability Category | Specific Factors | Impact on Treatment |
|---|---|---|
| Host-Specific Factors | Gut microbiome composition [129] | Modulates ICI efficacy via microbial metabolites |
| Immune repertoire and competence [130] | Determines capacity for antitumor response | |
| Metabolic and nutritional status [132] | Influences immune cell function and persistence | |
| Tumor-Context Factors | Genetic and epigenetic landscape [128] | Affects antigen presentation and immune recognition |
| TME composition and immunosuppression [131] [6] | Creates physical and functional barriers to immunity | |
| Tumor mutational burden and neoantigens [128] | Determines immunogenicity and T cell recognition |
Mechanisms of Variability and Resistance
Microbial Determinants of Response Heterogeneity
The gut microbiome critically regulates antitumor immunity through metabolic byproducts that serve as pivotal mediators of host-microbe crosstalk [129] [132]. These microbial metabolites exhibit profound functional duality, where the same metabolite can exert opposing immunomodulatory effects depending on concentration gradients, tissue-specific receptor expression, and the metabolic microenvironment. This context dependency explains the frequently observed divergent responses to immunotherapy across individuals [132]. Key metabolite classes include short-chain fatty acids (SCFAs) like butyrate, which enhances ICI efficacy through epigenetic modulation via histone deacetylase (HDAC) inhibition; tryptophan derivatives such as kynurenine, which drives resistance by polarizing macrophages toward an immunosuppressive phenotype; and bile acids, whose balance between primary and secondary forms dictates immune tone in the TME [129] [132]. The concentration-dependent effects of these metabolites create a complex regulatory network where therapeutic outcomes cannot be predicted from mere presence or absence but require precise quantification of metabolic gradients and receptor expression patterns across tumor types.
Tumor Microenvironment-Mediated Resistance
The TME fosters immune resistance through multiple interconnected mechanisms that exhibit significant context specificity [131] [6]. A primary resistance mechanism involves metabolic reprogramming wherein tumors create a metabolically hostile environment for immune cells. Lactate accumulation from aerobic glycolysis lowers extracellular pH, directly inhibiting T cell activation, proliferation, and cytokine production [6]. This acidic environment also promotes the polarization of immunosuppressive macrophages (M2 phenotype) and expands regulatory T cells (Tregs), further dampening antitumor immunity [6]. Additionally, ammonia—a byproduct of glutaminolysis in rapidly proliferating cells—induces a unique form of T cell death through lysosomal alkalization and mitochondrial damage, thereby limiting the efficacy of T cell-based immunotherapies [6]. Beyond metabolic suppression, tumors actively recruit and expand immunosuppressive cellular populations including Tregs and myeloid-derived suppressor cells (MDSCs), which inhibit effector T cells and natural killer (NK) cells through multiple mechanisms including cytokine secretion (IL-10, TGF-β), expression of immune checkpoints, and nutrient depletion [131] [6].
Immune Checkpoint Regulation
Tumor cells exploit physiological immune checkpoint pathways to evade immune destruction, with pronounced heterogeneity in checkpoint expression across cancer types and individual patients [131] [128]. While CTLA-4 and PD-1/PD-L1 represent the most extensively characterized checkpoints, numerous additional inhibitory molecules contribute to immune evasion, including LAG-3, TIM-3, TIGIT, and VISTA [131]. The expression patterns of these checkpoints are dynamically regulated by oncogenic signaling pathways and inflammatory cytokines within the TME. For instance, activation of the PI3K/AKT pathway in tumor cells can lead to increased PD-L1 expression, while IFN-γ in the TME can upregulate multiple checkpoint molecules simultaneously [6]. This complexity underscores the limitation of single-checkpoint targeting and highlights the need for comprehensive immune profiling to guide appropriate combination strategies tailored to the specific checkpoint landscape of individual tumors.
Assessment Methodologies
Multi-Omics Profiling Technologies
Comprehensive characterization of the factors underlying immunotherapy variability requires integrated multi-omics approaches that capture the complexity of tumor-immune interactions [129] [130]. Genomic profiling establishes the foundation by identifying tumor mutational burden, neoantigen landscape, and genetic alterations in immune-related pathways that may influence treatment response [128]. Microbiome sequencing (16S rRNA and shotgun metagenomics) enables characterization of microbial community structure and functional potential, with specific attention to taxa associated with immunotherapy response [129] [132]. Metabolomic profiling through mass spectrometry-based platforms quantifies the levels of immunomodulatory microbial metabolites (SCFAs, tryptophan derivatives, bile acids) in circulation and within the TME, providing functional readouts of host-microbe interactions [129] [132]. Single-cell RNA sequencing reveals the cellular composition and functional states of immune cells within the TME, enabling identification of resistant cell populations and therapeutic targets [130]. Epigenetic profiling assesses chromatin accessibility and histone modifications that regulate immune cell function and may be modulated by microbial metabolites [132]. The integration of these datasets through advanced computational methods is essential for developing predictive models of therapy response and resistance.
Table 2: Experimental Protocols for Assessing Variability Factors
| Methodology | Key Parameters | Application in Variability Assessment |
|---|---|---|
| 16S rRNA Microbiome Sequencing | DNA extraction, PCR amplification, sequencing, taxonomic assignment | Identifies microbial taxa associated with ICI response; requires standardized sample collection [129] |
| Mass Spectrometry-Based Metabolomics | Metabolite extraction, LC-MS/MS analysis, quantification | Measures immunomodulatory metabolites; establishes concentration-effect relationships [132] |
| Multiplex Immunofluorescence | Antibody panel validation, tissue staining, multispectral imaging | Spatial profiling of immune cells in TME; reveals context-specific immune architecture [128] |
| Single-Cell RNA Sequencing | Tissue dissociation, cell capture, library prep, bioinformatic analysis | Characterizes immune cell heterogeneity; identifies resistant subpopulations [130] |
Functional Assays for Mechanism Validation
Beyond correlative profiling, functional validation of identified mechanisms is crucial for establishing causality and developing targeted interventions. In vitro co-culture systems incorporating tumor cells, immune cells, and microbial metabolites enable dissection of specific immune-modulatory mechanisms under controlled conditions [132]. For metabolite screening, primary human T cells are cultured with physiological concentrations of microbial metabolites (e.g., 1-10 mM butyrate, 10-100 μM kynurenine) alongside tumor target cells, with immune cell function assessed through flow cytometric analysis of activation markers, cytokine production, and cytotoxic activity [132]. Organoid-based models that incorporate patient-derived tumor cells, immune cells, and microbiota components offer more physiologically relevant systems for studying patient-specific responses [129]. For TME metabolic studies, extracellular flux analyzers can simultaneously measure glycolytic and oxidative metabolic rates in immune and tumor cells under TME-mimetic conditions (low glucose, acidic pH, high lactate), revealing metabolic restrictions on immune function [6]. In vivo validation using gnotobiotic mouse models colonized with defined microbial communities from patient responders and non-responders provides a platform for establishing causal relationships between specific microbiota configurations and therapy outcomes [129] [132].
Therapeutic Strategies
Precision Microbiome Engineering
Targeted manipulation of the gut microbiome represents a promising approach for overcoming interindividual variability in immunotherapy response [129] [132]. Probiotic formulations containing defined bacterial species (e.g., Akkermansia muciniphila, Bifidobacterium spp.) associated with improved ICI outcomes can be administered as adjunctive therapy to potentiate antitumor immunity [129]. Prebiotic interventions involving specific dietary fibers (e.g., inulin, resistant starch) that promote the expansion of beneficial taxa and increase production of immunostimulatory metabolites like butyrate offer a complementary approach [132]. For more precise manipulation, fecal microbiota transplantation (FMT) from validated responders to non-responders has demonstrated feasibility in clinical studies and can reverse resistance to ICIs [129]. Looking toward the future, synthetic microbial consortia composed of rationally selected bacterial strains with complementary immunomodulatory functions are being developed to provide more consistent and controllable modulation of antitumor immunity [129] [132]. These approaches require careful matching of microbial interventions to individual patient's baseline microbiota composition and metabolic capacity to ensure engraftment and functionality.
Context-Tailored Combination Therapies
Overcoming the immunosuppressive TME requires combination strategies specifically tailored to the resistance mechanisms operative in individual tumor contexts [130] [6]. For tumors with predominant metabolic immunosuppression, combination approaches may include ICI together with inhibitors of lactic acid production (e.g., LDHA inhibitors) or agents that neutralize the acidic TME (e.g., proton pump inhibitors, bicarbonate) [6]. For tumors with multiple immune checkpoint expression, rational combinations of ICIs targeting complementary pathways (e.g., anti-PD-1 + anti-LAG-3) may be more effective than monotherapy [131] [128]. In contexts characterized by suppressive cellular populations, ICIs can be combined with agents that selectively deplete Tregs or MDSCs, or that reprogram their function [131] [6]. Emerging approaches also include combining ICIs with metabolic modulators that enhance T cell function in the TME, such as IL-Arg supplementation to counter MDSC-mediated arginine depletion or PI3Kγ inhibitors to reprogram macrophage polarization [132] [6]. The successful implementation of these strategies requires comprehensive immune profiling to identify the dominant resistance mechanisms in individual patients and match them with appropriate targeted interventions.
Framework for Addressing Variability in Immunotherapy
The Scientist's Toolkit
Table 3: Essential Research Reagents and Platforms
| Research Tool | Specific Application | Function in Variability Research |
|---|---|---|
| Gnotobiotic Mouse Models | Causal microbiome studies | Enables colonization with defined human microbiota to establish mechanism [129] |
| Extracellular Flux Analyzer | TME metabolic profiling | Measures real-time glycolytic and oxidative metabolism in immune cells [6] |
| Mass Cytometry (CyTOF) | High-dimensional immune profiling | Simultaneous measurement of 40+ immune cell markers in limited samples [130] |
| 3D Tumor Organoid Co-cultures | Patient-specific response modeling | Incorporates patient-derived tumor, immune, and microbial components [132] |
| LC-MS/MS Platforms | Metabolite quantification | Precise measurement of immunomodulatory metabolites in biospecimens [129] |
Addressing interindividual variability and tumor-context specificity represents the next frontier in cancer immunotherapy. The integration of multi-omics profiling, functional validation assays, and context-tailored therapeutic interventions provides a roadmap for overcoming the current limitations of immunotherapy. Precision microbiome engineering, informed by comprehensive metabolic and microbial profiling, offers novel avenues for modulating host-specific factors to enhance treatment efficacy [129] [132]. Simultaneously, targeting the diverse resistance mechanisms operative within specific tumor microenvironments through rational combination strategies promises to overcome context-dependent immunosuppression [130] [6]. The continued development and refinement of the experimental tools and analytical frameworks described herein will be essential for advancing toward truly personalized immunotherapy approaches that can maximize clinical benefit across diverse patient populations and cancer types.
Conclusion
The dynamic interplay between potent antitumor immunity and off-target toxicity defines the current landscape of cancer immunotherapy. A deep mechanistic understanding of immune checkpoint biology, the immunosuppressive tumor microenvironment, and the role of the host microbiome is crucial for advancing the field. Future progress hinges on the development of sophisticated strategies to separate efficacy from toxicity, including precision microbiome engineering, advanced biomarker-driven patient selection, and novel combination regimens that normalize the tumor vasculature and remodel the TME. Embracing artificial intelligence for multi-omics data integration and prioritizing cardio-oncology surveillance will be paramount. The next frontier lies in personalizing immunotherapy to maximize durable responses while minimizing adverse events, ultimately expanding its curative potential to a broader range of cancer patients.
References
- 1. Current state of cancer immunity cycle: new strategies and ... [https://pubmed.ncbi.nlm.nih.gov/40124373/]
- 2. The cancer-immunity cycle: Indication, genotype, and ... [https://www.sciencedirect.com/science/article/pii/S1074761323004168]
- 3. Enhancing the cancer-immunity cycle through innovative ... [https://www.news-medical.net/news/20251114/Enhancing-the-cancer-immunity-cycle-through-innovative-vaccines.aspx]
- 4. Current state of cancer immunity cycle: new strategies and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1535464/full]
- 5. Therapeutic targeting of cell death-immune crosstalk in cancer ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02491-8]
- 6. Immune evasion in cancer: mechanisms and cutting-edge ... [https://www.nature.com/articles/s41392-025-02280-1]
- 7. Quantitative cancer-immunity cycle modeling for predicting ... [https://www.nature.com/articles/s41540-025-00513-1]
- 8. Advances and challenges in cancer immunotherapy [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1602529/full]
- 9. CTLA-4 and PD-1 Pathways - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4892769/]
- 10. Regulatory mechanisms of immune checkpoints PD-L1 and ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-021-01987-7]
- 11. Dual blockade immunotherapy targeting PD-1/PD-L1 and ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-024-01581-2]
- 12. Current Understanding of Cytotoxic T Lymphocyte Antigen-4 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9385567/]
- 13. Current understanding of CTLA-4: from mechanism to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1198365/full]
- 14. PD-1/PD-L1 pathway: current researches in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7136921/]
- 15. Regulatory mechanisms of PD-1/PD-L1 in cancers [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02023-w]
- 16. Immune Checkpoint Molecules: A Review on Pathways ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004596/]
- 17. Unraveling the immune evasion mechanisms in the tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1597202/full]
- 18. Stromal cells in the tumor microenvironment [https://www.nature.com/articles/s41419-023-06110-6]
- 19. Immune evasion in cancer: mechanisms and cutting-edge ... [https://pubmed.ncbi.nlm.nih.gov/40739089/]
- 20. Immune evasion through mitochondrial transfer in the ... [https://www.nature.com/articles/s41586-024-08439-0]
- 21. Dual Relationship Between Stromal Cells and Immune Cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9019709/]
- 22. Immune Checkpoint Inhibitors and Their Side Effects [https://www.cancer.org/cancer/managing-cancer/treatment-types/immunotherapy/immune-checkpoint-inhibitors.html]
- 23. Adverse effects of immune-checkpoint inhibitors [https://www.nature.com/articles/s41571-019-0218-0]
- 24. Quantitative response assessment of combined ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-025-00597-8]
- 25. Recent advances in tumor immunotherapy based on NK cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1595533/full]
- 26. Natural Killer Cell-Mediated Antitumor Immunity: Molecular ... [https://pubmed.ncbi.nlm.nih.gov/40959206/]
- 27. Dual roles and therapeutic targeting of tumor-associated ... [https://www.nature.com/articles/s41392-025-02325-5]
- 28. M1 macrophages – unexpected contribution to tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350380/]
- 29. Dendritic Cell Immunotherapy for Solid Tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564614/]
- 30. Dendritic cell progenitors engineered to express ... [https://www.nature.com/articles/s41467-025-64172-w]
- 31. Gut microbiota shapes cancer immunotherapy responses [https://www.nature.com/articles/s41522-025-00786-8]
- 32. Clinical Evidence for Microbiome-Based Strategies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471457/]
- 33. A Review of Cancer Immunotherapy Toxicity - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8455777/]
- 34. Harnessing the Gut Microbiome in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394882/]
- 35. Microbiome meets immunotherapy: unlocking the hidden ... [https://www.nature.com/articles/s41522-025-00819-2]
- 36. The gut microbiome and cancer response to immune ... [https://www.jci.org/articles/view/184321]
- 37. Gut microbiota and metabolites signatures of clinical response ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00607-8]
- 38. Microbiota-derived metabolites: Key modulators of cancer ... [https://pubmed.ncbi.nlm.nih.gov/40695291/]
- 39. The Gut Microbiome as a Biomarker and Therapeutic ... [https://www.mdpi.com/2073-4409/14/22/1779]
- 40. Strategic modulation of the gastrointestinal microbiome to ... [https://www.sciencedirect.com/science/article/pii/S1359644625002417]
- 41. Mechanisms of immune checkpoint inhibitors: insights into ... [https://www.nature.com/articles/s41419-023-06389-5]
- 42. Advances in cancer immunotherapy: historical perspectives ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02305-x]
- 43. Overcoming resistance to PD-1 and CTLA-4 blockade ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1688699/full]
- 44. Combination of PD-1/PD-L1 and CTLA-4 inhibitors in the ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1680838/full]
- 45. Immune mechanisms of toxicity from checkpoint inhibitors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10330206/]
- 46. Immune checkpoint inhibitors in cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178997/]
- 47. Research progress and future perspectives of prodrug ... [https://www.sciencedirect.com/science/article/pii/S1040842825002938]
- 48. Advances in cancer immunotherapy: historical perspectives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057291/]
- 49. CAR T Cells: Engineering Immune Cells to Treat Cancer [https://www.cancer.gov/about-cancer/treatment/research/car-t-cells]
- 50. CAR-T cell therapy for cancer: current challenges and ... [https://www.nature.com/articles/s41392-025-02269-w]
- 51. Tumour-infiltrating lymphocyte therapy comes of age in the ... [https://pubmed.ncbi.nlm.nih.gov/41167225/]
- 52. Unlocking the potential of engineered immune cell therapy ... [https://www.nature.com/articles/s41467-025-56527-0]
- 53. Adoptive T cell therapy for solid tumors - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10972864/]
- 54. Adoptive cell therapy for cancer: combination strategies ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1603792/full]
- 55. CAR-T and CAR-NK as cellular cancer immunotherapy for ... [https://www.nature.com/articles/s41423-024-01207-0]
- 56. Recent advances in adoptive cell therapy for cancer ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1665488/full]
- 57. Technological advancements in antibody-based therapeutics ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-025-01190-2]
- 58. Impact of Monoclonal Antibody Aggregates on Effector ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12015860/]
- 59. Current Landscape and Future Directions in Cancer ... [https://www.mdpi.com/2072-6694/17/5/821]
- 60. Advances in Techniques for the Structure and Functional ... [https://www.mdpi.com/2227-9059/13/9/2055]
- 61. Revolutionizing cancer therapy: Monoclonal antibodies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501477/]
- 62. 2025 Cancer Immunotherapy Insights + Impact Report [https://www.cancerresearch.org/blog/cancer-immunotherapy-insights-impact-2025-report]
- 63. Cancer vaccines: current status and future directions [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01670-w]
- 64. Eliciting antitumor immunity via therapeutic cancer vaccines [https://www.nature.com/articles/s41423-025-01316-4]
- 65. Current Progress and Future Perspectives of RNA-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12153701/]
- 66. Microorganism delivery of cancer vaccines [https://www.sciencedirect.com/science/article/abs/pii/S0168365925009010]
- 67. Cancer researchers shape emerging strategies for ... [https://news.vt.edu/articles/2025/10/research-fralinbiomed-cancerreview-10032025.html]
- 68. The Role of Immune Checkpoint Inhibitors in Cancer Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497686/]
- 69. A real-world cohort study of immune-related adverse ... [https://www.nature.com/articles/s41698-025-01123-0]
- 70. Recent advances in biomarkers for predicting the efficacy ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554871/full]
- 71. NK cell adaptation in the tumor microenvironment:Insights ... [https://www.sciencedirect.com/science/article/abs/pii/S1359610125001376]
- 72. NKG2D CAR-NK adoptive cellular immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540238/]
- 73. NK-derived exosomes in anti-tumor strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12335398/]
- 74. Phenotypes, mechanisms, and therapeutic strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538774/]
- 75. Interplay Between NK Cell Activity and Cancer Onset ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468143/]
- 76. NK cell-derived extracellular vesicles enhance cytotoxicity ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1633010/full]
- 77. NK cell-derived artificial extracellular vesicles elicit potent anti ... [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00328-z]
- 78. Safety and efficacy of extracellular vesicles in individuals ... [https://pubmed.ncbi.nlm.nih.gov/40256224/]
- 79. T cell-mediated mechanisms of immune-related adverse ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825001969]
- 80. Current status of management of immune-related adverse ... [https://www.cancerbiomed.org/content/early/2025/09/23/j.issn.2095-3941.2025.0346]
- 81. Autoimmune-related adverse events induced by immune ... [https://www.sciencedirect.com/science/article/abs/pii/S0952791525000329]
- 82. Predictive factors and outcomes of immune-related ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1655724/full]
- 83. ICI-induced cardiovascular toxicity: mechanisms and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1550400/full]
- 84. Pathophysiology of Immune Checkpoint Inhibitor-Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9497311/]
- 85. Mechanisms of Cardiovascular Toxicities Associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8159878/]
- 86. Immune checkpoint inhibitor-induced myocarditis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12624509/]
- 87. Immunotherapy-associated cardiovascular toxicities [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1347140/full]
- 88. Cardiovascular Toxicities with Chimeric Antigen Receptor T ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10201875/]
- 89. Management of Cytokine Release Syndrome (CRS ... [https://link.springer.com/article/10.1007/s44272-025-00044-0]
- 90. Cardiovascular complications of cellular immunotherapies ... [https://www.nature.com/articles/s44325-025-00057-7]
- 91. Immune-Related Adverse Events Due to Cancer ... [https://www.mdpi.com/2072-6694/16/7/1440]
- 92. Immune-related adverse events occurring rapidly after a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458726/]
- 93. Associations between immune checkpoint inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083316/]
- 94. The Current and Future of Biomarkers of Immune Related ... [https://pubmed.ncbi.nlm.nih.gov/40287170/]
- 95. PPP2R1A mutations portend improved survival after ... [https://www.nature.com/articles/s41586-025-09203-8]
- 96. The molecular and functional landscape of resistance to ... [https://www.nature.com/articles/s41467-023-36979-y]
- 97. Local therapy overcomes primary resistance to target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511485/]
- 98. Resistance mechanisms to immune checkpoint inhibitors [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02212-7]
- 99. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12167185/]
- 100. Microbiome Integrity Enhances the Efficacy and Safety of ... [https://www.mdpi.com/2227-9059/13/2/422]
- 101. Combination strategies of gut microbiota in cancer therapy ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02275-z]
- 102. Microbiome-targeted nanoplatforms and engineering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574306/]
- 103. Microbiome engineering: unlocking therapeutic potential in ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1610029/full]
- 104. Mechanisms, combination therapy, and biomarkers in cancer ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01711-w]
- 105. Overview on Immunotherapy Biomarkers [https://www.linkedin.com/pulse/overview-immunotherapy-biomarkers-xiamenspacegen-decxc]
- 106. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 107. Clinicopathological characteristics and the relationship of PD - L status... 1 [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13938-y]
- 108. Microsatellite instability (MSI) and the tumor mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170210/]
- 109. Tumor Mutational Burden (TMB) as a Predictive Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7710563/]
- 110. in Pancreatic Cancer: Why Do We Keep Failing? Immunotherapy [https://pubmed.ncbi.nlm.nih.gov/35626033/]
- 111. Clinical Trial Endpoints in Cancer Research: Four Terms ... [https://www.astrazeneca-us.com/media/astrazeneca-us-blog/2018/clinical-trial-endpoints-in-cancer-research-four-terms-you-should-know-09242018.html]
- 112. Clinical endpoints in oncology - a primer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8085844/]
- 113. Recent Advances in Molecular Mechanisms of Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10216302/]
- 114. Immune mechanisms of toxicity from checkpoint inhibitors [https://pubmed.ncbi.nlm.nih.gov/37117135/]
- 115. Quantitative Imaging in Cancer Clinical Trials - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4717912/]
- 116. Highly variable timing renders immunotherapy efficacy and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1351739/full]
- 117. Exploring treatment options in cancer: tumor ... [https://www.nature.com/articles/s41392-024-01856-7]
- 118. Immunotherapy and Chemotherapy: What's the Difference? [https://www.cancerresearch.org/blog/difference-cancer-immunotherapy-and-chemotherapy]
- 119. MD Anderson experts spotlight key immunotherapy ... [https://www.mdanderson.org/newsroom/research-newsroom/md-anderson-experts-spotlight-key-immunotherapy-advances-at-2025.h00-159781179.html]
- 120. Targeted Therapy Vs. Immunotherapy In Oncology [https://globalrph.com/2025/03/targeted-therapy-vs-immunotherapy-in-oncology-advancements-and-comparisons-since-2022/]
- 121. ESMO 2025: Combination of immunotherapy and targeted ... [https://ecancer.org/en/news/27160-esmo-2025-combination-of-immunotherapy-and-targeted-therapy-improves-survival-for-patients-with-advanced-colorectal-cancer]
- 122. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 123. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376342/]
- 124. Navigating Cancer Complexity: Integrative Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553891/]
- 125. Multi-omics analyses inform mechanisms of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1673098/full]
- 126. Multiomics integration and machine learning reveal ... [https://www.nature.com/articles/s41598-024-82233-w]
- 127. Machine learning and multi-omics integration [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06425-2]
- 128. Therapeutic targets and biomarkers of tumor immunotherapy [https://www.nature.com/articles/s41392-022-01136-2]
- 129. Microbial metabolite-driven immune reprogramming in ... [https://pubmed.ncbi.nlm.nih.gov/41181090/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0p-7UVx6Uy-7CMGz2GkN-MTRkDXGnozxjWNzRjIwxvW&fc=None&ff=20251105123111&v=2.18.0.post22+67771e2]
- 130. SITC vision: Opportunities for deeper understanding of ... [https://pubmed.ncbi.nlm.nih.gov/40562704/]
- 131. Advances and challenges in cancer immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12202542/]
- 132. Microbial metabolite-driven immune reprogramming in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1603658/full]