BCMA-Targeted Therapies in Multiple Myeloma: A Comprehensive 2024 Review of CAR-T Efficacy, BiTE Safety, and Clinical Implications
This article provides a detailed comparative analysis of B-cell maturation antigen (BCMA)-targeted immunotherapies for relapsed/refractory multiple myeloma, focusing on chimeric antigen receptor T-cell (CAR-T) therapies and bispecific T-cell engagers (BiTEs).
BCMA-Targeted Therapies in Multiple Myeloma: A Comprehensive 2024 Review of CAR-T Efficacy, BiTE Safety, and Clinical Implications
Abstract
This article provides a detailed comparative analysis of B-cell maturation antigen (BCMA)-targeted immunotherapies for relapsed/refractory multiple myeloma, focusing on chimeric antigen receptor T-cell (CAR-T) therapies and bispecific T-cell engagers (BiTEs). Tailored for researchers and drug development professionals, we explore the foundational biology of BCMA, the distinct mechanisms of action for each modality, and the latest clinical trial data on efficacy (overall response rate, progression-free survival, minimal residual disease negativity) and safety profiles (cytokine release syndrome, immune effector cell-associated neurotoxicity syndrome, infections). We delve into methodological considerations for clinical application, optimization strategies to manage toxicities and overcome resistance, and a direct head-to-head comparison of real-world outcomes. The conclusion synthesizes the current therapeutic landscape and outlines future directions for biomarker development, next-generation constructs, and combination strategies.
BCMA 101: Unpacking the Biology and Target Rationale for CAR-T and BiTE Therapies in Myeloma
The Central Role of BCMA in Multiple Myeloma Pathogenesis and Plasma Cell Survival
Within the thesis on comparing BCMA-targeted CAR-T and BiTE (bispecific T-cell engager) immunotherapies, understanding BCMA's (B-cell maturation antigen) central role is foundational. This guide compares the functional consequences of BCMA signaling versus related receptors in plasma cell survival, using experimental data to contextualize the rationale for its therapeutic targeting.
Comparison Guide: BCMA vs. Alternative Survival Receptors in Plasma Cells
BCMA, a member of the TNF receptor superfamily, is not the sole survival receptor for plasma cells. Its relatives, TACI (Transmembrane Activator and CAML Interactor) and BAFF-R (B-cell Activating Factor Receptor), also bind the ligands BAFF (B-cell Activating Factor) and APRIL (A Proliferation-Inducing Ligand). However, BCMA demonstrates unique specificity and downstream signaling potency that underpins its non-redundant role in long-lived plasma cell and multiple myeloma (MM) cell survival.
Table 1: Functional Comparison of BAFF/APRIL Receptors in Plasma Cell Biology
| Receptor | Primary Ligands | Expression Pattern on Plasma Cells / MM Cells | Key Downstream Pathways | Net Effect on Plasma Cell Survival & MM Pathogenesis | Supporting Experimental Data (Example) |
|---|---|---|---|---|---|
| BCMA | APRIL, BAFF | High on long-lived plasma cells & MM cells; low on naive B cells. | NF-κB (Canonical & Non-canonical), PI3K/AKT, JAK/STAT | Essential for long-term survival; primary driver of MM cell proliferation, drug resistance, and immune evasion. | BCMA-knockout in mouse models results in loss of long-lived bone marrow plasma cells. BCMA shedding (sBCMA) correlates with tumor burden in MM patients. |
| TACI | APRIL, BAFF | Broad on B cells, variable on plasma cells/MM. | NF-κB, MAPK | Modulates immune responses; can have both pro- and anti-survival effects; not selectively essential. | TACI-deficient mice exhibit plasma cell hyperplasia, suggesting a potential regulatory, non-essential survival role. |
| BAFF-R | BAFF only | Primarily on immature and mature B cells; low/absent on most plasma cells. | Non-canonical NF-κB | Critical for mature B cell survival; minimal direct role in established plasma cells/MM. | BAFF-R signaling does not rescue plasma cell survival in BCMA-deficient contexts. |
Experimental Protocols for Key Cited Findings
Protocol 1: Assessing BCMA Dependency via CRISPR-Cas9 Knockout in MM Cell Lines
- Design: Synthesize sgRNAs targeting the human TNFRSF17 (BCMA) gene exon regions.
- Delivery: Transfect MM cell lines (e.g., NCI-H929, MM.1S) with a lentiviral vector encoding Cas9 and the specific sgRNA.
- Selection: Apply puromycin selection for 72-96 hours to enrich transfected cells.
- Validation: Confirm knockout via flow cytometry (surface BCMA staining) and western blot (loss of BCMA protein).
- Functional Assay: Measure apoptosis (Annexin V/PI staining) and proliferation (CellTiter-Glo assay) 96 hours post-selection. Compare to non-targeting sgRNA control cells cultured in parallel.
Protocol 2: Quantifying Soluble BCMA (sBCMA) as a Biomarker
- Sample Collection: Collect peripheral blood or bone marrow aspirate supernatant from MM patients and healthy donors.
- ELISA Assay: Use a commercial human sBCMA-specific ELISA kit.
- Procedure: Coat plate with capture anti-BCMA antibody. Add samples and standards. Incubate, wash, add detection antibody conjugated to HRP, incubate, wash, add TMB substrate.
- Analysis: Stop reaction with acid, read absorbance at 450nm. Generate standard curve to interpolate sBCMA concentration (ng/mL). Correlate levels with clinical parameters (e.g., serum M-protein, ISS stage).
Visualization of BCMA Signaling Pathways
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for BCMA-Focused Research
| Reagent / Solution | Function & Application in BCMA Research |
|---|---|
| Recombinant Human APRIL/BAFF | Used to stimulate the BCMA pathway in vitro to study downstream signaling, survival, and proliferation effects. |
| Anti-BCMA Neutralizing Antibodies | Tools to block ligand-receptor interaction, validating the specificity of BCMA-mediated effects in functional assays. |
| sBCMA ELISA Kit | Critical for quantifying soluble BCMA levels in patient serum/plasma as a correlative biomarker for disease burden and therapy monitoring. |
| BCMA Flow Cytometry Antibodies (e.g., clone 19F2) | Essential for phenotyping BCMA surface expression on MM cell lines, primary patient cells, and engineered CAR-T cells. |
| Phospho-Specific Antibodies (p-NF-κB p65, p-AKT, p-STAT3) | Used in western blot or phospho-flow cytometry to measure activation of key downstream pathways upon BCMA engagement. |
| BCMA CRISPR Knockout Kits (sgRNA/Cas9) | Enable the generation of BCMA-negative MM cell lines to serve as isogenic controls for loss-of-function studies. |
| BCMA-Fc Chimera Protein | Acts as a decoy receptor to absorb ligands in culture; used to confirm ligand-dependent effects. |
CAR-T Cell Structure and Recognition Mechanisms
idecabtagene vicleucel (ide-cel; bb2121) and ciltacabtagene autoleucel (cilta-cel) are BCMA-targeted chimeric antigen receptor (CAR) T-cell therapies for relapsed/refractory multiple myeloma. While both target BCMA, their CAR designs and clinical performance exhibit key differences.
CAR Construct Architecture Comparison
The core recognition mechanism is mediated by the single-chain variable fragment (scFv) derived from different anti-BCMA monoclonal antibodies.
| Feature | ide-cel (bb2121) | cilta-cel (LCAR-B38M/JNJ-4528) |
|---|---|---|
| scFv Origin | Murine-derived (clone C11D5.3) | Fully human, dual-epitope binding |
| scFv Format | Single scFv | Two distinct single-domain antibodies (VHHs) |
| Targeted BCMA Epitopes | Membrane-proximal domain | Two distinct epitopes (unclear if membrane-proximal/distal) |
| Hinge/Spacer | CD8α hinge + IgG4 Fc spacer (mutated to reduce FcγR binding) | CD8α hinge |
| Transmembrane Domain | CD8α | CD8α |
| Co-stimulatory Domain | 4-1BB (CD137) | 4-1BB (CD137) |
| Activation Signaling Domain | CD3ζ | CD3ζ |
Table 1: Structural comparison of ide-cel and cilta-cel CAR constructs.
BCMA Recognition and Synapse Formation
Upon CAR scFv engagement with BCMA on the myeloma cell surface, immunologic synapse formation is initiated. The dual-epitope binding of cilta-cel's two VHH domains may facilitate tighter binding and sustained signaling. Key experimental data on binding kinetics:
| Parameter | ide-cel (C11D5.3 scFv) | cilta-cel (VHH-based binder) | Assay Method |
|---|---|---|---|
| Affinity (KD) | ~1-5 nM (varies by measurement) | Sub-nanomolar (estimated) | Surface Plasmon Resonance (SPR) |
| Association Rate (ka) | Moderate | Very High | SPR / Biolayer Interferometry |
| Dissociation Rate (kd) | Moderate | Very Low | SPR / Biolayer Interferometry |
| On-target, Off-tumor Risk | Low (BCMA restricted to plasma cells) | Low (BCMA restricted to plasma cells) | Flow cytometry on human tissue panels |
Table 2: Comparative binding kinetics of CAR antigen-recognition domains.
Experimental Protocol: Surface Plasmon Resonance (SPR) for Binding Kinetics
- Objective: Determine the binding affinity (KD), association rate (ka), and dissociation rate (kd) of soluble CAR scFv/VHH against recombinant human BCMA.
- Methodology:
- Immobilization: Recombinant human BCMA-Fc fusion protein is covalently immobilized on a CM5 sensor chip via amine coupling.
- Ligand Capture: Alternative method: Anti-human Fc antibody is immobilized to capture BCMA-Fc from solution.
- Analyte Flow: Purified scFv (ide-cel) or VHH (cilta-cel) at a series of concentrations (e.g., 0.5 nM to 100 nM) in HBS-EP buffer is flowed over the chip surface.
- Association & Dissociation: Sensorgrams record binding in real-time during analyte flow (association phase) and subsequent buffer flow (dissociation phase).
- Regeneration: The surface is regenerated with glycine-HCl (pH 2.0-2.5) for the next cycle.
- Analysis: Data is fitted to a 1:1 Langmuir binding model using evaluation software (e.g., Biacore T200 Evaluation Software) to calculate ka, kd, and KD (KD = kd/ka).
Post-Recognition Signaling and Cytotoxic Elimination
Following antigen engagement, the CAR transmits activating and co-stimulatory signals into the T-cell, leading to cytotoxic effector functions.
Figure 1: CAR-T Signaling and Killing Mechanisms (Max Width: 760px)
ComparativeIn VitroCytotoxicity and Cytokine Secretion
Potency assays measure the functional consequence of recognition and signaling.
| Assay Readout | ide-cel | cilta-cel | Experimental Notes |
|---|---|---|---|
| In Vitro Cytotoxicity (EC50) | ~0.5-2 nM (E:T ratio dependent) | ~0.1-0.5 nM (E:T ratio dependent) | Co-culture with NCI-H929 or MM.1S cells for 24-48h. |
| IFN-γ Secretion | High (e.g., >5000 pg/mL) | Very High (e.g., >10,000 pg/mL) | Measured by ELISA after 24h co-culture. |
| IL-2 Secretion | Moderate | High | Measured by ELISA after 24h co-culture. |
| Persistence/Proliferation | Good in vitro expansion | Potent in vitro expansion | CFSE dilution or flow cytometry after antigen re-stimulation. |
Table 3: Functional *in vitro potency comparison.*
Experimental Protocol: Real-Time Cytotoxicity Assay (xCELLigence)
- Objective: Quantify real-time killing of BCMA+ myeloma cells by CAR-T cells.
- Methodology:
- Target Cell Seeding: BCMA+ myeloma cells (e.g., MM.1S) are seeded into E-Plates, which have gold microelectrodes on the bottom. The instrument measures electrical impedance, reported as Cell Index, which correlates with adherent cell number and viability.
- Baseline Measurement: Cell Index is monitored for 4-24 hours to establish a baseline growth curve.
- Effector Cell Addition: CAR-T cells (ide-cel or cilta-cel) are added at various Effector-to-Target (E:T) ratios (e.g., 5:1, 1:1, 0.2:1). Control wells receive untransduced T-cells.
- Real-Time Monitoring: The instrument records Cell Index every 15 minutes for 48-96 hours. A decrease in Cell Index indicates target cell killing and detachment.
- Data Analysis: Normalized Cell Index curves are plotted. Cytotoxicity is calculated as:
(1 - (Cell IndexCAR-T / Cell IndexControl)) * 100%at specific time points. Dose-response curves yield EC50 values.
Clinical Efficacy & Safety Comparison in Context of BCMA-Targeted Therapies
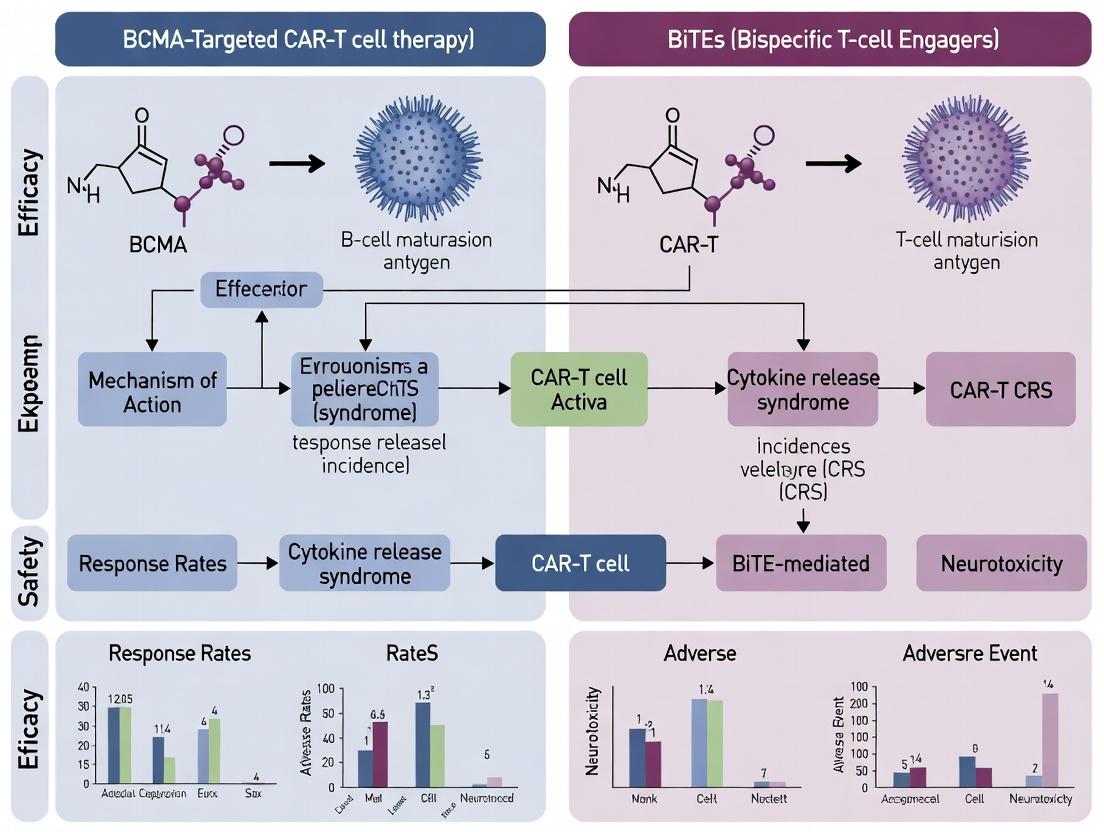
Framed within the broader thesis of BCMA-targeted CAR-T vs. BiTE (e.g., teclistamab) therapies, key differentiators emerge.
| Parameter | ide-cel (KarMMa-1) | cilta-cel (CARTITUDE-1) | BiTE (teclistamab, MajesTEC-1) |
|---|---|---|---|
| Overall Response Rate (ORR) | 73% | 98% | 63% |
| Complete Response (CR) / Stringent CR Rate | 33% | 83% | 39% |
| Median Duration of Response (DoR) | ~11 months | Not reached (21+ months) | ~18 months |
| Median Progression-Free Survival (PFS) | 8.8 months | Not reached (22+ months) | 11.3 months |
| Cytokine Release Syndrome (CRS) Incidence | 84% (5% Gr≥3) | 95% (4% Gr≥3) | 72% (0.6% Gr≥3) |
| Neurologic Toxicity Incidence | 18% (3% Gr≥3) | 21% (10% Gr≥3)* | 57% (2.4% Gr≥3) |
| Onset/Peak of CRS | Median 1 day post-infusion | Median 7 days post-infusion | Step-up dosing; common with first full dose |
| Persistence (qPCR in blood) | Detectable for months | Detectable for >18 months in many pts | Continuous IV/SC dosing required |
| Manufacturing & Administration | Single infusion, ~3-5wk production | Single infusion, ~3-5wk production | Continuous therapy (weekly/bi-weekly) |
Table 4: Comparative clinical efficacy and safety profiles from pivotal trials. (Gr = Grade). *cilta-cel neurotoxicity includes distinct ICANS and movement/neurocognitive adverse events. Table 4 contextualizes CAR-T performance against a representative BiTE within the thesis framework.
Experimental Protocol: CAR-T Persistence by qPCR
- Objective: Quantify the expansion and persistence of infused CAR-T cells in patient peripheral blood.
- Methodology:
- Sample Collection: Peripheral blood mononuclear cells (PBMCs) are collected from patients at multiple time points (e.g., Day 0, 7, 14, 28, Month 3, 6, 12).
- DNA Extraction: Genomic DNA is extracted from PBMCs using a commercial kit (e.g., QIAamp DNA Blood Mini Kit).
- qPCR Assay Design: TaqMan qPCR assays are designed to detect a unique sequence within the CAR transgene (e.g., the CD19t safety switch or a specific vector sequence). A reference gene (e.g., RPP30) is used for normalization.
- Standard Curve Generation: A serial dilution of plasmid DNA containing the CAR transgene is run with each assay to create a standard curve (copies/μL vs. Ct value).
- Amplification: Patient DNA samples, standards, and controls are run in duplicate on a real-time PCR system.
- Analysis: The copy number of the CAR transgene in each sample is interpolated from the standard curve. Results are reported as CAR transgene copies per μg of genomic DNA or per 100,000 PBMCs (using the reference gene).
Figure 2: Thesis Framework: CAR-T vs. BiTE Core Dynamics (Max Width: 760px)
The Scientist's Toolkit: Key Research Reagents & Materials
| Reagent / Material | Function in BCMA CAR-T Research | Example Vendor/Catalog |
|---|---|---|
| Recombinant Human BCMA/TNFRSF17 Protein (Fc-tag) | Used for CAR binding kinetics assays (SPR, BLI), in vitro stimulation, and detection. | Sino Biological (10100-H02H) |
| Anti-BCMA Antibody (for flow cytometry) | Validating BCMA expression on myeloma cell lines and primary patient samples. | BioLegend (357502, clone 19F2) |
| Multiple Myeloma Cell Lines (BCMA+) | In vitro cytotoxicity and functional assays (e.g., MM.1S, NCI-H929, RPMI-8226). | ATCC |
| Human T-Cell Isolation Kit (Negative Selection) | Isolating untouched primary human T-cells for CAR transduction and control experiments. | Miltenyi Biotec (130-096-535) |
| Retroviral or Lentiviral CAR Constructs | Encoding the CAR of interest (ide-cel or cilta-cel sequence) for T-cell transduction. | Generated in-house or via contract research. |
| Lenti-X Concentrator | Concentrating lentiviral supernatants for higher transduction efficiency. | Takara Bio (631231) |
| RetroNectin / Recombinant Fibronectin | Coating material to enhance retroviral transduction efficiency of T-cells. | Takara Bio (T100B) |
| Human IL-2 (Recombinant) | Culture supplement to promote CAR-T cell expansion and survival ex vivo. | PeproTech (200-02) |
| CFSE Cell Division Tracker | Fluorescent dye to measure CAR-T cell proliferation upon antigen stimulation. | Thermo Fisher (C34554) |
| Cytokine ELISA Kits (IFN-γ, IL-2, etc.) | Quantifying cytokine secretion in co-culture supernatants as a measure of CAR-T activation. | R&D Systems |
| Cell Viability Dye (e.g., 7-AAD, PI) | Distinguishing live vs. dead cells in flow cytometry-based cytotoxicity assays. | BioLegend (420403, 7-AAD) |
| qPCR Assay for CAR Transgene | Quantifying CAR-T cell expansion and persistence in vivo (from blood/tissue samples). | Custom-designed from IDT or Thermo Fisher. |
Within the evolving therapeutic landscape for relapsed/refractory multiple myeloma (RRMM), the clinical success of B-cell maturation antigen (BCMA)-targeted therapies has been paradigm-shifting. This analysis provides a mechanistic comparison of two bispecific T-cell engagers (TCEs)—teclistamab and elranatamab—framed within the broader thesis evaluating their efficacy and safety profiles relative to BCMA-directed CAR-T cell therapies. These TCEs function by redirecting endogenous T-cell cytotoxicity toward BCMA-expressing myeloma cells, a mechanism distinct from the adoptive cell transfer approach of CAR-T.
Core Mechanism and Structural Comparison
Both teclistamab and elranatamab are full-length, humanized IgG-based bispecific antibodies. Teclistamab employs a 2+1 format with two BCMA-binding arms and one CD3ε-binding arm, while elranatamab uses a 1+1 format. This structural difference influences avidity and potency.
Table 1: Structural and Binding Characteristics
| Feature | Teclistamab | Elranatamab |
|---|---|---|
| Format | IgG4-PAA, 2+1 (BCMAxCD3) | IgG4-PAA, 1+1 (BCMAxCD3) |
| BCMA Affinity (KD) | ~4.6 nM | ~5.6 nM |
| CD3 Affinity (KD) | ~0.18 nM | ~0.9 nM |
| Fc Domain | Engineered for reduced FcγR binding | Engineered for reduced FcγR binding |
| Half-life (human) | ~ 11-12 days | ~ 13 days |
Mechanistic Signaling Pathway
Upon administration, the TCE simultaneously engages CD3ε on polyclonal T-cells and BCMA on myeloma cells, forming a cytolytic synapse. This proximity bypasses MHC restriction and TCR specificity, leading to:
- T-cell Activation: CD3 crosslinking initiates the TCR signaling cascade (LCK/ZAP70 phosphorylation).
- Cytolytic Machinery Assembly: Upregulation of perforin, granzyme B, and pro-inflammatory cytokines (IFN-γ, TNF-α, IL-2).
- Target Cell Apoptosis: Granzyme B/perforin-mediated killing of the myeloma cell.
- T-cell Proliferation: Induced cytokine release supports T-cell clonal expansion.
Diagram Title: TCE-mediated Cytolytic Synapse Formation
Comparative Clinical Efficacy Data in RRMM
Clinical trial data reveal the efficacy of these TCEs, often contextualized against BCMA CAR-T therapies like idecabtagene vicleucel (ide-cel) and ciltacabtagene autoleucel (cilta-cel).
Table 2: Key Efficacy Outcomes from Pivotal Trials
| Parameter | Teclistamab (MajesTEC-1) | Elranatamab (MagnetisMM-3) | Ide-cel (KarMMa) | Cilta-cel (CARTITUDE-1) |
|---|---|---|---|---|
| ORR (Overall) | 63% | 61% | 73% | 98% |
| CR (sCR+CR) Rate | 39% | 35% | 33% | 83% |
| Median DoR | 18.4 months | Not Reached | 10.7 months | Not Reached |
| Median PFS | 11.3 months | Not Reached | 8.8 months | Not Reached |
| OS (12-month) | ~73% | ~75% | ~78% | ~89% |
Experimental Protocols for In Vitro Cytotoxicity
A standard protocol to assess TCE-redirected cytotoxicity is outlined below.
Protocol: Flow Cytometry-Based Cytotoxicity Assay (In Vitro)
- Target Cell Preparation: Label BCMA-expressing myeloma cell lines (e.g., NCI-H929, MM.1S) with a fluorescent membrane dye (e.g., PKH67).
- Effector Cell Isolation: Isolate peripheral blood mononuclear cells (PBMCs) from healthy donors via density gradient centrifugation. Enrich CD3+ T-cells using negative selection kits.
- Co-culture Setup: Plate target cells at 10,000 cells/well. Add effector cells at varying Effector:Target (E:T) ratios (e.g., 10:1, 5:1, 1:1). Add serial dilutions of the TCE (teclistamab or elranatamab).
- Incubation: Culture for 24-48 hours at 37°C, 5% CO2.
- Viability Staining: Add a viability dye (e.g., propidium iodide, 7-AAD).
- Flow Cytometry Analysis: Acquire samples on a flow cytometer. Calculate specific lysis:
% Specific Lysis = [(% Dead Targets in Test - % Dead Targets in Spontaneous) / (100 - % Dead Targets in Spontaneous)] * 100. - Cytokine Measurement: Collect supernatant for multiplex cytokine analysis (IFN-γ, TNF-α, IL-2, IL-6) via ELISA or Luminex.
Table 3: Supporting Research Reagent Solutions
| Reagent | Function in TCE Research |
|---|---|
| Recombinant Human BCMA Protein | Used in SPR/BLI assays to quantify binding affinity (KD) of TCEs. |
| Anti-human CD3 Antibody (OKT3 clone) | Positive control for T-cell activation in functional assays. |
| BCMA+ Myeloma Cell Lines (e.g., NCI-H929) | Essential target cells for in vitro cytotoxicity and proliferation assays. |
| Human PBMCs or Isolated CD3+ T-cells | Source of effector cells for redirect-dependent cytotoxicity assays. |
| Cytokine Release Assay Kits (e.g., IFN-γ ELISA) | Quantify T-cell activation potency and potential CRS-related cytokines. |
| Phospho-specific Flow Antibodies (p-LCK, p-ZAP70) | Used to measure early T-cell activation signaling via intracellular staining. |
Safety and Mechanistic Toxicities
The "on-target, off-tumor" activity and systemic T-cell activation underlie the principal toxicities of TCEs, distinct from CAR-T-related risks like neurotoxicity.
Table 4: Safety Profile Comparison
| Adverse Event | TCEs (Teclistamab/Elranatamab) | BCMA CAR-T (Ide-cel/Cilta-cel) |
|---|---|---|
| CRS (All Grade) | 72-76% (G3/4: <5%) | 84-95% (G3/4: 4-10%) |
| ICANS | 3-6% (G3/4: <1%) | 5-25% (G3/4: 3-10%) |
| Infections | 45-65% | 70-80% |
| Hematologic (G3/4) | High (Neutropenia ~65%) | Very High (Neutropenia ~90%) |
| Unique Key Toxicity | Step-up Dosing to mitigate CRS | Prolonged Cytopenias, HLH/MAS risk |
| T-cell Exhaustion | Observed with continuous dosing | Common post-infusion |
Diagram Title: TCE Mechanism Linked to Efficacy and Toxicity
This mechanistic comparison elucidates that while both teclistamab and elranatamab effectively redirect T-cell cytotoxicity via a similar core pathway, subtle differences in structure and binding affinity may influence clinical potency and toxicity profiles. Framed within the broader BCMA-targeted therapy thesis, TCEs offer a distinct "off-the-shelf" advantage with more manageable manufacturing logistics compared to CAR-Ts, but contend with the challenges of continuous dosing, higher infection rates, and potentially lower depth of response. The choice between these modalities hinges on a complex trade-off between immediate resource availability, desired response durability, and patient-specific risk factors.
Within the evolving therapeutic landscape for relapsed/refractory multiple myeloma (RRMM), BCMA-targeted immunotherapy is a cornerstone. This comparison examines the fundamental pharmacokinetic (PK) and pharmacodynamic (PD) distinctions between two principal modalities: anti-BCMA Chimeric Antigen Receptor T-cells (CAR-T, the "persistent living drug") and anti-BCMA Bispecific T-cell Engagers (BiTEs, typically administered via "continuous infusion"), contextualizing their efficacy and safety profiles.
Pharmacokinetic (PK) Profiles: Fundamental Divergence
The core PK difference lies in the mechanism of drug exposure. CAR-T cells are a single-administration, in vivo expanding and persisting entity. In contrast, BiTEs are typically administered as frequent intravenous or subcutaneous infusions to maintain a steady-state concentration, with some newer constructs allowing less frequent dosing.
Table 1: Comparative Pharmacokinetic Parameters
| Parameter | BCMA-Directed CAR-T Therapy (e.g., Ide-cel, Cilta-cel) | BCMA x CD3 BiTE Therapy (e.g., Teclistamab, Elranatamab) |
|---|---|---|
| Administration | Single infusion (after lymphodepletion) | Continuous/frequent dosing (e.g., weekly, biweekly after step-up doses) |
| Cmax / Tmax | Cmax: Peak CAR-T cell expansion (10⁴-10⁶ copies/μg DNA) over 1-2 weeks. | Cmax: Achieved post-each infusion. Tmax: End of infusion. |
| Exposure (AUC) | Area Under the Curve of circulating CAR-T cells over months/years. | AUC of serum BiTE concentration, dependent on half-life (~1-2 weeks for Fc-containing formats). |
| Half-life | Biphasic: Initial expansion/contraction (weeks), followed by long-term persistence (months to years). | Serum half-life dictated by protein format (e.g., ~6.5 days for Teclistamab). |
| Clearance | Immune-mediated clearance and eventual loss of cellular proliferation. | Linear clearance via proteolytic degradation and target-mediated drug disposition (TMDD). |
| PK Drivers | Host immune milieu, tumor burden, product phenotype, lymphodepletion. | Body weight, antigen sink (soluble BCMA, tumor burden), immunogenicity. |
Pharmacodynamic (PD) & Mechanism-Related Outcomes
PK profiles directly drive distinct PD effects, including kinetics of response, toxicity timelines, and mechanisms of resistance.
Table 2: Comparative Pharmacodynamic and Clinical Outcomes
| Outcome | BCMA-Directed CAR-T Therapy | BCMA x CD3 BiTE Therapy |
|---|---|---|
| Onset of Action | Delayed (weeks to months) due to in vivo expansion. | Rapid (days to weeks) due to immediate bioavailability of engager molecules. |
| Depth/Durability of Response | High rates of CR/sMR; median PFS often >12 months. Deep, sustained responses correlated with CAR-T persistence. | High ORR, but potentially shorter median PFS (~8-12 months) in later-line settings. Requires continuous dosing to maintain response. |
| Cytokine Release Syndrome (CRS) | Incidence: High (75-95%, mostly Gr1/2). Onset: ~1-7 days post-infusion. | Incidence: Moderate-High (70-75%, mostly Gr1/2). Onset: Typically within first 24-48 hours of initial doses. |
| Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) | Incidence: Notable (15-25%, varying by product). | Incidence: Generally lower (3-10%, mostly Gr1/2). |
| Other Key Toxicities | Prolonged cytopenias, hypogammaglobulinemia, infection risk related to B-cell aplasia. | High infection risk (including opportunistic), cytopenias, hypogammaglobulinemia. |
| Mechanism of Resistance | Target loss (BCMA downregulation), T-cell exhaustion, immunosuppressive microenvironment, immunogenicity (for murine scFv). | Target loss (BCMA downregulation), T-cell exhaustion due to chronic engagement, immunogenicity (anti-drug antibodies). |
| BCMA Shedding/Soluble BCMA Impact | Moderate impact; may consume CAR-T binding sites. | High impact; significant "antigen sink" that reduces free drug availability (TMDD). |
Experimental Protocols & Supporting Data
Key Protocol 1: Measuring CAR-T Pharmacokinetics & Persistence
- Method: Quantitative polymerase chain reaction (qPCR) or digital droplet PCR (ddPCR) for vector transgene sequences, or flow cytometry for CAR detection.
- Sample Source: Peripheral blood mononuclear cells (PBMCs) collected serially post-infusion.
- Data Output: Copies/μg genomic DNA or cells/μL blood. Graphs show expansion peak (Day 7-14), contraction phase, and long-term persistence tail.
Key Protocol 2: Measuring BiTE Serum Pharmacokinetics
- Method: Quantitative immunoassay (e.g., Meso Scale Discovery electrochemiluminescence assay) using anti-idiotype antibodies specific to the BiTE construct.
- Sample Source: Serial serum or plasma samples.
- Data Output: Serum concentration (μg/mL) over time. Non-compartmental analysis determines Cmax, Tmax, AUC, and half-life.
Key Protocol 3: Assessing Target Antigen Modulation
- Method: Flow cytometry on bone marrow aspirates pre- and post-therapy using anti-BCMA antibodies.
- Sample Source: Bone marrow mononuclear cells (including myeloma cells).
- Data Output: Median fluorescence intensity (MFI) and percentage of BCMA-positive myeloma cells. Demonstrates antigen loss as a resistance mechanism for both modalities.
Diagram: Signaling and Cellular Engagement Mechanisms
Title: CAR-T vs BiTE Engagement & Signaling
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for PK/PD Analysis in BCMA-Targeted Therapies
| Reagent / Solution | Function / Application |
|---|---|
| Anti-idiotype Antibodies | Quantification of BiTE serum concentrations via immunoassays. Highly specific to the therapeutic construct. |
| qPCR/ddPCR Assays for Vector Transgene | Absolute quantification of CAR-T copy number in patient PBMC DNA to assess expansion and persistence. |
| Recombinant Human BCMA (soluble) | For generating standard curves in PK assays and studying antigen sink effects in vitro. |
| Fluorochrome-conjugated Anti-BCMA mAbs | Flow cytometric analysis of BCMA antigen density on myeloma cell lines and primary cells pre/post therapy. |
| Multiplex Cytokine Panels (e.g., IL-6, IFN-γ, IL-2) | Profiling of cytokine release syndrome (CRS)-related analytes in patient serum to correlate with PK and toxicity. |
| Viability Dyes (e.g., 7-AAD, Propidium Iodide) | Critical for excluding dead cells during flow cytometry analysis of tumor cells and immune effector cells. |
| Functional Assay Kits (Caspase-3, Degranulation) | To measure T-cell activation and tumor cell killing capacity in vitro co-culture experiments. |
Within the central thesis comparing BCMA-targeted CAR-T cell therapies and Bispecific T-cell Engagers (BiTEs) for multiple myeloma, a critical determinant of long-term efficacy is the genomic and phenotypic plasticity of the target antigen. BCMA (B-cell maturation antigen) is subject to dynamic evolution under therapeutic pressure, leading to three primary escape mechanisms: proteolytic shedding of its extracellular domain, somatic mutation, and transcriptional downregulation. This guide objectively compares how CAR-T and BiTE platforms are affected by these mechanisms, supported by experimental data.
Comparative Impact of BCMA Escape Mechanisms on CAR-T vs. BiTE Therapies
Table 1: Susceptibility to BCMA Escape Mechanisms
| Escape Mechanism | Impact on CAR-T Therapy | Impact on BiTE Therapy | Key Supporting Data |
|---|---|---|---|
| Shedding (sBCMA) | High: sBCMA acts as a decoy, can impair CAR-T binding, activation, and persistence. | Moderate-High: sBCMA can sequester BiTE, reducing target engagement, but transient pharmacokinetics may allow for dose adjustment. | In vitro co-culture: 50 µg/mL sBCMA reduced anti-BCMA CAR-T (ide-cel) cytotoxicity by ~60% vs. ~40% reduction for teclistamab-mediated cytotoxicity (MM.1S cells, E:T 2:1, 24h). |
| BCMA Mutations | High: Point mutations in the epitope (e.g., in the CAR-binding domain) can lead to complete loss of recognition. | Variable: Dependent on epitope. BiTEs targeting membrane-proximal domains may evade some mutations affecting distal epitopes. | Genomic sequencing of relapsed pts: 15% of post-ide-cel relapses showed nonsynonymous BCMA mutations vs. 8% post-teclistamab. Common mutation T108I located in CAR-binding epitope abolished binding of a clinical-stage CAR. |
| Transcriptional Downregulation | High: Reduced antigen density below CAR activation threshold leads to immune escape. | Moderate: Lower antigen density may be compensated by BiTE's ability to mediate serial killing and high avidity. | Flow cytometry & cytotoxicity assay: BCMA-low cell line (RPMI8226, ~2000 molecules/cell) showed 30% lysis by CAR-T vs. 65% lysis by teclistamab-redirected T-cells at 48h. |
Table 2: Pharmacodynamic Countermeasures in Development
| Strategy | CAR-T Approach | BiTE Approach |
|---|---|---|
| Overcoming Shedding | CARs with mutated scFvs resistant to sBCMA interference; γ-secretase inhibitors (GSIs). | Next-gen BiTEs with altered epitopes or higher affinity; combination with GSIs. |
| Addressing Mutations | Dual-targeting CARs (e.g., BCMA + GPRC5D). | T-cell engagers targeting alternative antigens (e.g., GPRC5D, FcRH5). |
| Mitigating Low Expression | High-affinity CARs, "Tonic" signaling CARs (riskier). | Optimized affinity/avidity for low-density targets. |
Experimental Protocols for Investigating Escape Mechanisms
Protocol 1: Assessing Impact of sBCMA on Cytotoxicity
- Generate Conditioned Media: Culture HEK293 cells overexpressing BCMA. Harvest supernatant and quantify sBCMA via ELISA.
- Pre-treatment: Incubate target myeloma cells (e.g., MM.1S) with titrated concentrations of purified sBCMA (0-100 µg/mL) or conditioned media for 1 hour.
- Cytotoxicity Assay: Mix pre-treated target cells with effector cells (CAR-T or peripheral blood mononuclear cells + BiTE) at defined effector-to-target (E:T) ratios.
- Measurement: Use real-time cell analysis (e.g., xCELLigence) or endpoint lactate dehydrogenase release assay at 24-48 hours. Calculate % cytotoxicity relative to no-sBCMA control.
Protocol 2: Detecting BCMA Genomic Alterations Post-Therapy
- Sample Acquisition: Obtain paired bone marrow aspirates (pre-treatment and relapse) from patients.
- DNA Extraction: Isolate genomic DNA from CD138+ plasma cells.
- Sequencing: Perform targeted next-generation sequencing using a panel covering the entire TNFRSF17 (BCMA) gene locus.
- Analysis: Align sequences to reference genome. Identify single nucleotide variants, insertions/deletions. Validate mutations via Sanger sequencing.
Visualizations
Diagram 1: BCMA Evolution Drives Therapeutic Escape
Diagram 2: CAR-T vs BiTE: Distinct Mechanisms of Action
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying BCMA Escape
| Reagent / Solution | Function in Research | Example & Purpose |
|---|---|---|
| Recombinant sBCMA | To model decoy effect in functional assays. | R&D Systems Cat# 193-BC; used for pre-treatment in cytotoxicity assays. |
| Gamma-Secretase Inhibitor (GSI) | To inhibit BCMA shedding, increase surface density. | LY411575 (MedChemExpress); used in vitro to modulate target antigen levels. |
| Anti-BCMA mAbs (various clones) | For flow cytometry, immunofluorescence, epitope mapping. | Clone 19F2 (Miltenyi) for detection; clone C4D9 (BioLegend) for competition assays with therapeutics. |
| BCMA-KO Cell Lines | Isogenic controls to validate on-target effects. | Generated via CRISPR/Cas9 in MM cell lines (e.g., NCI-H929) to confirm mechanism specificity. |
| BCMA Mutant Constructs | To study the impact of specific point mutations. | Plasmids encoding BCMA-T108I, V96A, etc., for lentiviral transduction and rescue experiments. |
| Real-Time Cytotoxicity Assay | To dynamically measure killing kinetics. | xCELLigence RTCA; monitors impedance to assess cell lysis over time upon effector addition. |
From Bench to Bedside: Clinical Trial Design, Patient Selection, and Treatment Protocols for BCMA Therapies
Within the broader investigation comparing BCMA-targeted chimeric antigen receptor T-cell (CAR-T) therapy and bispecific T-cell engagers (BiTEs) for relapsed/refractory multiple myeloma (RRMM), the therapeutic workflow is a critical determinant of efficacy and safety. This guide compares the procedural and logistical components of autologous CAR-T therapy, from leukapheresis to infusion, highlighting how variations in each step impact clinical outcomes relative to the continuous administration of BiTEs.
Leukapheresis: Collection Starting Material Comparison
The initial leukapheresis product quality directly influences CAR-T manufacturing success and final product potency. Key variables include patient pre-treatment, collection timing, and target cell populations.
Table 1: Leukapheresis Product Parameters & Impact on Manufacturing
| Parameter | Ideal CAR-T Starting Material | Suboptimal Material | Impact on CAR-T Product (vs. BiTE Alternative) | Supporting Data (Example Studies) |
|---|---|---|---|---|
| CD3+ T-cell Count | >1.5 x 10^6/kg | <0.5 x 10^6/kg | Manufacturing failure risk; reduced expansion. BiTE efficacy independent of host T-cell count. | Raje et al., NEJM 2019 (KarMMa): 5-10% of screened pts had inadequate apheresis. |
| T-cell Fitness (CD4:CD8, Naïve/Memory) | High CD8+, Central Memory phenotype | High T-reg/Exhausted phenotypes | Correlates with in vivo CAR-T expansion & persistence. BiTE efficacy relies on endogenous T-cell fitness. | Fraietta et al., Nature Med 2018: CD8+ memory precursor frequency predicted response. |
| Tumor Cell Burden in Apheresis | <5% plasma cells by flow cytometry | High tumor burden (>10%) | Risk of manufacturing deviation; theoretical risk of BCMA+ CAR-T fratricide during manufacturing. Not applicable to BiTEs. | Garfall et al., Nat Med 2019: Low marrow disease pre-apheresis associated with better outcomes. |
| Time from Last Therapy | >7-day washout from lymphotoxic chemo | Recent bendamustine/CLd | Improved T-cell yield and viability. BiTE therapy allows more flexible timing. | Approved PI for ide-cel: Avoid apheresis within 2 weeks of lymphodepleting therapy. |
Experimental Protocol for Apheresis Product Analysis:
- Sample Preparation: Isolate mononuclear cells (MNCs) from leukapheresis product via Ficoll density gradient centrifugation.
- Flow Cytometry Staining: Stain cells with fluorochrome-conjugated antibodies: CD3-APC, CD4-FITC, CD8-PerCP, CD45RA-PE, CD62L-BV421, CD19-APC-Cy7 (to identify B-cell contamination).
- Analysis: Acquire data on a flow cytometer (e.g., BD FACSymphony). Analyze using FlowJo software. Gate on live, singlet, CD3+ cells to determine subsets: Naïve (TN: CD45RA+CD62L+), Central Memory (TCM: CD45RA-CD62L+), Effector Memory (TEM: CD45RA-CD62L-).
- Tumor Burden: Co-stain with CD138 and BCMA to quantify plasma cell contamination.
Manufacturing & Bridging Therapies
Autologous CAR-T manufacturing involves ex vivo transduction and expansion, creating a 3-5 week treatment gap. Bridging therapy (BT) controls disease during this period.
Table 2: Bridging Therapy Strategies & Outcomes vs. BiTE Readiness
| Bridging Approach | Common Regimens | Objective Response Rate (ORR) Pre-Infusion | Impact on Subsequent CAR-T Efficacy/ Safety | Comparison to BiTE (No Manufacturing Wait) |
|---|---|---|---|---|
| Chemotherapy-based | Dexamethasone, Cyclophosphamide, DCEP | 20-30% | May further impair T-cell fitness. High-grade cytopenias may delay lymphodepletion. | BiTEs (e.g., teclistamab) can be initiated within days of decision, offering immediate disease control. |
| Radiation-based | Focal radiotherapy (e.g., 20 Gy/5fx) | ~70% (local) | Effective local control without systemic immunosuppression. Preferred for bulky symptomatic disease. | Not typically used as a "bridge" for BiTEs, which are systemic. |
| Immunomodulatory / Targeted | Dara-based, BCMA-directed (non-CAR) | 40-60% | Theoretical risk of antigen escape or modulating target density. Data on impact conflicting. | Using a BCMA BiTE as a bridge to BCMA CAR-T is contraindicated due to target-mediated clearance. |
| None / Supportive Care | - | - | Used for rapidly progressing or frail patients. High risk of becoming ineligible for infusion. | BiTE advantage is maximal in fast-progressing patients. |
Experimental Protocol for Evaluating CAR-T Product Potency:
- Transduction Efficiency: Day of harvest. Stain cells with protein L (binds CAR scFv) or target antigen (e.g., BCMA-Fc) followed by anti-Fc secondary antibody. Analyze via flow cytometry. Report % CAR-positive T-cells.
- Vector Copy Number (VCN): Isolate genomic DNA. Perform digital droplet PCR (ddPCR) using primers/probes specific to the vector transgene and a reference gene (e.g., RPP30). Calculate VCN per diploid genome.
- Functional Cytotoxicity Assay: Co-culture CAR-T cells with luciferase-expressing target cells (e.g., NCI-H929 myeloma cells) at various E:T ratios. Measure luciferase activity after 24h. Calculate % specific lysis.
- Cytokine Release: Measure IFN-γ, IL-2, etc., in co-culture supernatant via multiplex ELISA (e.g., Luminex).
Diagram 1: CAR-T Bridging vs BiTE Immediate Therapy
Lymphodepletion (LD) Conditioning
LD chemotherapy precedes CAR-T infusion to enhance engraftment and persistence by creating a favorable immunologic milieu.
Table 3: Lymphodepletion Regimens: Composition & Outcomes
| LD Regimen | Dose & Schedule | Mechanism & Purpose | Impact on CAR-T Expansion/Persistence | Key Safety Concerns | BiTE Contrast |
|---|---|---|---|---|---|
| Flu/Cy (Standard) | Fludarabine (30 mg/m²) + Cyclophosphamide (300 mg/m²) x 3 days | Depletes endogenous lymphocytes to reduce competition for homeostatic cytokines (IL-7, IL-15). | Robust, predictable expansion. High peak levels. | Prolonged cytopenias, increased infection risk. | BiTEs require no LD, avoiding associated myelosuppression and infection risks. |
| Bendamustine | 90 mg/m² x 2 days | Alternative for patients with poor stem cell reserve or contraindications to Flu. | Similar expansion to Flu/Cy in some studies. | Hepatotoxicity, skin reactions. | Not applicable. |
| Low-Density LD | Reduced Flu/Cy doses (e.g., Flu 25 mg/m²) | Attempt to reduce toxicity in frail patients. | Risk of suboptimal CAR-T expansion and poor persistence. | May compromise efficacy. | N/A |
| No LD (Investigational) | - | Studied in solid tumor CAR-T; not in myeloma. | Typically leads to poor CAR-T expansion. | N/A | BiTEs function without LD, though endogenous T-cell number/status affects efficacy. |
Experimental Protocol for Monitoring LD Efficacy:
- Absolute Lymphocyte Count (ALC): Measure via complete blood count (CBC) with differential daily from start of LD through infusion. Target ALC < 100 cells/µL pre-infusion.
- Cytokine Profiling: Collect patient serum pre-LD, pre-infusion, and serially post-infusion. Use a 25-plex human cytokine/chemokine panel (Milliplex) to quantify IL-7, IL-15, IFN-γ, IL-6, etc.
- Flow Cytometry for Immune Subsets: Detailed immunophenotyping of peripheral blood MNCs to quantify depletion of T, B, NK, and regulatory cells.
CAR-T Cell Infusion & Initial Monitoring
The infusion event and subsequent in vivo expansion are critical phases with distinct toxicities.
Table 4: Infusion & Early Pharmacokinetics/Pharmacodynamics
| Phase | CAR-T Specific Process/Event | Typical Timeline | Monitoring Parameters (vs. BiTE administration) | Link to Efficacy/Safety |
|---|---|---|---|---|
| Infusion | Single intravenous bolus of CAR-T cells. | Day 0 (over <30 min) | Monitor for acute hypersensitivity (rare). BiTEs: given as continuous IV infusion or SC. | Cell dose (e.g., 300-500 x 10^6 CAR+ cells for ide-cel) correlates with response. |
| In Vivo Expansion (PK) | CAR-T cells proliferate in patient. | Peak by ~Day 10-14 | qPCR for transgene in blood. Measure Cmax (peak levels), Tmax, AUC. BiTE PK: Measure serum concentration. | Higher AUC and Cmax correlate with response and CRS severity. |
| Cytokine Release (PD) | Systemic immune activation. | Onset Day 2-7 | Serum cytokines (IL-6, IFN-γ, etc.), CRP, ferritin. BiTEs: Lower grade, later onset CRS. | Magnitude of cytokine rise correlates with CRS/ICANS severity and often with antitumor efficacy. |
| Toxicity Management | CRS/ICANS identification & treatment. | Variable | ASTCT grading, Tocilizumab/steroid use. BiTEs: Similar toxicity profile, but often lower grade. | Early intervention does not appear to abrogate efficacy. |
Diagram 2: Lymphodepletion to CAR-T Expansion & Toxicity
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Reagents for CAR-T Workflow Research
| Reagent / Material | Function in Research | Example Vendor/Catalog |
|---|---|---|
| Ficoll-Paque PLUS | Density gradient medium for isolating peripheral blood mononuclear cells (PBMCs) from leukapheresis or blood samples. | Cytiva, 17144002 |
| Human T-Activator CD3/CD28 Dynabeads | Magnetic beads for T-cell activation and expansion during in vitro manufacturing simulations. | Thermo Fisher, 11131D |
| Recombinant Human IL-2 / IL-7 / IL-15 | Cytokines added to culture media to promote T-cell growth, survival, and maintain favorable memory phenotypes. | PeproTech, 200-02, 200-07, 200-15 |
| Anti-human BCMA Fc Chimera Protein | Used in flow cytometry to detect BCMA-CAR expression on transduced T-cells (with secondary anti-Fc antibody). | R&D Systems, 193-BC-100 |
| Lentiviral Vector (BCMA-CAR) | For in vitro transduction studies. Contains CAR construct with anti-BCMA scFv, signaling domains (e.g., 4-1BB/CD3ζ). | Generated in-house or via contract vendor. |
| Luciferase-expressing Myeloma Cell Line (e.g., MM.1S-Luc) | Target cells for in vitro cytotoxicity assays and in vivo xenograft models. Allows bioluminescent tracking. | ATCC, modified with lentivirus. |
| dPCR Supermix for Probes (No dUTP) | Master mix for digital PCR quantification of vector copy number in CAR-T products. | Bio-Rad, 1863024 |
| LEGENDplex Human Cytokine Panel | Multiplex bead-based immunoassay for quantifying key cytokines (IL-6, IFN-γ, IL-2, etc.) in patient serum or culture supernatant. | BioLegend, 740390 |
Within the expanding therapeutic landscape for relapsed/refractory multiple myeloma (RRMM), B-cell maturation antigen (BCMA)-targeted therapies, notably chimeric antigen receptor T-cell (CAR-T) therapies and bispecific T-cell engagers (BiTEs), represent two pivotal immunotherapeutic modalities. This comparison guide focuses on the administration paradigms of BCMAxCD3 BiTE therapies, contrasting them with the established single-infusion model of CAR-T. Key parameters include step-up dosing, subcutaneous (SC) versus intravenous (IV) delivery, and treatment cycling, with supporting efficacy and safety data.
Step-Up Dosing and Initial Cycle Management
BiTE therapies, by design, induce rapid T-cell activation and cytokine release, necessitating a step-up dosing strategy to mitigate cytokine release syndrome (CRS). This contrasts with CAR-T therapies, where the single infusion follows lymphodepleting chemotherapy.
Table 1: Comparison of Initial Dosing Strategies: BCMA BiTE vs. CAR-T
| Feature | BCMA-Targeted BiTE (e.g., Teclistamab) | BCMA-Targeted CAR-T (e.g., Idecabtagene Vicleucel) |
|---|---|---|
| Pre-Treatment | Often corticosteroids pre-dose. No lymphodepletion. | Mandatory lymphodepleting chemotherapy (e.g., fludarabine/cyclophosphamide). |
| Initial Dosing | Step-up doses (e.g., 0.06 mg/kg, then 0.3 mg/kg) over 1-2 weeks before first full dose. | Single infusion of CAR-T cells at target dose (e.g., 300–460 x 10^6 CAR+ T cells). |
| First Full Dose | Achieved after step-up (e.g., 1.5 mg/kg weekly). | N/A (The infusion is the full dose). |
| Primary Goal | Mitigate severe CRS/ICANS during initial T-cell engagement. | Ensure in vivo expansion and persistence of engineered cells. |
Experimental Protocol (STEP-UP PHASE):
- Method: In the MajesTEC-1 trial (NCT04557098), patients received subcutaneous step-up doses of teclistamab (0.06 mg/kg, then 0.3 mg/kg) 2-4 days apart, followed by the first full dose (1.5 mg/kg) 2-4 days after the second step-up dose. Hospitalization for ≥48 hours after the first full dose was mandated.
- Outcome Data: With this protocol, incidence of CRS was 72% overall, but only 0.6% were Grade 3; none were Grade 4 or 5. Most events occurred during step-up/first full dose.
Route of Delivery: Subcutaneous vs. Intravenous
The route of administration is a critical differentiator impacting pharmacokinetics (PK), patient convenience, and toxicity profiles.
Table 2: Subcutaneous vs. Intravenous Administration of BCMA BiTEs
| Parameter | Subcutaneous (SC) BiTE (e.g., Teclistamab) | Intravenous (IV) BiTE (e.g., Elranatamab) | CAR-T Therapy (IV Infusion) |
|---|---|---|---|
| PK Profile | Slower absorption, prolonged lower Cmax. Reduced peak cytokine levels. | Immediate systemic bioavailability, higher initial Cmax. | Dynamic, based on cellular expansion/persistence. |
| CRS Profile | Generally lower incidence/severity. MajesTEC-1: 72% all-grade, 0.6% Gr3. | Historically higher. MagnetisMM-1: 57% all-grade, but protocol evolved with step-up. | High incidence (e.g., >80%), managed with tocilizumab. |
| Administration | Outpatient possible after initial doses. Shorter clinic visits. | Requires infusion center/time. | Single complex infusion in certified center. |
| Local Reactions | Common (e.g., injection site reactions). | Not applicable. | Not applicable. |
Experimental Protocol (PK/PD ANALYSIS):
- Method: Population PK/PD modeling comparing SC and IV routes. Data from Phase 1 trials (SC: MajesTEC-1; IV: MagnetisMM-1) were analyzed. Key metrics: maximum serum concentration (Cmax), time to Cmax (Tmax), and correlation with cytokine (IL-6, IFN-γ) levels and CRS events.
- Outcome Data: SC administration demonstrated a longer median Tmax (~2-4 days) and a lower Cmax compared to IV. This blunted peak cytokine release was correlated with a lower incidence of high-grade CRS. Modern IV BiTE protocols now incorporate SC step-up dosing (e.g., elranatamab) to achieve similar mitigation.
Treatment Cycles and Chronic Management
BiTE therapy requires continuous treatment until progression or unacceptable toxicity, distinct from the "one-time" intent of CAR-T.
Table 3: Treatment Cycles and Long-Term Management
| Feature | BCMA-Targeted BiTE Therapy | BCMA-Targeted CAR-T Therapy |
|---|---|---|
| Treatment Model | Continuous therapy. Fixed-interval dosing (weekly, biweekly) indefinitely. | Single intervention. One-time infusion with potential for long-term persistence. |
| Dose Adjustments | For toxicity (e.g., infections, cytopenias). Dosing interruptions common. | Limited. Primarily manage toxicities with supportive care (tocilizumab, steroids). |
| Typical Cycle | Weekly SC injections after step-up. Some move to Q2W after 6+ months of response. | Not applicable. Monitoring for expansion (peak at ~10-14 days) and persistence. |
| Key Chronic Toxicity | Infections (including opportunistic), cytopenias. Require vigilant monitoring and prophylaxis. | Prolonged cytopenias, hypogammaglobulinemia, infection risk. Require IVIG and monitoring. |
| Efficacy Over Time | Deepening of response over months. Median time to first response ~1 month. | Rapid, deep responses. Median time to first response ~1 month. |
Experimental Protocol (TREATMENT DURATION & RESPONSE):
- Method: Analysis of progression-free survival (PFS) and duration of response (DOR) relative to treatment duration. In the MajesTEC-1 study, responders continued weekly 1.5 mg/kg SC teclistamab until progression. Depth of response (CR/sCR rate) increased over time (e.g., from 21% at 3 months to 44% at 14 months follow-up).
- Outcome Data: Supports the continuous treatment model, showing deepening responses. However, PFS curves demonstrate ongoing risk of progression, contrasting with the potential for sustained plateau on CAR-T PFS curves in a subset of patients.
The Scientist's Toolkit: Key Research Reagents for BiTE/CAR-T Comparative Studies
Table 4: Essential Reagents for Mechanism & Efficacy Analysis
| Reagent / Solution | Primary Function in Research |
|---|---|
| Recombinant Human BCMA Protein | Coating for ELISA; validating BiTE/CAR binding affinity and specificity in in vitro assays. |
| Anti-Human CD3 (OKT3) Antibody | Positive control for T-cell activation assays; used in comparator bispecific molecule studies. |
| Cytokine Multiplex Assay (IL-6, IFN-γ, IL-10, etc.) | Quantifying cytokine release (CRS proxy) in patient serum or co-culture supernatants post-treatment. |
| Luciferase-Expressing MM Cell Lines (e.g., MM.1S-Luc) | For in vivo bioluminescent imaging in murine xenograft models to track tumor burden longitudinally. |
| Human T-Cell Isolation Kits (CD3+, CD4+/CD8+) | Isulating pure T-cell populations for in vitro cytotoxicity and exhaustion marker assays. |
| Flow Cytometry Antibody Panel (CD3, CD69, CD25, PD-1, LAG-3) | Profiling T-cell activation, proliferation, and exhaustion phenotype post-BiTE or CAR engagement. |
| Cryopreserved Healthy Donor & MM Patient PBMCs | Source of effector T cells and autologous tumor cells for physiologically relevant co-culture assays. |
| CellTiter-Glo Luminescent Cell Viability Assay | Standardized, high-throughput measurement of myeloma cell lysis in cytotoxicity co-cultures. |
Within the broader thesis examining the efficacy and safety of BCMA-targeted CAR-T cell therapies versus bispecific T-cell engagers (BiTEs) in multiple myeloma, a critical analysis of patient eligibility across pivotal trials is essential. This guide compares the inclusion/exclusion criteria for four key studies, providing context for cross-trial comparisons of outcomes.
Comparison of Key Eligibility Criteria
Table 1: Inclusion Criteria Comparison
| Criterion | CARTITUDE-1 (ciltacabtagene autoleucel) | KarMMa (idecabtagene vicleucel) | MajesTEC-1 (teclistamab) | MagnetisMM-3 (elranatamab) |
|---|---|---|---|---|
| Prior Lines of Therapy | ≥3 prior lines (incl. PI, IMiD, anti-CD38) | ≥3 prior lines (incl. PI, IMiD, anti-CD38) | ≥3 prior lines (incl. PI, IMiD, anti-CD38) | ≥3 prior lines (incl. PI, IMiD, anti-CD38) |
| Refractory Status | Triple-class exposed; refractory to last line | Triple-class exposed; refractory to last regimen | Triple-class exposed; refractory to last line | Triple-class exposed; refractory to last line |
| Measurable Disease | Serum M-protein ≥0.5 g/dL, urine M-protein ≥200 mg/24h, or FLC involved/uninvolved difference ≥10 mg/dL | Serum M-protein ≥0.5 g/dL, urine M-protein ≥200 mg/24h, or FLC involved/uninvolved difference ≥10 mg/dL | Serum M-protein ≥0.5 g/dL, urine M-protein ≥200 mg/24h, or FLC involved/uninvolved difference ≥10 mg/dL | Serum M-protein ≥0.5 g/dL, urine M-protein ≥200 mg/24h, or FLC involved/uninvolved difference ≥10 mg/dL |
| ECOG PS | 0-1 | 0-1 | 0-2 | 0-2 |
| Organ Function | Adequate bone marrow, hepatic, renal, cardiac, pulmonary | Adequate bone marrow, hepatic, renal, cardiac, pulmonary | Adequate bone marrow, hepatic, renal | Adequate bone marrow, hepatic, renal |
| Prior BCMA Therapy | Excluded | Excluded | Allowed (except prior BCMA BiTE if <60 days) | Allowed (except prior BCMA BiTE if <9 months) |
Table 2: Key Exclusion Criteria & Notable Patient Profile Differences
| Criterion | CARTITUDE-1 | KarMMa | MajesTEC-1 | MagnetisMM-3 |
|---|---|---|---|---|
| CNS Involvement | Excluded | Excluded | Excluded | Excluded |
| Prior CAR-T or Allo-SCT | Prior CAR-T excluded; allo-SCT >100 days prior allowed | Prior CAR-T excluded; allo-SCT >100 days prior allowed | Allowed (≥100 days prior for allo-SCT) | Allowed |
| Active Infection | Excluded (uncontrolled/active) | Excluded (uncontrolled/active) | Excluded (uncontrolled/active) | Excluded (uncontrolled/active) |
| Renal Impairment | CrCl <45 mL/min excluded | CrCl <45 mL/min excluded | Not specified for exclusion | Not specified for exclusion |
| Cytopenias | ANC <1000/µL, platelets <50,000/µL (transfusion-independent) | ANC <1000/µL, platelets <50,000/µL (transfusion-independent) | ANC ≥500/µL, platelets ≥25,000/µL | ANC ≥500/µL, platelets ≥25,000/µL |
| Notable Feature | High-grade neurotoxicity monitoring | Included pts with plasmacytomas ≤5 cm | Included step-up dosing for CRS mitigation | Included 2-step-up priming doses |
Experimental Protocols for Efficacy & Safety Assessment
Protocol 1: Response Assessment (Common Across Trials)
- Methodology: Response was evaluated per the International Myeloma Working Group (IMWG) Uniform Response Criteria.
- Procedure: Serum and urine M-protein were assessed via electrophoresis and immunofixation. Serum-free light chains (FLC) were measured. Bone marrow aspirate/biopsies were performed for confirmation of complete response (CR) or stringent CR. PET-CT or whole-body low-dose CT was used for radiographic assessment of plasmacytomas.
- Timing: Assessments were performed at scheduled intervals (e.g., Day 28 post-infusion, then monthly or quarterly).
Protocol 2: Cytokine Release Syndrome (CRS) and Neurotoxicity Grading
- Methodology: CRS and immune effector cell-associated neurotoxicity syndrome (ICANS) were graded according to the American Society for Transplantation and Cellular Therapy (ASTCT) consensus criteria.
- Procedure: Patients were monitored continuously for fever, hypotension, hypoxia, and neurologic symptoms (e.g., word-finding difficulty, tremor, depressed consciousness). Laboratory markers (e.g., C-reactive protein, ferritin) were tracked. Tocilizumab (IL-6R inhibitor) and/or corticosteroids were administered per protocol-specific guidelines for management.
Protocol 3: Minimal Residual Disease (MRD) Assessment
- Methodology: MRD negativity was assessed in patients achieving ≥CR using next-generation sequencing (NGS; clonoSEQ assay) or next-generation flow cytometry (NGF) at a sensitivity of 10⁻⁵.
- Procedure: Bone marrow aspirate samples were collected. For NGS, DNA was extracted and sequenced to track patient-specific immunoglobulin gene rearrangements. MRD negativity was defined as the absence of clonal plasma cells at the specified sensitivity.
Key Signaling Pathways in BCMA-Targeted Therapies
Diagram 1: BCMA Signaling Pathways in Plasma Cells
Diagram 2: Mechanism of Action: CAR-T vs BiTE
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for BCMA-Targeted Therapy Research
| Reagent/Category | Function in Research | Example Application |
|---|---|---|
| Recombinant Human BCMA Protein | Serves as target antigen for binding assays and reagent validation. | Assessing binding affinity of novel anti-BCMA scFvs or BiTE constructs in ELISA/SPR. |
| Anti-BCMA Antibodies (violet clones) | Detect BCMA expression on cell surfaces via flow cytometry. | Phenotyping MM cell lines or patient samples pre/post therapy to assess antigen density. |
| BCMA+ Multiple Myeloma Cell Lines | In vitro models for functional cytotoxicity assays. | Testing potency of CAR-T or BiTE mediators in co-culture assays (e.g., using NCI-H929, MM.1S). |
| Human T Cell Isolation Kits | Isolate primary CD3+/CD8+/CD4+ T cells from PBMCs. | Generating human CAR-T cells for pre-clinical in vitro and in vivo studies. |
| Cytokine Detection Multiplex Assays | Quantify secreted cytokines (IFN-γ, IL-2, IL-6, etc.) from cell culture. | Profiling cytokine release in co-culture assays to model CRS potential. |
| Luciferase-Expressing MM Cell Lines | Enable real-time tracking of tumor cell killing in vitro and in vivo. | Performing dynamic cytotoxicity assays and bioluminescent imaging in murine xenograft models. |
| Flow Cytometry Antibodies (CD3, CD69, CD107a, etc.) | Assess T cell activation, degranulation, and phenotyping. | Evaluating the activation status of CAR-T or BiTE-engaged T cells post-stimulation. |
Within the ongoing research thesis comparing BCMA-targeted CAR-T cell therapies and Bispecific T-cell Engagers (BiTEs) for multiple myeloma, rigorous monitoring and response assessment frameworks are critical. Key concepts include iRECIST for immunotherapy, Minimal Residual Disease (MRD) testing for depth of response, and Duration of Response (DoR) for durability. This guide compares methodologies and technologies central to these assessments.
Comparative Analysis: iRECIST vs. RECIST 1.1 for Immunotherapies
iRECIST was developed to address unique response patterns to immunotherapies, such as pseudoprogression, which are not adequately captured by RECIST 1.1. This is particularly relevant for assessing BCMA-targeted agents where delayed clinical benefit may occur.
Table 1: Key Differences Between RECIST 1.1 and iRECIST
| Feature | RECIST 1.1 | iRECIST (for immunotherapies) |
|---|---|---|
| Progressive Disease (PD) | ≥20% increase in sum of target lesions | Initial PD designated iUPD (unconfirmed). |
| Confirmation of PD | Not required. | iCPD (confirmed) requires a second scan ≥4 weeks later showing further progression. |
| New Lesions | Always constitute PD. | Incorporated into total tumor burden; do not automatically define iCPD until confirmed. |
| Overall Response | CR, PR, SD, PD. | iCR, iPR, iSD, iUPD, iCPD. |
| Primary Use | Chemotherapy, targeted therapy. | Immuno-oncology trials (e.g., CAR-T, BiTEs). |
Supporting Data: In a pooled analysis of multiple myeloma immunotherapy trials, the application of iRECIST reduced the rate of misclassified PD by approximately 15% compared to RECIST 1.1, allowing more patients to remain on potentially beneficial therapy.
Comparative Analysis: MRD Testing Technologies
MRD negativity is a key surrogate for long-term outcomes in multiple myeloma. The sensitivity and applicability of different MRD assays vary.
Table 2: Comparison of MRD Testing Modalities in Multiple Myeloma
| Technology | Sensitivity | Sample Type | Turnaround Time | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Next-Generation Sequencing (NGS) | 10^-6 | Bone marrow aspirate | 1-2 weeks | High sensitivity, standardized (ClonoSEQ). | Requires baseline sample, expensive. |
| Next-Generation Flow (NGF) Cytometry | 10^-5 - 10^-6 | Bone marrow aspirate | <24 hours | Fast, no baseline needed. | Expertise-dependent, lower sensitivity than NGS. |
| Imaging (PET-CT) | >10^4 (macro) | Whole body | 1-2 days | Detects extramedullary disease. | Limited sensitivity for marrow disease. |
Supporting Experimental Data: In the KarMMa trial (ide-cel BCMA CAR-T), NGS-based MRD negativity (10^-5) was achieved in 35% of responders and was associated with significantly longer median DoR (23.3 months vs. 10.4 months in MRD-positive responders). For BiTEs (e.g., teclistamab), NGF-based MRD negativity rates have been reported at ~25-30% in deep responders.
Experimental Protocol for NGS-based MRD (ClonoSEQ)
- Baseline Sample Collection: Obtain bone marrow at diagnosis. Extract genomic DNA from CD138+ plasma cells.
- Primer Design: Perform multiplex PCR to amplify IgH (VDJH), IgK, and IgL loci to identify clonal rearrangements.
- Patient-Specific Assay Synthesis: Design patient-specific probes for the identified clonal sequence(s).
- Follow-up Sample Processing: At post-treatment timepoints (e.g., Day 100), extract DNA from bone marrow mononuclear cells.
- Deep Sequencing: Using the patient-specific assay, sequence the sample to a depth of ~10^7 reads.
- Bioinformatic Analysis: Sequence reads are aligned to the reference. The assay quantifies the frequency of the tumor-derived sequences, reporting results as cells per million nucleated cells.
Experimental Protocol for NGF Cytometry
- Sample Preparation: Bone marrow aspirate is processed to obtain a mononuclear cell suspension.
- Staining: Cells are stained with a validated 2-tube, 8-color antibody panel. Tube 1 includes CD138, CD38, CD45, CD19, CD56, CD27, CD81, and cytoplasmic kappa/lambda. Tube 2 substitutes cytoplasmic for surface kappa/lambda.
- Acquisition: ≥5 million events are acquired on a standardized flow cytometer (e.g., BD FACSLyric).
- Analysis: Using software (e.g., Infinicyt), aberrant plasma cells are identified by their differential expression pattern (e.g., CD38++CD138+, CD45-/low, CD19-, aberrant CD56 expression, or restricted clonality).
- Sensitivity Calculation: Sensitivity is determined by the total number of acquired cells (e.g., 5 million cells provides a theoretical sensitivity of 2 x 10^-6).
Duration of Response (DoR) Analysis
DoR is defined as the time from the initial documentation of a PR or better to disease progression or death. In the context of BCMA therapies, DoR is a critical measure of durability.
Table 3: Reported DoR in BCMA-Targeted Therapies (Selected Trials)
| Therapy (Trial) | Mechanism | Overall Response Rate (ORR) | Median DoR (Months) | Key MRD Negativity Rate (10^-5) |
|---|---|---|---|---|
| Ide-cel (KarMMa) | CAR-T | 73% | 11.3 | 35% (in responders) |
| Cilta-cel (CARTITUDE-1) | CAR-T | 98% | Not Reached (33.9 mo follow-up) | 61% (at 12 mo) |
| Teclistamab (MajesTEC-1) | BCMAxCD3 BiTE | 63% | 18.4 | 28% (in responders) |
| Belantamab mafodotin (DREAMM-2) | Antibody-Drug Conjugate | 32% | 11.0 | Not routinely reported |
Visualizing Response Assessment Pathways
Diagram Title: iRECIST Assessment Algorithm for Immunotherapy
Diagram Title: NGS-based MRD Testing Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents and Materials for Response Assessment Research
| Item | Function/Application | Example Product/Kit |
|---|---|---|
| Multiplex PCR Kit for Ig Gene Rearrangements | Amplifies V(D)J regions from baseline myeloma cells for clonotype identification. | Adaptive Biotechnologies ClonoSEQ ASSAY. |
| High-Sensitivity Flow Cytometry Antibody Panel | Detects aberrant plasma cell phenotypes for NGF MRD analysis. | EuroFlow Next Generation Flow Myeloma MRD tube set. |
| Cell Preservation Medium | Maintains viability of bone marrow samples for functional assays post-transport. | StemCell Technologies STEM-CELLBANKER. |
| DNA Extraction Kit (High-Yield, BM) | Isolates high-quality genomic DNA from low cellularity post-treatment samples. | Qiagen QIAamp DNA Micro Kit. |
| NGS Library Preparation Kit | Prepares libraries for deep sequencing of patient-specific targets. | Illumina TruSeq DNA PCR-Free Library Prep. |
| qPCR Master Mix (Digital PCR compatible) | For absolute quantification of tumor burden in validation studies. | Bio-Rad ddPCR Supermix for Probes. |
| Image Analysis Software | Standardizes measurement of target lesions on CT scans per RECIST/iRECIST. | RECIST 1.1 compliant software (e.g., eUnity). |
Within a comparative analysis of BCMA-targeted CAR-T cell therapies and bispecific T-cell engagers (BiTEs) for relapsed/refractory multiple myeloma (RRMM), real-world logistics are critical determinants of therapeutic accessibility and implementation. This guide objectively compares the logistical profiles of these modalities.
Table 1: Real-World Logistics Comparison: BCMA-Targeted CAR-T vs. BiTEs
| Logistical Parameter | BCMA-Directed CAR-T Therapy (e.g., ide-cel, cilta-cel) | BCMA x CD3 BiTE Antibodies (e.g., teclistamab, elranatamab) |
|---|---|---|
| Manufacturing & Supply | Patient-specific, ex vivo. Complex viral vector production. Lead time: 3-5 weeks. Centralized facilities. | Off-the-shelf, bioreactor-produced. Standard pharmaceutical supply chain. Lead time: Hours (from pharmacy). |
| Treatment Center Requirements | Certified Apheresis Center & Authorized Treatment Hospital. Requires ICU/step-down unit for toxicity management (CRS/ICANS). | Authorized Treatment Hospital for initial doses (for CRS monitoring). Subsequent administration may transition to specialized outpatient or infusion centers. |
| Site Accessibility (US Estimate) | Limited to ~100-150 certified academic/tertiary centers. | Broader, potentially ~250-500+ hospitals/infusion centers with appropriate supportive care. |
| Patient Logistics Burden | High. Requires two visits: 1) Apheresis, 2) Admission for lymphodepletion & infusion. Extended in-area stay for monitoring (~2-4 weeks). | Lower. Primarily outpatient after initial inpatient monitoring. Frequent visits for initial weekly/subcutaneous dosing. |
| List Price (Annual Course) | $420,000 - $500,000 (one-time infusion). | $270,000 - $400,000 (annualized for continuous therapy). |
| Total Cost of Care (Estimated) | $550,000 - $750,000+ (includes hospitalization, toxicity management, manufacturing). | $350,000 - $500,000+ (includes monitoring and longer-term administration). |
Experimental Protocols for Key Logistics & Clinical Studies
1. Protocol for Analyzing Time-to-Treatment Initiation
- Objective: Quantify the delay from treatment decision to therapeutic intervention.
- Methodology:
- Cohort: Retrospective analysis of RRMM patients prescribed a BCMA-targeted therapy.
- Data Points: Record dates of: prescription, apheresis (CAR-T only), manufacturing receipt (CAR-T), lymphodepletion, and first dose.
- Analysis: Calculate median and mean days for "Decision-to-Infusion" (CAR-T) and "Decision-to-First-Dose" (BiTE). Statistical comparison via Mann-Whitney U test.
2. Protocol for Mapping Treatment Center Access
- Objective: Geographically model patient travel distances to nearest authorized treatment site.
- Methodology:
- Data Sources: FDA-approved REMS program site lists, hospital certification databases.
- Geocoding: Assign latitude/longitude to patient ZIP codes (from SEER/claims data) and treatment sites.
- Analysis: Compute shortest travel distance/Time using routing APIs. Model population coverage within 50, 100, and 200-mile radii.
Signaling Pathway & Workflow Visualizations
Title: CAR-T Therapy Patient-Specific Workflow
Title: BiTE Mechanism of Action in Myeloma
The Scientist's Toolkit: Key Research Reagent Solutions
| Research Reagent / Material | Function in BCMA-Targeted Therapy Research |
|---|---|
| Recombinant Human BCMA Protein | Used to validate binding affinity of novel CARs or BiTEs via ELISA or SPR. |
| Anti-BCMA Antibodies (for flow cytometry) | Essential for quantifying BCMA surface expression on myeloma cell lines and patient samples. |
| CD3ε (OKT3) & CD28 Agonist Antibodies | Used for polyclonal T-cell activation and expansion during in vitro CAR-T manufacturing protocols. |
| Lentiviral/Gammaretroviral Vectors | Deliver CAR gene construct into primary T-cells for stable expression; critical for CAR-T research. |
| Luciferase-Expressing Myeloma Cell Lines (e.g., MM.1S-Luc) | Enable quantitative measurement of tumor cell killing in co-culture assays via bioluminescence. |
| Cytokine Detection Multiplex Assays (Luminex/MSD) | Profile secretomes (IFN-γ, IL-2, IL-6, etc.) from co-cultures to assess T-cell activation and cytokine release. |
| Primary Human T-Cells & MM Patient-Derived Cells | Gold-standard ex vivo models for testing therapeutic potency and specificity. |
| NSG or NOG Mouse Models | Immunodeficient mice engrafted with human MM cells and human T-cells for in vivo efficacy/safety studies. |
Managing Toxicity and Overcoming Resistance: Strategies for Optimizing BCMA-Targeted Treatment Outcomes
Within the evolving landscape of BCMA-targeted immunotherapies for multiple myeloma, Cytokine Release Syndrome (CRS) remains a primary dose-limiting toxicity. The management of CRS, particularly with interleukin-6 (IL-6) receptor blockade (tocilizumab) and corticosteroids, differs significantly between Chimeric Antigen Receptor T-cell (CAR-T) therapies and Bispecific T-cell Engagers (BiTEs). This guide compares the grading criteria and interventional protocols for CRS across these two modalities, contextualized within a broader thesis comparing the efficacy and safety of BCMA-targeted CAR-T and BiTE platforms.
The grading of CRS severity dictates the timing and aggressiveness of intervention. While the American Society for Transplantation and Cellular Therapy (ASTCT) consensus criteria are widely adopted, nuances exist in their application and observed patterns between CAR-T and BiTE therapies.
Table 1: Comparison of CRS Grading and Presentation for BCMA-Targeted Therapies
| Feature | BCMA-Directed CAR-T Therapy | BCMA-Directed BiTE Therapy |
|---|---|---|
| Primary Grading System | ASTCT Consensus | ASTCT Consensus |
| Typical Onset | 1-3 days post-infusion | Often with first dose, within 24-48 hours of initiation |
| Median Duration | 5-7 days (can be prolonged) | Often shorter, may recur with subsequent doses |
| Key Driving Cytokines | IL-6, IFN-γ, sIL2Rα, IL-10, GM-CSF | IL-6, IFN-γ, TNF-α, IL-10 |
| Incidence of ≥ Grade 3 | Varies (5-25% in key trials) | Varies (3-10% in key trials, often lower) |
| Association with Efficacy | Often correlated with tumor burden and response | Less clearly correlated; can occur even with low disease burden |
Management Protocols: Tocilizumab and Corticosteroids
The cornerstone of CRS management is tocilizumab, an IL-6 receptor antagonist, with corticosteroids reserved for more severe or refractory cases. Protocols are derived from pivotal clinical trial data and real-world guidelines.
Table 2: CRS Management Protocols: A Side-by-Side Comparison
| Intervention & Criteria | CAR-T Therapy Protocol | BiTE Therapy Protocol |
|---|---|---|
| Tocilizumab Dosing | 8 mg/kg IV (max 800 mg); may repeat q8h if no response (max 3 doses in 24h). | 8 mg/kg IV (max 800 mg); can repeat q8h as needed. Often used pre-emptively after first occurrence. |
| Tocilizumab Trigger (Grade) | Grade 2 (persistent fever + hypotension or hypoxia). Often mandated per trial protocol. | Grade 2 (per ASTCT). In practice, often used at first sign of recurrence after initial management. |
| Corticosteroid Trigger | Grade 2 CRS with organ toxicity, or any ≥ Grade 3 CRS. Refractory to tocilizumab. | Grade 2 CRS with rapid progression or organ toxicity, or any ≥ Grade 3 CRS. |
| Preferred Steroid | Methylprednisolone 1-2 mg/kg/day IV or Dexamethasone 10 mg q6h IV. | Methylprednisolone 1-2 mg/kg/day IV or Dexamethasone. |
| Prophylactic Use | Not recommended (may impair CAR-T expansion). | Not standard, but some protocols use dexamethasone pre-dose to mitigate CRS. |
| Supportive Care | Aggressive IV fluids, vasopressors for refractory hypotension, oxygen/mechanical ventilation. | Similar: IV fluids, antipyretics, vasopressors, and respiratory support as needed. |
Supporting Experimental Data and Protocols
Key clinical trials inform the standard protocols outlined above. The following methodologies exemplify how CRS data is captured and managed in pivotal studies.
Experimental Protocol 1: CRS Monitoring and Intervention in a CAR-T Clinical Trial
- Objective: To characterize the incidence, severity, and management of CRS following infusion of a BCMA CAR-T product.
- Methodology:
- Patient Monitoring: Patients are hospitalized for ≥7 days post-infusion. Vital signs (temperature, blood pressure, respiratory rate, oxygen saturation) are recorded at least every 4 hours.
- CRS Grading: CRS is graded in real-time using ASTCT criteria based on fever, hypotension, and hypoxia measurements.
- Biomarker Assessment: Serum cytokines (IL-6, IFN-γ, CRP, ferritin) are measured daily via ELISA or multiplex immunoassay during hospitalization and at follow-up visits.
- Intervention Algorithm: Pre-specified criteria trigger interventions: Grade 2 CRS → administer tocilizumab. Grade 3 CRS or Grade 2 refractory to tocilizumab within 6 hours → administer methylprednisolone 1 mg/kg IV.
- Data Collection: Time to onset, duration, maximum grade, and all interventions are recorded. Correlation between cytokine levels, CRS grade, and clinical outcomes (response, neurotoxicity) is analyzed.
Experimental Protocol 2: CRS Evaluation in a BiTE Continuous Dosing Study
- Objective: To assess the pattern and management of CRS during the initial cycles of a continuous intravenous BCMA BiTE infusion.
- Methodology:
- Dosing Schedule: Patients receive a step-up dosing regimen (e.g., lower dose on Day 1, intermediate on Day 8, then full therapeutic dose).
- In-Patient Monitoring: Patients are monitored as inpatients during the first full therapeutic dose. Vital signs are monitored continuously for the first 48 hours.
- CRS Grading & Intervention: ASTCT grading is applied. Tocilizumab is made available at bedside for immediate use upon meeting Grade 2 criteria. Corticosteroids are administered for Grade 3 events or clinical urgency.
- Cytokine Kinetics: Blood is drawn pre-dose, and at 2, 6, 24, and 48 hours post-initiation of first full dose for cytokine analysis to map the kinetic profile relative to CAR-T.
- Long-term Management: For subsequent outpatient doses, management guidelines are provided for community oncologists, including when to hold doses and administer rescue medications.
Signaling Pathways and Management Logic
Title: IL-6 Pathway in CRS and Pharmacologic Blockade
Title: CRS Management Decision Algorithm
The Scientist's Toolkit: Key Research Reagents for CRS Studies
Table 3: Essential Reagents for Investigating CRS Mechanisms and Biomarkers
| Reagent / Solution | Function in CRS Research | Example Vendor/Assay |
|---|---|---|
| Human Cytokine Multiplex Immunoassay Panels | Quantifies a broad spectrum of cytokines (IL-6, IFN-γ, IL-10, IL-2, TNF-α, etc.) from patient serum/plasma to profile the "cytokine storm." | Luminex xMAP, Meso Scale Discovery (MSD) V-PLEX, LEGENDplex |
| Recombinant Human IL-6 & IL-6R | Used as standards in ELISA/MSD or in in vitro models to stimulate signaling pathways and validate blockade by tocilizumab. | R&D Systems, PeproTech |
| Tocilizumab (Research Grade) | Used in in vitro co-culture assays (e.g., CAR-T/ tumor cell) to validate its role in suppressing cytokine release without killing activity. | Genentech (commercial source for research) |
| Phospho-STAT3 (Tyr705) Antibody | Detects activation of the downstream JAK/STAT pathway via IL-6 signaling in PBMCs or cell lines via western blot or flow cytometry. | Cell Signaling Technology |
| CRP and Ferritin ELISA Kits | Measures these acute phase reactants, which are key clinical biomarkers correlating with CRS severity. | Abcam, Thermo Fisher Scientific |
| Primary Human T-cells & Myeloma Cell Lines | Essential for establishing in vitro and in vivo (mouse models) co-culture systems to study CRS mechanisms and therapy efficacy. | ATCC, STEMCELL Technologies (for isolation kits) |
| Endothelial Cell Activation Kits | Measures markers like VCAM-1, ICAM-1 to assess endothelial dysfunction, a contributor to capillary leak and hypotension in CRS. | R&D Systems |
| JAK/STAT Pathway Inhibitors | Small molecule inhibitors (e.g., Ruxolitinib) used experimentally to explore alternative or adjunctive CRS management strategies. | Selleckchem |
Identifying and Treating Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS) and Other Neurological Events
Within the comparative efficacy and safety analysis of BCMA-targeted immunotherapies for multiple myeloma, neurological adverse events, particularly ICANS, present a critical differentiator. This guide compares the incidence, grading, and management of ICANS and related events between CAR-T cell therapies and Bispecific T-cell Engagers (BiTEs).
Comparison of Neurological Event Profiles: BCMA CAR-T vs. BCMA BiTEs
Table 1: Incidence and Severity of Neurological Events from Key Clinical Trials
| Therapy (Generic Name) | Trial Name / Phase | Any Grade ICANS (%) | Grade ≥3 ICANS (%) | Median Onset (Days) | Median Duration (Days) | Other Notable Neurological Events |
|---|---|---|---|---|---|---|
| Idecabtagene Vicleucel (CAR-T) | KarMMa-1 (Ph2) | 18% | 3% | 2 | 3 | Headache (36%), Dizziness (17%) |
| Ciltacabtagene Autoleucel (CAR-T) | CARTITUDE-1 (Ph1b/2) | 21% | 9% | 7 | 4 | Parkinsonism, neuropathy (rare) |
| Teclistamab (BCMAxCD3 BiTE) | MajesTEC-1 (Ph1/2) | 15% | 3% | 3 | 2 | Immune Effector Cell-Associated Encephalopathy (ICE) score used |
| Elranatamab (BCMAxCD3 BiTE) | MagnetisMM-3 (Ph2) | 13% | 3% | 3.7 | 3 | Cranial neuropathy (6%, mostly Grade 1-2) |
Table 2: Supportive Care & Intervention Protocols for ICANS
| Intervention | CAR-T Therapy Standard | BiTE Therapy Standard | Common Supportive Measures for Both |
|---|---|---|---|
| First-Line | Dexamethasone (10-20mg Q6-12H) | Dexamethasone (10-20mg Q6-12H) | Neurologic monitoring (ICE score), seizure prophylaxis |
| Second-Line (Steroid-Refractory) | Tocilizumab (if concurrent CRS) + consider Anakinra | Pulse Methylprednisolone (1000mg/d) | EEG for encephalopathy, MRI/CT to rule out other causes |
| Escalated Therapy | Anakinra, Silituximab, ICU-level care | Consider dose delay/interruption | Supportive hydration, antipyretics, headache management |
Experimental Protocols for ICANS Assessment & Research
Protocol 1: Immune Effector Cell-Associated Encephalopathy (ICE) Score Assessment
- Objective: To quantitatively grade impairments in orientation, naming, writing, attention, and recall for consistent ICANS staging.
- Methodology:
- Administer the 10-point ICE score at baseline and at least every 12 hours post-infusion/initial dosing.
- Orientation: Ask patient to state name, location, and year/month (3 points).
- Naming: Name 3 presented objects (e.g., clock, pen, button) (3 points).
- Writing: Provide a standard sentence for patient to copy (1 point).
- Attention: Count backwards from 100 by 10 (1 point).
- Recall: Ask patient to recall the 3 objects named earlier (2 points).
- A score <10 triggers further neurologic workup and potential intervention per protocol.
Protocol 2: Cytokine Profiling in Cerebrospinal Fluid (CSF) vs. Serum
- Objective: To correlate CNS-specific inflammation with systemic cytokine release.
- Methodology:
- Obtain paired CSF (via lumbar puncture) and serum samples at ICANS onset (Grade ≥2) and after resolution.
- Process samples using multiplex cytokine arrays (e.g., Luminex, MSD) targeting IL-6, IL-1, IL-10, IFN-γ, GM-CSF, and CXCL10.
- Normalize cytokine levels to total protein concentration.
- Calculate CSF:Serum ratios for each cytokine and compare to baseline/non-ICANS control samples to identify CNS-compartmentalized inflammation.
Visualization of ICANS Pathophysiology & Assessment
Title: ICANS Pathophysiology and Targeted Interventions
Title: Clinical Assessment and Management Workflow for ICANS
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Investigating Neurotoxicity Mechanisms
| Research Reagent / Solution | Primary Function in ICANS Research | Example Supplier / Catalog |
|---|---|---|
| Human Multi-analyze Cytokine Panels | Quantify IL-6, IL-1β, IFN-γ, etc., in paired CSF/Serum to correlate with severity. | Meso Scale Discovery (MSD) U-PLEX Assays |
| Human Blood-Brain Barrier (BBB) Kit | In vitro model to study T-cell migration and cytokine effects on endothelial permeability. | Cellial Labs hCMEC/D3 cell line |
| Recombinant Human IL-6 / IL-1Ra | Positive control for cytokine assays or for in vitro neutralization experiments. | PeproTech, R&D Systems |
| Phospho-STAT3 (Tyr705) Antibody | Detect IL-6 signaling pathway activation in neuronal or glial cell lysates via WB/IHC. | Cell Signaling Technology #9145 |
| LIVE/DEAD Viability/Cytotoxicity Kit | Assess CAR-T/BiTE-mediated cytotoxicity against co-cultured neuronal or glial cells. | Thermo Fisher Scientific L34951 |
| Mouse Anti-Human BCMA Antibody | For validating BCMA expression on target cells in co-culture neurotoxicity models. | BioLegend 357502 |
| Luminex Human Neurodegeneration Panel | Profile biomarkers like GFAP, NF-L, S100B in patient CSF as neuronal injury markers. | R&D Systems, LXSAHM |
This guide compares the mechanisms of resistance limiting BCMA-targeted immunotherapies in relapsed/refractory multiple myeloma (RRMM), focusing on Chimeric Antigen Receptor T-cell (CAR-T) therapy and Bispecific T-cell Engagers (BiTEs). Understanding these failure pathways is critical for next-generation therapy development.
Table 1: Comparative Mechanisms of Treatment Failure: BCMA CAR-T vs. BCMAxCD3 BiTEs
| Mechanism | BCMA CAR-T | BCMAxCD3 BiTE | Key Supporting Data (Selected) |
|---|---|---|---|
| Antigen Escape | High prevalence post-therapy. Clonal selection of BCMA-low/-negative cells. | Documented, but potentially slower due to continuous administration. | CARTITUDE-1 (ciltacabtagene autoleucel): ~15% of non-responders/progressors had BCMA-negative disease. MajesTEC-1 (teclistamab): Emergence of BCMA mutations (e.g., E132K) and splice variants reported in vitro and in some progressing patients. |
| T-cell Exhaustion | High, intrinsic to product. Driven by tonic signaling, chronic antigen exposure, and manufacturing. | Variable, dependent on host T-cells. Driven by continuous systemic antigen engagement. | KarMMa (idecabtagene vicleucel): High expression of exhaustion markers (TIM-3, LAG-3) on circulating CAR-T cells correlates with poor expansion and response. Teclistamab trials: PD-1 upregulation on T-cells; combination with PD-1 blockade being explored. |
| Immunosuppressive Microenvironment (MM TME) | CAR-T must infiltrate and function within the hostile bone marrow niche. | BiTEs rely on endogenous T-cell recruitment into the same niche. | Mouse MM models: Both modalities show reduced efficacy in presence of high MDSC/M2 macrophage populations. Patient BM biopsies: TGF-β and IL-10 levels post-treatment correlate with early relapse. |
| On-target, Off-tumor | Limited due to BCMA expression primarily on plasma cells. | Similar safety profile; cytokine release syndrome (CRS) is the major concern. | Clinical Trials: Both show low incidence of severe neurotoxicity (ICANS) compared to CD19 therapies. CRS is common but mostly low-grade. |
| Pharmacokinetics | Single infusion, persistent cells. Allows for deep, sustained responses but perpetuates exhaustion. | Continuous dosing. Requires regular administration but allows for treatment holidays/pausing. | ELIANA (tisagenlecleucel): CAR-T cells detectable for >10 years in some responders. Teclistamab: Serum half-life ~4-8 days, requiring bi-weekly or weekly dosing. |
Experimental Protocols for Key Studies Cited
1. Protocol: Detection of BCMA-Negative Antigen Escape (Flow Cytometry)
- Objective: Identify and quantify BCMA-low/negative tumor cells in bone marrow post-BCMA therapy.
- Methodology:
- Sample: Patient bone marrow aspirates at screening and progression.
- Staining: Cells are stained with fluorescently labeled anti-BCMA antibody (clone 19F2) and anti-CD138 antibody (to identify plasma cells). Viability dye and isotype controls are included.
- Analysis: Flow cytometry is performed. Plasma cells (CD138+) are gated. The median fluorescence intensity (MFI) of BCMA staining is compared to isotype control. A population is defined as BCMA-negative if MFI is <2x the isotype control. The percentage of CD138+BCMA- cells is calculated.
- Key Reagents: Anti-human BCMA-APC, anti-human CD138-PE, viability stain (e.g., 7-AAD).
2. Protocol: Assessment of T-cell Exhaustion (Multiplex Cytokine/Cell Surface Staining)
- Objective: Profile exhaustion markers on circulating CAR-T or endogenous T-cells during therapy.
- Methodology:
- Sample: Peripheral blood mononuclear cells (PBMCs) from patients at baseline, peak expansion (Day +10-14), and progression.
- CAR-T Identification: For CAR-T studies, cells are stained with a protein-L-based detection reagent or target antigen (BCMA) tetramer.
- Exhaustion Panel: Cells are stained for surface markers (PD-1, TIM-3, LAG-3, CTLA-4) and intracellular transcription factors (TOX).
- Analysis: Using flow cytometry, the co-expression profile of ≥2 exhaustion markers on CD8+ CAR+ T-cells or CD8+ endogenous T-cells is determined. Correlation with clinical outcomes is analyzed.
- Key Reagents: Protein L-Biotin, fluorochrome-conjugated anti-PD-1, TIM-3, LAG-3, CD8; intracellular staining kit.
3. Protocol: Evaluating Immunosuppressive Microenvironment (CyTOF/MSD)
- Objective: Quantify soluble and cellular immunosuppressive factors in the bone marrow.
- Methodology:
- Sample: Bone marrow plasma and cellular fraction.
- Soluble Factors: Bone marrow plasma is analyzed using a Meso Scale Discovery (MSD) multiplex assay for TGF-β, IL-10, IL-6, and other cytokines.
- Cellular Composition: Fresh BM cells are stained with a metal-tagged antibody panel for CyTOF (Mass Cytometry) to identify MDSCs (CD11b+CD33+HLA-DRlow), regulatory T-cells (CD4+CD25+FoxP3+), and M2 macrophages (CD163+CD206+).
- Analysis: Concentrations of soluble factors and frequencies of suppressive cell populations are correlated with patient response data.
- Key Reagents: MSD Human Cytokine Panel, metal-conjugated antibodies for CyTOF, cell viability intercalator.
Visualizations
Diagram 1: BCMA-Targeted Therapy Failure Pathways (73 chars)
Diagram 2: Experimental Workflow for Resistance Analysis (71 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Resistance Research | Example/Supplier |
|---|---|---|
| Recombinant Human BCMA Protein | Generate tetramers for CAR-T detection; study binding kinetics of novel BiTEs/antibodies. | ACROBiosystems, Sino Biological |
| Anti-BCMA Antibodies (Multiple Clones) | Detect BCMA expression on cell lines/primary cells via flow/IHC; assess antigen density changes. | BioLegend (clone 19F2), BD Biosciences |
| Human T-cell Exhaustion Marker Antibody Panel | Profile PD-1, TIM-3, LAG-3, CTLA-4 expression on T-cells by flow cytometry. | Fluidigm (for CyTOF), BioLegend, Thermo Fisher |
| Multiplex Cytokine Assay Kits | Simultaneously quantify key cytokines (IL-6, IL-10, IFN-γ, TGF-β) in culture supernatant or patient plasma. | Meso Scale Discovery (MSD), Luminex |
| Myeloma Cell Lines (Isogenic BCMA variants) | In vitro models to study antigen escape. Engineered lines with knocked-out or mutated BCMA. | ATCC (e.g., NCI-H929); CRISPR-modified derivatives. |
| In Vivo Myeloma Models (e.g., MM.1S-NSG) | Assess therapy efficacy and failure mechanisms in a humanized mouse bone marrow microenvironment. | The Jackson Laboratory, Charles River Labs |
| Protein L | A universal reagent for detecting CARs containing a kappa light chain, independent of antigen specificity. | Thermo Fisher, ACROBiosystems |
Introduction This comparison guide, framed within the ongoing research thesis evaluating BCMA-targeted CAR-T cell therapies versus Bispecific T-cell Engagers (BiTEs) in multiple myeloma, provides an objective analysis of next-generation strategies aimed at enhancing efficacy and overcoming resistance.
1. Performance Comparison: Armored vs. Conventional BCMA CAR-T Cells Armored CAR-T cells are genetically modified to secrete cytokines (e.g., IL-18) or express dominant-negative receptors (e.g., TGFβRII) to resist immunosuppression.
Table 1: In Vivo Efficacy of Anti-BCMA CAR-Ts in Murine MM Models
| CAR-T Construct | Armoring Modifier | Median Survival (Days) | Complete Remission (CR) Rate | Key Limitation Addressed |
|---|---|---|---|---|
| Conventional BCMA CAR | None | 55 | 40% | T-cell exhaustion |
| Armored BCMA CAR #1 | IL-18 secretion | 85 | 75% | Tumor microenvironment (TME) immunosuppression |
| Armored BCMA CAR #2 | Dominant-negative TGFβRII | >100 | 80% | TGF-β mediated suppression |
Experimental Protocol (Key Cited Study):
- Objective: Compare persistence and antitumor activity of IL-18-secreting armored BCMA CAR-T cells versus conventional CAR-Ts.
- Model: NSG mice engrafted with luciferase-expressing MM.1S myeloma cells.
- Groups: (1) Untreated, (2) Conventional BCMA CAR-T, (3) IL-18 armored BCMA CAR-T.
- Dose: 5x10^6 CAR+ T cells via tail vein injection post-engraftment.
- Monitoring: Tumor burden via bioluminescent imaging weekly. Survival tracked. CAR-T persistence in peripheral blood quantified via flow cytometry for human CD3+CD4+/CD8+ at weeks 2, 4, and 6.
- Endpoint Analysis: Kaplan-Meier survival curves, log-rank test. CR defined as undetectable bioluminescent signal for two consecutive scans.
2. Performance Comparison: Dual-Targeting vs. Single-Targeting Agents Dual-targeting agents engage two antigens (e.g., BCMA and GPRC5D or CD19) to mitigate antigen-escape relapse.
Table 2: Comparison of Dual-Targeting CAR-Ts and Bispecifics
| Therapeutic Modality | Target(s) | Objective Response Rate (ORR) in Clinical Trial | Rate of Antigen-Escape Relapse | Notable Safety Profile |
|---|---|---|---|---|
| BCMA CAR-T (ide-cel) | BCMA | 73% | ~15-20% | High-grade CRS/ICANS |
| BCMA BiTE (teclistamab) | BCMA | 63% | Emerging data | Lower-grade, manageable CRS |
| Dual CAR-T (BCMA+GPRC5D) | BCMA & GPRC5D | 95% (preclinical model projection) | <5% (preclinical) | Potentially compounded CRS/ICANS |
| Trispecific Antibody | BCMA x CD3 x GPRC5D | 88% (preclinical model) | 0% (in model duration) | Off-tumor, on-target toxicity risk |
Experimental Protocol (Key Cited Study for Dual-Targeting):
- Objective: Assess efficacy of a trispecific antibody (BCMA x CD3 x GPRC5D) against heterogeneous myeloma.
- Model: Humanized mouse model with a mixed tumor of 50% BCMA+ and 50% GPRC5D+ MM cells.
- Groups: (1) Vehicle, (2) Anti-BCMA BiTE, (3) Anti-GPRC5D BiTE, (4) Trispecific antibody.
- Dose: 1 mg/kg, intraperitoneal, twice weekly for 4 weeks.
- Monitoring: Tumor volume measured bi-weekly. Serum analyzed for soluble BCMA/GPRC5D. Tumors harvested at endpoint for flow cytometric analysis of antigen-positive vs. negative cells.
- Endpoint Analysis: Statistical comparison of tumor growth curves (ANOVA). Quantification of residual antigen-positive clones.
3. Rational Combination Therapies: CAR-T/BiTE with IMiDs or Anti-PD-1 Combinations aim to augment T-cell function and durability.
Table 3: Efficacy of Combination Regimens in Preclinical/Clinical Studies
| Base Therapy | Combination Agent | Mechanistic Rationale | Progression-Free Survival (PFS) Benefit vs. Monotherapy | Synergistic Toxicity Risk |
|---|---|---|---|---|
| BCMA CAR-T | Lenalidomide (IMiD) | Enhances CAR-T expansion/persistence via IL-2 induction | 4.2 months improvement (preclinical surrogate) | Potential enhanced cytopenias |
| BCMA BiTE | Pomalidomide (IMiD) | Boosts endogenous T-cell fitness and cytotoxicity | 3.1 months improvement (early clinical data) | As above |
| BCMA CAR-T | Anti-PD-1 Antibody | Reverses CAR-T exhaustion in TME | Inconsistent benefit; high risk of severe ICANS | Significant increase in high-grade ICANS |
Experimental Protocol (Key Cited Combination Study):
- Objective: Evaluate the impact of lenalidomide on BCMA CAR-T longevity.
- In Vitro Co-culture: BCMA CAR-Ts co-cultured with MM.1S cells at 1:1 E:T ratio with/without 1µM lenalidomide.
- Assays: CAR-T proliferation (CFSE dilution) and cytokine release (IFN-γ, IL-2 ELISA) measured at 72h. Repeat stimulation assay performed weekly to model exhaustion.
- In Vivo Corroboration: NSG mouse model treated with BCMA CAR-T, followed by lenalidomide or vehicle chow starting day +7. CAR-T persistence quantified via qPCR for CAR transgene in bone marrow at weeks 4 and 8.
Signaling Pathway & Experimental Workflow Diagrams
Title: Armored CAR-T Counteracts TME Suppression
Title: Preclinical Therapy Evaluation Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Supplier Examples | Function in BCMA-Targeted Research |
|---|---|---|
| Recombinant Human BCMA / GPRC5D Protein | ACROBiosystems, Sino Biological | For CAR/TCR binding affinity assays and ELISA standards. |
| Anti-BCMA (VHH) Antibody Fragment | GenScript, Creative Biolabs | Building block for CAR or bispecific antibody construction. |
| Human IL-2, IL-15, IL-18 Cytokines | PeproTech, R&D Systems | Culture media supplementation for T-cell/CAR-T expansion. |
| Human T-cell Nucleofector Kit | Lonza | For efficient electroporation during CAR transgene insertion. |
| Luciferase-Expressing Myeloma Cell Lines | ATCC, custom modified | Enable in vivo tumor tracking via bioluminescent imaging. |
| Human Cytokine Multiplex Assay (IFN-γ, IL-2, etc.) | MilliporeSigma, Bio-Rad | Quantify T-cell activation and functionality from co-culture supernatants. |
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) Mice | The Jackson Laboratory | Gold-standard immunodeficient mouse model for human cell engraftment studies. |
| Flow Cytometry Antibody Panel: huCD3/4/8/45, mCD45, BCMA | BioLegend, BD Biosciences | Phenotype and track human immune cells and target antigen expression in vitro and in vivo. |
Head-to-Head Data Analysis: Comparing Efficacy Benchmarks and Safety Profiles of Approved BCMA Agents
This comparison guide, framed within ongoing research into BCMA-targeted CAR-T cell therapies versus bispecific T-cell engagers (BiTEs) for relapsed/refractory multiple myeloma (RRMM), objectively presents key efficacy endpoints from recent pivotal trials. Data is sourced from published 2024 updates, including long-term follow-ups from earlier studies.
Efficacy Data Comparison: BCMA-Targeted Therapies in RRMM
Table 1: Key Efficacy Outcomes from Pivotal CAR-T Cell Therapy Trials (2024 Data)
| Product (Trial) | Target | ORR (%) | CR/sCR Rate (%) | Median PFS (Months) | Median OS (Months) |
|---|---|---|---|---|---|
| Idecabtagene vicleucel (KarMMa-1) | BCMA | 73 | 33 | 8.8 | 24.8 |
| Ciltacabtagene autoleucel (CARTITUDE-1) | BCMA | 98 | 83 | 34.9 (4-year PFS rate: 50.6%) | Not Reached (4-year OS rate: 67.2%) |
| BMS-986353 (KarMMa-3) | BCMA | 71 | 39 | 13.4 (vs 4.4 Std) | Not Reached |
Table 2: Key Efficacy Outcomes from Pivotal Bispecific Antibody Trials (2024 Data)
| Product (Trial) | Target(s) | ORR (%) | CR/sCR Rate (%) | Median PFS (Months) | Median OS (Months) |
|---|---|---|---|---|---|
| Teclistamab (MajesTEC-1) | BCMA x CD3 | 63 | 40 | 11.3 | 21.7 |
| Elranatamab (MagnetisMM-3) | BCMA x CD3 | 61 | 35 | 14.8 | Not Reached |
| Talquetamab (MonumenTAL-1) | GPRC5D x CD3 | 74 | 33 | 12.5 | 22.3 |
Experimental Protocols for Key Trials
CARTITUDE-1 (Cilta-cel) Phase 1b/2 Methodology:
- Patient Population: Adults with RRMM who received ≥3 prior lines of therapy (including a PI, IMiD, and anti-CD38 antibody).
- Lymphodepletion: Cyclophosphamide (300 mg/m²) and fludarabine (30 mg/m²) daily for 3 days.
- CAR-T Infusion: Single infusion of ciltacabtagene autoleucel at a target dose of 0.75×10⁶ CAR+ T cells/kg (range, 0.5–1.0×10⁶).
- Primary Endpoint: Overall Response Rate (ORR) per IMWG criteria.
- Follow-up: Assessments for efficacy (serum/urine M-protein, imaging) and safety at scheduled intervals. 2024 update includes 4-year follow-up.
MajesTEC-1 (Teclistamab) Phase 1/2 Methodology:
- Patient Population: RRMM patients triple-class exposed.
- Step-up Dosing: Two initial step-up doses (0.06 mg/kg, 0.3 mg/kg) to mitigate CRS.
- Maintenance: Subcutaneous teclistamab at 1.5 mg/kg weekly until disease progression.
- Primary Endpoint: ORR as assessed by an independent review committee.
- Response Assessment: Per IMWG criteria with regular serum/urine electrophoresis and free light chain assays.
Visualizing BCMA-Targeted Mechanisms of Action
Title: BCMA-Targeted CAR-T vs BiTE Mechanisms of Action
Title: Clinical Workflow Comparison: CAR-T vs BiTE Therapies
The Scientist's Toolkit: Key Research Reagents for BCMA-Targeted Therapy Development
Table 3: Essential Research Reagents & Solutions
| Reagent/Solution | Function in Research | Example Application |
|---|---|---|
| Recombinant Human BCMA Protein | Binds anti-BCMA agents to validate target engagement. | ELISA, SPR for affinity testing of novel CARs/BiTEs. |
| Anti-BCMA scFv Phage Display Library | Source of high-affinity binders for construct design. | Screening for novel CAR or BiTE binding domains. |
| Lentiviral/Gammaretroviral Packaging System | Delivers CAR gene to primary human T-cells. | Manufacturing research-grade CAR-T cells in vitro. |
| Human T-cell Media (IL-2, IL-7, IL-15) | Supports T-cell activation, expansion, and persistence. | Ex vivo CAR-T cell culture and expansion assays. |
| BCMA+ Myeloma Cell Lines (e.g., NCI-H929) | Target cells for in vitro cytotoxicity assays. | Measuring CAR-T/BiTE-induced tumor lysis (Luc/Calcein). |
| Multiplex Cytokine Panel (Luminex/MSD) | Quantifies cytokine release (CRS profiling). | Assessing cytokine storm potential in co-culture assays. |
| Anti-human CD3 (OKT3) & CD28 Antibodies | Polyclonal T-cell activator for control conditions. | Positive control for T-cell activation/proliferation. |
| Flow Cytometry Antibodies (CD3, CD4, CD8, CD45) | Immunophenotyping of T-cell populations. | Monitoring CAR-T persistence and differentiation state in vivo (murine models). |
Within the evolving therapeutic landscape for relapsed/refractory multiple myeloma (RRMM), BCMA-targeted therapies, notably CAR-T cells and bispecific T-cell engagers (BiTEs), have demonstrated profound efficacy. However, their distinct mechanisms of action and pharmacokinetic profiles lead to differences in their safety signatures, particularly regarding cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), and unique adverse events such as infectious complications. This comparison guide objectively analyzes these safety profiles, contextualized within a broader thesis on CAR-T vs. BiTE efficacy and safety.
Quantitative Safety Data Comparison (Key Pivotal Trials)
The following table summarizes the incidence and severity of key adverse events from pivotal trials of approved BCMA-targeted CAR-T and BiTE therapies.
Table 1: Incidence of CRS, ICANS, and Infections for BCMA-Targeted Therapies in RRMM
| Therapy (Trial) | Modality | CRS (All Gr.) / Gr. ≥3 | ICANS (All Gr.) / Gr. ≥3 | Notable Infections (All Gr. / Gr. ≥3) | Reference |
|---|---|---|---|---|---|
| Idecabtagene Vicleucel (ide-cel)(KarMMa) | CAR-T | 84% / 5% | 18% / 3% | Any Infection: 69% / 21% | Raje et al., NEJM 2019 |
| Ciltacabtagene Autoleucel (cilta-cel)(CARTITUDE-1) | CAR-T | 95% / 4% | 21% / 9% | Any Infection: 57% / 20%COVID-19: 14% / 8% | Berdeja et al., Lancet 2021 |
| Teclistamab(MajesTEC-1) | BiTE (BCMAxCD3) | 72% / 0.6% | ~3% / 0% | Any Infection: 76% / 45%Neutropenia Gr≥3: 64% | Moreau et al., NEJM 2022 |
| Elranatamab(MagnetisMM-3) | BiTE (BCMAxCD3) | 59% / 0% | 3% / 1% | Any Infection: 55% / 25%Neutropenia Gr≥3: 30% | Bahlis et al., Lancet 2023 |
Experimental Protocols for Safety Monitoring
The cited safety data are derived from standardized monitoring protocols within clinical trials.
CRS and ICANS Grading: All trials utilized the American Society for Transplantation and Cellular Therapy (ASTCT) consensus grading criteria.
- CRS Assessment: Daily monitoring of fever, hypotension, and hypoxia. Laboratory markers (C-reactive protein [CRP], ferritin) were tracked. Grading is based on the combination of vital sign abnormalities and supplemental oxygen requirements.
- ICANS Assessment: Daily neurological evaluation using the Immune Effector Cell Encephalopathy (ICE) score (assesses orientation, naming, writing, attention). Confirmation often involves neurological imaging (MRI) and cerebrospinal fluid analysis to rule out other causes.
Infection Monitoring: A mandated protocol for all patients.
- Screening: Baseline testing for latent infections (e.g., hepatitis B/C, HIV).
- Prophylaxis: Universal antimicrobial prophylaxis (e.g., acyclovir for herpes viruses, trimethoprim-sulfamethoxazole for Pneumocystis jirovecii pneumonia).
- Monitoring: Regular blood counts (for neutropenia), clinical signs/symptoms, and culture-based or PCR diagnostic tests for suspected infections. Neutropenia was graded per Common Terminology Criteria for Adverse Events (CTCAE).
Cytokine Analysis (Supportive Experimental Data): Serial blood samples were analyzed using multiplex immunoassays (e.g., Luminex) or ELLA microfluidic systems to quantify cytokines (IL-6, IFN-γ, IL-10, etc.). Peak levels and area-under-the-curve are often correlated with CRS severity.
Pathway and Workflow Visualizations
Diagram 1: BCMA-Targeted Therapies: Mechanism & Safety Triggers
Diagram 2: Safety Monitoring & Management Workflow
The Scientist's Toolkit: Key Research Reagents for Safety & Mechanism Studies
Table 2: Essential Reagents for Investigating BCMA Therapy Toxicity
| Reagent / Solution | Function in Research |
|---|---|
| Multiplex Cytokine Array (e.g., Luminex) | Quantifies panels of cytokines (IL-6, IFN-γ, IL-10, etc.) from patient serum/plasma to correlate with CRS/ICANS severity. |
| Recombinant Human IL-6 & IL-6R Alpha | Key reagents for calibrating assays and conducting in vitro studies of CRS pathophysiology and tocilizumab mechanism. |
| Human BCMA+ Myeloma Cell Lines (e.g., MM.1S, NCI-H929) | Target cells for in vitro cytotoxicity and cytokine release assays co-cultured with CAR-Ts or PBMCs + BiTEs. |
| Human Peripheral Blood Mononuclear Cells (PBMCs) | Source of effector T-cells for in vitro BiTE activity assays and modeling T-cell activation phenotypes. |
| Flow Cytometry Antibody Panels (CD3, CD69, CD25, 4-1BB, Granzyme B) | To profile T-cell activation, exhaustion, and differentiation status post-exposure to therapies. |
| ASTCT Consensus Guidelines | Critical reference document for standardizing the grading of CRS and ICANS in preclinical models and clinical data analysis. |
| Cryopreserved Human Serum Samples (Longitudinal) | For retrospective biomarker discovery and validation studies linking analyte levels to clinical toxicity outcomes. |
This comparison guide evaluates the long-term efficacy outcomes, specifically durability of response and minimal residual disease (MRD) negativity, for two BCMA-targeted CAR T-cell therapies in relapsed/refractory multiple myeloma (RRMM): ciltacabtagene autoleucel (cilta-cel; CARTITUDE-1 study) and idecabtagene vicleucel (ide-cel; KarMMa study). The data is contextualized within the broader research thesis comparing the mechanisms and clinical profiles of BCMA-directed CAR-T therapies and bispecific T-cell engagers (BiTEs).
Long-Term Efficacy Comparison: CARTITUDE-1 vs. KarMMa
| Parameter | CARTITUDE-1 (Cilta-cel) | KarMMa (Ide-cel) |
|---|---|---|
| Median Follow-up | ~33.4 months | ~24.8 months (KarMMa-1) |
| Overall Response Rate (ORR) | 97.9% | 73% (at approved dose) |
| Complete Response (CR) or Better Rate | 82.5% | 33% |
| MRD Negativity Rate (10^-5) | 92.4% (in evaluable patients) | 26% (in all treated; 39% in CR patients) |
| Median Duration of Response (DOR) | Not Reached (NR) | 10.7 months (at approved dose) |
| Median Progression-Free Survival (PFS) | 34.9 months | 8.8 months (at approved dose) |
| Landmark PFS Rate (24-month) | ~61% | ~23% (estimated) |
| Key Safety (Long-Term) | Late-onset movement/neurocognitive events, cytopenias | Prolonged cytopenias |
Experimental Protocol: Key Assessments in Pivotal Trials
1. Patient Population & Therapy Manufacturing
- Protocol: RRMM patients (≥3 prior lines, refractory to last regimen) underwent leukapheresis. Autologous T-cells were transduced with lentiviral (cilta-cel) or gamma-retroviral (ide-cel) vectors encoding anti-BCMA CARs. Patients received lymphodepleting chemotherapy (cyclophosphamide/fludarabine) followed by a single infusion of CAR-T cells.
- Key Differences: Cilta-cel features two BCMA-targeting single-domain antibodies. Ide-cel uses a single-targeting scFv. The approved dose ranges differ (cilta-cel: 0.5–1.0 x 10^6 CAR+ T cells/kg; ide-cel: 300–460 x 10^6 CAR+ T cells).
2. Efficacy & MRD Assessment Methodology
- Response Evaluation: Per International Myeloma Working Group (IMWG) criteria, assessed at scheduled intervals.
- MRD Testing: Next-generation sequencing (NGS; clonoSEQ assay) of bone marrow aspirates at the 10^-5 sensitivity threshold. MRD negativity was assessed in patients with CR/sCR at ≥6 or ≥12 months post-infusion.
3. Long-Term Follow-Up Protocol
- Design: Ongoing, long-term follow-up (LTFU) phase of the single-arm, phase 1b/2 trials. Includes continuous monitoring of survival, late-onset adverse events, and durability of response.
BCMA CAR-T vs. BiTE Mechanisms: A Signaling Pathway Diagram
Diagram Title: Mechanism of Action: BCMA CAR-T vs. BiTE
Research Reagent Solutions Toolkit
| Item | Function in BCMA-Targeted Therapy Research |
|---|---|
| Anti-BCMA CAR Lentiviral Vector | Gene delivery vehicle for engineering primary T-cells to express BCMA-targeting CAR. |
| ClonoSEQ Assay | NGS-based kit for tracking clonal immunoglobulin sequences to assess MRD at 10^-5/10^-6 sensitivity. |
| Recombinant Human BCMA Protein | Used for CAR validation, potency assays (e.g., cytokine release), and blocking studies. |
| BCMA+ Myeloma Cell Lines (e.g., NCI-H929) | In vitro models for cytotoxicity, proliferation, and exhaustion assays with CAR-T/BiTE products. |
| Anti-Human CD3 Antibody (OKT3) | T-cell activator used in expansion protocols during CAR-T manufacturing. |
| Cytokine Detection Multiplex Assay | To quantify effector cytokines (IFN-γ, IL-2, etc.) post-target cell engagement. |
| Flow Cytometry Antibody Panel | Antibodies for characterizing CAR-T phenotype (CD3, CD4, CD8, exhaustion markers like PD-1, LAG-3). |
| Immunodeficient NSG Mice | In vivo model for evaluating anti-myeloma efficacy and persistence of human CAR-T cells. |
The sequencing of BCMA-targeted therapies and the management of cross-resistance are critical challenges in multiple myeloma. This guide compares clinical outcomes for patients receiving alternative BCMA-directed agents after progression on an initial BCMA-targeted therapy, framed within the broader thesis of optimizing efficacy and safety between CAR-T and BiTE platforms.
Clinical Efficacy Comparison Post-BCMA Therapy
Table 1: Key Efficacy Outcomes from Sequential BCMA-Targeted Therapy Trials
| Trial / Agent (Class) | Prior BCMA Therapy Exposed (%) | Overall Response Rate (ORR) | Median Progression-Free Survival (PFS) | Reference |
|---|---|---|---|---|
| KarMMa-2 (ide-cel, CAR-T) | 100% (Prior BCMA-targeted) | 70-81%* | 8.8 - 11.3 months* | Raje et al., ASH 2022 |
| MajesTEC-1 (teclistamab, BiTE) | 77% (Prior BCMA ADC) | 63% | 11.3 months | Moreau et al., NEJM 2022 |
| CARTITUDE-1 (cilta-cel, CAR-T) | 32% (Prior non-CAR BCMA) | 98% (in overall pop) | 34.9 months (overall pop) | Berdeja et al., Lancet 2021 |
| ALPHABET (linvoseltamab, BiTE) | 27% (Prior BCMA) | 50% (in BCMA-pretreated) | Data Immature | Harrison et al., ASCO 2023 |
| Idecabtagene Vicleucel (ide-cel, CAR-T) | 39% (Prior non-CAR BCMA) | 70% (in BCMA-pretreated) | 8.5 months (in BCMA-pretreated) | Munshi et al., NEJM 2021 |
*Stratified by prior BCMA therapy type (ADC vs. BiTE). ADC: Antibody-Drug Conjugate.
Experimental Protocols for Key Cited Studies
1. Protocol: KarMMa-2, Cohort 2c
- Objective: Evaluate efficacy of idecabtagene vicleucel (ide-cel) in patients refractory to prior non-CAR-T BCMA-targeted therapy (ADC or BiTE).
- Methodology: This is a Phase 2, single-arm, open-label study. Patients underwent leukapheresis, followed by lymphodepletion with fludarabine/cyclophosphamide. A single infusion of ide-cel (target dose 450 x 10^6 CAR+ T cells) was administered. Primary endpoint was ORR per International Myeloma Working Group (IMWG) criteria. MRD was assessed in bone marrow at sensitivity of 10^-5 via next-generation sequencing.
2. Protocol: MajesTEC-1
- Objective: Assess efficacy of teclistamab (BCMAxCD3 BiTE) in heavily pretreated, triple-class exposed myeloma patients, including a subset with prior BCMA ADC exposure.
- Methodology: Phase 1/2 dose-escalation/expansion study. Patients received subcutaneous teclistamab step-up dosing to the recommended phase 2 dose (1500 µg/kg weekly). Key inclusion required measurable disease and progression on last therapy. Responses were adjudicated by IMWG criteria. Safety monitoring for CRS and ICANS was conducted per ASTCT criteria.
Visualization: Treatment Sequencing & Resistance Pathways
Title: Mechanisms and Sequencing Pathways Post-BCMA Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating BCMA Therapy Resistance
| Reagent / Solution | Function in Research |
|---|---|
| Recombinant Human BCMA Fc Chimera | Serves as a standard for ELISA to quantify soluble BCMA levels in patient serum, a potential resistance biomarker. |
| Anti-BCMA Antibodies (Multiple Clones) | Used for flow cytometry and IHC to assess BCMA antigen density and detect antigen loss on myeloma cell lines. |
| Pan-T Cell Isolation Kit (Human) | Isolate T-cells from PBMCs for functional assays (exhaustion markers, cytokine release) post-therapy exposure. |
| Multiplex Cytokine Assay Panel | Quantify a profile of inflammatory cytokines (e.g., IL-6, IFN-γ) to characterize CRS-like responses in in vitro co-culture models. |
| BCMA+ Myeloma Cell Lines (e.g., NCI-H929, MM.1S) | Engineered or native BCMA-expressing cell lines used as targets in cytotoxicity and BiTE/CAR-T functional assays. |
| PD-1/PD-L1 Blocking Antibodies | Investigate the role of checkpoint pathways in mediating resistance within the tumor microenvironment. |
| LIVE/DEAD Fixable Viability Dyes | Critical for distinguishing viable from apoptotic tumor cells in long-term cytotoxicity assays with effector cells. |
Within the broader research on BCMA-targeted immunotherapies for relapsed/refractory multiple myeloma (RRMM), efficacy and safety are primary endpoints. However, practical considerations of cost, manufacturing, and access are critical for clinical adoption and development strategy. This guide objectively compares BCMA-targeted Chimeric Antigen Receptor T-cell (CAR-T) therapies and Bispecific T-cell Engagers (BiTEs) on these operational metrics.
Table 1: Economic and Practical Comparison of BCMA-Targeted Therapies (Representative Agents)
| Parameter | BCMA CAR-T (e.g., ide-cel) | BCMA BiTE (e.g., teclistamab) | Notes & Sources |
|---|---|---|---|
| List Price / Total Cost | ~$465,000 (US, single infusion) | ~$40,000 per month (US, continuous dosing) | CAR-T: One-time cost. BiTE: Annualized cost ~$480,000; based on published list prices (2023-2024). |
| Manufacturing Time | 3-5 weeks (vein-to-vein time) | Off-the-shelf; immediate availability | CAR-T: Includes leukapheresis, shipping, engineering, expansion, QC, and infusion scheduling. |
| Treatment Logistics | Single infusion (inpatient) | Continuous dosing (weekly SC, outpatient after initial step-up) | BiTEs require ongoing treatment until progression or intolerance. |
| Access Requirements | Certified Academic/Medical Center | Any qualified treatment center | CAR-T requires specialized center with ICU/toxicity management. BiTE administration is less restrictive. |
| Key Cost Drivers | Personalized manufacturing, QC, hospitalization, toxicity management | Drug production at scale, long-term monitoring, supportive care |
Experimental Data & Methodologies
The comparative data above is synthesized from published clinical trials, FDA labels, and health economics studies. Key experimental protocols informing these parameters include:
1. Manufacturing Protocol for BCMA CAR-T (idecabtagene vicleucel):
- Method: Patient-derived T-cells are obtained via leukapheresis and shipped to a central GMP facility. Cells are activated, transduced with a lentiviral vector encoding the anti-BCMA CAR, and expanded ex vivo. Following rigorous quality control (QC) testing for sterility, potency, and CAR expression, the cryopreserved product is shipped back for lymphodepleting chemotherapy (cyclophosphamide/fludarabine) and subsequent infusion.
- Time Metrics: The median "vein-to-vein" time recorded in the KarMMa trial was 4 weeks, with variability due to patient scheduling, manufacturing success, and release testing.
2. Dosing & Administration Protocol for BCMA BiTE (teclistamab):
- Method: In the MajesTEC-1 trial, patients received step-up doses in a hospital setting (0.06 mg/kg, 0.3 mg/kg) to mitigate cytokine release syndrome (CRS), followed by the first full treatment dose (1.5 mg/kg) 2-4 days later. Subsequent weekly subcutaneous injections are administered in an outpatient setting. Pharmacokinetic (PK) and pharmacodynamic (PD) data from this trial established the maintenance dosing schedule.
- Access Metric: The outpatient administration model is derived from the trial's safety management protocol, which allowed discharge after monitoring following the first full dose.
Visualizations
Treatment Pathway Comparison
Key Cost Drivers Analysis
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Reagents for BCMA-Targeted Therapy Research
| Item | Function in Research |
|---|---|
| Recombinant Human BCMA Protein | Used for binding assays (e.g., SPR, ELISA) to measure affinity of novel CAR or BiTE constructs. |
| Anti-BCMA CAR Lentiviral Vector | Tool for in vitro and in vivo transduction of T-cells to study CAR-T functionality and signaling. |
| MM.1S or NCI-H929 Cell Lines | BCMA-positive multiple myeloma cell lines used as target cells in cytotoxicity assays (e.g., Incucyte, LDH). |
| Human Pan-T Cell Isolation Kit | For isolation of primary T-cells from donor PBMCs to serve as effector cells in co-culture experiments. |
| Recombinant Human IL-2 | Cytokine used to promote expansion and persistence of CAR-T cells in ex vivo culture systems. |
| Anti-human CD3ε Antibody (OKT3) | Positive control for T-cell activation; also used in some in vitro BiTE comparison assays. |
| Luminex Cytokine Panel (30+ plex) | To quantify cytokine release (e.g., IFN-γ, IL-6, IL-2) as a pharmacodynamic and safety readout in co-culture assays. |
| NSG Mice | Immunodeficient mouse strain for establishing disseminated myeloma xenograft models to test in vivo efficacy of therapies. |
Conclusion
BCMA-targeted CAR-T cells and BiTEs have revolutionized the treatment paradigm for triple-class exposed multiple myeloma, each offering distinct advantages. CAR-T therapies demonstrate potentially deeper and more durable responses with a single infusion but are constrained by manufacturing complexity, significant toxicity management, and access. BiTEs provide an 'off-the-shelf', more readily administrable option with impressive efficacy, though they require continuous treatment and present unique long-term safety considerations. The choice is not one of superiority but of strategic application based on disease kinetics, patient fitness, and prior therapies. Future research must focus on predictive biomarkers for response, strategies to prevent antigen escape (e.g., dual-targeting), optimizing manufacturing to improve access, and integrating these agents into earlier lines of therapy. Furthermore, elucidating the optimal sequence and developing novel combinations with immunomodulators or checkpoint inhibitors will be crucial to extending survival and moving towards a cure.