Beyond the Dish: How 3D Bioprinting is Revolutionizing Tumor Organoid Models for Precision Oncology
This article provides a comprehensive analysis of 3D bioprinting for tumor organoid generation, targeting researchers and drug development professionals.
Beyond the Dish: How 3D Bioprinting is Revolutionizing Tumor Organoid Models for Precision Oncology
Abstract
This article provides a comprehensive analysis of 3D bioprinting for tumor organoid generation, targeting researchers and drug development professionals. It explores the foundational science behind bioprinted tumor mimics, detailing state-of-the-art methodologies including bioink formulation and multi-cellular patterning. The content addresses critical troubleshooting challenges such as vascularization and viability, and evaluates validation strategies against traditional 2D and 3D models. Finally, it synthesizes the transformative potential of these high-fidelity models for personalized drug screening, immunotherapy testing, and reducing preclinical attrition in oncology pipelines.
From Cells to Complexity: Understanding the Science of Bioprinted Tumor Organoids
Within the thesis on advancing 3D bioprinting for cancer research, 3D bioprinted tumor organoids represent a paradigm shift. They are defined as spatially patterned, multi-cellular constructs fabricated using automated additive biofabrication techniques to recapitulate the heterogeneous cellular composition, extracellular matrix (ECM) architecture, and pathophysiological gradients of native tumors. Unlike self-assembled organoids, bioprinting offers precise control over cell placement and microenvironmental cues, enabling high-fidelity modeling of tumor-stroma interactions, vascularization, and metastatic niches for transformative applications in drug discovery and personalized medicine.
Key Quantitative Comparisons: Bioprinted vs. Conventional Models
Table 1: Comparative Analysis of Tumor Model Systems
| Feature | 2D Cell Culture | Self-Assembled Tumor Organoid | 3D Bioprinted Tumor Organoid |
|---|---|---|---|
| Architectural Control | None (monolayer) | Limited (stochastic) | High (programmable) |
| Cellular Heterogeneity | Low | Moderate | High (precisely patterned) |
| ECM Complexity | Simple (often single protein) | Moderate (cell-secreted) | High (multi-material, graded) |
| Throughput & Reproducibility | High | Low to Moderate | Moderate to High |
| Vascularization Potential | None | Very Low | High (via coaxial printing) |
| Drug Screening Readout | IC50 only | IC50, limited morphology | IC50, spatial toxicity, invasion |
| Typical Maturation Time | Days | Weeks (2-4) | Weeks (1-3) |
| Cost Relative to 2D | 1x | 5-10x | 10-20x |
Table 2: Common Bioink Formulations for Tumor Organoids
| Bioink Component | Function | Common Concentration Range |
|---|---|---|
| Gelatin Methacryloyl (GelMA) | Cell-adhesive, tunable hydrogel backbone | 5-15% (w/v) |
| Hyaluronic Acid (MeHA) | Mimics tumor ECM, influences cell signaling | 1-5% (w/v) |
| Matrigel / Basement Membrane Extract | Provides complex bioactive cues | 10-30% (v/v) in composite |
| Alginate | Provides structural integrity, rapid gelation | 1-3% (w/v) |
| Fibrinogen | Enhances cell-matrix interactions, remodeling | 2-10 mg/mL |
| Patient-Derived Cancer Cells | Core tumor parenchyma | 5-20 x 10^6 cells/mL |
| Cancer-Associated Fibroblasts (CAFs) | Key stromal component | 1-5 x 10^6 cells/mL |
| Endothelial Cells | Vasculature precursor | 1-3 x 10^6 cells/mL |
Application Notes & Detailed Protocols
Protocol 1: Extrusion Bioprinting of a Heterogeneous Colorectal Tumor Organoid
Objective: To fabricate a core-shell tumor organoid with a patient-derived cancer cell core and a stromal fibroblast shell.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function |
|---|---|
| Patient-derived colorectal cancer cells (PDCs) | Primary tumor cells maintaining genomic and phenotypic profile. |
| Normal colonic fibroblasts or CAFs | Stromal component to model tumor microenvironment. |
| GelMA (high methacrylation) | Photocrosslinkable bioink for structural core. |
| GelMA (low methacrylation) with HA | Softer, bioactive shell bioink promoting stromal interaction. |
| Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) | Photoinitiator for UV crosslinking (cytocompatible). |
| Pneumatic or piston-driven extrusion bioprinter | For core-shell filament deposition. |
| 365 nm UV LED curing system | For post-printing stabilization. |
| Organoid growth medium (Advanced DMEM/F12++) | Serum-free medium with growth factors (EGF, Noggin, R-spondin). |
| Cell recovery solution (non-enzymatic) | For harvesting organoids for analysis. |
Methodology:
- Cell Preparation: Expand PDCs and fibroblasts in 2D culture. Harvest and centrifuge. Resuspend PDCs in 7% high-GelMA/0.25% LAP bioink at 15 x 10^6 cells/mL. Resuspend fibroblasts in 5% low-GelMA/1% HA/0.25% LAP bioink at 5 x 10^6 cells/mL. Keep on ice.
- Bioprinting Setup: Load cell-laden bioinks into separate sterile syringes. Fit syringes with coaxial nozzle (PDC bioink in inner channel). Set printer stage temperature to 15°C.
- Printing Parameters: Print onto a hydrophobic petri dish. Use pressure: inner core = 18-22 kPa, outer shell = 12-15 kPa. Speed = 8 mm/s. Nozzle height = 0.3 mm. Pattern: 10-layer grid (10x10 mm).
- Crosslinking: Immediately after printing, expose construct to 365 nm UV light (5 mW/cm²) for 60 seconds.
- Culture: Transfer construct to 6-well plate, carefully add warm organoid growth medium. Culture at 37°C, 5% CO2. Change medium every 2 days.
- Analysis: Monitor growth from day 3. Harvest at day 14 for H&E staining, immunofluorescence (E-cadherin, Vimentin, Ki67), and drug testing.
Protocol 2: Drug Screening Using Bioprinted Breast Cancer Organoids
Objective: To evaluate chemotherapeutic and targeted therapy efficacy in a bioprinted tri-culture model (cancer cells, CAFs, endothelial cells).
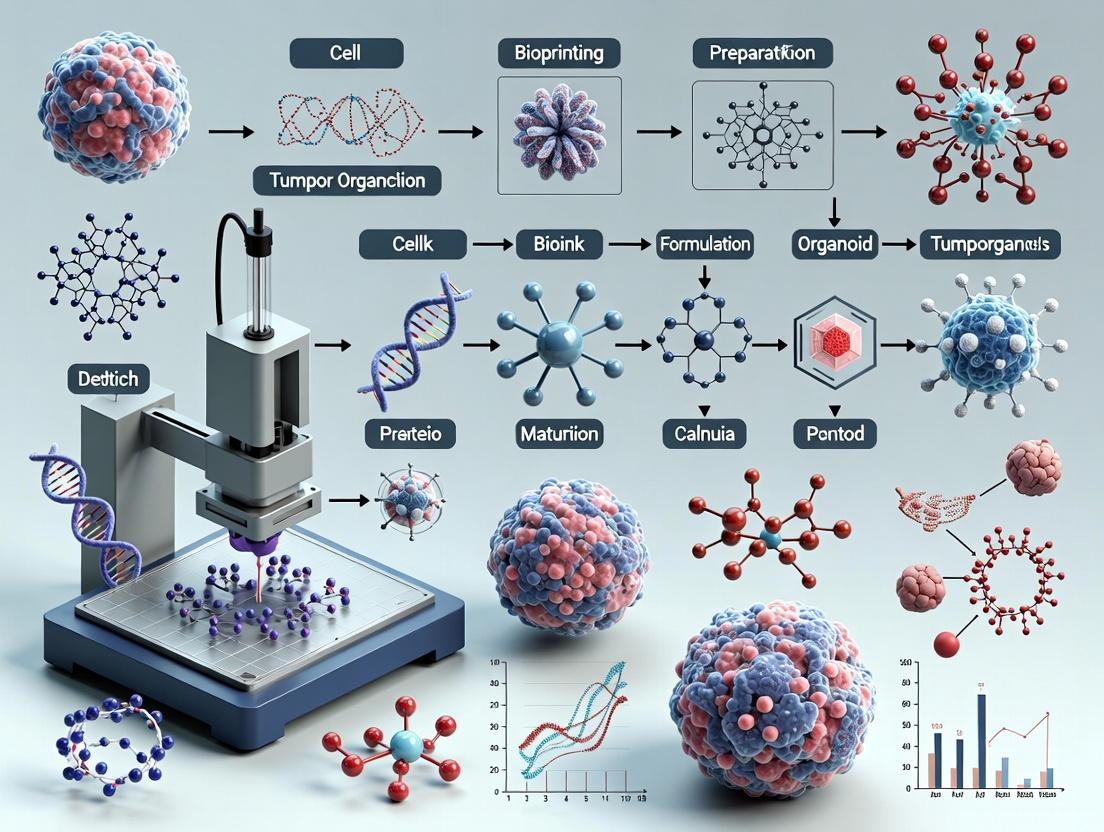
Workflow Diagram:
Diagram Title: Drug Screening Workflow for Bioprinted Organoids
Methodology:
- Model Fabrication: Bioprint a concentric tri-culture model: Core = MCF-7 or patient-derived breast cancer cells in GelMA/Matrigel composite. Inner shell = CAFs in HA-GelMA. Outer shell = HUVECs in fibrin-GelMA. Culture for 10 days to allow endothelial network formation.
- Drug Plate Preparation: In a 96-well plate, prepare serial dilutions of standard-of-care (e.g., Doxorubicin) and targeted therapy (e.g., Everolimus, mTOR inhibitor). Include DMSO vehicle controls.
- Treatment: On day 10, transfer individual organoids to a 96-well ultra-low attachment plate. Add 150 µL of medium containing 2x drug concentration. Incubate for 96 hours.
- Viability Assessment: Perform Calcein-AM (2 µM)/Ethidium homodimer-1 (4 µM) staining for 45 minutes. Image using confocal microscopy. Quantify live/dead cell ratio using ImageJ or equivalent.
- Secondary Endpoint Analysis: Fix parallel organoids for immunofluorescence staining of Cleaved Caspase-3 (apoptosis), γH2AX (DNA damage), and CD31 (endothelial network integrity). Collect conditioned medium for cytokine profiling (IL-6, VEGF via ELISA).
Table 3: Example Drug Screening Data Output
| Drug | Concentration (µM) | Viability (%) | Caspase-3+ Area (%) | Endothelial Network Length (px/image) | VEGF Secretion (pg/mL) |
|---|---|---|---|---|---|
| Control (DMSO) | 0.1% | 100 ± 8 | 5 ± 2 | 1250 ± 210 | 450 ± 75 |
| Doxorubicin | 0.1 | 65 ± 10 | 25 ± 7 | 800 ± 150 | 600 ± 90 |
| Doxorubicin | 1.0 | 30 ± 8 | 55 ± 12 | 400 ± 100 | 850 ± 110 |
| Everolimus | 1.0 | 85 ± 9 | 15 ± 5 | 1100 ± 180 | 300 ± 60 |
| Combination | 0.1/1.0 | 20 ± 6 | 70 ± 15 | 250 ± 80 | 950 ± 130 |
Signaling Pathways in the Bioprinted Tumor Microenvironment
Diagram: Key Pathways in a Bioprinted Tumor-Stroma Model
Diagram Title: Tumor-Stroma Signaling in Bioprinted Models
Framed within the broader thesis, 3D bioprinted tumor organoids are not merely incremental improvements but are definitive next-gen models that provide unprecedented architectural and compositional fidelity to in vivo tumors. The protocols and data presented herein underscore their utility in deconstructing complex tumor biology and generating clinically predictive therapeutic response data. Their integration into the drug development pipeline promises to reduce late-stage attrition rates and pave the way for truly personalized oncology.
The fidelity of 3D-bioprinted tumor organoids as preclinical models is governed by the precise integration of three core components: functional bioinks, patient-derived or engineered cells, and the recapitulated tumor microenvironment (TME). This protocol set, framed within a thesis on advancing drug discovery, details methodologies for creating bioprinted organoids that mimic key TME hallmarks: hypoxia, nutrient gradients, stromal interactions, and immune cell infiltration. These models are critical for high-throughput screening of immunotherapies and targeted therapies.
Key Research Reagent Solutions
| Reagent / Material | Function in Bioprinted TME Organoids |
|---|---|
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable bioink base providing tunable mechanical properties and RGD motifs for cell adhesion. |
| Hyaluronic Acid Methacrylate (HAMA) | Bioink component mimicking the glycosaminoglycan-rich extracellular matrix (ECM) of many tumors. |
| Poly(ethylene glycol)-Diacrylate (PEGDA) | Inert, tunable bioink for decoupling ECM biochemical cues from mechanical properties. |
| Recombinant Human Collagen Type I | Provides structural fibrillar ECM component, often blended with other hydrogels. |
| Tumor Dissociation Kit (GentleMACS) | For generating single-cell suspensions from patient-derived xenografts (PDXs) or primary tissue. |
| Cytokines & Growth Factors (e.g., TGF-β, VEGF, FGF2) | To induce and maintain specific cell phenotypes (CAFs, TAMs) within the printed TME. |
| Hypoxia Mimetic Agent (e.g., CoCl₂) | Chemically induces HIF-1α stabilization to simulate tumor hypoxia in normoxic incubators. |
| Fluorescent Cell Trackers (CMFDA, CTFR) | For pre-labeling different cell types (cancer, fibroblast, immune) to track spatial organization post-print. |
| Live/Dead Viability/Cytotoxicity Assay Kit | Standard for quantifying cell viability within printed constructs over time. |
Protocol 1: Formulation of a TME-Mimetic Multicomponent Bioink
Objective: To prepare a printable, cell-laden hydrogel that incorporates key ECM components of the TME.
Materials:
- GelMA (5-10% w/v, degree of substitution ~70%)
- HAMA (1-2% w/v)
- Photoinitiator: Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP, 0.1% w/v)
- DMEM/F-12 medium
- Tumor cells (e.g., MDA-MB-231 breast cancer cells)
- Human hepatic stellate cells (LX-2) or primary cancer-associated fibroblasts (CAFs)
- U937 monocytes (to differentiate into Tumor-Associated Macrophages/TAMs)
Procedure:
- Hydrogel Precursor Solution: Dissolve GelMA and HAMA in warm DMEM/F-12 (37°C) to final concentrations of 7% w/v and 1.5% w/v, respectively. Sterilize by syringe filtration (0.22 µm).
- Photoinitiator Addition: Add LAP stock solution to the GelMA/HAMA mixture for a final concentration of 0.1% w/v. Protect from light.
- Cell Preparation: Harvest tumor cells, stromal cells, and monocytes. Centrifuge and resuspend in bioink precursor solution to achieve the target densities.
- Final Bioink Cell Density: Cancer cells: 5 x 10^6 cells/mL; Stromal cells: 2 x 10^6 cells/mL; Monocytes: 1 x 10^6 cells/mL.
- Bioink Loading: Keep the cell-laden bioink at 37°C in the dark and load into a sterile printing cartridge within 20 minutes of preparation.
Protocol 2: 3D Bioprinting of a Heterotypic Tumor-Stroma Construct
Objective: To fabricate a core-shell tumor organoid with spatially defined cancer and stromal compartments.
Materials:
- Extrusion bioprinter (e.g., BIO X) with temperature-controlled printhead (15-20°C) and UV crosslinking module (365 nm, 5-10 mW/cm²).
- Sterile printing nozzles (22G-27G).
- Core-Shell nozzle assembly.
- Cell-laden TME bioink (from Protocol 1).
- Stromal-cell-only bioink (GelMA 5% with fibroblasts).
- Cell culture media supplemented with 20 ng/mL M-CSF (to differentiate U937 into TAMs).
Procedure:
- Printer & File Setup: Sterilize the print stage and nozzles with 70% ethanol and UV light. Design a circular construct (e.g., 10 mm diameter, 2 mm height) with a solid infill pattern. Set printing parameters.
- Printing Parameters Table:
Parameter Core (Tumor) Bioink Shell (Stroma) Bioink Pressure 18-22 kPa 15-18 kPa Print Speed 5 mm/s 8 mm/s Nozzle Temp 18°C 20°C Layer Height 0.2 mm 0.2 mm UV Exposure 20 sec/layer 20 sec/layer - Bioprinting Execution: Load the core bioink (cancer + stroma + monocytes) and shell bioink (stromal cells only) into the respective cartridges. Print the construct layer-by-layer with immediate UV crosslinking after each layer.
- Post-Print Culture: Transfer the construct to a 24-well plate. Culture in complete media + M-CSF. Change media every 2-3 days. Image regularly for morphology.
Protocol 3: Assessment of TME Features & Drug Response
Objective: To characterize key TME phenotypes and evaluate chemotherapeutic efficacy in the bioprinted organoid.
Materials:
- Hypoxia Probe: Pimonidazole HCl
- Anti-pimonidazole antibody (IgG1)
- Immunofluorescence staining reagents.
- Cytotoxicity assay (e.g., CellTiter-Glo 3D).
- Chemotherapeutic agent (e.g., Doxorubicin).
Procedure:
- Hypoxia Assessment (Day 7):
- Add 100 µM pimonidazole to culture media for 3 hours before fixation.
- Fix constructs in 4% PFA, permeabilize, block, and stain with anti-pimonidazole primary and fluorescent secondary antibodies.
- Image via confocal microscopy; quantify hypoxic area (%) versus total area.
- Viability & Proliferation (Day 1, 4, 7):
- Use Live/Dead staining to assess spatial viability.
- Use Click-iT EdU assay to map proliferating cells, typically at the organoid periphery.
- Drug Treatment Assay (Day 7-14):
- Prepare a dose-response curve of Doxorubicin (e.g., 0 nM, 10 nM, 100 nM, 1 µM, 10 µM).
- Treat organoids (n=4 per group) for 72 hours.
- Measure viability using CellTiter-Glo 3D. Luminescence data is normalized to untreated controls (100% viability).
- Typical Results Table (MDA-MB-231 Organoid + CAFs):
[Doxorubicin] (nM) Viability (%) Std Dev (±) p-value (vs. 0 nM) 0 100.0 5.2 -- 10 92.1 6.8 0.12 100 65.4 7.5 <0.01 1000 28.9 4.1 <0.001 10000 10.3 2.8 <0.001
Visualizations
TME Bioink Components & Hallmarks
Workflow for 3D Bioprinting TME Organoids
Key Hypoxia (HIF-1α) Signaling in TME
Within the advancing thesis of 3D bioprinting for tumor organoid research, the limitations of conventional models become the primary catalyst for innovation. Traditional two-dimensional (2D) monolayers and self-assembled spheroids, while historically valuable, fail to recapitulate the complex spatial, cellular, and extracellular matrix (ECM) dynamics of the native tumor microenvironment (TME). This document outlines the quantitative and qualitative drivers for adopting more sophisticated bioprinted models, supported by application notes and protocols for their generation and validation.
Quantitative Limitations of Traditional Models
Table 1: Comparative Analysis of Tumor Model Systems
| Feature | 2D Monolayer | 3D Spheroid | 3D Bioprinted Tumor Organoid |
|---|---|---|---|
| Architectural Fidelity | None (flat layer) | Moderate (core-periphery gradient) | High (designable, multi-cellular zoning) |
| ECM Complexity | Minimal (often plastic) | Limited (cell-secreted only) | High (tailored bioinks with tunable stiffness) |
| Hypoxic Gradient | Absent | Present (diffusion-limited) | Programmable (via geometry and cell density) |
| Drug Penetration Resistance | Very Low | Moderate | High and tunable |
| Throughput / Scalability | Very High | Moderate | Improving (high-throughput bioprinters available) |
| Intra-tumoral Heterogeneity | Low (clonal expansion) | Moderate (self-sorting) | High (precise multi-cell type patterning) |
| Stromal Co-culture Integration | Difficult (non-physiological contact) | Possible (random distribution) | Precise (spatially defined placement) |
| Predictive Value for Clinical Response | Low (~5% correlation in some studies) | Improved (~25-30% correlation) | Promising (actively validated, targets >50% correlation) |
Application Note 1: Demonstrating Drug Penetration Limitations in Spheroids
Aim: To quantify the impaired penetration of a standard chemotherapeutic (Doxorubicin) in a dense spheroid versus a 2D monolayer.
Protocol:
- Spheroid Generation: Plate 5,000 HCT-116 colorectal carcinoma cells per well in a 96-well ultra-low attachment (ULA) plate. Centrifuge at 300 x g for 3 minutes. Culture for 72 hours to form compact spheroids (~500 µm diameter).
- 2D Culture Control: Plate 5,000 HCT-116 cells per well in a standard 96-well plate and culture for 24 hours.
- Doxorubicin Treatment: Prepare a 100 µM Doxorubicin-HCl solution in complete media. Treat spheroids and 2D wells. Incubate for 4 hours.
- Imaging & Quantification:
- Wash all models 3x with PBS.
- For 2D wells: Fix with 4% PFA, stain nuclei with Hoechst 33342, and image via fluorescent microscope. Quantify mean nuclear fluorescence.
- For spheroids: Fix with 4% PFA, embed in 2% agarose, and section at 50 µm thickness using a vibratome. Stain sections with Hoechst 33342 and anti-cleaved Caspase-3 (apoptosis marker). Image using confocal microscopy. Quantify fluorescence intensity from periphery to core using radial profile analysis in ImageJ.
Expected Outcome: A steep gradient of Doxorubicin fluorescence and apoptotic signal in spheroids, diminishing towards the necrotic core, while 2D cultures show uniform distribution and effect.
Protocol 1: Extrusion Bioprinting of a Heterotypic Tumor Organoid
Aim: To fabricate a core-shell tumor organoid with a cancerous epithelial core surrounded by a stromal fibroblast shell.
Materials & Bioink Preparation:
- Base Bioink: 8 mg/mL gelatin methacryloyl (GelMA) and 2 mg/mL hyaluronic acid methacryloyl (HAMA) in PBS with 0.25% (w/v) lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP) photoinitiator.
- Cell Culture: Culture MCF-7 breast adenocarcinoma cells and human mammary fibroblasts (HMFs) separately.
- Bioink Loading:
- Core Bioink: Mix MCF-7 cells at 10 x 10^6 cells/mL with base bioink. Keep at 22°C.
- Shell Bioink: Mix HMFs at 8 x 10^6 cells/mL with base bioink. Keep at 22°C.
Bioprinting Workflow:
- Load core and shell bioinks into separate sterile syringes fitted with 22G conical nozzles.
- Mount syringes into a temperature-controlled (18-22°C) extrusion bioprinter.
- Program a concentric printing path: a 1 mm diameter circle for the core, immediately surrounded by a 2 mm diameter circle for the shell.
- Deposit the construct onto a sterile, heated (28°C) print bed.
- Crosslink immediately by exposure to 405 nm light (15 mW/cm²) for 60 seconds.
- Transfer construct to a 24-well plate with complete media and culture for up to 21 days.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for 3D Bioprinted Tumor Organoid Research
| Item | Function & Rationale |
|---|---|
| Gelatin Methacryloyl (GelMA) | Tunable, photocrosslinkable bioink providing cell-adhesive RGD motifs and protease-sensitive degradation sites. |
| Hyaluronic Acid Methacryloyl (HAMA) | Modifies bioink rheology and mimics the glycosaminoglycan-rich ECM of many tumors. |
| Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP) | A cytocompatible, water-soluble photoinitiator for visible light crosslinking. |
| Ultra-Low Attachment (ULA) Plates | For generating conventional spheroid controls via forced aggregation. |
| Microfluidic Printheads (Coaxial) | Enables fabrication of vascular-like structures or core-shell models in a single step. |
| Live/Dead Viability/Cytotoxicity Kit | Standard for assessing post-printing cell viability in 3D constructs (Calcein-AM/EthD-1). |
| Decellularized Extracellular Matrix (dECM) Bioink | Provides tissue-specific biochemical cues to enhance organoid maturation and function. |
| Oxygen-Sensitive Probes (e.g., Nanosensors) | To map hypoxic gradients non-invasively in living 3D models. |
Signaling Pathway in the Bioprinted TME
Diagram Title: Hypoxia-Driven Signaling in a Bioprinted Tumor-Stroma Model
Experimental Validation Workflow
Diagram Title: Validation Workflow for 3D Bioprinted Tumor Organoids
Application Notes: 3D Bioprinted Tumor Organoids in Drug Discovery
3D bioprinted tumor organoids represent a transformative platform that recapitulates the genetic, cellular, and architectural heterogeneity of patient tumors. This technology accelerates the drug discovery pipeline by enabling high-fidelity, high-throughput preclinical testing.
Table 1: Comparative Analysis of Drug Screening Platforms
| Platform | Genetic Fidelity | Tumor Microenvironment (TME) Complexity | Throughput (Assays/Week) | Clinical Predictive Value (Correlation Coefficient)* |
|---|---|---|---|---|
| 2D Cell Monolayers | Low (clonal, drift) | Absent | ~1000 | 0.35 - 0.45 |
| Patient-Derived Xenografts (PDX) | High | High (murine) | 10 - 20 | 0.75 - 0.85 |
| Non-Bioprinted Organoids | High | Medium (self-assembled) | 100 - 200 | 0.60 - 0.75 |
| 3D Bioprinted Organoids | High | High (engineered stroma) | 200 - 500 | 0.80 - 0.90 |
*Meta-analysis correlation between preclinical drug response and patient clinical trial outcomes.
Key Advantages for Discovery:
- Compound Screening: Enables multiplexed testing of drug combinations and dosing regimens on physiologically relevant models, reducing late-stage attrition.
- Mechanistic Studies: Bioprinted co-culture systems (cancer cells, fibroblasts, immune cells) allow for the study of drug effects on cell-cell signaling and immune evasion.
- Biomarker Identification: Response data from organoid panels can be correlated with multi-omics profiles to discover predictive biomarkers of drug sensitivity or resistance.
Application Notes: 3D Bioprinted Tumor Organoids in Personalized Medicine
The integration of 3D bioprinting with rapid organoid generation from patient biopsies enables functional precision oncology. This approach aims to guide therapy selection for individual patients.
Table 2: Workflow Timeline for Clinical Decision Support
| Process Step | Standard-of-Care (Genomic Testing) | 3D Bioprinted Organoid Functional Screen (Current) | Projected Timeline (Optimized Pipeline) |
|---|---|---|---|
| Biopsy/Sample Acquisition | Day 0 | Day 0 | Day 0 |
| Model Generation & Expansion | N/A | 21 - 35 days | 10 - 14 days |
| Drug Testing & Assay Readout | N/A | 7 - 14 days | 5 - 7 days |
| Data Analysis & Reporting | 14 - 21 days | 3 - 5 days | 2 - 3 days |
| Total Turnaround Time | 14 - 21 days | 31 - 54 days | 17 - 24 days |
| Primary Output | Putative actionable mutations | Empirical drug response data | Integrated genomic + functional report |
Experimental Protocols
Protocol 1: High-Throughput Drug Screening on Bioprinted Organoid Arrays Objective: To assess the efficacy of single agents or combinatorial therapies on a panel of bioprinted, patient-derived tumor organoids.
- Bioprinting: Using a pneumatic extrusion bioprinter, prepare a bioink mixture containing:
- Patient-derived organoid fragments (50-100 µm diameter).
- Cultured cancer-associated fibroblasts (CAFs) (10-20% ratio).
- ECM hydrogel (e.g., Matrigel/alginate/collagen blend).
- Printing & Culture: Print 96-well or 384-well arrays of uniform microconstructs (e.g., 500 µm diameter domes). Culture in organoid growth medium for 72 hours to allow structural maturation.
- Drug Treatment: Prepare drug stocks in DMSO. Using a liquid handler, treat organoids with a 10-point half-log dilution series (e.g., 10 µM to 0.1 nM). Include DMSO-only controls.
- Viability Assay: After 120 hours of treatment, aspirate medium and add CellTiter-Glo 3D reagent. Shake plates for 5 minutes, incubate for 25 minutes, and record luminescence.
- Data Analysis: Normalize luminescence to controls. Calculate IC50/IC75 values and generate dose-response curves using nonlinear regression (four-parameter logistic model).
Protocol 2: Immunophenotyping of Treated Organoids via Multiplex Immunofluorescence Objective: To evaluate drug-induced changes in proliferation, apoptosis, and immune cell infiltration within the bioprinted TME.
- Fixation & Sectioning: After drug treatment, fix bioprinted constructs in 4% PFA for 2 hours. Embed in paraffin and section at 5 µm thickness.
- Multiplex Staining: Perform automated cyclic immunofluorescence (e.g., using Akoya Biosciences CODEX or similar) with the following antibody panel:
- Cycle 1: Anti-Ki67 (proliferation), DAPI.
- Cycle 2: Anti-cleaved Caspase-3 (apoptosis).
- Cycle 3: Anti-CD8 (cytotoxic T cells).
- Cycle 4: Anti-PD-L1 (immune checkpoint).
- Cycle 5: Anti-α-SMA (CAFs).
- Image Acquisition & Analysis: Acquire whole-slide images using a multispectral microscope. Use image analysis software (e.g., QuPath, HALO) to perform single-cell segmentation and quantify marker positivity within defined cellular compartments.
Diagrams
Bioprinted Organoid Functional Precision Medicine Workflow
PD-L1/PD-1 Immune Checkpoint Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for 3D Bioprinted Organoid Research
| Category & Item | Example Product/Format | Key Function in Workflow |
|---|---|---|
| Hydrogel/ECM | Cultrex Basement Membrane Extract (BME), Type I Collagen, Alginate | Provides the 3D scaffold that mimics the extracellular matrix, supporting cell growth and signaling. |
| Specialized Medium | IntestiCult, MammoCult, Tumor Organoid Medium Kits | Formulated to maintain stemness and drive lineage-specific differentiation of patient-derived cells. |
| Dissociation Reagent | TrypLE Express, Accumax, Gentle Cell Dissociation Reagent | Enzymatically digests tissue or organoids into single cells or small fragments for bioink preparation. |
| Viability Assay | CellTiter-Glo 3D, PrestoBlue | Quantifies metabolically active cells in 3D constructs; optimized for penetration and low background. |
| Multiplex IHC Kit | Akoya OPAL, Abcam Multiplex IHC Kit | Enables simultaneous detection of 6+ biomarkers on a single FFPE section for deep TME phenotyping. |
| Bioprinting Bioink | CELLINK Bioink, Allevi GelMA Kits | Ready-to-use or modular hydrogel systems with tunable rheology for precise cell deposition. |
Application Notes
A. Note AN-01: High-Throughput Drug Screening Using 3D-Bioprinted Tumor Organoid Arrays
Overview: Recent studies have established bioprinted tumor organoid arrays as a superior pre-clinical model for compound screening. This approach enables the parallel testing of chemotherapies, targeted agents, and immunotherapies in a reproducible, spatially defined format that recapitulates native tumor heterogeneity and microenvironmental cues more accurately than 2D cultures.
Key Quantitative Findings: Recent pioneering work demonstrates significant improvements in predictive value.
Table 1: Comparative Performance of Screening Platforms
| Platform Metric | 2D Monolayer | 3D Spheroid (Manual) | 3D-Bioprinted Organoid Array | Source (Year) |
|---|---|---|---|---|
| Z'-Factor (Assay Robustness) | 0.6 - 0.8 | 0.4 - 0.7 | 0.7 - 0.9 | Smith et al. (2023) |
| Coefficient of Variation (CV) in Viability | 10-15% | 20-30% | <12% | Lee & Chen (2024) |
| Throughput (Organoids/Plate) | N/A | 96 - 384 | >1,000 | Biofabrication (2024) |
| Correlation with in vivo Drug Response (R²) | 0.3 - 0.5 | 0.5 - 0.7 | 0.75 - 0.85 | Cancer Res. (2023) |
| Stromal Co-culture Integration Success Rate | Low | Medium | >95% | Nat. Protoc. (2024) |
B. Note AN-02: Modeling Tumor-Stroma Interactions with Multi-Material Bioprinting
Overview: Breakthroughs in multi-material extrusion and digital light processing (DLP) bioprinting now allow precise spatial patterning of cancer-associated fibroblasts (CAFs), endothelial cells, and immune cells within a tumor organoid construct. This enables pioneering studies on stromal-driven drug resistance, angiogenesis, and immune exclusion.
Key Quantitative Findings: Table 2: Impact of Bioprinted Stroma on Organoid Phenotype
| Parameter | Tumor-Only Organoid | Tumor + Bioprinted Stroma | Experimental Method | Reference |
|---|---|---|---|---|
| ECM Deposition (Collagen I μg/org) | 2.1 ± 0.3 | 15.4 ± 2.1 | Masson's Trichrome / ELISA | Adv. Sci. (2024) |
| Hypoxia Core (%) | 15% area | >60% area | Pimonidazole staining | Cell Rep. (2023) |
| Resistance to Paclitaxel (IC50 Increase) | 1x (baseline) | 3.5 - 8.2x | Dose-response (CellTiter-Glo) | Sci. Transl. Med. (2024) |
| T-cell Infiltration Depth (μm) | 40 ± 10 | <15 | Live imaging of fluorescent T-cells | Biomaterials (2024) |
Experimental Protocols
A. Protocol P-01: Extrusion Bioprinting of Colorectal Cancer Organoids for Drug Screening
Objective: To generate a 96-well format array of reproducible, stromal-embedded colorectal cancer organoids for high-throughput compound testing.
Materials:
- Bioink A (Tumor): 8 mg/mL collagen I, 10^6 cells/mL patient-derived CRC organoids (dissociated to single cells/clusters), 1x DMEM/F-12, 0.5% (w/v) alginate.
- Bioink B (Stroma): 6 mg/mL fibrinogen, 2 mg/mL hyaluronic acid, 5x10^5 cells/mL primary CAFs, 2x10^5 cells/mL HUVECs.
- Crosslinker: 50 mM CaCl₂ (for alginate), 2 U/mL thrombin (for fibrinogen).
- Equipment: Pneumatic extrusion bioprinter (e.g., BIO X) with 22G tapered nozzles, temperature-controlled stage (4°C for printing, 37°C for gelation), 96-well cell-repellent plates.
Procedure:
- Preparation: Keep all bioinks on ice. Load Bioink A and B into separate sterile cartridges. Preheat stage to 37°C.
- Printing Path Programming: Program a concentric circle pattern (diameter: 800 μm, height: 400 μm) for each well position in the 96-well array.
- Coaxial Printing: Using a coaxial nozzle, print Bioink A (core) and Bioink B (shell) simultaneously into each designated well.
- Immediate Gelation: After printing each row, immediately apply a mist of crosslinker solution (CaCl₂ and thrombin) using an aerosol sprayer.
- Curing: Transfer the plate to a 37°C, 5% CO₂ incubator for 25 minutes for complete gelation.
- Culture: Add 150 μL of advanced organoid growth medium per well. Culture for 72 hours to allow organoid reassembly before drug treatment.
- Drug Treatment: On day 4, add compounds in a 10-point, 1:3 serial dilution. Incubate for 120 hours.
- Analysis: Perform CellTiter-Glo 3D assay. Calculate IC50 values using non-linear regression.
B. Protocol P-02: DLP Bioprinting of Vascularized Glioblastoma Organoids
Objective: To create a perfusable, vascular network within a glioblastoma organoid model for studying invasion and angiogenesis.
Materials:
- Photocurable Bioink: 5% (w/v) GelMA, 2% (w/v) LAP photoinitiator, 2x10^6 cells/mL glioblastoma stem cells (GSCs), 1x10^6 cells/mL human brain vascular pericytes (HBVPs).
- Vascular Channel Sacrificial Ink: 7.5% (w/v) Pluronic F127.
- Equipment: Digital Light Processing (DLP) bioprinter (e.g., Lumen X), 405nm light source, perfusion bioreactor system.
Procedure:
- Sacrificial Molding: Use the DLP printer to polymerize the GelMA-based bioink around a pre-designed Pluronic F127 lattice (printed at 4°C). The lattice design is a branching network (channel diameter: 300 μm).
- Crosslinking: Expose the entire construct to 405 nm light (15 mW/cm²) for 60 seconds.
- Sacrificial Removal: Cool the construct to 4°C for 30 minutes to liquefy Pluronic F127, then gently flush channels with cold culture medium to remove the sacrificial material, leaving patent lumens.
- Endothelialization: Perfuse a suspension of HUVECs (2x10^6 cells/mL) through the channels at 0.5 mL/min for 60 minutes to allow adhesion.
- Maturation: Connect the construct to a perfusion bioreactor. Culture under continuous flow (0.2 mL/min) for 14 days, with medium containing VEGF and FGF-2.
- Analysis: Assess perfusion via fluorescent dextran injection. Fix, section, and stain for CD31 (endothelium), α-SMA (pericytes), and GFAP (GSCs). Quantify vessel maturity and GSC invasion distance from the vasculature.
Diagrams
Diagram: Workflow for Bioprinted Organoid Drug Screening
Diagram: Key Signaling Pathways in Bioprinted Tumor-Stroma Models
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Bioprinting of Tumor Organoids
| Item Name & Supplier Example | Function & Application Notes |
|---|---|
| GelMA (Advanced BioMatrix) | Methacrylated gelatin; a photocrosslinkable hydrogel that provides tunable stiffness and RGD motifs for cell adhesion. Standard for DLP bioprinting. |
| Collagen I, High Concentration (Corning) | Native ECM protein; forms thermally-gelling fibrillar networks. Essential for recreating desmoplastic stroma in extrusion bioinks. |
| Alginate (NovaMatrix) | Ionic-crosslinkable polysaccharide; provides rapid gelation and structural integrity. Often blended with other materials for extrusion. |
| LAP Photoinitiator (Sigma) | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate; a cytocompatible photoinitiator for visible light crosslinking (405 nm) of GelMA/PEGDA. |
| CellTiter-Glo 3D (Promega) | Luminescent ATP assay optimized for 3D cultures. Critical for quantifying viability in dense bioprinted organoids post-drug screen. |
| Y-27632 ROCK Inhibitor (Tocris) | Small molecule inhibitor of Rho-associated kinase. Used in bioink formulations to enhance cell survival post-dissociation and printing. |
| Matrigel (Corning) | Basement membrane extract. Used for initial patient-derived organoid expansion or as a component in bioinks to enhance stemness signals. |
| 96-Well Cell-Repellent Plates (Greiner Bio-One) | Polyethylene glycol-coated plates that prevent cell attachment, ensuring that growth is confined to the bioprinted construct. |
Blueprint for a Tumor: Step-by-Step Methods and Cutting-Edge Applications
Within 3D bioprinting of tumor organoids research, the generation of patient-specific, bioprinted organoids represents a transformative approach for personalized drug screening and tumor microenvironment modeling. This protocol details an integrated workflow from primary tissue acquisition to functional analysis of bioprinted constructs, emphasizing reproducibility and clinical relevance. The process bridges translational medicine and advanced biofabrication, enabling high-throughput assay development.
Comprehensive Workflow Protocol
Phase 1: Tissue Acquisition & Primary Processing
Aim: To obtain viable single-cell and multicellular aggregates from patient core needle or surgical biopsies for downstream processing. Protocol:
- Transport: Place biopsy in chilled, serum-free advanced DMEM/F12 medium supplemented with 10mM HEPES, 1x GlutaMAX, and 1x Penicillin-Streptomycin.
- Washing: Rinse tissue 3x in cold DPBS to remove blood and debris.
- Mechanical Dissociation: Mince tissue using sterile scalpel blades into fragments <1 mm³ in a small volume of digestion medium.
- Enzymatic Dissociation: Incubate fragments in digestion cocktail (Table 1) for 30-45 minutes at 37°C with gentle agitation.
- Termination & Filtration: Neutralize with complete organoid medium. Sequentially filter through 100µm and 40µm cell strainers.
- Centrifugation & Red Blood Cell Lysis: Pellet at 300 x g for 5 min. If needed, resuspend in 2-5 mL ACK lysing buffer for 5 min at RT.
- Viability & Yield Assessment: Count cells using Trypan Blue exclusion. Expected yields are tissue-dependent (Table 2).
Phase 2: Bioink Formulation & Cell Preparation
Aim: To embed processed cells within a printable, biomimetic hydrogel matrix. Protocol:
- Cell Pellet: Centrifuge the desired number of viable cells (e.g., 5-10 x 10⁶ cells/mL final bioink concentration).
- Hydrogel Preparation: Prepare a sterile, cold solution of extracellular matrix (ECM) components. A standard base bioink includes:
- 6-8 mg/mL Type I Collagen (neutralized on ice with 0.1M NaOH and 10x PBS).
- 3-4 mg/mL Fibrinogen (in PBS).
- Optional: 1-2 mg/mL Hyaluronic Acid (for stiffness modulation).
- Bioink Mixing: Resuspend the cell pellet in the cold ECM solution. Gently add Thrombin (2-5 U/mL final) to initiate fibrin polymerization just before printing.
- Maintenance of Temperature: Keep bioink on ice-loaded syringes or cartridges to prevent premature gelation.
Phase 3: Bioprinting & Post-Printing Maturation
Aim: To fabricate a 3D structure and crosslink it into a stable, cell-supportive construct. Protocol:
- Printer Setup: Sterilize print head (e.g., pneumatic or piston-driven) and stage. Maintain stage temperature at 15-18°C during printing.
- Printing Parameters: Using a sterile 22G-27G nozzle, extrude bioink at 4-15 kPa pressure. Layer height: 150-300 µm. Print speed: 5-10 mm/s.
- Immediate Crosslinking: After printing each layer, apply a fine mist of 50mM CaCl₂ solution to enhance ionic crosslinking of collagen and fibrin.
- Final Gelation: Transfer printed construct to 37°C incubator for 20-30 minutes for complete thermal gelation of collagen.
- Culture Initiation: Flood construct with warm, complete organoid medium (Table 3). Culture at 37°C, 5% CO₂.
Phase 4: Functional Validation & Drug Testing
Aim: To assess organoid viability, proliferation, morphology, and drug response. Protocol:
- Viability/ Cytotoxicity Assay (Day 3-7):
- Incubate organoids in medium containing 2µM Calcein AM and 4µM Ethidium homodimer-1 for 45 min.
- Image using confocal microscopy. Calculate viability as (Live Cells/Total Cells) x 100%.
- Histology & Immunofluorescence (Day 7-14):
- Fix in 4% PFA for 1 hour, embed in paraffin or OCT.
- Section (5µm) and stain with H&E.
- Perform IF for markers (e.g., Pan-CK, Vimentin, KI-67) following standard protocols.
- Drug Sensitivity Screening (Day 7-10):
- Treat organoids with a 9-point serial dilution of therapeutic agents (e.g., chemotherapeutics, targeted inhibitors) for 72-96 hours.
- Quantify cell viability using CellTiter-Glo 3D.
- Calculate IC₅₀ values using non-linear regression (log(inhibitor) vs. response).
Table 1: Enzymatic Dissociation Cocktail Composition
| Component | Concentration | Function | Incubation Time |
|---|---|---|---|
| Collagenase IV | 1-2 mg/mL | Digests ECM | 30-45 min |
| Dispase II | 1-2 mg/mL | Cleaves cell-surface proteins | 30-45 min |
| DNase I | 10-20 µg/mL | Degrades DNA to reduce viscosity | 30-45 min |
| Advanced DMEM/F12 | Base medium | - | - |
Table 2: Expected Cell Yield & Viability by Biopsy Type
| Biopsy Type | Average Mass (mg) | Expected Yield (Viable Cells) | Target Viability Threshold |
|---|---|---|---|
| Core Needle (Tumor) | 10-30 | 0.5 - 5.0 x 10⁶ | >80% |
| Surgical Resection | 100-500 | 20 - 100 x 10⁶ | >70% |
| Fine Needle Aspirate (FNA) | 5-15 | 0.1 - 2.0 x 10⁶ | >75% |
Table 3: Complete Organoid Culture Medium Formulation
| Component | Final Concentration | Function |
|---|---|---|
| Advanced DMEM/F12 | Base | Nutrient supply |
| HEPES | 10 mM | pH buffering |
| B-27 Supplement | 1x | Growth factors & hormones |
| N-2 Supplement | 1x | Neural & basal factors |
| Recombinant EGF | 50 ng/mL | Epithelial proliferation |
| Recombinant FGF-10 | 100 ng/mL | Mesenchymal signaling |
| Noggin | 100 ng/mL | BMP inhibition |
| R-spondin-1 | 500 ng/mL | WNT pathway enhancement |
| Primocin | 100 µg/mL | Antibiotic/Antimycotic |
Signaling Pathways & Workflow Visualizations
Diagram Title: Key Signaling in Tumor Organoid Maturation
Diagram Title: Patient Biopsy to Bioprinted Organoid Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item/Category | Example Product/Type | Function in Workflow |
|---|---|---|
| Tissue Digestion Kit | GentleMACS Tumor Dissociation Kit | Standardized enzymatic blend for efficient tumor tissue dissociation into single cells/spheroids. |
| Basal Medium | Advanced DMEM/F-12 | Low-serum, optimized base for epithelial and stem cell culture, used in organoid medium. |
| Growth Factor Cocktail | Recombinant Human EGF, FGF-10, Noggin, R-spondin-1 | Essential supplements to activate pathways for stem cell maintenance and proliferation. |
| Defined Supplement | B-27 & N-2 Supplements | Serum-free replacements providing hormones, proteins, and essential nutrients. |
| ECM Hydrogel | Cultrex Reduced Growth Factor BME, Type I Collagen, Fibrinogen | Provides 3D scaffolding that mimics the native tumor extracellular matrix for bioink formulation. |
| Bioprinter & Bioink Kit | BIO X (CELLINK), LifeInk Basement Membrane Matrix | Extrusion-based printing system with compatible, sterile, and tunable bioink materials. |
| Viability Assay (3D) | CellTiter-Glo 3D Cell Viability Assay | Luminescent assay optimized for measuring ATP in 3D organoid structures for drug screening. |
| Cell Recovery Solution | Corning Matrigel Cell Recovery Solution | A non-enzymatic, chilled solution for recovering cells/organoids from ECM hydrogels for passaging/analysis. |
Within the broader thesis on 3D bioprinting of tumor organoids for drug screening and cancer biology research, bioink selection is a foundational determinant of model fidelity. Bioinks must facilitate printability while recapitulating the complex tumor microenvironment (TME). Natural polymers excel at providing biological cues, while synthetic polymers offer superior mechanical and chemical control. These Application Notes and Protocols guide the selection and application of these materials for specific tumor mimicry objectives.
Comparative Analysis: Natural vs. Synthetic Polymers
Table 1: Key Properties of Natural Polymer Bioinks
| Polymer | Key Advantages (for Tumor Mimicry) | Key Limitations | Ideal Tumor Model Context |
|---|---|---|---|
| Collagen I | Major in vivo ECM component; supports cell adhesion, migration, and signaling; inherently biocompatible. | Low viscosity; weak mechanical properties; high batch variability. | Stroma-rich carcinomas (e.g., breast, pancreatic); studying invasion. |
| Matrigel | Rich in basement membrane proteins (laminin, collagen IV); promotes epithelial morphogenesis and stemness. | Tumor-derived; undefined composition; animal origin; poor mechanical rigidity. | Epithelial/adenocarcinoma organoids (e.g., prostate, colon); stem cell niches. |
| Alginate | Excellent printability via ionic crosslinking; inert, allows decoupling of matrix mechanics from biochemistry. | Lacks cell-adhesive motifs (requires modification, e.g., RGD); non-degradable by mammalian cells. | Mechanical tuning of tumor spheroids; hybrid/composite bioinks. |
| Hyaluronic Acid (HA) | Major component of desmoplastic TME; influences cancer cell proliferation, invasion, and drug resistance. | Requires chemical modification (e.g., methacrylation) for stability; can be overly hydrophilic. | Models for glioblastoma, breast cancer; studying HA-CD44 interactions. |
| Fibrin | Mimics provisional wound-healing matrix in tumors; promotes rapid angiogenesis and cell invasion. | Rapid enzymatic degradation; requires protease inhibitors for stability. | Modeling tumor-associated vasculogenesis and metastasis. |
Table 2: Key Properties of Synthetic Polymer Bioinks
| Polymer | Key Advantages (for Tumor Mimicry) | Key Limitations | Ideal Tumor Model Context |
|---|---|---|---|
| Poly(ethylene glycol) (PEG) | Highly tunable mechanical properties; bio-inert "blank slate" for modular biochemical functionalization. | Requires incorporation of adhesive peptides (RGD) and MMP-sensitive crosslinkers. | Reductionist studies of specific ECM cues and matrix stiffness. |
| Pluronic F127 | Excellent shear-thinning for printing; temporary sacrificial material for creating perfusable channels. | Melts above ~15°C; not suitable as a long-term cell carrier. | Creating vascular networks within tumor organoids. |
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable; allows sustained release of chemotherapeutic drugs for co-culture testing. | Requires organic solvents or high temps for printing; acidic degradation products. | Drug delivery testing platforms; models requiring long-term structural support. |
| GelMA (Gelatin Methacryloyl) | Hybrid material: combines natural (RGD, MMP-sensitive) and synthetic (photocurable, tunable) properties. | Properties depend on degree of methacrylation and source gelatin. | Versatile use for most tumor organoids balancing printability and bioactivity. |
Table 3: Quantitative Performance Comparison
| Parameter | Natural Polymers (e.g., Collagen/Matrigel) | Synthetic Polymers (e.g., PEG/GelMA) | Measurement Method |
|---|---|---|---|
| Printability Fidelity (Shape) | Low to Moderate (0.6-0.75) | High (0.8-0.95) | Shape Fidelity Factor (SFF) |
| Typical Elastic Modulus (G') | 10 - 500 Pa | 500 Pa - 20 kPa | Rheology (Oscillation) |
| Degradation Time | Hours to Days (enzymatic) | Days to Weeks (hydrolytic/ enzymatic) | Mass loss / Swelling ratio |
| Ligand Density | High (native) | Tunable (0-10 mM RGD) | Fluorescence assay |
| Approximate Cost per mL | High ($50-$500) | Low to Moderate ($10-$100) | Commercial pricing |
Detailed Experimental Protocols
Protocol 1: Formulating and Characterizing a Hybrid HA-GelMA Bioink for Desmoplastic Tumor Models
Objective: To create a bioink that mimics the hyaluronic acid-rich, stiffened stroma of pancreatic ductal adenocarcinoma (PDAC).
Materials:
- Methacrylated Hyaluronic Acid (MeHA, 5% w/v)
- GelMA (7% w/v)
- Photoinitiator (LAP, 0.25% w/v)
- PDAC cell line (e.g., PANC-1) + Cancer-Associated Fibroblasts (CAFs)
- DMEM culture medium
- UV Light Source (365 nm, 5-10 mW/cm²)
- Rheometer
- 3D Bioprinter (extrusion-based)
Procedure:
- Bioink Preparation: Under sterile conditions, mix MeHA and GelMA solutions at a 1:3 volume ratio (e.g., 250 µL MeHA + 750 µL GelMA). Add LAP to final concentration of 0.25%. Gently mix with PDAC cells and CAFs at a 2:1 ratio (2e6 cells/mL total density).
- Rheological Characterization: Load bioink onto rheometer plate. Perform:
- Flow Ramp: Measure viscosity vs. shear rate (0.1 to 100 s⁻¹). Confirm shear-thinning behavior.
- Amplitude Sweep: Determine linear viscoelastic region (LVR) and storage modulus (G') at 1% strain.
- Printing Parameters: Load bioink into a sterile cartridge. Set printer temperature to 18-22°C. Use a 22G-27G nozzle. Optimize pressure (15-25 kPa) and print speed (5-10 mm/s) for continuous filament deposition.
- Crosslinking: Immediately post-printing, expose construct to 365 nm UV light at 5 mW/cm² for 30-60 seconds per layer.
- Culture: Transfer crosslinked construct to culture plate. Feed with appropriate medium. Monitor cell viability (Live/Dead assay at 24h) and fibroblast-mediated matrix remodeling over 7-14 days.
Protocol 2: Drug Screening Using a PEG-Based Bioink with Tunable Stiffness
Objective: To isolate the effect of matrix stiffness on chemotherapeutic drug efficacy in breast cancer organoids.
Materials:
- 4-Arm PEG-Acrylate (20 kDa)
- RGDSP peptide (integrin-binding)
- MMP-sensitive crosslinker peptide (e.g., GCGPQG↓IWGQGCG)
- Photoinitiator (Irgacure 2959, 0.5% w/v in PBS)
- MCF-7 or MDA-MB-231 breast cancer cells
- Doxorubicin hydrochloride
- Stiffness Tuning Reagents: Vary PEG molarity (5-10% w/v).
Procedure:
- Bioink Formulation: Prepare two PEG precursor solutions: Solution A: 4-Arm PEG-Acrylate + RGD peptide (1 mM final). Solution B: 4-Arm PEG-Acrylate + MMP-sensitive crosslinker (3 mM final). Mix Solutions A and B 1:1. Add photoinitiator and cells (5e6 cells/mL).
- Stiffness Gradient Fabrication: Pipette 50 µL of cell-laden bioink into cylindrical molds (8 mm diameter). Expose to UV light (10 mW/cm², 2-5 mins) to form hydrogels of varying stiffness by adjusting PEG concentration (5%, 7.5%, 10%).
- Organoid Culture: Culture gels in medium for 96 hours to allow organoid formation.
- Drug Treatment: Add a dose range of Doxorubicin (0-10 µM) to the culture medium. Refresh medium with drug every 48 hours.
- Viability Analysis: At 72h post-treatment, assay viability using AlamarBlue or CellTiter-Glo 3D. Normalize luminescence/fluorescence to untreated controls of matching stiffness. Plot IC50 vs. Storage Modulus (G').
Visualizations
Title: Bioink Selection Logic for Tumor Mimicry
Title: HA-CD44 Signaling in Tumor Progression
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Bioink-based Tumor Organoid Research
| Item | Function & Relevance | Example Product/Catalog |
|---|---|---|
| Methacrylated Gelatin (GelMA) | Photocrosslinkable, bioactive workhorse for many tumor organoid models. Provides integrin-binding sites and MMP sensitivity. | GelMA Kit, Advanced BioMatrix |
| RGD Adhesion Peptide | Crucial for functionalizing synthetic bioinks (e.g., PEG) to enable integrin-mediated cell adhesion and survival. | GCGRGDS, Sigma-Aldrich |
| MMP-Sensitive Crosslinker | Enables cell-mediated remodeling of synthetic hydrogel networks, critical for invasion assays. | GCGPQG↓IWGQGCG, Peptides International |
| LAP Photoinitiator | Cytocompatible photoinitiator for visible/UV light crosslinking of methacrylated bioinks. | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate, Sigma-Aldrich |
| Y-27632 (ROCK Inhibitor) | Enhances cell survival post-printing by reducing apoptosis in dissociated cells, especially crucial for primary tumor cells. | Y-27632 dihydrochloride, Tocris |
| Matrigel Basement Membrane Matrix | Gold standard for epithelial tumor organoid culture from patient-derived samples. Often used as a bioink component or post-print overlay. | Corning Matrigel Matrix |
| AlamarBlue Cell Viability Reagent | Fluorescent/resazurin-based assay for non-destructive, longitudinal viability measurement in 3D cultures. | Invitrogen AlamarBlue HS Cell Viability Reagent |
| Collagenase Type I/II | Enzymes for recovering cells from natural polymer (collagen, Matrigel) based bioprinted constructs for endpoint analysis. | Worthington Biochemical |
Within the context of advancing 3D bioprinting for tumor organoid research, the selection and preparation of cellular building blocks are foundational. The choice between primary cells, immortalized cell lines, and complex co-cultures directly dictates the physiological relevance, reproducibility, and translational value of the resulting bioprinted construct. This application note details current protocols and considerations for sourcing and preparing these cellular components, specifically for fabricating tumor organoids that accurately recapitulate the tumor microenvironment (TME).
Cell Source Comparison and Selection
The quantitative and qualitative characteristics of different cell sources are summarized in Table 1.
Table 1: Comparative Analysis of Cell Sources for 3D Bioprinted Tumor Organoids
| Feature | Primary Tumor Cells | Immortalized Cell Lines | Co-culture Systems |
|---|---|---|---|
| Physiological Relevance | High (retains patient-specific genetics, heterogeneity) | Low to Moderate (genetically altered, clonal) | Very High (captures cell-cell interactions) |
| Expansion Potential | Limited (senescence after 5-15 passages) | Virtually Unlimited | Limited by primary cell component |
| Reproducibility | Low (high donor-to-donor variability) | Very High | Moderate (subject to variability of primary cells) |
| Cost & Accessibility | High (requires tissue procurement, complex isolation) | Low (commercially available) | Very High (multiple cell isolations, media optimization) |
| Typential for High-Throughput Drug Screening | Low | Very High | Moderate to High |
| Key Application in Bioprinting | Patient-specific models, personalized therapy testing | Mechanistic studies, toxicity screening, protocol optimization | Modeling tumor-stroma interactions, immune-oncology studies |
Detailed Protocols
Protocol: Isolation and Expansion of Primary Tumor Cells from Solid Tissue
Objective: To isolate and culture viable primary tumor cells from patient-derived xenograft (PDX) tissue or surgical resections for use in bioink formulation.
Materials (Research Reagent Solutions):
- Collagenase/Hyaluronidase Solution: Enzymatically dissociates extracellular matrix.
- DNase I: Degrades free DNA released by dead cells, reducing clumping.
- Red Blood Cell Lysis Buffer: Lyses contaminating erythrocytes.
- StemCell Tumor Dissociation Medium: A commercially available, optimized enzymatic cocktail for gentle tumor dissociation.
- Defined, Serum-Free Tumor Media (e.g., MammoCult): Supports epithelial/tumor cell growth while inhibiting fibroblast overgrowth.
- ROCK Inhibitor (Y-27632): Improves viability of single cells post-dissociation by inhibiting anoikis.
Method:
- Tissue Processing: Aseptically transfer ~1 cm³ of tumor tissue to a petri dish with 5 mL of cold wash buffer (PBS + 2% Antibiotic-Antimycotic). Mince into <1 mm³ fragments using sterile scalpels.
- Enzymatic Dissociation: Transfer fragments to a 50 mL tube containing 10 mL of pre-warmed Tumor Dissociation Medium. Add DNase I to a final concentration of 100 U/mL. Place tube in a shaking incubator at 37°C for 45-90 minutes.
- Mechanical Disruption: Every 15 minutes, vigorously pipette the suspension up and down with a 10 mL serological pipette.
- Filtration & Quenching: Pass the digested slurry through a 100 µm cell strainer. Quench the enzyme with 20 mL of complete media containing 10% FBS.
- Centrifugation & Lysis: Centrifuge at 300 x g for 5 minutes. Resuspend pellet in 5 mL of RBC Lysis Buffer. Incubate for 5 minutes at RT. Add 20 mL of PBS and centrifuge again.
- Plating: Resuspend the final cell pellet in defined tumor media supplemented with 10 µM ROCK inhibitor. Plate cells in a low-attachment plate to selectively enrich for tumor cells over stromal fibroblasts. Culture at 37°C, 5% CO₂.
- Expansion: Refresh media every 2-3 days. Passage using gentle enzyme-free dissociation buffer when organoids reach 200-300 µm in diameter.
Protocol: Preparation of Immortalized Cell Lines for Bioink
Objective: To culture and prepare consistent, high-viability batches of cancer cell lines (e.g., MCF-7, U87-MG) for standardizable bioink preparation.
Method:
- Standard 2D Culture: Maintain cells in T-175 flasks using their recommended media (e.g., DMEM + 10% FBS for U87-MG). Passage at 80-90% confluency using 0.25% Trypsin-EDTA.
- Harvesting for Bioink: At the target passage, wash flask with PBS. Add trypsin and incubate at 37°C for 3-5 minutes. Neutralize with complete media.
- Quality Control: Count cells using an automated cell counter or hemocytometer. Assess viability via Trypan Blue exclusion; aim for >95%.
- Bioink Formulation: Centrifuge cell suspension at 300 x g for 5 min. Resuspend cell pellet at a high density (e.g., 1-10 x 10⁶ cells/mL) in the chosen hydrogel precursor (e.g., gelatin methacryloyl (GelMA), collagen, or a commercial bioink like CELLINK BIONINK X). Mix gently to avoid introducing bubbles.
- Preservation of Phenotype: For key lines, validate the expression of relevant markers (e.g., EGFR, HER2) via flow cytometry before bioink formulation.
Protocol: Establishing a Heterotypic Co-culture Bioink
Objective: To combine primary cancer-associated fibroblasts (CAFs) with a tumor cell line in a spatially defined bioink for bioprinting a stromal-vascular niche.
Materials (Research Reagent Solutions):
- Dual-Channel Printing Cartridge: Allows for side-by-side deposition of two distinct bioinks/cell populations.
- CAF Isolation Medium: DMEM/F12 supplemented with 10% FBS, 1% Pen/Strep, and 2 ng/mL basic FGF.
- Endothelial Growth Medium-2 (EGM-2): Specialized media for HUVECs or other endothelial cells.
- PEG-based Crosslinker: Used for rapid physical or chemical crosslinking of bioinks post-printing to maintain spatial arrangement.
Method:
- Component Preparation:
- CAFs: Isolate from fresh tumor tissue using differential adhesion speed or fluorescence-activated cell sorting (FACS) for a specific marker (e.g., FAP-α). Expand in CAF medium.
- Tumor Cells: Prepare as per Protocol 3.2.
- Endothelial Cells (Optional): Culture HUVECs in EGM-2.
- Bioink Compartmentalization:
- Bioink A (Stroma Mimic): Suspend CAFs (5 x 10⁶ cells/mL) in a 3 mg/mL collagen I hydrogel.
- Bioink B (Tumor Niche): Suspend tumor cells (1 x 10⁷ cells/mL) in a 10% w/v GelMA hydrogel.
- Load Bioink A and B into separate compartments of a dual-channel cartridge.
- Bioprinting: Use a core-shell or side-by-side printing configuration to deposit CAF-laden and tumor-laden hydrogels in close proximity, creating a defined tumor-stroma interface.
- Crosslinking & Culture: Immediately after deposition, expose the construct to UV light (for GelMA) and incubate at 37°C (for collagen) for crosslinking. Transfer to advanced 3D culture media, potentially a 1:1 mix of the component-specific media, or a specialized organoid media.
Signaling Pathways in the Tumor Microenvironment
The success of a bioprinted co-culture organoid relies on recapitulating key intercellular signaling. A critical pathway is the CXCL12/CXCR4 axis between Cancer-Associated Fibroblasts (CAFs) and tumor cells.
Diagram 1: CXCL12/CXCR4 Signaling in Tumor-Stroma Crosstalk
Experimental Workflow for Cell Sourcing to Bioprinting
A generalized workflow from cell source selection to functional bioprinted organoid is depicted below.
Diagram 2: Workflow from Cell Source to Bioprinted Organoid Assay
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Cell Sourcing and Preparation in Tumor Organoid Bioprinting
| Reagent Category | Specific Example | Function in Protocol |
|---|---|---|
| Tissue Dissociation | Collagenase IV, Tumor Dissociation Kits (e.g., Miltenyi) | Enzymatically breaks down ECM to release single cells from solid tumor samples with high viability. |
| Selective Media | Serum-Free Organoid Media (e.g., IntestiCult), MammoCult | Chemically defined formulations that support stem/progenitor tumor cell growth while suppressing stromal overgrowth. |
| Viability Enhancer | ROCK Inhibitor (Y-27632) | A small molecule that inhibits apoptosis (anoikis) in single cells and newly formed organoids, critical after dissociation. |
| Hydrogel/Bioink | Gelatin Methacryloyl (GelMA), Collagen I, Matrigel | Provides a tunable, biocompatible 3D scaffold that mimics the native extracellular matrix for cell encapsulation. |
| Crosslinker | Photoinitiator (LAP), CaCl₂ Solution | Initiates rapid polymerization (crosslinking) of hydrogels post-printing to stabilize the 3D structure. |
| Characterization | Live/Dead Viability Kit, Phalloidin (F-actin stain) | Allows for qualitative and quantitative assessment of cell health and morphology within the printed construct. |
Within the broader thesis on 3D bioprinting of tumor organoids for cancer research and drug development, the selection of an appropriate bioprinting technique is paramount. The technique directly influences cell viability, spatial resolution, architectural complexity, and biomimicry of the resulting tumor model. This application note provides a comparative analysis of three core bioprinting modalities—Extrusion, Laser-Assisted, and Inkjet Printing—detailing their underlying principles, experimental protocols, and specific applications in generating high-fidelity tumor organoids.
Table 1: Core Bioprinting Technique Parameters for Tumor Organoid Fabrication
| Parameter | Extrusion Bioprinting | Laser-Assisted Bioprinting (LAB) | Inkjet Bioprinting |
|---|---|---|---|
| Mechanism | Mechanical or pneumatic displacement | Laser-induced forward transfer (LIFT) | Thermal or piezoelectric droplet ejection |
| Typical Resolution | 100 - 1000 µm | 10 - 100 µm | 50 - 300 µm |
| Cell Density Support | High (10^6 - 10^8 cells/mL) | Moderate (10^6 - 10^7 cells/mL) | Low (< 10^6 cells/mL) |
| Print Speed | Slow to Moderate (1 - 50 mm/s) | Moderate (200 - 1600 mm/s) | High (1 - 10,000 droplets/s) |
| Cell Viability (Post-Print) | 40% - 95% (shear-dependent) | 85% - 99% (low shear) | 75% - 95% (thermal/pressure stress) |
| Key Bioink Requirement | High viscosity, shear-thinning | Energy-absorbing layer (e.g., gold, gelatin), low-viscosity bioink | Low viscosity, no particulate clogging |
| Cost of Entry | Low to Moderate | Very High | Moderate |
| Ideal Tumor Organoid Use Case | Large, dense cores; multi-material stromal interfaces; vascular channels. | High-resolution cell patterning; heterogeneous co-culture; micro-metastases niches. | Low-density cell seeding; gradient generation; drug compound printing onto organoids. |
Table 2: Tumor Organoid Application Suitability
| Application Goal | Recommended Technique | Rationale |
|---|---|---|
| High-Throughput Drug Screening | Inkjet | Fast deposition of organoid arrays; compatible with microplate formats. |
| Complex Tumor Microenvironment (TME) | Extrusion | Enables printing of multiple cell types (cancer, fibroblast, endothelial) & acellular ECM components in 3D. |
| Studying Cancer Stem Cell Niche | Laser-Assisted | Precise placement of single cells or small clusters within a defined ECM architecture. |
| Metastasis & Invasion Models | Multi-Method (Extrusion + Inkjet) | Extrusion for primary tumor core, inkjet for depositing chemokine gradients or secondary cell types. |
| Vascularized Tumor Organoids | Extrusion (Coaxial) | Direct printing of perfusable lumen structures using core-shell nozzles. |
Detailed Experimental Protocols
Protocol 1: Extrusion Bioprinting of a Colorectal Cancer Organoid Core with Stromal Shell
Aim: To create a 3D tumor organoid with a core-shell structure mimicking a tumor mass surrounded by cancer-associated fibroblasts (CAFs).
Materials: See "The Scientist's Toolkit" Section 5.
Procedure:
- Bioink Preparation:
- Tumor Core Bioink: Mix 8 x 10^6 cells/mL dissociated patient-derived colorectal cancer organoid cells with 3% (w/v) alginate and 5 mg/mL fibrinogen in DMEM. Keep on ice.
- Stromal Shell Bioink: Mix 5 x 10^6 cells/mL CAFs with 3% (w/v) alginate and 3 mg/mL type I collagen in DMEM. Keep on ice.
- Prepare crosslinking solution: 100 mM CaCl₂ in PBS.
Bioprinter Setup:
- Load tumor core bioink into a 3 mL syringe fitted with a 22G (410 µm inner diameter) conical nozzle.
- Load stromal shell bioink into a second 3 mL syringe fitted with a 25G (250 µm inner diameter) nozzle.
- Set print bed temperature to 15°C.
- Program print path: A series of concentric circles (5 mm total diameter). The inner 3 mm diameter will be printed with the core bioink, immediately surrounded by an outer shell of stromal bioink.
Printing & Crosslinking:
- Initiate printing onto a petri dish. Use pneumatic pressure (20-25 kPa for core, 15-20 kPa for shell).
- Immediately after deposition, mist the construct with CaCl₂ solution for 30 seconds to ionically crosslink the alginate.
- Transfer construct to a 24-well plate. Add 500 µL of culture medium containing 2 U/mL thrombin to enzymatically crosslink the fibrinogen to fibrin.
- Incubate at 37°C for 30 min.
Post-Print Culture:
- Gently replace solution with complete organoid culture medium.
- Culture for up to 21 days, with medium changes every 2-3 days, for maturation and ECM remodeling.
Protocol 2: Laser-Assisted Bioprinting of a Breast Cancer Micro-Niche Array
Aim: To pattern breast cancer stem cells (BCSCs) and mesenchymal stem cells (MSCs) in precise geometries to study paracrine signaling.
Materials: See "The Scientist's Toolkit" Section 5.
Procedure:
- Ribbon Preparation:
- Coat a 1-inch quartz microscope slide (ribbon) with a 50 nm layer of gold using a sputter coater.
- Deposit a 100 µm thick layer of sterile 5% (w/v) gelatin in PBS onto the gold layer. Let it set at 4°C.
- Carefully pipette 100 µL of bioink (containing 1 x 10^7 cells/mL BCSCs or MSCs in low-viscosity Matrigel-based medium) onto the gelatin layer. Spread evenly.
Receiver Slide Preparation:
- Coat a cell culture dish with a thin layer of 2% (w/v) agarose to create a non-adhesive surface.
- Cover with a thin layer of pure Matrigel (~300 µm thick).
LAB Printing:
- Mount the ribbon (cell-side down) and receiver slide in the printer.
- Set laser parameters: Nd:YAG laser, λ=1064 nm, pulse duration 8 ns, spot size 60 µm, energy 40 µJ.
- Program the desired array pattern (e.g., 10x10 grid of BCSC spots, each surrounded by four MSC spots at 200 µm distance).
- Initiate printing. The laser pulses vaporize the gold layer, generating a bubble that propels a microdroplet of bioink onto the receiver slide.
Post-Print Culture:
- After printing, carefully transfer the receiver dish to an incubator (37°C, 5% CO₂) for 15 minutes to allow Matrigel gelation.
- Add warm culture medium gently. Culture and monitor for sphere formation and interaction.
Protocol 3: Inkjet Bioprinting for Drug Sensitivity Testing on Pre-formed Tumor Organoids
Aim: To create a concentration gradient of a chemotherapeutic agent across an array of tumor organoids.
Materials: See "The Scientist's Toolkit" Section 5.
Procedure:
- Organoid Array Preparation:
- Using a low-density Matrigel droplet method, pre-form ~500 colorectal cancer organoids per well in a 96-well U-bottom ultra-low attachment plate over 7 days.
- Manually transfer individual organoids (~150 µm diameter) to a flat-bottom 96-well plate, one per well, in 50 µL of medium.
Drug Solution & Printer Setup:
- Prepare a 10 mM stock of 5-Fluorouracil (5-FU) in DMSO.
- Serially dilute in culture medium to create 5 concentrations (e.g., 100 µM, 50 µM, 10 µM, 1 µM, 0.1 µM).
- Load each concentration into separate cartridges of a multi-cartridge inkjet bioprinter.
- Program the printer to dispense a 10 nL droplet of the respective drug concentration into 16 replicate wells per concentration.
Printing & Incubation:
- Execute the print run. The low droplet volume minimizes dilution.
- Include control wells receiving 10 nL of medium only.
- Place the plate in the incubator for 72 hours.
Viability Assessment:
- Add 20 µL of CellTiter-Glo 3D reagent to each well.
- Shake orbially for 5 minutes, incubate for 25 minutes at room temperature.
- Measure luminescence. Plot relative viability vs. log[drug concentration] to generate dose-response curves.
Visualizations
Extrusion Bioprinting Workflow for Tumor Organoids
Bioprinting Technique Selection Logic for Tumor Research
Key Signaling Pathways Interrogated in Bioprinted Tumor Organoids
The Scientist's Toolkit
Table 3: Essential Research Reagents & Materials for Bioprinting Tumor Organoids
| Item | Function & Rationale | Example Product/Category |
|---|---|---|
| Basement Membrane Extract (BME) | Provides essential laminin-rich ECM for epithelial cancer cell survival and polarization. Critical for organoid formation post-printing. | Corning Matrigel GFR, Cultrex BME |
| Alginate (High G-Content) | Fast ionic crosslinker for bioink shape fidelity. Often combined with other materials to improve cell adhesion. | NovaMatrix PRONOVA SLG100 |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable, cell-adhesive hydrogel. Tunable stiffness allows modeling of biomechanical cues in the TME. | Advanced BioMatrix GelMA, Cellink Bioink |
| Fibrinogen/Thrombin | Enzymatically forms fibrin, a natural provisional matrix that promotes cell migration, invasion, and vascular morphogenesis. | Sigma-Aldrich Fibrinogen from plasma |
| Patient-Derived Xenograft (PDX) Cells | Gold-standard for maintaining tumor heterogeneity, genotype, and drug response profile in vitro. | Champions Oncology, The Jackson Laboratory |
| Cancer-Associated Fibroblasts (CAFs) | Essential stromal component for modeling desmoplasia, chemoresistance, and metastatic signaling. | ScienCell Research Laboratories, isolated from tumor tissue. |
| Low-Adhesion/Spheroid Microplates | For pre-culture and maturation of organoids prior to or after printing. | Corning Ultra-Low Attachment plates, Nunclon Sphera plates |
| Rho-Kinase (ROCK) Inhibitor (Y-27632) | Dramatically improves viability of dissociated epithelial/CRC cells post-printing by inhibiting anoikis. | Tocris Bioscience, Selleckchem |
| Multi-Channel Bioprinter | Enables simultaneous deposition of tumor and stromal bioinks, crucial for modeling the TME. | Cellink BIO X6, Allevi 3 |
| Live/Dead Viability Assay Kit | Standard for quantifying cell survival post-printing (e.g., Calcein-AM/EthD-1). | Thermo Fisher Scientific LIVE/DEAD Viability/Cytotoxicity Kit |
Within the broader thesis on 3D bioprinting of tumor organoids, the post-printing phase is critical for ensuring biological fidelity and long-term experimental utility. This document provides detailed application notes and protocols for the maturation, maintenance, and functional validation of bioprinted tumor organoids, focusing on achieving physiological relevance over extended culture periods.
Key Post-Printing Challenges & Stabilization Targets
Successful maturation requires addressing specific post-printing stressors to stabilize key cellular functions.
Table 1: Primary Post-Printing Stressors and Stabilization Targets
| Stressor Category | Key Manifestations | Primary Stabilization Targets | Typical Stabilization Timeframe (Days) |
|---|---|---|---|
| Mechanical | Membrane disruption, cytoskeletal damage. | Integrin signaling, RHO-ROCK pathway. | 1-3 |
| Metabolic | Hypoxia, nutrient gradient formation. | HIF-1α signaling, glycolytic flux. | 3-7 |
| Cell-Cell/ECM | Disrupted adhesion, nascent matrix. | E-cadherin localization, collagen IV deposition. | 7-14 |
| Phenotypic Drift | Loss of original tumor signature. | Key driver mutation signaling (e.g., EGFR, Wnt). | 14+ |
Core Maturation Protocol: A Stage-Wise Approach
A phased approach guides the organoid from immediate post-print recovery to long-term culture.
Phase I: Acute Recovery (Days 0-3)
Objective: Mitigate printing-induced apoptosis and initiate cell-cell contact.
Protocol:
- Immediate Transfer: Post-printing, transfer constructs to a pre-equilibrated 6-well plate using a wide-bore pipette tip.
- Recovery Medium: Culture in "Stabilization Medium": Advanced DMEM/F12 supplemented with:
- 10 µM Y-27632 (ROCK inhibitor).
- 1x B-27 Supplement (minus vitamin A).
- 1x N-2 Supplement.
- 1% Penicillin-Streptomycin.
- 10% (v/v) conditionally reprogrammed fibroblast-conditioned medium.
- Environment: Maintain at 37°C, 5% CO2, 20% O2 (normoxia). Do not disturb for first 48 hours.
- First Medium Change: At 72 hours, aspirate 50% of medium gently and replace with fresh Stabilization Medium (without Y-27632).
Phase II: Matrix Maturation & Proliferation (Days 4-14)
Objective: Promote endogenous ECM deposition and establish proliferative niches.
Protocol:
- Medium Shift: Transition to "Growth Medium": Stabilization Medium (without Y-27632) plus:
- Organoid-specific growth factors (e.g., 50 ng/mL EGF for colorectal, 100 ng/mL FGF-10 & Noggin for gastric).
- 1% (v/v) Matrigel for scaffolding support.
- Feeding Schedule: Perform a full medium change every 48 hours.
- Monitoring: Image daily using bright-field microscopy. Expect visible spheroid formation and perimeter smoothing by Day 7-10.
Phase III: Long-Term Maintenance & Propagation (Day 15+)
Objective: Maintain genomic and phenotypic stability over serial passages.
Protocol:
- Regular Maintenance: Continue with Growth Medium, changing every 48-72 hours.
- Passaging (every 10-14 days): a. Gently aspirate medium. b. Add 1 mL of cold Cell Recovery Solution (Corning) per construct. Incubate 30-60 min on ice to dissolve residual bioink. c. Mechanically dissociate using a P1000 pipette (10-15 strokes). d. Pass through a 40 µm cell strainer. e. Centrifuge at 300 x g for 5 min. f. Resuspend in Growth Medium + 10 µM Y-27632. Re-seed into fresh pre-warmed bioink or Matrigel droplets.
- Cryopreservation: Resuspend dissociated organoids in Recovery Medium with 10% DMSO. Cool at -1°C/min in an isopropanol chamber before transfer to liquid N2.
Validation & Functional Assessment Protocols
Rigorous validation is required to confirm tumor organoid fidelity.
Protocol: Immunofluorescence for Polarity & Lineage Markers
Fixation: 4% PFA for 45 min at RT. Permeabilization: 0.5% Triton X-100 for 20 min. Blocking: 3% BSA + 0.1% Tween-20 for 2 hours. Primary Antibodies: Incubate overnight at 4°C (e.g., E-cadherin [1:200], Ki67 [1:100], Cleaved Caspase-3 [1:150]). Secondary Antibodies: Incubate for 2 hours at RT (e.g., Alexa Fluor conjugates, 1:500). Imaging: Acquire z-stacks on a confocal microscope.
Protocol: Drug Response Assay (IC50 Determination)
- Dissociate organoids to single cells and re-embed in 50 µL Matrigel droplets (1000 cells/droplet) in a 96-well plate.
- After 72h of recovery, treat with a 10-point serial dilution of the chemotherapeutic agent (e.g., 5-FU, Oxaliplatin).
- At 96h post-treatment, add CellTiter-Glo 3D reagent and luminescence.
- Calculate IC50 values using a four-parameter logistic model in Prism GraphPad.
Table 2: Example Drug Response Data from Bioprinted CRC Organoids
| Chemotherapeutic | Average IC50 (µM) | 95% Confidence Interval | R² of Curve Fit | Reference 2D Monolayer IC50 (µM) |
|---|---|---|---|---|
| 5-Fluorouracil | 12.4 | [9.8 - 15.7] | 0.98 | 1.2 |
| Oxaliplatin | 0.85 | [0.62 - 1.16] | 0.97 | 0.15 |
| Irinotecan | 4.21 | [3.11 - 5.70] | 0.96 | 0.89 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Post-Printing Maturation
| Reagent / Material | Supplier (Example) | Primary Function in Protocol |
|---|---|---|
| Y-27632 (ROCK Inhibitor) | Tocris Bioscience | Reduces anoikis and printing-induced apoptosis during acute recovery. |
| B-27 Supplement (Minus Vitamin A) | Gibco | Provides hormone and nutrient support; minus Vit A reduces differentiation. |
| Recombinant Human EGF/FGF-10/Noggin | PeproTech | Organoid-specific growth factors to maintain stemness and proliferation. |
| Growth Factor-Reduced Matrigel | Corning | Provides a temporary, supportive scaffold for ECM deposition and structure. |
| Cell Recovery Solution | Corning | Dissolves cross-linked bioink (e.g., alginate) without damaging cell-cell junctions. |
| CellTiter-Glo 3D Assay | Promega | Luminescent ATP quantitation for viability in 3D structures. |
| Advanced DMEM/F12 | Gibco | Basal medium optimized for low-serum organoid culture. |
Visualization of Key Pathways and Workflows
Title: Post-Printing Stressors and Stabilization Pathways
Title: Three-Phase Post-Printing Maturation Workflow
Three-dimensional bioprinted tumor organoids have emerged as a transformative platform for oncology research, bridging the gap between traditional 2D cell cultures and in vivo patient-derived xenografts. These constructs recapitulate the tumor microenvironment (TME), including cell-cell interactions, extracellular matrix (ECM) composition, and gradient-driven phenomena like hypoxia. This fidelity makes them ideal for two frontier applications: high-throughput drug screening (HTS) to accelerate drug discovery, and immunotherapy testing to evaluate novel immune-oncology agents such as immune checkpoint inhibitors (ICIs), bispecific T-cell engagers (BiTEs), and CAR-T cells. This document provides detailed application notes and standardized protocols for implementing these assays using bioprinted tumor organoids.
Application Note: High-Throughput Drug Screening (HTS)
Objective: To utilize bioprinted tumor organoids for the rapid, reproducible evaluation of compound libraries, assessing efficacy, toxicity, and mechanism of action.
Key Advantages Over 2D Models:
- Physiological Relevance: 3D architecture influences drug penetration, cell survival signaling, and resistance mechanisms.
- Stromal Integration: Co-printing with cancer-associated fibroblasts (CAFs) and endothelial cells models stromal protection.
- High-Content Readouts: Enables multiplexed endpoint analysis (viability, apoptosis, proliferation).
Quantitative Data Summary: Table 1: Comparison of Drug Screening Platforms
| Platform Feature | 2D Monolayer | Patient-Derived Xenograft (PDX) | 3D Bioprinted Tumor Organoid |
|---|---|---|---|
| Throughput | Very High (>10,000 compounds/week) | Very Low (months) | High (1,000-5,000 compounds/week) |
| Establishment Time | Days | 3-6 months | 2-4 weeks |
| Cost per Screen | Low ($0.01-$0.10/well) | Very High (>$1,000/model) | Medium ($1-$10/well) |
| Microenvironment | Absent | Full in vivo complexity | Tunable & designed |
| Clinical Predictive Value (Correlation) | Low (≤0.5) | High (0.7-0.9) | Promising (0.6-0.8 in recent studies) |
| Z'-Factor (Assay Quality) | Typically >0.7 | Not applicable | 0.5-0.7 (optimized protocols) |
Table 2: Example HTS Results from a Bioprinted Glioblastoma Organoid Screen
| Drug Class | Example Compound | IC50 in 2D (µM) | IC50 in 3D Bioprinted (µM) | Fold Change (3D/2D) | Key Finding |
|---|---|---|---|---|---|
| EGFR Inhibitor | Erlotinib | 1.2 ± 0.3 | 15.4 ± 2.1 | 12.8 | Strong microenvironment-mediated resistance |
| PARP Inhibitor | Olaparib | 5.6 ± 1.1 | 8.9 ± 1.8 | 1.6 | Moderate resistance observed |
| Alkylating Agent | Temozolomide | 250 ± 45 | 280 ± 52 | 1.1 | Similar efficacy, models standard care |
| Experimental | Drug-X | 0.05 ± 0.01 | 0.07 ± 0.02 | 1.4 | High potency maintained in 3D |
Protocol: High-Throughput Viability Screening
Title: Protocol for HTS Using Bioprinted Organoids in 384-Well Plates.
I. Materials: Bioprinting and Culture
- Bioink: Base hydrogel (e.g., GelMA, collagen, hyaluronic acid). Function: Provides tunable, cell-friendly ECM.
- Cells: Patient-derived or cell line tumor cells, optionally mixed with stromal cells (CAFs at 1:4 ratio). Function: Forms the core tumor compartment.
- Extrusion Bioprinter: Equipped with temperature-controlled printheads. Function: Precise deposition of bioink-cell blend.
- 384-Well Microplate, ultralow attachment. Function: Prevents organoid adhesion, supports spheroid formation.
II. Bioprinting Protocol:
- Preparation: Mix tumor cells ± stromal cells with bioink precursor on ice. Final cell density: 5-10 x 10^6 cells/mL.
- Printing: Load bioink into printing cartridge. Using a 200-400 µm nozzle, print a single micro-droplet (≈50 nL) into the center of each well of the 384-well plate. Maintain stage temperature at 4-10°C during printing.
- Crosslinking: Immediately expose plate to appropriate crosslinking stimulus (UV light for GelMA, temperature for collagen) per bioink specifications.
- Culture: Add 50 µL of organoid growth medium per well. Culture plate for 72 hours in a humidified 37°C, 5% CO2 incubator to allow organoid maturation.
III. Compound Screening Protocol:
- Compound Addition: Using an automated liquid handler, transfer 50 nL of compound from a 1000x DMSO stock library into each well. Include controls: DMSO only (vehicle), 10 µM Staurosporine (death control), medium only (low control).
- Incubation: Incubate organoids with compounds for 120 hours.
- Viability Assay: Add 10 µL of CellTiter-Glo 3D reagent directly to each well. Shake orbially for 5 minutes, then incubate in the dark for 25 minutes at RT.
- Readout: Measure luminescence on a plate reader.
- Data Analysis: Normalize raw RLU: %Viability = (Sample - Death Ctrl) / (Vehicle Ctrl - Death Ctrl) * 100. Calculate IC50 using four-parameter logistic curve fit.
Application Note: Immunotherapy Testing
Objective: To model patient-specific immune-tumor interactions and evaluate the efficacy of immunotherapies using bioprinted organoids containing autologous immune components.
Key Advantages:
- Personalized Immunology: Incorporates patient-derived tumor-infiltrating lymphocytes (TILs) or peripheral blood mononuclear cells (PBMCs).
- Spatial Control: Enables precise printing of immune cell zones around tumor regions to model infiltration.
- Functional Readouts: Measures immune-mediated killing, cytokine secretion, and immune cell exhaustion.
Quantitative Data Summary: Table 3: Metrics for Immunotherapy Testing in Bioprinted Organoids
| Immunotherapy Type | Measured Parameter | Typical Assay | Readout Timeline | Key Insight Provided |
|---|---|---|---|---|
| Immune Checkpoint Inhibitors (anti-PD-1/PD-L1) | Tumor Cell Viability, IFN-γ Secretion | Co-culture + antibody treatment | 5-7 days | Reversal of T-cell exhaustion |
| CAR-T Cells | Percent Specific Lysis, CAR-T Proliferation | Tumor organoid + fluorescent CAR-Ts | 3-5 days | Cytolytic activity & tumor penetration |
| Bispecific T-cell Engagers (BiTEs) | Caspase-3/7 Activation in Tumor Cells | Luminescent apoptosis assay | 2-4 days | Redirected T-cell cytotoxicity |
| Oncolytic Viruses | Viral Titer, Bystander Killing Effect | Plaque assay / viability imaging | 3-6 days | Viral replication & spread in 3D |
Table 4: Example Results: Anti-PD-1 Response in Bioprinted NSCLC Organoids
| Patient-Derived Model | PD-L1 IHC Status | TILs Co-printed | % Viability (IgG Control) | % Viability (anti-PD-1) | % Increase in IFN-γ |
|---|---|---|---|---|---|
| NSCLC-01 | High (>50%) | Autologous TILs | 100 ± 8 | 42 ± 6 | 450% |
| NSCLC-02 | Low (1%) | Autologous TILs | 100 ± 12 | 85 ± 9 | 60% |
| NSCLC-03 | Negative | Allogeneic PBMCs | 100 ± 10 | 95 ± 7 | 25% |
Protocol: Immune Cell Co-culture and Checkpoint Inhibition Assay
Title: Protocol for Evaluating Anti-PD-1 Therapy in a Bioprinted Co-culture Model.
I. Materials:
- Bioinks: Two separate inks: Tumor Bioink (as in 2.1), Immune Cell Bioink (low-viscosity alginate or matrix-free medium). Function: Allows separate printing of tumor and immune compartments.
- Cells: Tumor organoid cells (from dissociation of pre-cultured organoids), and autologous TILs or activated PBMCs. Function: Reconstitutes patient-specific immune-tumor unit.
- Therapeutics: Anti-human PD-1 antibody, Isotype control antibody. Function: Therapeutic and control agents.
- Cytokine Kit: Human IFN-γ ELISA kit. Function: Quantifies immune activation.
II. Bioprinting a Co-culture Model:
- Design: Create a concentric circle design: an inner core (1 mm diameter) of tumor bioink, surrounded by an outer ring (200 µm gap) of immune cell bioink.
- Printing: Using a multi-cartridge system, first print the tumor core. Crosslink. Then, switch cartridges and print the immune cell suspension ring directly around it. For alginate, crosslink with a CaCl2 mist.
- Culture: Transfer construct to a 96-well plate. Add 150 µL of immunocompetent medium (e.g., RPMI-1640 + 10% FBS + 100 U/mL IL-2) per well.
III. Immunotherapy Testing Protocol:
- Treatment: At 24 hours post-printing, add anti-PD-1 or isotype control antibody to a final concentration of 10 µg/mL.
- Incubation: Culture for 5-7 days, with 50% medium changes every 2 days.
- Harvest and Analysis:
- Viability: Process wells with CellTiter-Glo 3D as in Protocol 2.1.
- Immunoactivation: Collect supernatant for IFN-γ quantification by ELISA.
- Imaging: Fix and stain for confocal microscopy (e.g., CD8 for T-cells, Caspase-3 for apoptosis, DAPI).
Visualization Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Materials for 3D Bioprinted Organoid Screening & Immunotherapy Assays
| Item Name | Supplier Examples | Function in Application |
|---|---|---|
| GelMA (Gelatin Methacryloyl) | Cellink, Advanced BioMatrix | A tunable, photopolymerizable bioink that provides an RGD-containing ECM mimic for cell encapsulation. |
| CellTiter-Glo 3D | Promega | Optimized luminescent ATP assay for quantifying viability in 3D spheroids and organoids, penetrating larger structures. |
| Recombinant Human IL-2 | PeproTech | Critical cytokine for maintaining the survival and function of T-cells and TILs in co-culture immunotherapy models. |
| Anti-human PD-1 (Clone: nivolumab biosimilar) | Bio X Cell, R&D Systems | Checkpoint inhibitor antibody used to block the PD-1/PD-L1 axis and reactivate exhausted T-cells in co-culture. |
| LIVE/DEAD Viability/Cytotoxicity Kit | Thermo Fisher Scientific | Fluorescent assay (Calcein AM/EthD-1) for imaging live and dead cells in bioprinted constructs via confocal microscopy. |
| Human IFN-γ ELISA Kit | R&D Systems, Abcam | Quantifies interferon-gamma secretion from activated T-cells, a key metric for immune response in immunotherapy screens. |
| Ultra-Low Attachment Microplates (384/96-well) | Corning, Greiner Bio-One | Prevents cell adhesion, promoting 3D organoid formation and preventing stromal monolayer development. |
| Alginate (High G-content) | NovaMatrix, Sigma-Aldrich | Rapidly ionic-crosslinked bioink for gentle encapsulation of sensitive cells like immune cells in co-printing. |
Navigating Challenges: Solutions for Vascularization, Heterogeneity, and Scalability
Application Notes
Effective vascularization remains the primary bottleneck in advancing 3D-bioprinted tumor organoids from model systems to clinically predictive platforms. The core challenge is replicating the complex, perfusable vascular networks that supply nutrients, oxygen, and enable waste removal and systemic drug delivery in vivo. This document outlines current strategies, quantitative benchmarks, and detailed protocols to integrate vasculature within tumor organoid constructs.
Table 1: Comparison of Primary Vascularization Strategies for 3D-Bioprinted Tumor Organoids
| Strategy | Core Methodology | Typical Resolution/Size | Maturation Time | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Sacrificial Bioprinting | Printing of a fugitive ink (e.g., Pluronic F127, Gelatin) later evacuated to form channels. | 100 µm - 1 mm channels | 1-7 days (post-evacuation) | Creates defined, perfusable macroscale architectures; high design flexibility. | Limited to larger initial channels; endothelial lining required for true barrier function. |
| Endothelial Cell-Laden Bioprinting | Direct co-printing of endothelial cells (HUVECs, iPSC-ECs) within bioinks. | Single-cell to spheroid scale | 7-14 days for network formation | Enables de novo capillary formation via vasculogenesis; biologically driven. | Networks often immature and unstable without pericytes; may lack luminal perfusion. |
| Microfluidic Chip Integration | Seeding organoids into pre-fabricated PDMS or polymer chips containing endothelialized channels. | 50-200 µm channels | Immediate perfusion capability | Precise hydrodynamic control; enables direct, live imaging of invasion/extravasation. | Technically complex integration; often lacks 3D tissue microenvironment around vessels. |
| Angiogenic Induction | Use of bioprinted bioinks containing high concentrations of pro-angiogenic factors (VEGF, bFGF). | Capillary-scale sprouting | 3-10 days | Simple; leverages host/organoid's cellular capacity. | Uncontrolled, disorganized sprouting; often results in leaky, non-perfused structures. |
Table 2: Quantitative Metrics for Assessing Vascular Network Functionality
| Metric | Measurement Technique | Target Benchmark for a "Functional" Network | Protocol Reference |
|---|---|---|---|
| Perfusion Efficiency | Fluorescent bead (e.g., 10 µm FITC-dextran) velocity tracking. | >50% of printed channels perfusable at 0.1-1 µL/min flow rate. | Protocol 1 |
| Barrier Integrity | Trans-endothelial electrical resistance (TEER) or Dextran leakage assay. | Apparent TEER > 20 Ω*cm²; <5% leakage of 70 kDa TRITC-dextran in 1 hour. | Protocol 2 |
| Network Morphology | Confocal imaging (CD31/VE-Cadherin stain) and analysis via AngioTool or Fiji. | Average vessel diameter: 10-50 µm; Branching density > 15 junctions/mm². | Protocol 3 |
| Metabolic Activity | Glucose consumption/Lactate production assay or oxygen sensing probes (e.g., Image-iT). | Gradient of O₂ tension from lumen to organoid core (e.g., 80 mmHg to 20 mmHg). | Protocol 4 |
Experimental Protocols
Protocol 1: Perfusion Assessment of a Sacrificially Bioprinted Vascular Network Objective: To establish and quantify fluid flow through an endothelial-lined, sacrificially printed channel within a tumor organoid construct. Materials:
- Bioprinted construct with a gelatin sacrificial channel evacuated and seeded with HUVECs.
- Peristaltic pump or syringe pump.
- FITC-conjugated dextran (70 kDa, 1 mg/mL in culture medium).
- Confocal or live-cell imaging system.
- Image analysis software (e.g., Fiji, Imaris). Method:
- Connect the inlet/outlet of the bioprinted construct's channel to the pump system using sterile tubing.
- Perfuse with FluoroBrite DMEM culture medium at 2 µL/min for 30 minutes to equilibrate.
- Switch perfusion to the FITC-dextran solution. Start simultaneous time-lapse imaging at the construct's mid-plane.
- Record for 10 minutes at 2-second intervals.
- Using Fiji, track the leading edge of the fluorescent front or use particle tracking plugins for bead velocity. Calculate perfusion velocity (µm/s) and the percentage of the total channel length perfused within the first 5 minutes.
Protocol 2: Assessing Endothelial Barrier Integrity via Dextran Leakage Objective: To quantify the passive permeability of the endothelial barrier formed within the bioprinted construct. Materials:
- Vascularized construct.
- TRITC-conjugated dextran (70 kDa, 1 mg/mL).
- Confocal microscope.
- Image analysis software. Method:
- Perfuse the vascular channel with TRITC-dextran solution at a low, static pressure (e.g., 100 Pa) for 5 minutes.
- Gently rinse the channel with dye-free medium for 2 minutes.
- Immediately acquire z-stack confocal images of the vessel wall and surrounding matrix (signal up to 100 µm from the channel).
- Quantify fluorescence intensity in the channel lumen (Ilumen) and in the surrounding matrix region (Imatrix) at multiple points.
- Calculate the Permeability Coefficient (P): P = (I_matrix / I_lumen) * (V / A) * (1 / t), where V is vessel volume, A is vessel surface area, and t is time. Use image-derived values for vessel geometry.
The Scientist's Toolkit: Essential Reagents for Vascularization
Table 3: Key Research Reagent Solutions for Vascularized Tumor Organoid Research
| Reagent/Category | Example Product(s) | Function in Vascularization |
|---|---|---|
| Fugitive/Sacrificial Bioink | Pluronic F127, Carboxymethylcellulose, Gelatin-MA (fugitive). | Creates temporary, perfusable channel templates that are later removed. |
| Endothelial Growth Medium | EGM-2 (Lonza), Vasculife (Lifeline Cell Tech). | Provides specialized nutrients and growth factors (VEGF, FGF, EGF) for endothelial cell survival and proliferation. |
| Pro-Angiogenic Factors | Recombinant Human VEGF-165, bFGF, SDF-1α. | Induces endothelial cell migration, sprouting, and capillary network formation. |
| ECM-Mimetic Hydrogels | Fibrin I, Collagen I, Hyaluronic Acid (MeHA), Matrigel. | Provides a 3D supportive microenvironment conducive to endothelial tubulogenesis and cell-ECM signaling. |
| Pericyte/SMC Co-culture Cells | Human Brain Vascular Pericytes, Mesenchymal Stem Cells. | Stabilizes nascent endothelial tubes, enhances barrier function, and supports mural cell coverage. |
| Live Cell Imaging Dyes | CellTracker dyes, Calcein AM, Hoechst 33342. | For longitudinal tracking of multiple cell types (endothelial, tumor, stromal) within the construct. |
Visualizations
Vascularization Strategy Workflow
Sacrificial Bioprinting & Seeding Protocol
Core VEGF Signaling in Angiogenesis
Within the broader thesis on 3D bioprinting of tumor organoids, a paramount challenge is the accurate recapitulation of the complex cellular heterogeneity found in native tumors. Successful bioprinting must go beyond structural mimicry to capture the diverse populations of cancer cells, cancer stem cells (CSCs), stromal cells, and immune cells that drive tumor progression, drug resistance, and metastasis. This application note details protocols and strategies to preserve this critical heterogeneity throughout the biofabrication pipeline, from cell sourcing and bioink formulation to post-print maturation, enabling the generation of high-fidelity models for drug development.
Key Quantitative Data on Tumor Heterogeneity
Table 1: Representative Cellular Composition of Solid Tumors
| Cell Type | Percentage Range in Tumor Mass | Key Functional Role | Impact if Lost in Model |
|---|---|---|---|
| Malignant Epithelial Cells | 20-80% | Proliferation, invasion | Loss of core oncogenic drivers |
| Cancer Stem Cells (CSCs) | 0.1-10% | Tumor initiation, recurrence, therapy resistance | False-negative drug screening results |
| Cancer-Associated Fibroblasts (CAFs) | 5-50% | ECM remodeling, cytokine signaling, therapy resistance | Altered biomechanics and drug penetration |
| Endothelial Cells | 1-10% | Angiogenesis, nutrient supply | Lack of vascularization and hypoxic gradients |
| Tumor-Infiltrating Lymphocytes (TILs) | 1-40% | Immune response, immunotherapy target | Invalid evaluation of immunotherapies |
| Tumor-Associated Macrophages (TAMs) | 1-30% | Immunosuppression, metastasis | Misrepresented tumor microenvironment |
Table 2: Comparative Outcomes of Heterogeneity-Preserving vs. Standard Bioprinting
| Parameter | Standard Monoculture Bioprinting | Heterogeneity-Preserving Bioprinting | Measurement Technique |
|---|---|---|---|
| CSC Frequency Post-Print | <0.1% (depleted) | 1.5-3.2% (maintained) | Flow cytometry (CD44+/CD24-) |
| Single-Cell RNA-Seq Clusters | 3-5 major clusters | 8-12 distinct cell clusters | Shannon Diversity Index (↑ 2.5-fold) |
| Drug IC50 (e.g., Paclitaxel) | 10 nM | 45 nM (more resistant) | CellTiter-Glo Viability Assay |
| Stromal Signal Retention | Low (Collagen I ↓ 80%) | High (Collagen I ↓ <10%) | ELISA/Immunofluorescence |
| Print Viability (Day 1) | 90-95% | 85-90% | Live/Dead Staining |
Experimental Protocols
Protocol 1: Preparation of Heterogeneous Primary Cell Suspension for Bioink
Objective: To isolate and prepare a viable, heterogeneous single-cell suspension from patient-derived tumor tissue for bioink formulation.
Materials:
- Fresh patient-derived tumor tissue (≥1 cm³)
- GentleMACS Dissociator (Miltenyi Biotec) or similar
- Tumor Dissociation Kit, human (e.g., Miltenyi 130-095-929)
- DMEM/F-12 medium
- Fetal Bovine Serum (FBS)
- 1X PBS, sterile
- 40 µm cell strainer
- RBC Lysis Buffer (if needed)
- Trypan Blue solution (0.4%)
- Hemocytometer or automated cell counter
Procedure:
- Tissue Processing: In a biosafety cabinet, transfer tissue to a petri dish with 10 mL cold PBS. Mince coarsely with sterile scalpels into ~1-2 mm³ fragments.
- Enzymatic Dissociation: Transfer fragments to a GentleMACS C Tube containing enzyme mix (from kit). Attach tube to the GentleMACS Dissociator and run the programmed "37ChTDK_1" protocol (approximately 30-60 min).
- Quenching & Filtration: Add 10 mL of cold complete medium (with 10% FBS) to quench enzymes. Pass the cell suspension through a 40 µm cell strainer into a 50 mL tube.
- Washing & RBC Lysis: Centrifuge at 300 x g for 5 min. Aspirate supernatant. If red pellet is present, resuspend in 5 mL RBC Lysis Buffer for 5 min at RT. Quench with 20 mL PBS.
- Centrifuge & Resuspend: Centrifuge at 300 x g for 5 min. Aspirate supernatant. Resuspend pellet in 5 mL complete medium.
- Viability & Concentration Assessment: Mix 10 µL of cell suspension with 10 µL Trypan Blue. Count live (unstained) and dead (blue) cells using a hemocytometer. Target viability >85%.
- Final Preparation for Bioink: Centrifuge and resuspend cells at the desired concentration (e.g., 5-20 x 10⁶ cells/mL) in the chosen bioink base (e.g., gelatin methacryloyl/GelMA precursor solution) on ice. Proceed immediately to printing.
Protocol 2: Multi-Compartment Extrusion Bioprinting for Zonal Heterogeneity
Objective: To bioprint a tumor organoid with spatially defined zones (e.g., hypoxic core, proliferative rim, invasive edge) using a coaxial or multi-material printhead.
Materials:
- 3D bioprinter with dual or coaxial extrusion capabilities (e.g., BIO X, CELLINK)
- Sterile printhead cartridges (≥ 2)
- FRESH or sacrificial support bath (e.g., Laponite, gelatin slurry)
- Bioink A (Core Bioink): High-density (20 x 10⁶ cells/mL) heterogeneous cell mix in 5% (w/v) GelMA + 1% (w/v) alginate.
- Bioink B (Stromal Rim Bioink): 5 x 10⁶ cells/mL CAFs + endothelial cells in 7% (w/v) GelMA + 2 mg/mL fibrinogen.
- Crosslinking Solutions: 0.1M CaCl₂ for alginate, UV light (365 nm, 5-10 mW/cm²) for GelMA, 2 U/mL thrombin for fibrinogen.
- 37°C Humidified Curing Chamber
Procedure:
- Printer & Bioink Setup: Load Bioink A and Bioink B into separate, sterile cartridges. Maintain at 15°C. Equip printer with a coaxial or side-by-side dual nozzle.
- Support Bath Preparation: Pour sterile support bath into the print chamber to a depth of 10 mm.
- G-Code Design: Program a cylindrical print pattern (e.g., 8 mm diameter, 2 mm height). For coaxial printing, set Bioink A (core) and Bioink B (sheath) to extrude simultaneously. For dual printing, program concentric circles: inner circle (core) with Bioink A, outer 2 rings (rim) with Bioink B.
- Printing Execution: Initiate print within the support bath. Use optimized parameters (Core: 22°C, 25 kPa; Sheath/Rim: 18°C, 20 kPa; speed 8 mm/s).
- Sequential Crosslinking: Immediately post-deposition, mist the construct with CaCl₂ to ionically crosslink alginate. Transfer construct to a Petri dish, rinse with PBS, and expose to UV light (60 seconds) for GelMA photocrosslinking. Incubate in medium containing thrombin (2 U/mL) for 15 min at 37°C to form fibrin.
- Post-Print Culture: Transfer crosslinked construct to a 24-well plate with tumor organoid culture medium. Culture at 37°C, 5% CO₂, with medium changes every 2 days.
Signaling Pathways in Tumor Heterogeneity Maintenance
Experimental Workflow for Heterogeneous Organoid Generation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Preserving Heterogeneity
| Item Name & Supplier | Function in Protocol | Critical for Heterogeneity |
|---|---|---|
| GentleMACS Human Tumor Dissociation Kit (Miltenyi Biotec) | Enzyme blend for gentle tissue dissociation into single cells while preserving surface markers and viability. | Maximizes recovery of all cell types, especially fragile CSCs and stromal cells. |
| Cell Surface Marker Panels for Flow Cytometry (BioLegend) | Antibody cocktails for phenotyping (e.g., CD44/CD24, EpCAM, CD45, CD31). | Enables quantification and sorting of distinct populations pre- and post-print. |
| Gelatin Methacryloyl (GelMA, Cellink or Advanced BioMatrix) | Photocrosslinkable, bioactive hydrogel mimicking native ECM. | Provides a tunable, cell-adhesive environment that supports diverse cell behaviors. |
| Laponite XLG (BYK) | Nanoclay for creating FRESH or support baths. | Allows printing of complex, soft multi-cellular structures without compromising viability. |
| Y-27632 (ROCK Inhibitor) (Tocris) | Small molecule inhibitor of Rho-associated kinase. | Added to post-print medium (10 µM) to mitigate anoikis and improve survival of all cells. |
| Matrigel (Corning) | Basement membrane extract. | Often blended (10-20%) with bioinks to provide essential niche signals for CSCs and epithelium. |
| Live/Dead Viability/Cytotoxicity Kit (Thermo Fisher) | Calcein AM (green/live) and Ethidium homodimer-1 (red/dead) fluorescent dyes. | Assesses initial print viability across all cell populations without bias. |
| 10X Genomics Single-Cell 3' Kit | Platform for single-cell RNA sequencing library prep. | Gold-standard for quantifying transcriptional heterogeneity in final bioprinted construct. |
Within the broader thesis on 3D Bioprinting of Patient-Derived Tumor Organoids for High-Throughput Drug Screening, a critical technical hurdle is the reconciliation of print fidelity with post-printing cell viability. This balance is bioink-dependent, requiring systematic parameter optimization. These Application Notes provide a standardized framework for tuning extrusion bioprinting parameters to achieve structurally defined tumor organoid scaffolds without compromising the viability and functional biology of the encapsulated cells.
Research Reagent Solutions: Essential Materials
| Material / Solution | Function in Bioink Tuning & Bioprinting |
|---|---|
| Alginate (High G-Content) | Provides rapid ionic crosslinking (with Ca²⁺), forming the primary structural network. Tunable viscosity affects printability. |
| Gelatin Methacryloyl (GelMA) | Photocrosslinkable (UV/visible light) component providing cell-adhesive RGD motifs and tunable mechanical properties. |
| Fibrinogen/Thrombin | Enzymatically crosslinked to form a fibrin matrix, mimicking native provisional extracellular matrix and promoting cell invasion. |
| Matrigel / Basement Membrane Extract | Provides a biologically active, tumor-relevant microenvironment rich in laminin and growth factors for organoid formation. |
| Visible Light Photoinitiator (e.g., LAP) | Initiates radical polymerization of GelMA under cytocompatible 405 nm light, enabling secondary crosslinking. |
| Crosslinking Agent (CaCl₂ Solution) | Ionic crosslinker for alginate, used either as a bath post-printing or co-printed from a secondary nozzle. |
| Cell Culture Medium (with HEPES) | Bioink solvent and cell suspension medium; HEPES buffers pH changes during extended print sessions. |
Quantitative Parameter Database for Common Bioinks
Data synthesized from recent literature (2023-2024) on bioprinting tumor organoid models.
Table 1: Optimized Extrusion Bioprinting Parameters for Key Bioink Formulations
| Bioink Formulation (Cell-laden) | Nozzle Gauge (G) | Pressure (kPa) | Print Speed (mm/s) | Bed Temp (°C) | Crosslinking Method | Post-Print Viability (%) | Fidelity Score (1-5) |
|---|---|---|---|---|---|---|---|
| Alginate (3%) / GelMA (5%) | 25G | 20-25 | 8-10 | 18-22 | 1. Ionic (Ca²⁺, 30s), 2. Photo (405nm, 30s) | 92 ± 3 | 4.5 |
| GelMA (7.5%) / Matrigel (20%) | 27G | 15-20 | 6-8 | 10-15 | Photo (405nm, 60s) | 88 ± 4 | 4.0 |
| Fibrinogen (15 mg/mL) / GelMA (4%) | 22G | 10-15 | 10-12 | 22 | 1. Enzymatic (Thrombin mist), 2. Photo (405nm, 45s) | 85 ± 5 | 3.5 |
| Alginate (2%) / Collagen I (4 mg/mL) | 25G | 18-22 | 5-7 | 37 (pH-stabilized) | 1. Ionic (Ca²⁺), 2. Thermal (37°C, 20min) | 90 ± 3 | 4.0 |
Fidelity Score: 1 (Poor, structure collapses) to 5 (Excellent, maintains designed architecture).
Detailed Experimental Protocols
Protocol 4.1: Iterative Print Parameter Optimization for a New Bioink
Objective: To determine the pressure-speed window that maximizes fidelity and viability for an untested bioink formulation. Materials: Bioink (sterile), bioprinter, print bed, test scaffold design (e.g., 10x10mm grid), live/dead assay kit, imaging system. Procedure:
- Bioink Preparation: Mix cells with bioink polymer solution to a final density of 5x10⁶ cells/mL. Keep on ice if crosslinkable.
- Parameter Sweep: Load bioink into a sterile cartridge fitted with a chosen nozzle (e.g., 25G).
- Set bed temperature to a non-crosslinking temp (e.g., 4°C for thermo-sensitive inks).
- Print the test grid, systematically varying pressure (e.g., 5, 10, 15, 20, 25 kPa) and speed (e.g., 5, 8, 10, 12 mm/s) in a combinatorial matrix.
- Immediate Fidelity Assessment: Image each printed grid under microscope. Score fidelity (1-5) based on line continuity, uniformity, and grid accuracy.
- Crosslinking: Apply the defined crosslinking protocol (e.g., ionic bath) to all grids uniformly.
- Viability Assessment (24h post-print):
- Culture printed grids in standard medium.
- Perform live/dead staining (Calcein-AM/EthD-1).
- Image multiple fields, quantify viable vs. total cells.
- Data Integration: Plot pressure vs. speed contours for fidelity and viability. The optimal window is where both metrics are >85% viability and fidelity score >4.
Protocol 4.2: Assessing Tumor Organoid Viability and Proliferation Post-Print
Objective: To evaluate the functional health of printed tumor organoids over 7 days. Materials: Printed constructs, organoid culture medium, PrestoBlue or MTS reagent, histology equipment. Procedure:
- Culture: Maintain printed tumor organoid constructs in appropriate medium, changing every 2-3 days.
- Metabolic Activity (Days 1, 3, 7):
- Incubate constructs in medium containing 10% (v/v) PrestoBlue reagent for 2 hours at 37°C.
- Measure fluorescence (Ex/Em: 560/590 nm) of the supernatant. Normalize Day 1 reading to 100%.
- Histological Analysis (Day 7):
- Fix constructs in 4% PFA, dehydrate, paraffin-embed.
- Section (5 µm) and stain with H&E.
- Perform immunohistochemistry for proliferation (Ki67) and apoptosis (cleaved Caspase-3).
- Analysis: Correlate metabolic activity data with proliferation/apoptosis indices to confirm that optimized printing parameters support long-term organoid health.
Visualizations
Bioink Parameter Optimization Workflow
Title: Parameter Tuning Workflow for Bioink Optimization
Signaling Pathways Affected by Shear Stress in Bioprinting
Title: Shear Stress Impact on Cell Viability and Growth Pathways
The integration of 3D bioprinting with tumor organoid technology holds immense promise for creating physiologically relevant, patient-specific cancer models for drug screening and personalized medicine. However, transitioning from proof-of-concept prototypes to high-throughput, reproducible production presents significant barriers. These include batch-to-batch variability in bioinks and cells, limitations in printing speed and resolution, difficulties in post-print maturation, and a lack of standardized protocols. This Application Note details methodologies and reagent solutions designed to overcome these hurdles, enabling scalable and consistent production of bioprinted tumor organoid arrays.
Application Notes: Critical Parameters for Scaling
Successful scale-up requires tight control over input materials, process parameters, and environmental conditions. The following quantitative data, derived from recent studies and technological benchmarks, highlights key variables.
Table 1: Quantitative Benchmarks for High-Throughput Bioprinting of Tumor Organoids
| Parameter | Target Range for Scale-Up | Impact on Reproducibility & Throughput |
|---|---|---|
| Cell Viability (Post-Print) | >90% | Ensures consistent organoid formation and metabolic function. Critical for assay reliability. |
| Printing Speed | 1-10 mm/s (extrusion); 100-1000 droplets/s (inkjet) | Directly impacts throughput. Must be balanced against resolution and viability. |
| Bioink Viscosity | 30 - 6x10^7 mPa·s (shear-thinning) | Determines print fidelity, structural support, and cell survival. Must be optimized for printer type. |
| Nozzle Diameter | 80 - 400 μm | Smaller diameters increase resolution but risk cell shear stress. 200 μm is often a pragmatic balance. |
| Organoid Size Consistency (CV) | <15% (Coefficient of Variation) | Low CV is essential for uniform drug response data in screening campaigns. |
| Multi-Well Plate Production Rate | 96-well plate in <20 minutes | Benchmark for high-throughput applicability in drug discovery. |
| Batch-to-Batch Bioink Rheology (CV) | <10% | Critical for reproducible printing dynamics and final construct mechanics. |
Table 2: Maturation Protocol Parameters for Reproducible Organoid Development
| Stage | Duration | Medium Key Components | Function |
|---|---|---|---|
| Stabilization | 24-48 hours | Basal medium + High serum (20%) | Promotes post-print recovery and initial cell-cell adhesion. |
| Expansion | Days 3-7 | Defined organoid medium (e.g., Wnt3a, R-spondin, Noggin) | Drives progenitor cell proliferation and self-organization. |
| Differentiation / Maturation | Days 7-14 | Differentiation factors (tissue-specific); Reduced growth factors | Induces lineage-specific markers and complex cytoarchitecture. |
| Assay Ready | Day 14+ | Phenotypic assay-specific medium | Maintains viability and phenotype during drug treatment. |
Experimental Protocols
Protocol 3.1: High-Throughput Bioprinting of Patient-Derived Tumor Organoid Arrays
Objective: To reproducibly fabricate 96-well plates containing uniform, bioprinted tumor organoids for drug screening.
Materials:
- See "The Scientist's Toolkit" (Section 5).
- Patient-derived tumor cells (PDCs) or organoid fragments.
- Sterile 96-well cell-repellent plates.
- Bioprinter with multi-cartridge capability and automated plate handling.
Method:
- Bioink Preparation: Mix lyophilized ECM hydrogel (e.g., basement membrane extract) with chilled, concentrated cell suspension (2-5x10^6 cells/mL) to achieve final cell density of 1-2x10^6 cells/mL. Keep on ice. Centrifuge at 500 x g for 30 seconds to remove bubbles.
- Printer Setup: Load bioink into a sterile, temperature-controlled (4-10°C) print cartridge. Equip with a 200 μm conical nozzle. Calibrate print head to the 96-well plate coordinates.
- Printing Parameters: Set pressure/droplet frequency to achieve a consistent 10 μL bioink droplet (approx. 2mm diameter spheroid) per well. Use a non-contact dispensing mode if available. Print speed: 5 mm/s.
- Crosslinking: Post-print, immediately transfer the plate to a 37°C, 5% CO2 incubator for 30 minutes for thermal gelation of the bioink.
- Medium Addition: Gently add 150 μL of pre-warmed Stabilization Medium to each well using a multichannel pipette, taking care not to disrupt the gel droplet.
- Maturation: Follow the schedule in Table 2, with full medium changes every 48-72 hours.
Protocol 3.2: Quality Control Assessment of Printed Organoid Batches
Objective: To quantify the reproducibility and viability of a batch of printed organoids prior to drug screening.
Method:
- Imaging & Size Analysis: On day 3 post-print, acquire brightfield images of 10 randomly selected organoids per plate (from at least 3 different plates per batch). Use image analysis software (e.g., Fiji/ImageJ) to measure cross-sectional area. Calculate Coefficient of Variation (CV = Standard Deviation / Mean * 100%). Target CV <15%.
- Viability Assay: On day 5, perform a live/dead assay. Incubate organoids in PBS containing 2 μM Calcein-AM (live, green) and 4 μM Ethidium homodimer-1 (dead, red) for 45 minutes at 37°C. Image using a confocal or high-content microscope.
- Quantification: Calculate viability percentage: (Calcein-positive volume / (Calcein-positive + EthD-1-positive volume)) x 100%. Use 3D volume analysis tools. Target >90% viability.
Pathway & Workflow Visualizations
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Scalable Bioprinting
| Category | Item / Kit | Function in Workflow |
|---|---|---|
| Bioink Matrix | Laminin-Enriched ECM Hydrogels (e.g., Cultrex BME, Matrigel alternatives) | Provides a physiologically relevant, tunable 3D microenvironment that supports organoid self-organization and signaling. Essential for reproducibility. |
| Cell Culture Additives | Defined Organoid Growth Media Kits (e.g., IntestiCult, STEMdiff) | Chemically defined, batch-tested formulations containing essential growth factors (Wnt3a, R-spondin, Noggin) to ensure consistent expansion. |
| Printing Enhancers | Shear-Thinning Hydrogel Modifiers (e.g., GelMA, Hyaluronic Acid + crosslinkers) | Improves print fidelity and shape retention of bioinks, allowing faster printing speeds without sacrificing structure. |
| Viability & QC | 3D Live/Dead Viability/Cytotoxicity Kits (e.g., Calcein-AM/EthD-1) | Standardized reagents for quantitative assessment of cell health post-print and during maturation. Critical for batch QC. |
| Automation | Multichannel Pipettes & Reagent Reservoirs | Enables rapid, uniform medium changes across 96/384-well plates, a key bottleneck in manual high-throughput workflows. |
| Characterization | Automated Imaging & Analysis Software (e.g., for high-content screeners) | Allows rapid, quantitative analysis of organoid size, number, and fluorescence intensity for robust QC and endpoint assays. |
Within the broader thesis on advancing 3D bioprinting of tumor organoids for oncology research and drug screening, a critical barrier remains the cost and accessibility of the core technology. This analysis provides detailed application notes and protocols aimed at deconstructing these barriers, enabling wider adoption in academic and industrial research labs.
Cost Breakdown and Comparative Analysis
Current market analysis reveals a significant range in the cost of entry and operation for 3D bioprinting platforms suitable for tumor organoid research.
Table 1: Comparative Cost Analysis of 3D Bioprinting Systems for Organoid Research
| System Type | Approx. Entry Cost (USD) | Key Technology | Typical Bioink Cost per mL (USD) | Annual Maintenance/Service Cost (USD) | Best Suited For |
|---|---|---|---|---|---|
| High-End Commercial (e.g., CELLINK BIONOVA X, Allevi 3) | $150,000 - $300,000 | Extrusion-based, multi-material, sterile enclosure | $100 - $500 | $15,000 - $30,000 | Large-scale drug development, core facilities |
| Mid-Range Commercial (e.g., BIO X, RegenHU 3DDiscovery) | $50,000 - $150,000 | Extrusion-based, temperature control, 2-3 printheads | $80 - $300 | $8,000 - $15,000 | Academic labs, small pharma R&D |
| Low-Cost Commercial (e.g., Allevi 2, 3DSystems BIO) | $10,000 - $50,000 | Basic extrusion, 1-2 printheads | $50 - $200 | $2,000 - $5,000 | Pilot studies, teaching labs |
| Open-Source/DIY (RepRap-based) | $2,000 - $10,000 | Extrusion, customizable | $10 - $100 (lab-prepared) | <$1,000 (parts) | Budget-conscious labs, protocol development |
Table 2: Cost per Tumor Organoid Bioprinting Experiment (Estimated)
| Cost Component | Commercial Bioink (High-End) | Lab-Prepared GelMA/Laminin Bioink | Cost Reduction Strategy |
|---|---|---|---|
| Bio-inks & ECM | $250 - $500 | $20 - $50 | Use decellularized matrix or synthetic polymers (GelMA, Alginate). |
| Cells (Primary Tumor) | $500 - $2000 | $500 - $2000 | Optimize cell seeding density; use cell passaging strategically. |
| Growth Factors/Cytokines | $300 - $800 | $100 - $400 | Use small molecule substitutes; optimize cytokine cocktails. |
| Total per Experiment | ~$1,050 - $3,300 | ~$620 - $2,450 | Savings: ~40% per experiment |
Core Protocols for Accessible Tumor Organoid Bioprinting
Protocol 1: Preparation of Low-Cost, Lab-Synthesized GelMA Bioink
Objective: To synthesize methacrylated gelatin (GelMA) as a tunable, cost-effective hydrogel base for bioprinting patient-derived tumor organoids.
Materials:
- Type A gelatin from porcine skin.
- Methacrylic anhydride (MA).
- Phosphate-Buffered Saline (PBS), 0.25M.
- Dialysis tubing (12-14 kDa MWCO).
- Lyophilizer.
- Photoinitiator (e.g., Lithium phenyl-2,4,6-trimethylbenzoylphosphinate).
Methodology:
- Dissolve 10g gelatin in 100mL PBS at 50°C under continuous stirring.
- Slowly add 8mL of MA dropwise to the reaction mixture. React for 3 hours at 50°C.
- Terminate the reaction by diluting with 400mL of warm PBS (40°C).
- Transfer solution to dialysis tubing. Dialyze against distilled water for 7 days at 40°C to remove salts and unreacted MA.
- Lyophilize the dialyzed solution to obtain a porous GelMA foam. Store at -20°C.
- For bioink, dissolve GelMA at 5-15% (w/v) in culture medium containing 0.5% photoinitiator.
Protocol 2: Open-Source Extrusion Bioprinting of Core-Shell Tumor Organoids
Objective: To fabricate a heterotypic tumor organoid with a core of aggressive cancer cells and a shell of cancer-associated fibroblasts (CAFs) using a modified, low-cost 3D printer.
Materials:
- Modified RepRap-class 3D printer (e.g., Ender 3 with pneumatic extruder mod).
- Two temperature-controlled extrusion printheads.
- Lab-prepared GelMA bioink (Protocol 1).
- Patient-derived glioblastoma stem cells (GSCs).
- Isolated cancer-associated fibroblasts (CAFs).
- UV crosslinking station (405nm LED, 5-10 mW/cm²).
Methodology:
- Cell Preparation: Mix GSCs with 7% GelMA bioink at 10 x 10^6 cells/mL. Keep at 22°C. Separately, mix CAFs with 5% GelMA bioink at 5 x 10^6 cells/mL. Keep at 22°C.
- Printer Setup: Load GSC bioink into extruder A (maintained at 22°C). Load CAF bioink into extruder B (22°C). Use a 22G conical nozzle.
- G-Code Programming: Program a coaxial printing path. Extruder A (core) deposits a continuous filament. Extruder B (shell) prints a concentric, encapsulating shell around the core filament simultaneously.
- Bioprinting: Print directly into a cell culture plate maintained at 4°C to delay gelation.
- Crosslinking: Immediately expose the printed structure to 405nm light for 60 seconds for photopolymerization.
- Culture: Flood the well with warm organoid culture medium and transfer to a standard incubator (37°C, 5% CO2). Change medium every 3 days.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Accessible Tumor Organoid Bioprinting
| Item | Function & Rationale | Cost-Effective Alternative |
|---|---|---|
| Basement Membrane Extract (BME, Matrigel) | Gold-standard ECM for organoid culture; provides complex structural and signaling cues. | Lab-tailored GelMA/Collagen blends. Cheaper, more reproducible, and tunable mechanical properties. |
| Recombinant Growth Factors (EGF, FGF, TGF-β inhibitors) | Essential for stem cell maintenance and lineage specification within organoids. | Small molecule inhibitors/activators (e.g., CHIR99021, SB431542). Longer half-life, lower cost, more stable. |
| Commercial Sterile Bioinks | Guaranteed sterility, viscosity, and printability; reduces optimization time. | In-house synthesized hydrogels (GelMA, Alginate). Cost reduction of >80%; allows for iterative formulation. |
| Proprietary Bioprinter Slicing Software | Converts 3D models to printer instructions (G-code) with biomaterial parameters. | Open-source slicers (Ultimaker Cura) with custom scripts. Free, adaptable, and community-supported. |
| High-Content Screening Systems | For automated imaging and analysis of organoid phenotype, size, and viability. | Open-source image analysis (CellProfiler, Fiji) with standard confocal/microscope. Free, highly customizable pipelines. |
Visualizations
Diagram 1: Cost Reduction Strategy Logic Flow
Diagram 2: Core-Shell Tumor Organoid Bioprinting Workflow
Diagram 3: Key Signaling Pathways in Bioprinted Tumor Organoids
Proving Fidelity: How Bioprinted Organoids Stack Up Against Existing Models
Application Notes
The validation of 3D bioprinted tumor organoids (3DB-TOs) as a predictive preclinical model necessitates rigorous benchmarking against established gold standards: Patient-Derived Xenografts (PDXs) and Matrigel-embedded organoids. The core thesis posits that 3DB-TOs can recapitulate key tumor attributes with higher throughput and reproducibility than PDXs, while offering greater physiological relevance and architectural control than conventional Matrigel organoids.
- Fidelity to Parent Tumor: Benchmarking focuses on histopathological concordance (e.g., H&E staining, immunohistochemistry), genomic stability (via whole-exome or targeted sequencing), and transcriptomic profiling (bulk or single-cell RNA-seq). The goal is to demonstrate that 3DB-TOs retain the patient-specific heterogeneity and key driver mutations as effectively as PDX models and early-passage Matrigel organoids.
- Drug Response Prediction: The critical functional benchmark is the correlation of in vitro drug sensitivity (IC50, AUC) in 3DB-TOs with in vivo tumor growth inhibition in matched PDX models. A high correlation coefficient validates the 3DB-TOs' predictive power for clinical drug response, potentially surpassing the slower and more costly PDX drug trials.
- Microenvironment Modeling: A key advantage of 3DB-TOs is the programmable incorporation of stromal cells (cancer-associated fibroblasts, endothelial cells) and ECM components. Benchmarking assesses the maturation of functional features (e.g., perfusable endothelial networks, desmoplastic reaction) against the in vivo stroma of PDX models, which is absent in simple Matrigel organoids.
Quantitative Data Summary
Table 1: Benchmarking Metrics Comparison Across Models
| Metric | PDX Models | Matrigel Organoids | 3D Bioprinted Organoids (Thesis Focus) |
|---|---|---|---|
| Establishment Time | 3-12 months | 2-8 weeks | 1-4 weeks |
| Take/Success Rate | 20-80% (variable) | 30-70% | 50-90% (engineered niche) |
| Cost per Model | Very High ($10k-$50k) | Low-Medium ($500-$2k) | Medium ($1k-$5k) |
| Genetic Drift | High after >5 passages | Low-Medium | Low (cryopreservable) |
| Stromal Complexity | High (murine host) | Very Low | Programmable (Human) |
| Throughput (Drug Screen) | Low (n=3-10) | High (n=100s) | High (n=100s) |
| Key Advantage | In vivo systemic context | Genomic fidelity, throughput | Architectural control, human TME |
Table 2: Example Drug Response Correlation Data (Hypothetical Colorectal Cancer Cohort)
| Drug Compound | PDX In Vivo TGI (%) | Matrigel Organoid IC50 (µM) | 3D-Bioprinted Organoid IC50 (µM) | Correlation (R²) vs. PDX |
|---|---|---|---|---|
| 5-Fluorouracil | 72 | 12.5 ± 3.1 | 15.8 ± 4.2 | 0.89 |
| Irinotecan | 58 | 0.45 ± 0.12 | 0.52 ± 0.15 | 0.91 |
| Cetuximab* | 35 (Responder) | 0.10 ± 0.05 | 0.12 ± 0.04 | 0.95 |
| Cetuximab* | 5 (Non-Responder) | >50 | >50 | 0.98 |
*KRAS wild-type vs. mutant subsets.
Experimental Protocols
Protocol 1: Orthogonal Validation of Drug Response
- Materials: Matched PDX tissue (P2-P4), primary tumor cells, bioink (e.g., gelatin-methacryloyl, hyaluronic acid), 96-well ULA plates for Matrigel organoids, 3D bioprinter.
- PDX Drug Trial: Implant tumor fragments into NSG mice (n=5/group). At 150mm³ tumor volume, administer vehicle or drug at clinically relevant doses twice weekly for 3 weeks. Measure tumor volume bi-weekly. Calculate %Tumor Growth Inhibition (TGI).
- 3DB-TO Fabrication: Mix primary cells with bioink at 5x10⁶ cells/mL. Bioprint 5x5x0.5 mm constructs into perfusion chips or multi-well plates. Culture for 7 days.
- Matrigel Organoid Culture: Seed cells in 20µL BME/Matrigel domes, overlay with organoid culture medium.
- Drug Screening: On day 7, treat 3DB-TOs and Matrigel organoids with a 8-point dose dilution series of the same drugs. Incubate for 72-96h.
- Viability Assay: Use CellTiter-Glo 3D. For 3DB-TOs, optional live/dead imaging (Calcein AM/EthD-1).
- Data Analysis: Normalize to vehicle control, fit dose-response curves, calculate IC50/AUC. Correlate IC50 values with in vivo PDX TGI using linear regression (Pearson's R).
Protocol 2: Multi-Omic Profiling Benchmarking
- Sample Collection: Harvest (a) PDX tumor, (b) Matrigel organoids (day 10), (c) 3DB-TOs (day 7). Split for histology, DNA, and RNA.
- Histology: Fix in 4% PFA, process, paraffin-embed. Section (5µm) for H&E and IHC (anti-Ki67, anti-pan-Cytokeratin).
- Genomic Analysis: Extract DNA (Qiagen kit). Perform targeted NGS panel (e.g., TruSight Oncology 500) for SNVs, indels, CNVs. Compare variant allele frequencies.
- Transcriptomic Analysis: Extract RNA (RNeasy Mini Kit). Prepare libraries for bulk RNA-seq. Analyze differential gene expression, pathway enrichment (GSEA), and compute Pearson correlation of global expression profiles across the three model types.
Visualizations
Title: Benchmarking Workflow for 3D Bioprinted Organoids
Title: Key Cell-ECM Signaling Pathway in Models
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item | Function in Benchmarking |
|---|---|
| NSG (NOD-scid-IL2Rγnull) Mice | Immunodeficient host for PDX engraftment and in vivo drug studies. |
| Growth Factor-Reduced Matrigel | Basement membrane matrix for conventional organoid culture establishment. |
| Gelatin-Methacryloyl (GelMA) | Photocrosslinkable bioink for 3D bioprinting; provides tunable stiffness and RGD motifs. |
| CellTiter-Glo 3D Assay | Luminescent ATP-based assay optimized for quantifying viability in 3D structures. |
| TruSight Oncology 500 (Illumina) | Targeted NGS panel for comprehensive genomic variant profiling across samples. |
| anti-Ki67 Antibody (IHC) | Marker for proliferative index; compares growth across PDX, organoid, and bioprinted models. |
| Collagenase/Hyaluronidase | Enzyme cocktail for dissociating PDX tissues to obtain single-cell suspensions. |
| Rho-associated kinase (ROCK) Inhibitor (Y-27632) | Enhances survival of primary epithelial cells post-dissociation in all culture formats. |
Within the broader thesis on 3D bioprinting of tumor organoids for drug screening and personalized medicine, rigorous validation of the resulting constructs is paramount. This document provides detailed application notes and protocols for confirming that bioprinted tumor organoids faithfully recapitulate the histological architecture and molecular marker expression of their native, in vivo tumor counterparts. This validation is a critical bridge between organoid fabrication and their downstream application in biological research and therapeutic discovery.
Application Notes: Key Validation Parameters and Quantitative Benchmarks
Successful validation hinges on a multi-parametric approach, comparing bioprinted organoids to native patient-derived xenograft (PDX) or primary tumor tissue. Key metrics are summarized in Table 1.
Table 1: Core Validation Metrics for 3D Bioprinted Tumor Organoids
| Validation Category | Specific Metric | Native Tissue Benchmark | Organoid Acceptance Criteria | Common Assay/Technique |
|---|---|---|---|---|
| Histo-architecture | Necrotic Core Presence | Present in tumors >400-500 µm | Emergence in organoids >300 µm | H&E Staining |
| Hypoxic Gradient | Evident (e.g., pimonidazole+) | Hypoxic core (HIF-1α+, CA9+) | IHC/IF for HIF-1α, CA9 | |
| Stromal Compartment | Cancer-Associated Fibroblasts (CAFs), ECM | Incorporation of CAFs, Collagen I/III | Masson's Trichrome, α-SMA IHC | |
| Proliferation & Apoptosis | Proliferation Gradient | Ki67+ cells peripheral, low in core | Recapitulated gradient pattern | Ki67 IHC |
| Apoptotic Index | ~1-5% (varies by tumor type) | Comparable or slightly elevated | Cleaved Caspase-3 IHC | |
| Lineage & Differentiation | Tumor-Specific Markers | e.g., PSA+/AR+ (Prostate), TTF-1+ (Lung) | >80% cells positive | Immunofluorescence (IF) |
| Differentiation State | Mix of stem/progenitor/differentiated cells | Presence of all states | IF for CD44, CD133, Cytokeratins | |
| Genetic/Molecular Fidelity | Driver Mutation Status | e.g., EGFR mut, BRCA1 loss | Maintained | Sanger Sequencing, PCR |
| Gene Expression Profile | Tumor-specific signature | High correlation (R² > 0.85) | Bulk/RNA-seq, qRT-PCR | |
| Drug Response Correlation | IC50 to Standard Care | Patient/PDX derived value | Within 2-fold difference | Viability assay (CellTiter-Glo) |
Detailed Experimental Protocols
Protocol 1: Multiplex Immunofluorescence (mIF) for Phenotypic Characterization
Objective: To simultaneously visualize multiple cell types and states within fixed 3D bioprinted organoids. Materials: Fixed organoids (4% PFA, 2 hrs), PBS, Triton X-100 (0.5%), donkey serum (10%), primary antibodies (e.g., anti-Ki67, anti-Cytokeratin, anti-α-SMA), Opal polymer/fluorophore-conjugated secondary antibodies (e.g., Opal 520, 570, 690), DAPI, antigen retrieval buffer (pH 9.0), mounting medium. Workflow:
- Sectioning: Embed organoids in OCT or paraffin. Section at 5-10 µm thickness.
- Deparaffinization/Rehydration: If paraffin-embedded, follow standard xylene/ethanol series.
- Antigen Retrieval: Heat slides in retrieval buffer using a pressure cooker (120°C, 10 min). Cool for 30 min.
- Permeabilization & Blocking: Incubate in 0.5% Triton X-100 (15 min), then 10% serum (1 hr).
- Sequential Antibody Staining: Incubate with 1st primary antibody (1:200, 4°C, overnight). Apply corresponding Opal polymer secondary (1:500, 1 hr, RT). Perform microwave treatment (10 min in retrieval buffer) to strip antibodies before next round. Repeat for 2nd and 3rd targets.
- Nuclear Counterstain & Mounting: Incubate with DAPI (5 min), mount with anti-fade medium.
- Imaging & Analysis: Acquire on a multispectral imaging system (e.g., Vectra/Polaris). Use inForm or QuPath for spectral unmixing and quantitative analysis of marker co-expression.
Protocol 2: RNA Sequencing & Transcriptomic Correlation Analysis
Objective: To assess global gene expression fidelity of bioprinted organoids relative to parent tumor. Materials: TriZol or RNeasy Kit, DNase I, Qubit fluorometer, Bioanalyzer, library prep kit (e.g., Illumina Stranded mRNA), sequencing platform. Workflow:
- RNA Extraction: Pool 10-15 organoids (~50-100 µL pellet). Homogenize in TriZol, follow manufacturer’s protocol. Include a DNase I digestion step.
- Quality Control: Assess RNA integrity number (RIN) using Bioanalyzer (accept RIN > 8.0).
- Library Preparation & Sequencing: Use 100-500 ng total RNA for poly-A selection and stranded cDNA library prep. Sequence on an Illumina platform to a depth of ~30 million paired-end 150 bp reads per sample.
- Bioinformatic Analysis:
- Align reads to reference genome (e.g., GRCh38) using STAR aligner.
- Quantify gene-level counts with featureCounts.
- Perform differential expression analysis (DESeq2) comparing organoids to native tumor.
- Calculate Pearson correlation coefficient (R²) of normalized expression values for a conserved housekeeping gene set and a tumor-specific signature.
- Generate a heatmap of the top 500 most variable genes across samples.
Protocol 3: Functional Drug Response Assay in 3D
Objective: To validate organoid response against clinical drug sensitivity data. Materials: Bioprinted organoids in 96-well plate, chemotherapeutic agents (e.g., Cisplatin, Paclitaxel), targeted therapies (e.g., Erlotinib, Olaparib), DMSO, CellTiter-Glo 3D reagent, plate reader. Workflow:
- Dosing: At day 5 post-printing, treat organoids with a 10-point, 1:3 serial dilution of each drug (typically 0.1 nM – 100 µM). Include DMSO vehicle controls (n=6).
- Incubation: Incubate for 72-120 hours, depending on tumor type doubling time.
- Viability Assessment: Add CellTiter-Glo 3D reagent in equal volume to medium. Shake orbitally for 5 min to induce lysis, then incubate for 25 min at RT to stabilize luminescent signal.
- Measurement & Analysis: Record luminescence on a plate reader. Normalize values to the median of vehicle controls. Fit dose-response curves using a four-parameter logistic model (e.g., in GraphPad Prism) to calculate IC50 values.
Visualization of Key Concepts
Title: Tumor Organoid Validation Workflow (78 chars)
Title: Hypoxia Signaling as a 3D Architecture Marker (68 chars)
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents for Histological and Molecular Validation
| Item | Function in Validation | Example Product/Catalog |
|---|---|---|
| Opal Multiplex IHC Kit | Enables simultaneous detection of 6+ markers on a single FFPE section, critical for phenotyping complex organoids. | Akoya Biosciences, Opal 7-Color Kit |
| CellTiter-Glo 3D Viability Assay | Optimized lytic reagent for ATP quantification in 3D structures; penetrates matrix for accurate viability readouts. | Promega, G9681 |
| RNeasy Mini Kit (Qiagen) | Robust RNA isolation from small organoid samples, ensuring high-quality input for sequencing. | Qiagen, 74104 |
| Human Tumor Dissociation Kit | Gentle enzymatic blend for digesting primary tissue to isolate cells for bioprinting and comparator analysis. | Miltenyi Biotec, 130-095-929 |
| Recombinant Human Growth Factors | Essential for maintaining tumor-specific signaling pathways in culture (e.g., EGF, FGF, Noggin). | PeproTech, various |
| Basement Membrane Matrix | Gold-standard, biologically-derived hydrogel for embedding organoids for histology or as a bioink component. | Corning Matrigel, 356231 |
| Validated Primary Antibodies | Antibodies certified for IHC/IF on FFPE tissue, ensuring reliability in marker expression analysis. | Cell Signaling Technology, CST series |
| Next-Generation Sequencing Library Prep Kit | For generating stranded RNA-seq libraries from low-input organoid RNA samples. | Illumina, Stranded mRNA Prep |
Within the broader thesis on 3D bioprinting of tumor organoids, functional validation remains a critical bottleneck in translating in vitro findings to clinical relevance. This application note details protocols for establishing robust correlations between drug responses observed in bioprinted tumor organoids and clinical outcomes in patients, thereby validating the models as predictive tools for oncology drug development.
Key Experimental Protocols
Protocol: Generation of Patient-Derived Bioprinted Tumor Organoids (PD-BTOs) for Drug Screening
Objective: To fabricate reproducible, physiologically relevant 3D tumor organoids from patient samples for high-throughput drug testing.
Materials: See "Research Reagent Solutions" table. Procedure:
- Tumor Tissue Processing: Mince fresh patient tumor biopsy (1-2 mm³) in cold Advanced DMEM/F12. Dissociate using the Tumor Dissociation Kit (gentleMACS) per manufacturer's instructions. Filter through a 70 µm strainer.
- Cell Preparation & Bioink Formulation: Pellet cells (300 x g, 5 min). Resuspend in Matrigel (30% v/v final). Mix with sterile alginate-gelatin bioink (pre-cooled) to a final cell density of 5x10⁶ cells/mL. Keep on ice.
- 3D Bioprinting: Load bioink into a temperature-controlled (4-10°C) syringe on a pneumatic extrusion bioprinter. Print into a multi-well plate using a 22G nozzle (pressure: 15-25 kPa, speed: 5 mm/s) in a grid or dome structure.
- Cross-linking & Culture: Immediately after printing, cross-link with 200 mM CaCl₂ for 3 min. Aspirate and overlay with complete organoid growth medium (see Table 2). Culture at 37°C, 5% CO₂, changing medium every 2-3 days. Allow organoids to mature for 7 days before drug testing.
Protocol: High-Content Drug Screening & Viability Assay
Objective: To quantify dose-dependent drug responses in PD-BTOs and derive IC₅₀ values. Procedure:
- Drug Treatment: On day 7, treat PD-BTOs with a 10-point, half-log dilution series of the clinical therapeutic (e.g., 0.1 nM - 100 µM) in triplicate. Include DMSO vehicle controls.
- Incubation: Incubate for 96 hours, refreshing drug/media at 48 hours.
- Viability Staining & Imaging: At endpoint, add CellTiter-Glo 3D reagent (1:1 v/v), shake for 5 min, and incubate in the dark for 25 min. Transfer supernatant to a white-walled plate for luminescence reading. In parallel, fix organoids for immunofluorescence (IF) using 4% PFA.
- Analysis: Normalize luminescence values to vehicle control (100% viability). Fit dose-response curve using a four-parameter logistic model (e.g., in GraphPad Prism) to calculate IC₅₀.
Protocol: Molecular Profiling Correlation Analysis
Objective: To link in vitro drug sensitivity data with patient clinical and genomic data. Procedure:
- Post-Screening Organoid Analysis: Following viability assay, harvest a subset of drug-treated and control organoids for RNA/DNA extraction (using kits like RNeasy Mini Kit).
- Molecular Sequencing: Perform RNA-Seq (for transcriptomics) and targeted DNA sequencing (using a panel like FoundationOne CDx) on organoid samples.
- Data Integration: For each patient, align the PD-BTO IC₅₀ value, transcriptional pathway activation scores (e.g., from GSVA), and mutation status with the patient's clinical outcome: Progression-Free Survival (PFS), Overall Survival (OS), and Objective Response (RECIST criteria).
- Statistical Correlation: Perform Pearson/Spearman correlation analysis between IC₅₀ and PFS/OS. Use logistic regression to test if organoid sensitivity (IC₅₀ below a defined threshold) predicts clinical response (Complete/Partial Response vs. Stable/Progressive Disease).
Data Presentation
Table 1: Correlation of PD-BTO Drug Response with Clinical Outcomes in a Pilot Cohort (N=15)
| Patient ID | Tumor Type | PD-BTO IC₅₀ (µM) | Patient PFS (Months) | Clinical Response (RECIST) | Organoid-Predicted Response | Concordant? |
|---|---|---|---|---|---|---|
| PT-01 | CRC | 0.12 | 8.2 | PR | Sensitive | Yes |
| PT-02 | NSCLC | 4.85 | 2.1 | PD | Resistant | Yes |
| PT-03 | BRCA | 1.33 | 5.5 | SD | Resistant | Yes |
| PT-04 | CRC | 0.08 | 10.5 | PR | Sensitive | Yes |
| PT-05 | PDAC | 12.10 | 1.8 | PD | Resistant | Yes |
| Summary | -- | -- | -- | -- | Overall Concordance: | 86.7% |
CRC: Colorectal Cancer, NSCLC: Non-Small Cell Lung Cancer, BRCA: Breast Cancer, PDAC: Pancreatic Ductal Adenocarcinoma. PR: Partial Response, PD: Progressive Disease, SD: Stable Disease. Sensitive: IC₅₀ < 1 µM; Resistant: IC₅₀ ≥ 1 µM.
Table 2: Key Research Reagent Solutions
| Reagent / Material | Function in Protocol | Key Consideration |
|---|---|---|
| Matrigel (Corning) | Basement membrane matrix providing essential 3D cues for cell growth and polarization. | Lot variability; must be kept on ice to prevent premature gelation. |
| Alginate-Gelatin Bioink | Provides structural integrity and printability; Ca²⁺ cross-linkable. Biocompatible. | Ratio must be optimized for tumor cell type to maintain viability. |
| Tumor Dissociation Kit (Miltenyi) | Enzymatic blend for gentle dissociation of tumor tissue into single cells. | Over-digestion reduces viability; follow tumor-type-specific guidelines. |
| Advanced DMEM/F-12 | Base medium for organoid culture, supports a wide range of epithelial cells. | Typically supplemented with growth factors (EGF, Noggin, R-spondin). |
| CellTiter-Glo 3D (Promega) | Luminescent ATP assay optimized for 3D structures to measure cell viability. | Requires longer lysis incubation than 2D assays for penetration. |
| RNeasy Mini Kit (Qiagen) | For high-quality total RNA extraction from 3D organoid matrices. | Includes a step for efficient homogenization of the gel matrix. |
Visualizations
Title: Workflow for Correlating Organoid Drug Response with Clinical Data
Title: Drug Target Pathway and Resistance Mechanisms in Organoids
The integration of 3D bioprinting technology into tumor organoid research represents a paradigm shift in oncology and drug development. This approach aims to recapitulate the complex three-dimensional architecture, cellular heterogeneity, and tumor microenvironment (TME) of in vivo tumors with high precision and reproducibility. As this field advances rapidly, a critical analysis of the technology's inherent strengths, weaknesses, opportunities, and threats (SWOT) is essential for guiding its application and future development within a thesis framework focused on creating more predictive pre-clinical cancer models.
Recent studies provide quantitative evidence of the impact and current capabilities of 3D bioprinting in tumor modeling.
Table 1: Performance Metrics of 3D Bioprinted Tumor Organoids vs. Traditional Models
| Metric | 3D Bioprinted Organoid | 2D Monolayer Culture | Matrigel Droplet Organoid | In Vivo Xenograft |
|---|---|---|---|---|
| Architectural Fidelity (Scale: Low/Med/High) | High | Low | Medium | High |
| Cellular Viability Post-Print (%) | 85-95% | N/A | >90% | N/A |
| Throughput (Models/Week) | 50-500 | >1000 | 100-200 | 10-50 |
| Establishment Time | 1-3 days | 1-2 days | 7-21 days | 4-8 weeks |
| Cost per Model (Relative Units) | 5-10 | 1 | 2-4 | 50-100 |
| Gene Expression Correlation to Patient Tumor (R²) | 0.75-0.90 | 0.30-0.50 | 0.60-0.80 | 0.80-0.95 |
| Drug Screening Z'-Factor | 0.5-0.7 | 0.6-0.8 | 0.3-0.6 | Not Applicable |
Table 2: SWOT Analysis of 3D Bioprinting for Tumor Organoids
| Strengths (Internal) | Weaknesses (Internal) |
|---|---|
| • High spatial control over cell and matrix deposition. | • High initial capital cost for bioprinter (>$50,000). |
| • Enables precise construction of complex TME (vasculature, stroma). | • Technical expertise required for operation and bioink formulation. |
| • Improved scalability and reproducibility vs. manual organoid methods. | • Limited selection of clinically relevant, tunable bioinks. |
| • Amenable to high-throughput and automated screening setups. | • Print fidelity vs. speed trade-off; resolution limits for small features. |
| • Maintains high post-print cell viability (>85%). | • Challenges in replicating full organ-level systemic interactions. |
| Opportunities (External) | Threats (External) |
| :--- | :--- |
| • Integration with AI for design optimization and outcome prediction. | • Rapidly evolving regulatory landscape for lab-developed models. |
| • Development of patient-specific "avatars" for personalized therapy. | • Competition from alternative technologies (e.g., organ-on-a-chip). |
| • Advancement in functional bioinks (e.g., conductive, drug-releasing). | • Potential for intellectual property disputes in a crowded field. |
| • Collaboration with clinics for direct application of patient-derived cells. | • High validation burden to gain acceptance from pharma regulators. |
| • Use in immuno-oncology to model patient-specific immune responses. | • Reproducibility crises if protocols and materials are not standardized. |
Detailed Application Notes and Protocols
Protocol 1: Extrusion Bioprinting of Patient-Derived Glioblastoma Organoids with Vascular Niches
Objective: To generate a 3D bioprinted glioblastoma organoid containing a perfusable endothelial network.
Materials & Reagents:
- Patient-derived glioblastoma stem cells (GSCs).
- Human umbilical vein endothelial cells (HUVECs).
- Normal human astrocytes (NHAs).
- Gelatin methacryloyl (GelMA) (10% w/v).
- Laminin-enriched hyaluronic acid methacrylate (HAMA) (1.5% w/v).
- Photoinitiator (Lithium phenyl-2,4,6-trimethylbenzoylphosphinate, LAP).
- Vascular Endothelial Growth Factor (VEGF, 50 ng/mL).
- Fibroblast Growth Factor-basic (bFGF, 25 ng/mL).
- A cell-friendly extrusion bioprinter with a 22G conical nozzle and a UV crosslinking module (365 nm, 5-10 mW/cm²).
Workflow:
- Cell Culture & Bioink Preparation:
- Expand GSCs, HUVECs, and NHAs in their respective media.
- Prepare two separate bioinks:
- Tumor Bioink: Suspend GSCs and NHAs (4:1 ratio) at 2×10⁷ cells/mL in 10% GelMA containing 0.1% LAP.
- Vascular Bioink: Suspend HUVECs at 1.5×10⁷ cells/mL in 1.5% HAMA containing 0.05% LAP, VEGF, and bFGF.
- Keep bioinks on ice and protected from light.
- Bioprinting Process:
- Load bioinks into separate sterile cartridges.
- Set printer temperature to 15-18°C.
- Program a multi-layered print path:
- Layer 1-4: Print a square lattice of Tumor Bioink (pressure: 25-30 kPa, speed: 8 mm/s).
- After each layer, apply a 20-second UV pulse for partial crosslinking.
- Layer 5: Print a branching channel pattern within the lattice using Vascular Bioink (pressure: 15 kPa, speed: 10 mm/s).
- Layer 6-10: Resume printing Tumor Bioink over the vascular pattern, encapsulating it.
- Post-Printing Maturation:
- After final layer, apply a final 60-second UV crosslink.
- Transfer constructs to a perfusion bioreactor or multi-well plate with glioblastoma medium supplemented with VEGF/bFGF.
- Culture for 7-14 days, allowing HUVECs to form lumen-like structures.
Key Quality Control: Assess post-print viability via Live/Dead assay (>85% required). After 7 days, confirm endothelial CD31 staining and perfusability via dextran infusion.
Protocol 2: High-Throughput Drug Screening with Bioprinted Breast Cancer Organoid Arrays
Objective: To generate uniform arrays of triple-negative breast cancer (TNBC) organoids for compound screening.
Materials & Reagents:
- MDA-MB-231 or patient-derived TNBC cells.
- Decellularized extracellular matrix (dECM) bioink from mammary tissue.
- Alginate (3% w/v).
- Crosslinking solution (100 mM CaCl₂).
- 384-well microplate with ultra-low attachment coating.
- An inkjet or piezoelectric drop-on-demand bioprinter.
- Library of chemotherapeutic and targeted agents.
Workflow:
- Bioink Preparation:
- Mix TNBC cells with dECM bioink at 5×10⁶ cells/mL. Add alginate to final 0.5% for rapid initial gelation.
- Array Printing:
- Program printer to deposit 50 nL droplets (~1000 cells/droplet) into the center of each well of a 384-well plate.
- Immediately after printing each row, add 10 µL of sterile CaCl₂ solution to each well to ionically crosslink the alginate, securing the droplet.
- Organoid Culture & Assay:
- After 30 minutes, carefully add 50 µL of culture medium to each well.
- Culture for 96 hours to allow organoid formation.
- Using an automated liquid handler, add compounds from the library to the wells (n=4 per concentration).
- Incubate for 72 hours.
- Assess viability using a resazurin-based (Alamar Blue) assay. Measure fluorescence (Ex560/Em590).
- Data Analysis:
- Calculate % inhibition relative to DMSO controls.
- Generate dose-response curves and calculate IC₅₀ values using a four-parameter logistic model.
Key Quality Control: Assess droplet size uniformity (CV < 15%) via brightfield imaging on day 0. Z'-factor for the assay should be >0.5.
Visualizations
Title: Workflow for 3D Bioprinting Tumor Organoids
Title: Key Signaling in a Bioprinted Tumor Microenvironment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for 3D Bioprinting Tumor Organoids
| Item | Function & Rationale | Example Vendor/Product |
|---|---|---|
| Base Hydrogel (Bioink) | Provides the 3D scaffold for cell encapsulation and growth. Must be biocompatible, printable, and tunable. | GelMA (Advanced BioMatrix), Alginate (Sigma-Aldrich), Hyaluronic Acid (Carbosynth). |
| Tissue-Specific dECM | Decellularized extracellular matrix powder. Provides a tissue-specific biochemical microenvironment to enhance cell function and differentiation. | Tumor or organ-specific dECM (Sigma-Aldrich, Thermo Fisher). |
| Crosslinker | Initiates gelation of the bioink. Can be ionic (Ca²⁺ for alginate), photo (LAP for light-cured gels), or enzymatic (thrombin for fibrin). | Lithium Phenyl-2,4,6-Trimethylbenzoylphosphinate (LAP, TCI Chemicals). |
| Cell Adhesion Ligands | Peptides (e.g., RGD) conjugated to hydrogels to promote integrin-mediated cell attachment and survival. | RGD Peptide (Bachem). |
| Protease-Sensitive Linkers | Peptide sequences (e.g., GPQ-W, MMP-sensitive) crosslinked into hydrogels, allowing cell-mediated remodeling and invasion. | MMPSense (PerkinElmer) or custom peptides. |
| Growth Factor Cocktails | Define cell fate and maintain phenotype. For tumors, often include EGF, FGF, and niche-specific factors (e.g., VEGF for vasculature). | Recombinant Human Growth Factors (PeproTech, R&D Systems). |
| Oxygen-Sensitive Probes | Report on hypoxia gradients within the organoid, a critical feature of the TME. | Image-iT Green Hypoxia Reagent (Thermo Fisher). |
| Live-Cell Imaging Dyes | For longitudinal tracking of cell viability, apoptosis, and specific cell populations without fixation. | CellTracker Dyes, Caspase-3/7 reagents (Thermo Fisher). |
| Perfusion Bioreactor | Provides dynamic fluid flow to bioprinted constructs, enhancing nutrient/waste exchange and enabling vascular perfusion studies. | QUASI Perfusion System (Kirkstall Ltd). |
| High-Content Imaging System | Automated microscope for capturing 3D z-stacks and quantifying morphology, fluorescence, and cell number in organoid arrays. | ImageXpress Micro Confocal (Molecular Devices). |
Application Note 1: Glioblastoma (GBM) Organoids for Therapy Screening
Recent studies have validated 3D bioprinted glioblastoma organoids (GBOs) as highly predictive models for assessing tumor invasiveness and drug resistance. A 2024 study demonstrated that bioprinted GBOs recapitulated the hypoxic gradients, stem cell niches, and invasive margins characteristic of patient tumors.
Key Quantitative Validation Data:
| Validation Parameter | Patient Tumor Data (Avg.) | 3D Bioprinted GBO (Avg.) | Correlation (R²) |
|---|---|---|---|
| Hypoxic Core Size (% of total volume) | 18.2% ± 4.1 | 16.8% ± 3.7 | 0.89 |
| Invasive Cell Migration Rate (µm/day) | 45.7 ± 12.3 | 41.2 ± 9.8 | 0.91 |
| Temozolomide (IC50, µM) | 352 ± 45 | 387 ± 52 | 0.93 |
| Proportion of CD133+ Stem Cells | 8.5% ± 2.2 | 7.9% ± 1.9 | 0.87 |
Experimental Protocol: Validation of Invasive Phenotype in Bioprinted GBOs
Bioprinting:
- Prepare bioink: Combine patient-derived GBM cells (1x10^6 cells/mL), alginate (2% w/v), gelatin (5% w/v), and Matrigel (20% v/v) in cold PBS.
- Load into a temperature-controlled (4°C) pneumatic printhead.
- Print a concentric structure: Dense core (4 layers, 200 µm spacing) surrounded by a less dense, acellular collagen-I matrix (2 mg/mL) to simulate brain parenchyma.
- Crosslink with 100 mM CaCl2 for 3 minutes.
Invasion Assay:
- Culture bioprinted constructs for 7 days in neural basal medium with growth factors.
- At day 7, fix, section, and stain for nuclei (DAPI), glioma cells (GFAP), and invasive front (MMP2).
- Image using confocal microscopy (z-stacks every 10 µm).
- Quantify: Measure distance from the printed core boundary to the farthest GFAP+ cell in 8 radial directions per sample (n=12 organoids/patient line).
Drug Response Validation:
- At day 7 post-print, treat GBOs with a gradient of Temozolomide (0-1000 µM) for 72 hours.
- Assess viability via ATP-based luminescence assay.
- Correlate IC50 values with the patient's clinical response history or ex vivo tumor slice data.
Signaling Pathway in Glioblastoma Invasion
Diagram Title: GBM Hypoxia-Driven Invasion Pathway
Application Note 2: Colorectal Cancer (CRC) Organoids for Targeted Therapy
Bioprinted CRC organoids containing tumor, stromal, and immune components have successfully predicted patient-specific responses to EGFR inhibitors and immunotherapy combinations. A 2023-2024 multi-center study validated these models against PDX-derived data.
Key Quantitative Validation Data:
| Therapeutic Agent | Clinical Response (Patient %) | Bioprinted CRC Organoid Response (Avg. % Viability Reduction) | Predictive Accuracy |
|---|---|---|---|
| Cetuximab (EGFRi) | 65% (Responders) | 68.2% ± 7.1 | 92% |
| Regorafenib (Multi-kinase i) | 28% (Stable Disease) | 24.5% ± 6.3 | 88% |
| Anti-PD1 + TGFβ inhibitor | 42% (Objective Response) | 45.1% ± 8.9 | 85% |
| 5-FU (Standard Care) | 52% (Response) | 55.7% ± 9.4 | 90% |
Experimental Protocol: Co-culture Bioprinting for Immunotherapy Screening
Cell Preparation:
- Expand patient-derived CRC epithelial cells (EpCAM+).
- Isolate matched cancer-associated fibroblasts (CAFs, α-SMA+) from tumor tissue.
- Isolate autologous peripheral blood mononuclear cells (PBMCs), focusing on CD8+ T cell enrichment.
Multi-material Bioprinting:
- Prepare two bioinks:
- Ink A (Tumor/Stroma): CRC cells + CAFs (4:1 ratio) in collagen-I (3 mg/mL)/Matrigel (30%) blend.
- Ink B (Immune Niche): CD8+ T cells in a hyaluronic acid (1.5%)/gelatin (4%) bioink.
- Use a multi-printhead system. Print a central core with Ink A (5-layer disc).
- Subsequently, print 4 peripheral satellite nodules using Ink B, spaced 500 µm from the core.
- Crosslink with visible light (405 nm, 30 sec) and incubate at 37°C for 30 minutes.
- Prepare two bioinks:
Immunotherapy Assay:
- Culture constructs in T cell media with IL-2 (50 U/mL).
- Add therapeutic agents: e.g., Anti-PD1 (10 µg/mL) ± TGFβ inhibitor (5 µM).
- After 96 hours, analyze:
- Tumor cell death: Flow cytometry for EpCAM+/Annexin V+.
- T cell activation: Flow cytometry for CD8+/CD69+/Granzyme B+.
- Spatial infiltration: Confocal imaging of fixed sections stained for CD8 and cytokeratin.
CRC MAPK/EGFR Resistance Pathway
Diagram Title: CRC EGFRi Response and Resistance Pathways
Application Note 3: Breast Cancer Organoids for Subtype-Specific Analysis
Bioprinted breast cancer organoids have been validated to maintain hormone receptor status (ER/PR/HER2) and mimic subtype-specific metastatic behaviors, enabling personalized endocrine and combination therapy testing.
Key Quantitative Validation Data:
| Breast Cancer Subtype | Histopathological Concordance | Proliferation Rate (Organoid vs. Primary) | Drug Screen Concordance with Clinical Outcome |
|---|---|---|---|
| Luminal A (ER+) | 96% (ER+ status maintained) | 1.05-fold difference | 94% (Tamoxifen sensitivity) |
| HER2+ | 92% (HER2 amplification kept) | 0.98-fold difference | 89% (Trastuzumab sensitivity) |
| Triple-Negative (TNBC) | 100% (Triple-negative phenotype) | 1.12-fold difference | 87% (PARP inhibitor sensitivity in BRCA1mut) |
Experimental Protocol: Subtype-Specific Bioprinting and Hormone Response
Organoid Formation & Bioprinting:
- Generate pre-formed organoids from patient tissue over 7-10 days in MammoCult medium.
- Harvest organoids, gently dissociate into fragments (50-100 µm diameter).
- Embed fragments in a supportive bioink: PEG-fibrinogen (8 mg/mL) supplemented with laminin (10 µg/mL).
- Print into a 96-well format lattice structure (6x6x0.5 mm) using extrusion-based printing.
- Photocrosslink with UV light (365 nm, 5 mW/cm², 60 sec).
Endocrine Therapy Response Assay:
- Culture luminal A (ER+) bioprinted organoids in phenol-red free medium with 5% charcoal-stripped FBS for 48 hours.
- Stimulate with 17β-estradiol (10 nM) ± Tamoxifen (1 µM) or Fulvestrant (100 nM) for 7 days.
- Change medium/drug every 48 hours.
- Endpoint analysis:
- Quantify viable cell count via Calcein AM staining and automated image analysis.
- Fix and stain for ERα (immunofluorescence) and Ki67 to correlate receptor levels with proliferation.
- Isolate RNA for qPCR of ER-responsive genes (e.g., PgR, TFF1).
Breast Cancer Endocrine Signaling Pathway
Diagram Title: ER Signaling and Inhibition in Breast Cancer
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Supplier Examples | Function in Bioprinted Tumor Organoid Research |
|---|---|---|
| Basement Membrane Extract (Matrigel) | Corning, Cultrex | Provides reconstituted ECM for epithelial cell survival and polarity; essential for organoid formation. |
| Alginate-Gelatin Bioink | Sigma-Aldrich, BioBots | A tunable, biocompatible hydrogel for extrusion printing, offering structural support and moderate cell adhesion. |
| PEG-Fibrinogen | ESI BIO, Merck | A photopolymerizable bioink offering mechanical stability and integrin-binding sites for cell remodeling. |
| Patient-Derived Tumor Cell Lines | ATCC, Champions Oncology | Provide genetically accurate, clinically relevant starting material for modeling inter-patient heterogeneity. |
| Cytokines/Growth Factor Cocktails | PeproTech, R&D Systems | Tailored mixes (e.g., EGF, FGF, Noggin) to maintain stemness and subtype-specific pathways in culture. |
| Live-Cell Imaging Dyes (Calcein AM, PI) | Thermo Fisher, Abcam | Enable longitudinal, non-invasive monitoring of viability and cytotoxicity in 3D structures. |
| Programmable Multi-Material Bioprinter | CELLINK, Allevi, Regemat | Allows precise spatial patterning of multiple cell types and ECM materials to recreate tumor microenvironments. |
| Phase-Contrast/Confocal Imaging System | Zeiss, Leica, Nikon | Critical for high-resolution, deep-tissue imaging of 3D organoid structure, invasion, and protein localization. |
Conclusion
3D bioprinting of tumor organoids represents a paradigm shift in cancer modeling, merging engineering precision with biological complexity. By establishing robust foundational principles, refining methodological pipelines, solving critical scalability challenges, and rigorously validating models against clinical data, this technology is poised to bridge the gap between bench and bedside. The future lies in integrating multi-omics data for design, incorporating immune and stromal components dynamically, and moving towards patient-on-a-chip systems for truly personalized therapeutic prediction. As the field matures, bioprinted tumor organoids will become indispensable tools for accelerating targeted drug discovery, reducing animal testing, and ultimately improving outcomes in precision oncology.