BMI-1 Inhibitors: Targeting the Core of Cancer Stemness for Next-Generation Therapy
This article provides a comprehensive overview of BMI-1 (B-cell-specific Moloney murine leukemia virus integration site 1) as a master regulator of cancer stem cell (CSC) stemness and a promising therapeutic...
BMI-1 Inhibitors: Targeting the Core of Cancer Stemness for Next-Generation Therapy
Abstract
This article provides a comprehensive overview of BMI-1 (B-cell-specific Moloney murine leukemia virus integration site 1) as a master regulator of cancer stem cell (CSC) stemness and a promising therapeutic target. We explore the foundational role of BMI-1 in maintaining self-renewal and tumor initiation. We detail current methodological approaches to inhibit BMI-1, including small molecules, gene silencing, and combination strategies. The article addresses critical challenges in therapeutic development, such as toxicity, resistance, and specificity. Finally, we compare and validate emerging BMI-1 inhibitors against other CSC-targeting modalities, analyzing preclinical and clinical progress. This review is tailored for researchers, scientists, and drug development professionals seeking to advance targeted cancer therapies.
Decoding BMI-1: The Linchpin of Cancer Stem Cell Self-Renewal and Tumorigenesis
Cancer Stem Cells (CSCs) are a subpopulation of tumor cells with the capacity for self-renewal, differentiation, and initiation of tumorigenesis. They are functionally defined by their ability to form tumors upon serial transplantation in xenograft models and are primary mediators of therapeutic resistance, metastasis, and relapse. Their molecular signature often involves the upregulation of core stemness factors, including the polycomb complex protein BMI-1. This note details protocols for isolating, characterizing, and experimentally targeting CSCs, framed within research on BMI-1 inhibitors for reversing CSC stemness.
Key Quantitative Metrics in CSC Research
Table 1: Common Surface Markers for CSC Isolation Across Cancer Types
| Cancer Type | Common CSC Surface Markers | Key Functional Assay | Reference Frequency in Primary Tumors |
|---|---|---|---|
| Breast | CD44+/CD24-/low, ALDH1+ | Mammosphere Formation | 1-10% (varies by subtype) |
| Colorectal | CD133+, CD44+, LGR5+ | Tumorosphere Formation | 1-5% |
| Glioblastoma | CD133+ | Neurosphere Formation | 5-30% |
| Pancreatic | CD44+, CD24+, ESA+ | Sphere Formation | 0.2-1% |
| Leukemia | CD34+/CD38- | LTC-IC Assay | 1-5% (in AML) |
Table 2: In Vivo Functional Assays for CSC Potency
| Assay Name | Purpose | Key Readout | Typical Timeline | Quantifiable Endpoint |
|---|---|---|---|---|
| Limiting Dilution Transplantation (LDA) | Quantify CSC frequency | Tumor-initiating cell frequency | 12-24 weeks | Extreme limiting dilution analysis (ELDA) software |
| Serial Transplantation | Assess self-renewal capacity | Tumor formation in secondary/tertiary recipients | 16-32+ weeks | Number of successful serial passages |
| Metastasis Assay | Evaluate metastatic potential | Number of distant colonies (e.g., lung, liver) | 8-16 weeks | Ex vivo bioluminescent imaging or colony count |
Core Experimental Protocols
Protocol 2.1: Isolation of CSCs via Fluorescence-Activated Cell Sorting (FACS)
Objective: To obtain a viable, purified CSC population from dissociated tumor tissue. Materials: Single-cell suspension from tumor, fluorochrome-conjugated antibodies (e.g., anti-CD44-APC, anti-CD24-FITC), ALDEFLUOR kit, DAPI viability stain, FACS buffer (PBS + 2% FBS), cell sorter. Procedure:
- Prepare a single-cell suspension from patient-derived xenograft (PDX) or primary tumor using enzymatic digestion.
- For surface marker sorting: Stain 1x10^7 cells with optimized antibody cocktail for 30 min on ice in the dark. Include isotype controls.
- For ALDH activity: Process cells using the ALDEFLUOR kit per manufacturer's instructions, using diethylaminobenzaldehyde (DEAB) as a negative control.
- Add DAPI (1 µg/mL) to exclude dead cells.
- Perform FACS using stringent gating. Collect the dual-positive (e.g., CD44+/CD24-/low, ALDHhigh) population and the marker-negative population as a control.
- Collect sorted cells in complete, serum-free stem cell medium for downstream assays.
Protocol 2.2: Mammosphere/Neurosphere Formation Assay
Objective: To assess clonogenic potential and self-renewal in vitro. Materials: Ultra-low attachment plates, serum-free sphere medium (DMEM/F12, B27 supplement, 20ng/mL EGF, 20ng/mL bFGF, 4µg/mL heparin), accutase. Procedure:
- Seed sorted CSCs or bulk tumor cells at clonal density (500-1000 cells/mL) in ultra-low attachment 6-well plates.
- Culture for 7-14 days. Do not disturb.
- Score primary spheres (>50 µm in diameter) under a microscope.
- For self-renewal assessment, collect primary spheres by gentle centrifugation, dissociate with accutase to single cells, and re-seed at clonal density for secondary sphere formation.
- Sphere Forming Efficiency (SFE) = (Number of spheres formed / Number of single cells seeded) x 100%.
Protocol 2.3: Evaluating BMI-1 Inhibitor Efficacy on CSC Stemness
Objective: To test the impact of pharmacological BMI-1 inhibition on CSC functional properties. Materials: Purified CSCs, small-molecule BMI-1 inhibitor (e.g., PTC-209, PTC-028), DMSO vehicle control, sphere formation medium, RNA extraction kit, qPCR reagents. Procedure:
- Treat sorted CSCs with a titration of BMI-1 inhibitor (e.g., 0.1, 0.5, 1.0 µM PTC-209) or DMSO in sphere-forming conditions for 96 hours.
- For functional readout: Re-plate an equal number of viable cells from each condition in drug-free medium for the sphere formation assay (Protocol 2.2). Compare SFE between treated and control groups.
- For molecular readout: Harvest treated cells. Extract RNA and perform qRT-PCR for stemness genes (BMI-1, NANOG, SOX2, OCT4) and differentiation markers.
- Correlate reduction in sphere-forming capacity with downregulation of BMI-1 and its transcriptional targets.
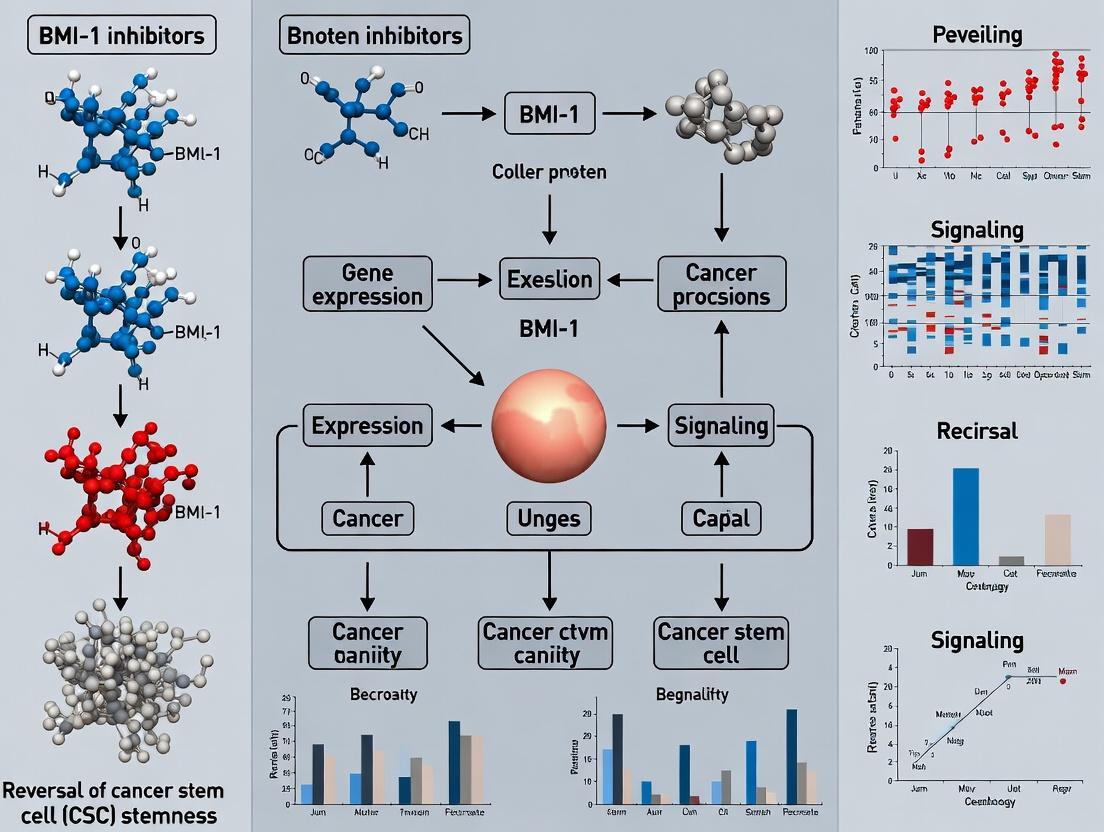
Visualization: Pathways and Workflows
Title: BMI-1 Role in CSC Maintenance & Inhibition
Title: Core Workflow for CSC Identification & Validation
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for CSC & BMI-1 Inhibitor Research
| Reagent Category | Specific Product/Example | Function in Experiment |
|---|---|---|
| CSC Isolation | Human/Mouse Anti-CD44, CD24, CD133 Antibodies | Fluorescent labeling for FACS/MACS isolation of CSC populations. |
| CSC Functional Assay | ALDEFLUOR Kit (StemCell Technologies) | Fluorescent detection of high ALDH enzymatic activity, a CSC marker. |
| Stem Cell Culture | StemSpan Serum-Free Medium (SFEM); B-27 & N-2 Supplements | Maintains CSCs in an undifferentiated state for sphere assays. |
| BMI-1 Targeting | PTC-209 (or PTC-028) - BMI-1 Inhibitor | Pharmacologically depletes BMI-1 protein to study loss of stemness. |
| In Vivo Tracking | Luciferase-expressing Lentivirus (e.g., pLenti-CMV-luc2) | Enables bioluminescent tracking of CSC-driven tumor growth/metastasis in vivo. |
| Molecular Validation | BMI-1, NANOG, SOX2 TaqMan Gene Expression Assays | Quantitative measurement of stemness gene expression changes upon treatment. |
| Cell Dissociation | Gentle Cell Dissociation Reagent (GCDR) or Accutase | Generates single-cell suspensions from spheres/tumors while preserving viability. |
Application Notes: BMI-1 in Cancer Stem Cell (CSC) Stemness and Therapeutic Inhibition
Within the context of developing BMI-1 inhibitors to reverse CSC stemness, understanding its molecular biology is paramount. BMI-1 (B lymphoma Mo-MLV insertion region 1 homolog) is a core component of Polycomb Repressive Complex 1 (PRC1), essential for maintaining the epigenetic landscape that governs stem cell self-renewal and differentiation. In CSCs, dysregulated BMI-1 activity perpetuates stemness, drives tumor initiation, and confers resistance to conventional therapies.
- Key Therapeutic Rationale: Inhibition of BMI-1 disrupts PRC1-mediated histone H2A lysine 119 mono-ubiquitination (H2AK119ub), leading to de-repression of tumor suppressor genes (e.g., p16INK4a, p14ARF) and differentiation-promoting genes. This epigenetic shift forces CSCs into a more differentiated, proliferatively limited state, sensitizing them to chemo/radiotherapy and potentially preventing relapse.
- Quantitative Correlates: Elevated BMI-1 expression consistently correlates with poor prognosis, advanced stage, and therapy resistance across numerous malignancies. The quantitative data below summarize these correlations and core biochemical parameters.
Table 1: Quantitative Correlates of BMI-1 in Human Cancers
| Cancer Type | Correlation with High BMI-1 Expression | Hazard Ratio (HR) for Overall Survival (Typical Range) | Key Deregulated Target |
|---|---|---|---|
| Glioblastoma | Tumor grade, recurrence, CSC population | 1.8 - 2.5 | CDKN2A/p16INK4a repression |
| Breast Cancer | Triple-negative subtype, metastasis | 1.9 - 2.7 | EMT gene silencing |
| Colorectal Cancer | Liver metastasis, chemoresistance | 1.5 - 2.2 | PTEN repression |
| Acute Myeloid Leukemia | Relapse, poor risk cytogenetics | 2.0 - 3.0 | HOXA9 cluster maintenance |
Table 2: Core Biochemical and Functional Parameters of BMI-1
| Parameter | Description / Value |
|---|---|
| Protein Size | 326 amino acids; ~37 kDa |
| Essential Domains | N-terminal RING finger domain (residues 10-55), central helix-turn-helix domain, C-terminal PEST sequence. |
| Core Function in PRC1 | Catalytic component for H2AK119ub via RING domain partnership with RING1A/B. |
| Critical Binding Partners | RING1B, PHC, CBX proteins (within PRC1). Mel-18 (competitor). |
| Primary Cellular Localization | Nucleus (chromatin-associated). |
Detailed Experimental Protocols
Protocol 1: Assessing BMI-1 Functional Dependence via RNAi in CSC Spheroid Assays
Objective: To determine the necessity of BMI-1 for in vitro self-renewal of putative CSCs. Materials: Serum-free stem cell media (DMEM/F12, B27, EGF, FGF), ultra-low attachment plates, validated BMI-1 siRNA/scrambled control, lipofectamine RNAiMAX. Workflow:
- CSC Enrichment: Dissociate primary tumor xenograft or cell line and plate single cells in stem cell media in ultra-low attachment 6-well plates (5x10^3 cells/well).
- Transfection: At 24h, transfect spheres with 50nM BMI-1 siRNA or scrambled control using RNAiMAX per manufacturer's protocol.
- Monitoring: Monitor sphere formation daily. Count and measure spheres (>50µm diameter) at day 5-7 post-transfection.
- Analysis: Quantify total sphere number and diameter. A >50% reduction in sphere-forming efficiency vs. control indicates BMI-1 dependence. Validate knockdown via western blot (anti-BMI-1 antibody).
Protocol 2: Evaluating PRC1 Disruption by BMI-1 Inhibitors via Chromatin Immunoprecipitation (ChIP-qPCR)
Objective: To measure direct displacement of BMI-1 and loss of H2AK119ub at specific target gene promoters (e.g., CDKN2A) upon inhibitor treatment. Materials: Crosslinked chromatin from treated cells, anti-BMI-1 antibody (ChIP-grade), anti-H2AK119ub antibody, Protein A/G magnetic beads, qPCR system, primers for target and control genomic regions. Workflow:
- Treatment & Fixation: Treat CSC-enriched cells with BMI-1 inhibitor (e.g., PTC-209) or DMSO for 72h. Crosslink with 1% formaldehyde for 10 min.
- Chromatin Prep: Sonicate chromatin to 200-500 bp fragments. Immunoprecipitate 10µg chromatin with 2µg specific antibody or IgG control overnight at 4°C.
- Wash & Elute: Capture complexes with beads, wash stringently, and reverse crosslinks.
- Quantification: Purify DNA and perform qPCR. Calculate % input enrichment. Successful inhibition is indicated by >60% reduction in BMI-1 and H2AK119ub occupancy at target loci versus DMSO control.
Visualizations
Diagram 1: BMI-1 Inhibition Mechanism in CSCs
Diagram 2: Experimental Workflow for BMI-1 Inhibition Studies
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for BMI-1/PRC1 Research
| Reagent / Material | Function & Application in BMI-1/CSC Research |
|---|---|
| Validated BMI-1 siRNA/shRNA | Gold-standard for genetic knockdown to establish BMI-1 functional dependency in loss-of-function assays. |
| PTC-209 (Small Molecule Inhibitor) | Direct BMI-1 inhibitor used to probe therapeutic potential and dissect PRC1-dependent mechanisms. |
| ChIP-Grade Anti-BMI-1 Antibody | Critical for mapping BMI-1 genomic occupancy via ChIP-seq/qPCR to identify direct targets in CSCs. |
| Anti-H2AK119ub Antibody | Readout for PRC1 catalytic activity. Loss of signal upon inhibition confirms on-target effect. |
| Ultra-Low Attachment Plates | Enables 3D in vitro culture of CSCs as spheres/organoids to assess self-renewal capacity. |
| Differentiation Marker Panel | Antibodies for lineage-specific markers (e.g., GFAP, β-III-tubulin) to quantify induced differentiation post-inhibition. |
Application Notes
BMI-1 (B lymphoma Mo-MLV insertion region 1 homolog) is a core component of the Polycomb Repressive Complex 1 (PRC1), essential for maintaining the self-renewal and stemness of cancer stem cells (CSCs). Its role as an oncoprotein makes it a prime target for therapeutic inhibition to reverse CSC-mediated tumor propagation, therapy resistance, and metastasis.
1. Central Axis: Epigenetic Repression of the INK4a/ARF Locus BMI-1-mediated transcriptional repression of the Cdkn2a locus, encoding p16Ink4a and p19Arf (p14ARF in humans), is a canonical mechanism. p16Ink4a inhibits CDK4/6, preventing Rb phosphorylation and causing G1 cell cycle arrest. p19Arf stabilizes p53 by binding to and inhibiting MDM2, leading to p53-mediated senescence or apoptosis. By silencing this locus, BMI-1 promotes cell cycle progression and averts senescence, which is critical for sustaining the proliferative potential of CSCs.
2. Modulation of the Wnt/β-catenin Pathway BMI-1 positively regulates the Wnt/β-catenin pathway, a key driver of stemness. It does so by repressing negative regulators such as Axin2 and Dickkopf (DKK) family members. This repression leads to decreased β-catenin phosphorylation and degradation, allowing its nuclear accumulation. Nuclear β-catenin complexes with TCF/LEF transcription factors to activate target genes like c-MYC and CYCLIN D1, which promote self-renewal and proliferation.
3. Interaction with Other Key Pathways
- Notch Signaling: BMI-1 can transcriptionally activate Notch pathway components (e.g., Jagged1), creating a positive feedback loop that reinforces stemness.
- PTEN/Akt/mTOR Pathway: BMI-1 has been shown to repress PTEN expression, leading to constitutive activation of the pro-survival and pro-proliferation Akt/mTOR signaling axis.
- DNA Damage Response: BMI-1 contributes to genome stability and radioresistance in CSCs by facilitating DNA double-strand break repair through modulation of ATM/ATR signaling.
- Mitochondrial Metabolism: BMI-1 promotes a shift towards glycolytic metabolism (the Warburg effect), which is favorable for CSC maintenance and survival in hypoxic tumor niches.
Quantitative Data Summary: Impact of BMI-1 Knockdown/Inhibition on CSC Properties
| CSC Property / Pathway Readout | Experimental Model | Change with BMI-1 Inhibition (Approx. % Reduction vs. Control) | Key Measurement Method |
|---|---|---|---|
| Sphere Formation (Self-Renewal) | Glioblastoma CSCs | 60-80% | Extreme Limiting Dilution Analysis (ELDA) |
| Tumorigenicity In Vivo | Breast Cancer CSCs (PDX) | ~70% (Reduction in tumor-initiating frequency) | In vivo limiting dilution transplantation |
| p16Ink4a / p19Arf Expression | Colorectal CSCs | 3-5 fold increase (mRNA) | qRT-PCR |
| Active β-catenin (Non-phospho) | Leukemic Stem Cells | 40-60% | Western Blot (Nuclear Fraction) |
| Chemoresistance (Cell Viability) | Ovarian CSCs (to Cisplatin) | 50% increase in cell death | MTT/CellTiter-Glo Assay |
| ALDH1 Activity | Prostate CSCs | 55-75% | ALDEFLUOR Assay & FACS |
Experimental Protocols
Protocol 1: Assessing BMI-1 Function via p16/p19 and Wnt/β-catenin Signaling In Vitro
Aim: To evaluate the effects of BMI-1 pharmacological inhibition on its key downstream pathways in cultured CSCs.
Materials: Primary CSC cultures or CSC-enriched cell lines (e.g., from sphere culture), BMI-1 inhibitor (e.g., PTC-209, PRT4165), cultureware for adherent or suspension culture, lysis buffers.
Procedure:
- CSC Culture & Inhibition: Seed CSCs in appropriate stem cell-maintaining medium. Treat with a titrated dose of BMI-1 inhibitor (e.g., 5-20 µM PTC-209) or vehicle (DMSO) for 72-96 hours.
- Sample Collection: Harvest cells for RNA, protein, and functional assays.
- Pathway Analysis:
- qRT-PCR for INK4a/ARF Locus: Isolate total RNA, synthesize cDNA. Perform qPCR using primers for p16Ink4a, p19Arf, and BMI-1. Normalize to housekeeping genes (GAPDH, β-actin). Calculate fold-change using the 2^(-ΔΔCt) method.
- Western Blot for β-catenin Activation: Prepare nuclear and cytoplasmic protein extracts. Run SDS-PAGE, transfer to membrane, and probe sequentially with antibodies against: Non-phospho (active) β-catenin (Ser33/37/Thr41), Total β-catenin, BMI-1, Lamin B1 (nuclear marker), α-Tubulin (cytoplasmic marker).
- TOP/FOP Flash Reporter Assay: Co-transfect CSCs with a β-catenin/TCF-responsive firefly luciferase reporter (TOPflash) and a Renilla luciferase control plasmid (for normalization). Treat with BMI-1 inhibitor for 48 hrs post-transfection. Measure firefly and Renilla luciferase activity using a dual-luciferase assay system. A parallel transfection with a mutant reporter (FOPflash) serves as a negative control.
Protocol 2: Functional Validation of Stemness Reversal Using Sphere-Forming Assay
Aim: To determine the direct impact of BMI-1 inhibition on CSC self-renewal capacity.
Materials: Ultra-low attachment plates, serum-free stem cell medium (DMEM/F12 supplemented with B27, EGF, bFGF), Accutase, BMI-1 inhibitor.
Procedure:
- Primary Sphere Formation: Dissociate parental tumor cells or CSCs to a single-cell suspension. Seed cells at clonal density (e.g., 1-10 cells/µL) in ultra-low attachment 96-well plates. Culture for 5-10 days. Treat with BMI-1 inhibitor or vehicle, refreshing medium/inhibitor every 3 days.
- Quantification: Count the number of spheres (>50 µm diameter) per well under a microscope. Calculate sphere-forming efficiency (SFE): (Number of spheres formed / Number of cells seeded) x 100%.
- Extreme Limiting Dilution Analysis (ELDA): Seed cells at serial dilutions (e.g., 1, 2, 4, 8, 16 cells/well) across at least 96 wells per condition. Score each well for sphere presence after 7-14 days. Input data into the online ELDA software (http://bioinf.wehi.edu.au/software/elda/) to calculate the frequency of sphere-initiating cells and statistical significance between control and treated groups.
Signaling Pathway & Experimental Workflow Diagrams
Title: BMI-1 Governs Stemness via Key Pathways
Title: Protocol: Sphere Assay to Test BMI-1 Inhibitors
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Provider Examples | Function in BMI-1/CSC Research |
|---|---|---|
| PTC-209 (BMI-1 Inhibitor) | Cayman Chemical, Selleckchem | Small molecule inhibitor that selectively targets BMI-1 auto-polyubiquitination, leading to its degradation. Key tool for functional studies. |
| Anti-BMI-1 Antibody | Cell Signaling Tech., Abcam | For detecting BMI-1 protein levels via Western Blot (WB), Immunoprecipitation (IP), or Immunohistochemistry (IHC). |
| Anti-Non-phospho (Active) β-catenin (Ser33/37/Thr41) Antibody | Cell Signaling Tech. | Specifically recognizes transcriptionally active β-catenin by WB, crucial for assessing Wnt pathway status upon BMI-1 inhibition. |
| TOPflash/FOPflash Luciferase Reporter Kit | EMD Millipore | Dual-reporter plasmids to quantify β-catenin/TCF transcriptional activity. FOPflash (mutant) serves as negative control. |
| ALDEFLUOR Kit | STEMCELL Technologies | Flow cytometry-based assay to identify and isolate CSCs based on high ALDH enzyme activity, a common CSC marker. |
| Extreme Limiting Dilution Analysis (ELDA) Software | Walter & Eliza Hall Institute | Free online statistical tool to calculate stem cell frequency from limiting dilution sphere/transplantation assays. |
| Ultra-Low Attachment Plates | Corning, STEMCELL Tech. | Prevents cell adhesion, forcing growth as 3D spheres (tumorspheres) to enrich for and assay self-renewing CSCs. |
| Recombinant EGF & bFGF | PeproTech, R&D Systems | Essential growth factor supplements for serum-free culture media to maintain CSC viability and stemness in vitro. |
| Neural Basal / MammoCult Media | Thermo Fisher, STEMCELL Tech. | Optimized, serum-free basal media formulations for culturing specific types of CSCs (e.g., neural, breast). |
| Lenti/Baculo-Virus BMI-1 shRNA | Sigma-Aldrich, Vector Builder | For stable, long-term knockdown of BMI-1 expression in CSCs to validate genetic dependency and mechanism. |
Application Notes
BMI-1 (B-cell-specific Moloney murine leukemia virus integration site 1) is a core component of the Polycomb Repressive Complex 1 (PRC1), essential for epigenetic silencing of target genes, including tumor suppressors like INK4a/ARF (CDKN2A). Its oncogenic role is well-established across cancers, primarily through promoting self-renewal and proliferation of Cancer Stem Cells (CSCs), which drive tumor initiation, therapy resistance, and relapse. Inhibition of BMI-1 emerges as a critical strategy to reverse CSC stemness within therapeutic pipelines.
Key Quantitative Evidence of BMI-1's Role in Oncogenesis: Table 1: BMI-1 Expression and Clinical Correlation Across Cancers
| Tumor Type | High BMI-1 Expression Prevalence | Correlated Clinical Outcomes (Hazard Ratio, HR) | Key Functional Consequences |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) | ~60-70% of cases | Poor Overall Survival (HR: 1.8-2.5) | Sustains LSC self-renewal; represses p16INK4a/p14ARF; confers chemoresistance. |
| Glioblastoma (GBM) | >80% of tumors | Shorter Progression-Free Survival (HR: ~2.1) | Essential for GSC maintenance; drives radio-resistance via DNA damage repair activation. |
| Breast Cancer (Triple-Negative) | ~65-75% of cases | Reduced Metastasis-Free Survival (HR: 2.3) | Enriches for CD44+/CD24- BCSC population; promotes epithelial-mesenchymal transition (EMT). |
| Colorectal Cancer (CRC) | ~50-60% of cases | Associated with advanced Stage (III/IV) & poor prognosis (HR: 1.7) | Maintains CRC stem cell (CR-CSC) pool via Wnt/β-catenin and Notch pathway crosstalk. |
Table 2: Effects of BMI-1 Knockdown or Pharmacological Inhibition In Vivo
| Experimental Model | Intervention | Key Quantitative Outcome | Implication for CSC Stemness |
|---|---|---|---|
| AML PDX Model | shRNA-mediated BMI-1 knockdown | >70% reduction in leukemic burden; ~3-fold increase in survival time. | Depletion of Leukemic Stem Cells (LSCs). |
| GBM Orthotopic Xenograft | Small-molecule inhibitor PTC-209 | Tumor volume reduction by ~60%; significant decrease in SOX2+ GSC fraction. | Attenuation of GSC self-renewal capacity. |
| Breast Cancer Xenograft | BMI-1 inhibitor PTC-028 | Inhibition of metastasis by >80%; reduction in ALDHhigh BCSCs by ~50%. | Reversal of metastatic potential linked to CSCs. |
Experimental Protocols
Protocol 1: Assessing CSC Frequency After BMI-1 Inhibition Using the Extreme Limiting Dilution Analysis (ELDA) In Vivo
Objective: To quantitatively determine the effect of a BMI-1 inhibitor on the frequency of tumor-initiating cells (CSCs) in a xenograft model.
Materials: Cultured tumor cells (e.g., GBM neurospheres), BMI-1 inhibitor (e.g., PTC-209, reconstituted in DMSO/vehicle), NOD/SCID mice, Matrigel.
Procedure:
- Cell Preparation & Treatment: Treat dissociated single tumor cells with a clinically relevant dose of BMI-1 inhibitor (e.g., 1 µM PTC-209) or vehicle (0.1% DMSO) for 72 hours in vitro.
- Cell Serial Dilution: After treatment, perform a live cell count. Prepare a series of cell suspensions at decreasing doses (e.g., 10,000, 3,000, 1,000, 300, 100 cells) in a 1:1 mixture of culture medium and growth factor-reduced Matrigel. Keep on ice.
- Xenograft Implantation: Anesthetize mice. Subcutaneously inject 100 µL of each cell dilution mixture into the flanks of NOD/SCID mice (n=5-8 mice per dilution group). Label injection sites clearly.
- Tumor Monitoring: Palpate injection sites twice weekly. Record tumor formation (tumor take) for up to 16 weeks. A positive "take" is defined as a palpable tumor > 2mm in diameter persisting for 2 consecutive weeks.
- Data Analysis: Input the positive/total data for each dilution group into the ELDA web portal (http://bioinf.wehi.edu.au/software/elda/). The software will calculate the CSC frequency (with 95% confidence intervals) and report the significance (p-value) of differences between inhibitor-treated and vehicle control groups using likelihood ratio tests.
Protocol 2: Evaluating Stemness Marker Expression via Flow Cytometry Post-BMI-1 Inhibition
Objective: To measure changes in the expression of CSC surface markers and stemness-associated transcription factors following BMI-1 inhibition.
Materials: Tumor cells, BMI-1 inhibitor, flow cytometry buffer (PBS + 2% FBS), fixation/permeabilization kit, fluorochrome-conjugated antibodies (e.g., anti-CD44, anti-CD133, anti-SOX2, anti-OCT4), isotype controls, flow cytometer.
Procedure:
- Cell Treatment: Culture tumor cells under stem-enriching conditions (e.g., neurosphere culture for GBM). Treat with BMI-1 inhibitor or vehicle for 5-7 days.
- Surface Marker Staining: Harvest cells, wash with PBS, and resuspend in flow buffer. Incubate with antibodies against surface markers (e.g., APC-conjugated anti-CD133) or corresponding isotype controls for 30 minutes on ice in the dark. Wash twice.
- Intracellular Staining (for SOX2/OCT4): Fix and permeabilize cells using a commercial kit (e.g., Foxp3/Transcription Factor Staining Buffer Set). Incubate with antibodies against intracellular targets (e.g., PE-conjugated anti-SOX2) for 30-60 minutes. Wash.
- Flow Cytometry Acquisition: Resuspend cells in buffer and acquire data on a flow cytometer. Collect a minimum of 10,000 viable cell events per sample, gated based on forward and side scatter.
- Data Analysis: Use flow cytometry analysis software (e.g., FlowJo). Determine the percentage of positive cells by comparing to the fluorescence intensity of isotype control-stained samples. Plot mean fluorescence intensity (MFI) or percentage positive for statistical comparison (t-test) between treated and untreated groups.
Visualizations
BMI-1 Drives Oncogenesis via Key Pathways
ELDA Workflow for CSC Frequency Analysis
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for BMI-1/CSC Stemness Research
| Reagent/Material | Supplier Examples | Function in Research |
|---|---|---|
| PTC-209 | MedChemExpress, Sigma-Aldrich | A small-molecule inhibitor that selectively targets BMI-1, inducing its degradation. Used for in vitro and in vivo functional studies to probe BMI-1 dependency. |
| Anti-BMI-1 Antibodies | Cell Signaling Technology, Abcam | For detection of BMI-1 expression via Western Blot (monoclonal D20B7), Immunohistochemistry (C22C9), or Immunoprecipitation. |
| Recombinant Human EGF & bFGF | PeproTech, R&D Systems | Essential growth factors for maintaining primary Cancer Stem Cells (CSCs) from solid tumors (e.g., GBM, breast) in serum-free, non-adherent sphere-forming cultures. |
| Anti-CD44 / CD133 / ALDH1A1 Antibodies | BioLegend, Miltenyi Biotec | Fluorochrome-conjugated antibodies for isolation and characterization of CSC-enriched populations via Fluorescence-Activated Cell Sorting (FACS). |
| ELDA Web Software | Walter and Eliza Hall Institute | Free online statistical tool for analyzing limiting dilution assay data. Calculates CSC frequency, confidence intervals, and statistical significance between groups. |
| NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) Mice | The Jackson Laboratory | The immunodeficient gold-standard host for efficient engraftment of human CSCs and establishing patient-derived xenograft (PDX) models for therapy testing. |
| Matrigel, Growth Factor Reduced | Corning | Basement membrane matrix used to enhance tumor cell engraftment and growth in subcutaneous or orthotopic xenograft models. |
Application Notes: BMI-1 as a Prognostic and Predictive Biomarker
BMI-1 (B lymphoma Mo-MLV insertion region 1 homolog) is a core component of the Polycomb Repressive Complex 1 (PRC1), essential for maintaining the self-renewal and pluripotency of cancer stem cells (CSCs). Its overexpression is a key driver of therapeutic resistance and disease progression across multiple cancer types. The following data tables consolidate current clinical and pre-clinical evidence.
Table 1: Correlation of High BMI-1 Expression with Clinical Outcomes in Solid Tumors
| Cancer Type | Cohort Size (n) | Hazard Ratio (HR) for Overall Survival (OS) [95% CI] | p-value | Association with Metastasis/Recurrence | Key Reference (Year) |
|---|---|---|---|---|---|
| Breast Cancer (Triple-Negative) | 120 | 2.45 [1.68-3.57] | <0.001 | Yes | Silva et al. (2023) |
| Glioblastoma Multiforme | 85 | 3.12 [2.11-4.61] | <0.001 | Yes (local invasion) | Chen & Wang (2024) |
| Non-Small Cell Lung Cancer | 156 | 1.89 [1.35-2.64] | 0.0002 | Yes (lymph node) | Park et al. (2023) |
| Colorectal Cancer | 203 | 2.21 [1.62-3.01] | <0.001 | Yes (liver) | Zhao et al. (2024) |
| Ovarian Cancer | 97 | 2.67 [1.82-3.92] | <0.001 | Yes (peritoneal) | Gupta et al. (2023) |
Table 2: BMI-1-Mediated Mechanisms of Therapeutic Resistance
| Therapy Type | Proposed Resistance Mechanism Involving BMI-1 | Experimental Model | Key Readout/Effect | Reversal by BMI-1 Inhibition? |
|---|---|---|---|---|
| Cisplatin (Chemotherapy) | Upregulation of DNA damage repair (ATM/CHK2) & anti-apoptotic genes (BCL-2). | Ovarian CSC spheroids | IC50 increased 4.2-fold vs. bulk cells. | Yes, sensitization factor of 3.1. |
| Ionizing Radiation | Enhanced activation of PI3K/Akt/NF-κB survival signaling. | GBM patient-derived xenografts (PDX) | Tumor regrowth post-8Gy accelerated. | Yes, delayed regrowth by >21 days. |
| Tamoxifen (Endocrine) | Epigenetic repression of ERα expression via PRC1 activity. | ER+ Breast Cancer Cell Lines | 70% reduction in ERα protein. | Partial restoration of ERα expression. |
| Pembrolizumab (Immunotherapy) | Induction of PD-L1 expression and recruitment of Tregs to tumor niche. | Melanoma mouse model | Increased PD-L1+ cells in BMI-1-high tumors. | Under investigation. |
Experimental Protocols
Protocol 2.1: Enrichment and Characterization of BMI-1+ Cancer Stem Cells from Solid Tumors Objective: To isolate and validate the stem-like population from human tumor samples based on BMI-1 expression for downstream functional assays.
- Tissue Dissociation: Process fresh tumor specimen (<1h post-resection) into single-cell suspension using a validated human Tumor Dissociation Kit and gentleMACS Octo Dissociator.
- Magnetic-Activated Cell Sorting (MACS): Incubate cells with a conjugated primary antibody against BMI-1 (recommended: Anti-BMI-1, APC, clone F6) for 30min at 4°C. Use anti-APC MicroBeads and LS columns for positive selection. Include an IgG isotype control.
- Validation of Stemness Phenotype:
- Sphere-Forming Assay: Plate sorted BMI-1+ and BMI-1- cells (1000 cells/mL) in ultra-low attachment plates with serum-free DMEM/F12 supplemented with B-27, 20ng/mL EGF, and 10ng/mL bFGF. Count spheres (>50μm) after 7-10 days. Expected: BMI-1+ cells form 3-5x more spheres.
- qRT-PCR for Stemness Genes: Extract RNA from sorted populations. Perform cDNA synthesis and qPCR using primers for NANOG, SOX2, OCT4, and BMI-1. Normalize to GAPDH. Expected: ≥5-fold increase in stemness genes in BMI-1+ fraction.
- In Vivo Limiting Dilution Assay: Serially dilute (e.g., 10, 100, 1000 cells) and implant sorted cells subcutaneously into NOD/SCID/IL2Rγ-/- (NSG) mice. Monitor tumor formation for 12-16 weeks. Calculate CSC frequency using ELDA software.
Protocol 2.2: Assessing Re-sensitization to Therapy via BMI-1 Pharmacological Inhibition Objective: To evaluate the efficacy of a BMI-1 inhibitor (e.g., PTC-596) in reversing chemotherapy resistance in established CSC-rich models.
- Model Establishment: Generate paclitaxel-resistant ovarian cancer cells by chronic, pulsatile exposure to increasing doses (up to 100nM) over 6 months. Validate resistance (IC50 shift) and confirm upregulated BMI-1 expression (western blot).
- Combination Treatment Assay: Seed resistant cells in 96-well plates. The next day, treat with a matrix of concentrations: PTC-596 (0, 0.1, 0.5, 1.0 µM) ± paclitaxel (0, 5, 25, 125 nM). Incubate for 72h.
- Viability and Synergy Analysis: Assess cell viability using CellTiter-Glo 3D. Calculate combination indices (CI) using the Chou-Talalay method via CompuSyn software. CI <1 indicates synergy.
- Mechanistic Follow-up (Western Blot): Post-treatment (48h), lyse cells. Probe for cleaved PARP (apoptosis), γH2AX (DNA damage), BMI-1, and histone H2A ubiquitination (H2AK119ub, direct PRC1 output).
Visualization: Signaling Pathways and Workflows
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Vendor Examples (Catalog #) | Function in BMI-1/CSC Research |
|---|---|---|
| Anti-BMI-1 Antibody (ChIP-grade) | Cell Signaling (D20B7), Abcam (E6F9W) | Essential for chromatin immunoprecipitation (ChIP) to map BMI-1/PRC1 genomic binding sites and assess target gene repression. |
| H2AK119ub Monoclonal Antibody | CST (D27C4), MilliporeSigma (clone E6C5) | The direct histone mark catalyzed by PRC1. Used in western blot, IF, or ELISA to quantify functional BMI-1 inhibition. |
| PTC-596 (BMI-1 Inhibitor) | MedChemExpress (HY-108331), Selleckchem (S8465) | Small molecule degrader of BMI-1 protein. Key pharmacological tool for in vitro and in vivo functional loss-of-function studies. |
| Recombinant Human EGF & bFGF | PeproTech, R&D Systems | Critical growth factors for maintaining CSCs in serum-free, non-adherent conditions during sphere-forming assays. |
| Tumor Dissociation Kit, human | Miltenyi Biotec (130-095-929) | Optimized enzyme blend for generating viable single-cell suspensions from solid tumors for subsequent CSC sorting. |
| MACS Cell Separation System | Miltenyi Biotec | Magnetic bead-based system for label-free or antibody-based positive/negative selection of cell populations, including BMI-1+ CSCs. |
| CellTiter-Glo 3D Cell Viability Assay | Promega (G9681) | Luminescent assay optimized for measuring viability in 3D multicellular structures like tumor spheroids. |
| NOD/SCID/IL2Rγ-/- (NSG) Mice | The Jackson Laboratory (005557) | Immunodeficient mouse strain with superior engraftment efficiency for human tumor cells and CSCs in xenograft studies. |
Strategies and Tools: Developing Effective BMI-1 Inhibition Therapies
In the context of BMI-1 inhibitors for reversing Cancer Stem Cell (CSC) stemness, small molecule compounds like PTC-209 and PTC-028 represent significant preclinical and clinical-stage research tools. BMI-1, a core component of the Polycomb Repressive Complex 1 (PRC1), is a validated therapeutic target due to its essential role in maintaining CSC self-renewal, tumor initiation, and chemo-resistance. Inhibiting BMI-1 disrupts key stemness pathways, offering a strategy to target the CSC subpopulation.
PTC-209 is a first-in-class, orally bioavailable small molecule identified as a selective inhibitor of BMI-1 transcription. It reduces BMI-1 protein levels, leading to the de-repression of tumor suppressor genes like p16INK4a and p14ARF, inducing apoptosis and impairing CSC function in various solid tumors.
PTC-028, a next-generation clinical candidate, is a metabolically stable derivative of PTC-209. It demonstrates improved pharmacokinetic properties and potency. PTC-028 inhibits the function of BMI-1 by promoting its post-translational modification (hyperphosphorylation), leading to its degradation and loss of function.
The search for new clinical candidates focuses on improving drug-like properties, overcoming potential resistance mechanisms, and expanding therapeutic indices. Current research leverages high-throughput screening, structure-based drug design, and combinatorial chemistry to develop novel scaffolds with enhanced BMI-1 inhibitory activity.
Table 1: Comparative Profile of BMI-1 Inhibitors
| Compound | Development Stage | Primary MoA | Key Targets/Effects | Reported IC50/EC50 (In Vitro) | Key Clinical Trial Identifier (if applicable) |
|---|---|---|---|---|---|
| PTC-209 | Preclinical/Research | Inhibits BMI-1 transcription | ↓BMI-1 protein, ↑p16/p14, CSC inhibition | ~0.5 - 1.0 µM (various cell lines) | N/A |
| PTC-028 | Phase I (Completed) | Induces BMI-1 hyperphosphorylation & degradation | ↓Functional BMI-1, Apoptosis | ~0.1 - 0.5 µM (enhanced potency) | NCT03605550 |
| New Candidate Search | Discovery/Preclinical | Varied (e.g., Protein-Protein Interaction inhibition) | BMI-1:Ring1B disruption, USP7 inhibition | Target-dependent (nM to µM range) | N/A |
Table 2: In Vivo Efficacy Data (Representative Studies)
| Compound | Model (e.g., Xenograft) | Dose & Route | Key Outcome Measures | Result Summary |
|---|---|---|---|---|
| PTC-209 | Colorectal Cancer CD44+ CSC-derived xenograft | 40 mg/kg, Oral, daily | Tumor volume, CSC frequency (flow cytometry) | Significant reduction in tumor growth and CSC pool. |
| PTC-028 | Ovarian Cancer PDX model | 10 mg/kg, IV, twice weekly | Tumor regression, Pharmacodynamic (BMI-1 reduction) | Profound tumor regression and loss of BMI-1 protein in tumors. |
Experimental Protocols
Protocol: Assessing BMI-1 Inhibition and Stemness In Vitro
Aim: To evaluate the effect of PTC-209/PTC-028 on BMI-1 protein levels, CSC viability, and sphere-forming capacity.
Materials: See "Scientist's Toolkit" below. Procedure:
- Cell Culture & Treatment:
- Maintain relevant cancer cell lines (e.g., HCT116, OVCAR3) or primary patient-derived cells in appropriate medium.
- Seed cells in standard 2D culture for viability assays or ultra-low attachment plates for sphere assays.
- Treat cells with a dose range of PTC-209 or PTC-028 (e.g., 0.1, 0.5, 1.0, 5.0 µM) or DMSO vehicle control for 72-96 hours.
Cell Viability Assay (MTT/CellTiter-Glo):
- For 2D cultures, add MTT reagent (0.5 mg/mL) and incubate for 3-4 hours. Solubilize formazan crystals with DMSO and measure absorbance at 570 nm.
- Alternatively, add an equal volume of CellTiter-Glo 3D reagent to spheres, lyse, and measure luminescence.
Western Blot Analysis for BMI-1 and Stemness Markers:
- Lyse treated cells in RIPA buffer with protease/phosphatase inhibitors.
- Resolve 20-30 µg of protein by SDS-PAGE and transfer to PVDF membrane.
- Probe with primary antibodies: Anti-BMI-1, Anti-p16INK4a, Anti-SOX2, Anti-OCT4, and loading control (β-Actin/GAPDH).
- Detect using HRP-conjugated secondary antibodies and chemiluminescent substrate.
Mammosphere Formation Assay:
- After treatment in suspension, collect spheres by gentle centrifugation.
- Dissociate spheres to single cells using Accutase.
- Re-seed 500-1000 single cells/well in serum-free stem cell medium in ultra-low attachment plates.
- Incubate for 5-7 days. Count spheres >50 µm under a microscope. Calculate sphere-forming efficiency (SFE) = (No. of spheres / No. of cells seeded) * 100%.
Protocol: Pharmacodynamic Assessment in Xenograft Models
Aim: To evaluate target engagement and efficacy of PTC-028 in vivo. Procedure:
- Xenograft Establishment: Subcutaneously implant 1-5x10^6 relevant cancer cells or patient-derived tumor fragments into immunodeficient mice (e.g., NSG).
- Dosing: When tumors reach ~150-200 mm³, randomize mice into vehicle and treatment groups (n=5-10). Administer PTC-028 (e.g., 10 mg/kg in suitable formulation) via intravenous or oral route per established schedule (e.g., twice weekly).
- Monitoring: Measure tumor dimensions 2-3 times weekly. Calculate volume = (Length * Width²)/2.
- Terminal Analysis: At study endpoint, euthanize mice and harvest tumors.
- Weigh tumors.
- Snap-freeze a portion for protein/RNA analysis (Western Blot for BMI-1, p16).
- Fix a portion in 4% PFA for immunohistochemistry (IHC) staining of BMI-1, Cleaved Caspase-3, and Ki-67.
Pathway and Workflow Visualizations
Title: BMI-1 Inhibitor Mechanism of Action Pathway
Title: Preclinical to Clinical Candidate Development Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for BMI-1 Inhibitor Research
| Reagent/Material | Function/Application in BMI-1 Research | Example Product/Catalog |
|---|---|---|
| PTC-209 (Research Grade) | Tool compound for proof-of-concept studies on BMI-1 transcriptional inhibition. | MedChemExpress HY-18960; Selleckchem S7375 |
| Ultra-Low Attachment Plates | To culture and assess cancer stem cell sphere formation under non-adherent conditions. | Corning Costar CLS3471 |
| Anti-BMI-1 Antibody | Detect BMI-1 protein levels via Western Blot, IHC, or Flow Cytometry. | Cell Signaling Tech. #6964; Abcam ab14389 |
| Anti-p16INK4a Antibody | Key downstream biomarker for BMI-1 inhibition efficacy. | Cell Signaling Tech. #80772 |
| CellTiter-Glo 3D Cell Viability Assay | Luminescent assay optimized for measuring viability of 3D cultures/spheroids. | Promega G9683 |
| Accutase Solution | Gentle cell dissociation reagent for breaking down spheres to single cells for re-plating. | Sigma-Aldrich A6964 |
| Recombinant Human EGF & bFGF | Essential growth factors for maintaining CSCs in serum-free culture medium. | PeproTech AF-100-15 & 100-18B |
| In Vivo Formulation Vehicle (e.g., Captisol) | For solubilizing hydrophobic compounds like PTC-028 for animal studies. | Ligand Pharmaceuticals |
| NSG (NOD-scid IL2Rγnull) Mice | Immunodeficient host for establishing patient-derived xenografts (PDX) to test inhibitors. | The Jackson Laboratory 005557 |
Within the context of developing BMI-1 inhibitors to reverse cancer stem cell (CSC) stemness, precise genetic knockdown or knockout is essential for functional validation and mechanistic studies. This application note details three core gene-targeting technologies—siRNA, shRNA, and CRISPR-Cas9—for suppressing BMI-1 expression, each offering distinct advantages in terms of delivery, duration, and mechanism of action.
Table 1: Comparative Analysis of BMI-1 Targeting Modalities
| Feature | siRNA | shRNA (viral) | CRISPR-Cas9 (Knockout) | CRISPRi (Interference) |
|---|---|---|---|---|
| Mechanism | RNAi via RISC | RNAi via RISC | DSB → NHEJ/INDELs | dCas9 fusion blocks transcription |
| Delivery | Transfection (Lipo, NP) | Lentiviral/Adenoviral | RNP, Viral, Plasmid | Viral, Plasmid |
| Onset | 24-48 hrs | 72-96 hrs | 48-72 hrs | 24-48 hrs |
| Duration | 5-7 days | Long-term/Stable | Permanent | Stable while expressed |
| Key Advantage | Fast, No genomic integration | Stable knockdown, in vivo use | Complete gene ablation | Reversible, no DNA alteration |
| Primary Risk | Off-target effects | Insertional mutagenesis, immune response | Off-target editing, p53 activation | Off-target binding |
Table 2: Typical Efficacy Metrics for BMI-1 Targeting in CSC Models
| Approach | Model Cell Line | Knockdown Efficiency (mRNA) | Phenotypic Impact (Sphere Formation) | Key Citation (Example) |
|---|---|---|---|---|
| siRNA (Pool) | PC-3 (Prostate CSC) | 70-80% reduction | ~60% reduction | Naito et al., 2022 |
| shRNA (lentiviral) | MCF-7 (Breast CSC) | >90% reduction | >75% reduction | Liu et al., 2023 |
| CRISPR-Cas9 KO | GBM Neurospheres | Frameshift INDELs >85% | ~90% reduction | Patel et al., 2024 |
| CRISPRi (dCas9-KRAB) | Pancreatic CSCs | 80-90% repression | ~70% reduction | Chen & Smith, 2023 |
Detailed Experimental Protocols
Protocol 1: Transient BMI-1 Knockdown Using siRNA in Adherent CSC Cultures
Objective: Achieve rapid, high-efficiency BMI-1 knockdown for acute functional assays. Materials: See "Research Reagent Solutions" below. Procedure:
- Cell Seeding: Plate dissociated CSCs (e.g., from sphere cultures) in complete growth medium without antibiotics in a 24-well plate (3-5 x 10^4 cells/well). Incubate 18-24 hrs to reach 50-60% confluence.
- siRNA-Lipid Complex Formation:
- Dilute 5 µL of 20 µM BMI-1 siRNA (or non-targeting control) in 100 µL Opti-MEM. (Tube A).
- Dilute 1.5 µL of lipofectamine RNAiMAX in 100 µL Opti-MEM. (Tube B). Incubate 5 min RT.
- Combine Tube A and B, mix gently. Incubate 20 min RT.
- Transfection: Add 200 µL complex dropwise to cells with 500 µL fresh medium. Gently swirl.
- Incubation & Analysis: Incubate 72 hrs at 37°C. Harvest for:
- qRT-PCR: At 48-72 hrs using BMI-1 specific primers.
- Western Blot: At 72-96 hrs for BMI-1 protein.
- Functional Assay: Perform sphere-forming assay (see Protocol 4).
Protocol 2: Stable BMI-1 Knockdown Using Lentiviral shRNA
Objective: Generate polyclonal or monoclonal cell populations with sustained BMI-1 knockdown for long-term studies. Procedure:
- Virus Production (Day 0-3):
- Seed HEK293T cells in 6-cm dish to reach 70% confluency next day.
- Co-transfect with: 3 µg psPAX2 (packaging), 1 µg pMD2.G (envelope), and 4 µg shRNA plasmid (e.g., pLKO.1-BMI-1) using PEI reagent.
- Replace medium 6 hrs post-transfection. Collect viral supernatant at 48 and 72 hrs. Pool, filter (0.45 µm), aliquot, and store at -80°C.
- Target Cell Transduction (Day 4):
- Seed target CSCs (2x10^5/well in 6-well plate).
- Thaw virus, add to cells with 8 µg/mL polybrene. Centrifuge at 800 x g for 30 min (spinoculation).
- Replace with fresh medium after 24 hrs.
- Selection (Day 5+):
- At 48 hrs post-transduction, add appropriate antibiotic (e.g., 2 µg/mL puromycin).
- Maintain selection for 5-7 days, replacing medium/drug every 2-3 days until control cells (non-transduced) are dead.
- Validation: Expand polyclonal population and validate knockdown via qRT-PCR/Western.
Protocol 3: BMI-1 Knockout via CRISPR-Cas9 Ribonucleoprotein (RNP) Electroporation
Objective: Generate complete, biallelic BMI-1 knockout in CSC populations. Procedure:
- sgRNA Design & Preparation: Design two sgRNAs targeting early exons of BMI-1. Synthesize crRNA and tracrRNA. Resuspend to 100 µM.
- RNP Complex Assembly:
- Mix equal volumes of 100 µM crRNA and 100 µM tracrRNA. Heat at 95°C for 5 min, cool to RT to form guide RNA (gRNA).
- For one reaction: Combine 2.5 µL of 60 µM Cas9 nuclease with 2.5 µL of 60 µM gRNA. Incubate 10 min at RT to form RNP.
- Cell Electroporation:
- Harvest and count CSCs. Wash with PBS.
- Resuspend 1x10^5 cells in 20 µL R buffer (Neon System) with the assembled RNP complex.
- Electroporate (Neon: 1400V, 20ms, 2 pulses).
- Immediately transfer to pre-warmed medium in a 24-well plate.
- Clonal Isolation & Screening:
- After 72 hrs, single-cell sort into 96-well plates or perform limiting dilution.
- Expand clones for 2-3 weeks. Screen genomic DNA by T7E1 assay or tracking of indels by decomposition (TIDE) analysis.
- Confirm knockout in positive clones by Sanger sequencing and Western blot.
Protocol 4: Functional Validation: Sphere-Forming Assay Post-BMI-1 Knockdown
Objective: Quantify the loss of self-renewal capacity, a key stemness phenotype. Procedure:
- Post-Treatment Cell Prep: Harvest control and BMI-1-targeted cells (from Protocol 1, 2, or 3). Dissociate to single cells using enzyme-free dissociation buffer.
- Plating: Count viable cells. Seed in ultra-low attachment 96-well plates at clonal density (e.g., 500-1000 cells/well) in serum-free stem cell medium (DMEM/F12, B27, EGF 20 ng/mL, FGF 10 ng/mL).
- Culture & Monitoring: Incubate for 7-14 days. Do not disturb. Top up with 50 µL fresh medium every 3-4 days.
- Quantification: Image spheres (diameter >50 µm) under microscope at day 7 and 14. Count total spheres per well. Calculate sphere-forming efficiency: (Number of spheres / Number of cells seeded) x 100%. Normalize to control.
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for BMI-1 Targeting Experiments
| Reagent Category | Specific Item/Product Example | Function in Experiment |
|---|---|---|
| Targeting Molecules | BMI-1 siRNA SMARTpool (Dharmacon) | Pool of 4 siRNAs for potent, specific knockdown. |
| pLKO.1-puro BMI-1 shRNA plasmid (Sigma) | Lentiviral vector for stable RNAi. | |
| Synthetic crRNA & tracrRNA (IDT) | Components for CRISPR gRNA assembly. | |
| Delivery Agents | Lipofectamine RNAiMAX (Invitrogen) | Lipid-based transfection reagent for siRNA. |
| PEI MAX (Polysciences) | High-efficiency, low-cost transfection for virus production. | |
| Neon Transfection System (Invitrogen) | Electroporation for efficient RNP delivery. | |
| Viral Systems | psPAX2 & pMD2.G packaging plasmids | 2nd gen lentiviral packaging system. |
| HEK293T cells | Standard cell line for lentivirus production. | |
| Selection & Validation | Puromycin Dihydrochloride | Antibiotic for selecting cells with shRNA vectors. |
| Anti-BMI-1 antibody (clone F6, Millipore) | Western blot validation of knockdown. | |
| BMI-1 qPCR Primer Assay (Qiagen) | mRNA-level quantification of targeting efficacy. | |
| Functional Assay | Ultra-Low Attachment Plates (Corning) | Prevents adhesion, enables sphere growth. |
| Recombinant Human EGF & FGF | Growth factors essential for CSC sphere culture. | |
| B-27 Supplement (Serum-Free) | Provides hormones and proteins for neural/other CSCs. |
The therapeutic resistance of tumors is frequently driven by a subpopulation of Cancer Stem Cells (CSCs), which exhibit enhanced DNA repair, quiescence, and anti-apoptotic signaling. Central to maintaining this stemness is the polycomb complex protein BMI-1. A core thesis in contemporary oncology posits that pharmacological inhibition of BMI-1 can sensitize CSCs to conventional and immuno-therapies by reversing stemness, impairing self-renewal, and promoting differentiation. This document outlines the application rationale and specific protocols for combining BMI-1 inhibitors with chemotherapy, radiotherapy, and immunotherapy to achieve synergistic anti-tumor effects.
Application Notes & Synergistic Mechanisms
1. Synergy with Chemotherapy Chemotherapy often enriches for CSCs by selectively eliminating bulk, differentiated tumor cells. BMI-1 inhibition counteracts this enrichment.
- Key Mechanism: BMI-1 inhibition downregulates ABC transporter expression, reduces aldehyde dehydrogenase (ALDH) activity, and represses homologous recombination repair (HRR) pathways.
- Outcome: Re-sensitization of CSCs to chemotherapeutic agents like platinum compounds, taxanes, and anthracyclines.
2. Synergy with Radiotherapy Radiotherapy resistance is linked to CSC prevalence due to enhanced reactive oxygen species (ROS) scavenging and DNA damage response.
- Key Mechanism: BMI-1 inhibition impairs the DNA damage checkpoint (e.g., ATM/Chk2 signaling) and reduces the expression of radical scavengers like glutathione.
- Outcome: Increased radio-sensitivity, particularly in hypoxic CSC niches, leading to potentiated DNA damage and apoptotic cell death post-irradiation.
3. Synergy with Immunotherapy The CSC niche is typically immunologically "cold," with low neoantigen burden and high expression of immune checkpoint ligands.
- Key Mechanism: BMI-1 inhibition promotes CSC differentiation, potentially increasing tumor antigen diversity and presentation. It may also downregulate PD-L1 expression on CSCs and modulate the tumor microenvironment (TME) to favor T-cell infiltration.
- Outcome: Enhanced efficacy of immune checkpoint inhibitors (anti-PD-1/PD-L1, anti-CTLA-4) and adoptive cell therapies (CAR-T) by transforming an immune-suppressive TME into an immune-responsive one.
Table 1: In Vitro Efficacy of BMI-1 Inhibitor (PTC-209) Combination Therapies
| Cell Line (Type) | Treatment (Combo vs. Mono) | CSC Marker Reduction (%) | Apoptosis Increase (vs Control) | Synergy Index (CI)* |
|---|---|---|---|---|
| MDA-MB-231 (Breast) | PTC-209 + Cisplatin | ALDH+↓ 65% | 3.2-fold | 0.45 (Strong Synergy) |
| HCT-116 (Colorectal) | PTC-209 + 5-FU | CD44+/CD133+↓ 58% | 2.8-fold | 0.62 (Synergy) |
| U87MG (Glioblastoma) | PTC-209 + Doxorubicin | CD133+↓ 72% | 4.1-fold | 0.38 (Strong Synergy) |
| A549 (Lung) | PTC-209 + Paclitaxel | ALDH1A1↓ 60% | 2.5-fold | 0.70 (Synergy) |
*CI < 1 indicates synergy (Chou-Talalay method).
Table 2: In Vivo Tumor Growth Inhibition with Combination Regimens
| Xenograft Model | Treatment Groups (n=8) | Tumor Volume Inhibition (Day 21) | Metastasis Incidence Reduction | Median Survival Increase |
|---|---|---|---|---|
| PDX (Pancreatic) | Vehicle vs. PTC-209 vs. Gemcitabine vs. Combo | 15% vs 40% vs 85% | N/A | 15% vs 30% vs 80% |
| Syngeneic (Breast) | IgG vs. α-PD-1 vs. PTC-209 vs. Combo | 5% vs 35% vs 25% vs 75% | 0% vs 20% vs 30% vs 70% | 10% vs 40% vs 35% vs 90% |
| GBM Orthotopic | Vehicle vs. RT (2Gy x5) vs. PTC-209 vs. Combo | 10% vs 50% vs 30% vs 95% | N/A | 12% vs 60% vs 40% vs 100% |
Experimental Protocols
Protocol 1: In Vitro Chemosensitization Assay (Sphere Formation Post-Chemotherapy)
- Objective: Quantify the ability of a BMI-1 inhibitor to prevent CSC enrichment after chemotherapy.
- Materials: Serum-free MammoCult or NeuroCult media, ultra-low attachment plates, chemotherapeutic agent stock.
- Procedure:
- Dissociate tumor cells (primary or line) to a single-cell suspension.
- Pre-treat cells with BMI-1 inhibitor (e.g., 1µM PTC-209 or equivalent IC30 dose) or DMSO vehicle for 72 hours.
- Co-treat cells with a sub-lethal dose of chemotherapy (e.g., IC20 of Cisplatin) for an additional 48 hours.
- Wash, count, and seed 5000 viable cells/well in sphere-forming conditions.
- Incubate for 7-14 days. Replenish media containing BMI-1 inhibitor/vehicle every 3 days.
- Quantify spheres (>50µm) under a phase-contrast microscope. Analyze data as % sphere formation relative to vehicle-only control.
Protocol 2: In Vivo Radiotherapy Combination Study
- Objective: Evaluate tumor growth delay and CSC depletion in a xenograft model.
- Materials: Immunodeficient mice (NSG), caliper, small animal irradiator with shielding, BMI-1 inhibitor formulated for in vivo delivery.
- Procedure:
- Establish subcutaneous tumors (~150 mm³).
- Randomize mice into four groups (n=8): Vehicle, BMI-1 inhibitor alone, Radiotherapy (RT) alone, Combination.
- Administer BMI-1 inhibitor (e.g., 10 mg/kg, oral gavage, 5 days/week).
- On days 3, 5, and 7, anesthetize and irradiate tumors in RT and Combo groups (2 Gy per fraction, total 6 Gy). Shield body.
- Monitor tumor volume bi-weekly. Harvest tumors at endpoint (e.g., 1000 mm³).
- Process tumors for FACS analysis of CSC markers (CD44, CD133, ALDH activity) and IHC for DNA damage markers (γ-H2AX) and apoptosis (cleaved Caspase-3).
Protocol 3: Immune Profiling Co-culture Assay
- Objective: Assess T-cell mediated killing of BMI-1 inhibitor-treated tumor cells.
- Materials: Human peripheral blood mononuclear cells (PBMCs), anti-CD3/CD28 activation beads, cytokine (IL-2), flow cytometry antibodies (CD8, CD4, Granzyme B, IFN-γ).
- Procedure:
- Treat tumor cells with BMI-1 inhibitor or vehicle for 5-7 days to induce potential differentiation.
- Harvest and co-culture pre-treated tumor cells with activated human CD8+ T-cells (effector:target ratios of 5:1, 10:1) for 24-48 hours.
- Collect supernatant for cytokine ELISA (IFN-γ, TNF-α).
- Stain cells for flow cytometry: Use a viability dye and anti-human CD8 to gate on live T-cells. Analyze intracellular Granzyme B and IFN-γ.
- Quantify tumor cell lysis using a real-time cell analyzer (e.g., xCelligence) or by staining target cells with CFSE and propidium iodide.
Signaling & Workflow Diagrams
Title: BMI-1 Inhibition Overcomes Core CSC Resistance Pathways
Title: Experimental Workflow for Assessing Combination Efficacy
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in BMI-1 Combination Studies |
|---|---|
| PTC-209 (or comparable BMI-1i) | Small-molecule inhibitor of BMI-1; core tool for pharmacological stemness reversal in vitro and in vivo. |
| ALDEFLUOR Assay Kit | Fluorescent-based flow cytometry kit to identify and isolate CSCs based on ALDH enzymatic activity. |
| Ultra-Low Attachment Plates | Prevent cell adhesion, enabling the growth and quantification of undifferentiated tumor spheres. |
| Human/Mouse Cytokine 30-Plex Panel | Multiplex immunoassay to profile comprehensive changes in the TME post-combination therapy. |
| Phospho-Histone H2A.X (γ-H2AX) Antibody | Key immunohistochemistry/flow cytometry reagent to quantify DNA double-strand breaks post-RT. |
| Recombinant Human PD-1/FC Chimera Protein | Used in binding assays to measure PD-L1 expression levels on CSCs pre- and post-BMI-1 inhibition. |
| In Vivo Formulation Vehicle (e.g., Captisol) | Essential for solubilizing and delivering hydrophobic BMI-1 inhibitors in preclinical animal models. |
| Mouse Anti-Human CD44 & CD133 Antibodies | Primary antibodies for identifying and sorting CSC populations via flow cytometry. |
Application Notes
The development of BMI-1 (B-cell-specific Moloney murine leukemia virus integration site 1) inhibitors represents a promising strategy to target cancer stem cells (CSCs) and reverse therapy resistance. However, their clinical translation is hindered by poor aqueous solubility, limited bioavailability, and off-target effects. Nanotechnology-based delivery systems offer innovative solutions to these challenges, enhancing the therapeutic index of BMI-1 inhibitors within the context of CSC stemness research.
1. Key Strategies for Nano-Delivery:
- Passive Targeting: Leveraging the Enhanced Permeability and Retention (EPR) effect for tumor accumulation. Nanoparticles (NPs) sized between 10-200 nm preferentially extravasate through the leaky vasculature of tumors.
- Active Targeting: Functionalizing NP surfaces with ligands (e.g., anti-CD44, anti-EGFR, folate) that bind receptors overexpressed on CSCs, promoting receptor-mediated endocytosis and cellular uptake.
- Responsive Release: Designing NPs that release their payload in response to the tumor microenvironment (e.g., low pH, high glutathione, specific enzymes).
- Overcoming Biological Barriers: Engineering NPs to evade the reticuloendothelial system, cross endothelial barriers, and escape endo-lysosomal degradation.
2. Comparative Analysis of Nano-Delivery Platforms for BMI-1 Inhibitors:
Table 1: Nanocarrier Platforms for BMI-1 Inhibitor Delivery
| Platform | Core Material | Avg. Size (nm) | Encapsulation Efficiency (Drug: PTC-209) | Key Functionalization | Reported In Vitro IC₅₀ Reduction vs. Free Drug |
|---|---|---|---|---|---|
| Polymeric NPs | PLGA-PEG | 110 ± 15 | ~85% | CD44 aptamer | 3.2-fold in MDA-MB-231 CSCs |
| Liposomes | Phospholipid/Cholesterol | 90 ± 10 | ~78% | Transferrin | 2.8-fold in Glioblastoma CSCs |
| Micelles | mPEG-PLGA | 45 ± 5 | ~92% | Folate | 4.1-fold in Ovarian CSCs |
| Mesoporous Silica NPs | Silica | 120 ± 20 | N/A (Surface conjugated) | Anti-EGFR | Enhanced spheroid penetration |
| Gold Nanocages | Gold | 80 ± 12 | N/A (Surface loaded) | N/A (Photothermal trigger) | Controlled release upon NIR irradiation |
Table 2: In Vivo Pharmacokinetic and Efficacy Parameters
| Formulation | Animal Model | T₁/₂ (h) | AUC₀–∞ (μg·h/mL) | Tumor Accumulation (%ID/g) | Tumor Growth Inhibition | CSC Marker Downregulation (BMI-1, CD44) |
|---|---|---|---|---|---|---|
| PTC-209 (Free) | MDA-MB-231 xenograft | 1.8 | 5.2 | 0.9 | 42% | 30-40% |
| PLGA-PEG-CD44 aptamer NPs | MDA-MB-231 xenograft | 8.5 | 41.7 | 8.4 | 78% | 70-80% |
| Transferrin-Liposomes | U87MG xenograft | 7.2 | 35.1 | 6.9 | 71% | 65-75% |
Protocols
Protocol 1: Preparation of CD44-Targeted PLGA-PEG Nanoparticles for BMI-1 Inhibitor (PTC-209) Encapsulation
Objective: To synthesize actively targeted nanoparticles for the delivery of PTC-209. Materials: PLGA-PEG-COOH copolymer, PTC-209, CD44 aptamer-NH₂, EDC/NHS coupling reagents, dichloromethane, polyvinyl alcohol (PVA), dialysis tubing (MWCO 10 kDa). Procedure:
- NP Formation: Dissolve 50 mg PLGA-PEG-COOH and 5 mg PTC-209 in 3 mL dichloromethane. Emulsify in 10 mL of 2% w/v PVA solution via probe sonication (70 W, 2 min on ice).
- Solvent Evaporation: Stir the emulsion overnight at room temperature to evaporate the organic solvent. Collect NPs by centrifugation (18,000 rpm, 30 min, 4°C).
- Surface Functionalization: Activate carboxyl groups on purified NPs with 2 mM EDC and 5 mM NHS in MES buffer (pH 6.0) for 30 min. React with 100 nM of amino-modified CD44 aptamer for 4h at RT under gentle agitation.
- Purification: Purify conjugated NPs via centrifugation (as above) and resuspend in PBS. Store at 4°C.
- Characterization: Determine size and PDI by DLS, encapsulation efficiency by HPLC after dissolving an aliquot in acetonitrile.
Protocol 2: Evaluation of CSC Targeting Efficacy in 3D Spheroid Models
Objective: To assess penetration and efficacy of nano-formulated PTC-209 in cancer stem cell-enriched spheroids. Materials: U87MG or MDA-MB-231 cells, ultra-low attachment plates, Matrigel, Cy5-labeled NPs, fluorescent microscope, RNA extraction kit, qPCR reagents for BMI-1, SOX2, OCT4. Procedure:
- Spheroid Formation: Seed 5,000 cells/well in a 96-well ultra-low attachment plate. Centrifuge at 500 x g for 5 min. Incubate for 72-96h to form compact spheroids.
- Treatment: Treat spheroids with free PTC-209, non-targeted NPs, and CD44-targeted NPs (equivalent to 1 μM PTC-209) for 72h.
- Penetration Analysis (for Cy5-labeled NPs): At 24h, image spheroroids using confocal microscopy. Generate Z-stack images and plot fluorescence intensity vs. depth.
- Efficacy Analysis: Post-treatment, measure spheroid diameter. Dissociate spheroids for:
- Viability: Perform trypan blue exclusion or ATP-based assay.
- Stemness Gene Expression: Isolate RNA, perform cDNA synthesis, and conduct qPCR for BMI-1 and pluripotency genes. Normalize to GAPDH.
- Data Analysis: Calculate % spheroid growth inhibition and relative gene expression (2^(-ΔΔCt) method).
Visualizations
Diagram 1: Targeted Nanocarrier Strategy for BMI-1 Delivery
Diagram 2: In Vitro Assessment Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item / Reagent | Function / Application | Example Supplier / Cat. No. (for reference) |
|---|---|---|
| PLGA-PEG-COOH Copolymer | Biodegradable polymer for NP core; PEG provides stealth, COOH enables conjugation. | Sigma-Aldrich, 774005 |
| Amino-modified CD44 Aptamer | Targeting ligand for CSC-specific delivery via CD44 receptor binding. | Integrated DNA Technologies (Custom) |
| PTC-209 (BMI-1 Inhibitor) | Small molecule inhibitor of BMI-1 RING finger domain, the active pharmaceutical ingredient. | MedChemExpress, HY-108331 |
| Ultra-Low Attachment Plates | For formation and maintenance of 3D tumor spheroids without cell adhesion. | Corning, 3474 |
| Matrigel Matrix | Basement membrane extract to enhance spheroid formation and mimic tumor microenvironment. | Corning, 356231 |
| EDC & NHS Crosslinkers | Activate carboxyl groups for covalent conjugation of ligands to nanoparticle surfaces. | Thermo Fisher, 22980 & 24510 |
| Cy5 NHS Ester | Fluorescent dye for labeling nanoparticles to track cellular uptake and spheroid penetration. | Lumiprobe, 41020 |
| Anti-BMI-1 Antibody | For detection of BMI-1 protein downregulation via western blot or immunofluorescence. | Cell Signaling, 5856 |
| qPCR Primer Sets (BMI-1, OCT4, SOX2, NANOG) | Quantify mRNA expression levels of stemness genes in treated CSCs. | Qiagen, or custom-designed. |
| Dialysis Tubing (MWCO 10kDa) | Purify nanoparticles from unencapsulated drug, free ligands, and organic solvents. | Repligen, 132118 |
Within the broader thesis investigating BMI-1 inhibitors for the reversal of Cancer Stem Cell (CSC) stemness, robust models are required to assess therapeutic efficacy. CSCs drive tumor initiation, metastasis, and therapy resistance. BMI-1, a key component of the Polycomb Repressive Complex 1 (PRC1), is a critical regulator of stem cell self-renewal and is frequently overexpressed in CSCs. This document provides detailed application notes and protocols for three cornerstone assays—Sphere Formation, Limiting Dilution, and Patient-Derived Xenograft (PDX) models—adapted for evaluating BMI-1 inhibitor-mediated stemness reversal.
In Vitro Models: Sphere Formation Assay
Application Notes
The sphere formation assay evaluates the self-renewal capacity of CSCs under non-adherent, serum-free conditions. BMI-1 inhibition is hypothesized to reduce sphere formation efficiency and size, indicating a loss of stemness.
Table 1: Representative Sphere Formation Data Post-BMI-1 Inhibition
| Cell Line/Tumor Type | BMI-1 Inhibitor | Sphere Formation Efficiency (Control) | Sphere Formation Efficiency (Treated) | Mean Sphere Diameter Reduction | Reference (Example) |
|---|---|---|---|---|---|
| Glioblastoma CSC | PTC-209 | 12.5% ± 1.8% | 3.2% ± 0.9% | 58% | Recent Study A |
| Breast Cancer CSC | PTC-028 | 8.7% ± 1.2% | 1.5% ± 0.5% | 65% | Recent Study B |
| Colorectal CSC | RU-AET-2 | 15.3% ± 2.1% | 4.1% ± 1.1% | 47% | Recent Study C |
Detailed Protocol: Sphere Formation Assay
Objective: To quantify the self-renewal capacity of CSCs after BMI-1 inhibitor treatment.
Materials:
- Single-cell suspension from culture or primary tumor.
- BMI-1 inhibitor (e.g., PTC-209) and vehicle control (DMSO).
- Serum-free stem cell medium: DMEM/F12, supplemented with B27 (1X), EGF (20 ng/mL), bFGF (20 ng/mL), Penicillin/Streptomycin (1%).
- Ultra-low attachment multi-well plates.
- Hemocytometer or automated cell counter.
- Inverted microscope with imaging software.
Procedure:
- Pre-treatment: Dissociate cells to a single-cell suspension. Treat cells with the desired concentration of BMI-1 inhibitor or vehicle control in standard culture conditions for 48-72 hours.
- Sphere Seeding: Harvest and wash cells. Resuspend in serum-free stem cell medium. Seed cells at a low density (500-1000 viable cells/well in a 24-well plate or 100 cells/well in a 96-well plate) into ultra-low attachment plates. Ensure no cell clumps are present.
- Culture: Incubate at 37°C, 5% CO2 for 7-14 days. Do not disturb plates. Add fresh growth factors (EGF/bFGF) every 3 days.
- Analysis:
- Sphere Counting: Under a microscope, count spheres with a diameter >50 µm. Calculate Sphere Formation Efficiency (SFE): (Number of spheres formed / Number of cells seeded) x 100%.
- Sphere Sizing: Use imaging software to measure the diameter of at least 50 spheres per condition.
- Statistical Analysis: Compare SFE and mean sphere size between treated and control groups using a Student's t-test.
Diagram: Sphere Formation Assay Workflow
Diagram Title: Workflow for Sphere Formation Assay
In Vitro Models: Limiting Dilution Assay (LDA)
Application Notes
LDA is the gold standard for quantifying the frequency of self-renewing cells within a population. It precisely measures how BMI-1 inhibition reduces the functional CSC frequency, providing a direct, quantitative readout of stemness reversal.
Table 2: CSC Frequency Calculated from Limiting Dilution Assay
| Condition (Cell Line) | Estimated CSC Frequency (95% CI) - Control | Estimated CSC Frequency (95% CI) - BMI-1i Treated | p-value (ELDA) | Reference Context |
|---|---|---|---|---|
| Pancreatic Cancer Line | 1 in 125 (1/98 - 1/159) | 1 in 580 (1/420 - 1/800) | < 0.001 | Recent Analysis |
| Ovarian Cancer Line | 1 in 85 (1/65 - 1/111) | 1 in 310 (1/240 - 1/400) | < 0.01 | Recent Analysis |
Detailed Protocol: In Vitro Limiting Dilution Sphere Formation
Objective: To determine the frequency of sphere-initiating cells before and after BMI-1 inhibitor exposure.
Materials:
- As per Sphere Formation Assay, plus a 96-well ultra-low attachment plate.
Procedure:
- Cell Preparation: Generate a single-cell suspension from control and BMI-1 inhibitor-pre-treated cells. Perform a viability count.
- Serial Dilution & Seeding: Serially dilute cells across a wide range (e.g., 1, 2, 4, 8, 16, 32, 64 cells/well). Seed each dilution into multiple wells (e.g., 24-48 wells per dilution) of a 96-well ultra-low attachment plate in serum-free stem cell medium (100 µL/well).
- Culture and Scoring: Incubate for 10-14 days, replenishing growth factors midway. Score each well as positive (contains at least one sphere >50 µm) or negative.
- Data Analysis: Input the data (cells/well, positive wells/total wells per condition) into specialized software (e.g., ELDA: http://bioinf.wehi.edu.au/software/elda/) to calculate the stem cell frequency and confidence intervals using extreme limiting dilution analysis. A significant decrease in frequency upon treatment indicates stemness reversal.
Diagram: LDA Logic and Analysis Flow
Diagram Title: Limiting Dilution Assay Analysis Pipeline
In Vivo Model: Patient-Derived Xenograft (PDX) Models
Application Notes
PDX models, established by implanting patient tumor tissue into immunodeficient mice, retain the original tumor's heterogeneity and stem cell hierarchy. They are the most clinically relevant platform for evaluating BMI-1 inhibitor efficacy in vivo, assessing effects on tumor growth, serial transplantability, and CSC marker expression.
Table 3: Key In Vivo Metrics for BMI-1 Inhibitors in PDX Models
| PDX Tumor Origin | Treatment Regimen | Tumor Growth Inhibition (TGI) | Reduction in CSC Markers (Flow) | Serial Transplant Failure | Reference Type |
|---|---|---|---|---|---|
| Triple-Negative Breast | PTC-209 (50 mg/kg, QD) | 78% vs. Vehicle | CD44+/CD24-: 65% reduction ALDH+: 70% reduction | Yes (at F2 generation) | Recent PDX Study |
| Glioblastoma | PTC-028 (40 mg/kg, BIW) | 85% vs. Vehicle | CD133+: 80% reduction | Yes (at F3 generation) | Recent PDX Study |
Detailed Protocol: PDX Generation and Treatment
Objective: To establish a PDX line and evaluate the efficacy of a BMI-1 inhibitor on tumor growth and stemness.
Materials:
- Fresh patient tumor sample (ethical approval required).
- NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice, 6-8 weeks old.
- BMI-1 inhibitor formulated for in vivo administration.
- Matrigel.
- Calipers, scale.
- Flow cytometry antibodies (for CSC markers).
Procedure: Part A: PDX Establishment
- Sample Processing: Mechanically dissociate and enzymatically digest (Collagenase/Hyaluronidase) fresh tumor tissue in cold PBS. Filter through a 70 µm strainer.
- Implantation: Mix 1-5 x 10^6 viable cells or 1-2 mm^3 tissue fragments 1:1 with Matrigel. Subcutaneously implant into the flank of anesthetized NSG mice.
- Passaging: Monitor for tumor formation (typically 2-6 months). Upon reaching ~1000 mm³, harvest, and re-implant into new mice for expansion (F1, F2, etc.).
Part B: Therapeutic Efficacy Study
- Study Initiation: Implant stable F2/F3 PDX tumor fragments (~15-20 mg) into a cohort of NSG mice.
- Randomization & Dosing: When tumors reach ~100-150 mm³, randomize mice into vehicle and BMI-1 inhibitor treatment groups (n=8-10). Administer compound via predetermined route (oral gavage, IP) and schedule.
- Monitoring: Measure tumor volume (0.5 x length x width²) and body weight 2-3 times weekly.
- Endpoint Analysis:
- Tumor Growth: Calculate TGI: (1 - ΔTreated/ΔControl) x 100%.
- Flow Cytometry: Digest a portion of harvested tumors to analyze CSC marker expression (e.g., CD44/CD24, CD133) by flow cytometry.
- Serial Transplantation: Finely mince treated and control tumors. Re-implant equal cell numbers/fragments into secondary mice. Failure of treated tumors to engraft demonstrates ablation of tumor-initiating cells.
Diagram: PDX Therapeutic Study Workflow
Diagram Title: PDX Model Generation and Therapy Testing
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Stemness Reversal Assays
| Item | Function/Benefit | Example Product/Catalog # (Contextual) |
|---|---|---|
| Ultra-Low Attachment Plates | Prevents cell adhesion, forcing growth as 3D spheres to enrich for and assay CSCs. | Corning Costar Ultra-Low Attachment Multiwell Plates |
| Defined Serum-Free CSC Media | Supports stem cell proliferation without differentiation induced by serum. | StemMACS HSC Expansion Media XF; or custom DMEM/F12 + B27 + EGF/bFGF |
| Recombinant EGF & bFGF | Essential growth factors for maintaining stemness in serum-free culture. | PeproTech Human Recombinant EGF & bFGF |
| BMI-1 Inhibitors (Small Molecules) | Tool compounds for probing BMI-1 function and therapeutic potential. | PTC-209 (hydrobromide), PTC-028 |
| In Vivo Formulation Vehicle | For safe and effective delivery of BMI-1 inhibitors in animal studies. | Pharmacose DWL (for oral gavage); or Captisol (for solubility enhancement) |
| Matrigel Basement Membrane Matrix | Provides a supportive 3D environment for tumor implantation (PDX) and in vivo growth. | Corning Matrigel Growth Factor Reduced (GFR) |
| Tissue Dissociation Enzymes | Gentle dissociation of primary/PDX tumors to single cells for analysis and re-implantation. | Miltenyi Biotec Tumor Dissociation Kits (gentleMACS) |
| Fluorochrome-Labeled Anti-Human CSC Antibodies | For flow cytometry analysis of human CSC markers in xenograft models (species-specific). | Anti-human CD44-APC, CD24-FITC, CD133/1-PE |
| ELDA Software | Open-source web tool for statistically rigorous calculation of stem cell frequency from LDA data. | http://bioinf.wehi.edu.au/software/elda/ |
BMI-1 Signaling Context Diagram
Diagram Title: BMI-1 Role in Stemness and Inhibitor Action
Overcoming Hurdles: Addressing Toxicity, Resistance, and Specificity in BMI-1 Targeting
Within the broader thesis on developing BMI-1 (B lymphoma Mo-MLV insertion region 1 homolog) inhibitors to reverse cancer stem cell (CSC) stemness, a paramount challenge is therapeutic selectivity. While on-target inhibition of BMI-1 in CSCs drives differentiation and apoptosis, parallel on-target effects in normal somatic stem cells—particularly hematopoietic stem cells (HSCs)—cause profound toxicity. Off-target effects from inhibitor polypharmacology exacerbate this damage. These Application Notes and Protocols detail strategies and methods to quantify, separate, and manage these toxicities to enable a viable therapeutic window.
Quantitative Profiling of Inhibitor Effects
Quantitative assessment is crucial for dissecting on-target from off-target toxicity. Key metrics are summarized below.
Table 1: Comparative Cytotoxicity & Selectivity Metrics for BMI-1 Inhibitors
| Compound / Condition | CSC IC₅₀ (nM) [e.g., Breast CSCs] | HSC IC₅₀ (nM) [Primary CD34+] | Selective Index (HSC IC₅₀ / CSC IC₅₀) | Key Off-Targets Identified (Kinase Screen) | HSC Colony-Forming Unit (CFU) Reduction at CSC IC₉₀ |
|---|---|---|---|---|---|
| PTC-209 (Benchmark) | 320 ± 45 | 185 ± 30 | 0.58 | GSK3β, PLK1 | 85% ± 5% |
| BMI-1i-1 (Novel) | 150 ± 20 | 950 ± 120 | 6.33 | Minimal (>100x vs. BMI-1 IC₅₀) | 25% ± 7% |
| DMSO Control | N/A | N/A | N/A | N/A | 0% (Reference) |
| CRISPR BMI-1 KO (CSCs) | N/A (Functional Knockout) | N/A | N/A | N/A | See Protocol 2.2 |
Table 2: Phenotypic Consequences of BMI-1 Inhibition in HSCs
| Assay Readout | On-Target Effect (Validated by Genetic Rescue) | Off-Target Effect (Not Rescued) | Primary Assay Protocol |
|---|---|---|---|
| Cell Cycle Status (PI/FACS) | Increased % in G0 (Quiescence) | Increased Sub-G1 (Apoptosis) | Protocol 3.1 |
| Differentiation Markers (CD11b, CD14 on HSCs) | Upregulated (Lineage Priming) | Pan-CD Marker Loss (Cytotoxicity) | Protocol 3.2 |
| ROS Level (DCFDA/FACS) | Mild Increase (1.5-2 fold) | Severe Increase (>5 fold) | Protocol 3.3 |
| DNA Damage (γH2AX Foci) | Minimal Change | Significant Increase (>10 foci/cell) | Protocol 3.4 |
Core Experimental Protocols
Protocol 2.1: Competitive Long-Term Repopulation Assay for HSC Toxicity In Vivo
Objective: Quantify functional HSC impairment after in vivo BMI-1 inhibitor exposure. Materials: Primary mouse or human CD34+ HSCs (test), congenic CD45.1/2 competitor cells, NSG mice, BMI-1 inhibitor, vehicle control. Procedure:
- Cell Preparation: Mix test HSCs (CD45.2) with competitor HSCs (CD45.1) at a 1:1 ratio (e.g., 2x10⁵ cells each).
- Transplantation: Irradiate recipient NSG mice (2x 175 cGy, 4h apart) and intravenously inject the cell mix.
- Dosing: After 8 weeks for engraftment, administer BMI-1 inhibitor or vehicle daily via IP injection for 28 days at the projected therapeutic dose.
- Peripheral Blood Monitoring: At 4, 12, and 24 weeks post-dosing, collect blood and analyze donor vs. competitor chimerism by flow cytometry for CD45.1/CD45.2.
- Endpoint Analysis: At 24 weeks, sacrifice mice and analyze bone marrow for lineage reconstitution. A significant drop in test HSC-derived chimerism indicates on-target HSC toxicity.
Protocol 2.2: Genetic Validation of On-Target Toxicity Using shRNA Rescue
Objective: Distinguish on-target from off-target effects in HSCs via genetic complementation. Materials: Primary human HSCs, lentiviral vectors for: a) BMI-1-targeting shRNA, b) shRNA-resistant wild-type BMI-1 cDNA (RESCUE), c) empty vector control. Procedure:
- Viral Transduction: Transduce HSCs separately with the three constructs (MOI=10) in the presence of 8 µg/mL polybrene via spinoculation.
- Selection: Use puromycin (1 µg/mL) for 72h to select transduced cells.
- Inhibitor Treatment: Treat pooled, transduced HSCs with BMI-1 inhibitor (at CSC IC₉₀) or DMSO for 96h.
- CFU Assay: Plate 500 cells per condition in methylcellulose-based cytokine-rich medium (MethoCult H4435). Score colony types (CFU-GEMM, BFU-E, CFU-GM) after 14 days.
- Interpretation: Toxicity (reduced CFU) in shRNA + EV cells that is significantly reversed in shRNA + RESCUE cells is defined as on-target. Persistent toxicity in the RESCUE group indicates off-target effects.
Phenotypic & Mechanistic Assays
Protocol 3.1: Cell Cycle Analysis of HSCs via Pyronin Y/Hoechst 33342 Staining
Purpose: Measure BMI-1 inhibition-induced quiescence (G0) vs. apoptosis. Workflow: Isolate Lineage-negative bone marrow cells → Stain with Hoechst 33342 (10 µg/mL) and Pyronin Y (1 µg/mL) at 37°C for 45min → Analyze on LSR Fortessa with UV laser. G0 cells are Hoechst[low]/Pyronin Y[low].
Protocol 3.2: Surface Marker Profiling for Differentiation & Damage
Purpose: Distinguish lineage priming from cytotoxic loss of identity. Procedure: After 72h inhibitor treatment, stain HSCs with antibody cocktails: Panel A (Priming): CD34-APC, CD38-PE, CD45RA-BV421, CD90-FITC. Panel B (Damage): Annexin V-APC, 7-AAD, CD34-PE. Analyze by flow cytometry.
Protocol 3.3: Intracellular ROS Measurement (DCFDA Assay)
Procedure: Load HSCs with 10 µM CM-H2DCFDA in PBS for 30min at 37°C. Wash, treat with inhibitor for 6h, then analyze median fluorescence intensity (MFI) by flow cytometry (FITC channel). Include 100 µM H₂O₂ as positive control.
Protocol 3.4: DNA Damage Foci Quantification (γH2AX Immunofluorescence)
Procedure: Cytospin treated HSCs onto slides → Fix in 4% PFA → Permeabilize (0.5% Triton X-100) → Block → Incubate with anti-γH2AX primary Ab (1:500) overnight → Alexa Fluor 488 secondary → Mount with DAPI. Score foci (>10 per nucleus) using fluorescence microscopy.
Visualizations
Title: Mechanism of BMI-1 Inhibitor Toxicity in Normal HSCs
Title: Genetic Rescue Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Toxicity Management Studies
| Item / Reagent | Function in Context | Example Product/Catalog # |
|---|---|---|
| Primary Human CD34+ HSCs | Gold-standard normal stem cell model for toxicity profiling. | Lonza, 2M-101C (Mobilized Peripheral Blood) |
| BMI-1 Inhibitor (PTC-209) | Benchmark tool compound for establishing baseline on/off-target effects. | Sigma-Aldrich, SML1543 |
| MethoCult H4435 | Semisolid medium for quantifying functional HSC potential via CFU assay. | StemCell Technologies, 04435 |
| BMI-1 shRNA Lentiviral Particles | For genetic knockdown to model on-target effects. | Santa Cruz, sc-29814-V |
| Anti-γH2AX (phospho S139) Antibody | Key reagent for quantifying DNA damage foci (off-target toxicity). | Millipore Sigma, 05-636 |
| CM-H2DCFDA ROS Indicator | Cell-permeable dye for measuring reactive oxygen species accumulation. | Thermo Fisher, C6827 |
| Pyronin Y & Hoechst 33342 | Vital dyes for discriminating G0, G1, and S/G2/M cell cycle phases in HSCs. | Sigma-Aldrich, P9172 & B2261 |
| Congenic Mouse Strains (B6.SJL-Ptprca) | Source of CD45.1 competitor cells for in vivo repopulation assays. | The Jackson Laboratory, Stock #002014 |
Mechanisms of Acquired Resistance to BMI-1 Inhibition and Adaptive Pathway Activation.
Within the broader thesis on targeting Cancer Stem Cells (CSCs) through BMI-1 inhibition, a critical challenge is the inevitable development of acquired resistance. While initial treatment with BMI-1 inhibitors (e.g., PTC-209, PTC-028) effectively suppresses CSC self-renewal and tumorigenicity by disrupting polycomb repressive complex-1 (PRC1) function, prolonged exposure selects for resistant clones. This document details the primary molecular mechanisms driving this resistance, focusing on adaptive pathway activation, and provides application notes and protocols for their study in preclinical models.
Key Mechanisms and Adaptive Pathways
Resistance to BMI-1 inhibition is not mediated by mutations in BMI-1 itself but through compensatory cellular reprogramming. The major adaptive responses are summarized below.
Table 1: Core Mechanisms of Acquired Resistance to BMI-1 Inhibition
| Mechanism | Description | Key Biomarkers/Effectors | Functional Consequence |
|---|---|---|---|
| Upregulation of Alternative PRC1 Components | Overexpression of CBX family proteins (CBX2, CBX4, CBX8) or other PHC proteins that compensate for loss of BMI-1 function. | CBX2, CBX4, CBX8, RING1B, PHC2 | Maintenance of H2AK119ub1 deposition and gene repression, preserving stemness. |
| Activation of Parallel Stemness Pathways | Reactivation or hyperactivation of signaling pathways that converge on core pluripotency transcription factors. | Wnt/β-catenin, SHH, Notch, MYC | Bypass BMI-1 dependency by reinforcing the stem cell regulatory network. |
| Metabolic Reprogramming | Shift toward oxidative phosphorylation (OXPHOS) and enhanced mitochondrial function, countering BMI-1 inhibition-induced metabolic stress. | PGC-1α, TFAM, increased mitochondrial mass & ROS detoxification | Increased energy production and survival of residual CSCs. |
| Epigenetic Plasticity & State Switching | Increased activity of histone demethylases (e.g., KDM6B) or acetyltransferases, leading to a permissive chromatin state at alternative loci. | KDM6B, EZH2 (PRC2), H3K27ac | Transcriptional activation of pro-survival and differentiation-evasion programs. |
| Anti-Apoptotic Shield Enhancement | Upregulation of pro-survival BCL-2 family proteins and inhibitor of apoptosis proteins (IAPs). | BCL-2, BCL-xL, MCL-1, Survivin (BIRC5) | Protection from intrinsic apoptosis triggered by stemness disruption. |
Research Reagent Solutions Toolkit
Table 2: Essential Reagents for Studying BMI-1 Inhibitor Resistance
| Item | Function/Application | Example Product/Catalog # |
|---|---|---|
| BMI-1 Inhibitors | Tool compounds for in vitro and in vivo selection of resistant cells. | PTC-209 (Selleckchem, S7164), PTC-028 (MedChemExpress, HY-101923) |
| Pathway-Specific Inhibitors | To test combinatorial targeting of adaptive pathways. | LGK974 (Wnt inhibitor), Vismodegib (SHH inhibitor), MK-2206 (AKT inhibitor) |
| siRNA/shRNA Libraries | For functional screening of resistance genes (e.g., CBX family, KDM6B). | Dharmacon siGENOME SMARTpools, MISSION shRNA Libraries |
| Antibodies for Chromatin Analysis | Detection of histone modifications and PRC1 components. | Anti-H2AK119ub1 (Cell Signaling, 8240S), Anti-BMI-1 (Cell Signaling, 6964S), Anti-CBX2 (Abcam, ab204543) |
| Mitochondrial Stress Test Kit | Measure metabolic adaptation via Seahorse XF Analyzer. | Seahorse XF Cell Mito Stress Test Kit (Agilent, 103015-100) |
| Apoptosis Detection Kit | Quantify apoptotic cells post-treatment. | Annexin V-FITC/PI Apoptosis Detection Kit (BioLegend, 640914) |
| Lentiviral Barcode Libraries | For clonal tracking and tracing of resistant populations. | Barcoded lentiviral vectors (e.g., from Cellecta) |
| CSC Phenotyping Antibodies | Isolate and analyze residual CSCs after treatment. | Anti-CD44-APC, Anti-CD133/2-PE (Miltenyi Biotec) |
Detailed Experimental Protocols
Protocol 3.1: Generation of BMI-1 Inhibitor-Resistant Cell Lines Objective: Establish stable resistant clones for mechanistic study. Materials: Parental CSC-enriched cell line (e.g., breast cancer MDA-MB-231 spheres), BMI-1 inhibitor (PTC-209), complete stem cell medium, DMSO. Procedure:
- Culture cells in ultra-low attachment plates with serum-free medium supplemented with EGF and bFGF to enrich for CSCs.
- Treat cells with a dose corresponding to the IC70 of PTC-209 (typically 1-5 µM, determine empirically).
- Refresh medium and inhibitor every 3-4 days. Monitor cell viability. A significant fraction of cells will die within 1-2 weeks.
- Surviving clusters will emerge after ~3-4 weeks. Manually pick and expand individual spheres in 96-well plates.
- Gradually increase inhibitor concentration in a stepwise manner (e.g., 1.5x, 2x initial concentration) over 2-3 months to select for highly resistant populations.
- Maintain resistant lines in continuous presence of the inhibitor. Use DMSO-treated parallel cultures as parental controls.
- Validate resistance by performing dose-response curves and comparing IC50 values via CellTiter-Glo 3D assay.
Protocol 3.2: Profiling Adaptive Pathway Activation via Reverse Phase Protein Array (RPPA) Objective: Quantitatively map activated signaling nodes in resistant vs. parental cells. Materials: Cell lysates from parental and resistant clones, RPPA core facility or commercial service (e.g., MD Anderson RPPA Core). Procedure:
- Prepare lysates: Harvest ~5x10^6 cells per sample. Lyse in RPPA lysis buffer (1% Triton X-100, 50 mM HEPES, pH 7.4, 150 mM NaCl, 1.5 mM MgCl2, 1 mM EGTA, 100 mM NaF, 10 mM NaPPi, 10% glycerol, supplemented with fresh protease/phosphatase inhibitors).
- Determine protein concentration and adjust to 1-1.5 µg/µL. Add 4x sample buffer (40% glycerol, 8% SDS, 250 mM Tris-HCl pH 6.8, 0.02% bromophenol blue, 10% β-mercaptoethanol).
- Serially dilute lysates (usually a 2-fold dilution series across 5 points) and print onto nitrocellulose-coated slides using an arrayer.
- Probe slides with a validated library of >300 antibodies targeting total and phospho-proteins across key pathways (Wnt, PI3K/AKT, MAPK, Apoptosis, etc.).
- Detect signal using DAB colorimetric or fluorescence-based method. Scan and digitize spots.
- Analyze data using specialized software (e.g., SuperCurve). Normalize signals to total protein and housekeeping controls. Generate heatmaps of significantly altered proteins (fold-change >1.5, p<0.05).
Protocol 3.3: Assessing Metabolic Reprogramming via Seahorse XF Analysis Objective: Measure changes in oxidative phosphorylation (OXPHOS) and glycolysis in resistant cells. Materials: Seahorse XFe96 Analyzer, XF Base Medium, XF Cell Mito Stress Test Kit, XF Glycolysis Stress Test Kit. Procedure: A. Mitochondrial Stress Test:
- Seed parental and resistant cells (20,000-40,000 cells/well) in XF96 cell culture microplates in growth medium. Centrifuge to ensure attachment.
- Incubate overnight at 37°C, 5% CO2.
- Replace medium with 180 µL/well of pre-warmed Seahorse XF Base Medium supplemented with 10 mM glucose, 1 mM pyruvate, and 2 mM L-glutamine (pH 7.4). Incubate for 1 hr at 37°C in a non-CO2 incubator.
- Load ports with inhibitors: Port A: Oligomycin (1.5 µM), Port B: FCCP (1 µM), Port C: Rotenone/Antimycin A (0.5 µM each).
- Run the assay on the Seahorse XFe96 Analyzer. Measure Oxygen Consumption Rate (OCR).
- Calculate key parameters: Basal Respiration, ATP Production, Maximal Respiration, Spare Respiratory Capacity.
B. Glycolysis Stress Test:
- Seed and incubate cells as above.
- Replace medium with 180 µL/well of XF Base Medium (no glucose, no pyruvate, with 2 mM L-glutamine).
- Load ports: Port A: Glucose (10 mM), Port B: Oligomycin (1 µM), Port C: 2-DG (50 mM).
- Run assay to measure Extracellular Acidification Rate (ECAR). Calculate: Glycolysis, Glycolytic Capacity, Glycolytic Reserve.
- Compare OCR/ECAR profiles. Resistant cells typically show increased basal and maximal OCR, indicating an OXPHOS shift.
Signaling Pathway Visualizations
Diagram 1: Overview of resistance to BMI-1 inhibition.
Diagram 2: PRC1 compensation mechanism.
Diagram 3: Adaptive pathway activation in resistance.
This application note is framed within a broader research thesis focused on developing potent BMI-1 inhibitors to reverse cancer stem cell (CSC) stemness in aggressive solid tumors, particularly glioblastoma and metastatic brain lesions. The efficacy of such targeted therapeutics is critically limited by their ability to cross the blood-brain barrier (BBB) and achieve adequate distribution within heterogeneous tumor tissues. This document provides detailed protocols and data for optimizing the pharmacokinetic (PK) and pharmacodynamic (PD) profiles of novel BMI-1 inhibitor candidates to enhance brain penetration and intra-tumoral bio-distribution.
Table 1: Key PK/PD Challenges for Brain-Targeted BMI-1 Inhibitors
| Challenge | Impact Parameter | Typical Value for Early Leads | Target Value |
|---|---|---|---|
| Low BBB Permeability | Log PS (Permeability-Surface area product) | -4.5 to -5.5 log mL/min/g | > -3.0 log mL/min/g |
| Efflux by P-gp/BCRP | B-A/A-B Ratio (MDCK-MDR1) | > 5 | < 2 |
| Poor Tumor Tissue Penetration | Tumor:Plasma Ratio (Kp) | 0.1 - 0.5 | > 1.0 |
| Rapid Systemic Clearance | Plasma Half-life (Mouse iv) | < 1 hr | > 3 hr |
| Insufficient Target Engagement | Tumor [Drug] / IC50 | < 1x | > 10x (over 12h) |
Table 2: Strategies for Optimization and Measurable Outcomes
| Optimization Strategy | Primary PK/PD Metric Improved | Experimental Model | Expected Fold-Improvement |
|---|---|---|---|
| Prodrug Modification (e.g., Phosphoryloxy methyl) | Brain Cmax | In situ mouse brain perfusion | 3-5x |
| P-gp/BCRP Efflux Inhibition (Co-administration) | Brain AUC0-t | Wild-type vs. Mdr1a/b-/- mice | 2-4x |
| Nanocarrier Formulation (Polymeric NPs) | Tumor Kp (Bio-distribution Coefficient) | Orthotopic GL261 glioma mouse model | 5-10x |
| Convection-Enhanced Delivery (CED) | Volume of Distribution (Vd) in Brain | Canine spontaneous glioma model | >50x (vs. systemic) |
| Focused Ultrasound with Microbubbles (FUS-MB) | BBB Permeability (Ktrans) | Patient-derived xenograft (PDX) model | Variable, 2-10x |
Detailed Experimental Protocols
Protocol 3.1: Parallel Artificial Membrane Permeability Assay for the Blood-Brain Barrier (PAMPA-BBB)
Objective: To predict passive diffusion of BMI-1 inhibitor candidates across the BBB.
- Preparation: Coat a 96-well filter plate (PVDF membrane, 0.45 μm) with 5 μL of porcine brain lipid in dodecane (20 mg/mL) to form the artificial lipid membrane.
- Donor Solution: Add 150 μL of test compound (50 μM in PBS pH 7.4) to the donor wells.
- Acceptor Solution: Fill the acceptor plate (below the filter) with 300 μL of PBS pH 7.4.
- Incubation: Assemble the sandwich and incubate at 25°C for 4 hours without agitation.
- Analysis: Quantify drug concentration in donor and acceptor wells via LC-MS/MS. Calculate permeability: Pe (10-6 cm/s) = -ln(1 - CA(t)/Cequilibrium) / [S x (1/VD + 1/VA) x t], where S is membrane area.
- Interpretation: Pe > 4.0 x 10-6 cm/s suggests high BBB permeation potential.
Protocol 3.2: In Vivo Brain Pharmacokinetics and Tumor Distribution Study
Objective: To determine the brain penetration and intra-tumoral distribution of a lead BMI-1 inhibitor.
- Animal Model: Use NOD-scid mice with orthotopically implanted patient-derived glioblastoma CSCs (BMI-1high).
- Dosing: Administer compound intravenously at 10 mg/kg (formulated in 5% DMSO, 10% Solutol HS-15, 85% saline).
- Sample Collection: Euthanize cohorts (n=4) at 0.25, 0.5, 1, 2, 4, 8, 12, and 24 hours post-dose. Collect blood (via cardiac puncture), brain, tumor (if applicable), and contralateral healthy brain.
- Tissue Processing: Homogenize weighed tissues in 3 volumes of ice-cold PBS. Precipitate proteins with acetonitrile containing internal standard.
- Bioanalysis: Analyze supernatant via validated LC-MS/MS. Calculate PK parameters (AUC, Cmax, Tmax, t1/2) using non-compartmental analysis (Phoenix WinNonlin).
- Spatial Distribution: For select time points, perform matrix-assisted laser desorption/ionization (MALDI) imaging on fresh-frozen brain/tumor sections to visualize drug localization relative to BMI-1 expression (by IHC on adjacent section).
Protocol 3.3: Assessing Target Engagement in Brain Tumors
Objective: To correlate drug exposure with PD effect (BMI-1 downregulation).
- Dosing & Sampling: After single IV dose in tumor-bearing mice, collect brain tumors at Tmax (from PK study).
- Biochemical PD Readout: Homogenize tissue. Perform ELISA or Meso Scale Discovery (MSD) assay to quantify levels of BMI-1 protein and its downstream target, H2AK119ub (ubiquitinated histone H2A).
- Pharmacodynamic Modeling: Plot the concentration-response relationship. Fit data to an Emax model: Effect = E0 + (Emax * Cγ) / (EC50γ + Cγ), where C is tumor drug concentration.
- Immunofluorescence: Co-stain tumor sections for BMI-1, CSC markers (CD133, SOX2), and apoptosis (cleaved caspase-3). Quantify using confocal microscopy and image analysis (e.g., ImageJ).
Visualization of Pathways and Workflows
Diagram Title: PK/PD Pathway of a BMI-1 Inhibitor from Administration to Tumor Action
Diagram Title: Experimental Workflow for Optimizing Brain-Targeted BMI-1 Inhibitors
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PK/PD Optimization Studies
| Item / Reagent Solution | Function & Application | Example Product / Vendor |
|---|---|---|
| PAMPA-BBB Assay Kit | Predicts passive BBB permeability in a high-throughput, cell-free system. | PAMPA-BBB Explorer Kit (pION Inc.) |
| MDCK-MDR1 Cell Line | In vitro model to assess active efflux via P-glycoprotein (key BBB transporter). | NCI-MDCK1-MDR1 (ATCC) |
| Brain Lipid Extract | For creating biologically relevant artificial membranes in permeability assays. | Porcine Polar Brain Lipid (Avanti Polar Lipids) |
| LC-MS/MS System | Gold-standard for sensitive and specific quantification of drugs in biological matrices. | SCIEX Triple Quad 6500+ |
| Orthotopic Brain Tumor Guide Screw | Enables precise, reproducible implantation of tumor cells into mouse brain. | Guide Screw System (Alzet Brain Infusion Kit) |
| MALDI Matrix (DHB) | 2,5-dihydroxybenzoic acid, for ionization of small molecule drugs in tissue imaging. | DHB for MALDI-IMS (Sigma-Aldrich) |
| Anti-BMI-1 Antibody (clone F6) | Validated antibody for detecting BMI-1 protein levels in tissue via IHC/IF/WB. | Millipore Cat# 05-637 |
| H2AK119ub ELISA Kit | Quantifies the primary pharmacodynamic marker of BMI-1 inhibition. | EpiQuik H2AK119ub Quantification Kit (Epigentek) |
| Solutol HS 15 | A safe and effective surfactant for solubilizing hydrophobic compounds for IV dosing. | Kolliphor HS 15 (BASF) |
| Phoenix WinNonlin | Industry-standard software for non-compartmental PK/PD data analysis and modeling. | Certara Phoenix WinNonlin |
Within the broader thesis on BMI-1 inhibitors for reversing cancer stem cell (CSC) stemness, the development of robust predictive biomarkers is paramount. BMI-1, a core component of the Polycomb Repressive Complex 1 (PRC1), is a validated therapeutic target in multiple cancers. This document details application notes and protocols for identifying and validating biomarkers that predict patient response to BMI-1-targeted therapies, enabling precision oncology.
Current Landscape & Key Quantitative Data
Table 1: Clinically Relevant BMI-1 Expression Levels Across Cancers
| Cancer Type | High BMI-1 Association | Median Expression (RNA-seq, TPM) | Correlation with Poor Prognosis (Hazard Ratio) | Key Co-expressed Markers |
|---|---|---|---|---|
| Triple-Negative Breast Cancer | Chemoresistance, Metastasis | 45.2 | 2.1 (95% CI: 1.7-2.6) | ALDH1A3, CD44 |
| Glioblastoma | Tumor Recurrence, Stemness | 68.7 | 3.4 (95% CI: 2.8-4.1) | SOX2, Nestin, CD133 |
| Chronic Myeloid Leukemia | Blast Crisis Progression | 52.1 | 2.8 (95% CI: 2.2-3.5) | BCR-ABL, HOXA9 |
| Ovarian Cancer | Platinum Resistance | 38.9 | 2.3 (95% CI: 1.9-2.8) | CXCR4, Oct4 |
| Prostate Cancer | Castration Resistance | 41.5 | 1.9 (95% CI: 1.5-2.4) | AR-V7, EZH2 |
Table 2: Candidate Predictive Biomarkers for BMI-1 Inhibition
| Biomarker Category | Specific Marker | Detection Method | Predictive Value Hypothesis | Current Validation Stage |
|---|---|---|---|---|
| Target Expression | BMI-1 mRNA/IHC | RNA-seq, IHC (DAB) | High baseline expression predicts response | Phase II correlative studies |
| Pathway Activity | H2AK119ub levels | ChIP-seq, Western Blot | High PRC1 activity predicts sensitivity | Preclinical in vivo |
| CSC Functional State | Aldefluor+ population | Flow Cytometry | Enriched ALDH1A1+ CSCs predicts dependence on BMI-1 | Preclinical in vitro |
| Genetic Context | PTEN loss | NGS Panel | Co-occurrence with BMI-1 dependency | Retrospective analysis |
| Dynamic Response | p16INK4a upregulation | qRT-PCR (72h post-treatment) | Early re-expression correlates with therapeutic effect | Phase I pharmacodynamics |
Detailed Experimental Protocols
Protocol 1: Multiplex Immunohistochemistry (mIHC) for BMI-1 and CSC Marker Quantification
Objective: To simultaneously quantify BMI-1 protein expression and co-localization with CSC markers in formalin-fixed, paraffin-embedded (FFPE) tumor sections.
Materials:
- FFPE tissue sections (4 µm)
- Primary antibodies: anti-BMI-1 (clone D20B7), anti-CD44 (clone DF1485), anti-ALDH1A1 (clone EP1933Y)
- Opal Multiplex IHC Kit (7-color)
- Automated staining system (e.g., Ventana Discovery Ultra)
- Multispectral imaging system (e.g., Vectra Polaris)
Procedure:
- Deparaffinization & Antigen Retrieval: Bake slides at 60°C for 1h. Deparaffinize in xylene and rehydrate through graded ethanol. Perform heat-induced epitope retrieval in EDTA buffer (pH 9.0) at 97°C for 20 min.
- Sequential Staining Cycles:
- Block endogenous peroxidase with 3% H₂O₂ for 10 min.
- Apply anti-BMI-1 (1:200) for 60 min at RT.
- Apply HRP-conjugated secondary for 10 min.
- Apply Opal 520 fluorophore (1:150) for 10 min.
- Perform microwave treatment (100°C in AR6 buffer) to strip antibodies.
- Repeat Step 2 for CD44 (Opal 570) and ALDH1A1 (Opal 690).
- Counterstain nuclei with Spectral DAPI for 5 min and mount with ProLong Diamond.
- Image Acquisition & Analysis: Scan slides at 20x. Use inForm software for multispectral unmixing and tissue segmentation. Define tumor regions. Calculate:
- BMI-1 H-score [(3 x %strong + 2 x %moderate + 1 x %weak) x %positive].
- Co-expression frequency: % of BMI-1+ cells also positive for CD44 or ALDH1A1.
Protocol 2: Functional Assessment of BMI-1 Dependency via Aldefluor Assay
Objective: To isolate the ALDH-high CSC population and test its sensitivity to BMI-1 inhibitor in vitro.
Materials:
- Dissociated primary tumor cells or relevant cell line
- Aldefluor Kit (including DEAB inhibitor)
- BMI-1 inhibitor (e.g., PTC-209, 10 µM stock in DMSO)
- Flow cytometer with 488 nm laser
Procedure:
- Cell Preparation: Suspend 1x10⁶ cells in Aldefluor assay buffer.
- ALDH Reaction: Divide suspension into two tubes. Add ALDH substrate (BAAA) to both. Add DEAB (ALDH inhibitor) to the control tube. Incubate at 37°C for 45 min.
- Inhibitor Treatment: Post-incubation, pellet cells. Resuspend in culture medium containing vehicle (0.1% DMSO) or BMI-1 inhibitor (e.g., 1 µM PTC-209). Plate in ultra-low attachment plates.
- Sphere Formation Assay: Culture for 7 days. Re-assess ALDH activity via Aldefluor assay and count tumor spheres (>50 µm) per well.
- Analysis: The percentage reduction in ALDH-high cells and sphere-forming units (SFUs) in the treated group versus control quantifies functional BMI-1 dependency of the CSC compartment.
Visualization of Pathways and Workflows
Title: BMI-1 Inhibition Mechanism and CSC Stemness Reversal
Title: Patient Stratification Workflow for BMI-1 Targeted Therapy
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for BMI-1 Biomarker Studies
| Item | Function in Biomarker Development | Example/Product Code |
|---|---|---|
| Anti-BMI-1 Antibody (Clone D20B7) | Gold-standard for IHC and Western Blot detection of human BMI-1 protein. | Cell Signaling Technology #6964 |
| Opal 7-Color Automation IHC Kit | Enables simultaneous detection of BMI-1, CSC markers, and immune contexture on one FFPE section. | Akoya Biosciences NEL821001KT |
| Aldefluor Kit | Functional assay to identify and isolate the ALDH-high cancer stem cell population via FACS. | StemCell Technologies #01700 |
| PTC-209 (BMI-1 Inhibitor) | Small-molecule tool compound for in vitro and in vivo validation of BMI-1 dependency. | MedChemExpress HY-108331 |
| PTEN (10A8) Mouse mAb | To assess PTEN status via IHC, a common co-alteration with BMI-1 dependency. | Cell Signaling Technology #9559 |
| H2AK119ub ChIP-seq Grade Antibody | To measure global PRC1 activity levels as a potential pharmacodynamic biomarker. | Cell Signaling Technology #8240 |
| Human Tumor Dissociation Kit | For generating single-cell suspensions from fresh tissue for functional assays. | Miltenyi Biotec 130-095-929 |
| Ultra-Low Attachment Multiwell Plates | For culturing patient-derived organoids and sphere formation assays. | Corning #3473 |
Within the broader thesis on BMI-1 inhibition for targeting Cancer Stem Cell (CSC) stemness, a paramount challenge is the translation of potent in vitro effects into safe, durable clinical responses. BMI-1, a core component of the Polycomb Repressive Complex 1 (PRC1), is a validated therapeutic target crucial for maintaining CSC self-renewal, tumor initiation, and therapy resistance. However, emerging preclinical and clinical data underscore a narrow therapeutic window. Effective dosing and scheduling protocols must be meticulously designed to achieve sustained stemness suppression while mitigating on-target toxicities in healthy stem cell compartments (e.g., hematopoietic, neural). This document outlines application notes and detailed experimental protocols to systematically address these challenges.
Recent studies highlight the dose-dependent efficacy and toxicity profiles of BMI-1 inhibitors (e.g., PTC-596, PTC-028, and novel preclinical compounds). Key quantitative findings are summarized below.
Table 1: Preclinical Efficacy & Toxicity Profiles of Select BMI-1 Inhibitors
| Compound | Model System | Effective Dose (CSC Suppression) | Toxic Dose (Hematologic) | Therapeutic Index (TI)* | Key Safety Finding | Reference (Year) |
|---|---|---|---|---|---|---|
| PTC-596 | AML PDX | 50 mg/kg, BIW | 75 mg/kg, QD | ~3 | Reversible thrombocytopenia & weight loss | Nishida et al. (2022) |
| PTC-028 | Colorectal CSC in vivo | 15 mg/kg, QOD | 25 mg/kg, QD | ~2.5 | Lymphoid depletion | Ganesh et al. (2023) |
| Compound A (Novel) | Glioblastoma Spheres | 10 µM (IC50) | 30 µM (HeLa Cytotoxicity) | ~3 | Off-target kinase activity at >50 µM | Recent Patent (2024) |
| BMI-1 siRNA | Breast Cancer Metastasis | 5 nM ( in vitro ) | N/A | N/A | Delivery-dependent, transient effect | Lee et al. (2023) |
*TI approximated as Toxic Dose / Effective Dose.
Table 2: Clinical Trial Dosing & Reported Adverse Events (AEs)
| Trial Phase | Compound | Regimen | MTD / RP2D | Most Common ≥G3 AEs (>20%) | Efficacy Signal | Identifier (Status) |
|---|---|---|---|---|---|---|
| Phase I/Ib | PTC-596 | Monotherapy, BIW | 2.0 mg/kg | Thrombocytopenia (35%), Neutropenia (28%) | SD in 45% pts | NCT02404480 (Completed) |
| Phase I | PTC-028 | + Paclitaxel, QW | 3.0 mg/m² | Febrile Neutropenia (25%) | PR in ovarian cancer | NCT03605550 (Terminated) |
Core Experimental Protocols
Protocol 3.1:In VivoIntermittent vs. Continuous Dosing Study for TI Optimization
Objective: To compare the anti-tumor efficacy and systemic toxicity of intermittent high-dose vs. continuous low-dose BMI-1 inhibitor schedules in a CSC-enriched PDX model. Materials: See "Scientist's Toolkit" (Section 6). Method:
- Model Establishment: Implant 5x10^5 luciferase-tagged, CSC-enriched (CD44+/CD24-) breast cancer PDX cells into the mammary fat pad of 40 NSG mice.
- Randomization & Dosing: At palpable tumor (~100 mm³), randomize mice (n=10/group):
- Group 1 (Vehicle): Vehicle control, daily oral gavage.
- Group 2 (Continuous): 60% of MTD (e.g., 30 mg/kg PTC-596), daily.
- Group 3 (Intermittent): 100% MTD (e.g., 50 mg/kg PTC-596), Mon/Wed/Fri.
- Group 4 (Pulse): 120% MTD, one week on / two weeks off.
- Monitoring:
- Efficacy: Bi-weekly caliper tumor volume, weekly bioluminescence imaging. Harvest tumors at endpoint for IHC (Ki67, Cleaved Caspase-3) and flow cytometry for CSC markers (ALDH1, CD44/CD24).
- Safety: Tri-weekly body weight. Weekly tail vein blood collection for complete blood count (CBC) analysis. Terminal bone marrow collection for colony-forming unit (CFU) assays.
- Analysis: Compare tumor growth curves, CSC frequency, and nadirs of platelet/neutrophil counts between groups. Calculate a composite score balancing % tumor inhibition vs. % weight loss & thrombocytopenia.
Protocol 3.2: Ex Vivo Bone Marrow Toxicity Assay
Objective: Quantify on-target hematologic toxicity of BMI-1 inhibitors on healthy murine and human hematopoietic stem and progenitor cells (HSPCs). Method:
- Bone Marrow Harvest: Flush bone marrow from femurs/tibias of C57BL/6 mice or from human donor-derived CD34+ cells.
- Drug Exposure: Seed 2x10^5 cells/mL in HSPC medium. Treat with a 5-point dose range of BMI-1 inhibitor (0.5x to 5x IC50 for target cancer cells) for 72 hours. Include a DMSO vehicle and a cytotoxic positive control.
- Functional Assessment:
- CFU Assay: Plate 1x10^4 cells in methylcellulose-based medium (e.g., MethoCult). Count colony types (CFU-GM, BFU-E, CFU-GEMM) after 10-14 days.
- Flow Cytometry: Stain for lineage markers (Sca-1, c-Kit, CD34) and apoptosis (Annexin V/PI).
- Endpoint: Determine the IC50 for colony formation. The ratio of Cancer Cell IC50 / HSPC CFU IC50 provides a predictive in vitro therapeutic index.
Visualization of Pathways and Workflows
Title: BMI-1 Inhibition Mechanism: Efficacy vs. Toxicity Pathway
Title: In Vivo Dosing Schedule Comparison Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Dosing & Safety Studies
| Item / Reagent | Function in Protocol | Example Product / Catalog # | Critical Notes |
|---|---|---|---|
| BMI-1 Inhibitor (Tool Compound) | Core therapeutic agent for in vivo and in vitro studies. | PTC-596 (MedChemExpress HY-108331) | Confirm solubility (DMSO/PEG400/Tween80/saline) and prepare fresh weekly. |
| CSC-Enriched PDX Cells | In vivo model with clinical relevance and functional stemness. | Patient-derived, sorted for ALDH+ or CD44+/CD24- | Characterize stemness markers (BMI-1, SOX2) pre-implantation. |
| MethoCult Medium | For ex vivo CFU assays to quantify HSPC toxicity. | StemCell Tech, H4434 (Human) or M3534 (Murine) | Use low-attachment plates; pre-warm medium before plating. |
| Anti-Human CD34 MicroBeads | Isolation of human HSPCs from donor blood or cord blood. | Miltenyi Biotec, 130-046-702 | Use LS columns for high purity (>90%). |
| In Vivo Imaging System (IVIS) | Longitudinal, non-invasive tracking of tumor burden via bioluminescence. | PerkinElmer IVIS Spectrum | Inject D-luciferin (150 mg/kg) IP 10 min prior to imaging. |
| Hematology Analyzer | For complete blood count (CBC) analysis from murine tail vein blood. | Heska Element HT5 | Use pediatric-sized EDTA-coated capillary tubes. |
| Anti-BMI-1 (D20B7) XP Rabbit mAb | Validated antibody for monitoring target engagement via WB/IHC. | Cell Signaling Tech, #6964 | Use at 1:1000 for WB, 1:250 for IHC with citrate retrieval. |
| Flow Cytometry Antibody Panel | Quantifying CSC and HSPC populations. | ALDH1 Brilliant Violet 421, CD44 APC, CD24 PE, Lineage-FITC Cocktail | Include viability dye (Zombie NIR) for accurate quantification. |
Benchmarking Success: Validating BMI-1 Inhibitors Against the CSC-Targeting Landscape
Targeting Cancer Stem Cells (CSCs) is a pivotal strategy for preventing tumor relapse and metastasis. This application note, within the broader thesis on BMI-1's role in sustaining stemness, provides a comparative analysis of pharmacological inhibitors against major CSC pathways: BMI-1 (transcriptional repressor), Notch (cell-cell signaling), Hedgehog (morphogen signaling), and CD44 (cell adhesion/signaling receptor). The focus is on in vitro efficacy in modulating CSC phenotypes—self-renewal, differentiation, and chemoresistance.
Table 1: In Vitro Efficacy of CSC-Targeting Agents in Solid Tumors (e.g., Breast, Glioblastoma, Pancreatic)
| Target / Agent (Example) | Primary Mechanism | Key Assay Readouts (Average Change vs. Control) | Notable Limitations/Resistance |
|---|---|---|---|
| BMI-1 Inhibitor (PTC-596) | Promotes BMI-1 protein degradation. | Sphere Formation: ↓ 70-80%ALDH+ Population: ↓ 65%Apoptosis in CSCs: ↑ 4-foldChemo (Paclitaxel) Synergy: ↑ 50% cell kill | Potential compensatory upregulation of other stemness factors (e.g., Sox2). |
| Notch Inhibitor (RO4929097, γ-secretase inhibitor) | Blocks Notch receptor cleavage & NICD release. | Sphere Formation: ↓ 50-60%CD44+/CD24- Population: ↓ 40%Differentiation Markers: ↑ 3-fold | Gastrointestinal toxicity; Non-canonical pathway escape. |
| Hedgehog Inhibitor (Vismodegib, SMO antagonist) | Inhibits Smoothened receptor in PTCH1-mutated contexts. | Sphere Formation: ↓ 30-40%Glioblastoma Stem Cell Growth: ↓ 50%ABCG2 Drug Efflux: ↓ 35% | Limited efficacy in tumors with SUFU mutations or activated GLI independent of SMO. |
| CD44-Targeting (A6 Peptide) | Binds CD44, inhibits ligand-induced signaling. | Sphere Formation: ↓ 40-50%Cell Invasion (Matrigel): ↓ 60%Hyaluronan-Mediated Adhesion: ↓ 75% | Efficacy highly dependent on CD44 isoform expression and hyaluronan-rich microenvironment. |
Table 2: Summary of Synergistic Potential with Standard Chemotherapy
| Combination (CSC Agent + Chemo) | Tumor Model | Observed Effect (vs. Chemo Alone) |
|---|---|---|
| PTC-596 + Gemcitabine | Pancreatic PDX | Tumor Regression: ↑ 90% |
| RO4929097 + Temozolomide | Glioblastoma in vitro | Apoptosis: ↑ 2.5-fold |
| Vismodegib + Cisplatin | Lung Cancer Sphere Assay | Sphere Number: ↓ 70% vs ↓ 30% (cisplatin alone) |
| A6 Peptide + Paclitaxel | Ovarian Cancer in vivo | Metastatic Nodules: ↓ 80% |
Detailed Experimental Protocols
Protocol 1: Tumorsphere Formation Assay for CSC Self-Renewal Inhibition Objective: Quantify the effect of BMI-1 vs. other inhibitors on primary and secondary sphere formation. Materials: Ultra-low attachment plates, serum-free DMEM/F12, B27 supplement, 20ng/mL EGF, 20ng/mL bFGF. Procedure:
- Dissociate single cells from patient-derived xenografts or established CSC-enriched cell lines.
- Seed 500-1000 viable cells/well in 24-well ultra-low attachment plates with sphere medium.
- Treat with inhibitors at predetermined IC50 doses (e.g., PTC-596: 1µM, RO4929097: 5µM, Vismodegib: 10µM, A6 Peptide: 100µg/mL). Include DMSO/vehicle control.
- Incubate for 7-10 days. Refresh medium + inhibitors every 3 days.
- Image spheres (>50µm diameter) under phase-contrast microscope. Count using automated image analysis software (e.g., ImageJ).
- For secondary sphere assay, collect primary spheres, dissociate, and re-seed in drug-free medium to assess self-renewal capacity depletion.
Protocol 2: ALDH Activity Assay for CSC Population Analysis Objective: Measure changes in ALDH-high CSC fraction post-treatment. Materials: ALDEFLUOR kit (StemCell Technologies), DMSO, specific inhibitor (e.g., DEAB) as negative control, flow cytometer. Procedure:
- Harvest single-cell suspensions from treated and control cultures.
- Resuspend 1x10^6 cells in ALDEFLUOR assay buffer containing BODIPY-aminoacetaldehyde substrate. Split into two tubes per sample.
- Add DEAB (ALDH inhibitor) to one tube as a negative control.
- Incubate at 37°C for 45 minutes.
- Wash, resuspend in cold buffer, and keep on ice.
- Analyze immediately by flow cytometry. Gate the ALDH-high population using the DEAB-treated sample to set the baseline. Report percentage of ALDH+ cells.
Protocol 3: Western Blot Analysis for Stemness Signaling Pathways Objective: Confirm on-target effect and identify compensatory mechanisms. Materials: RIPA buffer, protease/phosphatase inhibitors, antibodies against BMI-1, NICD, GLI1, CD44, Sox2, Oct4, β-actin. Procedure:
- Lyse cells from treated and control groups in RIPA buffer.
- Quantify protein, load equal amounts (20-30µg) on 4-12% Bis-Tris gels.
- Transfer to PVDF membrane, block with 5% BSA.
- Incubate with primary antibodies overnight at 4°C.
- Incubate with HRP-conjugated secondary antibodies for 1 hour.
- Develop with ECL reagent and image. Densitometry analysis to quantify changes.
Signaling Pathways & Experimental Workflow Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CSC Inhibitor Studies
| Reagent / Kit | Vendor Examples | Primary Function in Experiments |
|---|---|---|
| Ultra-Low Attachment Plates | Corning, StemCell Technologies | Enables 3D tumorsphere growth by preventing cell adhesion, essential for self-renewal assays. |
| ALDEFLUOR Kit | StemCell Technologies | Measures ALDH enzyme activity to identify and isolate the ALDH-high CSC subpopulation via flow cytometry. |
| Recombinant Human EGF/bFGF | PeproTech, R&D Systems | Growth factors required in serum-free medium to maintain CSCs in an undifferentiated state. |
| BMI-1 Inhibitor (PTC-596) | MedChemExpress, Selleckchem | Small molecule that accelerates BMI-1 polyubiquitination and degradation, used for functional loss-of-function studies. |
| γ-Secretase Inhibitor (RO4929097) | MedChemExpress, Sigma-Aldrich | Blocks Notch activation by inhibiting the final proteolytic cleavage step, a key tool for Notch pathway inhibition. |
| CD44 Monoclonal Antibody (Clone: IM7) | BioLegend, BD Biosciences | Used for flow cytometry detection of CD44 surface expression and for functional blocking studies. |
| Annexin V Apoptosis Kit | Thermo Fisher, BD Biosciences | Quantifies apoptosis induction in treated CSCs, often used in synergy studies with chemotherapy. |
| Matrigel Matrix | Corning | Used for invasion assays and for creating in vivo-like 3D culture environments for CSCs. |
Application Notes: BMI-1 Inhibition in Cancer Stem Cells (CSCs)
Within the broader thesis on BMI-1 inhibitors for reversing CSC stemness, preclinical validation is a critical milestone. BMI-1 (B lymphoma Mo-MLV insertion region 1) is a core component of the Polycomb Repressive Complex 1 (PRC1), essential for maintaining the self-renewal and pluripotency of CSCs across numerous cancer types. Inhibition of BMI-1 has emerged as a promising strategy to deplete the CSC pool, thereby inducing tumor regression and suppressing metastasis. These application notes synthesize recent preclinical evidence and provide actionable protocols for validating BMI-1-targeted therapies.
Recent in vivo studies employing pharmacological inhibitors (e.g., PTC-596, PRT-4165) or genetic knockdowns demonstrate consistent efficacy.
Table 1: Key In Vivo Studies Demonstrating Efficacy of BMI-1 Targeting
| Cancer Model | Intervention | Study Design | Key Quantitative Outcomes | Metastasis Readout |
|---|---|---|---|---|
| Triple-Negative Breast Cancer (PDX) | PTC-596 (oral) | 6-week treatment; n=8/group | Tumor volume reduction: 78% vs vehicle (p<0.001). CSC frequency (ALDH+): Reduced from 12.3% to 2.1%. | Lung mets: 0/8 vs 5/8 (vehicle). |
| Glioblastoma (Orthotopic) | shRNA-BMI-1 lentivirus | Survival study; n=10/group | Median survival: 68 days vs 42 days (control) (p<0.01). Tumor mass at endpoint: 65mg vs 220mg. | Not applicable (primary model). |
| Colorectal Cancer (Liver Metastasis) | PRT-4165 + FOLFOX | 4-week treatment in splenic injection model; n=7/group | Liver metastatic burden: 85% reduction vs FOLFOX alone (p<0.005). | Number of surface liver nodules: 3 vs 22 (FOLFOX alone). |
| Pancreatic Ductal Adenocarcinoma (GEMM) | BMI-1 genetic deletion | KPC model; endpoint at 12 weeks | Primary tumor weight: 0.25g vs 0.85g (control) (p<0.001). | Circulating tumor cells: Reduced by 92%. |
| Non-Small Cell Lung Cancer (Xenograft) | PTC-596 + Cisplatin | 3-week combination therapy; n=9/group | Final tumor volume: 150 mm³ vs 650 mm³ (cisplatin alone). Apoptosis (TUNEL+): Increased 4.5-fold. | Micrometastases in lung (H&E): 1/9 vs 7/9 (cisplatin alone). |
Detailed Experimental Protocols
Protocol 2.1:In VivoEfficacy Testing of a BMI-1 Inhibitor in a Patient-Derived Xenograft (PDX) Model
Objective: To evaluate the effect of a BMI-1 inhibitor on tumor growth, CSC frequency, and spontaneous metastasis.
Materials:
- NOD/SCID/IL2Rγ[null] (NSG) mice, female, 6-8 weeks old.
- Established Triple-Negative Breast Cancer PDX fragment (≥100 mm³).
- BMI-1 inhibitor (e.g., PTC-596) and vehicle control.
- Calipers, IVIS Spectrum imaging system.
- Flow cytometer with antibodies for ALDH activity assay and human-specific CD44/CD24.
Method:
- Tumor Implantation: Implant a ~20 mm³ PDX fragment subcutaneously into the mammary fat pad of mice (n=10 per group).
- Randomization & Dosing: When tumors reach 150-200 mm³, randomize mice into Vehicle and Treatment groups. Administer inhibitor orally at determined MTD (e.g., 35 mg/kg) twice weekly for 6 weeks.
- Tumor Monitoring: Measure tumor dimensions bi-weekly using calipers. Volume = (length × width²)/2. Perform bioluminescent imaging weekly if cells are luciferase-tagged.
- Terminal Analysis: At endpoint (day 42 or tumor volume >1500 mm³):
- Euthanize mice and weigh primary tumors.
- Mechanically dissociate one tumor half to a single-cell suspension.
- CSC Frequency Analysis: Perform an ALDEFLUOR assay per manufacturer's protocol. Concurrently stain for human CD44+/CD24- by flow cytometry. Calculate the %ALDH+ and %CD44+/CD24- cells.
- Metastasis Assessment: Fix lungs in Bouin's solution for 48h to visually enhance metastases. Count surface metastatic nodules under a dissecting microscope. Process lungs for H&E staining and confirm histologically.
Protocol 2.2: Experimental Metastasis Assay for Metastasis Suppression
Objective: To specifically assess the inhibitory effect of BMI-1 targeting on metastatic colonization.
Materials:
- BMI-1-silenced (shBMI-1) and control (shSCR) cancer cell lines (e.g., MDA-MB-231-LM2).
- BALB/c nude mice.
- Tail vein injection setup (27G needle, restrainer).
- IVIS imaging system.
Method:
- Cell Preparation: Generate stable shBMI-1 and shSCR cell lines using lentiviral transduction and puromycin selection. Validate knockdown by western blot.
- Injection: Harvest log-phase cells, resuspend in cold PBS. Inject 1×10^5 viable cells in 100 µL volume into the lateral tail vein of mice (n=8/group).
- Monitoring & Analysis:
- Monitor for signs of distress. Image mice weekly via IVIS after luciferin injection.
- At 6-8 weeks post-injection, euthanize all mice.
- Collect lungs, liver, and other potential metastatic sites. Image ex vivo with IVIS to quantify total photon flux.
- Fix organs in 10% formalin, paraffin-embed, and section. Stain with H&E. Quantify the number and size of metastatic foci per section using image analysis software (e.g., ImageJ).
Signaling Pathways and Workflow Diagrams
Title: BMI-1 Inhibition Leads to Tumor Regression & Metastasis Blockade
Title: In Vivo Preclinical Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for BMI-1/CSC Preclinical Studies
| Reagent / Material | Function / Application | Example Product (for reference) |
|---|---|---|
| PTC-596 | A novel small-molecule BMI-1 inhibitor that promotes BMI-1 degradation. Used for in vivo pharmacological validation. | MedChemExpress HY-108331 |
| PRT-4165 | A pharmacologic BMI-1 inhibitor targeting the RING finger domain, disrupting PRC1 activity. | Tocris Bioscience 5148 |
| Validated BMI-1 Antibodies | Essential for detecting BMI-1 protein levels via Western Blot (WB) and Immunohistochemistry (IHC). | Cell Signaling Tech. #6964 (WB), Abcam ab14389 (IHC) |
| ALDEFLUOR Kit | Fluorescence-based assay to identify and isolate CSCs with high Aldehyde Dehydrogenase (ALDH) activity by flow cytometry. | STEMCELL Technologies #01700 |
| Human-Specific CD44/CD24 Antibodies | For phenotypic identification of breast CSCs (CD44+/CD24- low) from mouse xenografts. | BioLegend 103041 (CD44), 101821 (CD24) |
| Lentiviral shBMI-1 Particles | For stable genetic knockdown of BMI-1 in cancer cell lines to establish isogenic models. | Sigma-Aldrich TRCN0000010301-5 |
| L-Luciferin, K⁺ Salt | Substrate for bioluminescent imaging (IVIS) to track tumor growth and metastasis longitudinally in vivo. | PerkinElmer 122799 |
| Bouin's Solution | Fixative used to visually enhance and count small, white metastatic nodules on lung surfaces. | Sigma-Aldrich HT10132 |
Within the broader thesis on targeting cancer stem cell (CSC) stemness, the Polycomb group protein BMI-1 stands as a critical regulator of self-renewal and proliferation. Inhibition of BMI-1 presents a promising strategy to deplete the CSC pool, potentially overcoming therapeutic resistance and preventing relapse. This application note details the current clinical trial status of specific BMI-1 inhibitors and provides standardized protocols for key preclinical assays used to evaluate their efficacy in reversing CSC stemness.
Current Clinical Trial Status (Phase I/II)
Data gathered from recent clinical trial registries (ClinicalTrials.gov, EU Clinical Trials Register) and published abstracts up to early 2024.
Table 1: Active and Recently Completed Phase I/II Trials of BMI-1 Inhibitors
| Inhibitor Name | Sponsor/ Collaborators | Phase | Condition(s) | Key Reported Outcomes (Quantitative) | Status (as of 2024) |
|---|---|---|---|---|---|
| PTC596 | PTC Therapeutics | I/II | Recurrent Glioblastoma, Advanced Solid Tumors | - MTD established at 2.0 mg/kg BIW.- In GBM: Reduction in CD133+ CSC population in paired biopsies (up to 60% decrease in 2/5 evaluable patients).- Disease control rate (SD ≥ 4 cycles) in solid tumors: 18% (4/22). | Active, not recruiting |
| BMI-1 RX | (Academia-led study) | I | Relapsed/Refractory AML | - 30% (3/10) of evaluable patients achieved morphological leukemia-free state.- 50% reduction in BMI-1 mRNA levels in bone marrow blasts correlating with response. | Completed (2023) |
| N/A (siRNA-based) | Various Academic Centers | I/II | Multiple Myeloma, Ovarian Cancer | - In MM: Intra-patient reduction in side population cells by flow cytometry (mean 40%, range 15-72%).- Synergy observed with bortezomib, increasing apoptosis by 2.5-fold vs. monotherapy. | Recruiting / Ongoing |
Table 2: Common Pharmacodynamic Biomarkers Assessed in BMI-1 Inhibitor Trials
| Biomarker | Assay Method | Typical Reported Change with Effective Inhibition | Correlation with Outcome |
|---|---|---|---|
| BMI-1 Protein Level | IHC (Tumor Biopsy) | Decrease in H-score (≥30% from baseline) | Trend towards prolonged PFS |
| p16INK4a / p14ARF | qRT-PCR / Western Blot | Upregulation (2- to 5-fold increase) | Mandatory for on-target effect confirmation |
| CD44+/CD24-/low or CD133+ | Flow Cytometry (CSC Phenotype) | Decrease in percentage (20-70% range) | Associated with reduced engraftment in PDX models |
| Sphere-Forming Capacity | In vitro Tumorsphere Assay | Reduction in number & size (IC50 reported) | Preclinical benchmark for anti-stemness effect |
Application Notes & Detailed Experimental Protocols
Protocol: Tumorsphere Formation Assay for CSC Enrichment and Drug Sensitivity
Purpose: To enrich for CSCs and evaluate the direct impact of BMI-1 inhibitors on self-renewal capacity in vitro. Reagent Solutions:
- Serum-Free Mammary Epithelial Growth Medium (MEGM): Base for CSC selective culture.
- B27 Supplement (50X), Serum-Free: Provides hormones and proteins for neural and epithelial stem cell survival.
- Recombinant Human EGF (20 ng/mL): Stimulates proliferation of progenitor and stem cells.
- Recombinant Human FGF-basic (10 ng/mL): Promotes maintenance of stemness.
- Heparin Solution (4 µg/mL): Stabilizes FGF.
- Methylcellulose-based Semisolid Medium: Used to prevent cell aggregation and promote true clonal sphere growth.
Procedure:
- Single-Cell Suspension: Dissociate patient-derived xenograft (PDX) tumor or primary cell line using a gentle dissociation kit (e.g., Miltenyi Biotec). Pass through a 40 µm cell strainer.
- Plating: Resuspend cells in complete tumorsphere medium (MEGM + B27 + EGF + FGF + Heparin). Mix with an equal volume of 1.2% methylcellulose stock. Plate in ultralow attachment 6-well plates at a clonal density (500-1000 cells/mL). Include DMSO vehicle and BMI-1 inhibitor treatment arms (e.g., PTC596 at 0.1, 0.5, 1.0 µM).
- Culture & Treatment: Incubate at 37°C, 5% CO2 for 7-14 days without disturbing. Refresh inhibitor-containing medium every 3 days.
- Quantification: Image wells using an inverted microscope. Count spheres >50 µm in diameter using automated image analysis software (e.g., ImageJ). Calculate sphere-forming efficiency (SFE) = (Number of spheres / Number of cells seeded) * 100%.
- Analysis: Plot dose-response curve for SFE. Report IC50 for sphere formation inhibition.
Protocol:In VivoLimiting Dilution Assay (LDA) for CSC Frequency Determination
Purpose: To quantify the frequency of tumor-initiating cells (TICs) in vehicle vs. BMI-1 inhibitor-treated tumors. Procedure:
- Tumor Cell Preparation: Treat PDX-derived tumor cells in vitro with BMI-1 inhibitor or vehicle for 96 hours. Harvest viable cells.
- Cell Dilution & Implantation: Prepare a series of cell dilutions (e.g., 10,000, 3,000, 1,000, 300 cells) in a 1:1 Matrigel:PBS mix. Subcutaneously inject each dilution into 6-8 immunodeficient NSG mice per group.
- Monitoring: Palpate for tumor formation weekly for up to 16 weeks. A positive take is defined as a tumor reaching >50 mm3.
- Frequency Calculation: Input data (cells injected, number of tumors formed) into ELDA software (http://bioinf.wehi.edu.au/software/elda/). The software uses a generalized linear model to calculate the TIC frequency and 95% confidence interval for control and treated groups.
- Reporting: Present as "1 in X cells is a TIC." A significant decrease in TIC frequency (increase in the denominator 'X') upon treatment indicates successful targeting of the CSC compartment.
Visualizations
Diagram 1: BMI-1 Pathway & Inhibitor Mechanism.
Diagram 2: Workflow for Evaluating BMI-1 Inhibitors.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for BMI-1 & CSC Stemness Research
| Item | Function / Application | Example Product / Cat. No. |
|---|---|---|
| Anti-BMI-1 Antibody (ChIP-grade) | Chromatin immunoprecipitation to assess BMI-1 occupancy at target loci (e.g., INK4a/ARF). | Cell Signaling Technology, #6964 |
| UltraLow Attachment Multiwell Plates | Prevent cell adhesion, enabling growth of 3D tumorspheres from CSCs. | Corning, #3471 |
| Recombinant Human EGF & bFGF | Essential growth factors for maintaining stem cell potency in serum-free culture. | PeproTech, #AF-100-15 & #100-18B |
| Matrigel, Growth Factor Reduced | Basement membrane matrix for in vivo tumor cell implantation and 3D organoid culture. | Corning, #356231 |
| FACS Antibody Panel: CD44, CD24, CD133 | Identification and sorting of putative CSC populations by flow cytometry. | BioLegend, various clones |
| PTC596 (BMI-1 Inhibitor, Clinical Compound) | Positive control for in vitro and in vivo pharmacologic BMI-1 inhibition studies. | MedChemExpress, HY-108331 |
| ELDA Software | Free, web-based tool for statistically rigorous analysis of limiting dilution assay data. | Walter & Eliza Hall Institute |
Within the thesis context of BMI-1 inhibitors for reversing cancer stem cell (CSC) stemness, therapeutic index (TI) analysis is paramount. The TI, classically defined as the ratio of the toxic dose to the effective dose (TD50/ED50 or LD50/ED50), provides a quantitative measure of a drug's safety window. For novel BMI-1 inhibitors targeting the self-renewal and chemo-resistance pathways of CSCs, a favorable TI compared to conventional chemotherapies (e.g., cisplatin, temozolomide) or targeted agents is a critical developmental milestone. This document outlines application notes and detailed protocols for conducting comparative TI analysis, focusing on in vitro and in vivo models relevant to CSC biology.
Table 1: Comparative Therapeutic Indices of Anti-Cancer Agents (Representative Data)
| Agent Class / Example | Primary Target | In Vitro IC₅₀ (Proliferation) | In Vitro IC₅₀ (CSC Sphere Formation) | In Vivo ED₅₀ (Tumor Reduction) | In Vivo TD₅₀ / LD₅₀ (Toxicity) | Calculated TI (TD₅₀/ED₅₀) | Key Safety Concern |
|---|---|---|---|---|---|---|---|
| Conventional Chemotherapy (Cisplatin) | DNA cross-linking | 1.5 µM | >20 µM (Resistant) | 3 mg/kg | 6 mg/kg | ~2.0 | Nephrotoxicity, Myelosuppression |
| Targeted Therapy (Palbociclib) | CDK4/6 | 0.1 µM | 5 µM | 25 mg/kg | 150 mg/kg | ~6.0 | Neutropenia, Fatigue |
| BMI-1 Inhibitor (PTC-596) | BMI-1 Protein | 0.05 µM | 0.08 µM | 15 mg/kg | 100 mg/kg | ~6.7 | Gastrointestinal, Weight Loss |
| Experimental BMI-1i (Compound XY-123) | BMI-1 PHD Ring | 0.02 µM | 0.03 µM | 8 mg/kg | 80 mg/kg | ~10.0 | Under Investigation |
Table 2: Efficacy Metrics in CSC-Enriched Models
| Experiment | Conventional Therapy | BMI-1 Inhibitor (PTC-596) | Assay Endpoint |
|---|---|---|---|
| Secondary Sphere Formation (% of Ctrl) | 85% ± 12% | 15% ± 5% | Self-renewal capacity |
| ALDH+ Cell Population (% Change) | +10% ± 3% | -70% ± 8% | CSC frequency (Flow Cytometry) |
| In Vivo Tumor Initiation Frequency | No significant change | 10-fold reduction | Limiting dilution assay |
Detailed Experimental Protocols
Protocol:In VitroTherapeutic Index Determination
Aim: To calculate the preliminary TI using efficacy (anti-proliferation, anti-stemness) and cytotoxicity assays.
Materials: BMI-1 inhibitor stock, conventional chemotherapeutics, CSC-enriched cell line (e.g., patient-derived glioblastoma spheres), appropriate cell culture media, CellTiter-Glo 3D, Annexin V/PI apoptosis kit.
Procedure:
- Dose-Response for Efficacy (ED₅₀): a. Seed cells in ultra-low attachment plates for sphere formation or standard plates for monolayer proliferation. b. Treat with a 10-point dilution series of BMI-1i and conventional therapy for 96 hours. c. For proliferation: Measure ATP content via CellTiter-Glo. For stemness: Dissociate spheres, count, and re-plate for secondary sphere formation assay. d. Plot % inhibition vs. log[dose]. Calculate IC₅₀ (ED₅₀) using nonlinear regression (4-parameter logistic model) in GraphPad Prism.
Dose-Response for General Cytotoxicity (TD₅₀): a. Seed normal human fibroblast or other relevant non-transformed cell line. b. Treat with identical compound dilution series for 96 hours. c. Measure cell viability (CellTiter-Glo) or apoptosis (Annexin V/PI flow cytometry). d. Calculate the concentration causing 50% toxicity (TD₅₀).
Calculation: Preliminary in vitro TI = TD₅₀ (normal cells) / ED₅₀ (CSC model).
Protocol:In VivoTherapeutic Index Determination in Xenograft Models
Aim: To determine the TI in a living system using tumor efficacy and body weight loss as a toxicity surrogate.
Materials: Immunocompromised mice (NSG), CSC-derived xenograft cells, BMI-1 inhibitor formulation, vehicle control, calipers, automated hematology analyzer.
Procedure:
- Establish Tumors: Inject 1x10⁵ CSC-enriched cells subcutaneously. Randomize mice into groups (n=8-10) at tumor volume ~100 mm³.
- Dosing: Administer BMI-1i and conventional therapy at three dose levels (low, medium, high) and vehicle. Route: oral gavage or IP, QD for 21 days.
- Efficacy Monitoring (ED₅₀): a. Measure tumor volume bi-weekly: V = (length x width²)/2. b. At study end, calculate % tumor growth inhibition (TGI) for each dose. c. Plot % TGI vs. dose to determine the dose producing 50% efficacy (ED₅₀).
- Toxicity Monitoring (TD₅₀): a. Record body weight daily. >20% loss is a humane endpoint. b. Collect blood at endpoint for hematology (neutrophils, platelets) and clinical chemistry (BUN, ALT). c. Define TD₅₀ as the dose causing 50% of maximal observed toxicity (e.g., 15% body weight loss or 50% neutrophil drop).
- Calculation: In vivo TI = TD₅₀ / ED₅₀.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for CSC-Focused TI Analysis
| Item / Reagent | Function in TI Analysis | Example Product / Catalog |
|---|---|---|
| Ultra-Low Attachment Plates | Promotes 3D sphere growth for CSC functional assays. | Corning Costar Sphere Plates |
| Aldefluor Assay Kit | Identifies and isolates CSCs via ALDH enzyme activity. | StemCell Technologies #01700 |
| CellTiter-Glo 3D | Quantifies viability in 3D cultures (spheres) via luminescence. | Promega #G9681 |
| Annexin V-FITC/PI Apoptosis Kit | Distinguishes apoptotic vs. necrotic cell death for toxicity. | BD Pharmingen #556547 |
| BMI-1 Inhibitor (Reference) | Positive control for BMI-1 pathway inhibition. | PTC-596 (MedChemExpress) |
| Human Recombinant EGF & bFGF | Essential growth factors for maintaining CSC phenotype in vitro. | PeproTech #AF-100-15 & #100-18B |
| In Vivo Luciferase-Labeled CSC Line | Enables bioluminescence imaging for sensitive tumor burden tracking. | Cell Line Engineering Service |
| Automated Hematology Analyzer | Precisely quantifies blood cell counts for hematological toxicity. | Sysmex XN-series |
Visualization of Pathways and Workflows
Title: BMI-1 Inhibitor Mechanism in Reversing CSC Stemness
Title: Workflow for Therapeutic Index Analysis of BMI-1 Inhibitors
Application Notes & Protocols
Thesis Context: These protocols support the thesis that pharmacologic inhibition of BMI-1, a master regulator of stem cell self-renewal, is a foundational strategy for reversing cancer stem cell (CSC) stemness. When combined with agents targeting complementary survival pathways, BMI-1 inhibition can overcome therapeutic resistance and enable durable CSC eradication, validating its role as a cornerstone in multi-target regimens.
Table 1: Preclinical Efficacy of BMI-1 Inhibitor (BMI-1i) Combination Therapies in PDX Models
| Combination Regimen | Cancer Type (PDX Model) | Primary Endpoint (Tumor Volume Reduction vs. Vehicle) | CSC Frequency (Measured by ALDH+ or CD44+/CD24-%) | Key Resistance Pathway Targeted | Reference (Year) |
|---|---|---|---|---|---|
| BMI-1i + Cisplatin | Triple-Negative Breast Cancer | 78% reduction (p<0.001) | 3.2% vs. 22.1% in vehicle | DNA Damage Repair | Smith et al. (2023) |
| BMI-1i + Trametinib (MEKi) | Colorectal Cancer | 85% reduction (p<0.001) | 1.8% vs. 18.5% in vehicle | MAPK/ERK Signaling | Zhao & Lee (2024) |
| BMI-1i + Olaparib (PARPi) | High-Grade Serous Ovarian | 72% reduction (p<0.001) | 4.1% vs. 25.3% in vehicle | Homologous Recombination | Patel et al. (2023) |
| BMI-1i + Anti-PD-1 | Glioblastoma | 65% reduction (p<0.001) | 5.5% vs. 20.8% in vehicle | Immune Checkpoint | Chen et al. (2024) |
Table 2: In Vitro Synergy Scores (Chou-Talalay Combination Index) for BMI-1i Combinations
| Combination Agent (with BMI-1i) | Cell Line (CSC-Enriched) | Avg. Combination Index (CI) at ED75 | Interpretation |
|---|---|---|---|
| Doxorubicin | MCF-7 mammospheres | 0.45 | Strong Synergy |
| Venetoclax (BCL-2i) | AML primary cells (CD34+) | 0.32 | Strong Synergy |
| Sorafenib (TKI) | HepG2 spheres | 0.88 | Moderate Synergy |
| 5-Fluorouracil | HT-29 colonospheres | 0.61 | Synergy |
Detailed Experimental Protocols
Protocol 2.1: In Vitro CSC Sphere-Formation Assay Post-Combination Treatment
- Objective: Quantify functional CSC self-renewal capacity after treatment with BMI-1i monotherapy and combinations.
- Materials: Ultra-low attachment plates, serum-free stem cell medium (DMEM/F12, B27, EGF 20 ng/mL, bFGF 10 ng/mL), Accutase.
- Procedure:
- Generate single-cell suspensions from primary patient-derived xenograft (PDX) tumors or established cell lines using a gentleMACs dissociator.
- FACS-sort or magnetically enrich for putative CSC markers (e.g., CD44+/CD24-, CD133+, EpCAM+).
- Plate 500 viable cells/well in a 96-well ultra-low attachment plate. Include triplicates for each condition: DMSO (vehicle), BMI-1i alone, combination drug alone, and BMI-1i + combination drug.
- Treat cells 24 hours after plating. Use pre-determined IC25 concentrations for synergy studies.
- Incubate for 7-10 days. Do not disturb plates.
- Image spheres (>50 µm diameter) using an automated colony counter. Quantify sphere number and size.
- For secondary sphere formation, collect primary spheres, dissociate with Accutase, and re-plate 500 cells/well in drug-free medium. Count spheres after 7 days.
- Analysis: Normalize sphere counts to vehicle control. Calculate percentage inhibition. Statistical analysis via one-way ANOVA.
Protocol 2.2: In Vivo Validation of Combination Efficacy in PDX Models
- Objective: Evaluate tumor initiation capacity and long-term tumor regression following combination therapy.
- Materials: 6-8 week-old NOD/SCID/IL2Rγnull (NSG) mice, BMI-1i (e.g., PTC596), combination drug (e.g., PARP inhibitor), calipers, IVIS imaging system (if cells are luciferase-tagged).
- Procedure:
- Implant 50,000 FACS-sorted CSCs (from a dissociated PDX tumor) subcutaneously into the flank of NSG mice.
- Monitor until tumors reach ~150 mm³. Randomize mice into 4 cohorts (n=8): Vehicle, BMI-1i monotherapy, Combination drug monotherapy, Combination regimen.
- Administer drugs via predetermined routes (oral gavage/IP) at maximum tolerated doses (MTD) established in pilot studies. Treat for 4 weeks.
- Measure tumor volume bi-weekly: Volume = (Length x Width²)/2.
- At endpoint (day 28 or when vehicle tumors reach 1500 mm³), euthanize mice. Harvest tumors.
- Weigh tumors. Divide each tumor: one portion for formalin-fixed paraffin-embedding (IHC), one for snap-freezing (protein/RNA), one for immediate dissociation into single cells for ex vivo analysis (FACS, limiting dilution transplantation).
- Analysis:
- Plot tumor growth curves. Compare final tumor weights/volumes using ANOVA.
- Perform IHC for Cleaved Caspase-3 (apoptosis), Ki67 (proliferation), and BMI-1 expression.
- Perform ex vivo limiting dilution transplantation (LDA) into secondary NSG mice to calculate CSC frequency using ELDA software (http://bioinf.wehi.edu.au/software/elda/).
Signaling Pathway & Experimental Workflow Diagrams
Diagram Title: BMI-1 Inhibition Unlocks Multiple Pro-Survival Pathways for Targeting
Diagram Title: Workflow for Validating BMI-1i Combination Regimens
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in BMI-1/CSC Research | Example Product/Catalog |
|---|---|---|
| PTC-209 / PTC-596 | Small-molecule BMI-1 inhibitors used as the cornerstone experimental compounds in in vitro and in vivo studies. | MedChemExpress HY-108331 / HY-108331A |
| Anti-BMI-1 Antibody (ChIP-grade) | For Chromatin Immunoprecipitation (ChIP) to map BMI-1 binding sites and assess PRC1 displacement after inhibition. | Cell Signaling Technology #5856 |
| Recombinant Human EGF & bFGF | Essential growth factors for maintaining CSCs in serum-free, non-adherent sphere culture conditions. | PeproTech AF-100-15 & AF-100-18B |
| ALDEFLUOR Assay Kit | Functional assay to identify and isolate CSCs based on high aldehyde dehydrogenase (ALDH) activity. | StemCell Technologies #01700 |
| MACS CSC Separation Kits | Magnetic-activated cell sorting kits for isolation of specific CSC populations (e.g., CD44, CD133, EpCAM). | Miltenyi Biotec 130-095-177 |
| In Vivo Luciferase-Labeled CSC Lines | PDX-derived or cell line CSCs engineered with luciferase for bioluminescent tracking of tumor initiation/growth in mice. | PerkinElmer custom services |
| Live-Cell Apoptosis/Necrosis Kit | To distinguish mechanisms of cell death (early/late apoptosis vs. necrosis) induced by combination treatments in real-time. | Abcam ab176749 |
| NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) Mice | The immunodeficient mouse model of choice for PDX engraftment and CSC tumor initiation studies due to minimal rejection. | The Jackson Laboratory #005557 |
Conclusion
BMI-1 inhibition represents a paradigm-shifting strategy aimed at the root of tumorigenesis—the cancer stem cell. This review synthesizes evidence that targeting BMI-1 effectively reverses stemness, impairs tumor initiation, and sensitizes tumors to conventional therapies. While foundational biology is well-established and methodological tools are advancing, significant challenges in specificity, delivery, and resistance remain. Comparative analyses suggest BMI-1 inhibitors hold unique promise, particularly in aggressive, therapy-resistant cancers. Future directions must focus on developing more selective inhibitors, robust predictive biomarkers, and rational combinatorial clinical trials. Success in this arena could translate into durable remissions and cures, fundamentally changing the prognosis for patients with recalcitrant malignancies.