Breaking the Barrier: Mechanisms of CD8+ T Cell Infiltration in Cold vs. Hot Tumors and Therapeutic Implications
This comprehensive review synthesizes current research on the biological mechanisms that govern cytotoxic CD8+ T lymphocyte infiltration into solid tumors, a critical determinant of immunotherapy response.
Breaking the Barrier: Mechanisms of CD8+ T Cell Infiltration in Cold vs. Hot Tumors and Therapeutic Implications
Abstract
This comprehensive review synthesizes current research on the biological mechanisms that govern cytotoxic CD8+ T lymphocyte infiltration into solid tumors, a critical determinant of immunotherapy response. We first explore the foundational biology distinguishing 'hot' (T cell-inflamed) from 'cold' (non-inflamed) tumor microenvironments, focusing on chemokine networks, endothelial barriers, and immunosuppressive stroma. We then detail cutting-edge methodologies for quantifying infiltration and models for studying trafficking, followed by an analysis of strategies to overcome infiltration barriers through combination therapies and novel targets. Finally, we validate and compare clinical biomarkers and therapeutic approaches designed to convert cold tumors into hot, response-permissive environments. This article provides researchers and drug developers with a mechanistic and applied framework for advancing next-generation immuno-oncology strategies.
Decoding the Tumor Microenvironment: The Fundamental Biology of T Cell Exclusion in Cold Tumors
This whitepaper provides a technical framework for classifying the tumor immune microenvironment (TIME) based on the density, functionality, and spatial distribution of cytotoxic CD8+ T cells—a critical determinant of immunotherapy response. Understanding the mechanisms governing T cell infiltration is fundamental to developing novel therapeutic strategies. The classification into "hot," "altered-immunosuppressed," and "cold" phenotypes provides a spectrum that reflects the dynamic interplay between tumor cells and the immune system.
The Immunophenotype Spectrum: Definitions and Quantitative Metrics
The classification is primarily defined by the presence and functional state of tumor-infiltrating lymphocytes (TILs), particularly CD8+ T cells, and the expression of immune checkpoint molecules.
Table 1: Defining Characteristics of Tumor Immunophenotypes
| Feature | Hot Tumors | Altered-Immunosuppressed Tumors | Cold Tumors (Immune-Desert) |
|---|---|---|---|
| CD8+ T Cell Density | High (>250 cells/mm² at invasive margin) | Variable, often moderate but dysfunctional | Very low (<100 cells/mm² in core and margin) |
| Spatial Distribution | Infiltrated both core and invasive margin; organized in tertiary lymphoid structures (TLS) | Excluded at the margin or present but suppressed in stroma; absent from core | Absent from both tumor core and invasive margin |
| Key Immune Checkpoint Expression (e.g., PD-L1) | High (Tumor Proportion Score often >50%) | Variable, can be high but with concurrent suppressive signals | Low or absent (Tumor Proportion Score often <1%) |
| T Cell Functional State | Proliferative (Ki67+), effector cytokine production (IFN-γ, TNF-α) | Exhausted (PD-1hi, TIM-3+, LAG-3+), anergic, or senescent | Naïve or absent |
| Dominant Myeloid Population | M1-like macrophages, dendritic cells (CD103+ cDC1) | Myeloid-derived suppressor cells (MDSCs), M2-like macrophages, TAMs | Immature myeloid cells, neutrophils |
| Tumor Mutational Burden (TMB) | Typically high (>10 mutations/Mb) | Variable | Typically low (<5 mutations/Mb) |
| Representative Cancer Types | Melanoma, NSCLC (subset), MSI-H colorectal | Pancreatic ductal adenocarcinoma, hepatocellular carcinoma, glioblastoma | Prostate adenocarcinoma, uveal melanoma, KRAS-driven NSCLC |
Mechanistic Insights into CD8+ T Cell Infiltration
The phenotype is dictated by a series of sequential biological mechanisms.
Cold Tumors: Failure of T Cell Priming and Recruitment
- Mechanism: Lack of tumor antigenicity (low neoantigen burden) or impaired antigen presentation (loss of MHC-I, defects in antigen processing machinery). Deficient secretion of T cell chemoattractants (e.g., CXCL9, CXCL10).
- Experimental Protocol for Assessing Antigen Presentation: MHC-I surface expression can be quantified via flow cytometry using antibodies against HLA-A,B,C. Functional antigen presentation is assessed using co-culture assays with T cell lines specific for defined tumor antigens (e.g., MART-1), measuring IFN-γ release by ELISA.
Altered-Immunosuppressed Tumors: Active Inhibition of Infiltrated T Cells
- Mechanism: Successful T cell priming and initial infiltration are counteracted by a highly suppressive TIME. This involves upregulation of multiple immune checkpoints (PD-L1/PD-1, CTLA-4), metabolic dysregulation (IDO, adenosine, arginase), and recruitment of suppressive cells (Tregs, MDSCs).
- Experimental Protocol for T Cell Exhaustion Profiling: Isolate TILs via tumor dissociation. Perform high-parameter flow cytometry (≥12 colors) staining for surface markers (PD-1, TIM-3, LAG-3, CD39, CD101) and intracellular transcription factors (TOX, TCF1). Analyze using dimensionality reduction tools (t-SNE, UMAP) to define exhausted subsets.
Hot Tumors: Permissive Microenvironment for T Cell Function
- Mechanism: Effective cancer-immunity cycle: release of neoantigens, dendritic cell maturation and migration, T cell priming in lymph nodes, T cell trafficking to tumor, and productive killing with memory formation. Presence of TLS supports ongoing adaptive immunity.
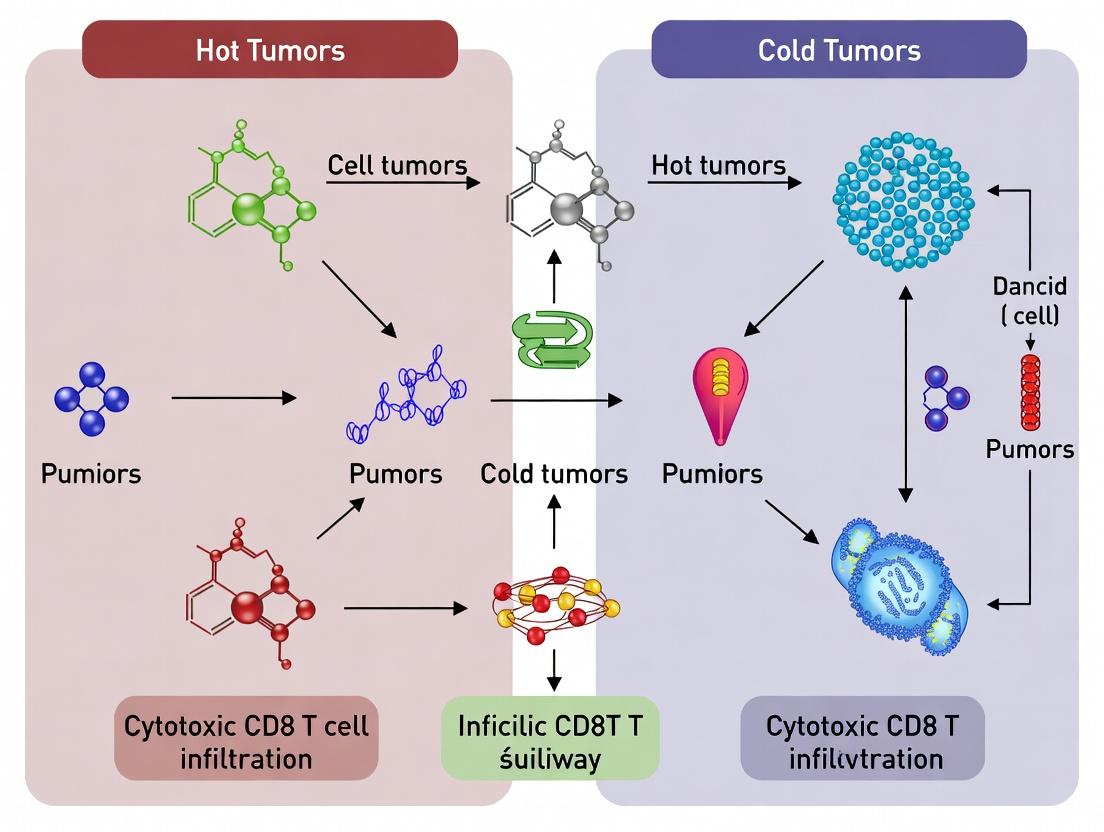
Visualizing Key Signaling Pathways and Workflows
Diagram Title: Core Pathways Defining Hot, Altered, and Cold Tumor Phenotypes
Diagram Title: Flow Cytometry Workflow for TIL Analysis
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Tumor Immunophenotyping Research
| Reagent Category | Specific Example(s) | Function in Research |
|---|---|---|
| Immune Cell Isolation Kits | Human/mouse Tumor Dissociation Kits (e.g., Miltenyi, STEMCELL); CD8+ T Cell Isolation Kits (negative selection). | Generate single-cell suspensions from solid tumors for downstream analysis. Isolate specific lymphocyte populations for functional assays. |
| Fluorochrome-conjugated Antibodies | Anti-human/mouse CD3, CD8, CD45, CD4, FoxP3, PD-1, PD-L1, TIM-3, LAG-3, Ki67. | Multi-color flow cytometry to define immune cell subsets, activation, and exhaustion states within the TIME. |
| Multiplex Immunohistochemistry/Ion Platforms | Opal Polychromatic IHC (Akoya), GeoMx Digital Spatial Profiler (NanoString), CODEX (Akoya). | Simultaneous detection of 6+ protein markers on a single FFPE section with spatial context. Enables phenotyping and interaction analysis in situ. |
| Cytokine/Chemokine Detection Assays | LEGENDplex bead-based immunoassays; ELISA kits for IFN-γ, TNF-α, Granzyme B, CXCL9/10. | Quantify soluble factors in tumor supernatants or serum that define chemokine gradients and effector function. |
| T Cell Functional Assays | CellTrace proliferation dyes; Fixable Viability Dyes; intracellular cytokine staining kits (ICS). | Measure proliferative capacity, viability, and effector cytokine production (IFN-γ, IL-2) upon stimulation. |
| Single-Cell RNA-Seq Solutions | 10x Genomics Chromium Next GEM; BD Rhapsody; Parse Biosciences kits. | Unbiased, high-throughput transcriptomic profiling of all cells in the TIME to discover novel states and interactions. |
The tripartite classification of hot, altered-immunosuppressed, and cold tumors is more than descriptive; it provides an actionable roadmap for drug development. Hot tumors may respond to single-agent immune checkpoint inhibitors (ICIs). Altered-immunosuppressed tumors likely require combination therapies targeting multiple inhibitory pathways (e.g., PD-1 + LAG-3) or depleting suppressive cell populations. Cold tumors present the greatest challenge, necessitating strategies to initiate the cancer-immunity cycle, such as oncolytic viruses, STING agonists, or cancer vaccines to create a "hotter" microenvironment. A deep mechanistic understanding of CD8+ T cell infiltration and function across this spectrum is essential for designing the next generation of immunotherapies and matching them to the appropriate patient population.
Within the broader thesis of understanding cytotoxic CD8+ T cell infiltration mechanisms in hot versus cold tumors, chemokine-directed trafficking is a pivotal regulatory checkpoint. This whitpaper provides an in-depth technical analysis of the CXCR3 axis, primarily governed by its ligands CXCL9, CXCL10, and CXCL11, alongside other critical chemokine signals that orchestrate T cell positioning within the tumor microenvironment (TME). The functional integrity of these pathways is a key determinant of whether a tumor is immunologically "hot" (T cell-inflamed) or "cold" (non-inflamed). We detail the molecular biology, quantitative expression profiles, experimental methodologies for investigation, and emerging therapeutic strategies aimed at modulating these axes to enhance cancer immunotherapy.
The infiltration of CD8+ cytotoxic T lymphocytes (CTLs) into solid tumors is a prerequisite for effective anti-tumor immunity and a strong predictor of response to immune checkpoint blockade (ICB). A "hot" tumor phenotype is characterized by a pre-existing, though often functionally suppressed, CTL infiltrate, while "cold" tumors lack such infiltration. This disparity is largely governed by a multi-step process involving T cell priming in lymph nodes, endothelial adhesion, and chemotactic migration into the TME. Chemokines and their receptors act as the principal coordinators of this final trafficking step. The CXCL9/10/11-CXCR3 axis is arguably the most dominant pathway for recruiting Th1-type CD4+ and effector CD8+ T cells, NK cells, and NKT cells. Dysregulation of this axis—through low ligand expression, receptor downregulation, or the presence of antagonistic chemokines—is a hallmark of the cold TME.
Core Biology of the CXCR3 Axis
Ligands and Receptor Isoforms
- CXCR3 Receptor: A G-protein coupled receptor (GPCR) primarily expressed on activated T cells, especially Th1 and CTLs, as well as NK cells. Two main isoforms exist:
- CXCR3A: Binds all three ligands (CXCL9, CXCL10, CXCL11) and signals through Gαi, leading to cell migration and activation.
- CXCR3B: Binds CXCL4, CXCL9, CXCL10, and CXCL11, and signals through Gαs, often associated with anti-proliferative and angiostatic effects.
- CXCL9 (MIG): Induced by IFN-γ. Known for its stability and potent chemotactic activity.
- CXCL10 (IP-10): Induced by IFN-γ and TNF-α. Most widely studied, often used as a biomarker for T cell inflammation.
- CXCL11 (I-TAC): Induced by IFN-γ and has the highest receptor-binding affinity. It also induces rapid receptor internalization.
These ligands are produced primarily by myeloid cells (e.g., dendritic cells, macrophages), endothelial cells, and stromal cells in response to inflammatory signals, particularly IFN-γ from immune cells.
Key Signaling Pathway
Diagram 1: CXCR3 Axis Signaling in T Cell Trafficking
Quantitative Expression in Hot vs. Cold Tumors
Empirical data consistently shows a strong correlation between CXCR3 ligand expression and CD8+ T cell infiltration.
Table 1: Representative CXCR3 Ligand Expression and Correlation with T Cell Infiltration
| Tumor Type | CXCL9/10/11 mRNA Level (Hot vs. Cold) | CD8+ T Cell Density (cells/mm²) Correlation | Key Regulator | Source (Example) |
|---|---|---|---|---|
| Melanoma | High in ICB-Responders | >500 in TME core | IFN-γ from TILs | RNA-seq analysis |
| Breast (TNBC) | High in Lymphocyte-Predominant | ~300-400 | Tumor-intrinsic STING | IHC/microarray |
| Colorectal (MSI-H) | Very High | >600 | Microbiome-derived signals | TCGA dataset |
| Pancreatic (PDAC) | Very Low (Cold) | <50 | Dominant TGF-β signaling | Spatial transcriptomics |
| Prostate | Low to Absent | <100 | Low IFN-γ, High IL-8 | Multiplex cytokine assay |
Other Critical Trafficking Signals
While CXCR3 is central, other chemokine axes play complementary or counter-regulatory roles.
- CCL5-CCR5: Important for recruiting T cells and monocytes. Often co-expressed with CXCR3 ligands in hot tumors.
- CCL2-CCR2/CCR4: Primarily recruits myeloid-derived suppressor cells (MDSCs) and Tregs, which can promote an immunosuppressive TME and counteract CXCR3-mediated anti-tumor immunity.
- CXCL12-CXCR4: Can sequester T cells in the tumor stroma or mediate exclusion to perivascular areas, contributing to a "cold" or "immune-excluded" phenotype.
- CXCL13-CXCR5: Critical for the formation of tertiary lymphoid structures (TLS), which are associated with improved CTL function and patient survival.
Experimental Protocols for Investigating Chemokine Trafficking
Protocol: In Vitro T Cell Migration (Transwell) Assay
Purpose: To quantitatively measure the chemotactic response of CD8+ T cells to specific chemokines. Key Reagents:
- Transwell Inserts (e.g., 5.0 μm pore size for T cells).
- Recombinant Human/Mouse Chemokines (CXCL9, CXCL10, CXCL11, CCL5).
- Isolated CD8+ T Cells (from human PBMCs or mouse spleen, activated with anti-CD3/CD28 + IL-2 for 3-5 days).
- Chemotaxis Buffer (RPMI-1640 + 0.5% BSA).
- Calcein AM or CellTrace Dye for fluorescent labeling and quantification. Methodology:
- Prepare chemokine dilutions in chemotaxis buffer and add to the lower chamber of a 24-well plate.
- Suspend activated, labeled CD8+ T cells (1x10^6 cells/mL) in chemotaxis buffer and add 100 μL to the upper chamber insert.
- Incubate plate at 37°C, 5% CO2 for 2-4 hours.
- Carefully remove the insert. Collect cells from the lower chamber.
- Quantify migrated cells using a flow cytometer (counting beads) or a fluorescence plate reader.
- Calculate % migration: (Number of cells migrated to chemoattractant / Number of cells migrated to media control) x 100.
Protocol: In Vivo Blocking/Modulation of Chemokine Axis
Purpose: To assess the functional role of a specific chemokine/receptor in T cell infiltration in a murine tumor model. Key Reagents:
- Syngeneic Tumor Cell Line (e.g., MC38, B16-F10).
- Neutralizing Antibodies (anti-CXCL10, anti-CXCR3) or Receptor Antagonists (e.g., AMG487).
- Isotype Control Antibody.
- Flow Cytometry Antibodies Panel: CD45, CD3, CD8, CD4, CXCR3, NK1.1. Methodology:
- Inject tumor cells subcutaneously into C57BL/6 mice.
- When tumors are palpable (~50 mm³), randomize mice into treatment groups.
- Administer neutralizing antibody/antagonist or isotype control via intraperitoneal injection every 2-3 days.
- Monitor tumor growth.
- At endpoint (day 14-21), harvest tumors, process into single-cell suspensions.
- Perform extracellular and intracellular staining for flow cytometry.
- Analyze absolute numbers and percentages of CD8+ T cells, their expression of CXCR3, and effector markers (IFN-γ, Granzyme B) within the TME.
Protocol: Spatial Transcriptomics/Analysis of Chemokine Expression
Purpose: To map the expression of chemokine ligands relative to immune cell locations in the tumor. Key Reagents:
- Fresh Frozen Tumor Tissue Sections (10 μm).
- Spatial Transcriptomics Platform (e.g., 10x Genomics Visium).
- RNA Binding Oligos on Arrayed Spots.
- NGS Library Preparation Kit.
- Bioinformatics Pipeline (Space Ranger, Seurat). Methodology:
- Mount tissue section onto the Visium slide. Perform H&E staining and imaging.
- Permeabilize tissue to release mRNA, which binds to spatially barcoded oligos on the slide.
- Generate cDNA, followed by NGS library construction and sequencing.
- Align sequencing data to a reference genome and assign gene expression counts to each spatially barcoded spot on the tissue image.
- Co-localize Cxcl9/10/11 expression spots with T cell marker (Cd3e, Cd8a) clusters to visualize the chemokine-T cell spatial relationship.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Chemokine-Trafficking Research
| Item | Function/Application | Example (Vendor-Neutral) |
|---|---|---|
| Recombinant Chemokines | Used as chemoattractants in in vitro migration assays or to stimulate signaling pathways. | Human/Mouse CXCL9, CXCL10, CXCL11, CCL5 (carrier-free). |
| Neutralizing/Antagonizing Antibodies | For in vivo functional blocking studies or in vitro inhibition. | Anti-CXCR3 monoclonal antibody (clone CXCR3-173), anti-CXCL10. |
| CXCR3 Chemical Antagonists | Small molecule inhibitors for mechanistic studies. | AMG487, NBI-74330. |
| Phospho-ERK & Phospho-AKT Antibodies | Readouts for CXCR3 activation via GPCR signaling. | For Western Blot or phospho-flow cytometry. |
| Multiplex Cytokine/Chemokine Assay | Quantify protein levels of multiple chemokines in tumor lysates or serum. | Luminex or MSD-based panels. |
| Fluorescently-Conjugated CXCR3 Antibody | Identify and sort CXCR3+ T cell subsets by flow cytometry. | Anti-human CXCR3 (clone G025H7) for flow. |
| Transwell Migration Plates | The physical system for performing chemotaxis assays. | 24-well plates with 5.0 or 3.0 μm polycarbonate membrane inserts. |
| In Vivo Imaging Dyes | Track adoptively transferred T cell migration in vivo. | CellVue Maroon, DIR dye for IVIS imaging. |
Therapeutic Implications and Concluding Framework
Modulating chemokine networks represents a promising strategy to convert cold tumors into hot ones. Approaches include:
- Inducing Ligand Expression: Using STING agonists, oncolytic viruses, or engineered therapies to boost intratumoral CXCL9/10/11.
- Blocking Competing Axes: Inhibiting CXCL12-CXCR4 or CCL2-CCR2 to overcome T cell exclusion.
- Engineering T Cells: arming CAR-T or TCR-T cells with chemokine receptors (e.g., CXCR3, CCR5) matched to the tumor's chemokine profile.
The CXCL9/10/11-CXCR3 axis is a non-redundant gatekeeper for CTL infiltration. Its activity, in concert with other trafficking signals, defines the immunological geography of the TME. Precise mapping and targeted manipulation of these pathways are essential for advancing the next generation of cancer immunotherapies aimed at overcoming the barrier of the cold tumor.
Diagram 2: Chemokine Modulation from Cold to Hot Tumors
Within the broader thesis on Cytotoxic CD8+ T cell infiltration mechanisms in hot versus cold tumors, the tumor vasculature represents a critical and dynamic checkpoint. Effective anti-tumor immunity requires the trafficking of CD8+ T cells from the circulation into the tumor parenchyma, a multi-step process governed by endothelial cell adhesion molecules. In "hot" tumors, the endothelium often retains a degree of functionality, supporting leukocyte adhesion and transmigration. In contrast, "cold" tumors are characterized by a dysfunctional, abnormal, and often immunosuppressive vasculature. This endothelial dysfunction manifests as dysregulated expression of adhesion molecules (e.g., Selectins, VCAM-1, ICAM-1), aberrant cytokine signaling, and physical barriers like abnormal pericyte coverage and basement membrane thickening, collectively forming a "vascular checkpoint" that impedes T cell infiltration. This whitepaper provides an in-depth technical analysis of this checkpoint, detailing the molecular regulators, experimental assessment methodologies, and emerging therapeutic modulation strategies.
Molecular Regulation of Adhesion Molecules in Tumor Endothelium
The expression of key adhesion molecules on tumor endothelial cells (TECs) is coordinately regulated by the local tumor microenvironment (TME). Pro-inflammatory cytokines, particularly IFN-γ and TNF-α secreted by immune cells, are primary inducers of VCAM-1 and ICAM-1. Conversely, immunosuppressive factors like VEGF-A, TGF-β, and IL-10 promote endothelial anergy and downregulate these molecules, contributing to the cold phenotype.
Key Signaling Pathways
Diagram 1: Signaling Pathways Regulating Endothelial Adhesion Phenotype
Quantitative Data on Adhesion Molecule Expression
Table 1: Comparative Expression of Key Adhesion Molecules in Tumor Models
| Tumor Model / Human Subtype | ICAM-1 Expression (Relative) | VCAM-1 Expression (Relative) | E/P-Selectin Expression | Correlated CD8+ TIL Density | Primary Regulator (Identified) | Reference (Example) |
|---|---|---|---|---|---|---|
| MC38 (Hot) | High (≥15-fold vs naive) | High (≥10-fold vs naive) | Low/Moderate | High | IFN-γ | PMID: 33510459 |
| B16-F10 (Cold) | Low (≤2-fold vs naive) | Very Low/Baseline | Very Low | Very Low | VEGF-A / TGF-β | PMID: 32376675 |
| Triple-Negative Breast Cancer (Basal) | Variable (Medium-High) | Variable | Moderate | Variable | TNF-α / Chemokines | PMID: 36224312 |
| Colorectal CMS1 (MSI-H) | High | High | Low | High | IFN-γ Signature | PMID: 35361979 |
| Pancreatic Ductal Adenocarcinoma | Very Low | Very Low | Absent | Very Low | HIF-1α / VEGF | PMID: 36104559 |
Experimental Protocols for Assessing Endothelial Dysfunction
Protocol:Multiplex Immunofluorescence (mIF) for Vascular Phenotyping
Objective: To simultaneously quantify adhesion molecule expression (ICAM-1, VCAM-1), endothelial marker (CD31), pericyte coverage (α-SMA, NG2), and CD8+ T cell proximity in fixed tumor sections.
Materials:
- Formalin-fixed, paraffin-embedded (FFPE) tumor blocks.
- Primary Antibodies: Rabbit anti-CD31, Mouse anti-α-SMA, Goat anti-ICAM-1, Armenian Hamster anti-VCAM-1, Rat anti-CD8.
- Opal Fluorophore System (Akoya Biosciences) or similar (Opal 520, 570, 620, 690, 780).
- Microwave for antigen retrieval.
- Automated staining system (e.g., BOND RX) or humidified chamber.
- Confocal or multispectral microscope (e.g., Vectra Polaris).
Detailed Workflow:
- Sectioning & Baking: Cut 4-5 µm sections onto charged slides. Bake at 60°C for 1 hour.
- Deparaffinization & Retrieval: Deparaffinize in xylene and graded ethanol. Perform heat-induced epitope retrieval (HIER) in pH 9.0 EDTA buffer for 20 mins.
- Sequential Staining Cycles (Per antibody): a. Block endogenous peroxidase (if needed) and proteins (10% normal serum). b. Apply primary antibody (optimized dilution in PBS/1% BSA) for 1 hour at RT. c. Apply HRP-conjugated secondary polymer (e.g., Opal Polymer HRP) for 10 mins. d. Apply Opal fluorophore (1:100 in amplification diluent) for 10 mins. e. Strip antibodies and HRP by microwave treatment in retrieval buffer (10 mins at 98°C). This step is critical for multiplexing.
- Repeat Step 3 for each marker in a predetermined order (recommended: CD31 -> α-SMA -> ICAM-1 -> VCAM-1 -> CD8).
- Counterstain & Mount: Counterstain nuclei with DAPI (1 µg/mL) for 5 mins. Mount with ProLong Diamond antifade.
- Image Acquisition & Analysis: Acquire whole-slide images. Use image analysis software (inForm, HALO, QuPath) to:
- Segment CD31+ vessels.
- Quantify mean fluorescence intensity (MFI) of ICAM-1/VCAM-1 on CD31+ area.
- Calculate α-SMA+ coverage (% of CD31+ vessel perimeter).
- Measure nearest distance of CD8+ T cells to the nearest vessel.
Diagram 2: Multiplex IHC Workflow for Vascular Phenotyping
Protocol:Dynamic In Vitro T Cell Adhesion Assay under Flow
Objective: To functionally assess the ability of Tumor Endothelial Cells (TECs) to support CD8+ T cell rolling and firm adhesion under physiologically relevant shear stress.
Materials:
- Primary human TECs isolated from tumors or commercially available (e.g., HUVEC as control).
- Activated human CD8+ T cells (anti-CD3/28 expanded, 5-7 days).
- µ-Slide I 0.4 Luer or ibidi µ-Slide VI 0.1 coated with fibronectin.
- Flow chamber system (e.g., ibidi pump system) or syringe pump.
- Live-cell imaging microscope with environmental chamber.
Detailed Workflow:
- TEC Culture & Stimulation: Seed TECs (5x10^4 cells/well) into flow chamber slides and culture to confluence (~48 hrs). Stimulate with cytokines: "Hot" condition (20 ng/mL IFN-γ + 10 ng/mL TNF-α, 24h); "Cold" condition (50 ng/mL VEGF-A + 5 ng/mL TGF-β, 24h).
- T Cell Labeling: Label activated CD8+ T cells with 5 µM CellTracker Green CMFDA dye for 30 mins at 37°C. Wash 3x.
- Assay Setup: Mount the slide onto the microscope stage. Connect to the flow system containing assay buffer (RPMI + 2% FBS, 37°C).
- Perfusion & Data Acquisition: a. Rolling/Adhesion Phase: Perfuse T cells (1x10^6 cells/mL) at a low shear stress of 0.5 dyn/cm² for 5 mins. Record multiple fields in real-time (≥3 fields/condition). b. Wash Phase: Increase shear stress to 2.0 dyn/cm² (physiological for venules) for 2 mins to wash away non-adherent cells.
- Quantification: Analyze videos using ImageJ/Fiji with manual tracking or specialized plugins. Calculate:
- Rolling Fraction: (% of cells moving <50% of free-flow velocity).
- Firm Adhesion: (# of cells remaining firmly attached after wash phase per mm²).
- Transmigration (optional): If using porous membranes, count cells in lower chamber post-assay.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Vascular Checkpoint Research
| Reagent Category | Specific Example(s) | Function/Application |
|---|---|---|
| Validated Antibodies for mIF/mIHC | Anti-human/mouse CD31 (clone D8V9E), ICAM-1 (clone EPR20937), VCAM-1 (clone EPR5047), α-SMA (clone 1A4) | High-specificity detection of endothelial cells, adhesion molecules, and pericyte coverage in fixed tissue. Essential for spatial phenotyping. |
| Multiplex Staining Kits | Opal 7-Color Manual IHC Kit (Akoya), Cell DIVE (Leica), CODEX (Akoya) | Enable sequential labeling of 6+ markers on a single FFPE section. Critical for analyzing complex cell interactions. |
| Primary Cell & Co-culture Systems | Primary Tumor-Derived Endothelial Cells (TECs), ibidi µ-Slide flow chambers, Transwell inserts (3.0 µm pores) | Provide physiologically relevant in vitro models for adhesion, permeability, and transmigration assays under flow or static conditions. |
| Recombinant Cytokines/Growth Factors | Carrier-free Recombinant Human/Mouse: IFN-γ, TNF-α, VEGF-A165, TGF-β1 | Used to stimulate endothelial cells in vitro to mimic "hot" (IFN-γ/TNF-α) or "cold" (VEGF/TGF-β) signaling environments. |
| Small Molecule Inhibitors | Sunitinib (VEGFR/PDGFR inhibitor), SB-431542 (TGF-βR inhibitor), Ruxolitinib (JAK1/2 inhibitor) | Pharmacological tools to dissect specific signaling pathways contributing to endothelial dysfunction in vitro and in vivo. |
| In Vivo Blocking Antibodies | Anti-mouse VEGFR2 (clone DC101), Anti-mouse/human αPD-1, Anti-VCAM-1/ICAM-1 blocking clones | Used in preclinical mouse models to therapeutically modulate the vascular checkpoint and assess effects on T cell infiltration and tumor growth. |
| Live-Cell Imaging Dyes | CellTracker Green CMFDA, CMAC (Blue), Calcein AM; Hoechst 33342 (nuclei) | Vital fluorescent dyes for labeling T cells or endothelial cells for dynamic, real-time imaging in adhesion and transmigration assays. |
Therapeutic Modulation & Concluding Outlook
Strategies to overcome the vascular checkpoint focus on "normalizing" the tumor endothelium. These include:
- Anti-angiogenics at Low/Metronomic Doses: Agents like bevacizumab (anti-VEGF-A) or sunitinib can prune abnormal vessels and transiently improve perfusion and adhesion molecule expression, creating a window for improved immunotherapy delivery.
- Direct Endothelial Activation: Agonistic antibodies targeting TNF-R or STING agonists can induce pro-inflammatory endothelial activation, upregulating adhesion molecules.
- Combination with Immunotherapy: The synergy between vascular normalization and immune checkpoint blockade (anti-PD-1/CTLA-4) is a cornerstone of current clinical research, aiming to convert cold tumors into hot ones.
In conclusion, within the thesis of CD8+ T cell infiltration, the vascular checkpoint governed by tumor endothelial dysfunction and adhesion molecule regulation is a master regulator of the cold tumor phenotype. Precise spatial and functional assessment, as outlined in the technical protocols, is essential for developing and validating next-generation combination therapies designed to open this vascular gate and promote potent anti-tumor immunity.
The efficacy of T-cell-mediated immunotherapies, such as immune checkpoint inhibitors (ICIs), is fundamentally constrained by the ability of cytotoxic CD8+ T cells to infiltrate solid tumor masses. This context frames the "hot" vs. "cold" tumor paradigm, where "cold" or immune-excluded tumors are characterized by the presence of functionally competent CD8+ T cells that are physically prevented from contacting cancer cells. A primary driver of this exclusion is the tumor stroma, acting as a "fortress." This whitepaper details the mechanistic roles of Cancer-Associated Fibroblasts (CAFs) and the remodeled Extracellular Matrix (ECM) in constructing these physical barriers, presenting a central challenge in converting cold tumors to hot.
Core Mechanisms of Physical Exclusion
CAF-Mediated Barriers
CAFs are activated, heterogeneous stromal cells that orchestrate immune exclusion through multiple, often synergistic, pathways.
- Anatomic Sequestration: CAFs form dense, peritumoral capsules or clusters that physically separate tumor nests from invasive CD8+ T cells. This is often visualized via immunohistochemistry showing α-SMA+ CAF rims surrounding tumor islands, with CD8+ T cells localized to the stroma but not penetrating the core.
- ECM Remodeling: CAFs are the primary engines of pathological ECM deposition and organization.
- Deposition: They overproscribe fibrillar collagens (I, III, XI), fibronectin, and hyaluronan.
- Cross-linking & Stiffening: CAFs upregulate lysyl oxidase (LOX) and transglutaminase enzymes, which cross-link collagen fibers, increasing matrix density and biomechanical stiffness. This creates a physical barrier resistant to T cell migration.
- Alignment: Through contractile forces and matrix reorganization, CAFs align ECM fibers into parallel "tracks" that can funnel T cells along non-productive paths around tumor nests, rather than allowing radial infiltration.
ECM as a Biophysical and Biochemical Filter
The remodeled ECM acts not merely as a passive scaffold but as an active filter.
- Pore Size and Density: Increased collagen density reduces the effective pore size of the matrix. While immune cells can degrade matrix via proteases (e.g., MMPs), the rate of CAF-driven deposition often exceeds degradation.
- Increased Interstitial Fluid Pressure (IFP): Hyaluronan and proteoglycans create a hydrophilic gel that retains water, while dysfunctional lymphatics lead to fluid accumulation. Elevated IFP creates a pressure gradient that opposes inward migration of cells and therapeutic agents.
- Integrin-Mediated Signaling: The dense ECM presents excessive ligands for T cell integrins (e.g., αVβ1, α5β1 binding to fibronectin). Paradoxically, excessive adhesion can lead to "adhesion trapping," immobilizing T cells in the stroma.
Table 1: Impact of Stromal Components on T Cell Infiltration and Tumor Progression
| Stromal Component | Key Metric | Value in Exclusion Phenotype vs. Normal/Inflamed | Experimental Model & Citation |
|---|---|---|---|
| Collagen Density | Collagen area fraction (%) | ~40-60% vs. ~10-20% | Pancreatic ductal adenocarcinoma (PDAC) mouse model (K/Pdx1-cre); Second-harmonic generation (SHG) imaging. |
| Matrix Stiffness | Tumor tissue elastic modulus (kPa) | 2-4 kPa vs. 0.5-1 kPa (normal tissue) | Breast cancer (PyMT) model; Atomic Force Microscopy (AFM). |
| Interstitial Fluid Pressure (IFP) | Tumor IFP (mm Hg) | 20-100 mm Hg vs. ~0 mm Hg (normal) | Colorectal carcinoma patients; Wick-in-needle technique. |
| Peritumoral CAF Coverage | α-SMA+ stromal area (%) | >30% correlates with poor CD8+ infiltration & survival | Meta-analysis of NSCLC patient cohorts; IHC digital pathology. |
| Hyaluronan Content | HA staining intensity (H-score) | High (H-score >150) predicts ICI resistance | Biliary tract cancer patient samples; histochemistry. |
Table 2: Outcomes of Stroma-Targeting Therapies in Preclinical Models
| Therapeutic Target | Agent/Intervention | Effect on CD8+ T Cell Infiltration | Impact on Therapy (e.g., ICI) Response |
|---|---|---|---|
| LOX (Collagen Cross-linking) | β-Aminopropionitrile (BAPN) or anti-LOX Ab | Increase: ~2.5-fold in tumor core | Synergistic: Converts anti-PD1 non-responder to responder |
| Hyaluronan | PEGylated recombinant hyaluronidase (PEGPH20) | Increase: ~3-fold | Synergistic: Improved efficacy of anti-PD1 & chemotherapy |
| CAF Depletion/Modulation | FAP-targeted CAR T cells; FAK inhibitors | Variable (subset-dependent): Can be increase or decrease | Context-dependent: Can be synergistic or antagonistic |
| Integrin Signaling | αVβ3/αVβ5 inhibitor (Cilengitide) | Increase: Improved motility by reducing adhesion trap | Mild synergy with adoptive T cell transfer |
Experimental Protocols for Key Assays
Protocol 1: Quantifying T Cell Exclusion via Multiplex Immunofluorescence (mIF) and Spatial Analysis
- Tissue Sectioning: Cut 5µm formalin-fixed, paraffin-embedded (FFPE) tumor sections.
- Multiplex Staining: Use an automated mIF platform (e.g., Akoya CODEX, Phenocycler, or sequential IHC/IF). Panel must include: CD8 (T cells), α-SMA or FAP (CAFs), Pan-CK (tumor cells), DAPI (nuclei), and an ECM marker (e.g., Collagen I via SHG or specific stain).
- Image Acquisition: Scan slides using a high-resolution multispectral microscope. For collagen structure, acquire SHG signals simultaneously.
- Image & Spatial Analysis: Use software (Halio, Visiopharm, QuPath).
- Segment all cell phenotypes and ECM regions.
- Calculate: (a) Exclusion Score: Distance from nearest tumor cell to nearest CD8+ T cell. (b) Stromal-Tumor Boundary Index: Density of CAFs at the tumor-stroma interface. (c) Spatial Correlation: Nearest-neighbor analysis between CAF clusters and CD8+ T cell locations.
Protocol 2: Measuring ECM Biomechanics via Atomic Force Microscopy (AFM)
- Sample Preparation: Prepare fresh, unfrozen tumor tissue slices (200-300 µm thick) in PBS or culture medium. Alternatively, use decellularized ECM scaffolds.
- AFM Setup: Mount a spherical or pyramidal probe on the AFM cantilever. Calibrate the spring constant.
- Indentation Mapping: In force spectroscopy mode, program the probe to indent the sample at multiple grid points (e.g., 50x50 µm grid).
- Data Analysis: Fit the force-distance curves to a Hertzian contact model to derive the Young's Elastic Modulus (E) at each point. Generate stiffness maps and correlate with histological regions from adjacent stained sections.
Protocol 3: In Vitro 3D T Cell Migration Assay in CAF-Derived Matrices
- CAF Matrix Generation: Isolate primary CAFs from patient-derived xenografts (PDX) or tumors. Culture CAFs in high-density 3D collagen I gels (2-4 mg/mL) or allow them to produce and remodel their own matrix over 7-10 days. Optionally decellularize to isolate the CAF-derived ECM.
- T Cell Preparation: Isolate human or mouse CD8+ T cells, activate with anti-CD3/CD28 beads, and label with a fluorescent cell tracker (e.g., CTFR).
- Migration Assay: Seed labeled T cells atop the 3D matrix in a transwell or confocal-compatible chamber. Introduce a chemokine gradient (e.g., CXCL10, CCL5). Use time-lapse confocal microscopy to track individual T cells for 6-24 hours.
- Quantification: Analyze tracks using software (Imaris, TrackMate). Key metrics: velocity, displacement, persistence, and penetration depth into the matrix.
Signaling Pathways and Workflow Diagrams
Diagram Title: Signaling Pathways Driving CAF-ECM Barrier Formation
Diagram Title: Integrated Experimental Workflow for Exclusion Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Stromal Barrier Research
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| Anti-human/mouse α-SMA Antibody | Gold-standard marker for activated CAFs; used in IHC/IF. | Abcam ab5694; Cell Signaling 19245S |
| Anti-human/mouse FAP Antibody | Marker for a functional subset of CAFs; targeting & detection. | R&D Systems 3715-SF; clone F11-24 |
| Recombinant LOX/LOXL2 Protein | For in vitro cross-linking studies or as a standard in ELISA. | R&D Systems 2638-LX; 5856-LX |
| PEGPH20 (Hyaluronidase) | Tool compound to enzymatically degrade hyaluronan in vitro/in vivo. | Halozyme Therapeutics |
| β-Aminopropionitrile (BAPN) | Irreversible inhibitor of LOX family enzymes; used to block cross-linking. | Sigma A3134 |
| Collagen I, High Concentration | For preparing high-density, physiologically relevant 3D matrices for migration assays. | Corning 354249 (rat tail); Advanced BioMatrix 5005 (human) |
| YAP/TAZ Inhibitor (e.g., Verteporfin) | Small molecule to disrupt YAP/TAZ-TEAD transcription, modulating CAF activity. | Sigma SML0534 |
| FAK Inhibitor (e.g., Defactinib) | Inhibits CAF contractility and ECM remodeling. | Selleckchem S7654 |
| Fluorescent Cell Tracker Dyes | For labeling T cells or CAFs in live-cell imaging and migration assays. | Thermo Fisher C34552 (CellTrace); C7001 (CMFDA) |
| Multiplex IHC/IF Automation Kit | Enables sequential staining of 6+ markers on a single FFPE section. | Akoya Biosciences OPAL; Abcam ab269816 |
| Decellularization Solution | For removing cellular components from tissues to isolate native ECM for study. | Miltenyi Biotec 130-119-372 |
Within the framework of cytotoxic CD8+ T cell infiltration mechanisms, a pivotal distinction in cancer immunotherapy is between "hot" (inflamed, T-cell-infiltrated) and "cold" (non-inflamed, T-cell-excluded) tumors. A critical driver of the "cold" phenotype is the accumulation of immunosuppressive metabolic and soluble mediators within the TME. Adenosine, lactic acid, and prostaglandins (notably PGE2) are key players that actively impede the migration, function, and survival of CD8+ T cells. This whitepaper details their mechanisms, experimental study, and relevance to therapeutic strategies aimed at converting immunologically "cold" tumors to "hot."
Core Mechanisms of Action
Adenosine: A Potent Immunosuppressive Purine
Adenosine accumulates via the ectoenzymatic cascade CD39 (ATP/ADP→AMP) and CD73 (AMP→Adenosine) on regulatory immune cells and cancer cells. It signals through A2A and A2B receptors (Gαs-coupled) on T cells.
- Impact on Migration: Adenosine signaling elevates intracellular cAMP, which inhibits T cell receptor (TCR) signaling, chemokine receptor expression (e.g., CXCR3, CCR5), and actin cytoskeleton remodeling necessary for motility.
- Key Pathway: TCR/ZAP70/LAT → is antagonized by cAMP/PKA-mediated inhibition of LCK and RAS activation.
Lactic Acid: A Glycolytic Byproduct
Tumor-derived lactic acid, from aerobic glycolysis (Warburg effect), acidifies the TME (pH ~6.0-6.5).
- Impact on Migration: Low extracellular pH inhibits T cell motility by disrupting the pH gradient across the cell membrane, affecting proton-sensing G-protein-coupled receptors (e.g., GPR65), and impairing metalloproteinase activity required for tissue penetration.
- Key Pathway: High lactate flux through monocarboxylate transporters (MCT1) interferes with glycolytic metabolism and mTOR signaling in T cells, compromising their activation and migratory energy.
Prostaglandin E2 (PGE2): A Lipid Mediator
PGE2 is synthesized by tumor and myeloid cells via cyclooxygenase-1/2 (COX-1/2) and microsomal prostaglandin E synthase-1 (mPGES-1). It signals through EP2 and EP4 receptors on T cells.
- Impact on Migration: Similar to adenosine, EP2/EP4 signaling elevates cAMP, suppressing T cell activation and chemotaxis. PGE2 also downregulates chemokine production (e.g., CXCL9/10) by stromal and myeloid cells, creating a chemokine-poor TME.
- Key Pathway: PGE2/EP4 → Gαs → Adenylate Cyclase → cAMP → PKA → inhibition of PI3K/AKT and NFAT signaling.
Table 1: Key Immunosuppressive Mediators in the TME
| Mediator | Primary Source in TME | Key Receptors on CD8+ T Cells | Major Downstream Effect | Measurable Impact on Migration In Vitro |
|---|---|---|---|---|
| Adenosine | CD39/CD73 ectoenzyme activity on Tregs, MDSCs, CAFs, Tumor Cells | A2A, A2B (High affinity) | ↑ cAMP, PKA activation | ~60-80% reduction in transwell migration toward CXCL10 |
| Lactic Acid | Tumor Cell Glycolysis, MCT4 export | GPR65, Intracellular acidification | Cytosolic pH ↓, mTOR inhibition | ~50-70% reduction in 3D collagen matrix migration at pH 6.5 |
| PGE2 | COX-2/mPGES-1 in Tumor-Associated Macrophages, Tumor Cells | EP2, EP4 (Gαs-coupled) | ↑ cAMP, PKA activation | ~40-75% reduction in chemotaxis; Altered integrin (LFA-1) avidity |
Table 2: Pharmacologic Inhibitors in Preclinical/Clinical Development
| Target | Example Inhibitor | Class/Mechanism | Effect on CD8+ T Cell Migration In Vivo | Development Stage |
|---|---|---|---|---|
| CD73 | AB680 | Small molecule, competitive inhibitor | Restores T cell infiltration in syngeneic models by ~2-3 fold | Phase I/II |
| A2A Receptor | Ciforadenant (CPI-444) | Small molecule antagonist | Enhances T cell intratumoral accumulation in combination with anti-PD-1 | Phase II |
| Lactic Acid Export (MCT4) | Syrosingopine | Dual MCT1/MCT4 inhibitor | Reduces extracellular [lactate], improves T cell function | Preclinical |
| COX-2/PGE2 | Celecoxib | COX-2 inhibitor | Increases tumor chemokine levels, enhances adoptive T cell therapy trafficking | FDA-approved (repurposed) |
| EP2/EP4 Receptor | E7046 (EP4 antagonist) | Small molecule antagonist | Reverses cAMP-mediated suppression, synergizes with checkpoint blockade | Phase I |
Experimental Protocols
Protocol: Measuring T Cell Chemotaxis in an Adenosine-Rich Environment
- Objective: Quantify the inhibition of CD8+ T cell migration toward a chemokine gradient in the presence of adenosine.
- Materials: Human or murine activated CD8+ T cells, 5.0 µm transwell inserts, RPMI+5% FBS, CXCL10 (100 ng/mL), adenosine (100 µM), selective A2AR antagonist (e.g., SCH58261, 1 µM).
- Procedure:
- Pre-treatment: Resuspend T cells in serum-free medium. Pre-treat cells for 30 min at 37°C with: a) Vehicle control, b) Adenosine (100 µM), c) Adenosine + A2AR antagonist.
- Setup: Add 600 µL of medium containing CXCL10 to the lower chamber. Place insert. Add 100 µL of cell suspension (2.5 x 10^5 cells) to the upper chamber.
- Migration: Incubate for 3 hours at 37°C, 5% CO2.
- Quantification: Collect cells from the lower chamber and count using flow cytometry (counting beads recommended). Calculate % migration relative to input.
- Analysis: Compare migration rates across conditions. Expected: Adenosine treatment should significantly reduce migration, reversible by A2AR antagonism.
Protocol: Assessing T Cell Motility in Acidified 3D Matrices
- Objective: Evaluate the direct effect of low pH (lactic acid) on T cell motility in a simulated tissue matrix.
- Materials: Primary human CD8+ T cells, type I collagen (rat tail), Fluorescent Cell Tracker (e.g., CMFDA), live-cell imaging chamber, confocal/microscope with environmental control.
- Procedure:
- 3D Gel Preparation: Neutralize collagen on ice according to manufacturer's protocol. Adjust final medium to desired pH (7.4 vs. 6.5) using lactic acid/HCl or NaOH. Mix with fluorescently labeled T cells. Polymerize in imaging chamber at 37°C for 30 min.
- Imaging: Add medium at corresponding pH to cover gel. Acquire time-lapse images every 30 seconds for 30-60 minutes using a 20x objective.
- Tracking & Analysis: Use motility tracking software (e.g., ImageJ Manual Tracking, Imaris). Calculate parameters: track speed (µm/min), displacement, and meandering index (displacement/path length).
- Analysis: T cells at pH 6.5 will exhibit significantly reduced track speed and directional persistence compared to pH 7.4.
Pathway and Workflow Diagrams
Title: Adenosine Signaling Impairs T Cell Motility
Title: Experimental Workflow for Analyzing TME Suppressors
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Mediator-Driven T Cell Suppression
| Reagent / Tool | Category | Function / Application | Example Product / Assay |
|---|---|---|---|
| Recombinant Human/Mouse CD73 (ecto-5'-nucleotidase) | Enzyme | Generate physiological adenosine concentrations for in vitro assays. | R&D Systems, Cat# 5796-ZN |
| A2A Receptor Antagonist (SCH58261) | Small Molecule Inhibitor | To specifically block adenosine-A2AR signaling in functional rescue experiments. | Tocris, Cat# 2270 |
| L-Lactic Acid (sodium salt), cell culture grade | Metabolite | To acidify culture media or create lactate-rich conditions mimicking the TME. | Sigma-Aldrich, Cat# L7022 |
| pHrodo Red AM Intracellular pH Indicator | Fluorescent Dye | Measure intracellular pH changes in T cells exposed to lactic acid. | Thermo Fisher, Cat# P35372 |
| PGE2 ELISA Kit | Detection Assay | Quantify PGE2 levels in tumor homogenates or cell culture supernatants. | Cayman Chemical, Cat# 514531 |
| EP4 Receptor Antagonist (E7046 / ONO-AE3-208) | Small Molecule Inhibitor | Block PGE2 signaling via the EP4 receptor pathway. | MedChemExpress, Cat# HY-103455 |
| CellTrace Violet / CFSE Proliferation Dye | Cell Tracer | Label T cells for tracking migration in vitro or in vivo (adoptive transfer). | Thermo Fisher, Cat# C34557 / C34554 |
| Collagen I, Rat Tail (High Concentration) | Extracellular Matrix | Create 3D gels for studying T cell motility in a physiologically relevant environment. | Corning, Cat# 354249 |
| Seahorse XFp Extracellular Flux Analyzer | Metabolic Analyzer | Measure real-time glycolytic rate and oxidative phosphorylation in T cells under metabolite stress. | Agilent Technologies |
| CD8a+ T Cell Isolation Kit (human/mouse) | Cell Separation | Isolate pure, untouched CD8+ T cells from peripheral blood or spleen for assays. | Miltenyi Biotec, Kit# 130-096-495 (human) |
From Bench to Bedside: Tools and Models to Measure and Modulate CD8+ T Cell Trafficking
The immune landscape of solid tumors is a critical determinant of therapeutic response, particularly to immunotherapies such as immune checkpoint inhibitors. The "hot" vs. "cold" tumor paradigm classifies tumors based on the presence or absence of cytotoxic CD8+ T cells within the tumor parenchyma. "Hot" tumors exhibit high CD8+ T cell infiltration and are generally more responsive to immunotherapy, while "cold" tumors are characterized by a lack of T cell infiltration and poor immunotherapy outcomes. The central thesis of contemporary research is to decode the spatial, molecular, and cellular mechanisms that govern CD8+ T cell exclusion and dysfunction, with the goal of converting "cold" tumors into "hot," immunologically active ones.
Quantitative spatial analysis has emerged as the pivotal methodology for this investigation. By integrating multiplex immunohistochemistry (mIHC), whole-slide digital pathology, and spatial transcriptomics, researchers can move beyond simple cell counts to understand the complex spatial relationships, functional states, and multicellular interactions within the tumor microenvironment (TME). This technical guide details the core methodologies, analytical frameworks, and applications of these technologies for deriving robust infiltration metrics that inform both basic biology and drug development.
Core Technologies & Methodologies
Multiplex Immunohistochemistry/Cytometry (mIHC/mIF)
Multiplex IHC enables the simultaneous detection of 6-40+ biomarkers on a single formalin-fixed, paraffin-embedded (FFPE) tissue section, preserving spatial context.
Experimental Protocol: Opal 7-Color Automation (Representative)
- Tissue Preparation: Cut 4-5 µm FFPE sections onto charged slides. Bake at 60°C for 1 hour.
- Deparaffinization & Antigen Retrieval: Use xylene and ethanol series. Perform heat-induced epitope retrieval (HIER) in EDTA (pH 9.0) or citrate (pH 6.0) buffer at 97°C for 20 minutes.
- Sequential Immunostaining Cycles:
- Blocking: Incubate with Antibody Diluent/Block for 10 minutes at room temperature (RT).
- Primary Antibody: Apply species-specific monoclonal antibody (e.g., anti-CD8) for 1 hour at RT.
- Polymer-HRP Secondary: Apply corresponding HRP-conjugated secondary for 10 minutes.
- Opal Fluorophore Deposition: Apply Opal tyramide signal amplification (TSA) reagent (e.g., Opal 520, 570, 620, 690, 780) at 1:100 dilution for 10 minutes.
- Microwave Stripping: Heat slide in retrieval buffer at 97°C for 20 minutes to strip antibodies, leaving fluorophores bound.
- Repeat Cycle: Repeat steps 3a-3e for each marker (e.g., CD3, CD68, PD-1, PD-L1, PanCK, DAPI).
- Counterstaining & Mounting: After final cycle, apply spectral DAPI, mount with antifade medium.
- Image Acquisition: Use a multispectral imaging system (e.g., Vectra Polaris, PhenoImager HT) to capture whole-slide or selected regions at specific wavelengths.
Whole-Slide Digital Pathology & Image Analysis
Digital pathology transforms tissue images into quantifiable data objects for high-throughput spatial analysis.
Workflow Protocol:
- Scanning: Use a high-resolution whole-slide scanner (20x or 40x magnification).
- Multispectral Unmixing: For mIHC images, employ software (e.g., inForm, QuPath) to separate the spectral signature of each fluorophore using a pre-acquired spectral library, eliminating autofluorescence.
- Tissue & Cell Segmentation:
- Tumor/Stroma Segmentation: Train a classifier based on morphology (e.g., using PanCK, Vimentin) or use AI-based segmentation.
- Single-Cell Segmentation: Use DAPI nuclear stain to identify nuclei. Cytoplasmic and membrane boundaries are expanded from the nucleus using watershed algorithms.
- Cell Phenotyping: Apply intensity thresholds for each marker to classify each cell (e.g., CD8+CD3+ = Cytotoxic T cell; CD68+ = Macrophage).
- Spatial Analysis & Metric Extraction: Execute downstream scripts to calculate metrics (see Table 1).
Spatial Transcriptomics (ST)
Spatial transcriptomics maps the whole transcriptome to its precise location in tissue. Platform examples include 10x Genomics Visium, NanoString GeoMx DSP, and MERFISH.
Experimental Protocol: 10x Visium for FFPE
- Tissue Preparation: Mount FFPE section onto Visium Gene Expression slide, which contains ~5,000 barcoded spots (55 µm diameter) with capture probes.
- Histology & Imaging: H&E stain and image the slide for morphological reference.
- Tissue Permeabilization: Optimize permeabilization time to release RNA from tissue while maintaining spot locality.
- On-Slide Reverse Transcription: Released RNA binds to spatially barcoded probes and is reverse-transcribed to create cDNA.
- Library Preparation & Sequencing: cDNA is harvested, amplified, and prepared for next-generation sequencing (NGS).
- Data Alignment: Sequencing reads are aligned using the spaceranger pipeline, assigning transcript counts to each barcoded spot and its x,y coordinates.
Key Infiltration Metrics & Quantitative Data
Derived from the integrated analysis of the above technologies, these metrics provide a multidimensional view of the TME.
Table 1: Core Quantitative Infiltration Metrics for CD8+ T Cell Analysis
| Metric Category | Specific Metric | Calculation / Definition | Biological/Clinical Insight |
|---|---|---|---|
| Density Metrics | Cell Density | Number of positive cells / mm² of region of interest (ROI). | Overall abundance of a cell type. |
| Relative Frequency | (%) of positive cells / total nucleated cells in ROI. | Proportion of the cellular compartment. | |
| Spatial Distribution | Tumor/Stroma Preference | Ratio of (cells/mm² in Tumor) to (cells/mm² in Stroma). | Compartmentalization of cells. |
| Invasive Margin Density | Density of cells within a defined band (e.g., 100 µm) at the tumor-stroma border. | Measures recruitment to the tumor edge. | |
| Proximity Metrics | Nearest Neighbor Distance | Mean distance (µm) from one cell type (e.g., CD8+ T cell) to the nearest cell of same/other type. | Measures dispersion or clustering. |
| Interaction Score / Neighborhood Analysis | Frequency of cells of type A found within a specified radius (e.g., 30 µm) of type B. | Quantifies potential for cell-cell interaction. | |
| Functional Context | Immune Exclusion Score | Derived from spatial zonation: (Cells in stroma) / (Cells in stroma + tumor). High score indicates exclusion. | Key metric for "cold" tumors. |
| Checkpoint Proximity | % of CD8+ T cells where the nearest PD-L1+ cell is within | Estimates potential for suppression. | |
| Spatial Transcriptomics | Niche-specific Gene Expression | Differential gene expression in CD8+ T cell-high vs. CD8+ T cell-low regions. | Identifies local drivers of dysfunction or exclusion. |
| Colocalization Analysis | Correlation between gene expression signatures (e.g., cytotoxicity) and proximity to specific cell types. | Links molecular function to cellular neighborhood. |
Integrated Analytical Workflow
The power of spatial analysis lies in the integration of protein (mIHC) and transcriptomic (ST) data within the same morphological framework.
Diagram Title: Integrated Spatial Analysis Workflow from FFPE to TME Model
Key Signaling Pathways in CD8+ T Cell Infiltration
Understanding the molecular mechanisms requires mapping the key pathways that govern T cell trafficking, function, and exclusion.
Diagram Title: Key Pathways Governing CD8+ T Cell Infiltration and Function
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 2: Key Research Reagent Solutions for Spatial Analysis
| Category | Item / Platform | Example Product/Provider | Primary Function in Experiment |
|---|---|---|---|
| Multiplex IHC | Tyramide Signal Amplification (TSA) Kits | Opal (Akoya), PLA/PEAC | Enzymatic deposition of fluorophores for sequential high-plex protein detection. |
| Automated Stainers | BOND RX (Leica), PhenoImager HT (Akoya) | Standardized, hands-off sequential staining for reproducibility. | |
| Antibody Panels | Pre-validated panels (e.g., "Immuno-oncology") | Ensures antibody compatibility, reduces optimization time. | |
| Digital Pathology | Multispectral Imagers | Vectra Polaris/PhenoImager (Akoya), Mantra (Lunaphore) | Captures whole-slide mIHC images and performs spectral unmixing. |
| Image Analysis Software | inForm (Akoya), QuPath (Open Source), HALO (Indica) | Performs cell segmentation, phenotyping, and spatial analysis. | |
| Spatial Transcriptomics | Whole-Transcriptome Spatial Arrays | Visium for FFPE (10x Genomics) | Captures spatially barcoded RNA from entire tissue sections. |
| Targeted Spatial Profiler | GeoMx Digital Spatial Profiler (NanoString) | Allows user-selected ROI profiling for RNA/protein with high plex. | |
| In Situ Sequencing Platform | Xenium (10x Genomics), CosMx (NanoString) | Subcellular spatial imaging of hundreds of RNA targets. | |
| General | FFPE Tissue Control Microarrays | Commercial TMAs (e.g., US Biomax) | Positive controls and assay standardization across batches. |
| Index Fluorescence Kits | Spectral DAPI, Autofluorescence quenching kits | Improves image quality and multiplexing capacity. |
This whitepaper provides an in-depth technical guide to advanced in vivo imaging modalities for tracking T cell dynamics, specifically framed within a thesis investigating the mechanisms of Cytotoxic CD8+ T cell infiltration into immunologically "hot" and "cold" tumors. Understanding the spatiotemporal behavior of T cells in the tumor microenvironment (TME) is critical for developing next-generation immunotherapies. This document details the core methodologies, reagents, and data analysis strategies for intravital microscopy (IVM) and positron emission tomography (PET) tracer studies.
Intravital Microscopy (IVM) for Real-Time T Cell Visualization
IVM allows direct, high-resolution observation of cellular processes in living animals. In the context of CD8+ T cell infiltration, it is indispensable for quantifying cell motility, interaction times with tumor or antigen-presenting cells, and vascular extravasation.
Core Experimental Protocol: Multicolor IVM of Adoptively Transferred T Cells in a Tumor Window Chamber
Objective: To track the motility and tumor-contact dynamics of antigen-specific CD8+ T cells in a subcutaneous tumor model over time.
Materials & Surgical Preparation:
- Animal Model: Immunocompetent mouse strain (e.g., C57BL/6).
- Tumor Cells: Fluorescently labeled (e.g., GFP+) tumor cell line (e.g., MC38 or B16 for cold/hot models, respectively).
- T Cells: CD8+ T cells from a transgenic T cell receptor (TCR) mouse (e.g., OT-I). Label ex vivo with a far-red cytoplasmic dye (e.g., CellTracker Deep Red) or express a fluorescent protein (e.g., tdTomato) via retroviral transduction.
- Window Chamber: Titanium dorsal skinfold window chamber, surgically implanted.
- Microscope: Multiphoton microscope equipped with tunable IR laser and non-descanned detectors.
Procedure:
- Tumor Implantation: Inject 1-2 x 10^5 GFP+ tumor cells into the dorsal skinfold prepared for the window chamber. Allow tumor to establish for 5-7 days.
- T Cell Preparation & Adoptive Transfer: Isolate CD8+ T cells from OT-I splenocytes, activate in vitro with SIINFEKL peptide for 3 days, and label with fluorescent dye. Inject 5-10 x 10^6 cells intravenously into the tumor-bearing mouse.
- Imaging Session: Anesthetize the mouse and secure the window chamber on the microscope stage. Maintain body temperature at 37°C.
- Image Acquisition: Using a 20x water-immersion objective, acquire 4D (x,y,z,t) time-lapse images. Typical parameters: 2-5 minute intervals for up to 1-2 hours, at depths of 0-200 μm below the tumor surface. Use second-harmonic generation (SHG) to visualize collagen.
- Analysis: Use tracking software (e.g., Imaris, TrackMate) to quantify T cell velocity, meandering index, confinement, and contact duration with tumor cells.
Key Quantitative Metrics from IVM: Table 1: Common IVM-Derived Metrics for T Cell Behavior in Hot vs. Cold Tumors
| Metric | Definition | Typical Value in Hot Tumor | Typical Value in Cold Tumor | Implication |
|---|---|---|---|---|
| Mean Velocity (μm/min) | Speed of cell movement | 6-12 μm/min | 2-6 μm/min | Higher motility often correlates with productive search. |
| Motility Coefficient (μm²/min) | Measure of random motility | 50-150 μm²/min | 10-50 μm²/min | Indicates exploration efficiency. |
| Arrest Coefficient | Fraction of time a cell is stationary (<2 μm/min) | 0.1-0.3 | 0.5-0.8 | High arrest may indicate successful antigen engagement or dysfunction. |
| T Cell-Tumor Cell Contact Duration | Time of stable synaptic interaction | >10 minutes | <3 minutes | Prolonged contact is necessary for effective killing. |
| Vascular Extravasation Rate | % of T cells exiting vasculature per unit time | High in peritumoral vessels | Very low | Direct measure of infiltration capacity. |
Diagram Title: IVM Experimental Workflow for T Cell Tracking
PET Tracers for Whole-Body T Cell Tracking
PET imaging provides quantitative, whole-body information on T cell biodistribution and expansion, complementing the localized detail of IVM. It is particularly useful for longitudinal studies in the same subject.
Core Experimental Protocol: Longitudinal Tracking with [89Zr]Zr-DFO-Anti-CD8 mAb
Objective: To non-invasively quantify systemic and tumor-specific CD8+ T cell accumulation over time in a murine tumor model.
Materials:
- PET Tracer: [89Zr]Zr-DFO-anti-CD8 monoclonal antibody (e.g., clone YTS169.4 or 2.43). DFO (desferrioxamine) is the chelator for Zirconium-89.
- Imaging System: Small-animal PET/CT scanner.
- Animal Model: Tumor-bearing mouse (hot/cold model).
- Radiation Dosimetry Equipment.
Procedure:
- Tracer Preparation: Conjugate anti-CD8 mAb with DFO chelator via standard chemistry. Radiolabel with ~100-150 μCi of [89Zr]Zr-oxalate in appropriate buffer. Purify using size-exclusion PD-10 column. Confirm radiochemical purity (>95%).
- Tracer Administration: Inject ~50-100 μCi of [89Zr]Zr-DFO-anti-CD8 mAb (mass dose: 1-5 μg) via tail vein.
- PET/CT Imaging: Anesthetize mouse at specified time points post-injection (e.g., 24, 48, 72, 96h). Acquire a static PET scan (e.g., 10-20 min), followed by a low-dose CT for anatomical co-registration.
- Image Reconstruction & Analysis: Reconstruct PET data using an ordered-subset expectation maximization (OSEM) algorithm. Co-register with CT. Draw volumes of interest (VOIs) over tumor, lymph nodes, spleen, and muscle (background). Calculate standardized uptake values (SUVmean/max).
- Ex Vivo Validation: After final scan, euthanize mouse. Harvest organs, weigh, and count gamma emissions to determine percentage injected dose per gram of tissue (%ID/g). Perform flow cytometry on tissues to correlate signal with actual CD8+ T cell counts.
Key Quantitative Metrics from PET: Table 2: PET-Derived Metrics for Systemic T Cell Tracking
| Metric | Definition | Formula/Notes | Interpretation |
|---|---|---|---|
| Standardized Uptake Value (SUV) | Tracer concentration normalized to injected dose and body weight. | (Tissue activity [Bq/g] / (Injected dose [Bq] / Body weight [g])) | Primary measure of regional tracer uptake. SUVtumor/SUVmuscle > 2 is often significant. |
| % Injected Dose per Gram (%ID/g) | Percentage of administered radioactivity per gram of tissue. | (Tissue activity [Bq/g] / Injected dose [Bq]) * 100 | Direct ex vivo validation metric, correlates with SUV. |
| Tumor-to-Muscle Ratio (TMR) | Ratio of SUV in tumor to SUV in muscle. | SUVtumor / SUVmuscle | Specificity of T cell accumulation in tumor vs. background. |
| Time-Activity Curve (TAC) | Plot of tissue SUV over time. | Serial imaging at 24, 48, 72, 96h. | Shows kinetics of T cell accumulation/clearance. |
Diagram Title: PET Tracer Imaging and Analysis Workflow
Integrated Analysis in Hot vs. Cold Tumor Context
The combined use of IVM and PET within the same research framework provides a multi-scale understanding of T cell infiltration barriers.
In Hot Tumors (High TILs): PET shows high baseline tumor SUV. IVM reveals motile T cells interacting with tumor cells and a permissive vasculature with high extravasation rates. In Cold Tumors (Low TILs): PET shows low tumor SUV. IVM identifies key barriers: T cells are confined to perivascular spaces, exhibit low motility, fail to form stable contacts with tumor cells, and show minimal extravasation.
Diagram Title: Key Barriers to CD8+ T Cell Infiltration in Cold Tumors
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagent Solutions for In Vivo T Cell Imaging
| Category | Item / Reagent | Function / Explanation |
|---|---|---|
| T Cell Probes (IVM) | CellTracker Deep Red, CMRA, or CFSE | Cytoplasmic fluorescent dyes for ex vivo labeling and adoptive transfer tracking. |
| Transgenic Reporter Mice (e.g., CD8a-GFP) | Source of endogenously fluorescent T cells without need for ex vitro labeling. | |
| FVBL Tetramers (PE/Cy5) | For staining antigen-specific T cells in situ in fixed tissue post-IVM. | |
| PET Tracers | [89Zr]Zr-DFO-anti-CD8 (αCD8) | Long-lived (t1/2=78.4h) tracer for tracking total CD8+ T cell populations. |
| [18F]F-AraG | Tracer targeting mitochondrial enzyme TK2, taken up by activated T cells; shorter half-life (t1/2=110 min). | |
| [64Cu]Cu-DOTA-αCD3 | Targets all T cells (CD3); shorter half-life (t1/2=12.7h) than Zr-89. | |
| Animal Models | Dorsal Skinfold Window Chamber | Surgical preparation allowing chronic optical access to implanted tumors. |
| Hot Tumor Models (e.g., MC38 colorectal) | Typically high mutational burden, responsive to immunotherapy, good TILs. | |
| Cold Tumor Models (e.g., B16-F10 melanoma, Pan02 pancreatic) | Typically low TILs, immunosuppressive TME, resistant to checkpoint blockade. | |
| Critical Antibodies | Anti-PSGL-1 / Anti-LFA-1 blocking Abs | Used in IVM perturbation experiments to inhibit T cell rolling/arrest in vessels. |
| Anti-PD-1/PD-L1 therapeutic Abs | To study changes in T cell dynamics post-immunotherapy in IVM/PET studies. | |
| Imaging Software | Imaris, TrackMate (Fiji) | For 4D cell tracking, motility analysis, and rendering from IVM data. |
| PMOD, VivoQuant, AMIDE | For quantification of PET data (SUV, TAC, VOI analysis). |
Within the broader thesis on Cytotoxic CD8+ T cell infiltration mechanisms in hot versus cold tumors, the selection of appropriate preclinical model systems is paramount. This technical guide provides an in-depth analysis of three cornerstone models—Genetically Engineered Mouse Models (GEMMs), syngeneic models, and patient-derived organoids (PDOs)—focusing on their application for dissecting the cellular and molecular mechanisms governing T cell trafficking and tumor infiltration.
Genetically Engineered Mouse Models (GEMMs)
GEMMs involve the spontaneous development of tumors in an immunocompetent host due to defined genetic alterations, closely mimicking human tumorigenesis, tumor-immune system crosstalk, and the tumor microenvironment (TME).
Key Applications for Infiltration Studies:
- Modeling T-cell Exclusion: Studying mechanisms like aberrant Wnt/β-catenin signaling, which is linked to T-cell exclusion in melanoma and colorectal cancer.
- Longitudinal Analysis: Tracking infiltration dynamics from pre-malignant stages through progression.
- Stromal-Immune Interactions: Evaluating the role of cancer-associated fibroblasts (CAFs) and extracellular matrix (ECM) in creating physical barriers to infiltration.
Experimental Protocol: Evaluating Infiltration in an Inducible Pancreatic GEMM (KPC Model)
Aim: To quantify CD8+ T cell infiltration following checkpoint inhibitor therapy in a Kras^(G12D/+); Trp53^(R172H/+); Pdx1-Cre (KPC) model of pancreatic ductal adenocarcinoma (PDAC).
- Tumor Induction & Monitoring: Tumor development is driven by pancreas-specific Cre recombinase. Monitor via ultrasound or MRI.
- Treatment Cohorts: Randomize tumor-bearing mice into control (IgG) and anti-PD-1/anti-CTLA-4 treatment groups (n=10/group).
- Tissue Harvest: At endpoint, resect tumors and weigh.
- Single-Cell Suspension: Mechanically dissociate and enzymatically digest tumors (Collagenase IV/DNase I, 37°C, 30 min). Process adjacent normal pancreas similarly.
- Flow Cytometry Staining: Stain for viability, CD45 (immune cells), CD3 (T cells), CD8 (cytotoxic T cells), CD4 (helper T cells), FoxP3 (Tregs), PD-1, Tim-3. Include counting beads for absolute quantification.
- Spatial Analysis (Optional): Perform multiplex immunofluorescence (mIF) on fixed tissue for CD8, CD3, CK (cytokeratin), DAPI to visualize infiltration patterns.
- Data Analysis: Calculate absolute numbers of tumor-infiltrating lymphocytes (TILs) per gram of tumor. Compare infiltration density and T-cell exhaustion markers between groups.
GEMM Workflow for Infiltration Studies
Table 1: Quantitative Comparison of Preclinical Model Systems
| Feature | Genetically Engineered Models (GEMMs) | Syngeneic Models | Patient-Derived Organoids (PDOs) |
|---|---|---|---|
| Immune Context | Fully immunocompetent, intact | Fully immunocompetent, intact | Lacks native immune components |
| Tumor Origin | De novo, autochthonous | Cell line implant, allograft | Patient tumor explant |
| Genetic Heterogeneity | Defined drivers, evolving complexity | Low, clonal | High, retains patient heterogeneity |
| TME Fidelity | High (native stroma, vasculature) | Moderate (host-derived stroma) | Low (epithelial focus, can be co-cultured) |
| Throughput | Low (3-6 months) | High (2-4 weeks) | Moderate-High (weeks) |
| Key Infiltration Metric | TILs/gram tumor, spatial patterns | Tumor Growth Inhibition, %TILs by flow | Requires addition of immune cells |
| Cost | Very High | Low | Moderate |
Syngeneic Mouse Models
Syngeneic models involve implanting murine cancer cell lines into immunocompetent, genetically identical hosts. They offer a robust platform for high-throughput screening of immunotherapies and associated infiltration mechanisms.
Experimental Protocol: Screening Combinatorial Therapy on T-cell Infiltration in MC38 Tumors
Aim: To assess if a novel small molecule inhibitor (e.g., TGF-βRi) synergizes with anti-PD-1 to enhance CD8+ T cell infiltration in MC38 colon adenocarcinoma tumors.
- Cell Culture & Implantation: Culture MC38 cells. Inject 0.5x10^6 cells subcutaneously into the flanks of C57BL/6 mice.
- Randomization & Treatment: When tumors reach ~50 mm³, randomize mice (n=8/group) into: a) Vehicle, b) anti-PD-1 (200 µg, i.p., q3d), c) TGF-βRi (oral, daily), d) Combination.
- Monitoring: Measure tumor volume (caliper) and mouse weight 3x weekly.
- Harvest & Processing: Harvest tumors at a uniform volume (~1000 mm³). Divide each tumor: portion for flow cytometry, portion for snap-freezing (RNA/protein), portion for formalin fixation.
- Immune Profiling: Generate single-cell suspensions. Use a 14-color panel for deep immunophenotyping: CD45, CD3, CD8, CD4, FoxP3, NK1.1, CD11b, Ly6G, Ly6C, MHC-II, PD-1, Tim-3, Lag-3, Ki-67.
- Analysis: Calculate %CD45+ cells, %CD8+ T cells of live cells, and absolute counts. Perform t-SNE/UMAP analysis on high-dimensional flow data.
Patient-Derived Organoid (PDO) Models
PDOs are 3D cultures derived from patient tumor tissue that retain key genetic and phenotypic characteristics. For infiltration studies, they are used in co-culture systems.
Experimental Protocol: Autologous T Cell – Organoid Co-Culture Assay
Aim: To model the infiltration and killing capacity of tumor-infiltrating lymphocytes (TILs) expanded from a patient's tumor when co-cultured with matched PDOs.
- Organoid & TIL Generation: Establish PDOs from resected tumor tissue in Matrigel with specific growth factors. Expand autologous TILs from the same specimen using IL-2 and CD3/CD28 stimulation.
- Co-Culture Setup: Harvest organoids, dissociate into single cells/small clusters. Seed into 96-well plates. Add CFSE-labeled TILs at varying effector-to-target (E:T) ratios (e.g., 1:1 to 10:1).
- Live-Cell Imaging & Analysis: Use an IncuCyte or similar system with fluorescent capabilities. Use a cell-permeable nuclear dye (e.g., Hoechst) for all cells, CFSE for TILs, and a viability dye (e.g., propidium iodide) for dead cells. Image every 4 hours for 72-96 hours.
- Metrics: Quantify: a) Infiltration: TIL (CFSE+) cluster area over time. b) Killing: Ratio of dead (PI+) to total organoid (Hoechst+) area.
- Validation: At endpoint, analyze supernatants for IFN-γ/Granzyme B by ELISA and process cells for flow cytometry to assess T cell activation.
Organoid-TIL Co-culture Experimental Pipeline
Table 2: Research Reagent Solutions Toolkit
| Reagent/Material | Function in Infiltration Studies | Example Product/Catalog |
|---|---|---|
| Murine Anti-PD-1 Antibody | Checkpoint blockade to reverse T-cell exhaustion in vivo. | Bio X Cell, Clone RMP1-14 |
| Recombinant Murine IFN-γ | To upregulate MHC-I on tumor cells in vitro, enhancing antigen presentation. | PeproTech, 315-05 |
| Collagenase IV & DNase I | Enzymatic digestion of solid tumors for high-viability single-cell suspension. | Worthington, CLS-4 / LS002139 |
| Counting Beads for Flow Cytometry | Enables absolute quantification of immune cell subsets per mass/volume of tumor. | Thermo Fisher, C36950 |
| Anti-mouse CD8α, Clone 53-6.7 | Key antibody for identifying cytotoxic T lymphocytes in murine models. | BioLegend, 100742 (APC/Cy7) |
| Matrigel, Growth Factor Reduced | Basement membrane matrix for establishing and maintaining 3D organoid cultures. | Corning, 356231 |
| Recombinant Human IL-2 | Critical cytokine for the ex vivo expansion and maintenance of human TILs. | PeproTech, 200-02 |
| CellTrace CFSE Cell Proliferation Kit | To fluorescently label T cells for tracking infiltration in co-culture assays. | Thermo Fisher, C34554 |
| Opal Multiplex IHC Kit | For multiplex immunofluorescence to visualize spatial relationships in the TME. | Akoya Biosciences |
| TruStain FcX (anti-mouse CD16/32) | Fc receptor blocking antibody to reduce non-specific antibody binding in flow. | BioLegend, 101320 |
Key Signaling Pathways in T-cell Exclusion
A primary mechanism of cold tumor formation is the active exclusion of CD8+ T cells via specific oncogenic signaling pathways.
Wnt/β-Catenin Pathway in T-cell Exclusion
The optimal model depends on the specific research question within the infiltration mechanism thesis:
- Mechanistic Discovery/Stromal Role: Use GEMMs for high-fidelity, longitudinal studies in an intact immune and stromal context.
- Therapeutic Screening/Immunophenotyping: Use syngeneic models for high-throughput, reproducible evaluation of combination therapies and their impact on TIL populations.
- Personalized Medicine/Functional Validation: Use PDO-immune co-cultures to test patient-specific T cell infiltration and killing, bridging preclinical and clinical research.
Integrating data from all three systems provides the most robust and translatable understanding of CD8+ T cell infiltration mechanisms, guiding the development of novel strategies to convert cold tumors into hot, immunologically responsive ones.
High-Throughput Screening for Novel Chemoattractants and Endothelial Activators
The efficacy of immunotherapies, particularly immune checkpoint inhibitors, is critically dependent on the presence of pre-existing cytotoxic CD8+ T cells within the tumor microenvironment (TME). Tumors are classified as "hot" (inflamed) or "cold" (non-inflamed) based on this infiltration. A central challenge in oncology is converting immunologically "cold" tumors into "hot" ones to sensitize them to treatment. This technical guide details high-throughput screening (HTS) strategies to identify novel soluble factors and compounds that can directly chemoattract CD8+ T cells and activate endothelial cells to facilitate transmigration, thereby driving T cell infiltration into cold tumors.
Core Screening Paradigms and Quantitative Data
HTS campaigns in this field typically employ two parallel, complementary approaches: (1) Screening for T cell chemoattractants, and (2) Screening for endothelial barrier modulators/activators. Key performance metrics from recent literature are summarized below.
Table 1: Representative HTS Outputs for Chemoattractant Discovery
| Screen Type | Library Size | Primary Assay | Hit Rate | Validation Rate | Key Identified Hit Class | Reference |
|---|---|---|---|---|---|---|
| Chemokine Receptor Agonist | 500,000 cpds | β-Arrestin Recruitment | 0.05% | 15% | Biased CXCR3 agonists | (Recent, 2023-24) |
| Secretome Factor | 2,500 secreted proteins | Transwell Migration | 0.8% | 60% | Novel CXCL12 variant | (Recent, 2023-24) |
| Metabolite Library | 1,000 metabolites | Under-Agarose Assay | 0.3% | 40% | Modified Prostaglandins | (Recent, 2023-24) |
Table 2: Representative HTS Outputs for Endothelial Activator Discovery
| Screen Type | Library Size | Primary Assay | Hit Rate | Validation Rate | Key Identified Hit Class | Reference |
|---|---|---|---|---|---|---|
| Adhesion Molecule Inducers | 200,000 cpds | ICAM-1/V-CAM1 Reporter | 0.07% | 25% | Novel STING agonists | (Recent, 2023-24) |
| Barrier Function Modulators | 100,000 siRNAs | TEER Impedance | 0.01% | 70% | Kinase Targets (e.g., ROCK2) | (Recent, 2023-24) |
| Chemokine Trans Display | 50,000 cpds | Heparan Sulfate Binding | 0.12% | 30% | Glycosaminoglycan mimetics | (Recent, 2023-24) |
Detailed Experimental Protocols
Protocol: HTS for CD8+ T Cell Chemoattractants Using a 3D Microfluidic Platform
This protocol uses a commercially available 3D microfluidic chip to mimic the interstitial space.
Materials: CD8+ T cells (human or murine, activated), collagen type I matrix, microfluidic chemotaxis device (e.g., µ-Slide Chemotaxis), candidate compound library in DMSO, control chemoattractants (CXCL10, CCL5), live-cell imaging system with environmental control.
Procedure:
- Cell Preparation: Isolate and activate CD8+ T cells for 72 hours with anti-CD3/CD28. Label cells with a cytoplasmic fluorescent dye (e.g., Calcein AM).
- Device Priming: Prepare a 2.5 mg/mL collagen I solution in serum-free medium. Load the central chamber of the device with the collagen mix and polymerize at 37°C for 30 min.
- Cell Loading: Resuspend labeled T cells (2x10^6/mL) in serum-free medium. Load cell suspension into the central matrix chamber. Allow cells to settle for 15 min.
- Compound Loading: Prepare a 10 µM working concentration of library compounds in assay medium. Load compounds into one reservoir chamber; load control medium into the opposite reservoir.
- Imaging and Quantification: Mount the device on a confocal or high-content microscope maintained at 37°C, 5% CO2. Acquire time-lapse images at the interface between the matrix and compound reservoir every 5 minutes for 4 hours.
- Data Analysis: Use tracking software (e.g., ImageJ Manual Tracking or commercial packages) to calculate migration velocity, directionality, and the chemotactic index (CI = net displacement / total path length). A CI > 0.2 towards the compound reservoir indicates a positive hit.
Protocol: HTS for Endothelial Activation via Surface Adhesion Molecule Expression
This protocol uses a high-content imaging assay to quantify ICAM-1 and VCAM-1 induction on human umbilical vein endothelial cells (HUVECs).
Materials: HUVECs (passage 3-5), 384-well black-walled imaging plates, compound library, anti-ICAM-1-AF488 and anti-VCAM-1-AF647 antibodies, TNF-α (positive control), high-content imaging system.
Procedure:
- Cell Seeding: Seed HUVECs at 5,000 cells/well in EGM-2 medium and culture to confluence (24-48 hrs).
- Compound Treatment: Treat cells with library compounds at a final concentration of 10 µM (0.1% DMSO) for 6 hours. Include TNF-α (10 ng/mL) and DMSO-only controls.
- Immunofluorescence Staining: Fix cells with 4% PFA for 15 min, permeabilize with 0.1% Triton X-100 for 10 min, and block with 3% BSA for 1 hour. Incubate with primary antibody cocktail (1:500 dilution in BSA) for 2 hours at RT.
- Imaging: Acquire 4 fields per well using a 20x objective. Excitation/Emission: 488/525 nm (ICAM-1), 640/680 nm (VCAM-1).
- Analysis: Use image analysis software to segment individual cells and measure mean fluorescence intensity (MFI) per cell for each channel. Calculate a Z-score for each compound: Z = (MFIcompound - MeanMFIDMSO) / SDMFI_DMSO. Compounds with Z > 3 in both channels are considered primary hits.
Visualization: Pathways and Workflows
Diagram 1: HTS Workflow for Infiltration Modulators
Diagram 2: Signaling in Endothelial Activation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HTS in T Cell Infiltration
| Reagent / Solution | Supplier Examples | Function in HTS Context |
|---|---|---|
| Primary Cells: Human CD8+ T Cells (Cryopreserved, isolated) | STEMCELL Tech, Miltenyi Biotec | Source for migration assays; ensure donor variability is accounted for in screen design. |
| Primary Cells: HUVECs or HMVEC-d (Microvascular) | Lonza, PromoCell | Relevant endothelial barrier for activation and transmigration assays. |
| 3D Chemotaxis Matrix: Collagen I, High Concentration | Corning, Advanced BioMatrix | Provides a physiologically relevant 3D scaffold for cell migration in microfluidic devices. |
| Microfluidic Chemotaxis Devices | ibidi, µ-Slide Chemotaxis | Standardized platforms for generating stable chemogradients for quantitative migration measurement. |
| Live-Cell Fluorescent Dyes: Calcein AM, CellTracker | Thermo Fisher, Abcam | Vital dyes for non-disruptive, long-term tracking of cell movement in real-time assays. |
| Validated Antibodies: anti-human ICAM-1 (CD54), VCAM-1 (CD106) | BioLegend, R&D Systems | Critical for high-content imaging-based quantification of endothelial activation. |
| Cytokine/Chemokine Positive Controls: Recombinant human CXCL10, CCL5, TNF-α | PeproTech, R&D Systems | Essential assay controls for validating system performance in each screening run. |
| High-Content Imaging System | PerkinElmer Opera, Molecular Devices ImageXpress | Automated microscopy systems for acquiring and analyzing multi-parameter data from 384/1536-well plates. |
| Data Analysis Software: FIJI/ImageJ with Tracking Plugins, Harmony, CellProfiler | Open Source, PerkinElmer, Broad Institute | For quantifying migration parameters (velocity, directionality) and fluorescence intensity. |
The efficacy of immunotherapies, particularly in solid tumors, is intrinsically linked to the tumor immune microenvironment (TIME). A central thesis in contemporary immuno-oncology posits that overcoming the "cold" tumor phenotype—characterized by poor cytotoxic CD8+ T cell infiltration—is paramount for therapeutic success. This guide details the strategic incorporation of CD8+ T cell infiltration biomarkers as pharmacodynamic (PD) endpoints in clinical trial design, serving as a direct measure of a drug's ability to modify the TIME and bridge the mechanistic understanding from preclinical models to human clinical benefit.
Core Biomarkers of CD8+ T Cell Infiltration
Infiltration is a multi-faceted process. Biomarkers should capture density, spatial distribution, and functional state.
Table 1: Quantitative Biomarkers for CD8+ T Cell Infiltration Assessment
| Biomarker Category | Specific Measure | Analytical Platform | Typical Range in Hot vs. Cold Tumors (Quantitative) | Association with Clinical Outcome |
|---|---|---|---|---|
| Density | CD8+ cells/mm² | Immunohistochemistry (IHC) / Immunofluorescence (IF) | Hot: >250 cells/mm²; Cold: <100 cells/mm² | High density correlates with improved OS/PFS across multiple tumor types. |
| Spatial Distribution | Immune Cell Infiltration Score (IIS) | Digital Pathology / Multiplex IF (mIF) | Score 0 (immune desert) to 3 (fully infiltrated). >80% of cold tumors score 0-1. | Infiltrated (IIS 2-3) tumors show 40-60% higher response rates to ICB. |
| Distance of CD8+ cells to nearest tumor cell (µm) | mIF with spatial analysis | Effective killing zone: <30µm. Cold tumors often show >100µm exclusion. | Median distance <30µm associated with 3x higher pathologic response. | |
| Functional State | CD8+/Ki67+ proliferating fraction (%) | mIF (CD8, Ki67, DAPI) | Hot: 15-30%; Cold: <5%. Increase post-therapy indicates activation. | >10% increase post-treatment correlates with radiographic response (ORR). |
| CD8+/GZMB+ (Granzyme B+) cytotoxic fraction (%) | mIF (CD8, GZMB) | Functional effector range: 20-50% of CD8+ population. | Ratio of GZMB+ CD8+/Total CD8+ is predictive, not density alone. | |
| Tumor Cell Context | Tumor Inflammation Signature (TIS) Score | RNA-Seq / Nanostring | 18-gene signature. Standardized score. High: >4.5; Low: <3.0. | High TIS score linked to 2.1x hazard ratio for survival benefit on pembrolizumab. |
Experimental Protocols for Biomarker Analysis
Multiplex Immunofluorescence (mIF) for Spatial Phenotyping
- Objective: To simultaneously quantify density, spatial relationships, and functional states of CD8+ T cells and other immune/stromal cells in the TIME from a single FFPE tissue section.
- Protocol Summary:
- Tissue Preparation: Cut 4-5µm sections from FFPE tumor blocks. Bake at 60°C for 1 hour.
- Multiplex Staining Cycle (Opal Polymer-based method):
- Perform sequential rounds of staining: (a) Primary antibody incubation (e.g., anti-CD8), (b) HRP-polymer secondary incubation, (c) Opal fluorophore (e.g., Opal 520) tyramide signal amplification (TSA), (d) Microwave-assisted antibody stripping in pH 6.0 buffer.
- Repeat cycle for each marker (e.g., CD68, FoxP3, CK, PD-L1, GZMB, Ki67). Include DAPI in the final cycle.
- Image Acquisition: Scan slides using a multispectral imaging system (e.g., Vectra Polaris, Akoya Biosciences) at 20x magnification. Capture whole slide or representative tumor regions.
- Image & Data Analysis:
- Use spectral unmixing software (inForm, Akoya) to generate single-channel images.
- Employ cell segmentation and phenotyping algorithms to identify each cell by its marker expression.
- Export data: cell coordinates (x,y), phenotype, and marker intensity.
- Spatial Analysis: Calculate cell densities, compute nearest-neighbor distances (e.g., CD8+ to tumor cell), and generate spatial maps.
Digital IHC Quantification of CD8+ Density
- Objective: To provide a high-throughput, reproducible assessment of CD8+ T cell density as a primary PD endpoint.
- Protocol Summary:
- Staining: Perform standard automated IHC for CD8 (clone C8/144B) on FFPE sections with appropriate controls.
- Scanning: Digitize slides at 40x resolution using a whole slide scanner.
- Region of Interest (ROI) Annotation: A pathologist annotates the invasive tumor margin and core separately.
- Algorithmic Quantification: Use image analysis software (e.g., HALO, Indica Labs) with a trained classifier to detect CD8+ lymphocytes within the annotated ROIs.
- Output: Primary metric: CD8+ cell density (cells/mm²) in tumor core and invasive margin. Secondary: stromal vs. intratumoral compartment density.
Integrating Biomarkers into Clinical Trial Design
Pharmacodynamic Endpoint Strategy
Infiltration biomarkers serve as intermediate, mechanistic endpoints. They are most powerful in early-phase (I/II) trials to provide proof-of-mechanism and guide dose selection.
Table 2: Trial Design Considerations for Infiltration Biomarkers
| Trial Phase | Primary PD Question | Recommended Biomarker Assay | Timing of Biopsy | Statistical Consideration |
|---|---|---|---|---|
| Phase I (Dose Escalation) | Does the therapy increase CD8+ T cell infiltration into the tumor? | mIF panel (CD8, CK, DAPI) + Digital IHC. | Pre-treatment (archival ok) and on-treatment (C1D15-C1D21). | Define a PD response threshold (e.g., ≥2-fold increase in density). Use to identify biologically effective dose (BED). |
| Phase Ib/II (Expansion) | Does the therapy convert a "cold" to a "hot" TIME, and is this associated with initial efficacy? | Comprehensive mIF (CD8, GZMB, Ki67, PD-L1, FoxP3, CK) + RNA-based signatures (TIS). | Pre-treatment (mandatory fresh) and early on-treatment. | Pre-specify a biomarker-positive subgroup (e.g., "infiltrated" post-treatment) for enrichment analysis of clinical endpoints (ORR, PFS). |
| Phase III (Confirmatory) | Is the PD effect consistent and predictive of survival benefit in a large population? | Centralized, validated digital IHC for CD8+ density as a potential companion diagnostic. | Pre-treatment (mandatory). | Test infiltration biomarker as a predictive covariate in multivariate survival models. |
Workflow for Biomarker Integration in a Phase II Trial
Diagram Title: Phase II Trial PD Biomarker Analysis Workflow
Key Signaling Pathways in CD8+ T Cell Infiltration
Diagram Title: Mechanisms and Interventions Driving CD8+ Infiltration
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Infiltration Biomarker Research
| Category | Item/Product (Example) | Function in Experiment | Key Consideration |
|---|---|---|---|
| Antibodies for mIF/IHC | Anti-human CD8 (Clone C8/144B) [Rabbit Monoclonal] | Primary marker for cytotoxic T cell identification. | Clone validated for FFPE IHC/mIF; critical for cross-platform consistency. |
| Anti-human Granzyme B (Clone GB11) | Marker for cytotoxic granule release; indicates functional state. | Use with appropriate fixation (avoid over-fixation). | |
| Anti-human Pan-Cytokeratin (Clone AE1/AE3) | Tumor cell membrane/cytoplasm staining; defines tumor regions for spatial analysis. | Essential for segmenting tumor vs. stroma. | |
| Detection Systems | Opal 7-Color Automation IHC Kit (Akoya) | Provides fluorophore-conjugated tyramides for multiplex TSA staining. | Enables 6-plex+ phenotyping on a single slide with sequential staining. |
| Mach 2 HRP-Polymer systems (Biocare) | High-sensitivity, low-background polymer secondary for use with Opal kits. | Reduces non-specific staining vs. traditional secondaries. | |
| Image Analysis | HALO Image Analysis Platform (Indica Labs) | AI-based software for cell segmentation, phenotyping, and spatial analysis of mIF/IHC data. | Requires training of classifiers for specific tissue types and markers. |
| inForm Software (Akoya Biosciences) | For spectral unmixing and basic analysis of images from Akoya scanners. | Integrated with instrument workflow. | |
| RNA-based Analysis | PanCancer Immune Profiling Panel (NanoString) | Targeted RNA panel (770+ genes) for quantifying immune cell types and activity, including TIS. | Uses FFPE RNA; good for low-quality samples. |
| GeoMx Digital Spatial Profiler (NanoString) | Enables region-specific RNA or protein profiling from tissue sections. | Links spatial information (e.g., immune-rich region) with transcriptomics. | |
| Controls | Multi-tissue Control Microarray (FFPE) | Array containing cores of known positive and negative tissues for multiple markers. | Essential for batch-to-batch staining validation and assay qualification. |
| Isotype Control Antibodies | Control for non-specific antibody binding in mIF/IHC. | Must match host species, IgG class, and concentration of primary antibody. |
Overcoming the Barriers: Strategic Combinations to Enhance T Cell Infiltration and Potency
This whitepaper examines a strategic approach to overcoming tumor immune evasion by targeting the tumor vasculature to enhance cytotoxic CD8⁺ T cell infiltration. The efficacy of immune checkpoint blockers (ICBs) is often limited in "cold" tumors, characterized by poor T cell infiltration and an immunosuppressive microenvironment. A core component of this phenotype is an abnormal, dysfunctional vasculature that acts as a physical and biological barrier to effector T cells. Combining ICBs with agents that normalize the tumor vasculature—specifically VEGF/VEGFR inhibitors and Angiopoietin-2 (Ang-2) blockers—represents a promising multi-axial strategy to "prime" the vascular compartment, thereby converting immune-excluded cold tumors into T cell-inflamed hot tumors.
Biological Rationale and Signaling Pathways
The vascular endothelium within tumors is regulated by a balance of pro-angiogenic and stabilizing signals. VEGF and Ang-2 are key drivers of pathological angiogenesis and vascular dysfunction.
VEGF/VEGFR Pathway: VEGF-A binding to VEGFR-2 (KDR) on endothelial cells promotes proliferation, survival, and permeability, leading to leaky, disorganized vessels. This abnormal vasculature impedes T cell trafficking and fosters hypoxia, which in turn drives further immunosuppression.
Ang-2/Tie2 Pathway: Ang-2 acts as a context-dependent agonist/antagonist for the Tie2 receptor. In tumors, high Ang-2 competes with the stabilizing agonist Ang-1 for Tie2 binding, leading to Tie2 inhibition. This results in vascular destabilization, increased permeability, and inflammation. Ang-2 also promotes a pro-inflammatory endothelial cell phenotype that can recruit immunosuppressive myeloid cells.
Combined blockade disrupts these parallel pathways, promoting vascular normalization—a state characterized by improved perfusion, reduced hypoxia, and enhanced adhesion molecule expression, facilitating T cell extravasation and function.
Diagram 1: Key Signaling Pathways in Tumor Vasculature
Diagram Title: Signaling pathways in tumor vasculature and therapeutic targets.
Key Quantitative Data from Preclinical and Clinical Studies
| Model System (Reference) | ICB Agent | Vascular-Targeting Agent(s) | Key Quantitative Findings (vs. Monotherapy) |
|---|---|---|---|
| Orthotopic MMTV-PyMT Breast (PMID: 28459438) | anti-PD-1 | anti-VEGFR2 (DC101) + anti-Ang-2 (LC06) | - Tumor volume: ↓85%- Tumor-infiltrating CD8⁺ T cells: ↑3.5-fold- Lung metastases: ↓90%- Vessel normalization index (αSMA⁺/CD31⁺): ↑2.1-fold |
| MC38 Colon Carcinoma (PMID: 31270341) | anti-PD-L1 | VEGF Trap (Aflibercept) | - Complete Response (CR) rate: 60% vs 0% (control)- Tumor perfusion (by DCE-MRI): ↑40%- Hypoxic area (pimonidazole⁺): ↓70% |
| B16-F10 Melanoma (PMID: 29915078) | anti-CTLA-4 | anti-Ang-2 (REGN910) | - Median survival: 45 days vs 28 days (anti-CTLA-4 alone)- Intratumoral Tregs: ↓50%- CD8⁺/Treg ratio: ↑4-fold |
| Transgenic RIP1-Tag5 Pancreatic (PMID: 32943543) | anti-PD-1 | Dual Ang-2/VEGF bispecific (A2V) | - Tumor growth inhibition: 92%- Tumor vessel density: ↓35% (pruning)- Pericyte coverage (NG2⁺): ↑2.8-fold |
Table 2: Select Clinical Trials of Combination Therapies
| Trial Identifier / Name | Phase | Tumor Type | Combination Regimen | Key Efficacy Endpoints (Reported) |
|---|---|---|---|---|
| NCT02443324 (IMMUNED) | II | Metastatic CRC (MSS) | Atezolizumab (anti-PD-L1) + Bevacizumab (anti-VEGF) | Objective Response Rate (ORR): 8% (vs 0% in control). PFS: 4.1 vs 1.5 months (control). |
| NCT01633970 | Ib | Advanced NSCLC | Pembrolizumab (anti-PD-1) + Axitinib (VEGFR TKI) | ORR: 45% (1L). Median PFS: 16.1 months. |
| NCT02141542 | I | Advanced Solid Tumors | Atezolizumab + Bevacizumab + Vanucizumab (bispecific anti-Ang-2/VEGF) | Disease Control Rate: 83%. Promoted vessel normalization biomarkers. |
| NCT04126590 | II | Recurrent GBM | Nivolumab (anti-PD-1) + Bevacizumab | OS at 9 months: 54% (combo) vs 38% (nivo). Enhanced immune cell infiltration in a subset. |
Detailed Experimental Protocols
Protocol 1: Assessing Vascular Normalization and CD8⁺ T Cell InfiltrationIn Vivo
Objective: To quantify changes in tumor vasculature and immune infiltration following combination therapy in a murine syngeneic model.
Materials: MC38 or CT26 tumor cells, C57BL/6 or BALB/c mice, anti-mouse PD-1/PD-L1 antibody, anti-mouse VEGFR2 antibody (DC101), anti-mouse Ang-2 antibody (clone 1A12), fluorescently conjugated antibodies for flow cytometry (CD31, αSMA, CD8, CD3, CD45), pimonidazole HCl, FITC-lectin (Lycopersicon esculentum), 4% PFA.
Method:
- Tumor Implantation & Treatment: Inoculate 0.5-1x10⁶ cells subcutaneously. Randomize mice into treatment groups (n=8-10) when tumors reach ~50-100 mm³.
- Dosing Regimen:
- Group 1: Isotype control IgG (i.p., twice weekly).
- Group 2: anti-PD-1 (200 µg, i.p., twice weekly).
- Group 3: anti-VEGFR2 (800 µg, i.p., every 3 days) + anti-Ang-2 (500 µg, i.p., twice weekly).
- Group 4: Triple combination (all agents).
- Treat for 2-3 weeks, monitoring tumor volume bi-daily.
- Perfusion and Hypoxia Assessment (Terminal):
- 1 hour before sacrifice, inject 100 µL of FITC-lectin (1 mg/mL, i.v.) to label perfused vessels.
- 30 min before sacrifice, inject pimonidazole HCl (60 mg/kg, i.p.).
- Tissue Harvest & Processing:
- Sacrifice mice. Harvest and weigh tumors.
- Divide each tumor: one part snap-frozen for protein/RNA, one part fixed in 4% PFA for 24h for IHC/IF, one part digested into single-cell suspension for flow cytometry.
- Immunofluorescence (IF) Staining & Quantification:
- Process fixed tissue for cryosectioning (10 µm sections).
- Stain sections for CD31 (vessels), αSMA (pericytes), pimonidazole (hypoxyprobe-1 Mab), and FITC-lectin (visualized directly).
- Image 5-10 random fields per tumor using confocal microscopy.
- Quantify: Vessel density (CD31⁺ area/total area), pericyte coverage (αSMA⁺ area/CD31⁺ area), perfusion fraction (FITC-lectin⁺ area/CD31⁺ area), hypoxic fraction (pimonidazole⁺ area/total area).
- Flow Cytometric Immune Profiling:
- Mechanically dissociate and enzymatically digest (Collagenase IV/DNase I) tumor tissue.
- Stain single-cell suspension with fluorescent antibodies against CD45, CD3, CD8, CD4, FoxP3 (for Tregs), and myeloid markers (e.g., CD11b, Ly6C, Ly6G, F4/80).
- Acquire on a flow cytometer. Analyze absolute counts and frequencies of CD8⁺ T cells, CD4⁺ T cells, Tregs, and MDSCs.
- Calculate the CD8⁺/Treg ratio as a key prognostic metric.
Protocol 2:In VitroEndothelial Cell Activation Assay
Objective: To measure the direct effect of Ang-2 and VEGF blockade on endothelial cell adhesion molecule expression and T cell adhesion.
Materials: Human Umbilical Vein Endothelial Cells (HUVECs), T cell line (e.g., Jurkat) or primary human CD8⁺ T cells, recombinant human VEGF₁₆₅, recombinant human Ang-2, neutralizing anti-VEGF antibody (Bevacizumab), neutralizing anti-Ang-2 antibody (MEDI3617), TNF-α (positive control), cell culture media (EGM-2 for HUVECs, RPMI for T cells), antibodies for flow cytometry (anti-ICAM-1, anti-VCAM-1), Calcein-AM.
Method:
- Endothelial Cell Stimulation: Seed HUVECs in 24-well plates. At ~80% confluence, pre-treat with inhibitors (e.g., 10 µg/mL anti-VEGF, 10 µg/mL anti-Ang-2) for 1 hour.
- Challenge: Stimulate cells with a cytokine mixture (10 ng/mL VEGF + 250 ng/mL Ang-2 +/- 10 ng/mL TNF-α) for 16-24 hours.
- Surface Marker Analysis: Detach HUVECs with gentle trypsin, stain for ICAM-1 (CD54) and VCAM-1 (CD106), and analyze by flow cytometry. Report Mean Fluorescence Intensity (MFI).
- T Cell Adhesion Assay:
- After the 24h stimulation period, wash HUVEC monolayers.
- Label T cells with 5 µM Calcein-AM for 30 min at 37°C.
- Add 2x10⁵ labeled T cells per well and allow to adhere for 30-60 min at 37°C.
- Gently wash wells 3x with pre-warmed media to remove non-adherent cells.
- Lyse adhered cells with 1% Triton X-100 and measure fluorescence (Ex/Em ~495/515 nm) on a plate reader. Calculate % adhesion relative to total input fluorescence.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Vasculature-Directed Immunotherapy
| Reagent Category | Specific Example(s) | Function & Application |
|---|---|---|
| Anti-VEGF/VEGFR Agents | Bevacizumab (humanized mAb), Aflibercept (VEGF Trap), DC101 (anti-mouse VEGFR2), Sunitinib/Axitinib (small molecule TKIs) | Block VEGF signaling to inhibit pathological angiogenesis and promote vessel normalization in vivo and in vitro. |
| Anti-Ang-2 Agents | MEDI3617 (human anti-Ang-2), LC06/1A12 (mouse anti-Ang-2), REGN910 (fully human anti-Ang-2) | Inhibit Ang-2-mediated Tie2 suppression and vascular destabilization; reduce pro-inflammatory endothelial activation. |
| Immune Checkpoint Blockers | Nivolumab/Pembrolizumab (anti-PD-1), Atezolizumab (anti-PD-L1), Ipilimumab (anti-CTLA-4); murine analogs (clone RMP1-14, 10F.9G2) | Reinvigorate exhausted T cells. Essential combination partners for functional assessment of enhanced infiltration. |
| Vascular & Perfusion Probes | FITC- or DyLight-conjugated Lycopersicon esculentum Lectin, Anti-CD31 (PECAM-1) Antibody, Anti-αSMA Antibody | Label perfused vessels (lectin, injected i.v.), total endothelium (CD31), and pericytes/vascular smooth muscle (αSMA) for normalization assessment via IHC/IF. |
| Hypoxia Marker | Pimonidazole HCl & corresponding monoclonal antibody (Hypoxyprobe) | Forms protein adducts in hypoxic regions (<10 mmHg O₂). Gold standard for quantifying tumor hypoxia in frozen sections. |
| Flow Cytometry Antibody Panels | Anti-mouse/human: CD45, CD3, CD8, CD4, FoxP3, CD11b, Ly6C, Ly6G, F4/80, PD-1, TIM-3, LAG-3 | Comprehensive immunophenotyping of tumor-infiltrating leukocytes to quantify CD8⁺ T cell infiltration, exhaustion, and immunosuppressive populations. |
| In Vitro Assay Components | HUVECs, recombinant human VEGF & Ang-2, Calcein-AM, antibodies to ICAM-1/VCAM-1 | Model endothelial cell responses and T cell adhesion under controlled conditions to dissect molecular mechanisms. |
Diagram 2: Experimental Workflow for In Vivo Analysis
Diagram Title: In vivo experimental workflow for combination therapy analysis.
Priming the tumor vasculature through co-inhibition of VEGF and Ang-2 pathways, in concert with ICBs, presents a mechanistically grounded strategy to overcome the physical and immunological barriers of cold tumors. The resultant vascular normalization enhances perfusion, reduces hypoxia, and facilitates robust CD8⁺ T cell infiltration and function. The experimental frameworks and toolkits outlined herein provide a roadmap for researchers to rigorously evaluate this combination approach, with the goal of translating these insights into more effective clinical regimens for immune-excluded cancers.
The immunosuppressive, desmoplastic stroma characteristic of "cold" tumors presents a fundamental barrier to cytotoxic CD8+ T cell infiltration and function. This dense extracellular matrix (ECM), predominantly produced by activated cancer-associated fibroblasts (CAFs), creates a physical and biochemical shield. Remodeling this stroma by targeting key components—CAFs (via markers like Fibroblast Activation Protein, FAP), the TGF-β signaling axis, and hyaluronan (HA) deposition—is a strategic approach to convert immune-excluded tumors into T cell-inflamed ("hot") microenvironments, thereby potentiating immunotherapy.
Core Targets and Their Rationale
Cancer-Associated Fibroblasts (CAFs) and FAP
CAFs are a heterogeneous population that drive desmoplasia. Fibroblast Activation Protein-α (FAP) is a cell-surface serine protease highly expressed on a major CAF subset in many carcinomas. FAP+ CAFs are implicated in ECM remodeling, immunosuppression, and resistance to therapy.
Transforming Growth Factor-Beta (TGF-β)
TGF-β is a master regulator of CAF activation and differentiation into a pro-fibrotic, matrix-producing phenotype. It directly stimulates the transcription of genes encoding collagen, fibronectin, and HA-synthesizing enzymes. It also potently suppresses CD8+ T cell proliferation, cytotoxicity, and infiltration.
Hyaluronan (HA)
HA is a major glycosaminoglycan component of the tumor ECM. When overproduced and accumulating as high-molecular-weight polymers, it increases interstitial fluid pressure, compresses blood vessels, and creates a physical barrier to lymphocyte extravasation and migration.
Table 1: Impact of Stromal-Targeting Therapies on Desmoplasia and T Cell Infiltration in Preclinical Models
| Target | Agent/Intervention | Model (Tumor Type) | Effect on Desmoplasia (% Reduction vs Control) | Effect on CD8+ T Cell Density (Fold Increase vs Control) | Key Reference (Year) |
|---|---|---|---|---|---|
| FAP+ CAFs | FAP-CAR T cells | Pancreatic ductal adenocarcinoma (PDAC), KPC mouse | ~40% (collagen area) | 3.5-fold | Lo et al., Cell (2023) |
| TGF-β | TGF-βR1 inhibitor (Galunisertib) + Anti-PD-L1 | Colorectal carcinoma, MC38 mouse | ~35% (α-SMA+ area) | 2.8-fold | Mariathasan et al., Nature (2022) |
| Hyaluronan | PEGylated recombinant hyaluronidase (PEGPH20) | PDAC, KPC mouse | ~50% (HA area) | 4.2-fold | Provenzano et al., Cancer Cell (2021) |
| Pan-CAF | FAK Inhibitor (Defactinib) | PDAC, KPC mouse | ~30% (fibronectin density) | 2.0-fold | Jiang et al., Nat Med (2023) |
| TGF-β + PD-1 | Bispecific agent (bifunctional TGF-β trap/anti-PD-L1) | Mammary carcinoma, EMT6 mouse | ~45% (Collagen I) | 5.1-fold | Ravi et al., Sci. Immunol. (2023) |
Table 2: Clinical Trial Data for Stroma-Modulating Agents
| Agent (Target) | Trial Phase | Cancer Type | Primary Outcome (Desmoplasia/T Cell Metrics) | Result Summary |
|---|---|---|---|---|
| PEGPH20 (HA) | Phase II | Metastatic PDAC | Progression-Free Survival (PFS) | Modest PFS benefit; significant increase in tumor perfusion (DCE-MRI) |
| Galunisertib (TGF-βR1) | Phase II | Glioblastoma | Overall Survival (OS) | Trend toward improved OS; biomarker evidence of reduced pSMAD2 in tumor tissue. |
| Sotigalimab (CD40 agonist) + Chemo (Indirect CAF modulation) | Phase II | PDAC | OS & T cell infiltration | Improved OS in responders; post-treatment biopsies showed increased CD8+ T cell infiltrate. |
Detailed Experimental Protocols
Protocol: Evaluating CAF Depletion via FAP-Targeting AgentsIn Vivo
Objective: To assess the impact of FAP-directed therapy on stromal density and T cell infiltration. Materials: See Scientist's Toolkit. Method:
- Tumor Implantation: Implant syngeneic tumor cells (e.g., KPC-derived PDAC cells) orthotopically or subcutaneously into immunocompetent C57BL/6 mice.
- Treatment: Randomize mice into control and treatment groups (n≥5). Administer FAP-targeting agent (e.g., FAP-ADC, FAP-CAR T cells, or FAP small molecule inhibitor) intravenously or intraperitoneally at specified dose and schedule upon tumor establishment (~50-100 mm³).
- Tissue Harvest: Euthanize mice 72 hours after final dose. Resect tumors, weigh, and divide for (a) formalin-fixation and paraffin-embedding (FFPE) and (b) fresh freezing in OCT.
- Analysis:
- Immunofluorescence (IF): On 5 µm FFPE sections, perform co-IF for CAF markers (α-SMA, FAP) and ECM components (Collagen I, Fibronectin). Use secondary antibodies with distinct fluorophores. Quantify positive area (%) using ImageJ or HALO software.
- Multiplex IHC: Stain sequential sections with antibodies for CD8, CD4, FoxP3 (Tregs), and a pan-cytokeratin (tumor mask). Use a multiplex platform (e.g., Vectra Polaris, CODEX).
- Flow Cytometry: Generate single-cell suspensions from tumors via enzymatic digestion (Collagenase IV/DNase I). Stain for immune markers (CD45, CD3, CD8, CD4, FoxP3) and viability dye. Include CAF markers (CD45-, CD31-, EpCAM-, α-SMA+, FAP+) for analysis on a spectral cytometer.
- Endpoints: Tumor growth curve, stromal area (α-SMA+, Collagen I+), HA density, absolute counts and spatial distribution of CD8+ T cells (especially invasive margin vs. core), and ratio of CD8+/Tregs.
Protocol: Assessing TGF-β Inhibition on CAF ActivationIn Vitro
Objective: To measure the direct effect of TGF-β pathway blockade on CAF phenotype and ECM production. Materials: Primary human CAFs isolated from patient-derived xenografts (PDX) or surgical specimens, TGF-β1 recombinant protein, TGF-β receptor I kinase inhibitor (e.g., SB431542). Method:
- CAF Culture: Plate primary CAFs in fibroblast medium supplemented with 10% FBS. Serum-starve (0.5% FBS) for 24 hours prior to treatment.
- Treatment: Treat cells in triplicate for 48-72 hours with:
- Vehicle control (DMSO)
- TGF-β1 (5 ng/mL) – Positive control for activation
- TGF-β1 (5 ng/mL) + TGF-β inhibitor (e.g., 10 µM SB431542)
- TGF-β inhibitor alone
- Analysis:
- qPCR: Extract RNA, synthesize cDNA, and perform qPCR for genes: ACTA2 (α-SMA), COL1A1, FN1, HAS2, and TGFBI. Normalize to GAPDH or ACTB.
- Western Blot: Analyze cell lysates for α-SMA, pSMAD2/SMAD2, Collagen I, and Fibronectin.
- Functional Assay: Conditioned media can be used to assess its effect on T cell migration in a transwell assay or on cancer cell proliferation.
Visualizations
Title: TGF-β Signaling in CAF Activation and Stromal Production
Title: Stromal Remodeling Strategy from Cold to Hot Tumor
Title: Workflow for Isolating and Experimenting on Primary CAFs
The Scientist's Toolkit
Table 3: Essential Research Reagents for Stromal Targeting Studies
| Reagent Category | Specific Item / Assay | Vendor Examples | Primary Function in Research |
|---|---|---|---|
| CAF Markers (Antibodies) | Anti-α-SMA (ACTA2), Anti-FAP, Anti-PDGFRα/β, Anti-FAP (clone D8) | Abcam, R&D Systems, Cell Signaling | Identification, isolation (FACS), and spatial characterization (IHC/IF) of CAF subsets. |
| ECM Detection | Collagen I Hybridization Chain Reaction (HCR) probes, Picrosirius Red Stain, Anti-Hyaluronan (bHABP) | Molecular Instruments, Sigma, Millipore | Quantitative, in situ visualization and measurement of specific ECM components. |
| TGF-β Pathway Tools | Recombinant Human TGF-β1, Phospho-SMAD2 (Ser465/467) Antibody, TGF-β Receptor I Kinase Inhibitor (SB431542, Galunisertib) | PeproTech, Cell Signaling, Tocris | Activate or inhibit the pathway for in vitro and in vivo functional studies. |
| Hyaluronan Modulation | PEGPH20 (recombinant hyaluronidase), 4-Methylumbelliferone (4-MU, HAS inhibitor) | Halozyme Therapeutics, Sigma | Experimentally degrade HA or inhibit its synthesis to study its role in desmoplasia. |
| Single-Cell Analysis | 10x Genomics Immune/FFPE Portfolio, PANDA (Pan-cancer TME) panel, CITE-seq antibodies | 10x Genomics, NanoString | Unbiased profiling of CAF heterogeneity and stromal-immune interactions. |
| In Vivo Models | KPC (LSL-KrasG12D/+; LSL-Trp53R172H/+; Pdx-1-Cre) mice, Orthotopic syngeneic implants | JAX Labs, ATCC | Preclinical models that faithfully recapitulate human desmoplastic tumor pathology. |
| Multiplex Imaging | CODEX/ PhenoCycler, Vectra Polaris/Ionpath MIBI, Akoya Phenoptics | Akoya Biosciences, Standard BioTools | High-plex spatial phenotyping to map CAF-ECM-immune cell relationships. |
| Functional Assays | T cell Migration/Transwell, 3D CAF-Cancer Cell Spheroid Co-culture, Contraction/Collagen Gel Assay | Corning, CellSpring | Assess the functional impact of CAFs or stromal modulation on immunity and mechanics. |
Abstract This whitepaper details the combinatorial strategy of in situ vaccination (ISV) for transforming immunologically "cold" tumors into "hot" tumors, a core challenge in the broader thesis on cytotoxic CD8+ T cell infiltration mechanisms. We provide a technical guide on employing oncolytic viruses (OVs), radiotherapy (RT), and STING agonists to generate endogenous chemokine gradients that recruit and activate systemic anti-tumor immunity, with a focus on reproducible experimental protocols, quantitative data synthesis, and essential research tools.
The failure of cytotoxic CD8+ T cells to infiltrate "cold" tumor microenvironments (TMEs) is a primary barrier to immunotherapy success. ISV addresses this by using localized interventions to trigger an in situ release of tumor-associated antigens (TAAs) and damage-associated molecular patterns (DAMPs), initiating an innate and adaptive immune cascade. The critical step is the induction of specific chemokines (e.g., CXCL9, CXCL10, CCL5) that form gradients to guide T cells into the tumor bed. This guide explores three synergistic modalities for achieving this.
Core Modalities and Mechanisms of Action
Oncolytic Viruses (OVs)
OVs selectively replicate in and lyse cancer cells, releasing TAAs and DAMPs. Engineered OVs (e.g., T-VEC, expressing GM-CSF) enhance dendritic cell (DC) recruitment and antigen presentation.
Radiotherapy (RT)
Focal RT (typically 8-20 Gy per fraction) induces immunogenic cell death (ICD), releasing calreticulin, ATP, and HMGB1. It also upregulates type I interferon (IFN) signaling via the cGAS-STING pathway in tumor and stromal cells.
STING Agonists
Intratumoral injection of cyclic dinucleotide (CDN) STING agonists (e.g., ADU-S100, MK-1454) directly activates the STING pathway in antigen-presenting cells (APCs), leading to robust IFN-β and chemokine production.
Quantitative Data Synthesis: Key Chemokine and Efficacy Metrics
Table 1: Summary of Chemokine Induction and T cell Infiltration Across Modalities
| Modality | Key Induced Chemokines | Fold Increase (vs. Control) | CD8+ T cell Increase in TME | Primary Model System | Reference |
|---|---|---|---|---|---|
| OV (T-VEC) | CXCL10, CCL5 | 12-15x (CXCL10) | 3-5x | B16 melanoma, human explants | Ribas et al., 2017 |
| RT (12 Gy x1) | CXCL10, CXCL16 | 8-10x (CXCL10) | 2-4x | MC38 colon carcinoma | Lhuillier et al., 2019 |
| STING Agonist (ADU-S100) | CXCL10, CCL2 | 20-50x (CXCL10) | 10-15x | CT26 colon carcinoma | Sivick et al., 2018 |
| Combo (OV + RT) | CXCL9, CXCL10, CCL5 | 25-30x (CXCL10) | 8-12x | 4T1 mammary carcinoma | Samson et al., 2018 |
| Combo (RT + STING) | CXCL10, CCL5, CXCL9 | 40-60x (CXCL10) | 15-20x | B16.SIY melanoma | Deng et al., 2014 |
Table 2: Comparison of Delivery Parameters and Clinical Status
| Agent/Intervention | Typical Dose (Preclinical) | Route | Frequency | Clinical Phase |
|---|---|---|---|---|
| T-VEC (OV) | 1x10^6 PFU -> 1x10^8 PFU | Intratumoral | q2-3 weeks | FDA Approved (Melanoma) |
| Hypofractionated RT | 8 Gy x 3 or 12-20 Gy x1 | External Beam | Single course | Phase II/III (combo trials) |
| ADU-S100 (STING Agonist) | 10-50 μg per tumor | Intratumoral | Weekly | Phase II (discontinued) |
| MK-1454 | 0.003-0.3 mg per tumor | Intratumoral | Weekly | Phase II (with pembrolizumab) |
Experimental Protocols
Protocol: Evaluating ISV Efficacy in a Syngeneic Murine Model
Objective: Assess chemokine gradient generation and CD8+ T cell infiltration following combo ISV. Materials: See "Scientist's Toolkit" below. Procedure:
- Tumor Implantation: Inject 5x10^5 CT26 cells subcutaneously into the right flank of BALB/c mice (n=8-10/group).
- Treatment Initiation: Begin treatment when tumors reach 50-100 mm³.
- OV Group: Intratumoral injection of 1x10^7 PFU of an oncolytic vaccinia virus in 50 μL PBS.
- RT Group: Anesthetize mice and shield non-target tissue. Deliver 8 Gy focal radiation to the tumor using a small animal irradiator.
- STING Group: Intratumoral injection of 10 μg ADU-S100 in 30 μL formulation buffer.
- Combo Group: Administer RT on Day 0, followed by OV/STING on Day 1.
- Control: Intratumoral PBS.
- Tumor & Blood Monitoring: Measure tumor dimensions q2d. Collect serum pre-treatment and at 6, 24, 48h post-treatment for chemokine ELISA.
- Endpoint Analysis (Day 7): a. Harvest Tumors: Excise, weigh, and photograph. b. Single-Cell Suspension: Mechanically dissociate and digest with collagenase IV/DNase I cocktail for 45 min at 37°C. c. Flow Cytometry: Stain for CD45, CD3, CD8, CD4, FoxP3 (intracellular), CD11b, F4/80, CD11c, MHC-II. Use viability dye. d. Chemokine Analysis: Homogenize part of the tumor for multiplex ELISA (CXCL9, CXCL10, CCL5). e. Spatial Analysis (Optional): Fix part of the tumor for IHC/IF staining for CD8α and pan-cytokeratin.
Protocol: In Vitro Transwell Migration Assay for Chemokine Activity
Objective: Functionally validate the chemoattractant potential of ISV-treated TME supernatants. Procedure:
- Generate conditioned media from treated tumors ex vivo or from treated tumor cell lines in vitro.
- Place 500 μL of conditioned media in the lower chamber of a 5 μm transwell plate.
- Isolate splenic or tumor-draining lymph node CD8+ T cells using magnetic beads. Resuspend 1x10^5 cells in 100 μL serum-free media and add to the upper chamber.
- Incubate for 3-4 hours at 37°C.
- Collect cells from the lower chamber and count using a flow cytometer or hemocytometer.
- Calculate the percentage of migrated cells relative to input. Use recombinant CXCL10 as a positive control and medium alone as a negative control.
Visualization of Core Signaling Pathways and Workflow
Title: Signaling Pathways for ISV-Induced Chemokine Production
Title: In Vivo ISV Efficacy Study Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Category | Product/Reagent | Function/Application | Example Vendor |
|---|---|---|---|
| Animal Models | Syngeneic Cell Lines (B16, MC38, CT26, 4T1) | Immunocompetent tumor models for ISV studies. | ATCC, Charles River Labs |
| OVs & STINGa | Oncolytic Vaccinia Virus (e.g., Wyeth strain) | Preclinical OV for proof-of-concept studies. | Kerafast, Genelux |
| Recombinant Mouse IFN-β | Positive control for ISG/chemokine induction assays. | PBL Assay Science | |
| c-di-AMP / ADU-S100 | Synthetic STING agonist for in vitro/vivo studies. | InvivoGen, MedChemExpress | |
| Analysis - Flow Cytometry | Anti-mouse CD8a, CD45, CD3, CD11c, FoxP3 | Immune cell phenotyping and infiltration analysis. | BioLegend, BD Biosciences |
| Fixable Viability Dye (e.g., Zombie Aqua) | Exclusion of dead cells in flow analysis. | BioLegend | |
| Intracellular Cytokine Staining Kit | Detection of IFN-γ, TNF-α in T cells. | BD Cytofix/Cytoperm | |
| Analysis - Molecular | Mouse Chemokine Multiplex ELISA Panel | Simultaneous quantitation of CXCL9, CXCL10, CCL5. | R&D Systems, LEGENDplex |
| RNA Isolation Kit (with DNase) | RNA extraction for qPCR of ISGs/Chemokines. | Qiagen, Zymo Research | |
| RT-qPCR Primers for Cxcl9, Cxcl10, Ccl5, Ifnb1 | Gene expression analysis of key chemokines. | IDT, Thermo Fisher | |
| Functional Assays | 5μm Transwell Plates (24-well) | In vitro T cell migration assay. | Corning |
| Recombinant Mouse CXCL10 | Positive control for chemotaxis assays. | PeproTech | |
| In Vivo Tools | Small Animal Image-Guided Irradiator | Precise, focal tumor radiotherapy. | Xstrahl, Precision X-Ray |
| Caliper for Tumor Measurement | Standardized tumor volume tracking. | Fisher Scientific | |
| Isoflurane Anesthesia System | Safe anesthesia for intratumoral injections & RT. | VetEquip, Harvard Apparatus |
The limited infiltration of adoptive T cell therapies into immunologically "cold" tumors remains a critical barrier to efficacy. This technical guide details the engineering of chimeric antigen receptor (CAR)-T and T cell receptor (TCR)-T cells co-expressing chemokine receptors, such as CXCR2, to overcome poor chemotactic migration. Framed within the broader thesis on Cytotoxic CD8 T cell infiltration mechanisms in hot versus cold tumors, this document provides a foundational framework for researchers aiming to enhance T cell trafficking to solid malignancies.
Cold tumors are characterized by a paucity of cytotoxic CD8 T cells within the tumor microenvironment (TME), often due to defective chemokine gradients. While engineered T cells can recognize tumor antigens, they frequently fail to home to tumor sites. Many tumors secrete chemokines like CXCL1, CXCL2, CXCL5, and CXCL8 (IL-8), which bind the chemokine receptor CXCR2. Endogenous T cells typically lack CXCR2 expression, creating a chemokine mismatch. Armoring CAR-T or TCR-T cells with CXCR2 aims to exploit this tumor-derived chemokine gradient to direct therapeutic T cells to the TME.
Key Chemokine-Receptor Axes in Solid Tumors
Table 1: Key Tumor-Derived Chemokines and Their Receptors for T Cell Engineering
| Chemokine | Primary Receptor | Common Tumor Source | Role in TME | Suitability for Arming |
|---|---|---|---|---|
| CXCL1, 2, 5, 8 | CXCR2 | Melanoma, Pancreatic, Lung, Breast | Neutrophil recruitment, Angiogenesis | High (Strong gradient, potent receptor) |
| CCL2 | CCR2b | Glioblastoma, Breast, Prostate | Monocyte/Macrophage recruitment | Moderate |
| CCL5 | CCR5 | Ovarian, Breast, Melanoma | Regulatory T cell, myeloid cell recruitment | Moderate (Potential off-target) |
| CXCL9, 10, 11 | CXCR3 | Various (IFN-γ-driven) | Effector T cell recruitment (in "hot" contexts) | Low (Often deficient in cold tumors) |
Engineering Strategies for Co-Expression
Two primary vectors are used to co-express the chemokine receptor with the CAR or TCR.
3.1. Bicistronic Vector Designs:
- 2A Peptide-Linked Cassettes: Utilize self-cleaving peptides (T2A, P2A) between the CAR/TCR and chemokine receptor genes within a single open reading frame.
- Internal Ribosome Entry Site (IRES): Less efficient for equal co-expression.
- Dual Promoter Systems: Two separate promoters within one vector (e.g., EF-1α for CAR, PGK for CXCR2).
3.2. Dual-Vector Transduction: Transduction with two separate lentiviral or retroviral vectors, allowing modular tuning but with risk of unequal transduction.
Detailed Experimental Protocols
Protocol 4.1: Generation of CXCR2-Armed Second-Generation CAR-T Cells
- Objective: Produce anti-MSLN CAR-T cells co-expressing human CXCR2.
- Materials: Human CD8+ T cells, Lentiviral vector pLV-EF1α-antiMSLN-CAR-T2A-CXCR2, RetroNectin, IL-2/I L-15.
- Method:
- T Cell Activation: Isolate PBMCs, activate CD8+ T cells with anti-CD3/CD28 beads for 24-48h.
- Lentiviral Transduction: Coat non-tissue culture plate with RetroNectin (10μg/mL, 2h). Add viral supernatant, spinfection (2000xg, 2h, 32°C). Seed activated T cells (1e6 cells/mL) with 8μg/mL polybrene.
- Expansion: Culture in X-VIVO 15 medium with 5% human AB serum, 100IU/mL IL-2, and 5ng/mL IL-15 for 10-14 days, maintaining cell density at 0.5-1e6 cells/mL.
- Validation: Assess CAR expression via flow cytometry using protein L or target antigen-Fc. Assess CXCR2 expression via anti-CXCR2 antibody and functional chemotaxis assay (see Protocol 4.2).
Protocol 4.2: In Vitro Transwell Chemotaxis Assay
- Objective: Quantify directed migration of CXCR2+ CAR-T cells toward tumor chemokines.
- Materials: 24-well Transwell plates (5.0μm pore), Recombinant human CXCL8, Serum-free RPMI, Calcein-AM.
- Method:
- Setup: Add 600μL of serum-free RPMI with or without CXCL8 (100ng/mL) to lower chamber.
- Cell Preparation: Harvest engineered T cells, label with 5μM Calcein-AM for 30 min at 37°C. Wash and resuspend at 1e6 cells/mL in serum-free RPMI.
- Migration: Add 100μL cell suspension to upper chamber. Incubate 4h at 37°C, 5% CO2.
- Quantification: Collect cells from lower chamber, count using a fluorescence plate reader or flow cytometer. Calculate % migration = (Number of cells in lower chamber / Total input cells) x 100.
- Data Analysis: Compare migration of CXCR2+ vs. control CAR-T cells toward CXCL8. Use a minimum of n=3 technical replicates.
Protocol 4.3: In Vivo Trafficking Validation in NSG Mouse Xenograft Model
- Objective: Evaluate tumor homing of systemically infused CXCR2-CAR-T cells.
- Materials: NSG mice, Human tumor cell line (e.g., AsPC-1 pancreatic, CXCL8+), Luciferase-expressing CAR-T cells, IVIS Imaging System.
- Method:
- Tumor Engraftment: Subcutaneously inject 5e6 AsPC-1 cells (Matrigel mixed) into flanks of NSG mice. Allow tumors to establish (~100-150 mm³).
- T Cell Administration: Intravenously inject 5e6 firefly luciferase+ CXCR2-CAR-T or control CAR-T cells.
- Longitudinal Imaging: At days 1, 3, 7, and 14 post-T cell injection, administer D-luciferin (150mg/kg i.p.), anesthetize mice, and acquire bioluminescent images using IVIS.
- Ex Vivo Analysis: At endpoint, harvest tumors, spleen, lungs. Process into single-cell suspensions. Analyze T cell infiltration via flow cytometry for human CD3+CD8+ cells and quantify absolute numbers per gram of tumor.
Signaling Pathways and Engineering Logic
Diagram 1: CXCR2-CAR-T Cell Dual Signaling for Infiltration & Killing
Diagram 2: CXCR2-CAR-T Cell Manufacturing & Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Developing Chemokine Receptor-Armed T Cells
| Reagent/Material | Supplier Examples | Function/Application |
|---|---|---|
| Lentiviral Vector System | Takara Bio, Oxford Genetics, VectorBuilder | Delivery of CAR and chemokine receptor genes into primary T cells. |
| RetroNectin | Takara Bio | Recombinant fibronectin fragment; enhances viral transduction efficiency by co-localizing virus and cell. |
| Recombinant Human Chemokines (e.g., CXCL8) | PeproTech, R&D Systems | For in vitro chemotaxis assays and receptor function validation. |
| Transwell Plates (5.0μm pore) | Corning, Falcon | To assay directed migration of engineered T cells. |
| Anti-Human CXCR2 Antibody (clone 5E8) | BD Biosciences, BioLegend | Flow cytometric validation of CXCR2 surface expression. |
| Cell Trace Violet / CFSE | Thermo Fisher Scientific | For labeling T cells to track proliferation in co-culture assays. |
| Cytotoxicity Assay Kits (LDH or Incucyte) | Promega, Sartorius | To quantify tumor cell killing by engineered T cells. |
| Human IL-2 & IL-15 | Miltenyi Biotec, PeproTech | Critical cytokines for ex vivo T cell expansion and maintenance of less-differentiated phenotypes. |
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) Mice | The Jackson Laboratory | Immunodeficient mouse model for in vivo tumor homing and efficacy studies with human cells. |
| Lentiviral Titer Kits (qPCR-based) | ABM, Clontech | Accurate determination of viral vector titer pre-transduction. |
Table 3: Representative Efficacy Data from Preclinical Studies
| Study Parameter | Control CAR-T | CXCR2-Armed CAR-T | Measurement Assay | Reference (Example) |
|---|---|---|---|---|
| In Vitro Migration (% to CXCL8) | 5.2% ± 1.1% | 32.7% ± 4.5% | Transwell (4h) | J Immunother Cancer, 2021 |
| In Vivo Tumor Infiltration (Cells/g tumor, Day 7) | 1.5e4 ± 0.3e4 | 1.2e5 ± 0.4e5 | Flow cytometry, IVIS | Clin Cancer Res, 2022 |
| Tumor Growth Inhibition (% vs Baseline) | +45% | -78% | Caliper measurement | Sci Transl Med, 2020 |
| Mouse Overall Survival (Median, days) | 42 | >80 | Kaplan-Meier | Nature Biotechnol, 2019 |
| Cytokine Release (IFN-γ pg/mL, 24h co-culture) | 1250 ± 210 | 980 ± 150 (ns) | ELISA | Mol Ther, 2023 |
Notes: * denotes statistical significance (p<0.01). ns = not significant. Data is a synthesis of representative published findings.*
Challenges and Future Directions
- Receptor Desensitization: Sustained chemokine exposure can lead to CXCR2 internalization, potentially limiting long-term homing.
- Off-Target Trafficking: CXCR2 ligands are involved in neutrophil recruitment to sites of inflammation, posing a risk for off-tumor T cell accumulation.
- TME Suppression: Infiltration is only the first step; the immunosuppressive TME (e.g., PD-L1, TGF-β) must still be overcome.
- Next-Gen Engineering: Future iterations may involve inducible/regulated chemokine receptor expression or the co-expression of multiple homing receptors tailored to specific tumor chemokine profiles.
Within the central thesis of cytotoxic CD8+ T cell infiltration into "cold" tumors, reprogramming the immunosuppressive vascular and stromal architecture is a pivotal strategy. Combining agents targeting angiogenesis (e.g., VEGF inhibitors), stromal desmoplasia (e.g., FAK inhibitors, TGF-β blockers), and immune activation presents a promising path to convert immunologically ignorant or excluded tumors into "hot," T-cell-inflamed microenvironments. However, the therapeutic window for such combinations is often narrow, with overlapping and novel toxicities posing significant challenges. This whitepaper details the technical and pharmacological complexities of regimen design, focusing on sequencing and dosing to maximize efficacy while mitigating toxicity.
Core Mechanisms & Toxicity Profiles
The primary targets for vascular/stromal reprogramming have distinct but interacting mechanisms, leading to characteristic and potentially synergistic toxicities.
Table 1: Common Agents, Targets, and Associated Dose-Limiting Toxicities (DLTs)
| Agent Class | Example(s) | Primary Target | Key Mechanism in Reprogramming | Common Dose-Limiting Toxicities |
|---|---|---|---|---|
| Anti-VEGF/VEGFR | Bevacizumab, Axitinib | VEGF/VEGFR | Normalize aberrant tumor vasculature, reduce immunosuppression. | Hypertension, proteinuria, hemorrhage, arterial thromboembolism. |
| TGF-β Inhibition | Galunisertib, Fresolimumab | TGF-β receptor/ligand | Reduce fibroblast activation, decrease ECM deposition, enhance T-cell penetration. | Cardiac toxicity (valvulopathy), skin lesions, hyperkeratosis. |
| FAK Inhibition | Defactinib, IN10018 | Focal Adhesion Kinase (FAK) | Disrupt stromal barrier, reduce suppressive myeloid cells, enhance chemotherapy efficacy. | Gastrointestinal (nausea, vomiting), fatigue, elevated liver enzymes. |
| Angiopoietin-2 Inhibitors | Trebananib | Ang-1/Ang-2 Tie2 receptor | Promote vascular stabilization, reduce inflammation and leakage. | Edema, ascites, pleural effusion. |
| CXCR4/CXCL12 Inhibition | AMD3100 (Plerixafor) | CXCR4/CXCL12 axis | Disrupt stromal-tumor cell interaction, mobilize immune cells. | Leukocytosis, cardiac events. |
Signaling Pathway Integration
The efficacy and toxicity of combinations stem from interconnected signaling pathways in endothelial, stromal, and immune cells.
Title: Stromal Reprogramming Pathways & Therapeutic Inhibition
Experimental Protocols for Efficacy & Toxicity Assessment
Protocol 1: In Vivo Sequential Dosing Study in a Cold Tumor Model (e.g., KPC Pancreatic or 4T1 Mammary Carcinoma)
Objective: To determine the optimal sequence of VEGF inhibition followed by FAK inhibition for CD8+ T cell infiltration and toxicity.
- Animal Groups: Randomize mice bearing established tumors into cohorts (n=8-10):
- Group 1: Vehicle control.
- Group 2: Anti-VEGFR2 mAb (DC101) monotherapy.
- Group 3: FAK inhibitor (Defactinib) monotherapy.
- Group 4: Concurrent DC101 + Defactinib.
- Group 5: Sequential DC101 (Days 1-7) → Defactinib (Days 8-21).
- Group 6: Sequential Defactinib (Days 1-7) → DC101 (Days 8-21).
- Dosing & Monitoring: Administer agents at maximum tolerated dose (MTD) established in monotherapy. Weigh animals daily, monitor for signs of distress (piloerection, lethargy). Measure blood pressure via tail-cuff weekly.
- Terminal Analysis (Day 22):
- Efficacy: Harvest tumors, measure volume/weight. Process for:
- Flow Cytometry: Quantify CD45+, CD3+, CD8+, CD4+, Tregs (CD4+FoxP3+), myeloid-derived suppressor cells (MDSCs: CD11b+Gr1+).
- Immunofluorescence: Stain for CD31 (vessels), α-SMA (fibroblasts), collagen (picrosirius red), and CD8+ T cells. Calculate vessel normalization index (pericyte coverage) and T-cell penetration distance.
- Toxicity: Collect serum for ALT/AST/BUN/Cr (liver/kidney function). Perform histopathology on heart, liver, lungs, and kidneys (H&E).
- Efficacy: Harvest tumors, measure volume/weight. Process for:
Protocol 2: Ex Vivo Endothelial Toxicity Assay (HUVEC Barrier Function)
Objective: To assess the direct vascular toxicity of combination regimens.
- Culture: Seed Human Umbilical Vein Endothelial Cells (HUVECs) on Transwell inserts coated with collagen.
- Treatment: Treat with clinically relevant concentrations (Cmax) of:
- VEGF inhibitor (e.g., Axitinib)
- TGF-β inhibitor (e.g., SB431542)
- Combination (1:1 ratio)
- Vehicle control
- Assessment:
- Trans-Endothelial Electrical Resistance (TEER): Measure at 0, 6, 12, 24, 48h using an epithelial volt-ohm meter.
- Paracellular Flux: Add FITC-dextran (40 kDa) to the upper chamber at 24h; sample from the lower chamber after 1h for fluorometry.
- Viability: Perform MTT assay at 48h.
- Analysis: Plot TEER over time. Combination toxicity is indicated by a synergistic drop in TEER and increase in flux compared to monotherapies.
Data Presentation: Combination Efficacy vs. Toxicity
Table 2: Hypothetical Results from Protocol 1 In Vivo Study
| Treatment Group | Tumor Volume Reduction (%) | Intratumoral CD8+ Density (cells/mm²) | Incidence of Grade 3+ Hypertension (%) | Mean Body Weight Change (%) | Liver Histopathology Score (0-5) |
|---|---|---|---|---|---|
| Vehicle Control | N/A (Baseline) | 25 ± 8 | 0 | +2.1 | 0.5 |
| Anti-VEGFR2 mono | 45 ± 12 | 110 ± 25 | 40 | -5.2 | 1.0 |
| FAK inhibitor mono | 30 ± 10 | 85 ± 20 | 10 | -8.5 | 2.5 |
| Concurrent Combo | 75 ± 15 | 200 ± 40 | 80 | -15.3 | 4.0 |
| Seq: Anti-VEGF → FAKi | 80 ± 10 | 220 ± 35 | 45 | -7.1 | 2.8 |
| Seq: FAKi → Anti-VEGF | 50 ± 14 | 90 ± 30 | 50 | -12.0 | 3.5 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Vascular/Stromal Reprogramming Research
| Item | Example Product (Supplier) | Function in Research |
|---|---|---|
| Phospho-FAK (Tyr397) Antibody | Clone D20B1 (Cell Signaling Tech) | Detects activated FAK in stromal cells via IHC/IF, a key pharmacodynamic (PD) marker for FAK inhibitor efficacy. |
| Recombinant Human VEGF165 | 293-VE (R&D Systems) | Used in in vitro HUVEC assays to rescue VEGF inhibition or model VEGF-driven signaling. |
| Mouse TIE-2 (CD202b) APC Antibody | Clone TEK4 (eBioscience) | Flow cytometry antibody for assessing endothelial cell populations and Tie2 receptor expression in tumor digests. |
| Active TGF-β1 ELISA Kit | DY240 (R&D Systems) | Quantifies levels of active (not latent) TGF-β in tumor homogenates or cell culture supernatant, a critical biomarker. |
| Collagenase/Dispase Blend | Liberase TM (Roche) | High-activity enzyme blend for gentle dissociation of dense, stromal-rich tumors for high-quality single-cell suspensions. |
| Multiplex Immunofluorescence Kit | Opal 7-Color IHC Kit (Akoya Biosciences) | Enables simultaneous visualization of CD8, CD31, α-SMA, cytokeratin, DAPI etc., on one slide to study spatial relationships. |
| C57BL/6 Mouse Pan-T Cell Antibody Cocktail | (Bio X Cell) | For in vivo CD8+ T cell depletion studies (anti-CD8α) to validate their necessity in combination regimen efficacy. |
| Non-Invasive Blood Pressure System | CODA Monitor (Kent Scientific) | For longitudinal monitoring of hypertension, a key on-target toxicity of VEGF pathway inhibitors in mice. |
Benchmarking Success: Biomarkers, Clinical Outcomes, and Comparative Efficacy of Infiltration-Promoting Therapies
Within the broader investigation of Cytotoxic CD8+ T cell infiltration mechanisms in hot versus cold tumors, validated biomarkers are critical for patient stratification, therapeutic monitoring, and drug development. This guide details three core, validated biomarker classes: direct quantification of CD8+ T cells, transcriptomic immune gene signatures, and non-invasive radiomic correlates. Their integration provides a multi-scale view of the tumor immune microenvironment (TIME).
Core Biomarker Classes: Data & Validation
Table 1: Validated Biomarker Classes for CD8+ T Cell Infiltration
| Biomarker Class | Specific Measure | Platform/Method | Typical Output | Validation Context (Hot vs. Cold Tumors) |
|---|---|---|---|---|
| CD8+ Density | Cells/mm² (tumor core, invasive margin) | Immunohistochemistry (IHC), Immunofluorescence (IF), Digital Pathology | Spatial density maps; High vs. Low categorical score | Direct gold standard. Hot tumors show high, organized density; cold tumors show absent/low, disordered infiltration. |
| Immune Gene Signatures | Gene Expression Scores (e.g., CXCL9, CXCL10, IFNG, GZMB, PRF1) | Bulk RNA-seq, Nanostring, RT-qPCR | Continuous score (e.g., ssGSEA, z-score) | Reflect functional immune activity. High in hot tumors; suppressed in cold tumors (T-cell excluded/desert). |
| Radiomic Correlates | Texture, Shape, Intensity Features from Medical Imaging | CT, MRI (T1w, T2w), FDG-PET | Quantitative feature vectors (e.g., GLCM entropy, skewness) | Non-invasive surrogate. High textural heterogeneity often correlates with immune-rich hot tumors. |
Table 2: Key Quantitative Correlations from Recent Studies (2023-2024)
| Study Focus | Biomarkers Correlated | Correlation Coefficient (Range) | P-value Significance | Implication for Drug Development |
|---|---|---|---|---|
| NSCLC (Anti-PD-1) | Radiomic Texture (CT) vs. CD8+ IHC Density | Spearman ρ = 0.65 - 0.78 | p < 0.001 | Pre-treatment CT can identify responders. |
| Melanoma | IFN-γ Signature Score vs. Pathological Response | AUC = 0.82 - 0.89 | p < 0.0001 | Predictive biomarker for checkpoint inhibitor efficacy. |
| Colorectal Cancer | CD8+ Margin Density vs. Overall Survival | Hazard Ratio (High vs. Low) = 0.45 | p = 0.003 | Prognostic validation for patient stratification. |
| Glioblastoma (Cold) | Radiomic "Edema Pattern" vs. T-cell Exclusion | ρ = -0.71 | p < 0.01 | Identifies cold tumor physiology non-invasively. |
Detailed Experimental Protocols
Protocol 3.1: Multiplex Immunofluorescence (mIF) for CD8+ Density and Spatial Analysis
Objective: To quantitatively assess CD8+ T cell density and spatial relationship to tumor cells and other immune checkpoints (e.g., PD-L1). Key Reagents: See Scientist's Toolkit. Procedure:
- Tissue Sectioning: Cut 4-5 µm formalin-fixed, paraffin-embedded (FFPE) tumor sections.
- Deparaffinization & Antigen Retrieval: Bake slides, deparaffinize in xylene, rehydrate. Perform heat-induced epitope retrieval (HIER) in Tris-EDTA buffer (pH 9.0).
- Multiplex Staining Cycle (Iterative):
- Blocking: Incubate with protein block (10% normal serum) for 30 min.
- Primary Antibody: Apply primary antibody (e.g., anti-CD8, clone C8/144B) for 1 hr at RT.
- Secondary Detection: Use tyramide signal amplification (TSA) conjugated to a fluorophore (e.g., Opal 520).
- Microwave Stripping: Heat slide in microwave to strip antibodies, leaving fluorophores intact.
- Repeat for additional markers (e.g., CD3, PD-L1, CK, DAPI).
- Image Acquisition: Scan slides using a multispectral imaging system (e.g., Vectra Polaris, Akoya Biosciences) at 20x magnification.
- Image & Data Analysis:
- Use digital pathology software (inForm, HALO, QuPath) for cell segmentation (DAPI nuclei) and phenotyping.
- Calculate cells/mm² in defined regions (tumor core, invasive margin).
- Perform spatial analysis (e.g., nearest neighbor distance, cell-cell interaction mapping).
Protocol 3.2: Immune Gene Signature Profiling via Nanostring nCounter
Objective: To generate a quantitative immune gene expression profile from limited FFPE RNA. Key Reagents: nCounter PanCancer Immune Profiling Panel (770+ genes), RNA isolation kit for FFPE. Procedure:
- RNA Isolation: Extract total RNA from FFPE scrolls (≥ 5 x 10 µm) using a column-based FFPE RNA kit. Assess RNA integrity (DV200 > 50% acceptable).
- Hybridization: Combine 100-300 ng of RNA with the reporter code set and capture probe set. Hybridize at 65°C for 18-24 hours.
- Purification & Immobilization: Transfer the reaction to the nCounter Prep Station for automated purification and immobilization of probe-transcript complexes on a cartridge.
- Data Acquisition: Insert the cartridge into the nCounter Digital Analyzer. Count individual fluorescent barcodes. Data is exported as an RCC file.
- Data Analysis:
- Normalize counts using housekeeping genes.
- Calculate signature scores (e.g., "Cytotoxic Score" = mean normalized counts of PRF1, GZMA, GZMB, IFNG).
- Use pre-defined algorithms (e.g., nCounter Advanced Analysis) for cell type scoring.
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Biomarker Analysis
| Item / Reagent | Vendor Examples | Function in Context |
|---|---|---|
| Anti-Human CD8 Antibody (C8/144B) | Agilent Dako, Cell Signaling Tech | Primary antibody for IHC/mIF; definitive marker for cytotoxic T cells. |
| Opal TSA Fluorophore Multiplex Kit | Akoya Biosciences | Enables sequential, high-sensitivity multiplex detection on a single FFPE section. |
| nCounter PanCancer Immune Panel | Nanostring Technologies | Targeted gene expression panel for profiling 770+ immune genes from FFPE RNA. |
| FFPE RNA Isolation Kit | Qiagen (RNeasy FFPE), Thermo Fisher | Purifies degraded RNA from archived FFPE samples for downstream transcriptomics. |
| Multispectral Slide Scanner | Akoya (Vectra/Polaris), Leica (Aperio) | Captures high-resolution, multi-channel whole slide images for quantitative analysis. |
| Digital Pathology Analysis Software | Indica Labs (HALO), Akoya (inForm), QuPath (Open Source) | Performs automated cell segmentation, phenotyping, and spatial analysis on mIF images. |
| Radiomics Feature Extraction Software | PyRadiomics (Open Source), LIFEx, 3D Slicer | Extracts quantitative texture, shape, and intensity features from DICOM images (CT/MRI). |
Visualization of Workflows and Relationships
Diagram 1: Multi-Scale Biomarker Integration Workflow (100 chars)
Diagram 2: Biomarker Patterns in Hot vs. Cold Tumors (93 chars)
Thesis Context: This analysis is framed within the broader investigation of cytotoxic CD8+ T cell infiltration mechanisms, a pivotal determinant in converting immunologically "cold" tumors into "hot," T-cell-inflamed microenvironments to improve response to immunotherapies.
The tumor microenvironment (TME) presents dual barriers to effective immune infiltration: an abnormal, dysfunctional vasculature and a dense, immunosuppressive stroma. Stroma-targeting (e.g., focusing on cancer-associated fibroblasts (CAFs), extracellular matrix (ECM)) and vascular-targeting (e.g., angiogenesis normalization, vascular disruption) combination therapies represent two strategic fronts to overcome these barriers. This whitepaper provides a head-to-head comparison of clinical outcomes from trials combining these approaches with immune checkpoint inhibitors (ICIs), evaluating their efficacy in promoting CD8+ T cell tumor infiltration and subsequent antitumor activity.
Clinical Trial Data Synthesis
| Therapy Category | Drug Combination (Target) | Cancer Type (Phase) | Primary Endpoint (ORR/PFS/OS) | Key CD8+ T Cell Infiltration Biomarker Outcome | Reference / NCT Number |
|---|---|---|---|---|---|
| Stroma-Targeting | Atezolizumab (anti-PD-L1) + Bevacizumab (anti-VEGF-A) | Hepatocellular Carcinoma (Phase III) | OS: 19.2 vs 13.4 mo (HR 0.66) | Increased CD8+ density in responders; associated with CXCL11 expression | IMbrave150 (NCT03434379) |
| Durvalumab (anti-PD-L1) + Oleclumab (anti-CD73) | NSCLC (Phase II) | ORR: 20-29% in biomarker high | Reduction in stromal adenosine; trend for increased CD8+ in tumor nests | COAST (NCT03822351) | |
| Nivolumab (anti-PD-1) + Pegylated hyaluronidase (PEGPH20) (HA degradation) | HA-High Pancreatic Cancer (Phase II) | ORR: 13% | Decreased stromal HA; increased tumor vasculature and T cell access | HALO-202 (NCT03634332) | |
| Vascular-Targeting (Normalization) | Pembrolizumab (anti-PD-1) + Lenvatinib (multi-TKI: VEGFR, FGFR) | Endometrial Carcinoma (Phase III) | PFS: 7.2 vs 3.8 mo (HR 0.56) | Increased pericyte coverage (vessel normalization); enhanced T cell infiltration | KEYNOTE-775 (NCT03517449) |
| Atezolizumab + Cabozantinib (multi-TKI: VEGFR2, MET, AXL) | RCC (Phase III) | PFS: 10.3 vs 10.2 mo (NS) | Improved vessel structure; correlation with myeloid cell modulation | CONTACT-03 (NCT04338269) | |
| Vascular-Targeting (Disruption) | Pembrolizumab + Vorolanib (VEGFR/PDGFR TKI) | RCC (Phase II) | ORR: 55% | Data pending on immune cell changes post-vascular modulation | (NCT05366816) |
Experimental Protocols for Key Biomarker Analyses
Protocol 1: Multiplex Immunofluorescence (mIF) for Spatial T Cell Analysis
- Objective: Quantify and spatially resolve CD8+ T cells relative to tumor cells (CK+), stroma (αSMA+), and vasculature (CD31+).
- Methodology:
- Tissue Sectioning: Cut 4-5 µm formalin-fixed, paraffin-embedded (FFPE) tumor biopsies (pre- & post-treatment).
- Multiplex Staining: Employ sequential immunohistochemistry (IHC) with tyramide signal amplification (TSA) or antibody elution. A typical panel: DAPI, Pan-Cytokeratin (CK), α-Smooth Muscle Actin (αSMA), CD8, CD31, PD-L1.
- Image Acquisition: Scan slides using a multispectral microscope (e.g., Vectra/Polaris, Akoya Biosciences; or equivalent).
- Image Analysis: Use digital pathology software (inForm, HALO, QuPath). Train algorithms to:
- Segment tissue into tumor, stromal, and vascular compartments.
- Identify and count all positively stained cells.
- Calculate densities (cells/mm²) and proximity metrics (e.g., CD8+ to CD31+ vessel distance).
Protocol 2: Flow Cytometry for Immune Profiling of Dissociated Tumors
- Objective: Perform high-dimensional immunophenotyping of tumor-infiltrating leukocytes.
- Methodology:
- Tumor Dissociation: Mechanically dissociate and enzymatically digest (e.g., Collagenase IV/DNase I) fresh tumor samples to single-cell suspension.
- Staining: Stain cells with viability dye, then surface antibodies (e.g., CD45, CD3, CD8, CD4, CD19, CD11b, Ly6G, Ly6C). For intracellular markers (IFN-γ, Granzyme B), perform fixation/permeabilization after ex vivo stimulation.
- Acquisition & Analysis: Acquire on a ≥15-parameter flow cytometer. Analyze using FlowJo software. Gate: Live CD45+ > Lymphocytes > CD3+ > CD8+ or CD4+. Report frequency of CD8+ T cells as % of CD45+ or total live cells.
Visualizations
Diagram Title: Stroma-Targeting Therapy Mechanism to Enhance T Cell Infiltration
Diagram Title: Vascular-Targeting Therapy Mechanism to Enhance T Cell Infiltration
Diagram Title: Biomarker Analysis Workflow for Combination Therapy Trials
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for TME & T Cell Infiltration Analysis
| Reagent Category | Specific Example(s) | Primary Function in Research |
|---|---|---|
| Enzymatic Digestion Kit | Miltenyi Biotec Tumor Dissociation Kit; Collagenase IV/Hyaluronidase/DNase I cocktails | Generates single-cell suspensions from solid tumors for downstream flow cytometry or single-cell RNA-seq. |
| Multiplex IHC/IF Panels | Akoya Biosciences PhenoCycler/PhenoImager panels; Standardized panels for CD8/PD-1/PD-L1/αSMA/CD31 etc. | Enables simultaneous spatial profiling of immune cells, stroma, and vasculature in FFPE tissue. |
| Phospho-/Total Antibody Panels | Cell Signaling Technology (CST) Multiplex IF Panels for signaling (pSTAT, pAKT, pERK). | Assesses activation states of signaling pathways in specific cell types within the TME. |
| Recombinant Cytokines/Chemokines | Recombinant human/mouse CXCL9, CXCL10, CXCL11, IFN-γ. | Used in functional assays (e.g., T cell migration) to test mechanisms of enhanced trafficking. |
| Endothelial Cell Markers | Anti-CD31 (PECAM-1), Anti-Endoglin (CD105), Anti-VE-Cadherin antibodies. | Labels blood vessels for assessment of vascular density, maturity, and normalization. |
| Live/Dead & Viability Dyes | Zombie Aqua (BioLegend), LIVE/DEAD Fixable Viability Dyes (Thermo Fisher). | Critical for excluding dead cells in flow cytometry to ensure accurate immunophenotyping. |
| Intracellular Staining Kits | Foxp3/Transcription Factor Staining Buffer Set (e.g., from Thermo Fisher or BD). | Permits staining of intracellular targets like transcription factors (FoxP3, T-bet) and cytokines. |
Within the broader context of cytotoxic CD8+ T cell infiltration mechanisms in "hot" versus "cold" tumor research, a central therapeutic challenge is overcoming the physical and immunosuppressive barriers that limit lymphocyte entry into solid tumor microenvironments (TMEs). This whitepaper provides an in-depth technical comparison of three major immunotherapeutic modalities—T cell engagers (TCEs), bispecific antibodies (BsAbs), and cellular therapies (including TCR-T and CAR-T)—focusing on their engineered mechanisms to circumvent infiltration hurdles. Each class employs distinct strategies to bridge the gap between systemic administration and effective intratumoral cytotoxicity.
T Cell Engagers (TCEs) & Bispecific Antibodies
These recombinant proteins are designed to create an artificial immunological synapse between a T cell (via CD3 engagement) and a tumor-associated antigen (TAA) on a cancer cell, independent of MHC presentation.
Mechanism to Overcome Infiltration
TCEs/BsAbs are administered systemically and do not require the pre-existence of tumor-infiltrating lymphocytes (TILs). Their small size (relative to cells) allows for better initial vascular extravasation. They actively recruit circulating T cells to the tumor site by binding to TAAs on the endothelial cell surface or within the perivascular space, initiating local T cell activation and cytokine release. This can alter the vascular endothelium and increase permeability, potentially initiating an in situ "warming" of cold tumors.
Key Experimental Protocol: Evaluation of TCE-Induced T Cell RecruitmentIn Vivo
- Objective: To quantify the spatial redistribution of circulating T cells following systemic TCE administration in a cold tumor model.
- Methodology:
- Model Establishment: Implant antigen-positive tumor cells subcutaneously in immunodeficient mice. Adoptively transfer fluorescently labeled human CD8+ T cells intravenously.
- Treatment: Administer a single dose of anti-CD3 x anti-TAA TCE or control IgG.
- Longitudinal Imaging: Use intravital microscopy (IVM) at 0, 6, 24, and 48 hours post-treatment to monitor T cell behavior in tumor vessels and parenchyma.
- Endpoint Analysis: Harvest tumors at 72 hours. Process for multiplex immunofluorescence (mIF) staining (CD8, CD3, Granzyme B, endothelial markers). Quantify T cell density (cells/mm²) in defined regions (perivascular, invasive margin, core) using digital pathology software.
- Flow Cytometry: Digest tumors and analyze for T cell activation markers (CD69, CD25) and exhaustion markers (PD-1, LAG-3).
Table 1: Quantitative Comparison of Infiltration-Related Parameters for Immunotherapies
| Parameter | T Cell Engagers/Bispecifics | Cellular Therapies (CAR-T/TCR-T) |
|---|---|---|
| Primary Infiltration MoA | Systemic delivery & recruitment of endogenous circulating T cells. | Direct infusion of ex vivo expanded, tumor-targeted T cells. |
| Dependence on Pre-existing TILs | No. Can function in "cold" environments. | Yes/No. Requires infused cells to traffic; may not expand in cold TME. |
| Key Trafficking Signals | T cell activation (via CD3) releases cytokines (IFN-γ, TNF-α) that upregulate vascular adhesion molecules (VCAM-1, ICAM-1). | Relies on chemokine receptor-ligand matching (e.g., CXCR3-CXCL9/10) and adhesion molecules (LFA-1/ICAM-1). |
| Typical Time to Detectable Intratumoral Activity | Hours to days. | Days to weeks (requires expansion). |
| Major Physical Barrier | Tumor vasculature abnormal permeability; antigen heterogeneity/low density. | Tumor vasculature (inadequate homing signals); dense stroma (e.g., fibrosis). |
| Representative Clinical Response Rate in Solid Tumors (e.g., Prostate, NSCLC) | ~20-40% (e.g., BiTE platforms). | ~10-30% (varies greatly with target and tumor type). |
Diagram 1: T Cell Engager Mechanism for Recruiting T Cells.
Cellular Therapies: CAR-T and TCR-T Cells
These therapies involve the genetic modification of a patient's own T cells to express either a Chimeric Antigen Receptor (CAR) or a T Cell Receptor (TCR) with specificity for a tumor target.
Mechanism to Overcome Infiltration
The infiltration hurdle is a critical bottleneck. Success depends on the trafficking, extravasation, and persistence of the infused cells.
- Trafficking: Requires homing signals. Engineering T cells to express chemokine receptors (e.g., CXCR2 for pancreatic cancer, CCR4 for lymphomas) matching tumor-secreted chemokines can improve directed migration.
- Extravasation: Relies on adhesion molecule interactions (e.g., LFA-1/ICAM-1). Pre-conditioning with lymphodepleting chemotherapy (e.g., cyclophosphamide/fludarabine) induces inflammatory cytokines that upregulate endothelial adhesion molecules.
- Overcoming Stromal Barriers: Co-expressing enzymes like heparinase to degrade the extracellular matrix or using armored CARs secreting TGF-β inhibitors can facilitate penetration into the tumor core.
Key Experimental Protocol: Evaluating Engineered T Cell TraffickingIn Vivo
- Objective: To compare the tumor infiltration efficiency of standard vs. chemokine receptor-engineered CAR-T cells.
- Methodology:
- Cell Engineering: Generate two lentiviral constructs: a) Standard anti-mesothelin CAR; b) Same CAR + CXCR2 receptor. Transduce human primary CD8+ T cells.
- Model & Labeling: Establish orthotopic or subcutaneous tumors in NSG mice. Label CAR-T cell products with distinct fluorescent (e.g., CellTrace Violet) and luciferase (firefly luc) reporters for tracking.
- Infusion & Imaging: Infuse cells intravenously. Perform serial bioluminescence imaging (BLI) over 14 days to monitor whole-body trafficking.
- Ex Vivo Analysis: At endpoint, harvest tumors and organs (spleen, lungs, blood). Create single-cell suspensions. Use flow cytometry to quantify CAR+ T cell numbers. Perform spatial analysis via mIF (anti-human CD3, anti-CAR idiotype, tumor markers) to map intratumoral distribution.
The Scientist's Toolkit: Key Research Reagents
| Reagent/Category | Example(s) | Function in Infiltration Research |
|---|---|---|
| Chemokine Receptor Kits | Human Chemokine Receptor PCR Array, Recombinant Chemokines (CXCL9, CCL2, etc.) | Identify tumor chemokine profiles and match engineered T cell receptors. |
| Intravital Dyes | CellTrace Violet/CFSE, Qtracker nanocrystals | Long-term, non-transferable fluorescent labeling of infused T cells for in vivo tracking. |
| Bioluminescence Reporters | Firefly luciferase (fluc) lentivirus, D-Luciferin substrate | Non-invasive, longitudinal monitoring of cell localization and expansion. |
| Multiplex IHC/IF Panels | Antibodies: CD8, CD3, Granzyme B, PD-1, α-SMA (stroma), CD31 (vessels) | Spatial profiling of T cell infiltration depth, activation state, and relationship to barriers. |
| Lymphodepleting Agents | Cyclophosphamide, Fludarabine (for mouse models) | Pre-condition host to enhance engraftment and create a pro-inflammatory milieu. |
| Microfluidic Assays | Tumor-on-a-chip with endothelial barriers | In vitro modeling of T cell trans-endothelial migration under flow. |
Diagram 2: Cellular Therapy Infiltration Hurdles & Solutions.
While TCEs/BsAbs act as "recruiters" leveraging systemic circulation, cellular therapies are "engineered infiltrators" whose success is defined by overcoming multi-step trafficking barriers. The future lies in combination strategies and next-generation engineering: priming the TME with oncolytic viruses or radiation to increase chemokine production before cellular therapy, or developing conditionally active TCEs that only bind CD3 within the TME to reduce systemic toxicity while promoting local infiltration. Understanding and quantifying these distinct mechanisms through the protocols and tools outlined above is essential for rationally designing the next wave of solid tumor immunotherapies.
Within the broader thesis of cytotoxic CD8+ T cell infiltration mechanisms in "hot" versus "cold" tumors, a critical paradox has emerged: successful enhancement of T cell tumor infiltration does not consistently correlate with improved patient survival. This whitepaper analyzes failed clinical trials to dissect this disconnect, moving beyond the simplistic "if you build it, they will come" hypothesis to a more nuanced understanding of the tumor immune microenvironment (TIME).
Case Studies of Failed Translation
The following clinical trials demonstrated significant increases in CD8+ T cell tumor infiltration, measured via biopsy and immunohistochemistry, yet failed to achieve their primary overall survival (OS) or progression-free survival (PFS) endpoints.
Table 1: Summary of Clinical Trials with Failed Infiltration-to-Survival Translation
| Trial Identifier / Drug Name | Target/Mechanism | Cancer Type | Phase | Key Infiltration Metric (Increase vs. Control) | Primary Survival Endpoint Result | Proposed Reason for Failure |
|---|---|---|---|---|---|---|
| CheckMate 026 (Nivolumab) | PD-1 inhibition | Non-small cell lung cancer (NSCLC) | III | ↑ CD8+ density in tumor nests (p<0.001) | No OS benefit vs. chemotherapy (HR 1.15, p=0.25) | Pre-existing, non-productive infiltration; high tumor mutational burden (TMB) defined benefit subset. |
| MASTERKEY-265 (T-VEC + Pembrolizumab) | Oncolytic virus + PD-1 inhibition | Melanoma | III | ↑ intratumoral CD8+ cells (geometric mean ratio 5.33) | No significant OS improvement (HR 0.96, p=0.42) | Insufficient reversal of immunosuppressive myeloid compartment; viral-induced inflammation not sustained. |
| CA184-043 (Ipilimumab) | CTLA-4 inhibition | Metastatic castration-resistant prostate cancer | III | ↑ inflamed tumor phenotype in biopsies | No OS benefit (HR 0.85, p=0.07) | Highly immunosuppressive, "cold" stromal microenvironment limited T cell function despite infiltration. |
| JAVELIN Renal 101 (Avelumab + Axitinib) | PD-L1 inhibition + TKI | Renal cell carcinoma (RCC) | III | ↑ CD8+ T cell density in PD-L1+ tumors | PFS benefit but no OS benefit (HR 0.82, p=0.067) | Compensatory upregulation of alternative immune checkpoints (e.g., TIM-3, LAG-3). |
| IMpassion130 (Atezolizumab + Nab-paclitaxel) | PD-L1 inhibition + Chemo | Triple-Negative Breast Cancer (TNBC) | III | ↑ TILs in tumor stroma (pre-specified exploratory) | OS benefit in PD-L1+ population not sustained in final OS analysis | Inadequate T cell priming and clonal diversity; T cell exhaustion programs remained intact. |
Mechanistic Dissection of Failure Modes
The analysis of tumor biopsies and correlative science from these trials reveals distinct biological failure modes.
Table 2: Quantitative Analysis of Failure Modes from Trial Correlative Studies
| Failure Mode | Measurable Biomarker | Typical Assay | Representative Finding from Failed Trial |
|---|---|---|---|
| Pre-Existing Non-Functional Infiltrate | PD-1hi TOXhi CD8+ T cells | Multiplex IHC, RNA-seq | In CheckMate 026, high baseline "exhausted" CD8+ signature predicted poor response to anti-PD-1 monotherapy. |
| Persistent Immunosuppressive Microenvironment | FoxP3+ Treg density, CD68+ M2-like TAMs | IHC, Flow Cytometry | In MASTERKEY-265, post-treatment biopsies showed persistent M2 macrophages and TGF-β signature. |
| Inadequate T Cell Priming & Clonality | T cell receptor (TCR) clonality, Neoantigen quality | TCR sequencing, Exome-seq | In IMpassion130 TNBC, low baseline TCR clonality and few immunogenic neoantigens were observed in non-responders. |
| Compensatory Inhibitory Pathway Upregulation | TIM-3, LAG-3, VISTA co-expression | Multiplex IHC, scRNA-seq | In JAVELIN RCC, TIM-3 expression on infiltrating lymphocytes increased post-avelumab treatment. |
| Metabolic Inhibition & Hypoxia | HIF-1α, ARG1, Extracellular Adenosine | IHC, Mass Spec | In CA184-043 prostate cancer, hypoxic cores with high adenosine signaling rendered infiltrating T cells anergic. |
Key Experimental Protocols for Investigating the Paradox
Protocol 1: Multiplex Immunohistochemistry (mIHC) for Spatial Phenotyping of Infiltrates
- Objective: To quantify and spatially map functional and exhausted T cells alongside immunosuppressive cells within the tumor microenvironment.
- Procedure:
- Tissue Sectioning: Cut 4-5 μm formalin-fixed, paraffin-embedded (FFPE) tumor biopsy sections.
- Multiplex Staining: Use an automated system (e.g., Akoya Phenocycler or Vectra) with a validated antibody panel (e.g., CD8, CD3, PD-1, TIM-3, Ki67, FoxP3, CD68, Pan-CK).
- Cyclic Staining: Perform iterative rounds of antibody application, fluorescence imaging, and dye inactivation.
- Image Analysis: Use digital pathology software (e.g., HALO, QuPath) for cell segmentation and phenotyping. Define "functional niches" (CD8+Ki67+PD-1lo) and "exhausted/ suppressed niches" (CD8+PD-1hiTIM-3+ in proximity to FoxP3+ or CD68+ cells).
- Spatial Statistics: Calculate nearest-neighbor distances, cellular colocalization, and infiltration patterns relative to tumor islands and stroma.
Protocol 2: Single-Cell RNA Sequencing (scRNA-seq) with TCR Sequencing
- Objective: To dissect the transcriptional states and clonal relationships of tumor-infiltrating lymphocytes (TILs).
- Procedure:
- Fresh Tissue Dissociation: Process fresh tumor biopsies immediately into a single-cell suspension using a gentle, enzymatic dissociation kit (e.g., Miltenyi Tumor Dissociation Kit).
- Live Immune Cell Enrichment: Isolate live CD45+ cells using magnetic-activated cell sorting (MACS).
- Single-Cell Partitioning: Load cells onto a platform like the 10x Genomics Chromium to generate Gel Bead-In-Emulsions (GEMs).
- Library Preparation: Construct gene expression (GEX) and paired V(D)J (TCR) libraries per manufacturer's protocol.
- Bioinformatics Analysis: Process data using Cell Ranger. Use Seurat or Scanpy for clustering, UMAP visualization, and differential expression. Integrate with TCR data (via Cell Ranger VDJ) to track clonal expansion across exhausted, effector, and memory clusters.
Protocol 3: Ex Vivo T Cell Functional Suppression Assay
- Objective: To directly test the functional capacity of infiltrating CD8+ T cells and the suppressive nature of the myeloid compartment.
- Procedure:
- Cell Isolation: From dissociated tumor, sort purified populations: CD8+ T cells (CD3+CD8+), autologous myeloid-derived suppressor cells (MDSCs; CD11b+CD33+HLA-DRlo/-), and tumor cells (if feasible).
- Co-culture Setup: Plate sorted CD8+ T cells with anti-CD3/CD28 activation beads. Add back sorted autologous myeloid cells at varying ratios (e.g., 1:1, 1:0.5 T cell:MDSC).
- Functional Readouts:
- Proliferation: After 72-96h, measure by CFSE dilution or EdU incorporation via flow cytometry.
- Cytokine Production: After 6h re-stimulation with PMA/ionomycin in the presence of brefeldin A, intracellularly stain for IFN-γ and TNF-α.
- Cytotoxicity: Co-culture activated T cells with fluorescently labeled autologous tumor organoids or cell lines, measuring target cell death via live-cell imaging or LDH release.
Signaling and Cellular Relationship Diagrams
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Investigating Infiltration Efficacy
| Reagent Category | Specific Product/Kit (Example) | Primary Function in Analysis |
|---|---|---|
| Tissue Dissociation | Miltenyi Biotec Human Tumor Dissociation Kit | Gentle enzymatic degradation of tumor stroma to generate viable single-cell suspensions for flow cytometry or scRNA-seq. |
| Cell Isolation & Sorting | StemCell Technologies EasySep Human CD8+ T Cell Isolation Kit; BD FACSAria Cell Sorter | Negative selection magnetic beads for high-purity CD8+ T cell isolation. High-speed sorter for precise purification of rare immune subsets (e.g., Tregs, specific macrophage phenotypes). |
| Multiplex IHC/IF | Akoya Biosciences Opal 7-Color Automation IHC Kit; Standard validated antibodies (CD8, PD-1, TIM-3, etc.) | Enables simultaneous detection of 6+ biomarkers on one FFPE section to define spatial relationships and co-expression patterns in the TIME. |
| Single-Cell Genomics | 10x Genomics Chromium Next GEM Single Cell 5' Kit v2 with Feature Barcode for Cell Surface Protein | Captures paired gene expression and TCR sequencing from thousands of single cells, allowing clonal tracking and deep phenotyping. |
| Functional Assays | Thermo Fisher CellTrace CFSE Cell Proliferation Kit; BioLegend LEGENDplex Human CD8/NK Panel | Tracks T cell division history. Multiplex bead-based assay quantifies secretion of key cytotoxic (IFN-γ, Granzyme B) and exhaustion (IL-10) proteins. |
| Spatial Transcriptomics | 10x Genomics Visium Spatial Gene Expression Kit | Correlates transcriptional profiles with histological location in intact tissue sections, bridging mIHC and scRNA-seq data. |
| Metabolic Profiling | Agilent Seahorse XFp Cell Energy Phenotype Test Kit | Measures real-time extracellular acidification and oxygen consumption rates in isolated TILs to assess metabolic fitness (glycolysis vs. oxidative phosphorylation). |
Within the broader thesis of Cytotoxic CD8+ T cell infiltration mechanisms in hot versus cold tumors, this whitepaper delineates a proposed future standard for defining the pathological and molecular criteria that constitute a successful "cold-to-hot" conversion. This conversion represents a paradigm shift in immuno-oncology, aiming to reprogram immunologically quiescent ("cold") tumors into inflamed ("hot") microenvironments susceptible to immune attack.
The clinical dichotomy of "hot" and "cold" tumors is a cornerstone of modern immuno-oncology. While hot tumors, characterized by robust CD8+ T cell infiltration, often respond to immune checkpoint inhibitors (ICIs), cold tumors remain refractory. The field's central challenge is inducing de novo or enhancing existing T cell infiltration—a process termed "cold-to-hot" conversion. However, a lack of standardized, multi-modal criteria to define and measure this conversion hampers biomarker development, clinical trial design, and therapeutic comparison. This guide establishes a framework integrating histopathological, genomic, transcriptomic, and cellular criteria.
Defining Baseline States: Core Characteristics of Cold vs. Hot Tumors
Table 1: Defining Characteristics of Cold and Hot Tumor Microenvironments (TME)
| Criteria | Cold TME (Immune-Desert/Excluded) | Hot TME (Immune-Inflamed) |
|---|---|---|
| Pathological (IHC) | Low CD8+ density (< 100 cells/mm² at invasive margin); absence of TLS; high stromal content. | High CD8+ density (> 250 cells/mm²), particularly in tumor core; presence of TLS. |
| Molecular Signature | Non-inflamed gene signature (e.g., low IFN-γ, CXCL9/10, Granzyme B). | Inflamed signature (high IFN-γ response, cytolytic activity score). |
| Immune Cell Context | Low CD8+/Treg ratio (< 1); high M2 macrophage/TAM infiltration; low DC density. | High CD8+/Treg ratio (> 3); presence of mature DCs (CD103+). |
| Tumor-Intrinsic Factors | Low TMB (< 5 mut/Mb); deficient antigen presentation (β2M, HLA loss); oncogenic pathways (WNT/β-catenin). | Higher TMB (> 10 mut/Mb); intact antigen presentation machinery. |
| Vascular/Stromal | Poorly functional, immature vasculature (low PDGFR-β+ pericyte coverage); dense, aligned collagen. | Mature vasculature; disorganized, porous stromal matrix. |
Multimodal Criteria for 'Cold-to-Hot' Conversion
A successful conversion must be validated across multiple orthogonal assays. The proposed standard requires meeting thresholds in at least two of the three following categories.
Table 2: Quantitative Thresholds for Defining Conversion
| Category | Primary Metric | Threshold for Conversion | Validated Assay |
|---|---|---|---|
| Cellular Infiltration | CD8+ T cell density in tumor core | ≥ 2-fold increase from baseline, achieving > 200 cells/mm² | Multiplex IHC (mIHC) |
| Functional Immune Activation | IFN-γ Gene Signature Score (e.g., 18-gene set) | ≥ 1.5-fold increase & shift to top 40th percentile vs. baseline | RNA-seq (NanoString) |
| Spatial Reorganization | CD8+ cells within 30μm of CK+ tumor cells | ≥ 3-fold increase in proximity index | Digital Spatial Profiling |
| Tertiary Lymphoid Structure (TLS) Neogenesis | Presence of DC-LAMP+ DCs & CD20+ B cell aggregates | De novo formation of PNAd+ vessels and T/B cell zones | Sequential IHC staining |
Experimental Protocols for Key Validation Assays
Protocol: Multiplex Immunohistochemistry (mIHC) for TME Profiling
Objective: Quantify density and spatial relationships of immune cells.
- Tissue Preparation: Formalin-fixed, paraffin-embedded (FFPE) sections (4μm) mounted on charged slides.
- Multiplex Staining: Employ a tyramide signal amplification (TSA)-based cyclic method (e.g., Opal, Akoya).
- Panel: CD8 (cytotoxic T cells), CD4 (Helper T cells), FoxP3 (Tregs), CK (tumor cells), CD68 (macrophages), DAPI (nuclei).
- Cycle: Primary Ab incubation → HRP-polymer secondary → TSA-fluorophore application → microwave-mediated antibody stripping. Repeat for 5-7 markers.
- Image Acquisition: Scan slides using a multispectral imaging system (Vectra/Polaris).
- Image & Data Analysis: Use inForm or QuPath software for spectral unmixing, cell segmentation (DAPI), and phenotyping. Calculate cell densities and proximity analyses.
Protocol: Spatial Transcriptomics for Niche Analysis
Objective: Correlate gene expression signatures with histological features.
- Region of Interest (ROI) Selection: Based on prior H&E/mIHC, select ROIs (e.g., invasive margin, tumor core, TLS) for profiling.
- Platform: Utilize the Visium Spatial Gene Expression platform (10x Genomics).
- Workflow: FFPE tissue section placed on Visium slide → H&E imaging → tissue permeabilization → cDNA synthesis in situ from poly-adenylated mRNA bound to spatially barcoded primers → library construction → next-generation sequencing.
- Data Integration: Align sequencing data to histological image. Use Seurat or Space Ranger for analysis to identify "cold-to-hot" signature genes within specific morphological contexts.
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Reagent Solutions for 'Cold-to-Hot' Research
| Reagent/Solution | Provider Examples | Primary Function in Research |
|---|---|---|
| Opal Multiplex IHC Kits | Akoya Biosciences | Enable sequential detection of 6+ biomarkers on a single FFPE section for deep phenotyping. |
| Mouse syngeneic "Cold" tumor models (e.g., B16-F10, 4T1) | ATCC, Charles River | Preclinical models with known low immunogenicity and T cell infiltration for testing conversion agents. |
| PANORAMIC Spatial barcoding slides | Vizgen (MERSCOPE) | Enable high-resolution, single-cell spatial transcriptomics to map gene expression in the TME. |
| TruSight Oncology 500 | Illumina | Comprehensive genomic profiling assay to assess TMB, MSI, and specific mutations (e.g., STK11, B2M) that influence cold phenotype. |
| Recombinant cytokines: mIL-12, hIFN-γ | PeproTech, BioLegend | Used as positive controls in vitro to induce inflammatory gene signatures or to validate pathway activity. |
| LIVE/DEAD Fixable Viability Dyes | Thermo Fisher Scientific | Critical for flow cytometry to exclude dead cells, ensuring accurate immune population analysis from dissociated tumors. |
| Anti-mouse/human CD8α depleting antibodies | Bio X Cell, InvivoMab | Used in validation experiments to confirm the functional dependency of therapeutic efficacy on CD8+ T cells. |
Key Signaling Pathways in Conversion
Diagram Title: Key Pathways Targeted for Cold-to-Hot Conversion
Integrated Experimental Workflow for Conversion Studies
Diagram Title: Integrated Preclinical Validation Workflow
The transition from a cold to a hot TME is a complex, multi-factorial process. This proposed standard, integrating quantitative pathological metrics with molecular and spatial profiling, provides a necessary framework for consistent evaluation across preclinical and clinical studies. Widespread adoption will accelerate the development of effective combination therapies, validate predictive biomarkers, and ultimately improve outcomes for patients with immunologically cold tumors. The future of immuno-oncology depends on our ability to not just induce inflammation, but to define, measure, and standardize it.
Conclusion
The infiltration of cytotoxic CD8+ T cells into the tumor core is a non-redundant, multi-step process whose failure defines the cold tumor phenotype and limits the efficacy of immunotherapies. This review has delineated the foundational biological barriers—dysfunctional vasculature, immunosuppressive stroma, and deficient chemokine signaling—that must be systematically addressed. Methodological advances now allow precise quantification of infiltration, enabling the rational design of combination strategies targeting these specific checkpoints. While promising, optimizing these combinations requires careful management of toxicity and sequencing. Validation studies underscore that simply increasing T cell numbers is insufficient; their functional quality and the reprogramming of the entire suppressive microenvironment are paramount. The future of immuno-oncology lies in moving beyond PD-1/PD-L1 blockade to integrated, mechanism-based approaches that ensure effective T cell delivery and sustained activity within the tumor, thereby converting immunological 'deserts' into fertile ground for therapeutic response. This will require continued collaboration between basic immunologists, translational scientists, and clinical trialists to develop the next wave of transformative cancer treatments.