Cancer Immunoediting Explained: From Immune Surveillance Principles to Immunotherapy Application
This article provides a comprehensive examination of the core principles of cancer immunoediting and immune surveillance, tailored for researchers and drug development professionals.
Cancer Immunoediting Explained: From Immune Surveillance Principles to Immunotherapy Application
Abstract
This article provides a comprehensive examination of the core principles of cancer immunoediting and immune surveillance, tailored for researchers and drug development professionals. We begin by establishing the historical and mechanistic foundations of the 'Three E's' framework—Elimination, Equilibrium, and Escape. We then explore the critical methodologies and tools, from murine models to humanized systems, used to study these processes and their direct application in therapeutic discovery. A dedicated section addresses common experimental pitfalls and optimization strategies for enhancing model fidelity and data interpretation. Finally, we evaluate and compare key biomarkers, predictive models, and clinical validation strategies that bridge preclinical findings to patient outcomes. This synthesis aims to equip scientists with both the fundamental understanding and practical toolkit needed to advance next-generation cancer immunotherapies.
Decoding the Three E's: Foundational Principles of Cancer Immunoediting and Surveillance
The conceptual framework for understanding the dynamic interaction between a developing tumor and the host immune system has undergone a profound evolution. This whitepaper, situated within the thesis on the basic principles of cancer immunoediting, traces the trajectory from the foundational Immune Surveillance Theory to the comprehensive three-phase Immunoediting Paradigm. This evolution reflects a shift from a linear, protective model to a dynamic, dual-host-protective and tumor-sculpting process, fundamentally informing modern cancer immunotherapy research and drug development.
The Immune Surveillance Theory: A Foundational Hypothesis
Proposed by Macfarlane Burnet and Lewis Thomas in the mid-20th century, the Immune Surveillance Theory posited that the immune system continuously patrols the body to recognize and eliminate nascent transformed cells, thereby preventing cancer. It was largely a theory of host defense.
Key Supporting & Challenging Experimental Evidence: Table 1: Foundational Experiments in Immune Surveillance
| Experiment / Model | Key Finding | Interpretation & Limitation |
|---|---|---|
| Chemical Carcinogenesis in Immunodeficient Mice (Prehn et al., 1970s) | Mice treated with methylcholanthrene (MCA) developed tumors more readily if immunosuppressed. | Supported a protective role for immunity. |
| Nude Mouse Studies (Stutman, 1970s) | Athymic (T-cell deficient) nude mice showed no marked increase in spontaneous tumors. | Challenged the comprehensiveness of surveillance, suggesting it was not absolute for all cancers. |
| IFN-γ and Perforin Knockout Mice (Kaplan et al., Shankaran et al., 1990s-2000s) | Mice deficient in key immune effector molecules showed increased susceptibility to spontaneous and induced tumors. | Provided molecular validation of immune surveillance components. |
Detailed Protocol: Chemical Carcinogenesis Susceptibility Assay
- Animal Groups: Establish two cohorts: wild-type (WT) C57BL/6 mice and immunodeficient (e.g., Rag2-/- lacking T and B cells) mice on the same background.
- Carcinogen Administration: At 6-8 weeks of age, administer a single subcutaneous (s.c.) injection of 100-400 µg of MCA in 100 µL of corn oil into the flank.
- Tumor Monitoring: Palpate injection sites weekly for 100-150 days. Measure tumor dimensions with calipers. Define tumor incidence (% of mice with tumor) and latency (time to tumor >1-2 mm in diameter).
- Analysis: Compare tumor incidence and growth kinetics between WT and immunodeficient groups using Kaplan-Meier survival curves and log-rank tests.
The Immunoediting Paradigm: A Three-Phase Synthesis
The contradictory data led to a refined model: the Cancer Immunoediting concept, formalized by Schreiber, Old, and Smyth. It encompasses three sequential, interconnected phases: Elimination, Equilibrium, and Escape (the "Three E's").
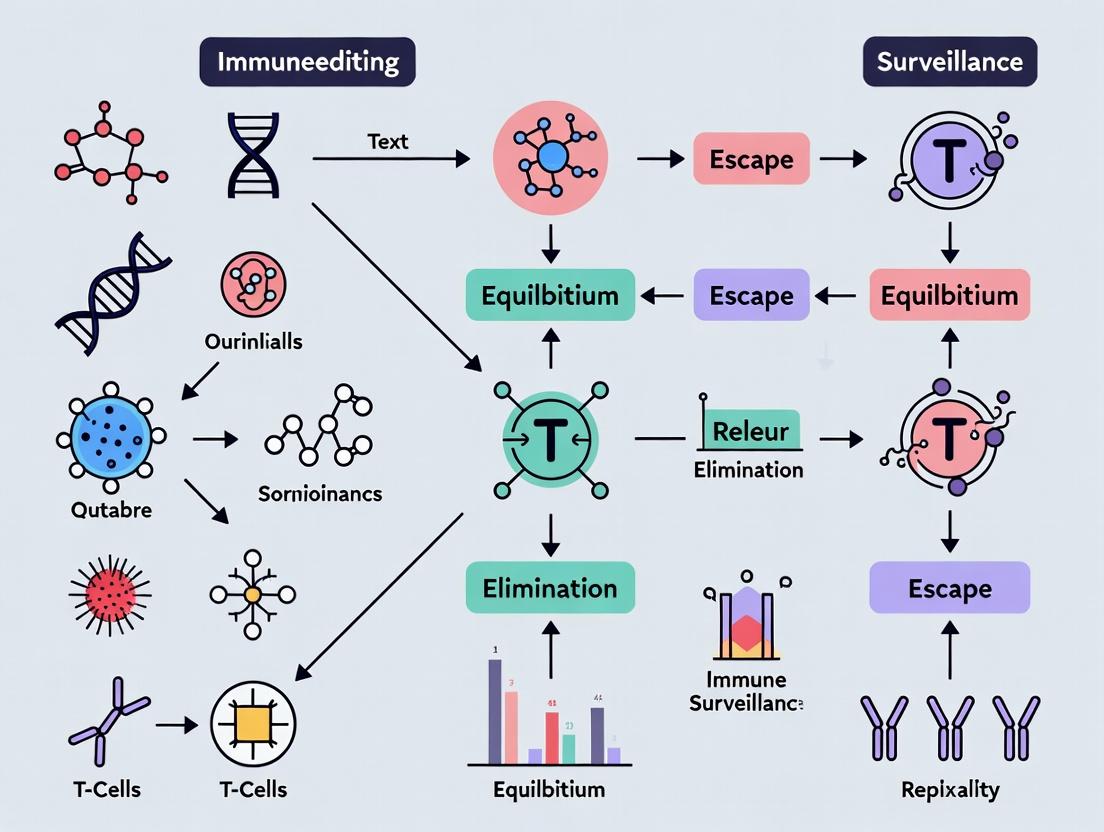
Diagram Title: The Three Phases of Cancer Immunoediting
Phase 1: Elimination – This phase is the classic immune surveillance, where innate and adaptive immunity detect and destroy immunogenic tumor cells. Phase 2: Equilibrium – A prolonged, dynamic stalemate where immune pressure constrains but does not eradicate a tumor population, while selecting for less immunogenic variants. This is a tumor "dormancy" phase. Phase 3: Escape – Edited tumor variants, shaped by immune pressure, acquire mechanisms to evade immune destruction, leading to outgrowth and clinically apparent disease.
Experimental Validation of the Equilibrium Phase
The Equilibrium phase was the most novel and challenging to demonstrate.
Key Experimental Model: Dormancy & Escape in vivo Table 2: Key Equilibrium Phase Experiments
| Experimental System | Intervention | Quantitative Outcome | Implication |
|---|---|---|---|
| Immunoediting of MCA-induced Sarcomas (Koebel et al., 2007) | Transfer of "edited" Rag2-/- tumor cells into WT vs. Rag2-/- hosts. | Tumor growth only in Rag2-/- hosts; stable dormancy (>60 days) in WT hosts. | Demonstrated immunity enforces dormancy (Equilibrium) on edited tumors. |
| Interferon-γ Signaling in Equilibrium | Antibody-mediated blockade of IFN-γ in dormancy model. | Cessation of dormancy; tumor outgrowth. | Identified IFN-γ as a critical mediator of Equilibrium. |
Detailed Protocol: In vivo Tumor Dormancy & Escape Assay
- Generate "Edited" Tumors: Induce tumors in Rag2-/- mice using MCA. These tumors develop in the absence of adaptive immunity and are considered "unedited."
- Transplant into Immunocompetent Hosts: Surgically remove tumor, create single-cell suspension, and inject 10^5-10^6 viable cells subcutaneously into WT syngeneic mice.
- Monitor for Dormancy: Tumors may grow initially then regress (Elimination) or stabilize at a small, palpable size for >60 days (Equilibrium/Dormancy).
- Provoke Escape: In mice with dormant tumors, administer 500 µg of anti-IFN-γ neutralizing antibody (e.g., clone XMG1.2) intraperitoneally twice weekly for 2-3 weeks.
- Analysis: Measure tumor volume. Escape is defined as progressive growth following antibody treatment, confirming immune-mediated dormancy.
Molecular Mechanisms of Immune Escape
The Escape phase is driven by tumor-intrinsic and -extrinsic adaptations.
Diagram Title: Tumor Immune Escape Mechanisms
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Immunoediting Research
| Reagent / Material | Function / Application | Example (Specific Clone/Product) |
|---|---|---|
| Syngeneic Mouse Models | In vivo study of immunocompetent tumor-immune interactions. | C57BL/6 (B16 melanoma, MC38 colon carcinoma), BALB/c (CT26 colon carcinoma, 4T1 breast carcinoma). |
| Immunodeficient Mice | Assessing tumorigenesis in the absence of specific immune components. | Rag1-/- or Rag2-/- (no T/B cells), NSG (NOD-scid-IL2Rγnull, no adaptive + deficient innate immunity). |
| Anti-Mouse PD-1 / PD-L1 Antibody | Blockade of checkpoint to reverse T-cell exhaustion in Escape models. | InVivoPlus anti-mouse PD-1 (RMP1-14), anti-PD-L1 (10F.9G2). |
| Anti-Mouse IFN-γ Antibody | Neutralizing IFN-γ to disrupt Equilibrium and provoke Escape. | InVivoPlus anti-mouse IFN-γ (XMG1.2). |
| Recombinant Mouse IFN-γ | Stimulate tumor cell MHC expression; study signaling pathways in vitro. | PeproTech carrier-free recombinant cytokine. |
| Fluorochrome-conjugated MHC Tetramers | Ex vivo detection of antigen-specific T cells by flow cytometry. | Custom tetramers for model antigens (e.g., gp100, AH1). |
| LIVE/DEAD Fixable Viability Dyes | Distinguish live from dead cells in immune cell/tumor co-cultures. | Thermo Fisher Scientific Aqua or Near-IR Dead Cell Stains. |
| Cell Isolation Kits (Magnetic Beads) | Purify specific immune cell populations from tumors (TILs). | Miltenyi Biotec kits for CD8⁺ T cells, Tregs (CD4⁺CD25⁺), MDSCs. |
| Luminex Cytokine Assay Panels | Multiplex quantification of immunosuppressive/effector cytokines from tumor homogenates or serum. | R&D Systems or Bio-Rad mouse cytokine panels (TGF-β, IL-10, IL-6, IFN-γ, TNF-α). |
The evolution from Immune Surveillance to Immunoediting represents a paradigm shift in oncology. It provides the mechanistic rationale for immunotherapy: checkpoint blockade (reversing Escape), cancer vaccines (enhancing Elimination), and adoptive cell therapy (overcoming Escape). Current research focuses on targeting the Equilibrium phase to prevent progression, understanding neoantigen quality through editing, and identifying novel escape mechanisms to develop the next generation of immunotherapeutics. This framework is now the foundational thesis for understanding host-tumor immune dynamics.
Within the foundational thesis of Basic principles of cancer immunoediting and immune surveillance research, the process of cancer immunoediting is conceptualized as a dynamic triad of phases: Elimination, Equilibrium, and Escape. This framework describes the complex interaction between a developing tumor and the host immune system over time. This whitepaper provides an in-depth technical guide to the core mechanistic pillars defining each phase, serving as a critical reference for researchers, scientists, and drug development professionals aiming to develop novel immunotherapeutic strategies.
Core Mechanistic Pillars: A Phase-Wise Analysis
The Elimination Phase (Cancer Immunosurveillance)
The Elimination phase represents the body's innate and adaptive immune system successfully identifying and destroying nascent tumor cells.
Key Mechanistic Pillars:
- Innate Immune Activation: Recognition of tumor-associated molecular patterns (TAMPs) and damage-associated molecular patterns (DAMPs) via pattern recognition receptors (PRRs) on dendritic cells (DCs), macrophages, and NK cells. This leads to phagocytosis, cytokine release (e.g., type I IFNs, IL-12), and inflammation.
- Antigen Presentation and Priming: DCs phagocytose tumor debris, process tumor-associated antigens (TAAs), and present them via MHC-I and MHC-II to naïve CD8+ and CD4+ T cells in tumor-draining lymph nodes, respectively.
- Adaptive Effector Response: Primed CD8+ cytotoxic T lymphocytes (CTLs) infiltrate the tumor site, recognize TAAs presented on tumor cell MHC-I, and induce apoptosis via perforin/granzyme and FAS/FASL pathways. CD4+ T helper cells (particularly Th1) secrete IFN-γ to amplify CTL and macrophage activity.
- Immunogenic Cell Death (ICD): Successful killing via certain modalities (e.g., some chemotherapies, radiotherapy) further enhances antitumor immunity by releasing more DAMPs and TAAs, perpetuating the cycle.
Supporting Quantitative Data:
Table 1: Key Immune Metrics During Effective Elimination
| Metric | Typical Observation in Elimination | Primary Assay/Method |
|---|---|---|
| Intratumoral CD8+ T Cell Density | High (> 250 cells/mm²) | Immunohistochemistry (IHC), Flow Cytometry |
| CD8+/Treg Ratio | High (> 5:1) | Flow Cytometry, Multiplex IHC |
| IFN-γ Signature | Strongly Upregulated | RNA-seq, Nanostring, ELISA of tumor homogenate |
| Tumor Apoptosis Index | High (> 20%) | TUNEL Assay, Cleaved Caspase-3 IHC |
| Serum HMGB1 (DAMP) | Elevated | ELISA |
The Equilibrium Phase
Equilibrium describes a prolonged stalemate where the immune system controls but cannot fully eradicate tumor cells, applying a selective pressure that shapes tumor immunogenicity.
Key Mechanistic Pillars:
- T Cell Editing: Immune selection pressure leads to the outgrowth of tumor cell clones with reduced immunogenicity (e.g., loss of high-affinity TAAs).
- Adaptive Immune Resistance: Tumors upregulate inhibitory checkpoint ligands (e.g., PD-L1) in response to IFN-γ secreted by infiltrating T cells, creating an immunosuppressive microenvironment.
- Cellular Senescence & Dormancy: Immune cytokines (e.g., IFN-γ, TNF) can induce tumor cell senescence or dormancy, leading to a non-proliferative but viable state.
- Chronic Inflammation: A low-grade, smoldering inflammatory environment can paradoxically promote tumor survival and genomic instability.
Supporting Quantitative Data:
Table 2: Characteristics of the Tumor Microenvironment in Equilibrium
| Metric | Typical Observation in Equilibrium | Primary Assay/Method |
|---|---|---|
| Tumor Mutation Burden (TMB) | Evolving/Decreasing | Whole-exome sequencing |
| MHC-I Expression on Tumor Cells | Heterogeneous (Patchy Loss) | IHC for HLA-A,B,C |
| PD-L1 Expression | Inducible (IFN-γ dependent) | IHC, Flow Cytometry |
| T Cell Clonality | Restricted, Stable T Cell Receptor (TCR) repertoire | TCR sequencing (TCR-Seq) |
| Ki67 Index in Tumor Cells | Low to Moderate (< 10%) | IHC for Ki67 |
The Escape Phase
Escape occurs when tumor cell variants, shaped by immune pressure, acquire traits that allow them to circumvent immune destruction, leading to clinically apparent disease.
Key Mechanistic Pillars:
- Loss of Antigenicity: Complete downregulation or loss of MHC-I molecules, defects in antigen processing machinery (APM), or loss of TAAs.
- Creation of an Immunosuppressive Microenvironment: Recruitment of regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and tumor-associated macrophages (TAMs). Secretion of immunosuppressive cytokines (e.g., TGF-β, IL-10).
- Upregulation of Intrinsic Resistance: Constitutive expression of immune checkpoint ligands (PD-L1), activation of oncogenic pathways (e.g., WNT/β-catenin) that exclude T cells ("immune desert").
- Induction of T Cell Dysfunction: Chronic antigen exposure leads to T cell exhaustion, characterized by upregulation of multiple inhibitory receptors (e.g., PD-1, TIM-3, LAG-3) and loss of effector function.
Supporting Quantitative Data:
Table 3: Hallmarks of the Escape Phase Tumor Microenvironment
| Metric | Typical Observation in Escape | Primary Assay/Method |
|---|---|---|
| Treg or MDSC Infiltration | High (> 20% of CD45+ cells) | Flow Cytometry (FoxP3+CD4+; CD11b+Gr1+) |
| T Cell Exclusion Signature | Present | RNA-seq Gene Signature (e.g., β-catenin) |
| Exhausted T Cell Phenotype | PD-1^hi TIM-3^hi LAG-3^hi | High-parameter Flow Cytometry |
| MHC-I Loss | Complete or near-complete loss | IHC for HLA-A,B,C & β2-microglobulin |
| Lactate & Hypoxia | High | Biochemical assay, HIF-1α IHC |
Experimental Protocols for Phase Investigation
Protocol 1: Longitudinal Tumor Modeling for Immunoediting Study
- Objective: To observe all three phases in vivo.
- Model: Immunocompetent mouse (e.g., C57BL/6) injected with a syngeneic, immunogenic tumor cell line (e.g., MC38, MCA205).
- Method:
- Inject 1x10^5 to 5x10^5 cells subcutaneously.
- Monitor tumor volume by caliper measurement every 2-3 days.
- Elimination Cohort: Sacrifice mice at day 7-10, analyze tumors by flow cytometry for CD8+/Treg ratio, IFN-γ+ T cells, and perform RNA-seq.
- Equilibrium Cohort: Isolate and culture tumor cells from a regressing tumor. Re-inject into a new cohort. Some tumors may enter equilibrium (dormant). Serially transplant small tumor fragments over multiple generations to model immunoediting.
- Escape Cohort: Identify a progressively growing tumor from the equilibrium cohort. Characterize its phenotype (MHC-I, PD-L1) and microenvironment compared to the parental line.
- Key Readouts: Tumor growth kinetics, immune profiling, tumor genome sequencing across generations.
Protocol 2: In Vitro T Cell Killing Assay with Immune Editing Pressure
- Objective: To model T cell-mediated selection of tumor escape variants.
- Method:
- Co-culture a heterogeneous tumor cell population (e.g., CRISPR-modified pool with varying MHC-I expression) with tumor-antigen-specific CTLs at a 1:1 to 1:5 (tumor:T cell) ratio.
- Repeat cycles of co-culture (48-72 hrs) and recovery of surviving tumor cells.
- After 5-10 cycles, isolate surviving tumor cell clones.
- Genotype/phenotype clones for MHC-I expression, PD-L1 expression, and mutations in antigen presentation pathways (e.g., B2M).
- Key Readouts: Survival of tumor clones over cycles, phenotypic shift towards immune evasion traits.
Visualization of Core Pathways and Workflows
Title: Core Immune Pathway in Elimination Phase
Title: Selective Pressure Drives Equilibrium
Title: Mechanisms of Immune Escape in Tumors
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Cancer Immunoediting Research
| Reagent/Material | Primary Function | Example Application |
|---|---|---|
| Syngeneic Mouse Tumor Cell Lines (e.g., MC38, B16, 4T1) | Provide immunocompetent in vivo models to study host-tumor immune interactions. | Longitudinal tumor growth studies, immunotherapy efficacy testing. |
| Immune Checkpoint Blocking Antibodies (anti-PD-1, anti-CTLA-4, anti-PD-L1) | Inhibit ligand/receptor interactions to reverse T cell exhaustion. | Studying equilibrium/escape mechanisms; positive control in therapy experiments. |
| Fluorochrome-Conjugated Antibody Panels for Flow Cytometry | Multiplexed identification and phenotyping of immune cell subsets. | Profiling tumor-infiltrating lymphocytes (TILs) for CD8, CD4, Treg, exhaustion markers. |
| Cytokine ELISA or Luminex Kits | Quantification of soluble immune mediators. | Measuring IFN-γ, TGF-β, IL-10 levels in serum or tumor homogenate. |
| MHC-I / PD-L1 Antibodies for IHC | Spatial visualization of protein expression in tumor tissue. | Assessing antigen presentation and adaptive resistance in tumor cells. |
| TCR Sequencing Kit | Analysis of T cell receptor diversity and clonality. | Tracking T cell repertoire evolution from equilibrium to escape. |
| CRISPR-Cas9 Gene Editing System | Targeted knockout of genes in tumor or immune cells. | Functional validation of escape mechanisms (e.g., B2M KO for MHC-I loss). |
| IFN-γ Recombinant Protein & Neutralizing Antibody | To modulate IFN-γ signaling pathway in vitro or in vivo. | Testing the role of IFN-γ in inducing PD-L1 or editing tumor immunogenicity. |
Within the framework of cancer immunoediting—comprising the three phases of elimination, equilibrium, and escape—immune surveillance is executed by a complex network of cellular and molecular entities. This whitepaper provides an in-depth technical analysis of the core effector cells, cytokines, and immune checkpoint pathways that underpin this dynamic process. Understanding these players is critical for developing novel immunotherapeutic strategies in oncology.
Effector Cells in Immune Surveillance
Effector cells are the armed lymphocytes that directly recognize and destroy cancer cells.
CD8+ Cytotoxic T Lymphocytes (CTLs)
CTLs are the primary killers of antigen-expressing tumor cells.
- Mechanism: Upon T-cell receptor (TCR) engagement with peptide-MHC Class I complexes, CTLs release perforin and granzymes to induce target cell apoptosis. They also express Fas ligand (FasL) to engage death receptors.
- Key Markers: CD3ε, CD8αβ, TCRαβ, Granzyme B, Perforin.
CD4+ T Helper (Th) Cells
Th cells provide essential licensing signals for innate and adaptive immunity.
- Subsets:
- Th1: Secrete IFN-γ and IL-2, promoting CTL and macrophage activation.
- Th2: Secrete IL-4, IL-5, IL-13; generally associated with humoral immunity and can be pro-tumorigenic.
- Th17: Secrete IL-17, promoting inflammation; dual roles in tumor immunity.
- T follicular helper (Tfh): Aid B cell responses in tertiary lymphoid structures.
- Regulatory T Cells (Tregs): A specialized CD4+ subset (Foxp3+) that suppresses effector responses, crucial for maintaining self-tolerance but a major barrier to anti-tumor immunity.
Natural Killer (NK) Cells
Innate lymphocytes that kill target cells lacking MHC Class I ("missing-self" recognition) or expressing stress-induced ligands.
- Activation Receptors: NKG2D (binds MICA/B, ULBP), Natural Cytotoxicity Receptors (e.g., NKp46).
- Inhibitory Receptors: Killer-cell Immunoglobulin-like Receptors (KIRs), CD94/NKG2A (binds HLA-E).
Other Myeloid Effectors
- M1 Macrophages: Pro-inflammatory, anti-tumor; secrete IL-12, TNF-α, and reactive nitrogen/oxygen species.
- Dendritic Cells (DCs): Professional antigen-presenting cells (APCs) critical for priming naive T cells. Cross-presenting DCs (cDC1 subset) are essential for CTL responses.
Table 1: Key Effector Cell Types and Functions
| Cell Type | Primary Surface Markers | Key Effector Molecules | Primary Anti-Tumor Function |
|---|---|---|---|
| CD8+ CTL | CD3, CD8, TCR | Perforin, Granzymes, IFN-γ, FasL | Direct cytotoxicity, apoptosis induction |
| Th1 Cell | CD3, CD4, CXCR3, T-bet | IFN-γ, IL-2, TNF-α | Activate CTLs/Macrophages, promote cellular immunity |
| Treg | CD3, CD4, CD25, Foxp3 | IL-10, TGF-β, IL-35 | Immune suppression, maintain tolerance |
| NK Cell | CD56, CD16 (human), NK1.1 (mouse) | Perforin, Granzymes, IFN-γ | Direct cytotoxicity (MHC-I independent), ADCC |
| cDC1 | CD11c, XCR1, Clec9A (DNGR-1) | IL-12, Cross-presented antigen | Cross-priming of CD8+ T cells |
Cytokine Networks
Cytokines are soluble signaling proteins that mediate communication between immune cells.
Pro-Inflammatory, Anti-Tumor Cytokines
- Interferon-gamma (IFN-γ): Master regulator of anti-tumor immunity. Upregulates MHC expression, promotes Th1 differentiation, activates macrophages, and has direct anti-proliferative effects on tumors.
- Interleukin-12 (IL-12): Produced by activated APCs; induces IFN-γ production from T and NK cells, promotes Th1/CTL differentiation.
- Tumor Necrosis Factor-alpha (TNF-α): Can directly induce tumor cell apoptosis and promote inflammatory cell infiltration.
Immunosuppressive, Pro-Tumorigenic Cytokines
- Transforming Growth Factor-beta (TGF-β): Potently inhibits CTL and NK cell function; promotes Treg differentiation and epithelial-to-mesenchymal transition (EMT) in tumors.
- Interleukin-10 (IL-10): Suppresses APC function and pro-inflammatory cytokine production; often produced by Tregs and tumor-associated macrophages (TAMs).
Table 2: Major Cytokines in Cancer Immunoediting
| Cytokine | Primary Cellular Source | Major Receptor | Net Effect in Immunoediting |
|---|---|---|---|
| IFN-γ | CTLs, Th1, NK cells | IFNGR1/IFNGR2 | Anti-Tumor: Promotes elimination via MHC upregulation, effector activation. Can drive immunoediting. |
| IL-2 | Activated T cells | CD25 (IL-2Rα)/IL-2Rβ/γc | Dual: Expands effector T cells at high dose; critical for Treg homeostasis at low dose. |
| IL-12 | Activated DCs, Macrophages | IL-12Rβ1/IL-12Rβ2 | Anti-Tumor: Drives Th1/CTL/NK cell IFN-γ production. |
| TGF-β | Tregs, Stromal cells, Cancer cells | TGFBRII/TGFBRI | Pro-Tumor: Drives escape via suppression of effectors, promoting Tregs and EMT. |
| IL-10 | Tregs, M2 Macrophages, Bregs | IL-10RA/IL-10RB | Pro-Tumor: Suppresses APC function, inhibits inflammation, promotes tolerance. |
| IL-6 | Myeloid cells, Fibroblasts | IL-6R/gp130 | Dual: Can promote acute inflammation but is often associated with chronic pro-tumorigenic signaling. |
Immune Checkpoint Pathways
Checkpoint pathways are regulatory circuits that modulate immune response amplitude and duration. Tumors co-opt inhibitory checkpoints to facilitate immune escape.
Inhibitory Checkpoints (Immune "Brakes")
- PD-1/PD-L1 Axis: PD-1 on activated T cells engages PD-L1 (or PD-L2) on tumors/APCs, delivering an inhibitory signal that suppresses TCR signaling, cytokine production, and cytotoxicity.
- CTLA-4/CD80/CD86 Axis: CTLA-4 on T cells outcompetes CD28 for binding to B7 ligands (CD80/86) on APCs, delivering a potent inhibitory signal primarily during T cell priming in lymph nodes.
- Other Key Inhibitory Pathways: LAG-3/MHC-II, TIM-3/Galectin-9, TIGIT/CD155.
Costimulatory Pathways (Immune "Accelerators")
- CD28/CD80/CD86: The primary signal 2 for naive T cell activation.
- 4-1BB (CD137)/4-1BBL: Enhances T cell survival, proliferation, and effector function upon TCR engagement.
- OX40 (CD134)/OX40L: Promotes T cell expansion, survival, and cytokine production.
Diagram 1: T Cell Activation and Checkpoint Pathways
Experimental Protocols for Key Assays
Protocol: In Vitro Cytotoxic T Lymphocyte (CTL) Killing Assay
Purpose: Quantify the ability of antigen-specific CD8+ T cells to kill labeled target cells. Materials: See Scientist's Toolkit below. Method:
- Target Cell Preparation: Harvest tumor cells (e.g., B16-OVA, MC38). Label with 5-10 μM CFSE (CFSE
hipopulation) for 10 min at 37°C. Quench with complete media. For control "feeder" cells, label a separate aliquot with a low concentration of CFSE (0.5-1 μM; CFSElopopulation). - Effector Cell Preparation: Isolate CD8+ T cells from immunized mice or an in vitro priming culture using a negative selection magnetic bead kit.
- Co-culture: Mix CFSE
hitarget cells and CFSElofeeder cells at a 1:1 ratio. Plate in a 96-well U-bottom plate. Add effector CTLs at varying Effector:Target (E:T) ratios (e.g., 40:1, 20:1, 10:1, 5:1). Include target-only and effector-only controls. - Incubation: Culture for 4-6 hours at 37°C, 5% CO₂.
- Staining & Analysis: Add a viability dye (e.g., DAPI or 7-AAD) to distinguish live/dead cells. Acquire on a flow cytometer. Gate on CFSE
hitarget cells and calculate specific lysis:% Specific Lysis = (1 - (% Viable Targets in Test / % Viable Targets in Target-only Control)) * 100.
Protocol: Multiplex Cytokine Analysis (Luminex)
Purpose: Simultaneously quantify multiple cytokines from serum or cell culture supernatant. Method:
- Sample Prep: Centrifuge samples to remove debris. Store at -80°C if not used immediately.
- Assay Setup: Using a commercial multiplex panel (e.g., 25-plex mouse cytokine panel), prepare antibody-conjugated magnetic bead mixtures, standards, and controls per manufacturer's protocol.
- Incubation: Add 50 μL of sample/standard to a 96-well filter plate containing the bead mix. Incubate for 2h on a plate shaker.
- Detection: Wash beads, then add biotinylated detection antibody mixture. Incubate for 1h. Wash, then add Streptavidin-PE. Incubate for 30 min.
- Reading: Wash, resuspend beads in reading buffer, and analyze on a Luminex MAGPIX or FLEXMAP 3D instrument.
- Analysis: Use instrument software with a 5-parameter logistic (5PL) curve fit to calculate cytokine concentrations from standard curves.
Protocol: Immune Checkpoint Blockade In Vivo
Purpose: Evaluate therapeutic efficacy of anti-PD-1/CTLA-4 antibodies in a syngeneic mouse tumor model. Method:
- Tumor Engraftment: Subcutaneously inject 5x10⁵ to 1x10⁶ syngeneic tumor cells (e.g., CT26 colon carcinoma, MC38 colon adenocarcinoma) into the right flank of 6-8 week old C57BL/6 or BALB/c mice.
- Randomization: When tumors reach ~50-100 mm³ (typically 7-10 days post-injection), measure tumors with calipers and randomize mice into treatment groups (n=5-10) with similar average tumor volumes.
- Treatment: Administer via intraperitoneal (i.p.) injection:
- Isotype Control Group: Rat IgG2a/k isotype, 200 μg/dose, Q3-4 days.
- Anti-PD-1 Group: Clone RMP1-14, 200 μg/dose, Q3-4 days.
- Anti-CTLA-4 Group: Clone 9D9, 100 μg/dose, Q3-4 days.
- Combination Group: Both antibodies at above doses.
- Monitoring: Measure tumor dimensions 2-3 times weekly. Calculate volume:
(length x width²)/2. Monitor mouse body weight and health. Endpoint is typically when control group tumors reach a volume of 1500-2000 mm³ or ulcerate. - Analysis: Plot tumor growth curves. Perform statistical analysis (e.g., two-way ANOVA) at study endpoint. For immune profiling, harvest tumors at an early timepoint (e.g., after 2 doses) for flow cytometry analysis of TILs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials
| Reagent/Material | Supplier Examples | Key Function in Research |
|---|---|---|
| Fluorochrome-conjugated Antibodies | BioLegend, BD Biosciences, Thermo Fisher | Multiparameter flow cytometry phenotyping of immune cells (e.g., CD3, CD4, CD8, CD45, Foxp3). |
| Recombinant Cytokines (Murine/Human) | PeproTech, R&D Systems | In vitro polarization/differentiation of T cell subsets (e.g., IL-2, IL-12, TGF-β), cell culture supplementation. |
| Immune Checkpoint Modulating Antibodies (In Vivo Grade) | Bio X Cell, InvivoGen | Functional blockade (αPD-1, αCTLA-4) or agonism (α4-1BB, αOX40) in preclinical mouse models. |
| Magnetic Cell Isolation Kits | Miltenyi Biotec, STEMCELL Technologies | Negative/positive selection of specific cell populations (e.g., CD8+ T cells, NK cells) from spleen/tumor with high purity. |
| Luminex Multiplex Assay Kits | Thermo Fisher, R&D Systems, MilliporeSigma | High-throughput, simultaneous quantification of multiple cytokines/chemokines from serum or supernatant. |
| Cell Trace Proliferation Dyes (CFSE, CellTrace Violet) | Thermo Fisher | Label cells to track division history and proliferation dynamics via flow cytometry. |
| Syngeneic Mouse Tumor Cell Lines | ATCC, Kerafast | Preclinical models with intact immune systems (e.g., B16-F10 (melanoma), MC38 (colon), 4T1 (breast)). |
| Foxp3 / Transcription Factor Staining Buffer Set | Thermo Fisher, BioLegend | Permeabilization buffers required for intracellular staining of transcription factors and cytokines (IFN-γ, Granzyme B). |
Diagram 2: Tumor-Infiltrating Lymphocyte (TIL) Analysis Workflow
The Role of Tumor Mutational Burden (TMB) and Neoantigen Generation in Immune Recognition
This whitepaper explores the critical roles of Tumor Mutational Burden (TMB) and neoantigen generation within the established framework of cancer immunoediting. The immunoediting hypothesis, encompassing the three phases of elimination, equilibrium, and escape, provides the foundational context for understanding how somatic mutations are processed into immune targets and how this process ultimately dictates clinical outcomes.
The concept that the immune system patrols for and eliminates nascent transformed cells, termed immunosurveillance, has evolved into the more comprehensive paradigm of cancer immunoediting. This dynamic process consists of:
- Elimination: The immune system successfully identifies and destroys tumor cells.
- Equilibrium: A state of functional dormancy where immune control contains but does not eradicate the tumor.
- Escape: Tumor cells evolve mechanisms to evade immune destruction, leading to clinical disease.
TMB and neoantigen generation are central determinants of whether a tumor is eliminated or progresses to escape. High TMB increases the statistical probability of generating immunogenic neoantigens—novel peptides derived from somatic mutations that are presented on Major Histocompatibility Complex (MHC) molecules and recognized as non-self by T cells.
Technical Guide: Quantifying TMB and Neoantigen Load
Tumor Mutational Burden (TMB) Measurement
TMB is defined as the total number of somatic, coding, base substitution, and indel mutations per megabase (mut/Mb) of genome examined. Standardized measurement is critical for its use as a predictive biomarker.
Experimental Protocol for TMB Assessment via Whole Exome Sequencing (WES):
- Sample Preparation: Matched tumor and normal (e.g., blood or adjacent tissue) DNA extraction.
- Library Preparation & Sequencing: Whole exome capture using a commercial kit (e.g., IDT xGen Exome Research Panel, Agilent SureSelect) followed by high-throughput sequencing (Illumina NovaSeq) to a minimum coverage of 100x for tumor and 60x for normal.
- Bioinformatic Pipeline:
- Alignment: Map sequence reads to a reference genome (e.g., GRCh38) using BWA-MEM or STAR.
- Variant Calling: Identify somatic mutations using paired tumor-normal pipelines (MuTect2 for SNVs, Strelka for indels).
- Filtering: Remove known germline variants (using dbSNP, gnomAD), sequencing artifacts, and variants in low-complexity regions.
- TMB Calculation:
TMB (mut/Mb) = (Total number of passing somatic mutations) / (Size of the captured coding region in Mb)
Table 1: TMB Classification Across Cancer Types
| Cancer Type | Typical TMB Range (mut/Mb) | Threshold for "High TMB" (Commonly Used) |
|---|---|---|
| Melanoma | 5 - 50+ | ≥ 10 mut/Mb |
| Lung (NSCLC) | 5 - 20+ | ≥ 10 mut/Mb |
| Colorectal (MSI-H) | 20 - 80+ | ≥ 10 mut/Mb |
| Glioblastoma | 0.5 - 5 | ≥ 10 mut/Mb |
| Prostate | 0.5 - 4 | ≥ 10 mut/Mb |
Neoantigen Prediction and Validation
Not all mutations generate neoantigens. The immunogenic potential of a mutation depends on its successful processing and presentation.
Experimental Protocol for In Silico Neoantigen Prediction:
- Input: List of somatic mutations (VCF file).
- Step 1 - Epitope Prediction: Use algorithms (NetMHCpan, MHCflurry) to predict mutant peptide binding affinity to patient-specific MHC Class I alleles (determined via HLA typing from normal DNA).
- Step 2 - Filtering: Retain peptides with strong binding affinity (IC50 < 50 nM or %Rank < 0.5).
- Step 3 - Confirmatory Assays:
- Mass Spectrometry: Immunopeptidomics to physically confirm MHC presentation of the mutant peptide.
- Functional Validation: In vitro co-culture of patient T-cells with antigen-presenting cells pulsed with the candidate neoantigen peptide to assess T-cell activation (IFN-γ ELISpot) and cytotoxicity.
Table 2: Key Steps and Outputs in Neoantigen Prediction Workflow
| Step | Primary Tool/Method | Key Output | Success Criteria |
|---|---|---|---|
| HLA Typing | OptiType, Polysolver | Patient's MHC Class I alleles | High-confidence allele calls |
| Peptide Generation | pVACtools | 8-11mer mutant peptides | All possible mutant peptides |
| Binding Prediction | NetMHCpan 4.1 | Predicted binding affinity (nM) | IC50 < 50 nM |
| Immunogenicity | NetCTL, DeepImmuno | Predicted T-cell recognition score | High probability score |
| Experimental Validation | IFN-γ ELISpot | Spot-forming units (SFU) | Significant SFU vs. wild-type |
Mechanisms and Signaling Pathways
The recognition of neoantigens is the culmination of the cancer-immunity cycle. The following diagram illustrates the core pathway from mutation to immune-mediated killing.
Diagram 1: Neoantigen-Driven Immune Elimination
Table 3: Key Research Reagent Solutions for TMB/Neoantigen Studies
| Item/Category | Example Product/Source | Function in Research |
|---|---|---|
| Exome Capture Kits | Agilent SureSelect Human All Exon V7, IDT xGen Exome Research Panel v2 | Enrichment of coding genomic regions for efficient sequencing of the exome. |
| HLA Typing Assay | Illumina TruSight HLA v2, SeCore HLA Sequencing Kits | High-resolution determination of patient-specific MHC alleles for accurate neoantigen prediction. |
| Peptide Synthesis | Custom peptide synthesis services (e.g., GenScript, Peptide 2.0) | Production of predicted mutant and wild-type peptides for in vitro validation assays. |
| T-Cell Functional Assay | IFN-γ ELISpot Kit (e.g., Mabtech, BD Biosciences) | Quantification of antigen-specific T-cell responses by measuring cytokine secretion. |
| pMHC Multimers | Tetramer/Dextramer synthesis (e.g., Immudex, MBL) | Direct staining and isolation of neoantigen-specific T-cell clones from patient samples. |
| Immunopeptidomics | Anti-MHC Class I Immunoaffinity Columns (e.g., BioLegend) | Isolation of MHC-presented peptides for mass spectrometry-based identification of neoantigens. |
Clinical Implications and Drug Development
High TMB has emerged as a robust, pan-cancer biomarker predicting response to immune checkpoint inhibitors (ICIs). Tumors with high TMB are more likely to contain neoantigens that make them visible to the immune system, and ICIs (anti-PD-1, anti-CTLA-4) release the brakes on these primed T-cells. This underpins the FDA approval of pembrolizumab for any unresectable or metastatic solid tumor with TMB-H (≥10 mut/Mb).
Current drug development strategies leveraging these principles include:
- Personalized Neoantigen Vaccines: Administering patient-specific neoantigen peptides or mRNA to boost pre-existing immune responses.
- Targeting Low TMB Tumors: Combining radiotherapy or targeted therapies with ICIs to increase mutational load or neoantigen presentation ("immunogenic modulation").
- Adoptive Cell Therapy (ACT): Engineering patient T-cells to express TCRs specific for validated neoantigens.
Within the framework of cancer immunoediting, TMB serves as a quantifiable genomic metric that proxies for the likelihood of neoantigen generation. The resulting neoantigens are the key targets driving the elimination phase. Their successful recognition by T-cells dictates whether a tumor is controlled or evolves into escape. Continued refinement in measuring TMB, predicting immunogenic neoantigens, and therapeutically targeting this axis remains a central focus in translational oncology, bridging fundamental principles of immune surveillance with precision medicine.
Tools of the Trade: Methodologies for Studying Immunoediting and Translational Applications
This technical guide explores three principal murine model systems—genetically engineered, carcinogen-induced, and syngeneic models—within the context of cancer immunoediting and immune surveillance research. These models are foundational for dissecting the dynamic interplay between tumors and the immune system through its three phases: elimination, equilibrium, and escape.
Genetically Engineered Mouse Models (GEMMs)
GEMMs involve germline or somatic manipulation of specific oncogenes or tumor suppressor genes to recapitulate spontaneous tumorigenesis within an intact immune system.
Key Applications in Immunoediting
- Study of neoantigen emergence and immunogenicity.
- Investigation of the equilibrium phase in autochthonous settings.
- Analysis of cell-intrinsic and -extrinsic immune escape mechanisms.
Core Protocols and Examples
Protocol: Generation of a Conditional Knockout/Oncogene GEMM (e.g., KrasLSL-G12D/+; Trp53fl/fl Lung Adenocarcinoma Model)
- Genetic Design: Utilize Cre-loxP system. Lox-Stop-Lox (LSL) cassette precedes the mutant KrasG12D allele. Trp53 alleles are floxed.
- Mouse Breeding: Cross KrasLSL-G12D/+ mice with Trp53fl/fl mice and a tissue-specific Cre driver line (e.g., Ad5-Cre for lung).
- Tumor Initiation: Administer Cre (e.g., via intranasal adenoviral-Cre delivery) to locally excise the STOP cassette and Trp53 floxed exons, initiating tumorigenesis.
- Monitoring: Track tumor burden via in vivo imaging (e.g., micro-CT) and monitor immune infiltrates by flow cytometry of digested tumors at serial timepoints.
Quantitative Data Summary: Common GEMMs in Immunoediting Research
| Model Name (Common Abbreviation) | Genetic Alteration | Primary Tumor Type | Median Latency (Weeks) | Key Immune Features Studied |
|---|---|---|---|---|
| KrasLSL-G12D/+;Trp53fl/fl (KP) | Inducible KRAS G12D; p53 loss | Lung Adenocarcinoma | 10-16 | T-cell exhaustion, myeloid suppressive cells |
| BrafV600E;Tyr-CreERT2 | Inducible BRAF V600E | Melanoma | 4-8 | Role of CD8+ T-cells in equilibrium |
| ApcMin/+ | Germline APC truncation | Intestinal Adenomas | 12-20 | Immunoprevention, cytokine roles |
Carcinogen-Induced Models
These models use chemical or physical agents to initiate tumors, generating a heterogeneous tumor microenvironment (TME) with a high mutational burden.
Key Applications in Immunoediting
- Modeling immunosurveillance against neoantigen-rich tumors.
- Studying the impact of mutational load on immune recognition.
- Testing immunopreventive strategies.
Core Protocols
Protocol: Induction of Colorectal Tumors using Azoxymethane (AOM)/Dextran Sulfate Sodium (DSS)
- Mouse Strain: Use immunocompetent strains (e.g., C57BL/6).
- Initiation: Inject AOM (10 mg/kg, i.p.) once.
- Promotion: Administer 1-3 cycles of DSS (2-3% w/v in drinking water) for 5-7 days, followed by recovery periods.
- Monitoring: Track weight loss, occult blood, and colon inflammation. Sacrifice at endpoint (e.g., 12 weeks) for tumor multiplicity and size analysis. Immune profiling via IHC of colon sections (CD3, CD8, FoxP3).
Syngeneic Murine Tumor Models
These models involve implanting murine tumor cell lines into genetically identical (syngeneic) hosts. They are a cornerstone for testing immunotherapies.
Key Applications in Immunoediting
- High-throughput screening of immunotherapy agents.
- Mechanistic dissection of specific immune cell subsets via depletion/blockade.
- Studying therapy-induced changes in the TME.
Core Protocols
Protocol: Subcutaneous Implantation and Immunotherapy Treatment
- Cell Preparation: Culture syngeneic cell line (e.g., MC38, CT26, B16F10). Harvest in log phase, wash, and resuspend in PBS/Matrigel.
- Implantation: Inject 0.5-1x10^6 cells subcutaneously into the flank of mice (e.g., C57BL/6 for MC38, BALB/c for CT26).
- Randomization & Treatment: When tumors reach ~50-100 mm³, randomize mice into cohorts. Administer therapy (e.g., anti-PD-1, 200 µg, i.p., twice weekly).
- Endpoint Analysis: Monitor tumor volume (caliper measurement: V = (length x width²)/2) and survival. Analyze tumors by flow cytometry for immune infiltrates.
Quantitative Data Summary: Common Syngeneic Models
| Tumor Cell Line | Host Strain | Tumor Type | Immunogenicity | Typical Response to anti-PD-1/CTLA-4 |
|---|---|---|---|---|
| MC38 | C57BL/6 | Colon Adenocarcinoma | High | Strong, durable response |
| CT26 | BALB/c | Colon Carcinoma | Moderate | Responsive |
| B16F10 | C57BL/6 | Melanoma | Low (Cold Tumor) | Poor response, requires combo |
| 4T1 | BALB/c | Breast Carcinoma | Low (Immunosuppressive) | Poor response |
| RENCA | BALB/c | Renal Cell Carcinoma | Moderate | Moderately responsive |
The Scientist's Toolkit: Essential Reagents
| Reagent/Material | Function in Model Research |
|---|---|
| Cre Recombinase (Adenoviral, Lentiviral) | Activates conditional alleles in GEMMs in a tissue-specific manner. |
| Tamoxifen | Induces CreERT2 activity for temporally controlled genetic recombination in GEMMs. |
| Azoxymethane (AOM) | DNA alkylating agent used to initiate colorectal tumors in carcinogen models. |
| Dextran Sulfate Sodium (DSS) | Colitis-inducing agent used to promote tumorigenesis in AOM/DSS models. |
| Matrigel Basement Membrane Matrix | Extracellular matrix hydrogel used to enhance syngeneic tumor cell engraftment. |
| InVivoMab anti-mouse PD-1 (CD279) | Immune checkpoint blocking antibody for therapy studies in syngeneic models. |
| Collagenase IV/DNase I Digestion Cocktail | Enzymatic mixture for dissociating solid tumors into single-cell suspensions for flow cytometry. |
| Fluorochrome-conjugated Antibodies (CD45, CD3, CD8, CD4, FoxP3, etc.) | Essential for immunophenotyping tumor-infiltrating leukocytes via flow cytometry. |
| In Vivo Imaging System (IVIS) / Micro-CT | For non-invasive longitudinal monitoring of tumor burden, especially in orthotopic or GEMMs. |
Visualizing the Cancer Immunoediting Workflow in Murine Models
Title: Murine Models in Cancer Immunoediting Phases
Visualizing a Key Signaling Pathway in Tumor-Immune Crosstalk
Title: PD-1/PD-L1 Checkpoint Pathway in Immunotherapy
Advanced Humanized Mouse Models and Ex Vivo Co-Culture Systems for Translational Research
The principles of cancer immunoediting—encompassing the three phases of elimination, equilibrium, and escape—provide the fundamental framework for understanding tumor-immune system interactions. Translational research aimed at exploiting immune surveillance and overcoming immune escape requires sophisticated platforms that accurately recapitulate the human immune system and tumor microenvironment (TME). Advanced humanized mouse models and ex vivo co-culture systems have emerged as indispensable tools for dissecting these mechanisms and evaluating novel immunotherapies.
Part 1: Advanced Humanized Mouse Models
Humanized mice are generated by engrafting human hematopoietic stem cells (HSCs) and/or tissues into immunodeficient mice, creating a chimeric model with a functional human immune system.
Model Classification and Quantitative Comparison
The evolution of immunodeficient host strains has dramatically improved human cell engraftment and functionality. Key genetically modified strains include NSG (NOD-scid IL2Rγnull), NOG (NOD-shiscid IL2Rγnull), and more recently, strains expressing human cytokines.
Table 1: Comparison of Common Immunodeficient Mouse Strains for Humanization
| Strain (Common Name) | Key Genetic Modifications | Average Human CD45+ Engraftment (at 12-16 weeks) | Key Human Immune Cell Populations Present | Common Use Cases |
|---|---|---|---|---|
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) | Prkdcscid, Il2rgnull | 60-80% in periphery | T, B, NK, Myeloid cells | Baseline HSC engraftment, PDX co-engraftment |
| NOG (NOD/Shi-scid Il2rgnull) | Prkdcscid, Il2rgnull (Shionogi allele) | 70-85% in periphery | T, B, NK, Myeloid cells | Similar to NSG, often used in Japan/EU |
| NSG-SGM3 (NSG Il3/GM-CSF/SF) | Il2rgnull, expresses human SCF, GM-CSF, IL-3 | >80% in periphery | Enhanced myeloid & granulocyte development | AML, myeloid-targeted therapies, antigen presentation studies |
| BRGS (BALB/c Rag2-/- Il2rg-/- SIRPαNOD) | Rag2null, Il2rgnull, human SIRPα polymorphism | 50-70% in periphery | Improved macrophage function, lower anaphylaxis risk | Monoclonal antibody therapy, macrophage engagement |
| MISTRG (Rag2-/-Il2rg-/- with human M-CSF, IL-3, GM-CSF, TPO knock-ins) | Multiple human cytokine knock-ins in endogenous loci | >80% in bone marrow & periphery | Robust human innate immunity (macrophages, NK cells) | Innate immune cell function, tumor microenvironment modeling |
Protocol: Generation of CD34+ HSC-Engrafted Humanized Mice (Hu-CD34+ NSG)
Objective: To create a humanized mouse model with a multilineage human immune system for studying immune surveillance and immunotherapy.
Materials & Reagents:
- Immunodeficient mice (e.g., NSG, 6-8 weeks old).
- Purified human CD34+ hematopoietic stem cells (from cord blood, fetal liver, or mobilized peripheral blood).
- Sublethal irradiation source (e.g., X-ray or γ-irradiator).
- Anti-mouse CD122 antibody (for NK cell depletion, optional).
- Matrigel (for intra-bone marrow injection, optional).
- Flow cytometry antibodies: anti-human CD45, CD3, CD19, CD33, CD56.
Detailed Methodology:
- Host Preparation: Irradiate recipient NSG mice with a sublethal dose (1-1.5 Gy). 24 hours prior to transplantation, administer an intraperitoneal (i.p.) injection of anti-mouse CD122 antibody (0.25 mg per mouse) to deplete residual mouse NK cells.
- Cell Preparation: Thaw and viability-check human CD34+ cells. Resuspend in PBS at a concentration of 1-5 x 105 cells per 20 µL for intrahepatic injection (newborns) or 1-2 x 105 cells per 30 µL PBS for intravenous (tail vein) or intra-femoral injection (adults).
- Engraftment: For adult mice, inject cells via tail vein or directly into the femoral bone marrow cavity. For maximum engraftment efficiency, intra-bone marrow injection is preferred.
- Monitoring: At 12-16 weeks post-transplant, collect peripheral blood (50-100 µL) via retro-orbital or submandibular bleed. Lyse red blood cells and stain with anti-human CD45 antibody. Successful humanization is typically defined as >25% human CD45+ cells in peripheral blood leukocytes.
- Immune Profiling: Sacrifice a subset of mice. Analyze bone marrow, spleen, and thymus by flow cytometry using lineage-specific antibodies (CD3 for T cells, CD19 for B cells, CD33 for myeloid cells, CD56 for NK cells) to assess multi-lineage reconstitution.
Tumor Engraftment in Humanized Mice: Modeling the Equilibrium and Escape Phases
To study immunoediting, human tumors are introduced into the established human immune system.
Protocol: Patient-Derived Xenograft (PDX) Co-Engraftment
- Humanized Host: Use Hu-CD34+ NSG or NSG-SGM3 mice at >16 weeks post-HSC transplant, with confirmed human immune reconstitution.
- Tumor Implantation: Implant a small fragment (~1-2 mm³) of a patient-derived tumor (PDX) subcutaneously or orthotopically. Alternatively, inject 0.5-2 x 10⁶ human tumor cell lines.
- Monitoring & Treatment: Monitor tumor volume with calipers. When tumors reach ~100 mm³, randomize mice into treatment groups (e.g., anti-PD-1, CAR-T cells, bispecific antibodies). Monitor tumor growth and survival.
- Endpoint Analysis: Harvest tumors and lymphoid organs. Use flow cytometry, immunohistochemistry (IHC), and cytokine profiling to analyze tumor-infiltrating human lymphocytes (TILs), immune checkpoint expression, and changes in the TME, providing direct insight into immune escape mechanisms.
Part 2: Ex Vivo Co-Culture Systems
These systems provide a reductionist, highly controlled platform to dissect specific cellular interactions within the TME, complementary to in vivo models.
3D Co-Culture Systems: Modeling the Tumor Niche
Protocol: Tumor Organoid - Immune Cell Co-Culture Objective: To study dynamic interactions between patient-derived tumor organoids and autologous tumor-infiltrating lymphocytes (TILs).
Materials:
- Basement Membrane Extract (BME/Matrigel): Provides a 3D scaffold mimicking the extracellular matrix.
- Advanced Culture Medium: Tumor organoid medium (tissue-specific, with growth factors) mixed with immune cell medium (RPMI-1640 + 5-10% human serum + IL-2 (50-100 IU/mL) + IL-15 (10 ng/mL)).
- Patient-Derived Tumor Organoids (PDOs): Expanded and digested to single cells/small clusters.
- Autologous Immune Cells: TILs expanded from the same tumor sample, or peripheral blood mononuclear cells (PBMCs).
- Checkpoint Inhibitors: Recombinant anti-PD-1/PD-L1 antibodies (10 µg/mL).
Detailed Methodology:
- Prepare Organoid Matrix: Mix dissociated PDO cells with cold BME at a 1:1 volume ratio. Plate 20 µL droplets in pre-warmed tissue culture plates. Allow to polymerize at 37°C for 30 min.
- Add Immune Cells and Medium: Carefully layer the co-culture medium containing 1-5 x 10⁴ immune cells (TILs or PBMC-derived T cells) per well on top of the BME droplet. Include experimental conditions with immune checkpoint blockade.
- Culture and Monitor: Culture for 3-7 days. Refresh 50% of the medium every 2-3 days, maintaining cytokines.
- Analysis:
- Viability: Use ATP-based luminescence or live/dead staining (Calcein-AM/Propidium Iodide) on recovered organoids.
- Immune Cell Activation: Recover immune cells from supernatant/BME; stain for CD8, CD4, PD-1, Tim-3, LAG-3, and intracellular IFN-γ (via flow cytometry).
- Cytokine Secretion: Analyze supernatant via Luminex multiplex assay for IFN-γ, TNF-α, Granzyme B, IL-2, IL-6, IL-10.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Humanized Mouse and Co-Culture Studies
| Reagent Category | Specific Example | Function & Application |
|---|---|---|
| Immunodeficient Mouse Strains | NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) | Gold-standard host for high-level engraftment of human HSCs and tumor tissues. |
| Human Cytokine-Expressing Strains | NSG-SGM3 (B6;129S-Il2rgtm1(IL3,CSF2,KITLG)Rav*), MISTRG | Express human cytokines (e.g., GM-CSF, IL-3) to support enhanced development of human myeloid and innate immune cells. |
| Human Hematopoietic Stem Cells | CD34+ HSCs from Cord Blood | Primary cells used to reconstitute the human immune system in mice. Critical for personalized models. |
| Basement Membrane Matrix | Corning Matrigel Basement Membrane Matrix, Geltrex | 3D scaffold for culturing tumor organoids and establishing co-culture systems ex vivo and in vivo. |
| Organoid Culture Media | Stemcell Technologies IntestiCult, customized formulations | Chemically defined media containing essential growth factors (Wnt, R-spondin, Noggin) to maintain and expand patient-derived organoids. |
| Immune Cell Culture Additives | Recombinant Human IL-2, IL-15, IL-7 | Cytokines essential for the expansion, survival, and functional maintenance of human T cells and NK cells in vitro and in vivo. |
| Checkpoint Blockade Reagents | Recombinant Anti-human PD-1 (Nivolumab biosimilar), Anti-PD-L1 | High-purity antibodies for modulating immune checkpoint pathways in co-culture assays and humanized mouse therapy studies. |
| Human-Specific Flow Cytometry Antibodies | Anti-human CD45, CD3, CD8, CD4, PD-1, Tim-3 | Antibody panels for tracking, quantifying, and phenotyping human immune cell engraftment and activation states. |
| In Vivo Imaging Agents | Luciferase-expressing tumor cell lines, IVIS substrates | Enable non-invasive, longitudinal monitoring of tumor burden and metastasis in live humanized mice. |
This technical guide explores three pivotal high-dimensional analytical tools—Multiplex Immunohistochemistry (mIHC), Cytometry by Time-of-Flight (CyTOF), and Single-Cell RNA Sequencing (scRNA-seq)—within the framework of cancer immunoediting and immune surveillance research. The immunoediting hypothesis posits a dynamic process encompassing elimination, equilibrium, and escape phases, sculpted by continuous immune-tumor interactions. Understanding this complex interplay requires tools capable of dissecting the spatial, proteomic, and transcriptomic heterogeneity of the tumor microenvironment (TME). This document details the principles, protocols, and applications of these technologies, providing a resource for advancing immunotherapy and oncology drug development.
Multiplex Immunohistochemistry (mIHC)
Multiplex IHC enables simultaneous detection of multiple biomarkers on a single tissue section, preserving spatial context critical for studying cell-cell interactions within the TME.
Core Principles & Workflow
mIHC typically employs sequential staining, imaging, and signal inactivation cycles. Common platforms include Opal (Akoya Biosciences), which uses tyramide signal amplification (TSA), and CODEX (Akoya Biosciences), which utilizes DNA-barcoded antibodies.
Workflow Diagram:
Diagram 1: Sequential mIHC Workflow with TSA.
Key Experimental Protocol: Opal 7-Color mIHC
- Tissue Preparation: 4µm FFPE sections mounted on charged slides. Bake, deparaffinize, rehydrate.
- Antigen Retrieval: Heat-induced epitope retrieval (HIER) using pH 6 or pH 9 buffer in a pressure cooker (100°C, 20 min).
- Endogenous Blocking: Block peroxidase (3% H₂O₂, 10 min), then protein (10% normal goat serum, 30 min).
- Sequential Staining Cycles (Repeat for each marker):
- Apply primary antibody (e.g., anti-CD8, 1:200) for 60 min at RT.
- Apply HRP-conjugated secondary polymer (e.g., Anti-Rabbit HRP) for 10 min.
- Apply Opal fluorophore (e.g., Opal 520, 1:150) diluted in Amplification Diluent for 10 min.
- Perform microwave stripping (100°C, 20 min in AR6 buffer) to remove antibodies.
- Counterstaining & Mounting: After final cycle, apply spectral DAPI for nuclei, mount with ProLong Diamond.
- Image Acquisition & Analysis: Use Vectra/Polaris or similar multispectral imagers. Perform spectral unmixing with inForm or QuPath software for single-cell segmentation and phenotyping.
The Scientist's Toolkit: mIHC Reagents
| Reagent/Solution | Function in Experiment |
|---|---|
| FFPE Tissue Sections | Preserves tissue morphology and antigenicity for long-term analysis. |
| Opal Fluorophores | Tyramide-based, HRP-activated fluorescent dyes for high-sensitivity signal amplification. |
| Multispectral Imaging System | Captures full emission spectrum per pixel; enables unmixing of overlapping fluorophores. |
| Phenochart / inForm Software | For defining regions of interest, spectral unmixing, and cell segmentation/classification. |
| Antibody Validation Panel | Primary antibodies rigorously validated for IHC and compatibility with stripping cycles. |
Cytometry by Time-of-Flight (CyTOF)
CyTOF, or mass cytometry, combines flow cytometry principles with time-of-flight mass spectrometry, enabling high-parameter single-cell proteomic analysis (>40 markers) using metal-tagged antibodies.
Core Principles & Workflow
Cells are stained with antibodies conjugated to stable lanthanide isotopes. The nebulized sample is ionized in an argon plasma, and the atomic mass of each metal isotope is quantified per cell, eliminating spectral overlap.
Workflow Diagram:
Diagram 2: CyTOF Experimental and Analysis Pipeline.
Key Experimental Protocol: CyTOF for Tumor-Infiltrating Immune Cells
- Sample Preparation: Generate single-cell suspension from fresh or viably frozen tumor tissue using mechanical dissociation and enzymatic digestion (e.g., collagenase IV/DNase I). Preserve viability.
- Viability Staining: Stain with Cell-ID Intercalator-Ir (DNA intercalator) in PBS for live/dead discrimination.
- Surface Staining: Fc receptor block, then stain with pre-titrated panel of metal-tagged antibodies (Maxpar) for 30 min at RT.
- Cell Fixation & Barcoding: Fix with 1.6% PFA. For multiplexing, use Cell-ID 20-Plex Pd Barcoding Kit to pool samples, reducing technical variability.
- Intracellular Staining (Optional): Permeabilize (FoxP3/Transcription Factor kit), stain for intracellular targets.
- Data Acquisition: Resuspend cells in EQ Four Element Calibration Beads/Cell Acquisition Solution. Run on Helios or Symphony, acquiring ~500 events/second.
- Data Preprocessing & Analysis: Normalize data using bead standards. Debarcode if pooled. Use Cytobank, OMIQ, or R (cytofkit2) for viSNE/UMAP, FlowSOM/PhenoGraph clustering, and differential abundance analysis.
Quantitative Data from Recent Studies (2023-2024)
Table 1: Comparative Output of High-Dimensional Tools in Cancer Studies.
| Tool | Typical Parameters per Cell | Cells per Run (Typical) | Key Readouts in Immunoediting | Key Reference (Example) |
|---|---|---|---|---|
| Multiplex IHC | 6-9 protein markers + spatial | 1,000 - 1,000,000 (per slide) | Spatial relationships (e.g., CD8+ T cell distance to PD-L1+ cell), neighborhood analysis. | Nat Cancer. 2023;4(2): 231-246. |
| CyTOF | 40-50 protein markers | 100,000 - 1,000,000 | Deep immune phenotyping (e.g., exhausted T cell subsets, myeloid diversity), signaling states (phospho-protein). | Cell. 2024;187(3): 704-723.e22. |
| scRNA-seq | 20,000+ genes | 5,000 - 20,000 (per lane) | Transcriptional states, lineage trajectories, TCR/BCR clonality, gene regulatory networks. | Science. 2023;380(6648): eabn7980. |
Single-Cell RNA Sequencing (scRNA-seq)
scRNA-seq profiles the transcriptome of individual cells, uncovering cellular heterogeneity, novel subtypes, and dynamic gene expression programs within the TME.
Core Principles & Workflow
Single cells are isolated (via droplet, nanowell, or plate-based methods), barcoded, and their cDNA is prepared for next-generation sequencing.
Workflow Diagram:
Diagram 3: Core scRNA-seq Experimental Pipeline.
Key Experimental Protocol: Droplet-Based scRNA-seq (10x Genomics)
- Single-Cell Preparation: Prepare a high-viability (>80%) single-cell suspension in appropriate buffer. Aim for concentration of 700-1,200 cells/µl. Filter through a 40µm flow cell strainer.
- Gel Bead-in-Emulsion (GEM) Generation: Load Chromium Chip with cells, Master Mix, and Gel Beads containing Unique Molecular Identifiers (UMIs) and cell barcodes. The controller generates oil-coated GEMs where single cells are lysed and mRNA is barcoded.
- Post-GEM-RT Cleanup & cDNA Amplification: Break emulsions, recover barcoded cDNA. Perform cleanup with DynaBeads and amplify cDNA via PCR.
- Library Construction: Fragment and size-select amplified cDNA. Add sample index and sequencing adapters via end-repair, A-tailing, adapter ligation, and PCR.
- Sequencing: Pool libraries and sequence on Illumina NovaSeq (recommended depth: ~50,000 reads/cell).
- Primary Data Analysis: Use Cell Ranger (10x) for demultiplexing, alignment, UMI counting, and initial clustering. Downstream analysis in R/Seurat or Python/Scanpy includes normalization, highly variable gene selection, PCA, UMAP, graph-based clustering, and differential expression.
Integrative Analysis in Immunoediting Research
Combining these tools provides a holistic view. CITE-seq (cellular indexing of transcriptomes and epitopes) allows simultaneous scRNA-seq and protein measurement. Spatial transcriptomics (e.g., Visium, Xenium) bridges scRNA-seq data with tissue architecture.
Integration Logic Diagram:
Diagram 4: Multi-modal Data Integration for Immunoediting.
Multiplex IHC, CyTOF, and scRNA-seq are indispensable, complementary tools for deconstructing the complexities of cancer immunoediting. mIHC provides essential spatial context, CyTOF offers deep proteomic phenotyping at single-cell resolution, and scRNA-seq reveals transcriptional dynamics and cellular hierarchies. Their integrated application accelerates the identification of novel therapeutic targets, predictive biomarkers, and a foundational understanding of immune evasion mechanisms, ultimately driving advances in precision immuno-oncology.
This whitepaper situates itself within the broader thesis that cancer immunoediting—comprising the three phases of Elimination, Equilibrium, and Escape—is the foundational framework for understanding tumor-immune system interactions. Immune surveillance, a component of the Elimination phase, represents the body's intrinsic defense against malignant transformation. The transition from Equilibrium to Escape, driven by tumor immunoediting, creates the therapeutic targets for modern immuno-oncology. This guide details the application of these principles to engineer next-generation checkpoint inhibitors and therapeutic cancer vaccines.
Core Immunoediting Mechanisms Informing Drug Design
The immunoediting process sculpts both the tumor and its microenvironment, selecting for less immunogenic clones and fostering an immunosuppressive niche. Key mechanisms include:
- Antigenic Modulation: Downregulation or loss of tumor antigen expression to evade T-cell recognition.
- Alteration in Antigen Presentation Machinery: Defects in MHC class I expression or interferon-gamma signaling pathways.
- Recruitment of Immunosuppressive Cells: Infiltration of regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and M2 macrophages.
- Upregulation of Immune Checkpoint Ligands: Expression of PD-L1, CTLA-4 ligands, and other inhibitory molecules on tumor and stromal cells.
Table 1: Quantitative Evolution of Tumor and Immune Parameters Across Immunoediting Phases
| Immunoediting Phase | Key Tumor Biomarker (Example Median Expression Level) | Dominant Immune Cell Infiltrate (Approximate Composition) | Representative Cytokine Milieu |
|---|---|---|---|
| Elimination | High Neoantigen Burden (>150 non-synonymous mutations) | CD8+ Cytotoxic T cells (60-70%) | IFN-γ, IL-12, TNF-α |
| Equilibrium | Intermediate PD-L1 (10-30% of cells by IHC) | Mixed: CD8+ T cells, CD4+ T cells, NK cells | IFN-γ, IL-2, TGF-β (low) |
| Escape | High PD-L1 (>50% of cells by IHC) | Tregs & MDSCs (combined >40%) | TGF-β, IL-10, IL-6, VEGF |
Diagram 1: The Cancer Immunoediting Cycle and Therapeutic Reversal
Application to Checkpoint Inhibitor Design
Checkpoint inhibitors (CPIs) aim to reverse the Escape phase by blocking inhibitory receptors on T cells or their ligands.
Targeting Novel Editable Checkpoints Beyond PD-1/CTLA-4
Research focuses on checkpoints upregulated during immunoediting.
- LAG-3: Upregulated on exhausted T cells in equilibrium/escape. Inhibits T-cell function upon binding to MHC class II.
- TIGIT: Expressed on tumor-infiltrating lymphocytes. Binds CD155 on tumor cells, transducing an inhibitory signal.
- TIM-3: Marker of terminal exhaustion. Multiple ligands (Galectin-9, CEACAM-1) are often overexpressed in tumors.
Table 2: Novel Immune Checkpoint Targets in Clinical Development
| Target | Primary Ligand(s) | Role in Immunoediting Escape | Clinical Stage (Example Agents) |
|---|---|---|---|
| LAG-3 | MHC Class II | Mediates Treg suppression & CD8+ T cell exhaustion | Approved (Relatlimab + Nivolumab) |
| TIGIT | CD155 (PVR) | Inhibits NK & T cell activation in TME | Phase III (Tiragolumab, Vibostolimab) |
| TIM-3 | Galectin-9, CEACAM-1 | Associated with adaptive resistance to anti-PD-1 | Phase II (Sabatolimab, Cobolimab) |
| VISTA | VSIG-3, PSGL-1 | Suppresses T-cell activation in acidic TME | Phase I/II (CA-170, JNJ-61610588) |
Experimental Protocol: Evaluating CPI Efficacy inVivo
Title: In Vivo Assessment of Checkpoint Inhibitor Combination in a Syngeneic Mouse Model Objective: To test the anti-tumor efficacy and immune correlates of a novel anti-TIGIT antibody combined with anti-PD-L1. Workflow:
- Tumor Inoculation: Inject 0.5 x 10^6 MC38 colon carcinoma cells (C57BL/6 background) subcutaneously into the right flank of 8-week-old female C57BL/6 mice (n=10 per group).
- Randomization & Dosing: When tumors reach ~50 mm³, randomize mice into four groups: (a) Isotype control, (b) anti-PD-L1 (10 mg/kg), (c) anti-TIGIT (10 mg/kg), (d) combination. Administer antibodies via intraperitoneal injection every 3 days for 4 cycles.
- Monitoring: Measure tumor dimensions with calipers every 2-3 days. Calculate volume = (length x width²)/2.
- Endpoint Analysis: At Day 28 or when tumor volume exceeds 1500 mm³ in control group:
- Harvest tumors, digest to single-cell suspension.
- Perform flow cytometry staining: CD45, CD3, CD8, CD4, FoxP3 (Tregs), PD-1, TIGIT, TIM-3 (exhaustion markers).
- Isolate RNA for NanoString PanCancer Immune Profiling Panel.
- Statistical Analysis: Compare tumor growth curves (Repeated Measures ANOVA) and immune cell populations (one-way ANOVA with Tukey's post-test).
Diagram 2: In Vivo CPI Efficacy Study Workflow
Application to Therapeutic Cancer Vaccine Design
Vaccines aim to enhance the Elimination phase and disrupt Equilibrium by expanding tumor-specific T cell clones.
Neoantigen Vaccine Platform
Neoantigens, arising from tumor somatic mutations, are ideal targets as they are foreign and not subject to central tolerance. The vaccine design pipeline is a direct application of immunoediting genomics.
Experimental Protocol: Personalized Neoantigen Vaccine Production (mRNA-based) Title: Personalized Neoantigen Prediction and mRNA Vaccine Manufacturing Workflow:
- Tumor & Normal Sequencing: Perform whole-exome sequencing (WES) of tumor biopsy and matched normal DNA (150x coverage). Perform tumor RNA-seq (100M reads).
- Variant Calling: Align sequences (BWA to GRCh38). Call somatic variants (MuTect2 for SNVs, Strelka2 for indels).
- Neoantigen Prediction:
- Input somatic variants to NetMHCpan (v4.1) for HLA class I binding prediction (IC50 < 50 nM considered strong binder).
- Use HLA type from RNA-seq data (OptiType).
- Filter for mutations with high expression (FPKM > 1 from RNA-seq).
- Prioritize clonal mutations (cancer cell fraction >0.8 from copy-number analysis).
- mRNA Vaccine Design & Synthesis:
- Design mRNA sequence encoding up to 20 selected neoantigen peptides (each 27 amino acids, including mutant residue centered).
- Use codon optimization for human cells.
- Incorporate sequence into a proprietary mRNA vector with 5' cap1 and poly-A tail.
- Manufacture vaccine via in vitro transcription (IVT) and lipid nanoparticle (LNP) encapsulation under GMP.
Table 3: Key Reagents for Neoantigen-Specific T-Cell Validation
| Research Reagent | Vendor Examples | Function in Experiment |
|---|---|---|
| HLA-A*02:01 Monomer (Empty) | BioLegend, MBL Int. | Peptide loading to create pHLA complexes for tetramer synthesis |
| PE-conjugated Streptavidin | Thermo Fisher, BD Biosc. | Tetramerization of biotinylated pHLA monomers via streptavidin binding |
| Anti-CD3/CD28 Dynabeads | Thermo Fisher | Polyclonal T cell activation and expansion from PBMCs |
| Human IL-2 (Proleukin) | Clinigen, Novartis | Cytokine for maintaining growth and viability of activated T cells |
| IFN-γ ELISpot Kit | Mabtech, BD Biosc. | Detection of neoantigen-specific T-cell responses at single-cell level |
Diagram 3: Personalized Neoantigen mRNA Vaccine Pipeline
Combining CPIs and Vaccines: A Synergistic Approach
Rational combination targets vaccine-primed T cells that have entered an exhausted state in the TME, releasing their brakes.
Key Clinical Data: A Phase 1b trial combining a personalized neoantigen vaccine (NEO-PV-01) with nivolumab (anti-PD-1) in metastatic melanoma showed a 1.5-fold increase in neoantigen-specific CD8+ T cell clones compared to pre-treatment, with a significant expansion of T cells recognizing vaccine-targeted neoantigens (median increase of 8.3-fold). The objective response rate was 59%.
Table 4: Mechanisms of Synergy Between Vaccines and Checkpoint Inhibitors
| Component | Primary Role in Immunoediting Context | Synergistic Mechanism with Partner |
|---|---|---|
| Therapeutic Vaccine | Amplifies the Elimination phase; expands high-avidity neoantigen-specific T cell clones. | Increases frequency of tumor-specific T cells in circulation and TME, creating a more favorable target for CPI. |
| Checkpoint Inhibitor | Reverses the Escape phase; blocks inhibitory signals in the TME. | Prevents the exhaustion/deletion of vaccine-primed T cells upon encountering the immunosuppressive TME. |
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Research Reagent Solutions for Immunoediting & Therapy Studies
| Reagent Category | Specific Example(s) | Function & Application |
|---|---|---|
| Syngeneic Mouse Models | MC38 (colon), B16-F10 (melanoma), 4T1 (breast) | In vivo study of immunoediting and therapy in immunocompetent hosts. |
| Recombinant Immune Checkpoint Proteins | Human/mouse PD-1-Fc, CTLA-4-Fc, TIGIT-Fc | Blocking assays, ligand binding studies (ELISA, SPR), flow cytometry compensation. |
| Antibody Panels for Exhaustion Phenotyping | Anti-mouse/human: PD-1, TIM-3, LAG-3, TIGIT (conjugated to fluorophores) | Multiparametric flow cytometry to profile T cell states in tumor digests or PBMCs. |
| Cytokine Multiplex Assays | LEGENDplex (BioLegend), ProcartaPlex (Thermo Fisher) | Quantify panels of cytokines (IFN-γ, TNF-α, IL-6, IL-10, etc.) from serum or culture supernatant. |
| Human Tumor Organoid Kits | Cultrex BME, IntestiCult, proprietary media | Establish ex vivo 3D tumor models for autologous co-cultures with immune cells. |
| MHC Tetramer & Dextramer Kits | Immudex, MBL International, Tetramer Shop | Direct detection and isolation of antigen-specific T cells by flow cytometry or sorting. |
Navigating Challenges: Troubleshooting Common Pitfalls in Immunoediting Research
Integrating the principles of cancer immunoediting—encompassing elimination, equilibrium, and escape—into preclinical models remains a central challenge. This whitepaper details technical strategies to address three critical limitations confounding immune surveillance research: the dynamic variability of the microbiome, the polygenic influence of host genetics, and the spatial discrepancies within the tumor microenvironment (TME). By providing updated data, standardized protocols, and visualization tools, we aim to enhance the translational fidelity of models used in immunotherapy development.
Microbiome Variability: Quantification and Standardization
The commensal microbiota modulates systemic and anti-tumor immunity, influencing responses to checkpoint inhibitors. Controlling for this variable is essential for reproducible studies.
Current Data on Microbial Impact
Table 1: Impact of Specific Bacterial Taxa on Immunotherapy Efficacy
| Bacterial Taxon | Associated Cancer Therapy | Effect on Response | Proposed Mechanism (Key Immune Pathway) | Key Reference (Year) |
|---|---|---|---|---|
| Bifidobacterium spp. | Anti-PD-L1 (melanoma) | Enhancement | Cross-presentation by dendritic cells; Enhanced CD8+ T cell priming | Matson et al., 2018 |
| Akkermansia muciniphila | Anti-PD-1 (lung, renal) | Enhancement | IL-12-dependent recruitment of CCR9+CXCR3+CD4+ T cells to TME | Routy et al., 2018 |
| Faecalibacterium prausnitzii | Anti-CTLA-4 (melanoma) | Enhancement | Inflammasome activation & IL-1β/IL-12 production | Chaput et al., 2017 |
| Bacteroidales spp. | Anti-CTLA-4 | Resistance | Induction of regulatory T cells (Tregs) & T cell exhaustion | Veitzou et al., 2015 |
Experimental Protocol: Gnotobiotic Mouse Model Generation for Immunotherapy Studies
Objective: To establish murine cohorts with defined microbial compositions to assess causal effects on immunoediting. Materials: Germ-free (GF) C57BL/6 mice, anaerobic chamber, gavage needles, bacterial culture media. Procedure:
- Preparation of Bacterial Consortium: Anaerobically culture target bacterial species (e.g., a cocktail of Bifidobacterium and Akkermansia). Harvest at mid-log phase, centrifuge, and resuspend in reduced PBS with 20% glycerol.
- Colonization: House GF mice in flexible film isolators. For oral gavage, administer 200µL of bacterial suspension (10^8 CFU total) to each mouse.
- Verification: At 7 and 21 days post-gavage, collect fecal pellets. Perform 16S rRNA gene sequencing and quantitative PCR (qPCR) for specific taxa to confirm stable engraftment.
- Tumor Implantation & Treatment: Implant syngeneic tumor cells (e.g., MC38 or B16-F10) subcutaneously. Initiate anti-PD-1 therapy when tumors reach ~100 mm³. Monitor tumor growth and endpoint immune profiling via flow cytometry of tumor-infiltrating lymphocytes (TILs).
Diagram Title: Gnotobiotic Mouse Model Workflow for Microbiome Studies
Host Genetics: Accounting for Polygenic Diversity
Inbred mouse strains fail to capture the genetic heterogeneity of human populations, leading to divergent immune responses.
Data on Genetic-Driven Immune Variation
Table 2: Host Genetic Factors Influencing Immunoediting Phenotypes
| Genetic Model / Locus | Immune Phenotype | Impact on Immunoediting Phase | Relevance to Human Cancer |
|---|---|---|---|
| Collaborative Cross (CC) Mice | Extreme diversity in T cell repertoire, cytokine production | Alters efficiency of both Elimination and Escape | Models variable patient responses to immunotherapy |
| MHC (H-2) Haplotype | Peptide presentation diversity | Determines tumor antigen immunogenicity (Elimination) | Direct correlate of HLA diversity in humans |
| Pdl1 gene polymorphism | Variable PD-L1 expression on tumor/immune cells | Modulates T cell exhaustion (Escape) | Biomarker for anti-PD-1/PD-L1 therapy |
| Ifng receptor pathway variants | Differential STAT1 signaling & antigen presentation | Affects immune-mediated killing (Elimination) | Linked to resistance in multiple cancer types |
Experimental Protocol: Utilizing the Collaborative Cross (CC) for Tumor Challenge Studies
Objective: To map quantitative trait loci (QTLs) associated with immunoediting outcomes using genetically diverse mice. Materials: CC or Diversity Outbred (DO) mice, tumor cell line, genomic DNA isolation kit, microarray or NGS platform. Procedure:
- Cohort Generation: Acquire a cohort of 200+ CC or DO mice from a repository. Ensure balanced representation of founder haplotypes.
- Phenotyping Challenge: Implant a uniform number of syngeneic tumor cells. Measure primary phenotypes: tumor incidence, growth rate, survival, and spontaneous regression rate.
- High-Density Genotyping: Isolate genomic DNA from tail snips. Use a pre-designed array (e.g., GigaMUGA) to genotype at ~100,000 SNPs.
- QTL Mapping & Analysis: Using statistical software (e.g., R/qtl2), perform genome-wide association between genotype data and tumor phenotypes. Identify significant loci linked to "immune clearance" (elimination) or "rapid progression" (escape).
Diagram Title: Genetic Mapping of Immunoediting Traits in Diverse Mice
Microenvironment Discrepancies: BridgingIn VitroandIn VivoGaps
Standard 2D monocultures lack the spatial, cellular, and physicochemical complexity of the in vivo TME, which is critical for the equilibrium phase.
Data on TME Components and Model Discrepancies
Table 3: Key TME Components and Their Representation in Models
| TME Component | Function in Immunoediting | Standard 2D Model | Advanced 3D Model (e.g., Organoid/Spheroid Co-culture) |
|---|---|---|---|
| Hypoxic Gradient | Drives immunosuppression, upregulates PD-L1, inhibits T cell function | Absent | Can be modeled in core of large spheroids |
| Extracellular Matrix (ECM) | Physical barrier to T cell infiltration; scaffold for signaling | None or simple coating (Matrigel) | Tunable hydrogels (collagen, fibrin) with defined stiffness |
| Stromal Cells (CAFs, MSCs) | Secrete immunosuppressive cytokines; exclude T cells | Not included | Can be co-cultured in ratio-controlled systems |
| Immune Cell Populations | Dynamic interactions (killing, exhaustion, anergy) | Limited, often endpoint add-back | Sustained multi-culture with temporal tracking |
Experimental Protocol: Establishing a 3D Immunocompetent Tumor Spheroid Co-culture
Objective: To model T cell infiltration and exhaustion within a structured TME in vitro. Materials: U-bottom ultra-low attachment plates, tumor cell line, activated T cells, matrigel/collagen I, hypoxia-inducing agents (e.g., CoCl₂), live-cell imaging system. Procedure:
- Spheroid Formation: Seed 5,000 tumor cells/well in a U-bottom plate. Centrifuge at 300xg for 3 min to aggregate cells. Culture for 72h to form compact spheroids.
- T Cell Activation & Labeling: Isolate CD8+ T cells from mouse spleen or human PBMCs. Activate with anti-CD3/CD28 beads and IL-2 for 48h. Label with fluorescent dye (e.g., CellTracker).
- Co-culture Initiation: Carefully add 2,000 labeled T cells to each well containing a pre-formed spheroid. For embedded conditions, mix spheroid and T cells in liquid Matrigel and polymerize.
- Monitoring & Analysis: Use live-cell confocal microscopy to track T cell migration into the spheroid every 6-12h. At endpoint (96h), dissociate spheroids and analyze T cell phenotype (PD-1, TIM-3, LAG-3 expression via flow cytometry) and viability.
Diagram Title: 3D Immunocompetent Spheroid Co-culture Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Addressing Model Limitations
| Item Name | Supplier Examples | Function in Context |
|---|---|---|
| Gnotobiotic Isolators | Taconic, The Jackson Laboratory | Maintain germ-free or defined-flora murine colonies for microbiome studies. |
| Defined Microbial Consortia | Evergreen, ATCC | Provide standardized, characterized bacterial mixtures for colonization. |
| Collaborative Cross (CC) Mice | The Jackson Laboratory (J:DO, J:CC) | Offer a genetically diverse mouse population for mapping host genetic effects. |
| GigaMUGA Genotyping Array | Neogen Genomics | High-density SNP array for precise genetic mapping in outbred mouse populations. |
| Ultra-Low Attachment (ULA) Plates | Corning, Greiner Bio-One | Enable formation of uniform 3D tumor spheroids from most cell lines. |
| Tunable Hydrogels (e.g., Collagen I) | Corning, Advanced BioMatrix | Provide a physiologically relevant 3D extracellular matrix for cell migration studies. |
| Multiplex Immunofluorescence Kits | Akoya Biosciences (PhenoCycler), Standard BioTools | Enable spatial profiling of immune and tumor cells within intact TME sections. |
| Live-Cell Tracking Dyes (CellTracker) | Thermo Fisher Scientific | Fluorescently label specific cell populations for dynamic co-culture imaging. |
Optimizing Antigen Discovery and Validation Strategies to Override Immune Evasion
Cancer immunoediting is the fundamental process describing the dynamic interaction between tumors and the host immune system, comprising three phases: Elimination, Equilibrium, and Escape. The Escape phase, characterized by tumor immune evasion, represents the clinical manifestation of disease. Overcoming evasion requires the discovery and validation of targetable antigens that are not susceptible to downregulation or editing by the tumor. This guide details advanced strategies for identifying and validating such antigens within the framework of immunoediting principles.
Quantitative Landscape of Current Antigen Classes
The table below summarizes the key characteristics, advantages, and limitations of major tumor antigen classes targeted in discovery pipelines.
Table 1: Comparative Analysis of Tumor Antigen Classes
| Antigen Class | Prevalence in Solid Tumors (%) | Immunogenicity Potential | Susceptibility to Immune Editing | Clinical Validation Status |
|---|---|---|---|---|
| Tumor-Associated Antigens (TAAs) | 60-80 | Low-Moderate (self-tolerance) | High | High (Multiple approved therapies) |
| Tumor-Specific Antigens (TSAs) / Neoantigens | 10-95 (varies by TMB) | Very High | Low (ideal target) | Moderate-High (Personalized vaccines, TCR-T) |
| Cancer-Testis Antigens (CTAs) | 20-60 | Moderate | Moderate (epigenetic silencing) | Moderate (NY-ESO-1 targeted) |
| Viral Antigens | 5-15 (virus-associated cancers) | High | Low | High (HPV-E6/E7 targets) |
| Alternative Reading Frame Antigens | 5-20 | Moderate | Unknown/Low | Low (Preclinical) |
Core Experimental Protocols for Antigen Discovery
Integrated Multi-Omic Neoantigen Discovery Workflow
This protocol defines a robust pipeline for identifying candidate neoantigens from patient tumor samples.
Materials & Reagents:
- Fresh frozen or optimally preserved tumor tissue and matched germline (blood) sample.
- High-quality DNA/RNA extraction kits (e.g., Qiagen AllPrep).
- Next-generation sequencing (NGS) platforms for whole exome sequencing (WES) and RNA-Seq.
- MHC binding prediction algorithms (NetMHCpan, MHCflurry).
- Mass spectrometry (LC-MS/MS) system for immunopeptidomics.
Procedure:
- Sequencing & Variant Calling:
- Perform WES on tumor and germline DNA. Align reads (BWA, STAR) to reference genome (GRCh38).
- Call somatic mutations using paired variant callers (MuTect2, VarScan2). Filter for high-confidence variants.
- Perform RNA-Seq on tumor RNA to quantify transcript expression (FPKM > 1.0).
- Neoepitope Prediction:
- Translate non-synonymous somatic mutations into candidate peptide sequences (8-11 amino acids).
- Predict binding affinity of candidate peptides to patient-specific HLA alleles (using NetMHCpan, IC50 < 50 nM considered strong binder).
- Integrate RNA expression data to filter for peptides derived from expressed mutations.
- Immunopeptidomic Validation:
- Isolate HLA-peptide complexes from tumor tissue or cell lines via immunoaffinity purification.
- Elute and sequence peptides via LC-MS/MS.
- Cross-reference identified peptides with the predicted neoantigen list for direct biochemical validation.
Functional Validation of Antigen Immunogenicity
Candidate antigens require functional validation of T-cell recognition.
Materials & Reagents:
- Candidate peptide libraries.
- Autologous or HLA-matched peripheral blood mononuclear cells (PBMCs).
- Recombinant human cytokines (IL-2, IL-7, IL-15).
- ELISA or ELISpot kits for IFN-γ detection.
- Flow cytometry antibodies (CD3, CD8, CD137, intracellular IFN-γ/TNF-α).
Procedure:
- In Vitro T-Cell Priming:
- Pulse autologous antigen-presenting cells (APCs) with candidate peptides.
- Co-culture peptide-pulsed APCs with autologous PBMCs in the presence of IL-2 (50 IU/mL) and IL-7 (10 ng/mL).
- Re-stimulate weekly for 3-4 cycles.
- T-Cell Response Assay:
- After the final stimulation, re-expose T-cells to peptide-pulsed APCs.
- Measure T-cell activation via: a. ELISpot: Quantify IFN-γ spot-forming units (SFUs). A positive response is >50 SFUs/10^6 cells and at least 2x background. b. Intracellular Cytokine Staining (ICS): Analyze CD8+ T-cells for IFN-γ and TNF-α production by flow cytometry. c. CD137 Activation Marker Assay: Measure surface CD137 expression on CD8+ T-cells after 24-hour co-culture.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Antigen Discovery & Validation
| Reagent/Tool | Supplier Examples | Primary Function |
|---|---|---|
| HLA Class I/II Immunoprecipitation Antibodies | BioLegend, Miltenyi Biotec | Isolation of native peptide-HLA complexes for immunopeptidomics. |
| Single-Cell RNA-Seq Kits (3' or 5') | 10x Genomics, Parse Biosciences | Profiling of tumor-infiltrating lymphocyte (TIL) clonality and antigen specificity. |
| Peptide-MHC (pMHC) Multimers (Tetramers/Dextramers) | Immudex, MBL International | Direct ex vivo staining and isolation of antigen-specific T-cells. |
| CRISPR/Cas9 Knockout Libraries | Synthego, Horizon Discovery | High-throughput screening for genes regulating antigen presentation (e.g., β2-microglobulin, TAP1/2). |
| Patient-Derived Organoid (PDO) Co-culture Systems | STEMCELL Technologies, Cultrex | Autologous tumor-immune cell functional assays in a physiologically relevant model. |
| Cytokine Release Assay Kits | Promega, MSD | Quantification of T-cell activation and functional potency. |
Strategic Diagrams
Title: Integrated Multi-Omic Antigen Discovery Pipeline
Title: Evasion Mechanisms and Strategic Countermeasures
Immune profiling is a critical tool for dissecting the complex interplay between tumors and the immune system, a cornerstone of the cancer immunoediting framework. This process, encompassing elimination, equilibrium, and escape, relies on precise measurement of immune cell phenotypes and functions. Inaccurate profiling due to technical pitfalls can obscure the mechanisms of immune surveillance and misdirect therapeutic development. This guide details major technical challenges in three core areas: panel design, sample processing, and data normalization.
Panel Design: Balancing Depth and Resolution
The design of flow or spectral cytometry panels dictates the breadth and specificity of immune interrogation. Common pitfalls include fluorophore spillover, antigen co-expression conflicts, and inadequate controls.
Quantitative Considerations for Panel Design
Table 1: Key Parameters in Cytometry Panel Design
| Parameter | Optimal Range/Target | Consequence of Deviation |
|---|---|---|
| Panel Size (Colors) | 20-40 parameters for spectral; 10-30 for conventional | Higher complexity increases spillover and requires more compensation. |
| Brightness Index (Antigen-Fluorophore) | >3 for low-abundance antigens; 1-3 for high-abundance. | Poor sensitivity or saturation, leading to loss of population resolution. |
| Spillover Spreading Matrix (SSM) | <5% for major neighbors; aim for minimal spreading. | Increased population spread, reduced resolution, and potential false positives. |
| Titration Validation | Use optimal stain index (SI) peak; typically 1:50 - 1:200 antibody dilution. | Reduced signal-to-noise ratio, increased cost, and non-specific binding. |
Detailed Protocol: Panel Validation and Spillover Assessment
Protocol 1.1: Single Stain Control Preparation for Compensation
- Sample: Use cell lines or primary cells (e.g., PBMCs) expressing the target antigen. Compensation beads (e.g., anti-mouse/rat Ig κ beads) are an alternative.
- Staining: For each fluorophore in the panel, prepare an individual tube staining for its target antigen. Include a fully unstained control.
- Data Acquisition: Acquire data on the cytometer, ensuring voltages are set to the same levels used for the full panel.
- Analysis: Use cytometry software (e.g., FlowJo, Cytobank) to calculate a compensation matrix. Manually verify compensation by checking that the median fluorescence intensity (MFI) of the positive population is identical in all other channels.
Protocol 1.2: Stain Index Calculation for Titration
- Titration: Stain identical cell aliquots with a serial dilution of the antibody-fluorophore conjugate (e.g., 1:25, 1:50, 1:100, 1:200, 1:400).
- Acquisition: Acquire data.
- Calculation: For each dilution, calculate the Stain Index (SI).
SI = (MFI_positive - MFI_negative) / (2 * SD_negative), where SD is the standard deviation of the negative population. - Selection: Choose the dilution at or near the peak SI value, balancing signal strength and cost.
Panel Design & Validation Workflow
Sample Processing: Preserving the Native Immune State
Pre-analytical variables during sample collection, handling, and storage introduce significant artifacts that can be misinterpreted as biological changes in immunoediting studies.
Quantitative Impact of Processing Variables
Table 2: Effects of Sample Processing Delays on Immune Cell Viability and Marker Expression
| Processing Step | Variable | Recommended Standard | Observed Change After 24h Delay (PBMCs at RT) |
|---|---|---|---|
| Blood Collection | Anticoagulant | EDTA or Heparin (avoid Heparin for RNA work) | N/A |
| Time to Processing | Ambient Temperature | < 4 hours (ideal: < 2h) | ↓ 15-30% lymphocyte viability; ↑ monocyte activation markers (CD62L↓, CD11b↑). |
| Separation Method | Density Gradient | Ficoll-Paque PLUS (or equivalent) | Increased granulocyte contamination. |
| Cryopreservation | Freeze Medium | 90% FBS + 10% DMSO | ↓ 5-15% recovery; potential shifts in rare subset frequencies (e.g., Tregs). |
| Thawing | Wash Medium | RPMI + 50% FBS | Rapid cell death if DMSO not diluted quickly. |
Detailed Protocol: Standardized PBMC Processing for Immune Profiling
Protocol 2.1: PBMC Isolation and Cryopreservation (SOP for Multi-site Studies)
- Materials: Blood collection tubes (EDTA), Ficoll-Paque Plus, DPBS (Ca2+/Mg2+-free), RPMI-1640, heat-inactivated FBS, DMSO, freezing containers.
- Dilution: Dilute fresh blood 1:1 with room temperature DPBS.
- Separation: Carefully layer 25 mL of diluted blood over 15 mL of Ficoll in a 50mL conical tube. Centrifuge at 400 × g for 30 minutes at room temperature with no brake.
- Harvest: Carefully collect the mononuclear cell layer at the interface and transfer to a new tube.
- Wash: Wash cells twice with DPBS (centrifuge at 300 × g for 10 min). Count using a viability stain (e.g., Trypan Blue).
- Freeze: Resuspend cell pellet at 10-20x10^6 cells/mL in cold freeze medium (90% FBS, 10% DMSO). Aliquot into cryovials. Place vials in an isopropanol freezing container at -80°C for 24h, then transfer to liquid nitrogen vapor phase for long-term storage.
Sample Processing Workflow & Pitfall Zone
Data Normalization and Analysis: Ensuring Robust Biological Interpretation
Raw immune profiling data requires rigorous normalization and batch correction to enable comparisons across samples and time points—essential for tracking immunoediting dynamics.
Quantitative Data Normalization Strategies
Table 3: Common Data Normalization Methods in High-Dimensional Immune Profiling
| Method | Primary Use Case | Key Advantage | Limitation/Pitfall |
|---|---|---|---|
| Bead-based (e.g., CS&T) | Daily instrument calibration. | Standardizes laser time, PMT voltages. | Does not correct for biological sample variation. |
| Arcsinh Transformation | CyTOF or flow cytometry data. | Stabilizes variance, handles zeroes. | Co-factor choice (e.g., 150 for CyTOF, 5 for flow) impacts downstream clustering. |
| Quantile Normalization | Batch correction across runs/days. | Forces identical distributions across batches. | Can over-correct and remove subtle biological signals. |
| CytofRUV / RUV-III | CyTOF batch effect removal. | Uses stable controls or replicate samples. | Requires carefully designed control samples. |
| ComBat (Empirical Bayes) | Flow/CyTOF batch adjustment. | Preserves biological variance well. | May struggle with very small batch sizes. |
Detailed Protocol: Batch Effect Correction Using bead-based Normalization
Protocol 3.1: Using BD FACS CS&T Beads for Inter-day Normalization
- Acquisition: Prior to sample acquisition, run a tube of CS&T beads according to the manufacturer's protocol. The cytometer software (e.g., FACSDiva) creates an application setting file that records baseline performance.
- Daily Calibration: On each acquisition day, run CS&T beads again. The software compares the new data to the baseline and calculates a target value, automatically adjusting PMT voltages to match the baseline.
- Validation: Run a standardized control sample (e.g., stained PBMCs from a cryopreserved aliquot) to verify that MFI for key markers is within an acceptable CV% (e.g., <15%) across days.
- Post-acquisition: For advanced integration of datasets, apply additional algorithms like
CytofRUVorComBatimplemented in R/Python, using the control sample data as an anchor.
The Scientist's Toolkit: Essential Reagents & Materials
Table 4: Key Research Reagent Solutions for Immune Profiling
| Item | Function & Purpose | Example Product/Catalog |
|---|---|---|
| Viability Dye | Distinguishes live/dead cells; critical for accurate frequency analysis and excluding artifacts. | Zombie NIR Fixable Viability Kit (BioLegend), LIVE/DEAD Fixable Aqua (Thermo Fisher). |
| Fc Receptor Block | Reduces non-specific antibody binding via Fcγ receptors, decreasing background noise. | Human TruStain FcX (BioLegend), Mouse BD Fc Block (BD Biosciences). |
| Cell Stimulation Cocktail | Activates cells to measure functional cytokines (e.g., IFN-γ, TNF) as part of immune competence. | Cell Activation Cocktail (with Brefeldin A) (BioLegend), PMA/Ionomycin. |
| Permeabilization Buffer | Allows intracellular staining for cytokines, transcription factors (e.g., FoxP3), and cytotoxic granules. | Foxp3 / Transcription Factor Staining Buffer Set (e.g., Thermo Fisher). |
| Compensation Beads | Ultra-bright particles used to create single-color controls for accurate spillover compensation. | UltraComp eBeads (Thermo Fisher), ArC Amine Reactive Beads (Thermo Fisher). |
| Standardized PBMCs | Commercially sourced healthy donor PBMCs used as inter-assay controls and normalization anchors. | Leukocytes, Human Peripheral Blood (HemaCare), AllCells. |
Data Normalization & Analysis Pipeline
Strategies to Overcome Primary and Acquired Resistance Mechanisms in Preclinical Testing
Within the broader thesis on the Basic Principles of Cancer Immunoediting and Immune Surveillance Research, this whitepaper examines the evolving challenge of tumor resistance to immunotherapies. Cancer immunoediting outlines three phases: elimination, equilibrium, and escape. Resistance mechanisms, both primary (intrinsic) and acquired (evolved post-therapy), represent the culmination of escape, undermining T cell-mediated tumor destruction. This guide details preclinical strategies to model, identify, and overcome these barriers, integrating cutting-edge technologies and quantitative assays to develop more durable cancer immunotherapies.
The immune system shapes tumor development through cancer immunoediting. Immunotherapies, particularly immune checkpoint inhibitors (ICIs), aim to reinvigorate the elimination phase. However, tumors utilize complex resistance mechanisms. Primary resistance involves pre-existing tumor-intrinsic (e.g., low mutational burden, impaired antigen presentation) and tumor-extrinsic factors (e.g., immunosuppressive microenvironment). Acquired resistance develops following initial response, driven by genomic and epigenetic evolution, and adaptation of the tumor microenvironment (TME). Preclinical modeling must faithfully recapitulate these dynamics to enable effective therapeutic breakthroughs.
Key Resistance Mechanisms and Preclinical Modeling Strategies
Effective preclinical testing requires accurate models of human resistance. The following table categorizes core mechanisms and corresponding preclinical models.
Table 1: Core Resistance Mechanisms and Representative Preclinical Models
| Mechanism Category | Specific Mechanism | In Vitro Model | In Vivo Model | Readout |
|---|---|---|---|---|
| Tumor-Intrinsic | Defective Antigen Presentation (MHC-I/LMP/TAP loss) | Co-culture of tumor spheroids with TCR-transgenic T cells | Syngeneic or GEMM with CRISPR-mediated gene knockouts | T cell activation (IFN-γ ELISA), tumor cell lysis (incucyte) |
| Oncogenic Signaling (e.g., WNT/β-catenin, PTEN loss) | 3D organoids with pathway inhibitors | Orthotopic models with constitutive pathway activation | PD-L1 expression (flow cytometry), T cell exclusion (IHC) | |
| Low Tumor Mutational Burden (TMB) | Patient-derived organoids (PDOs) | Syngeneic "cold" tumor models (e.g., B16-F10) | Neoantigen prediction by RNA-seq, TIL infiltration (multiplex IHC) | |
| Tumor-Extrinsic | Immunosuppressive Myeloid Cells (MDSCs, TAMs) | Transwell migration assays with conditioned media | Transfer of fluorescently labeled myeloid progenitors | Flow cytometry for CD11b⁺Gr1⁺ cells, Arg1/iNOS activity |
| Exhausted T Cell Phenotype (upregulated co-inhibitory receptors) | Chronic antigen stimulation of OT-I T cells | Repeated antigen exposure models (e.g., chronic LCMV infection) | Multiplex cytokine assay, scRNA-seq for exhaustion markers (TOX, PD-1, LAG-3) | |
| Dysfunctional Metabolic TME (nutrient depletion, hypoxia) | Seahorse assay of T cells from high-lactate medium | Window chamber models or hypoxia-reporter mice (e.g., HIF-1α-GFP) | Glucose/lactate measurement, pO₂ sensing, T cell mitochondrial mass |
Detailed Experimental Protocols
Protocol:In VivoModeling of Acquired Resistance to Anti-PD-1 Therapy
Objective: To generate and characterize a murine tumor model with acquired resistance to checkpoint blockade. Materials: C57BL/6 mice, MC38 colorectal adenocarcinoma cells (responsive), anti-mouse PD-1 clone RMP1-14, isotype control. Procedure:
- Tumor Inoculation: Inject 5x10⁵ MC38 cells subcutaneously into the right flank of 8-week-old mice (n=20).
- Initial Treatment: When tumors reach ~100 mm³, randomize mice into two groups: (a) anti-PD-1 (200 µg i.p., every 3 days for 4 doses), (b) isotype control.
- Resistance Selection: Monitor tumor volume bi-daily. In the treatment group, ~70% will respond. Allow tumors in initial responders that begin to regrow (>3 consecutive measurements of increase) to reach ~500 mm³. Excise these "relapsed" tumors under aseptic conditions.
- Tumor Cell Re-establishment: Digest tumor single-cell suspensions and re-culture in vitro for 2 passages. Re-inject these cells into new naive mice (n=10).
- Challenge Test: Treat tumor-bearing mice from Step 4 with anti-PD-1 or control as in Step 2. Confirmed resistance is defined as no significant difference in growth kinetics between treatment and control groups (p>0.05, two-way ANOVA).
- Analysis: Perform ex vivo immune profiling (flow cytometry for TAMs, Tregs, exhausted T cells) and tumor whole-exome sequencing on parental and resistant lines to identify evolved mechanisms.
Protocol: High-ThroughputIn VitroCRISPR Screen for Primary Resistance Genes
Objective: To identify tumor-intrinsic genes whose loss confers resistance to T cell-mediated killing. Materials: A375 melanoma cell line, Human genome-wide CRISPR knockout library (e.g., Brunello), Cas9-expressing A375 line, HLA-matched Tumor-Infiltrating Lymphocytes (TILs) or engineered T cells. Procedure:
- Library Transduction: Infect Cas9⁺ A375 cells with the CRISPR library at an MOI of ~0.3 to ensure single guide RNA (sgRNA) integration. Culture for 10 days under puromycin selection to generate a stable knockout pool.
- Selection Co-culture: Split the pool into two arms: "Pressure" Arm: Co-culture with TILs at a 1:1 effector:target ratio. "Control" Arm: Culture without TILs. Maintain co-culture for 7 days, replenishing TILs every 48 hours.
- Genomic DNA Extraction & Sequencing: Harvest genomic DNA from both arms at endpoint. Amplify integrated sgRNA sequences via PCR and subject to next-generation sequencing.
- Bioinformatic Analysis: Align sequences to the reference library. Using MAGeCK or similar algorithm, compare sgRNA abundance between "Pressure" and "Control" arms. Genes with significantly enriched sgRNAs (FDR < 0.05) in the "Pressure" arm represent candidate resistance genes whose knockout allowed tumor cell survival.
Visualization of Key Pathways and Workflows
Diagram 1: Generating Acquired Resistance Models
Diagram 2: IFN-γ Pathway & Key Resistance Mutations
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Resistance Mechanism Research
| Item | Function/Application | Example Product/Specification |
|---|---|---|
| Immune-Competent Mouse Models | Model intact host-tumor-immune interactions for in vivo therapy testing. | C57BL/6 or BALB/c syngeneic models (e.g., MC38, CT26); Genetically Engineered Mouse Models (GEMMs). |
| Recombinant Immune Modulators | To manipulate specific pathways in vitro and in vivo (e.g., cytokines, pathway agonists/antagonists). | Recombinant mouse/human IFN-γ, TGF-β, G-CSF; Agonistic anti-CD40, anti-OX40 antibodies. |
| Multiparametric Flow Cytometry Panels | Deep immunophenotyping of tumor infiltrate, exhaustion markers, intracellular signaling. | Antibody panels for mouse: CD45, CD3, CD4, CD8, PD-1, Tim-3, LAG-3, FoxP3, CD11b, F4/80, Gr-1. |
| CRISPR Knockout Libraries | For genome-wide or pathway-specific loss-of-function screens to identify resistance genes. | Human Brunello or Mouse Brie genome-wide KO libraries (Addgene). |
| Live-Cell Analysis Imaging System | Real-time, label-free quantification of T cell-mediated tumor killing in co-culture assays. | Incucyte with Cytotoxicity Assay Software. |
| Spatial Biology Platform | To map the geographic relationship between immune cells and tumor cells in the TME. | Nanostring GeoMx Digital Spatial Profiler, Akoya CODEX. |
| scRNA-seq & TCR-seq Kits | For transcriptomic profiling and clonal tracking of tumor and immune cells at single-cell resolution. | 10x Genomics Chromium Single Cell 5' Immune Profiling Solution. |
| Seahorse XF Analyzer Kits | To measure real-time metabolic flux (glycolysis, OXPHOS) of T cells or tumor cells from the TME. | XF T Cell Metabolic Assay Kit, XF Glycolysis Stress Test Kit. |
Overcoming resistance in cancer immunotherapy requires a deep understanding of immunoediting dynamics. Preclinical strategies must move beyond static models to incorporate evolving tumor-immune ecosystems. By integrating sophisticated in vivo resistance induction models, high-throughput functional genomics, multi-omic analyses, and advanced spatial profiling, researchers can deconvolute the mechanistic basis of both primary and acquired resistance. This systematic approach, grounded in the principles of immune surveillance, is essential for designing rational combination therapies that preempt or reverse resistance, leading to more durable clinical responses.
Bench to Bedside: Validating and Comparing Immunoediting Biomarkers and Models
Cancer immunoediting, comprising the three phases of elimination, equilibrium, and escape, provides the foundational context for understanding predictive biomarkers in immuno-oncology. Immune surveillance, primarily executed by CD8+ cytotoxic T lymphocytes (CTLs), is responsible for the elimination phase. Biomarkers such as PD-L1, Tumor Mutational Burden (TMB), CD8+ Tumor-Infiltrating Lymphocytes (TILs), and gene expression signatures (GES) each quantify different aspects of the dynamic host-tumor interaction. They reflect either the immune system's attempt to control the tumor (e.g., CD8+ TILs) or the tumor's adaptive escape mechanisms (e.g., PD-L1 upregulation). This analysis compares these biomarkers on technical, biological, and clinical validation grounds.
Table 1: Core Characteristics of Predictive Biomarkers
| Biomarker | Biological Significance | Typical Assay(s) | Common Cut-off(s) | Key Associated Therapies |
|---|---|---|---|---|
| PD-L1 Expression | Immune checkpoint ligand; indicates adaptive immune resistance | IHC (22C3, SP142, SP263, 28-8), RNA-Seq | Tumor Proportion Score (TPS) ≥1%, ≥50%; Immune Cell (IC) Score | Anti-PD-1/PD-L1 (Pembrolizumab, Atezolizumab) |
| Tumor Mutational Burden (TMB) | Proxy for neoantigen load; correlates with immunogenicity | Whole Exome Sequencing (WES), Targeted NGS Panels (e.g., FoundationOne CDx) | ≥10 mutations/Mb (high TMB) | Anti-PD-1/PD-L1 (Pembrolizumab in TMB-H solid tumors) |
| CD8+ TIL Density | Direct measure of cytotoxic anti-tumor effector immune cells | IHC (CD8 antibody), Multiplex IF/IHC, Flow Cytometry | Varies by cancer type; often median/quartile splits | Adoptive Cell Therapy, predictive for multiple ICIs |
| Gene Expression Signatures (GES) | Holistic capture of tumor microenvironment state; e.g., inflamed vs. excluded | RNA-Seq, Nanostring Panels (e.g., PanCancer IO 360) | Signature-specific scores (e.g., IFN-γ score, T-cell inflamed GEP) | Anti-PD-1 (Pembrolizumab in melanoma via T-cell inflamed GEP) |
Table 2: Clinical Performance & Limitations
| Biomarker | Key Strengths | Key Limitations | Standardization Status |
|---|---|---|---|
| PD-L1 | Clinically validated for multiple indications; IHC is routine. | Dynamic expression; intratumoral heterogeneity; multiple antibody clones. | Partial; companion diagnostics exist but are not interchangeable. |
| TMB | Agnostic to cancer type; strong biological rationale. | Cost of NGS; cutoff variability; influenced by sequencing panel size/algorithm. | Evolving; efforts by Friends of Cancer Research to harmonize. |
| CD8+ TILs | Direct functional relevance; spatial context via IHC/mIF. | Requires precise enumeration/ localization; dynamic; lacks universal scoring. | Low; consensus guidelines emerging from SITC/IJCP. |
| GES | Comprehensive; can define "hot" vs. "cold" tumors; captures functional state. | Requires high-quality RNA; complex data analysis; high dimensionality. | Low; multiple proprietary signatures; validation ongoing. |
Experimental Protocols for Key Assays
Protocol 3.1: PD-L1 Immunohistochemistry (IHC) Staining and Scoring (22C3 pharmDx)
- Tissue Sectioning: Cut 4-μm formalin-fixed, paraffin-embedded (FFPE) tumor sections.
- Deparaffinization & Rehydration: Bake slides, then treat with xylene and graded alcohols.
- Antigen Retrieval: Use EnVision FLEX Target Retrieval Solution, High pH (Agilent), at 97°C for 20 minutes.
- Primary Antibody Incubation: Apply mouse anti-human PD-L1 monoclonal antibody (clone 22C3) for 30 minutes at room temperature.
- Detection: Use EnVision FLEX+ detection system (horseradish peroxidase-labeled polymer). Apply DAB+ chromogen for 10 minutes.
- Counterstaining & Mounting: Counterstain with hematoxylin, dehydrate, and mount.
- Scoring (TPS): Calculate TPS = (Number of PD-L1 staining viable tumor cells / Total number of viable tumor cells) x 100%.
Protocol 3.2: TMB Assessment via Targeted Next-Generation Sequencing (NGS)
- DNA Extraction: Isolate high-quality genomic DNA from FFPE tumor tissue and matched normal blood/saliva.
- Library Preparation & Hybridization Capture: Fragment DNA, ligate adapters, and perform hybrid capture using a panel covering ~0.8-1.2 Mb of coding genome (e.g., FoundationOne CDx).
- Sequencing: Perform massively parallel sequencing on an Illumina platform to achieve >500x median coverage.
- Bioinformatics Pipeline:
- Alignment: Map reads to the human reference genome (hg19/GRCh37).
- Variant Calling: Identify somatic mutations (SNVs, indels) in the tumor compared to normal. Filter out germline polymorphisms and known sequencing artifacts.
- TMB Calculation: TMB (mutations/Mb) = (Total number of somatic, coding, base substitutions, and indels per megabase of genome examined). Exclude known driver mutations and synonymous variants.
Protocol 3.3: Multiplex Immunofluorescence (mIF) for CD8+ TILs and Spatial Analysis
- Slide Preparation: Cut 4-5 μm FFPE sections onto charged slides.
- Multiplex Staining Cycle (using Akoya Biosciences OPAL or similar): a. Round 1: Perform antigen retrieval, block, incubate with primary antibody (e.g., anti-CD8), then with HRP-conjugated secondary. Apply Opal fluorophore (e.g., Opal 520), then perform microwave treatment to strip antibodies. b. Repeat Rounds 2-n: For additional markers (e.g., PD-1, PD-L1, CK, DAPI), with distinct fluorophores.
- Image Acquisition: Scan slides using a multispectral imaging system (Vectra Polaris).
- Image & Data Analysis: Use inForm or HALO software for:
- Spectral Unmixing to separate fluorophore signals.
- Cell Segmentation and Phenotyping (identify CD8+ cells).
- Spatial Analysis (calculate densities, distances to tumor cells).
Diagrams of Signaling Pathways and Workflows
Title: PD-1/PD-L1 Checkpoint Inhibition Pathway
Title: TMB Leading to Immunogenicity and ICI Response
Title: Comparative Experimental Workflows for Key Biomarkers
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions
| Item / Reagent | Function & Application | Example Product/Clone (Research Use) |
|---|---|---|
| Anti-PD-L1 IHC Antibody | Detection of PD-L1 protein expression in FFPE tissue. Critical for correlative studies. | Clone 22C3 (Agilent), SP142 (Spring Bioscience), E1L3N (CST) |
| Anti-CD8 IHC/mIF Antibody | Identification and quantification of cytotoxic TILs. Enables spatial analysis. | Clone C8/144B (Agilent), SP16 (Spring), 4B11 (Leica) |
| Multiplex IF Detection Kit | Enables simultaneous detection of 6+ markers on one FFPE section for TME phenotyping. | Opal 7-Color Automation Kit (Akoya), UltraVIEW Dyes (PerkinElmer) |
| Targeted NGS Panel for TMB | Harmonized gene panel for somatic mutation calling and TMB calculation from FFPE DNA. | Oncomine Tumor Mutation Load Assay (Thermo Fisher), TruSight Oncology 500 (Illumina) |
| Gene Expression Profiling Panel | Targeted RNA measurement of immune-relevant genes for signature generation. | nCounter PanCancer IO 360 Panel (Nanostring), HTG EdgeSeq Immuno-Oncology Assay |
| Immune Cell Markers Antibody Panel | Flow cytometry characterization of dissociated tumor immune infiltrates. | Anti-human CD45, CD3, CD8, CD4, FoxP3, PD-1 (Multiple vendors) |
| DNA/RNA Co-isolation Kit | Simultaneous purification of nucleic acids from a single FFPE scroll for multi-omics. | AllPrep DNA/RNA FFPE Kit (Qiagen), RecoverAll Multi-Sample Kit (Thermo) |
| Spectral Imaging System | Captures multiplex IF images and performs spectral unmixing for quantitative analysis. | Vectra Polaris/PhenoImager (Akoya), ZEISS Axioscan 7 |
The paradigm of cancer immunoediting, encompassing the three phases of Elimination, Equilibrium, and Escape, provides the fundamental rationale for immunotherapy. Preclinical models are indispensable for dissecting these phases. However, their predictive validity for human clinical outcomes hinges on rigorous correlation with human genomic and immunologic data. This guide details the methodologies for such validation, ensuring preclinical findings are grounded in human biology.
Quantitative Landscape of Model-Human Discrepancies
Table 1: Comparative Genomics & Immunology of Common Preclinical Models
| Feature | Syngeneic Mouse Models | Patient-Derived Xenografts (PDXs) | Genetically Engineered Mouse Models (GEMMs) | Human Cancers (TCGA/ICGC) |
|---|---|---|---|---|
| Tumor Mutational Burden (TMB) | Low (~10-50 Mut/Mb) | Preserved from donor (~1-100 Mut/Mb) | Variable, often low | Highly variable (0.1 >600 Mut/Mb) |
| Neoantigen Landscape | Model-specific, limited diversity | Preserved human neoantigens | Mouse-specific, engineered | Complex, patient-unique |
| Immune Infiltrate Composition | Fully murine, intact adaptive immunity | Lacks human adaptive immunity in standard NSG hosts | Fully murine, develops de novo | Human, often suppressed/exhausted |
| Key Immunosuppressive Pathways | Mouse PD-1, CTLA-4, TIGIT | Limited human myeloid activity | Mouse-specific microenvironment | Complex (human PD-L1, IDO1, LAG-3, etc.) |
| Major Histocompatibility Complex | Mouse H-2 | Absent (human HLA lost in murine host) | Mouse H-2 | Polymorphic Human HLA |
Core Validation Methodologies
Protocol 1: Cross-Species Transcriptomic Alignment
Objective: To map gene expression signatures from murine models to conserved human pathways.
- RNA Sequencing: Isolate total RNA from tumor biopsies (model and human). Perform paired-end sequencing (Illumina NovaSeq, 150bp).
- Ortholog Mapping: Map murine genes to human orthologs using the Mouse Genome Informatics (MGI) homology database. Filter for one-to-one orthologs.
- Pathway Enrichment Analysis: For both species' datasets, perform Gene Set Enrichment Analysis (GSEA) using the MSigDB Hallmark and Immunologic Signatures collections.
- Correlation Metric: Calculate Spearman's rank correlation coefficient (ρ) between the normalized enrichment scores (NES) of conserved pathways across species.
Protocol 2: Neoantigen Similarity Assessment
Objective: Quantify the overlap between model-predicted and human-relevant neoantigens.
- Variant Calling: From model & human WES data, call somatic variants (MuTect2 for human, SomaticSniper for murine).
- Neoantigen Prediction: Use pVACseq pipeline. For mouse: binders to H-2 alleles (e.g., H-2-Db, H-2-Kb). For human: binders to patient-specific HLA alleles.
- Similarity Scoring: For shared driver mutations (e.g., KRAS G12D), compare the predicted binding affinity (netMHCpan %Rank) and the core peptide sequence homology. Develop a Neoantigen Conservation Index:
(# of conserved strong binders) / (total # of unique strong binders).
Protocol 3: Immune Contexture Validation via Multiplex IHC
Objective: To spatially validate immune cell infiltration patterns against human tissue.
- Panel Design: Design a 7-plex immunofluorescence panel (e.g., CD8, CD4, FoxP3, CD68, PD-L1, Pan-CK, DAPI).
- Staining & Imaging: Use the Akoya Biosciences Opal system on FFPE sections from murine and human tumor samples. Acquire whole-slide images (Vectra/Polaris).
- Spatial Analysis: Use inForm or QuPath software for cell segmentation and phenotyping. Calculate densities (cells/mm²) and spatial metrics (e.g., distance of CD8+ T cells to nearest tumor cell).
- Validation Benchmark: Compare the immune "phenotype" (e.g., inflamed, excluded, desert) classification between the model and its matched human cancer subtype.
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 2: Key Research Reagent Solutions for Validation
| Reagent/Platform | Provider Example | Function in Validation |
|---|---|---|
| FOXP3 / RORγt Reporter Mice | Jackson Laboratory | Visualize and isolate specific Treg or Th17 subsets in syngeneic/GEMM models to compare with human T cell states. |
| Humanized MHC (HLA) Transgenic Mice | Taconic Biosciences | Evaluate human tumor antigen-specific T cell responses in vivo using human HLA restriction. |
| CITE-seq/TotalSeq Antibodies | BioLegend | Simultaneously measure protein expression (e.g., immune checkpoints) and transcriptome in single cells from model tumors, aligning to human scRNA-seq clusters. |
| Multiplex IHC Panels (Opal) | Akoya Biosciences | Standardized, quantitative spatial profiling of immune cells in FFPE tissues from both models and patients. |
| CellTrace Proliferation Dyes | Thermo Fisher | Track tumor-infiltrating lymphocyte proliferation and dynamics ex vivo, correlating with human TIL functional assays. |
| Oncopanel NGS Assays | Illumina/Dana-Farber | Target sequencing of >300 cancer genes for consistent variant calling across model and human samples. |
| Neoantigen Peptide Pools | GenScript | Synthesize predicted neoantigens from model tumors to test cross-reactivity with T cells from human PBMCs or tumor digests. |
Pathway Validation: Mouse vs. Human PD-1/PD-L1 Axis
Interpretation: While the core PD-1/PD-L1 signaling pathway is conserved, the validation step requires confirming that specific antibodies/therapeutics targeting the human proteins (PDCD1, CD274) cross-react with or are mirrored by tools for the murine orthologs (Pdcd1, Cd274) in the model system. Discrepancies in expression regulation or binding affinity must be quantified.
Systematic validation, bridging model systems and human data, is not a final step but an integral, iterative component of preclinical cancer immunology research. It directly tests the relevance of discoveries made within the Elimination-Equilibrium-Escape framework. By employing the genomic, computational, and spatial protocols outlined here, researchers can significantly de-risk the translation of immunotherapeutic strategies from bench to bedside.
The cancer immunoediting hypothesis delineates three sequential phases: elimination, equilibrium, and escape. While elimination represents initial immune-mediated tumor destruction and escape characterizes outgrowth of immunoevasive clones, the equilibrium phase is a prolonged, clinically undetectable state where adaptive immunity exerts dynamic, selective pressure on tumor cells without achieving eradication. This review evaluates the clinical manifestations of equilibrium—specifically tumor dormancy and late recurrence—and explores the therapeutic paradigm of adaptive therapy, which aims to deliberately maintain a stable tumor burden rather than pursue maximal cell kill. This discussion is framed within the foundational principles of immune surveillance, where the immune system functions as a central extrinsic tumor suppressor.
Quantitative Analysis of Equilibrium Phenomena
Table 1: Clinical Evidence for Dormancy and Late Recurrence Across Cancer Types
| Cancer Type | Median Time to Late Recurrence (Years) | Estimated % of Recurrences Classified as "Late" (>5 years) | Key Immune Correlates (if measured) | Supporting Studies (Examples) |
|---|---|---|---|---|
| Breast Cancer (ER+) | 10 - 20+ | 30-50% | High TILs in primary tumor; persistent disseminated tumor cells (DTCs) in bone marrow with low MHC-I. | Mansi et al., 2020; Aguirre-Ghiso, 2018 |
| Renal Cell Carcinoma | 10 - 15 | ~10% | T cell exhaustion signatures; angiogenic dormancy signals. | Uzzo et al., 2021 |
| Melanoma | 5 - 15 | 5-15% | Presence of tumor-infiltrating lymphocytes (TILs) and IFN-γ signatures. | Tarhini et al., 2019 |
| Prostate Cancer | 7 - 15+ | 20-40% | Inflammatory microenvironment with TGF-β and IFN signaling. | Gomella et al., 2022 |
Table 2: Key Molecular Regulators of Tumor Dormancy
| Regulator Category | Specific Factor/Pathway | Proposed Function in Maintaining Dormancy | Experimental Model |
|---|---|---|---|
| Microenvironmental Signals | TGF-β, Bone Morphogenetic Proteins (BMPs) | Induce G0/G1 cell cycle arrest in disseminated tumor cells (DTCs). | In vivo mouse models (e.g., 4T1, MDA-MB-231) |
| Immune Effectors | CD8+ T cells, IFN-γ, NK cells | Cytostatic control via pSTAT1/p27 signaling; direct killing of proliferating clones. | Syngeneic mouse models (e.g., B16, CT26) |
| Angiogenic Switch | Thrombospondin-1 (TSP-1), angiostatin | Inhibition of neovascularization, enforcing avascular micrometastasis. | Dormancy models in lung/liver. |
| Tumor Cell Intrinsic | NR2F1, DEC2, p38α/β MAPK | Upregulation of stemness and quiescence programs; stress response. | In vitro 3D dormancy models. |
Experimental Protocols for Investigating Equilibrium
Protocol 1: In Vivo Modeling of Immunomediated Dormancy
- Model Generation: Inject immunocompetent mice (e.g., C57BL/6) with a low dose (e.g., 10^5 cells) of syngeneic, immunogenic tumor cells (e.g., B16OVA melanoma, CT26 colon carcinoma) via intravenous (for systemic dormancy) or subcutaneous (for primary site control) route.
- Monitoring: Use in vivo bioluminescence imaging (BLI) weekly for 60-100 days to track tumor burden. A stable, low-level signal indicates potential equilibrium.
- Immune Depletion: To confirm immune maintenance of dormancy, administer depleting antibodies (e.g., anti-CD8α, anti-CD4, anti-IFN-γ) or use knockout mice (e.g., Rag2^-/-). Loss of equilibrium and outgrowth validate the model.
- Endpoint Analysis: Harvest organs (lung, liver, bone marrow) for histological analysis (H&E, immunohistochemistry for Ki-67, CD3) and flow cytometry to characterize immune infiltrate and tumor cell phenotype.
Protocol 2: Isolation and Profiling of Disseminated Tumor Cells (DTCs) from Bone Marrow
- Sample Collection: Obtain human bone marrow aspirates from early-stage cancer patients (e.g., breast, prostate) in remission.
- Enrichment: Use density gradient centrifugation (Ficoll-Paque) to isolate mononuclear cells (MNCs).
- Tumor Cell Detection/Isolation: Stain MNCs with antibodies against epithelial markers (e.g., EpCAM, Cytokeratins) and lineage-specific markers (e.g., HER2 for breast), excluding hematopoietic markers (CD45). Use fluorescence-activated cell sorting (FACS) to isolate pure DTC populations.
- Downstream Analysis:
- Single-Cell RNA-seq: Profile transcriptomes to identify quiescence (e.g., p27, NR2F1) and immune evasion signatures.
- Ex Vivo Co-culture: Co-culture DTCs with autologous or allogeneic T cells to assess immunogenicity and T-cell mediated killing/proliferation suppression.
Signaling Pathways in Equilibrium and Escape
Adaptive Therapy: A Clinical Application of Equilibrium Principles
Adaptive therapy shifts the treatment goal from maximum cell kill to long-term tumor control by exploiting competitive interactions between drug-sensitive and -resistant subclones. The strategy involves modulating drug dosing (dose, frequency, holidays) based on real-time tumor response to maintain a stable population of therapy-sensitive cells that suppress the outgrowth of resistant clones.
Table 3: Clinical Trials of Adaptive Therapy Paradigms
| Cancer Type | Therapeutic Agent | Adaptive Strategy | Primary Outcome | Status/Reference |
|---|---|---|---|---|
| Metastatic Castration-Resistant Prostate Cancer | Abiraterone Acetate | Dose interruption/reduction based on PSA levels, maintaining PSA at 50% of baseline. | Extended time to progression vs. standard continuous dosing. | Phase II (NCT02415621), Zhang et al., 2022 |
| BRAF-Mutant Melanoma | BRAF/MEK Inhibitors | Drug holidays based on radiographic tumor volume, allowing for regrowth of drug-sensitive cells. | Delayed emergence of resistance, improved overall survival in preclinical models. | Preclinical/Phase I concepts. |
| Ovarian Cancer | Paclitaxel | Low-dose, frequent metronomic dosing to maintain stable disease via anti-angiogenic effects. | Improved progression-free survival in subset analyses. | Various metronomic therapy trials. |
Experimental Protocol: Preclinical Adaptive Therapy Simulation
- Cell Line Preparation: Establish a mixed-population xenograft or syngeneic model comprising both drug-sensitive (e.g., parental) and drug-resistant (e.g., engineered with resistance mutation) tumor cells (e.g., 75:25 ratio).
- Treatment Arms:
- Control: Continuous maximum tolerated dose (MTD).
- Adaptive Arm: Administer therapy only when tumor volume increases by a pre-set threshold (e.g., 20% from nadir). Cease treatment upon regression to baseline/nadir volume.
- Monitoring: Measure tumor volume 2-3 times weekly. Perform serial biopsies or liquid biopsy (ctDNA) at decision points to assess clonal dynamics via ddPCR or NGS.
- Analysis: Compare time to treatment failure, overall survival, and final clonal composition between arms.
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Reagents for Investigating Tumor Dormancy and Equilibrium
| Reagent/Solution | Provider Examples (for identification) | Function in Research |
|---|---|---|
| Recombinant Human/Mouse Cytokines (TGF-β1, IFN-γ, BMPs) | PeproTech, R&D Systems | Used in in vitro assays to induce dormancy-like quiescence in tumor cell cultures. |
| Phospho-Specific Antibodies (pSTAT1, p-p38 MAPK, p27) | Cell Signaling Technology, Abcam | Detection of activated signaling pathways in dormant tumor cells via flow cytometry or IHC. |
| MHC Tetramers/Pentamers (for specific tumor antigens) | MBL International, ProImmune | Tracking and isolation of antigen-specific T cells from models of equilibrium. |
| In Vivo Depleting/Antibody Blocks (anti-CD8α, anti-CD4, anti-IFN-γ, anti-PD-1) | Bio X Cell, InvivoGen | Functionally validating the role of specific immune components in maintaining dormancy in vivo. |
| Luciferase-Expressing Tumor Cell Lines | ATCC, generated via lentiviral transduction (e.g., pGL4.50[luc2]) | Enables sensitive, longitudinal tracking of minimal residual disease and tumor burden in live animals. |
| Quiescence-Sensitive Dyes (e.g., CellTrace Violet, PKH26) | Thermo Fisher Scientific, Sigma-Aldrich | Tracking cell division history; non-dividing (dormant) cells retain bright dye signal. |
| Bone Marrow Disseminated Tumor Cell (DTC) Enrichment Kits (EpCAM/CD45 based) | Miltenyi Biotec, StemCell Technologies | Isolation of rare DTC populations from bone marrow for downstream molecular analysis. |
| 3D Extracellular Matrix (ECM) for Culture (Matrigel, Collagen I) | Corning, Cultrex | Creating physiologically relevant in vitro models to study microenvironment-induced dormancy. |
Cancer immunoediting is the fundamental process encompassing three phases: elimination, equilibrium, and escape. Immune surveillance, a component of the elimination phase, represents the body's intrinsic defense against malignant transformation. The efficacy of immunotherapeutic drugs hinges on their ability to modulate this complex interplay. Consequently, preclinical drug screening mandates the use of immunocompetent models that recapitulate the intact host immune system and the tumor-immune microenvironment (TIME). This guide provides a technical comparison of prevalent immunocompetent models, evaluating their predictive power for clinical translation.
Table 1: Comparison of Key Immunocompetent Mouse Models
| Model Type | Genetic Background | Immune System Fidelity | Tumor Origin | Throughput | Cost | Key Strengths | Key Limitations | Predictive Correlation (Estimated) |
|---|---|---|---|---|---|---|---|---|
| Syngeneic Models | Inbred (e.g., C57BL/6, BALB/c) | Fully intact, murine | Mouse tumor cell line (e.g., MC38, 4T1) | High | Low | Intact, reproducible TIME; high throughput | Non-human antigens; limited genetic diversity | Moderate (Immune activation) |
| Genetically Engineered Mouse Models (GEMMs) | Various, often mixed | Fully intact, murine | De novo (autochthonous) | Very Low | Very High | Spontaneous, heterogeneous tumors; native TIME | Long latency, high variability, low throughput | High (Tumor-immune evolution) |
| Humanized Immune System Models | Immunodeficient host (e.g., NSG) engrafted with human cells | Reconstituted human immune system | Human tumor cell line or PDX | Moderate | High | Enables study of human-specific therapeutics and immune components | Incomplete reconstitution; lack of murine stromal cues; graft-vs-host disease risk | Moderate-High (Human target engagement) |
| Carcinogen-Induced Models | Inbred or outbred | Fully intact, murine | De novo (induced by e.g., DMBA) | Low | Moderate | Recapitulates environmental carcinogenesis; immune-competent | Multiorgan toxicity; variable tumorigenesis | Moderate (Inflammation-linked cancer) |
Table 2: Quantitative Efficacy Metrics Across Models (Example Drug: Anti-PD-1)
| Model Type | Typical Tumor Growth Inhibition (TGI) Range | Treatment Response Rate | Median Survival Increase | Immune Cell Infiltration (Post-Rx) | Reference Clinical Correlation |
|---|---|---|---|---|---|
| MC38 Syngeneic (C57BL/6) | 60-90% | 40-60% | 50-100% | High CD8+ T-cell influx | Moderate for CPI response |
| GEMM (e.g., KPC pancreatic) | 30-70% | 20-40% | 30-80% | Variable, often suppressive | High for therapy-resistant phenotypes |
| HIS + Hu-PDX (NSG) | 40-80% | 30-50% | N/A (endpoint often tumor volume) | Human T-cells detected | High for target validation on human immune cells |
Experimental Protocols for Key Model Utilization
Protocol 1: Establishing and Treating a Syngeneic Tumor Model
Objective: To evaluate the efficacy of an immune checkpoint inhibitor in immunocompetent mice.
- Animal Preparation: House 8-10 week old female C57BL/6 mice under specific pathogen-free conditions.
- Cell Preparation: Cultivate MC38 colon carcinoma cells in DMEM + 10% FBS. Harvest at 80% confluence, wash, and resuspend in PBS at 5 x 10^6 cells/mL on ice.
- Inoculation: Inject 100 µL of cell suspension (5 x 10^5 cells) subcutaneously into the right flank using a 27-gauge needle.
- Randomization & Treatment: Palpate tumors until they reach ~50 mm³ (Volume = 0.5 x length x width²). Randomize mice into control (IgG) and treatment (anti-PD-1) groups (n=10). Administer 200 µg of antibody via intraperitoneal injection every 3 days for 4 cycles.
- Monitoring: Measure tumors bi-weekly with calipers. Euthanize when tumor volume exceeds 1500 mm³ or at protocol endpoint.
- Analysis: Excise tumors, process for flow cytometry (immune profiling) and histology (IHC for CD3, CD8, FoxP3).
Protocol 2: Drug Screening in a Humanized Immune System Model
Objective: To test a human-specific immunomodulatory drug.
- Humanization: Irradiate NOD-scid IL2Rγ[null] (NSG) mice with 1 Gy. Inject 1x10^5 human CD34+ hematopoietic stem cells via tail vein.
- Immune Reconstitution Validation: At 12-16 weeks, retro-orbitally bleed mice. Assess human immune cell (hCD45+) engraftment via flow cytometry (>25% in peripheral blood is acceptable).
- Tumor Engraftment: Subcutaneously implant a human tumor cell line (e.g., A375 melanoma) or a fragment of a patient-derived xenograft (PDX) into humanized mice.
- Treatment: Once tumors are established (~100 mm³), randomize and treat with human-targeted therapeutic (e.g., anti-human PD-1). Use an isotype control.
- Endpoint Analysis: Measure tumor growth. Harvest tumors and blood for analysis of human immune cell subsets (e.g., hCD8+/hCD4+ T cells) and cytokine levels (e.g., human IFN-γ).
Visualizations: Pathways and Workflows
Title: Immunoediting Phases and Model Predictive Power
Title: PD-1/PD-L1 Checkpoint Blockade Mechanism
Title: Immunocompetent Model Screening Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Immunocompetent Model Research
| Reagent Category | Specific Example(s) | Function in Experiment | Key Considerations |
|---|---|---|---|
| Syngeneic Cell Lines | MC38 (colon), 4T1 (breast), B16-F10 (melanoma) | Provide immunogenic murine tumors for implantation in matched mouse strains. | Select based on genetic background (C57BL/6 vs. BALB/c) and immunogenicity. |
| Checkpoint Inhibitor Antibodies | InVivoMab anti-mouse PD-1 (CD279), anti-mouse CTLA-4 | Function-blocking antibodies to modulate the murine immune system in syngeneic/GEMM studies. | Use purified, endotoxin-free, carrier-free formulations for in vivo use. |
| Humanization Components | CD34+ Hematopoietic Stem Cells (HSCs), PBMCs | To reconstitute a human immune system in immunodeficient mice (e.g., NSG). | Source (cord blood vs. mobilized peripheral blood), donor variability, and HSC quality are critical. |
| Flow Cytometry Antibody Panels | Anti-mouse: CD45, CD3, CD4, CD8, FoxP3, CD11b, Gr-1, F4/80. Anti-human: hCD45, hCD3, hCD19, hCD56. | For comprehensive immune phenotyping of tumor infiltrates, spleen, and blood. | Optimize multi-color panels for spectral overlap; include viability dye. |
| Tumor Dissociation Kits | GentleMACS or similar enzymatic (Collagenase/DNase) dissociation systems | To generate single-cell suspensions from solid tumors for downstream analysis (flow, sequencing). | Protocol must balance yield with preservation of surface markers, especially on immune cells. |
| In Vivo Imaging Agents | Luciferin (for bioluminescent cells), Fluorescent dyes (DiR, ICG) | Enables non-invasive, longitudinal tracking of tumor growth and metastasis. | Requires prior engineering of tumor cells (luciferase) or use of labeled probes. |
| Multiplex Cytokine Assays | LEGENDplex or Luminex-based mouse or human cytokine panels | Quantifies a broad spectrum of soluble immune mediators from serum or tumor homogenate. | Essential for assessing systemic and local immune activation or suppression. |
Conclusion
The framework of cancer immunoediting provides an indispensable lens through which to view the dynamic interplay between tumors and the immune system. A deep understanding of the foundational Three E's phases, coupled with robust methodological approaches, is critical for therapeutic innovation. Success requires meticulous troubleshooting of model systems and a clear path for validating preclinical discoveries against clinical realities. The future of the field lies in moving beyond static biomarkers to dynamic, integrated models that can predict patient-specific trajectories through the immunoediting process. This will enable the rational design of combination therapies that not only block escape but also actively reprogram the tumor microenvironment, potentially re-engaging the equilibrium or elimination phases for durable clinical benefit. The ongoing challenge is to translate this sophisticated biological understanding into reliable and personalized clinical strategies.