Cancer Stem Cell Markers: Navigating Identification Challenges and Therapeutic Opportunities
This article provides a comprehensive overview for researchers, scientists, and drug development professionals on the critical role of Cancer Stem Cells (CSCs) in tumor persistence, relapse, and therapy resistance.
Cancer Stem Cell Markers: Navigating Identification Challenges and Therapeutic Opportunities
Abstract
This article provides a comprehensive overview for researchers, scientists, and drug development professionals on the critical role of Cancer Stem Cells (CSCs) in tumor persistence, relapse, and therapy resistance. It explores the foundational biology of CSCs, detailing key stemness markers and their origins. The content covers current methodological approaches for CSC identification and isolation, addresses significant challenges in the field such as marker heterogeneity and plasticity, and evaluates emerging validation strategies using advanced technologies like single-cell sequencing and genome-wide CRISPR screens. The review synthesizes these insights to discuss future therapeutic avenues and the movement towards personalized cancer medicine.
The Biology of Cancer Stem Cells: Origins, Markers, and Stemness Pathways
The cancer stem cell (CSC) niche represents a specialized, anatomically distinct microenvironment within tumors that is essential for maintaining CSC properties, including self-renewal capacity, clonal tumor initiation, and clonal long-term repopulation potential [1]. Analogous to niches that regulate normal stem cells, the CSC niche provides critical cues through cell-cell contacts, secreted factors, and physical interactions that preserve CSC phenotypic plasticity, protect CSCs from immune surveillance, and facilitate metastatic spread [1] [2]. This niche constitutes a fundamental component of the broader tumor microenvironment (TME), comprising various stromal elements including fibroblastic cells, immune cells, endothelial and perivascular cells, extracellular matrix (ECM) components, and intricate networks of cytokines and growth factors [1]. The bidirectional communication between CSCs and their niche creates a dynamic ecosystem that not only sustains tumor progression but also presents significant challenges for therapeutic interventions, as CSCs residing within these protective niches demonstrate remarkable resilience to conventional cancer treatments including immunotherapy [1] [2].
Cellular and Molecular Composition of the CSC Niche
The CSC niche is a complex, multi-faceted microenvironment composed of diverse cellular populations and molecular components that collectively support CSC maintenance and function.
Cellular Components
- Immune Cells: The niche contains various immune cell types that typically exhibit immunosuppressive properties. These include tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs) [3] [2]. These cells create an immune-privileged sanctuary for CSCs by suppressing anti-tumor immune responses.
- Cancer-Associated Fibroblasts (CAFs): CAFs are key stromal cells that support CSCs through the secretion of growth factors, cytokines, and ECM components [3]. They actively participate in creating and maintaining the niche structure.
- Mesenchymal Stem Cells (MSCs): MSCs can migrate to tumor sites and influence cancer progression through multiple mechanisms. They release various bioactive factors that influence CSC stemness, drug resistance, and phenotype maintenance [3]. In ovarian cancer, MSCs produce BMP4 and BMP2, thereby amplifying the CSC population [3].
- Endothelial and Perivascular Cells: These vascular components contribute to niche function by supporting CSC maintenance and participating in angiogenic processes [1].
Molecular Components
- Extracellular Matrix (ECM): The ECM provides structural support and biochemical signals that influence CSC behavior. It serves as a reservoir for growth factors and cytokines and modulates mechanotransduction pathways [1].
- Secreted Factors: The niche is rich in various signaling molecules including cytokines (e.g., IL-6, IL-8), chemokines, growth factors (e.g., VEGF, TGF-β), and metabolites that regulate CSC self-renewal and survival [3] [4]. These factors can be freely released or encapsulated in extracellular vesicles.
- Exosomes and Extracellular Vesicles (EVs): CSCs and niche cells release EVs that enable the transfer of biomolecular cargos between different cell types, facilitating intercellular communication and modulation of the TME [4].
Table 1: Key Cellular Constituents of the CSC Niche and Their Functions
| Cell Type | Primary Functions in CSC Niche | Representative Signaling Molecules |
|---|---|---|
| TAMs/MDSCs | Create immunosuppressive environment; promote CSC survival | IL-10, TGF-β, ARG1 [3] [2] |
| Tregs | Suppress antitumor immunity; inhibit T-cell function | IL-10, TGF-β, CTLA-4 [3] [2] |
| CAFs | ECM remodeling; secrete growth factors; metabolic support | HGF, CXCL12, TGF-β [3] [4] |
| MSCs | Enhance stemness; increase CSC population; metabolic modulation | BMP4, BMP2, exosomes [3] |
| Endothelial Cells | Vascular niche formation; promote CSC self-renewal | Notch ligands, EGF, Angiopoietins [1] |
Functional Dynamics: How the Niche Influences CSC Behavior
The CSC niche employs multiple mechanisms to maintain CSC stemness, promote therapy resistance, and facilitate immune evasion.
Maintenance of Stemness and Plasticity
The niche actively maintains CSC stemness through the provision of specific molecular signals that activate key developmental pathways. These include Wnt/β-catenin, Notch, and Hedgehog signaling pathways, which are crucial for regulating self-renewal and differentiation [4]. The concept of CSC plasticity—the dynamic ability of CSCs to transition between stem-like and differentiated states in response to external stimuli—is fundamentally regulated by niche-derived signals [2]. Under therapeutic pressure or environmental stressors, the niche can promote dedifferentiation of non-CSCs back into the CSC pool, contributing to tumor heterogeneity and therapeutic resistance [1] [3]. This plasticity represents a sophisticated adaptive mechanism that allows tumors to survive diverse therapeutic assaults.
Therapy Resistance and Immune Evasion
The niche provides a physical sanctuary that protects CSCs from conventional therapies and immune-mediated attack. CSCs within their niche employ multiple intrinsic and extrinsic mechanisms to evade immune surveillance:
- Immune Checkpoint Expression: CSCs frequently upregulate immune checkpoint proteins such as PD-L1, which binds to PD-1 on T cells, inhibiting their activation and function [2]. Other checkpoints including B7-H4, B7-H3, CD47, and CD24 are also utilized by CSCs to evade immune surveillance [2].
- Antigen Presentation Downregulation: CSCs often downregulate major histocompatibility complex (MHC) class I molecules, reducing their visibility to cytotoxic T lymphocytes [2].
- Soluble Factor Secretion: CSCs and niche cells secrete immunosuppressive factors including TGF-β, IL-10, and prostaglandin E2 that actively dampen antitumor immune responses [2] [4].
- Metabolic Adaptations: CSCs exhibit metabolic plasticity, allowing them to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids based on environmental conditions [5]. This adaptability enhances their survival under metabolic stress induced by therapies.
Table 2: CSC Immune Evasion Mechanisms Facilitated by the Niche
| Evasion Mechanism | Molecular Players | Functional Outcome |
|---|---|---|
| Immune Checkpoint Upregulation | PD-L1, B7-H4, CD47, CD24 | Suppression of T-cell function; inhibition of phagocytosis [2] |
| Reduced Antigen Presentation | Downregulated MHC class I | Decreased recognition by cytotoxic T cells [2] |
| Immunosuppressive Secretome | TGF-β, IL-10, PGE2 | Recruitment of Tregs and MDSCs; T-cell inhibition [2] [4] |
| Metabolic Competition | Nutrient consumption; lactate secretion | Creation of metabolically hostile TME for immune cells [5] |
Experimental Approaches for CSC Niche Characterization
Advanced methodologies are required to dissect the complex architecture and function of the CSC niche.
Single-Cell and Spatial Analysis Technologies
Single-cell RNA sequencing (scRNA-seq) enables the resolution of cellular heterogeneity within the CSC niche by providing transcriptomic profiles of individual cells [5] [6]. This approach has revealed significant differences in immune cell composition between extramedullary multiple myeloma TME and bone marrow counterparts, identifying T and NK cells as the most abundant immune subsets with distinct functional states [6]. Spatial transcriptomics complements scRNA-seq by preserving the geographical context of cellular interactions, allowing researchers to map the precise localization of CSCs within their niche [5] [6]. These technologies collectively facilitate the identification of unique gene expression patterns and cell-cell communication networks that define the niche.
Artificial Intelligence in TME Analysis
Artificial intelligence (AI) approaches are increasingly employed to characterize the TME and CSC niche from standard histopathological images. The HistoTME platform represents a novel weakly supervised deep learning approach that can infer TME composition directly from hematoxylin and eosin (H&E)-stained histopathology images [7]. This method accurately predicts the expression of 30 distinct cell type-specific molecular signatures and can classify tumor microenvironments into immune phenotypes such as "Immune-Inflamed" and "Immune-Desert" with clinical relevance for predicting immunotherapy response [7].
AI-Based TME Analysis Workflow
CSC Marker Identification and Validation
The identification and validation of CSC markers within their native niche context remains challenging due to CSC heterogeneity and plasticity. Methodologies include:
- Multiple Immunohistochemistry: Simultaneous staining for multiple putative CSC markers (e.g., p75NTR, ALDH1A1, BMI1) enables the visualization of different CSC subpopulations and their spatial relationships within the niche [8]. This approach has revealed that multiple stem cell subpopulations with distinct phenotypes can co-exist within a tumor, each impacting different clinical parameters [8].
- Flow Cytometry and FACS: Fluorescence-activated cell sorting (FACS) allows for the isolation and functional characterization of CSC subpopulations based on surface marker expression [8]. Studies demonstrate that CSC subpopulations identified by different markers are dynamic populations capable of phenotypic switching, with p75NTR+ cells exhibiting higher expression of proliferative and self-renewal markers compared to ALDH1A1+ cells [8].
- 3D Organoid Models: Three-dimensional organoid cultures recapitulate key aspects of the CSC niche in vitro, enabling the investigation of CSC-stroma interactions in a more physiologically relevant context [5].
Table 3: Essential Research Reagents for CSC Niche Characterization
| Research Reagent | Primary Function | Experimental Application |
|---|---|---|
| Anti-p75NTR Antibody | CSC surface marker detection | IHC, Flow Cytometry for CSC identification [8] |
| Anti-ALDH1A1 Antibody | Intracellular CSC marker detection | IHC, identifies ALDH1A1+ CSC subpopulation [8] |
| Anti-BMI1 Antibody | Self-renewal marker detection | IHC, evaluation of CSC self-renewal capacity [8] |
| Anti-Ki67 Antibody | Proliferation marker detection | IHC, assessment of CSC proliferative status [8] |
| CD44, CD133 Antibodies | CSC surface marker detection | Flow Cytometry, CSC isolation and enrichment [5] [9] |
| CRISPR-based Screens | Functional genomics | Identification of essential niche factors [5] |
Signaling Pathways Governing CSC-Niche Interactions
The functional interplay between CSCs and their niche is mediated by evolutionarily conserved signaling pathways that regulate stemness, survival, and adaptation.
Core Stemness Pathways
- Wnt/β-catenin Signaling: The canonical Wnt pathway serves as a vital regulator of tumor cell plasticity [4]. Activation of this pathway enhances the expression of CSC surface markers and promotes self-renewal, while also contributing to immune evasion through positive feedback loops with PD-L1 expression [2] [4].
- Notch Signaling: The Notch pathway regulates stem cell differentiation and self-renewal, with aberrant signaling stimulating CSC self-renewal in various cancers including ovarian, breast, and hepatocellular carcinoma [4]. Epigenetic regulation through histone modifications further modulates NOTCH1 signaling in CSCs [4].
- Hedgehog Signaling: The Hedgehog pathway drives tumor growth, invasion, and recurrence following therapeutic intervention [4]. In colorectal cancer, cancer-initiating cells express the Indian hedgehog (IHH) gene, which contributes to their maintenance [4].
Integrin-Mediated Niche Interactions
Integrins function as critical mediators of CSC-niche adhesion and signaling. These heterodimeric cell surface receptors promote cell proliferation, differentiation, adhesion to ECM, and migration by sensing the cellular microenvironment [4]. Specific integrins have been implicated in CSC biology:
- Integrin α6: Strongly expressed in glioblastoma cells and used as a biomarker for CSC identification [4].
- Integrin αVβ3: Implicated in developing resistance to receptor tyrosine kinase inhibitors in lung cancer [4].
- Integrin α3: Shows context-dependent functions, inhibiting metastasis in prostate cancer while promoting invasion in glioblastoma [4].
Signaling Pathways in CSC-Niche Crosstalk
Therapeutic Implications and Targeting Strategies
Targeting the CSC niche represents a promising therapeutic approach to overcome treatment resistance. Several strategies are under investigation:
- Dual Metabolic Inhibition: Targeting the metabolic plasticity of CSCs through combination approaches that simultaneously inhibit multiple metabolic pathways [5].
- Niche-Disrupting Agents: Therapeutic interventions aimed at disrupting the protective niche microenvironment, thereby sensitizing CSCs to conventional treatments [1] [10].
- Immune-Based Approaches: Engineering immune cells such as CAR-T cells to target CSC-specific markers, and developing immune checkpoint inhibitors specific to CSC-expressed checkpoints [5] [2].
- Synthetic Biology-Based Interventions: Utilizing advanced engineered systems to precisely target CSC-niche interactions [5].
The integrative targeting of both CSCs and their niche components holds significant promise for developing more effective cancer therapies that can overcome the formidable challenges posed by therapy resistance and tumor recurrence.
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with unique self-renewal capacity, differentiation potential, and resistance to conventional therapies, driving tumor initiation, progression, metastasis, and recurrence [11]. The concept of CSCs has evolved significantly since its initial formulation, with contemporary research revealing complex origins and dynamic behavior. The cellular origin of CSCs remains a fundamental question in cancer biology, with compelling evidence indicating two primary sources: transformed tissue-resident stem cells or dedifferentiated mature cells that reacquire stem-like properties [12]. This cellular plasticity allows non-CSCs to regain stemness characteristics under specific environmental pressures, creating a dynamic hierarchy within tumors that complicates therapeutic targeting [5] [2]. Understanding these origins provides crucial insights into the molecular mechanisms driving tumor heterogeneity, therapy resistance, and disease recurrence, offering potential avenues for more effective cancer interventions that address the root sources of tumor propagation and resilience.
Dual Origin Theory of Cancer Stem Cells
The initiation of CSCs can follow two distinct pathways, each with implications for tumor behavior and therapeutic response. The transformation process involves overexpression of oncogenes and inactivation of tumor suppressors, leading to uncontrolled growth and the acquisition of stem cell characteristics [12].
Origin from Tissue-Resident Stem Cells
Tissue-resident stem cells, with their inherent self-renewal capabilities and prolonged lifespan, represent natural candidates for CSC transformation. These cells already possess the molecular machinery for unlimited proliferation, potentially requiring fewer genomic alterations for malignant transformation compared to differentiated cells [12]. Research across multiple cancer types supports this origin model:
- Gastric cancers: Slow-cycling Mist1-expressing cells in the gastric corpus and Lgr5-expressing cells in the gastric antrum have been identified as cells of origin [12].
- Squamous cell carcinomas: Basal stem cells in trachea and main bronchi self-renew and form heterogeneous spheres, potentially leading to hyperplasia and eventual squamous cell carcinoma [12].
- Hematological malignancies: In acute myeloid leukemia (AML), the cell of origin is typically a hematopoietic stem or progenitor cell, while in chronic myeloid leukemia (CML), it is characterized by Bcr-Abl oncogene expression in stem/progenitor cells [12].
The differentiation phenotype and aggressiveness of resulting tumors appear influenced by the specific tissue-resident stem cell population of origin. For example, in breast cancer, tumors originating from luminal progenitors are generally associated with better prognosis, while those from basal-like progenitors display more aggressive phenotypes [12].
Origin from Differentiated Cells via Dedifferentiation
Differentiated cells can undergo transformation into CSCs through dedifferentiation processes, regaining stem-like properties through genetic and epigenetic alterations:
- Colon cancers: Studies demonstrate that differentiated intestinal epithelial cells can potentially become CSCs under certain conditions [12].
- Liver cancer: Cell tracking studies show that hepatocytes (mature liver cells) can serve as cells of origin for liver cancer [12].
- Cellular plasticity: Non-CSCs can acquire stem-like features in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure [5] [2].
This dedifferentiation process challenges the notion of a fixed CSC hierarchy and highlights the dynamic nature of stemness in cancer, representing a transient functional state rather than a static subpopulation [5].
Table 1: Comparative Features of CSC Origins Across Cancer Types
| Cancer Type | Tissue-Resident Stem Cell Origin | Differentiated Cell Origin | Key Evidence |
|---|---|---|---|
| Gastric Cancer | Mist1+ cells, Lgr5+ cells | Not specified | Mouse models showing stem cell transformation [12] |
| Colon Cancer | Not specified | Differentiated intestinal epithelial cells | Lineage tracing studies [12] |
| Liver Cancer | Hepatoblasts, hepatic progenitors | Adult hepatocytes | Cell tracking, in vivo studies [12] |
| Breast Cancer | Luminal progenitors, basal-like progenitors | Not specified | Association with differentiation phenotypes [12] |
| Leukemia | Hematopoietic stem/progenitor cells | Lymphoid progenitors (in some AML) | Expression profiling, transplantation models [12] |
Molecular Mechanisms and Signaling Pathways in CSC Biology
CSCs utilize complex molecular pathways to maintain their stemness properties and survival advantages. Understanding these mechanisms is crucial for developing targeted therapeutic approaches.
Core Stemness Signaling Pathways
Multiple evolutionarily conserved signaling pathways play pivotal roles in regulating CSC self-renewal, differentiation, and survival:
- Wnt/β-catenin signaling: Regulates CSC maintenance and interacts with immune checkpoint proteins like PD-L1, creating feedback loops that enhance both stemness and immune evasion [2] [11].
- Hedgehog signaling: Contributes to CSC self-renewal and tissue patterning, often dysregulated in various cancers [11].
- Notch signaling: Mediates cell-cell communication and fate decisions, maintaining CSC populations in multiple cancer types [11].
- JAK/STAT pathway: Particularly STAT3 activation, promotes survival and proliferation of CSCs [11].
- TGF-β/SMAD signaling: Regulates epithelial-mesenchymal transition (EMT) and stemness acquisition [11].
- PI3K/AKT/mTOR pathway: Integrates metabolic and growth signals to support CSC survival under stress conditions [11].
These pathways form interconnected networks that sustain CSC populations and create therapeutic resistance. Their plasticity allows CSCs to adapt to therapeutic pressure and environmental changes, maintaining tumor propagating capacity despite targeted interventions [5] [11].
Metabolic Adaptations of CSCs
CSCs exhibit remarkable metabolic plasticity that enables survival under diverse environmental conditions. This adaptability represents a key mechanism of therapy resistance:
- Metabolic flexibility: CSCs can switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids depending on environmental conditions [5].
- Lip metabolism adaptations: Alterations in fatty acid oxidation (FAO) and lipogenesis support CSC resilience under stress [11].
- Metabolic symbiosis: Interactions with stromal cells, immune components, and vascular endothelial cells facilitate metabolic cooperation that promotes CSC survival [5].
This metabolic plasticity allows CSCs to persist despite therapies that target specific metabolic pathways, making them a persistent reservoir for tumor recurrence [5].
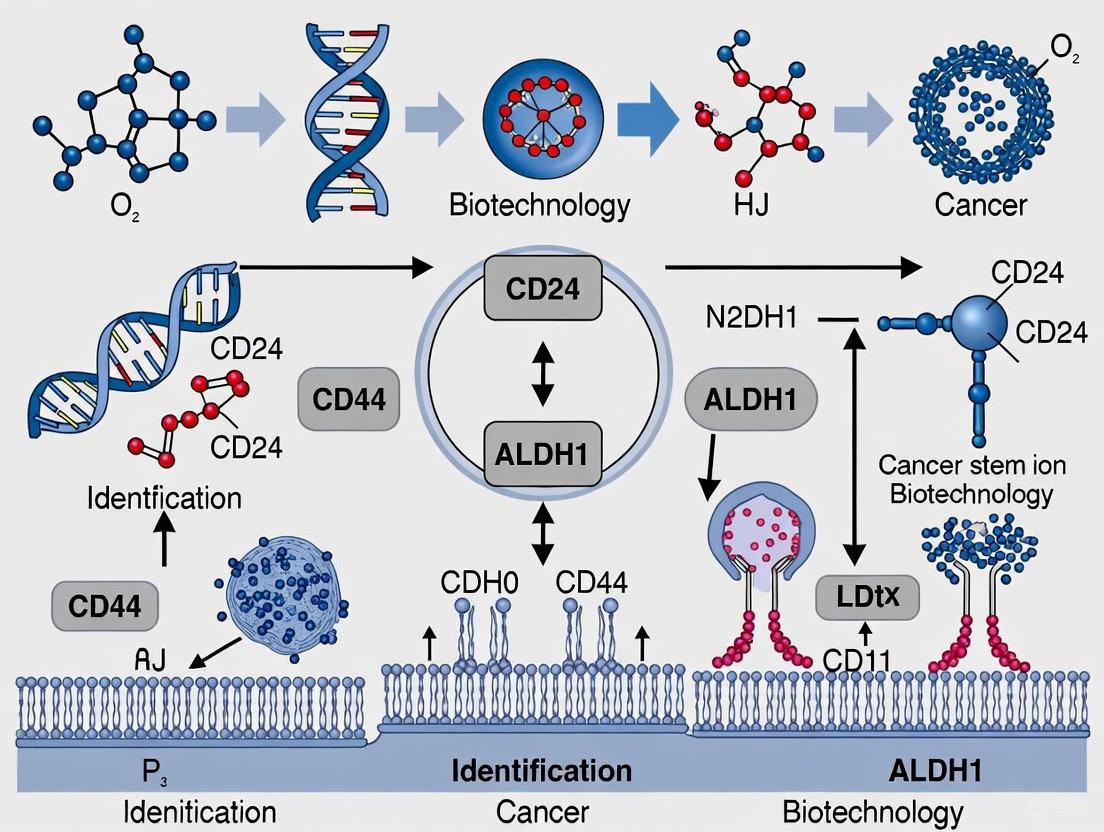
Diagram 1: CSC Origins and Signaling Pathways. This diagram illustrates the dual origins of CSCs and the core signaling pathways that maintain their stemness properties.
CSC Markers and Identification Challenges
The reliable identification and isolation of CSCs remains a significant challenge in cancer research due to marker heterogeneity and dynamic expression patterns.
Established and Emerging CSC Markers
Several cell surface proteins and functional markers have been employed to identify and isolate CSC populations across different cancer types:
- CD44: A hyaluronic acid receptor widely used as a CSC marker in multiple cancers including breast, pancreatic, and head and neck cancers [5] [11].
- CD133 (Prominin-1): A transmembrane glycoprotein marking CSC populations in glioblastoma, colon cancer, and others [5] [11].
- ALDH1 (Aldehyde Dehydrogenase 1): An intracellular detoxifying enzyme with high activity in CSCs of various cancers, detected via Aldefluor assay [8] [11].
- EpCAM (Epithelial Cell Adhesion Molecule): Used as a CSC marker in prostate and gastrointestinal cancers [5].
- CD24: Functions as an immune checkpoint by binding Siglec-10 on macrophages while also serving as a CSC marker [2].
- CD47: A "don't eat me" signal molecule upregulated in leukemia and other CSCs to evade phagocytosis [2].
These markers are often used in combination to enrich for CSC populations, though their expression varies significantly across cancer types and even within individual tumors [5] [8].
Challenges in CSC Marker Interpretation
Several critical challenges complicate the use of these markers for CSC identification:
- Lack of universal markers: No single marker is exclusively expressed by CSCs across different cancer types, and marker expression patterns are influenced by tissue origin and microenvironmental context [5].
- Marker heterogeneity: Multiple stem cell subpopulations with distinct phenotypes can coexist within a single tumor, each impacting different clinical parameters [8].
- Dynamic plasticity: CSC subpopulations identified by different markers represent dynamic populations capable of switching phenotypes over time [8].
- Non-specificity: Most markers expressed in CSCs are also found in normal stem cells or non-tumorigenic cancer cells, complicating specific targeting [5] [12].
Table 2: Common CSC Markers Across Cancer Types and Their Limitations
| Marker | Cancer Types | Functional Role | Limitations/Challenges |
|---|---|---|---|
| CD44 | Breast, pancreatic, HNSCC | Hyaluronan receptor, adhesion, signaling | Also expressed on normal stem cells and immune cells [5] |
| CD133 | Glioblastoma, colon cancer | Transmembrane glycoprotein, function not fully understood | Expression varies with tumor stage and hypoxia [5] |
| ALDH1 | Breast, colon, OSCC | Detoxifying enzyme, retinoic acid metabolism | Isoform-specific functions, technical variability in detection [8] |
| EpCAM | Prostate, GI cancers | Cell adhesion, signaling | Widespread epithelial expression limits targeting specificity [5] |
| p75NTR | OSCC, melanoma, esophageal | Nerve growth factor receptor | Heterogeneous expression within tumors [8] |
| LGR5 | Gastric cancer | Wnt pathway regulator, stem cell marker | Limited to specific cancer types and locations [12] |
Methodological Approaches for CSC Identification and Validation
Robust experimental frameworks are essential for accurate CSC characterization, combining surface marker analysis with functional validation.
Core Methodologies for CSC Isolation and Characterization
- Surface marker-based isolation: Flow cytometry enables precise enrichment of CSC subpopulations using specific marker combinations such as CD44+CD24-/low in breast cancer or CD34+CD38- in AML [5] [11].
- Aldefluor assay: Detects elevated aldehyde dehydrogenase (ALDH) activity, allowing fluorescence-based separation of ALDH-high cells with stem-like properties [11].
- Sphere formation assays: When cultured in serum-free, non-adherent conditions, CSCs generate three-dimensional spheres, reflecting self-renewal capacity and stemness maintenance over multiple passages [11].
- In vivo tumorigenicity assays: The gold standard for CSC validation, wherein sorted cells are injected into immunocompromised mice to evaluate tumor-initiating potential, with minimal cell populations often sufficient to generate tumors [11].
These methodologies establish a framework for identifying and characterizing CSCs, bridging molecular observations with clinically relevant phenotypes. Integration of these approaches provides complementary evidence for CSC properties and functions [11].
Advanced Technologies in CSC Research
Emerging technologies are refining our ability to characterize CSCs and their dynamic behavior:
- Single-cell sequencing: Enables characterization of CSC heterogeneity and stem-like features at unprecedented resolution [5].
- CRISPR-based functional screens: Identify genes essential for CSC maintenance and survival [5].
- Patient-derived organoids (PDOs): Bridge the gap between in vitro cell lines and in vivo models, preserving tumor heterogeneity and enabling precision medicine approaches [11].
- AI-driven multiomics analysis: Integrates complex datasets to identify CSC vulnerabilities and predictive biomarkers [5].
Diagram 2: Experimental Workflow for CSC Identification. This diagram outlines the key methodological approaches for isolating and validating cancer stem cells.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for CSC Studies
| Reagent/Material | Primary Function | Application Examples | Technical Considerations |
|---|---|---|---|
| Fluorescently-labeled antibodies (CD44, CD133, EpCAM) | Surface marker detection and FACS isolation | Immunophenotyping, CSC enrichment | Validation for specific applications essential [11] |
| Aldefluor assay kit | Detection of ALDH enzyme activity | Functional identification of CSCs | Requires specific inhibition controls [11] |
| Serum-free sphere culture media | Support CSC growth in non-adherent conditions | Sphere formation assays, CSC expansion | Formulations often require growth factor supplementation [11] |
| Matrigel/ECM components | 3D culture substrate | Organoid generation, invasion assays | Batch variability requires standardization [11] |
| Immunodeficient mice (NSG, NOG) | In vivo tumorigenicity studies | Limiting dilution assays, therapeutic testing | Strain-specific engraftment characteristics [11] |
| Single-cell RNA sequencing kits | Transcriptomic profiling | Heterogeneity analysis, subpopulation identification | Requires fresh viable cells, computational expertise [5] |
Understanding the dual origins of CSCs from both tissue-resident stem cells and dedifferentiated cells has profound implications for cancer therapy development. The dynamic plasticity of CSCs and their ability to transition between stem-like and differentiated states represents a significant challenge for targeted therapies [2]. Furthermore, the presence of multiple CSC subpopulations with distinct phenotypes within individual tumors suggests that effective therapeutic approaches will need to address this heterogeneity [8]. Emerging strategies such as dual metabolic inhibition, immune-based approaches using CAR-T cells targeting CSC markers like EpCAM, and niche-targeting agents show promise in overcoming CSC-mediated therapy resistance [5] [2]. However, major challenges remain in targeting CSCs without affecting normal stem cells and in developing reliable biomarkers for patient stratification [5]. Moving forward, integrative approaches combining metabolic reprogramming, immunomodulation, and targeted inhibition of CSC vulnerabilities will be essential for developing effective CSC-directed therapies that address both the origins and adaptive capabilities of these critical tumor-propagating cells.
Core stemness transcription factors—OCT4, SOX2, NANOG, and SALL4—constitute a critical regulatory network that maintains pluripotency in embryonic stem cells. In oncogenesis, these factors are re-expressed and drive cancer stem cell (CSC) pathogenesis, contributing to tumor initiation, therapeutic resistance, and metastatic dissemination. This whitepaper delineates the molecular functions, interrelationships, and clinical relevance of these factors, framing them within the significant challenge of CSC identification and targeting. Supported by contemporary research, we provide methodologies for their investigation and discuss their emerging role as biomarkers and therapeutic targets in precision oncology.
Cancer stem cells (CSCs) are a minor subpopulation within tumors endowed with self-renewal, differentiation capacity, and enhanced resistance to conventional therapies, thereby driving tumor relapse and metastatic spread [5] [13]. The CSC hypothesis posits that a hierarchical organization exists within tumors, with CSCs at its apex, and their identification remains a central challenge in oncology [14]. A major obstacle is the lack of universal CSC markers, as surface proteins like CD44 and CD133 are not exclusive to CSCs and vary significantly across tumor types [5].
Attention has therefore shifted to intrinsic molecular regulators of stemness, particularly the core transcription factors OCT4 (Octamer-binding transcription factor 4), SOX2 (SRY-box transcription factor 2), NANOG (Nanog homebox), and SALL4 (Spalt-like transcription factor 4). These factors are paramount for maintaining pluripotency and self-renewal in embryonic stem cells (ESCs) [15] [16]. After development, their expression is largely silenced in adult tissues but is aberrantly re-activated in numerous cancers [14] [16]. They form a complex interconnected regulatory network that promotes the CSC phenotype, and their expression is frequently correlated with aggressive disease, resistance to treatment, and poor prognosis [17] [15]. Thus, understanding these factors is crucial for advancing CSC research and developing novel therapeutic strategies.
Molecular Functions and Interrelationships
The core transcription factors do not operate in isolation but form a tightly knit, self-reinforcing network that maintains pluripotency and stemness.
The Core Pluripotency Network (OCT4, SOX2, NANOG)
OCT4, SOX2, and NANOG form a critical core circuit that auto-regulates and co-occupies target gene promoters to sustain the pluripotent state [15] [18]. OCT4 is a POU-family transcription factor essential for maintaining the self-renewal of ESCs; its precise expression level is critical, as deviation can lead to differentiation [16]. SOX2, an HMG-box transcription factor, frequently co-operates with OCT4, forming heterodimers on composite DNA elements to regulate a common set of target genes, including their own promoters [18]. NANOG, a homeodomain protein, functions as a key determinant of pluripotency by blocking differentiation pathways [15]. This core circuit is reinforced by direct protein-protein interactions between the factors. For instance, research has demonstrated that OCT4, SOX2, and NANOG each individually form complexes with nucleophosmin (Npm1), a protein highly expressed in ESCs, suggesting a mechanism for their coordinated activity in maintaining the stem cell phenotype [18].
SALL4 as an Integrative Regulator
SALL4 is a zinc-finger transcription factor that serves as a vital integrator within the pluripotency network. Similar to the core factors, SALL4 is highly expressed in ESCs and is mostly silenced in adult tissues, with expression restricted to germ cells [16]. It participates in an interconnected autoregulatory loop with OCT4, SOX2, and NANOG, where each factor can regulate its own expression and that of the others [16]. SALL4 is known to antagonize OCT4's activation function to balance its expression level, fine-tuning the network [16]. Furthermore, SALL4 is a downstream target of the canonical WNT signaling pathway, positioning it as a nexus that integrates external signals with the core transcriptional machinery [16]. Its function is critical, as SALL4-null embryos do not survive beyond embryonic day E6.5 [16].
Table 1: Core Stemness Transcription Factors: Functions and Interactions
| Transcription Factor | Key Structural Features | Primary Molecular Function | Key Interaction Partners |
|---|---|---|---|
| OCT4 | POU DNA-binding domain | Maintains self-renewal; prevents differentiation [18] | SOX2, NANOG, Npm1, SALL4 [16] [18] |
| SOX2 | HMG-box domain | Cooperates with OCT4; regulates shared target genes [18] | OCT4, NANOG, Npm1, SALL4 [16] [18] |
| NANOG | Homeodomain | Blocks differentiation; sustains pluripotency [15] | OCT4, SOX2, Npm1, SALL4 [16] [18] |
| SALL4 | Multiple zinc-finger clusters | Integrates signals (e.g., WNT); fine-tunes core network [16] | OCT4, SOX2, NANOG, epigenetic modifiers [16] |
Experimental Analysis and Methodologies
Investigating the expression and function of core stemness factors requires a multifaceted approach. Below is a detailed protocol for assessing protein-protein interactions, a key methodology for understanding the functional network.
Protocol: Detecting Protein-Protein Interactions viaIn SituProximity Ligation Assay (PLA)
The in situ PLA technique allows for the visualization of direct protein-protein interactions within the cellular context with high specificity and sensitivity [18].
1. Sample Preparation and Staining:
- Cell Culture: Grow embryonic stem cells (ESCs) or CSCs on sterile glass coverslips in appropriate medium.
- Fixation and Permeabilization: Fix cells with 4% paraformaldehyde for 15 minutes at room temperature. Permeabilize cells with 0.1% Triton X-100 in PBS for 10 minutes.
- Blocking: Incubate cells with a blocking solution (e.g., 10% goat serum in PBS) for 1 hour at room temperature to prevent non-specific antibody binding.
2. Primary Antibody Incubation:
- Incubate the fixed and permeabilized cells with pairs of primary antibodies raised in different host species targeting the proteins of interest (e.g., rabbit anti-OCT4 and mouse anti-Npm1) [18].
- Dilute antibodies in blocking buffer according to their optimal concentrations (e.g., 1:1600 for OCT4 [17]) and incubate overnight at 4°C.
3. PLA Probe Incubation and Ligation:
- After washing, incubate the samples with secondary antibodies (PLA probes) conjugated to unique DNA oligonucleotides. These are typically anti-mouse MINUS and anti-rabbit PLUS probes.
- Perform a ligation reaction by adding a connector oligonucleotide that hybridizes to the two PLA probes. Only if the two target proteins are in close proximity (<40 nm) will the circle be completed by a DNA ligase.
4. Amplification and Detection:
- Amplify the ligated DNA circle through rolling-circle amplification using a fluorescently labelled nucleotide (e.g., Alexa Fluor 594).
- Counterstain the cell nuclei with Hoechst 33342 or DAPI.
- Mount the coverslips and visualize the red fluorescent signals (each representing a single protein-protein interaction event) using confocal microscopy [18].
Troubleshooting Notes:
- High Background: Optimize antibody concentrations and increase the stringency of washes. Include a no-primary-antibody control.
- No Signal: Validate antibody compatibility for immunostaining and PLA. Ensure all enzymatic reaction steps are performed correctly.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Investigating Core Stemness Factors
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Validated Antibodies | Rabbit anti-OCT4 (C52G3, CST) [17]; Mouse anti-SOX2 (L1D6A2, CST) [17]; Mouse anti-NANOG (1E6C4, CST) [17] | Immunofluorescent staining, Western blot, co-immunoprecipitation for protein detection and interaction studies. |
| Cell Culture Models | Embryonic Stem Cells (ESCs); Induced Pluripotent Stem (iPS) cells; Patient-derived CSC organoids [5] | In vitro models for studying stemness mechanisms, differentiation, and drug screening. |
| Gene Manipulation Tools | CRISPR-Cas9; shRNA vectors for knockdown [5] [16] | Functional studies to determine the role of specific factors in self-renewal and pluripotency. |
| Detection Kits | In Situ PLA Kits (e.g., Duolink) [18] | Sensitive detection of protein-protein interactions in situ. |
| Differentiation Inducers | Retinoic Acid; Dimethyl Sulfoxide (DMSO); LIF Withdrawal [18] | Tools to induce differentiation and study the downregulation of stemness factors. |
Clinical and Prognostic Significance in Cancer
The expression of OCT4, SOX2, NANOG, and SALL4 in cancers is not merely incidental but is strongly correlated with aggressive clinicopathological features and poor patient outcomes, underscoring their prognostic utility.
A pivotal 2017 study on rectal cancer (RC) patients provides compelling quantitative evidence. The study demonstrated that tumor tissue expressions of OCT4, SOX2, and NANOG were significantly higher than in adjacent normal tissues (p<0.001 for OCT4 and NANOG, p=0.003 for SOX2) [17]. Critically, OCT4 expression was positively correlated with pathological grade (R=0.185, p=0.022), tumor size (R=0.224, p=0.005), and lymph node metastasis (N stage, R=0.170, p=0.036). NANOG expression was also positively associated with larger tumor size (R=0.169, p=0.036) [17]. Kaplan-Meier survival analysis revealed that OCT4 positivity was associated with significantly worse overall survival (OS) compared to OCT4-negative patients (p<0.001). Furthermore, the study established that having at least two positive markers was associated with shorter OS, and patients with all three markers positive had the worst prognosis [17]. Multivariate Cox analysis confirmed OCT4 as an independent prognostic factor for shorter OS (p<0.001) [17].
This prognostic significance extends beyond gastrointestinal cancers. A 2025 systematic review of salivary gland malignancies confirmed that the immunohistochemical expression of SOX2, OCT4, and NANOG is linked to tumor aggressiveness and poor prognosis, suggesting their combined assessment could serve as a powerful tool for risk stratification [15]. SALL4, as an oncofetal protein, is also re-expressed in various aggressive cancers, including hepatocellular carcinoma and leukemias, and its presence is often a marker of poor differentiation and treatment resistance [16].
Table 3: Prognostic Correlations of Core Stemness Factors in Human Cancers
| Transcription Factor | Cancer Type(s) Studied | Correlation with Clinicopathological Features | Impact on Survival |
|---|---|---|---|
| OCT4 | Rectal Cancer [17] | Poor differentiation, Larger tumor size, Higher N stage [17] | Independent predictor of shorter overall survival [17] |
| SOX2 | Rectal Cancer, Salivary Gland Malignancies [17] [15] | Overexpression in tumor vs. normal tissue [17] [15] | Not an independent factor in RC; associated with aggressiveness in SGM [17] [15] |
| NANOG | Rectal Cancer, Salivary Gland Malignancies [17] [15] | Larger tumor size (RC) [17] | Not an independent factor in RC; prognostic in SGM [17] [15] |
| SALL4 | Hepatocellular Carcinoma, Leukemias [16] | Poor differentiation, Therapy resistance [16] | Marker of aggressive disease and poor outcome [16] |
Therapeutic Targeting and Future Perspectives
Targeting the core stemness pathway network represents a frontier in overcoming therapy resistance and preventing cancer relapse. The inherent challenges include the plasticity of CSCs, the lack of unique surface markers, and the risk of on-target toxicity against normal stem cells [5] [13]. Several promising strategies are under investigation.
1. Direct Transcriptional Targeting: A major focus is developing inhibitors that disrupt the function of these transcription factors or their upstream regulators. This includes targeting the key signaling pathways (Wnt/β-catenin, Notch, and Hedgehog) that sustain the expression and activity of the core network [13] [19]. For instance, molecular targeting of OCT4 and its associated pathways is being explored to sensitize CSCs to conventional therapies [20].
2. Immunological Approaches: Chimeric Antigen Receptor (CAR) T-cell therapies and cancer vaccines are being designed to target CSC-specific antigens. While identifying unique targets is difficult, the shared expression of these factors with ESCs offers a potential avenue, albeit with safety challenges. Preclinical studies targeting EpCAM, a marker associated with CSCs, have shown promise [5]. The development of "Boolean logic" CAR T-cells that require recognition of two CSC-associated markers to activate is a promising strategy to enhance specificity and spare normal tissues [21].
3. Combination Therapies: Given the resilience and adaptability of CSCs, the most viable strategy may be combining conventional cytoreductive therapies (chemotherapy, radiation) with novel agents that specifically target the CSC population. This approach aims to eradicate the bulk tumor while disabling the engine of recurrence and metastasis [19]. Experts forecast that advances in 2025 will include the clinical evaluation of such combinatorial approaches, alongside improved biomarkers for patient selection [21].
The following diagram illustrates the interconnected regulatory relationships and external pathways influencing the core stemness factors, highlighting potential therapeutic intervention points.
Diagram Title: Core Stemness Factor Network and Therapeutic Targeting
The core stemness transcription factors OCT4, SOX2, NANOG, and SALL4 are central orchestrators of the pluripotent state in ESCs and are critically re-activated in CSCs. They form a robust, self-reinforcing network that promotes self-renewal, inhibits differentiation, and confers formidable resistance to conventional cancer therapies. Their expression provides valuable prognostic information and represents a promising, though challenging, avenue for therapeutic intervention. Future research, leveraging single-cell multi-omics, advanced organoid models, and AI-driven analysis, will be essential to decode the context-specific functions of these factors and translate this knowledge into effective CSC-targeted therapies that can ultimately improve long-term patient survival [5] [21].
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [5]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies. The reliable identification and isolation of CSCs represent a fundamental challenge in cancer research, as the absence of universal CSC markers and significant heterogeneity across tumor types complicates their study [5] [13]. Among the numerous biomarkers investigated, four surface markers—CD44, CD133, ALDH1, and ICAM1—have emerged as particularly significant across multiple cancer types. These markers facilitate not only the identification of CSCs but also participate in critical functional mechanisms including maintenance of stemness, immune evasion, and therapeutic resistance. This technical guide provides an in-depth analysis of these four key markers, detailing their biological functions, expression patterns, methodological approaches for detection, and their interrelationships within the CSC signaling network, framed within the context of ongoing challenges in CSC marker research.
Marker Profiles and Functional Significance
CD44: A Multifunctional CSC Marker with Immunological Significance
CD44, a transmembrane glycoprotein receptor for hyaluronic acid, is one of the most extensively studied cancer stem cell markers across numerous malignancies. It plays a crucial role in cell-to-cell and cell-to-matrix adhesion, while also participating in angiogenesis, invasion, and migration in oral and oropharyngeal cancer [22]. CD44 exists as a standard isoform (CD44s) or alternatively spliced variant isoforms (CD44v), with these variants frequently undergoing alternative splicing to support cancer progression and are associated with poor survival [23].
Recent pan-cancer analyses have revealed that elevated CD44 expression correlates with tumor stage and prognosis in several different cancers [23]. Gene Set Enrichment Analysis (GSEA) results demonstrate that upregulated CD44 involves cancer stem cell-associated processes, antigen processing and presentation, and immune cell proliferation and activation [23]. CD44 plays an essential role in tumor immune regulation and immune checkpoint inhibitor response, with its expression positively correlated with regulatory CD4 T cells, macrophages M1 and M2 in several analyzed cancers [23]. In terms of diagnostic utility, studies in oral and oropharyngeal squamous cell carcinoma (OOSCC) have demonstrated distinctive expression patterns across differentiation states, with strong CD44 immunopositivity observed in 29 out of 31 well-differentiated OOSCC cases, while none of the poorly differentiated OOSCC cases showed strong staining intensity [22]. This pattern of decreasing CD44 expression from well-differentiated to poorly differentiated OSCC highlights its context-dependent expression and potential role in maintaining differentiated phenotypes in certain cancer types [22].
Table 1: CD44 Expression Patterns and Clinical Correlations Across Cancers
| Cancer Type | Expression Pattern | Clinical Correlation | Technical Notes |
|---|---|---|---|
| Oral & Oropharyngeal SCC | Strong in well-differentiated (29/31 cases); decreases with dedifferentiation | Statistically significant correlation with histological grade (p < 0.05) [22] | IHC staining intensity graded strong, moderate, or weak |
| Pan-Cancer Analysis | Upregulated in multiple cancer types | Correlates with tumor stage, prognosis, and immune infiltration [23] | Bioinformatics analysis of TCGA data |
| Triple-Negative Breast Cancer & NSCLC | Positively regulates PD-L1 expression | Potential role in immune checkpoint regulation [23] | Binds to regulatory region of PD-L1 locus |
CD133 (PROM1): A Conserved Stem Cell Glycoprotein
CD133 (prominin-1), a pentaspan transmembrane glycoprotein, is widely expressed in the stem cell population of various tumor types and represents one of the most extensively studied CSC markers [24]. In colorectal cancer (CRC), CD133 serves as a reliable marker for identifying cancer stem-like cells, with CD133+ cells demonstrating higher proliferation, colony-forming ability, drug resistance, and tumorigenicity compared to CD133- cells [25]. These functional characteristics confirm the stem-like properties of CD133+ populations and their critical role in tumor maintenance and progression.
In early-stage non-small cell lung cancer (NSCLC), CD133 is significantly upregulated in tumor tissues compared with adjacent normal tissues and healthy controls [24]. Its high expression correlates with poor differentiation, larger tumor size (≥3 cm), lymph node metastasis, and advanced stage (IB-IIA) [24]. The diagnostic performance of CD133 in NSCLC is robust, with ROC analysis showing an AUC of 0.809, demonstrating its value as a diagnostic biomarker [24]. When combined with OCT4, another stemness marker, the diagnostic accuracy improves substantially (AUC=0.893), with combined sensitivity of 88.7% and specificity of 82.5% [24]. From a prognostic perspective, patients with high CD133 expression exhibit markedly reduced 2-year overall survival compared with low-expression cases, and multivariate Cox regression identifies high CD133 expression as an independent prognostic risk factor (HR=2.45, 95% CI: 1.38-4.36, P=0.003) [24].
Table 2: CD133 Diagnostic and Prognostic Performance Across Studies
| Study Context | Diagnostic Performance | Prognostic Value | Key Findings |
|---|---|---|---|
| Early-stage NSCLC (80 patients) | AUC: 0.809; Combined with OCT4: AUC=0.893 [24] | HR=2.45, 95% CI: 1.38-4.36, P=0.003 [24] | Independent prognostic factor; associated with aggressive disease |
| Colorectal Cancer (multiple cell lines) | Reliable identification of CRC stem-like cells [25] | Associated with metastasis and relapse [25] | CD133+ cells show higher proliferation, drug resistance, and tumorigenicity |
ALDH1: Metabolic Marker of Stemness
Aldehyde dehydrogenase 1 (ALDH1) represents a functional CSC marker based on enzymatic activity rather than surface expression alone. ALDH1 is a detoxifying enzyme responsible for the oxidation of intracellular aldehydes and exists in different isoforms, with the ALDEFLUOR assay system specifically developed to detect ALDH1 isoform activity [26]. This enzymatic activity-based identification approach provides a complementary method to surface marker detection for isolating putative CSCs.
The ALDEFLUOR assay was originally developed for identifying ALDH-expressing hematopoietic stem cells but has since been adapted for solid tumors [26]. The assay detects cells with high ALDH enzyme activity, which characterizes stem and progenitor cells across various tissues. In breast cancer research, ALDH-positive cells isolated from human breast tumors contain CSCs capable of generating tumors in NOD/SCID mice, while ALDH-negative cells lack this tumor-initiating capacity [26]. Similar findings have been reported in CSCs from the colon, brain, and liver [26]. The expression of ALDH varies between different types of cell lines, with SKBR3 cells serving as a positive control due to high ALDH expression, while MCF7 cells express little to no ALDH and can function as a negative control [26]. Optimal staining conditions for the ALDEFLUOR assay require incubation between 30-45 minutes in a 37°C water bath, as extended incubation (60 minutes) diminishes ALDH staining intensity [26].
Recent advancements in ALDH detection include the development of novel fluorescent probes such as AldeCou1-4, designed using a coumarin-linker-benzaldehyde scaffold [27]. Among these, AldeCou-1 exhibits a significant Stokes shift of 125 nm (λex/λem = 380/505 nm), which enhances the signal-to-noise ratio and minimizes inner-filter effects [27]. Compared to conventional ALDH activity assay kits like ALDEFLUOR, which require additional buffers and inhibitors that complicate imaging protocols, AldeCou-1 enables simplified assay conditions by eliminating the need for ATP-binding cassette (ABC) transporter inhibitors and specialized buffers [27].
ICAM1: Emerging Regulator of CSC Stemness and Immune Evasion
Intercellular adhesion molecule 1 (ICAM1) has recently emerged as a key regulator of CSC stemness and tumorigenicity, particularly in glioblastoma (GBM), where it promotes an immunosuppressive microenvironment via β-catenin/PD-L1 signaling [28]. ICAM1 is a cell surface glycoprotein typically expressed on endothelial cells and specific leukocytes, historically known for facilitating endothelial-leukocyte transmigration through its interaction with lymphocyte function-associated antigen 1 (LFA-1) and macrophage antigen 1 (MAC-1) [28].
In GBM, ICAM1 overexpression is associated with adverse patient outcomes, with elevated levels observed in various patient-derived GBM stem cells (GSCs) [28]. Mechanistically, ICAM1 interacts with ZNRF3, leading to its autoubiquitination and clearance, which stabilizes LRP6 and activates β-catenin signaling, subsequently upregulating PD-L1 expression [28]. This ICAM1/β-catenin/PD-L1 signaling axis establishes a critical link between stemness maintenance and immune evasion in GBM. ICAM1's role extends to the recurrent GBM setting, where hypoxic conditions induce endothelial cells to upregulate ICAM1 expression, facilitating the recruitment of bone marrow-derived macrophages (BMDMs) [29]. Concurrently, endothelial-derived CCL2 induces the expression of adrenomedullin (ADM) in BMDMs, and this macrophage-derived ADM subsequently accelerates angiogenesis in endothelial cells while enhancing the proliferation and migration of tumor cells [29]. This feedforward loop in the endothelial-BMDM-tumor cell axis provides mechanistic insights into the tumor microenvironment of recurrent GBM.
Therapeutic targeting of ICAM1 in combination with immune checkpoint blockade shows promising results. Combined treatment with anti-ICAM1 and anti-PD-1 antibodies results in the most effective tumor inhibition and significantly extends survival in ICAM1-overexpressing GBM models [28]. CyTOF and flow cytometry analyses reveal that ICAM1 overexpression reduces cytotoxic CD8+ T cell populations via PD-L1/PD-1 interactions, an effect reversible by PD-1 blockade [28].
Table 3: ICAM1 Expression and Functional Roles in GBM
| Aspect | Findings | Experimental Evidence |
|---|---|---|
| Expression Pattern | Elevated in recurrent GBM and specific GSC lines (528, 83, GSC209) [28] | scRNA-seq, flow cytometry, IHC |
| Stemness Regulation | Maintains self-renewal, proliferation, and tumorigenicity of GSCs [28] | Knockdown reduces sphere formation; overexpression enhances it |
| Immune Modulation | Reduces CD8+ T cell populations via PD-L1/PD-1 [28] | CyTOF, flow cytometry, reversible by PD-1 blockade |
| Therapeutic Targeting | Combined anti-ICAM1 + anti-PD-1 most effective [28] | Mouse GBM models showing survival extension |
Methodological Approaches for CSC Marker Analysis
Immunohistochemistry (IHC) Protocols
Immunohistochemistry represents a fundamental methodology for detecting CSC markers in tissue sections, providing spatial context that is crucial for understanding tumor heterogeneity. A standardized IHC protocol for CD44 and similar markers involves several critical steps [22] [24]:
Tissue Section Processing: Formalin-fixed, paraffin-embedded tissue sections are cut at 4μm thickness, mounted on glass slides, and baked at 60°C for 2 hours. Deparaffinization is performed with xylene (2×10 minutes), followed by gradient rehydration using 100%, 95%, 85%, and 75% ethanol (5 minutes each). After rinsing with tap water, antigen retrieval is performed using 0.01 mol/L citrate buffer (pH 6.0) heated in a microwave at medium-high power for 10 minutes, then naturally cooled to room temperature. Endogenous peroxidase activity is blocked by incubating with 3% hydrogen peroxide for 10 minutes at room temperature, followed by PBS washing (3×) [24].
Antibody Incubation and Staining: Slides are incubated with normal goat serum blocking solution for 20 minutes at room temperature to block non-specific binding. Primary antibodies are then applied: for CD133 (Abcam, Cat# ab19898, dilution 1:200) and OCT4 (Abcam, Cat# ab19857, dilution 1:150) as an example [24]. Slides are incubated in a humid chamber at 4°C overnight, followed by PBS washes and application of HRP-conjugated secondary antibody incubated at room temperature for 30 minutes. DAB is used for color development (3-8 minutes), monitored under a microscope for optimal effect. Hematoxylin counterstaining is performed for 30 seconds, followed by dehydration, clearing, and mounting [24].
Interpretation of Staining Results: Evaluation should be performed by two experienced pathologists independently in a double-blinded manner. A semi-quantitative scoring method is recommended, with total score = staining intensity × percentage of positive cells. Staining intensity is scored as: no color (0), light yellow (1), brown-yellow (2), or brown (3). Positive cell percentage is scored as: <5% (0), 5-25% (1), 26-50% (2), 51-75% (3), or >75% (4). The total score ranges from 0 to 12, with scores ≥6 typically defined as "high expression" and <6 as "low expression" [24].
Flow Cytometry and Cell Sorting
Flow cytometry enables quantitative analysis and sorting of live CSC populations based on surface marker expression. The following protocols detail specific approaches for different markers:
ALDEFLUOR Assay for ALDH1 Activity Detection: The ALDEFLUOR assay requires pre-warming cell culture medium, Trypsin-EDTA, D-PBS and all ALDEFLUOR Kit reagents to room temperature [26]. Cells are trypsinized to create a single-cell suspension and centrifuged at 300 × g for 7 minutes. After supernatant removal, the cell pellet is resuspended in 1 mL of room temperature ALDEFLUOR assay buffer. Viable cell concentration is determined by Trypan Blue exclusion and adjusted to 1×10^5–1×10^6 cells/mL. The cell suspension is divided into "test" and "control" tubes, with 5 μL of 1.5 mM DEAB solution added to the control tube. Then, 5 μL of activated ALDEFLUOR substrate per mL of sample is added to the test tube, immediately followed by transfer of 0.5 mL to the DEAB control tube (final DEAB concentration 15μM). Samples are incubated for 30-45 minutes in a 37°C water bath (not exceeding 60 minutes). Following incubation, tubes are centrifuged at 4°C for 5 minutes at 300 × g, supernatant aspirated, and cell pellet resuspended in 0.5 mL of ice-cold ALDEFLUOR assay buffer. Samples are kept on ice and analyzed by flow cytometry shortly after staining [26].
CD133 Cell Sorting Using Magnetic-Activated Cell Sorting (MACS): For identification of colorectal cancer stem-like cells, CD133+ cells can be isolated from human (LoVo, HCT116, and SW620) and mouse (CT26) CRC cell lines using magnetic-activated cell sorting and flow cytometry [25]. The isolated CD133+ cells demonstrate higher proliferation, colony-forming ability, drug resistance, and tumorigenicity compared to CD133- cells, validating their stem-like characteristics [25].
Molecular Analysis Techniques
Quantitative Real-Time PCR (qRT-PCR): For gene expression analysis of CSC markers, qRT-PCR provides sensitive quantification. RNA is extracted from tissues or sorted cells, reverse transcribed to cDNA, and amplified using marker-specific primers. In CD133/OCT4 studies in NSCLC, expression levels are assessed relative to control genes and compared between tumor tissues and adjacent normal tissues [24].
Single-Cell RNA Sequencing (scRNA-seq): Advanced scRNA-seq protocols enable comprehensive analysis of CSC heterogeneity. For ICAM1 studies in GBM, researchers process single-cell RNA data using Seurat v5.1.0, applying quality control steps to remove cells with nFeature <500 or >7,000, mitochondrial gene expression >10%, erythrocyte gene expression >3%, or nCount <1,000 [29]. Principal component analysis and Harmony integration are performed after data normalization and feature selection, with t-Distributed Stochastic Neighbor Embedding for visualization. Marker genes are identified using FindAllMarkers, and malignant/non-malignant cells are distinguished using inferCNV [29].
Signaling Pathways and Molecular Mechanisms
The four CSC markers function within interconnected signaling networks that regulate stemness maintenance, survival, and immune evasion. Understanding these pathways is essential for developing effective CSC-targeted therapies.
Diagram 1: CSC Marker Signaling Network. This diagram illustrates the molecular interactions between key CSC markers and their downstream signaling pathways that regulate stemness, immune evasion, and therapy resistance.
Integrated CSC Marker Signaling
The signaling network illustrates how these four CSC markers coordinate to maintain the stem cell state. ICAM1 activates β-catenin signaling through ZNRF3 interaction and LRP6 stabilization, leading to PD-L1 upregulation [28]. This mechanism directly links adhesion molecule signaling with immune checkpoint regulation. CD44 contributes to stemness maintenance through multiple mechanisms, including direct regulation of PD-L1 expression in triple-negative breast cancer and NSCLC by binding to the regulatory region of the PD-L1 locus [23]. CD133 functions as a core component of stemness maintenance machinery, though its specific signaling partners vary by cancer type. ALDH1 provides metabolic support for stemness through detoxification of reactive oxygen species (ROS) and other aldehydes, creating a permissive environment for CSC maintenance [26] [27]. Together, these markers create a robust network that sustains the CSC phenotype while enabling immune evasion and therapy resistance.
Research Reagent Solutions
Table 4: Essential Research Reagents for CSC Marker Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Antibodies for IHC | Anti-CD133 (Abcam ab19898), Anti-OCT4 (Abcam ab19857) | Marker detection in tissue sections | Dilutions 1:150-1:200; citrate buffer antigen retrieval [24] |
| Flow Cytometry Assays | ALDEFLUOR Kit (StemCell Technologies #01700) | Detection of ALDH enzyme activity | Incubate 30-45 min at 37°C; DEAB control essential [26] |
| Cell Separation | Magnetic-activated cell sorting (MACS) for CD133 | Isolation of live CSC populations | Enables functional studies of sorted populations [25] |
| Novel Probes | AldeCou1-4 fluorescent probes | ALDH detection with improved S/N ratio | 125 nm Stokes shift; simplified protocol vs. ALDEFLUOR [27] |
| Cell Culture Models | Patient-derived GSCs (e.g., 528, 83, GSC209) | Functional studies of CSC populations | Maintain stemness in defined conditions [28] |
Experimental Workflows for CSC Identification
Diagram 2: Comprehensive CSC Identification Workflow. This workflow outlines the key methodological steps from sample collection through data integration for rigorous identification and validation of cancer stem cells using multiple complementary approaches.
Challenges and Future Perspectives in CSC Marker Research
Despite significant advances in CSC marker identification, several challenges persist in the field. The absence of universally reliable CSC biomarkers across cancer types remains a major obstacle, compounded by significant heterogeneity even within specific cancer types [5]. Marker expression varies considerably across tumor types, reflecting the influence of tissue origin and microenvironmental context on CSC phenotypes [5]. Furthermore, stem-like features can be acquired de novo by non-CSCs in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure, indicating that CSCs may represent a dynamic functional state rather than a static subpopulation [5].
The clinical translation of CSC marker knowledge faces additional hurdles. While CD44, CD133, ALDH1, and ICAM1 show promise as therapeutic targets, their expression in normal stem cells raises concerns about on-target, off-tumor effects [5] [13]. The dynamic plasticity of CSCs further complicates therapeutic targeting, as elimination of one CSC subpopulation may enable the emergence of alternative subpopulations utilizing different markers and signaling pathways [13].
Future perspectives in CSC marker research include the development of multi-marker panels that better capture CSC heterogeneity, the integration of single-cell technologies for refined subpopulation characterization, and the creation of novel therapeutic approaches that simultaneously target multiple CSC features. Emerging strategies such as dual metabolic inhibition, synthetic biology-based interventions, and immune-based approaches hold promise for overcoming CSC-mediated therapy resistance [5]. The combination of ICAM1 inhibition with PD-1 blockade demonstrates the potential of targeting both stemness and immune evasion pathways simultaneously [28]. Similarly, CD44's role in regulating PD-L1 expression suggests opportunities for combination strategies targeting both stemness and immune checkpoint mechanisms [23].
As technologies advance, the development of more sophisticated tools for CSC identification and targeting will continue to evolve. Novel approaches such as PET-leveraged ALDH probes [27], improved fluorescent probes with better signal-to-noise ratios, and advanced computational methods for analyzing CSC heterogeneity will enhance our ability to study and target these critical cell populations. Through continued refinement of marker identification techniques and elucidation of signaling networks, progress toward effective CSC-targeted therapies that address treatment resistance and recurrence may be achieved.
Cancer stem cells (CSCs) constitute a specialized subpopulation within tumors characterized by their capacity for self-renewal, differentiation into heterogeneous cancer cells, and enhanced resistance to conventional therapies. These cells are now recognized as central drivers of tumor initiation, progression, metastasis, and relapse [5]. The functional properties of CSCs—particularly their chemoresistance and immune evasion capabilities—are fundamentally regulated by a core set of evolutionarily conserved stemness signaling pathways [30]. These pathways, including Wnt/β-catenin, Notch, Hedgehog, and others, not only maintain stem-like properties but also enable CSCs to manipulate their microenvironment and evade immune destruction [31] [32].
The clinical significance of these pathways cannot be overstated. Their activity correlates strongly with poor patient outcomes across multiple cancer types, including digestive tract tumors, ovarian cancer, and breast cancer [33] [34]. Understanding the intricate workings of these signaling networks is therefore paramount for developing novel therapeutic strategies that can effectively target the CSC population and overcome the challenges of treatment resistance and disease recurrence [5] [30]. This technical review comprehensively examines the molecular mechanisms by which stemness signaling pathways coordinate self-renewal, chemoresistance, and immune evasion, providing a scientific framework for researchers and drug development professionals working to translate these insights into clinical applications.
Core Stemness Signaling Pathways: Molecular Mechanisms and Functional Outputs
Wnt/β-Catenin Signaling
The Wnt/β-catenin pathway serves as a master regulator of stem cell maintenance and fate decisions. In the canonical pathway, Wnt ligand binding to Frizzled receptors prevents the destruction complex from phosphorylating β-catenin, allowing β-catenin accumulation and nuclear translocation [34]. Once in the nucleus, β-catenin forms complexes with TCF/LEF transcription factors to activate target genes including c-MYC, CYCLIN D1, and CD44, which collectively promote self-renewal and cell cycle progression [5] [34]. Aberrant activation of this pathway is frequently observed in colorectal cancers and other gastrointestinal malignancies, where it drives CSC maintenance and tumor aggressiveness [34]. The pathway also contributes to chemoresistance through upregulation of drug efflux transporters and enhancement of DNA repair mechanisms [5].
Notch Signaling
Notch signaling operates via cell-to-cell communication, where transmembrane-bound ligands (Jagged and Delta-like) on one cell activate Notch receptors on adjacent cells, triggering proteolytic cleavage and release of the Notch intracellular domain (NICD) [30]. NICD translocates to the nucleus and forms a complex with CSL transcription factors, activating target genes such as HES and HEY that maintain the undifferentiated, self-renewing state of CSCs [33] [30]. In ovarian cancer, Notch signaling collaborates with the tumor microenvironment to enhance CSC survival following chemotherapy, and its inhibition has been shown to sensitize tumors to conventional treatments [33]. The pathway also supports immune evasion by modulating cytokine secretion and immune cell recruitment within the tumor niche [32].
Hedgehog Signaling
The Hedgehog (Hh) pathway is initiated by binding of Hedgehog ligands (SHH, IHH, DHH) to Patched receptors, which relieves suppression of Smoothened and enables activation of GLI transcription factors [35] [30]. GLI targets including SOX2, NANOG, and BMI-1 reinforce stemness and self-renewal capacity [30]. Hedgehog signaling exhibits extensive crosstalk with other stemness pathways and is particularly important in maintaining the CSC niche through stromal-epithelial interactions [33]. In digestive tract tumors, aberrant Hh signaling promotes epithelial-mesenchymal transition (EMT) and metastatic progression, making it a compelling therapeutic target [34].
Additional Key Regulatory Pathways
Several other signaling cascades contribute significantly to CSC regulation. The PI3K/AKT/mTOR pathway integrates growth factor signals to promote CSC survival, metabolic adaptation, and therapy resistance [5] [36]. TGF-β/SMAD signaling supports CSC maintenance and immune suppression through modulation of the tumor microenvironment [35] [33]. Hippo signaling, through its effectors YAP/TAZ, interfaces with mechanical cues from the extracellular matrix to influence CSC plasticity and expansion [5]. These pathways rarely operate in isolation; instead, they form an interconnected network that allows CSCs to adapt to therapeutic pressure and environmental challenges [35].
Table 1: Core Stemness Signaling Pathways in Cancer Stem Cells
| Pathway | Key Components | Primary Functions in CSCs | Therapeutic Inhibitors |
|---|---|---|---|
| Wnt/β-catenin | Frizzled, β-catenin, TCF/LEF | Self-renewal, differentiation, EMT, chemoresistance | Porcupine inhibitors, Tankyrase inhibitors, β-catenin disruptors |
| Notch | DLL/Jagged, Notch receptors, NICD, CSL | Cell fate decisions, survival, chemoresistance, immune modulation | γ-Secretase inhibitors, monoclonal antibodies |
| Hedgehog | SHH/IHH, Patched, Smoothened, GLI | Self-renewal, niche maintenance, metastasis | Smoothened antagonists (vismodegib, sonidegib) |
| PI3K/AKT/mTOR | PI3K, AKT, mTOR, PTEN | Metabolism, survival, proliferation, therapy resistance | AKT inhibitors, mTOR inhibitors, dual PI3K/mTOR inhibitors |
| TGF-β | TGF-β ligands, SMADs | EMT, immune suppression, metastasis, stromal remodeling | TGF-β receptor kinase inhibitors, neutralizing antibodies |
| Hippo | MST1/2, LATS1/2, YAP/TAZ | Mechanical signaling, proliferation, organ size control, stemness | YAP/TAZ inhibitors, verteporfin |
Diagram 1: Core stemness signaling pathways converge on chemoresistance and immune evasion. Each pathway initiates with ligand-receptor interaction, transduces signals through cytoplasmic components, activates transcription factors, and ultimately regulates genes controlling CSC properties.
Mechanisms of Therapy Resistance Mediated by Stemness Pathways
Intrinsic Chemoresistance Mechanisms
CSCs exhibit multiple intrinsic resistance mechanisms that are directly regulated by stemness signaling pathways. The Wnt/β-catenin pathway enhances the expression of ATP-binding cassette (ABC) drug transporters, including ABCB1 and ABCG2, which efficiently efflux chemotherapeutic agents from CSCs [5]. Notch signaling promotes cell cycle quiescence, enabling CSCs to evade cell cycle-dependent chemotherapeutics [33]. Additionally, multiple stemness pathways enhance DNA repair capacity through upregulation of DNA damage response proteins and detoxifying enzymes such as ALDH1, which inactivates certain chemotherapeutic agents like cyclophosphamide [8] [30].
The PI3K/AKT/mTOR pathway contributes significantly to therapy resistance by inhibiting apoptosis and promoting survival under stress conditions. AKT phosphorylation inactivates pro-apoptotic proteins while stabilizing anti-apoptotic factors, creating a robust protective mechanism against chemotherapy-induced cell death [36]. In ovarian cancer, the convergence of multiple stemness pathways creates a reinforced network of resistance mechanisms that allows CSCs to survive first-line chemotherapy and initiate disease recurrence [33].
Metabolic Adaptations
CSCs exhibit remarkable metabolic plasticity, enabled by stemness signaling pathways that facilitate adaptation to nutrient deprivation and therapeutic stress. The PI3K/AKT/mTOR axis coordinates a shift between glycolysis and oxidative phosphorylation depending on environmental conditions [5]. Hedgehog signaling promotes lipid metabolism rewiring, while Wnt activation enhances glutamine metabolism—adaptations that support CSC survival under chemotherapeutic stress [5] [30].
This metabolic reprogramming serves dual purposes: it maintains energy production and redox homeostasis in CSCs while simultaneously creating a metabolite-rich microenvironment that inhibits immune cell function. Lactate secretion from glycolytic CSCs acidifies the tumor microenvironment and suppresses cytotoxic T cell activity, while kynurenine production from tryptophan metabolism promotes regulatory T cell expansion [32]. These metabolic adaptations represent a crucial interface between chemoresistance and immune evasion mechanisms.
Table 2: Stemness Pathway-Mediated Resistance Mechanisms
| Resistance Mechanism | Key Pathway Regulators | Functional Consequences | Experimental Targeting Approaches |
|---|---|---|---|
| Drug efflux transporter upregulation | Wnt/β-catenin, Hedgehog | Reduced intracellular drug accumulation | ABC transporter inhibitors combined with pathway antagonists |
| Enhanced DNA repair capacity | Notch, PI3K/AKT | Reduced DNA damage from genotoxic agents | PARP inhibitors with Notch inhibitors |
| Metabolic plasticity | PI3K/AKT/mTOR, HIF-1α | Survival under nutrient and oxygen stress | Metabolic inhibitors (metformin, 2-DG) with pathway modulators |
| Epithelial-mesenchymal transition | TGF-β, Wnt, Notch | Enhanced invasive capacity, survival | Dual TGF-β/Wnt inhibition |
| Quiescence/G0 arrest | Notch, TGF-β | Evasion of cell cycle-active drugs | CDK4/6 inhibitors to force cell cycle entry |
| Autophagy activation | PI3K/AKT/mTOR, Hedgehog | Recycling of damaged organelles and proteins | Hydroxychloroquine with pathway inhibitors |
| Anti-apoptotic protein expression | PI3K/AKT, NF-κB | Resistance to apoptosis-inducing agents | BCL-2 inhibitors with AKT antagonists |
Immune Evasion Strategies Regulated by Stemness Pathways
Modulation of Immune Cell Infiltration and Function
Stemness signaling pathways enable CSCs to actively shape their immune microenvironment through the secretion of cytokines, chemokines, and exosomes that recruit and polarize immunosuppressive cells while excluding cytotoxic immune populations. CSCs secrete TGF-β, IL-10, CCL2, and CCL5, which recruit regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and tumor-associated macrophages (TAMs) [32]. These immune cells create a protective niche around CSCs through multiple mechanisms: TAMs promote CSC stemness via IL-6 and TGF-β secretion; MDSCs inhibit T cell function through arginase-1 and reactive oxygen species production; and Tregs suppress antitumor immunity through CTLA-4 and IL-35-mediated mechanisms [32].
The Wnt/β-catenin pathway has been specifically linked to T cell exclusion from the tumor microenvironment, creating an "immune-privileged" site for CSCs [31]. This pathway activation leads to downregulation of chemokines that attract CD8+ T cells, effectively creating a physical barrier against immune attack. In digestive tract tumors, CSC-immune cell crosstalk establishes a self-reinforcing immunosuppressive loop that protects the CSC population from elimination [34] [32].
Immune Checkpoint Expression and Antigen Presentation Alterations
CSCs upregulate multiple immune checkpoint molecules as another mechanism of immune evasion. Notch and PI3K/AKT signaling induce PD-L1 expression on CSCs, enabling them to directly inhibit T cell activation through PD-1 engagement [32]. Additionally, CSCs exhibit reduced MHC class I expression, limiting their antigen presentation capacity and ability to be recognized by cytotoxic T cells [32]. Some CSC populations also upregulate non-classical MHC molecules such as HLA-G, which further suppresses immune responses [31].
The Hippo pathway effector YAP has been shown to promote PD-L1 expression in CSCs, while TGF-β signaling induces TIM-3 and LAG-3 checkpoint expression [5]. This multifaceted approach to immune checkpoint regulation allows CSCs to deploy numerous parallel mechanisms to resist immune-mediated killing, explaining why single-agent checkpoint blockade often fails to eliminate the CSC compartment.
Diagram 2: Stemness pathways orchestrate multifaceted immune evasion. Pathway activation in CSCs leads to secretion of immunomodulatory factors, metabolite release, checkpoint expression, and antigen presentation alterations that collectively establish an immunosuppressive microenvironment protective of CSCs.
Experimental Approaches for Studying Stemness Signaling
Methodologies for Pathway Analysis and Targeting
Advanced experimental models and methodologies are essential for delineating the complex functions of stemness signaling pathways in CSCs. 3D organoid cultures derived from patient tumors preserve the cellular heterogeneity and signaling interactions found in native tumors, making them particularly valuable for studying pathway activity in a context that closely mimics the in vivo environment [5]. Organoids can be genetically manipulated using CRISPR/Cas9 systems to knockout or activate specific pathway components, allowing for functional validation of their roles in maintaining stemness properties [5] [8].
Single-cell RNA sequencing (scRNA-seq) has emerged as a powerful tool for dissecting CSC heterogeneity and identifying distinct subpopulations with activated stemness pathways. This approach has revealed context-specific pathway dependencies in different cancer types—for instance, LGR5+ CSCs in colorectal cancer show distinct Wnt signaling patterns compared to CD44+ CSCs in breast cancer [5] [34]. Spatial transcriptomics further enhances this understanding by mapping pathway activity within the architectural context of the tumor, revealing how niche location influences stemness signaling [33].
For functional studies, limiting dilution transplantation assays remain the gold standard for assessing CSC frequency and self-renewal capacity following pathway modulation [8]. These in vivo experiments provide critical validation of pathway importance in maintaining tumor-initiating potential. Additionally, reporter systems (such as TOP-GFP for Wnt signaling) enable real-time tracking of pathway activity in living cells, allowing researchers to monitor dynamic changes in stemness states in response to therapeutic interventions [34].
Research Reagent Solutions for Stemness Pathway Investigation
Table 3: Essential Research Reagents for Stemness Signaling Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Pathway reporters | TOP-flash/FOP-flash (Wnt), Gli-luciferase (Hh), CBF-luciferase (Notch) | Pathway activity quantification, inhibitor screening | Normalize to control reporters; confirm specificity with inhibitors |
| Small molecule inhibitors | XAV939 (Wnt), DAPT (Notch), vismodegib (Hh), MK-2206 (AKT) | Pathway inhibition studies, combination therapy testing | Optimize dosing to avoid off-target effects; use multiple inhibitors per pathway |
| Recombinant proteins | Wnt3a, Dll4, Shh, BMP4 | Pathway activation, stemness maintenance in culture | Use validated bioactivity lots; titrate for optimal effect |
| Antibodies for flow cytometry | Anti-CD44, anti-CD133, anti-ALDH1A1, anti-LGR5 | CSC identification and isolation | Validate combinations for specific cancer types; include viability dyes |
| CRISPR/Cas9 systems | sgRNAs targeting CTNNB1, Notch1, Smo, PTEN | Genetic validation of pathway components | Use multiple sgRNAs per target; include rescue experiments |
| Cytokine/Chemokine arrays | TGF-β, IL-6, CCL2, CCL5 measurement | Secretome analysis of CSC-immune interactions | Use conditioned media from purified CSCs; normalize to cell number |
| Metabolic probes | Seahorse extracellular flux analyzers, glucose/glutamine uptake assays | Metabolic profiling of CSCs | Compare under normoxia vs hypoxia; profile after pathway inhibition |
Therapeutic Implications and Future Directions
The pivotal role of stemness signaling pathways in mediating therapy resistance and immune evasion makes them compelling therapeutic targets. Emerging clinical strategies focus on combining conventional therapies with CSC-targeted approaches to achieve more durable responses. For example, in ovarian cancer, where the recurrence rate exceeds 70-80% in advanced stages, combining platinum-based chemotherapy with Hedgehog or Notch pathway inhibitors is showing promise in preclinical models for reducing CSC-mediated resistance [33]. Similarly, in digestive tract tumors, Wnt pathway inhibitors are being evaluated in combination with standard regimens to target the CSC compartment responsible for recurrence [34].
Immunotherapy combinations represent another promising frontier. The demonstrated ability of stemness pathways to regulate immune checkpoint expression and create immunosuppressive microenvironments suggests that pathway inhibitors could synergize with checkpoint blockade [32]. Early clinical trials are exploring anti-PD-1/PD-L1 antibodies in combination with Wnt, Notch, or PI3K/AKT pathway inhibitors, with the goal of simultaneously targeting both the immune evasive properties and the self-renewal capacity of CSCs [31] [32].
Despite these advances, significant challenges remain. CSC plasticity and heterogeneity enable adaptive resistance to targeted therapies, as inhibition of one pathway may lead to compensatory activation of another [8] [30]. Additionally, the shared regulation of normal stem cell and CSC populations raises concerns about on-target toxicities, necessitating careful therapeutic windows and dosing strategies [30]. Future research directions should prioritize the identification of context-specific pathway dependencies, the development of biomarkers to identify patients most likely to benefit from pathway-targeted approaches, and innovative clinical trial designs that incorporate CSC-directed endpoints alongside traditional response metrics [5] [34].
The continued elucidation of stemness signaling networks and their interface with therapy resistance and immune evasion mechanisms holds tremendous promise for transforming cancer treatment. By developing strategies that effectively target these fundamental pathways, the research community moves closer to overcoming the challenges of treatment resistance and recurrence, ultimately improving outcomes for cancer patients.
Isolating and Profiling CSCs: Techniques from FACS to Single-Cell Omics
Fluorescence-Activated Cell Sorting (FACS) and Magnetic-Based Sorting Using Surface Markers
The isolation and analysis of cancer stem cells (CSCs) represent a critical frontier in modern oncology research. CSCs are defined as a small subset of cells within tumors characterized by self-renewal capacity, continuous proliferation, and the ability to drive tumorigenesis, metastasis, and therapeutic resistance [37]. The fundamental challenge in CSC research lies in their identification and isolation from the bulk tumor population, which is essential for understanding their biology and developing targeted therapies. The CSC model, also known as the hierarchical model, provides a paradigm for understanding intratumoral heterogeneity, as CSCs can differentiate into various cancer cell phenotypes and maintain their population [37]. Surface markers serve as indispensable tools for identifying and isolating these elusive cell populations, with technologies like Fluorescence-Activated Cell Sorting (FACS) and Magnetic-Activated Cell Sorting (MACS) providing the technical foundation for these endeavors.
The significance of CSCs in clinical oncology cannot be overstated. Despite advances in cancer detection and treatment, cancer remains a significant global disease burden, with CSCs implicated in treatment failure and disease recurrence [37] [5]. CSCs demonstrate remarkable resilience to conventional therapies, including chemotherapy and radiotherapy, due to several intrinsic properties: enhanced DNA repair mechanisms, drug efflux capabilities, and the ability to remain in a quiescent state [5]. Furthermore, their dynamic interactions with the tumor microenvironment create protective niches that shield them from therapeutic assaults [2]. This resilience underscores the critical need for precise isolation techniques to study CSC biology and develop CSC-directed therapies.
A primary challenge in CSC research is the lack of universal CSC markers. While surface proteins such as CD44, CD133, and ALDH1A1 have been widely used to isolate CSC populations, these markers are not exclusive to CSCs and are often expressed in normal stem cells or non-tumorigenic cancer cells [5]. Moreover, their expression varies significantly across tumor types, reflecting the influence of tissue origin and microenvironmental context on CSC phenotypes [5]. This heterogeneity necessitates sophisticated sorting approaches that can accommodate complex marker combinations and adapt to the unique characteristics of different cancer types.
Technical Foundations of Cell Sorting Technologies
Fluorescence-Activated Cell Sorting (FACS)
Principles and Process
Fluorescence-Activated Cell Sorting (FACS) is an advanced variant of flow cytometry that leverages fluorescent labels to sort and analyze cells with high precision [38]. The technology was pioneered in the 1960s by geneticists at Stanford University, with significant contributions from Dr. Leonard Herzenberg, who introduced the first commercial FACS machine in the late 1970s [38]. The FACS process operates through four integrated phases that transform a heterogeneous cell mixture into purified populations.
The initial phase involves sample preparation and labeling, where researchers ensure cell viability and uniform suspension before introducing fluorescent labels attached to antibodies specific to cell surface markers [38]. These fluorophores act as molecular beacons that will later facilitate cell identification. The labeled cells then undergo laser excitation and cell interrogation, where they are funneled through the flow cytometer one at a time, encountering a laser beam that excites the fluorescent tags [38]. This excitation causes each cell to emit light at characteristic wavelengths, creating a unique fluorescent signature for each cell type.
Following excitation, the system enters the signal detection and analysis phase, where sophisticated detectors capture both the emitted fluorescence and the light scattered by each cell [38]. Forward scatter (FSC) provides information about cell size, while side scatter (SSC) reveals internal complexity or granularity [38]. The combination of these parameters enables comprehensive cellular characterization. Finally, in the cell sorting and collection phase, the stream forms droplets containing single cells, which are electrically charged based on their fluorescence profile and deflected by an electromagnetic field into appropriate collection tubes [38]. This elegant physical separation mechanism enables the isolation of highly pure cell populations for downstream applications.
FACS Workflow Visualization
The following diagram illustrates the comprehensive FACS sorting process, from sample preparation to cell collection:
Magnetic-Activated Cell Sorting (MACS)
Principles and Process
Magnetic-Activated Cell Sorting (MACS) employs magnetic fields to isolate specific cell populations from heterogeneous mixtures [39] [40]. This technology utilizes superparamagnetic beads conjugated with antibodies, lectins, or enzymes that recognize specific surface markers on target cells [39] [40]. The fundamental principle underlying MACS is the immunomagnetic separation of cells based on their surface antigen expression profiles, offering a simpler and more accessible alternative to FACS for many applications.
The MACS process begins with magnetic labeling, where magnetic beads functionalized with specific binding molecules are added to a cell suspension [39] [40]. This labeling can be achieved through two primary approaches: direct labeling, where beads are pre-conjugated with primary antibodies, and indirect labeling, where cells are first incubated with unlabeled primary antibodies followed by secondary antibody-conjugated beads [40]. Indirect labeling provides greater flexibility but may increase non-specific binding. Following incubation, the labeled cell mixture is transferred to a separation column positioned within a strong magnetic field [39].
During magnetic separation, cells bound to magnetic beads are retained within the column due to the magnetic force, while unlabeled cells pass through in the effluent [39] [40]. This process enables two fundamental selection strategies: positive selection, where target cells are magnetically labeled and retained, and negative selection (depletion), where unwanted cells are magnetically labeled and removed, leaving the target population unlabeled in the effluent [40]. For complex isolation needs, sequential selection strategies combining both approaches can be employed [40]. After washing to remove nonspecifically bound cells, the magnetic field is removed, and the retained cells are eluted from the column [39].
MACS Workflow Visualization
The following diagram illustrates the key steps in the MACS cell sorting process:
Comparative Analysis of FACS and MACS Technologies
Technical Specifications and Performance Metrics
The selection between FACS and MACS technologies requires careful consideration of their respective capabilities, limitations, and suitability for specific research applications. The following table provides a comprehensive comparison of their key characteristics:
Table 1: Comparative Analysis of FACS and MACS Technologies
| Feature | FACS | MACS |
|---|---|---|
| Technology Basis | Fluorescence-based sorting using lasers and electrostatic deflection [41] [38] | Magnetic bead-based separation using columns and magnetic fields [41] [39] |
| Sorting Resolution | High - can distinguish subtle differences in marker expression levels [38] [42] | Moderate - limited discrimination between cells with similar phenotypes [42] |
| Multiparametric Capability | High - simultaneous analysis of multiple markers, size, and granularity [38] [42] | Low - typically limited to one or two parameters per separation [42] |
| Sorting Speed | Medium to High (up to thousands of cells per second) [38] | High - rapid processing of large sample volumes [41] [42] |
| Cell Viability | Variable - can induce cellular stress or apoptosis [38] [43] | Moderate - magnetic beads may damage delicate cells [41] [39] |
| Purity of Sorted Cells | Very High (up to 99%) [43] | High (typically >90%) [43] |
| Equipment Cost | High - expensive instrumentation and maintenance [41] [38] | Moderate - lower equipment costs but recurring consumable expenses [41] [42] |
| Technical Expertise | High - requires specialized training and careful calibration [38] [42] | Moderate - relatively straightforward protocols [42] |
| Typical Applications | Rare cell isolation, complex phenotyping, single-cell analysis [38] [42] | Bulk cell isolation, pre-enrichment, high-throughput processing [39] [42] |
| Sample Throughput | Lower - sequential sample processing | Higher - potential for parallel processing of multiple samples [39] |
Complementary Applications in CSC Research
In contemporary CSC research, FACS and MACS often serve complementary rather than competitive roles. MACS is frequently employed as an initial enrichment step to simplify complex samples before more refined FACS analysis [42]. This approach leverages the strengths of both technologies: the high throughput and simplicity of MACS for preliminary isolation, followed by the high-resolution capabilities of FACS for precise population discrimination [42]. This combined strategy is particularly valuable when working with rare CSC populations, where direct FACS sorting from heterogeneous samples would be inefficient or impractical.
The decision between these technologies ultimately depends on experimental requirements, available resources, and specific research questions. FACS excels when high-precision sorting based on multiple parameters is essential, such as in single-cell genomics, functional heterogeneity studies, or when investigating complex CSC subpopulations [38] [42]. Conversely, MACS offers advantages for processing large sample volumes, routine isolations, or when specialized flow cytometry equipment or expertise is unavailable [39] [42]. Furthermore, MACS is often preferred when subsequent functional assays require minimal cellular perturbation, as the magnetic labeling process is generally gentler than the fluidic and electrostatic forces in FACS [43].
Application in Cancer Stem Cell Research: Experimental Approaches
CSC Marker Panels and Sorting Strategies
The isolation of CSCs relies on specific surface marker combinations that vary across cancer types. Research has identified numerous CSC markers, including CD44, CD133, CD338, CD271, and ALDH1A1, though their expression profiles are cancer-specific [5] [44]. A critical consideration in CSC sorting is the inherent plasticity of these populations, wherein non-CSCs can acquire stem-like properties under certain conditions, and CSCs can differentiate, creating dynamic equilibrium within tumors [5] [2]. This plasticity necessitates careful experimental design and interpretation of sorting outcomes.
An exemplary application of FACS in CSC research comes from a 2019 study on esophageal squamous cell carcinoma (ESCC), where researchers established a method to identify and isolate CSCs using combined surface biomarkers CD71, CD271, and CD338 [44]. The CD71⁻/CD271⁺/CD338⁺ subpopulation demonstrated enhanced stem cell properties, including increased proliferation, self-renewal, differentiation capacity, metastasis, drug resistance, and tumorigenicity [44]. This study highlights the importance of multi-parameter sorting strategies for reliably isolating functionally validated CSCs.
Detailed Experimental Protocol: CSC Isolation from ESCC
The following protocol summarizes the methodology employed in the aforementioned ESCC study [44]:
Cell Preparation: Cultured ESCC cell lines (ECa9706, ECa109, KYSE50, and CAES17) are harvested during logarithmic growth phase, washed with phosphate-buffered saline (PBS), and resuspended in sorting buffer at appropriate concentration (typically 1×10⁷ cells/mL).
Antibody Staining: Cells are incubated with fluorescently conjugated antibodies against CD71, CD271, and CD338. Optimization of antibody concentrations and incubation conditions (typically 30-60 minutes at 4°C protected from light) is essential for specific binding.
Propidium Iodide Exclusion: Viability staining with propidium iodide (PI) is performed to exclude dead cells from sorting and analysis.
FACS Configuration and Sorting: The flow cytometer is configured with appropriate laser lines and filter sets for the fluorophores used. Sorting gates are established based on isotype controls and single-stained samples for compensation. The target population (CD71⁻/CD271⁺/CD338⁺) is sorted into collection tubes containing culture medium.
Post-Sort Analysis: An aliquot of sorted cells is reanalyzed to determine sorting purity, which should exceed 90% for meaningful experiments. Cell viability is assessed via trypan blue exclusion or similar methods.
Functional Validation: Sorted cells undergo functional assays including sphere formation assays, drug sensitivity tests, proliferation assays, and in vivo tumorigenicity studies to confirm CSC properties.
Research Reagent Solutions for CSC Sorting
Table 2: Essential Research Reagents for CSC Sorting Experiments
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| Fluorescent Antibodies | Anti-CD44, Anti-CD133, Anti-CD338, Anti-CD271 [44] | Specific recognition of CSC surface markers for detection and sorting |
| Magnetic Beads | Anti-CD44 MicroBeads, Anti-CD133 MicroBeads [40] | Magnetic labeling of CSCs for separation in MACS protocols |
| Viability Stains | Propidium Iodide (PI), 7-AAD [43] | Exclusion of dead cells during sorting to improve purity and viability |
| Separation Columns | MACS MS, LS, or LD Columns [39] [43] | Matrix for retaining magnetically labeled cells during MACS separation |
| Cell Culture Media | Serum-free DMEM/F12 medium [44] | Maintenance of stemness in sorted CSCs for functional assays |
| Enzymatic Dissociation Reagents | Trypsin-EDTA, Accutase, Collagenase | Tissue dissociation to obtain single-cell suspensions for sorting |
| Analysis Software | FlowJo, FCS Express [42] | Data analysis and interpretation of sorting results |
Emerging Technologies and Future Perspectives
Innovations in Cell Sorting Platforms
The field of cell sorting continues to evolve with emerging technologies that address limitations of both FACS and MACS. Buoyancy-Activated Cell Sorting (BACS) represents one such innovation, utilizing buoyant microbubbles functionalized with specific antibodies to float target cells to the surface for gentle separation [41]. This approach offers several advantages, including minimal cellular stress, rapid processing (30-60 minutes), no requirement for specialized equipment, and compatibility with delicate cell types like primary CSCs [41]. While not yet as widely adopted as FACS or MACS, this technology demonstrates the ongoing pursuit of gentler, more accessible sorting methodologies.
Advanced microfluidic-based sorting systems are also gaining traction, offering reduced sample volumes, lower reagent costs, and decreased mechanical stress on cells [42]. These chip-based platforms enable precise manipulation of cellular populations using various principles including acoustics, dielectrophoresis, and hydrodynamic focusing. When integrated with artificial intelligence algorithms, these systems show promise for automated identification and sorting of rare cell populations based on complex phenotypic patterns rather than predefined marker panels [42]. Such capabilities could be particularly valuable for CSCs, which may exhibit considerable heterogeneity that transcends conventional marker-based classifications.
Future Directions in CSC Sorting and Analysis
The future of CSC sorting lies in the integration of multiple technological approaches to overcome current limitations. Multi-omics integration at the single-cell level, combining transcriptomic, proteomic, and epigenetic data from sorted CSCs, will provide unprecedented insights into their biology and regulatory networks [5]. The development of universal CSC biomarkers remains a critical goal, though current evidence suggests that marker panels will need to be context-specific, reflecting the tissue of origin, tumor stage, and microenvironmental influences [5].
From a technical perspective, the convergence of sorting technologies with functional screening approaches represents a promising direction. For instance, FACS-based sorting followed by CRISPR-based functional screens in isolated CSCs can identify genetic dependencies and therapeutic vulnerabilities [5]. Similarly, the development of metabolic profiling techniques compatible with sorted cells will enhance understanding of CSC metabolic plasticity, potentially revealing new targeting strategies [5]. As these technologies mature, they will increasingly enable researchers to address the fundamental challenges in CSC biology, ultimately contributing to more effective therapeutic strategies for treatment-resistant cancers.
Fluorescence-Activated Cell Sorting and Magnetic-Based Sorting represent complementary pillars in modern cancer stem cell research. FACS offers unparalleled resolution and multi-parametric capabilities for discerning complex CSC subpopulations, while MACS provides a robust, accessible platform for high-throughput isolation and enrichment. The selection between these technologies depends on specific research objectives, required purity, available resources, and downstream applications. As CSC biology continues to reveal increasing complexity and plasticity, advanced sorting methodologies will remain essential tools for unraveling the mechanisms underlying tumor initiation, progression, and therapeutic resistance. The integration of these sorting technologies with emerging analytical approaches promises to accelerate the development of CSC-targeted therapies, potentially overcoming one of the most significant challenges in contemporary oncology.
Within cancer stem cell (CSC) research, the challenges of marker-based identification are well-documented. Putative CSC markers such as CD133, CD44, and ALDH often lack universality, demonstrate phenotypic heterogeneity, and can be dynamically regulated, limiting their reliability for prospective isolation [45] [5] [46]. Consequently, functional assays have become the gold standard for defining CSCs based on their biological capabilities rather than surface protein expression. This technical guide details two cornerstone functional assays: the sphere formation assay and serial xenotransplantation. These methods are critical for investigating CSC self-renewal, tumorigenicity, and therapy resistance, directly addressing the limitations of marker-based identification.
Sphere Formation Assay
The sphere formation assay is a widely used in vitro functional method for identifying and studying cancer stem-like cells (CSCs) based on their unique ability to survive and proliferate under anchorage-independent conditions.
Core Principle and Rationale
This assay leverages the principle of anoikis, a form of programmed cell death that occurs when most adherent cells detach from the extracellular matrix. CSCs, however, possess inherent anoikis resistance, enabling them to survive in suspension and form clonal, three-dimensional structures known as tumorspheres or spheres [47]. The capacity of a single cell to form a sphere in vitro is considered a functional surrogate for CSC properties, including self-renewal and differentiation potential [47] [48]. It serves as a marker-agnostic approach to circumvent issues of phenotypic plasticity and the lack of universal CSC surface markers [5] [47].
Detailed Experimental Protocol
Standard Workflow
The following protocol describes a high-throughput, microfluidic-based approach to ensure clonality, though the core steps apply to conventional methods using low-attachment multi-well plates.
Step 1: Single-Cell Suspension Preparation
- Harvest cancer cells using a standard method (e.g., 0.05% Trypsin/EDTA for 5 minutes).
- Centrifuge at 100 × g for 5 minutes and resuspend in a known volume of complete culture media.
- Perform a viable cell count and adjust cell density to a final concentration of 1x10^6 cells/mL in sphere formation media [49].
Step 2: Device Seeding and Culture
- For microfluidic devices, seed the cell suspension onto a polyHEMA or Pluronic F-108-coated chip containing thousands of micro-wells. A representative device may contain 1,024 to 10,000 micro-wells to ensure physical isolation of single cells [47] [49].
- Allow cells to settle for approximately 5 minutes.
- Replace the loading media with fresh serum-free sphere formation media. A standard formulation includes:
- Base: DMEM/F12 medium.
- Supplements: 1% N-2 Supplement, 1% Antibiotic-Antimycotic, 1% GlutaMAX.
- Growth Factors: 20 ng/mL Recombinant Human EGF, 20 ng/mL Recombinant Human FGF basic.
- Other: 10 ng/mL Insulin, 1 µM Dexamethasone [49].
- Culture cells in a humidified incubator at 37°C with 5% CO2 for up to 14 days, exchanging media every 48 hours to maintain nutrient levels and remove waste [49].
Step 3: Sphere Quantification and Analysis
- Monitor sphere formation regularly using microscopy.
- After the culture period (typically 7-14 days), score a structure as a positive sphere if its diameter exceeds a threshold, commonly 40-50 µm [47] [49].
- Calculate the Sphere Formation Efficiency (SFE) as:
(Number of spheres formed / Number of single cells seeded) × 100%.
Table 1: Key Parameters and Reagents for Sphere Formation Assays
| Parameter/Reagent | Specification | Function/Rationale |
|---|---|---|
| Culture Surface | PolyHEMA/Pluronic F-108 coated micro-wells or plates | Creates a non-adherent surface to enforce anchorage-independent growth and prevent anoikis in non-CSCs. |
| Culture Media | Serum-free, supplemented with EGF & FGF | Selects for stem-like cells by suppressing differentiation; growth factors support CSC proliferation. |
| Cell Seeding Density | Clonal density (e.g., in micro-wells) | Prevents cell aggregation, ensuring spheres are clonally derived from a single cell. |
| Culture Duration | 7-14 days | Allows for sufficient time for slow-cycling CSCs to initiate proliferation and form detectable spheres. |
| Quantification Metric | Sphere Formation Efficiency (SFE) | Provides a quantitative measure of the frequency of sphere-initiating cells in a population. |
Technical Considerations and Advancements
- Ensuring Clonality: Conventional low-attachment plates are prone to cell aggregation, leading to overestimation of SFE. Microfluidic platforms with hydrodynamic single-cell capture overcome this, with capture rates exceeding 70% [47].
- Assay Acceleration: Traditional sphere assays are time-consuming. Machine learning models using convolutional neural networks (CNNs) can now predict sphere formation potential by analyzing single-cell morphology on Day 4, accurately estimating the final SFE and reducing assay time by 3.5-fold [49].
- Interpretation Caveats: The sphere-forming cell may represent a progenitor with limited renewal potential, not a true CSC. The assay evaluates stem cell potential under specific in vitro conditions, which may not fully recapitulate the in vivo niche [50] [48].
Serial Xenotransplantation Assay
Serial xenotransplantation is considered the in vivo gold standard functional assay for definitively confirming the self-renewal and tumor-initiating capacity of CSCs.
Core Principle and Rationale
This assay tests the defining properties of CSCs—self-renewal and tumorigenicity—by repeatedly transplanting cancer cells from a primary xenograft into secondary and tertiary immunodeficient mouse recipients [45] [46]. The sustained ability to recapitulate tumor heterogeneity through multiple passages demonstrates the presence of cells with long-term renewal capacity, a hallmark of stemness. It is the most rigorous in vivo validation of the CSC hypothesis [45].
Detailed Experimental Protocol
Standard Workflow
The protocol below outlines the process using the NOD/SCID gamma (NSG) mouse model, which is highly permissive due to its lack of mature T cells, B cells, and NK cell activity.
Step 1: Primary Tumor Cell Preparation
- Obtain a single-cell suspension from a human tumor sample (patient-derived xenograft or cell line).
- Optionally, sort cells based on a prospective marker (e.g., CD44+/CD24-/low) or leave unsorted for unbiased enrichment [45] [46].
- Resuspend cells in an appropriate buffer like PBS or Matrigel for injection.
Step 2: Primary Transplantation and Tumor Monitoring
- Inject cells subcutaneously or orthotopically into immunodeficient mice (e.g., NSG mice). A common injection volume is 100-200 µL.
- Monitor mice regularly for tumor formation. Measure tumor dimensions with calipers 2-3 times per week.
- Calculate tumor volume using the formula:
Volume = (Length × Width^2) / 2. - Once the primary xenograft reaches a predetermined endpoint size (e.g., 1.5 cm in diameter), euthanize the mouse and harvest the tumor.
Step 3: Serial Passaging and Analysis
- Mechanically dissociate and/or enzymatically digest the primary xenograft tumor to create a single-cell suspension.
- Transplant these cells into a new cohort of secondary recipient mice, using the same method and cell number (or limiting dilution) as the primary transplant.
- Repeat this process for tertiary and subsequent passages. The demonstration of sustained or enhanced tumorigenicity across passages is key evidence of CSC enrichment [45].
- Throughout the process, cells can be isolated for in vitro analysis (e.g., gene expression, ALDH activity) to correlate functional changes with molecular signatures [45].
Table 2: Key Parameters and Outcomes in a Serial Xenotransplantation Study
| Parameter | Representative Data from Rhabdomyosarcoma Study [45] | Interpretation |
|---|---|---|
| Mouse Model | NOD/SCID gamma (NSG) | Provides a highly immunocompromised environment for efficient engraftment of human cells. |
| Tumorigenic Efficiency | 1st Passage: 3/3 (100%)2nd Passage: 6/9 (67%)3rd Passage: 27/27 (100%) | Demonstrates the presence and maintenance of tumor-initiating cells across generations. |
| Tumor Growth Rate | 1st Passage: 2.89 ± 0.74 mm³/day3rd Passage: 5.66 ± 0.72 mm³/day | A statistically significant increase (1.95-fold) indicates enrichment for more aggressive, tumorigenic cells (CSCs). |
| Functional Enrichment (in vitro) | Increased colony/sphere formation and ALDH activity in later passage cells. | Corroborates in vivo data, showing that serially passaged cells possess enhanced stem-like properties. |
Technical Considerations and Molecular Insights
- Enrichment and Aggressiveness: Serial passaging often selects for increasingly aggressive CSCs. In rhabdomyosarcoma, this led to a 1.95-fold higher daily tumor volume increase in the third passage compared to the first [45].
- Unbiased Target Discovery: Using unsorted cells for serial transplantation can serve as an unbiased platform for CSC enrichment. This approach has revealed molecular changes associated with stemness, such as a hybrid epithelial/mesenchymal signature and upregulation of stemness regulators (SOX4, PAX3) [45].
- Correlative Functional Analysis: Xenotransplantation-derived cells should be analyzed with other functional assays. For instance, Aldefluor assays on serially passaged rhabdomyosarcoma cells showed a significant increase in ALDH activity, a common functional CSC marker [45].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these functional assays requires specific reagents and models to accurately mimic the selective pressures for CSCs.
Table 3: Essential Research Reagents for CSC Functional Assays
| Reagent/Model | Function in Assay | Key Examples & Specifications |
|---|---|---|
| Ultra-Low Attachment Surfaces | Prevents cell adhesion, enforcing selection for anoikis-resistant CSCs. | PolyHEMA coatings, Pluronic F-108 solutions, commercial low-attachment plates [47] [49]. |
| Defined Serum-Free Media | Supports CSC growth while inhibiting differentiation of non-CSCs. | DMEM/F12 base supplemented with growth factors (EGF, FGF), N-2 supplement, and insulin [49]. |
| Immunodeficient Mouse Models | Enables engraftment and growth of human tumor cells in vivo. | NOD/SCID gamma (NSG) mice, which lack T, B, and NK cells, are the gold standard for xenotransplantation [45] [46]. |
| Extracellular Matrix Substitutes | Provides a 3D scaffold for cell growth and can be used for orthotopic injections. | Matrigel, used to suspend cells for injection, enhancing engraftment efficiency. |
| Dissociation Enzymes | Generates single-cell suspensions from solid tumors or spheres for passaging and analysis. | Trypsin/EDTA, collagenase, or commercial dissociation kits (e.g., Tumor Dissociation Kits). |
Visualizing Experimental Workflows
Sphere Formation Assay Workflow
The following diagram illustrates the key steps in a high-throughput, microfluidic-based sphere formation assay.
Diagram 1: Sphere formation assay workflow.
Serial Xenotransplantation Workflow
This diagram outlines the iterative process of serial xenotransplantation for enriching and validating CSCs.
Diagram 2: Serial xenotransplantation workflow.
Sphere formation and serial xenotransplantation are indispensable, complementary tools in the functional identification and characterization of CSCs. The sphere formation assay provides a relatively rapid, high-throughput in vitro system for initial screening and functional isolation. In contrast, serial xenotransplantation offers the most stringent in vivo validation of CSC self-renewal and tumorigenic potential. Used in concert, these assays powerfully address the fundamental challenges in CSC research posed by marker heterogeneity and plasticity, driving the discovery of novel molecular signatures and advancing the development of targeted therapeutic strategies aimed at eradicating the root of cancer.
The reanalysis of existing public single-cell RNA sequencing (scRNA-seq) data represents a powerful, cost-effective strategy for generating novel biological insights, particularly in the complex field of cancer stem cell (CSC) biology. CSCs constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [5]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies [5]. However, the identification and targeting of CSCs remain challenging due to dynamic marker expression and significant heterogeneity across and within tumor types [5] [51].
scRNA-seq technology enables researchers to interrogate cellular diversity and function at unprecedented resolution, moving beyond the limitations of bulk sequencing approaches that obscure rare cell populations like CSCs [52] [53]. The growing wealth of publicly available scRNA-seq datasets provides opportunities to explore CSC signatures, heterogeneity, and interactions within the tumor microenvironment (TME) without the need for new experiments [54]. This technical guide outlines comprehensive methodologies for leveraging these public data resources to advance CSC research, providing detailed protocols for data acquisition, processing, analysis, and integration specifically focused on overcoming key challenges in CSC identification and characterization.
Accessing Public scRNA-seq Data Repositories
Major Public Data Repositories
Publicly available scRNA-seq data is housed in several major repositories that collect, curate, and distribute genomic data. The table below summarizes key repositories relevant to CSC research.
Table 1: Major Public Repositories for scRNA-seq Data
| Repository | Key Features | Data Types | Access Methods |
|---|---|---|---|
| Gene Expression Omnibus (GEO) | Free public repository from NCBI; contains over 4000 datasets including scRNA-seq | Processed data, raw counts, metadata | Web search, advanced search builder, direct download |
| Sequence Read Archive (SRA) | NCBI repository for raw sequencing data; stores alignment information and annotation files | Raw sequencing data, alignment files | Simple search, advanced search, command-line tools |
| ArrayExpress | European counterpart to GEO; contains functional genomics data | Processed and raw data | Web interface, API access |
| The Single Cell Data Portal | Curated resource specifically for single-cell datasets | Single-cell specific datasets and analyses | Dedicated web portal |
Effective Search Strategies for CSC-Relevant Data
To locate CSC-relevant scRNA-seq data in these repositories, researchers should employ systematic search strategies:
GEO Advanced Search: Use the GEO DataSets Advanced Search Builder with specific field selections. For identifying scRNA-seq data, select "Expression profiling by high throughput sequencing" as the DataSet type and "single cell" as the Sample source [54]. Additional filters can include specific cancer types (e.g., "hepatocellular carcinoma"), cell types (e.g., "cancer stem cells"), or markers (e.g., "CD44," "CD133").
Boolean Operators: Effectively combine search terms using Boolean operators (OR, AND, NOT) to refine results. For example:
"single cell RNA-seq" AND "breast cancer" AND (CD44 OR CD133)[54].SRA Hierarchical Accessions: Utilize SRA's hierarchical accession system to find all samples within a study. The four levels include STUDY (SRP#, ERP#, DRP#), SAMPLE (SRS#, ERS#, DRS#), EXPERIMENT (SRX#, ERX#, DRX#), and RUN (SRR#, ERR#, DRR#) [54].
When evaluating datasets for reanalysis, critical assessment of experimental design, sequencing platform, protocol details, and sample metadata is essential to ensure data quality and relevance to specific CSC research questions.
Computational Pipeline for scRNA-seq Reanalysis
Data Preprocessing and Quality Control
The initial phase of scRNA-seq reanalysis involves rigorous quality control (QC) and preprocessing to ensure data reliability. The standard workflow consists of:
Quality Control Metrics: Filter out low-quality cells based on thresholds for unique gene counts (fewer than 300 genes per cell) and mitochondrial content (>30% of total UMI count) [52]. Additional QC measures include removing potential doublets and genes expressed in fewer than three cells [52].
Normalization and Scaling: Use SCTransform, a regularized negative binomial regression method, to normalize and scale scRNA-seq data while preserving biological heterogeneity and removing technical artifacts [52].
Batch Effect Correction: Apply integration methods such as the IntegrateData function in Seurat to remove batch effects when combining multiple datasets [52].
Dimension Reduction: Perform principal component analysis (PCA) for linear dimension reduction, followed by non-linear methods such as UMAP (Uniform Manifold Approximation and Projection) or tSNE (t-distributed Stochastic Neighbor Embedding) for visualization [52] [55].
Diagram 1: scRNA-seq Preprocessing Workflow
Cell Type Identification and CSC Annotation
Accurately identifying and annotating CSCs within heterogeneous tumor samples presents significant challenges due to the lack of universal CSC markers and the dynamic nature of stemness states [5]. The following computational approaches facilitate CSC identification:
Automated Cell Type Labelling: Both cluster-based and cell-based algorithms can be employed for cell type identification. Recent evaluations of 26 labelling algorithms in cancer contexts revealed that cell-based methods generally achieve higher performance (F1 scores ≥0.9 for top performers) compared to cluster-based methods (F1 scores ~0.5) [56]. Top-performing algorithms include scPred, CaSTLe, scANVI, and SVM [56].
CSC-Specific Marker Detection: Identify CSCs using known markers in specific cancer types. For example, in colorectal cancer, CSCs may express TFF3, AGR2, KRT8, and KRT18 [57], while in hepatocellular carcinoma, common markers include CD133, CD90, CD44, OV6, EpCAM, CD13, CD24, DLK1, and CD47 [58].
Stemness Signature Scoring: Calculate stemness indices based on established CSC gene signatures. Bioinformatics-driven approaches using machine learning-based stemness index analysis allow for identification of CSC-specific features across various cancer types [5].
Table 2: Performance Comparison of scRNA-seq Labelling Algorithms in Cancer Data
| Algorithm | Type | Average F1 Score | Strengths | Limitations |
|---|---|---|---|---|
| scPred | Cell-based | 0.97 | High performance with cancer data; handles large datasets | Longer runtime with large datasets |
| SVM | Cell-based | 0.96 | Strong overall performance; widely implemented | Performance may vary with heterogeneity |
| CaSTLe | Cell-based | 0.96 | High accuracy with complex cell populations | Computationally intensive |
| SingleR | Cell-based | 0.94 | Reference-based annotation | Requires comprehensive reference data |
| ORA | Cluster-based | 0.56 | Best performing cluster-based method | Limited by marker gene availability |
| GSVA | Cluster-based | 0.51 | Pathway-level analysis | Lower performance with rare cell types |
Advanced Analytical Frameworks for CSC Characterization
Identification of CSC Subpopulations
The process of identifying CSC subpopulations from public scRNA-seq data involves multiple analytical steps that leverage both unsupervised and supervised computational approaches:
Unsupervised Clustering: After quality control and normalization, cells are grouped based on gene expression similarity using graph-based clustering algorithms. The Seurat package typically constructs a shared nearest neighbor (SNN) graph using the top 30 principal components, then identifies cell clusters [52].
Differential Gene Expression Analysis: Identify genes significantly upregulated in potential CSC clusters compared to other cell populations using statistical tests such as Wilcoxon rank-sum test. Criteria typically include |logFC| > 0.5 and adjusted p-value < 0.05 [57] [59].
CSC Signature Validation: Validate identified CSC populations using established markers. For example, in hepatocellular carcinoma, CSC-related genes including ADM, CCL5, CD274, DLGAP5, HOXD9, IGF1, S100A9, SOCS2, and TNFRSF11B have been used to construct prognostic signatures [58].
Trajectory Inference and Cellular Dynamics
Trajectory analysis methods reconstruct the developmental continuum of cells, allowing researchers to hypothesize about CSC differentiation pathways and cellular plasticity:
Pseudotemporal Ordering: Tools such as Monocle, Slingshot, and SCANPY's PAGA algorithm model cells along a pseudotime trajectory to reconstruct differentiation processes [55]. In colorectal cancer, trajectory analysis has revealed that CSCs primarily differentiate toward cancer cells and fibroblasts [57].
RNA Velocity Analysis: The Velocyto and scVelo packages quantify RNA splicing dynamics to predict future cell states, revealing directionality in stem cell differentiation and state transitions [55] [56].
Diagram 2: CSC Identification and Analysis Workflow
Cell-Cell Communication Analysis in the TME
Understanding how CSCs interact with other components of the tumor microenvironment is critical for deciphering mechanisms of therapy resistance and immune evasion. Computational methods can infer cell-cell communication networks from scRNA-seq data:
Ligand-Receptor Interaction Mapping: Tools such as CellPhoneDB, NicheNet, and CellChat database-curated ligand-receptor pairs to identify significant interactions between CSCs and other cell types [57] [55].
Pathway Activity Analysis: Examine coordinated signaling between CSCs and other cells. In colorectal cancer, analysis has revealed that CSCs coordinate with cancer cells through CEACAM, CDH, DESMOSOME, SEMA4, EPHA, EPHB, CDH1, CSPG4, OCLN, and SEMA5 signaling pathways [57].
Spatial Relationship Inference: Emerging algorithms like Giotto and SpaOTsc can infer spatial relationships from scRNA-seq data alone, potentially identifying niche signals that maintain CSC properties [55].
Integration with Complementary Data Modalities
Combining scRNA-seq with Bulk RNA-seq Data
Integrating single-cell resolution data with bulk transcriptomic profiles enables the development of CSC prognostic signatures and validation of findings:
Identification of CSC-Associated Genes: Process scRNA-seq data to distinguish CSC subpopulations, then identify differentially expressed genes specific to CSCs compared to other cell types [57] [58].
Prognostic Model Construction: Extract CSC-related genes from scRNA-seq analysis and validate their prognostic significance using bulk RNA-seq data from sources like The Cancer Genome Atlas (TCGA). For example, in hepatocellular carcinoma, this approach identified a nine-gene CSC signature (ADM, CCL5, CD274, DLGAP5, HOXD9, IGF1, S100A9, SOCS2, TNFRSF11B) with significant prognostic value [58].
Risk Stratification Modeling: Use machine learning approaches such as LASSO-Cox regression to build multivariate prognostic models based on CSC-related genes. One study on colorectal cancer developed a risk model incorporating 16 CSC-related genes including CISD2, RNH1, DCBLD2, VDAC3, ALDH2, YBX3, FDFT1, RBM3, FKBP4, PSMG3, LRRC59, KIF9, TIMP1, ETS2, PSMA5, and RPS17 [57].
Multi-Omics Integration Approaches
Advanced integration methods combine scRNA-seq with other data types to comprehensively characterize CSC biology:
scRNA-seq with GWAS Integration: Methods like RolyPoly and LDSC-cts can integrate GWAS summary statistics with scRNA-seq data to identify cell types associated with disease risk. In chronic liver disease, this approach identified B cells and natural killer cells as hepatocellular carcinoma-associated cell types [52].
Epigenomic Data Integration: Combine scRNA-seq with single-cell ATAC-seq (scATAC-seq) to link CSC transcriptional programs with regulatory elements. Tools like Signac and ArchR facilitate this integration [55].
Proteogenomic Integration: Emerging technologies such as CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing) enable simultaneous measurement of RNA and cell surface proteins, allowing for more precise identification of CSCs using both transcriptomic and proteomic markers [55].
Experimental Validation and Translational Applications
Functional Validation of Computational Findings
Computational predictions from scRNA-seq reanalysis require experimental validation to establish biological significance:
In Vitro Functional Assays: Validate CSC properties through sphere formation assays, drug sensitivity testing, and differentiation potential assessment. For instance, studies have demonstrated that CSC-enriched tumor spheres show elevated PD-L1 levels and activate the SGK2/β-catenin pathway, promoting epithelial-mesenchymal transition [58].
Lineage Tracing and Clonal Analysis: Employ DNA barcoding techniques to track the fate of putative CSCs identified through computational methods, assessing their self-renewal and differentiation capacities [51].
CRISPR-Based Functional Screens: Validate gene essentiality in CSCs through CRISPR knockout or inhibition screens targeting computationally identified CSC-associated genes [5].
Therapeutic Translation and Clinical Implications
The ultimate goal of CSC-focused scRNA-seq reanalysis is to translate findings into improved clinical strategies:
Prognostic Biomarker Development: CSC-related gene signatures derived from integrated analysis can stratify patients by risk. In hepatocellular carcinoma, a nine-gene CSC signature significantly separated high-risk and low-risk patients, with high-risk patients showing shorter overall survival [58].
Drug Repurposing Opportunities: Identify potential CSC-targeting compounds through connectivity mapping approaches that link CSC gene expression signatures with drug response databases. One study identified several drugs capable of targeting the expression or signaling network of CSC-associated genes, including modulators of APOC1 in breast cancer and SLC44A5/CAV2 in lung cancer [59].
Immunotherapy Applications: Explore CSC-immune cell interactions to identify potential immunotherapeutic targets. For instance, CSC markers have been shown to correlate with the immunosuppressive tumor microenvironment, offering valuable insights for immunotherapy in HCC patients [58].
Table 3: Essential Research Reagent Solutions for CSC-focused scRNA-seq Analysis
| Reagent/Category | Specific Examples | Function in Analysis |
|---|---|---|
| Analysis Platforms | Seurat, Scanpy, Monocle | Primary environments for scRNA-seq data processing and analysis |
| Cell Type Labelling Algorithms | scPred, SVM, SingleR | Automated annotation of cell types, including CSCs |
| Trajectory Analysis Tools | Monocle, PAGA, Slingshot, RNA Velocity | Inference of differentiation trajectories and cellular dynamics |
| Cell-Cell Communication Tools | CellPhoneDB, NicheNet, CellChat | Analysis of ligand-receptor interactions in the TME |
| Reference Datasets | TCGA, ICGC, GEO datasets | Validation and integration with bulk transcriptomic data |
| CSC Marker Databases | CSC-specific signatures (CD44, CD133, ALDH1A1, etc.) | Identification and validation of CSC subpopulations |
The reanalysis of public scRNA-seq datasets represents a powerful approach for advancing our understanding of cancer stem cell biology, offering opportunities to overcome key challenges in CSC identification, characterization, and targeting. By applying sophisticated computational methods to existing data, researchers can extract novel insights into CSC heterogeneity, plasticity, and interactions within the tumor microenvironment. The integration of scRNA-seq with complementary data modalities, including bulk RNA-seq, epigenomic data, and clinical information, further enhances the potential to develop clinically relevant prognostic signatures and therapeutic strategies. As public data repositories continue to expand and computational methods evolve, the systematic reanalysis of existing scRNA-seq datasets will play an increasingly important role in unlocking the mysteries of cancer stem cells and developing more effective approaches for cancer treatment.
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [5]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies [5]. The fundamental challenge in CSC research lies in their remarkable heterogeneity and the absence of universal biomarkers, as surface proteins such as CD44 and CD133 are not exclusive to CSCs and are often expressed in normal stem cells or non-tumorigenic cancer cells [5]. This heterogeneity suggests that CSC identity is shaped by both intrinsic genetic programs and extrinsic cues, with stem-like features that can be acquired de novo by non-CSCs in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure [5].
Single-cell transcriptomics has revolutionized our ability to dissect this complexity at unprecedented resolution. By enabling the characterization of gene expression profiles in individual cells, this technology provides powerful insights into CSC heterogeneity, plasticity, and their role in treatment resistance [60]. The integration of transcriptomic data with genomic and epigenomic information from the same single cells creates a multi-dimensional view of CSC biology that was previously unattainable with bulk sequencing approaches [60] [61]. This technical guide explores how single-cell transcriptomics is illuminating the complex interplay between the genome, epigenome, and transcriptome of CSCs, providing researchers with sophisticated tools to overcome long-standing challenges in CSC identification and targeting.
Core Computational Methods for CSC Identification
Distinguishing Malignant from Non-Malignant Cells
A critical first step in single-cell CSC analysis is distinguishing malignant cells from non-malignant cells of the same lineage in tumor samples. Computational approaches typically leverage three main features, either alone or in combination: expression of cell-of-origin marker genes, inter-patient tumor heterogeneity, and inferred copy-number alterations [62].
Table 1: Computational Methods for Identifying Malignant Cells in scRNA-seq Data
| Method | Primary Approach | Key Features | Applicability to CSCs |
|---|---|---|---|
| InferCNV [62] | Compares smoothed gene expression along chromosomes to reference cells | Uses hidden Markov model; optional Bayesian mixture refinement | Identifies malignant cell clusters based on CNA patterns |
| CopyKAT [62] | Combines hierarchical clustering with Gaussian mixture model | Identifies "confident normal" cells to estimate diploid baseline | Classifies cells as diploid or aneuploid with high accuracy |
| SCEVAN [62] | Joint segmentation algorithm to identify breakpoints | Starts with small set of confident normal cells | Detects subclonal populations within tumors |
| Numbat [62] | Integrates gene expression with haplotype information | Leverages allelic imbalance estimates | Supports CNA calls with haplotype phasing |
| CaSpER [62] | Combines gene expression with allelic shift signal | Estimates genome-wide loss-of-heterozygosity | Identifies both large and focal CNA events |
Cell-of-origin markers provide an initial filtering step but are insufficient alone, as tumors often contain both malignant and normal epithelial cells [62]. For example, in head-and-neck squamous cell carcinoma (HNSCC), Puram et al. applied a signature of epithelial genes to identify malignant cells, then validated this classification with orthogonal CNA readouts [62]. Similarly, in nasopharyngeal carcinoma, Chen et al. first distinguished epithelial cells using marker-based annotation, then applied InferCNV to separate normal from malignant epithelial cells [63]. This two-step approach is particularly valuable for CSC identification, as CSCs often share lineage markers with their normal counterparts while harboring distinct genomic alterations.
Copy Number Alteration Inference from scRNA-seq Data
Copy-number alterations and aneuploidy are hallmarks of cancer cells, present in approximately 90% of solid tumors and 75% of hematopoietic cancers [62]. These alterations can be inferred from scRNA-seq data by analyzing patterns of gene expression across chromosomal regions, as genomic duplications or deletions create characteristic increases or decreases in average expression levels across affected regions [62].
The analytical workflow for CNA inference typically begins with quality control and normalization of the gene expression matrix, followed by gene ordering based on genomic coordinates. A reference set of diploid cells (often immune cells or normal cells from the same lineage) is used to establish baseline expression patterns. The algorithm then calculates moving averages of expression along chromosomes and applies statistical models to identify regions with significant deviations from the baseline [62].
Recent benchmarks indicate that methods exploiting allelic shift signals (Numbat, CaSpER) show superior performance for CNA identification, while CopyKAT is recommended when only expression matrices are available [62]. For CSC research, these approaches enable the identification of malignant cell clusters that may represent CSC-enriched populations, particularly when combined with stemness marker expression.
Figure 1: Computational Workflow for CSC Identification. The process integrates cell-of-origin marker expression with copy-number alteration analysis and stemness scoring to identify putative CSC populations.
Experimental Design and Methodologies
Single-Cell Isolation and Library Preparation
The foundation of successful single-cell transcriptomics lies in robust cell isolation and library preparation. Several advanced isolation strategies have been developed to meet the technical demands of high-resolution analysis [61]:
- Fluorescence-Activated Cell Sorting (FACS): Enables high-throughput isolation based on fluorescently labeled surface markers. Particularly valuable for CSC studies where markers like CD44, CD133, or ALDH1 activity can be used for enrichment [61].
- Microfluidic Technologies: Platforms like 10x Genomics Chromium provide high-throughput, low-noise capture with minimal cellular stress. The commercially available 10x Genomics system has significantly expanded the scalability and precision of scRNA-seq [61].
- Laser Capture Microdissection (LCM): Allows precise isolation of cells from specific tissue regions while preserving spatial context, making it suitable for studying CSC niche interactions [61].
Following isolation, library preparation for scRNA-seq incorporates efficient mRNA reverse transcription, cDNA amplification, and the use of unique molecular identifiers (UMIs) and cell-specific barcodes to minimize technical noise [61]. These technical optimizations have enabled the detection of rare cell types, characterization of intermediate cell states, and reconstruction of developmental trajectories across diverse biological contexts [61].
Table 2: Essential Research Reagents for Single-Cell CSC Studies
| Reagent Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| Cell Isolation Reagents | FACS antibodies (CD44, CD133, ALDH1); MACS kits | Enrichment of putative CSC populations prior to sequencing |
| Single-Cell Library Prep Kits | 10x Genomics Chromium Single Cell 3' Reagent Kit; BD Rhapsody HT-Xpress | Generation of barcoded single-cell libraries for transcriptome analysis |
| Epigenetic Assay Kits | scATAC-seq Kit; CUT&Tag Kit | Mapping chromatin accessibility and histone modifications in single cells |
| Cell Viability Reagents | Propidium iodide; DAPI; Calcein AM | Assessment of cell viability during isolation procedures |
| Surface Protein Detection | CITE-seq antibodies | Simultaneous profiling of transcriptome and surface proteins |
Multi-Omics Integration at Single-Cell Resolution
While transcriptomics provides crucial information about cellular states, a comprehensive understanding of CSCs requires integration across multiple molecular layers. Single-cell multi-omics technologies now enable coupled measurements of the genome, epigenome, transcriptome, and proteome from the same cells [61]:
- scATAC-seq: Maps chromatin accessibility using Tn5 transposase-mediated insertion, identifying accessible regulatory elements that define cellular identity [61].
- scCUT&Tag: Profiles histone modifications through antibody-guided capture of specific epigenetic marks, offering insights into the epigenetic regulation of stemness [61].
- CITE-seq: Simultaneously measures transcriptome and surface protein expression by using oligonucleotide-labeled antibodies, allowing correlation of stemness markers with transcriptional states [61].
The integration of these modalities is particularly powerful for CSC research. For example, in colorectal cancer, single-cell analyses have revealed that non-coding RNAs exhibit significantly higher cell type specificity compared to protein-coding genes, with 996 lncRNAs strongly enriched in epithelial cells and 98 differentially expressed in tumor samples [64]. This integration helps bridge the gap between molecular alterations and their functional consequences in the tumor ecosystem [61].
Analytical Frameworks for CSC Characterization
Stemness Indices and Trajectory Inference
Computational methods for quantifying stemness and differentiation trajectories from scRNA-seq data have become essential tools in CSC research. Machine learning-based stemness index analysis allows for the identification of CSC-specific features across various cancer types, guiding personalized treatment approaches [5]. These approaches typically involve:
- RNA Velocity Analysis: Predicts cell states over time periods by incorporating splicing information, promoter state switching, translation, and RNA/protein degradation [63].
- Pseudotemporal Ordering: Reconstructs differentiation trajectories from stem-like to differentiated states using tools like Monocle or Slingshot.
- Regulatory Network Inference: Identifies key transcription factors maintaining stemness by integrating transcriptome and epigenome data.
In a study of pancreatic ductal adenocarcinoma (PDAC), single-cell RNA sequencing revealed substantial heterogeneity in malignant subtypes, consisting of multiple subpopulations with distinct proliferation and migration capabilities [60]. Similar approaches in lung cancer identified residual disease cells that showed a transition to a primitive cell state under therapeutic pressure [60], illustrating how single-cell technologies can capture the dynamic plasticity of CSCs in response to treatment.
Dissecting the CSC Niches and Immune Microenvironment
CSCs reside within a specialized microenvironment—the "CSC niche"—which plays an indispensable role in sustaining their stemness and immune evasion capabilities [2]. This niche comprises a heterogeneous array of cell types including immune cells, stromal cells, endothelial cells, and fibroblasts, along with cytokines, growth factors, metabolites, and extracellular matrix components [2]. Single-cell transcriptomics enables deconvolution of these complex ecosystems by:
- Cell-Cell Communication Analysis: Using tools like CellChat or NicheNet to infer ligand-receptor interactions between CSCs and niche components.
- Spatial Transcriptomics Integration: Correlating transcriptional profiles with spatial positioning to identify niche geographical organization.
- Immune Context Characterization: Profiling tumor-infiltrating immune cells and their functional states relative to CSC localization.
The CSC niche actively shapes the tumor immune landscape by promoting immune suppression. For instance, CSCs employ intrinsic immune evasion mechanisms including upregulation of checkpoint proteins like PD-L1, downregulation of antigen-presentation machinery, and recruitment of immunosuppressive cells through cytokine secretion [2]. In bladder cancer, the stem cell marker ALDH1A1 is positively correlated with PD-L1 expression, linking stemness with immune evasion [2]. Single-cell approaches are essential for unraveling these interconnected networks.
Figure 2: CSC-Niche Interactions. Cancer stem cells engage in bidirectional communication with various components of their microenvironment, creating an immunosuppressive and protective niche.
Technical Considerations and Limitations
While single-cell technologies offer unprecedented insights into CSC biology, several technical challenges must be considered in experimental design and data interpretation:
- Sparse Data and Dropout Effects: The low RNA content of individual cells combined with inefficient capture leads to missing data points (dropouts), particularly affecting lowly expressed transcripts, including key regulatory genes in CSCs.
- Integration Across Platforms and Batches: Combining datasets from different patients, conditions, or technological platforms requires sophisticated normalization and integration approaches to remove technical artifacts while preserving biological signals.
- Cell Viability and Stress Responses: Isolation procedures may induce cellular stress, potentially altering transcriptional profiles, particularly in sensitive populations like CSCs.
- Computational Resources and Expertise: Analysis of single-cell datasets demands substantial computational resources and specialized bioinformatics expertise, creating barriers to adoption.
Recent technological advances are addressing these limitations. Platforms such as 10x Genomics Chromium X and BD Rhapsody HT-Xpress now enable profiling of over one million cells per run with improved sensitivity and multimodal compatibility [61]. Additionally, computational methods like Harmony provide unified frameworks for data integration, visualization, analysis, and interpretation of single-cell genomics data across discrete timepoints [63].
Therapeutic Implications and Future Directions
The application of single-cell transcriptomics to CSC research has profound implications for therapeutic development. By revealing the molecular pathways that maintain stemness and drive resistance, these approaches enable more effective targeting strategies:
- Metabolic Dependencies: Single-cell analyses have revealed that metabolic plasticity allows CSCs to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, enabling survival under diverse environmental conditions [5].
- Combination Therapies: Integration of CSC-targeting agents with immunotherapy shows particular promise. For example, targeting CD47 in combination with PD-L1 blockade can synergistically enhance anti-tumor immunity [2].
- Dynamic Resistance Mechanisms: Tracking CSC evolution under treatment pressure reveals adaptive resistance pathways. In metastatic lung cancer, single-cell analyses identified distinct gene expression patterns in residual disease, with cells showing a transition to a primitive state [60].
Future directions in the field include the development of 3D organoid models, CRISPR-based functional screens, and AI-driven multiomics analysis to further advance precision-targeted CSC therapies [5]. Emerging strategies such as dual metabolic inhibition, synthetic biology-based interventions, and immune-based approaches hold promise for overcoming CSC-mediated therapy resistance [5].
As single-cell technologies continue to evolve, they will increasingly enable the mapping of CSC trajectories across disease progression and treatment, providing unprecedented opportunities for intervention. The integration of single-cell transcriptomics with spatial information, proteomics, and computational modeling will be essential for developing the next generation of CSC-targeted therapies aimed at reducing cancer recurrence and improving patient outcomes.
Cancer stem cells (CSCs) represent a functionally distinct subpopulation within tumors that possess self-renewal capacity, differentiation potential, and enhanced therapy resistance. These cells are increasingly recognized as drivers of tumor initiation, progression, metastasis, and recurrence [5]. The identification and characterization of CSCs rely heavily on specific biomarkers, which vary significantly across cancer types and even within subtypes of the same cancer. Understanding the correlation between the expression of these markers and clinical outcomes is paramount for developing more accurate prognostic tools and targeted therapeutic strategies [20]. This technical guide examines the current landscape of CSC marker research, focusing on the evidence linking marker expression to diagnostic and prognostic applications, detailed experimental methodologies, and the underlying biological networks that govern CSC behavior.
Cancer Stem Cell Marker Expression and Clinical Correlations
The prognostic significance of CSC markers has been demonstrated across a wide spectrum of malignancies. The expression levels of specific markers consistently correlate with aggressive disease features, including advanced stage, metastasis, and poor survival outcomes.
Solid Tumors
Non-Small Cell Lung Cancer (NSCLC): In stage IIIA NSCLC, high expression of the transcription factor OCT4 is significantly associated with poorer overall survival, particularly in the lung adenocarcinoma subtype [65] [66]. A composite Tumor Stemness Index (TSI), which integrates multiple CSC marker expressions with clinical parameters like age and micropapillary components, has also been validated as a significant prognostic tool [66]. For early-stage NSCLC (Stages I-IIA), combined detection of CD133 and OCT4 provides superior diagnostic accuracy compared to single markers, with an Area Under the Curve (AUC) of 0.893 in ROC analysis. High expression of both markers correlates with poor differentiation, larger tumor size (≥3 cm), lymph node metastasis, and advanced stage (IB-IIA) [67].
Colorectal Carcinoma (CRC): The co-expression of CD133 and CD44 is a powerful predictor of metastatic potential. Studies show that 71.4% of patients with metastatic CRC exhibit high co-expression of both markers, compared to only 37.9% in patients without distant metastases [68]. This co-expression is statistically significantly associated with advanced disease stage, deeper tumor invasion (T-category), and higher nodal status (N-category) [68].
Bladder Cancer: A recent systematic review and meta-analysis identified CD44, its variant CD44v9, and ALDH1A1 as significantly associated with poor survival outcomes [69]. The combined expression of CD44 and the transcription factor Nanog emerged as an independent prognostic factor for recurrence-free survival, while other markers like SOX2, SOX4, Notch-1, and OCT-4 correlated with tumor progression and aggressiveness [69].
Oral Squamous Cell Carcinoma (OSCC): Research indicates that distinct CSC subpopulations, identified by different markers, impact different clinical parameters. p75NTR+ cells are associated with smaller tumor size and poorer differentiation but correlate with poor survival in patients otherwise deemed to have a better prognosis. In contrast, ALDH1A1+ cells are significantly linked to lymph node metastasis [8].
Table 1: Prognostic Significance of Key CSC Markers Across Different Cancers
| Cancer Type | Marker | Prognostic/Diagnostic Value | Clinical Correlation |
|---|---|---|---|
| NSCLC (Stage IIIA) | OCT4 | Poor Prognosis | Significantly associated with poorer overall survival, especially in lung adenocarcinoma [65] [66]. |
| NSCLC (Early-Stage) | CD133 & OCT4 | Diagnosis & Poor Prognosis | Combined AUC=0.893 for diagnosis; high expression linked to aggressive features and reduced 2-year overall survival [67]. |
| Colorectal Cancer | CD133 & CD44 | Metastatic Potential | High co-expression (71.4%) in metastatic disease vs. non-metastatic (37.9%); linked to advanced stage and nodal status [68]. |
| Bladder Cancer | CD44 / CD44v9 | Poor Prognosis | Significantly associated with adverse survival outcomes; CD44+Nanog+ an independent factor for recurrence-free survival [69]. |
| Hepatocellular Carcinoma | CD133, EpCAM, CD90 | Diagnosis & Aggressiveness | Associated with chemoresistance, tumorigenicity, and metastatic potential; high predictive value for recurrence and aggression [70]. |
| Oral Squamous Cell Carcinoma | p75NTR | Poor Prognosis | Associated with poorer survival in clinically lower-risk patients and smaller, less-differentiated tumors [8]. |
| ALDH1A1 | Metastatic Potential | High frequency of positive cells associated with lymph node metastasis [8]. |
Underlying Mechanisms Linking Markers to Aggressive Phenotypes
The correlation between CSC marker expression and poor clinical outcomes is driven by well-defined biological mechanisms:
- Therapy Resistance: CSCs utilize multiple mechanisms to evade conventional treatments. They often exist in a quiescent state, avoiding therapies that target rapidly dividing cells. They also upregulate drug efflux pumps like ABCG2 and enhance DNA repair capacity [5] [70]. For instance, CD133+ HCC cells demonstrate resistance to doxorubicin and 5-FU via activation of Akt/PKB and Bcl-2 pathways [70].
- Metastatic Potential: CSCs are master regulators of the epithelial-mesenchymal transition (EMT), a key process in metastasis. Markers such as CD44 are intimately involved in cell adhesion, migration, and invasion, facilitating detachment from the primary tumor and colonization of distant sites [70] [20].
- Tumor Initiation and Regeneration: The defining functional property of CSCs is their ability to initiate and recapitulate a tumor. Xenotransplantation assays consistently show that marker-positive cells (e.g., CD133+, EpCAM+, CD90+) can form tumors with very few cells, whereas marker-negative cells cannot, explaining their role in tumor recurrence [70].
Experimental Protocols for Marker Analysis
Robust and standardized experimental protocols are essential for validating the correlation between CSC marker expression and clinical outcomes. The following section details key methodologies.
Immunohistochemistry (IHC) for Protein Detection
IHC is a cornerstone technique for visualizing protein expression within the context of tissue architecture and pathology.
Detailed Protocol [66]:
- Tissue Preparation: Formalin-fixed, paraffin-embedded (FFPE) tumor tissues are sectioned at a thickness of 4 μm and mounted on poly-L-lysine-coated glass slides. Slides are baked at 60°C for 2 hours to ensure adhesion.
- Deparaffinization and Rehydration: Slides are immersed in xylene to remove paraffin, followed by a graded series of ethanol (e.g., 100%, 95%, 70%) and finally distilled water.
- Antigen Retrieval: To unmask epitopes, slides are subjected to heat-induced epitope retrieval using a pressure cooker with sodium citrate buffer (pH 6.0) at 121°C for 2 minutes. Slides are then allowed to cool to room temperature.
- Peroxidase Blocking: Endogenous peroxidase activity is quenched by incubating sections with 3% hydrogen peroxide for 10 minutes.
- Protein Blocking: Non-specific binding sites are blocked using 10% normal goat serum for 30 minutes at room temperature.
- Primary Antibody Incubation: Sections are incubated with optimally titrated primary antibodies (e.g., anti-OCT4 at 1:200, anti-CD133 at manufacturer's recommended dilution) overnight at 4°C in a humidified chamber.
- Secondary Antibody Incubation: After washing, HRP (Horseradish Peroxidase)-labeled secondary antibodies (e.g., goat anti-rabbit, 1:500) are applied and incubated for 30 minutes at 37°C.
- Chromogenic Detection: The enzyme reaction is developed using 3,3'-Diaminobenzidine (DAB) as a chromogen, which produces a brown precipitate at the antigen site.
- Counterstaining and Mounting: Slides are counterstained with hematoxylin to visualize nuclei, dehydrated, cleared, and mounted with a permanent mounting medium.
- Controls: Positive control tissues known to express the target antigen and negative controls (omission of the primary antibody) must be included in each run to ensure specificity.
Scoring and Analysis: Staining is typically evaluated by a pathologist. A semi-quantitative H-score is often used, which incorporates both the intensity of staining and the percentage of positive cells. For some studies, expression is classified as "high" or "low" based on a predefined threshold (e.g., more than 50% of tumor cells positive) [66] [68].
Quantitative Real-Time PCR (qRT-PCR) for Gene Expression
qRT-PCR allows for the precise quantification of marker mRNA levels.
Detailed Protocol [67]:
- RNA Extraction: Total RNA is isolated from fresh-frozen or optimally preserved FFPE tissue sections using commercial kits based on silica-membrane columns or magnetic beads. RNA concentration and purity are assessed spectrophotometrically.
- cDNA Synthesis: High-Capacity cDNA Reverse Transcription kits are used. Typically, 1 μg of total RNA is reverse-transcribed in a reaction containing reverse transcriptase, random hexamers, dNTPs, and reaction buffer.
- qPCR Amplification: The synthesized cDNA is amplified in a real-time PCR instrument using gene-specific primers and probes. A typical reaction mix includes: cDNA template, forward and reverse primers, SYBR Green or TaqMan probe master mix, and nuclease-free water.
- Thermal Cycling Conditions: A standard two-step cycling protocol is used:
- Hold Stage: 95°C for 10 minutes (polymerase activation).
- PCR Cycle (40 repeats): 95°C for 15 seconds (denaturation) followed by 60°C for 1 minute (annealing/extension).
- Data Analysis: The comparative Ct (ΔΔCt) method is used for relative quantification. Expression levels of the target genes (e.g., PROM1 (CD133), POU5F1 (OCT4)) are normalized to an endogenous reference gene (e.g., GAPDH, ACTB) and compared to a calibrator sample (e.g., healthy control tissue).
Diagram 1: IHC staining workflow
Signaling Pathways and Marker Networks in CSCs
The expression and function of CSC markers are regulated by a complex interplay of conserved signaling pathways that maintain stemness, promote survival, and drive therapeutic resistance.
Core Signaling Pathways
- Wnt/β-catenin Pathway: This is a critically dysregulated pathway in many CSCs. Nuclear β-catenin activates the transcription of key stemness genes, including PROM1 (CD133) and EPCAM. Mutations in pathway components (e.g., CTNNB1, AXIN1) are common in cancers like HCC, leading to constitutive activation [70].
- Notch Signaling Pathway: Notch activation promotes stem-like traits, inhibits differentiation, and induces EMT. It frequently crosstalks with other pathways like Hedgehog to sustain the CSC population [70] [20].
- Hedgehog (Hh) Pathway: Hh signaling is involved in cell fate determination and self-renewal. Its activation upregulates CSC-specific genes and contributes to tumor maintenance [70].
- PI3K/Akt/mTOR Axis: This central pathway regulates cell growth, proliferation, and metabolism. Its activation in CSCs promotes survival and is a key mediator of resistance to chemotherapy and targeted therapies [5] [71].
- TGF-β Pathway: This pathway is a potent inducer of EMT, enhancing the invasive and metastatic potential of CSCs [70].
These pathways do not operate in isolation but form a robust, interconnected network. Furthermore, epigenetic regulators like miRNAs and lncRNAs fine-tune these pathways, adding another layer of complexity to CSC regulation [70].
Diagram 2: Core signaling pathways in CSCs
Network Biology of CSC Markers
Computational approaches are revealing the complex distribution and co-expression patterns of CSC markers. Hypergraph theory models markers as "hyperedges" that connect all the organs or cancer types in which they are expressed. For example, a marker like CD44 forms a hyperedge linking organs such as breast, colon, and pancreas [71]. This framework helps identify which markers are ubiquitously expressed and which are tissue-specific. Analysis of such networks shows that the same CSC markers are often shared between certain primary and metastatic organs, suggesting pre-determined metastatic routes based on shared microenvironmental niches that support specific CSC phenotypes [71]. Mutual information analysis can then quantify the strength of these organ-marker associations, identifying key markers that may drive metastasis to specific sites.
The Scientist's Toolkit: Essential Research Reagents and Materials
The experimental investigation of CSC markers requires a suite of well-validated reagents and tools.
Table 2: Essential Research Reagents for CSC Marker Studies
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| Primary Antibodies | Detection of specific CSC marker proteins via IHC, IF, and Flow Cytometry. | Anti-CD44, Anti-CD133 (clone AC133), Anti-OCT4, Anti-ALDH1A1. Validation for specific applications (IHC on FFPE) is critical [66] [8]. |
| Validated Secondary Antibodies | Conjugated to enzymes (HRP) or fluorophores to detect primary antibody binding. | HRP-goat anti-rabbit for IHC; Fluorophore-conjugated antibodies for flow cytometry and immunofluorescence [66]. |
| IHC Detection Kits | Amplify signal and visualize antibody binding in tissue sections. | Avidin-Biotin Complex (ABC) or polymer-based EnVision detection systems [66] [68]. |
| RNA Isolation Kits | Extract high-quality total RNA from tissues or cells for gene expression analysis. | Kits based on silica-membrane columns or magnetic beads; optimized for FFPE tissues if required [67]. |
| qRT-PCR Assays | Quantify mRNA expression levels of CSC marker genes. | Gene-specific TaqMan assays or SYBR Green primer sets for genes like PROM1 (CD133), POU5F1 (OCT4) [67]. |
| Flow Cytometry Panel | Identify, isolate (FACS), and characterize live CSC populations from dissociated tumors. | Antibodies against cell surface markers (CD44, CD133, CD90) combined with viability dyes and ALDH activity assays (ALDEFLUOR) [8]. |
| Cell Culture Media | Support the growth and maintenance of primary tumor cells or CSC-enriched spheroids. | Serum-free media supplemented with growth factors (EGF, bFGF) for non-adherent sphere formation [5]. |
The systematic correlation of CSC marker expression with clinical outcomes has firmly established the prognostic and diagnostic utility of this class of biomarkers. The evidence shows that markers like OCT4, CD133, and CD44, particularly in combination, provide significant value for risk stratification, predicting metastasis, and informing prognosis in cancers ranging from NSCLC and colorectal carcinoma to bladder and liver cancer. The clinical application of these findings, however, hinges on standardized, validated experimental protocols like IHC and qRT-PCR, and a deep understanding of the complex signaling networks that regulate stemness. Future research integrating single-cell multi-omics, advanced computational models, and functional genomics will be essential to dissect the full heterogeneity of CSCs and translate these biomarkers into precise diagnostic tools and effective targeted therapies that ultimately improve patient outcomes.
Overcoming Key Challenges: Marker Plasticity, Heterogeneity, and Therapy Resistance
The cancer stem cell (CSC) paradigm provides a compelling explanation for tumor initiation, progression, and therapeutic resistance. A central tenet of this model is that CSCs constitute a subpopulation responsible for driving intratumoral heterogeneity. However, a significant challenge in validating and therapeutically targeting this population is the stark absence of universal CSC markers. This whitepaper synthesizes current evidence demonstrating that CSC marker expression is highly variable across and within tumor types, dynamic over time, and influenced by cellular plasticity and the tumor microenvironment. We summarize quantitative data on marker heterogeneity, detail standard and emerging experimental protocols for CSC identification, and provide a toolkit of essential research reagents. Confronting the non-universality of CSC markers is paramount for developing robust, context-specific strategies to eradicate the root of tumorigenesis.
The cancer stem cell (CSC) theory posits that tumors are organized hierarchically, with a small subset of cells—CSCs—driving tumorigenesis, metastasis, and relapse due to their self-renewal and differentiation capacities [5] [72]. This hierarchy is a fundamental source of intratumoral heterogeneity, the phenotypic and functional variation observed within a single tumor [73].
A critical obstacle in CSC research is the inability to define this population using a consistent set of biological markers. Unlike normal stem cells in certain tissues, CSCs across different cancer types, and even within the same tumor, do not share a universal surface protein or genetic signature [5] [8]. This lack of universality stems from several factors: the influence of the cell and tissue of origin, the remarkable plasticity of CSCs that allows them to interconvert with non-CSCs, and the dynamic crosstalk with the tumor microenvironment (TME) [37] [73]. The reliance on non-universal markers complicates the isolation, study, and therapeutic targeting of CSCs, posing a major hurdle in translating CSC biology into clinical applications.
Evidence for Marker Heterogeneity
Empirical data from numerous studies consistently reveal extensive heterogeneity in the expression profiles of putative CSC markers. The tables below summarize key findings.
Table 1: Variability of Common CSC Markers Across Different Cancer Types
| Cancer Type | Putative CSC Markers | Reported Frequency in Tumors | Functional Evidence |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) | CD34⁺/CD38⁻ | <1% [37] | Tumor initiation in immunodeficient mice [5] |
| Breast Cancer | CD44⁺/CD24⁻/low | Highly variable [37] | 200 cells sufficient for tumor formation [37] |
| Breast Cancer | ALDH1High | <1% (minimal overlap with CD44⁺/CD24⁻) [37] | Tumorigenicity and self-renewal [37] |
| Glioblastoma & Colon Cancer | CD133⁺ (PROM1) | Up to 20% [37] | Debated; both CD133⁺ and CD133⁻ populations can be tumorigenic [37] |
| Oral Squamous Cell Carcinoma (OSCC) | p75NTR⁺ | Associated with small-size, poorer-differentiated tumors [8] | Correlated with proliferation and self-renewal markers [8] |
| Oral Squamous Cell Carcinoma (OSCC) | ALDH1A1⁺ | Associated with lymph node metastasis [8] | Subpopulations can emerge de novo from marker-negative cells [8] |
Table 2: Key Studies Demonstrating CSC Marker Heterogeneity and Plasticity
| Study Model | Key Finding on Heterogeneity | Implication |
|---|---|---|
| Oral Squamous Cell Carcinoma (OSCC) [8] | p75NTR and ALDH1A1 markers rarely co-localized; distinct subpopulations impacted different clinical parameters (tumor size vs. metastasis). | Multiple CSC subpopulations with distinct phenotypes can co-exist within a single tumor. |
| Breast Cancer [37] | ALDH1High and CD44⁺/CD24⁻/low identified largely non-overlapping cell populations, both with tumor-initiating capacity. | No single marker can isolate the entire CSC pool, even within one cancer type. |
| Various Cancers (Plasticity) [72] [73] | Non-CSCs can dedifferentiate and re-acquire CSC markers and properties upon stimulation (e.g., TGF-β, HGF). | CSC identity is a dynamic state, not a fixed attribute; marker expression is fluid. |
| Colon Cancer [5] | No single marker (e.g., CD133) was fully reliable; combinatorial marker sets (CD44, EpCam, CD166) enabled more robust CSC enrichment. | Identification of CSCs may require patient- or tumor-specific combinatorial marker panels. |
Methodologies for CSC Identification and Characterization
Given the lack of universal markers, the field relies on functional assays to define CSCs, often used in conjunction with surface marker enrichment.
Core Experimental Protocols
1. Fluorescence-Activated Cell Sorting (FACS) with Surface Marker Panels This is the gold standard for isolating putative CSC populations based on cell surface antigen expression [74].
- Workflow:
- Tissue Processing: Create a single-cell suspension from a fresh tumor sample via mechanical dissociation and enzymatic digestion (e.g., collagenase/hyaluronidase).
- Antibody Staining: Incubate cells with fluorochrome-conjugated antibodies against putative CSC markers (e.g., anti-CD44, anti-CD24, anti-CD133) and relevant isotype controls.
- FACS Analysis and Sorting: Use a flow cytometer to sort distinct populations (e.g., CD44⁺CD24⁻, CD133⁺) into separate collection tubes.
- Validation: Proceed to functional validation assays (see below).
2. Side Population (SP) Assay A functional assay that isolates cells based on their ability to efflux Hoechst 33342 dye via ATP-binding cassette (ABC) transporters like ABCG2, a characteristic of some stem cells [74].
- Workflow:
- Hoechst Staining: Incubate a single-cell suspension with the DNA-binding dye Hoechst 33342 at a defined concentration (e.g., 5 µg/mL) for 90 minutes at 37°C.
- Control for Specificity: Include a parallel sample stained with Hoechst 33342 in the presence of an ABC transporter inhibitor like verapamil (e.g., 50 µM). This control should cause the SP to disappear.
- FACS Analysis: Analyze cells using dual-wavelength flow cytometry (blue vs. red emission). The SP appears as a distinct, low-staining "tail" on the density plot.
- Collection and Validation: Sort the SP and non-SP populations for functional assays.
3. In Vivo Tumorigenicity Limiting Dilution Assay (LDA) The definitive functional test for CSCs, which assesses the capacity of sorted cells to initiate and recapitulate tumor heterogeneity in immunocompromised mice [5] [74].
- Workflow:
- Cell Transplantation: Inoculate serial dilutions of FACS-sorted putative CSCs (e.g., 10, 100, 1000 cells) orthotopically or subcutaneously into NOD/SCID or NSG mice. Co-inject with Matrigel to enhance engraftment.
- Tumor Monitoring: Palpate and measure tumor formation weekly over 12-24 weeks.
- Data Analysis: Use LDA software to calculate the frequency of tumor-initiating cells (TICs) in each sorted population. A significantly higher TIC frequency in the marker-enriched population confirms the presence of CSCs.
- Serial Transplantation: Excise the primary xenograft, dissociate it into a single-cell suspension, and repeat the transplantation process to confirm self-renewal capacity.
Diagram 1: Experimental workflow for isolating and validating CSCs, integrating surface marker sorting and functional assays.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for CSC Identification and Functional Analysis
| Research Reagent / Tool | Function / Application | Specific Examples |
|---|---|---|
| Fluorochrome-Conjugated Antibodies | Label cell surface antigens for FACS-based isolation of putative CSCs. | Anti-human CD44-FITC, CD24-PE, CD133/1-APC [5] [37]. |
| Hoechst 33342 | DNA-binding dye used in the Side Population (SP) assay to identify cells with high ABC transporter activity. | Used at 2.5-5 µg/mL for 90 min at 37°C; verapamil control is essential [74]. |
| Immunodeficient Mouse Models | In vivo hosts for tumorigenicity assays, allowing the engraftment of human tumor cells. | NOD/SCID, NSG (NOD-scid IL2Rγnull) mice [5] [37]. |
| Matrigel / Basement Membrane Matrix | Extracellular matrix supplement co-injected with cells to enhance tumor engraftment and growth in vivo. | Corning Matrigel Matrix, Geltrex [5]. |
| ALDEFLUOR Assay Kit | Functional assay to identify cells with high aldehyde dehydrogenase (ALDH) activity, a CSC marker in many cancers. | StemCell Technologies Kit; uses BODIPY-aminoacetate substrate [8] [37]. |
| CRISPR-Cas9 Systems | For functional genomic screens to identify genes essential for CSC self-renewal and survival. | Lentiviral sgRNA libraries, Cas9-expressing cell lines [5]. |
Underlying Mechanisms Driving Marker Heterogeneity
The failure to identify universal CSC markers is not a technical limitation but a reflection of the fundamental biology of cancers. The primary drivers are:
Cellular Plasticity: The concept of a rigid cellular hierarchy is being supplanted by a model of dynamic plasticity, where non-CSCs can dedifferentiate into CSCs and vice versa [72] [73]. This plasticity is influenced by pathways like Wnt/β-catenin, Notch, and Hedgehog, and can be induced by therapies or microenvironmental signals like TGF-β and HGF [72] [2]. Consequently, marker expression is transient and context-dependent.
Influence of the Tumor Microenvironment (TME): The CSC niche—comprising immune cells, fibroblasts, endothelial cells, and extracellular matrix—provides critical signals that maintain CSC stemness and dictate their phenotype [73] [2]. Factors like hypoxia can upregulate markers like CD133, and interaction with niche cells can induce epigenetic reprogramming, further altering marker expression profiles [5] [2].
Clonal Evolution and Genetic Diversity: The stochastic clonal evolution model operates alongside the CSC model [72] [73]. As tumor cells accumulate genetic and epigenetic alterations, new subclones emerge, each with the potential to generate a unique CSC population with its own distinct marker signature, contributing to the overall heterogeneity.
Diagram 2: Key biological drivers contributing to the heterogeneity of CSC marker expression.
The lack of universal CSC markers is an inherent consequence of the complex, dynamic, and heterogeneous nature of cancer. This reality necessitates a shift away from a one-size-fits-all approach to CSC identification. Future research and therapeutic development must account for this plasticity and context-dependence. Promising paths forward include:
- Combinatorial Marker Panels: Developing patient- or cancer-subtype-specific sets of markers for more reliable CSC identification [8] [73].
- Functional Signature-Based Targeting: Focusing on core biological pathways and vulnerabilities (e.g., metabolic dependencies, immune evasion mechanisms) that underpin the CSC state, rather than surface markers alone [5] [2].
- Single-Cell Multi-Omics: Utilizing technologies like single-cell RNA sequencing to deconstruct the full spectrum of cellular states within a tumor and define CSC populations based on integrated functional and molecular signatures, moving beyond a handful of pre-selected markers [5] [37].
Embracing this complexity is essential for advancing our fundamental understanding of tumor biology and for designing the next generation of therapies capable of targeting the root of cancer.
Cancer stem cells (CSCs) represent a subpopulation within tumors that possess the dual capabilities of self-renewal and differentiation, driving tumor initiation, progression, metastasis, and therapeutic resistance [5]. The concept of CSC plasticity has emerged as a fundamental aspect of cancer biology, referring to the dynamic ability of cancer cells to interconvert between stem-like and non-stem-like states, as well as to transition among different phenotypic subsets in response to environmental cues and therapeutic pressures [75]. This phenotypic flexibility represents a major ongoing challenge in oncology, as it contributes significantly to intratumoral heterogeneity, a key driver of therapeutic failure and disease recurrence [76] [75].
The historical understanding of CSCs has evolved substantially from early hierarchical models toward more complex paradigms that incorporate cellular plasticity. The traditional CSC model proposed a rigid hierarchy with CSCs exclusively generating non-CSCs, while the contemporary plasticity model recognizes that non-CSCs can regain stem-like properties through dedifferentiation processes [75] [77]. This dynamic equilibrium between CSC and non-CSC states is maintained by intricate molecular networks and microenvironmental influences, creating a continuously adapting ecosystem within tumors [76] [5]. The recognition of "unlocking phenotypic plasticity" as an emerging hallmark of cancer further underscores its fundamental importance in tumor biology [76].
Molecular Mechanisms Governing CSC Plasticity
Key Signaling Pathways and Transcription Factors
CSC plasticity is regulated by an intricate network of signaling pathways and transcription factors that enable rapid phenotypic adaptations. The epithelial-mesenchymal transition (EMT) program serves as a central regulator, allowing cancer cells to acquire mesenchymal characteristics along with enhanced migratory capacity and stemness properties [76] [78]. This process is governed by transcription factors including SNAIL, TWIST, and ZEB1/2, which suppress epithelial programs while activating mesenchymal and stemness-associated genes [76] [78]. These molecular switches are further modulated by signaling pathways such as TGF-β, WNT, Notch, and Hippo, which integrate extracellular signals to fine-tune cellular phenotypes [78].
Beyond the core EMT program, pluripotency factors including OCT3/4, SOX2, and NANOG play pivotal roles in maintaining and modulating stem-like states [75] [79]. The coordinated expression of these factors establishes regulatory networks that promote cellular plasticity across multiple cancer types. For instance, dual expression of SOX2 and OCT4 has been identified as a key driver for stem cell-mediated tumorigenesis in cholangiocarcinoma, where it correlates significantly with poor patient survival [79]. These core pluripotency factors cooperate to activate stemness maintenance programs while suppressing differentiation signals, thereby preserving phenotypic flexibility.
Metabolic Plasticity in CSCs
CSCs exhibit remarkable metabolic adaptability, allowing them to survive under diverse environmental conditions and resist metabolic stressors induced by therapy [5]. This metabolic plasticity enables CSCs to dynamically switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids depending on nutrient availability and environmental constraints [5]. Research has revealed that EMT-driven CSCs particularly display metabolic flexibility, often relying on distinct energetic pathways compared to their non-stem counterparts [76]. This metabolic reprogramming is not merely a passive response to environmental conditions but an active strategy that supports stemness maintenance and therapeutic resistance.
Table 1: Key Molecular Mechanisms Regulating CSC Plasticity
| Mechanism Category | Key Components | Functional Consequences |
|---|---|---|
| Signaling Pathways | TGF-β, WNT, Notch, Hippo | Integration of microenvironmental signals to fine-tune phenotypic states |
| Transcription Factors | SNAIL, TWIST, ZEB1/2, OCT3/4, SOX2, NANOG | Direct regulation of stemness and differentiation programs |
| Epigenetic Regulators | DNA methyltransferases, histone modifiers | Establishment of reversible phenotypic states without genetic alterations |
| Metabolic Programs | Glycolysis/OXPHOS switching, fatty acid oxidation, glutamine metabolism | Adaptation to nutrient availability and resistance to metabolic stress |
Experimental Models for Studying CSC Plasticity
Tumorsphere Formation Assays
The tumorsphere formation assay represents a fundamental methodology for investigating CSC plasticity in vitro. This approach exploits the ability of CSCs to survive and proliferate under anchorage-independent conditions in serum-free media without exogenous mitogenic stimulation [77]. The protocol involves culturing dissociated cancer cells in low-attachment plates with serum-free media supplemented with basic fibroblast growth factor (bFGF) and epidermal growth factor (EGF), although some cell lines can form tumorspheres without these supplements [77]. After 7-14 days, spheres that form are quantified, with sphere-forming efficiency serving as an indicator of the CSC population. This model has demonstrated remarkable plasticity, as cancer cells grown under routine culture conditions become multidrug-resistant when grown as floating tumorspheres, but quickly re-attach and lose this acquired resistance upon re-incubation in serum-containing media [77].
Live Reporter Systems for Single-Cell Analysis
Advanced reporter systems enable real-time tracking of CSC dynamics at single-cell resolution. The SORE6-dsCopGFP reporter system is particularly valuable, as it responds to the binding of SOX2 and OCT4 transcription factors to regulatory elements from the NANOG promoter [79]. The experimental workflow involves:
- Lentiviral transduction of cancer cell lines with the SORE6-dsCopGFP construct
- Fluorescence-activated cell sorting (FACS) to isolate GFP-positive (SORE6POS) and GFP-negative (SORE6NEG) populations
- Live-cell imaging to track phenotypic transitions over time
- Functional validation through differentiation assays, drug treatment studies, and in vivo tumorigenicity tests [79]
This system has revealed that SORE6POS CCA cells possess self-renewal capacity, can differentiate into SORE6NEG cells, and that chemotherapy induces transitions from SORE6NEG to SORE6POS populations [79]. The reporter approach provides significant advantages over surface marker-based methods by capturing the dynamic nature of stemness states.
Organoid and 3D Culture Models
Organoid technologies offer physiologically relevant platforms for investigating CSC plasticity within complex, tissue-like architectures. The pioneering work of Hans Clevers and colleagues established LGR5 as a marker for intestinal epithelial stem cells and subsequently developed 3D organoid protocols that enable long-term, stable stem cell cultures in vitro [76]. These organoids faithfully recapitulate key aspects of their tissue of origin, providing unprecedented opportunities to study cellular plasticity in near-physiological contexts. Recent advancements include the transition from 3D to 2D organoid cultures using integrin-activating Yersinia protein Invasin, which enables long-term expansion of epithelial cells in a format compatible with improved imaging, functional assays, and high-throughput screening [76].
Table 2: Experimental Models for Investigating CSC Plasticity
| Experimental Model | Key Features | Applications | Limitations |
|---|---|---|---|
| Tumorsphere Assays | Anchorage-independent growth in serum-free conditions; enrichment for CSCs | Assessment of self-renewal capability; drug sensitivity testing | May not fully recapitulate tumor microenvironment complexity |
| Live Reporter Systems | Real-time tracking of CSC states based on pluripotency factor activity | Single-cell dynamics; dedifferentiation studies; drug-induced plasticity | Requires genetic modification; potential artifacts from reporter expression |
| Organoid Cultures | 3D architecture preserving cell-cell and cell-matrix interactions | Modeling tumor heterogeneity; drug screening; personalized medicine | Technically challenging; variable success across cancer types |
| Lineage Tracing | Genetic labeling enabling fate mapping of specific cell populations | Understanding cellular hierarchies; plasticity in vivo | Complex experimental setup; limited to animal models |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying CSC Plasticity
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| CSC Markers | CD44, CD133, ALDH1A1, LGR5, p75NTR | Identification and isolation of CSC subpopulations by FACS or immunohistochemistry |
| Pluripotency Factor Reporters | SORE6-dsCopGFP | Live tracking of CSC states based on SOX2/OCT4 activity |
| Signaling Pathway Modulators | TGF-β inhibitors, WNT agonists/antagonists, Notch inhibitors | Manipulation of pathways regulating CSC plasticity |
| Differentiation Inducers | All-trans retinoic acid (ATRA) | Induction of CSC differentiation to study plasticity mechanisms |
| Metabolic Inhibitors | Drugs targeting glycolysis, OXPHOS, fatty acid oxidation | Investigation of metabolic dependencies and vulnerabilities |
| Cytokines/Growth Factors | EGF, bFGF, FBS | Modulation of microenvironmental cues influencing plasticity |
Therapy-Induced Plasticity and Clinical Implications
Chemotherapy-Induced Phenotypic Transitions
Conventional cancer therapies frequently induce adaptive plasticity in surviving cell populations, leading to the emergence of treatment-resistant clones. Exposure to chemotherapeutic agents can promote dedifferentiation of non-CSCs into CSC-like states, effectively replenishing and often expanding the therapy-resistant compartment [78] [79]. In cholangiocarcinoma, standard chemotherapy not only enriches for existing SORE6POS CSCs but actively induces their emergence from SORE6NEG populations, demonstrating the dynamic nature of therapy-induced plasticity [79]. Similarly, in colorectal cancer, treatment with anticancer drugs stimulates the conversion between LGR5+ and LGR5- cellular states, with each population capable of regenerating the other upon drug withdrawal [75]. This bidirectional interconversion represents a fundamental mechanism of adaptive resistance that complicates therapeutic efficacy.
Metabolic Adaptations Under Therapeutic Pressure
CSCs deploy metabolic plasticity as a strategic defense mechanism against anticancer treatments. Under therapeutic pressure, CSCs can rapidly alter their metabolic configuration to evade drug-induced cytotoxicity, often by shifting toward quiescent states with reduced metabolic activity or by engaging alternative bioenergetic pathways [5] [78]. This metabolic flexibility enables CSCs to survive the metabolic stress imposed by many chemotherapeutic agents, which frequently target rapidly dividing cells with high metabolic demands. The identification of metabolic plasticity as a key feature of EMT-driven CSCs has revealed new therapeutic opportunities for targeting these adaptive mechanisms [76]. Preclinical studies suggest that combining conventional therapies with metabolic inhibitors may prevent these adaptive responses and sensitize CSCs to treatment.
Diagram 1: Therapy-Induced CSC Plasticity and Clinical Consequences. This workflow illustrates how different cancer treatments trigger distinct plasticity responses in CSCs, leading to adverse clinical outcomes.
Emerging Therapeutic Strategies Targeting CSC Plasticity
Differentiation Therapy Approaches
Differentiation therapy represents a promising strategy to counteract CSC plasticity by forcing transition from stem-like to differentiated states, thereby reducing tumorigenic potential. All-trans retinoic acid (ATRA) has demonstrated efficacy in inducing differentiation of CSC populations across multiple cancer types, including cholangiocarcinoma where it significantly reduces the proportion of SORE6POS cells in a dose-dependent manner [79]. This approach essentially leverages the inherent plasticity of CSCs against them, directing their adaptive capacity toward less dangerous phenotypic states. The successful implementation of differentiation therapy could potentially convert aggressive, therapy-resistant tumors into more manageable, treatment-sensitive conditions by eliminating the self-renewing CSC compartment.
Metabolic Intervention Strategies
Targeting the metabolic vulnerabilities of CSCs offers another promising avenue for therapeutic intervention. Dual metabolic inhibition approaches that simultaneously target multiple energetic pathways can circumvent the adaptive capabilities of CSCs by preventing their ability to switch between metabolic states [5]. For instance, combining inhibitors of glycolysis with disruptors of oxidative phosphorylation may effectively eliminate CSC populations by blocking their escape routes under metabolic stress. Additionally, targeting specific metabolic dependencies of EMT-driven CSCs, such as their reliance on lipid metabolism or specific mitochondrial functions, represents an area of active investigation [76]. These strategies aim to exploit metabolic features that are essential for maintaining the plastic nature of CSCs.
Microenvironment-Targeted Interventions
The tumor microenvironment plays a crucial role in regulating CSC plasticity through various signaling molecules, metabolic interactions, and physical cues. Therapeutic strategies that disrupt these supportive niches can indirectly target CSCs by altering the signals that maintain their plastic nature [76] [75]. This includes targeting cytokine-mediated crosstalk between CSCs and non-CSCs that maintains dynamic equilibrium, disrupting metabolic symbiosis with stromal cells, or interfering with hypoxia-induced signaling that promotes stemness [75]. Such approaches may be particularly effective when combined with direct CSC-targeting agents, as they address both the intrinsic plasticity mechanisms and the extrinsic signals that support them.
Diagram 2: Therapeutic Strategies Targeting CSC Plasticity. This diagram illustrates the interconnected approaches for countering CSC plasticity, their molecular targets, and intended therapeutic outcomes.
CSC plasticity represents a fundamental challenge in oncology, contributing significantly to therapeutic resistance, tumor recurrence, and metastatic progression. The dynamic interconversion between stem-like and non-stem-like states, driven by molecular networks, metabolic adaptations, and microenvironmental influences, creates a moving target that evades conventional therapeutic approaches. Future advances in cancer management will require innovative strategies that account for and directly target this plasticity, potentially through differentiation therapy, metabolic interventions, microenvironment disruption, or combination approaches that address multiple aspects of this adaptive phenomenon simultaneously. As our understanding of the mechanisms governing CSC plasticity continues to evolve, so too will our ability to develop more effective therapeutic strategies that can overcome the challenges posed by this dynamic cellular behavior.
Cancer therapy resistance represents a formidable challenge in clinical oncology, leading to treatment failure and disease recurrence. This whitepaper examines the complex molecular and cellular mechanisms that enable cancer cells to survive chemotherapy and radiotherapy. Within the context of cancer stem cell (CSC) research, we explore how these therapy-resistant cells employ diverse strategies including enhanced DNA damage repair, drug efflux, epigenetic adaptation, and interactions with the tumor microenvironment to evade treatment. We synthesize current understanding of CSC markers and identification challenges, providing detailed experimental methodologies and visual frameworks to guide future research directions for overcoming therapeutic resistance.
Therapeutic resistance remains a primary obstacle in oncology, with approximately 90% of chemotherapy failures in metastatic cancer attributed to drug resistance [80]. While radiotherapy is considered standard care for most solid tumors, radiation resistance leads to local treatment failure and cancer recurrence [81]. The cancer stem cell (CSC) paradigm provides a compelling framework for understanding these resistance mechanisms, proposing that a subpopulation of cells with stem-like properties drives tumor initiation, progression, and treatment evasion [5]. CSCs exhibit remarkable plasticity, allowing them to transition between functional states in response to therapeutic pressure and microenvironmental cues [82]. This dynamic adaptability, combined with challenges in reliably identifying universal CSC markers, complicates therapeutic targeting [8]. This review examines the principal mechanisms of therapy resistance, with particular emphasis on CSC-mediated pathways, and provides technical guidance for research approaches aimed at overcoming these challenges.
Core Mechanisms of Therapy Resistance
Enhanced DNA Damage Repair
Radiotherapy and many chemotherapeutic agents exert their cytotoxic effects primarily through DNA damage. Ionizing radiation causes both direct DNA damage and indirect effects through generation of reactive oxygen species that result in single-strand breaks (SSBs), double-strand breaks (DSBs), and base damage [81]. The most deleterious of these lesions are DSBs, which are primarily repaired through two key pathways: non-homologous end joining (NHEJ) and homologous recombination (HR) [81].
Table 1: Key DNA Damage Repair Proteins in Therapy Resistance
| Protein/Complex | Function | Role in Resistance | Cancer Types with Observed Involvement |
|---|---|---|---|
| DNA-PKcs | Critical for NHEJ; phosphorylates itself and downstream targets | Upregulated in resistant cancers; stabilizes SOX2 to maintain stem cell state | Multiple myeloma, Glioblastoma, Nasopharyngeal carcinoma |
| PARP | Recognizes and repairs SSBs; recruits repair proteins | Base excision repair prevents conversion of SSBs to DSBs | Breast, Prostate, Pancreatic (particularly with BRCA1/2 mutations) |
| MRN Complex (Mre11-Rad50-Nbs1) | Recognizes and initiates DSB repair pathway | Overexpression increases radioresistance | Rectal cancer |
| ATM/ATR | Core kinases in DNA damage response (DDR) | Activate downstream signaling for repair | Various solid tumors |
| γH2AX | Early marker of DSBs | Correlates with number of radiation-induced DSBs | Various cancers |
Cancer cells, particularly CSCs, develop resistance by enhancing these DNA repair mechanisms. Key sensors including ATRIP, Rad24p, γH2AX, and NBS1 recognize damage signals and recruit DDR core kinases such as ATM, ATR, and DNA-dependent protein kinase (DNA-PK) to break sites [81]. DNA-PKcs play a particularly crucial role in classical NHEJ repair. Studies demonstrate that cells lacking DNA-PKcs exhibit higher radiosensitivity, while upregulation of DNA-PKcs correlates with radioresistance in multiple myeloma [81]. In glioblastoma, DNA-PK stabilizes SOX2 through phosphorylation, promoting treatment resistance by maintaining glioma stem-like cells (GSCs) in a stem cell state [81].
The clinical relevance of targeting DNA repair pathways is evidenced by the development of inhibitors against key players like DNA-PKcs and PARP. The oral DNA-PKcs inhibitor M3814 induced significant sensitization to radiotherapy in preclinical models, while AZD7648 improved anti-tumor activity in combination with radiotherapy across various cancer models [81]. PARP inhibitors exploit the "synthetic lethal" effect in BRCA1/2 mutant cells, with clinical trials in triple-negative breast cancer demonstrating improved radiotherapy efficacy when combined with PARP inhibitors like olaparib and niraparib [81].
Drug Efflux and Metabolic Adaptation
The overexpression of ATP-binding cassette (ABC) transporter proteins represents a major mechanism of multi-drug resistance (MDR) in cancer cells, particularly CSCs [80] [9]. These transporters utilize ATP hydrolysis to actively efflux chemotherapeutic agents from cells, reducing intracellular drug accumulation to sublethal concentrations [80].
Table 2: Major ABC Transporters in Cancer Drug Resistance
| Transporter | Other Names | Substrate Drugs | Role in CSCs |
|---|---|---|---|
| P-glycoprotein | P-gp, ABCB1 | Doxorubicin, Vinblastine, Taxol | Highly expressed; maintains stemness |
| MRP1 | ABCC1 | Anthracyclines, Taxanes | Extrudes drugs in various solid tumors |
| BCRP | ABCG2 | Mitoxantrone, Topotecan | Originally identified in mitoxantrone-resistant cells; CSC marker |
The MDR mechanism involves both reduced drug absorption and increased drug efflux. Mutations in specific transporters, such as the human folate carrier (hRFC) gene mutation in acute lymphoblastic leukemia, can reduce drug binding affinity and cellular uptake [80]. Simultaneously, ABC transporters function as efflux pumps: P-glycoprotein binds to chemotherapeutic agents, and following ATP hydrolysis, undergoes structural changes that release drugs into extracellular space [80].
CSCs additionally exhibit remarkable metabolic plasticity that contributes to therapy resistance. They can switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, enabling survival under diverse environmental conditions including hypoxia [5]. This metabolic flexibility is further enhanced through interactions with stromal cells, immune components, and vascular endothelial cells that facilitate metabolic symbiosis [5].
Epigenetic Plasticity and CSC State Transition
The dynamic and plastic nature of CSCs enables them to transition between functional states in response to therapeutic pressure. Rather than representing a fixed subpopulation, CSCs are now recognized as a fluid functional state that tumor cells can enter or exit, driven by intrinsic programs, epigenetic reprogramming, and microenvironmental cues [82]. This plasticity complicates identification due to inconsistent marker expression and enables resistance, dormancy, and metastasis.
Epigenetic modifications, including DNA methylation, histone modifications, and miRNA expression, play crucial roles in maintaining CSC stemness under therapeutic stress [83]. Studies have demonstrated the importance of epigenetic modifications in drug-tolerant persister (DTP) cells and their role in increased tolerance to higher drug pressure [83]. Additionally, altering epigenetic landscapes through DNA methylation and histone modifications aids in the maintenance and survival of CSCs which exhibit resistance features [83].
This plasticity is evident in studies of oral squamous cell carcinoma (OSCC), where multiple stem cell subpopulations with distinct phenotypes co-exist within tumors, each impacting different clinical parameters [8]. The cell subpopulations identified by different CSC markers were found to be dynamic populations, able to switch between phenotypes over time [8]. This phenotypic diversity raises significant challenges for using CSC markers as predictive biomarkers and therapeutic targets.
Diagram 1: CSC plasticity in therapy resistance. The diagram illustrates how therapeutic pressure induces epigenetic changes that drive transitions between different CSC functional states, ultimately leading to therapy resistance. Key epigenetic mechanisms include DNA methylation, histone modifications, and miRNA expression, while CSC states include quiescent, activated, and epithelial-mesenchymal transition (EMT) states.
Tumor Microenvironment and CSC Niche Interactions
The tumor microenvironment (TME) plays a crucial role in mediating therapy resistance through multiple mechanisms. The TME comprises various components including stromal cells, immune cells, extracellular matrix (ECM), and soluble factors that collectively create protective niches for CSCs [80] [84]. Environment-mediated drug resistance (EM-DR) encompasses both cell adhesion-mediated drug resistance (CAM-DR) and soluble factor-mediated drug resistance (SM-DR) [80].
Key soluble factors in the TME that promote resistance include vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), stromal cell-derived factor-1 (SDF-1), interleukin-6 (IL-6), and various colony-stimulating factors [80]. These factors provide additional signals for tumor cell growth and survival despite therapeutic intervention. The acidic extracellular pH (approximately 6.8) in tumor tissues favors metalloproteinases, activates several signaling pathways, and serves as a barrier for many anticancer drugs, further accentuating cancer cell malignancy and aggressiveness [85].
CSCs actively modify their surrounding stroma by secreting proteins and molecular components such as ECM proteins, which helps maintain CSCs in a dormant state to regulate their fate, plasticity, and resistance against conventional therapies [85]. This bidirectional communication between CSCs and their microenvironment creates a symbiotic relationship that enhances therapeutic resistance through multiple pathways, including hypoxia-mediated stemness preservation, immune evasion, and enhanced DNA repair capacity.
Experimental Approaches for Studying Therapy Resistance
CSC Identification and Isolation Methods
The identification and isolation of CSCs remain challenging due to the lack of universal markers and the dynamic nature of stem cell states [5] [8]. Current approaches primarily rely on a combination of surface markers, functional assays, and multi-omics integration.
Table 3: Common CSC Markers and Technical Approaches
| Marker/Technique | Technical Application | Experimental Considerations | Associated Cancers |
|---|---|---|---|
| CD44 | Flow cytometry, Immunohistochemistry | Often used with other markers; not CSC-specific | Breast, Prostate, OSCC |
| CD133 | Flow cytometry, Cell sorting | Expression varies with tumor progression | Glioblastoma, Colon |
| ALDH1 Activity | ALDEFLUOR assay | Functional marker; detects enzyme activity | Breast, Colon, OSCC |
| p75NTR | Immunohistochemistry, FACS | Correlates with proliferation in OSCC | OSCC, Melanoma, Esophageal |
| Side Population | Hoechst 33342 efflux | Functional assay for ABC transporters | Various |
| Sphere Formation | Ultra-low attachment cultures | Functional assay for self-renewal | Various |
Multiple immunohistochemical staining techniques enable simultaneous investigation of several putative CSC markers. A study on oral squamous cell carcinoma employed triple immunohistochemistry to examine the overlap of p75NTR and ALDH1A1-positive cell subpopulations, revealing that co-localization of these two markers was rare in OSCC compared to normal oral mucosa or oral dysplasia [8]. Cells positive for p75NTR exhibited higher expression of proliferative and self-renewal markers (BMI1 and Ki-67) compared to ALDH1A1+ or double-positive cells [8].
Technical protocols for CSC isolation typically involve:
- Tissue dissociation into single-cell suspensions using enzymatic digestion (collagenase/hyaluronidase)
- Antibody staining for surface markers (30-45 minutes, 4°C)
- Flow cytometry-based cell sorting (FACS) or magnetic bead separation
- Functional validation through sphere formation assays and in vivo limiting dilution transplantation
Recent advances incorporate single-cell RNA sequencing, spatial transcriptomics, and multi-omics integration to better understand CSC heterogeneity and metabolic adaptability beyond surface marker expression [5].
DNA Damage Repair Assay Protocols
Assessment of DNA damage repair capacity provides critical insights into radiotherapy resistance mechanisms. Standardized protocols include:
Immunofluorescence Staining for γH2AX Foci:
- Cell culture on chamber slides with appropriate treatments
- Fixation with 4% paraformaldehyde (15 minutes, room temperature)
- Permeabilization with 0.5% Triton X-100 (10 minutes)
- Blocking with 5% BSA in PBS (1 hour)
- Primary antibody incubation (anti-γH2AX, 1:1000, overnight at 4°C)
- Secondary antibody with fluorescent conjugate (1 hour, protected from light)
- DAPI counterstaining and mounting
- Microscopy analysis with foci counting (minimum 50 cells per condition)
The number of γH2AX foci correlates with radiation-induced DSBs, making this a sensitive marker for genotoxic stress and repair capacity [81].
Colony Formation Assay for Radiosensitivity:
- Seed appropriate cell numbers in triplicate (typically 100-10,000 cells depending on expected survival)
- Allow cell attachment (6-8 hours)
- Irradiate with graded doses (0-10 Gy) using clinical irradiator
- Incubate for 10-14 days to allow colony formation (>50 cells)
- Fix with methanol/acetic acid (3:1) and stain with crystal violet
- Count colonies and calculate surviving fractions
- Plot survival curves and calculate parameters (D0, D10, SF2)
This gold-standard assay provides quantitative data on cellular radiosensitivity and can be modified with DNA repair inhibitors to assess their potential as radiosensitizers [81].
Diagram 2: Experimental workflow for CSC isolation and characterization. The diagram outlines key technical steps from sample preparation through functional validation and advanced multi-omics analysis, highlighting the comprehensive approach required to study therapy-resistant CSC populations.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Studying Therapy Resistance
| Reagent/Category | Specific Examples | Experimental Function | Technical Notes |
|---|---|---|---|
| CSC Surface Markers | Anti-CD44, Anti-CD133, Anti-ICAM1/CD54 | Identification and isolation of CSC populations | Antibody validation critical; combination markers improve specificity |
| DNA Damage Detection | Anti-γH2AX, Anti-53BP1, Anti-RAD51 | Immunofluorescence staining for DNA repair foci | Foci counting automated with image analysis software |
| ABC Transporter Assays | Hoechst 33342, Verapamil, Ko143 | Side population analysis; transporter inhibition | Controls with inhibitors essential for specificity |
| Epigenetic Modulators | 5-Azacytidine, Trichostatin A, JQ1 | Investigate plasticity and epigenetic regulation | Dose optimization required to avoid pleiotropic effects |
| Signal Pathway Inhibitors | PARP inhibitors (Olaparib), DNA-PK inhibitors (AZD7648) | Target specific resistance mechanisms | Combination with chemo/radiotherapy requires timing optimization |
| Viability Assays CCK-8, MTT, Resazurin | Assess cell proliferation and drug sensitivity | 3D culture models may provide more physiological relevance | |
| Sphere Formation Media | DMEM/F12 with B27, EGF, FGF | Assess self-renewal capability in ultra-low attachment plates | Primary cells may require optimized growth factor combinations |
Emerging Therapeutic Strategies and Research Directions
Novel approaches to overcome therapy resistance focus on targeting CSC-specific vulnerabilities and disrupting resistance mechanisms. Promising strategies include:
Dual Metabolic Inhibition: Targeting the metabolic plasticity of CSCs through combined inhibition of glycolysis, oxidative phosphorylation, and alternative fuel pathways [5]. This approach recognizes that CSCs can switch between different energy sources, making single-pathway inhibition insufficient.
Nanoparticle-Mediated Therapies: Nanocarriers (typically 20-200 nm) leverage the enhanced permeability and retention (EPR) effect to accumulate in tumors, bypass efflux pumps through endocytosis, and enable targeted delivery of therapeutic agents to CSCs [85]. Co-delivery of anticancer drugs with multiple drug resistance modulators and CSC-targeting ligands using nanocarriers shows promise for overcoming drug resistance [85].
Immunotherapy Approaches: Despite CSCs being inherently immunoevasive, emerging strategies including CAR-T cells targeting CSC markers such as EpCAM have shown preclinical success [5] [9]. The challenge remains in identifying targets that distinguish CSCs from normal stem cells.
Epigenetic Therapeutics: Modulators targeting the epigenetic machinery that maintains CSC stemness and plasticity represent another promising avenue. These approaches aim to lock CSCs in therapy-sensitive states or prevent adaptation to treatment pressure [82] [83].
The integration of advanced technologies including 3D organoid models, CRISPR-based functional screens, and AI-driven multiomics analysis is paving the way for precision-targeted CSC therapies [5]. Moving forward, an integrative approach combining metabolic reprogramming, immunomodulation, and targeted inhibition of CSC vulnerabilities will be essential for developing effective CSC-directed therapies that address the challenge of therapy resistance.
The mechanisms underlying therapy resistance in cancer represent a complex, multi-faceted challenge centered around the dynamic biology of cancer stem cells. Through enhanced DNA damage repair, drug efflux capabilities, metabolic plasticity, epigenetic adaptation, and sophisticated interactions with the tumor microenvironment, CSCs evade conventional chemo- and radiotherapy. The inherent heterogeneity and functional plasticity of CSCs, coupled with challenges in their reliable identification, complicate therapeutic targeting. Future research directions must integrate advanced technologies including single-cell multi-omics, functional genomics, and nanotherapeutic approaches to develop effective strategies that overcome therapy resistance. The scientific toolkit and methodologies outlined in this review provide a framework for advancing our understanding and intervention against these resilient cellular populations that drive cancer recurrence and treatment failure.
The Impact of Senescence and the SASP on CSC Dynamics and Tumor Relapse
Cellular senescence (CS) and cancer stem cells (CSCs) represent two pivotal paradigms in oncology, each playing complex, context-dependent roles in tumor progression and therapy resistance. Senescence is a state of irreversible cell cycle arrest that can be triggered by various stressors, including telomere attrition, DNA damage, oncogene activation (oncogene-induced senescence, OIS), and anticancer therapies (therapy-induced senescence, TIS) [86] [87] [88]. Senescent cells are characterized by a distinctive secretome known as the senescence-associated secretory phenotype (SASP), which comprises a complex mixture of cytokines, chemokines, growth factors, and proteases that profoundly reshape the tumor microenvironment (TME) [86] [88]. CSCs, conversely, constitute a subpopulation of tumor cells with self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies, driving tumor initiation, progression, metastasis, and relapse [5] [20].
The interplay between CS/SASP and CSCs creates a dynamic axis that significantly influences tumor fate. Initially perceived as a tumor-suppressive mechanism, senescence can arrest the proliferation of damaged cells and, through an acute SASP, promote immune-mediated clearance of premalignant cells [87]. However, persistent senescent cells and a chronic SASP can foster a pro-tumorigenic niche that promotes CSC survival, plasticity, and expansion, ultimately leading to therapy resistance and tumor recurrence [89] [88]. This whitepaper delves into the mechanistic underpinnings of this interplay, framing it within the broader challenges of CSC marker identification and targeting. It provides a technical guide for researchers and drug development professionals, complete with structured data, experimental protocols, and visualization tools to advance this critical field.
The Dual Nature of Senescence and SASP in Cancer
The impact of cellular senescence on tumorigenesis is fundamentally paradoxical, acting as both a barrier to and a promoter of cancer progression.
Tumor-Suppressive Roles
Senescence serves as a crucial innate defense mechanism against cancer by halting the proliferation of cells at risk of malignant transformation. Oncogene-induced senescence (OIS) acts as an initial barrier to cancer development, preventing the progression of benign lesions into malignant tumors. A classic example is melanocytic nevi, where OIS driven by oncogenes like BRAF(V600E) prevents progression to melanoma [87]. The tumor-suppressive function of OIS involves key pathways, including the p53/p21CIP1 and p16INK4a/RB axes, which enforce cell cycle arrest [87] [88]. Furthermore, an acute or short-term SASP can stimulate antitumor immunity. Secreted factors like IL-6, IL-8, and CCL5 can recruit and activate immune cells such as CD8+ T cells, CD4+ Th1 cells, and NK cells, leading to the clearance of senescent tumor cells [87]. In rectal cancer, for instance, post-therapy SASP factors were correlated with increased CD8+ T-cell infiltration and improved tumor regression [87].
Tumor-Promotive Roles
Despite its protective role, when senescent cells persist, they can undergo a phenotypic switch that drives malignancy. A chronic SASP creates a pro-inflammatory and immunosuppressive TME that fosters cancer progression, therapy resistance, and metastasis [86] [88]. Key SASP components such as IL-6, IL-8, VEGF, and various MMPs stimulate angiogenesis, epithelial-mesenchymal transition (EMT), and immune evasion [86]. The SASP is highly heterogeneous and dynamic, varying with the cell type, inducing stressor, and time [89] [88]. Therapy-induced senescent (TISnt) cells, in particular, can accumulate post-treatment and drive therapy resistance through mechanisms involving the SASP, metabolic dysregulation, and immune evasion [89]. In head and neck squamous cell carcinoma (HNSCC), for example, radiation-induced SASP drives therapy resistance through NFκB-dependent signaling [89].
Table 1: Key Components of the Senescence-Associated Secretory Phenotype (SASP)
| SASP Category | Key Components | Primary Functions in Cancer |
|---|---|---|
| Cytokines | IL-6, IL-8 (CXCL8), TNF-α, IL-1β | Promote inflammation, cancer cell survival, EMT, and immune cell recruitment. |
| Chemokines | CCL2 (MCP-1), CCL5 (RANTES), CCL20, CXCL1, CXCL12 | Recruit immune cells (neutrophils, monocytes, T cells) to the TME. |
| Growth Factors | VEGF, FGF, HGF, TGF-β, Amphiregulin, GDF15 | Stimulate angiogenesis, tumor cell proliferation, and stromal activation. |
| Proteases | MMP2, MMP9, MMP3, UPA | Remodel extracellular matrix (ECM) to facilitate invasion and metastasis. |
| Other Factors | TIMP2, PAI-1, IGFBPs | Regulate protease activity, ECM remodeling, and cell growth. |
Senescence and SASP as Modulators of Cancer Stem Cell Dynamics
The TME remodeled by senescent cells and the SASP directly influences CSC populations, affecting their maintenance, expansion, and functional properties.
Impact on CSC Plasticity and Niche Maintenance
The SASP can induce dedifferentiation of non-CSC cancer cells into a stem-like state. Factors such as IL-6 and IL-8 have been implicated in activating pathways like Wnt/β-catenin, Notch, and Hedgehog, which are critical for maintaining CSC stemness [86] [5]. Furthermore, the SASP contributes to the formation and maintenance of the CSC niche. For instance, SASP from therapy-induced senescent stromal cells can create a supportive microenvironment that enhances CSC self-renewal and protects them from therapy [89]. Senescent cancer-associated fibroblasts (CAFs) have been shown to promote stemness in adjacent cancer cells through paracrine signaling [88].
Therapy-Induced Senescence and CSC Fate
The relationship between TIS and CSCs is complex and critical for understanding relapse. While CSCs were historically considered resistant to senescence due to their dormancy and robust DNA repair mechanisms, emerging evidence indicates they can undergo TIS under specific conditions [89]. For example, Bone Morphogenetic Protein 7 (BMP7) secreted by stromal cells can trigger senescence in prostate CSCs, characterized by increased SA-β-Gal activity and p21 expression [89]. Similarly, a subpopulation of ALDHhigh breast CSCs can maintain a SASP-induced phenotype [89]. The clinical consequence of this is profound. The persistence of TISnt cells post-therapy can lead to a chronic SASP that promotes the re-emergence and expansion of CSCs that survived treatment, ultimately driving tumor relapse [89]. This establishes a dangerous cycle where therapy intended to kill cancer cells instead creates a senescent, pro-inflammatory environment that fuels the regeneration of the tumor from its therapy-resistant stem cells.
Technical and Methodological Approaches
Experimental Models for Studying the Senescence-CSC Axis
In Vitro Models:
- Senescence Induction: Primary cells or cancer cell lines can be induced into senescence using genotoxic chemotherapeutics (e.g., cisplatin, doxorubicin), radiation (2-10 Gy IR), or targeted agents (e.g., CDK4/6 inhibitors) [89] [88]. Doses should be calibrated to cause significant DNA damage without inducing widespread apoptosis.
- CSC Co-culture: Senescent cells (e.g., fibroblasts, cancer cells) are co-cultured with enriched CSCs in Transwell systems or direct contact cultures to study paracrine and juxtacrine effects on CSC phenotypes [89].
- CSC Functional Assays: The impact of senescent cell-conditioned media or direct co-culture on CSCs is assessed using sphere-forming assays (e.g., tumorspheres), colony formation assays, and invasion assays [90].
In Vivo Models:
- Xenograft Models: Immunocompromised mice (e.g., NSG) are injected with CSCs alone or co-injected with senescent stromal cells. Tumor growth, metastasis, and relapse are monitored post-treatment with senolytic agents (e.g., Dasatinib + Quercetin) to elucidate the role of senescent cells in supporting CSCs in vivo [89].
- Genetically Engineered Mouse Models (GEMMs): These models allow for the inducible senescence and lineage tracing of CSCs within an intact immune system and native TME, providing the most physiologically relevant insights [87].
Key Analytical Techniques and Reagents
A multi-parameter approach is essential for accurately identifying and characterizing senescent cells and CSCs, given the lack of a single universal marker for either population.
Table 2: Research Reagent Solutions for Studying Senescence and CSCs
| Reagent / Assay | Specific Example(s) | Function and Application |
|---|---|---|
| SA-β-Gal Kit | Senescence β-Galactosidase Staining Kit | Detects lysosomal β-galactosidase activity at pH 6.0, a hallmark of senescence. |
| Antibodies for IHC/IF | Anti-p16INK4a, Anti-p21CIP1, Anti-γH2AX | Detect key senescence and DNA damage markers in tissue sections (FFPE) or cells. |
| Flow Cytometry Antibodies | Anti-CD44, Anti-CD133, Anti-ALDH1A1, Anti-p75NTR | Identify and isolate CSC subpopulations from bulk tumors or cell lines. |
| ELISA / Multiplex Assays | IL-6, IL-8, CCL2, VEGF ELISA Kits | Quantify specific SASP factors in cell culture supernatants or patient sera. |
| qRT-PCR Panels | SASP Factor PCR Array, CSC Marker PCR Array | Profile the expression of a comprehensive set of SASP-related genes and CSC markers. |
Diagram 1: SASP-Mediated Impact on CSC Phenotypes. This workflow illustrates how various senescence triggers lead to the secretion of specific SASP factors, which in turn promote distinct, pro-tumorigenic outcomes in Cancer Stem Cells.
Data Integration and Computational Analysis
Modern research into the senescence-CSC axis relies heavily on computational biology to integrate complex, multi-modal datasets.
Pan-Cancer Analysis of Senescence Heterogeneity
A recent comprehensive pan-cancer analysis of 33 cancer types identified five distinct molecular subgroups of cellular senescence based on the expression of 525 CS-related genes. These subgroups, named Inflamm-aging, DNA Damage Response, Autophagy, Immunologically Quiet, and Metabolic Disorder, exhibit cancer-type-specific distributions and are significantly associated with patient prognosis, immunophenotypic features, and therapy response [91]. This classification provides a refined framework beyond a simple "senescence score" for understanding how different senescence states might uniquely influence CSC dynamics across cancer types.
Single-Cell and Multi-Omics Integration
Single-cell RNA sequencing (scRNA-seq) is pivotal for deconvoluting the heterogeneity of both senescent and CSC populations within tumors. It allows for the simultaneous identification of senescent cells (by expression of p16, p21, SASP factors), CSC subsets (by expression of CD44, CD133, ALDH1A1), and their intermingled states in the same tumor [91] [5]. Coupling scRNA-seq with CRISPR-based functional screens can identify genes essential for survival in specific senescence or CSC states, revealing novel therapeutic vulnerabilities [5]. Furthermore, AI-driven multi-omics analysis is being used to integrate genomic, transcriptomic, epigenomic, and proteomic data to build predictive models of how senescence influences CSC-mediated tumor relapse [5].
Table 3: Pan-Cancer Senescence Subgroups and Their Features
| Senescence Subgroup | Key Biological Features | Association with Prognosis | Potential CSC Interaction |
|---|---|---|---|
| Inflamm-aging | Dominated by SASP factors (cytokines, chemokines); high immune infiltration. | Varies by cancer type; often poor. | High potential for paracrine activation of CSCs via inflammatory signals. |
| DNA Damage Response (DDR) | Enriched for DNA repair pathways; genomic instability. | Often associated with therapy response. | May represent a source of genomic diversity for CSCs. |
| Autophagy | Upregulation of autophagy-related genes; metabolic adaptation. | Context-dependent. | Could promote CSC survival under metabolic stress. |
| Immunologically Quiet | Low immune cell recruitment and SASP; immune-evasive. | May facilitate immune escape. | Could provide a "sanctuary" niche for CSCs. |
| Metabolic Disorder | Alterations in oxidative phosphorylation, glycolysis, etc. | Often poor. | May create a metabolically supportive niche for CSCs. |
Therapeutic Implications and Emerging Strategies
Targeting the senescence-CSC axis offers promising avenues for preventing tumor relapse. Two main strategic approaches have emerged: eliminating senescent cells or modulating their secretome.
Senolytics and Senomorphics
Senolytics are a class of drugs that selectively induce apoptosis in senescent cells. Examples include Dasatinib and Quercetin (D+Q). By clearing TISnt cells after conventional therapy, senolytics can prevent the establishment of a pro-tumorigenic SASP, thereby reducing CSC expansion and delaying relapse [87] [89]. This forms the basis of the "one-two punch" sequential therapy: initial cancer treatment (e.g., chemotherapy) to induce senescence and tumor regression, followed by a senolytic agent to eliminate the residual senescent cells [89]. Senomorphics, in contrast, do not kill senescent cells but inhibit the SASP. Drugs that target the NF-κB or mTOR pathways can suppress the production of key SASP factors, mitigating their tumor-promoting effects on CSCs without removing the senescent cells themselves [86] [88].
Immunotherapy and Precision Targeting
Given that a short-term SASP can promote immune clearance, strategies are being developed to harness this effect. This includes combining pro-senescence therapy with immune checkpoint inhibitors (e.g., anti-PD-1/PD-L1) to enhance the immune-mediated elimination of both senescent cells and CSCs [87] [88]. For direct CSC targeting, therapies are being developed against CSC-specific surface markers (e.g., CD44, CD133). Chimeric Antigen Receptor T-cell (CAR-T) therapy targeting EpCAM has shown preclinical efficacy in eliminating prostate CSCs [5]. The future lies in combinatorial strategies that integrate senolytics/senomorphics, CSC-targeted agents, and immunotherapy to simultaneously attack multiple pillars of tumor relapse.
Diagram 2: Therapeutic Strategy to Disrupt the Senescence-CSC Axis. This diagram outlines the logical sequence from initial therapy-induced senescence to the application of targeted strategies designed to block its pro-tumorigenic effects on CSCs.
The intricate interplay between cellular senescence, the SASP, and cancer stem cells represents a critical determinant of tumor fate, particularly in the context of therapeutic response and relapse. The dual nature of senescence necessitates a nuanced understanding of its context, timing, and heterogeneity. The persistent accumulation of therapy-induced senescent cells and their associated SASP can create a permissive niche that enhances CSC plasticity, survival, and self-renewal, ultimately driving tumor recurrence. Overcoming the challenges of CSC marker identification and targeting requires an integrated approach, leveraging advanced experimental models, single-cell multi-omics technologies, and sophisticated computational analyses. The promising therapeutic strategies of senolytics, senomorphics, and their rational combination with CSC-targeted agents and immunotherapy herald a new frontier in precision oncology. By dismantling the supportive network that sustains CSCs, these innovative approaches hold the potential to break the cycle of therapy resistance and relapse, ultimately improving long-term outcomes for cancer patients.
The core challenge in modern oncology is the reliable identification and targeting of Cancer Stem Cells (CSCs), a highly plastic and therapy-resistant cell subpopulation that drives tumor initiation, progression, metastasis, and relapse [5]. The CSC model posits that tumors are organized hierarchically, with a small population of CSCs at the apex possessing the capacity for self-renewal and differentiation into the heterogeneous bulk of the tumor [92]. This model provides a compelling explanation for therapeutic resistance and cancer recurrence; however, its experimental validation hinges on robust functional assays that themselves present significant limitations.
The field is currently constrained by two parallel methodological challenges: the biological and technical limitations of xenotransplantation assays (the historical "gold standard" for identifying CSCs) and the incomplete mimicry of the tumor microenvironment (TME) by emerging in vitro models [92] [93]. This whitepaper provides a technical guide for researchers and drug development professionals, framing these assay limitations within the broader context of CSC marker discovery. It details current constraints, summarizes optimized experimental protocols, and presents innovative strategies to enhance the reliability and predictive power of CSC research.
Limitations of the Gold Standard: The Xenotransplantation Assay
The xenotransplantation assay, which involves transplanting human tumor cells into immunocompromised mice, remains the definitive functional test for a CSC's tumor-initiating capacity [92]. Despite its status, this method is fraught with technical and biological variables that can drastically alter experimental outcomes and confound the identification of genuine CSC markers.
Key Technical and Biological Constraints
The functional read-out of CSC frequency and potency is highly sensitive to specific experimental parameters, leading to considerable inter-laboratory variability [92]. The table below summarizes the major limitations of this assay system.
Table 1: Key Limitations of Xenotransplantation Assays in CSC Research
| Limitation Category | Specific Challenge | Impact on CSC Identification |
|---|---|---|
| Recipient Immunology | Varying degrees of immunodeficiencies in mouse models (e.g., NOD/SCID vs. NSG mice) [92]. | Alters engraftment efficiency and may fail to identify CSCs dependent on human-specific immune interactions [8]. |
| Niche Incompatibility | Lack of species-specific paracrine signaling; murine niche factors may not be functionally homologous to human counterparts [92]. | May fail to support the growth of human CSCs that depend on specific stromal signals, leading to an underestimation of the CSC pool [92]. |
| Assay Procedure | Variability in tumor cell dissociation protocols, injection sites (orthotopic vs. heterotopic), and use of supportive matrices like Matrigel [92]. | Influences cell viability, fitness, and the instructive signals received, biasing the functional read-out of stemness. |
| CSC Plasticity | The non-CSC population can acquire stemness properties upon depletion of the original CSCs or in response to niche signals [5] [92]. | Challenges the concept of a fixed, marker-defined hierarchy and suggests stemness can be a transient, functional state. |
Optimized Protocol for Xenotransplantation Assay
To enhance the reproducibility and relevance of xenotransplantation data, the following optimized protocol is recommended.
Protocol: Functional Validation of Putative CSCs via Orthotopic Xenotransplantation
Cell Preparation and Sorting:
- Obtain a single-cell suspension from patient-derived xenografts (PDX) or fresh patient tumor samples using a gentle enzymatic dissociation kit to maximize viability.
- Sort the cell population into marker-positive and marker-negative fractions using Fluorescence-Activated Cell Sorting (FACS). Include a "bulk" unsorted population as a control. Use antibodies against putative CSC markers (e.g., CD44, CD133) and viability dyes [8] [9].
Recipient Preparation:
- Utilize highly immunocompromised NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice, aged 6-8 weeks.
- For orthotopic models, perform a minimal surgical procedure to expose the target organ. For co-transplantation studies, prepare a suspension of relevant human stromal cells, such as cancer-associated fibroblasts (CAFs), mixed with the tumor cells in a 1:1 ratio in a buffer containing 50% Matrigel to provide structural and signaling support [92].
Cell Transplantation:
- Perform serial dilutions of the sorted cells (e.g., 10, 100, 1000, 10,000 cells) to determine the frequency of tumor-initiating cells.
- Inject the cell suspension orthotopically into the corresponding organ of origin (e.g., intra-mammary fat pad for breast cancer) to preserve tissue-specific niche signals. A total volume of 20-30 µL is typically used.
Post-Operative Monitoring and Analysis:
- Monitor tumor formation weekly using bioluminescent imaging (if luciferase-tagged cells are used) or caliper measurements.
- The experiment endpoint is typically when tumors in any group reach 1.5 cm in diameter.
- Analyze the resulting tumors by flow cytometry and immunohistochemistry to assess whether they recapitulate the heterogeneity of the original tumor and the presence of the original marker profile.
Experimental xenotransplantation workflow for validating CSCs.
Advancing In Vitro Models: From 2D to Complex Microenvironments
While in vitro models avoid the complexities of cross-species interactions, they have historically struggled to replicate the intricate TME that sustains CSCs. Recent innovations in 3D culture systems are closing this gap, offering more physiologically relevant contexts for studying CSC biology.
Limitations of Traditional In Vitro Systems
Traditional 2D cultures fail to recapitulate critical aspects of the CSC niche, including:
- Three-dimensional architecture: The lack of 3D cell-cell and cell-matrix interactions alters signaling and drug penetration [94].
- Metabolic gradients: They cannot model the hypoxia and nutrient deprivation found in solid tumors, which are key drivers of CSC plasticity and therapy resistance [5] [93].
- Cellular complexity: The absence of immune cells, fibroblasts, and vascular endothelial cells removes critical paracrine and juxtacrine signals that regulate CSC self-renewal and quiescence [5] [92].
Protocol: Establishing a Complex In Vitro CSC Organoid Co-Culture
This protocol outlines the generation of a patient-derived cancer organoid model co-cultured with stromal cells to better mimic the TME.
Key Research Reagent Solutions for Organoid Co-Culture
Table 2: Essential Reagents for Complex In Vitro CSC Modeling
| Reagent / Material | Function | Example |
|---|---|---|
| Basement Membrane Matrix | Provides a 3D scaffold that mimics the extracellular matrix, supporting polarized organoid growth and signaling. | Corning Matrigel, GFR [92]. |
| Advanced Organoid Medium | A defined, serum-free medium formulation tailored to the tumor type, containing essential growth factors and niche signals (e.g., WNT, R-spondin, Noggin). | STEMCELL Technologies IntestiCult or custom formulations [92]. |
| Patient-Derived Tumor Cells | The primary cellular material that retains the genetic and phenotypic heterogeneity of the original tumor. | Digested tumor tissue from surgical resections or biopsies. |
| Human Stromal Cells | Provides essential niche signals; can include mesenchymal stem cells, cancer-associated fibroblasts (CAFs), or endothelial cells. | Commercially available primary CAFs or isolated from tissue. |
| Cytokines for Exhaustion | Used to induce a dysfunctional state in immune cells, mimicking the TME. | Recombinant Human TGF-β1, IL-10 [93]. |
Initial Organoid Establishment:
- Embed digest patient tumor tissue in 100% Matrigel domes (30 µL per dome) in a pre-warmed 24-well plate. Polymerize the domes for 30 minutes at 37°C.
- Overlay each dome with 500 µL of advanced organoid medium, supplemented with a tailored cocktail of growth factors (e.g., 50 ng/mL EGF, 100 ng/mL Noggin, 500 ng/mL R-spondin-1 for colorectal cancers). Culture at 37°C with 5% CO₂.
- Passage organoids every 7-14 days by mechanically breaking them up and re-embedding in fresh Matrigel.
Stromal Co-Culture Integration:
- One day after passaging the organoids, trypsinize and count the required stromal cells (e.g., CAFs).
- Resuspend the stromal cells in the organoid medium at a density of 1x10⁵ cells/mL.
- Carefully remove the existing medium from the organoid cultures and replace it with the new medium containing the stromal cells. The stromal cells will attach to the plate and surround the Matrigel dome, establishing paracrine communication.
In Vitro Exhaustion Modeling:
- To model T-cell exhaustion within the TME, isolate Vγ9Vδ2 T cells from human peripheral blood using a Ficoll gradient and subsequent negative selection kit.
- Culture the expanded T cells with the established organoid co-culture system. To induce exhaustion, add sustained, low-dose stimulation (e.g., 1 µM Zoledronate) along with immunosuppressive cytokines (5 ng/mL TGF-β and 20 ng/mL IL-10) to the culture medium for 10-14 days [93].
Functional Read-outs:
- Drug Screening: Treat organoids with serial dilutions of chemotherapeutics or targeted agents for 72-96 hours. Assess viability using a CellTiter-Glo 3D assay.
- Self-Renewal Potential: Dissociate organoids to a single-cell state and re-plate in Matrigel at clonal density. The number of new organoids formed is a measure of self-renewing capacity.
- Exhaustion Phenotype: Analyze T cells from the co-culture for expression of exhaustion markers (PD-1, TIM-3, LAG-3) via flow cytometry and functional impairment via IFN-γ ELISpot [93].
Workflow for establishing a complex CSC organoid co-culture model.
Emerging and Integrated Strategies for Future Research
To overcome the limitations of individual models, the field is moving towards an integrative approach that leverages advanced technologies.
Table 3: Emerging Strategies to Overcome Model Limitations
| Strategy | Description | Application in CSC Research |
|---|---|---|
| CRISPR-based Lineage Tracing | Enables the fate mapping of individual CSCs and their progeny within a growing tumor or organoid, directly testing hierarchical organization [5] [92]. | Introduce an inducible Cre recombinase or a fluorescent barcode into the locus of a putative CSC marker (e.g., LGR5) to track clonal evolution and plasticity in real-time. |
| AI-Driven Multiomics | Integrates single-cell RNA sequencing, spatial transcriptomics, and proteomic data to deconvolute CSC heterogeneity and identify novel regulatory networks [5]. | Identify conserved transcriptional programs of stemness across different marker-defined subpopulations and predict key vulnerabilities. |
| Synthetic Biology & CAR-T Cells | Uses engineered immune cells or signaling modules to target CSC-specific surface markers or activate precise signaling pathways [5] [93]. | Develop CAR-T cells or bispecific engagers targeting CSC markers like EpCAM or specific γδ T cell receptors to eliminate CSCs in a humanized model [5] [93]. |
| Humanized Mouse Models | Immunodeficient mice engrafted with human immune system components (e.g., CD34+ hematopoietic stem cells) to create a more relevant human immune niche [93]. | Study CSC-immune cell interactions (e.g., T cell exhaustion, macrophage polarization) and test immunotherapies in a more physiologically accurate context. |
The persistent challenges in identifying universal and reliable CSC markers are intrinsically linked to the limitations of the experimental models used to define them. The dynamic plasticity of CSCs, the critical dependence on niche signals, and the profound impact of technical assay parameters mean that no single model is sufficient. The path forward requires a disciplined, multi-faceted approach. Researchers must rigorously standardize xenotransplantation protocols while simultaneously embracing complex in vitro models that incorporate essential stromal and immune components. By integrating these refined assays with next-generation lineage tracing and omics technologies, the field can move closer to its ultimate goal: precisely identifying and eradicating the cancer stem cells that drive patient mortality.
Validating Markers and Future Directions: From Novel Targets to Clinical Trials
Genome-Wide CRISPR-Cas9 Screens for Identifying Novel Pathway-Based Targets
Genome-wide CRISPR-Cas9 screening has emerged as a powerful functional genomics approach for systematically identifying genes and pathways essential for specific biological processes and disease states. Within cancer research, this technology provides an unprecedented tool for addressing one of the most challenging frontiers: the identification and targeting of cancer stem cells (CSCs). CSCs constitute a highly plastic, therapy-resistant cell subpopulation that drives tumor initiation, progression, metastasis, and relapse, yet their reliable identification and targeting remain formidable challenges due to their dynamic nature and heterogeneity [5]. This technical guide outlines comprehensive methodologies for designing, executing, and analyzing genome-wide CRISPR screens specifically focused on uncovering novel pathway-based targets, with emphasis on applications within CSC biology. We detail experimental protocols, analytical frameworks, and visualization approaches to equip researchers with the tools necessary to advance therapeutic development against these critical drivers of cancer malignancy.
The Cancer Stem Cell Challenge
Cancer stem cells exhibit self-renewal capacity, enhanced survival mechanisms, and resistance to conventional therapies, leading to tumor relapse and progression [5]. Their ability to evade treatment and drive metastasis makes them critical targets for improving cancer therapies; however, a major challenge is the absence of universal CSC markers. While surface proteins such as CD44 and CD133 have been widely used to isolate CSC populations, these markers are not exclusive to CSCs and are often expressed in normal stem cells or non-tumorigenic cancer cells [5]. Furthermore, CSC identity appears to be a dynamic functional state rather than a static subpopulation, with non-CSCs capable of acquiring stem-like features in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure [5]. This plasticity, combined with the profound heterogeneity within and across tumor types, necessitates powerful systematic approaches like genome-wide CRISPR screening to functionally interrogate CSC biology beyond surface marker identification.
CRISPR Screening Fundamentals
CRISPR screening represents a paradigm shift in functional genomics, enabling systematic loss-of-function or gain-of-function studies at unprecedented scale and precision. The technology leverages the bacterial CRISPR-Cas9 system, which consists of a programmable guide RNA (gRNA) and a Cas9 nuclease that together form a ribonucleoprotein complex capable of creating double-strand breaks in DNA [95]. In CRISPR knockout screens, these breaks lead to insertions or deletions that disrupt gene function, while CRISPR interference and activation approaches utilize a deactivated Cas9 fused to transcriptional repressors or activators to modulate gene expression without altering DNA sequence [96].
Pooled CRISPR screens involve introducing a complex library of sgRNAs into a single population of cells, allowing for the functional interrogation of thousands of genes in parallel [95]. The power of this approach lies in its ability to connect genetic perturbations to phenotypic outcomes through sequencing-based quantification of sgRNA abundance, enabling the identification of genes essential for specific biological processes, including those central to CSC maintenance and function [96] [95].
Experimental Design and Workflow
Screening Strategies and Library Selection
The design phase of a CRISPR screen is critical for obtaining meaningful results. Researchers must first determine the screening format based on their specific biological question, available resources, and phenotypic readouts.
Table 1: Comparison of Pooled vs. Arrayed CRISPR Screen Formats
| Parameter | Pooled Screen | Arrayed Screen |
|---|---|---|
| Library Delivery | Lentiviral transduction of mixed sgRNA population | Individual sgRNAs delivered per well |
| Compatible Assays | Binary assays (viability, FACS sorting) | Multiparametric assays (imaging, high-content) |
| Phenotype-Genotype Linking | Requires NGS deconvolution | Direct as targets are physically separated |
| Throughput | High (entire genome in one vessel) | Moderate (one gene per well) |
| Cost and Infrastructure | Lower cost, requires NGS | Higher cost, requires automation |
| Best Applications | Initial discovery, positive/negative selection | Validation, complex phenotypic readouts |
For CSC-focused applications, pooled screens are typically employed as primary discovery tools to identify genes essential for CSC maintenance, drug resistance, or specific functional states, while arrayed formats are valuable for secondary validation and detailed mechanistic studies using more complex assays [95]. Library design considerations include targeting early exons to maximize frameshift mutations, using multiple sgRNAs per gene to account for variable efficiency, and incorporating controls for normalization and quality assessment [95]. For studies focusing on CSC biology, libraries can be tailored to include genes previously implicated in stemness pathways, epigenetic regulation, and drug resistance mechanisms.
Core Experimental Protocol
The following detailed protocol outlines the key steps for performing a pooled genome-wide CRISPR knockout screen targeting cancer stem cell properties:
Step 1: Library Selection and Preparation
- Select an appropriate genome-wide sgRNA library (e.g., Brunello, GeCKO v2) with approximately 4-6 sgRNAs per gene and including non-targeting control sgRNAs.
- Amplify the plasmid library following manufacturer protocols and prepare high-titer lentiviral particles. Determine viral titer by transducing cells with serial dilutions and selecting with appropriate antibiotics.
Step 2: Cell Line Engineering and Viral Transduction
- Engineer recipient cell lines to stably express Cas9 nuclease. Validate editing efficiency using surrogate reporters or T7E1 assays.
- Transduce cells with the sgRNA library lentivirus at a low multiplicity of infection (MOI ~0.3-0.4) to ensure most cells receive a single sgRNA. Include appropriate controls (non-targeting sgRNAs).
- Culture transduced cells under selection pressure (e.g., puromycin) for 5-7 days to eliminate non-transduced cells.
Step 3: Phenotypic Selection
- For CSC-focused screens, implement appropriate phenotypic selection strategies:
- Drug Treatment: Apply chemotherapeutic agents at relevant IC50 concentrations to identify genes conferring resistance or sensitivity.
- FACS Sorting: Isolate CSC-enriched populations using established surface markers (CD44, CD133, EpCAM) or reporter systems.
- Sphere Formation Assays: Culture under ultra-low attachment conditions to select for self-renewing populations.
- Metabolic Selection: Utilize culture conditions that exploit CSC metabolic dependencies (e.g., hypoxia, altered nutrient availability).
- Maintain adequate library coverage (minimum 500x, recommended 1000x) throughout selection to prevent stochastic sgRNA loss.
Step 4: Genomic DNA Extraction and Sequencing
- Harvest a minimum of 50 million cells per condition (pre- and post-selection) to maintain library representation.
- Extract genomic DNA using scalable methods (e.g., phenol-chloroform, commercial kits). Quantity and quality control are critical.
- Amplify integrated sgRNA sequences using PCR with barcoded primers for multiplexing. Use a minimum of PCR cycles to maintain representation.
- Sequence amplified products on Illumina platforms (minimum 75bp single-end reads).
Step 5: Sequencing Data Preprocessing
- Perform quality control on raw sequencing data using tools like FastQC. Require Q20 > 90% or Q30 > 85% for high-quality data [97].
- Trim adapter sequences and low-quality bases using tools like Skewer.
- Align cleaned reads to the reference sgRNA library using exact matching or specialized aligners.
- Generate count tables for each sgRNA in all conditions.
Data Analysis and Bioinformatics Pipeline
Quality Control and Read Processing
The initial phase of CRISPR screen analysis focuses on ensuring data quality and integrity. Raw sequencing files must undergo rigorous quality assessment based on Q20 and Q30 scores, with Q20 > 90% or Q30 > 85% considered acceptable thresholds [97]. Following quality assessment, reads are aligned to the reference sgRNA library, with sequencing depth evaluation critical for reliable results. A minimum sequencing depth of 300x is recommended (calculated as mapped reads divided by number of sgRNAs in the library) [97]. This ensures sufficient coverage to detect meaningful changes in sgRNA abundance across conditions.
Differential Enrichment Analysis
The core of CRISPR screen analysis involves identifying sgRNAs and genes that show significant enrichment or depletion between experimental conditions. The Robust Rank Aggregation algorithm, as implemented in the widely used MAGeCK software, has become a standard approach for this purpose [96] [97]. RRA analyzes the distribution of sgRNA rankings across all conditions, scoring each gene based on whether sgRNAs targeting it are enriched at the extreme ends of the distribution rather than randomly distributed [96] [97]. Genes are then ranked by their RRA scores, with lower scores indicating higher ranking and greater likelihood of being true hits [97].
Multiple statistical frameworks have been developed for CRISPR screen analysis, each with particular strengths:
Table 2: Bioinformatics Tools for CRISPR Screen Analysis
| Tool | Statistical Approach | Key Features | Best Applications |
|---|---|---|---|
| MAGeCK (RRA) | Negative binomial distribution, Robust rank aggregation | Comprehensive workflow, QC, visualization | Genome-wide knockout screens |
| BAGEL | Reference gene set distribution, Bayes factor | Benchmarking against essential genes | Essential gene identification |
| CRISPhieRmix | Hierarchical mixture model | Accounts for multiple sgRNA efficacy | Screens with variable sgRNA efficiency |
| JACKS | Bayesian hierarchical modeling | Models sgRNA efficacy explicitly | Improved quantification of gene effects |
| DrugZ | Normal distribution, Sum z-score | Specifically designed for chemogenetic screens | Drug-gene interaction studies |
For CSC-focused analyses, researchers should consider employing multiple analytical approaches to enhance confidence in identified hits, particularly given the heterogeneity and plasticity of CSC populations.
Hit Selection and Validation
Following statistical analysis, candidate genes must be prioritized for experimental validation. Three primary approaches facilitate this process:
Rank-Based Selection: Genes are prioritized based on their RRA ranking, with the top 20-30 candidates typically selected for downstream validation [97]. For example, Liu et al. identified the target gene Cop1 through RRA algorithm ranking [97].
Statistical Thresholding: Combined thresholds of p-value < 0.01 and log fold change (LFC) ≤ -2 can identify genes with both statistical significance and strong biological effects [97]. This approach was used by Guo et al. to identify CDC7 as a synergistic target of chemotherapy in resistant small-cell lung cancer [97].
False Discovery Rate Control: Applying FDR < 0.05 provides the most stringent selection criteria but may eliminate true positives due to the extreme multiple testing burden in genome-wide screens [97].
Following hit identification, enrichment analyses including Gene Ontology and GSEA help place candidate genes in biological context, revealing pathways and processes important for the phenotype of interest [97].
Applications in Cancer Stem Cell Research
Identifying CSC Dependencies and Vulnerabilities
Genome-wide CRISPR screens have proven particularly powerful for identifying genetic dependencies specific to CSCs. By applying positive selection for stem-like properties (e.g., sphere formation, marker expression) or negative selection against differentiation, researchers can pinpoint genes essential for CSC maintenance. A recent genome-wide CRISPR screen in primary human natural killer cells identified critical checkpoints regulating resistance to immunosuppressive pressures, with ablation of MED12, ARIH2, and CCNC significantly improving antitumor activity against multiple treatment-refractory human cancers [98]. These findings highlight how CRISPR screening can reveal previously unappreciated regulators of cell function with direct therapeutic implications.
In hepatic cancer research, integrative approaches combining CRISPR screening with proteomic analysis of CSC populations have identified novel markers and vulnerabilities. For example, proteomic profiling of CD133+ Huh7 cells revealed elevated expression of S100 family members, suggesting these calcium-binding proteins as potential novel CSC markers and therapeutic targets [99]. Such integrated approaches leverage the unbiased nature of CRISPR screening while providing mechanistic insights through multi-omics validation.
Overcoming Therapy Resistance
CSCs represent a major source of therapy resistance and tumor recurrence, making them prime targets for combination therapies. CRISPR screens conducted in the presence of chemotherapeutic agents or targeted therapies can identify genes whose disruption sensitizes CSCs to treatment. For instance, a CRISPR screen identifying CDC7 as a synergistic target of chemotherapy in resistant small-cell lung cancer demonstrated how combination approaches could overcome resistance mechanisms [97]. Similarly, CRISPR screens in CAR-T cells for multiple myeloma have identified time- and context-specific regulators of persistence, with CDKN1B emerging as a key late-stage brake on proliferation and function whose ablation boosted expansion, cytotoxicity and tumour clearance [100].
Mapping CSC-Specific Pathway Dependencies
Beyond individual gene discoveries, CRISPR screening enables the systematic mapping of pathway dependencies in CSCs. By analyzing screen hits through pathway enrichment and protein-protein interaction networks, researchers can identify coordinated genetic modules and signaling pathways essential for CSC function. This approach has revealed the importance of metabolic pathways, epigenetic regulators, and niche interaction signals in maintaining CSC states. The development of advanced analytical frameworks, including hypergraph approaches that model multi-node connections through hyperedges, allows for more sophisticated modeling of CSC marker networks and their distribution across organs, providing insights into metastatic potential and tissue-specific vulnerabilities [71].
Research Reagent Solutions
Successful execution of CRISPR screens requires carefully selected reagents and tools. The following table outlines essential components and their functions:
Table 3: Essential Research Reagents for CRISPR Screening
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| CRISPR Libraries | Brunello, GeCKO v2, Human CRISPR Knockout Library | Comprehensive sgRNA collections targeting entire genome or specific gene sets |
| Cas9 Systems | Lentiviral Cas9, Cell lines with stable Cas9 expression | Nuclease component for creating targeted DNA breaks |
| Delivery Tools | Lentiviral packaging systems (psPAX2, pMD2.G), Transfection reagents | Introduction of CRISPR components into target cells |
| Selection Markers | Puromycin, Blasticidin, GFP/RFP reporters | Selection and tracking of successfully transduced cells |
| Cell Culture Models | Patient-derived organoids, CSC-enriched cell lines, Immortalized lines | Biologically relevant systems for screening |
| Antibodies for Sorting | Anti-CD44, Anti-CD133, Anti-EpCAM | Isolation of CSC populations by surface markers |
| Analysis Software | MAGeCK, BAGEL, CRISPhieRmix | Bioinformatics tools for screen hit identification |
| Validation Reagents | siRNA pools, Small molecule inhibitors, Antibodies for Western blot | Independent confirmation of screening hits |
Genome-wide CRISPR-Cas9 screening represents a transformative approach for identifying novel pathway-based targets in cancer research, with particular relevance for addressing the challenges of cancer stem cell biology. The integrated experimental and computational framework outlined in this guide provides researchers with a robust methodology for uncovering genetic dependencies, mapping functional pathways, and identifying therapeutic vulnerabilities in these critical cell populations. As screening technologies continue to evolve—incorporating single-cell readouts, spatial resolution, and more sophisticated analytical frameworks—their power to dissect the complex biology of CSCs will only increase. By applying these systematic approaches, researchers can accelerate the development of targeted therapies capable of overcoming treatment resistance and preventing tumor recurrence, ultimately improving outcomes for cancer patients.
The cancer stem cell (CSC) hypothesis proposes that tumors are maintained by a subpopulation of cells with stem-like properties, including self-renewal capacity, differentiation potential, and enhanced therapeutic resistance [5] [101]. These cells are responsible for tumor initiation, progression, metastasis, and relapse. While CSCs have been identified in both solid tumors and hematological malignancies, their biology, marker expression, and microenvironmental interactions exhibit significant differences based on tissue origin and pathological context.
The first conclusive evidence for CSCs emerged from studies of acute myeloid leukemia (AML), which identified a CD34⁺CD38⁻ cell subpopulation with leukemia-initiating potential in immunodeficient mice [5] [101]. This foundational work paved the way for discovering CSCs in various solid tumors, including breast, brain, colon, and pancreatic cancers [5]. This review provides a comprehensive comparative analysis of CSC biology across solid tumors and hematological malignancies, focusing on identification challenges, marker networks, and therapeutic implications.
Historical Evolution and Fundamental Concepts
The conceptual origins of CSCs date back to the 19th century. In 1858, Rudolf Virchow introduced the principle "omnis cellula e cellula" (every cell from a cell), suggesting tumors originate from pathological alterations in normal cells [5]. Julius Cohnheim later proposed the "embryonal rest hypothesis," suggesting tumors arise from residual embryonic cells that persist in adult tissues [5]. Modern CSC theory was solidified between 1994-1997 by John Edgar Dick's groundbreaking research on AML, which functionally identified SCID-leukemia-initiating cells (SL-ICs) characterized as CD34⁺CD38⁻ cells [5].
The CSC compartment is not static but exhibits remarkable plasticity, allowing transitions between stem-like and differentiated states in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure [5] [2]. This adaptability underscores CSCs' role in therapeutic resistance and tumor recurrence, presenting significant challenges for cancer eradication.
Comparative Analysis of CSC Markers and Identification
Marker Expression Patterns
CSCs are primarily identified and isolated using specific cell surface markers, though these markers are not always universal across cancer types and often share expression with normal stem cells.
Table 1: Key CSC Markers in Solid Tumors and Hematological Malignancies
| CSC Marker | Solid Tumors | Hematological Malignancies | Shared with Normal Stem Cells |
|---|---|---|---|
| CD44 | Breast, prostate, colon, glioma, pancreas, OSCC [8] [71] [9] | AML, multiple myeloma [9] | Adult stem cells [102] |
| CD133 | Brain, colon, liver, lung, ovary [102] | AML [71] | Hematopoietic stem cells [102] |
| CD34 | Limited expression | AML (CD34⁺CD38⁻) [5] [101] | Hematopoietic stem cells [102] |
| CD38 | Not typically used | AML (CD34⁺CD38⁻) [101] | Differentiated hematopoietic cells |
| ALDH1 | Breast, colon, OSCC [8] | AML [2] | Embryonic and adult stem cells [102] |
| LGR5 | Gastrointestinal cancers [5] | Limited expression | Intestinal, stomach adult stem cells [102] |
| p75NTR | OSCC, melanoma, esophageal carcinoma [8] | Not typically reported | Normal oral keratinocyte stem cells [8] |
Technical Challenges in CSC Identification
Several technical challenges complicate CSC identification across both cancer types:
- Lack of Universal Markers: No single marker exclusively identifies CSCs across all cancer types. Markers such as CD44 and CD133 are not CSC-specific and are expressed on normal stem cells [5] [102].
- Marker Heterogeneity: Multiple CSC subpopulations with distinct marker profiles can coexist within a single tumor. In oral squamous cell carcinoma (OSCC), p75NTR⁺ and ALDH1A1⁺ cells represent largely non-overlapping subpopulations with different clinical correlations [8].
- Dynamic Plasticity: CSC marker expression is not fixed. Studies demonstrate that marker-negative populations can regenerate marker-positive cells over time, and CSCs can transition between different phenotypic states [8] [2].
- Functional Validation Requirements: Ultimately, CSC identity must be confirmed through functional assays, notably tumor-initiating capacity in immunodeficient mice, as surface markers alone are insufficient for definitive identification [101].
Methodological Approaches for CSC Study
Experimental Workflows
Diagram Title: CSC Identification & Validation Workflow
Research Reagent Solutions
Table 2: Essential Research Tools for CSC Investigation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Surface Marker Antibodies | Anti-CD44, Anti-CD133, Anti-CD34, Anti-CD38, Anti-ALDH1A1 | Flow cytometry, cell sorting, immunohistochemistry |
| Fluorescence-Activated Cell Sorting (FACS) | BD FACS Aria, Beckman Coulter MoFlo | Isolation of pure CSC subpopulations based on surface markers |
| Aldefluor Assay | ALDH enzymatic activity kit | Identification of CSCs with high ALDH activity |
| In Vivo Modeling | NOD/SCID/NSG mice | Functional validation of tumor-initiating capacity |
| 3D Culture Systems | Ultra-low attachment plates, defined growth factors | Sphere formation assays (mammospheres, tumorspheres) |
| Stemness Pathway Inhibitors | Wnt/β-catenin, Notch, Hedgehog inhibitors | Investigation of signaling pathways governing stemness |
| Single-Cell RNA Sequencing | 10x Genomics, Smart-seq2 | Analysis of CSC heterogeneity and transcriptional programs |
Computational and Modeling Approaches
Advanced computational methods are increasingly important for CSC research:
- Stemness Indices: Machine learning algorithms like one-class logistic regression (OCLR) can derive stemness indices from transcriptomic data. For hematological malignancies, the HSCsi (Hematopoietic Stem Cell stemness index) effectively identifies leukemia stem cells and predicts clinical outcomes [103].
- Hypergraph Theory: This approach models CSC marker co-expression across multiple organs, capturing complex relationships that traditional pairwise methods miss. Hypergraphs can identify key markers driving metastasis, such as CD44⁺CD133⁺ coupling in liver, stomach, and colon cancers [71].
- Multiomics Integration: Combining genomic, transcriptomic, epigenomic, and proteomic data provides comprehensive insights into CSC regulatory networks and heterogeneity.
Therapeutic Implications and Resistance Mechanisms
CSC-Mediated Treatment Resistance
CSCs employ multiple mechanisms to evade conventional therapies:
- Enhanced DNA Repair Capacity: CSCs possess robust DNA damage response systems, enabling survival after radiation or chemotherapy [5].
- Drug Efflux Pumps: Upregulation of ATP-binding cassette (ABC) transporters such as ABCG2 allows CSCs to expel chemotherapeutic agents [102].
- Quiescence: Many CSCs remain in a slow-cycling or dormant state, evading treatments that target rapidly dividing cells [2].
- Metabolic Plasticity: CSCs can switch between glycolysis, oxidative phosphorylation, and alternative fuel sources to survive under diverse conditions [5].
Immune Evasion Strategies
CSCs utilize both intrinsic and extrinsic mechanisms to avoid immune detection:
- Immune Checkpoint Expression: CSCs upregulate PD-L1, B7-H4, CD47, and CD24, which inhibit T-cell function and macrophage phagocytosis [2].
- Antigen Presentation Downregulation: Reduced MHC class I expression limits CSC visibility to cytotoxic T lymphocytes [2].
- Immunosuppressive Niche Remodeling: CSCs recruit regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs) while secreting immunosuppressive cytokines [2].
Diagram Title: CSC Immune Evasion Mechanisms
Future Directions and Concluding Remarks
The comparative analysis of CSCs across solid tumors and hematological malignancies reveals both shared fundamental properties and critical context-dependent differences. Future research directions should focus on:
- Overcoming Marker Limitations: Developing functional assays and combinatorial marker panels that account for CSC plasticity and heterogeneity.
- Niche-Targeting Strategies: Developing therapies that disrupt the protective CSC microenvironment while sparing normal stem cell niches.
- Advanced Modeling Approaches: Implementing 3D organoid models, CRISPR-based functional screens, and AI-driven multiomics integration to identify novel CSC vulnerabilities.
- Dual-Targeting Therapies: Combining conventional therapies with CSC-directed agents to address both bulk tumors and treatment-resistant subpopulations.
The continued refinement of CSC investigation methodologies, coupled with innovative therapeutic approaches targeting stemness pathways, holds promise for overcoming therapy resistance and improving patient outcomes across the spectrum of malignant diseases.
The precise identification and characterization of cancer stem cells (CSCs) represents one of the most significant challenges in modern oncology. These cells constitute a highly plastic and therapy-resistant subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [5]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies. However, the absence of universal CSC biomarkers and their dynamic phenotypic and functional plasticity have hindered progress in effectively targeting these cells [5].
Emerging technologies in spatial transcriptomics and artificial intelligence (AI) are now revolutionizing our approach to CSC research. Spatial transcriptomics technologies enable the mapping of gene expression within tissues while preserving crucial spatial context, allowing researchers to visualize the spatial distribution of RNA molecules and gain insights into cellular organization, interactions, and functions in their native environments [104]. When combined with AI-driven digital pathology platforms, these technologies provide unprecedented capabilities for deciphering the intricate stem cell niches that maintain CSCs and influence therapeutic resistance [105]. This technological convergence is particularly valuable for investigating the spatial relationships and cellular cross-talk within specific CSC niches, which are often characterized by unique microenvironmental properties such as hypoxia and glucose deprivation [105].
This whitepaper provides an in-depth technical examination of how these emerging technologies are transforming CSC research, with a focus on practical implementation, methodological considerations, and applications in overcoming identification challenges. We present comprehensive comparisons of available platforms, detailed experimental protocols, computational workflows, and specialized tools for the research and drug development community.
Core Technologies: Spatial Transcriptomics Platforms and Architectures
Spatial transcriptomics technologies can be broadly categorized into two groups: imaging-based and sequencing-based platforms [104]. While both approaches reveal the spatial locations of gene expression, their underlying technologies differ drastically in capturing spatial information and determining abundance of specific mRNA molecules within tissue.
Imaging-Based Spatial Transcriptomics Platforms
Imaging-based technologies employ single-molecule fluorescence in situ hybridization (smFISH) as their backbone technology, enabling simultaneous detection of up to several thousand RNA transcripts through cyclic, highly multiplexed smFISH [104].
Table 1: Comparative Analysis of Major Imaging-Based Spatial Transcriptomics Platforms
| Platform | Core Technology | Key Differentiating Features | Gene Capacity | Resolution | Best Applications in CSC Research |
|---|---|---|---|---|---|
| 10X Xenium | Hybrid ISS/ISH with padlock probes | Padlock probes with rolling circle amplification (RCA) for signal enhancement | Hundreds to thousands | Subcellular | CSC niche mapping with high sensitivity |
| MERSCOPE | Binary barcoding strategy | Four "1"s in predetermined barcode order reduce optical crowding | Hundreds to thousands | Subcellular | Long-term CSC monitoring and tracking |
| CosMx SMI | Combinatorial color and positional encoding | 16-round imaging with UV cleavage and branched signal amplification | Whole transcriptome (6,000+ genes) | Subcellular | Comprehensive CSC heterogeneity profiling |
Xenium utilizes a hybrid technology combining in situ sequencing (ISS) and in situ hybridization (ISH). An average of 8 padlock probes, each containing a gene-specific barcode, hybridize to the target RNA transcript. Upon successful binding, these probes undergo highly specific ligation to form circular DNA constructs, which are then enzymatically amplified through rolling circle amplification (RCA), producing multiple copies to enhance signal sensitivity [104].
MERSCOPE employs a distinctive binary barcode strategy for gene identification. Each gene is assigned a unique binary barcode consisting of a series sequence of "0"s and "1"s. Thirty to fifty gene-specific primary probes hybridize to different regions of the targeted gene, each with "hangout tails" for secondary probe binding. The decoding process occurs over multiple rounds of imaging, signal stripping, and new secondary probe introduction, where fluorescence detection corresponds to a "1" in the barcode [104].
CosMx SMI incorporates both hybridization and positional dimensions for gene identification. The process begins with a pool of five gene-specific probes, each containing a target-binding domain and a readout domain with 16 sub-domains. Each secondary probe includes a primary probe binding domain linked to a branched, fluorescently labeled readout domain through a UV-cleavable linker. The branched readout domain allows attaching multiple fluorophores to effectively enhance signal intensity [104].
Sequencing-Based Spatial Transcriptomics Platforms
Sequencing-based technologies integrate spatially barcoded arrays with next-generation sequencing to determine the locations and expression levels of transcripts within tissues.
Table 2: Comparative Analysis of Major Sequencing-Based Spatial Transcriptomics Platforms
| Platform | Core Technology | Spatial Barcoding Approach | Tissue Capture Area | Resolution | Throughput Considerations |
|---|---|---|---|---|---|
| 10X Visium | Spatially barcoded RNA-binding probes | 55μm spots with oligo-dT capture | 6.5×6.5mm (standard), 11×11mm (extended) | Multi-cellular | High throughput for CSC screening |
| Visium HD | Enhanced Visium with smaller features | 2μm spots with same chemistry as Visium V2 | 6.5×6.5mm | Cellular | Fine mapping of CSC boundaries |
| Stereo-seq | DNA nanoball (DNB) technology | 0.5μm center-to-center DNB spacing | Customizable arrays | Subcellular | Ultra-high resolution CSC mapping |
10X Visium and Visium HD rely on spatially barcoded RNA-binding probes attached to the slide surface. These probes contain several domains, including a spatial barcode for decoding location, a random molecular tag (UMI) for quantifying unique mRNA transcripts, and an oligo-dT sequence for mRNA binding [104]. Visium HD uses the same fundamental technology as the Visium V2 workflow but features a significantly smaller spot size of 2μm compared to the standard 55μm feature size in original Visium, dramatically enhancing spatial resolution.
Stereo-seq utilizes DNA nanoball (DNB) technology for in situ RNA capture. Unlike 10X Visium, which directly attaches oligo probes to the slide, Stereo-seq oligo probes are circularized and used as templates to generate DNA nanoballs (DNBs) via rolling circle amplification (RCA). The DNBs are then loaded onto a grid-patterned array to create the capture slides, with a diameter of approximately 0.2μm and a center-to-center distance of 0.5μm [104].
AI-Driven Digital Pathology: Computational Frameworks for CSC Analysis
Artificial intelligence is transforming digital pathology through advanced computational frameworks that enhance and extend the capabilities of spatial transcriptomics for CSC research.
Integrated AI-Spatial Transcriptomics Frameworks
The iSCALE (inferring Spatially resolved Cellular Architectures in Large-sized tissue Environments) framework represents a significant advancement for large tissue analysis [106]. This machine learning approach is designed to predict gene expression for large-sized tissues with cellular-level resolution by leveraging the relationship between gene expression and histological features learned from a small set of training ST captures.
iSCALE Computational Workflow
The iSCALE workflow begins with a large H&E-stained histology image (mother image) and selects regions from the same tissue block that fit standard ST platform capture areas (daughter captures). After spatial clustering analysis on daughter ST data, a semi-automatic alignment process maps daughter captures onto the mother image. The framework then integrates gene expression and spatial information across aligned daughter captures and employs a feedforward neural network to learn relationships between histological image features and gene expression. The resulting model predicts gene expression for each 8μm × 8μm superpixel across the entire mother image, enabling annotation of cell types and identification of enriched cell types in each tissue region [106].
In benchmarking experiments on a large gastric cancer sample, iSCALE significantly outperformed existing methods like iStar and RedeHist in accurately identifying key tissue structures including tumor, tumor-infiltrated stroma, and tertiary lymphoid structures [106]. When focused on regions containing signet ring cells (associated with aggressive gastric cancer), iSCALE accurately identified boundaries between poorly cohesive carcinoma regions with CSCs and adjacent normal mucosa, where other methods failed.
Multimodal AI Platforms for Clinical Translation
MUSK (Multimodal Transformer with Unified Mask Modeling) represents a foundational AI model that incorporates both visual information from medical images and text-based data from clinical notes and pathology reports [107]. After training on 50 million medical images and more than 1 billion pathology-related texts, MUSK outperformed standard methods in predicting cancer prognoses across diverse cancer types, identifying patients likely to benefit from immunotherapy, and pinpointing individuals with melanoma at high risk of recurrence [107].
For all cancer types evaluated, MUSK accurately predicted disease-specific survival 75% of the time, compared to 64% accuracy for standard predictions based on cancer stage and clinical risk factors [107]. For non-small cell lung cancer, MUSK correctly identified patients who benefited from immunotherapy treatment about 77% of the time, significantly outperforming the standard method of predicting immunotherapy response based on PD-L1 expression alone (61% accuracy) [107].
Nuclei.io is an AI-based digital pathology framework that adopts a human-in-the-loop approach, learning from pathologists and adapting to individual workflows [108]. Rather than replacing pathologists, it provides personalized assistance in spotting cells linked to disease and allows pathologists to share models with colleagues collaboratively. The platform significantly reduces time-consuming tasks, such as identifying plasma cells in stromal portions of biopsies, which traditionally required additional immunohistochemical stains and 5-10 minutes of manual scanning, now accomplished in seconds through AI assistance [108].
Experimental Protocols: Integrated Workflows for CSC Niche Characterization
Large Tissue Spatial Profiling with iSCALE
Objective: To comprehensively map CSC distributions and their niches in large tissue specimens beyond the size limitations of conventional spatial transcriptomics platforms.
Materials and Reagents:
- Large-sized formalin-fixed paraffin-embedded (FFPE) or fresh frozen tissue section
- Standard H&E staining reagents
- Spatial transcriptomics platform (Visium, Xenium, or MERSCOPE)
- Tissue nucleic acid extraction kits
- Library preparation reagents compatible with chosen ST platform
- DAPI staining solution for nuclear visualization
Methodology:
- Tissue Preparation and Histology: Generate large-sized tissue sections (up to 25mm × 75mm) and process for standard H&E staining. Create serial sections for spatial transcriptomics analysis.
- Daughter Capture Selection: Identify multiple representative regions (typically 3-6) within the large tissue section that capture key histological features and potential CSC niches based on H&E morphology.
- ST Processing: Process selected daughter regions using appropriate ST platform protocol (Visium, Xenium, or MERSCOPE) following manufacturer instructions.
- Image Alignment and Integration: Utilize iSCALE's semi-automatic alignment algorithm to map daughter ST captures onto the mother H&E image, achieving >99% alignment accuracy [106].
- Model Training: Train iSCALE's neural network to learn relationships between histological features from the mother image and gene expression patterns from aligned daughter captures.
- Prediction and Validation: Apply the trained model to predict gene expression across the entire mother image at 8μm × 8μm superpixel resolution. Validate predictions using orthogonal methods such as immunohistochemistry or RNAscope.
- CSC Niche Identification: Leverage predicted gene expression maps to identify CSC-enriched regions based on known CSC markers (CD44, CD133, LGR5, etc.) and characterize associated niche components.
Technical Considerations: The number of daughter captures required depends on tissue heterogeneity, with more complex tissues benefiting from 5-6 captures. Alignment accuracy is critical and should be verified through manual inspection. For CSC research, include known CSC markers in the gene panel and focus validation efforts on regions with predicted high CSC abundance.
Multimodal AI for CSC Prognostication
Objective: To predict clinical outcomes and therapy responses in cancers with significant CSC involvement by integrating histopathology images with clinical data.
Materials and Reagents:
- Whole slide images (WSI) of H&E-stained tumor sections
- Clinical data including patient demographics, treatment history, and outcomes
- Computational resources with GPU acceleration
- MUSK or similar multimodal AI framework
- Data annotation tools for pathologist input
Methodology:
- Data Curation: Collect and preprocess WSIs and corresponding clinical data, ensuring data quality and consistency.
- Region of Interest Annotation: Have expert pathologists annotate regions with putative CSCs based on morphological features (e.g., tumor buds, specific nuclear features).
- Model Pretraining: Utilize foundation models pretrained on large-scale pathology image datasets (50+ million images) to initialize the AI model [107] [109].
- Multimodal Integration: Train the model to integrate features from WSIs with clinical variables using cross-attention mechanisms and transformer architectures.
- Task-Specific Fine-tuning: Adapt the general model to specific CSC-related tasks such as prognosis prediction, therapy response forecasting, or recurrence risk assessment.
- Validation and Interpretation: Evaluate model performance on independent validation cohorts and utilize attention mechanisms to identify histopathological features most predictive of outcomes.
Technical Considerations: For optimal CSC detection, include rare cell detection algorithms to account for the typically low abundance of CSCs within tumors. Model interpretation is critical for biological insights—focus on understanding which morphological features the model associates with poor outcomes and therapy resistance, as these may represent CSC correlates.
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Table 3: Essential Research Reagents and Computational Tools for CSC Spatial Analysis
| Category | Specific Product/Platform | Key Function in CSC Research | Technical Specifications | Application Notes |
|---|---|---|---|---|
| Spatial Transcriptomics Platforms | 10X Visium HD | Whole transcriptome mapping with cellular resolution | 2μm spot size, 6.5×6.5mm capture area | Ideal for CSC niche boundary definition |
| Xenium In Situ | Targeted subcellular transcript localization | Subcellular resolution, 500+ gene panel | Optimal for rare CSC detection | |
| MERSCOPE | High-plex subcellular transcript imaging | 500-1000 genes, binary barcoding | Suitable for CSC plasticity studies | |
| AI-Digital Pathology Tools | Nuclei.io | Human-in-the-loop CSC annotation | Adapts to pathologist workflow | Reduces CSC identification time by 80% [108] |
| MUSK Multimodal AI | Prognostic prediction from images and text | Processes 50M+ images and 1B+ text tokens [107] | 75% accuracy in cancer survival prediction | |
| iSCALE Framework | Large tissue gene expression prediction | 8μm superpixel resolution | Enables CSC mapping in entire organs | |
| Specialized Analysis Packages | sc-MTOP Framework | Single-cell morphological profiling | Analyzes 410M+ cells from WSIs [110] | Identifies CSC-associated ecotypes |
| CAPAI Biomarker | Risk stratification in ctDNA-negative patients | Combines H&E features with clinical data | Identifies high-risk CSC-driven recurrences |
Applications in Cancer Stem Cell Research: Overcoming Identification Challenges
Spatial transcriptomics and AI are directly addressing the fundamental challenges in CSC research, particularly the lack of universal biomarkers and dynamic phenotypic plasticity.
Resolving CSC Heterogeneity and Niche Interactions
CSCs exhibit significant functional and phenotypic heterogeneity, with their identity shaped by both intrinsic genetic programs and extrinsic cues from the microenvironment [5]. Spatial transcriptomics enables deconvolution of this heterogeneity by mapping distinct CSC subpopulations within their anatomical contexts. For example, in glioblastoma, CSCs frequently express neural lineage markers such as Nestin and SOX2, while gastrointestinal cancers may harbor CSCs characterized by LGR5 or CD166 expression [5]. The spatial relationships between these distinct CSC populations and their microenvironments can be precisely characterized through integrated AI-spatial analysis.
Advanced frameworks like iSCALE have demonstrated particular utility in identifying fine-grained tissue structures associated with CSCs, such as tertiary lymphoid structures (TLS) in gastric cancer [106]. These structures are crucial indicators of the tumor microenvironment's immune dynamics and have implications for CSC-mediated immune evasion. Similarly, the sc-MTOP (single-cell morphological and topological profiling) framework has enabled identification of distinct breast cancer ecotypes by extracting specific features from 410 million cells from whole slide images of 637 breast cancer samples [110]. This analysis, coupled with multiomics, revealed that tumors with locally clustered inflammatory cells respond better to immunotherapy in triple-negative breast cancers, providing insights into CSC-immune interactions.
Metabolic Plasticity and Therapy Resistance Mapping
CSCs exhibit remarkable metabolic plasticity, allowing them to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, enabling survival under diverse environmental conditions [5]. Spatial transcriptomics technologies can map this metabolic heterogeneity by visualizing the spatial distribution of metabolic enzymes and transporters within tumors. When combined with AI-based digital pathology, this enables correlation of metabolic states with morphological features observable in standard H&E stains.
AI tools have demonstrated capability in predicting therapy resistance mechanisms associated with CSCs. For instance, Stanford's MUSK model accurately identified which patients with lung or gastroesophageal cancers are likely to benefit from immunotherapy, significantly outperforming standard PD-L1 biomarker testing [107]. Similarly, the CAPAI (Combined Analysis of Pathologists and Artificial Intelligence) biomarker can stratify recurrence risk in stage III colon cancer patients, even in those with false-negative circulating tumor DNA results [109]. Among ctDNA-negative patients, CAPAI high-risk individuals showed 35% three-year recurrence rates versus 9% for low/intermediate-risk patients, suggesting an enhanced ability to identify CSC-driven recurrence risk [109].
Dynamic CSC Plasticity and State Transitions
CSCs represent a dynamic functional state rather than a static subpopulation, with non-CSCs capable of acquiring stem-like features in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure [5]. Longitudinal spatial analysis using AI-guided platforms enables tracking of these state transitions over time and in response to therapeutic interventions.
Spatial technologies enable the delineation of spatial patterns for niche-specific properties such as hypoxia, glucose deprivation, and other microenvironmental remodeling through multilevel spatial sequencing [105]. This is particularly valuable for understanding the dynamic transitions between CSC states, as these niche characteristics are known to influence CSC plasticity. Computational tools have been developed to specifically address the characterization of NSC and CSC niches, which are often hindered by technological limitations, but can be mitigated through appropriate computational solutions [105].
The integration of spatial transcriptomics with AI-powered digital pathology represents a paradigm shift in cancer stem cell research. These technologies are overcoming fundamental limitations in CSC identification by preserving crucial spatial context, enabling large-scale tissue analysis, and revealing previously inaccessible aspects of CSC biology. The ability to map CSCs within their native tissue architecture while correlating their spatial distribution with morphological features standardly assessed in pathology practice opens new avenues for understanding therapy resistance, metastasis, and recurrence.
For research and drug development professionals, these technologies offer powerful new approaches for identifying novel CSC targets, developing more effective therapeutic strategies, and designing clinical trials with improved patient stratification. As these technologies continue to evolve, particularly with advancements in multimodal AI and large-scale spatial profiling, they promise to accelerate the translation of CSC biology insights into clinical applications that ultimately improve patient outcomes in cancer.
Cancer stem cells (CSCs) are a subpopulation of tumor cells with self-renewal capacity, chemoresistance, and immune evasive properties that drive tumor initiation, progression, metastasis, and relapse. This technical review comprehensively examines three emerging immunotherapeutic approaches—chimeric antigen receptor (CAR)-T cells, antibody-drug conjugates (ADCs), and cancer vaccines—specifically targeting CSC populations. We explore the biological rationale, current evidence, and technical considerations for each modality, with detailed experimental protocols and analytical frameworks for preclinical and clinical evaluation. The content is framed within the broader context of CSC marker identification challenges and therapeutic resistance mechanisms, providing researchers and drug development professionals with a comprehensive resource for advancing CSC-targeted therapies.
Cancer stem cells (CSCs), also known as tumor-initiating cells, represent a functionally distinct subpopulation within tumors that possess the capacity for self-renewal, differentiation into heterogeneous progeny, and tumor reconstitution [111] [5]. These cells are pivotal drivers of tumor initiation, progression, therapy resistance, and recurrence. The CSC model proposes a hierarchical organization within tumors, contrasting with the clonal evolution model which attributes tumor growth primarily to random mutations [111]. Experimental evidence, such as the ability of just 100 CD133+ cells to initiate glioblastoma tumors in mice while 100,000 CD133- cells cannot, validates the tumor-initiating potency of CSCs [111].
CSCs exhibit several biological properties that confer resistance to conventional therapies:
- Enhanced DNA repair mechanisms: CSCs demonstrate heightened ability to repair DNA damage induced by chemotherapy or radiotherapy [111] [112]
- Drug efflux capabilities: Upregulated ABC transporters (e.g., ABCG2, ABCB1, ABCC1) actively expel chemotherapeutic agents [111] [112]
- Anti-apoptotic protein expression: Elevated levels of BCL-2, BCL-xL, and AKT enhance resistance to programmed cell death [112]
- Metabolic plasticity: Ability to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources to survive under diverse conditions [5]
- Microenvironment interaction: Dynamic crosstalk with stromal and immune cells in the tumor microenvironment (TME) promotes survival and immunosuppression [5] [9]
A fundamental challenge in CSC-targeted therapy is the identification of specific and reliable surface markers. CSC markers vary significantly across tumor types and even within individual tumors, reflecting substantial heterogeneity and plasticity [5] [8]. Common CSC markers include CD133, CD44, ALDH1A1, EpCAM, LGR5, and GD2, though none are universally specific to CSCs across all cancer types [5] [9] [112]. This marker heterogeneity necessitates sophisticated approaches for CSC identification and targeting, which we explore in the subsequent sections.
CAR-T Cell Therapy Targeting CSCs
Scientific Rationale and Biological Basis
Chimeric antigen receptor (CAR)-T cell therapy involves genetic engineering of T lymphocytes to express synthetic receptors that recognize specific tumor surface antigens independent of major histocompatibility complex (MHC) presentation [113] [112]. CARs are composed of an extracellular single-chain variable fragment (scFv) derived from monoclonal antibodies, a transmembrane domain, and intracellular signaling domains containing CD3ζ and costimulatory molecules (e.g., CD28, 4-1BB) [111] [113]. CAR-T cells targeting CSC-specific antigens offer a promising strategy to eliminate the root cause of tumor persistence and recurrence.
The fundamental advantage of CAR-T cells over conventional T-cell receptors is their ability to recognize a broader range of antigens including proteins, glycolipids, and carbohydrates in a non-MHC-restricted manner [113]. This is particularly valuable for targeting CSCs, which often employ MHC downregulation as an immune evasion mechanism. Furthermore, CAR-T cells combine the precision targeting of monoclonal antibodies with the cytolytic potency, persistence, and adaptive memory features of T lymphocytes [113].
Key CSC Antigens for CAR-T Targeting
Table 1: CSC Antigens Targeted by CAR-T Cells in Clinical Development
| Target Antigen | Cancer Types | Clinical Trial Phase | NCT Identifier | Key Findings |
|---|---|---|---|---|
| CD133 | Liver, pancreatic, brain, breast, ovarian, colorectal carcinoma, acute leukemia | Early-phase trials | NCT02541370, NCT03423992 | Targeting of CSC-rich populations; evaluation ongoing [112] |
| EGFR/IL13Rα2 | Glioblastoma (GBM) | Phase I | NCT05168423 | Tumor shrinkage in 85% of evaluable patients; median reduction of 35% [114] [115] |
| B7H3 | Glioblastoma (GBM) | Phase I | NCT05474378 | Median overall survival of 14.6 months; manageable neurotoxicity [114] [115] |
| HER2 | Breast cancer | Phase I | ChiCTR2500096093 | 75% disease control rate; hematologic toxicities observed [114] [115] |
| Mesothelin | Ovarian, pancreatic, NSCLC | Phase I | NCT06051695 | Tumor infiltration without dose-limiting toxicity; logic-gated approach [114] |
| Claudin 18.2 | Gastric/GEJ adenocarcinoma | Phase I | NCT05539430 | Lesion shrinkage in 83% of patients; ~41% maximum reduction [114] |
| GPC3 | Hepatocellular carcinoma | Phase I | NCT05652920 | Ongoing complete response at 9 months in one patient [114] |
Technical Protocols for CSC-Targeted CAR-T Development
CAR Construct Design and Validation
Fourth-Generation "ARMORED" CAR Design Protocol:
- scFv Selection: Clone variable heavy (VH) and variable light (VL) chains from CSC-specific monoclonal antibodies via phage display
- Extracellular Domain: Fuse scFv to IgG4 Fc spacer or CD8α hinge region to optimize binding geometry
- Transmembrane Domain: Incorporate CD28 or CD8α transmembrane domains for stability
- Intracellular Signaling: Combine CD3ζ with dual costimulatory domains (CD28 + 4-1BB)
- Cytokine Secretion Module: Insert IL-12 or IL-15 expression cassette under NFAT-responsive promoter
- Validation: Confirm surface expression by flow cytometry and functionality via cytokine release assays upon exposure to CSC-enriched populations [111] [112]
CSC Enrichment for Potency Testing
Tumor Sphere Formation Assay:
- Mechanically dissociate fresh tumor specimens to single-cell suspension
- Culture in serum-free DMEM/F12 medium supplemented with:
- 20 ng/mL EGF
- 10 ng/mL bFGF
- B27 supplement (1:50)
- 4 μg/mL heparin
- Plate at clonal density (1-10 cells/μL) in ultra-low attachment plates
- Incubate at 37°C, 5% CO₂ for 7-14 days
- Harvest primary spheres for limiting dilution transplantation assays or CAR-T cytotoxicity testing [111] [8]
Signaling Pathways in CSC-Targeted CAR-T Therapy
Diagram Title: CAR-T Cell Intracellular Signaling Cascade
Antibody-Drug Conjugates (ADCs) for CSC Targeting
Mechanism of Action and Rationale
Antibody-drug conjugates (ADCs) are bifunctional molecules comprising a monoclonal antibody specific for a CSC surface antigen, connected via a chemical linker to a potent cytotoxic payload [116]. The fundamental advantage of ADCs for CSC targeting lies in their ability to deliver highly toxic agents specifically to CSCs while minimizing systemic exposure, thereby overcoming the therapeutic index limitations of conventional chemotherapy [116].
ADCs target CSCs through three sequential mechanisms:
- Antibody-mediated binding to CSC-specific surface antigens
- Internalization of the ADC-antigen complex via receptor-mediated endocytosis
- Intracellular payload release through linker cleavage in endosomal/lysosomal compartments
The released payload then induces cell death through mechanisms including microtubule disruption, DNA damage, or topoisomerase inhibition [116].
ADC Payload Classes and Their Applications in CSC Targeting
Table 2: ADC Payload Classes for CSC Targeting
| Payload Class | Specific Agents | Mechanism of Action | Advantages for CSC Targeting | Clinical-Stage Examples |
|---|---|---|---|---|
| Microtubule-disrupting agents | MMAE, MMAF, DM1, DM4 | Inhibit tubulin polymerization, cause mitotic arrest | Overcome taxane resistance via different binding sites | Enfortumab vedotin, Trastuzumab emtansine [116] |
| Topoisomerase I inhibitors | Deruxtecan (DXd), Exatecan | Stabilize TOPI-DNA complex, induce single-strand breaks | Synergy with HR-deficient tumors; suppress HIF-1α | Trastuzumab deruxtecan [116] |
| DNA alkylating agents | Pyrrolobenzodiazepines, Calicheamicin | Cause DNA double-strand breaks, overcome repair mechanisms | Potent against quiescent CSCs; bystander effect | Approved for hematologic malignancies [116] |
Technical Protocol for ADC Evaluation Against CSCs
ADC Internalization and Payload Release Assay
Methodology:
- ADC Labeling: Conjugate pH-sensitive fluorophore (e.g., pHrodo Red) to ADC using amine-reactive chemistry
- CSC Culture: Seed CSC-enriched tumor spheres in 96-well imaging plates
- Treatment: Incubate with labeled ADC (1-10 μg/mL) for 0-24 hours
- Live-cell Imaging: Monitor internalization via fluorescence increase in acidic compartments (pH<6.0)
- Payload Detection: Fix cells at timepoints, immunostain for payload with specific antibodies
- Correlation Analysis: Quantify relationship between internalization kinetics and cytotoxic effect [116]
ADC Bystander Killing Effect on Heterogeneous CSC Populations
Diagram Title: ADC Bystander Killing Mechanism
Cancer Vaccines Targeting CSC Antigens
Principles and Approaches
Cancer vaccines designed to target CSCs aim to generate de novo or boost existing immune responses against CSC-associated antigens, potentially providing long-term immunological control against tumor recurrence and metastasis [117]. Unlike CAR-T cells and ADCs which are passive immunotherapies, cancer vaccines actively engage the host immune system to develop sustained anti-tumor memory.
CSC-targeted vaccines face unique challenges including:
- Immune tolerance: Many CSC antigens are self-antigens also expressed on normal stem cells
- Immunosuppressive TME: CSCs create an inhibitory microenvironment through cytokine secretion
- Antigenic heterogeneity: CSC populations exhibit dynamic marker expression [8]
- Limited T-cell infiltration: Physical and chemical barriers prevent immune cell access to CSC niches [117]
CSC Vaccine Platforms and Antigen Selection Strategies
Table 3: CSC-Targeted Vaccine Platforms
| Vaccine Platform | Composition | Advantages | Challenges | Development Status |
|---|---|---|---|---|
| Dendritic cell vaccines | Autologous DCs loaded with CSC antigen peptides | Potent antigen presentation; personalized approach | Logistically complex; requires patient-specific manufacturing | Phase I/II trials for glioblastoma, AML [117] |
| mRNA vaccines | Lipid nanoparticle-formulated mRNA encoding CSC antigens | Rapid development; endogenous antigen production | Delivery efficiency; potential inflammatory reactions | Preclinical development for multiple solid tumors [117] |
| Viral vector vaccines | Recombinant viruses expressing CSC antigens | Strong immunogenicity; versatile antigen capacity | Pre-existing immunity; safety concerns | Preclinical evaluation [117] |
| Whole-cell vaccines | Irradiated CSCs with or without genetic modification | Broad antigen repertoire; no need for antigen identification | Potential autoimmunity; standardization difficulties | Phase I trials in various malignancies [117] |
Technical Protocol for CSC Vaccine Development
CSC Neoantigen Discovery Pipeline
Methodology for Identification of CSC-Specific Neoantigens:
- CSC Isolation: FACS-sort CSCs based on established markers (e.g., CD44+CD133+ for solid tumors)
- Whole Exome Sequencing: Sequence CSC and non-CSC populations from same tumor
- RNA Sequencing: Identify expressed mutations in CSC population
- HLA Ligand Prediction:
- Use netMHCpan (v4.0) to predict HLA class I binding affinity
- Apply MHCflurry for peptide-HLA stability predictions
- Filter for strong binders (IC50 < 50nM)
- Immunogenicity Validation:
Research Reagent Solutions for CSC-Targeted Therapy Development
Table 4: Essential Research Reagents for CSC-Targeted Therapy Development
| Reagent Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| CSC surface markers | Anti-CD133, Anti-CD44, Anti-ALDH1A1, Anti-EpCAM | Identification and isolation of CSC populations | Validate specificity for each cancer type; account for heterogeneity [8] [9] |
| CSC functional assay reagents | Matrigel, EGF, bFGF, B27 supplement | Tumor sphere formation assays | Use ultra-low attachment plates; optimize growth factor concentrations [8] |
| CAR construction reagents | Lentiviral/retroviral vectors, scFv sequences, Transfection reagents | CAR-T cell engineering | Monitor transduction efficiency; validate CAR surface expression [113] [112] |
| ADC linker-payload systems | Valine-citrulline (vc) linker, SMCC linker, MMAE, DM1, Deruxtecan | ADC assembly and testing | Optimize drug-antibody ratio (DAR 3-4 ideal); validate stability [116] |
| Vaccine adjuvants | Poly(I:C), CpG ODN, GM-CSF | Enhance immunogenicity of CSC vaccines | Test different combinations for optimal T-cell activation [117] |
| TME modeling components | Cancer-associated fibroblast lines, M2 macrophage conditioned media | 3D co-culture systems for therapy testing | Represents immunosuppressive TME; more predictive than monoculture [5] |
The therapeutic targeting of cancer stem cells represents a paradigm shift in oncology, moving beyond bulk tumor reduction to address the fundamental cells driving tumor recurrence and therapeutic resistance. CAR-T cells, ADCs, and cancer vaccines each offer distinct advantages and face unique challenges in eradicating CSCs. CAR-T cells provide potent, specific cytotoxicity but face barriers related to TME suppression and antigen escape. ADCs deliver highly potent payloads directly to CSCs but require careful management of on-target, off-tumor toxicity. Cancer vaccines offer potential for long-term immune control but must overcome immune tolerance to CSC-associated antigens.
Future directions in CSC-targeted therapy will likely focus on:
- Multi-antigen targeting to address CSC heterogeneity and plasticity
- Rational combination therapies that simultaneously target CSCs and the immunosuppressive TME
- Advanced delivery systems including localized delivery for solid tumors [114] [115]
- Biomarker-driven patient selection based on comprehensive CSC profiling
- Next-generation engineering including logic-gated CARs [114], conditionally active antibodies, and novel ADC linker chemistry
The integration of single-cell technologies, functional genomics, and artificial intelligence in CSC research will accelerate the identification of novel therapeutic targets and resistance mechanisms. As these advanced therapeutic modalities progress through clinical development, they hold the promise of transforming cancer into a more manageable chronic disease or achieving durable cures by addressing the root cellular drivers of malignancy.
The persistence of minimal residual disease (MRD) following curative-intent therapy is a primary cause of cancer recurrence, driven by resistant cell populations such as cancer stem cells (CSCs). This whitepaper examines the integration of circulating tumor DNA (ctDNA) analysis for MRD detection into clinical trial frameworks. We detail how ctDNA assays enable ultra-sensitive monitoring of molecular relapse and facilitate adaptive trial designs that dynamically escalate or de-escalate therapy based on MRD status. Furthermore, we explore the critical intersection between MRD and CSCs, whose plasticity, immune evasion capabilities, and dormancy contribute to treatment resistance and metastatic regrowth. By synthesizing current methodologies, clinical evidence, and emerging strategies, this guide provides a roadmap for developing trials that concurrently target MRD and the CSC niche, aiming to overcome therapeutic resistance and improve long-term patient survival.
The clinical challenge of cancer recurrence after ostensibly successful treatment is fundamentally linked to two interconnected biological phenomena: MRD and CSCs. Minimal Residual Disease (MRD) refers to the presence of cancer cells that survive therapy at levels undetectable by conventional radiographic imaging or clinical examination [118]. These residual cells can eventually lead to relapse. A key driver of MRD persistence and its clinical consequences is the Cancer Stem Cell (CSC) population. CSCs are a subpopulation of tumor cells characterized by self-renewal capacity, differentiation potential, enhanced survival mechanisms, and resistance to conventional therapies [5] [2]. Their ability to remain in a quiescent or slow-cycling state allows them to evade treatments targeting rapidly dividing cells, making them a primary reservoir for MRD [5] [2].
The detection of MRD has been revolutionized by liquid biopsy technologies, particularly the analysis of circulating tumor DNA (ctDNA), which are fragments of tumor-derived DNA found in the bloodstream. The presence of ctDNA after curative-intent therapy provides a direct molecular biomarker for MRD and is strongly prognostic for recurrence [119] [120] [121]. The biological connection is clear: CSCs, through their role in driving tumor initiation and their therapy-resistant nature, contribute significantly to the MRD state. Consequently, modern clinical trial designs must account for both the measurable signal of MRD (via ctDNA) and the biological driver (CSCs) to effectively prevent recurrence and improve patient outcomes.
Current ctDNA Assay Technologies for MRD Detection
The core of MRD-driven trials is the sensitive and specific detection of ctDNA. Current technologies can be broadly classified into tumor-informed and tumor-naïve (or "plasma-only") assays, each with distinct methodologies, sensitivities, and use-cases.
Tumor-informed assays require sequencing of the patient's tumor tissue (e.g., via whole-exome or whole-genome sequencing) to identify a set of patient-specific somatic mutations (typically 16-48 variants). A custom panel is then designed to track these specific mutations in serial plasma samples via ultra-deep sequencing. This personalized approach generally achieves higher sensitivity for MRD detection because it focuses the sequencing effort on known, clonal tumor variants [120].
Tumor-naïve assays, in contrast, use a fixed panel of genes commonly mutated in cancer and do not require prior tumor sequencing. While more convenient and offering a faster turnaround time, their sensitivity can be lower, especially in early-stage disease where ctDNA levels are minimal [120].
The following table summarizes the key characteristics of leading ctDNA-MRD detection assays:
Table 1: Comparison of ctDNA-Based MRD Detection Assays
| Assay Name | Type | Methodological Principle | Reported Sensitivity (VAF) |
|---|---|---|---|
| Signatera (Natera) | Tumor-informed | Whole-exome sequencing of tumor to design a custom panel (16 clonal variants) for multiplex PCR and deep sequencing of plasma. | ~0.01% [120] |
| RaDaR (Inivata/NeoGenomics) | Tumor-informed | Whole-genome sequencing of tumor to select up to 48 tumor-specific mutations, followed by ultra-deep amplicon sequencing of plasma. | ~0.001% [120] |
| PhasED-Seq (Foresight Diagnostics) | Tumor-informed | Detection of multiple mutations on a single DNA fragment (phased variants), significantly reducing error rates compared to single-mutation methods. | ~0.0001% [120] |
| Guardant Reveal (Guardant Health) | Tumor-naïve | Combines targeted sequencing of a fixed ~500 kb cancer gene panel with analysis of abnormal methylation patterns in plasma. | ~0.01% [120] |
| CAPP-Seq | Tumor-informed or Tumor-naïve | Hybrid-capture NGS targeting a panel of common cancer genes (e.g., 100-200 genes in NSCLC) with error suppression. | ~0.003% [120] |
Abbreviations: VAF, Variant Allele Frequency; NGS, Next-Generation Sequencing; PCR, Polymerase Chain Reaction. The choice of assay impacts trial design, with tumor-informed assays being preferred for their high sensitivity in the adjuvant setting, where ctDNA burden is extremely low.
Experimental Protocol for ctDNA-Based MRD Monitoring
A standardized protocol for longitudinal MRD monitoring in clinical trials is critical for data consistency. The following workflow, derived from current best practices, outlines the key steps [120] [121]:
- Pre-Treatment Baseline Collection: Collect and biobank:
- Tumor Tissue: Formalin-fixed paraffin-embedded (FFPE) block or fresh frozen tissue from primary tumor or metastasis.
- Germline Control: Peripheral blood mononuclear cells (PBMCs) or oral swab (buccal) samples to filter out germline variants and clonal hematopoiesis of indeterminate potential (CHIP)-related mutations.
- Pre-treatment Plasma: Baseline blood sample for ctDNA analysis.
- Tumor Sequencing & Panel Design (For Tumor-Informed Assays):
- Extract genomic DNA from tumor and germline control samples.
- Perform whole-exome sequencing (WES) or whole-genome sequencing (WGS) on both.
- Identify somatic mutations (SNVs, INDELs) by comparing tumor and germline sequences.
- Select 16-48 high-confidence, clonal mutations to create a patient-specific tracking panel.
- Longitudinal Plasma Collection and Processing:
- Collect peripheral blood (typically 8-10 mL) in specialized cell-free DNA blood collection tubes (e.g., Streck) at predefined timepoints (e.g., post-operatively, post-adjuvant therapy, during surveillance).
- Process plasma within 48-72 hours by double centrifugation to isolate platelet-poor plasma.
- Extract cell-free DNA (cfDNA) using validated commercial kits (e.g., QIAamp Circulating Nucleic Acid Kit).
- Library Preparation and Sequencing:
- Prepare sequencing libraries from cfDNA (e.g., using KAPA HyperPrep Kit).
- For tumor-informed assays, perform multiplex PCR amplification of the patient-specific variants.
- For tumor-naïve assays, use hybrid-capture-based enrichment with the fixed gene panel.
- Sequence using high-throughput NGS platforms (e.g., Illumina NovaSeq) to achieve high depth (often >50,000x coverage for cfDNA).
- Bioinformatic Analysis and MRD Calling:
- Align sequencing reads to the reference genome (e.g., hg19).
- Call variants using specialized algorithms (e.g., VarScan2) and filter against the germline control and population databases.
- For tumor-informed assays, MRD positivity is called when a predefined number of patient-specific mutations are detected above a noise threshold.
- For tumor-naïve assays, MRD is called based on the detection of one or more somatic mutations in the predefined gene panel.
- ctDNA burden can be quantified as mean variant allele frequency (VAF) or as haploid genomic equivalents per milliliter of plasma (hGE/mL) [121].
Diagram 1: ctDNA MRD Detection Workflow. This diagram outlines the core steps for detecting Minimal Residual Disease using circulating tumor DNA, highlighting parallel paths for tumor-informed and tumor-naïve assays.
Clinical Trial Designs Incorporating ctDNA and MRD
The integration of ctDNA analysis is transforming clinical trials from static, population-based designs to dynamic, patient-specific paradigms. The table below summarizes the core design models.
Table 2: Models for ctDNA-Guided Clinical Trial Designs
| Trial Model | Primary Objective | Key Features | Example Trial |
|---|---|---|---|
| MRD-Guided Adjuvant Escalation | Determine if therapy escalation for ctDNA+ patients post-surgery improves outcomes. | Patients with detectable ctDNA after curative-intent surgery are randomized to standard vs. intensified therapy. | DYNAMIC-III (Colon Cancer): ctDNA+ patients randomized to doublet (FOLFOX) vs. triplet (FOLFOXIRI) chemotherapy. [119] |
| MRD-Guided Adjuvant De-escalation | Determine if therapy can be safely omitted for ctDNA- patients post-surgery. | Patients with undetectable ctDNA after surgery are randomized to standard adjuvant therapy vs. active surveillance. | CIRCULATE-North America (Colon Cancer): ctDNA- patients after surgery are randomized to standard chemo vs. serial ctDNA monitoring alone. [118] |
| MRD-Directed Adaptive Therapy | Evaluate if switching therapies based on emerging ctDNA resistance mutations improves outcomes. | Patients on maintenance therapy are monitored for specific ctDNA mutations, prompting a pre-emptive switch to a targeted therapy. | SERENA-6 (Breast Cancer): Patients on AI + CDK4/6i switched to camizestrant (SERD) upon detection of ESR1 mutations, improving PFS. [119] |
| Novel Agents in MRD+ Setting | Test efficacy of novel therapies (immunotherapies, targeted agents) specifically in the MRD+ population. | Patients who are ctDNA+ after standard therapy with no radiographic disease receive an investigational agent. | ACT3 (Colon Cancer): ctDNA+ patients after chemo receive biomarker-directed therapy (e.g., Nivolumab for MSI-H) or FOLFIRI vs. surveillance. [118] |
These designs address the "one-size-fits-all" limitation of traditional adjuvant therapy. The SERENA-6 trial, presented at ASCO 2025, is a landmark demonstration of clinical utility, showing that switching therapy based on molecular progression (ctDNA ESR1 mutation) before radiographic progression significantly improved progression-free survival (PFS) and quality of life (QoL) in advanced breast cancer [119]. Conversely, the DYNAMIC-III trial in stage III colon cancer highlighted a current challenge: while ctDNA status was prognostic, treatment escalation in ctDNA+ patients did not improve recurrence-free survival, suggesting that simply intensifying conventional chemotherapy may be insufficient and that novel approaches are needed [119]. This is precisely where targeting CSCs becomes relevant.
The Crucial Intersection: CSC Biology and MRD
Cancer Stem Cells are implicated as key mediators of MRD persistence and eventual relapse. Their biological properties directly align with the clinical behavior of MRD.
- Therapy Resistance and Dormancy: CSCs possess potent mechanisms of resistance, including enhanced DNA repair, expression of drug efflux pumps, and a shift to quiescence, allowing them to survive conventional chemo- and radiotherapy that constitutes standard adjuvant treatment [5] [2]. This quiescent state is a fundamental characteristic of the residual cells that constitute MRD.
- CSC Plasticity and Heterogeneity: The CSC state is dynamic, not fixed. Non-CSCs can dedifferentiate into CSCs in response to environmental stimuli like therapy or hypoxia, a process known as CSC plasticity [5] [8] [2]. This complicates eradication, as even if the CSC population is initially reduced, it can be replenished. Furthermore, multiple CSC subpopulations, defined by different markers (e.g., p75NTR, ALDH1A1, CD44), can co-exist within a single tumor, each potentially contributing to different clinical outcomes such as metastasis or local recurrence [8].
- Immune Evasion: CSCs employ multiple intrinsic mechanisms to evade immune surveillance, which is critical for their survival as MRD. These include:
- Upregulation of Immune Checkpoints: CSCs in various cancers show high expression of PD-L1, CD47 ("don't eat me" signal), and CD24, which inhibit T-cell and macrophage activity [2].
- Low Antigen Presentation: Downregulation of MHC class I molecules makes CSCs less visible to cytotoxic T cells [2].
- Immunosuppressive Niche: CSCs recruit regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs), creating a protective local microenvironment that shields them from immune attack [2].
These properties make CSCs a resilient reservoir for MRD. Therefore, the mere detection of ctDNA (MRD) after therapy may signal the persistence of a CSC-enriched population, arguing for trial designs that specifically target CSC vulnerabilities.
Targeting CSC Vulnerabilities in MRD-Driven Trials
Future clinical trials must integrate strategies to target CSCs alongside ctDNA monitoring to achieve durable cures. The following table outlines key therapeutic approaches and their connection to CSC biology.
Table 3: Strategies for Targeting Cancer Stem Cells in Clinical Trials
| Therapeutic Strategy | Molecular Target / Agent Class | Rationale in CSC Biology | Trial Design Consideration |
|---|---|---|---|
| Differentiation Therapy | Retinoic acid pathway agonists; BMP signaling inducers. | Forces CSCs to exit their self-renewing, quiescent state and differentiate into therapy-sensitive progeny. | Combine with conventional chemotherapy in MRD+ patients; use ctDNA clearance as an early efficacy endpoint. |
| Immune Evasion Blockade | Anti-CD47 antibodies; CSC marker-directed CAR-T/NK cells (e.g., TROP2-CAR-NK). | Overcomes "don't eat me" signals and directs immune effector cells to specifically recognize and eliminate CSCs. | Ideal for MRD+ trials post-chemo; monitor for CSC-specific ctDNA mutations as biomarkers of resistance. |
| Niche Disruption | Anti-CSF1R antibodies (e.g., AMB-05X); CXCR4 inhibitors. | Depletes tumor-associated macrophages or disrupts CSC-stromal interactions that maintain stemness and immune privilege. | Test in MRD+ setting to eliminate the protective microenvironment; correlate with changes in ctDNA levels. |
| Metabolic Inhibition | Dual OXPHOS/glycolysis inhibitors; glutamine antagonists. | Targets the metabolic plasticity of CSCs, which can switch between energy pathways to survive stress. | Use in combination regimens for MRD+ disease; challenging due to potential toxicity to normal stem cells. |
| Epigenetic Modulation | EZH2 inhibitors; BET bromodomain inhibitors. | Reverses epigenetic programs that maintain stemness and plasticity. | Can reverse immune exclusion; trial designs should include pre- and post-treatment biopsies to assess CSC frequency. |
Several ongoing trials are pioneering this integrated approach. The ACT3 trial for stage III colon cancer uses ctDNA to identify high-risk patients and then assigns them to biomarker-directed therapies, a strategy that could indirectly target CSCs dependent on specific pathways [118]. A phase II trial of AMB-05X (an anti-CSF1R antibody) in ctDNA+ colorectal cancer patients aims to modulate the tumor microenvironment and enhance T-cell infiltration, potentially disrupting the CSC niche [118]. Another trial employs RO7198457, a personalized mRNA neoantigen vaccine, to stimulate an immune response against tumor cells in ctDNA+ patients, which could potentially target CSCs presenting neoantigens [118]. Finally, a phase I study is investigating TROP2-CAR-NK cells combined with cetuximab in CRC patients with MRD, directly engaging the immune system to eliminate residual disease, which may include CSCs expressing TROP2 [118].
The Scientist's Toolkit: Key Reagents for CSC and MRD Research
Table 4: Essential Research Reagents for Investigating CSCs and MRD
| Reagent / Tool | Function / Target | Application in Experimental Protocols |
|---|---|---|
| Streck Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells for up to 14 days, preventing genomic DNA contamination and preserving cfDNA profile. | Essential for reproducible pre-analytical collection of plasma for ctDNA-based MRD detection in multi-center trials. [121] |
| Anti-p75NTR & Anti-ALDH1A1 Antibodies | Cell surface and intracellular markers for isolating and studying CSC subpopulations via FACS/IHC. | Used in multiplex IHC and FACS to identify, quantify, and isolate distinct CSC populations from tumor tissues and cell lines. [8] |
| QIAamp Circulating Nucleic Acid Kit | Silica-membrane-based spin column technology for the efficient purification of cfDNA from plasma. | Standardized extraction of high-quality cfDNA from patient plasma samples prior to NGS library construction. [121] |
| KAPA HyperPrep Kit | Enzymatic fragmentation and library construction for NGS from low-input and degraded DNA samples like cfDNA and FFPE-derived DNA. | Preparation of sequencing-ready libraries from cfDNA for both tumor-informed and tumor-naïve MRD assays. [121] |
| Hemasalus Panel (475 genes) | Targeted NGS panel covering genes frequently mutated in hematopoietic and lymphoid neoplasms. | Used in research to sequence tumor gDNA and plasma cfDNA for mutation identification and MRD tracking in liquid biopsies. [121] |
The integration of ctDNA-based MRD detection into clinical trial design represents a paradigm shift towards personalized, dynamic cancer care. These assays provide an unprecedented window into the molecular trajectory of a patient's disease, enabling early intervention and rational therapy escalation or de-escalation. However, as the DYNAMIC-III trial suggests, detecting MRD is only the first step; the next, more critical challenge is effectively eliminating it.
Success in this endeavor requires a deep integration of CSC biology into trial strategy. The resilient, immune-evasive, and plastic nature of CSCs likely underpins much of the MRD that ctDNA detects. Future trials must therefore move beyond simply intensifying conventional chemotherapy and instead incorporate novel agents—differentiation inducers, immune niche modulators, and targeted cellular therapies—designed to vulnerabilities specific to the CSC state. The convergence of highly sensitive ctDNA monitoring for patient stratification and CSC-targeted therapies for intervention holds the greatest promise for overcoming therapeutic resistance, preventing relapse, and ultimately achieving long-term remissions for cancer patients.
Conclusion
The precise identification of cancer stem cells remains a formidable challenge due to marker heterogeneity, plasticity, and the dynamic interplay with the tumor microenvironment. However, the integration of advanced technologies like single-cell multi-omics, genome-wide functional screens, and AI-driven spatial analysis is rapidly refining our understanding of CSC biology. Moving forward, the clinical translation of this knowledge hinges on the development of robust, validated biomarker panels and the design of innovative clinical trials that effectively target the CSC population. The future of oncology lies in combinatorial strategies that pair conventional therapies with novel CSC-targeting agents—such as next-generation immunotherapies and signaling pathway inhibitors—to overcome therapeutic resistance, prevent relapse, and ultimately improve patient outcomes through personalized medicine approaches.
References
- 1. The Cancer Stem Cell Niche - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4355577/]
- 2. Cancer stem cells and niches: challenges in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02265-2]
- 3. Exploring the dynamic interplay between cancer stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10546755/]
- 4. Cross-talk between cancer stem cells and immune cells [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01748-4]
- 5. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 6. Composition and functional state of T and NK cells in the ... [https://pubmed.ncbi.nlm.nih.gov/41236394/]
- 7. Predicting the tumor microenvironment composition and ... [https://www.nature.com/articles/s41698-024-00765-w]
- 8. Identification of Phenotypically Distinct Cancer Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606748/]
- 9. Cancer Stem Cell markers: Symphonic masters of ... [https://www.sciencedirect.com/science/article/pii/S0024320524006052]
- 10. Tumor microenvironment as niche constructed by cancer ... [https://www.sciencedirect.com/science/article/pii/S2090123224002510]
- 11. Cancer stem cells in personalized therapy [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1619597/full]
- 12. Cancer Stem Cells—Origins and Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC7426526/]
- 13. Biology of stem cell paradox: a double-edged sword ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03981-x]
- 14. The Relevance of Transcription Factors in Gastric and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00442/full]
- 15. Expression profile of cancer stem cell markers SOX2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550392/]
- 16. SALL4, the missing link between stem cells, development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4823161/]
- 17. Correlation of Cancer Stem-Cell Markers OCT4, SOX2, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5725361/]
- 18. Core transcription factors, Oct4, Sox2 and Nanog ... [https://www.aging-us.com/article/100222/text]
- 19. Cancer Stem Cell Research: A New Frontier in the Fight ... [https://www.jons-online.com/interview-with-the-innovators/cancer-stem-cell-research-a-new-frontier-in-the-fight-against-cancer]
- 20. Cancer stem cells as a biomarker – A mini review [https://www.probiologists.com/article/cancer-stem-cells-as-a-biomarker-a-mini-review]
- 21. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 22. Expression of CD44 and Its Correlation With ... [https://pubmed.ncbi.nlm.nih.gov/40291275/]
- 23. CD44 on cancer stem cell is a potential immunological and ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03748-4]
- 24. Combined Detection of Tumor Stem Cell Markers CD133 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456660/]
- 25. A Validation Study of CD133 as a Reliable Marker for ... [https://link.springer.com/article/10.1007/s10517-024-06026-x]
- 26. Identification of ALDH-Expressing Cancer Stem Cells ... [https://www.stemcell.com/identification-aldh-expressing-cancer-stem-cells-using-aldefluor-lp.html]
- 27. PET-leveraged ALDH probe toward cancer stem cells [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb01253h]
- 28. Inhibition of ICAM1 diminishes stemness and enhances ... [https://www.nature.com/articles/s41467-025-63796-2]
- 29. ICAM1-Mediated Endothelial Cells and Macrophage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596846/]
- 30. Biology of stem cell paradox: a double-edged sword ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560468/]
- 31. Cancer Stem Cell markers: Symphonic masters of chemoresistance ... [https://pubmed.ncbi.nlm.nih.gov/39182567/]
- 32. Frontiers | Targeting CSC- immune cell crosstalk to overcome... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1620807/full]
- 33. A comprehensive overview of ovarian cancer stem cells: correlation... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02345-3]
- 34. Decoding the role of cancer stem cells in digestive tract tumors... [https://www.spandidos-publications.com/10.3892/ijo.2025.5767]
- 35. Pharmacological modulation of stem cells signaling ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 36. Molecular mechanisms and signaling pathways related to ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1585668/full]
- 37. Cancer stem cells: advances in knowledge and ... - Nature [https://www.nature.com/articles/s41392-024-01851-y]
- 38. FACS Sorting: What Is Fluorescence-Activated Cell Sorting? [https://www.akadeum.com/technology/facs-fluorescence-activated-cell-sorting/?srsltid=AfmBOoqWziK80XNJmZjtVldZ39yOCYEcqOtW4fqNzQIo8yFacJMBn6q9]
- 39. Magnetic Activated Cell Sorting: Principle of MACS... [https://www.akadeum.com/technology/macs-magnetic-activated-cell-sorting/?srsltid=AfmBOor15xuhUQqAw__UOeC3TlRds1zZAmGkZJ6SLxiTlLUASN1pW6Ki]
- 40. What You Have to Know about Magnetic-activated Cell ... [https://www.cd-bioparticles.com/blog/applications/what-you-have-to-know-about-magnetic-activated-cell-sorting/]
- 41. MACS vs. FACS vs. BACS™: The Advantages of BACS™ [https://www.akadeum.com/blog/macs-vs-facs-vs-bacs/?srsltid=AfmBOooIo09m7C-SOLObA4QuobdTIeN3q_85wMrsXwEA-29sJ3G73ok-]
- 42. Sorting out the difference between FACS and MACS [https://www.bostonind.com/blog/Sorting-out-the-difference-between-FACS-and-MACS?srsltid=AfmBOopwb6u9INghA-NBzvAUdQcnX9d74xEREYx4k-5CIJtmr5KybfhA]
- 43. Magnetic cell sorting and flow cytometry sorting methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2789528/]
- 44. Identification of Cancer Stem Cell Molecular Markers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6521292/]
- 45. Serial Xenotransplantation in NSG Mice Promotes a Hybrid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7016569/]
- 46. New Opportunities and Challenges to Defeat Cancer Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5958547/]
- 47. High-Throughput Single-Cell Derived Sphere Formation for ... [https://www.nature.com/articles/srep27301]
- 48. Eyes Wide Open: A Critical Review of Sphere-Formation as an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3633588/]
- 49. Early Prediction of Single-cell Derived Sphere Formation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9552208/]
- 50. Eyes Wide Open: A Critical Review of Sphere-Formation ... [https://www.sciencedirect.com/science/article/pii/S193459091100172X]
- 51. New Advances and Challenges of Targeting Cancer Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5833988/]
- 52. Leveraging Single-Cell RNA-seq Data to Uncover ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7982650/]
- 53. Single‐cell RNA sequencing in cancer research [https://jeccr.biomedcentral.com/articles/10.1186/s13046-021-01874-1]
- 54. Leveraging Public scRNA-seq Data: A Guide to ... [https://www.biomage.net/blog/public-scrna-seq-data]
- 55. High-throughput single-сell sequencing in cancer research [https://www.nature.com/articles/s41392-022-00990-4]
- 56. Evaluation of single-cell RNAseq labelling algorithms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9851326/]
- 57. Integration of single-cell sequencing and bulk RNA-seq to ... [https://www.nature.com/articles/s41598-024-62913-3]
- 58. Identification of a Cancer Stem Cell-Related Gene ... [https://www.mdpi.com/1422-0067/26/7/2933]
- 59. Identification of Cancer Stem Cell (CSC)-Associated Genes ... [https://www.mdpi.com/2227-9709/11/4/95]
- 60. Single-cell sequencing technology applied to epigenetics for ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-023-01574-x]
- 61. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02426-3]
- 62. Identification of malignant cells in single ... [https://www.nature.com/articles/s42003-025-08695-4]
- 63. Single-Cell Analysis of the Transcriptome and Epigenome [https://pmc.ncbi.nlm.nih.gov/articles/PMC9352558/]
- 64. Single-Cell Transcriptomic Approaches for Decoding Non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932299/]
- 65. Expression of cancer stem cell markers and their ... [https://pubmed.ncbi.nlm.nih.gov/41025099/]
- 66. Expression of cancer stem cell markers and their prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476815/]
- 67. Combined Detection of Tumor Stem Cell Markers CD133 ... [https://pubmed.ncbi.nlm.nih.gov/40995538/]
- 68. Co-expression of Stem Cell Markers CD133 and CD44 as ... [https://turkjsurg.com/articles/co-expression-of-stem-cell-markers-cd133-and-cd44-as-predictors-of-metastatic-potential-of-colorectal-carcinoma/doi/turkjsurg.2025.6837]
- 69. Clinicopathological and Prognostic Significance of Cancer ... [https://pubmed.ncbi.nlm.nih.gov/40473997/]
- 70. Liver cancer stem cells as novel diagnostic biomarkers [https://www.sciencedirect.com/science/article/pii/S0009898125006187]
- 71. Unveiling cancer stem cell marker networks: A hypergraph ... [https://www.sciencedirect.com/science/article/abs/pii/S1476927125003457]
- 72. Cancer stem cells: understanding tumor hierarchy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5599210/]
- 73. Intra-tumor heterogeneity from a cancer stem cell perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC5314464/]
- 74. Characterization of normal and cancer stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5410217/]
- 75. Cancer Stem Cell Plasticity – A Deadly Deal - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7203492/]
- 76. Advancing Cancer Biology: Highlights from the 2025 FASEB ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599846/]
- 77. Cancer Cell Plasticity: Rapid Reversal of Chemosensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5444977/]
- 78. Cancer cell plasticity and therapeutic resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465352/]
- 79. A live single-cell reporter system reveals drug-induced ... [https://www.nature.com/articles/s41598-024-73581-8]
- 80. The Different Mechanisms of Cancer Drug Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC5651054/]
- 81. Molecular mechanisms of tumor resistance to radiotherapy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01801-2]
- 82. Cancer stem cells in focus: Deciphering the dynamic ... [https://www.sciencedirect.com/science/article/pii/S0304419X25001829]
- 83. Unveiling the mechanisms and challenges of cancer drug ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01302-1]
- 84. EMT and cancer stem cells: Drivers of therapy resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764625000792]
- 85. Nanomaterials targeting cancer stem cells to overcome drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178904/]
- 86. The controversial role of senescence-associated secretory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595836/]
- 87. Cellular senescence in cancer: from mechanism paradoxes to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333312/]
- 88. Cellular senescence and SASP in tumor progression and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02096-7]
- 89. Persistent accumulation of therapy-induced senescent cells [https://www.nature.com/articles/s41368-025-00380-w]
- 90. Identification of Phenotypically Distinct Cancer Stem Cell ... [https://www.mdpi.com/2072-6694/17/21/3547]
- 91. Pan-cancer landscape of cellular senescence ... [https://www.nature.com/articles/s41598-025-23412-1]
- 92. Are There Specific Cancer Stem Cell Markers? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9872977/]
- 93. From ex vivo to in vitro models: towards a novel approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12052970/]
- 94. Human-based complex in vitro models: their promise and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1526306/full]
- 95. CRISPR Screens: Approaches, Strategies, and Workflow [https://www.synthego.com/guide/crispr-methods/crispr-screen/]
- 96. Bioinformatics approaches to analyzing CRISPR screen data [https://pmc.ncbi.nlm.nih.gov/articles/PMC10019185/]
- 97. How to Analyze CRISPR Screen Data to Find Targets? [https://www.ubigene.us/application/crispr-screen-analysis.html]
- 98. Genome-wide CRISPR screens identify critical targets to ... [https://pubmed.ncbi.nlm.nih.gov/40845844/]
- 99. Identification of new biomarkers of hepatic cancer stem ... [https://www.e-jlc.org/journal/view.php?number=593]
- 100. CMN Weekly (26 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-26-september-2025-your-weekly-crispr-medicine-news/]
- 101. Cancer Stem Cells in Hematopoietic Malignancies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2330330/]
- 102. Cancer stem cell surface markers on normal stem cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5498139/]
- 103. Characterization of stem cell landscape and assessing the ... [https://www.nature.com/articles/s41598-024-74806-6]
- 104. A practical guide for choosing an optimal spatial ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11235-3]
- 105. Deciphering normal and cancer stem cell niches by spatial ... [https://pubmed.ncbi.nlm.nih.gov/39496456/]
- 106. Scaling up spatial transcriptomics for large-sized tissues [https://www.nature.com/articles/s41592-025-02770-8]
- 107. Unique Stanford Medicine-designed AI predicts cancer ... [https://med.stanford.edu/news/all-news/2025/01/ai-cancer-prognosis.html]
- 108. AI tool gives pathologists speed, accuracy and a new way to ... [https://med.stanford.edu/news/all-news/2025/09/ai-tool-pathology.html]
- 109. Digital Pathology and AI Highlights from ASCO 2025 [https://proscia.com/digital-pathology-and-ai-highlights-from-asco-2025/]
- 110. Use of AI Histopathology in Breast Cancer Diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565969/]
- 111. Targeting cancer stem cells with CAR-based immunotherapy: biology, evidence, and future directions | Cancer Cell International | Full Text [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03846-3]
- 112. Cancer stem cell-targeted chimeric antigen receptor (CAR) [https://pmc.ncbi.nlm.nih.gov/articles/PMC8343118/]
- 113. Chimeric Antigen Receptor T-Cells: An Overview of Concepts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9256991/]
- 114. Emerging advances in CAR-T therapy for solid tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628604/]
- 115. latest clinical trial updates from 2025 ASCO annual meeting [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01760-9]
- 116. The evolving landscape of antibody-drug conjugates ... [https://www.nature.com/articles/s41698-025-01131-0]
- 117. Next-generation immunotherapeutic approaches for blood cancers: Exploring the efficacy of CAR-T and cancer vaccines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12084993/]
- 118. Minimal Residual Disease (MRD) Trials [https://fightcolorectalcancer.org/blog/mrd-trials/]
- 119. Circulating tumour DNA assays in focus - Nature [https://www.nature.com/articles/s44276-025-00181-y]
- 120. A comprehensive overview of minimal residual disease in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12166047/]
- 121. Clinical implications of ctDNA-based minimal residual disease ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02438-y]