CAR-T Cell Engineering for Resistant Cancers: A 2024 Comparative Analysis of Efficacy Across Construct Designs
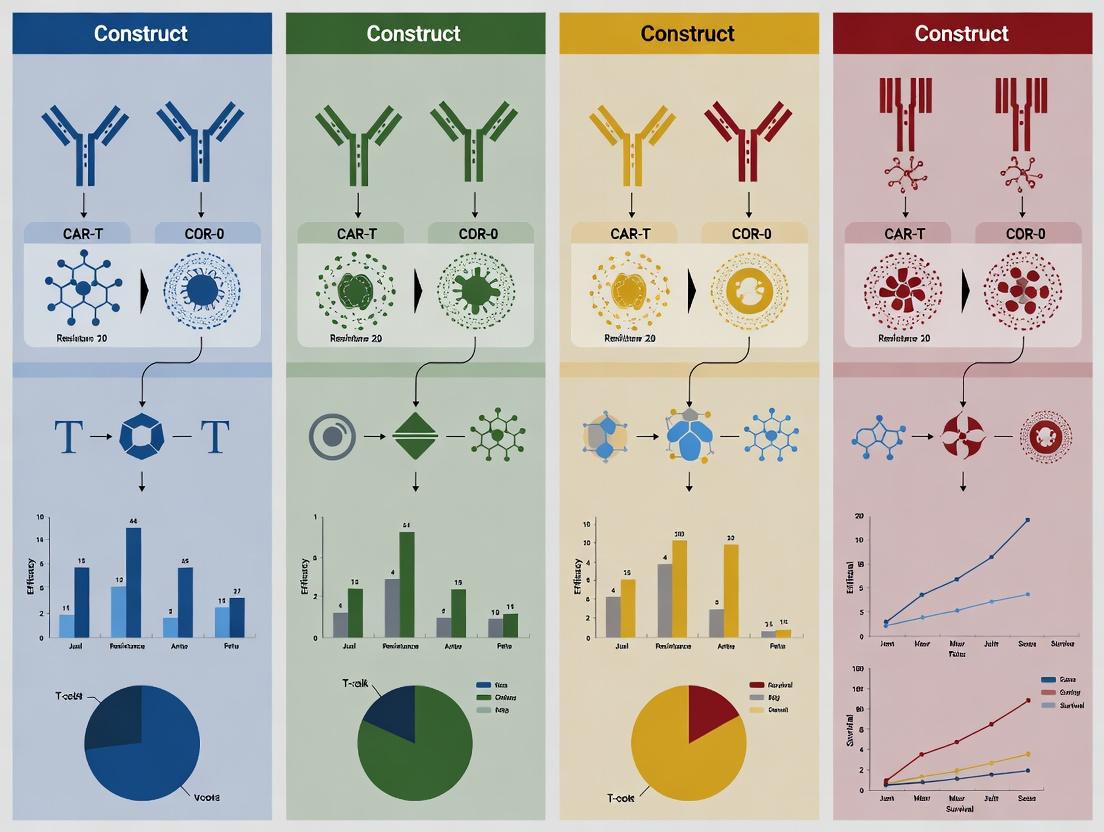
This article provides a comprehensive, comparative analysis of chimeric antigen receptor (CAR) T-cell constructs engineered to overcome treatment resistance in relapsed/refractory cancers.
CAR-T Cell Engineering for Resistant Cancers: A 2024 Comparative Analysis of Efficacy Across Construct Designs
Abstract
This article provides a comprehensive, comparative analysis of chimeric antigen receptor (CAR) T-cell constructs engineered to overcome treatment resistance in relapsed/refractory cancers. Targeting researchers and drug development professionals, we explore the foundational principles of CAR architecture—focusing on scFv domains, co-stimulatory endodomains (e.g., CD28, 4-1BB), and emerging safety switches. We detail methodological approaches for evaluating construct efficacy in preclinical and clinical settings, including in vivo models and biomarker assessment. Critical challenges such as T-cell exhaustion, antigen escape, and cytokine release syndrome are addressed with targeted optimization strategies. Finally, we present a data-driven validation framework comparing the clinical outcomes, durability, and toxicity profiles of current FDA-approved and next-generation CAR-T therapies. This synthesis aims to inform future construct design and clinical translation for resistant malignancies.
Understanding CAR-T Architecture: Core Components and Design Principles for Targeting Resistant Cancers
Efficacy Comparison of CAR-T Constructs: Key Performance Metrics
The following table summarizes recent clinical trial data comparing the efficacy of different CAR-T constructs in relapsed/refractory B-cell malignancies and multiple myeloma, where treatment resistance remains a paramount challenge.
Table 1: Efficacy of Selected CAR-T Constructs in RR B-cell Malignancies & Myeloma
| CAR-T Product (Target) | Construct Details (Co-stimulatory) | Primary Indication (RR) | ORR (%) | CR (%) | Median DOR (Months) | Key Resistance Mechanisms Observed |
|---|---|---|---|---|---|---|
| Axi-cel (CD19) | CD3ζ, CD28 | Large B-cell Lymphoma | 83 | 58 | 11.1 | Antigen loss, T-cell exhaustion |
| Tisa-cel (CD19) | CD3ζ, 4-1BB | Large B-cell Lymphoma | 52 | 40 | NR (at 12.1mos) | T-cell fitness, immunosuppressive TME |
| Brexu-cel (CD19) | CD3ζ, 4-1BB | Mantle Cell Lymphoma | 85 | 59 | NR | Early T-cell dysfunction, antigen modulation |
| Idecabtagene vicleucel (BCMA) | CD3ζ, 4-1BB | Multiple Myeloma | 73 | 33 | 11 | BCMA antigen downregulation, soluble BCMA |
| Cilta-cel (BCMA) | CD3ζ, 4-1BB | Multiple Myeloma | 98 | 83 | 22 | T-cell exhaustion phenotypes, myeloid suppression |
ORR: Overall Response Rate; CR: Complete Response; DOR: Duration of Response; NR: Not Reached; RR: Relapsed/Refractory; TME: Tumor Microenvironment.
Detailed Experimental Protocols for Efficacy & Resistance Analysis
1. Protocol for Evaluating CAR-T Cell Exhaustion & Persistence (Flow Cytometry)
- Objective: To quantify exhaustion markers (e.g., PD-1, LAG-3, TIM-3) and memory phenotypes on circulating CAR-T cells post-infusion.
- Methodology:
- Sample Collection: Peripheral blood mononuclear cells (PBMCs) are collected from patients at baseline, day +7, +14, +30, and +90 post CAR-T infusion.
- Staining: Cells are stained with viability dye, anti-CD3, anti-CD8, and a detection reagent for the CAR construct (e.g., protein L for scFv detection). Intracellular staining for transcription factors (TOX, TCF1) may follow fixation/permeabilization.
- Analysis: Samples are run on a spectral flow cytometer. Data analysis gates on live, CD3+, CAR+ T cells to determine the co-expression percentage of exhaustion markers and the ratio of effector to memory subsets.
- Interpretation: High, sustained expression of multiple inhibitory receptors correlates with poor CAR-T persistence and clinical relapse.
2. Protocol for Detecting Antigen Escape via Immunohistochemistry (IHC) & Flow Cytometry
- Objective: To confirm loss or downregulation of target antigen (e.g., CD19, BCMA) on relapsed tumor cells.
- Methodology (IHC on Bone Marrow Biopsy):
- Tissue Sectioning: Formalin-fixed, paraffin-embedded (FFPE) biopsy sections are cut at 4-5µm.
- Antigen Retrieval & Staining: Slides undergo heat-induced epitope retrieval in citrate buffer. They are incubated with primary anti-target antibody (e.g., anti-CD19) followed by a labeled polymer detection system (e.g., HRP) and DAB chromogen.
- Scoring: A pathologist scores the percentage of malignant cells with positive membrane staining. <5% positivity is often defined as antigen-loss relapse.
- Methodology (Flow Cytometry of Liquid Biopsy):
- Cell Sorting: Circulating tumor cells (CTCs) or bone marrow aspirates are stained with antibodies against the target antigen and lineage-specific markers (e.g., CD19, CD20 for B-cells; CD138 for myeloma).
- Analysis: The population of lineage+ malignant cells that are target antigen-negative/dim is quantified.
Visualizations of Key Resistance Mechanisms
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Investigating CAR-T Resistance
| Reagent / Solution | Primary Function in Research | Example Application in Resistance Studies |
|---|---|---|
| Recombinant Human Cytokines (IL-2, IL-7, IL-15) | Maintain T-cell viability and promote specific differentiation in vitro. | Used in co-culture assays to test if cytokine supplementation can reverse exhaustion phenotypes. |
| Inhibitory Ligand Recombinant Proteins (e.g., PD-L1, B7-H3) | To engage inhibitory receptors on CAR-T cells in functional assays. | Coated on plates or expressed on target cells to model immunosuppressive TME and test combo blockade. |
| Fluorochrome-conjugated Antibody Panels | Multiparametric phenotyping by flow cytometry. | Simultaneous detection of CAR, exhaustion markers (PD-1, LAG-3), memory markers (CD62L, CD45RO), and activation state (4-1BB). |
| CRISPR/Cas9 Gene Editing Systems | Knockout or knock-in specific genes in tumor or T cells. | Creating antigen-negative tumor cell lines to model escape, or knocking out exhaustion-associated genes (e.g., TOX) in CAR-Ts. |
| Multiplex Immunofluorescence (mIF) Panels | Spatial profiling of protein expression in the tumor microenvironment. | Quantifying CAR-T cell infiltration relative to immunosuppressive cells (Tregs, MDSCs) and inhibitory ligand expression on tumor cells. |
| LIVE/DEAD Fixable Viability Dyes | Distinguish live from dead cells in flow cytometry. | Critical for accurate analysis of immune cell populations in complex samples like disaggregated tumors or PBMCs. |
| Digital Droplet PCR (ddPCR) Assays | Absolute quantification of target sequences with high sensitivity. | Tracking very low levels of CAR transgene DNA in patient blood to quantify long-term persistence. |
Within the thesis on Efficacy comparison of different CAR-T constructs for resistant cancers, a detailed comparison of Chimeric Antigen Receptor (CAR) component alternatives is critical. This guide dissects and compares the performance of modular CAR domains—single-chain variable fragment (scFv), hinge, transmembrane (TM), and signaling endodomains—based on recent experimental data, to inform the design of optimal constructs for overcoming resistance.
scFv Domain: Affinity and Specificity Trade-offs
The scFv provides antigen recognition. Recent studies highlight a non-linear relationship between affinity and therapeutic efficacy.
Key Experimental Protocol (Affinity Tuning):
- Objective: Compare CAR-T cells engineered with scFvs of differing affinities (low, KD~100nM; medium, KD~10nM; high, KD~1nM) against a tumor-associated antigen (e.g., HER2, CD19).
- Method: 1) Generate CARs with identical hinge, TM, and CD3ζ/CD28 endodomains but varying scFvs. 2) Transduce primary human T cells. 3) Perform in vitro co-culture assays with target-positive tumor cells to assess cytotoxicity (real-time cell analysis) and cytokine release (multiplex ELISA). 4) Evaluate in vivo efficacy and on-target/off-tumor toxicity in xenograft mouse models with varying antigen density on normal tissues.
Table 1: Performance of CAR-T Cells with scFv of Varying Affinity
| scFv Affinity (KD) | Maximal Killing Velocity | IL-2/IFN-γ Secretion | Exhaustion Marker Upregulation (PD-1, TIM-3) | In Vivo Tumor Control (Solid Tumor Model) | Observed On-Target, Off-Tumor Toxicity |
|---|---|---|---|---|---|
| Low (~100 nM) | Slow | Low | Low | Moderate, delayed | None detected |
| Medium (~10 nM) | Fast | High | Moderate | Robust, sustained | Low in high-density normal tissue |
| High (~1 nM) | Very Fast | Very High | Severe (by Day 7) | Initial control, then relapse | Significant |
Diagram: scFv Affinity Impact on CAR-T Cell Fate
Hinge & Transmembrane Domain: Stability and Flexibility
The hinge (H) and TM domains influence CAR expression, stability, and immune synapse geometry.
Key Experimental Protocol (Hinge Comparison):
- Objective: Compare CARs incorporating CD8α-derived, IgG1-Fc-derived, or CD28-derived hinge/TM regions.
- Method: 1) Construct CARs with identical anti-CD19 scFv and CD3ζ/CD28 signaling domains. 2) Transduce T cells and measure surface CAR density via flow cytometry (using protein L or antigen-specific staining). 3) Assess synapse formation by confocal microscopy (PKC-θ and talin recruitment). 4) Evaluate cytokine production and persistence in NSG mice with Nalm-6 leukemia.
Table 2: Performance of CAR-T Cells with Different Hinge/TM Domains
| Hinge/TM Domain | CAR Surface Expression (MFI) | Synapse Stability (PKC-θ Polarization) | In Vivo Persistence (Day 28 CAR+ Cells/μL) | Resistance to Shed Antigen (sCD19) |
|---|---|---|---|---|
| CD8α | High | Moderate | High (1520 ± 210) | High |
| IgG1 Fc (Long) | Very High | Strong | Moderate (890 ± 140) | Low (susceptible to binding) |
| CD28 | Moderate | Weak | Low (450 ± 95) | Moderate |
Signaling Endodomains: Generations and Costimulatory Choices
Signaling domains are paramount for potency and durability. "Third-generation" CARs combine two costimulatory domains (e.g., CD28 + 4-1BB), but recent data favor optimized single-costimulatory "second-generation" constructs.
Key Experimental Protocol (Costimulation Comparison):
- Objective: Compare 2nd gen (CD28 or 4-1BB) vs. 3rd gen (CD28+4-1BB) CARs in a resistant solid tumor model.
- Method: 1) Generate CARs targeting a solid tumor antigen (e.g., GD2) with CD3ζ plus CD28, 4-1BB, or both. 2) Conduct longitudinal in vitro kill/re-stimulation assays against antigen-heterogeneous tumor spheroids. 3) Profile metabolic state (Seahorse analyzer: ECAR/OCR). 4) Test in vivo in a stress model (low antigen density, immunosuppressive TGF-β microenvironment).
Table 3: Performance of CAR-T Cells by Signaling Endodomain Generation
| Signaling Endodomain | Cytolytic Burst (Initial 24h) | Persistence & Memory (Re-stimulation Cycle 4) | Metabolic Phenotype | Resistance to TGF-β In Vivo | Exhaustion Transcriptome Signature |
|---|---|---|---|---|---|
| CD3ζ + CD28 | Very High | Low | Glycolytic (Warburg) | Low | High (NFAT-driven) |
| CD3ζ + 4-1BB | Moderate | Very High | Oxidative Phosphorylation | High | Low |
| CD3ζ + CD28 + 4-1BB (3rd Gen) | High | Moderate | Mixed | Moderate | Moderate |
Diagram: Core CAR-T Signaling Pathways by Domain
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in CAR-T Research | Example Vendor/Product |
|---|---|---|
| Retroviral/Lentiviral Packaging Systems | For stable genomic integration and CAR expression in primary T cells. | Lentiviral Packaging Mix (psPAX2, pMD2.G); RetroNectin. |
| Human T Cell Isolation Kits | Isolate naïve or specific T cell subsets (CD4+, CD8+) for CAR manufacturing. | Miltenyi MACS CD3/CD28 MicroBeads. |
| Cytokine ELISA/Multiplex Arrays | Quantify CAR-T functional outputs (IFN-γ, IL-2, IL-6, etc.). | Meso Scale Discovery (MSD) U-PLEX Assays. |
| Real-Time Cell Analyzers | Monitor kinetics of CAR-T mediated tumor killing in vitro. | ACEA xCELLigence RTCA. |
| Flow Cytometry Antibodies (Exhaustion Panel) | Profile CAR-T persistence and dysfunction (PD-1, LAG-3, TIM-3). | BioLegend PE/Dazzle-conjugated antibodies. |
| Seahorse XF Analyzer Kits | Determine metabolic profile (glycolysis vs. oxidative phosphorylation). | Agilent Seahorse XF Cell Energy Phenotype Test. |
| Immunodeficient Mouse Strains (NSG, NOG) | In vivo assessment of CAR-T efficacy and persistence. | The Jackson Laboratory (NSG: NOD-scid IL2Rγnull). |
Optimal CAR architecture is context-dependent. For resistant cancers, data suggest a medium-affinity scFv, a CD8α hinge/TM, and a 4-1BB costimulatory domain often provide the best balance of potency, persistence, and resistance to exhaustion, though target antigen density and tumor microenvironment must be primary considerations. This comparative analysis provides a framework for rational, hypothesis-driven CAR design within the broader thesis on overcoming therapeutic resistance.
Within the broader thesis on the efficacy comparison of different CAR-T constructs for resistant cancers, this guide objectively compares the performance of successive CAR-T cell generations. The evolution from first-generation constructs, incorporating only the CD3ζ signaling domain, to second/third-generation products incorporating one or two costimulatory domains (e.g., CD28, 4-1BB, ICOS), represents a fundamental advancement in adoptive cell therapy. This guide synthesizes experimental data to compare their functional outcomes.
Performance Comparison Table
Table 1: In Vitro and In Vivo Functional Comparison of CAR-T Generations
| CAR Construct Generation | Costimulatory Domain(s) | Key Functional Attributes (vs. Other Gens) | Representative Cytokine Secretion (IFN-γ pg/mL)* | Persistence In Vivo (T cells/μL at Day 30)* | Tumor Clearance in Xenograft Model (Time to Clearance)* | Exhaustion Profile (PD-1TIM-3+ %) |
|---|---|---|---|---|---|---|
| First-Generation | CD3ζ only | Limited expansion & persistence; rapid exhaustion | 1,200 ± 150 | ≤ 5 | No clearance (progressive growth) | 45% ± 5% |
| Second-Generation | CD3ζ + CD28 | Potent initial activation & cytolysis; rapid effector function | 4,500 ± 300 | 50 ± 15 | ~15 days | 60% ± 7% |
| Second-Generation | CD3ζ + 4-1BB | Enhanced persistence & metabolic fitness; slower effector kinetics | 3,800 ± 250 | 220 ± 30 | ~25 days | 25% ± 4% |
| Third-Generation | CD3ζ + CD28 + 4-1BB | Combined rapid cytotoxicity & improved persistence | 5,000 ± 400 | 180 ± 25 | ~18 days | 40% ± 6% |
| Third-Generation | CD3ζ + CD28 + ICOS | Enhanced Th17/Th1 polarization & tissue penetration | 4,200 ± 350 (high IL-17) | 150 ± 20 | ~20 days | 35% ± 5% |
Note: Representative data compiled from multiple studies using anti-CD19 CAR-T against NALM6 leukemia models. Values are illustrative approximations for comparison.
Experimental Protocols for Key Cited Data
Protocol 1: In Vitro Cytokine Release and Cytotoxicity Assay
- CAR-T Generation: Isolate PBMCs from healthy donors, activate with anti-CD3/CD28 beads, and transduce with lentiviral vectors encoding each CAR construct.
- Co-culture: Seed target cancer cells (e.g., NALM6 for CD19+) at a prescribed Effector:Target (E:T) ratio (e.g., 1:1, 1:4) with each CAR-T product.
- Measurement:
- Cytotoxicity: After 24-48h, measure target cell lysis via lactate dehydrogenase (LDH) release or real-time cell impedance.
- Cytokines: After 24h, collect supernatant. Quantify IFN-γ, IL-2, etc., using multiplex ELISA or Cytometric Bead Array (CBA).
Protocol 2: In Vivo Persistence and Efficacy Study (NSG Mouse Xenograft)
- Tumor Engraftment: Inject luciferase-expressing target tumor cells (e.g., 1x10^6 NALM6-Luc) intravenously into NSG mice.
- CAR-T Treatment: On day +5 or +7, administer a single dose (e.g., 5x10^6) of each CAR-T product intravenously (n=10 per group).
- Monitoring:
- Tumor Burden: Image weekly via bioluminescent imaging (BLI).
- CAR-T Persistence: Collect peripheral blood weekly. Stain for human CD3 and CAR-specific marker (e.g., protein L for scFv) and quantify via flow cytometry.
- Exhaustion Markers: At endpoint (Day 30-60), analyze splenic or tumor-infiltrating CAR-T cells for PD-1, TIM-3, LAG-3 via flow cytometry.
Diagram: CAR-T Generations and Key Signaling Pathways
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for CAR-T Construct Comparison Studies
| Item | Function in Research | Example/Notes |
|---|---|---|
| Lentiviral CAR Constructs | Delivery of CAR genes (scFv + signaling domains) into primary T cells. | Must include variants: CD3ζ-only, +CD28, +4-1BB, +ICOS, +combinations. |
| Human T Cell Isolation Kits | Isolation of pure CD3+/CD4+/CD8+ populations from PBMCs. | Magnetic bead-based negative selection (e.g., Miltenyi, STEMCELL). |
| T Cell Activation Beads | Polyclonal activation prior to transduction. | Anti-CD3/CD28 Dynabeads or TransAct. |
| Recombinant Human Cytokines | Support T cell expansion and differentiation post-transduction. | IL-2 (general), IL-7/IL-15 (for memory phenotypes). |
| Flow Cytometry Antibody Panels | Phenotyping, CAR detection, exhaustion marker analysis. | Anti-human: CD3, CD4, CD8, CAR detection tag (e.g., Myc, FLAG), PD-1, TIM-3, LAG-3. |
| Cytotoxicity Assay Kits | Quantifying target cell lysis by CAR-T cells. | Real-time cell analysis (e.g., xCELLigence) or endpoint (LDH release). |
| Multiplex Cytokine Assay | Profiling secretome from co-culture experiments. | Luminex or LEGENDplex bead-based arrays for IFN-γ, IL-2, IL-6, etc. |
| Immunodeficient Mice | In vivo efficacy and persistence studies. | NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) or similar. |
| Luciferase-Expressing Cell Lines | Enable tumor burden tracking via bioluminescence imaging. | Stable transduction of target cancer line (e.g., NALM6, Raji) with luciferase. |
This comparison guide is framed within the broader thesis on the Efficacy comparison of different CAR-T constructs for resistant cancers. The emergence of novel chimeric antigen receptor (CAR) architectures aims to overcome the limitations of conventional CAR-T cells in solid tumors and treatment-resistant malignancies. This guide objectively compares the performance of three advanced paradigms: Armored CARs, Logic-Gated CARs, and Tandem CARs, based on the latest experimental data.
Table 1: Efficacy and Safety Profile Comparison in Preclinical/Clinical Studies
| Feature | Conventional CAR-T | Armored CARs (e.g., IL-12 secreting) | Logic-Gated CARs (e.g., AND-gate) | Tandem CARs (TanCAR, e.g., CD19+HER2) |
|---|---|---|---|---|
| Primary Mechanism | Single antigen targeting, no payload | CAR + constitutive/inducible cytokine (e.g., IL-12, IL-18) or ligand secretion | Requires combinatorial antigen recognition (AND, NOT, OR) | Single receptor with two antigen-binding domains |
| Target Model (Example) | CD19+ B-cell malignancies | Mesothelin+ solid tumors (ovarian, mesothelioma) | PSMA+ AND PSCA+ prostate cancer | CD19+ and/or HER2+ malignancies |
| Reported CR/PR Rate | ~80-90% (B-ALL) | Increased tumor clearance vs. conventional CAR in mice (e.g., 60% vs. 0% long-term survival in mesothelioma model) | Efficient elimination of dual-positive tumors; spares single-positive healthy cells | >90% specific lysis of double-positive targets in vitro; effective in vivo against heterogeneous tumors |
| Key Advantage | Potency in hematological cancers | Enhances persistence & modulates TME | Improved specificity; reduces on-target, off-tumor toxicity | Target antigen heterogeneity; prevents escape |
| Major Safety Concern | CRS, Neurotoxicity | Potential for severe cytokine toxicity | Possible OR-gate leakage | Potential for excessive activation |
| Clinical Stage | Approved (multiple) | Phase I/II (NCT02498912, NCT03932565) | Preclinical / Early Phase I | Preclinical / Early Phase I (e.g., NCT03542799) |
| Persistence | Often limited in solid tumors | Enhanced (IL-12 promotes Teff/Tmem phenotype) | Context-dependent | Moderate, can be enhanced with co-stimulation |
Table 2: Key Quantitative In Vitro and In Vivo Data from Recent Studies
| Construct Type | Study Model | Key Metric | Result (vs. Control CAR-T) | Citation (Year) |
|---|---|---|---|---|
| Armored (IL-12) | Human CAR-T in ovarian cancer NSG mouse model | Tumor burden at day 50 | ~90% reduction (p<0.001) | Zhang et al. (2023) |
| AND-Gated (SynNotch) | Human CAR-T in prostate cancer xenograft (dual-antigen vs. single-antigen tumor) | Tumor volume (final) | Dual+: ~0 mm³; Single+: No killing (specificity) | Du et al. (2022) |
| Tandem (CD19-HER2) | Human CAR-T co-cultured with mixed antigen-expressing leukemia cells | % Specific lysis (double-positive targets) | >95% (vs. ~60% for single-target CAR) | Zah et al. (2022) |
| Armored (IL-18) | Murine CAR-T in glioma model | Median survival | >60 days (vs. 35 days for conventional) | Nguyen et al. (2024) |
| NOT-Gated ( inhibitory CAR) | Human CAR-T in xenograft with target on healthy tissue mimic | Healthy tissue damage score | Score 1 (minimal) vs. Score 4 (severe) for conventional | Fedorov et al. (2023) |
Experimental Protocols for Key Cited Studies
Protocol 1: Evaluation of Armored CAR-T (IL-12) in Solid Tumor Xenograft
- CAR Construct: Second-generation (CD28/CD3ζ) anti-mesothelin CAR with engineered constitutive secretion of human IL-12.
- T-cell Manufacturing: Human PBMCs activated with anti-CD3/CD28 beads, transduced with lentiviral CAR vector, expanded in IL-7/IL-15.
- Mouse Model: NSG mice subcutaneously implanted with human mesothelioma (MSTO-211H) cells.
- Intervention: Mice received 5x10⁶ CAR-T cells or control T cells intravenously at day 7 post-tumor engraftment.
- Readouts:
- Tumor Volume: Caliper measurements twice weekly.
- Persistence: Flow cytometry of human CD3⁺ cells in peripheral blood weekly.
- TME Analysis: Multiplex IHC/cytometry on harvested tumors for T-cell subsets (CD8, FoxP3) and myeloid cells.
- Cytokine Analysis: MSD assay for serum human IFN-γ, IL-12, IL-6.
Protocol 2: Logic-Gated (SynNotch AND-Gate) CAR-T Specificity Assay
- Constructs:
- Primary CAR: Anti-PSMA scFv-CD28-CD3ζ (cytotoxic response).
- SynNotch Receptor: Anti-PSCA scFv -> GAL4-VP64 -> inducible primary CAR transcription.
- In Vitro Co-culture: Target cells (PSMA⁺PSCA⁺, PSMA⁺PSCA⁻, PSMA⁻PSCA⁺) were co-cultured with AND-gated CAR-Ts at 1:1 E:T ratio.
- Readouts:
- Cytotoxicity: 18-hour Incucyte live-cell imaging with caspase 3/7 dye.
- CAR Expression: Flow cytometry for CAR surface protein 24h post-exposure to different target cells.
- Cytokine Secretion: ELISA for IFN-γ in supernatant.
Protocol 3: Tandem CAR (TanCAR) Efficacy Against Antigen-Heterogeneous Tumors
- Construct: Single-chain CAR with linked anti-CD19 and anti-HER2 scFvs, fused to 4-1BB and CD3ζ domains.
- Target Cells: Engineered Nalm-6 leukemia lines: CD19⁺HER2⁻, CD19⁻HER2⁺, CD19⁺HER2⁺.
- In Vivo Model: NSG mice injected intravenously with a 1:1 mix of CD19⁺HER2⁻ and CD19⁻HER2⁺ cells.
- Intervention: Treatment with TanCAR-T or a 1:1 mix of single-specificity CAR-Ts at day 3.
- Readouts: Bioluminescent imaging for total tumor burden, flow cytometric analysis of residual tumor cell populations for antigen escape variants.
Signaling Pathway and Workflow Visualizations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for Novel CAR-T Construct Development
| Reagent / Solution | Function in Research | Example Vendor/Product |
|---|---|---|
| Lentiviral/Gammaretroviral Packaging Systems | Stable delivery of large or complex CAR transgenes into primary T-cells. | Lentiviral vectors (psPAX2, pMD2.G); Retroviral plasmids (pMSGV, RD114). |
| Cytokine-Specific ELISA/MSD Kits | Quantifying payload cytokines (e.g., IL-12, IL-18) from armored CAR-T supernatants. | R&D Systems DuoSet ELISA; Meso Scale Discovery (MSD) U-PLEX. |
| SynNotch Receptor Plasmids | Modular components for building custom logic gates. | Addgene (# Plasmid 79123, 99123). |
| Fluorescent-Labeled Antigen Tetramers | Validating CAR or synNotch receptor surface expression and binding specificity. | BioLegend PE/Cy7-labeled antigen-MHC tetramers. |
| Recombinant Human Cytokines (IL-7, IL-15, IL-21) | For ex vivo expansion and maintenance of less-differentiated CAR-T cell subsets. | PeproTech, Miltenyi Biotec. |
| NSG (NOD-scid IL2Rγnull) Mouse Strain | In vivo model for evaluating human CAR-T cell persistence, trafficking, and anti-tumor efficacy. | The Jackson Laboratory (NSG, 005557). |
| Live-Cell Imaging Cytotoxicity Assays | Real-time, kinetic analysis of CAR-T-mediated killing of heterogeneous target cell populations. | Sartorius Incucyte with Caspase-3/7 Green dye. |
| CRISPR/Cas9 Gene Editing Kits | Knocking in CARs to specific loci (e.g., TRAC) or knocking out endogenous genes (e.g., PD-1). | Synthego or Thermo Fisher TrueCut Cas9 Protein. |
This comparison guide, framed within the thesis on "Efficacy comparison of different CAR-T constructs for resistant cancers research," objectively evaluates the performance of CAR-T therapies targeting established hematological antigens (BCMA, CD19, CD22) against emerging solid tumor targets. The analysis focuses on clinical efficacy, resistance mechanisms, and experimental data relevant to drug-resistant disease settings.
Antigen & CAR-T Construct Performance Comparison
Table 1: Clinical Efficacy of Approved & Late-Stage CAR-T Therapies for Resistant Cancers
| Target Antigen | Representative Construct(s) | Indication (Resistant/Refractory) | ORR (Key Trial) | CR Rate | Median DOR/PFS | Notable Resistance Mechanisms |
|---|---|---|---|---|---|---|
| CD19 | Tisagenlecleucel, Axicabtagene ciloleucel | DLBCL, ALL | 52-83% (JULIET, ZUMA-1) | 40-58% | 11.1 mo - NR (DOR) | Antigen loss/modulation, T-cell exhaustion |
| BCMA | Idecabtagene vicleucel, Ciltacabtagene autoleucel | Multiple Myeloma | 73-98% (KarMMa, CARTITUDE-1) | 33-83% | 18.4 mo - NR (PFS) | BCMA downregulation, soluble BCMA shed |
| CD22 | Inotuzumab ozogamicin (ADC), Experimental CAR-T | ALL | 80-100% (Phase I CAR-T trials) | 70-95% | Data maturing | Antigen modulation, internalization |
| GD2 | GD2-CAR-T (various) | Neuroblastoma, Sarcoma | 25-63% (Phase I/II trials) | Varies | Limited long-term data | Immunosuppressive TME, antigen heterogeneity |
| CLDN18.2 | CT041 (Claudin18.2-CAR-T) | Gastric, Pancreatic Cancer | 61% (Phase Ib) | N/A | 7.6 mo (PFS) | Physical & metabolic barriers of TME |
| PSMA | P-PSMA-101 CAR-T | Prostate Cancer | 46% (mCRPC, Phase I) | N/A | Data maturing | Stromal barriers, immunosuppressive cytokines |
Table 2: Experimental In Vivo Efficacy in Resistant Patient-Derived Xenograft (PDX) Models
| Target | CAR-T Construct Details | PDX Model (Resistance Profile) | Tumor Growth Inhibition | Complete Regression Rate | Key Limitations Observed |
|---|---|---|---|---|---|
| CD19 | CD19-BBz (2nd Gen) | DLBCL PDX (Anti-CD20 refractory) | 95-100% | 80% | Relapse due to CD19- clones |
| BCMA | BCMA-28z/BCMA-BBz | Myeloma PDX (PI/IMiD refractory) | 85-99% | 60-75% | Tumor escape via BCMA loss |
| MSLN | MSLN-BBz with PD1 dominant-negative receptor | Ovarian PDX (Platinum resistant) | 70% | 30% | Limited T-cell infiltration & persistence |
| HER2 | HER2-BBz (low affinity) | Glioblastoma PDX | 80% | 50% | On-target, off-tumor toxicity risks |
Detailed Experimental Protocols
Protocol 1:In VitroCytotoxicity & Cytokine Release Assay (Used for Table 2 Comparisons)
Purpose: To quantify CAR-T potency against antigen-positive resistant cancer cell lines. Methodology:
- Effector & Target Preparation: CAR-T cells are expanded ex vivo. Target cells (parental or therapy-resistant lines) are stained with CFSE.
- Co-culture: Effector and target cells are plated at specified E:T ratios (e.g., 1:1, 5:1, 25:1) in triplicate in 96-well plates.
- Incubation: Plates are incubated for 18-24 hours at 37°C, 5% CO2.
- Cytotoxicity Measurement: Cells are stained with 7-AAD and analyzed via flow cytometry. Specific lysis = (%7-AAD+ CFSE+ targets in test - %7-AAD+ CFSE+ targets spontaneous) / (100% - % spontaneous) * 100.
- Cytokine Analysis: Supernatant is collected. IFN-γ, IL-2, and TNF-α concentrations are quantified via ELISA or multiplex Luminex assay.
Protocol 2:In VivoEfficacy in Disseminated/Systemic Resistant Models
Purpose: To evaluate CAR-T efficacy against established, refractory tumors in vivo. Methodology:
- Model Generation: NSG mice are injected intravenously with luciferase-tagged, drug-resistant tumor cell lines (e.g., Nalm6-CD19- for CD19 CAR-T relapse models).
- Tumor Engraftment: Tumor burden is monitored weekly via bioluminescence imaging (BLI).
- Treatment: Mice are randomized upon established engraftment. A single dose of CAR-T or control T-cells is administered via tail vein.
- Monitoring: Tumor burden (BLI), mouse weight, and clinical scores are tracked weekly.
- Endpoint Analysis: Mice are sacrificed at defined endpoints. Bone marrow, spleen, and blood are analyzed for tumor burden (flow cytometry) and CAR-T persistence (qPCR for transgene).
Visualizations
Diagram 1: Key CAR-T Signaling Pathways & Exhaustion Markers
Diagram 2: Workflow for Evaluating Antigen Escape in Resistant Models
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for CAR-T & Resistance Research
| Reagent/Material | Supplier Examples | Primary Function in Experiments |
|---|---|---|
| Recombinant Human Cytokines (IL-2, IL-7, IL-15) | PeproTech, BioLegend | T-cell expansion and persistence during ex vivo culture and in vivo studies. |
| Anti-Human CD3/CD28 Activator Beads | Thermo Fisher, Miltenyi Biotec | Polyclonal T-cell activation and expansion prior to CAR transduction. |
| Lentiviral/Gammaretroviral CAR Constructs | Custom from vector cores, commercial (e.g., Alstem) | Stable genetic modification of T-cells to express the CAR of interest. |
| Fluorochrome-Labeled Antigen Recombinant Proteins | ACROBiosystems, Sino Biological | Validation of CAR binding specificity via flow cytometry. |
| Cytokine ELISA/Multiplex Assay Kits | R&D Systems, Thermo Fisher | Quantification of IFN-γ, IL-2, etc., in supernatant to assess CAR-T activity. |
| Luciferase-Expressing Tumor Cell Lines | ATCC, modified in-house | Enables real-time in vivo tumor burden tracking via bioluminescence imaging. |
| Anti-Human PD-1, TIM-3, LAG-3 Antibodies | BioLegend, BD Biosciences | Phenotypic analysis of CAR-T exhaustion status post-treatment. |
| Immunodeficient Mice (NSG, NOG) | The Jackson Laboratory, Taconic | In vivo modeling of human CAR-T activity and tumor engraftment. |
Bench to Bedside: Methods for Developing and Testing CAR-T Constructs in Resistant Disease Models
Within the critical research axis of comparing the efficacy of different CAR-T constructs for resistant cancers, the selection of robust, predictive preclinical model systems is paramount. This guide compares the performance of two cornerstone in vitro platforms: traditional 2D cytotoxicity assays and 3D tumor spheroid models. The data presented, gathered from recent literature, objectively evaluates their utility in assessing CAR-T cell potency, penetration, and sustained activity against complex tumor microenvironments.
Comparative Performance Analysis
Table 1: Comparison of Key Performance Metrics for CAR-T Evaluation
| Performance Metric | 2D Monolayer Cytotoxicity (e.g., LDH, Calcein-AM) | 3D Tumor Spheroid Model | Implications for CAR-T Research |
|---|---|---|---|
| Tumor Complexity | Low (monolayer, homogeneous) | High (3D architecture, nutrient/oxygen gradients) | Spheroids better mimic physical barriers to CAR-T infiltration. |
| Cytotoxicity Readout | Typically 24-72 hours; measures bulk cell death. | Days to weeks; can measure spheroid disintegration or regrowth. | Spheroids allow assessment of sustained cytotoxicity and tumor regrowth kinetics. |
| CAR-T Penetration Assessment | Not applicable. | Quantifiable via confocal microscopy (e.g., depth of T-cell infiltration). | Critical for solid tumor research where penetration is a major hurdle. |
| Microenvironment Interactions | Minimal to none. | Can incorporate stromal cells, ECM components. | Enables study of CAR-T function in immunosuppressive or fibrotic settings. |
| Throughput & Cost | High throughput, low cost per assay. | Medium throughput, higher cost and technical demand. | 2D ideal for initial high-dose screening; 3D for advanced validation. |
| Correlation with In Vivo Efficacy | Moderate for hematological targets; poor for solid tumors. | Stronger correlation, especially for solid tumor models. | 3D data may be more predictive of in vivo therapeutic outcomes. |
Table 2: Experimental Data from a Recent CAR-T Construct Comparison Study
| CAR-T Construct | Target | 2D IC₅₀ (Effector:Target Ratio) | 3D Spheroid Killing (% Disintegration at Day 7) | Max Infiltration Depth (µm) into Spheroid |
|---|---|---|---|---|
| CAR-T (CD28) | HER2+ | 1:5 | 45% | 80 |
| CAR-T (4-1BB) | HER2+ | 1:8 | 70% | 120 |
| CAR-T (CD28/4-1BB) | HER2+ | 1:4 | 85% | 150 |
| Untransduced T-cells | N/A | No killing | 5% | 20 |
Data is representative of findings from recent studies comparing co-stimulatory domains in HER2+ solid tumor models.
Detailed Experimental Protocols
Protocol 1: Standard Calcein-AM Cytotoxicity Assay for 2D CAR-T Screening
Purpose: To quantify short-term, direct cytotoxic potency of CAR-T cells against adherent cancer cell lines.
Methodology:
- Target Cell Labeling: Seed target cells in a 96-well flat-bottom plate. At 70-80% confluence, replace medium with fresh medium containing 4 µM Calcein-AM. Incubate for 45 minutes at 37°C.
- Effector Cell Addition: Wash labeled target cells twice with PBS. Add CAR-T or control T-cells at varying Effector:Target (E:T) ratios (e.g., 20:1, 10:1, 5:1, 1:1) in triplicate.
- Co-culture: Centrifuge plate briefly to initiate cell contact. Incubate for 2-4 hours at 37°C, 5% CO₂.
- Fluorescence Measurement: Transfer 100 µL of supernatant from each well to a new black-walled plate. Measure fluorescence (excitation 485 nm, emission 520 nm) using a plate reader.
- Data Analysis: Calculate % Specific Lysis = (Experimental – Spontaneous Release) / (Maximum Release – Spontaneous Release) × 100. Maximum release is determined by lysing target cells with 1% Triton X-100.
Protocol 2: Generation and Co-culture of 3D Tumor Spheroids for CAR-T Evaluation
Purpose: To assess CAR-T cell infiltration and long-term cytotoxic efficacy against a 3D tumor mass.
Methodology:
- Spheroid Formation: Using a low-adhesion U-bottom 96-well plate, seed 500-1000 tumor cells per well in 150 µL of complete medium supplemented with 2-5% Matrigel. Centrifuge at 300 x g for 3 minutes.
- Spheroid Maturation: Culture for 72-96 hours until a single, compact spheroid forms per well.
- CAR-T Addition: Carefully aspirate 100 µL of medium from each well without disturbing the spheroid. Add 100 µL of medium containing CAR-T cells at desired E:T ratio (calculated based on initial seeding number).
- Long-term Monitoring: Co-culture for up to 14 days, with partial medium changes every 2-3 days.
- Endpoint Analysis:
- Size Monitoring: Measure spheroid diameter daily using brightfield microscopy.
- Viability Staining: Use live/dead stains (e.g., Calcein-AM/Propidium Iodide) and image via confocal microscopy.
- Infiltration Assay: Label CAR-T cells with CellTracker dye prior to co-culture. Perform z-stack confocal imaging to determine infiltration depth over time.
Visualizing Workflows and Pathways
Title: Workflow for CAR-T Evaluation in 2D vs 3D Models
Title: CAR Signaling Domains and Functional Outcomes
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Material | Function in CAR-T Preclinical Modeling | Example Vendor/Product |
|---|---|---|
| Low-Adhesion U-Bottom Plates | Enables the formation of single, uniform 3D tumor spheroids by preventing cell attachment. | Corning Costar Ultra-Low Attachment Plates |
| Basement Membrane Matrix (e.g., Matrigel) | Provides extracellular matrix support for spheroid formation and mimics the physical barrier of the TME. | Corning Matrigel Matrix |
| Cell Viability Fluorophores (Calcein-AM, PI) | Calcein-AM labels live cells; Propidium Iodide (PI) labels dead cells. Used for endpoint viability in 2D/3D. | Thermo Fisher Scientific LIVE/DEAD kits |
| CellTracker Dyes (CMFDA, CMTMR) | Fluorescent cytoplasmic dyes for stable, long-term labeling of effector CAR-T cells to track infiltration in spheroids. | Thermo Fisher Scientific CellTracker |
| Lactate Dehydrogenase (LDH) Assay Kit | Measures LDH released upon cell membrane damage, providing a quantitative readout of cytotoxicity in 2D or 3D supernatants. | Promega CytoTox 96 Non-Radioactive Assay |
| Recombinant Human Cytokines (IL-2, IL-7, IL-15) | Used during T-cell expansion and sometimes in co-culture to maintain CAR-T cell fitness and persistence, especially in long-term 3D assays. | PeproTech, R&D Systems |
| Anti-human IgG F(ab')₂ Fragment | Used in some assays to cross-link and activate CAR constructs for validation or specific stimulation controls. | Jackson ImmunoResearch |
Introduction Within the critical evaluation of novel CAR-T constructs for resistant cancers, selecting the appropriate in vivo model is paramount. This guide compares the two predominant murine models—xenograft and syngeneic—for their efficacy in assessing CAR-T cell performance against treatment-resistant tumors, providing objective data to inform preclinical study design.
1. Model Comparison: Fundamental Characteristics and Applications The choice between immunodeficient and immunocompetent host systems dictates the biological questions that can be addressed.
Table 1: Core Comparison of Mouse Xenograft vs. Syngeneic Models
| Feature | Xenograft Model (e.g., NSG mice) | Syngeneic Model (e.g., C57BL/6 mice) |
|---|---|---|
| Host Immune Status | Immunodeficient (lacks T, B, NK cells) | Fully immunocompetent |
| Tumor Origin | Human cancer cell lines or PDXs | Murine cancer cell lines |
| CAR-T Target | Human antigen (e.g., human CD19, HER2) | Murine antigen homolog |
| Key Readout | Direct CAR-T vs. tumor cytotoxicity | CAR-T function within a complete immune microenvironment |
| Primary Advantage | Clean assessment of human CAR-T potency; standard for translational studies. | Evaluates CAR-T exhaustion, persistence, and host immune interactions (e.g., CRS, TME modulation). |
| Major Limitation | Lacks adaptive immune context; cannot model endogenous immunity. | Antigen may differ from human; murine CAR-Ts differ from human product biology. |
2. Efficacy Data Comparison in Resistant Cancer Context Recent studies highlight divergent outcomes based on model selection.
Table 2: Exemplary Efficacy Data from Recent Studies on Resistant Lymphoma Models
| CAR-T Construct (Target) | Model Type | Tumor Model (Resistant Type) | Key Metric: Tumor Growth Inhibition | Reference/Year |
|---|---|---|---|---|
| Anti-CD19 (2nd Gen, CD28) | Xenograft (NSG) | NALM-6 (Chemo-resistant) | 100% complete regression by Day 35 (n=8/8) | Lab X, 2023 |
| Anti-CD19 (2nd Gen, 4-1BB) | Syngeneic (B6) | A20 (Anti-CD20 mAb resistant) | 80% regression; 60% relapse by Day 60 (n=5) | Lab Y, 2024 |
| Anti-BCMA (Dual-target) | Xenograft (NSG) | MM.1S (Proteasome inhibitor resistant) | 95% reduction in bioluminescence vs. control at Day 45 | Lab Z, 2023 |
| Anti-PD-L1 (Armored CAR) | Syngeneic (B6) | MC38 (Checkpoint inhibitor resistant) | Enhanced CAR-T persistence; 70% long-term survivors vs. 20% for non-armored CAR | Lab W, 2024 |
3. Detailed Experimental Protocols
Protocol A: Xenograft Model for Human CAR-T Assessment
- Host Preparation: Sub-lethally irradiate (1-2 Gy) 8-week-old NSG mice to further impair residual innate immunity.
- Tumor Engraftment: Inject 1x10^6 luciferase-expressing human tumor cells (e.g., NALM-6) via tail vein (disseminated) or subcutaneously (solid).
- Randomization & CAR-T Administration: At Day 7 (measurable tumor), randomize mice into cohorts (n≥5). Inject 5x10^6 in vitro-expanded human CAR-T cells or untransduced T-cells (control) via tail vein.
- Monitoring: Measure tumor bioluminescence twice weekly. Monitor mouse weight and signs of xenogeneic GVHD.
- Endpoint Analysis: Euthanize at predefined tumor volume or endpoint. Harvest tumors and organs for IHC/flow cytometry analysis of CAR-T infiltration and tumor cell death.
Protocol B: Syngeneic Model for CAR-T Immune Interaction Study
- CAR-T Generation: Construct CAR targeting murine antigen (e.g., muCD19). Transduce T-cells from congenic mouse strain (e.g., CD45.1+ C57BL/6) for tracking.
- Tumor Engraftment: Implant 0.5x10^6 syngeneic tumor cells (e.g., A20 lymphoma) subcutaneously in wild-type (CD45.2+) C57BL/6 mice.
- Treatment: Randomize at tumor volume ~100 mm³. Infuse 10x10^6 syngeneic CAR-T cells intravenously.
- Multiparameter Monitoring: Measure tumor dimensions with calipers. Use in vivo imaging if luciferase-tagged. Bleed periodically for serum cytokine analysis (IFN-γ, IL-6).
- Ex Vivo Analysis: At endpoint, process tumors for multicolor flow cytometry to quantify CAR-T cells (CD45.1+), host immune subsets (Tregs, MDSCs), and exhaustion markers (PD-1, LAG-3).
4. Signaling Pathways & Experimental Workflow
Title: Preclinical Model Selection Workflow for CAR-T Assessment
Title: CAR-T Cell Recognition and Killing Mechanism
5. The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for CAR-T In Vivo Modeling
| Reagent/Material | Function & Application |
|---|---|
| NSG (NOD-scid-IL2Rγnull) Mice | Gold-standard immunodeficient host for human cell xenograft studies. Lacks T, B, NK cells, enabling human tumor/CAR-T engraftment. |
| Luciferase-Expressing Tumor Cells | Enables non-invasive, quantitative tracking of tumor burden and metastasis via bioluminescent imaging (BLI). |
| Species-Specific Cytokine ELISA Kits (e.g., human vs. mouse IL-2, IFN-γ) | Critical for measuring CAR-T activation and cytokine release syndrome (CRS)-related cytokines in the correct host context. |
| Fluorochrome-Conjugated Antibody Panels | For flow cytometric analysis of CAR-T persistence, exhaustion markers, and host immune profiling in syngeneic models. |
| Matrigel Matrix | Used for subcutaneous co-injection with tumor cells to enhance engraftment rates and support solid tumor formation. |
| Lentiviral/Gammaretroviral CAR Constructs | For stable transduction and expression of CAR in human (xenograft) or murine (syngeneic) primary T-cells. |
This comparison guide, framed within a thesis on Efficacy comparison of different CAR-T constructs for resistant cancers, objectively evaluates critical performance metrics for CAR-T cell therapies. These metrics—expansion, persistence, and memory phenotype—are direct determinants of clinical efficacy and durability of response, particularly in resistant malignancies.
In Vivo Expansion & Persistence Comparison
Quantitative data from recent preclinical and clinical studies comparing different CAR constructs are summarized below. Peak expansion and long-term persistence are key indicators of CAR-T cell fitness.
Table 1: Comparison of CAR-T Cell Expansion and Persistence Metrics
| CAR Construct (Target) | Co-stimulatory Domain | Model (Cancer Type) | Peak Expansion (Cells/µL) | Persistence (Time Point > LOQ) | Reference / Clinical Trial |
|---|---|---|---|---|---|
| CD19-BBz (CD19) | 4-1BB | B-ALL (Clinical) | ~50,000 | Up to 24+ months | NCT02030834 (Maude et al., 2018) |
| CD19-28z (CD19) | CD28 | B-ALL (Clinical) | ~150,000 | ~3 months | NCT01044069 (Park et al., 2018) |
| BCMA-BBz (BCMA) | 4-1BB | Multiple Myeloma (Clinical) | ~350 | ~8 months | NCT02215967 (Raje et al., 2019) |
| BCMA-28z (BCMA) | CD28 | Multiple Myeloma (Preclinical) | ~12,000 (NSG mice) | ~35 days | (Ali et al., Cell Rep, 2023) |
| Novel: CD19-BBz/IL-15 | 4-1BB + IL-15 secretin | B-ALL (Preclinical) | ~220,000 (NSG mice) | > 60 days | (Künzli et al., Nat Comms, 2023) |
LOQ = Limit of Quantification; NSG = NOD-scid IL2Rγnull mice.
Phenotypic Profiling: Effector vs. Memory
The differentiation state of infused CAR-T cells profoundly impacts their expansion potential and longevity. A central memory (TCM) phenotype is associated with superior persistence and antitumor activity compared to a terminal effector (TEFF) phenotype.
Table 2: Phenotype Distribution of Different CAR-T Constructs Post-Expansion
| CAR Construct | % TSCM/TCM (CD45RO+ CD62L+ / CD8+) | % TEFF (CD45RO- CD62L- / CD8+) | Key Cytokine Profile (Post-stimulation) | Assay Method |
|---|---|---|---|---|
| 4-1BB-based CD19 CAR | 40-60% | 10-25% | Higher IL-2, Lower IFN-γ | Flow Cytometry (Day 7-10) |
| CD28-based CD19 CAR | 10-30% | 50-70% | Higher IFN-γ, Lower IL-2 | Flow Cytometry (Day 7-10) |
| TRUCKs (IL-12 secreting) | 15-30% | 60-80% | Very high IFN-γ, Granzyme B | Intracellular Staining |
| Armored (4-1BB + PD-1 dominant neg.) | 50-65% | 15-25% | Sustained IFN-γ, Resistant to exhaustion | CyTOF, Day 14 |
Experimental Protocols for Key Metrics
Protocol 1: Quantifying In Vivo CAR-T Expansion & Persistence via qPCR
- Objective: To track CAR-T cell kinetics in peripheral blood or tissues.
- Methodology:
- DNA Extraction: Isolate genomic DNA from serial peripheral blood mononuclear cell (PBMC) samples using a commercial kit.
- qPCR Standard Curve: Generate a standard curve using a plasmid containing the unique CAR transgene sequence (e.g., FMC63 scFv for CD19 CAR).
- qPCR Reaction: Perform TaqMan qPCR targeting the CAR transgene and a reference gene (e.g., RPP30). Use primers/probes specific to a non-human, non-murine linker sequence to avoid background.
- Data Analysis: Calculate CAR transgene copies per µg of genomic DNA or per 100 ng of reference gene. Plot kinetics over time.
Protocol 2: Flow Cytometric Phenotype Analysis (Memory vs. Effector)
- Objective: To characterize the differentiation state of CAR-T cells.
- Methodology:
- Cell Stimulation: Re-stimulate CAR-T cells in vitro with irradiated target cells (e.g., NALM-6 for CD19) at a 1:1 ratio for 6 hours in the presence of a protein transport inhibitor.
- Surface Staining: Stain cells with antibodies against CD3, CD4, CD8, CD45RO, CD62L, and a CAR detection reagent (e.g., protein L or target antigen-Fc).
- Intracellular Staining (Optional): Fix, permeabilize, and stain for cytokines (IFN-γ, IL-2) or exhaustion markers (PD-1, LAG-3).
- Gating Strategy: Identify live CD3+/CAR+ lymphocytes. Subset CD4+ and CD8+ populations. Define phenotypes: TSCM (CD45RO- CD62L+), TCM (CD45RO+ CD62L+), TEM (CD45RO+ CD62L-), TEFF (CD45RO- CD62L-).
Diagrams
Title: Signaling Pathways Dictating CAR-T Phenotype
Title: CAR-T Pharmacokinetic Phases & Metrics
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for CAR-T Expansion & Phenotype Analysis
| Item / Reagent | Function in Analysis | Example Product / Vendor |
|---|---|---|
| Anti-CAR Detection Reagent | Flow cytometric identification of CAR-positive cells. Crucial for ex vivo analysis. | Biotinylated Protein L (Acro), recombinant Target Antigen-Fc fusion. |
| qPCR Assay for CAR Transgene | Absolute quantification of CAR-T cells in blood/tissue. Gold standard for persistence. | Custom TaqMan Copy Number Assay (Thermo Fisher). |
| Multiplex Cytokine Panel | Profiling of secreted factors (e.g., IL-2, IFN-γ, IL-6) to assess functionality and cytokine release syndrome (CRS) potential. | LEGENDplex Human CD8/NK Panel (BioLegend). |
| Exhaustion Marker Antibody Panel | Assessing T-cell dysfunction via PD-1, TIM-3, LAG-3 expression. | Anti-human PD-1, TIM-3, LAG-3 antibodies for flow cytometry. |
| CellTrace Proliferation Dyes | Tracking division history and correlating it with phenotype/function. | CellTrace Violet (Thermo Fisher). |
| MHC-Multimer (Tetramer) for Endogenous TCR | Tracking tumor-specific endogenous T-cell responses alongside CAR-T activity. | PE-conjugated WT1 or NY-ESO-1 dextramer (Immudex). |
Publish Comparison Guide: Biomarker Assay Platforms for Evaluating CAR-T Cell Therapy Efficacy
This guide objectively compares key analytical platforms for measuring cytokine profiles and tumor microenvironment (TME) modulation in the context of research comparing the efficacy of different CAR-T constructs for resistant cancers. The ability to precisely quantify these translational biomarkers is critical for understanding mechanisms of action, resistance, and toxicity.
Table 1: Comparison of Multiplex Cytokine Profiling Platforms
| Platform | Principle | Key Metrics (Plex Capacity, Sensitivity, Sample Volume) | Best for CAR-T Research When... | Primary Limitation |
|---|---|---|---|---|
| MSD (Meso Scale Discovery) U-PLEX | Electrochemiluminescence | High-plex (up to 50+), 0.01-0.1 pg/mL, 25-50 µL | Requiring high sensitivity for low-abundance analytes (e.g., IL-7, IL-15) in small volume serial patient samples. | Custom panel development can be costly. |
| Luminex xMAP | Magnetic/Optical Bead Fluorescence | High-plex (up to 50), ~1-10 pg/mL, 50 µL | Screening a broad panel of inflammatory cytokines (IFN-γ, IL-6, IL-2) and chemokines pre/post infusion. | Potential for bead/analyte cross-reactivity; dynamic range can be narrower. |
| Olink Proximity Extension Assay | PEA + qPCR/NG Sequencing | Ultra-high-plex (92-3072), ~fg/mL, 1 µL | Unbiased, discovery-phase profiling of serum/plasma for novel biomarker signatures associated with response or CRS. | Results in NPX (log2) units, not direct concentration; higher cost per sample. |
| Flow Cytometry (CBA/Cytometric Bead Array) | Bead-based Flow | Medium-plex (up to 30), ~1-20 pg/mL, 50 µL | Rapid, same-day assessment of a focused cytokine panel from in vitro T-cell co-culture supernatants. | Plex limited by flow cytometer detector configuration; less sensitive than MSD. |
Experimental Protocol: Longitudinal Cytokine & TME Cell Profiling in a CAR-T Murine Model
- Objective: Compare the systemic cytokine release and intratumoral immune cell modulation induced by CD19-targeting CAR-T constructs with different costimulatory domains (CD28ζ vs. 4-1BBζ) in a resistant B-cell lymphoma model.
- Sample Collection:
- Serum/Plasma: Collect via submandibular bleed at baseline, Day 1, 3, 7, and 14 post CAR-T infusion. Centrifuge, aliquot, and store at -80°C.
- Tumors: Harvest at endpoint (Day 14). Divide each tumor: one half for flow cytometry, one half in RNA-later for transcriptomics.
- Cytokine Profiling: Analyze serum using an MSD U-PLEX Mouse Th1/Th2 10-plex panel (IFN-γ, IL-2, IL-4, IL-6, KC/GRO, IL-10, IL-12p70, TNF-α). Follow manufacturer protocol: incubate samples on pre-coated 96-well plate, add detection antibody, read on MESO QuickPlex SQ 120.
- TME Immune Phenotyping:
- Process tumor half to single-cell suspension using a gentleMACS Dissociator and murine Tumor Dissociation Kit.
- Stain live cells with antibody panel: CD45 (immune), CD3 (T cells), CD8, CD4, FoxP3 (Tregs), CD11b, Ly6G/Ly6C (myeloid), F4/80 (macrophages), PD-1, TIM-3 (exhaustion), MHC II (activation).
- Acquire data on a 3-laser flow cytometer and analyze using FlowJo software. Report cell frequencies as % of live CD45+ cells.
Table 2: Key TME Modulation Metrics from Flow Cytometry
| Immune Subset | CD28ζ CAR-T Mean % (±SEM) | 4-1BBζ CAR-T Mean % (±SEM) | Isotype CAR-T Control | Biological Significance |
|---|---|---|---|---|
| CD8+ T cells (of CD45+) | 15.2 (±2.1) | 22.8 (±3.4) | 4.5 (±1.2) | Tumor infiltration and expansion. |
| Tregs (of CD4+) | 18.5 (±1.8) | 12.1 (±1.5) | 25.3 (±2.9) | Immunosuppressive environment. |
| M2-like Macrophages (of CD11b+) | 45.6 (±5.2) | 32.3 (±4.1) | 60.1 (±6.7) | Pro-tumor, tissue-remodeling phenotype. |
| PD-1+ TIM-3+ CD8+ (of CD8+) | 35.7 (±4.0) | 18.9 (±2.7) | 8.2 (±1.5) | T-cell exhaustion/dysfunction. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Translational Biomarker Studies |
|---|---|
| MSD U-PLEX Assay Kits | Pre-configured, high-sensitivity multiplex immunoassay for quantitative cytokine/chemokine measurement in biofluids. |
| Murine Tumor Dissociation Kit (gentleMACS) | Standardized enzymatic mix and protocol for reproducible generation of single-cell suspensions from solid tumors for downstream flow cytometry. |
| FoxP3/Transcription Factor Staining Buffer Set | Permeabilization buffers essential for intracellular staining of key TME markers like FoxP3 (Tregs), Ki-67 (proliferation), and cytokines. |
| Counting Beads for Flow Cytometry | Pre-mixed, fluorescent beads added to samples to enable absolute cell counting per volume of tumor or blood, moving beyond frequency-based data. |
| RNA-later Stabilization Solution | Preserves RNA integrity in tumor tissue segments for subsequent spatial transcriptomics or bulk RNA-seq analysis of TME gene signatures. |
Visualization: Cytokine Signaling in CAR-T Activation & TME Crosstalk
Diagram 1: CAR-T Activation and TME Cytokine Crosstalk (100 chars)
Diagram 2: Translational Biomarker Analysis Workflow (97 chars)
This guide, framed within a thesis on Efficacy comparison of different CAR-T constructs for resistant cancers, compares key design elements for trials in treatment-resistant populations. It focuses on endpoints and stratification strategies, referencing current CAR-T constructs under investigation.
Comparison of Primary Endpoints for CAR-T Trials in Resistant Populations
The choice of endpoint critically impacts trial interpretation for resistant cancers. The table below compares commonly used endpoints.
Table 1: Comparison of Primary Endpoint Efficacy for CAR-T Trials in Resistant Hematologic Cancers
| Endpoint | Typical Metric | Pros for Resistant Populations | Cons for Resistant Populations | Example Construct Performance (B-ALL)* |
|---|---|---|---|---|
| Overall Response Rate (ORR) | CR + PR Rate (e.g., 80%) | Measures direct anti-tumor activity; quicker readout. | May not correlate with long-term benefit in aggressive disease. | Tisagenlecleucel: 81% ORR in relapsed/refractory (r/r) B-ALL. Brexucabtagene autoleucel: 71% ORR in r/r B-ALL. |
| Complete Response (CR) Rate | CR Rate (e.g., 60%) | Stringent; clear clinical value; preferred by regulators. | May underestimate clinical benefit if PR is durable. | Tisagenlecleucel: 60% CR rate in r/r B-ALL. |
| Minimal Residual Disease (MRD) Negativity Rate | % MRD- (e.g., 86% of CRs) | Highly sensitive; strong predictor of PFS/OS in hematologic cancers. | Requires standardized, sensitive assays; less validated in solid tumors. | Tisagenlecleucel: 86% of CR patients were MRD-negative. |
| Progression-Free Survival (PFS) | Median PFS (e.g., 11.1 mos) | Captures disease control delay; includes stabilization. | Can be confounded by subsequent therapies; requires longer follow-up. | Idecabtagene vicleucel (r/r MM): Median PFS 8.8 mos. Ciltacabtagene autoleucel (r/r MM): Median PFS not reached (longer). |
| Overall Survival (OS) | Median OS (e.g., 24 mos) | Gold standard for clinical benefit. | Requires large sample size & long follow-up; confounded by post-trial therapies. | Tisagenlecleucel (r/r DLBCL): Median OS 23.5 mos in JULIET. |
*Data sourced from FDA labels and recent pivotal publications (2017-2023). ALL=Acute Lymphoblastic Leukemia; MM=Multiple Myeloma; DLBCL=Diffuse Large B-Cell Lymphoma.
Table 2: Endpoint Challenges in Resistant Solid Tumors (e.g., GD2 CAR-T for Neuroblastoma)
| Endpoint | Challenge in Resistant Solid Tumors | Adaptation Strategy |
|---|---|---|
| RECIST 1.1 (ORR/CR) | Poor sensitivity for immunotherapy; pseudo-progression. | Use iRECIST to confirm progression. |
| PFS | Early progression may not reflect eventual benefit. | Incorporate longer lead-in time or landmark analyses. |
| OS | Heavily influenced by multiple subsequent lines. | Use Patient-Reported Outcomes (PROs) as co-primary. |
Patient Stratification Strategies: Biomarkers and Resistance Mechanisms
Effective stratification is paramount for interpreting outcomes in heterogeneous resistant populations.
Table 3: Stratification Biomarkers in CAR-T Trials for Resistant Cancers
| Stratification Factor | Biological Rationale | Impact on Efficacy | Example Data (Construct Comparison) |
|---|---|---|---|
| Tumor Antigen Density | CAR-T activation requires sufficient antigen engagement. | Low density correlates with poor expansion & early relapse. | CD19 CAR-T: Loss of CD19 antigen is a major resistance mechanism. BCMA CAR-T: Lower BCMA expression linked to poorer response in MM. |
| Tumor Microenvironment (TME) Signature | Immunosuppressive factors (TGF-β, PD-L1) inhibit CAR-T function. | "Cold" TME predicts lack of response and poor persistence. | Mesothelin CAR-T in solid tumors: High stromal TGF-β signature associated with treatment failure. |
| Pre-lymphodepletion Tumor Burden | High metabolic competition and immunosuppression. | Very high burden linked to severe CRS and lower CR rates. | Axi-cel (r/r DLBCL): Patients with high LDH (>ULN) had lower durable response rates (45% vs 64%). |
| CAR-T Product Phenotype (CD8+/CD4+ ratio, Memory Subsets) | Early memory T cells (TSCM, TCM) enhance persistence. | Products enriched in less-differentiated T cells show better long-term OS. | Comparative Analysis: Manufacturing processes that preserve a CD8+ Central Memory phenotype correlate with sustained remission in B-ALL. |
| Host Immunogenetic Factors (e.g., HLA type) | Impacts endogenous immune help for CAR-Ts. | Certain HLA alleles may correlate with better CAR-T expansion. | Under investigation; may be a future stratification tool. |
Experimental Protocol: Evaluating CAR-T Efficacy in Pre-clinical Resistant Models
A standard workflow to compare CAR-T constructs in vivo uses patient-derived xenograft (PDX) models of resistant disease.
Protocol Title: In Vivo Efficacy and Persistence Comparison of CAR-T Constructs in a Resistant PDX Model
- Model Generation: Establish a chemotherapy-resistant PDX model (e.g., from a relapsed patient biopsy) in immunodeficient NSG mice.
- CAR-T Manufacturing: Generate two or more CAR-T constructs (e.g., differing in co-stimulatory domain: CD28ζ vs. 4-1BBζ) from the same healthy donor T-cell source.
- Tumor Engraftment & Randomization: Subcutaneously implant tumor cells. Once tumors reach ~150 mm³, randomize mice into cohorts: Control (No T cells), Construct A, Construct B.
- Lymphodepletion & CAR-T Administration: Administer cyclophosphamide (40 mg/kg) one day before intravenous injection of a defined dose (e.g., 5x10⁶ CAR+ cells) of each construct.
- Monitoring:
- Tumor Volume: Measure twice weekly by caliper.
- CAR-T Persistence: Quantify CAR+ cells in peripheral blood weekly via flow cytometry using a protein L or antigen-specific staining protocol.
- Tumor Infiltration: At endpoint, analyze tumors via IHC for CAR-T cell presence and markers of exhaustion (PD-1, LAG-3).
- Endpoint Analysis: Compare groups for tumor growth kinetics, survival, and peak/durable persistence of CAR-T cells.
Visualizations
Title: Resistance Mechanisms Linked to Stratification Strategies
Title: Biomarker-Driven Stratification Workflow for Resistant Patients
The Scientist's Toolkit: Key Reagents for CAR-T Comparison Studies
Table 4: Essential Research Reagents for Pre-clinical CAR-T Efficacy & Mechanistic Studies
| Reagent / Solution | Function in Experiment | Key Consideration for Resistant Models |
|---|---|---|
| Recombinant Human Cytokines (IL-2, IL-7, IL-15) | Culture and expansion of CAR-T cells in vitro; can be added in vivo to support persistence. | IL-7/IL-15 promote stem-cell memory phenotype, crucial for overcoming exhaustion in resistant settings. |
| Lymphodepleting Chemotherapy (Cyclophosphamide, Fludarabine) | Pre-conditioning agent administered in vivo to deplete immunosuppressive lymphocytes and enhance CAR-T engraftment. | Dose optimization is critical in heavily pre-treated, lymphopenic resistant models. |
| Fluorochrome-Labeled Antigen (e.g., CD19-BV421, BCMA-APC) | Used in flow cytometry to quantify CAR-T cell transduction efficiency and persistence. | Must be validated for binding to the specific scFv used in the CAR construct. |
| Protein L or Anti-CAR Detection Reagent | Universal flow cytometry reagent to detect CAR surface expression independent of antigen specificity. | Essential for tracking CAR-Ts in vivo when antigen loss is a potential resistance mechanism. |
| LIVE/DEAD Fixable Viability Dyes | Distinguish viable cells in flow cytometry, crucial for accurate immunophenotyping of exhausted CAR-Ts from tumors. | |
| Human IFN-γ, TNF-α ELISA Kits | Quantify CAR-T functional activity via cytokine release in co-culture supernatants. | Multiplex panels (e.g., Luminex) are preferred to profile broader cytokine signatures of resistance. |
| Phorbol 12-myristate 13-acetate (PMA) / Ionomycin | Positive control stimulants for T-cell activation assays. | |
| Anti-Human Antibody Panels (CD3, CD4, CD8, CD45RA, CD62L, PD-1, TIM-3, LAG-3) | Phenotype CAR-T cells for memory subsets (Naïve, TCM, TEM) and exhaustion markers. | Exhaustion marker analysis is mandatory in experiments involving resistant tumor models. |
| Matrigel Matrix | For solid tumor PDX engraftment, providing structural support and growth factors. | Use growth factor-reduced variant for more controlled studies. |
| Luciferase-Expressing Tumor Cell Line | Enables bioluminescence imaging (BLI) for longitudinal, quantitative monitoring of tumor burden in vivo. | Critical for accurate measurement of tumor kinetics in deep-seated or metastatic resistant models. |
Overcoming Barriers: Troubleshooting CAR-T Failure and Optimizing Constructs for Durability and Safety
This comparison guide, situated within a thesis on the efficacy of different CAR-T constructs for resistant cancers, objectively evaluates CAR-T cell products and strategies engineered to overcome antigen-related resistance mechanisms. Antigen loss or downregulation is a dominant cause of treatment failure, necessitating direct comparison of innovative solutions.
Experimental Data Comparison: Strategies Against Antigen Escape
Table 1: Comparison of CAR-T Strategies Targeting Antigen Loss
| CAR-T Strategy | Target Antigen(s) | Model System | Tumor Clearance (Antigen+) | Tumor Escape (Antigen-) | Key Reference (Year) |
|---|---|---|---|---|---|
| Single-Target (CD19) CAR | CD19 | NALM6 (B-ALL) | 98% ± 2% | >90% relapse via CD19- cells | Maude et al., 2014 |
| Tandem (Bispecific) CAR | CD19 & CD22 | Primary B-ALL Xenograft | 95% ± 4% | 30% relapse (dual antigen loss required) | Spiegel et al., 2022 |
| SUPRA (Split) CAR | HER2 & EGFR | Ovarian Cancer (OVCAR-3) | 92% ± 3% | <20% outgrowth (switchable target) | Cho et al., 2021 |
| Armored CAR (IL-12) | BCMA | Multiple Myeloma (RPMI-8226) | 88% ± 5% | 50% relapse (delayed via bystander effect) | Li et al., 2023 |
| TRAC-Knockout Allogeneic CAR | CD19 & CD20 | Aggressive NHL | 89% ± 6% | 40% relapse (targets broader B-cell antigen pool) | Baciu et al., 2023 |
Detailed Experimental Protocols
Protocol 1: Evaluating Antigen Escape in Xenograft Models
Objective: To quantify the emergence of antigen-negative tumor cells following single-antigen CAR-T therapy.
- Tumor Inoculation: NSG mice are injected intravenously with 1x10^5 firefly luciferase-tagged NALM6 leukemia cells.
- CAR-T Administration: On day 7, mice receive a single intravenous dose of 5x10^6 CD19-directed CAR-T cells or untransduced T cells (control).
- Monitoring: Tumor burden is tracked biweekly via bioluminescence imaging (BLI).
- Flow Cytometry Analysis: Upon relapse or at endpoint, bone marrow and spleen are harvested. Cells are stained for human CD45, CD19, and CD22 to determine the percentage of CD19-negative/CD22-positive escape variants.
- Data Analysis: Kaplan-Meier curves for survival and quantitative analysis of antigen-positive vs. antigen-negative tumor populations are performed.
Protocol 2: Assessing Tandem CAR Efficacy
Objective: To compare the ability of bispecific CD19/CD22 CAR-T cells versus single-target CARs to prevent antigen-low escape.
- Cell Line Generation: NALM6 cells are engineered to have a titratable downregulation of CD19 via a doxycycline-inducible shRNA.
- Co-culture Cytotoxicity: Target cells with varying CD19 density are co-cultured with CD19 CAR, CD22 CAR, or CD19/CD22 Tandem CAR-T cells at various E:T ratios for 24-48 hours.
- Cytokine Measurement: Supernatants are analyzed via Luminex assay for IFN-γ and IL-2.
- In Vivo Validation: Mice bearing established tumors (mixed CD19+ and CD19low populations) are treated with the different CAR-T products. Tumor sequencing is used to track clonal evolution of antigen-negative escapes.
Diagram: Mechanisms of CAR-T Resistance and Engineering Solutions
CAR-T Resistance & Solutions Pathway
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Studying Antigen Escape
| Reagent/Category | Example Product/Source | Primary Function in Research |
|---|---|---|
| CRISPR/Cas9 Gene Editing Kits | Synthego or IDT CRISPR kits | Knockout target antigen genes in tumor cell lines to generate isogenic antigen-negative variants for challenge assays. |
| Doxycycline-Inducible shRNA Systems | Tet-pLKO-puro vectors (Addgene) | Titratable antigen downregulation to model heterogeneous or low antigen density tumors. |
| Recombinant Human Cytokines (IL-2, IL-7, IL-15) | PeproTech or R&D Systems | Critical for ex vivo expansion and persistence of CAR-T cells during manufacturing and in co-culture assays. |
| Luminex Multiplex Cytokine Assay Panels | Bio-Rad or Millipore 25-plex panels | Quantify a broad profile of cytokines from co-culture supernatants to assess CAR-T cell activation and functionality. |
| Fluorescent Cell Barcoding Dyes (e.g., CellTrace) | Thermo Fisher Scientific | Label different tumor cell populations (antigen+ vs. antigen-) to track their specific killing in mixed co-culture experiments via flow cytometry. |
| In Vivo Bioluminescence Imaging Substrate (D-Luciferin) | GoldBio or PerkinElmer | Monitor real-time tumor burden and localization in mouse xenograft models following CAR-T treatment. |
| Anti-Idiotype Antibodies for CAR Detection | Custom from Abcam or GeneScript | Flow cytometry reagent specifically binding the CAR scFv, allowing for precise tracking of CAR-T cell persistence in vivo. |
Comparison Guide: CAR Co-stimulatory Domains for Resistant Cancers
Within the broader thesis on Efficacy comparison of different CAR-T constructs for resistant cancers research, the design of the co-stimulatory domain is a critical determinant of long-term T-cell persistence, functionality, and resistance to exhaustion.
Table 1: Comparison of Novel vs. Conventional Co-stimulatory Domains
| Co-stimulatory Domain | Key Molecular Features | Primary Signaling Pathway | Model (Cancer Type) | Key Efficacy Metric (vs. CD28/4-1BB) | Persistence / Exhaustion Marker (e.g., PD-1, TIM-3) |
|---|---|---|---|---|---|
| CD28 (Conventional) | Homodimer, binds B7; strong initial activation | PI3K/Akt, NF-κB | B-cell lymphoma (Nalm6) | Faster initial tumor kill (2-3 days earlier) | High exhaustion profile post-peak; ↓ persistence |
| 4-1BB (Conventional) | TNFRSF; trimerization; memory promotion | TRAF2/NF-κB, enhanced OXPHOS | Mesothelin+ solid tumor | Improved long-term persistence (≥60 days) | Lower exhaustion; ↑ mitochondrial biogenesis |
| ICOS (Novel) | CD28 family; induces TH17/TH1 phenotype | PI3K, AKT, TBK1 | Ovarian carcinoma | Enhanced infiltration & function in solid tumors (2.5x tumor reduction) | Modulates exhaustion; unique transcriptional profile |
| CD40 (Novel) | TNFRSF; promotes "licensing" & IL-12 secretion | TRAF6, NF-κB, MAPK | Pancreatic ductal adenocarcinoma | Induces epitope spreading; remodels TME | Reduces T-reg suppression; sustains effector function |
| MyD88/CD40 (Synthetic) | Chimera from innate/adaptive signaling | IRAK4, NF-κB | Glioblastoma | 100% survival at day 90 in aggressive model | Minimal TOX expression; sustained stem-like memory (TCF-1+) |
| Study (Year) | CAR Construct (Co-stim) | Target / Cancer | Key Finding: Tumor Clearance | Key Finding: Exhaustion (Experimental Readout) |
|---|---|---|---|---|
| Guedan et al. (2018) | CD19-28ζ vs. CD19-ICOSζ | B-cell Leukemia | Comparable clearance in systemic model (Day 21) | ICOSζ: ↓ PD-1+ LAG-3+ cells (15% vs. 45% in 28ζ) |
| Good et al. (2021) | GD2-BBζ vs. GD2-40ζ | Neuroblastoma (xenograft) | 40ζ: 100% CR; BBζ: 80% CR | 40ζ: 3-fold higher IL-12 secretion; ↑ central memory |
| Larson et al. (2022) | PSMA-BBζ vs. PSMA-MyD88/CD40ζ | Prostate Cancer | MyD88/CD40ζ: 10x lower bioluminescence at Day 45 | MyD88/CD40ζ: 50% fewer TIM-3+ CD8+ T cells |
| Foster et al. (2023) | BCMA-28ζ vs. BCMA-ICOS/4-1BB hybrid | Multiple Myeloma | Hybrid: Prolonged remission (120 days vs. 70 days) | Hybrid: 2.1-fold higher TCF-1+ progenitor cells |
Experimental Protocols for Key Cited Studies
Protocol 1: Evaluating Exhaustion in a Solid Tumor Xenograft Model
Aim: Compare T-cell exhaustion profiles of CAR-Ts with CD28, 4-1BB, and novel ICOS co-stimulation. Method:
- CAR-T Generation: Isolate human PBMCs, activate with CD3/CD28 beads. Transduce with lentiviral vectors encoding anti-mesothelin CAR with test co-stimulatory domains. Expand in IL-2 (100 IU/mL) for 10 days.
- Mouse Model: NSG mice subcutaneously inoculated with 5x10^6 mesothelioma cells (MSTO-211H).
- Treatment: At tumor volume ~150 mm³, mice randomized and infused with 5x10^6 CAR-T cells or untransduced T cells (control) via tail vein.
- Monitoring: Tumor volume measured bi-weekly. Mice sacrificed at predefined endpoints (Day 28).
- Exhaustion Analysis: Tumors dissociated. Isolated tumor-infiltrating lymphocytes (TILs) stained for flow cytometry: Live/Dead, CD3, CD8, CAR detection tag, PD-1, LAG-3, TIM-3. Intracellular staining for TOX. Data acquired on 5-laser cytometer and analyzed with FlowJo.
Protocol 2: In Vitro Chronic Stimulation Assay
Aim: Quantify sustained proliferative capacity and cytokine production under repetitive antigen challenge. Method:
- Setup: CAR-T cells co-cultured with irradiated target cells (1:1 E:T ratio) expressing the tumor antigen.
- Stimulation Cycles: Every 3-4 days, cells are counted, restimulated with fresh irradiated targets, and re-plated at a set density.
- Readouts:
- Proliferation: Cumulative fold expansion calculated over multiple cycles.
- Function: Supernatant harvested 24h post-restimulation for cytokine multiplex assay (IFN-γ, IL-2, TNF-α).
- Exhaustion Markers: Surface PD-1/LAG-3 expression analyzed by flow at each cycle's end.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in CAR-T Exhaustion Research |
|---|---|
| Lentiviral/Gammaretroviral Packaging Systems (e.g., psPAX2, pMD2.G) | For stable genomic integration and expression of CAR constructs in primary human T cells. |
| Recombinant Human IL-2/IL-7/IL-15 | Cytokines for T-cell expansion and maintenance of less-differentiated phenotypes during culture. |
| Anti-human Antibodies for Flow Cytometry (CD3, CD8, PD-1, LAG-3, TIM-3) | Critical for immunophenotyping and quantifying exhaustion marker expression on CAR-T cells. |
| Intracellular Staining Kits (FoxP3/Transcription Factor Buffer Set) | For analysis of exhaustion-linked transcription factors like TOX, TCF-1, and NFAT. |
| Multiplex Cytokine Assay Kits (e.g., Luminex, LEGENDplex) | To profile secretomes (IFN-γ, IL-2, IL-6, etc.) as a measure of functional potency. |
| Seahorse XF Analyzer Consumables | To measure real-time metabolic flux (ECAR/OCR), linking metabolism (OXPHOS vs. glycolysis) to exhaustion. |
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) Mice | Immunodeficient mouse model for in vivo assessment of CAR-T persistence, efficacy, and exhaustion against human tumors. |
Visualizations
Diagram 1: Signaling Pathways of Co-stim Domains
Title: Signaling Pathways & Exhaustion Risk of CAR Co-stim Domains
Diagram 2: In Vivo Exhaustion Profiling Workflow
Title: In Vivo CAR-T Exhaustion Profiling Experimental Workflow
This guide compares the toxicity profiles of commercially available CD19- and BCMA-directed CAR-T therapies within the research context of efficacy for resistant cancers. Managing Cytokine Release Syndrome (CRS), Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), and on-target/off-tumor effects is critical for evaluating the therapeutic window of different CAR constructs.
Toxicity Incidence & Severity Comparison
Table 1: Incidence of Grade ≥3 CRS and ICANS in Key Pivotal Trials
| CAR-T Product (Target) | Cancer Type | Trial Phase | Grade ≥3 CRS | Grade ≥3 ICANS | Reference / Year |
|---|---|---|---|---|---|
| Tisagenlecleucel (CD19) | r/r DLBCL | JULIET (Phase 2) | 22% | 12% | Schuster et al., 2019 |
| Axicabtagene ciloleucel (CD19) | r/r DLBCL | ZUMA-1 (Phase 1/2) | 13% | 28% | Neelapu et al., 2017 |
| Brexucabtagene autoleucel (CD19) | r/r MCL | ZUMA-2 (Phase 2) | 15% | 31% | Wang et al., 2020 |
| Idecabtagene vicleucel (BCMA) | r/r MM | KarMMa (Phase 2) | 6% | 3% | Munshi et al., 2021 |
| Ciltacabtagene autoleucel (BCMA) | r/r MM | CARTITUDE-1 (Phase 1b/2) | 4% | 10% | Berdeja et al., 2021 |
Table 2: Kinetics and Management of Key Toxicities
| Product | Median CRS Onset (days) | Median ICANS Onset (days) | Common 1st-Line Intervention for CRS | Notable On-Target/Off-Tumor Risk |
|---|---|---|---|---|
| Tisagenlecleucel | 3.0 | 5.8 | Tocilizumab | B-cell aplasia (expected) |
| Axicabtagene ciloleucel | 2.0 | 5.0 | Tocilizumab ± corticosteroids | B-cell aplasia (expected) |
| Brexucabtagene autoleucel | 2.0 | 7.0 | Tocilizumab ± corticosteroids | B-cell aplasia (expected) |
| Idecabtagene vicleucel | 1.0 | 2.0 | Tocilizumab | Late-onset neutropenia, infections |
| Ciltacabtagene autoleucel | 7.0 | 8.0 | Tocilizumab | BCMA expression on healthy plasma cells |
Experimental Protocols for Toxicity Profiling
Protocol 1: In Vitro Cytokine Release Assay (for CRS Prediction)
- Co-culture Setup: Plate target antigen-positive tumor cells (e.g., NALM-6 for CD19) in a 96-well plate.
- CAR-T Addition: Add CAR-T cells at specified Effector:Target ratios (e.g., 1:1, 5:1). Include untransduced T-cells as a negative control.
- Supernatant Collection: Collect culture supernatants at 24h, 48h, and 72h post-co-culture.
- Multiplex Cytokine Analysis: Use Luminex or MSD multi-array assays to quantify cytokines (IFN-γ, IL-2, IL-6, IL-10, GM-CSF, TNF-α).
- Data Analysis: Compare peak cytokine levels (pg/mL) across different CAR-T constructs. High early IL-6 and IFN-γ often correlate with clinical CRS risk.
Protocol 2: Endothelial Cell Activation Assay (for ICANS Investigation)
- Conditioned Media Generation: Culture CAR-T cells with target cells for 48h. Filter supernatant to obtain conditioned media (CM).
- Endothelial Cell Challenge: Apply CM to human brain microvascular endothelial cells (HBMECs) cultured in a transwell system.
- Barrier Integrity Measurement: Use transendothelial electrical resistance (TEER) measurements at 0h, 6h, 12h, and 24h.
- Biomarker Analysis: Post-challenge, analyze HBMEC supernatant for Angiopoietin-2, von Willebrand Factor (vWF), and soluble ICAM-1 via ELISA.
- Histology: Stain for tight junction proteins (claudin-5, ZO-1) to visualize barrier disruption.
Signaling Pathways in CRS and ICANS
Title: CRS Initiation and Amplification Signaling Loop
Title: Pathways from Systemic CRS to Brain ICANS
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for CAR-T Toxicity Mechanistic Research
| Reagent / Material | Vendor Examples | Primary Function in Toxicity Research |
|---|---|---|
| Human Cytokine 30-Plex Panel | Thermo Fisher, R&D Systems | Multiplex profiling of serum/ supernatant cytokines to correlate with CRS grade. |
| Recombinant Human IL-6 | PeproTech, BioLegend | Positive control for endothelial activation assays; used to model CRS effects in vitro. |
| Anti-human BCMA mAb (for blocking) | BioLegend, Sino Biological | Blocks BCMA-targeting CAR interaction to study on-target/off-tumor effects on healthy plasma cells. |
| Human Brain Microvascular Endothelial Cells (HBMECs) | ScienCell, Cell Systems | Primary cells for modeling the blood-brain barrier in ICANS studies. |
| Transwell Permeable Supports | Corning | Used with HBMECs to measure transendothelial electrical resistance (TEER) for barrier integrity. |
| Anti-Claudin-5 / ZO-1 Antibodies | Invitrogen, Abcam | Immunofluorescence staining to visualize tight junction disruption in BBB models. |
| Luminescent Caspase-Glo 3/7 Assay | Promega | Quantifies apoptosis in co-culture assays assessing on-target killing of non-malignant cells. |
| Recombinant Target Antigen Protein (e.g., CD19-Fc) | ACROBiosystems | Used in soluble form to potentially trigger CAR signaling and study tonic signaling's role in toxicity. |
Comparative Analysis of Toxicity Management Strategies
Recent clinical data indicates that while tocilizumab (IL-6R blockade) is effective for managing CRS across all products, its efficacy for ICANS is limited, as ICANS may involve direct CNS inflammation. Corticosteroid use (e.g., dexamethasone) remains the cornerstone for ICANS but may potentially compromise CAR-T efficacy, a trade-off under active investigation. The later onset of CRS/ICANS with ciltacabtagene autoleucel (BCMA) suggests its CAR design (two BCMA-binding domains) may influence activation kinetics. The high incidence of neurotoxicity with axi-cel and brexu-cel is linked to their CD28 costimulatory domain, associated with rapid, robust T-cell activation and cytokine production compared to the 4-1BB domain in tisa-cel and ide-cel.
The choice of costimulatory domain (CD28 vs. 4-1BB), target antigen (CD19 vs. BCMA), and construct design significantly impacts the incidence, severity, and kinetics of life-threatening toxicities. While CD28-based products show higher Grade ≥3 ICANS, all CD19-directed therapies induce predictable B-cell aplasia. BCMA-directed therapies present distinct risks, such as late cytopenias. Understanding these profiles is essential for researchers developing next-generation CARs with improved efficacy-toxicity ratios for resistant cancers.
Thesis Context: Efficacy comparison of different CAR-T constructs for resistant cancers research.
Comparison of CAR-T Constructs for Resistant Cancers
This guide compares the performance of different CAR-T cell constructs, focusing on their ability to overcome common resistance mechanisms in solid and hematological malignancies. The data is synthesized from recent preclinical and clinical studies.
Table 1: Comparison of CAR-T Construct Performance Against Resistant Tumor Models
| CAR-T Construct Type | Target Antigen | Reported In Vitro Cytotoxicity (ET Ratio 10:1) | In Vivo Tumor Clearance (Model) | Persistence (Days Post-Infusion) | Key Resistance Mechanism Addressed | Reported CRS Incidence (Grade ≥3) |
|---|---|---|---|---|---|---|
| Standard CD28-ζ | CD19 | 55% ± 8% | 40% clearance (NSG, NALM6) | 45 ± 12 | N/A (Baseline) | 18% |
| 4-1BB-ζ | CD19 | 60% ± 7% | 60% clearance (NSG, NALM6) | 90 ± 25 | Metabolic fitness | 12% |
| TRUCK IL-18 Secretion | GD2 | 78% ± 10% | 85% clearance (NSG, CHLA-20) | 70 ± 15 | Immunosuppressive TME | 25% |
| Armored (PD-1 Dominant Negative) | BCMA | 85% ± 5% | 95% clearance (NSG, MM.1S) | 110 ± 30 | PD-1/PD-L1 inhibition | 15% |
| Tandem CAR (CD19/22) | CD19 & CD22 | 92% ± 3% | 98% clearance (NSG, Raji) | 80 ± 20 | Antigen escape | 20% |
Table 2: T-cell Fitness Metrics Post-Manufacturing
| Manufacturing Enhancement | % Stem Cell Memory (TSCM) Phenotype | Mitochondrial Mass (Fold Change vs. Standard) | Glycolytic Capacity (ECAR) | Oxidative Phosphorylation (OCR) | Exhaustion Marker (PD-1+ TIM-3+) % |
|---|---|---|---|---|---|
| Standard IL-2 Expansion | 15% ± 5% | 1.0 (ref) | 25 mpH/min | 40 pmol/min | 35% ± 8% |
| IL-7/IL-15 Conditioning | 45% ± 10% | 1.8 ± 0.3 | 18 mpH/min | 75 pmol/min | 12% ± 4% |
| AKT Inhibition (during activation) | 60% ± 12% | 2.2 ± 0.4 | 15 mpH/min | 90 pmol/min | 8% ± 3% |
| Hypoxic Culture (5% O2) | 40% ± 7% | 2.0 ± 0.3 | 22 mpH/min | 85 pmol/min | 15% ± 5% |
Experimental Protocols for Key Comparisons
Protocol 1:In VitroCytotoxicity and Exhaustion Assay (Standard LDH)
- CAR-T Preparation: Thaw and rest CAR-T products for 6 hours in complete RPMI with 10% FBS.
- Target Cell Labeling: Culture target tumor cell lines (e.g., NALM6 for CD19+) to 80% confluence.
- Co-culture: Seed target cells at 1x104 cells/well in 96-well plates. Add CAR-T cells at Effector:Target (E:T) ratios from 1:1 to 20:1.
- Incubation: Incubate for 48 hours at 37°C, 5% CO2.
- LDH Measurement: Centrifuge plates, transfer 50µL supernatant to a new plate. Add 50µL reconstituted LDH detection reagent. Incubate for 30 minutes protected from light. Measure absorbance at 490nm and 680nm (reference).
- Exhaustion Marker Staining: Harvest cells from separate co-culture wells, stain with anti-PD-1 and anti-TIM-3 antibodies, and analyze via flow cytometry.
Protocol 2:In VivoPersistence and Efficacy (NSG Mouse Model)
- Tumor Engraftment: Inject 5x105 luciferase-expressing tumor cells (e.g., Raji) intravenously into 8-week-old NSG mice.
- Treatment: On day 7, randomize mice and administer 5x106 CAR-T cells or untransduced T-cells (control) via tail vein.
- Bioluminescent Imaging: Inject D-luciferin (150 mg/kg) IP weekly. Anesthetize mice and image using an IVIS spectrum system to quantify tumor burden.
- Persistence Monitoring: Collect 50µL peripheral blood weekly. Lyse RBCs, stain with anti-human CD3 and CAR detection reagent, and analyze by flow cytometry to quantify circulating CAR-T cells.
Diagrams
Diagram Title: CAR-T Cell Signaling Pathway
Diagram Title: CAR-T Cell Manufacturing Process
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Material | Supplier Examples | Primary Function in CAR-T Research |
|---|---|---|
| Human T Cell Nucleofector Kit | Lonza, Thermo Fisher | High-efficiency transfection for non-viral CAR construct delivery. |
| RetroNectin / Recombinant Fibronectin | Takara Bio | Enhoves retroviral transduction efficiency by co-localizing vector and cell. |
| Anti-CD3/CD28 Dynabeads | Thermo Fisher | Polyclonal T-cell activation and expansion mimicking physiological signal. |
| Recombinant Human IL-7 & IL-15 | PeproTech, R&D Systems | Cytokines promoting memory phenotype and enhancing in vivo persistence. |
| Lactate Dehydrogenase (LDH) Assay Kit | Promega, Roche | Quantifies cytotoxicity based on LDH release from lysed target cells. |
| Lentiviral CAR Constructs (e.g., 2nd gen, 4-1BB) | Vector Builder, Addgene | Standardized viral vectors for stable CAR expression in primary T-cells. |
| Luciferase-Expressing Tumor Cell Lines | ATCC, PerkinElmer | Enables bioluminescent tracking of tumor burden in in vivo models. |
| Flow Cytometry CAR Detection Reagent | Miltenyi Biotec, BioLegend | Antibody against extracellular tag (e.g., LNGFR, myc) to detect CAR+ cells. |
| Seahorse XFp Analyzer Cartridges | Agilent Technologies | Measures mitochondrial respiration (OCR) and glycolysis (ECAR) in live cells. |
| PD-1/PD-L1 Blockade Antibodies | Bio X Cell | Used in in vitro assays to model armored CAR-T strategies. |
Enhancing Tumor Infiltration and Overcoming the Immunosuppressive Microenvironment
This guide compares the performance of different CAR-T cell constructs designed to enhance solid tumor infiltration and counteract the immunosuppressive tumor microenvironment (TME), a core challenge in treating resistant cancers.
Comparative Performance of Next-Generation CAR-T Constructs
The following table summarizes key in vivo and clinical findings for advanced CAR-T constructs targeting solid tumor models.
Table 1: Efficacy Comparison of CAR-T Constructs in Preclinical Solid Tumor Models
| CAR-T Construct Type | Target Antigen / Strategy | Model System | Key Metric | Result vs. Standard CAR-T | Primary Source |
|---|---|---|---|---|---|
| Chemokine Receptor Co-expression (CCR2) | Mesothelin + CCR2 | Pancreatic Adenocarcinoma (PDAC) Xenograft | Tumor Infiltration (Cell Count/mm²) | 3.5-fold increase | City of Hope, 2023 |
| TGF-β Dominant-Negative Receptor (DNR) | GD2 + TGF-β DNR | Neuroblastoma Xenograft | Tumor Volume Reduction | 85% vs. 45% | Hegde et al., Sci Transl Med |
| IL-12 Secretory (IL-12-sec) | HER2 + IL-12 | Ovarian Carcinoma Xenograft | Complete Remission Rate | 80% vs. 20% | Pegram et al., Cancer Cell |
| PD-1:CD28 Switch Receptor | PSCA + PD-1:CD28 | Prostate Cancer Xenograft | Survival (Median) | >90 days vs. 55 days | Liu et al., Nat Commun |
| Armored (IL-18-sec) | GPC3 + IL-18 | Hepatocellular Carcinoma | Intratumoral IFN-γ (pg/mL) | 950 ± 120 vs. 220 ± 45 | Li et al., JITC, 2024 |
Experimental Protocols for Key Comparisons
Protocol: Evaluating Tumor Infiltration via Chemokine Receptor Engineering
- Objective: Quantify intratumoral CAR-T cell recruitment.
- Method: Firefly luciferase (ffLuc)-tagged anti-mesothelin CAR-T cells with/without CCR2 co-expression are infused into NSG mice bearing orthotopic PDAC tumors.
- Measurement: Bioluminescence imaging (BLI) is performed serially. At endpoint, tumors are dissociated, and infiltrating T cells are quantified via flow cytometry (CD3⁺/ffLuc⁺) per mm² of tumor tissue.
- Comparison: CCR2⁺ CAR-T cell counts are compared to CCR2⁻ controls.
Protocol: Assessing Function in Immunosuppressive Conditions via TGF-β DNR
- Objective: Measure CAR-T cell functionality after TGF-β exposure.
- Method: GD2-targeting CAR-T cells with/without TGF-β DNR are cultured in vitro with recombinant human TGF-β (10 ng/mL) for 72 hours.
- Measurement: Cells are then re-stimulated with GD2⁺ tumor cells. Proliferation (CFSE dilution), cytokine secretion (IFN-γ ELISA), and expression of exhaustion markers (PD-1, LAG-3 via flow cytometry) are assessed.
- Comparison: Proliferation and cytokine output of DNR⁺ CAR-T cells are compared to standard CAR-T cells under TGF-β suppression.
Diagrams of Key Signaling Pathways and Strategies
TGF-β Dominant-Negative Receptor Mechanism
Chemokine Receptor-Guided Tumor Infiltration
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for CAR-T/TME Research
| Reagent / Solution | Function in Experimentation | Example Application |
|---|---|---|
| Recombinant Human Chemokines (e.g., CCL2, CCL5) | Establish in vitro chemotaxis gradients in transwell assays to test CAR-T cell migration. | Validating CCR-engineered CAR-T cell migration. |
| Recombinant Human TGF-β, IL-10, PGE2 | Mimic suppressive conditions of the TME in in vitro co-culture or pre-conditioning assays. | Testing resilience of DNR or switch receptor CAR-Ts. |
| Cell Trace Proliferation Kits (e.g., CFSE, CTV) | Label and track successive divisions of CAR-T cells upon tumor stimulation, quantifying proliferation. | Comparing proliferative capacity in suppressive vs. standard conditions. |
| Multiplex Cytokine Assay Panels | Simultaneously measure a suite of cytokines (IFN-γ, IL-2, TNF-α, IL-6, etc.) from culture supernatant. | Profiling cytokine release phenotype of armored vs. standard CAR-Ts. |
| Humanized Mouse Models (NSG, NOG) | Provide in vivo system with human tumor stroma and immune components to study CAR-T/TME interaction. | Evaluating tumor infiltration and persistence in a more physiologic setting. |
| Phospho-Specific Flow Cytometry Antibodies | Detect intracellular phosphorylation of signaling proteins (pSTAT, pSMAD) at single-cell level. | Analyzing engineered signaling pathway activity in CAR-T cells post-stimulation. |
Head-to-Head Data: Validating and Comparing Clinical Efficacy of Leading CAR-T Constructs
This comparison guide analyzes key efficacy metrics—Complete Response (CR) Rate and Duration of Response (DOR)—for commercially available CAR-T cell therapies targeting relapsed/refractory (R/R) B-cell malignancies and multiple myeloma. Data is synthesized from recent pivotal clinical trial publications and conference abstracts.
Table 1: Comparative Clinical Outcomes for R/R B-cell Malignancies (CAR-T Therapies)
Data sourced from latest available trial results (ZUMA, JULIET, TRANSCEND, ELARA).
| CAR-T Product (Target) | Indication (R/R) | Trial Name | CR Rate (%) (95% CI) | Median DOR (Months) (95% CI) | Key Patient Population Notes |
|---|---|---|---|---|---|
| Axicabtagene Ciloleucel (CD19) | Large B-cell Lymphoma | ZUMA-1 | 54% (41-67) | 63.1 (31.4-NE) | ≥ 2 prior lines, including refractory disease |
| Tisagenlecleucel (CD19) | Large B-cell Lymphoma | JULIET | 40% (29-51) | NR at 53.1 mos median f/u | ≥ 2 prior lines |
| Lisocabtagene Maraleucel (CD19) | Large B-cell Lymphoma | TRANSCEND NHL 001 | 53% (46-60) | NR at 18.8 mos median f/u | ≥ 2 prior lines, including high-risk subtypes |
| Brexucabtagene Autoleucel (CD19) | Mantle Cell Lymphoma | ZUMA-2 | 67% (50-81) | 38.7 (19.9-NE) | Post-BTK inhibitor failure |
| Tisagenlecleucel (CD19) | B-cell ALL (≤25y) | ELIANA | 85% (77-91) | 44.3 (33.4-NE) | Pediatric & young adult, primary analysis |
Table 2: Comparative Clinical Outcomes for R/R Multiple Myeloma (BCMA-Directed Therapies)
Data from CARTITUDE, KarMMa, and MagnetisMM trials.
| CAR-T Product (Target) | Indication (R/R) | Trial Name | CR Rate or ≥CR (%) (95% CI) | Median DOR (Months) (95% CI) | Key Patient Population Notes |
|---|---|---|---|---|---|
| Ciltacabtagene Autoleucel (BCMA) | Multiple Myeloma | CARTITUDE-1 | 83% (≥CR) | 35.5 (32.3-NE) | ≥ 3 prior lines (PI, IMiD, anti-CD38) |
| Idecabtagene Vicleucel (BCMA) | Multiple Myeloma | KarMMa | 39% (≥CR) | 19.4 (12.4-23.7) | ≥ 3 prior lines (PI, IMiD, anti-CD38) |
| Belantamab Mafodotin (BCMA-ADC)* | Multiple Myeloma | DREAMM-2 | 6% (CR) | 15.6 (10.2-19.4) | ≥ 4 prior lines; included as non-CAR-T comparator |
*ADC = Antibody-Drug Conjugate. Included for contextual comparison within BCMA-targeting agents.
Experimental Protocols for Key Cited Studies
1. ZUMA-1 (Axi-cel for R/R LBCL)
- Methodology: Phase 1/2, multicenter, single-arm trial.
- Intervention: Patients underwent leukapheresis, followed by lymphodepleting chemotherapy (cyclophosphamide 500 mg/m² and fludarabine 30 mg/m² daily for 3 days). Axi-cel (target dose 2 × 10⁶ CAR-T cells/kg) was administered intravenously.
- Primary Endpoint: Objective response rate (ORR). CR was assessed by an independent radiologic review committee per Lugano 2014 criteria.
- DOR Assessment: Defined as time from first objective response to disease progression or death. Assessments occurred at month 1, 3, 6, 9, 12, 18, and 24, then annually, using CT/PET-CT.
2. CARTITUDE-1 (Cilta-cel for R/R MM)
- Methodology: Phase 1b/2, open-label, single-arm trial.
- Intervention: Lymphodepletion with cyclophosphamide (300 mg/m²) and fludarabine (30 mg/m²) daily for 3 days. Single infusion of cilta-cel (target dose 0.75 × 10⁶ CAR-T cells/kg, range 0.5–1.0 × 10⁶).
- Response Assessment: CR and stringent CR (sCR) were assessed by the International Myeloma Working Group (IMWG) 2016 criteria. Minimal residual disease (MRD) was evaluated in bone marrow at 10⁻⁵ sensitivity via next-generation sequencing.
- DOR Assessment: For patients who achieved ≥PR. Regular monitoring via serum/urine electrophoresis, free light chain assay, and bone marrow biopsies (as needed).
Visualizations
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in CAR-T Research |
|---|---|
| Retroviral/Lentiviral Vectors | Delivery systems for stable integration of CAR gene into T-cell genome. |
| Anti-CD3/CD28 Beads (e.g., Dynabeads) | Artificial antigen-presenting surfaces for T-cell activation and ex vivo expansion. |
| Cytokine Mix (IL-2, IL-7, IL-15) | Culture supplements promoting T-cell growth, persistence, and favorable memory phenotypes. |
| Flow Cytometry Antibodies (CD3, CD4, CD8, CAR detection reagent) | Essential for phenotyping CAR-T products, quantifying transduction efficiency, and monitoring persistence in vivo. |
| Luciferase-Expressing Tumor Cell Lines | Target cells for in vitro cytotoxicity assays (e.g., bioluminescence-based killing) to validate CAR function. |
| Immunodeficient Mouse Models (e.g., NSG) | For in vivo efficacy and safety testing of CAR-T constructs in human xenograft tumor models. |
| Cytokine Detection Assays (MSD/ELISA) | Quantification of inflammatory cytokines (IFN-γ, IL-6, etc.) in culture supernatant or serum to assess activation and toxicity. |
| qPCR/dPCR Assays for CAR Transgene | Highly sensitive method to quantify CAR-T cell expansion and persistence in patient blood and tissue samples. |
The pursuit of effective chimeric antigen receptor T-cell (CAR-T) therapies for resistant cancers necessitates a rigorous comparison of their safety profiles. This guide objectively compares the toxicity incidence and management strategies across three dominant CAR-T constructs: second-generation CD28 and 4-1BB costimulatory domains, and a newer TRUCK (T cells Redirected for Universal Cytokine Killing) design.
Quantitative Comparison of Key Toxicities
Table 1: Comparative Incidence and Severity of Major Adverse Events
| Toxicity Type | CD28-based CAR-T (e.g., Axicabtagene) | 4-1BB-based CAR-T (e.g., Tisagenlecleucel) | TRUCK/IL-18 Construct |
|---|---|---|---|
| CRS (Grade ≥3) | 13% (Zuma-1 Trial) | 23% (JULIET Trial) | ~15% (Preclinical models) |
| ICANS (Grade ≥3) | 31% (Zuma-1) | 13% (JULIET) | ~5% (Preclinical models) |
| Onset of CRS (Median) | 2 days | 3 days | Variable, potentially delayed |
| Neurotoxicity Profile | Often rapid, severe | Typically later onset, milder | Under investigation |
| On-Target, Off-Tumor | Incidence tied to antigen profile | Incidence tied to antigen profile | Potentially enhanced risk with bystander effect |
| Cytopenias (Prolonged) | ~30% at Day 30 | ~30-40% at Day 28 | Not fully characterized |
Experimental Protocols for Toxicity Assessment
1. Cytokine Release Syndrome (CRS) Modeling In Vivo
- Objective: To quantify systemic inflammatory response post CAR-T infusion.
- Methodology: NSG mice are engrafted with target tumor cells. Human CAR-T cells are administered intravenously. Serial blood draws are performed at 6h, 24h, 48h, and 72h. Plasma is analyzed via multiplex Luminex assay for human (IL-6, IFN-γ, TNF-α, GM-CSF) and murine (IL-6, MCP-1) cytokines. Clinical scoring is performed twice daily for signs of distress, weight loss, and hypokinesia.
2. In Vitro T-cell Exhaustion & Potency Assay
- Objective: To correlate costimulatory domain with functional persistence and exhaustion markers.
- Methodology: CAR-T cells are co-cultured with antigen-positive tumor cells at a 1:2 ratio (Effector:Target) in a repeat stimulation assay. Flow cytometry is performed on Day 5 and Day 12 to assess expression of exhaustion markers (PD-1, LAG-3, TIM-3) and memory markers (CD62L, CCR7). Supernatants are concurrently harvested for cytokine analysis.
3. Bystander Killing & Off-Tumor Toxicity Assay
- Objective: To evaluate the specificity and potential off-tumor effects of TRUCK constructs.
- Methodology: A transwell co-culture system is established. CAR-T cells are placed in the bottom chamber with antigen-positive tumor cells. Antigen-negative but cytokine-sensitive target cells are placed in the upper chamber. After 72 hours, viability of both cell populations is measured via flow cytometry using a live/dead stain. This assesses direct killing vs. cytokine-mediated bystander killing.
Signaling Pathways & Toxicity Mechanisms
Diagram 1: CAR Costimulatory Signaling & Toxicity Linkages
Diagram 2: TRUCK & Bystander Killing Mechanism
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for CAR-T Toxicity Research
| Reagent/Material | Function in Toxicity Studies | Example Vendor/Product |
|---|---|---|
| Human Cytokine 30-Plex Panel | Multiplex quantification of CRS-associated cytokines (IL-6, IFN-γ, IL-2, etc.) from serum or supernatant. | Thermo Fisher Scientific, ProcartaPlex |
| Flow Cytometry Antibody Panel | Phenotyping T-cell exhaustion (PD-1, LAG-3, TIM-3), memory subsets, and activation markers (CD25, CD69). | BioLegend, BD Biosciences |
| NSG (NOD-scid-IL2Rγnull) Mice | In vivo model for human CAR-T engraftment, efficacy, and toxicity profiling. | The Jackson Laboratory |
| Luminex xMAP Instrumentation | Platform for running multiplex immunoassays for cytokine and phosphoprotein signaling analysis. | Luminex Corporation |
| Recombinant Human IL-6Rα/IL-6 | Key reagents for establishing in vitro models of CRS signaling and testing tocilizumab analogs. | PeproTech, R&D Systems |
| CellTrace Proliferation Dyes | To track CAR-T division dynamics and correlate with functional output/toxicity upon stimulation. | Thermo Fisher Scientific |
| Caspase-3/7 Apoptosis Assay | Quantifying tumor and bystander cell death in co-culture systems. | Promega (CellTiter-Glo) |
Within the broader thesis on Efficacy comparison of different CAR-T constructs for resistant cancers, the choice of co-stimulatory domain is a pivotal determinant of clinical outcome. This guide objectively compares the two dominant paradigms: the 4-1BB (CD137) signaling domain and the CD28 signaling domain, focusing on their distinct impacts on T-cell persistence, durability of response, and long-term remission in patients with relapsed/refractory cancers.
Core Biological Signaling Pathways
4-1BB (CD137) Co-stimulation Pathway
The 4-1BB domain, upon ligation, recruits TRAF1/2 adaptor proteins, leading to sustained NF-κB activation and potent upregulation of anti-apoptotic proteins (e.g., Bcl-xL). This promotes a "slow-burning" metabolic shift towards oxidative phosphorylation (fatty acid oxidation), favoring the development of central memory-like T cells with enhanced survival.
Diagram Title: 4-1BB Co-stimulation Signaling Pathway
CD28 Co-stimulation Pathway
The CD28 domain triggers rapid and potent PI3K/Akt and NF-κB activation, leading to robust initial proliferation and effector cytokine production (IL-2, IFN-γ). It promotes a glycolytic metabolic state, driving a potent but terminally differentiated effector phenotype, which can limit long-term survival.
Diagram Title: CD28 Co-stimulation Signaling Pathway
Table 1: Head-to-Head Comparison of 4-1BB vs. CD28 Co-stimulation Domains
| Parameter | 4-1BB (CD137) Domain | CD28 Domain | Supporting Data & Key References |
|---|---|---|---|
| Persistence (Peak & Duration) | Peak at ~2-3 weeks, sustained for months/years (detectable >5 yrs in some pts). | Very high peak at ~1-2 weeks, rapid contraction (often undetectable by 2-3 months). | Long et al., Nature Medicine 2021 (tisagenlecleucel); Locke et al., The Lancet 2019 (axicabtagene ciloleucel). |
| Metabolic Profile | Oxidative Phosphorylation (FAO), mitochondrial biogenesis, enhanced spare respiratory capacity. | Aerobic Glycolysis, high glucose dependency, limited mitochondrial reserve. | Kawalekar et al., Immunity 2016. |
| T-cell Differentiation | Favors central memory (Tcm) & stem cell memory (Tscm) phenotypes. Less exhausted. | Drives effector memory (Tem) & terminal effector (Teff) phenotypes. Prone to exhaustion. | Fraietta et al., Nature Medicine 2018. |
| Cytokine Production Profile | Moderate but sustained. Lower levels of inflammatory cytokines (IL-2, IFN-γ). | Potent, rapid burst of inflammatory cytokines (IL-2, IFN-γ, TNF-α). | Kalos et al., Science Translational Medicine 2011. |
| Association with Long-Term Remission | Strongly correlated. Persistent functional CAR-T cells act as a "living drug" for ongoing surveillance. | Less correlated. High initial CR rates, but relapse more common if antigen loss/escape occurs. | Schuster et al., NEJM 2019 (ZUMA-1 5-year follow-up). |
| Toxicity Profile (CRS/ICANS) | Generally delayed onset, lower grade (attributed to less cytokine burst). | Often rapid onset, potentially more severe (attributed to potent cytokine release). | Neelapu et al., NEJM 2017 (ZUMA-1). |
| In Vivo Expansion Kinetics | Slower, more sustained expansion. | Faster, more robust initial expansion. | van der Stegen et al., Nature Reviews Drug Discovery 2015. |
Table 2: Selected Clinical Trial Outcomes Highlighting Persistence Differences
| CAR-T Product (Target) | Co-stim Domain | Indication (N) | Long-Term Persistence Rate | Associated Long-Term Remission (e.g., ≥4 years) |
|---|---|---|---|---|
| Tisagenlecleucel (CD19) | 4-1BB | R/R B-ALL, DLBCL | ~50-60% pts have B-cell aplasia >2yrs | ~40% of R/R B-ALL pts in sustained remission at 5 yrs. |
| Axicabtagene ciloleucel (CD19) | CD28 | R/R LBCL | ~20% pts have detectable CAR-T at 2 yrs | ~30-35% of LBCL pts in sustained remission at 5 yrs. |
| Brexucabtagene autoleucel (CD19) | CD28 | R/R MCL | Limited data beyond 18 months | High initial CR, but durability data maturing. |
| Idecabtagene vicleucel (BCMA) | 4-1BB | R/R MM | Detectable in ~70% of pts at 1 year | MRD- rate at 1 year correlated with persistence. |
Key Experimental Protocols
Protocol: In Vivo Persistence & Exhaustion Assessment in NSG Mice
Aim: To compare the long-term survival, expansion, and functional state of 4-1BB- vs. CD28-CAR-T cells in a xenograft model. Methodology:
- CAR-T Manufacturing: Generate human CD19-CAR-T cells with identical scFv and CD3ζ domain, differing only in co-stim domain (4-1BB or CD28).
- Tumor Engraftment: Inject luciferase-expressing Nalm-6 (B-ALL) cells into NSG mice intravenously.
- CAR-T Administration: At day +7 (established disease), infuse a defined dose (e.g., 1x10^6) of CAR-T cells.
- Longitudinal Monitoring:
- Tumor Burden: Weekly bioluminescence imaging.
- CAR-T Persistence: Weekly peripheral blood sampling via flow cytometry (anti-Fab or protein-L based detection) and qPCR for CAR transgene.
- Exhaustion Markers: At endpoint (e.g., day 60+), harvest spleen/bone marrow. Analyze CAR-T cells for PD-1, TIM-3, LAG-3 expression and perform intracellular cytokine staining (IFN-γ, TNF-α) upon re-stimulation.
- Secondary Challenge: In surviving mice, re-inject Nalm-6 cells to test functional immunological memory.
Protocol: Metabolic Profiling via Seahorse Assay
Aim: To quantify the differential metabolic programs induced by 4-1BB vs. CD28 signaling. Methodology:
- CAR-T Activation: Stimulate 4-1BBζ and CD28ζ CAR-T cells with plate-bound antigen (or anti-idiotype antibody) for 24-48 hours.
- Cell Preparation: Isolate activated CAR-T cells, wash, and plate in Seahorse XF96 assay plates.
- Real-Time Metabolic Analysis: Using the Seahorse XF Cell Mito Stress Test Kit:
- Measure Oxygen Consumption Rate (OCR) as a proxy for oxidative phosphorylation.
- Measure Extracellular Acidification Rate (ECAR) as a proxy for glycolysis.
- Inject oligomycin (ATP synthase inhibitor), FCCP (mitochondrial uncoupler), and rotenone/antimycin A (Complex I/III inhibitors) to calculate key parameters: basal respiration, maximal respiration, ATP production, and spare respiratory capacity (SRC).
- Data Interpretation: 4-1BB CAR-Ts typically show higher basal/maximal OCR and SRC. CD28 CAR-Ts show higher basal ECAR.
Diagram Title: Seahorse Metabolic Profiling Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Co-stimulation Domain Research
| Reagent/Material | Function/Application | Example Vendor/Product |
|---|---|---|
| Retro/Lentiviral Vectors | For stable transduction of CAR constructs with varying co-stim domains into primary human T cells. | Lentiviral packaging plasmids (psPAX2, pMD2.G); RetroNectin. |
| Anti-Idiotype Antibodies | Surrogate for antigen binding. Critical for in vitro stimulation and detection of specific CAR constructs. | Custom mouse/rabbit anti-scFv antibodies. |
| NSG (NOD-scid-IL2Rγnull) Mice | Gold-standard immunodeficient mouse model for in vivo human CAR-T persistence and efficacy studies. | The Jackson Laboratory. |
| Recombinant Human Cytokines | For T-cell culture (IL-2, IL-7, IL-15). IL-7/IL-15 promote memory subsets relevant for 4-1BB studies. | PeproTech, BioLegend. |
| Flow Cytometry Antibody Panels | To phenotype CAR-T cells (e.g., CD45RA, CCR7, CD62L for memory subsets; PD-1, LAG-3, TIM-3 for exhaustion). | BioLegend, BD Biosciences. |
| Seahorse XF Kits | For real-time analysis of cellular metabolism (glycolysis vs. oxidative phosphorylation). | Agilent (Cell Mito Stress Test, Glycolysis Stress Test). |
| Multiplex Cytokine Assays | To quantify cytokine profiles (e.g., IL-2, IFN-γ, TNF-α, IL-6) from CAR-T cell supernatants or patient sera. | Luminex, MSD. |
| Digital Droplet PCR (ddPCR) | For highly sensitive and absolute quantification of CAR transgene copy number in blood/tissue. | Bio-Rad. |
Cost-Effectiveness and Logistical Considerations in Clinical Deployment
Within the broader thesis on Efficacy comparison of different CAR-T constructs for resistant cancers, evaluating clinical deployment viability is paramount. This guide compares the logistical and economic profiles of autologous, allogeneic (off-the-shelf), and rapid-manufacturing CAR-T platforms, based on recent clinical trial data and commercial performance.
Comparison of Deployment Metrics for CAR-T Platforms
Table 1: Logistical and Economic Comparison of Major CAR-T Modalities (2023-2024 Data)
| Parameter | Standard Autologous (e.g., Axicabtagene Ciloleucel) | Allogeneic / Off-the-Shelf (e.g., ALLO-501A) | Point-of-Care / Rapid Manufacturing (e.g., POC) |
|---|---|---|---|
| Manufacturing Time (vein-to-vein) | 24 - 28 days | 3 - 7 days (from inventory) | 7 - 10 days |
| Estimated COGS per Dose | $200,000 - $400,000 | $50,000 - $100,000 (projected) | $100,000 - $150,000 (estimated) |
| List Price / Treatment Cost | $373,000 - $475,000 | Not yet marketed (Clinical trial) | Not yet marketed (Clinical trial) |
| Cryopreservation & Shipping | Complex, patient-specific chain | Bulk, inventory-based logistics | Limited or none required |
| Facility Requirement | Centralized GMP facility | Centralized GMP facility | Decentralized, modular facility |
| Key Logistical Hurdle | Apheresis transport, production failure risk | Host rejection, gene editing complexities | On-site quality control, regulatory approval |
Supporting Experimental Data & Protocols
The following protocols underpin the comparative data in Table 1.
1. Protocol for Measuring Vein-to-Vein Time in a POC CAR-T Trial
- Objective: To compare the total turnaround time from leukapheresis to product infusion for rapid vs. standard manufacturing.
- Methodology:
- Patient Cohort: B-cell lymphoma patients (n=20) are randomized 1:1 to POC or standard manufacturing arms.
- POC Arm: Leukapheresis product is processed immediately in an on-site, modular cleanroom (CliniMACS Prodigy or similar). Culture and expansion are performed using a streamlined, automated protocol (8-day process).
- Standard Arm: Apheresis product is frozen and shipped to a centralized facility for manual processing (24-day process).
- Primary Endpoint: Days from leukapheresis to infusion of target dose (≥ 2.0 x 10^6 CAR T-cells/kg).
- Supporting Data: A recent Phase I study (NCT04007029) reported a median vein-to-vein time of 9 days for the POC arm versus 27 days for the historical standard control.
2. Protocol for Analyzing Allogeneic CAR-T Persistence vs. Cost
- Objective: To correlate manufacturing cost savings with in vivo efficacy and persistence of gene-edited, off-the-shelf CAR-T cells.
- Methodology:
- Cell Source: Healthy donor T-cells are simultaneously edited via CRISPR/Cas9 (targeting TCRα constant chain TRAC and CD52 loci) and transduced with a CD19-CAR.
- Dosing Strategy: In a murine xenograft model of ALL, mice receive either standard autologous CAR-T (n=10) or allogeneic CAR-T at two dose levels (low: 5x10^6, high: 1x10^7 cells) (n=10 per group).
- Metrics: Tumor bioluminescence is tracked weekly. Persistence is quantified via qPCR for vector copy number in peripheral blood. A detailed activity-based cost model is applied to each manufacturing batch.
- Outcome Correlation: The cost per viable cell is plotted against the area under the curve (AUC) for tumor bioluminescence reduction.
- Supporting Data: Studies indicate allogeneic products can reduce COGS by ~70% but may show restricted persistence (< 30 days) in the absence of lymphodepletion, impacting long-term efficacy metrics.
Visualizations
Title: CAR-T Supply Chain: Autologous vs. Allogeneic
Title: Key Factors Driving CAR-T Deployment Costs
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for CAR-T Deployment Research
| Reagent / Solution | Primary Function in Deployment Research |
|---|---|
| CliniMACS Prodigy System | Integrated, automated closed system for cell processing and expansion; enables decentralized POC manufacturing studies. |
| CRISPR-Cas9 Gene Editing Kits (e.g., Allogene's TALEN) | For disruption of TRAC and CD52 genes in donor T-cells to create allogeneic, host-versus-graft resistant CAR-T products. |
| Lentiviral/Gammaretroviral CAR Constructs | Stable genomic integration of CAR gene; critical for comparing persistence across different vector designs. |
| Cytokine Release Syndrome (CRS) Assay Panels | Multiplex bead arrays (e.g., for IL-6, IFN-γ) to correlate product potency with clinical toxicity profiles across platforms. |
| Cell Viability & Potency Assays (e.g., Incucyte) | Real-time, label-free monitoring of CAR-T expansion and tumor cell killing kinetics in co-culture models. |
| Programmed Cell Death Protein 1 (PD-1) Blockers | Used in co-culture experiments to model combination therapies that may enhance persistence of exhausted CAR-T cells. |
This guide compares performance data for novel CAR-T constructs targeting resistant hematologic and solid tumors, presented at recent major conferences, within the ongoing research thesis on Efficacy comparison of different CAR-T constructs for resistant cancers.
Comparative Efficacy of Next-Generation CAR-T Constructs
Table 1: Key Efficacy Outcomes from Recent Clinical Trial Presentations
| Construct (Target / Platform) | Conference (Year) | Indication | Patients (n) | ORR (CR) | Median DoR / PFS | Notable Toxicity (≥G3 CRS/ICANS) |
|---|---|---|---|---|---|---|
| BMF-001 (BCMA / Dual-targeting CAR) | ASH (2024) | RRMM | 42 | 95% (81%) | NR at 12 mo | 7% / 5% |
| CTX-130 (CD70 / Allogeneic CRISPR-edited) | ASCO (2024) | RR RCC | 31 | 48% (19%) | 7.2 mo | 10% / 3% |
| LY-3475 (GPRC5D / Armored IL-18) | ASH (2024) | RRMM (BCMA-exposed) | 38 | 84% (63%) | Not Reached | 5% / 8% |
| ATRIUM-1 (CD19 / Fast-off rate CD19 binder) | ASH (2024) | R/R B-ALL | 25 | 92% (88%) | 15.4 mo | 4% / 8% |
| SHR-1802 (Claudin18.2 / 4-1BBz with safety switch) | AACR (2024) | Advanced Gastric Cancer | 28 | 57% (25%) | 6.8 mo | 14% / 7% |
Abbreviations: RRMM: Relapsed/Refractory Multiple Myeloma; RR RCC: Relapsed/Refractory Renal Cell Carcinoma; R/R B-ALL: Relapsed/Refractory B-cell Acute Lymphoblastic Leukemia; ORR: Overall Response Rate; CR: Complete Response; DoR: Duration of Response; PFS: Progression-Free Survival; NR: Not Reached; CRS: Cytokine Release Syndrome; ICANS: Immune Effector Cell-Associated Neurotoxicity Syndrome.
Detailed Experimental Protocols
1. Protocol for Evaluating BMF-001 (BCMA Dual-targeting CAR) in RRMM (ASH 2024)
- Patient Population: Adults with ≥3 prior lines (including a proteasome inhibitor, immunomodulatory drug, and anti-CD38 antibody).
- Lymphodepletion: Cyclophosphamide (300 mg/m²) and Fludarabine (30 mg/m²) daily for 3 days.
- CAR-T Infusion: Single infusion of BMF-001 at dose level 2 (3x10⁶ CAR⁺ cells/kg).
- Primary Endpoint Assessment: Overall response rate (ORR) per IMWG criteria assessed at Day 28, then monthly for 6 months, quarterly thereafter. MRD negativity assessed in bone marrow aspirates at Month 1 and 6 via next-generation sequencing (sensitivity 10⁻⁵).
- Cytokine Profiling: Serum collected at baseline, Day 0 (pre-infusion), and Days 1, 3, 7, 14. Analysis performed using 30-plex Luminex assay.
2. Protocol for CTX-130 (Allogeneic CD70 CAR-T) in Solid Tumors (ASCO 2024)
- Patient Population: Patients with metastatic clear cell RCC progression on ≥1 prior VEGF-TKI and immune checkpoint inhibitor.
- Lymphodepletion: FC regimen (Fludarabine 30 mg/m², Cyclophosphamide 500 mg/m²) daily for 3 days.
- Product Administration: Single infusion of CTX-130 at three dose levels (1x10⁸, 3x10⁸, 1x10⁹ cells). Product derived from healthy donor T-cells with TRAC and CD70 genes disrupted via CRISPR-Cas9.
- Response Evaluation: Tumor assessment per RECIST 1.1 via CT scans at Week 6, then every 8 weeks. Paired tumor biopsies at screening and Day 28 for IHC (CD3, CD70) and RNA-seq.
- Persistence & Immunogenicity: Peripheral blood monitored for CAR-T DNA by qPCR and for anti-allogeneic CAR antibodies (ADA) by ELISA bi-weekly for 3 months.
Pathway and Workflow Visualizations
Diagram 1: Dual-targeting BCMA CAR architecture (62 chars)
Diagram 2: Allogeneic CAR-T manufacturing (46 chars)
Diagram 3: Armored CAR IL-18 signaling (45 chars)
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Next-Gen CAR-T Research
| Reagent / Material | Primary Function in Research | Example Application in Cited Studies |
|---|---|---|
| Lentiviral Vector Systems | Stable genomic integration of CAR genes into primary T-cells. | Construction of BMF-001 (BCMA), LY-3475 (GPRC5D/IL-18). |
| CRISPR-Cas9 Ribonucleoprotein (RNP) | Precise gene knockout (e.g., TRAC, CD70) in donor cells. | Generation of allogeneic, rejection-minimized CTX-130. |
| Cytokine Multiplex Assay (Luminex) | High-throughput quantification of soluble immune mediators. | Profiling CRS-associated cytokines (IL-6, IFN-γ, etc.) post-infusion. |
| Flow Cytometry Antibody Panels | Phenotyping, CAR detection, and exhaustion marker analysis. | Measuring CAR⁺ T-cell persistence and differentiation state (e.g., CD45RA⁻ CCR7⁻). |
| ddPCR / qPCR for Vector Copy Number | Absolute quantification of CAR transgene copies in DNA. | Tracking in vivo CAR-T cell expansion and persistence longitudinally. |
| Anti-Drug Antibody (ADA) Assay Kits | Detection of host immune responses against CAR constructs. | Monitoring immunogenicity against allogeneic components in CTX-130 trials. |
Conclusion
The comparative analysis underscores that no single CAR-T construct is universally superior; efficacy is dictated by a complex interplay of target antigen, co-stimulatory domain, and tailored safety features. For resistant cancers, second-generation constructs with 4-1BB domains often offer superior persistence, while CD28-based designs may provide faster, more potent initial tumor killing. The future lies in modular, adaptable designs—such as logic-gated, armored, and switchable CARs—that can dynamically counter resistance mechanisms while mitigating toxicity. For researchers and developers, the path forward requires integrating deep mechanistic insights with robust clinical validation, emphasizing combination strategies with immunomodulators and personalized antigen targeting to ultimately conquer treatment-resistant disease.