ELISpot Assay in Cancer Immunotherapy: A Complete Guide to Monitoring T-Cell Responses in Research & Clinical Trials
This comprehensive guide explores the ELISpot (Enzyme-Linked Immunospot) assay as a critical tool for monitoring antigen-specific immune responses in cancer research and immunotherapy development.
ELISpot Assay in Cancer Immunotherapy: A Complete Guide to Monitoring T-Cell Responses in Research & Clinical Trials
Abstract
This comprehensive guide explores the ELISpot (Enzyme-Linked Immunospot) assay as a critical tool for monitoring antigen-specific immune responses in cancer research and immunotherapy development. We cover foundational principles of T-cell detection via cytokine secretion, detailed step-by-step methodologies for assay execution, common troubleshooting and optimization strategies for robust data, and a comparative analysis with other immune monitoring techniques like flow cytometry and multiplex ELISA. Tailored for researchers, scientists, and drug development professionals, this article provides actionable insights for implementing ELISpot in preclinical studies and clinical trials to evaluate vaccine efficacy, checkpoint inhibitor responses, and adoptive cell therapies.
ELISpot Fundamentals: How This Assay Detects Cancer-Specific T-Cell Activity
Within the broader thesis on using ELISpot assays to monitor cancer immune responses, visualizing single-cell cytokine secretion represents a cornerstone technology. It enables the quantification of functional, antigen-specific T cells, which is critical for evaluating therapies like immune checkpoint inhibitors, cancer vaccines, and adoptive cell therapies (e.g., CAR-T). Unlike bulk assays, single-cell secretion assays preserve the heterogeneity of the immune response, identifying rare but potent effector cells. Key analytes include:
- IFN-γ: A master regulator of anti-tumor immunity, indicating Th1 and CD8+ cytotoxic T cell activation.
- Granzyme B: A direct mediator of tumor cell apoptosis, released by cytotoxic lymphocytes.
The data generated provides quantitative metrics essential for correlating immunogenicity with clinical outcomes.
Experimental Protocols
Protocol A: Fluorospot (Modified ELISpot) for Dual Cytokine Detection
Principle: This protocol details a dual-color Fluorospot assay for the simultaneous detection of IFN-γ and Granzyme B secreted by single cells, offering higher sensitivity and multiplexing capability than traditional colorimetric ELISpot.
Materials: See "Research Reagent Solutions" table. Workflow:
- Plate Coating: Coat a PVDF-membrane 96-well plate with 100 µL/well of capture antibody cocktail (anti-IFN-γ and anti-Granzyme B) in sterile PBS. Incubate overnight at 4°C.
- Plate Blocking: Aspirate and block with 200 µL/well of complete cell culture medium (e.g., RPMI-1640 + 10% FBS) for 2 hours at 37°C.
- Cell Stimulation & Plating:
- Prepare immune cells (e.g., PBMCs, tumor-infiltrating lymphocytes) from patient samples.
- Stimulate with relevant antigens (e.g., tumor-associated peptide pools, anti-CD3/28 beads, or negative/positive controls).
- Add cells to the pre-washed plate in triplicate at densities from 2.5x10^4 to 2.5x10^5 cells/well. Incubate for 24-48 hours at 37°C, 5% CO₂.
- Cell Removal & Detection: Discard cells and wash plates thoroughly. Add fluorescently conjugated detection antibody pairs (e.g., anti-IFN-γ-Alexa Fluor 488 and anti-Granzyme B-Alexa Fluor 647) diluted in assay buffer. Incubate for 2 hours at room temperature in the dark.
- Analysis: Wash and air-dry plate. Analyze using an automated Fluorospot reader. Software identifies individual spots (representing single cells) and assigns fluorescence channels to differentiate between IFN-γ⁺, Granzyme B⁺, and double-positive cells.
Protocol B: Single-Cell Secretion Capture via Microengraving
Principle: This nanowell-based method captures secreted proteins from individual cells onto a functionalized glass slide for subsequent imaging, allowing for deeper phenotyping of secreting cells.
Workflow:
- Nanowell Array Preparation: A polydimethylsiloxane (PDMS) nanowell array (e.g., 100 µm x 100 µm wells) is placed onto a glass slide pre-coated with capture antibodies.
- Cell Loading: A suspension of stimulated immune cells is seeded onto the array at a limiting dilution, ensuring <20% well occupancy to maximize single-cell resolution.
- Incubation & Secretion Capture: The array is incubated for 4-6 hours, allowing secreted cytokines to be captured on the glass surface directly beneath each well.
- Immunostaining & Imaging: The array is removed, and the slide is stained with fluorescent detection antibodies. High-throughput microscopy (e.g., automated fluorescence scanner) is used to image the capture surface.
- Data Correlation: The same wells can be imaged for cell morphology or subsequently harvested for single-cell RNA sequencing, linking secretion profiles to transcriptional states.
Data Presentation
Table 1: Representative Data from a Dual-Color IFN-γ/Granzyme B Fluorospot Assay in Melanoma PBMC Samples
| Sample Condition | Spots per 2.5x10⁵ PBMCs (Mean ± SD) | Cell Frequency (%) | ||||
|---|---|---|---|---|---|---|
| IFN-γ⁺ | Granzyme B⁺ | Double-Positive | IFN-γ⁺ | Granzyme B⁺ | Double-Positive | |
| No Peptide (Background) | 12 ± 5 | 8 ± 3 | 2 ± 1 | 0.005 | 0.003 | 0.001 |
| MART-1 Peptide Pool | 450 ± 60 | 280 ± 45 | 195 ± 30 | 0.18 | 0.11 | 0.08 |
| Anti-CD3/CD28 (Positive Control) | 1850 ± 210 | 1550 ± 180 | 1420 ± 165 | 0.74 | 0.62 | 0.57 |
Table 2: Comparison of Single-Cell Secretion Assay Platforms
| Parameter | Fluorospot | Microengraving | Flow Cytometry-Based Secretion Assay |
|---|---|---|---|
| Primary Readout | Secretion spots on membrane | Secretion spots on planar surface | Captured analyte on cell surface |
| Multiplexing Capacity | High (4+ plex) | Moderate (2-3 plex) | Low (typically 1-2) |
| Throughput | High (96/384-well) | Low to Moderate | High |
| Recovery of Secreting Cell | No | Yes, for downstream analysis | Yes, for sorting |
| Key Advantage | Standardized, high sensitivity | Links secretion to other single-cell data | Live cell sorting based on secretion |
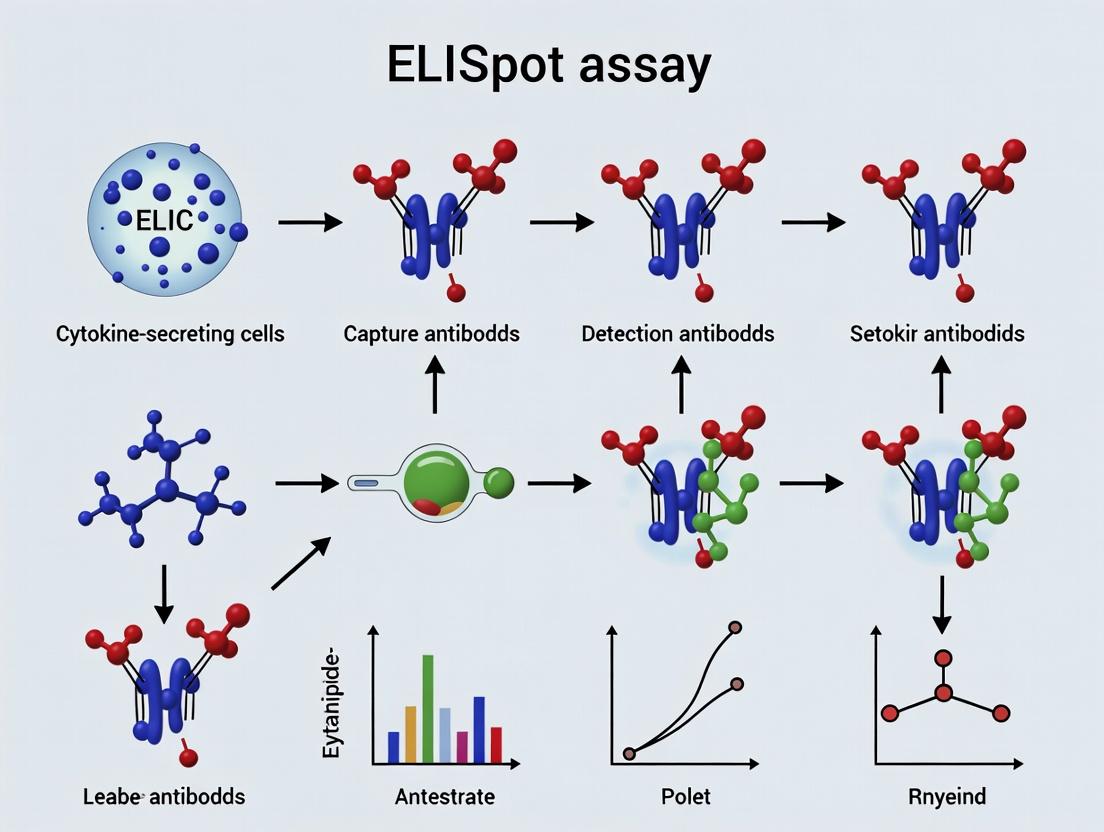
Visualization of Pathways & Workflows
Title: Signaling from TCR Engagement to Cytokine Secretion
Title: Fluorospot Assay Key Steps
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Single-Cell Secretion Assays
| Item | Function & Importance in Context |
|---|---|
| Pre-Coated ELISpot/Fluorospot Plates (PVDF) | Provides a solid-phase matrix for high-efficiency antibody capture; essential for spot localization and clarity. |
| Human IFN-γ/Granzyme B Capture/Detection Ab Pair (Matched) | Antibody pairs validated for lack of cross-reactivity; critical for specific, low-background detection in single-plex or multiplex assays. |
| Cell Culture Medium (Serum-Free/XT) | Used during assay incubation to minimize background secretion and provide defined conditions for cell stimulation. |
| Peptide Pools (e.g., CEF, Viral, Tumor-Associated) | Antigens used to specifically stimulate memory T cells from patient samples; key for measuring antigen-specific responses in cancer immunology. |
| Phorbol Myristate Acetate (PMA)/Ionomycin | Pharmacological T cell stimulators used as a positive control to determine maximum secretory capacity of cells in the assay. |
| Fluorospot Plate Reader & Analysis Software | Automated imaging system with filters for different fluorophores and software to count, size, and assign spots to specific analytes. |
| Polydimethylsiloxane (PDMS) Nanowell Arrays | For micro-engraving methods; physically isolates single cells for correlative secretion and phenotypic analysis. |
| Fluorochrome-Conjugated Secondary Reagents (e.g., Streptavidin-ΔFluor) | High-sensitivity fluorescent detection systems used to amplify signal in Fluorospot assays for low-abundance cytokines. |
Within a research thesis focused on utilizing the ELISpot assay to monitor antigen-specific T-cell responses in cancer immunotherapy, the precise selection and optimization of core components are paramount. The ELISpot assay's power lies in its ability to visualize and quantify functional, cytokine-secreting immune cells at the single-cell level. This provides critical data on the magnitude and quality of vaccine-induced or checkpoint-inhibitor-mediated immune responses. The performance of this assay is fundamentally governed by three key components: the plates, the antibody pair, and the substrate system. This document provides detailed application notes and protocols for these components, incorporating current best practices.
Table 1: Comparison of ELISpot Plate Types
| Plate Type | Surface Coating | Typical Well Density | Key Advantage | Primary Application in Cancer Immune Monitoring |
|---|---|---|---|---|
| PVDF-backed | Hydrophobic Polyvinylidene Fluoride | 96-well | Superior protein binding, high spot clarity and contrast. | High-sensitivity detection of low-frequency antigen-specific T-cells (e.g., neoantigen responses). |
| Nitrocellulose | Nitrocellulose Membrane | 96-well | Very high protein binding capacity. | Detection of high-avidity T-cells secreting large cytokine amounts (e.g., tumor-infiltrating lymphocyte assays). |
| PVDF-bottomed | PVDF Membrane | 96-well | Combines clarity of PVDF with plate rigidity. | Standardized assays for multicenter clinical trial samples. |
| High-Density | PVDF or Nitrocellulose | 384-well | Low sample/reagent consumption, high throughput. | Large-scale epitope mapping or combinatorial peptide screening. |
Table 2: Characteristics of Antibody Pairs for Common Cancer-Immune Cytokines
| Cytokine Target | Typical Capture Ab Concentration (μg/mL) | Typical Detection Ab Concentration (μg/mL) | Critical Function in Cancer Immunity |
|---|---|---|---|
| IFN-γ | 5 - 15 | 0.5 - 2 | Measures Th1/CD8+ T-cell effector function; primary correlate of vaccine efficacy. |
| Granzyme B | 2 - 10 | 0.5 - 1.5 | Direct marker of cytotoxic T-cell and NK cell degranulation/killing potential. |
| Perforin | 5 - 15 | 1 - 2 | Complementary to Granzyme B; indicates cytotoxic machinery. |
| IL-2 | 4 - 10 | 0.5 - 1.5 | Indicates T-cell proliferation and helper function. |
| TNF-α | 4 - 12 | 0.5 - 2 | Pro-inflammatory cytokine from activated T-cells and macrophages. |
Table 3: Substrate Systems for ELISpot
| Substrate Type | Chromogen/Precipitate Color | Sensitivity | Development Time | Key Consideration |
|---|---|---|---|---|
| BCIP/NBT | Dark Purple/Black | Very High | 5-30 minutes | Most common; high contrast; can over-develop. |
| AEC | Red | High | 10-45 minutes | Alcohol-soluble; requires aqueous mounting. |
| Vector VIP | Violet | High | 5-30 minutes | Excellent contrast on white membranes. |
| NovaRED | Red-Brown | High | 5-20 minutes | Alcohol-stable, can be dehydrated & stored. |
Detailed Experimental Protocols
Protocol A: Coating of PVDF Plates with Capture Antibody
- Objective: To immobilize cytokine-specific capture antibodies onto the PVDF membrane.
- Materials: Sterile, 96-well PVDF-backed ELISpot plate, 70% ethanol, sterile PBS, cytokine-specific capture antibody, fetal bovine serum (FBS).
- Procedure:
- Plate Pre-wetting: Under sterile conditions, add 15-25 μL of 70% ethanol per well. Incubate at room temperature (RT) for 1 minute. Immediately aspirate.
- Wash: Wash wells 3x with 200 μL sterile PBS. After final wash, aspirate completely.
- Coating: Dilute capture antibody in sterile PBS to the optimal concentration (e.g., 10 μg/mL for IFN-γ). Add 100 μL per well.
- Incubation: Seal plate and incubate overnight at 4°C or for 2 hours at 37°C in a humidified incubator.
- Blocking: Aspirate antibody solution. Block plates with 200 μL per well of culture medium containing 5-10% FBS for at least 2 hours at 37°C or 30 minutes at 37°C followed by overnight at 4°C.
- Ready for Use: Aspirate blocking solution. Plates can be used immediately or stored dried for later use.
Protocol B: Cell Stimulation and Assay Development
- Objective: To detect and visualize cytokine-secreting cells.
- Materials: Coated/blocked ELISpot plate, patient PBMCs or tumor-derived lymphocytes, peptide pools/antigens, positive control (e.g., PHA), culture medium, detection antibody, Streptavidin-Enzyme conjugate, substrate solution, distilled water, plate reader/imager.
- Procedure:
- Cell Seeding & Stimulation: Add antigens/peptides (e.g., cancer-testis antigens, neoantigen pools) in 100 μL medium. Add cells (e.g., 2.5x10^5 PBMCs/well) in 100 μL medium. Include negative (cells only) and positive (cells + mitogen) controls. Incubate 24-48 hours at 37°C, 5% CO2.
- Cell Removal & Wash: Discard cell suspension. Wash plate 6x with 200 μL PBS-Tween 20 (0.05%) per well using a multichannel pipette or plate washer.
- Detection Antibody: Add biotinylated detection antibody (diluted in PBS/1% BSA) at optimized concentration. Incubate 2 hours at RT or overnight at 4°C.
- Conjugate: Wash plate 3x. Add Streptavidin-Alkaline Phosphatase (or HRP) conjugate. Incubate 1-2 hours at RT.
- Substrate Development: Wash plate 4x. Prepare substrate immediately before use (e.g., BCIP/NBT). Add 100 μL per well. Monitor spot development.
- Reaction Stop: When spots are distinct and background is minimal, stop reaction by rinsing thoroughly with distilled water. Air-dry plate in the dark.
- Analysis: Count spots using an automated ELISpot reader/imaging system. Data expressed as Spot Forming Units (SFU) per million cells.
Visualizations
Title: ELISpot Assay Core Workflow for T-Cell Detection
Title: From T-Cell Activation to ELISpot Signal Generation
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for ELISpot in Cancer Immunotherapy Research
| Item | Function & Importance in Context |
|---|---|
| Human IFN-γ ELISpot Kit | Pre-optimized, matched antibody pair and reagents. Critical for standardized, GLP-compliant analysis of clinical trial samples. |
| Peptide Pools (e.g., CEF, viral, neoantigen) | Antigens for T-cell stimulation. Neoantigen pools are essential for personalized cancer vaccine assessment. |
| RPMI-1640 with 5% Human AB Serum | Preferred culture medium for human PBMCs; reduces background vs. FBS. |
| Cell Counting Kit (e.g., with Trypan Blue) | Accurate determination of viable cell concentration is crucial for SFU normalization. |
| Sterile PBS (Ca/Mg-free) | For wash steps and antibody dilutions. Essential for maintaining cell and assay integrity. |
| Plate Sealer & Sterile Reservoir | Maintains sterility during cell culture incubation and facilitates reagent dispensing. |
| Automated ELISpot Plate Washer | Ensures consistent, thorough washing to reduce background and improve reproducibility. |
| BCIP/NBT Stock Solution | Ready-to-use, stable substrate concentrate for consistent spot development. |
| ELISpot Plate Reader & Analysis Software | For automated, unbiased spot counting and size/intensity analysis. Key for high-throughput studies. |
Within the broader thesis on ELISpot assay for monitoring cancer immune responses, the enumeration of Spot-Forming Units (SFUs) stands as the primary, quantitative readout. It directly correlates with the frequency of antigen-specific T-cells secreting cytokines (e.g., IFN-γ, Granzyme B) in response to tumor-associated antigens (TAAs) or neoantigens. This application note details the protocols and considerations for utilizing SFU data in cancer immunotherapy research and development, from preclinical models to clinical trial immune monitoring.
Key Concepts and Quantitative Data
Table 1: Common Cytokine Targets in Cancer ELISpot and Their Immunological Significance
| Cytokine Detected | Primary T-cell Subset | Significance in Cancer Immune Response | Typical SFU Background (Unstimulated Control) |
|---|---|---|---|
| IFN-γ | CD8⁺ Cytotoxic, Th1 | Indicates cytotoxic potential and Th1-type anti-tumor response. | 0-5 SFU/10⁶ PBMCs |
| Granzyme B | CD8⁺ Cytotoxic | Direct measure of cytotoxic degranulation and target cell killing capability. | 0-3 SFU/10⁶ PBMCs |
| IL-2 | CD4⁺ Helper, Memory | Indicates T-cell activation, proliferation potential, and memory responses. | 0-4 SFU/10⁶ PBMCs |
| TNF-α | CD8⁺, CD4⁺ Th1 | Pro-inflammatory cytokine contributing to tumor cell apoptosis. | 0-5 SFU/10⁶ PBMCs |
| IL-5 / IL-13 | CD4⁺ Th2 | May indicate a non-cytotoxic, pro-tumorigenic response in some contexts. | 0-2 SFU/10⁶ PBMCs |
Table 2: SFU Data Interpretation Criteria in Clinical Trials
| Response Category | Criteria (vs. Baseline or Control) | Implication for Therapy (e.g., Vaccine, Checkpoint Inhibitor) |
|---|---|---|
| Positive Response | ≥2-fold increase AND statistically significant (p<0.05) increase in antigen-specific SFU count. | Suggests induction or enhancement of antigen-specific immunity. |
| Negative Response | No statistically significant change. | Therapy may not be immunogenic for that antigen. |
| Technical Failure | Negative Control wells show high SFU count (>10% of test or >20 SFU/well). | Assay invalid; results cannot be interpreted. |
Experimental Protocols
Protocol 1: Human PBMC ELISpot for Monitoring T-cell Responses to TAAs
Objective: To quantify circulating antigen-specific T-cells from cancer patient blood samples. Materials: See Scientist's Toolkit. Procedure:
- Coating: Coat sterile PVDF-plate with anti-IFN-γ capture antibody (15μg/mL in PBS) overnight at 4°C.
- Blocking: Wash plate 3x with PBS. Block with complete RPMI-1640 + 10% FBS for 2 hours at 37°C.
- Cell Plating & Stimulation: Isolate PBMCs via density gradient centrifugation. Resuspend in complete medium.
- Positive Control: Plate 2.5x10⁵ PBMCs/well + 5μg/mL PHA.
- Test Wells: Plate 2.5x10⁵ PBMCs/well + peptide pools (e.g., NY-ESO-1, MAGE-A3) at 1-2μg/mL per peptide.
- Negative Control: Plate 2.5x10⁵ PBMCs/well + DMSO (peptide solvent) or medium alone.
- Run all conditions in duplicate or triplicate.
- Incubation: Incubate plate for 24-48 hours at 37°C, 5% CO₂ in a humidified incubator.
- Detection: a. Discard cells, wash plate 5x with PBS + 0.05% Tween-20 (PBST). b. Add biotinylated detection antibody (1μg/mL in PBS/1% BSA) for 2 hours at RT. c. Wash 5x with PBST. d. Add Streptavidin-ALP (1:1000 dilution) for 1 hour at RT. e. Wash 5x with PBST, then 2x with PBS.
- Development: Add BCIP/NBT chromogenic substrate. Develop for 5-20 minutes until spots appear. Stop reaction by rinsing with distilled water. Air-dry plate in the dark.
- Analysis: Enumerate SFUs using an automated ELISpot reader. SFU count = (Mean of test wells) - (Mean of negative control wells). Report as SFUs per million PBMCs.
Protocol 2: Murine Splenocyte ELISpot for Preclinical Vaccine Studies
Objective: To assess immunogenicity of cancer vaccines in mouse models. Procedure:
- Follow steps 1-2 from Protocol 1.
- Cell Plating & Stimulation: Prepare single-cell suspension from spleen of vaccinated mice.
- Plate 2-5x10⁵ splenocytes/well.
- Stimulate with vaccine-specific peptides (10μg/mL) or tumor cell lysate (50μg/mL).
- Use ConA (5μg/mL) as positive control, medium as negative control.
- Incubation: Incubate for 24-36 hours (IFN-γ) or 48-72 hours (IL-2).
- Follow steps 5-7 from Protocol 1. Report as SFUs per million splenocytes.
Visualizations
Title: SFU Formation from Antigen Recognition
Title: ELISpot Assay Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Pre-coated IFN-γ/IL-2/etc. ELISpot Plates | Sterile, ready-to-use plates ensure consistency, reduce hands-on time, and minimize variability between labs. Essential for GLP/GCP-compliant clinical trials. |
| Defined Fetal Bovine Serum (FBS) | Supports cell viability during incubation. Must be low in endotoxin and tested for ELISpot performance to avoid high background. |
| Peptide Pools (e.g., CEF, Viral, TAAs) | Positive control pools (CEF/viral) validate assay performance. TAAs (e.g., WT1, Survivin) are used as test stimuli to detect tumor-specific responses. |
| AIM V Serum-Free Medium | Alternative to FBS-containing media. Redances batch-to-batch variability and is ideal for clinical assays where serum components may interfere. |
| Recombinant Human/Murine Cytokines | Used for assay validation and as a standard for detection antibody functionality. |
| Automated ELISpot Plate Reader & Software | Objective, high-throughput spot enumeration. Software distinguishes spots from artifacts and calculates SFU frequency, critical for large-scale studies. |
| Cell Counting Kit (Viability Stain) | Accurate counting of viable PBMCs/splenocytes is crucial for normalizing SFU data (SFU/10⁶ cells). |
| Peptide Solvents (e.g., High-Grade DMSO) | For dissolving synthetic peptides. Must be sterile, endotoxin-free, and used at a final concentration (<0.1%) non-toxic to cells. |
The efficacy of immunotherapies, including checkpoint inhibitors, cancer vaccines, and adoptive T-cell therapies, hinges on the generation and maintenance of robust T-cell responses against tumor antigens. These antigens are broadly classified into Tumor-Associated Antigens (TAAs) – self-proteins overexpressed in tumors – and neoantigens – unique peptides derived from tumor-specific mutations. The Enzyme-Linked Immunospot (ELISpot) assay is a cornerstone technique for monitoring the frequency and functional status of antigen-specific T-cells by quantifying cytokine-secreting cells, providing critical insights into treatment-induced immune responses.
Antigen Classes: TAAs vs. Neoantigens
Table 1: Comparative Overview of Tumor Antigen Classes
| Feature | Tumor-Associated Antigens (TAAs) | Neoantigens |
|---|---|---|
| Origin | Normal self-proteins | Tumor-specific somatic mutations |
| Expression | Overexpressed or re-expressed in tumors | Unique to individual tumors |
| Immunogenicity | Lower (subject to central tolerance) | Higher (bypasses central tolerance) |
| Prevalence | Shared across patients/cancer types | Patient- and tumor-specific |
| Therapeutic Target | "Off-the-shelf" vaccines, TCR therapies | Personalized vaccines, adoptive cell therapy |
| Monitoring Challenge | Low-frequency, potentially anergic T-cells | Requires prior identification of immunogenic mutations |
Key Protocols for ELISpot-Based Monitoring
Protocol 3.1: IFN-γ ELISpot for Detecting Antigen-Specific T-Cells
Purpose: To quantify T-cells secreting IFN-γ in response to specific TAAs or neoantigen peptides.
Materials:
- Pre-coated IFN-γ ELISpot plates (e.g., Human IFN-γ ELISpotPRO, Mabtech)
- RPMI-1640 complete medium
- Peptide pools (15mer peptides overlapping by 11aa for protein TAAs; 15-20mer mutant peptides for neoantigens)
- Positive controls: PHA (5 µg/mL) or CEF/CEFX peptide pools
- Negative control: DMSO/PBS or irrelevant peptide
- Detection antibodies (biotinylated anti-IFN-γ, streptavidin-ALP)
- BCIP/NBT substrate
- ELISpot plate reader
Procedure:
- Plate Preparation: Add 100 µL of complete medium to wells and incubate for 10 min at room temperature. Decant.
- Cell & Antigen Seeding: Isolate PBMCs via density gradient centrifugation. Seed PBMCs (2-5 x 10^5 cells/well) with:
- Test wells: Peptide pools (1-2 µg/mL per peptide) or individual neoantigen peptides.
- Positive control: PHA or CEF pool.
- Negative control: Medium + solvent.
- Incubation: Incubate plates for 24-48 hours at 37°C, 5% CO₂ in a humidified incubator.
- Cell Removal & Detection: Decant cells, wash plates. Add biotinylated detection antibody (1 µg/mL, 2 hours). Add streptavidin-ALP (1 hour). Develop with BCIP/NBT substrate (10-20 min).
- Analysis: Stop reaction with water. Air-dry plates. Count spots using an automated ELISpot reader. Express results as Spot-Forming Cells (SFC) per 10^6 PBMCs.
Data Interpretation: A response is typically considered positive if the mean SFC in test wells is at least 2-fold greater than the mean negative control and exceeds a predefined threshold (e.g., >50 SFC/10^6 PBMCs, with statistical significance, p<0.05).
Protocol 3.2: Multiplex Cytokine ELISpot (IFN-γ & Granzyme B)
Purpose: To simultaneously assess cytotoxic potential (Granzyme B) and Th1 response (IFN-γ) for a more comprehensive functional profile.
Procedure: Follow Protocol 3.1 using dual-color ELISpot kits (e.g., Human IFN-γ/Granzyme B ELISpot, ImmunoSpot). Use distinct enzyme-substrate systems (e.g., ALP/BCIP-NBT for blue spots and HRP/AEC for red spots) for each cytokine. Analyze spots for each color channel separately.
Data Presentation: Quantitative Analysis of T-Cell Responses
Table 2: Example ELISpot Data from a Melanoma Vaccine Trial
| Patient ID | Antigen Type | Peptide Sequence/ID | Pre-Treatment SFC/10^6 PBMCs | Post-Treatment SFC/10^6 PBMCs | Fold Change | p-value |
|---|---|---|---|---|---|---|
| PT-01 | Neoantigen | MUTKRASG12D | 12 | 245 | 20.4 | 0.003 |
| PT-01 | TAA | MART-1 (26-35) | 45 | 120 | 2.7 | 0.04 |
| PT-02 | Neoantigen | MUTTP53R175H | 8 | 15 | 1.9 | 0.32 (NS) |
| PT-02 | TAA | NY-ESO-1 (157-165) | 22 | 310 | 14.1 | 0.001 |
| PT-03 | Negative Control | DMSO | 5 | 8 | 1.6 | 0.45 |
NS: Not Significant. Assay background (negative control) typically <20 SFC/10^6 PBMCs.
Visualizing Pathways and Workflows
Title: Workflow for TAA & Neoantigen-Specific T-Cell Monitoring
Title: T-Cell Activation & ELISpot Detection Principle
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Antigen-Specific ELISpot Monitoring
| Reagent Category | Example Product(s) | Function & Application Notes |
|---|---|---|
| ELISpot Kits | Human IFN-γ ELISpotPLUS (Mabtech), Human IFN-γ Single-Color (Cellular Technology) | Pre-coated plates with capture antibody. Ensure high affinity, low background. |
| Peptide Libraries | PepTivator (Miltenyi), Peptrix (JPT) | Overlapping peptide pools covering full-length TAAs (e.g., NY-ESO-1, MAGE-A3). |
| Neoantigen Peptides | Custom synthesis (Genscript, Pepscan) | 15-20mer peptides containing the mutation, typically >90% purity. |
| Positive Control | CEF/CEFX Ultra Super Stimulus (Cellular Technology), PHA | Stimulates strong T-cell response for assay validation. |
| Cell Culture Medium | ImmunoCult-XF (STEMCELL), TexMACS (Miltenyi) | Serum-free, optimized for human T-cell maintenance during assay. |
| Detection System | ALP/BCIP-NBT, HRP/AEC substrates | Colorimetric development. Dual-color kits allow multiplex cytokine detection. |
| Plate Reader | AID iSpot, ImmunoSpot S6 Ultra (Cellular Technology) | Automated spot counting with size and intensity gating for accuracy. |
| Cell Isolation Kits | Pan T-Cell Isolation Kit (Miltenyi), RosetteSep (STEMCELL) | Isolate specific lymphocyte subsets for precise response analysis. |
Within the field of cancer immunotherapy research, the ELISpot (Enzyme-Linked Immunospot) assay remains a cornerstone for monitoring antigen-specific T-cell responses. This application note contextualizes the assay’s utility within a broader thesis on monitoring cancer immune responses, emphasizing its critical advantages: exceptional sensitivity, true single-cell resolution, and the delivery of functional output. These attributes make it indispensable for evaluating vaccine efficacy, adoptive cell therapy, and immune checkpoint blockade.
Comparative Advantages of Immune Monitoring Assays
The following table quantifies key performance metrics of ELISpot against other common immune monitoring techniques, highlighting its unique position.
Table 1: Comparative Analysis of Immune Monitoring Techniques
| Assay | Sensitivity (Detection Limit) | Single-Cell Resolution | Functional Output Measured | Primary Application in Cancer Immunology |
|---|---|---|---|---|
| ELISpot | 1 in 100,000 – 1 in 1,000,000 PBMCs | Yes | Cytokine secretion (e.g., IFN-γ, Granzyme B) | Detection of rare, antigen-specific T-cells; vaccine response monitoring. |
| Flow Cytometry | ~0.01% of parent population | Yes | Surface markers, intracellular cytokines, proliferation | Phenotypic characterization and polylfunctionality of T-cells. |
| Multiplex ELISA | ~1-10 pg/mL | No | Bulk cytokine concentration in supernatant | Measurement of broad immune signatures and soluble factors. |
| Single-Cell RNA Seq | Individual transcriptome | Yes | Gene expression profile | Deep profiling of immune cell heterogeneity and state. |
| Tetramer Staining | ~0.1% of CD8+ T-cells | Yes (via flow) | T-cell receptor specificity | Frequency of antigen-specific T-cells (non-functional). |
Detailed Protocol: IFN-γ ELISpot for Detecting Tumor Antigen-Specific T-Cells
This protocol is optimized for detecting rare, functional T-cells from patient peripheral blood mononuclear cells (PBMCs) in response to tumor-associated antigens (TAAs).
Day 1: Plate Coating and PBMC Preparation
- Coat Plate: Add 100 µL/well of anti-human IFN-γ capture antibody (clone: 1-D1K) at 15 µg/mL in sterile PBS to a PVDF-backed 96-well microplate. Seal plate and incubate overnight at 4°C.
- Isolate PBMCs: Isolate PBMCs from heparinized blood via density gradient centrifugation (Ficoll-Paque). Count and assess viability using trypan blue (>90% required).
- Prepare Antigens: Reconstitute peptide pools (e.g., NY-ESO-1, MART-1) or single peptides in DMSO and dilute in complete RPMI-1640 media (10% FBS, 1% Pen/Strep, 1% L-Glut). Final DMSO concentration in wells must not exceed 0.1%. Include controls: Positive (PHA, 5 µg/mL), Negative (Media only), and Peptide Solvent (DMSO at 0.1%).
Day 2: Cell Stimulation and Incubation
- Block & Wash Plate: Decant coating antibody. Wash plate 4x with sterile PBS. Block wells with 200 µL/well of complete RPMI-1640 for 2 hours at 37°C, 5% CO₂.
- Seed Cells & Stimulate: After blocking, decant media. Add 100 µL of antigen/control solutions to respective wells in triplicate. Immediately add 100 µL of PBMC suspension (2.5 x 10⁵ cells/well in complete RPMI) for a final density of 2.5 x 10⁵ cells/well. Incubate plate for 24-48 hours at 37°C, 5% CO₂.
Day 3 or 4: Detection and Spot Development
- Discard Cells & Wash: Decant cells and media. Wash plate 6x with PBS, then 3x with PBS-Tween 20 (0.05%).
- Add Detection Antibody: Add 100 µL/well of biotinylated anti-human IFN-γ detection antibody (clone: 7-B6-1) at 1 µg/mL in PBS-1% BSA. Incubate 2 hours at RT.
- Add Streptavidin-Enzyme Conjugate: Wash plate 3x with PBS-T. Add 100 µL/well of Streptavidin-ALP (diluted per manufacturer's instructions in PBS-1% BSA). Incubate 1 hour at RT.
- Add Substrate: Wash plate 4x with PBS. Add 100 µL/well of BCIP/NBT chromogenic substrate. Develop at RT in the dark for 5-20 minutes until spots are distinct.
- Stop Reaction: Rinse plate extensively under tap water to stop development. Air-dry completely in the dark.
Day 4 or 5: Analysis
- Enumerate Spots: Count spots using an automated ELISpot reader. Each spot represents an individual cytokine-secreting cell.
- Data Analysis: Calculate mean spot-forming units (SFU) per triplicate. Antigen-specific response = Mean SFU (antigen well) – Mean SFU (negative control). A positive response is typically defined as ≥2x the negative control SFU and >10 SFU/10⁶ PBMCs.
Visualizations
ELISpot Workflow: From Coating to Spot Formation
Signaling from TCR Engagement to ELISpot Detection
The Scientist's Toolkit: Essential Reagents for ELISpot
Table 2: Key Research Reagent Solutions for ELISpot
| Reagent/Material | Function & Importance |
|---|---|
| PVDF-Backed 96-Well Plates | Membrane backbone for irreversible antibody binding and spot localization. |
| Paired Cytokine Antibodies (Clone 1-D1K/7-B6-1 for IFN-γ) | Matched monoclonal antibody pair for specific, high-affinity capture and detection. |
| Peptide Pools (e.g., CEF, Viral, TAAs) | Antigens to stimulate memory or antigen-specific T-cells. Peptide pools increase breadth of response detection. |
| RPMI-1640 with 10% Fetal Bovine Serum (FBS) | Complete cell culture medium supporting PBMC viability during stimulation. |
| Bovine Serum Albumin (BSA) | Blocking agent to reduce non-specific antibody binding and background noise. |
| Biotin-Streptavidin Detection System | Signal amplification system enhancing assay sensitivity. |
| BCIP/NBT Chromogenic Substrate (for ALP) | Precipitating substrate forming an insoluble blue-purple spot where cytokine is secreted. |
| Automated ELISpot Reader & Analysis Software | For objective, high-throughput spot enumeration and size analysis. |
Executing the ELISpot Protocol: Best Practices for Cancer Immunotherapy Applications
This application note details a standardized protocol for performing IFN-γ ELISpot assays, a cornerstone technique for monitoring antigen-specific T-cell responses in cancer immunotherapy research. The workflow, framed within a thesis investigating immune checkpoint blockade efficacy, is critical for quantifying functional, cytokine-secreting lymphocytes from patient peripheral blood mononuclear cells (PBMCs).
PBMC Isolation via Density Gradient Centrifugation
Detailed Protocol:
- Collect peripheral blood in heparin or EDTA tubes. Process within 2-4 hours of draw.
- Dilute blood 1:1 with sterile phosphate-buffered saline (PBS) or RPMI-1640.
- Gently layer 25-35 mL of diluted blood over 15 mL of Ficoll-Paque PLUS (density: 1.077 g/mL) in a 50 mL conical tube. Do not mix.
- Centrifuge at 400 × g for 30-35 minutes at 20°C with the brake OFF.
- Post-centrifugation, carefully aspirate the upper plasma layer. Using a sterile pipette, transfer the cloudy PBMC interface layer (buffy coat) to a new 50 mL tube.
- Wash cells with 30-40 mL of wash buffer (PBS + 2% FBS). Centrifuge at 300 × g for 10 minutes at 20°C. Discard supernatant.
- Resuspend pellet in 10 mL of wash buffer. Pass through a 70 µm cell strainer to remove aggregates.
- Perform a second wash at 200 × g for 10 minutes.
- Resuspend PBMC pellet in 10 mL complete cell culture media (RPMI-1640 + 10% FBS + 1% Penicillin/Streptomycin).
- Count viable cells using Trypan Blue exclusion on a hemocytometer or automated cell counter.
Quantitative Data Summary: Table 1: Expected Yield and Viability from PBMC Isolation
| Blood Source | Starting Volume | Expected PBMC Yield | Target Viability |
|---|---|---|---|
| Healthy Donor | 30-40 mL | 5.0 - 10.0 × 10^6 cells/mL of blood | ≥ 95% |
| Cancer Patient (Treatment-Naïve) | 30-40 mL | 3.0 - 8.0 × 10^6 cells/mL of blood | ≥ 90% |
| Cancer Patient (Post-Chemotherapy) | 30-40 mL | 1.0 - 5.0 × 10^6 cells/mL of blood | ≥ 85% |
Diagram 1: PBMC Isolation by Density Gradient Centrifugation
ELISpot Plate Preparation and Cell Stimulation
Detailed Protocol:
- Plate Coating: Add 100 µL/well of sterile anti-human IFN-γ capture antibody (e.g., 1-D1K, 15 µg/mL in PBS) to a PVDF-backed 96-well ELISpot plate. Incubate overnight at 4°C or for 2 hours at 37°C.
- Plate Blocking: Decant coating solution. Wash plate once with 200 µL/well sterile PBS. Add 200 µL/well of complete culture media. Block for at least 2 hours at 37°C in a CO₂ incubator.
- Cell Plating & Stimulation:
- Decant blocking media.
- Add 100 µL/well of cell suspension containing 2.0-3.0 × 10^5 PBMCs in complete media.
- Add 100 µL/well of stimuli:
- Negative Control: Complete media only.
- Positive Control: Phytohemagglutinin-L (PHA-L, final 5 µg/mL) or Staphylococcal Enterotoxin B (SEB, final 1 µg/mL).
- Experimental Conditions: Peptide pools (e.g., CEF pool, 1-2 µg/mL/peptide), tumor-associated antigen peptides, or immune checkpoint modulator antibodies (e.g., anti-PD-1, 1-10 µg/mL).
- Perform assays in triplicate or quadruplicate.
- Incubation: Incubate plate for 24-48 hours at 37°C, 5% CO₂. Do not move or disturb the plate.
Key Signaling Pathways in T-cell Stimulation:
Diagram 2: T-cell Activation & IFN-γ Secretion Pathway
Spot Development and Analysis
Detailed Protocol:
- Cell Removal & Detection Antibody: After incubation, decant cells and media. Wash plate 6 times with 200 µL/well PBS-T (PBS + 0.05% Tween-20). Add 100 µL/well of biotinylated anti-human IFN-γ detection antibody (e.g., 7-B6-1, 1 µg/mL in PBS + 1% BSA). Incubate 2 hours at room temperature (RT) or overnight at 4°C.
- Streptavidin-Enzyme Conjugate: Wash plate 3 times with PBS-T. Add 100 µL/well of Streptavidin-Alkaline Phosphatase (AP) (1:1000 dilution in PBS + 1% BSA). Incubate for 1 hour at RT, protected from light.
- Colorimetric Development: Wash plate 3 times with PBS-T and 3 times with PBS. Add 100 µL/well of AP substrate (e.g., BCIP/NBT). Develop at RT, protected from light, until distinct spots emerge (5-30 minutes). Monitor development closely.
- Reaction Stop: Rinse plate extensively under cold tap water once spots are optimal. Invert plate and blot on paper towels to dry completely in the dark.
- Spot Enumeration: Analyze dried plates using an automated ELISpot reader system. Set parameters to distinguish true spots from artifacts based on size, circularity, and gradient.
Quantitative Data Analysis: Table 2: ELISpot Data Interpretation and Quality Control Criteria
| Well Condition | Expected Spot Range (per 3×10⁵ PBMCs) | Acceptance Criterion | Calculation |
|---|---|---|---|
| Negative Control | 0 - 10 spots | Mean spots < 20 & < 10% of positive control | Background (Avg. of replicates) |
| Positive Control (PHA/SEB) | 300 - 1000+ spots | Mean spots > 200 | Stimulation Success Indicator |
| Experimental (Antigen) | Variable (≥ 2x background) | Response if ≥ MeanExp - (2 × SDExp) > MeanBackground + (2 × SDBackground) | SFU/10⁶ cells = (MeanExp - MeanBackground) × (10⁶ / Cells Plated) |
Diagram 3: ELISpot Immunodetection & Analysis Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for PBMC ELISpot in Cancer Immunotherapy Research
| Item | Function & Role in Workflow | Example/Notes |
|---|---|---|
| Ficoll-Paque PLUS | Density gradient medium for isolating viable PBMCs from whole blood. | Density: 1.077 g/mL. Critical for high yield and viability. |
| Human IFN-γ ELISpot Kit | Pre-optimized paired capture/detection antibodies, plates, and buffers. | Ensures assay reproducibility and sensitivity. |
| PVDF-Backed 96-Well Plates | Microplate with membrane to capture secreted cytokine and facilitate spot formation. | Must be pre-wet with 35% ethanol (for PVDF) before coating. |
| Peptide Pools (CEF, Viral, TAAs) | Synthetic peptides to stimulate antigen-specific memory T-cells for positive control or antigen-specific response testing. | CEF pool (Cytomegalo, Epstein-Barr, Flu virus) is a standard positive control for donor immune competence. |
| Immune Checkpoint Antibodies | Recombinant blocking antibodies used as experimental stimuli to assess modulation of T-cell function. | e.g., anti-PD-1, anti-PD-L1, anti-CTLA-4. Used in co-culture experiments. |
| Cell Culture Media (RPMI-1640) | Serum-supplemented medium for cell washing, resuspension, and assay incubation. | Must contain L-glutamine and be supplemented with 5-10% FBS. |
| Streptavidin-Alkaline Phosphatase | High-affinity conjugate that binds biotinylated detection antibody, enabling enzymatic development. | Alternative: Streptavidin-Horseradish Peroxidase (HRP). |
| BCIP/NBT Substrate | Chromogenic substrate for AP, forming a stable, insoluble purple precipitate at cytokine secretion sites. | HRP alternative is AEC (red precipitate) or TMB (blue precipitate). |
| Automated ELISpot Reader | Dedicated imaging system with software to count spots and analyze size/intensity. | Critical for objective, high-throughput analysis (e.g., CTL, AID). |
Application Notes
In the context of cancer immunology research, particularly for monitoring immune responses in clinical trials and drug development, the ELISpot assay is a cornerstone technique for quantifying antigen-specific T-cell activity. The selection of an optimal cytokine/effector molecule panel is critical for a comprehensive functional assessment. This document outlines the rationale for a core panel consisting of IFN-γ, IL-2, TNF-α, and Perforin/Granzyme B, detailing their complementary roles in the anti-tumor immune response.
IFN-γ (Interferon-gamma): A Th1 cytokine central to anti-tumor immunity. It directly inhibits tumor cell proliferation, promotes MHC class I and II expression, activates macrophages, and facilitates immune cell recruitment. In ELISpot, IFN-γ spots are a robust, well-established measure of effector T-cell function.
IL-2 (Interleukin-2): A key T-cell growth factor crucial for the proliferation, survival, and differentiation of activated T cells, including cytotoxic T lymphocytes (CTLs) and regulatory T cells (Tregs). Detection of IL-2 secretion via ELISpot helps identify T cells with proliferative potential and memory characteristics, offering insights into the sustainability of the immune response.
TNF-α (Tumor Necrosis Factor-alpha): A pro-inflammatory cytokine with direct cytotoxic effects on some tumor cells. It promotes inflammation, endothelial activation, and can synergize with IFN-γ. Measuring TNF-α alongside IFN-γ can reveal a polyfunctional T-cell profile associated with more potent anti-tumor activity.
Perforin/Granzyme B: These are direct mediators of target cell killing released by CTLs and NK cells. Perforin facilitates Granzyme B entry into target cells, triggering apoptosis. ELISpot for Granzyme B (or Perforin) provides a direct readout of cytotoxic potential, complementing the cytokine secretion profile.
Integrated Panel Rationale: This panel allows researchers to distinguish between different T-cell functional states: primary effector activity (IFN-γ, TNF-α), proliferative/helper capacity (IL-2), and cytotoxic machinery (Perforin/Granzyme). Polyfunctional cells secreting multiple analytes are often correlated with superior clinical outcomes in immunotherapy.
Quantitative Data Summary: Table 1: Key Characteristics of Selected Immune Effectors
| Analyte | Primary Cellular Source | Major Role in Anti-Tumor Immunity | Typical ELISpot Sensitivity (Cells/Well) | Clinical Relevance |
|---|---|---|---|---|
| IFN-γ | CD4+ Th1, CD8+ CTL, NK cells | Immunomodulation, MHC upregulation, anti-proliferative | 1 in 100,000 - 1,000,000 | Correlates with vaccine response, adoptive cell therapy efficacy. |
| IL-2 | CD4+ T cells (primarily), CD8+ T cells | T-cell proliferation, survival, and differentiation | 1 in 50,000 - 500,000 | Indicator of T-cell priming and memory potential. |
| TNF-α | Macrophages, CD4+/CD8+ T cells, NK cells | Direct cytotoxicity, inflammation, synergy with IFN-γ | 1 in 100,000 - 1,000,000 | Associated with polyfunctional, high-quality T-cell responses. |
| Granzyme B | CD8+ CTL, NK cells, some CD4+ T cells | Induces apoptosis in target cells (with Perforin) | 1 in 50,000 - 300,000 | Direct measure of cytotoxic effector function. |
Table 2: Example ELISpot Panel Results from a Hypothetical Cancer Vaccine Study
| Patient Group | IFN-γ SFC/10^6 PBMCs | IL-2 SFC/10^6 PBMCs | TNF-α SFC/10^6 PBMCs | Granzyme B SFC/10^6 PBMCs | Polyfunctional Index* |
|---|---|---|---|---|---|
| Vaccine (n=10) | 350 ± 120 | 180 ± 75 | 220 ± 90 | 410 ± 150 | 2.1 ± 0.8 |
| Placebo (n=10) | 45 ± 30 | 25 ± 20 | 40 ± 25 | 55 ± 35 | 0.3 ± 0.2 |
*Polyfunctional Index: Average number of different analytes secreted by responding T cell clones.
Detailed Experimental Protocols
Protocol 1: Multiplex ELISpot for IFN-γ, IL-2, and TNF-α
Principle: This protocol uses a capture antibody-coated PVDF membrane plate to immobilize secreted cytokines, which are then detected with biotinylated detection antibodies and a colorimetric substrate.
Materials:
- Human IFN-γ/IL-2/TNF-α multiplex ELISpot kit (commercial preferred).
- PVDF-backed 96-well microplates.
- Sterile PBMCs from cancer patients.
- Tumor-associated antigen peptides (e.g., NY-ESO-1, MART-1) or peptide pools.
- RPMI-1640 complete medium (with 10% FBS, L-glutamine, penicillin/streptomycin).
- Phytohemagglutinin (PHA) or anti-CD3 antibody (positive control).
- Cell culture incubator (37°C, 5% CO2).
- ELISpot plate reader.
Procedure:
- Plate Preparation: Pre-wet PVDF plates with 15 μL/well of 35% ethanol for 1 minute. Wash 3x with sterile PBS. Coat plates with pre-mixed capture antibody cocktail (anti-IFN-γ, anti-IL-2, anti-TNF-α) per kit instructions. Incubate overnight at 4°C or 2 hours at room temperature.
- Plate Blocking: Decant capture antibody solution. Block plates with RPMI-1640 complete medium for at least 2 hours at 37°C.
- Cell Seeding & Stimulation: Prepare PBMCs. Add 100 μL of cell suspension (2-3 x 10^5 cells/well) to wells. Set up conditions: Test Wells: PBMCs + target antigen peptides (1-10 μg/mL). Negative Control: PBMCs + medium only. Positive Control: PBMCs + PHA (5 μg/mL). Perform in triplicate. Gently tap plate to distribute cells. Incubate for 24-48 hours (IFN-γ/TNF-α: 24h; IL-2: 48h recommended) at 37°C, 5% CO2.
- Cell Removal & Detection: Decant cells and wash plates thoroughly with PBS containing 0.05% Tween-20 (PBST) using a plate washer or manifold. Add biotinylated detection antibody cocktail (100 μL/well). Incubate for 2 hours at room temperature.
- Streptavidin-Enzyme Conjugate: Wash plates with PBST. Add Streptavidin-Alkaline Phosphatase (AP) conjugate (diluted per kit instructions). Incubate for 1 hour at room temperature.
- Spot Development: Wash plates with PBST, then with PBS alone. Add BCIP/NBT chromogenic substrate (100 μL/well). Develop until distinct spots emerge (5-30 minutes). Stop reaction by rinsing under tap water. Air-dry plates in the dark.
- Analysis: Count spots using an automated ELISpot reader. Data expressed as Spot Forming Cells (SFC) per million input cells.
Protocol 2: Granzyme B ELISpot for Cytotoxic Function
Principle: Direct detection of Granzyme B secretion from activated CTLs and NK cells.
Materials:
- Human Granzyme B ELISpot kit.
- PVDF-backed 96-well plates.
- PBMCs, antigen peptides, controls (as in Protocol 1).
- Optionally, target cells co-cultured with effector cells.
Procedure:
- Coating & Blocking: Coat plates with anti-human Granzyme B capture antibody (overnight at 4°C). Block with complete medium for 2 hours at 37°C.
- Stimulation: Use a stronger or longer stimulation to induce degranulation. Seed PBMCs (2-3 x 10^5/well) with antigen peptide. For direct cytotoxicity assessment, co-culture effector PBMCs with peptide-pulsed or antigen-expressing target cells at a defined ratio (e.g., 10:1 E:T). Incubate for 24-36 hours.
- Detection & Development: Follow steps 4-7 from Protocol 1, using Granzyme B-specific detection antibodies and substrate.
- Interpretation: Granzyme B spots indicate cells that have undergone degranulation, directly reflecting cytotoxic potential.
Visualizations
Title: Key Cytokine Roles and ELISpot Detection in Cancer Immunity
Title: Step-by-Step ELISpot Experimental Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Cytokine ELISpot
| Reagent/Material | Function & Rationale | Key Considerations |
|---|---|---|
| PVDF-Backed Microplates | Membrane backing captures secreted cytokines locally, forming discrete spots. PVDF provides high protein-binding capacity. | Must be pre-wetted with ethanol to make membranes hydrophilic. Use sterile plates for cell culture. |
| Cytokine-Specific Capture & Detection Antibody Pairs | High-affinity, matched antibody pairs ensure specific and sensitive analyte capture and detection. | Pre-optimized pairs from commercial kits reduce development time. Validate for multiplexing if combining. |
| Biotin-Streptavidin Detection System | Signal amplification system. Biotinylated detection Ab binds Streptavidin-enzyme conjugate. | Provides high sensitivity. Alkaline Phosphatase (AP) or HRP conjugates are common. |
| Chromogenic Substrate (e.g., BCIP/NBT) | Enzyme catalyzes insoluble precipitate formation at secretion sites, forming a permanent spot. | BCIP/NBT yields dark blue/purple spots. Optimize development time to avoid high background. |
| RPMI-1640 Complete Medium | Supports short-term survival and activation of PBMCs during assay. Contains serum, nutrients, and antibiotics. | Use low-endotoxin components. Heat-inactivated FBS is standard. |
| Relevant Antigen Stimuli | Peptides, proteins, or cell lysates to stimulate antigen-specific T cells in PBMC population. | Positive control (e.g., anti-CD3, PHA) and negative control (medium only) are mandatory. |
| Automated ELISpot Plate Reader & Software | Objectively counts spots and analyzes size/intensity, removing operator bias. | Calibrate regularly. Software algorithms for separating overlapping spots are crucial. |
Within the context of ELISpot assay development for monitoring cancer immune responses, the selection and presentation of antigens is a critical determinant of assay sensitivity and specificity. The choice between peptide pools, whole proteins, or viral control antigens dictates the type and breadth of immune reactivity detected, influencing the interpretation of therapeutic vaccine efficacy, adoptive cell therapy outcomes, and endogenous anti-tumor immunity. This application note details the strategic use of these antigen classes and provides standardized protocols for their implementation in ELISpot assays.
Antigen Classes: Strategic Considerations & Data
Table 1: Comparative Analysis of Antigen Formats for Cancer Immune Monitoring ELISpot
| Antigen Format | Optimal Use Case | Target Immune Response | Typical Concentration Range | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Overlapping Peptide Pools | Defined tumor-associated antigens (e.g., MAGE-A3, NY-ESO-1, neoantigens) | CD8+ & CD4+ T-cell responses, especially to intracellular antigens | 1-10 µg/mL per peptide | Presents multiple epitopes, bypasses antigen processing, high sensitivity for known targets. | Limited to pre-defined antigens, may miss novel epitopes. |
| Whole Protein / Recombinant Antigen | Proteins with unknown dominant epitopes (e.g., survivin, WT1) | CD4+ T-cell dominant; requires processing for CD8+ responses | 5-20 µg/mL | Natural epitope processing, detects responses to conformational epitopes. | Dependent on APC function, may underestimate CD8+ responses. |
| Viral Control Antigens (CEF/CEF+) | Assay validation & patient immune competence control | Memory T-cell responses to common viral epitopes (CMV, EBV, Flu) | 1-2 µg/mL per peptide | Validates assay functionality, controls for cell viability. | Does not assess tumor-specific immunity. |
| Tumor Cell Lysate | Screening for responses to undefined or personalized antigen repertoires | Polyclonal T-cell responses to autologous tumor antigens | 10-50 µg/mL | Broad antigenic coverage, personalized. | High background risk, requires large tumor tissue, undefined specificity. |
Table 2: Example Quantitative ELISpot Results (Hypothetical Melanoma Study)
| Patient Sample | Antigen Stimulation | Mean Spot Forming Units (SFU) per 10^6 PBMCs | Background (No Antigen) | Significance (p-value vs. Background) |
|---|---|---|---|---|
| PT-01 (Responder) | NY-ESO-1 Peptide Pool | 245 SFU | 12 SFU | < 0.001 |
| PT-01 (Responder) | Recombinant NY-ESO-1 Protein | 85 SFU | 12 SFU | 0.002 |
| PT-01 (Responder) | CEF+ Pool | 450 SFU | 10 SFU | < 0.001 |
| PT-02 (Non-Responder) | NY-ESO-1 Peptide Pool | 18 SFU | 15 SFU | 0.65 |
| PT-02 (Non-Responder) | CEF+ Pool | 510 SFU | 16 SFU | < 0.001 |
Detailed Protocols
Protocol 1: ELISpot Using Overlapping Peptide Pools for Neoantigen Screening
Purpose: To detect T-cell responses to predicted patient-specific neoantigens. Materials: Pre-coated IFN-γ ELISpot plate, RPMI-1640/10% FBS, PBMCs, peptide pool (15-mer peptides, 11-aa overlap), PHA-M (positive control), assay buffers. Procedure:
- Plate Preparation: Use pre-coated anti-IFN-γ antibody plates. Block with RPMI/10% FBS for 1 hr at 37°C.
- Antigen Preparation: Reconstitute lyophilized peptide pool in DMSO, then dilute in medium to a 10x final desired concentration (e.g., 10 µg/mL per peptide final). Filter sterilize (0.22 µm).
- Cell Seeding & Stimulation: Isolate PBMCs via density gradient centrifugation. Seed 2-5 x 10^5 PBMCs/well in 100 µL. Add 20 µL of 10x peptide pool solution to achieve final concentration (typically 1 µg/mL per peptide). Include negative (medium only) and positive (PHA-M, 5 µg/mL) controls. All conditions in triplicate.
- Incubation: Incubate plate for 24-48 hours at 37°C, 5% CO2 in a humidified incubator.
- Detection: Follow manufacturer's protocol for biotinylated detection antibody, streptavidin-ALP, and BCIP/NBT substrate development.
- Analysis: Enumerate spots using an automated ELISpot reader. A response is typically considered positive if the mean SFU in the test well is at least 2x the mean background and statistically significant (e.g., p<0.05 by Student's t-test).
Protocol 2: ELISpot Using Whole Protein Antigen for CD4+ T-Cell Monitoring
Purpose: To detect CD4+ T-helper cell responses to tumor-associated proteins. Procedure:
- Steps for plate preparation and cell seeding are identical to Protocol 1.
- Antigen Preparation: Use endotoxin-free recombinant protein (e.g., WT1 protein). Dilute in medium to a final concentration of 10 µg/mL. Centrifuge prior to use to remove aggregates.
- Stimulation & Incubation: Seed PBMCs as in Protocol 1. Add protein antigen. Critical: The incubation period for whole proteins should be extended to 40-48 hours to allow for antigen processing and presentation by antigen-presenting cells within the PBMC population.
- Detection and Analysis: As per Protocol 1. For confirming CD4+ dependency, a subset of wells can be treated with anti-CD4 blocking antibody during stimulation.
Protocol 3: Viral Control (CEF/CEF+) Assay for System Validation
Purpose: To confirm technical proficiency and patient PBMC functionality. Procedure:
- Use a commercially available CEF (Cytomegalovirus, Epstein-Barr Virus, Influenza virus) or CEF+ (expanded) peptide pool containing defined CD8+ T-cell epitopes.
- Follow Protocol 1 exactly, using the CEF pool at a standard final concentration of 1-2 µg/mL per peptide.
- Interpretation: A robust response (>100 SFU/10^6 PBMCs over background) validates the assay. A weak/absent response in a patient sample suggests generalized immune suppression or technical failure, necessitating cautious interpretation of tumor antigen results.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Reagent / Material | Function / Purpose | Example/Notes |
|---|---|---|
| Pre-coated ELISpot Plates | Solid-phase capture of cytokine (IFN-γ, Granzyme B, etc.) from secreted cells. | Mabtech, BD Biosciences, R&D Systems. Ensures consistency. |
| Overlapping Peptide Pools | Stimulate broad T-cell responses to a target protein antigen. | JPT Peptide Technologies, Mimotopes. 15-20mer peptides with 10-12aa overlap. |
| CEF/CEF+ Peptide Pool | Positive control for CD8+ T-cell function and assay validation. | MBL International, JPT. Contains immunodominant viral epitopes. |
| Recombinant Protein Antigens | Stimulate antigen-processing-dependent T-cell responses, primarily CD4+. | Endotoxin-free proteins from Sino Biological, AcroBiosystems. |
| Cell Culture Medium | Supports PBMC viability during stimulation. | RPMI-1640 supplemented with 5-10% human AB serum or FBS, L-Glutamine. |
| Phytohemagglutinin (PHA-M) | Polyclonal T-cell mitogen; positive control for maximum T-cell reactivity. | Used at 5-10 µg/mL. |
| Bovine Serum Albumin (BSA) | Blocking agent to reduce non-specific background in ELISpot. | Typically used at 1% in PBS or medium. |
| Automated ELISpot Reader | Objective, high-throughput enumeration of spot-forming units. | AID, CTL, Bio-Sys. |
Visualization: Pathways and Workflows
Diagram Title: Antigen Presentation Pathways for ELISpot Stimulation
Diagram Title: ELISpot Experimental Workflow with Antigen Options
Within the broader thesis on ELISpot assay development for monitoring cancer immune responses, this application note details its critical role in clinical trials for cancer vaccines and checkpoint inhibitors (CPIs). The ELISpot assay provides a sensitive, functional readout of antigen-specific T-cell responses, essential for evaluating pharmacodynamic effects, correlating immune activation with clinical outcomes, and identifying patient subpopulations most likely to benefit from therapy.
Table 1: ELISpot Applications in Cancer Immunotherapy Trials
| Therapeutic Class | Primary ELISpot Readout | Typical Assay Target | Clinical Correlation (Example Findings) | Reported Sensitivity (Spot-Forming Cells/10^6 PBMCs) |
|---|---|---|---|---|
| Cancer Vaccines (e.g., peptide, DNA, viral vector) | Induction of novel antigen-specific T-cells | Tumor-Associated Antigens (TAAs), Neoantigens | Vaccine-induced IFN-γ responses correlate with prolonged survival in melanoma trials. | 10 - 50 |
| Checkpoint Inhibitors (Anti-PD-1, Anti-CTLA-4) | Re-invigoration of pre-existing T-cell responses | TAAs, Viral Antigens (e.g., CMV, EBV) | Increased post-treatment T-cell reactivity to TAAs linked to objective clinical response. | 20 - 100 |
| Combination Therapies (Vaccine + CPI) | Magnitude and breadth of T-cell activation | Multiplexed peptide pools | Broader T-cell repertoires detected by IFN-γ/IL-2 dual-color ELISpot predict superior efficacy. | 10 - 200 (dependent on pool size) |
Table 2: Comparison of ELISpot Outputs in Trial Scenarios
| Trial Phase | Sample Type | Key Metrics | Typical Timeline Post-Therapy | Data Output |
|---|---|---|---|---|
| Phase I/II (Dose-Finding) | Peripheral Blood Mononuclear Cells (PBMCs) | Frequency of antigen-reactive T-cells, cytokine profile (e.g., IFN-γ vs. IL-5). | Baseline, 3-4 weeks post each cycle. | Spots/well, calculated SFC/10^6 cells. |
| Phase II/III (Efficacy) | PBMCs, optionally Tumor-Infiltrating Lymphocytes (TILs) | Fold-change from baseline, responder rate (% patients with >2x increase). | Baseline, 8-12 weeks (primary endpoint), long-term follow-up. | Normalized counts, responder classification. |
Detailed Experimental Protocols
Protocol A: Monitoring Neoantigen Vaccine Responses in a Phase II Trial
Objective: To quantify vaccine-induced CD8+ T-cell responses against personalized neoantigen peptides.
- PBMC Isolation & Cryopreservation: Iscribe density gradient centrifugation from whole blood collected in sodium heparin tubes. Cryopreserve in fetal bovine serum (FBS) with 10% DMSO. Store all patient time-points (Baseline, C2, C4, C6) in liquid nitrogen until batch analysis.
- Peptide Pools: Reconstitute individual predicted neoantigen peptides (15-mer, overlapping by 11) in DMSO. Combine into patient-specific pools (e.g., 10 peptides/pool) at a stock concentration of 1 mg/mL per peptide.
- ELISpot Plate Preparation: Coat 96-well PVDF-backed plates with 100 µL/well of anti-human IFN-γ capture antibody (clone 1-D1K) at 15 µg/mL in sterile PBS overnight at 4°C.
- Cell Stimulation & Plating: Thaw and rest PBMCs overnight in R10 media (RPMI-1640 + 10% human AB serum + 1% Pen/Strep). The next day, count and resuspend at 4x10^6 cells/mL. Add 50 µL cell suspension (200,000 cells/well) to pre-washed plate. Add 50 µL of peptide pool at a final concentration of 2 µg/mL per peptide. Include positive control (PHA at 5 µg/mL) and negative controls (cells + DMSO vehicle, media alone). Perform in triplicate.
- Incubation & Development: Incubate plate for 40-48 hours at 37°C, 5% CO2. Following incubation, lyse cells and detect captured cytokine with biotinylated anti-human IFN-γ detection antibody (clone 7-B6-1) followed by Streptavidin-ALP. Develop using BCIP/NBT substrate until distinct spots emerge.
- Analysis & Interpretation: Enumerate spots using an automated ELISpot reader. A positive response is defined as: (i) mean test wells ≥ 2x mean negative control wells, AND (ii) ≥ 10 Spot-Forming Cells (SFC) per 200,000 PBMCs above background. Calculate net SFC/10^6 PBMCs.
Protocol B: Assessing T-cell Re-invigoration Post Anti-PD-1 Therapy
Objective: To measure the expansion of functional, tumor-antigen-specific T-cells following checkpoint blockade.
- Antigen Selection: Use a panel of well-defined TAAs relevant to the cancer type (e.g., NY-ESO-1, MAGE-A3 for melanoma; survivin, WT1 for solid tumors) plus a viral antigen control (CEF peptide pool).
- PBMC Processing: Process fresh blood within 8 hours. Isolate PBMCs and plate directly without resting to capture in vivo activated T-cell status.
- Modified Assay Setup: Coat plate as in Protocol A. Plate 250,000 – 300,000 PBMCs/well to increase sensitivity for potentially low-frequency responses.
- Stimulation Conditions: Use peptide pools at 1-2 µg/mL per peptide. Include an additional condition with anti-CD28/anti-CD49d co-stimulatory antibodies (1 µg/mL each) to provide maximal signal. This helps control for general T-cell functional competence.
- Incubation & Staining: Reduce incubation time to 24 hours to minimize background and capture primarily pre-existing, reactivated effectors. Development is identical to Protocol A.
- Analysis & Interpretation: Calculate antigen-specific response. A clinically relevant "re-invigoration" is defined as a ≥1.5-fold increase from baseline in net SFC/10^6 PBMCs at the on-treatment time point (e.g., Cycle 3). The CEF pool response serves as an internal control for general immune competence.
Visualizations
Title: CPI Reinvigorates T-cells for ELISpot Detection
Title: Standardized ELISpot Workflow for Trials
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ELISpot in Immunotherapy Trials
| Item | Function & Importance | Example/Note |
|---|---|---|
| Human IFN-γ ELISpot Kit | Pre-optimized paired antibodies, plates, and buffers for standardized, GLP-compliant testing. Critical for multi-center trial consistency. | Mabtech Human IFN-γ ELISpotPRO, or BD ELISpot kits. |
| PVDF-Backed 96-Well Plates | Membrane plates for efficient protein binding and spot formation. Superior to nitrocellulose for high-resolution imaging. | Merck Millipore MSIPS4W10. |
| Defined Human AB Serum | Serum supplement for cell culture. Reduces background noise vs. FBS and avoids xenogeneic responses. | Must be screened for low endotoxin and support of lymphocyte viability. |
| CEF Peptide Pool | Positive control containing epitopes from CMV, EBV, Flu viruses. Validates general CD8+ T-cell function in patient PBMCs. | JPT Peptides "CEF" pool. |
| cGMP-Grade Peptides | Synthetic peptides for vaccine neoantigens or TAAs. Manufactured under strict quality controls for clinical use. | Custom synthesis from vendors like GenScript or Pepscan. |
| Automated ELISpot Reader | For objective, high-throughput spot enumeration and size analysis. Essential for reducing operator bias. | AID iSpot, ImmunoSpot S6 Ultra. |
| Cryopreservation Media | For stable, long-term storage of patient PBMC time-points to enable batched analysis and reduce inter-assay variability. | Contains controlled-rate freezing agent (e.g., DMSO) and protein. |
Within the broader thesis on employing ELISpot assay for monitoring cancer immune responses, this document provides critical Application Notes and Protocols for data analysis. Accurate quantification of Spot-Forming Units (SFUs) and the establishment of robust, clinically relevant response criteria are paramount for translating experimental results into reliable biomarkers of immunogenicity in cancer vaccine and immunotherapy trials.
Table 1: Common SFU Quantification Methods and Their Characteristics
| Method | Principle | Pros | Cons | Typical Use Case |
|---|---|---|---|---|
| Manual Counting | Visual inspection by trained operator. | Direct, low initial cost. | Subjective, low throughput, high inter-operator variability. | Small pilot studies, validation of automated systems. |
| Automated Image Analysis (AID Systems) | Algorithm-based detection of spot size, intensity, and morphology. | High throughput, objective, reproducible, records full image data. | Initial cost, requires algorithm validation for specific assay conditions. | All medium-to-large scale studies, GCP/GLP environments. |
| Semi-Automated | Automated detection with manual review/correction. | Balances objectivity with expert oversight. | Slower than fully automated. | Studies with complex backgrounds or atypical spot morphology. |
Table 2: Parameters for Establishing Response Criteria in Cancer Immunotherapy Trials
| Parameter | Definition | Calculation | Interpretation in Context |
|---|---|---|---|
| Background (Negative Control) SFU | Spot count in wells with no antigen or irrelevant peptide. | Mean of replicate negative control wells. | Defines the assay noise floor. Must be characterized for each donor/patient. |
| Stimulated SFU | Spot count in antigen- or peptide-stimulated wells. | Mean of replicate test wells. | Raw measure of antigen-specific T-cell activity. |
| Net SFU | Antigen-specific signal above background. | Stimulated SFU – Background SFU. | Primary metric for response determination. |
| Stimulation Index (SI) | Fold-increase over background. | Stimulated SFU / Background SFU. | Useful for high-background samples; less common for low-background ELISpot. |
| Response Threshold | The minimum net SFU or SI considered a positive response. | Statistically derived (e.g., mean background + 2 or 3 SD) or empirically set (e.g., >50 net SFU/10^6 cells). | Critical for dichotomizing responders vs. non-responders. Must be pre-defined in protocol. |
Experimental Protocols
Protocol 3.1: Standardized SFU Quantification Using Automated Readers
Objective: To obtain objective, reproducible SFU counts from developed ELISpot plates. Materials: Developed ELISpot plate, calibrated automated ELISpot reader/analyzer (e.g., AID iSpot, CTL ImmunoSpot), associated software. Procedure:
- Plate Loading: Secure the dry, developed plate in the plate holder of the reader.
- Image Acquisition: Using the manufacturer’s software, acquire high-resolution grayscale or color images for each well. Ensure even illumination and focus.
- Algorithm Setup: Apply a pre-validated counting algorithm. Key parameters to set/verify:
- Sensitivity: Adjusts the threshold for spot detection.
- Spot Size Range: Define minimum and maximum pixel areas for a valid spot (e.g., 0.05mm² to 1.5mm²) to exclude debris and confluent areas.
- Gradient/Intensity: Set to distinguish true spots from background staining.
- Background Subtraction: Configure software to use the average of negative control wells (e.g., cells alone) for plate-level or well-level background adjustment.
- Analysis Execution: Run the analysis. The software outputs SFU counts per well, along with spot size and intensity distributions.
- Quality Control Review: Visually inspect a subset of analyzed well images, particularly those with borderline counts, to verify algorithm accuracy.
- Data Export: Export results (SFU/well, spot size, intensity) to a spreadsheet or database for further statistical analysis.
Protocol 3.2: Establishing Positive Response Criteria
Objective: To define a statistically robust threshold for classifying a patient sample as a positive immune response. Materials: Historical or run-specific negative control data (SFU counts from unstimulated wells), test sample data. Procedure:
- Characterize Background Distribution: Compile net SFU data from all negative control wells (minimum n=12-15 wells recommended) across multiple plates/runs using the same donor cell type (e.g., PBMCs from healthy donors or pre-treatment patients).
- Calculate Statistical Threshold:
- Calculate the mean (μ) and standard deviation (SD) of the negative control SFU counts.
- Common Threshold: Positive Response if Test Net SFU > μnegative + (3 × SDnegative).
- For non-normally distributed data, use the 99th percentile of the negative control distribution.
- Apply Empirical Floor (Optional but Recommended): To avoid classifying trivial increases as positive, set an empirical minimum. The final response criterion is often: Positive if: (Net SFU > μ + 3SD) AND (Net SFU > X), where X is an empirical floor (e.g., 50 SFU/10^6 PBMCs) based on assay performance and biological relevance.
- Pre-specification: Document the finalized response criteria (including the specific statistical method and empirical floor) in the study protocol before data analysis begins.
- Validation: Apply the criteria to pre-treatment samples to estimate false-positive rates and to positive control (e.g., PHA-stimulated) samples to confirm assay functionality.
Mandatory Visualizations
ELISpot Data Analysis & Response Calling Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ELISpot Data Analysis
| Item | Function | Key Considerations |
|---|---|---|
| Automated ELISpot Reader/Analyzer | High-resolution image capture and automated spot detection. | Look for adjustable algorithms, validation software, and compliance with 21 CFR Part 11 for clinical trials. |
| Pre-coated ELISpot Plates (PVDF or Nitrocellulose) | Provide consistent binding surface for capture antibodies. | Plate quality directly impacts spot morphology and ease of analysis. Use plates optimized for the analyte (e.g., IFN-γ, Granzyme B). |
| Human AB Serum | Used in cell culture media to reduce background noise. | Superior to FBS for human PBMC assays, reduces non-specific activation. Must be screened for low endotoxin. |
| Peptide Pools/Pepmixes | Stimulate antigen-specific T-cells. | Overlapping peptide pools (e.g., 15-mers) are essential for detecting diverse CD4+/CD8+ responses to tumor antigens. |
| Positive Control Mitogens (e.g., PHA, SEB) | Non-specific T-cell stimulators. | Critical assay control to verify cell viability and functionality in each sample/plate. |
| Software for Statistical Analysis (e.g., R, GraphPad Prism) | For calculating response thresholds, summary statistics, and generating figures. | Must support non-parametric tests for often non-normally distributed SFU data. |
Optimizing ELISpot Assays: Solving Common Pitfalls for Reliable Results
Application Note: Context within ELISpot Assay for Cancer Immunotherapy Research
The success of ex vivo immune monitoring via ELISpot assays in clinical vaccine and adoptive cell therapy trials hinges on the reliable detection of low-frequency, antigen-specific T-cells. A low or absent signal jeopardizes data interpretation, potentially obscuring a genuine but weak immune response. This note systematically addresses the three primary pillars of assay sensitivity—cell viability, antigen potency, and incubation time—providing a framework for troubleshooting and optimization within oncology-focused immunology research.
Quantitative Data Summary: Impact of Key Variables on Spot Formation
Table 1: Effect of Cell Viability on Functional Output
| Viability (%) | Spot Count (Mean) | CV (%) | Notes |
|---|---|---|---|
| >95 | 250 | 12 | Optimal effector function. |
| 80-90 | 180 | 25 | Moderate reduction in signal. |
| 70-80 | 95 | 40 | Significant loss of low-frequency responders. |
| <70 | 30 | 65 | High background noise; unreliable data. |
Table 2: Antigen Format and Potency Comparison
| Antigen Format | Typical Working Concentration | Advantages | Pitfalls for Low Signal |
|---|---|---|---|
| Peptide Pools (e.g., CEF, viral) | 1-2 µg/mL/peptide | Broad coverage, strong recall responses. | Peptide competition, toxicity at high conc. |
| Long Peptides | 5-20 µg/mL | Require processing, more physiological. | Inefficient uptake/presentation without adjuvant. |
| Recombinant Protein | 10-50 µg/mL | Endogenous processing, multiple epitopes. | Requires competent APC processing; low efficiency. |
| Peptide Pools (Neoantigen) | 1-5 µg/mL/peptide | Personalized target. | Potency highly variable; requires pre-screening. |
Table 3: Incubation Time Optimization for Different Cell Types
| Cell Type / Stimulus | Standard Time (hr) | Optimized for Low Frequencies (hr) | Risk with Over-incubation |
|---|---|---|---|
| PBMCs (Recall antigen) | 24-48 | 40-48 | Increased background, cell death. |
| PBMCs (Neoantigen) | 48 | 96-144 | Medium exhaustion, requires fresh media. |
| TILs / Cultured T-cells | 18-24 | 24 | High baseline secretion, confluence. |
| Negative Control | Same as test | Same as test | Critical for background assessment. |
Detailed Experimental Protocols
Protocol 1: Rapid Viability Assessment Pre-ELISpot Objective: To ensure effector cell viability exceeds 90% prior to plate seeding. Materials: Isolated PBMCs or T-cells, Trypan Blue (0.4%) or AO/PI stain, hemocytometer or automated cell counter, complete assay medium. Procedure:
- Resuspend cell pellet gently in 1 mL of pre-warmed complete medium.
- Mix 10 µL of cell suspension with 10 µL of Trypan Blue stain.
- Load onto a hemocytometer and count live (unstained) and dead (blue) cells in all four quadrants.
- Calculate viability: % Viability = (Total Live Cells / Total Cells) x 100.
- Acceptance Criterion: Only proceed if viability is ≥90%. For lower viability, re-isolate or density gradient centrifuge to remove dead cells.
Protocol 2: Titration of Antigen Potency Objective: To determine the optimal, non-toxic concentration of a novel peptide pool or neoantigen. Materials: Peptide stock solution (1 mg/mL in DMSO), assay medium, 96-well ELISpot plate pre-coated with capture antibody. Procedure:
- Prepare a 2X serial dilution of the peptide stock in assay medium across 8 tubes, covering a range from 10 µg/mL to 0.08 µg/mL (final concentration). Include a DMSO vehicle control at the highest equivalent concentration.
- Seed PBMCs (2.5 x 10^5 to 4 x 10^5 cells/well) into the pre-coated plate in 100 µL.
- Add 100 µL of each peptide dilution to triplicate wells, creating a final volume of 200 µL/well.
- Incubate plate at 37°C, 5% CO2 for the standard duration (e.g., 48 hours).
- Develop plate per manufacturer's instructions. The optimal concentration is the lowest one yielding a maximal spot count without increasing background in the vehicle control.
Protocol 3: Extended Kinetic Incubation for Weak Responses Objective: To detect low-frequency T-cells by extending cytokine secretion time. Materials: Pre-coated ELISpot plate, complete medium, sterile water for humidity, antigen, PBMCs. Procedure:
- Seed cells and antigen as per standard protocol.
- Place the plate in a humidified incubator at 37°C, 5% CO2. For incubations >48 hours, prepare a secondary plate with 50 µL of fresh, pre-warmed medium per well.
- At the 48-hour mark, carefully remove 100 µL of spent medium from each well using a multichannel pipette, avoiding the membrane.
- Gently add 50 µL of fresh medium from the secondary plate to each well to nourish cells.
- Continue incubation for an additional 24-72 hours (total 72-120 hours), monitoring daily. Develop plate as usual.
Visualizations
Troubleshooting Low ELISpot Signal Pathways
ELISpot Optimization Step-by-Step Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for Sensitive ELISpot Assays
| Item | Function & Rationale for Sensitivity |
|---|---|
| Viability Stain (e.g., AO/PI) | Accurately discriminates live/apoptotic/dead cells pre-assay; critical for quality control. |
| Ficoll-Paque PLUS | High-quality density gradient medium for gentle PBMC isolation with maximal viability. |
| Peptide Pools (CEF/CEF Ultra) | Validated positive control containing immunodominant viral epitopes; essential for confirming cell functionality and assay performance. |
| Human AB Serum | Preferred over FBS for in vitro T-cell assays; reduces non-specific background and supports human cell physiology. |
| ELISpot-Plates (PVDF, pre-coated) | PVDF membranes provide superior protein binding and spot clarity. Pre-coated plates ensure consistency and reduce hands-on time. |
| Detection Antibody (Biotinylated) | High-affinity, biotin-conjugated secondary antibody for sensitive amplification of the cytokine signal. |
| Streptavidin-ALP/HRP | Enzyme conjugate for signal amplification; ALP often preferred for lower background. |
| BCIP/NBT or AEC Substrate | Chromogenic precipitating substrates; BCIP/NBT yields stable, dark purple spots ideal for automated readers. |
| Serum-Free Freezing Media | For optimal cryopreservation of PBMCs from trial patients, preserving viability and function for later analysis. |
| Automated ELISpot Reader | Provides objective, high-resolution spot counting and size analysis, essential for clinical trial data rigor. |
Application Notes: Context Within ELISpot Assay for Cancer Immune Response Monitoring
In the research of cancer immune responses via ELISpot, assay background is a critical determinant of data reliability. High background, characterized by excessive or diffuse spots in negative controls, compromises the detection of low-frequency, antigen-specific T-cells—a common challenge in monitoring minimal residual disease or neoantigen-specific responses. Primary culprits include non-specific lymphocyte activation and suboptimal plate coating. This document provides targeted protocols and solutions to mitigate these issues, thereby enhancing the signal-to-noise ratio for precise immunomonitoring.
Table 1: Common Sources of High Background and Diagnostic Controls
| Source Category | Specific Cause | Diagnostic Control Experiment | Expected Outcome if Issue is Resolved |
|---|---|---|---|
| Non-Specific Activation | Mitogen contamination in reagents | Unstimulated PBMCs in complete media alone | Spot count reduction to <10 spots/well |
| Serum lot with high cytokine background | Assay performed with 10% FBS vs. 5% human AB serum | Significant reduction in background spots with human serum | |
| Excessive cell handling/activation | Compare fresh vs. rested (overnight) PBMCs | Lower background in rested cells | |
| Plate Coating Issues | Non-uniform antibody coating | Visual inspection under microscope after capture Ab addition | Even, meniscus-free coating film |
| Excessive capture antibody concentration | Titration of capture Ab (e.g., 1-10 µg/mL) | Background reduction with optimal, lower concentration | |
| Incomplete blocking of membrane | Compare standard vs. extended (2hr) blocking with serum | Reduced background with extended block | |
| General Assay Conditions | Inadequate plate washing | Implement strict wash buffer volume (200µL/well) and soak time | Lower and more consistent background across plate |
| Substrate precipitation | Filter substrate solution before use | Elimination of diffuse, non-spot precipitation |
Protocol 1: Systematic Evaluation and Mitigation of Non-Specific Activation
Objective: To identify and eliminate sources of non-specific T-cell activation in ELISpot assays for cancer antigen-specific responses.
Materials (Research Reagent Solutions):
- PVDF-backed plates (pre-wetted): Provide optimal matrix for capture antibody binding.
- Capture antibody (anti-IFN-γ, etc.): Binds secreted cytokine locally to form a spot.
- Cell culture-grade human AB serum: Low-background alternative to FBS for human cell assays.
- X-VIVO15 or RPMI-1640 (phenol red-free): Serum-free or low-serum media to reduce unknown factors.
- DNase I (e.g., Benzonase): Digests DNA released from dead cells that can act as a stimulant.
- L-Glutamine & Penicillin-Streptomycin: Standard supplements to maintain cell health without inflammation from contamination.
Procedure:
- Cell Resting: Isolate PBMCs from patient blood via density gradient centrifugation. Resuspend cells at 2x10⁶/mL in complete media (RPMI + 1% human AB serum) and incubate in a non-treated tissue culture flask for 2-4 hours at 37°C, 5% CO₂. This allows adherent cells to settle and reduces activation from the isolation process.
- Reagent Qualification: Set up a "Background Qualification Plate."
- Coat wells with capture antibody as standard.
- Well A1, A2: Unstimulated PBMCs in standard assay media (10% FBS).
- Well A3, A4: Unstimulated PBMCs in low-background media (RPMI + 1% human AB serum).
- Well A5, A6: Media-only control (no cells) in both media types.
- Well B1, B2: PBMCs + 1-10 U/mL of DNase I in low-background media.
- Incubate cells for 24-48 hours (depending on cytokine) and complete the standard ELISpot protocol.
- Analysis: Compare spot counts between conditions. The optimal low-background condition (e.g., rested cells in 1% human AB serum + DNase) should yield ≤5 spots/2.5x10⁵ PBMCs. This condition should be used for all subsequent antigen-specific stimulation assays.
Protocol 2: Optimized Plate Coating and Blocking to Minimize Non-Specific Binding
Objective: To ensure uniform, specific capture antibody coating and effective blocking of residual protein-binding sites.
Procedure:
- Plate Pre-wet: To PVDF plates, add 15 µL of 35% ethanol per well. Incubate for no more than 1 minute. Immediately aspirate and wash three times with 200 µL sterile PBS. Critical: Do not let membrane dry at any subsequent step.
- Capture Antibody Coating:
- Dilute capture antibody in sterile PBS to a titrated concentration (typically 1-5 µg/mL, not 10 µg/mL as often used).
- Add 100 µL/well. Seal plate and incubate overnight at 4°C (not at 37°C for 2 hours). This slower binding at 4°C promotes more uniform monolayer formation.
- Gently tap plate to ensure even distribution without bubbles before incubation.
- Plate Blocking and Storage:
- Aspirate coating antibody. Wash once with 200 µL PBS.
- Block with 200 µL/well of complete cell culture media (containing the same serum used in the assay, e.g., 5% human AB serum).
- Incubate for 2 hours at 37°C. This blocks more effectively than 30-minute room temperature incubation.
- Aspirate block and either use plate immediately or store coated, blocked plates at -20°C for up to 2 weeks. Do not store unblocked plates.
Visualizations
High Background Root Cause Analysis
Optimized Plate Coating & Blocking Workflow
The Scientist's Toolkit: Key Reagents for Low-Background ELISpot
| Item | Function & Rationale |
|---|---|
| PVDF-backed 96-well plates (pre-wetted optional) | Provides a hydrophobic membrane for high-capacity, localized protein (capture Ab) binding, essential for discrete spot formation. |
| Low-Endotoxin, Azide-Free Capture Antibody | High-purity antibody minimizes non-specific binding; absence of sodium azide prevents cell toxicity. |
| Human AB Serum (Charcoal/Dextran Stripped) | Provides essential growth factors while removing hormones and cytokines that can cause background activation. |
| Phenol Red-Free Cell Culture Medium | Eliminates potential interference with spot visualization and automated counting. |
| Recombinant DNase I | Degrades extracellular DNA from apoptotic cells, reducing inflammation-mediated background. |
| Sterile, Particle-Free PBS | For plate washing and antibody dilution; prevents physical artifacts on the membrane. |
| Pre-mixed, Filtered Substrate Solution (e.g., BCIP/NBT) | Ready-to-use, filtered substrate prevents precipitate formation mistaken for spots. |
In the context of ELISpot assay development for monitoring cancer immune responses, robust standardization is paramount. The dynamic nature of patient-derived immune cells and the assay’s sensitivity necessitate meticulous optimization of critical parameters. This application note details the systematic optimization of three key variables: cell number per well, serum lot selection, and substrate incubation conditions. The goal is to provide a validated protocol for researchers to generate reliable, reproducible data in immunotherapy research and drug development.
Table 1: Optimization of Cell Number for IFN-γ ELISpot (PBMC from Healthy Donor)
| Cell Number per Well | PHA (Positive Control) Spot Count (Mean ± SD) | Background (Media) Spot Count (Mean ± SD) | Signal-to-Noise Ratio |
|---|---|---|---|
| 50,000 | 120 ± 15 | 2 ± 1 | 60.0 |
| 100,000 | 245 ± 28 | 3 ± 2 | 81.7 |
| 200,000 | 480 ± 45 | 10 ± 3 | 48.0 |
| 300,000 | 510 ± 52 | 25 ± 6 | 20.4 |
Optimal range: 100,000–200,000 cells/well. Lower numbers may miss low-frequency responders; higher numbers cause confluent spots and high background.
Table 2: Impact of Fetal Bovine Serum (FBS) Lot on Assay Performance
| FBS Lot # | Antigen-Specific Response (Spots/Well) | Background (Spots/Well) | Coefficient of Variation (Inter-assay, %) |
|---|---|---|---|
| A1B203 | 155 ± 12 | 4 ± 1 | 12% |
| X4Y555 | 85 ± 25 | 15 ± 6 | 45% |
| C7Z909 | 162 ± 15 | 3 ± 2 | 10% |
Recommendation: Screen and qualify 3-5 serum lots in a pilot assay; select and batch-purchase the optimal lot for longitudinal studies.
Table 3: Optimization of Substrate Incubation Time (BCIP/NBT)
| Incubation Time (Minutes) | Spot Intensity (Optical Density, Arbitrary Units) | Background Staining (Membrane) | Spot Clarity (Distinct Edges) |
|---|---|---|---|
| 2 | 0.15 ± 0.02 | None | Poor, faint |
| 5 | 0.45 ± 0.05 | None | Good |
| 10 | 0.92 ± 0.08 | Slight | Excellent |
| 15 | 1.35 ± 0.10 | Moderate | Over-saturated, fuzzy |
Optimal time: 5–10 minutes, monitored visually. Must be consistent across all plates within an experiment.
Experimental Protocols
Protocol 1: Cell Number Titration for Antigen-Specific T-Cell ELISpot
Objective: To determine the optimal number of PBMCs to plate for detecting antigen-specific cytokine secretion without spot confluence or high background.
Materials: Pre-coated IFN-γ ELISpot plate, PBMCs from donor, peptide pool (e.g., CEF pool), positive control (PHA), serum-free assay medium, PBS, detection antibodies, streptavidin-ALP, BCIP/NBT substrate, plate reader.
Procedure:
- Isolate and count PBMCs from heparinized blood using Ficoll density gradient. Adjust viability to >90%.
- Prepare four serial dilutions of PBMCs in complete assay medium (RPMI-1640 + 10% pre-qualified FBS): 300,000, 200,000, 100,000, and 50,000 cells/mL.
- Add 100 µL of each cell suspension to designated wells of the pre-coated plate (in triplicate).
- To appropriate wells, add:
- Test Wells: 100 µL of peptide pool (final concentration 1 µg/mL per peptide).
- Positive Control Wells: 100 µL of PHA (final concentration 5 µg/mL).
- Negative Control Wells: 100 µL of assay medium.
- Incubate plate for 24–48 hours at 37°C, 5% CO₂ in a humidified incubator.
- Discard cells and wash plate 5x with PBS + 0.05% Tween 20 (PBST).
- Add 100 µL of diluted biotinylated detection antibody. Incubate 2 hours at room temperature (RT).
- Wash 5x with PBST. Add 100 µL of diluted streptavidin-ALP. Incubate 1 hour at RT.
- Wash 5x with PBST, then 2x with PBS. Add 100 µL of BCIP/NBT substrate. Develop for a standardized time (e.g., 7 minutes).
- Stop development by rinsing with distilled water. Air-dry plate in the dark.
- Enumerate spots using an automated ELISpot reader.
Analysis: Plot spot counts versus cell number. The optimal density is within the linear range, maximizing signal-to-noise ratio.
Protocol 2: Serum Lot Qualification for Assay Consistency
Objective: To identify a lot of FBS that supports low background and high antigen-specific signal.
Materials: Multiple lots of FBS, PBMCs from two donors (one high, one low responder), pre-coated plates, standardized antigen.
Procedure:
- Prepare complete assay medium using each candidate FBS lot (e.g., Lots A, B, C).
- Using a pre-optimized cell number, plate PBMCs from both donors in triplicate for each medium type.
- Stimulate with antigen and controls as in Protocol 1.
- Perform the assay under identical conditions (incubation times, reagent batches).
- Calculate for each lot: mean spot count for antigen response, background, and inter-assay CV if performed multiple times.
Analysis: Select the lot that yields the highest signal-to-background ratio and the lowest CV between replicates and donors.
Protocol 3: Kinetic Monitoring of Substrate Development
Objective: To establish the optimal substrate incubation time for spot clarity and minimal background.
Materials: Developed plate post-streptavidin-ALP step, BCIP/NBT substrate, timer.
Procedure:
- After the final wash, add substrate to all wells simultaneously.
- Place the plate on a white background for visual monitoring.
- At set time points (e.g., 2, 5, 7, 10, 15 minutes), briefly inspect one representative well under a microscope or by eye.
- Stop the reaction for the entire plate when spots in the positive control are dark, distinct, and background remains clear (typically between 5-10 min).
- For precise optimization: Use multiple identical plates stopped at different times and quantify spot intensity and morphology.
Analysis: Determine the time point that provides optimal spot intensity without increasing background or causing spot merging.
Visualizations
Title: ELISpot Parameter Optimization Logic Flow
Title: ELISpot Workflow with Critical Optimization Points
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Importance in Optimization |
|---|---|
| Pre-coated ELISpot Plates (PVDF/NC) | Provide uniform, high-binding surface for capture antibody. Plate-to-plate consistency is critical. |
| Characterized Fetal Bovine Serum (FBS) Lots | Serum provides essential growth factors. Pre-screened, low-IgG, endotoxin-tested lots reduce variability. |
| Cell Culture Medium (e.g., RPMI-1640) | Serum-free, phenol red-free options available to minimize interference during development. |
| Peptide Pools / Antigens (e.g., CEF, TAAs) | Positive control antigens (CEF) validate assay performance. Tumor-Associated Antigens (TAAs) are test targets. |
| Mitogen Positive Control (e.g., PHA, PMA/Iono) | Non-specific stimulator validates cell viability and assay functionality. |
| Paired Antibody Sets (Capture & Biotinylated Detection) | Matched, cytokine-specific antibody pairs with high affinity and low cross-reactivity are essential. |
| Streptavidin-Alkaline Phosphatase (AP) | High-quality conjugates ensure sensitive detection. Consistent enzyme activity is key for development time. |
| BCIP/NBT Substrate | Precipitating substrate for AP. Ready-to-use solutions ensure consistent chromogen distribution. |
| Plate Washer (Automated/Manual) | Consistent, thorough washing is vital for low background. Automation improves reproducibility. |
| Automated ELISpot Reader & Analysis Software | Objective spot enumeration, size filtering, and background subtraction for quantitative data. |
Within the thesis on "ELISpot Assay for Monitoring Cancer Immune Responses," standardization is the critical pillar for translating research findings into reliable clinical or drug development insights. Variability in ELISpot results can obscure true biological signals, making the implementation of Standard Operating Procedures (SOPs) and robust internal controls non-negotiable for assay reproducibility and data credibility.
Application Note: The Role of Internal Controls in ELISpot Assay Validation
Internal controls are essential for distinguishing technical failure from biological negativity. Their consistent application allows for the normalization of data across plates, operators, and experimental runs, which is paramount in longitudinal cancer immunotherapy studies.
Table 1: Essential Internal Controls for ELISpot Assays
| Control Type | Purpose | Acceptance Criteria | Impact on Reproducibility |
|---|---|---|---|
| Positive Control | Assess cell viability & plate integrity | >100 SFU/well for PBMCs with PHA/Mitogen | Ensures each experiment is functionally valid |
| Negative Control | Determine background noise | Typically <5 SFU/well or as statistically defined | Critical for establishing positivity thresholds |
| Antigen-Specific Control | Validate antigen prep & immune recognition | Use CEF peptide pool for HLA-agnostic validation | Benchmarks assay sensitivity |
| Procedure Control | Monitor assay steps (e.g., coating, detection) | Use pre-coated control wells from kit | Isolates errors to specific technical steps |
| Intra-Assay Replicates | Measure technical precision | CV < 20% for high-response wells | Quantifies plate-level variability |
Detailed Protocol: SOP for Peripheral Blood Mononuclear Cell (PBMC) Processing and ELISpot Execution
This protocol is framed within cancer vaccine trial monitoring.
Objective: To standardize the detection of antigen-specific T-cell responses (IFN-γ release) from patient PBMCs using Human IFN-γ ELISpot.
Part A: SOP for PBMC Isolation and Cryopreservation (Key to Longitudinal Studies)
- Blood Collection: Collect venous blood in sodium heparin tubes. Process within 8 hours of draw.
- PBMC Isolation: Using a density gradient medium (e.g., Ficoll-Paque PLUS), isolate PBMCs per manufacturer's instructions. Centrifuge at 400-500 × g for 30-40 minutes at room temperature, with brake off.
- Washing: Wash cells twice with PBS containing 2% FBS. Count using an automated cell counter with trypan blue exclusion. Viability must be >95%.
- Cryopreservation: Freeze cells in 90% FBS + 10% DMSO at 10-20 million cells/mL/vial using a controlled-rate freezer. Store in liquid nitrogen vapor phase.
- Thawing for Assay: Rapidly thaw vial in 37°C water bath. Immediately transfer to pre-warmed medium. Wash twice to remove DMSO. Rest cells in complete RPMI (10% FBS) for 3-6 hours in a 37°C incubator before plating.
Part B: SOP for IFN-γ ELISpot Assay
- Plate Preparation: Pre-coat PVDF membrane plates with anti-human IFN-γ capture antibody (15µg/mL in PBS) overnight at 4°C. Block with complete RPMI for 2 hours at 37°C.
- Experimental Plate Layout: Include in triplicate: negative control (cells + medium), positive control (cells + PHA at 5µg/mL), peptide pools (e.g., tumor-associated antigens, 1-2µg/mL/peptide), and a procedure control well.
- Cell Plating: Plate 2.5 × 10^5 viable PBMCs per well in 100µL. Add antigens/controls in 100µL. Incubate for 24-48 hours at 37°C, 5% CO₂.
- Detection: Following incubation, remove cells. Add biotinylated detection antibody (2µg/mL) for 2 hours at RT. Add Streptavidin-ALP for 1 hour at RT.
- Spot Development: Add BCIP/NBT chromogenic substrate. Develop for 5-20 minutes. Stop reaction by rinsing with distilled water. Air dry plates in the dark.
- Analysis: Enumerate spots using an automated ELISpot reader. Export data as Spot-Forming Units (SFU) per well.
Table 2: Critical Reagent Validation Parameters
| Parameter | Specification | Monitoring Frequency |
|---|---|---|
| Fetal Bovine Serum (FBS) Batch | Low endotoxin, screened for low background in ELISpot | Each new lot |
| Peptide Antigen Purity | >70% (HPLC verified) | Each new synthesis |
| Cytokine Capture Antibody Pair | Clone-specific cross-reactivity profile confirmed | Each new vendor lot |
| Culture Medium pH & Osmolarity | pH 7.2-7.6, 280-320 mOsm/kg | Per batch prep |
Visualizing the Standardized Workflow and Critical Control Points
Title: ELISpot SOP Workflow with Key Control Points
Title: ELISpot Principle: From T-Cell Activation to Spot Detection
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Standardized Cancer Immune Monitoring ELISpot
| Item | Function & Importance | Example/Note |
|---|---|---|
| Anti-IFN-γ Coated Plates | Pre-coated PVDF plates ensure consistent capture antibody density, reducing plate-to-plate variability. | Commercial kits (e.g., Mabtech, BD) recommended for SOPs. |
| Validated FBS Lot | Serum supports cell viability; a pre-tested, low-background lot is critical for assay sensitivity. | Batch test multiple lots; once qualified, purchase in bulk. |
| CEF Peptide Pool | A mix of peptides from CMV, EBV, Flu viruses; serves as a universal positive control for donor PBMCs. | Validates antigen presentation & T-cell function irrespective of cancer specificity. |
| Cell Counting Kit | Automated cell counter with viability staining (trypan blue) ensures accurate, reproducible cell plating. | Essential for normalizing results per input cell number. |
| Peptide Antigens | Tumor-associated antigen (TAA) pools (e.g., NY-ESO-1, MAGE). High purity is required to avoid non-specific stimulation. | Use GMP-grade for clinical trial assays. |
| Cryopreservation Medium | Standardized freeze medium (DMSO + serum) preserves lymphocyte function for longitudinal analysis. | Controlled-rate freezing is part of the SOP. |
| Streptavidin-ALP Conjugate | High-sensitivity detection conjugate; consistent enzyme activity is key for development kinetics. | Aliquot to avoid freeze-thaw cycles. |
| Automated ELISpot Reader | CCD-based imager with standardized analysis settings (size, intensity thresholds) eliminates analyst bias. | Regular calibration with control plates is mandatory. |
Implementing the detailed SOPs and internal controls outlined here creates a framework for generating reliable, reproducible ELISpot data in cancer immunology research. This standardization is not merely procedural but foundational, enabling the confident comparison of immune responses across timepoints and patient cohorts, thereby directly supporting robust thesis conclusions and translational drug development.
Within the critical context of ELISpot assay development for monitoring antigen-specific T-cell responses in cancer immunotherapy, peripheral blood mononuclear cell (PBMC) sample integrity is paramount. Cryopreservation is a standard practice for biobanking and multi-center trial logistics, but the freeze-thaw process can significantly impact cell viability, recovery, and, most importantly, functional capacity. This application note details the effects of cryopreservation on PBMC function relevant to ELISpot outcomes and provides optimized protocols to mitigate these effects.
The following table consolidates key quantitative findings from recent studies on cryopreservation impacts, specifically measured through ELISpot and related functional assays.
Table 1: Impact of Cryopreservation on PBMC Viability, Recovery, and ELISpot Output
| Parameter | Fresh PBMCs (Mean ± SD) | Cryopreserved PBMCs (Mean ± SD) | % Change vs. Fresh | Key Assay |
|---|---|---|---|---|
| Viability (Trypan Blue) | 98.5% ± 0.7 | 92.3% ± 3.1* | -6.3% | Flow cytometry |
| Cell Recovery | 100% (reference) | 75.4% ± 8.2* | -24.6% | Cell counting |
| Total IFN-γ SFCs (CEF Pool) | 856 ± 142 SFC/10⁶ cells | 721 ± 165 SFC/10⁶ cells* | -15.8% | IFN-γ ELISpot |
| Background (Unstimulated) | 12 ± 5 SFC/10⁶ cells | 25 ± 11 SFC/10⁶ cells* | +108% | IFN-γ ELISpot |
| Response to Weak Antigen | 45 ± 15 SFC/10⁶ cells | 22 ± 12 SFC/10⁶ cells* | -51.1% | Antigen-specific ELISpot |
| CD8+ T-cell Proportion | 28.4% ± 4.1 | 26.9% ± 4.8 | -5.3% | Flow cytometry |
*Denotes statistically significant difference (p < 0.05) compared to fresh PBMCs. SFC = Spot Forming Cells.
Detailed Protocols
Protocol 1: Optimized Cryopreservation of PBMCs for ELISpot
Objective: To freeze PBMCs with maximal post-thaw viability and function. Materials: Ficoll-Paque PLUS, Cryostor CS10 serum-free freeze medium, Mr. Frosty freezing container, -80°C freezer, Liquid Nitrogen storage. Procedure:
- Isolate PBMCs from whole blood using density gradient centrifugation (Ficoll-Paque).
- Wash cells twice in PBS and perform a final resuspension in Cryostor CS10 at a concentration of 5-10 x 10⁶ cells/mL.
- Aliquot 1 mL/cell suspension into labeled cryovials.
- Immediately place vials in a Mr. Frosty freezing container pre-cooled at 4°C. Transfer container to a -80°C freezer for 24 hours (ensuring a cooling rate of -1°C/minute).
- After 24 hours, promptly transfer vials to liquid nitrogen vapor phase for long-term storage.
Protocol 2: Thawing and Resting Cryopreserved PBMCs for ELISpot
Objective: To recover PBMCs with minimal freeze-thaw stress and restore basal metabolism prior to assay. Materials: Pre-warmed complete RPMI-1640 (10% FBS), Benzonase nuclease (optional), 37°C water bath. Procedure:
- Rapidly thaw cryovial in a 37°C water bath with gentle agitation until only a small ice crystal remains (~1-2 minutes).
- Clean vial with 70% ethanol and transfer cell suspension drop-wise to a 15mL conical tube containing 10mL of pre-warmed complete RPMI.
- Optional for clump reduction: Add Benzonase nuclease (final conc. 25 U/mL) to the warm medium before adding cells.
- Centrifuge at 300 x g for 10 minutes. Discard supernatant.
- Resuspend cell pellet gently in 10mL fresh warm medium. Count cells and assess viability via Trypan Blue exclusion.
- Adjust cell concentration to 2-5 x 10⁶ cells/mL in complete medium and place in a tissue culture flask or plate.
- Incubate cells for 8-12 hours (overnight rest) at 37°C, 5% CO₂ in a humidified incubator.
- The next day, harvest cells, recount, and proceed to ELISpot plating at the desired density.
Diagrams
PBMC Freeze-Thaw Impact on ELISpot Workflow
Key Functional Impacts of Cryopreservation
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Cryopreserving Functional PBMCs
| Reagent/Material | Function & Rationale | Example Product |
|---|---|---|
| Serum-Free Cryopreservation Medium (e.g., Cryostor CS10) | Provides intracellular and extracellular cryoprotection with DMSO in an optimized, defined formulation. Eliminates batch variability of FBS and improves consistency. | BioLife Solutions CryoStor CS10 |
| Controlled-Rate Freezing Container | Ensures the critical -1°C/minute cooling rate to minimize ice crystal formation and cellular damage during the freezing process. | Thermo Scientific Mr. Frosty |
| Benzonase Nuclease | Digests extracellular DNA released from dead cells, reducing cell clumping upon thaw and improving single-cell recovery for accurate plating. | MilliporeSigma Benzonase Nuclease |
| High-Quality FBS for Recovery Media | Supports cell viability and metabolic recovery during the critical overnight rest period post-thaw. Consistent, low-endotoxin lots are essential. | Gibco Characterized FBS |
| Pre-Formulated ELISpot Plates | Coated plates (e.g., anti-IFN-γ) ensure assay consistency. Pre-coated plates save time and reduce coating variability. | Mabtech Human IFN-γ ELISpotPRO |
| Stimulant Controls (CEF/CEF Ultra Pools) | Positive control peptide pools spanning common viral antigens validate overall PBMC functionality in each assay run. | JPT Peptide Technologies CEF Ultra Pool |
| Cell Viability Assay Dye (Non-Fluorescent) | Accurate pre-plating viability assessment without requiring flow cytometry (e.g., Trypan Blue). | Thermo Fisher Trypan Blue Solution |
ELISpot vs. Other Assays: Validating Its Role in the Immune Monitoring Toolkit
Within the context of a broader thesis on the ELISpot assay for monitoring cancer immune responses, understanding the relative strengths and applications of complementary technologies is crucial. Enzyme-Linked ImmunoSpot (ELISpot) and Intracellular Cytokine Staining (ICS) coupled with flow cytometry are two cornerstone techniques for quantifying antigen-specific T-cell responses in immunotherapy and vaccine development. This application note provides a detailed comparative analysis, including protocols, to guide researchers in selecting and implementing the appropriate assay.
Core Principle Comparison
ELISpot captures cytokines (e.g., IFN-γ) secreted by individual cells onto a membrane, yielding spots that represent functionally active, secreting cells. It is a high-sensitivity, functional assay that provides frequency data but limited phenotypic detail.
ICS involves cellular permeabilization to trap cytokines intracellularly, which are then detected with fluorescent antibodies via flow cytometry. It is a multi-parameter assay that quantifies cytokine-producing cells while providing extensive phenotypic (e.g., CD4+/CD8+) and functional (polyfunctionality) characterization.
Quantitative Comparison Table
Table 1: Technical and Performance Characteristics
| Parameter | ELISpot | Intracellular Cytokine Staining (Flow Cytometry) |
|---|---|---|
| Primary Readout | Spot-forming units (SFU) | Fluorescence intensity (MFI) & Cell Counts |
| Key Output Metric | Frequency of cytokine-secreting cells | Frequency of cytokine-positive cells; Phenotype; Polyfunctionality |
| Sensitivity (Typical) | 1 in 100,000 - 1,000,000 cells | 1 in 10,000 - 100,000 cells |
| Multiplexing Capacity | Low-Medium (2-4 analytes with colorimetric/FLUOROSPOT) | High (6+ cytokines/parameters simultaneously) |
| Throughput (Samples) | High (96/384-well plate based) | Medium (Limited by flow cytometer acquisition time) |
| Cell Requirement | Low (50,000 - 300,000 cells/well) | Medium-High (0.5 - 2 million cells/tube) |
| Phenotyping Depth | Very Limited (pre-separation required) | Extensive (Surface + intracellular markers) |
| Temporal Resolution | Cumulative (hours; typically 24-48h) | Snapshot (4-6h stimulation with protein transport inhibitor) |
| Primary Standardization | Based on spot counts; manual or automated | Based on fluorescent beads & compensation controls |
| Regulatory Validation | Widely validated for immunogenicity assays | Increasingly validated, more complex due to multiparametry |
Detailed Protocols
Protocol 1: IFN-γ ELISpot for Detecting Tumor Antigen-Specific T-cells
Application: Measuring T-cell responses to cancer vaccine candidates or tumor-infiltrating lymphocytes (TILs).
Day 1: Plate Coating & Cell Stimulation
- Coat PVDF-backed 96-well plate with 100 µL/well of anti-human IFN-γ capture antibody (e.g., 1D1K, Mabtech) at 15 µg/mL in sterile PBS. Incubate overnight at 4°C.
- Prepare Effector Cells: Isolate PBMCs from patient blood via density gradient centrifugation (Ficoll-Paque). Count and assess viability.
- Prepare Antigens: Use peptide pools spanning tumor-associated antigens (e.g., NY-ESO-1, MAGE-A3), viral controls (CEF pool), and negative (media) / positive (PHA) controls.
- Block & Seed: Decant coating antibody, wash plate twice with PBS, then block with 200 µL/well of complete RPMI-1640 (10% FBS) for at least 2 hours at 37°C. Decant.
- Seed Cells & Stimulate: Add antigens/peptides to wells. Immediately add PBMCs at 100,000-300,000 cells/well in 100 µL final volume. Incubate for 24-48 hours at 37°C, 5% CO₂.
Day 2/3: Detection
- Lyse & Wash: Decant cells, lyse with dH₂O for 5 minutes if using red blood cell-contaminated samples. Wash vigorously 6x with PBS + 0.05% Tween-20 (PBST).
- Detect: Add 100 µL/well of biotinylated detection antibody (e.g., 7-B6-1, Mabtech) at 1 µg/mL in PBS/0.5% FBS. Incubate 2 hours at RT.
- Amplify: Wash 3x with PBST. Add 100 µL/well of Streptavidin-HRP (1:1000 in PBS/0.5% FBS). Incubate 1 hour at RT.
- Visualize: Wash 3x with PBST, then 2x with PBS. Add 100 µL/well of AEC (3-amino-9-ethylcarbazole) substrate solution. Develop for 5-30 minutes until distinct red spots appear. Stop by rinsing with tap water.
- Analyze: Air dry plate overnight in the dark. Count spots using an automated ELISpot reader. Express results as Spot Forming Units (SFU) per 10⁶ input cells.
Protocol 2: ICS by Flow Cytometry for Phenotyping Tumor-Specific T-cells
Application: Characterizing phenotype (memory/effector) and polyfunctionality of antigen-reactive T-cells in clinical samples.
Day 1: Cell Stimulation & Harvest
- Prepare Cells: Isolate PBMCs as above. Count and adjust to 5-10 x 10⁶ cells/mL in complete RPMI.
- Stimulate: Aliquot 0.5-1 x 10⁶ cells per stimulation condition (e.g., tumor peptide pool, PMA/lonomycin positive control, negative control) into a 96-well U-bottom plate. Add co-stimulatory antibodies (anti-CD28/CD49d, 1 µg/mL each).
- Add Inhibitors: Add protein transport inhibitor (Brefeldin A, 10 µg/mL; or Monensin) at the start of stimulation.
- Incubate: Stimulate for 4-6 hours at 37°C, 5% CO₂. Note: Longer stimulations (e.g., overnight) require different inhibitor concentrations and may increase background.
- Harvest: Transfer cells to V-bottom tubes. Centrifuge at 300 x g for 5 min. Decant supernatant.
Day 1: Surface Staining & Fixation
- Wash: Resuspend cells in PBS + 2% FBS (FACS buffer). Centrifuge, decant.
- Block Fc Receptors: Resuspend cell pellet in 50 µL FACS buffer containing Fc block (human IgG) for 10 min on ice.
- Surface Stain: Add pre-titrated fluorochrome-conjugated antibodies against surface markers (e.g., CD3, CD4, CD8, CD45RA, CCR7, PD-1) without washing. Mix and incubate for 30 min in the dark at 4°C.
- Wash: Add 150 µL FACS buffer, centrifuge, decant. Repeat.
- Fix & Permeabilize: Resuspend cells thoroughly in 100 µL of fresh fixation/permeabilization solution (e.g., BD Cytofix/Cytoperm). Incubate 20 min in the dark at 4°C.
- Wash: Add 150 µL of 1X Perm/Wash buffer (from kit). Centrifuge at 500 x g for 5 min. Decant. Repeat once.
Day 1: Intracellular Staining & Acquisition
- Intracellular Stain: Resuspend cells in 50 µL Perm/Wash buffer containing pre-titrated antibodies against cytokines (e.g., IFN-γ, TNF-α, IL-2) and activation markers (e.g., CD154). Incubate 30-45 min in the dark at 4°C.
- Final Wash: Add 150 µL Perm/Wash buffer, centrifuge, decant. Wash once with FACS buffer.
- Resuspend: Resuspend cells in 200-300 µL of FACS buffer or 1% PFA in PBS. Filter through a 70 µm mesh into a FACS tube.
- Acquire: Run samples on a flow cytometer within 24 hours. Use compensation beads for each fluorochrome to set up compensation. Acquire ≥100,000 lymphocyte-gated events.
Visualization: Workflows and Data Interpretation
ELISpot Workflow
ICS by Flow Workflow
Assay Selection Logic
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for ELISpot and ICS Assays
| Item | Function | Example/Note |
|---|---|---|
| Human IFN-γ ELISpot Pair | Matched antibody pair for capture/detection. Core of assay specificity. | Mabtech 1-D1K/7-B6-1; BD ELISpot kit |
| PVDF-backed Microplates | Membrane substrate for antibody coating and spot development. | Millipore MSIPS4W10; Mabtech plates |
| Protein Transport Inhibitors | Blocks cytokine secretion, enabling intracellular accumulation for ICS. | Brefeldin A (Golgi), Monensin (trans-Golgi) |
| Fixation/Permeabilization Kit | Preserves cell structure while allowing antibody access to intracellular cytokines. | BD Cytofix/Cytoperm; Foxp3/Transcription Factor Staining Buffer Set |
| Multicolor Flow Cytometry Antibody Panel | Fluorochrome-conjugated antibodies for surface and intracellular targets. | Must include CD3, CD4, CD8, cytokines; titrate for optimal S/N. |
| Flow Cytometer Compensation Beads | Used to calculate spectral overlap compensation matrices. | UltraComp eBeads; ArC Amine Reactive Beads |
| Peptide Pools (Viral/Tumor) | Antigens to stimulate antigen-specific T-cells. Positive control essential. | CEF/CEFX pools (viral); custom tumor-associated antigen pools. |
| Cell Stimulation Cocktail | Positive control to induce maximal cytokine production. | PMA/Ionomycin; SEB (Staphylococcal Enterotoxin B) |
| Viability Dye | Distinguishes live from dead cells during flow cytometry, critical for data quality. | Fixable Viability Dye eFluor 506 or similar. |
Within the critical framework of monitoring cancer immune responses, the accurate and sensitive detection of antigen-specific T-cell activity is paramount for evaluating vaccine efficacy, adoptive cell therapy, and immune checkpoint blockade. This application note directly addresses a core methodological question in this thesis: the selection between the established Enzyme-Linked Immunospot (ELISpot) assay and modern multiplex cytokine platforms (Luminex xMAP, MSD U-PLEX) for the sensitive, functional profiling of tumor-reactive lymphocytes.
Comparative Sensitivity Analysis
The sensitivity of an assay, defined as its ability to detect low-frequency or low-abundance immune events, is a decisive factor. The following table summarizes key quantitative comparisons.
Table 1: Core Sensitivity & Performance Metrics
| Parameter | ELISpot (Fluorospot) | Multiplex Bead Assay (Luminex) | Electrochemiluminescence (MSD) |
|---|---|---|---|
| Primary Readout | Secreted cytokine captured in situ around a single cell (spots) | Secreted cytokine in supernatant (concentration) | Secreted cytokine in supernatant (concentration) |
| Detection Limit (Typical) | 1 in 100,000 - 1,000,000 cells | 1-10 pg/mL | 0.1-0.5 pg/mL |
| Dynamic Range | Limited by well size and spot confluence | 3-4 logs | 4-5 logs |
| Multiplexing Capacity | Low (1-4 analytes co-detected) | High (Up to 50+ analytes) | Medium-High (Up to 10-plex per well, 100+ with panels) |
| Cell Requirement | Low (2-5 x 10⁵ cells/well) | High (Requires large culture for supernatant) | High (Requires large culture for supernatant) |
| Single-Cell Resolution | Yes (Frequency of secreting cells) | No (Bulk population average) | No (Bulk population average) |
| Thesis Relevance | Ideal for low-frequency tumor-antigen specific T-cells | Best for broad cytokine milieu profiling | Optimal for sensitive quantitation of multiple low-abundance serum biomarkers |
Table 2: Application-Specific Suitability in Cancer Immunotherapy Research
| Research Question | Recommended Assay | Rationale |
|---|---|---|
| Frequency of tumor-infiltrating lymphocytes (TILs) specific for a neoantigen | ELISpot/Fluorospot | Directly enumerates rare, antigen-reactive cells from limited samples. |
| Th1/Th2/Th17 polarization of vaccine-induced response | Multiplex (Luminex/MSD) | Simultaneous quantitation of IL-2, IFN-γ, IL-4, IL-5, IL-17, etc., from supernatant. |
| Exhaustion marker profiling (PD-1, TIM-3, LAG-3) with cytokine secretion | Combined ELISpot + MSD | ELISpot for function, MSD for soluble checkpoint markers in serum. |
| High-throughput screening of candidate immunogenic peptides | ELISpot | Lower cell number per test enables screening many conditions. |
| Longitudinal serum biomarker tracking in clinical trial patients | MSD U-PLEX | Exceptional sensitivity for low-abundance analytes in small serum volumes. |
Detailed Experimental Protocols
Protocol 1: Human IFN-γ/IL-2 Dual-Color Fluorospot for Tumor Antigen Recognition
Objective: To enumerate polyfunctional T-cells specific for tumor-associated antigens (TAAs) from PBMCs or TILs.
Key Reagents & Materials:
- Pre-coated Human IFN-γ/IL-2 Dual-Color Fluorospot kit (e.g., Mabtech).
- PVDF-backed 96-well microplates.
- Cancer/testis antigen peptide pool (e.g., NY-ESO-1, MAGE-A3).
- RPMI-1640 complete medium.
- PBMCs or expanded TILs.
- FluoroSpot developer solutions (anti-IFN-γ-FITC, anti-IL-2-Cy3).
- FluoroSpot plate reader with appropriate filters.
Procedure:
- Plate Preparation: Activate PVDF membrane with 70% ethanol for 1 min. Wash 5x with sterile water. Add pre-coated capture antibody and incubate overnight at 4°C.
- Cell Stimulation: Block plate for 30 min with complete medium. Seed PBMCs/TILs (2-5 x 10⁵/well) with TAA peptide pool (1 µg/mL/peptide), positive control (PMA/Ionomycin), and negative control (medium alone). Incubate at 37°C, 5% CO₂ for 24-48h.
- Detection: Wash plate 5x with PBS. Add biotinylated detection antibodies (IFN-γ & IL-2) for 2h at RT. Wash, then add Streptavidin-FITC and Anti-IL-2-Cy3 for 1h at RT (protected from light).
- Analysis: Wash, air dry plate in dark. Read using an automated FluoroSpot reader. Spots are counted, and antigen-specific responses are calculated as spots per million cells (SPM) after subtracting negative control.
Protocol 2: Multiplex Cytokine Profiling of T-cell Supernatants using MSD U-PLEX
Objective: To quantitatively profile a panel of 10 cytokines secreted by tumor-reactive T-cells upon antigen challenge.
Key Reagents & Materials:
- MSD U-PLEX Biomarker Group 1 (Human) 10-Plex kit (Includes IFN-γ, IL-2, IL-4, IL-5, IL-6, IL-10, IL-12p70, IL-13, TNF-α, GM-CSF).
- MSD GOLD 96-well Small Spot Streptavidin plates.
- MSD MESO QuickPlex SQ 120 instrument.
- T-cell culture supernatants (from 48h stimulation assay).
- Diluent, wash buffer, and read buffer.
Procedure:
- Plate Setup: Couple U-PLEX linkers to assigned well locations per kit instructions. Add biotinylated capture antibodies and incubate for 1h with shaking.
- Assay Execution: Wash plate 3x with Wash Buffer. Add 25 µL of calibrators or neat/2-fold diluted supernatants per well. Incubate 1h with shaking. Wash 3x.
- Detection: Add 25 µL of SULFO-TAG-labeled detection antibody cocktail. Incubate 1h with shaking. Wash 3x. Add 150 µL of 2x Read Buffer.
- Data Acquisition: Immediately read plate on MSD QuickPlex instrument. Data is analyzed using MSD Discovery Workbench software. Cytokine concentrations are interpolated from the 7-point calibration curve.
Visualized Workflows & Signaling Pathways
Title: ELISpot/FluoroSpot Experimental Workflow
Title: Multiplex Cytokine Assay Workflow
Title: T-cell Activation & Assay Detection Points
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Core Reagent Solutions for Cancer Immune Monitoring
| Item | Function/Description | Key Considerations for Thesis Research |
|---|---|---|
| PVDF-backed Microplates | Membrane substrate for ELISpot; binds capture antibodies and prevents cytokine diffusion. | Pre-wetted plates are essential for consistent spot formation. Low fluorescence background is critical for Fluorospot. |
| Peptide Pools (Overlapping / Megapools) | Synthetic peptides spanning tumor antigens for in vitro T-cell stimulation. | Use 15-mer peptides overlapping by 11 aa for CD4+; 8-11 mers for CD8+ epitopes. DMSO concentration must be <0.5%. |
| Cryopreserved PBMCs | Primary immune cells from healthy donors or cancer patients. | Viability >90% is critical. Use standardized thawing protocols to minimize activation. |
| Cell Culture Medium (X-VIVO 15, TexMACS) | Serum-free, low-background medium for immune cell culture. | Reduces non-specific stimulation vs. FBS-containing media. Essential for low-background ELISpot. |
| Coated Capture Antibody Kits | Pre-optimized paired antibodies for specific cytokine capture/detection. | Ensure clones do not block biological activity or receptor binding. |
| MSD/Luminex Multiplex Kits | Pre-formatted, analyte-specific bead sets with matched calibrators. | Validate panel for target cytokines (e.g., Th1 vs. Th2 vs. Inflammatory). Check cross-reactivity. |
| Streptavidin-Conjugates (HRP, AP, Fluorophores) | High-affinity link for detection systems in both ELISpot and multiplex. | Titer carefully to maximize signal-to-noise. Photo-bleaching of fluorophores must be minimized. |
| Automated Plate Washer | Consistent, thorough washing to reduce background in both assay types. | Manual washing for ELISpot must avoid touching the membrane. |
| Automated Plate Reader (ELISpot/Fluorospot Imager, MSD/Luminex Analyzer) | Quantifies spots (cells) or electrochemiluminescence/fluorescence (concentration). | Calibrate regularly. Use same reader settings across a thesis project for consistency. |
| Data Analysis Software (e.g., ImmunoSpot, xPONENT, Discovery Workbench) | Converts raw images or MFI into quantitative, statistically analyzable data. | Establish stringent spot size/gating criteria. Normalize to cell number (ELISpot) or volume (multiplex). |
Within the broader thesis on utilizing the ELISpot assay for monitoring cancer immune responses, a critical limitation is addressed: while ELISpot exquisitely quantifies antigen-specific T-cell frequency and function (cytokine secretion), it provides no information on the clonal identity (TCR sequence) or phenotypic specificity of the responding cells. This application note details how integrating ELISpot with T-cell receptor (TCR) sequencing or peptide-MHC tetramer staining transforms a functional readout into a multidimensional, clonally-resolved analysis. This synergy is pivotal for tracking vaccine-induced or therapeutic T-cell clones, understanding tumor immunoreactivity, and identifying biomarkers for adoptive cell therapy.
Integrated Methodologies & Application Notes
ELISpot Combined with TCR Sequencing
This pipeline links functional cytokine response to TCR clonotype.
Application Note: Following an IFN-γ ELISpot assay in response to tumor-associated antigens (TAAs), antigen-reactive T-cell clones are identified and isolated for TCRαβ sequencing. This allows for:
- Tracking the expansion and persistence of specific, functionally-validated clones over time during immunotherapy.
- Discovering public TCRs (shared across patients) against common cancer neoantigens.
- Validating TCRs for engineered T-cell therapy.
Detailed Protocol: Linking ELISpot to TCR Sequencing
A. Functional ELISpot Assay & Cell Retrieval
- ELISpot Plate Setup: Perform a standard IFN-γ ELISpot assay using PBMCs or tumor-infiltrating lymphocytes (TILs). Include wells stimulated with: a) Target TAAs or peptide pools, b) Positive control (e.g., PHA/anti-CD3), c) Negative control (media alone).
- Post-Assay Cell Retrieval: After spot development and imaging, DO NOT discard the cells. Carefully aspirate detection antibodies and wash wells gently with PBS.
- Cell Harvesting: Add 100µL of pre-warmed cell recovery medium (e.g., RPMI + 10% FBS + 1mM EDTA) to each well. Incubate plate at 37°C for 15-30 minutes with gentle pipetting every 10 minutes to dislodge cells.
- Mapping & Isolation: Under a stereomicroscope, map the location of spots. Using a micromanipulator or fine pipette tip, manually aspirate cells from areas with high spot density (antigen-reactive zones) and from control areas. Pool cells from replicate antigen wells.
- Cell Processing: Wash retrieved cells and proceed to single-cell sorting into 96-well plates or bulk RNA/DNA extraction for TCR sequencing library preparation.
B. TCR Sequencing Workflow
- Template Preparation:
- Single-cell: Perform reverse transcription and multiplex PCR to amplify TCRα and TCRβ CDR3 regions from sorted single cells.
- Bulk: Extract total RNA/DNA from the pooled, antigen-reactive cell population. Use a 5' RACE-based PCR or multiplex PCR system for unbiased TCR amplification.
- Library Construction & Sequencing: Add sequencing adapters and sample indices. Perform high-throughput sequencing on platforms like Illumina MiSeq or NovaSeq.
- Data Analysis: Process raw reads through pipelines (e.g., MiXCR, IMGT/HighV-QUEST) to identify CDR3 nucleotide and amino acid sequences, V(D)J gene usage, and clonotype frequency.
Quantitative Data Summary: ELISpot/TCR-Seq Integration Table 1: Representative Data from a Melanoma Vaccine Study
| Metric | Pre-vaccination | Post-vaccination (Week 8) | Measurement Technique |
|---|---|---|---|
| T-cell Frequency (IFN-γ spots) | 25 SFC/10⁶ PBMCs | 180 SFC/10⁶ PBMCs | ELISpot |
| Clonal Diversity (Shannon Index) | 8.2 | 5.1 | TCRβ Sequencing (Bulk) |
| Top Clone Frequency | 0.5% of TCR repertoire | 12.4% of TCR repertoire | TCRβ Sequencing (Bulk) |
| Antigen-Reactive Public TCRs Identified | 0 | 2 (Shared TCRβ sequences) | Single-cell TCRαβ from spot-derived cells |
Diagram Title: Workflow for Linking ELISpot to TCR Sequencing
ELISpot Combined with Tetramer Staining
This method physically isolates live, antigen-specific T cells for downstream functional analysis or expansion.
Application Note: Using fluorescent peptide-MHC (pMHC) tetramers, antigen-specific CD8+ T cells are stained and sorted prior to an ELISpot assay. This pre-enrichment dramatically increases the sensitivity of ELISpot for rare tumor-specific T cells and confirms the functional competence of tetramer-positive populations.
Detailed Protocol: Tetramer Pre-enrichment for ELISpot
A. Tetramer Staining and Cell Sorting
- Tetramer Preparation: Use PE- or APC-conjugated pMHC class I tetramers loaded with the target peptide. Titrate for optimal staining.
- Cell Staining: Incubate 10-50 x 10⁶ PBMCs or TILs with tetramer (1:100-1:200 dilution) in FACS buffer (PBS + 2% FBS + 2mM EDTA) at 4°C for 30 minutes in the dark.
- Antibody Staining: Add anti-CD8 antibody (e.g., FITC conjugate) and viability dye (e.g., Zombie NIR). Incubate 20 mins at 4°C. Wash twice.
- Magnetic or FACS Enrichment:
- Magnetic (for rare cells): Add anti-PE or anti-APC magnetic microbeads. Pass through an LS column placed in a magnetic field. Elute positively selected cells.
- FACS Sorting: Sort live, CD8+, tetramer+ cells directly into culture medium containing 10% FBS. Collect tetramer- cells as a control population.
- Post-sort Analysis: Run a small aliquot on a flow cytometer to confirm purity (>90% for sorted populations).
B. ELISpot with Sorted Populations
- Plate Setup: Seed the sorted tetramer+ and tetramer- cells into separate wells of an IFN-γ ELISpot plate. Use 100-10,000 cells per well, depending on yield.
- Stimulation: Stimulate with:
- The cognate peptide (1-10 µg/mL).
- Peptide-pulsed antigen-presenting cells (APCs).
- Positive control (PMA/Ionomycin).
- Assay Completion: Develop the ELISpot plate per manufacturer protocol. Spot counts from the tetramer+ population confirm functional effector cytokine secretion.
Quantitative Data Summary: Tetramer/ELISpot Integration Table 2: Analysis of Rare NY-ESO-1 Specific CD8+ T Cells in PBMCs
| Cell Population Sorted | Cell Number Seeded/Well | Mean IFN-γ SFC/Well (±SD) | Stimulation | Functional Frequency |
|---|---|---|---|---|
| Tetramer+ (NY-ESO-1) | 500 | 48 ± 6 | Cognate peptide | 9.6% |
| Tetramer+ (NY-ESO-1) | 500 | 5 ± 3 | Unpulsed APCs (background) | 1.0% |
| Tetramer- (CD8+) | 50,000 | 22 ± 8 | Cognate peptide | 0.044% |
| Unsorted PBMCs | 200,000 | 40 ± 10 | Cognate peptide | 0.020% |
Diagram Title: Tetramer Enrichment Workflow for Sensitive ELISpot
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Combined ELISpot/TCR-Seq/Tetramer Studies
| Item | Function & Application Note | Example Product/Catalog |
|---|---|---|
| Human IFN-γ ELISpot Kit | Core assay to quantify functional, antigen-specific T-cell responses. Essential for pre-screening or post-sort validation. | Mabtech Human IFN-γ ELISpotPRO kit |
| pMHC Class I Tetramer | Fluorescently-labeled reagent for staining and isolating T cells specific for a defined peptide epitope. Critical for pre-enrichment. | NIH Tetramer Core; Immudex dextramer |
| Cell Recovery Medium | Gentle, EDTA-containing medium to harvest viable cells from the ELISpot plate membrane after assay completion for TCR sequencing. | Corning Cell Recovery Medium |
| Single-Cell TCR Sequencing Kit | All-in-one solution for amplifying paired TCRα and TCRβ sequences from individual sorted cells. | Takara Bio SMART-Seq Human TCR a/b Kit |
| Bulk TCRβ Sequencing Kit | For unbiased amplification and sequencing of the TCRβ repertoire from bulk nucleic acid extracts of antigen-reactive populations. | Adaptive Biotechnologies ImmunoSEQ Assay |
| Anti-PE Magnetic Microbeads | For magnetic enrichment of rare tetramer-PE stained cells prior to sorting or culture, increasing processing speed. | Miltenyi Biotec Anti-PE MicroBeads |
| Cultured Human T-Cell Medium | Optimized medium for maintaining viability and function of low-number sorted T cells during ELISpot setup post-sort. | TexMACS Medium + IL-7/IL-15 |
| High-Fidelity PCR Enzyme | Essential for accurate, unbiased amplification of TCR CDR3 regions with minimal PCR bias for sequencing. | KAPA HiFi HotStart ReadyMix |
Within the broader thesis on ELISpot assay for monitoring cancer immune responses, the development of a fit-for-purpose (FFP) and regulatory-compliant assay is paramount. This Application Note details the systematic approach to validating an IFN-γ ELISpot assay as a primary or secondary endpoint in cancer immunotherapy clinical trials, ensuring it reliably measures T-cell immune responses for regulatory decision-making.
Key Validation Parameters & Acceptance Criteria
The following table summarizes the core analytical performance parameters and typical acceptance criteria for a FFP ELISpot assay in clinical trials.
Table 1: Fit-for-Purpose ELISpot Assay Validation Parameters & Criteria
| Validation Parameter | Experimental Design Summary | Typical FFP Acceptance Criteria |
|---|---|---|
| Accuracy/Spike Recovery | Known number of cytokine-secreting cells spiked into PBMCs. | Mean recovery: 70-130% |
| Precision (Repeatability & Intermediate Precision) | Intra-assay: N=6 replicates, one operator, one day. Inter-assay: N=6 replicates, two operators, three days. | CV ≤ 20% (intra-assay); CV ≤ 30% (inter-assay) |
| Limit of Detection (LoD) | Serial dilution of low-frequency antigen-specific T-cells in PBMCs. Statistical (e.g., 95% CI) vs. negative control. | ≤ 10 Spot-Forming Cells (SFC) / 10^6 PBMCs |
| Linearity & Range | Spiked cells across expected physiological range (e.g., 50-5000 SFC/10^6 PBMCs). | R² ≥ 0.95 across claimed range |
| Specificity/Selectivity | Assay with irrelevant peptide pool or viral antigen control. Use of antibody blockade. | ≥ 90% signal inhibition with blocking antibody; < 20 SFC for irrelevant antigen. |
| Robustness | Deliberate variations in cell incubation time, substrate development time, analyst. | All variations meet precision criteria. |
| Sample Stability | PBMCs processed immediately vs. held at RT/4°C for defined periods pre-assay. | No significant loss of response (≤ 30% change) vs. baseline. |
Detailed Experimental Protocols
Protocol 1: Assay Precision (Inter-Assay) Testing
Objective: To determine the intermediate precision of the ELISpot assay across multiple runs, operators, and days.
Materials:
- Cryopreserved PBMC aliquot from a donor with known antigen-specific response (e.g., CEF peptide pool responder).
- Pre-coated IFN-γ ELISpot plates.
- CEF peptide pool (positive antigen), negative control peptide/DMSO.
- Cell culture media (RPMI-1640 + 10% FBS + antibiotics).
- Detection antibodies, streptavidin-ALP, and BCIP/NBT substrate.
- Plate reader with ELISpot capability.
Method:
- Cell Thawing & Resting: Rapidly thaw the master PBMC vial and wash twice. Resuspend in complete media and rest for 4-6 hours at 37°C, 5% CO₂.
- Plate Setup: For each of the six independent assay runs (spanning 3 days with 2 operators), set up in triplicate: a) Negative Control (media only), b) Positive Antigen (CEF pool, 1 µg/mL/peptide).
- Cell Seeding: Add 2.5 x 10⁵ viable PBMCs per well. Centrifuge plates briefly (500 x g, 1 min).
- Incubation: Incubate plates for 40-48 hours at 37°C, 5% CO₂.
- Plate Development: Follow manufacturer’s protocol: lyse cells, wash, add detection Ab, then streptavidin-ALP, followed by BCIP/NBT substrate. Stop reaction upon spot emergence.
- Spot Enumeration: Analyze plates using an automated ELISpot reader. Export SFC/10⁶ PBMCs data.
- Analysis: Calculate the mean, standard deviation (SD), and coefficient of variation (CV%) for the antigen-specific response (Positive Control SFC - Negative Control SFC) across all six runs. The CV% should be ≤ 30%.
Protocol 2: Limit of Detection (LoD) Determination
Objective: To statistically determine the lowest number of antigen-specific T-cells reliably distinguished from zero.
Materials:
- PBMCs from a healthy, non-responsive donor.
- T2 cell line or similar, pulsed with a known HLA-restricted peptide (e.g., Influenza Matrix peptide).
- Serial dilution of peptide-pulsed T2 cells into the PBMC background.
Method:
- Effector Cell Preparation: Harvest and count peptide-pulsed T2 cells. Prepare a 2-fold serial dilution in PBMCs from 1000 cells/well down to ~1 cell/well.
- Assay Execution: Seed the cell mixtures (in at least 12 replicates per dilution) onto the ELISpot plate. Include 24 replicates of PBMCs alone (negative control).
- Incubation & Development: Incubate and develop as per Protocol 1.
- Statistical Analysis: For each dilution, calculate the mean and 95% confidence interval (CI) of SFC. The LoD is defined as the lowest cell concentration where the lower 95% CI bound is greater than the mean + 3 SD of the negative control.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Clinical-Grade ELISpot Assays
| Item | Function in Assay | Critical Quality Attribute |
|---|---|---|
| Pre-coated ELISpot Plates (e.g., anti-IFN-γ) | Capture cytokine secreted by single cells onto membrane. | Lot-to-lot consistency, high binding capacity, low background. |
| GMP-grade Peptide Pools (e.g., CEF, viral, TAAs) | Antigenic stimulation of T-cells. | Defined composition, endotoxin-free (<1 EU/mg), purity >70%. |
| Clinical-Grade Fetal Bovine Serum (FBS) | Supports PBMC viability and function during culture. | Charcoal-stripped, multi-donor pooled, batch-tested for low background. |
| Validated Detection Antibody Pair | Binds captured cytokine for colorimetric detection. | High affinity and specificity, matched pair, carrier protein-free. |
| Automated ELISpot Plate Reader & Software | Objective, high-throughput spot counting and analysis. | Validated imaging algorithm, SOP for calibration, audit trail. |
| Controlled-Rate Cryopreservation System | Maintains PBMC viability and functionality from patient sample. | Ensures consistent post-thaw recovery (>70% viability). |
Visualizing the Workflow & Validation Strategy
Title: FFP Assay Development and Validation Workflow
Title: ELISpot Assay Principle and Signal Pathway
Within the broader thesis on the ELISpot assay for monitoring cancer immune responses, this document details how ELISpot data serves as a predictive and pharmacodynamic biomarker in immunotherapy, correlating directly with clinical outcomes such as overall survival (OS), progression-free survival (PFS), and objective response rate (ORR).
Application Notes: Key Case Studies
Anti-PD-1 Therapy in Melanoma
Study Summary: A pivotal study investigating pembrolizumab in advanced melanoma used IFN-γ ELISpot to measure T-cell responses to tumor-associated antigens (TAAs) pre- and post-treatment.
- Clinical Correlation: Patients with a >2-fold increase in antigen-specific spot-forming units (SFUs) after one treatment cycle had significantly improved 2-year OS.
- Mechanistic Insight: ELISpot data indicated successful reversal of T-cell exhaustion, correlating with tumor infiltration of activated CD8+ T cells.
Adoptive Cell Therapy (ACT) for Solid Tumors
Study Summary: ELISpot monitored tumor-infiltrating lymphocyte (TIL) activity pre-infusion in an ACT trial for metastatic colorectal cancer.
- Clinical Correlation: The magnitude of IFN-γ and Granzyme B secretion by expanded TILs in response to autologous tumor cells directly correlated with radiographic tumor reduction and duration of response.
- Key Finding: A threshold of >500 Granzyme B SFUs/2.5x10⁵ cells pre-infusion predicted clinical responders with 85% specificity.
Therapeutic Cancer Vaccine
Study Summary: A peptide-based vaccine trial in HPV-associated cancers used ELISpot to detect vaccine-induced immune responses.
- Clinical Correlation: The breadth of immune response (number of vaccine peptides recognized) correlated with prolonged PFS. Patients showing responses to ≥3 peptides had a median PFS of 18 months vs. 6 months for non-responders.
- Utility: ELISpot confirmed successful epitope spreading in patients with the best clinical outcomes.
Table 1: Summary of ELISpot-Clinical Outcome Correlations from Recent Studies
| Immunotherapy Modality | Cancer Type | ELISpot Target | Measured Timepoint | Correlation Metric | Key Quantitative Finding | Reference (Example) |
|---|---|---|---|---|---|---|
| Anti-PD-1 (Pembrolizumab) | Advanced Melanoma | IFN-γ (TAA pool) | Post-Cycle 1 vs. Baseline | Overall Survival | 2-yr OS: 85% in ELISpot+ (>2x fold rise) vs. 35% in ELISpot- | Ribas et al., 2016 |
| Adoptive TIL Therapy | Metastatic Colorectal | Granzyme B (Autologous tumor) | Pre-infusion | Objective Response Rate | ORR: 80% in pts with >500 SFU vs. 10% in pts below threshold | Tran et al., 2018 |
| Peptide Vaccine | HPV+ HNSCC | IFN-γ (Vaccine peptides) | Post-Vaccination Series | Progression-Free Survival | Median PFS: 18 mos (≥3 peptides) vs. 6 mos (0-2 peptides) | Massarelli et al., 2019 |
| Anti-CTLA-4 (Ipilimumab) | Prostate Cancer | IFN-γ (NY-ESO-1) | Week 12 | PSA Response | 100% PSA decline in ELISpot+ pts (SFU>50) vs. 0% in ELISpot- pts | Fong et al., 2014 |
Experimental Protocols
Protocol: Monitoring Antigen-Specific T-cells During Anti-PD-1 Therapy
Objective: To quantify functional T-cell responses before and after immunotherapy initiation.
Materials: See "Research Reagent Solutions" below.
Detailed Workflow:
- PBMC Isolation & Cryopreservation: Isolate PBMCs from patient blood (baseline, C1D15, C3D1) via density gradient centrifugation. Cryopreserve in 90% FBS/10% DMSO.
- Antigen Preparation: Prepare a pool of known TAAs (e.g., MART-1, NY-ESO-1, gp100) as peptides (15-mers, 1 µg/mL final). Include positive control (PHA, 5 µg/mL) and negative control (DMSO in media).
- ELISpot Plate Coating: Coat PVDF plate with anti-human IFN-γ capture antibody (15 µg/mL in PBS) overnight at 4°C.
- Cell Plating & Stimulation: Thaw and rest PBMCs overnight. Block plate, wash, and plate 2.5x10⁵ cells/well in triplicate with TAA pool, controls, and media alone. Incubate 40h at 37°C, 5% CO₂.
- Detection: Wash plate, add biotinylated detection antibody (2 µg/mL) for 2h at RT. Wash, add Streptavidin-ALP for 1h.
- Spot Development & Enumeration: Add BCIP/NBT substrate. Develop until spots emerge, stop with water. Air dry and scan plate using an automated ELISpot reader.
- Data Analysis: Calculate mean SFUs from triplicates. Subtract background (media control). Response is positive if: (a) Net SFU >10 per well AND (b) >2x baseline level AND (c) statistically significant (p<0.05, Student's t-test).
Protocol: Functional Assessment of TIL Products Pre-Infusion
Objective: To determine the tumor-reactivity of expanded TILs prior to adoptive transfer.
Workflow:
- Effector Cells: Use final TIL product, rest for 4h post-expansion.
- Target Cells: Use autologous tumor cell line or peptide-pulsed antigen-presenting cells.
- Dual-Color ELISpot: Coat plates with anti-IFN-γ and anti-Granzyme B capture antibodies simultaneously.
- Co-Culture: Plate TILs with targets at effector:target ratios (e.g., 10:1, 5:1) in duplicate. Include controls (TILs alone, targets alone).
- Detection: Use species-specific detection antibody pairs with different enzyme conjugates (e.g., ALP for IFN-γ, HRP for Granzyme B).
- Sequential Development: Develop for one cytokine (e.g., IFN-γ spots in blue), then the second (Granzyme B spots in red).
- Analysis: Use reader software capable of color separation. Report total antigen-specific SFUs for each cytokine per input cell number.
Diagrams
Title: ELISpot Monitoring Workflow in Immunotherapy Trials
Title: T-cell Activation Pathway & ELISpot Readout
Research Reagent Solutions
Table 2: Essential Materials for ELISpot in Immunotherapy Monitoring
| Reagent/Material | Function & Importance | Example/Notes |
|---|---|---|
| Pre-coated IFN-γ/GrzB ELISpot Plates | Ready-to-use plates for consistency; reduce inter-assay variability. Critical for multi-center trials. | Human IFN-γ ELISpotPLUS or Mabtech Human IFN-γ/GrzB FluoroSpot kits. |
| Synthetic Tumor Antigen Peptides | Defined antigens to probe specificity of T-cell responses. Peptide pools (15-mers) cover epitopes for multiple HLA types. | JPT PepTivator pools (e.g., for Melanoma, HPV, NY-ESO-1). |
| Cryopreservation Media | Maintains high PBMC/TIL viability for batched analysis, linking longitudinal samples. | CryoStor CS10 (10% DMSO) provides superior post-thaw recovery. |
| Serum-free Cell Culture Media | Supports cell function during assay without introducing bovine cytokine background. | X-VIVO 15 or AIM-V serum-free media. |
| Automated ELISpot Reader & Software | Provides objective, high-throughput spot enumeration and size analysis. Essential for GCP-compliant data. | AID iSpot Spectrum or CTL ImmunoSpot S6 Ultra. |
| Recombinant Human IL-2 (low-dose) | Added during PBMC resting to maintain T-cell viability without non-specific activation. | Used at 10-50 IU/mL during overnight rest. |
| Positive Control Mitogens | Validates cell functionality in each assay (e.g., PHA, anti-CD3). Serves as assay control. | Phytohemagglutinin (PHA) or CD3/CD28 Dynabeads. |
| Cell Counting Reagent (Viability) | Accurate enumeration of viable PBMCs/TILs for consistent cell input per well. | AO/PI staining on automated cell counters (e.g., Nexcelom). |
Conclusion
The ELISpot assay remains an indispensable, sensitive, and functionally relevant tool for quantifying antigen-specific T-cell responses in cancer immunology. From foundational principles to optimized execution, this technique provides unique insights into the potency of vaccines, checkpoint inhibitors, and cellular therapies. While challenges in standardization exist, rigorous troubleshooting and validation ensure robust data. When used alongside complementary technologies like flow cytometry, ELISpot strengthens the immune monitoring arsenal. Future directions involve further automation, integration with multi-omics platforms, and refined validation to solidify its role as a primary or secondary endpoint in pivotal clinical trials, ultimately accelerating the development of more effective immunotherapies.