ESR1 Mutations in Breast Cancer: Mechanisms of Hormone Therapy Resistance and Next-Generation Therapeutic Strategies
This comprehensive review addresses the critical role of ESR1 mutations in driving resistance to endocrine therapy for hormone receptor-positive (HR+) metastatic breast cancer.
ESR1 Mutations in Breast Cancer: Mechanisms of Hormone Therapy Resistance and Next-Generation Therapeutic Strategies
Abstract
This comprehensive review addresses the critical role of ESR1 mutations in driving resistance to endocrine therapy for hormone receptor-positive (HR+) metastatic breast cancer. Aimed at researchers, scientists, and drug development professionals, it explores the foundational biology of ESR1 mutations, including their genesis and key variants (e.g., Y537S, D538G). It details methodological approaches for detection and analysis, from liquid biopsy ctDNA assays to functional characterization. The article further examines current clinical challenges in overcoming resistance, reviews the mechanism of action and efficacy of next-generation Selective Estrogen Receptor Degraders (SERDs) and novel agents, and provides a comparative analysis of emerging therapies in clinical trials. The synthesis offers a roadmap for future research and therapeutic development targeting this pivotal resistance pathway.
Understanding ESR1 Mutations: The Biological Basis of Acquired Endocrine Resistance
HR+ metastatic breast cancer (MBC) is initially responsive to endocrine therapies (ET) targeting estrogen receptor alpha (ERα/ESR1) signaling. However, acquired resistance inevitably develops, leading to disease progression and mortality. Within the context of advancing research on ESR1 mutations, this document details the central role of these genetic alterations as a predominant mechanism of acquired resistance to standard-of-care ET, including aromatase inhibitors (AIs) and selective ER degraders (SERDs).
The ESR1 Mutation Landscape in Acquired Resistance
ESR1 mutations are rare in primary breast cancer but are highly enriched in AI-treated, ER+ MBC. These mutations primarily occur in the ligand-binding domain (LBD), leading to constitutive, ligand-independent ER activation.
Table 1: Prevalence and Impact of Key ESR1 Mutations in HR+ MBC
| Mutation (Hotspot) | Approximate Prevalence in AI-Resistant MBC | Functional Consequence | Clinical Implication |
|---|---|---|---|
| Y537S | 10-15% | High constitutive activity, low affinity for ligand | Strongest driver of resistance; poor prognosis |
| D538G | 5-10% | Moderate constitutive activity | Most common mutation; associated with prior AI exposure |
| E380Q | 3-5% | Altered co-factor recruitment | Often co-occurs with other LBD mutations |
| Y537N/C | 3-7% | Constitutive activity, structural distortion | Reduced sensitivity to all current SERDs |
Table 2: Detection Methods and Sensitivities for ESR1 Mutations
| Method | Detection Limit (VAF*) | Sample Type | Key Advantage | Key Limitation |
|---|---|---|---|---|
| ddPCR | 0.1% | ctDNA, Tissue | Ultra-sensitive, quantitative | Targeted; only known variants |
| NGS (Plasma) | 0.5-1.0% | ctDNA | Broad, untargeted discovery | Lower sensitivity vs. ddPCR |
| NGS (Tissue) | 5% | Tumor Biopsy | Comprehensive genomic profile | Invasive; misses spatial heterogeneity |
| BEAMing | 0.01% | ctDNA | Extremely high sensitivity | Technically complex, expensive |
*Variant Allele Frequency
Experimental Protocols for Studying ESR1-Driven Resistance
Protocol 1: In Vitro Assessment of ESR1 Mutant Constitutive Activity
Objective: To quantify ligand-independent ER transcriptional activity and proliferation in engineered cell lines.
- Cell Model Generation: Stably introduce ESR1 wild-type (WT) or mutant (Y537S, D538G) cDNA into ER-negative breast cancer cells (e.g., MDA-MB-231) or create knock-in mutations in ER+ cells (e.g., MCF-7) using CRISPR-Cas9.
- Luciferase Reporter Assay: Transfect cells with an estrogen response element (ERE)-driven luciferase reporter plasmid and a Renilla control plasmid. Culture in phenol-red free media with 10% charcoal-stripped serum for 72 hours ± 1 nM estradiol (E2).
- Measurement: Lyse cells and measure firefly and Renilla luciferase luminescence. Normalize firefly to Renilla signal. Constitutive activity = (Mutant -E2 / WT -E2).
- Proliferation Assay: Plate 5,000 cells/well in steroid-depleted conditions ± E2 ± drug (e.g., 100 nM fulvestrant). Monitor viability via ATP-based assay (CellTiter-Glo) over 5-7 days. Calculate IC50.
Protocol 2: Evaluating Drug Efficacy in ESR1 Mutant Patient-Derived Xenografts (PDXs)
Objective: To test novel SERDs/SERMs in vivo using clinically relevant models.
- PDX Engraftment: Implant fragments of an ESR1-mutant (e.g., D538G) HR+ MBC PDX subcutaneously into female NSG mice. Upon establishment (~200 mm³), randomize mice into cohorts (n=8-10).
- Treatment Regimens: Administer treatments via appropriate routes for 4-6 weeks:
- Cohort 1: Vehicle control (daily oral gavage).
- Cohort 2: Fulvestrant (5 mg/week, s.c.).
- Cohort 3: Experimental oral SERD (e.g., 10 mg/kg, daily oral gavage).
- Cohort 4: Combination therapy (e.g., oral SERD + CDK4/6 inhibitor).
- Endpoint Analysis: Measure tumor volume bi-weekly. At endpoint, harvest tumors for:
- Western Blot: Analysis of ERα protein levels, cleavage markers (PARP), and pathway markers (pRB, pERK).
- RNA-seq: Transcriptomic profiling to identify resistance signatures.
- IHC: Staining for Ki67 (proliferation) and ERα localization.
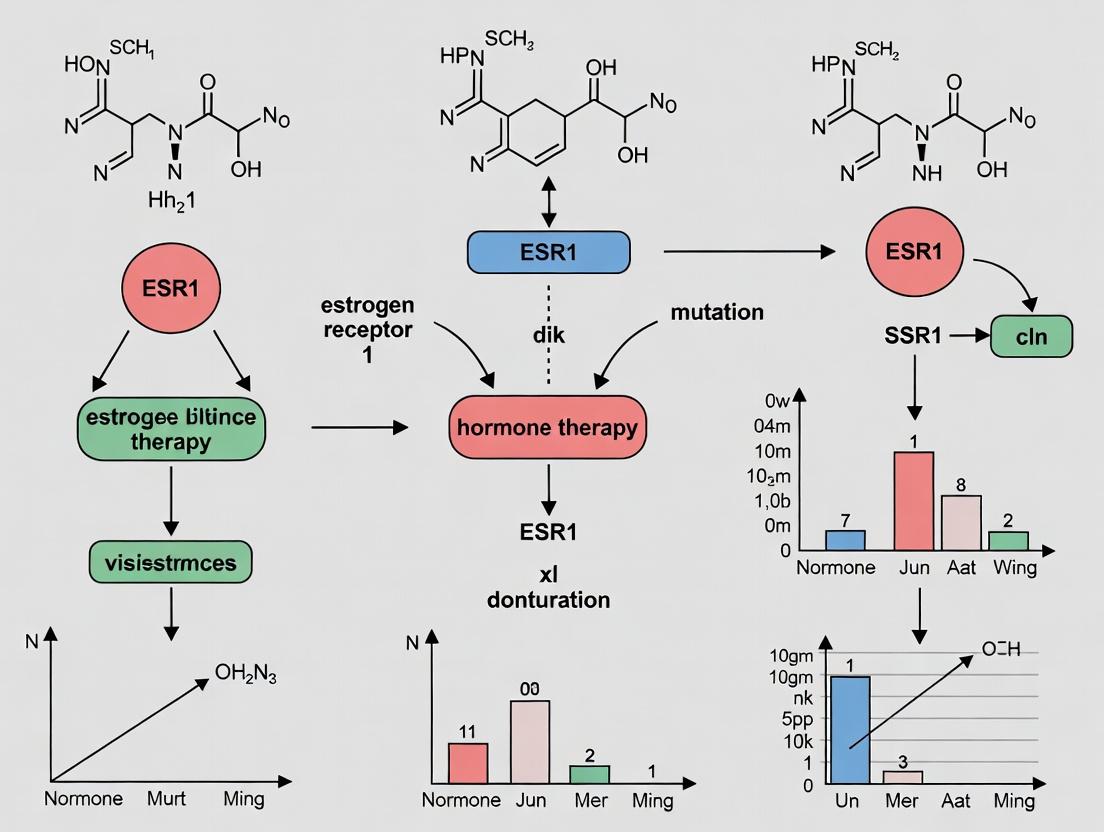
Visualizing ESR1 Mutation-Driven Signaling and Research Workflows
Title: ESR1 Mutant Constitutive Activity Drives Therapy Resistance
Title: ESR1 Mutation Detection & Research Translation Workflow
The Scientist's Toolkit: Key Reagents for ESR1 Resistance Research
Table 3: Essential Research Reagent Solutions
| Item | Function & Application | Example(s) | Key Consideration |
|---|---|---|---|
| ESR1-Mutant Cell Lines | Isogenic models to isolate mutation-specific effects. | MCF-7 Y537S knock-in, T47D D538G ectopic. | Verify mutation status and ER expression routinely. |
| Patient-Derived Xenografts (PDXs) | In vivo models preserving tumor heterogeneity and clinical response. | PDX from a patient progressing on an AI. | Characterize ESR1 mutation VAF and stability across passages. |
| Anti-ERα Antibodies | Detect total ERα, phospho-ERα, and assess degradation (Western, IHC). | Clone SP1 (IHC), Clone D6H2 (Western, IP). | Choose clones validated for specific applications (IHC vs. Western). |
| ERE-Luciferase Reporter | Quantify ER transcriptional activity in a high-throughput format. | Plasmid with tandem EREs driving firefly luc. | Normalize with Renilla or thymidine kinase-Renilla control. |
| Ultra-Sensitive ctDNA Kits | Isolate and prepare ctDNA from patient plasma for ddPCR/NGS. | QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit. | Minimize contamination with genomic DNA from lysed blood cells. |
| Selective ER Degraders (SERDs) | Tool compounds for in vitro and in vivo inhibition of mutant ER. | Fulvestrant (clinical), GDC-0810, AZD-9833 (investigational). | Solubility and formulation are critical for in vivo dosing. |
| Droplet Digital PCR Assays | Absolute quantification of low-frequency ESR1 mutations in ctDNA. | Bio-Rad ddPCR ESR1 Mutation Assays (Y537S, D538G). | Design includes wild-type and mutant probes for multiplexing. |
ESR1 Gene and Estrogen Receptor Alpha (ERα) Structure-Function Relationship
Within the critical context of understanding ESR1 mutations in hormone therapy resistance, elucidating the precise structure-function relationship of the Estrogen Receptor Alpha (ERα) is paramount. ERα, encoded by the ESR1 gene, is a ligand-activated transcription factor and a primary driver in approximately 70% of breast cancers. Resistance to endocrine therapies like tamoxifen and aromatase inhibitors is frequently driven by acquired mutations in ESR1, particularly in the ligand-binding domain (LBD). This whitepaper provides a technical dissection of ERα's structure, its functional domains, and how mutations perturb this relationship, culminating in therapeutic resistance.
ESR1 Gene Organization and ERα Domain Architecture
The human ESR1 gene is located on chromosome 6q25.1, spanning approximately 140 kb with 8 exons. It translates into a 595-amino acid protein for the primary isoform (ERα66). The functional domains are modular.
Table 1: Functional Domains of ERα (Isoform 66)
| Domain | Amino Acid Residues | Primary Function | Key Structural Features |
|---|---|---|---|
| A/B (AF-1) | 1-180 | Ligand-independent transactivation | Intrinsically disordered, phosphorylation sites (Ser118, Ser167). |
| C (DBD) | 181-263 | DNA Binding | Two zinc finger motifs, P-box (Glu203, Gly204, Ala207) for ERE specificity. |
| D (Hinge) | 264-302 | Nuclear Localization, Modulation | Contains nuclear localization signal (NLS), interaction with co-regulators. |
| E (LBD with AF-2) | 303-553 | Ligand Binding, Dimerization, Transactivation | 12 α-helices (H1-H12), ligand-binding pocket, AF-2 surface (Helices 3,4,5,12). |
| F | 554-595 | Modulatory Function | Isoform-specific, influences receptor stability and activity. |
Structural Basis of Ligand Binding and Activation
The LBD (domain E) is the allosteric heart of ERα function and the hotspot for resistance mutations. Its core is a three-layered anti-parallel α-helical sandwich (H1-H12) forming a hydrophobic ligand-binding pocket (LBP).
Mechanism: Upon agonist (e.g., 17β-estradiol, E2) binding, H12 repositions over the LBP, sealing the ligand and forming a charged clamp with H3 and H4. This creates the transcriptionally active AF-2 surface, a groove for binding LxxLL motifs of coactivators (e.g., SRC-3). Antagonists (e.g., 4-hydroxytamoxifen) project a side chain that sterically displaces H12, preventing coactivator recruitment.
Table 2: Common ESR1 LBD Mutations in Therapy Resistance
| Mutation | Frequency in MBC* | Structural/Functional Consequence | Impact on Therapy |
|---|---|---|---|
| Y537S | ~15-20% | Stabilizes H12 in active conformation, constitutive activity. | Resistance to AIs, Tamoxifen, Fulvestrant (reduced sensitivity). |
| D538G | ~10-15% | Alters H12 dynamics, increases basal activity, alters cofactor affinity. | Resistance to AIs, Tamoxifen. |
| E380Q | ~3-5% | Affects H3-H5 interface, may alter ligand affinity and dimerization. | Associated with AI resistance. |
| L536H/P/Q/R | ~2-5% | Located in H11, affects H12 positioning and dimer interface. | Constitutive activity, fulvestrant resistance. |
*MBC: Metastatic Breast Cancer
Key Experimental Protocols for Studying Structure-Function
Protocol: Assessing ERα Conformational Change and Coactivator Recruitment (SPR/Biolayer Interferometry)
Objective: Quantify the binding affinity of wild-type vs. mutant ERα LBD for a coactivator peptide (e.g., SRC-3 NR2) in the presence of different ligands. Methodology:
- Protein Purification: Express and purify recombinant His-tagged ERα LBD (wild-type and mutant, e.g., Y537S) from E. coli or insect cells.
- Sensor Immobilization: For Surface Plasmon Resonance (SPR), immobilize anti-His antibody on a CMS chip. For BLI, load His-tagged ERα LBD onto anti-His biosensors.
- Ligand Loading: Dilute ligands (E2, 4-OHT, Fulvestrant) in running buffer (e.g., HBS-EP+). Inject over the sensor to achieve saturated receptor-ligand complex formation.
- Coactivator Binding Analysis: Inject serial dilutions of biotinylated SRC-3 NR2 peptide across the ligand-bound receptor surface.
- Data Analysis: Record association/dissociation curves. Fit data to a 1:1 binding model to calculate kinetic (ka, kd) and equilibrium (KD) constants.
Protocol: Determining Transcriptional Activity via Luciferase Reporter Assay
Objective: Measure the ligand-dependent and constitutive transcriptional activity of ESR1 mutants. Methodology:
- Cell Transfection: Seed ER-negative cells (e.g., MDA-MB-231) in 96-well plates. Co-transfect with:
- Plasmid expressing ERα (wild-type or mutant).
- Reporter plasmid containing an Estrogen Response Element (ERE) driving firefly luciferase.
- Renilla luciferase plasmid for normalization.
- Ligand Treatment: 24h post-transfection, treat cells with vehicle, E2 (10 nM), 4-OHT (100 nM), or Fulvestrant (100 nM) for 18-24 hours.
- Luciferase Measurement: Lyse cells and measure Firefly and Renilla luminescence using a dual-luciferase assay system.
- Data Analysis: Calculate Firefly/Renilla ratio. Normalize activity of treated samples to vehicle-treated wild-type ERα control. Plot dose-response curves for IC50/EC50 determination.
Protocol: Structural Determination via X-ray Crystallography
Objective: Solve the atomic structure of mutant ERα LBD in complex with ligands. Methodology:
- Protein Crystallization: Purify ERα LBD at high concentration (>5 mg/mL). Set up crystallization trials (sitting-drop vapor diffusion) with commercial screens. Co-crystallize with ligand.
- Crystal Harvesting & Freezing: Flash-cool crystals in liquid nitrogen using a cryoprotectant solution.
- Data Collection: Collect X-ray diffraction data at a synchrotron beamline.
- Structure Solution & Refinement: Solve the phase problem by molecular replacement using a known ERα LBD structure (e.g., PDB: 1A52). Iteratively refine the model (ligand, water, side-chain placement) using programs like Phenix and Coot.
Visualization of Key Pathways and Concepts
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for ERα Structure-Function Research
| Reagent/Category | Example Product/Description | Function in Research |
|---|---|---|
| Recombinant ERα Proteins | Purified human ERα LBD (wild-type & mutants), full-length. | In vitro binding assays (SPR, ITC), crystallization, biochemical studies of direct interactions. |
| Cell Lines (Isogenic) | MCF-7 engineered to express ESR1 Y537S or D538G via CRISPR. | Study mutant signaling in a native cellular context, screen for mutant-specific vulnerabilities. |
| Reporter Assay Systems | ERE-TATA-Luciferase plasmid (e.g., pGL4-ERE). | Quantify transcriptional output of ERα variants under different ligand conditions. |
| Selective Ligands | Agonist: 17β-Estradiol (E2). SERM: 4-Hydroxytamoxifen (4-OHT). SERD: Fulvestrant (ICI 182,780). SERCA: GDC-9545 (Giredestrant). | Probe receptor conformation, assess antagonist efficacy, and evaluate novel therapeutics. |
| Coactivator/Repressor Peptides | Biotinylated SRC-3 NR2 box (LxxLL motif) peptide. | Measure AF-2 surface availability in in vitro recruitment assays (SPR, BLI). |
| ERα-Specific Antibodies | ChIP-grade: Anti-ERα (clone HC-20, sc-543). IHC: Anti-ERα (clone SP1, 6F11). | Chromatin Immunoprecipitation (ChIP), Immunohistochemistry, Western Blot, Immunoprecipitation. |
| Next-Gen Sequencing Kits | RNA-Seq library prep kits (e.g., Illumina TruSeq). ChIP-Seq kits. | Profile global transcriptome and ERα cistrome changes driven by mutations. |
Abstract This whitepaper examines the origin and selection of ESR1 mutations as a direct consequence of evolutionary pressure exerted by aromatase inhibitor (AI) therapy in estrogen receptor-positive (ER+) metastatic breast cancer. Framed within the broader thesis of ESR1 mutation's role in hormone therapy resistance, we detail the molecular mechanisms, clinical detection methodologies, and preclinical modeling that define this evolutionary paradigm. The content is intended to guide researchers and drug developers in understanding and targeting this fundamental driver of therapeutic resistance.
1. Introduction: The Evolutionary Landscape Aromatase inhibitors suppress estrogen synthesis, creating a potent selective pressure on ER+ breast cancer cells. Within this low-estrogen environment, clones harboring mutations in the ESR1 gene, particularly in the ligand-binding domain (LBD), gain a proliferative advantage. These mutations confer constitutive, estrogen-independent activity and resistance to AI therapy, representing a classic case of clonal evolution under therapeutic stress. The study of their genesis is central to understanding and overcoming endocrine resistance.
2. Key ESR1 Mutations and Their Functional Impact The most prevalent mutations are missense mutations at key residues, leading to ligand-independent activation and altered co-regulator binding.
Table 1: Prevalent ESR1 LBD Mutations and Functional Consequences
| Mutation | Prevalence in AI-Resistant MBC* | Primary Functional Consequence | Response to Endocrine Agents |
|---|---|---|---|
| Y537S | ~15-25% | High constitutive activity, stabilizes AF-2 helix. | Resistant to Tamoxifen, Fulvestrant (reduced sensitivity). |
| D538G | ~10-20% | Moderate constitutive activity, alters co-factor interface. | Resistant to Tamoxifen, retains some Fulvestrant sensitivity. |
| E380Q | ~5-10% | Alters receptor stability and dynamics. | Variable resistance profile. |
| Y537N/C | ~5-10% | High constitutive activity (Y537N similar to Y537S). | Resistant to Tamoxifen, Fulvestrant. |
| *Data aggregated from circulating tumor DNA (ctDNA) sequencing studies of AI-resistant metastatic breast cancer (MBC). |
3. Experimental Protocols for Studying ESR1 Mutation Genesis 3.1. In Vitro Evolution Protocol: Long-Term Estrogen Deprivation (LTED)
- Objective: To recapitulate the selection of ESR1 mutations under AI-mimicking conditions.
- Cell Line: Estrogen-dependent ER+ breast cancer cell line (e.g., MCF-7).
- Procedure:
- Culture cells in phenol red-free media supplemented with 10% charcoal-stripped fetal bovine serum (CSS) to remove steroids.
- Maintain cells in this estrogen-deprived (ED) media for >6 months, with regular passaging.
- Monitor for the emergence of estrogen-independent growth.
- Perform whole-exome or targeted sequencing of the ESR1 LBD at multiple time points (e.g., 0, 3, 6 months) to track mutation acquisition.
- Validate functional impact via luciferase reporter assays (ERE-luc) in ED conditions.
3.2. In Vivo Selection Model: Patient-Derived Xenograft (PDX) under AI Pressure
- Objective: To study clonal selection and tumor evolution in a physiological context.
- Protocol:
- Establish PDX from an ER+ AI-naïve patient tumor in immunocompromised mice (e.g., NSG).
- Treat cohorts with a third-generation AI (e.g., letrozole, 10 µg/day orally) or vehicle control.
- Monitor tumor growth. Biopsy tumors at progression.
- Perform deep sequencing of ctDNA from serial blood draws and matched tumor tissue to identify and track ESR1 mutant allele frequency over time.
- Analyze phylogenetic relationships between pre- and post-treatment samples.
4. Signaling Pathways in ESR1 Mutant-Driven Resistance ESR1 LBD mutations rewire transcriptional programs, engaging distinct growth and survival pathways.
Diagram Title: Contrasting Signaling in Wild-Type vs. Mutant ERα under AI Therapy
5. The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for ESR1 Mutation Studies
| Reagent/Material | Function/Application | Example/Notes |
|---|---|---|
| Charcoal-Stripped Serum | Creates estrogen-depleted culture conditions for LTED and functional assays. | Essential for in vitro selection experiments. |
| ESR1 LBD Mutant Plasmids | For overexpression studies to characterize mutation-specific functions. | Common: pCDNA3-ESR1-Y537S, -D538G. |
| ERE-Luciferase Reporter | Measures constitutive and ligand-induced ER transcriptional activity. | Core tool for functional validation. |
| Selective ER Degraders (SERDs) | Tool compounds to probe mutant ERα stability and degradation. | Fulvestrant, novel oral SERDs (e.g., AZD9833). |
| ddPCR or BEAMing Assay Kits | Ultra-sensitive quantification of mutant allele frequency in ctDNA. | Critical for monitoring clonal evolution in patients/PDX models. |
| Anti-ERα (Phospho-Specific) Antibodies | Assess activation state and post-translational modification. | e.g., pS118-ERα, pS167-ERα. |
| CDK4/6 & PI3K Inhibitors | To study combination therapies and pathway crosstalk in mutant models. | Palbociclib, Alpelisib. |
6. Detection and Analysis Workflow The gold standard for tracking ESR1 mutation genesis involves longitudinal ctDNA analysis.
Diagram Title: Workflow for Tracking ESR1 Mutation Evolution via ctDNA
7. Conclusion and Future Directions The genesis of ESR1 mutations is a definitive adaptation to AI-imposed evolutionary pressure. Understanding this process requires integrating sensitive detection methods, robust experimental evolution models, and a deep analysis of the altered mutant ERα transcriptome. Future research must focus on targeting mutant ERα effectively (with next-generation SERDs and PROTACs) and designing combination therapies that preempt or overcome this resistance mechanism, guided by the principles of evolutionary biology applied to cancer treatment.
1. Introduction: ESR1 Mutations in the Context of Hormone Therapy Resistance
The estrogen receptor alpha (ERα), encoded by the ESR1 gene, is the principal driver and therapeutic target in the majority of hormone receptor-positive (HR+) breast cancers. Endocrine therapies, including aromatase inhibitors (AIs) and selective estrogen receptor degraders (SERDs) like fulvestrant, are cornerstone treatments. However, acquired resistance remains a major clinical challenge. A critical mechanism of resistance is the acquisition of somatic mutations in the ligand-binding domain (LBD) of ESR1, which emerge under the selective pressure of AI therapy. These mutations confer ligand-independent constitutive activity, altered co-regulator recruitment, and reduced affinity for certain therapeutics. This whitepaper provides a technical guide to three key 'hotspot' mutations—Y537S, D538G, and E380Q—detailing their prevalence, functional impact, and methodologies for their study within the broader thesis of understanding and overcoming endocrine resistance.
2. Prevalence and Clinical Characteristics
Hotspot ESR1 mutations are rarely found in primary, treatment-naïve breast cancers (<1%) but are highly prevalent in metastatic HR+ breast cancer, particularly following prolonged AI exposure. Prevalence data, compiled from recent ctDNA sequencing studies (2023-2024), are summarized below.
Table 1: Prevalence and Clinical Associations of Key ESR1 Hotspot Mutations
| Mutation | Domain | Prevalence in Metastatic HR+ BC (Post-AI) | Common Co-occurring Genomic Alterations | Association with Prior Therapy Duration |
|---|---|---|---|---|
| D538G | Helix 12 | ~10-15% | PIK3CA, TP53, FGFR1 amp | Strongly associated with longer AI exposure (>2-3 years) |
| Y537S | Helix 12 | ~5-10% | TP53, RB1 loss, CCNE1 amp | Associated with more aggressive disease and shorter time to progression |
| E380Q | Helix 3 | ~2-5% | PIK3CA, CDH1 mutations | Often found in conjunction with other ESR1 mutations |
3. Structural and Functional Impact on ERα Signaling
These mutations fundamentally alter ERα conformation and dynamics.
- Y537S and D538G (Helix 12 Stabilizers): These mutations, located in the activation function-2 (AF-2) surface, stabilize Helix 12 in the active, agonist-like conformation. This mimics the estradiol-bound state, enabling constitutive, ligand-independent transcriptional activity and altered co-activator (e.g., SRC-3) recruitment. Y537S is particularly potent, conferring higher basal activity and greater resistance to fulvestrant compared to D538G.
- E380Q (Helix 3 Allosteric Modulator): Located away from the AF-2 surface, E380Q weakens a salt bridge, increasing the dynamics of the LBD. This allosterically facilitates Helix 12 stabilization, promoting constitutive activity and conferring resistance to AIs but often remaining sensitive to high-dose fulvestrant.
Diagram 1: ESR1 Mutant-Driven Constitutive Signaling
4. Experimental Protocols for Functional Characterization
4.1. In Vitro Transcriptional Reporter Assay
- Purpose: Quantify ligand-independent and ligand-dependent transcriptional activity of mutant vs. wild-type ERα.
- Protocol:
- Cell Seeding: Plate ER-negative cells (e.g., HEK293T, MDA-MB-231) in 24-well plates.
- Transfection: Co-transfect with:
- Expression plasmids for wild-type or mutant ESR1.
- Reporter plasmid (ERE-TATA-luciferase, e.g., pGL4-ERE).
- Renilla luciferase control plasmid (e.g., pRL-TK) for normalization.
- Treatment: 24h post-transfection, treat cells with vehicle, 17β-estradiol (1-10 nM), fulvestrant (100 nM), or other SERDs/SERMs.
- Luciferase Assay: After 24h of treatment, lyse cells and measure Firefly and Renilla luciferase activity using a dual-luciferase assay kit. Normalize Firefly luminescence to Renilla.
4.2. Growth Inhibition Assay in Engineered Cell Lines
- Purpose: Assess the impact of mutations on endocrine therapy sensitivity in a relevant cellular background.
- Protocol:
- Model Generation: Create isogenic MCF-7 or T47D cell lines stably expressing wild-type, Y537S, D538G, or E380Q ERα via lentiviral transduction and puromycin selection. Verify expression by immunoblot.
- Proliferation Assay: Seed cells in estrogen-depleted charcoal-stripped serum media. After 72h, treat with a dose range of fulvestrant, tamoxifen, or novel oral SERDs (e.g., elacestrant).
- Viability Measurement: After 5-7 days, measure cell viability using CellTiter-Glo 3D. Calculate IC50 values using non-linear regression analysis (GraphPad Prism).
Diagram 2: In Vitro Mutant Characterization Workflow
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for ESR1 Mutation Research
| Item | Function & Application | Example Product/Catalog |
|---|---|---|
| Isogenic Mutant Cell Lines | Pre-engineered models for functional studies; save time vs. in-house generation. | Horizon Discovery: MCF-7 ESR1 Y537S (HD 102-011) |
| ESR1 LBD Mutant Plasmids | For transient expression and reporter assays in heterologous systems. | Addgene: pCMV-ESR1-D538G (#146893) |
| ERE Luciferase Reporter | Standardized vector for measuring ERα transcriptional activity. | Promega: pGL4-ERE-luciferase (pGL4.23[luc2/minP]) + ERE insert |
| Anti-ERα (Phospho-Ser118) Antibody | Detect activated ERα; useful for assessing constitutive activity. | Cell Signaling Technology: #2511S |
| Next-Gen SERDs | Tool compounds for evaluating potency against mutants in vitro. | MedChemExpress: Elacestrant (RAD1901) (HY-103717) |
| ctDNA Reference Standard | Positive controls for developing/validating ddPCR or NGS assays. | Seraseq ESR1 Mutant ctDNA Reference Material |
6. Implications for Drug Development and Future Directions
The prevalence of these hotspot mutations has driven the development of next-generation SERDs with improved potency against mutants (e.g., elacestrant, camizestrant). Current clinical research focuses on:
- Combination Therapies: Targeting parallel pathways (e.g., CDK4/6, PI3K, mTOR) to overcome resistance.
- Proteolysis-Targeting Chimeras (PROTACs): Designing ERα degraders with enhanced efficacy against mutants.
- Selective ERα Covalent Antagonists (SERCAs): Irreversibly inactivating both wild-type and mutant ERα.
- Early Detection: Using liquid biopsy to monitor ESR1 mutation emergence as a guide for therapy switching.
Understanding the distinct biophysical properties and preclinical drug sensitivities of Y537S, D538G, and E380Q remains critical for designing the next wave of targeted therapies and optimizing treatment sequences for HR+ metastatic breast cancer.
This whitepaper explores the fundamental cellular mechanisms of constitutive receptor activation, with a specific focus on ligand-independent signaling and co-regulator interaction dysregulation. This discussion is framed within the critical context of endocrine resistance in breast cancer, particularly the role of mutant Estrogen Receptor Alpha (ESR1). Acquired mutations in the ESR1 ligand-binding domain (LBD) are a dominant driver of resistance to aromatase inhibitor therapy. These mutations, such as the prevalent D538G and Y537S, confer constitutive, ligand-independent transcriptional activity and altered interactions with transcriptional coregulators, enabling tumor progression in low-estrogen environments. Understanding these precise mechanisms is paramount for developing next-generation Selective Estrogen Receptor Degraders (SERDs) and proteolysis-targeting chimeras (PROTACs) to overcome therapy resistance.
Core Mechanisms of Constitutive Activation
2.1 Ligand-Independent Activity Wild-type ESR1 is activated primarily upon binding its ligand, estradiol (E2), which stabilizes the receptor in an active conformation. In contrast, constitutively active ESR1 mutants achieve this state in the absence of ligand. Key structural changes include:
- Destabilization of Helix 12 (H12): Mutations like Y537S weaken interactions that stabilize H12 in the antagonistic position, favoring its spontaneous adoption of the active "agonist" position.
- Altered Receptor Dynamics: Mutations reduce the free energy required for the transition from an inactive to an active state, leading to constitutive activity.
- Ligand-Independent Phosphorylation: Enhanced phosphorylation (e.g., at Ser118/167) via growth factor signaling pathways (MAPK, AKT) further stabilizes the active conformation and facilitates co-activator recruitment.
2.2 Altered Co-regulator Recruitment The transcriptional output of ESR1 is determined by its binding of co-activators (e.g., SRC-3, AIB1) or co-repressors (e.g., NCoR, SMRT). ESR1 LBD mutations fundamentally shift this equilibrium:
- Increased Affinity for Co-activators: Mutant receptors exhibit a significantly higher intrinsic affinity for canonical co-activator motifs (LxxLL motifs).
- Reduced Dependence on Co-activator Peptide Sequence: While wild-type ESR1 is selective for specific LxxLL sequences, mutants like Y537S promiscuously bind a wider array, potentially diversifying transcriptional programs.
- Evasion of Co-repressors: The constitutive active conformation creates a surface incompatible with co-repressor binding, effectively silencing repressive pathways.
Table 1: Biophysical & Transcriptional Properties of Common ESR1 Mutants
| ESR1 Variant | Basal Transcriptional Activity (Fold vs WT) | Co-activator SRC-3 Binding Affinity (KD, nM) | Corepressor NCoR Binding | Response to 4-OHT (Tamoxifen) |
|---|---|---|---|---|
| Wild-Type | 1.0 (Reference) | ~1000 (E2-dependent) | Strong (in 4-OHT bound state) | Antagonist |
| Y537S | 8.5 - 12.0 | ~50 (Ligand-independent) | Severely Impaired | Partial Agonist |
| D538G | 4.0 - 6.0 | ~150 (Ligand-independent) | Impaired | Partial Agonist/Weak Antagonist |
| E380Q | 2.0 - 3.0 | ~700 | Moderately Impaired | Largely Antagonist |
Data compiled from recent surface plasmon resonance (SPR), mammalian two-hybrid, and luciferase reporter assays (2022-2024).
Table 2: Efficacy of Therapies Against ESR1 Mutant Models
| Therapeutic Agent | Mechanism | Growth Inhibition (IC50) Y537S MCF7 | Effect on Mutant ER Protein Levels |
|---|---|---|---|
| Fulvestrant (1st gen SERD) | ER Degradation & Antagonism | ~50 nM | Reduction >80% |
| Elacestrant (2nd gen SERD) | ER Degradation & Antagonism | ~10 nM | Reduction >90% |
| GDC-9545 (Oral SERD) | ER Degradation & Antagonism | ~5 nM | Reduction >95% |
| AZD9833 (Oral SERD) | ER Degradation & Antagonism | ~15 nM | Reduction >90% |
| Tamoxifen | Partial Antagonist/Antiestrogen | >1000 nM | No Reduction |
Data from cell viability assays (CellTiter-Glo) and immunoblotting in engineered cell lines (2023-2024).
Key Experimental Protocols
Protocol 1: Mammalian Two-Hybrid Assay for Co-regulator Recruitment Purpose: To quantify the interaction strength between ESR1 (wild-type or mutant) and a specific co-regulator peptide in live cells. Methodology:
- Plasmid Construction: Clone the coding sequence for the ESR1 LBD (wild-type or mutant) into the pBIND vector (encoding the Gal4 DNA-binding domain, DB). Clone the LxxLL motif from a co-regulator (e.g., SRC-3) into the pACT vector (encoding the VP16 activation domain, AD).
- Cell Transfection: Seed HEK293T cells in 96-well plates. Co-transfect with:
- pBIND-ESR1-LBD (DB fusion)
- pACT-CoReg-Peptide (AD fusion)
- pG5-luc reporter plasmid (containing Gal4 response elements)
- Renilla luciferase control plasmid for normalization.
- Treatment & Measurement: After 24h, treat cells with vehicle, E2 (10 nM), or 4-OHT (100 nM) for an additional 24h. Lyse cells and measure Firefly and Renilla luciferase activities using a dual-luciferase reporter assay system.
- Analysis: Calculate the ratio of Firefly/Renilla luminescence. Interaction strength is reported as fold-change relative to the DB-empty + AD-co-regulator control.
Protocol 2: Cellular Thermal Shift Assay (CETSA) for Conformational Stability Purpose: To assess ligand-independent stabilization of ESR1 mutant protein conformation, indicative of constitutive activation. Methodology:
- Cell Preparation: Culture ESR1-mutant (Y537S) and wild-type MCF7 cells. Treat with vehicle, E2 (10 nM), or drug candidate (e.g., SERD, 100 nM) for 2 hours.
- Heat Denaturation: Harvest cells, wash, and resuspend in PBS with protease inhibitors. Aliquot equal volumes into PCR tubes. Heat each aliquot at a distinct temperature (e.g., 37°C to 65°C in 3°C increments) for 3 minutes in a thermal cycler.
- Lysis & Clarification: Lyse heated samples by freeze-thaw cycles. Centrifuge at high speed (20,000 x g) to separate soluble (non-denatured) protein from aggregates.
- Detection: Analyze the soluble fraction by immunoblotting for ESR1. Quantify band intensity.
- Analysis: Plot the fraction of remaining soluble ESR1 against temperature. A rightward shift in the melting curve (higher Tm) indicates ligand- or mutation-induced stabilization of the protein.
Visualizations
Diagram 1: Constitutive ERα activation and co-regulator switching.
Diagram 2: ER degradation and CETSA workflow for stability assessment.
The Scientist's Toolkit
Table 3: Essential Research Reagents for ESR1 Constitutive Activity Studies
| Reagent / Material | Supplier Examples | Function & Application |
|---|---|---|
| Engineered ESR1 Mutant Cell Lines (e.g., MCF7 Y537S, D538G) | ATCC, Horizon Discovery | Isogenic models for studying mutation-specific biology and drug screening. |
| Next-Gen Oral SERDs (GDC-9545, AZD9833, Elacestrant) | MedChemExpress, Selleckchem | Tool compounds for testing efficacy against mutant ER in vitro and in vivo. |
| Co-activator/Co-repressor Peptide Kits | Peptide International, JPT | Biotinylated LxxLL or CoRNR box peptides for SPR or pulldown assays. |
| ESR1 Mutant-Specific Antibodies (pS118, pS167, total ERα) | Cell Signaling Technology, Abcam | Detecting phosphorylation states and total protein in IHC, WB, IP. |
| Dual-Luciferase Reporter Assay System | Promega | Gold-standard for quantifying transcriptional activity in reporter assays. |
| CETSA / Thermal Shift Buffer Kits | Thermo Fisher Scientific | Optimized buffers and protocols for protein stability assays. |
| SPR Biosensor Chips (CM5 Series S) | Cytiva | Sensor chips for label-free, quantitative binding kinetics analysis. |
| PROTAC Molecules (e.g., ARV-471 derivatives) | Tocris, Cayman Chemical | Inducing targeted ER degradation via the ubiquitin-proteasome system. |
This whitepaper details the mechanism by which constitutively active, ligand-independent mutant Estrogen Receptor Alpha (ERα/mutant ESR1) drives a transcriptional program promoting metastasis, a core component of the broader thesis on ESR1 mutations as a primary driver of endocrine therapy resistance in advanced estrogen receptor-positive (ER+) breast cancer.
Mechanism of Mutant ERα-Driven Transcriptional Reprogramming
Mutant ERα (e.g., Y537S, D538G) exhibits altered conformation, enhanced coactivator recruitment (e.g., SRC-3), and reduced corepressor binding, leading to constitutive chromatin binding and transcriptional activity even in the absence of estrogen or the presence of aromatase inhibitors (AIs) and selective estrogen receptor degraders (SERDs).
Key Altered Transcriptional Features
| Transcriptional Feature | Wild-Type ERα | Mutant ERα (Y537S/D538G) |
|---|---|---|
| Ligand Dependency | Strictly estrogen-dependent | Constitutive, ligand-independent |
| Chromatin Occupancy | Dynamic, ligand-regulated | Expanded and stabilized |
| Coactivator Binding (SRC-3) | Moderate, induced | High, constitutive |
| Corepressor Binding (NCOR1) | Present in absence of ligand | Severely diminished |
| Primary Transcriptional Output | Proliferation genes | Pro-metastatic & invasion genes |
| Response to Fulvestrant | Degraded, activity abolished | Partial resistance, residual activity |
Pro-Metastatic Gene Signature
Mutant ERα directly upregulates a core set of genes involved in epithelial-to-mesenchymal transition (EMT), invasion, and metastatic colonization.
Quantitative Gene Expression Data
Table: Fold-change in expression of pro-metastatic genes in mutant vs. wild-type ERα MCF7 cells (under estrogen-deprived conditions). Data derived from RNA-seq studies.
| Gene Symbol | Gene Name | Function in Metastasis | Avg. Fold-Change (Mutant/WT) |
|---|---|---|---|
| CDH2 | N-cadherin | EMT, loss of adhesion | +8.5 |
| VIM | Vimentin | Mesenchymal marker, motility | +6.2 |
| SNAI1 | Snail | EMT transcription factor | +5.8 |
| MMP9 | Matrix Metallopeptidase 9 | Extracellular matrix degradation | +7.1 |
| CXCR4 | C-X-C Chemokine Receptor 4 | Homing to metastatic sites | +4.3 |
| MYC | c-Myc | Cell growth & invasion | +3.5 |
Experimental Protocols for Key Studies
Protocol: Chromatin Immunoprecipitation Sequencing (ChIP-seq) for Mutant ERα
Objective: Map genome-wide binding sites of mutant ERα.
- Cell Culture: MCF7 cells engineered to express wild-type or mutant ESR1 (Y537S) are maintained in phenol-red free media with 10% charcoal-stripped FBS for 5 days.
- Crosslinking: Add 1% formaldehyde for 10 min at room temp. Quench with 125mM glycine.
- Cell Lysis & Sonication: Lyse cells and sonicate chromatin to ~200-500 bp fragments.
- Immunoprecipitation: Incubate chromatin with anti-ERα antibody (e.g., HC-20, Santa Cruz) or IgG control overnight at 4°C. Capture with protein A/G beads.
- Wash, Elution, Reverse Crosslink: Stringent washes, elute, and reverse crosslinks at 65°C overnight.
- DNA Purification & Library Prep: Purify DNA and prepare sequencing library using KAPA HyperPrep Kit.
- Sequencing & Analysis: Sequence on Illumina platform. Align reads to hg38, call peaks with MACS2.
Protocol: Invasion Assay (Transwell) PostESR1Knockdown
Objective: Functionally validate the role of mutant ERα in driving invasion.
- Knockdown: Transfect mutant ERα-expressing cells with ESR1-specific siRNA or non-targeting control using Lipofectamine RNAiMAX.
- Matrix Coating: Coat top side of 8µm pore Transwell inserts with diluted Matrigel (50µg/mL) and let solidify.
- Cell Plating: Seed 5x10^4 serum-starved transfected cells in serum-free media into the top chamber.
- Chemoattractant: Add media with 10% FBS to the lower chamber.
- Invasion: Incubate for 48 hours at 37°C.
- Fix, Stain & Count: Remove non-invaded cells with cotton swab. Fix invaded cells with 4% PFA, stain with 0.1% crystal violet, image, and count in 5 random fields.
Visualization of Signaling and Workflows
Title: Mutant ERα drives pro-metastatic gene transcription.
Title: ChIP-seq workflow for mutant ERα binding sites.
The Scientist's Toolkit: Key Research Reagents
| Reagent/Category | Example Product (Supplier) | Function in Research |
|---|---|---|
| Mutant ESR1 Cell Lines | MCF7-Y537S (ATCC) | Isogenic models to study mutant-specific biology vs. wild-type. |
| Charcoal-Stripped FBS | Gibco (Thermo Fisher) | Removes steroids to create estrogen-depleted conditions. |
| Anti-ERα ChIP-seq Antibody | ERα (HC-20) (Santa Cruz, sc-543) | Immunoprecipitates ERα for chromatin binding studies. |
| ChIP-seq Kit | Magna ChIP A/G (Millipore Sigma) | Streamlined protocol for chromatin IP and purification. |
| siRNA for ESR1 | ON-TARGETplus (Horizon Discovery) | Knocks down ERα expression to assess functional dependency. |
| Matrigel for Invasion | Corning Matrigel Matrix | Basement membrane extract to coat Transwells for invasion assays. |
| Selective ER Degrader | Fulvestrant (MedChemExpress) | Positive control for ERα degradation; tests mutant resistance. |
| Selective Inhibitor | Elacestrant (RAD1901) (Selleckchem) | Tests next-generation SERD efficacy against mutants. |
1. Introduction within the Thesis Context The investigation of ESR1 mutations represents a pivotal chapter in the broader thesis on mechanisms of hormone therapy resistance in estrogen receptor-positive (ER+) metastatic breast cancer (MBC). While initial resistance often involves altered growth factor signaling, acquired resistance following prolonged aromatase inhibitor (AI) therapy is frequently driven by the emergence of ligand-binding domain mutations in ESR1. These mutations confer ligand-independent, constitutive transcriptional activity, rendering tumors resistant to estrogen deprivation. This whitepaper examines the evolving role of ESR1 mutations not merely as resistance markers, but as sophisticated biomarkers with clinical implications for metastatic tropism and quantitative disease assessment.
2. ESR1 Mutation Prevalence and Quantitative Association with Disease Burden
The prevalence of ESR1 mutations is strongly correlated with prior AI exposure and the extent of metastatic disease. Data from recent ctDNA analysis studies illustrate this relationship.
Table 1: ESR1 Mutation Prevalence by Clinical Context
| Clinical Context | Prevalence Range | Key Associations |
|---|---|---|
| Primary Breast Cancer (Treatment-naïve) | <1% | Very rare, often subclonal. |
| MBC with no prior AI exposure | 5-15% | Associated with de novo resistance. |
| MBC after 1st-line AI therapy | 20-30% | Correlates with progression. |
| MBC after ≥2 lines of endocrine therapy | 30-40% | High clonal dominance. |
| Metastatic Disease Burden (High vs. Low ctDNA fraction) | 3-5x higher odds | Strong correlation with variant allele frequency (VAF). |
Table 2: Association of ESR1 Mutation VAF with Metastatic Site
| Metastatic Site | Relative ESR1 Mutation VAF | Notes |
|---|---|---|
| Liver | High (Often >10% VAF) | Associated with higher overall ctDNA fraction and poor prognosis. |
| Bone | Moderate to High | Most common site; mutations frequently detected. |
| Lymph Nodes | Variable | Can be moderate; accessible for tissue biopsy. |
| Lung/Pleura | Moderate | Commonly detected. |
| Brain | Lower (Often <1% VAF) | Blood-brain barrier may limit ctDNA shed; cerebrospinal fluid analysis may be superior. |
3. Experimental Protocols for Detection and Functional Analysis
3.1. Circulating Tumor DNA (ctDNA) Analysis by Digital Droplet PCR (ddPCR)
- Purpose: Ultrasensitive quantification of known ESR1 mutations (e.g., Y537S, Y537N, D538G) in plasma.
- Protocol:
- Blood Collection: Collect peripheral blood (2 x 10mL) in Streck Cell-Free DNA BCT tubes. Process within 6 hours.
- Plasma Isolation: Double-centrifugation (1,600 x g for 10 min, then 16,000 x g for 10 min at 4°C).
- cfDNA Extraction: Use silica-membrane based kits (e.g., QIAamp Circulating Nucleic Acid Kit). Elute in 50-60 µL.
- ddPCR Assay Setup: Prepare reaction mix with ddPCR Supermix for Probes, wild-type and mutant-specific TaqMan probes (differentially labeled), and restriction enzyme (e.g., HaeIII) to reduce wild-type genomic DNA interference.
- Droplet Generation & PCR: Generate droplets using a droplet generator. Run PCR: 95°C for 10 min; 40 cycles of 94°C for 30s and 58°C for 60s; 98°C for 10 min.
- Quantification: Read plate on a droplet reader. Analyze with QuantaSoft software. Calculate mutant allele frequency (MAF) = (mutant droplets / total droplets) * 100.
3.2. Next-Generation Sequencing (NGS) of ESR1 Ligand-Binding Domain
- Purpose: Comprehensive detection of known and novel ESR1 mutations in ctDNA or tissue.
- Protocol (Targeted Panel):
- Library Preparation: Using 20-50 ng cfDNA, perform ligation-based library prep with unique molecular identifiers (UMIs).
- Target Enrichment: Hybridize libraries with biotinylated probes covering ESR1 exons 4-8. Capture with streptavidin beads.
- Sequencing: Perform paired-end sequencing (2x150 bp) on an Illumina platform to achieve >10,000x raw coverage.
- Bioinformatics: Process with UMI-aware pipeline: align to reference genome, group reads by UMI, call variants with a sensitivity threshold of ~0.1% VAF.
3.3. In Vitro Functional Characterization of ESR1 Mutants
- Purpose: Assess constitutive activity and drug sensitivity.
- Protocol (Transcriptional Reporter Assay):
- Cell Transfection: Co-transfect ER-negative cells (e.g., HEK293T) with expression vectors for wild-type or mutant ESR1, an estrogen-response element (ERE)-driven luciferase reporter, and a Renilla luciferase control.
- Treatment: Culture transfected cells in phenol-red free media with charcoal-stripped serum. Treat with vehicle, 17β-estradiol (E2, 1 nM), or various therapeutics (e.g., fulvestrant 100 nM, oral SERDs 100 nM).
- Measurement: After 24-48h, harvest cells and measure firefly and Renilla luciferase activity using a dual-luciferase assay kit. Normalize firefly to Renilla signal.
4. Signaling Pathways and Clinical Implications
Diagram Title: Constitutive Signaling by ESR1 Mutants Driving AI Resistance
Diagram Title: Evolution of ESR1 Mutations from Subclone to Metastatic Driver
5. The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for ESR1 Mutation Research
| Item | Function / Purpose | Example Product/Catalog |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Stabilizes blood cells to prevent genomic DNA contamination during plasma isolation. | Streck cfDNA BCT (Cat# 230254) |
| Silica-Membrane cfDNA Kits | High-recovery, low-elution volume extraction of circulating free DNA. | QIAamp Circulating Nucleic Acid Kit (Cat# 55114) |
| ddPCR Mutation Assays | Pre-designed, validated probe assays for absolute quantification of specific ESR1 mutations. | Bio-Rad ddPCR ESR1 Mutation Assays (e.g., dHsaMDV2010587 for D538G) |
| NGS Hybridization Capture Probes | Biotinylated oligonucleotide probes for enriching the ESR1 locus from cfDNA libraries. | Twist Comprehensive Cancer Panel (includes full ESR1 LBD) |
| UMI Adapter Kits | Attaches unique molecular identifiers to DNA fragments pre-PCR to correct for sequencing errors/duplicates. | IDT xGen UDI-UMI Adapters |
| Wild-Type & Mutant ESR1 Expression Vectors | For functional characterization of mutation impact in cell-based assays. | Addgene plasmids #plasmid1 (WT ESR1), #plasmid2 (Y537S) |
| ERE-Luciferase Reporter Plasmid | Standardized reporter to measure ER transcriptional activity. | Addgene plasmid #plasmid_3 (ERE-TATA-Luc) |
| Charcoal/Dextran-Stripped FBS | Removes steroid hormones for estrogen-depletion cell culture. | Gibco charcoal-stripped FBS (Cat# 12676029) |
| Selective ER Degraders (SERDs) | Reference compounds (fulvestrant) and next-generation oral SERDs for sensitivity testing. | Fulvestrant (Selleckchem Cat# S1191); Elacestrant (Selleckchem Cat# S9116) |
Detecting and Analyzing ESR1 Mutations: From Liquid Biopsy to Functional Assays
The emergence of acquired ESR1 mutations as a predominant mechanism of resistance to aromatase inhibitor therapy in metastatic estrogen receptor-positive (ER+) breast cancer has created an urgent need for robust, repeatable mutation detection. This technical guide evaluates tissue biopsy against circulating tumor DNA (ctDNA) analysis as methodological standards, contextualized within the imperative to dynamically monitor clonal evolution during endocrine therapy.
Technical Comparison of Methodologies
Core Characteristics and Performance Metrics
Table 1: Methodological Comparison for ESR1 Mutation Detection
| Parameter | Tissue Biopsy (Gold Standard) | Liquid Biopsy (ctDNA Analysis) |
|---|---|---|
| Invasiveness | High (surgical or core needle) | Minimal (peripheral blood draw) |
| Tumor Representativeness | Single-site, subject to heterogeneity | Captures shed DNA from multiple sites |
| Turnaround Time | 7-14 days (fixation, processing) | 3-5 days (plasma separation, analysis) |
| Repeatability | Limited by patient safety/consent | High-frequency serial monitoring feasible |
| Analytical Sensitivity | ~5% mutant allele frequency (ddPCR) | ~0.1% mutant allele frequency (ddPCR/NGS) |
| Key ESR1 Targets | Y537S, Y537N, Y537C, D538G, E380Q | Y537S, Y537N, Y537C, D538G, E380Q |
| Approved Companion Diagnostics | Yes (e.g., Oncomine Dx TT) | Emerging (e.g., Guardant360 CDx, FoundationOne Liquid CDx) |
| Primary Clinical Context | Diagnosis, initial staging | Monitoring therapy resistance, metastasis |
Table 2: Quantitative Performance Data from Recent Studies (2023-2024)
| Study (PMID) | Tissue Sensitivity | ctDNA Sensitivity | Concordance Rate | Key Platform |
|---|---|---|---|---|
| PALOMA-3 Sub-study | 95% | 93% | 97% | ddPCR (BEAMing) |
| SoFEA Study | 91% | 89% | 94% | NGS (Guardant360) |
| PlasmaMATCH B Cohort | N/A | 96% (vs. tissue reference) | 99% (PPA) | NGS (Signatera) |
| EMERALD Trial Analysis | Reference | 0.1% LOD | High for Y537S/D538G | NGS (FoundationOne Liquid) |
Detailed Experimental Protocols
Protocol A: UltrasensitiveESR1Mutation Detection via ddPCR from Plasma
- Blood Collection & Processing: Collect 10mL blood in Streck Cell-Free DNA BCT tubes. Centrifuge at 1600× g for 20 min at 4°C within 2 hours. Transfer plasma to microtube; high-speed centrifuge at 16,000× g for 10 min to remove debris.
- cfDNA Extraction: Use the QIAamp Circulating Nucleic Acid Kit (Qiagen). Elute in 40 µL AVE buffer.
- Droplet Digital PCR (ddPCR) Assay: Prepare 20 µL reaction with ddPCR Supermix for Probes (No dUTP), 20ng cfDNA, and ESR1 mutation-specific FAM probes (e.g., Y537S) with HEX-labeled reference assay (ESR1 wild-type). Generate droplets on QX200 Droplet Generator. Thermocycle: 95°C for 10 min; 40 cycles of 94°C for 30s and 55-60°C (annealing) for 60s; 98°C for 10 min.
- Analysis: Read droplets on QX200 Droplet Reader. Quantify mutant allele frequency (MAF) using QuantaSoft software. Threshold for positivity: ≥3 mutant droplets and MAF ≥0.1%.
Protocol B: NGS-BasedESR1Profiling from FFPE Tissue
- Tissue Sectioning & Macrodissection: Cut 5-10 µm sections from FFPE block. Hematoxylin and eosin stain; mark tumor-rich areas (>20% nuclei). Macrodissect corresponding region.
- DNA Extraction: Use the QIAamp DNA FFPE Tissue Kit with deparaffinization and Proteinase K digestion. Quantify via Qubit dsDNA HS Assay.
- Library Preparation & Hybrid Capture: Use 50ng DNA. Prepare libraries with the KAPA HyperPrep Kit. Hybridize with a custom panel (e.g., Illumina TruSeq Custom Amplicon) targeting ESR1 ligand-binding domain hotspots. Capture with streptavidin beads.
- Sequencing & Analysis: Sequence on Illumina MiSeq (500x median coverage). Align to hg19 with BWA. Call variants using GATK Mutect2 (tumor-only mode). Annotate with VEP. Report ESR1 mutations with ≥5% MAF and ≥100x supporting reads.
Visualizing Workflows and Biology
Diagram 1: Comparative Workflows for ESR1 Detection
Diagram 2: ESR1 Mutation Biology and Therapy
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Research Reagent Solutions for ESR1 Mutation Studies
| Item & Vendor (Example) | Function in ESR1 Research | Key Application Note |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Preserves blood cfDNA for up to 14 days; inhibits white cell lysis. | Critical for pre-analytical standardization in multi-center trials. |
| QIAamp Circulating Nucleic Acid Kit (Qiagen) | Extracts high-quality, short-fragment cfDNA from plasma. | Optimized for low-abundance ESR1 mutant allele recovery. |
| Bio-Rad ddPCR ESR1 Mutation Assays | FAM/HEX probe assays for Y537S, D538G, etc. | Ultrasensitive (0.1% MAF) quantification for serial monitoring. |
| Illumina TruSight Oncology 500 ctDNA | Hybrid-capture NGS panel covering ESR1 LBD. | Detects known/novel ESR1 mutations and co-alterations. |
| Cobas ESR1 Mutation Test v2 (Roche) | CE-IVD PCR test for plasma ESR1 mutations. | Standardized companion diagnostic utility. |
| Aromasin (Exemestane) Resistant MCF-7 Cells | Cell line models with acquired ESR1 Y537S/N mutations. | In vitro functional validation of mutation impact. |
| Anti-ESR1 (clone SP1) for IHC (Abcam) | Confirms ER protein expression in tumor tissue. | Validates ER positivity prior to ESR1 mutation testing. |
| IDT xGen Pan-Cancer Panel | Custom hybridization probes for targeted sequencing. | Allows inclusion of ESR1 and other resistance genes in custom panels. |
Integrated Clinical-Research Application
The methodological gold standard is context-dependent. Tissue biopsy remains the anatomic and diagnostic benchmark for primary tumor characterization. However, for the specific research question of monitoring the acquisition and clonal dynamics of ESR1 mutations under the selective pressure of endocrine therapy, ctDNA analysis is now the functional gold standard due to its feasibility for serial assessment and superior analytical sensitivity for low-frequency mutations. Future trials (e.g., those evaluating next-generation SERDs like elacestrant) rely on baseline and on-treatment ctDNA profiling to stratify patients and understand resistance. The combined use of both methods—tissue for baseline genotyping and ctDNA for longitudinal surveillance—represents the most robust approach in advanced ER+ breast cancer research.
The emergence of acquired ESR1 mutations is a predominant mechanism of resistance to aromatase inhibitor (AI) therapy in estrogen receptor-positive (ER+) metastatic breast cancer. Within the broader thesis on ESR1's role in hormone therapy resistance, tracking these mutations (e.g., Y537S, D538G) in circulating tumor DNA (ctDNA) via liquid biopsy is paramount. It enables real-time monitoring of clonal evolution, assessment of treatment efficacy, and early detection of resistance, guiding sequential therapeutic strategies. This technical guide details three core platforms—ddPCR, BEAMing, and NGS—for sensitive ESR1 mutation tracking.
Platform Technical Specifications and Quantitative Comparison
Table 1: Comparative Performance Metrics of ESR1 Detection Platforms
| Platform | Theoretical Limit of Detection (LOD) | Typical Input DNA | Multiplexing Capacity | Key Strengths | Key Limitations |
|---|---|---|---|---|---|
| ddPCR | ~0.01% VAF (Variant Allele Frequency) | 5-20 ng ctDNA | Low (2-4 plex) | Absolute quantification, high precision, cost-effective for known variants. | Targeted; discovers only predefined mutations. |
| BEAMing | ~0.01% VAF | 5-30 ng ctDNA | Moderate (Up to ~20-plex) | High sensitivity, digital counting, can couple to flow cytometry. | Complex workflow, proprietary, lower throughput. |
| NGS (Capture-based) | ~0.1% - 0.5% VAF (routine); ~0.02% with UMI | 20-100 ng ctDNA | Very High (Panels to whole exome) | Discovery of novel mutations, broad genomic context, detection of co-mutations. | Higher cost, complex bioinformatics, longer turnaround. |
Table 2: Clinical Validation Performance for Key ESR1 Mutations (Y537S/N/C, D538G)
| Study Reference (Example) | Platform | Sensitivity | Specificity | Key Finding |
|---|---|---|---|---|
| Chandarlapaty et al., 2016 | ddPCR | 97% | 100% | ESR1 mutations in ctDNA predict shorter PFS on subsequent AI therapy. |
| Gyanchandani et al., 2016 | BEAMing | >95% | >99% | Detection of ESR1 mutations post-AI therapy correlated with resistance. |
| Fribbens et al., 2016 | NGS (Guardant360) | 92% | >99% | Longitudinal tracking shows ESR1 mutations emerge under AI pressure. |
Detailed Experimental Protocols
Protocol:ESR1Mutation Detection via ddPCR
This protocol details the detection of the ESR1 p.D538G mutation.
- ctDNA Isolation: Extract ctDNA from 2-4 mL of patient plasma using the QIAamp Circulating Nucleic Acid Kit (Qiagen). Elute in 20-40 µL of AVE buffer. Quantify using the Qubit dsDNA HS Assay.
- Assay Design: Use commercially available or custom-designed TaqMan hydrolysis probe assays. One assay targets the mutant allele (FAM-labeled), and one targets the wild-type allele (HEX/VIC-labeled) for the same genomic locus.
- Droplet Generation and PCR:
- Prepare a 20 µL reaction mix per sample: 10 µL ddPCR Supermix for Probes (No dUTP), 1 µL each primer/probe assay (20X), up to 20 ng ctDNA, nuclease-free water.
- Generate droplets using the QX200 Droplet Generator. Transfer 40 µL of generated droplets to a 96-well PCR plate.
- Perform PCR on a thermal cycler: 95°C for 10 min (enzyme activation), followed by 40 cycles of 94°C for 30 sec and 55-60°C (assay-specific) for 60 sec, then 98°C for 10 min (enzyme deactivation). Ramp rate: 2°C/sec.
- Droplet Reading and Analysis:
- Read the plate on the QX200 Droplet Reader.
- Analyze using QuantaSoft software. Set thresholds to distinguish positive (FAM+/HEX+ for wild-type, FAM+/HEX- for mutant) and negative droplets. The software calculates the concentration (copies/µL) and VAF: [Mutant/(Mutant + Wild-type)] * 100.
Protocol:ESR1Mutation Detection via BEAMing (Beads, Emulsification, Amplification, and Magnetics)
- ctDNA Isolation & Amplification: Isolate ctDNA. Perform a first-stage PCR to amplify the ESR1 region of interest (e.g., exon 8) using biotinylated primers.
- Bead Coupling & Emulsification PCR:
- Bind the biotinylated amplicons to streptavidin-coated magnetic beads.
- Create a water-in-oil emulsion, partitioning single DNA-bound beads and PCR reagents into millions of microreactors.
- Perform a second PCR inside each droplet to clonally amplify the DNA on the bead surface.
- Mutation Detection:
- Break the emulsion.
- Hybridize fluorescently labeled allele-specific probes (for mutant and wild-type sequences) to the amplified DNA on beads.
- Analyze beads via flow cytometry. Wild-type beads bind only the wild-type probe, mutant beads bind only the mutant probe. The ratio of mutant to total beads gives the VAF.
Protocol:ESR1Mutation Detection via Targeted NGS with UMIs
- ctDNA Isolation & Library Prep: Isolate ctDNA. Prepare sequencing libraries using a hybrid-capture panel (e.g., MSK-IMPACT, FoundationOne Liquid CDx) that includes ESR1 exons.
- Critical Step: Incorporate Unique Molecular Identifiers (UMIs) during initial adapter ligation or early PCR cycles to tag each original DNA molecule, enabling error correction.
- Target Capture & Sequencing: Perform hybrid capture of the ESR1 and other target regions. Amplify the captured libraries. Sequence on an Illumina platform (e.g., NovaSeq) to achieve high coverage (>10,000x).
- Bioinformatic Analysis:
- Align reads to the reference genome (hg38).
- Group reads by their UMI to identify and collapse PCR duplicates, creating consensus reads.
- Call variants using a specialized, high-sensitivity caller (e.g., MuTect, VarScan2) with a low allele frequency threshold (e.g., 0.02%). Annotate variants.
Visualization of Workflows and Pathways
Title: ddPCR Workflow for ESR1 Mutation Detection
Title: ESR1 Wild-type vs. Mutant Signaling in Resistance
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ESR1 Mutation Tracking Experiments
| Item | Supplier Examples | Function in Context |
|---|---|---|
| cf/ctDNA Isolation Kit | QIAamp Circulating Nucleic Acid Kit (Qiagen), Maxwell RSC ccfDNA Plasma Kit (Promega) | High-yield, reproducible isolation of fragmented ctDNA from plasma. |
| ddPCR Supermix for Probes | Bio-Rad (ddPCR Supermix for Probes, No dUTP) | Optimized mix for droplet generation and robust probe-based amplification. |
| TaqMan SNP Genotyping Assays | Thermo Fisher Scientific (Custom or predesigned for ESR1 mutations) | Sequence-specific primers and FAM/HEX-labeled probes for allele discrimination. |
| Targeted NGS Panels with UMIs | MSK-IMPACT, FoundationOne Liquid CDx, AVENIO ctDNA kits (Roche) | Comprehensive, validated hybrid-capture panels for sensitive, multi-gene ctDNA analysis. |
| UMI Adapter Kits | KAPA HyperPrep, xGen cfDNA & Methyl-Seq Kit (IDT) | Library prep kits incorporating UMIs for accurate error correction. |
| Reference Genomic DNA (Wild-type) | Coriell Institute, Promega | Essential control for assay optimization and establishing baseline signals. |
| Synthetic ESR1 Mutation Controls | Horizon Discovery, gBlocks (IDT) | Precisely quantified mutant DNA for determining assay LOD, sensitivity, and standard curves. |
| Droplet Generation & Reading Oil | Bio-Rad (Droplet Generation Oil, Droplet Reader Oil) | Specialized oils for stable droplet formation and accurate fluorescence reading. |
This whitepaper provides a technical guide for the functional characterization of Estrogen Receptor Alpha (ERα/ESR1) mutations using advanced in vitro models. Framed within the broader thesis on the role of ESR1 mutations in driving resistance to endocrine therapies in breast cancer, this document details the establishment, validation, and application of cell lines and patient-derived organoids (PDOs) expressing mutant ERα. These models are indispensable for deconvoluting mutation-specific mechanisms of therapy resistance and for screening next-generation targeted therapies.
ESR1 Mutations: Key Variants and Clinical Prevalence
Activating mutations in the ligand-binding domain (LBD) of ESR1 are a major mechanism of acquired resistance to aromatase inhibitors (AIs) in metastatic ER+ breast cancer. These mutations confer ligand-independent transcriptional activity and reduced affinity for current Selective Estrogen Receptor Degraders (SERDs).
Table 1: Common ESR1 LBD Mutations and Their Functional Impact
| Mutation | Prevalence in AI-Resistant MBC* | Primary Functional Consequence | Reported Impact on Fulvestrant IC50 |
|---|---|---|---|
| Y537S | ~15-20% | High constitutive activity, stabilizes active helix 12 | 3 to 10-fold increase |
| D538G | ~10-15% | Moderate constitutive activity, alters co-factor binding | 2 to 5-fold increase |
| Y537N | ~5% | High constitutive activity | 4 to 8-fold increase |
| E380Q | ~3-5% | Alters ligand interaction; often co-occurs with other mutations | Modest increase |
| L536H | ~2-4% | Alters helix 12 positioning | Data evolving |
MBC: Metastatic Breast Cancer. Prevalence data is a composite from recent ctDNA sequencing studies (2023-2024).
In Vitro Model Systems: Generation and Selection
Engineered Cell Lines
Protocol: Generation of Isogenic Cell Lines Expressing Mutant ESR1 via CRISPR-Cas9
- Design gRNAs: Design two CRISPR RNAs (crRNAs) targeting exon 8 of ESR1 near the codon for Y537 or D538.
- Design HDR Template: Synthesize a single-stranded DNA oligonucleotide (ssODN) donor template (~200 nt) containing the desired mutation (e.g., TAC→TCC for Y537S) and a silent PAM-disrupting mutation.
- Transfection: Co-transfect ERα-positive breast cancer cells (e.g., MCF-7) with Cas9 protein, tracrRNA, crRNAs (as ribonucleoprotein complex), and the ssODN donor using a high-efficiency method (e.g., nucleofection).
- Clonal Selection: 48 hours post-transfection, begin selection with appropriate antibiotics if a resistance cassette is included. Otherwise, single-cell clone via limiting dilution.
- Genotyping: Screen clones by Sanger sequencing of PCR-amplified ESR1 exon 8. Confirm absence of random integration via genomic PCR.
- Validation: Validate protein expression and constitutive activity via immunoblotting for ERα and an ERα-target gene (e.g., PGR) under hormone-deprived conditions.
Patient-Derived Organoids (PDOs)
Protocol: Establishment and Culture of ER+ Breast Cancer PDOs
- Sample Acquisition: Obtain malignant pleural effusion or core biopsy from a patient with metastatic ER+ breast cancer (preferably post-AI progression).
- Processing: Mechanically dissociate tissue, followed by enzymatic digestion with collagenase/hyaluronidase for 1-2 hours at 37°C.
- Red Blood Cell Lysis: Use ammonium-chloride-potassium (ACK) lysis buffer.
- Matrigel Embedding: Resuspend cell pellets in reduced-growth factor Matrigel and plate as 40μL domes in pre-warmed culture plates. Polymerize for 30 min at 37°C.
- Culture Medium: Overlay with advanced DMEM/F12 supplemented with:
- Essential: B27, N2, HEPES, GlutaMAX, Primocin.
- Growth Factors: 50ng/mL EGF, 100ng/mL FGF-10, 10nM Heregulin-β1, 500nM A83-01 (TGF-βRi), 10μM Y-27632 (ROCKi).
- Hormones: 1nM β-estradiol (for WT ERα cultures), 5% charcoal-stripped FBS.
- Passaging: Digest Matrigel domes with Cell Recovery Solution, mechanically/enzmatically dissociate organoids, and re-embed in fresh Matrigel at 1:3-1:4 split ratio.
- Mutation Profiling: Perform whole-exome or targeted sequencing (e.g., ctDNA or organoid DNA) to identify endogenous ESR1 mutation status.
Core Functional Assays and Protocols
Transcriptional Activity Profiling
Protocol: Luciferase Reporter Assay for Constitutive Activity
- Seed Cells: Plate isogenic or organoid-derived cells in phenol-red free media with 5% charcoal-stripped serum for 5 days.
- Transfect: Co-transfect with an Estrogen Response Element (ERE)-luciferase reporter plasmid and a Renilla luciferase control plasmid.
- Treat: Treat with vehicle (0.1% DMSO), 1nM E2, or 100nM Fulvestrant for 24 hours.
- Lyse & Measure: Use a dual-luciferase assay kit. Measure firefly and Renilla luminescence.
- Analysis: Normalize firefly to Renilla luminescence. Constitutive activity is reported as fold-change over vehicle-treated WT ERα cells.
Table 2: Example Transcriptional Output of ESR1 Mutants (Relative Luminescence Units)
| ERα Variant | Vehicle | 1nM Estradiol (E2) | E2 + 100nM Fulvestrant | Constitutive Activity (Vehicle vs WT) |
|---|---|---|---|---|
| Wild-Type | 1.0 ± 0.2 | 8.5 ± 1.1 | 0.8 ± 0.3 | 1x |
| Y537S | 6.8 ± 0.9 | 9.1 ± 1.3 | 4.2 ± 0.7 | 6.8x |
| D538G | 3.2 ± 0.5 | 8.8 ± 1.0 | 1.9 ± 0.4 | 3.2x |
Growth and Survival Assays
Protocol: Long-Term 3D Clonogenic Survival Assay in Matrigel
- Embed Cells: Mix 500 cells with 40μL Matrigel and seed in pre-warmed 24-well plates.
- Treatment: After polymerization, overlay with assay media containing vehicle, 1nM E2, 100nM Fulvestrant, or novel SERDs/SERMs. Include a full estrogen deprivation (ED) arm.
- Culture & Feed: Culture for 14-21 days, refreshing treatments and media twice weekly.
- Fix & Stain: Fix colonies with 4% PFA, stain with 0.1% Crystal Violet.
- Quantify: Image wells and quantify colony number and area using software (e.g., ImageJ). Calculate % survival relative to vehicle-treated control.
Co-factor Interaction Analysis
Protocol: Proximity Ligation Assay (PLA) for ERα-cofactor Interaction
- Culture Cells: Grow cells on chamber slides under hormone-deprived conditions.
- Fix & Permeabilize: Fix with 4% PFA, permeabilize with 0.5% Triton X-100.
- Block & Incubate: Block and incubate with primary antibodies from different hosts (e.g., mouse anti-ERα, rabbit anti-SRC-3/NCOA3).
- PLA Probes: Incubate with PLA probes (MINUS and PLUS).
- Ligation & Amplification: Perform ligation and amplification steps using commercial PLA kit reagents.
- Image & Analyze: Mount with DAPI-containing medium. Image with fluorescence microscopy. Each red dot represents a single protein-protein interaction event. Quantify dots per nucleus.
Key Signaling Pathways in Mutant ERα-Driven Resistance
The constitutive activity of mutant ERα rewires cellular signaling, engaging both canonical genomic and non-genomic pathways to promote survival and proliferation.
Pathways of Mutant ERα-Driven Transcription and Resistance
Experimental Workflow for Model Characterization
A systematic approach is required to fully characterize novel in vitro models of ESR1 mutation.
Workflow for Characterizing Mutant ERα In Vitro Models
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Mutant ERα Functional Studies
| Reagent Category | Specific Example(s) | Function & Rationale |
|---|---|---|
| Cell Line Models | MCF-7 (ERα+), T47D (ERα+), HCC1428 (ERα+ Luminal) | Parental backgrounds for engineering isogenic mutant ESR1 lines. |
| Culture Supplements | Charcoal-stripped FBS, Phenol-red free media | Removes exogenous steroids and estrogen-like compounds for hormone-depletion studies. |
| Reference Ligands | β-Estradiol (E2), Fulvestrant (ICI 182,780), 4-Hydroxytamoxifen (4-OHT) | Gold-standard agonists and antagonists for benchmarking mutant ERα response. |
| Antibodies (IHC/WB) | Anti-ERα (clone SP1, D6H2), Anti-PGR, Anti-GREB1, Anti-PS2 | Validate ERα expression and monitor classic target gene activation. |
| Reporter Plasmids | ERE-TATA-Luciferase (e.g., pGL4-3xERE) | Quantify constitutive and ligand-induced transcriptional activity. |
| Organoid Culture | Reduced-growth Factor Matrigel, B27 supplement, A83-01, Y-27632 | Essential for establishing and maintaining patient-derived organoids. |
| CRISPR Tools | Synthetic crRNAs/tracrRNAs, Cas9 protein, HDR donor templates | For precise knock-in of ESR1 mutations in cell lines. |
| Detection Kits | Dual-Luciferase Reporter Assay, Proximity Ligation Assay (PLA) | Quantify transcriptional output and protein-protein interactions. |
Data Integration and Therapeutic Profiling
Functional data from these models must be integrated with transcriptomic (RNA-seq) and cistromic (ChIP-seq) analyses to define mutation-specific signatures. The ultimate application is high-throughput screening of novel SERDs, PROTACs, and combination therapies (e.g., with CDK4/6 or mTOR inhibitors). Dose-response curves (IC50 values) generated in mutant vs. WT models are the primary metric for identifying compounds that overcome mutation-driven resistance.
Patient-derived xenografts (PDXs) have emerged as a gold-standard preclinical model, particularly for studying complex, clinically relevant phenomena like endocrine therapy resistance in hormone receptor-positive (HR+) breast cancer. A primary driver of this resistance is the acquisition of mutations in the ESR1 gene, which encodes the estrogen receptor alpha (ERα). PDX models, established by directly implanting patient tumor tissue into immunodeficient mice, retain the original tumor's genetic, histopathological, and phenotypic heterogeneity. This fidelity makes them indispensable for elucidating the role of ESR1 mutations (e.g., Y537S, D538G) in promoting ligand-independent ER activity and resistance to aromatase inhibitors (AIs) and selective estrogen receptor degraders (SERDs). This whitepaper serves as a technical guide for deploying PDX models in preclinical drug testing, with a focused lens on ESR1-mutant breast cancer.
Key Experimental Protocols for PDX Generation and Drug Testing
PDX Establishment and Propagation
Objective: To engraft and serially propagate patient tumor tissue in mice while preserving original characteristics, including ESR1 mutation status.
Methodology:
- Source Tissue: Obtain fresh tumor samples from biopsies or surgeries (primary or metastatic) under IRB-approved protocols. Tissue is placed in cold, serum-free culture medium with antibiotics.
- Processing: Mince tissue into 1-3 mm³ fragments using sterile scalpels.
- Implantation: Mix fragments with Matrigel and implant subcutaneously (s.c.) into the flank of anesthetized NOD-scid IL2Rγ[null] (NSG) or similar immunodeficient mouse. Orthotopic (mammary fat pad) or metastatic site implants are used for specific studies.
- Monitoring: Tumor growth is measured weekly with calipers. Volume = (Length × Width²) / 2.
- Passaging: Upon reaching 1000-1500 mm³, the mouse is euthanized. The tumor is excised, divided, and re-implanted into new mice (P1 generation). This repeats for P2, P3, etc.
- Biobanking: Snap-freeze fragments in liquid N₂ for nucleic acid extraction; fix in formalin for histology; cryopreserve live fragments for reconstitution.
Preclinical Drug Efficacy Study inESR1-Mutant PDXs
Objective: To evaluate the in vivo efficacy of novel agents (e.g., next-gen SERDs, PROTACs, combination therapies) against ESR1-mutant PDX models.
Methodology:
- Model Selection: Use a characterized ESR1 Y537S or D538G mutant PDX line and a wild-type ESR1 control line.
- Cohort Design: Implant tumor fragments into a cohort of mice (n=8-10 per group). Randomize mice into treatment groups when tumors reach ~200 mm³.
- Treatment Regimens:
- Control: Vehicle
- Standard of Care: Fulvestrant (5 mg/mouse, s.c., weekly) or AI (Letrozole, 10 µg/day, oral gavage)
- Experimental Arm: Novel SERD (e.g., oral elacestrant, 30 mg/kg, daily, oral gavage)
- Combination Arm: Experimental agent + CDK4/6 inhibitor (e.g., palbociclib, 75 mg/kg, daily, oral gavage).
- Monitoring & Endpoints: Measure tumors 2-3 times weekly. End study when control tumors reach endpoint volume. Calculate:
- Tumor Growth Inhibition (TGI%) = [1 - (ΔT/ΔC)] × 100, where ΔT and ΔC are mean tumor volume changes in treatment and control groups.
- Regression: % of mice with tumor volume < starting volume.
- Pharmacodynamic Analysis: At study end, harvest tumors. Analyze phospho-ERK, phospho-S6, ERα degradation (western blot), and proliferation index (Ki67 IHC).
Table 1: Efficacy of Therapeutic Agents in ESR1 Mutant vs. Wild-Type PDX Models
| PDX Model (ESR1 Status) | Treatment (Dose, Route) | Median PFS (Days) | Best Avg. TGI % | Tumor Regression Rate (%) | Reference/Study ID |
|---|---|---|---|---|---|
| HCI-013 (Y537S) | Vehicle Control | 14 | 0 | 0 | (Bertucci et al., 2019) |
| HCI-013 (Y537S) | Fulvestrant (5 mg/wk, SC) | 28 | 45 | 0 | (Bertucci et al., 2019) |
| HCI-013 (Y537S) | Elacestrant (30 mg/kg/d, PO) | 56 | 98 | 40 | (Lai et al., 2023) |
| ST941 (D538G) | Vehicle Control | 21 | 0 | 0 | (Spoerke et al., 2016) |
| ST941 (D538G) | Fulvestrant + Palbociclib | 70+ | 110 | 100 | (Spoerke et al., 2016) |
| WHIM16 (WT) | Fulvestrant (5 mg/wk, SC) | 50+ | 95 | 75 | (Li et al., 2020) |
Table 2: Molecular Characterization of Breast Cancer PDX Panels
| PDX Line | Origin (Patient Site) | ESR1 Mutation | ER Status (IHC) | PgR Status | HER2 Status | Common Engraftment Rate (%) |
|---|---|---|---|---|---|---|
| HCI-013 | Pleural Effusion | Y537S | Positive | Negative | Negative | ~85 |
| ST941 | Primary Breast | D538G | Positive | Positive | Negative | ~75 |
| WHIM16 | Primary Breast | Wild-type | Positive | Positive | Negative | ~80 |
| MAXF-401 | Primary Breast | L536H | Positive | Negative | Negative | ~70 |
| Overall (HR+ Breast Cancer) | - | ~30% in AI-resistant | Retained | Often Lost | Retained | 60-80 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PDX Workflow in ESR1 Research
| Item | Function & Rationale |
|---|---|
| NSG (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) Mice | Immunodeficient host for successful engraftment of human tissue. Lacks T, B, and NK cells. |
| Matrigel (Growth Factor Reduced) | Basement membrane matrix. Co-implantation supports tumor cell survival, angiogenesis, and engraftment. |
| RNAlater Stabilization Solution | Preserves RNA integrity in tumor tissue snap-frozen for downstream ESR1 sequencing and transcriptomics. |
| Droplet Digital PCR (ddPCR) Assay for ESR1 Mutations | Ultrasensitive quantitation of ESR1 mutant allele frequency in PDX tissue and circulating tumor DNA. |
| Phospho-ERα (Ser118) Antibody | Key pharmacodynamic marker. Detects ligand-independent, phosphorylated (active) ER in ESR1-mutant tumors post-treatment. |
| Next-Generation SERDs (e.g., Elacestrant, Camizestrant) | Investigational oral agents for direct in vivo comparison against fulvestrant in mutant PDX efficacy studies. |
| CDK4/6 Inhibitors (Palbociclib, Abemaciclib) | Standard-of-care combinatory agents for testing synergy with endocrine therapies in resistance models. |
| In Vivo Imaging System (IVIS) with Luciferase Transduction | Enables non-invasive tracking of orthotopic/metastatic PDX growth if tumors are engineered to express luciferase. |
Pathway and Workflow Visualizations
Diagram 1: ESR1 Mutant vs. Wild-Type ERα Signaling and Drug Action
Diagram 2: PDX Establishment and Drug Testing Workflow
Transcriptomic and Proteomic Profiling to Uncover Downstream Signaling Networks
Within the critical research paradigm of ESR1 mutation-driven endocrine resistance in breast cancer, understanding the resultant rewiring of cellular signaling is paramount. Transcriptomic and proteomic profiling provides a powerful, multi-omics lens to systematically map these adaptive downstream networks. This guide details the integrative methodologies and analytical frameworks used to elucidate these pathways, offering a technical roadmap for researchers aiming to identify novel therapeutic vulnerabilities.
Core Signaling Networks Perturbed by ESR1 Mutations
ESR1 mutations (e.g., Y537S, D538G) confer constitutive, ligand-independent activation and alter co-regulator binding. This leads to a profound reprogramming of the cellular transcriptome and proteome, activating growth and survival pathways that bypass traditional hormonal blockade.
Diagram 1: ESR1 Mutation-Driven Signaling Crosstalk
Integrated Multi-Omics Profiling Workflow
A robust profiling strategy requires parallel and integrated analysis of RNA and protein-level changes to distinguish transcriptional regulation from post-translational effects.
Diagram 2: Integrated Profiling Experimental Workflow
Detailed Experimental Protocols
3.1 Transcriptomic Profiling via Bulk RNA-Seq
- Cell Culture & Treatment: Maintain isogenic MCF-7 cells (ESR1 WT vs. Y537S) in phenol-red free media with charcoal-stripped serum. Treat with vehicle or 100 nM fulvestrant for 72 hours. n=6 biological replicates per condition.
- RNA Extraction & QC: Use TRIzol reagent with Phase Lock Gel tubes. Assess RNA integrity (RIN > 9.0) via Bioanalyzer.
- Library Preparation & Sequencing: Prepare libraries using Illumina Stranded mRNA Prep. Sequence on NovaSeq 6000 (PE 150bp) to a depth of 40 million reads per sample.
- Bioinformatic Analysis: Align reads to GRCh38 with STAR. Quantify gene counts with featureCounts. Perform differential expression (DE) analysis using DESeq2 (FDR < 0.05, |log2FC| > 1). Conduct GSEA on Hallmark and KEGG gene sets.
3.2 Proteomic and Phosphoproteomic Profiling via LC-MS/MS
- Protein Extraction & Digestion: Lyse cells in 8M Urea buffer. Digest proteins with Lys-C and trypsin. Desalt peptides using C18 StageTips.
- Phosphopeptide Enrichment: Enrich phosphorylated peptides from 1 mg peptide input using TiO2 or Fe-IMAC magnetic beads.
- LC-MS/MS Analysis: Analyze peptides on a Q Exactive HF-X mass spectrometer coupled to an EASY-nLC 1200. Use a 120-min gradient. Operate in data-dependent acquisition (DDA) mode.
- Data Processing: Search raw files against UniProt human database using MaxQuant (v2.0.x). Set fixed modification: carbamidomethyl (C); variable: oxidation (M), phosphorylation (S,T,Y). Use a 1% FDR cutoff. Normalize label-free quantification (LFQ) intensities. Perform statistical analysis with Perseus or LIMMA.
Key Quantitative Data from Profiling Studies
Table 1: Representative Omics Signatures in ESR1 Y537S vs. WT Models
| Omics Layer | Analytical Method | Key Upregulated Pathways (FDR < 0.01) | Representative Key Molecules (Log2FC) | Therapeutic Implication |
|---|---|---|---|---|
| Transcriptome | RNA-Seq | E2F Targets, G2M Checkpoint, mTORC1 Signaling | CCNE1 (+2.1), MYC (+1.8), AKT1S1 (+1.5) | CDK2/4/6, mTOR inhibitors |
| Proteome | Label-Free LC-MS/MS | Myc Targets, DNA Repair | PCNA (+1.2), MCM7 (+1.4) | PARP, ATR inhibitors |
| Phosphoproteome | TiO2-enriched LC-MS/MS | MAPK, PI3K-Akt Signaling | p-ERK1/2 T202/Y204 (+3.0), p-AKT S473 (+2.2) | MEK, AKT, PI3K inhibitors |
Table 2: Research Reagent Solutions Toolkit
| Reagent / Material | Supplier Examples | Function in Profiling ESR1 Mutant Signaling |
|---|---|---|
| Charcoal-Stripped FBS | Gibco, Sigma-Aldrich | Depletes steroids to create hormone-depleted cell culture conditions. |
| Fulvestrant (ICI 182,780) | Tocris, Selleckchem | Selective estrogen receptor degrader (SERD) for treatment resistance studies. |
| TRIzol Reagent | Thermo Fisher | Simultaneous isolation of high-quality RNA, DNA, and protein from single samples. |
| Illumina Stranded mRNA Prep | Illumina | Library prep kit for preserving strand orientation in RNA-Seq. |
| Q Exactive HF-X Mass Spectrometer | Thermo Fisher | High-resolution, accurate-mass LC-MS/MS system for deep proteome coverage. |
| TiO2 Magnetic Beads | GL Sciences, Thermo Fisher | Enrich for phosphorylated peptides prior to MS analysis. |
| MaxQuant Software | Max Planck Institute | Computational platform for MS-based proteomics data analysis. |
| DESeq2 R Package | Bioconductor | Statistical analysis of differential gene expression from RNA-Seq count data. |
Integrative Bioinformatics & Network Visualization
The true power of multi-omics lies in integration. Use tools like CausalPath or IPA to merge transcript and protein/phosphoprotein data, inferring upstream regulators and causal networks.
Diagram 3: Integrative Analysis Logic for Network Inference
Transcriptomic and proteomic profiling, as outlined, is an indispensable approach for deconstructing the complex, compensatory signaling networks established by ESR1 mutations. The integrated data and resultant models directly inform the development of rational combination therapies—such as SERDs with CDK4/6, PI3K, or mTOR inhibitors—to overcome hormone therapy resistance. This systematic profiling and validation cycle is fundamental to translating basic resistance mechanisms into actionable clinical strategies.
The discovery of activating mutations in the ESR1 gene (encoding the Estrogen Receptor Alpha) has fundamentally altered our understanding of acquired resistance to endocrine therapy in estrogen receptor-positive (ER+) metastatic breast cancer. This whitepaper positions the clinical application of ESR1 mutation status within the broader thesis that these mutations are a primary driver of ligand-independent ER signaling, representing a pivotal mechanism of resistance to aromatase inhibitors and selective estrogen receptor degraders (SERDs). Consequently, stratifying patients based on ESR1 mutation status is no longer a research consideration but a clinical necessity for the development of next-generation hormonal agents and combination therapies.
Current Landscape of ESR1 Mutations in Clinical Trials
ESR1 mutations are predominantly found in the hormone-binding domain (HBD) and are rare in primary breast cancer but emerge under the selective pressure of aromatase inhibitor therapy in up to 40% of metastatic ER+ breast cancers. The most common mutations (Y537S, Y537N, D538G, E380Q) confer varying degrees of constitutive activity and differential resistance profiles.
Table 1: Prevalence and Functional Impact of Key ESR1 Mutations
| Mutation | Approximate Prevalence in mBC (%) | Constitutive Activity Level | Relative Resistance to Fulvestrant |
|---|---|---|---|
| D538G | ~15-20% | Moderate | Intermediate |
| Y537S | ~10-15% | High | High |
| Y537N | ~5-10% | High | High |
| E380Q | ~5% | Low | Low |
Table 2: Selected Pivotal Clinical Trials Stratifying by ESR1 Mutation Status
| Trial Name | Phase | Agent(s) | Primary Endpoint | ESR1 Stratification Outcome |
|---|---|---|---|---|
| EMERALD (NCT03778931) | 3 | Elacestrant vs SOC | PFS in ESR1-mut pts | HR=0.55 in ESR1-mut; FDA approval |
| PADA-1 (NCT03079011) | 3 | Palbociclib + Fulv vs Switch to AI | PFS | Switching improved PFS in ESR1-mut |
| SERENA-2 (NCT04214288) | 2 | Camizestrant (various doses) vs Fulv | PFS | Dose-dependent PFS benefit in ESR1-mut |
| AMERA-3 (NCT04191382) | 3 | Amcenestrant + Palbo vs Letrozole + Palbo | PFS (1L) | Trial failed; no significant benefit |
Methodologies for ESR1 Mutation Detection in Trial Context
Accurate detection of ESR1 mutations from circulating tumor DNA (ctDNA) is the standard for patient screening and enrollment due to the challenges of sequential metastatic tissue biopsies.
Protocol: ctDNA Collection and Extraction forESR1Testing
- Sample Collection: Collect 10-20 mL of whole blood into dedicated cell-stabilizing tubes (e.g., Streck Cell-Free DNA BCT). Process within 6-96 hours per manufacturer protocol to prevent leukocyte lysis and background wild-type DNA contamination.
- Plasma Separation: Double-centrifugation protocol.
- First spin: 1600-2000 x g for 10-20 minutes at 4°C. Transfer supernatant (plasma) to a fresh tube, avoiding buffy coat.
- Second spin: 16,000 x g for 10 minutes at 4°C. Transfer cleared plasma to a final tube.
- ctDNA Extraction: Use a validated column- or bead-based extraction kit (e.g., QIAamp Circulating Nucleic Acid Kit, MagMax Cell-Free DNA Isolation Kit). Elute in a low-volume buffer (e.g., 20-50 µL AE buffer).
- Quality Control: Quantify using a fluorometric assay specific for double-stranded DNA (e.g., Qubit dsDNA HS Assay). Fragment analysis (e.g., Bioanalyzer) should show a peak ~170 bp.
Protocol: Digital Droplet PCR (ddPCR) forESR1Mutation Screening
- Principle: Absolute quantification of mutant allele fraction (MAF) without need for a standard curve. Ideal for tracking specific known mutations.
- Procedure:
- Assay Design: Use validated, locked hydrolysis (TaqMan) probe assays for specific ESR1 mutations (e.g., Y537S, D538G) with distinct fluorophores (FAM for mutant, HEX/VIC for wild-type).
- Reaction Setup: Prepare 20 µL reaction mix containing 1x ddPCR Supermix for Probes (no dUTP), 900 nM primers, 250 nM probes, and up to 8 µL of extracted ctDNA.
- Droplet Generation: Use a QX200 AutoDG or manual droplet generator to partition the reaction into ~20,000 nanoliter-sized oil-emulsion droplets.
- PCR Amplification: Thermal cycling: 95°C for 10 min (enzyme activation), then 40 cycles of 94°C for 30 s and 55-60°C (assay-specific) for 60 s, with a final 98°C for 10 min. Ramp rate: 2°C/s.
- Droplet Reading & Analysis: Read droplets on a QX200 Droplet Reader. Analyze using QuantaSoft software. Set amplitude thresholds to distinguish mutant-positive, wild-type-positive, and negative droplets. Calculate MAF = [Nmut/(Nmut + N_wt)].
- Threshold for Positivity: Typically, ≥ 0.5% MAF with a minimum of 3 mutant droplets is considered clinically actionable for trial enrollment.
Protocol: Next-Generation Sequencing (NGS) for BroadESR1Interrogation
- Principle: Captures all mutations within the ESR1 HBD, enabling discovery of rare variants.
- Procedure:
- Library Preparation: Use a targeted hybrid-capture panel (e.g., Guardant360 CDx, FoundationOne Liquid CDx) covering the full ESR1 coding sequence. Perform adapter ligation and sample barcoding.
- Target Enrichment: Hybridize libraries to biotinylated probes for ESR1 and other cancer-related genes. Wash and capture with streptavidin beads.
- Sequencing: Perform massively parallel sequencing on platforms like Illumina NovaSeq or NextSeq. Aim for a minimum mean coverage of 5,000x for ctDNA panels.
- Bioinformatics: Align reads to reference genome (GRCh38). Call variants using specialized ctDNA callers (e.g., Mutect2 with
--f1r2-tar-gnuoptions) that account for low MAF and sequencing artifacts. Filter against population databases (gnomAD) and panel-of-normals.
- Reporting: Report all non-synonymous ESR1 mutations with MAF ≥ 0.5% (or platform-specific validated limit of detection).
Diagrams
Diagram 1: ESR1 Mutation-Driven Resistance Pathway
Diagram 2: Trial Screening & Stratification Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for ESR1 Mutation Research & Testing
| Item | Function/Benefit | Example Product/Catalog |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes blood cells to prevent genomic DNA contamination of plasma, critical for accurate low-MAF detection. | Streck Cell-Free DNA BCT; Roche Cell-Free DNA Collection Tube |
| Ultra-Sensitive dsDNA Quantitation Kit | Accurate quantification of low-concentration ctDNA extracts, essential for input normalization in ddPCR/NGS. | Thermo Fisher Qubit dsDNA HS Assay |
| Validated ddPCR Assay for ESR1 Mutations | Ready-to-use, optimized probe-primer mixes for absolute quantification of specific hotspot mutations. | Bio-Rad ddPCR Mutation Assay for ESR1 p.D538G (dHsaMDV2010586) |
| Targeted Hybrid-Capture NGS Panel | Comprehensive panel covering ESR1 HBD and other resistance genes from ctDNA; includes library prep reagents. | Illumina TruSight Oncology 500 ctDNA; Thermo Fisher Oncomine Breast cfDNA Assay |
| ER Mutant Cell Lines | Pre-clinical models for studying mutation biology and drug response. | MCF7 Engineered lines (Y537S, D538G); HCC1428 (ESR1 Y537S endogenous) |
| Reference Standard ctDNA | Contains known ESR1 mutations at defined MAFs for assay validation and quality control. | Seraseq ctDNA Mutation Mix; Horizon Multiplex I cfDNA Reference Standard |
This whitepaper explores the critical role of circulating tumor DNA (ctDNA) analysis in monitoring therapeutic response and the emergence of resistance, framed within a broader thesis investigating the pivotal role of ESR1 mutations in driving resistance to endocrine therapy (ET) in hormone receptor-positive (HR+) metastatic breast cancer (MBC). The dynamic, non-invasive profiling of ctDNA provides an unprecedented window into the evolving genomic landscape of tumors under therapeutic pressure, enabling the early detection of resistance mechanisms such as ESR1 mutations (e.g., Y537S, D538G) that render aromatase inhibitors ineffective.
Core Principles of ctDNA Dynamics in Resistance Monitoring
ctDNA refers to fragmented DNA shed by tumor cells into the bloodstream. Its quantitative level (variant allele frequency, VAF) and qualitative makeup (specific mutations) correlate with tumor burden and clonal evolution. In the context of ET for HR+ MBC:
- Response: Effective therapy leads to a decline in total ctDNA concentration and the VAF of driver mutations.
- Stable Disease: ctDNA levels may plateau, indicating a balance between cell death and proliferation.
- Emerging Resistance: A rise in total ctDNA and/or the de novo detection or increasing VAF of resistance mutations (e.g., ESR1) often precedes radiographic progression by weeks or months.
Key Quantitative Data on ctDNA andESR1Mutations
Table 1: Clinical Performance of ctDNA in Detecting ESR1 Mutations and Predicting Progression
| Parameter | Value Range / Finding | Study Context (Example) | Implication |
|---|---|---|---|
| Lead Time | 2.5 - 10.5 months | Detection of ESR1 mutations in ctDNA ahead of clinical/radiographic progression in MBC. | Provides a window for therapeutic intervention before overt progression. |
| Prevalence in AI-Resistant MBC | 25% - 40% | Found in plasma of patients progressing on Aromatase Inhibitor (AI) therapy. | Establishes ESR1 mutations as a major resistance mechanism. |
| Concordance with Tissue | 85% - 98% | Comparison of ESR1 mutation status in ctDNA vs. metastatic tissue biopsy. | Validates ctDNA as a reliable, less invasive alternative to biopsy. |
| Predictive Value for PFS | Hazard Ratio (HR): 1.5 - 3.2 | Patients with detectable ESR1 mutations in ctDNA have significantly shorter PFS on subsequent AI therapy. | ctDNA genotyping can guide therapy selection (e.g., switch to SERDs). |
| ctDNA Clearance (Molecular Response) | Associated with 60-80% reduction in progression risk | Rapid clearance of ESR1 mutations after initiating effective therapy (e.g., Elacestrant). | Serves as an early pharmacodynamic biomarker of drug activity. |
Table 2: Common ESR1 Ligand-Binding Domain Mutations and Functional Impact
| Mutation (Hotspot) | Prevalence Rank | Constitutive Activity | Impact on Ligand Binding | Resistance to |
|---|---|---|---|---|
| D538G | 1 | Moderate | Altered | Aromatase Inhibitors, Tamoxifen |
| Y537S | 2 | High | Reduced | Aromatase Inhibitors, Tamoxifen, Fulvestrant (partial) |
| Y537N | 3 | High | Reduced | Aromatase Inhibitors, Tamoxifen, Fulvestrant (partial) |
| E380Q | 4 | Low | Mildly Altered | Aromatase Inhibitors |
Experimental Protocols for ctDNA Analysis in Resistance Research
Protocol 1: Longitudinal ctDNA Collection and Processing for ESR1 Monitoring
- Blood Collection: Collect 2x10 mL peripheral blood into cell-stabilizing tubes (e.g., Streck Cell-Free DNA BCT) to prevent leukocyte lysis.
- Plasma Separation: Double-centrifugation protocol. First spin: 1600-2000 x g for 10 min at 4°C. Transfer supernatant to a fresh tube. Second spin: 16,000 x g for 10 min at 4°C to remove residual cells.
- cfDNA Extraction: Use silica-membrane column or bead-based kits optimized for low-concentration, short-fragment DNA (e.g., QIAamp Circulating Nucleic Acid Kit). Elute in low-EDTA buffer.
- Quantification & QC: Use fluorometric assays (e.g., Qubit dsDNA HS Assay) and fragment analyzer (e.g., Bioanalyzer) to assess yield and fragment size profile (~167 bp peak).
- Library Preparation & Sequencing: Use hybrid-capture or amplicon-based NGS panels covering ESR1 LBD hotspots and other relevant genes (e.g., PIK3CA, ERBB2). Aim for high sequencing depth (>10,000X) to detect low-VAF mutations.
- Bioinformatic Analysis: Align reads to reference genome (hg38). Use ultra-sensitive variant callers (e.g., MuTect2, LoFreq) with duplex-sequencing error suppression. Annotate variants and track VAF longitudinally.
Protocol 2: Digital PCR (dPCR) for Ultra-Sensitive ESR1 Mutation Tracking
- Assay Design: Design TaqMan hydrolysis probe assays for wild-type and specific mutant alleles (e.g., Y537S).
- Partitioning: Partition the extracted cfDNA sample into 20,000+ nanoscale reactions using droplet (ddPCR) or chip-based systems.
- Amplification: Perform endpoint PCR amplification within each partition.
- Detection & Quantification: Read fluorescence in each partition. Count positive droplets/chambers for mutant and wild-type signals.
- Calculation: Use Poisson statistics to calculate the absolute concentration (copies/mL plasma) and VAF of the ESR1 mutation. This method is optimal for tracking known mutations with sensitivity down to 0.01%.
Visualizing Pathways and Workflows
ESR1 Mutation-Driven Resistance Pathway
ctDNA Analysis Workflow for Resistance Monitoring
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for ctDNA-Based Resistance Studies
| Item | Function in Protocol | Example Product/Catalog | Critical Specification |
|---|---|---|---|
| Cell-Free DNA Blood Collection Tube | Preserves blood sample, prevents genomic DNA contamination from white blood cell lysis during transport/storage. | Streck Cell-Free DNA BCT; Roche Cell-Free DNA Collection Tube. | Stability for up to 14 days at room temperature. |
| cfDNA Extraction Kit | Isolate short-fragment, low-concentration cfDNA from plasma with high purity and recovery. | QIAamp Circulating Nucleic Acid Kit (Qiagen); Maxwell RSC ccfDNA Plasma Kit (Promega). | Optimized for 1-5 mL plasma input; elution volume ≤ 50 µL. |
| Ultra-Sensitive NGS Library Prep Kit | Prepare sequencing libraries from low-input (<30 ng) cfDNA with minimal bias and high complexity. | KAPA HyperPrep Kit (Roche); ThruPLEX Plasma-seq Kit (Takara Bio). | Includes efficient end-repair, A-tailing, and adapter ligation. |
| Hybrid-Capture Panels | Enrich for a targeted gene panel (including ESR1 LBD) prior to sequencing. | xGen cfDNA & MSI Panel (IDT); SureSelect XT HS2 (Agilent). | Includes baits for SNVs, indels; high on-target rate. |
| dPCR Mutation Assay | For absolute quantification of specific ESR1 hotspot mutations (e.g., Y537S) with ultra-high sensitivity. | Bio-Rad ddPCR ESR1 Mutation Assay; Thermo Fisher TaqMan dPCR Assay. | Validated LoD of 0.1% VAF or lower; includes wild-type control. |
| Fragment Analyzer Kit | Quality control of extracted cfDNA, confirming characteristic ~167 bp peak size and absence of high-molecular-weight gDNA contamination. | DNF-474 Standard Sensitivity NGS Fragment Analysis Kit (Agilent). | Size range: 35-1500 bp. |
| Reference Standard | Positive control for assay validation and run quality control. Contains known ESR1 mutations at defined VAF in a background of wild-type DNA. | Seraseq ctDNA Mutation Mix (SeraCare); Horizon Multiplex I cfDNA Reference. | Matrices include matched mutant/wild-type and fragmented DNA. |
Overcoming ESR1-Mediated Resistance: Clinical Challenges and Therapeutic Optimization
Resistance to endocrine therapy represents the principal challenge in managing estrogen receptor-positive (ER+) breast cancer. Within the broader thesis on the role of ESR1 mutations in hormone therapy resistance, this analysis details the mechanistic and clinical limitations of two cornerstone first-line therapies: Aromatase Inhibitors (AIs) and Selective Estrogen Receptor Degraders (SERDs). ESR1 mutations, particularly those in the ligand-binding domain (LBD), evolve under selective AI pressure and confer constitutive, estrogen-independent ERα activity and relative insensitivity to current SERDs, driving therapeutic failure.
Core Mechanisms of Failure
Aromatase Inhibitor (AI) Failure
AIs (e.g., letrozole, anastrozole) suppress estrogen synthesis. Their failure is intrinsically linked to the acquisition of ESR1 mutations (Y537S, D538G, etc.), which render ERα active in a ligand-independent manner. AI therapy creates the selective pressure that enriches these mutations.
Selective Estrogen Receptor Degrader (SERD) Inefficacy
SERDs like fulvestrant competitively bind ERα and induce its degradation. However, certain ESR1 mutations stabilize the receptor, reduce binding affinity, and alter co-regulator recruitment, leading to partial degradation and residual transcriptional activity—termed "partial SERD inefficacy."
Table 1: Prevalence of ESR1 Mutations in Metastatic Breast Cancer Post-AI Therapy
| Study Cohort (Source) | Sample Type | Detection Method | ESR1 Mutation Prevalence | Most Common Mutations |
|---|---|---|---|---|
| PALOMA-3 (Circulating DNA) | cfDNA | ddPCR, NGS | 25.3% (Baseline) | D538G, Y537S, E380Q |
| SoFEA (Plasma) | cfDNA | BEAMing | 39.1% (Progression) | D538G, Y537S |
| BOLERO-2 (Tumor/Plasma) | Tissue/cfDNA | NGS | 28.8% (Progression) | D538G, Y537S, L536H |
Table 2: Impact of ESR1 Mutations on SERD Efficacy In Vitro
| ESR1 Mutation | Fulvestrant IC50 Shift vs. Wild-Type (Fold Change) | ERα Degradation Efficiency (% of Wild-Type) | Constitutive Activity (Fold vs. WT+E2) | Key Reference |
|---|---|---|---|---|
| Y537S | 6.5 - 12.8 | 30-45% | 8.2 | Toy et al., 2013 |
| D538G | 3.2 - 5.1 | 50-65% | 5.7 | Jeselsohn et al., 2015 |
| E380Q | ~1.5 | ~85% | 2.1 | Zhao et al., 2020 |
Detailed Experimental Protocols
Protocol: AssessingESR1Mutation Prevalence in cfDNA
Objective: Isolate and quantify ESR1 mutations from patient plasma. Methodology:
- Plasma Collection & cfDNA Extraction: Collect 10 mL blood in Streck tubes. Isolate plasma via double centrifugation. Extract cfDNA using the QIAamp Circulating Nucleic Acid Kit.
- Library Preparation & Target Enrichment: Construct sequencing libraries from 20-50 ng cfDNA. Perform targeted enrichment for ESR1 exons 4-8 using a hybrid-capture panel.
- Ultra-Deep Sequencing: Sequence on an Illumina platform to achieve >10,000X coverage. Use unique molecular identifiers (UMIs) for error correction.
- Bioinformatic Analysis: Align reads to hg19. Call variants using specialized tools (e.g., MuTect2 for cfDNA). Report variants with allele frequency >0.5% after UMI deduplication.
Protocol: Evaluating SERD Efficacy inESR1-Mutant Cell Lines
Objective: Measure ERα degradation and transcriptional activity post-SERD treatment in isogenic models. Methodology:
- Cell Model Generation: Use CRISPR/Cas9 to introduce specific ESR1 point mutations (Y537S, D538G) into ER+ MCF-7 breast cancer cells. Validate via Sanger sequencing.
- ERα Degradation Assay: Seed mutant and WT cells in 6-well plates. Treat with a dose range of fulvestrant (1 nM - 1 µM) or vehicle for 24h. Lyse cells and perform Western blotting for ERα (clone HC-20). Normalize to β-actin. Quantify band intensity to calculate DC50.
- Transcriptional Activity Assay: Co-transfect cells with an ERE-driven luciferase reporter and a Renilla control plasmid. After 24h, treat with fulvestrant +/- E2 (1 nM). Measure luciferase activity after 18h. Data presented as fold-change relative to vehicle control.
Signaling Pathways and Experimental Workflows
Title: AI-Driven ESR1 Mutation Leads to SERD Inefficacy
Title: cfDNA ESR1 Mutation Detection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating ESR1-Mediated Resistance
| Item Name | Supplier (Example) | Function in Research Context |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Streck | Preserves cfDNA profile in blood samples by preventing leukocyte lysis and genomic DNA contamination. |
| QIAamp Circulating Nucleic Acid Kit | Qiagen | Optimized for isolation of short-fragment, low-concentration cfDNA from plasma/serum. |
| ERα Antibody (clone HC-20) | Santa Cruz Biotechnology | Rabbit polyclonal antibody targeting the C-terminus of ERα; used for immunoblot detection of full-length and degraded ER. |
| ERE-TATA-Luc Reporter Plasmid | Addgene (plasmid #11354) | Firefly luciferase reporter under control of estrogen response elements (EREs); used to quantify ER transcriptional activity. |
| CRISPR/Cas9 Gene Editing System | Synthego or IDT | For precise introduction of ESR1 point mutations (e.g., Y537S) into ER+ cell lines to create isogenic models. |
| Fulvestrant (ICI 182,780) | Tocris Bioscience | The prototypical SERD used as a benchmark compound in in vitro and in vivo efficacy studies against mutant ESR1. |
| Validated ESR1 Mutant Cell Lines (Y537S, D538G) | ATCC or Horizon Discovery | Pre-engineered, characterized cell models (e.g., MCF-7 ESR1 Y537S) for consistent study of mutant ER biology. |
Endocrine therapy remains the cornerstone for treating estrogen receptor-alpha (ERα)-positive breast cancer. However, acquired resistance, frequently driven by mutations in the ESR1 gene, presents a major clinical challenge. These mutations, primarily found in the ligand-binding domain (LBD), lead to constitutive, estrogen-independent activation of the ER, rendering traditional agents like aromatase inhibitors (AIs) ineffective. This context has driven the development of a new class of agents: oral Selective Estrogen Receptor Degraders (SERDs). Unlike the intramuscular SERD fulvestrant, oral SERDs like elacestrant offer the promise of potent ER degradation with convenient dosing, directly targeting the mechanism of ESR1-mutant driven resistance.
Elacestrant: Core Mechanism of Action
Elacestrant is a novel, nonsteroidal, oral SERD. Its mechanism is dual, involving both antagonism and degradation of the ER.
- Competitive Antagonism: Elacestrant competes with endogenous estrogen (17β-estradiol, E2) for binding to the ER's ligand-binding domain (LBD). It binds with high affinity, including to common mutant forms like D538G and Y537S.
- Receptor Degradation: Upon binding, elacestrant induces a conformational change in the ER that promotes its ubiquitination and subsequent degradation by the 26S proteasome. This reduces total cellular ER protein levels, a critical function against mutants that exhibit ligand-independent activity.
- Inhibition of Transcriptional Activity: The elacestrant-ER complex is transcriptionally inert. It fails to recruit coactivators and cannot initiate transcription at estrogen response elements (EREs), blocking the proliferative and pro-survival gene programs driven by both wild-type and mutant ER.
Diagram 1: Elacestrant's Dual Mechanism of Action
The EMERALD Trial: Protocol and Key Findings
EMERALD (NCT03778931) was a global, open-label, randomized, Phase III registrational trial designed to evaluate elacestrant versus standard-of-care (SOC) endocrine monotherapy in patients with ER+/HER2- metastatic breast cancer (mBC).
Detailed Experimental Protocol
A. Study Design & Population:
- Patients: 478 postmenopausal women and men with ER+/HER2- mBC.
- Prior Therapy: Disease progression on/after 1-2 lines of endocrine therapy and 1 line of a CDK4/6 inhibitor.
- Stratification: ESR1 mutation status (detected in circulating tumor DNA, ctDNA), prior fulvestrant use, and visceral metastasis presence.
- Randomization: 1:1 to either elacestrant (345 mg oral, daily) or SOC (investigator's choice of fulvestrant or an aromatase inhibitor).
B. Key Endpoints:
- Primary Endpoint: Progression-free survival (PFS) by blinded independent review committee (BIRC) in the overall population and the ESR1-mutant subgroup.
- Key Secondary Endpoints: Overall survival (OS), objective response rate (ORR), safety, and quality of life.
C. ctDNA Analysis Protocol:
- Sample Collection: Plasma samples collected at baseline.
- Technology: Next-generation sequencing (NGS) of ctDNA using a validated assay (e.g., Guardant360).
- Analysis: Centralized testing for hotspot mutations in ESR1 (including D538G, Y537S/N/C). Patients were categorized as ESR1-mutant (detected) or ESR1-non-mutant (not detected).
Table 1: EMERALD Trial Primary Efficacy Results (BIRC-Assessed PFS)
| Population / Parameter | Elacestrant Arm | Standard-of-Care (SOC) Arm | Hazard Ratio (HR) [95% CI] | P-value | |
|---|---|---|---|---|---|
| Overall (N=478) | Median PFS | 2.8 months | 1.9 months | 0.70 [0.55, 0.88] | 0.0018 |
| 6-month PFS Rate | 34.3% | 20.4% | |||
| 12-month PFS Rate | 22.3% | 9.4% | |||
| ESR1-mutant (n=228) | Median PFS | 3.8 months | 1.9 months | 0.55 [0.39, 0.77] | 0.0005 |
| 6-month PFS Rate | 40.8% | 19.1% | |||
| 12-month PFS Rate | 26.8% | 8.2% | |||
| ESR1-non-mutant (n=250) | Median PFS | 2.2 months | 1.9 months | 0.86 [0.63, 1.19] | 0.19 |
Table 2: Key Safety Profile of Elacestrant (EMERALD Trial)
| Adverse Event (All Grades) | Elacestrant (n=239) | SOC (n=238) |
|---|---|---|
| Nausea | 35.0% | 18.8% |
| Fatigue | 19.0% | 19.2% |
| Arthralgia | 14.9% | 11.1% |
| Vomiting | 19.0% | 7.6% |
| Decreased Appetite | 11.5% | 5.9% |
| Serious Adverse Events | 12.5% | 13.2% |
| Discontinuation due to AE | 3.4% | 0.4% |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying Oral SERDs and ESR1 Mutations
| Reagent / Material | Function & Application in Research |
|---|---|
| Isogenic Cell Lines | Engineered to express wild-type or specific ESR1 mutations (Y537S, D538G). Crucial for head-to-head comparison of drug effects in a controlled genetic background. |
| ERα Reporter Assays | Luciferase-based constructs with ERE promoters. Quantify transcriptional activity of ER in response to ligand (E2) or drug (elacestrant). |
| Selective ER Degradation Assays | Immunoblotting (Western Blot) or immunofluorescence using anti-ERα antibodies (e.g., Clone SP1, D6H2). Measures drug-induced reduction in ER protein levels over time. |
| Proliferation Assays | CellTiter-Glo or similar ATP-based assays. Determine the anti-proliferative IC50 values of SERDs in 2D or 3D culture models. |
| Cellular Thermal Shift Assay (CETSA) | Measures drug-target engagement in cells by quantifying the thermal stabilization of ER upon elacestrant binding. |
| Patient-Derived Xenografts (PDXs) | ESR1-mutant PDX models recapitulate the patient's tumor biology. The gold standard for in vivo efficacy testing of SERDs. |
| ctDNA NGS Kits | Commercial plasma NGS panels (e.g., Guardant360, FoundationOne Liquid). Enable non-invasive tracking of ESR1 mutation status and clonal evolution in preclinical and clinical studies. |
| Co-Immunoprecipitation (Co-IP) Reagents | Antibodies against ER and ubiquitin or specific E3 ligases. Used to investigate the mechanism of drug-induced ER ubiquitination. |
Diagram 2: EMERALD Trial Design Workflow
The EMERALD trial established elacestrant as the first oral SERD with proven efficacy in ESR1-mutant, ER+ advanced breast cancer post-CDK4/6 inhibitor therapy. Its success validates the targeting of ESR1 mutations as a critical strategy to overcome endocrine resistance. The trial paradigm—patient selection via ctDNA genotyping, head-to-head comparison against standard endocrine therapy, and stratification by ESR1 status—sets a new standard for future drug development in this space. Elacestrant's arrival heralds a shift towards more convenient, targeted endocrine options and provides a backbone for novel combinations aiming to further delay chemotherapy and improve outcomes.
The acquisition of mutations in the estrogen receptor alpha gene (ESR1) is a principal mechanism of resistance to aromatase inhibitor (AI) therapy in estrogen receptor-positive (ER+), HER2-negative metastatic breast cancer (mBC). These mutations, predominantly found in the ligand-binding domain (e.g., Y537S, D538G), confer constitutive, estrogen-independent ER activity and relative resistance to selective ER degraders (SERDs) like fulvestrant. This necessitates the development of optimized rational combination therapies to overcome resistance and improve patient outcomes. This guide details the scientific rationale, current data, and experimental approaches for combining next-generation oral SERDs with key downstream pathway inhibitors: CDK4/6, PI3K, and mTOR.
Scientific Rationale and Pathway Analysis
The persistent signaling through mutant ESR1 drives continuous transcription of genes regulating cellular proliferation and survival. Combination strategies target both the receptor itself and these critical downstream effector pathways, which often see compensatory upregulation.
Core Signaling Pathway
The following diagram illustrates the primary signaling network connecting mutant ESR1 to the key therapeutic targets.
Pathway Title: Mutant ESR1 Drives Proliferation via CDK4/6 and PI3K/mTOR
Recent data from clinical trials and preclinical studies inform combination strategy optimization. The tables below summarize key efficacy and safety metrics.
Table 1: Clinical Efficacy of SERD Combinations in ESR1-mutant mBC
| Combination (Phase) | Trial Name / Model | Key Efficacy Metric (ESR1-mut) | Result (vs. Control) | Key Reference (Year) |
|---|---|---|---|---|
| Fulvestrant + Palbociclib (CDK4/6i) | PALOMA-3 (Phase III) | Median PFS | 9.5 mo vs. 4.2 mo (Fulv + Plac) | Turner et al., NEJM (2018) |
| Elacestrant (oral SERD) monotherapy | EMERALD (Phase III) | Median PFS (ESR1-mut) | 3.8 mo vs. 1.9 mo (SOC) | Bidard et al., JCO (2022) |
| Fulvestrant + Alpelisib (PI3Kαi) | SOLAR-1 (Phase III) | Median PFS (ESR1-mut/PIK3CA-mut) | 5.7 mo vs. 2.0 mo (Fulv + Plac) | André et al., NEJM (2019) |
| Fulvestrant + Vistusertib (mTORi) | MANTA (Phase II) | Clinical Benefit Rate | 36.4% vs. 20.0% (Fulv alone) | Schmid et al., Ann Oncol (2019) |
| Camizestrant (oral SERD) + Palbociclib | SERENA-4 (Phase III) | Median PFS (Interim) | Not Reached vs. 16.8 mo (Let + Palbo) | Oliveira et al., SABCS (2023) |
Table 2: Preclinical Synergy Data of Novel SERD Combinations
| SERD | Combination Agent (Class) | Model System (ESR1 status) | Synergy Metric (e.g., Bliss Score) | Key Mechanistic Insight |
|---|---|---|---|---|
| Fulvestrant | Abemaciclib (CDK4/6i) | MCF7 Y537S Xenograft | Strong Synergy (Tumor Regression) | Enhanced G1 arrest & senescence |
| Giredestrant | Inavolisib (PI3Kαi) | PDX Y537S Mutant | Combination Index (CI) < 0.7 | Dual suppression of ER+PI3K pathway output |
| Amcenestrant | Everolimus (mTORi) | T47D D538G Cells | ~80% Growth Inhibition | Blockade of mTOR feedback to ER |
| Elacestrant | Ribociclib (CDK4/6i) | CAMA-1 D538G | Significant ΔLog10 Cell Kill | Suppression of Rb phosphorylation & E2F targets |
Experimental Protocols for Key Investigations
Protocol: Evaluating Combination EfficacyIn Vivo
Title: PDX Efficacy Study of Oral SERD + CDK4/6 Inhibitor Objective: Assess tumor growth inhibition of a combination regimen in an ESR1-mutant Patient-Derived Xenograft (PDX) model.
Materials & Workflow:
- PDX Model Establishment: Implant a confirmed ESR1 Y537S or D538G mutant breast tumor fragment into the mammary fat pad of female NSG mice.
- Randomization: When tumors reach ~200 mm³, randomize mice (n=8-10/group) into four arms: Vehicle control, SERD monotherapy, CDK4/6i monotherapy, and Combination.
- Dosing: Administer compounds orally, 5 days/week. SERD at clinically relevant dose (e.g., 10 mg/kg). CDK4/6i at MTD-established dose (e.g., Palbociclib, 50 mg/kg).
- Monitoring: Measure tumor volumes via calipers 2-3 times weekly. Monitor body weight for toxicity.
- Endpoint Analysis: At study endpoint (tumor volume ~1500 mm³ in control), harvest tumors.
- Pharmacodynamic (PD) Analysis: Snap-freeze tissue for immunoblotting (pRb, ERα, Ki67, Cleaved Caspase-3).
- RNA-seq: Analyze gene expression changes to identify pathway modulation.
Workflow Title: In Vivo PDX Efficacy Study Workflow
Protocol: Assessing Pathway ModulationIn Vitro
Title: Immunoblot Analysis of Combination Effects on Signaling Nodes Objective: Determine the effect of single and combined agents on key pathway proteins (pRb, AKT, S6) in ESR1-mutant cell lines.
Detailed Methodology:
- Cell Culture: Seed ESR1-mutant (e.g., MCF7 Y537S) and wild-type isogenic control cells in 6-well plates.
- Treatment: After 24h, treat cells for 6h (acute signaling) or 24h (downstream effects) with:
- DMSO vehicle
- SERD (e.g., 100 nM Elacestrant)
- CDK4/6i (e.g., 500 nM Palbociclib)
- Combination of both
- Lysis: Aspirate media, wash with PBS, lyse cells in RIPA buffer + protease/phosphatase inhibitors.
- Immunoblotting:
- Load 20-30 µg protein per lane on 4-12% Bis-Tris gels.
- Transfer to PVDF membranes.
- Block for 1h in 5% BSA/TBST.
- Incubate with primary antibodies overnight at 4°C: pRb (S780), Total Rb, pAKT (S473), pS6 (S240/244), ERα, β-actin.
- Incubate with HRP-conjugated secondary antibodies for 1h at RT.
- Develop using enhanced chemiluminescence and image.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Investigating SERD Combinations
| Item / Reagent | Example Product/Catalog # | Function in Research Context |
|---|---|---|
| ESR1-Mutant Cell Lines | MCF7-Y537S (Horizon Discovery), T47D-D538G (ATCC CRL-2865) | Isogenic models to study mutant-specific biology and drug response. |
| Patient-Derived Xenografts (PDXs) | PDX from ESR1 Y537S mBC (e.g., JAX PDX repository) | Clinically relevant in vivo models preserving tumor heterogeneity. |
| Oral SERD Compounds | Elacestrant (MedChemExpress HY-135991), Giredestrant (Selleckchem S9576) | Next-generation SERDs for in vitro and in vivo combination studies. |
| Phospho-Specific Antibodies | pRb (S780) (CST 8180), pAKT (S473) (CST 4060), pS6 (S240/244) (CST 5364) | Key pharmacodynamic markers for target engagement and pathway inhibition. |
| Viable Cell Assay | CellTiter-Glo 3D (Promega G9683) | Quantify cell viability and proliferation in 2D/3D cultures post-treatment. |
| Synergy Analysis Software | Combenefit (Open Source), SynergyFinder (Web App) | Calculate combination indices (CI) and visualize synergy/antagonism using Loewe, Bliss, or HSA models. |
| ERα Chromatin Immunoprecipitation Kit | MAGnify ChIP Kit (Thermo Fisher 492024) | Assess ER chromatin binding and transcriptional activity after treatment. |
The research landscape for overcoming endocrine resistance in estrogen receptor-positive (ER+) breast cancer is dominated by the challenge of ESR1 mutations. These ligand-binding domain mutations, such as Y537S and D538G, confer constitutive activity and resistance to standard-of-care aromatase inhibitors. The broader thesis of this field posits that effective targeting of mutant ERα requires novel agents that achieve sustained and sufficient target engagement to suppress this constitutive signaling. This whitepaper provides a technical guide to the pharmacokinetic (PK) hurdles—absorption, distribution, metabolism, and excretion (ADME)—that must be overcome to translate potent in vitro activity into clinical efficacy for next-generation Selective Estrogen Receptor Degraders (SERDs), PROTACs, and other novel agents.
Core Pharmacokinetic Hurdles in TargetingESR1Mutants
Achieving therapeutic concentrations at the tumor site, particularly in metastatic lesions, is a primary challenge. Key hurdles include:
- Oral Bioavailability: Many novel ERα binders are large, lipophilic molecules with poor aqueous solubility, limiting absorption.
- Plasma Protein Binding: High binding to albumin and α1-acid glycoprotein reduces free, active drug fraction.
- Distribution to Metastatic Sites: Penetrating bone, liver, and brain metastases requires favorable physicochemical properties.
- Metabolic Clearance: Rapid phase I/II metabolism (e.g., via CYP3A4, UGTs) can limit exposure.
- On-Target Off-Tissue Toxicity: Engaging ERα in the uterus and bone necessitates a therapeutic window.
Table 1: Pharmacokinetic Parameters of Clinical-Stage Novel ER-Targeting Agents
| Agent (Class) | Oral Bioavailability (%) | Cmax (ng/mL) | t1/2 (hours) | Free Fraction (%) | Key ADME Challenge | Clinical Status (as of 2024) |
|---|---|---|---|---|---|---|
| Fulvestrant (SERD) | 0 (IM only) | 2.5-5.0 | ~40 | <1 | No oral route, high PPB | Approved |
| Elacestrant (oral SERD) | ~10 | 70-100 | 20-30 | ~3 | First-pass metabolism, PPB | Approved (EMERALD) |
| Camizestrant (oral SERD) | ~30 | 140-200 | 25-35 | 5-8 | Moderate CYP3A4 substrate | Phase III (SERENA) |
| Giredestrant (oral SERD) | ~25 | 110-180 | 15-25 | ~2.5 | High PPB, food effect | Phase III (persevERA) |
| ARV-471 (PROTAC) | <10 (preclinical) | N/A | N/A | N/A | Molecular size/efflux | Phase II |
Experimental Protocols for Assessing Target Engagement
Protocol 1: Quantitative Assessment of ERα Degradation and Turnover (Cellular Pharmacodynamics)
- Objective: To measure the potency and kinetics of novel SERD/ERD-induced ERα degradation and subsequent recovery.
- Materials: MCF-7 (ER+ WT), MCF-7 Y537S engineered cells, novel agent, fulvestrant (control), cycloheximide, lysis buffer, anti-ERα antibody (e.g., HC-20), β-actin antibody.
- Method:
- Seed cells in 6-well plates. At 80% confluence, treat with a 10-point dose-response of the test agent (e.g., 1 pM – 10 µM) for 6, 24, and 48 hours.
- For turnover studies, treat cells with a maximally degrading concentration (DC90) for 24h. Wash and replenish with drug-free media. Harvest cells at 0, 12, 24, 48, 72h post-washout.
- Lyse cells, perform SDS-PAGE, and immunoblot for ERα.
- Quantify band intensity, normalize to β-actin, and plot % ERα remaining vs. log[concentration] to calculate DC50. From turnover data, calculate the rate of ERα resynthesis.
- Interpretation: Agents achieving deeper, more durable degradation at lower concentrations indicate superior in vitro target engagement.
Protocol 2: In Vivo Microdialysis for Measuring Free Tumor Drug Concentrations
- Objective: To directly measure the unbound, pharmacologically active concentration of a novel agent within the tumor interstitium over time.
- Materials: Mouse xenograft model (e.g., patient-derived ESR1mut), microdialysis system (CMA), stereotactic frame, test agent formulated for dosing, artificial CSF/physiological perfusate.
- Method:
- Implant a microdialysis probe into the center of a established tumor (~500 mm³).
- Perfuse probe with isotonic saline at 0.5 µL/min. Allow 1-2h equilibration.
- Administer the test agent (PO or IV) at the therapeutic dose.
- Collect microdialysate fractions every 20-30 minutes for 12-24h. Collect matching plasma samples.
- Analyze samples using LC-MS/MS. Correct for probe recovery via retrodialysis.
- Interpretation: The area under the curve of unbound tumor concentration (AUCu, tumor) must exceed the in vitro DC90 for sufficient target engagement. Compare to plasma AUCu to determine distribution ratio.
Table 2: Research Reagent Solutions Toolkit
| Reagent / Material | Function & Application | Example Vendor/Cat # |
|---|---|---|
| Engineered ESR1 mutant cell lines | Isogenic models to study mutant-specific PK/PD relationships. | Horizon Discovery: MCF-7 Y537S, D538G |
| Recombinant mutant ERα LBD protein | For binding affinity (Kd) assays, crystallography, and in vitro metabolism studies. | Thermo Fisher (custom expression) |
| Stable Isotope-labeled Drug Internal Standard | Essential for accurate LC-MS/MS quantification of drug levels in complex matrices (plasma, tissue homogenate). | Sigma-Aldrich (custom synthesis) |
| Human Liver Microsomes (HLM) / Hepatocytes | To predict human-specific phase I metabolic clearance and identify major metabolites. | Corning Gentest |
| MDCK-MDR1 or Caco-2 cells | To assess permeability and P-glycoprotein efflux liability, predicting oral absorption. | ATCC |
| Phospho-ERα S118/S167 Antibodies | Biomarkers of receptor activity; assess functional target engagement downstream of binding. | Cell Signaling Technology #2511, #2514 |
Strategic Approaches to Overcome PK Hurdles
- Molecular Optimization: Reducing molecular weight and rotatable bonds while maintaining potency to improve absorption. Incorporating metabolic soft spots to reduce clearance.
- Formulation Strategies: Utilizing lipidic nanoparticles, amorphous solid dispersions, or co-crystals to enhance solubility and bioavailability of poorly soluble agents.
- Dosing Regimen Rationale: Employing pharmacokinetic/pharmacodynamic (PK/PD) modeling from preclinical data to design clinical loading and maintenance dosing schedules that maintain tumor concentrations above the target engagement threshold.
Diagram 1: PK/PD Pathway for ESR1-Targeting Agents
Diagram 2: Integrated PK/PD Optimization Workflow
Successfully addressing the pharmacokinetic hurdles for novel ESR1-targeting agents requires an integrated, quantitative approach from early discovery through clinical development. The goal is to ensure that the in vitro potency translates to sufficient in vivo target engagement, defined by sustained unbound tumor concentrations above the DC90 for mutant ERα degradation. Rigorous application of the protocols and strategies outlined herein, centered on measuring and optimizing the free drug exposure at the site of action, is critical for breaking the cycle of endocrine resistance in advanced ER+ breast cancer.
Within the broader thesis on the role of ESR1 mutations in hormone therapy resistance, a critical challenge is the heterogeneity of resistance mechanisms. This guide addresses the complex scenario of polyclonal ESR1 mutations—where multiple distinct mutations coexist within a single tumor or across metastases—and their frequent co-occurrence with other genetic alterations. This heterogeneity drives differential response to therapy and constitutes a major barrier to durable disease control in advanced estrogen receptor-positive (ER+) breast cancer. Understanding and troubleshooting this biological complexity is essential for developing effective therapeutic strategies.
Current Landscape and Quantitative Data
Recent studies using circulating tumor DNA (ctDNA) and single-cell sequencing have illuminated the prevalence and clinical impact of polyclonal ESR1 mutations. Key quantitative findings are summarized below.
Table 1: Prevalence and Impact of Polyclonal ESR1 Mutations
| Metric | Reported Value (%) / Frequency | Key Study / Method | Clinical Implication |
|---|---|---|---|
| Patients with ≥2 ESR1 mutations in ctDNA | 15-30% | Ultra-deep sequencing (ctDNA) | Associates with longer prior AI exposure |
| Most common co-occurring ESR1 mutations | Y537S, D538G, E380Q | Targeted NGS panels | May confer differential agonist activity & drug resistance |
| Co-occurrence with PIK3CA mutations | ~40-50% of ESR1-mutant cases | FoundationOne Liquid CDx | Rationale for combination PI3Ki + SERD |
| Co-occurrence with ERBB2 amplifications | ~5-10% of ESR1-mutant cases | NGS of metastatic biopsies | Potential driver of parallel resistance |
| Co-occurrence with RB1 loss | ~8-12% of ESR1-mutant cases | Whole-exome sequencing | Linked to lineage plasticity & small cell neuroendocrine features |
Table 2: Therapeutic Vulnerabilities in Polyclonal Contexts
| Alteration Combination | Model System | Vulnerability Identified | Proposed Mechanism |
|---|---|---|---|
| ESR1 Y537S + PIK3CA H1047R | MCF7-derived xenograft | Enhanced sensitivity to Elacestrant + Alpelisib | Co-targeting of mutant ER and PI3K/mTOR signaling |
| ESR1 D538G + FGFR1 amp | Patient-derived organoid | Resistance to Fulvestrant, sensitive to FGFR inhibitor | FGFR pathway sustains ER-independent growth |
| Polyclonal ESR1 mutations (≥3 variants) | ctDNA-guided therapy | Lower clinical benefit rate to single-agent SERD | Requires broader spectrum ER degraders or combinations |
Experimental Protocols for Investigating Heterogeneity
Protocol 3.1: Detection and Quantification of PolyclonalESR1Mutations from ctDNA
Objective: To identify and quantify multiple, low-frequency ESR1 mutations in plasma samples.
- Sample Collection: Collect 10-20 mL of blood in cell-stabilization tubes (e.g., Streck). Process within 6 hours to isolate plasma via double centrifugation (1600g, 10 min; 16,000g, 10 min).
- ctDNA Extraction: Use a validated circulating nucleic acid kit (e.g., QIAamp Circulating Nucleic Acid Kit). Elute in 40-60 µL.
- Library Preparation & Target Enrichment: Prepare libraries from 20-50 ng ctDNA using a hybrid capture-based NGS panel (e.g., focused on ESR1 ligand-binding domain hotspots: exons 4-8). Include unique molecular identifiers (UMIs) for error correction.
- Sequencing: Perform ultra-deep sequencing (≥50,000x raw coverage) on an Illumina platform to ensure detection of variants down to ~0.1% variant allele frequency (VAF).
- Bioinformatic Analysis: Process data through a UMI-aware pipeline (e.g., bwa-mem → fgbio group/consensus → GATK Mutect2). Call mutations with a sensitivity threshold of 0.1% VAF. Clonality is inferred from VAFs and phylogenetic analysis.
Protocol 3.2: Functional Validation Using Isogenic Cell Line Pools
Objective: To model polyclonality and test drug responses in vitro.
- Generation of Polyclonal Models: Use CRISPR-Cas9 or lentiviral transduction to introduce distinct, barcoded ESR1 mutations (e.g., Y537S, D538G) into an ER+ breast cancer cell line (e.g., MCF7). Maintain separate populations and mix them in defined ratios (e.g., 50:50, 70:30) to create polyclonal pools.
- Drug Sensitivity Assays: Plate polyclonal pools in estrogen-depleted medium. Treat with a dose range of:
- Selective Estrogen Receptor Degraders (SERDs): Fulvestrant, Elacestrant.
- Selective Estrogen Receptor Modulators (SERMs): Tamoxifen.
- Combination therapies: SERD + PI3K inhibitor (e.g., Alpelisib). Incubate for 6-10 days.
- Endpoint Analysis: Assess viability via CellTiter-Glo. Simultaneously, harvest genomic DNA from treated and untreated wells.
- Clonal Tracking: Amplify and sequence the barcodes or the mutant alleles via droplet digital PCR (ddPCR) to quantify shifts in the relative abundance of each mutant clone under selective drug pressure.
Protocol 3.3: Spatial Mapping in Metastatic Tissue
Objective: To assess geographic heterogeneity of ESR1 mutations within a single metastasis.
- Multiregion Sampling: From a fresh-frozen metastatic biopsy, take 4-6 spatially distinct punches (1-2 mm³ each) using sterile coring tools under a dissection microscope.
- Nucleic Acid Co-extraction: Use AllPrep DNA/RNA FFPE Kit for simultaneous isolation of genomic DNA and RNA from each region.
- Parallel Analysis:
- DNA: Perform deep targeted NGS for ESR1 and co-alterations.
- RNA: Perform quantitative RT-PCR for ER-responsive genes (PGR, TFF1) and a proliferation marker (MKI67).
- Data Integration: Correlate regional mutation VAFs with transcriptional output to determine functional impact of heterogeneity.
Visualizing Pathways and Workflows
Title: Co-occurring Alterations Drive Resistance Signaling
Title: Workflow for Detecting Polyclonal ESR1 Mutations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for ESR1 Heterogeneity Research
| Item | Function & Application | Example Product / Assay |
|---|---|---|
| ctDNA Stabilization Tubes | Preserves cell-free DNA profile by preventing leukocyte lysis during blood storage/transport. | Streck Cell-Free DNA BCT, Roche Cell-Free DNA Collection Tubes |
| UMI-Integrated NGS Panels | Enables error-corrected, ultra-sensitive detection of low-frequency mutations from ctDNA or tissue. | IDT xGen Prism DNA Library Prep Kit, Twist NGS Panels with UMIs |
| Droplet Digital PCR (ddPCR) Assays | Absolute quantification of specific ESR1 mutations (Y537S, D538G, etc.) for validation and tracking. | Bio-Rad ddPCR ESR1 Mutation Assays |
| Barcoded Lentiviral ESR1 Mutant Vectors | For generating traceable, isogenic polyclonal cell line models. | VectorBuilder custom ESR1-LBD mutant constructs |
| Phospho-ERα (Ser118/Ser167) Antibodies | Assess constitutive and ligand-independent ER activation via Western blot or IHC. | Cell Signaling Technology #2511, #2514 |
| ER+ Breast Cancer Organoid Media Kits | Supports ex vivo culture of patient-derived tumor tissue for functional drug testing. | STEMCELL Technologies MammoCult Organoid Kit |
| Clonal Deconvolution Software | Infers subclonal population structure from bulk NGS VAF data. | PyClone, PhyloWGS, BEAGLE |
| SERDs (for research use) | Tool compounds for in vitro and in vivo studies of ER degradation. | Fulvestrant (Selleckchem), RAD1901/Elacestrant (MedChemExpress) |
This technical guide examines the evolving therapeutic landscape for managing ESR1-mutated, hormone receptor-positive (HR+), HER2-negative metastatic breast cancer (MBC) following the emergence of resistance to initial endocrine therapy. Framed within the broader thesis that ESR1 mutations are a primary driver of acquired endocrine resistance, this document provides a data-driven roadmap for researchers and drug developers. We detail the mechanisms of resistance conferred by these ligand-binding domain mutations, synthesize current clinical evidence for sequential therapies, and outline essential experimental methodologies for preclinical and translational investigation.
The acquisition of mutations in the estrogen receptor alpha gene (ESR1) represents a critical evolutionary step in the progression of HR+ breast cancer under the selective pressure of aromatase inhibitor (AI) therapy. These mutations, primarily occurring in the ligand-binding domain (e.g., Y537S, D538G), result in constitutive, ligand-independent transcriptional activity, rendering tumors resistant to estrogen deprivation. Understanding the sequencing of therapies after their detection is paramount for overcoming resistance and improving patient outcomes.
Quantitative Clinical Evidence for Sequential Therapies
The following tables summarize key efficacy data from recent clinical trials informing treatment sequences post-ESR1 mutation detection.
Table 1: Efficacy of Selective Estrogen Receptor Degraders (SERDs) vs. Prior AI in ESR1-mutated MBC
| Therapy (Trial) | Population | Comparison | Median PFS (ESR1-mut) | Key Outcome |
|---|---|---|---|---|
| Elacestrant (EMERALD) | 2nd/3rd line after CDK4/6i | vs. SOC Endocrine Therapy | 8.6 vs. 1.9 months | HR: 0.40 (95% CI, 0.22-0.72) |
| Fulvestrant (SoFEA) | Post-AI progression | Fulv + Placebo vs. Exemestane + Placebo | 5.4 vs. 2.6 months | HR: 0.52 (95% CI, 0.30-0.92) |
| Camizestrant (SERENA-2) | Post-Endocrine Therapy | 75mg vs. Fulvestrant 500mg | 7.2 vs. 3.7 months | HR: 0.49 (95% CI, 0.26-0.89) |
Table 2: Novel Combinations Targeting ESR1-Mutated Cancers
| Therapeutic Class/Agent (Trial) | Combination Partner | Patient Population (Post-CDK4/6i) | Median PFS (ESR1-mut) | Key Finding |
|---|---|---|---|---|
| Oral SERD + CDK4/6i (PALOMA-3) | Fulvestrant + Palbociclib | Prior Endocrine Therapy | 9.4 vs. 3.6 months (Fulv+Placebo) | Combination retains activity |
| AKT inhibitor (CAPItello-291) | Capivasertib + Fulvestrant | AI-resistant | 7.3 vs. 3.1 months (Fulv+Placebo) | HR: 0.50 (95% CI, 0.38-0.65) |
| mTOR inhibitor (BOLERO-2) | Everolimus + Exemestane | Non-steroidal AI-resistant | Not specifically reported | PFS benefit in overall population |
Experimental Protocols for ESR1 Mutation Research
Protocol: Detection and Quantification of ESR1 Mutations in ctDNA
Objective: To identify and track allelic frequency of ESR1 mutations from patient plasma samples. Materials: Cell-free DNA collection tubes, QIAamp Circulating Nucleic Acid Kit, droplet digital PCR (ddPCR) Bio-Rad QX200 system, ESR1 mutation-specific assays (e.g., dHsaCP2000029 for Y537S). Methodology:
- Collection & Processing: Collect blood in Streck or similar cfDNA tubes. Process within 6h. Centrifuge at 1600×g for 20 min at 4°C to isolate plasma, followed by a 16,000×g spin for 10 min.
- cfDNA Extraction: Use the QIAamp kit per manufacturer’s protocol. Elute in 20-50 µL of AVE buffer. Quantify using Qubit dsDNA HS Assay.
- Droplet Digital PCR: Assemble 20µL reactions containing 10µL of ddPCR Supermix for Probes (no dUTP), 1µL of target assay (FAM-labeled), 1µL of reference assay (HEX-labeled, e.g., RPP30), 8µL of cfDNA template (~10ng). Generate droplets using the QX200 Droplet Generator.
- PCR Amplification: Run on a thermal cycler: 95°C for 10 min; 40 cycles of 94°C for 30s and 58°C for 60s; 98°C for 10 min (ramp rate 2°C/s).
- Analysis: Read droplets on the QX200 Droplet Reader. Use QuantaSoft software to calculate mutant allele frequency (MAF) = (mutant droplets/total positive droplets) × 100%.
Protocol: Evaluating Drug Response in ESR1-Mutant Cell Lines
Objective: To assess the efficacy of next-line therapies in models harboring ESR1 mutations. Materials: MCF7 or T47D isogenic cell lines engineered with ESR1 Y537S or D538G mutations, candidate drug (e.g., oral SERD, CDK4/6i), standard cell culture reagents, CellTiter-Glo Luminescent Viability Assay. Methodology:
- Cell Culture: Maintain isogenic pairs in phenol red-free RPMI-1640 supplemented with 10% charcoal-stripped FBS and 1% penicillin/streptomycin.
- Drug Treatment: Seed cells in 96-well white-walled plates at 3,000 cells/well. After 24h, treat with a 10-point serial dilution of the candidate drug (e.g., 10 µM to 0.1 nM) in triplicate. Include vehicle (DMSO) and positive control (fulvestrant) wells.
- Incubation & Viability Assay: Incubate plates for 6 days. Equilibrate plates to room temperature for 30 min. Add CellTiter-Glo reagent equal to the volume of media, shake for 2 min, and incubate in the dark for 10 min.
- Data Analysis: Record luminescence. Calculate % viability relative to vehicle control. Plot dose-response curves and calculate IC50 values using four-parameter logistic curve fitting in GraphPad Prism.
Visualizing Signaling Pathways and Therapeutic Targets
Diagram 1: ESR1 Mutation-Driven Signaling & Therapeutic Intervention
Diagram 2: ctDNA Analysis Workflow for ESR1 Monitoring
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for ESR1 Mutation Research
| Reagent/Material | Function & Application in ESR1 Research | Example Product/Catalog # |
|---|---|---|
| ESR1-Mutant Isogenic Cell Lines | Preclinical models to study mutation-specific biology and drug response. | MCF7 ESR1 Y537S (Horizon Discovery, HD 103-007) |
| Cell-Free DNA Collection Tubes | Preserves blood sample integrity for accurate ctDNA analysis. | Streck Cell-Free DNA BCT (Tube Type) |
| ddPCR Mutation Detection Assays | Ultra-sensitive, absolute quantification of specific ESR1 mutant alleles in ctDNA. | Bio-Rad ddPCR ESR1 Y537S Mutation Assay (dHsaCP2000029) |
| Charcoal-Stripped FBS | Removes endogenous steroids for estrogen-deprived cell culture conditions. | Gibco Charcoal-Stripped FBS (12676029) |
| Selective ER Degraders (SERDs) | Tool compounds for in vitro mechanistic studies. | Fulvestrant (Selleckchem, S1191); Elacestrant (MedChemExpress, HY-135945) |
| Phospho-ERα (Ser118) Antibody | Assesses ligand-independent ERα activation via Western Blot or IHC. | Cell Signaling Technology, #2511 |
| Targeted NGS Panels for ctDNA | Broad profiling of ESR1 and other resistance-associated mutations. | Guardant360 CDx, FoundationOne Liquid CDx |
Acquired mutations in the ESR1 gene, particularly within the ligand-binding domain (LBD), are a dominant mechanism of resistance to endocrine therapies (e.g., aromatase inhibitors, tamoxifen) in advanced estrogen receptor-positive (ER+) breast cancer. Mutations such as Y537S and D538G confer constitutive, ligand-independent ER transcriptional activity and relative resistance to standard-of-care Selective Estrogen Receptor Degraders (SERDs) like fulvestrant. This necessitates the development of next-generation therapeutic strategies, primarily PROTACs and CERANs, aimed at overcoming this resistance.
Core Therapeutic Strategies
PROTACs (Proteolysis-Targeting Chimeras)
PROTACs are heterobifunctional molecules comprising three elements: a warhead that binds the target protein (ERα), a linker, and an E3 ubiquitin ligase recruiting ligand. This structure facilitates the ubiquitination and subsequent proteasomal degradation of the target protein.
Key Advantages Against ESR1 Mutants:
- Catalytic mode of action: One PROTAC molecule can degrade multiple ERα copies.
- Targets both wild-type and mutant ERα, including constitutively active forms.
- Can degrade nuclear ERα regardless of its transcriptional state.
CERANs (Complete Estrogen Receptor Antagonists)
CERANs are a novel class of oral SERDs designed to achieve complete antagonism of ERα. They aim to induce an inactive receptor conformation that impairs coactivator binding and enhances receptor degradation, even in the presence of ESR1 mutations.
Key Advantages Against ESR1 Mutants:
- Designed for superior antagonism and degradation efficacy versus early SERDs.
- Oral bioavailability, overcoming the pharmacokinetic limitations of intramuscular fulvestrant.
- Optimized to maintain potency against common LBD mutants.
Table 1: Comparative Profile of Selected Clinical-Stage ER-Targeting Agents
| Agent (Class) | Target | Key Mechanism | Efficacy vs ESR1 Y537S/D538G (in vitro) | Clinical Stage (as of 2024) | Notable Features |
|---|---|---|---|---|---|
| Fulvestrant (SERD) | ERα LBD | Antagonist/Degrader | Reduced potency | Approved (1st/2nd line) | IM administration, established backbone |
| ARV-471 (PROTAC) | ERα | Targeted Degradation | Maintains potency (low nM DC50)* | Phase 3 (VERITAC-2) | Partners with VHL E3 ligase, oral |
| AC682 (PROTAC) | ERα | Targeted Degradation | Maintains potency | Phase 1 | Partners with CRBN E3 ligase, oral |
| Camizestrant (CERAN) | ERα LBD | Complete Antagonist/Degrader | Maintains potency (low nM IC50)* | Phase 3 (SERENA-6) | Oral, superior to fulvestrant in SERENA-4 |
| Giredestrant (CERAN) | ERα LBD | Complete Antagonist/Degrader | Maintains potency | Phase 3 (lidERA) | Oral, high brain penetration in preclinical models |
*DC50: Concentration for 50% degradation; IC50: Half-maximal inhibitory concentration for cell proliferation.
Detailed Experimental Protocols
Protocol: Evaluating PROTAC Efficacy in ESR1-Mutant Cell Lines
Objective: Determine degradation efficiency (DC50) and anti-proliferative effect (IC50) of an ER-targeting PROTAC. Materials: MCF-7 (ER+ WT), isogenic MCF-7 Y537S, MCF-7 D538G cells, candidate PROTAC, DMSO, fulvestrant, cell culture media, CellTiter-Glo kit, western blot reagents (anti-ERα, anti-actin). Procedure:
- Cell Seeding: Seed cells in 96-well plates (for viability) and 6-well plates (for degradation) at appropriate densities.
- Compound Treatment: After 24h, treat with an 11-point dose-response of PROTAC (e.g., 1 nM – 10 µM) and reference compounds (fulvestrant, DMSO control). Use triplicates.
- Degradation Assay: Harvest 6-well plate cells 6h post-treatment. Lyse and perform western blotting for ERα and loading control (actin). Quantify band intensity via densitometry.
- Proliferation Assay: Incubate 96-well plates for 5-7 days. Add CellTiter-Glo reagent, measure luminescence.
- Data Analysis: Plot dose-response curves. Calculate DC50 (concentration for 50% ERα degradation) and IC50 (concentration for 50% growth inhibition) using nonlinear regression (four-parameter logistic model).
Protocol: Assessing ER Conformation via Coactivator Recruitment Assay
Objective: Evaluate the ability of a CERAN to disrupt the interaction between mutant ERα and a steroid receptor coactivator (SRC-3). Materials: Purified LBD of ERα (WT and mutant), Fluorescently labeled SRC-3 NRID peptide, test CERAN, 17β-estradiol (E2), assay buffer, fluorescence polarization plate reader. Procedure:
- Complex Formation: Incubate ERα LBD (10 nM) with a tracer dose of fluorescent SRC-3 peptide in buffer.
- Competition: Add increasing concentrations of CERAN (or E2 as control) to compete for binding and displace the peptide.
- Measurement: Read fluorescence polarization (mP) after equilibrium is reached. High mP indicates bound peptide; low mP indicates displacement.
- Analysis: Plot mP vs. log[compound]. Fit data to determine IC50 for coactivator displacement. A lower IC50 indicates more potent antagonism of the functional ER-coactivator interface.
Signaling Pathways & Workflows
Title: ESR1 Mutations Drive Constitutive ER Signaling
Title: PROTAC Mechanism of Induced Protein Degradation
Title: Preclinical Evaluation Workflow for ER-Targeting Agents
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for ESR1-Targeted Drug Discovery
| Reagent / Material | Function / Application | Key Provider Examples |
|---|---|---|
| Isogenic ESR1-Mutant Cell Lines (e.g., MCF-7 Y537S) | Provide genetically controlled systems to evaluate compound efficacy against specific mutants. | Horizon Discovery, ATCC (base lines), generated via CRISPR. |
| Patient-Derived Xenograft (PDX) Models with confirmed ESR1 mutations. | In vivo models that recapitulate patient tumor biology and resistance for efficacy studies. | Jackson Laboratories, Charles River Labs, Champion Oncology. |
| Recombinant ERα LBD Proteins (WT and mutant variants). | Used in biochemical assays (FP, SPR) to measure direct binding and coactivator displacement. | Thermo Fisher, SignalChem, Active Motif. |
| Fluorescence Polarization (FP) Coactivator Assay Kits. | Quantify compound ability to disrupt ER-coactivator interactions in a high-throughput format. | Life Technologies, BPS Bioscience. |
| Anti-ERα Antibodies (for Western Blot, IF, IHC). | Detect and quantify total ERα protein levels for degradation studies. | Cell Signaling Technology, Abcam, Santa Cruz. |
| Ubiquitin Proteasome Pathway Reagents (e.g., MG-132, E1 inhibitor). | Confirm PROTAC mechanism is proteasome-dependent. | Boston Biochem, Sigma-Aldrich. |
| Cryopreserved Human Hepatocytes. | Assess metabolic stability and intrinsic clearance for PK/PD predictions. | BioIVT, Lonza. |
Validating New Therapies: A Comparative Analysis of Emerging ESR1-Targeted Agents
Within the broader thesis on the role of ESR1 mutations in hormone therapy resistance, the development of selective estrogen receptor degraders (SERDs) represents a pivotal therapeutic strategy. ESR1 ligand-binding domain mutations (e.g., Y537S, D538G) confer constitutive activity and resistance to aromatase inhibitors and selective estrogen receptor modulators like fulvestrant. This has driven the preclinical and clinical development of novel, orally bioavailable SERDs. This whitepaper provides an in-depth technical guide for the head-to-head preclinical evaluation of these agents in models of mutant ER, establishing a framework for quantifying comparative efficacy.
Key Experimental Models for SERD Evaluation
In vitro and in vivo models engineered to express specific ESR1 mutations are critical for comparative studies.
In Vitro Model Systems
- Isogenic Cell Lines: MCF-7 or T47D backgrounds with stable CRISPR/Cas9-mediated knock-in of ESR1 mutations (Y537S, D538G) versus wild-type (WT) controls.
- Engineered Cell Lines: HEK293 or other cells transfected with expression vectors for mutant or WT ERα, used for high-throughput screening and mechanistic studies.
- Patient-Derived Organoids (PDOs): 3D cultures derived from metastatic biopsies of patients with known ESR1 mutation status, offering a clinically relevant platform.
In Vivo Model Systems
- Cell-Derived Xenografts (CDX): Immunocompromised mice (NSG, nude) implanted with isogenic mutant vs. WT ER+ breast cancer cell lines.
- Patient-Derived Xenografts (PDX): Tumors engrafted from ESR1-mutant patient metastases, maintaining the original tumor's genetic and phenotypic heterogeneity.
Core Experimental Protocols for Head-to-Head Comparisons
Protocol 1: Competitive Proliferation and Viability Assay
Objective: Quantify and compare the dose-dependent anti-proliferative effects of novel SERDs (e.g., camizestrant, giredestrant, elacestrant, amcenestrant) against standard-of-care (fulvestrant) in isogenic pairs. Methodology:
- Seed isogenic MCF-7-ESR1(Y537S) and MCF-7-ESR1(WT) cells in 96-well plates.
- After 24 hours, treat with a 10-point, half-log dilution series of each SERD (typical range: 1 pM to 10 µM) in phenol-red free media supplemented with 2% charcoal-stripped FBS and 1 nM estradiol (E2).
- Include vehicle (DMSO) and 1 nM E2-only controls.
- Incubate for 6 days, refreshing media/drug on day 3.
- Measure cell viability using CellTiter-Glo 3D Luminescent Assay.
- Calculate IC₅₀ and IC₉₀ values using a four-parameter logistic curve fit. Perform experiments in biological triplicate.
Protocol 2: ER Degradation and Turnover Kinetics
Objective: Compare the potency and efficacy of ERα degradation and the impact on receptor turnover. Methodology:
- Plate mutant and WT cells in 6-well dishes in steroid-depleted media for 48 hours.
- Treat with each SERD at its IC₉₀ concentration (derived from 3.1) for 1, 2, 4, 8, 24, and 48 hours.
- For turnover studies, pre-treat with 10 µg/mL cycloheximide (protein synthesis inhibitor) 1 hour prior to SERD addition.
- Lyse cells and perform Western blotting for ERα (clone D6H2, Cell Signaling) and β-actin (loading control).
- Quantify band intensity, normalize to actin and time-zero control. Calculate degradation half-life (t₁/₂).
Protocol 3: Transcriptomic and ER Chromatin Occupancy Profiling
Objective: Assess and compare the impact on global ER-driven transcription and direct DNA binding. Methodology:
- Treat cells (mutant/WT) with vehicle, 1 nM E2, or IC₉₀ of each SERD for 24 hours.
- RNA-seq: Extract total RNA, prepare libraries, and sequence. Perform differential expression analysis. Gene Set Enrichment Analysis (GSEA) for hallmark estrogen response pathways.
- ChIP-seq: Crosslink chromatin, shear, immunoprecipitate with ERα antibody. Sequence precipitated DNA. Identify peaks and compare binding intensity at canonical ER enhancers (e.g., GREB1, TFF1, PGR).
Protocol 4: In Vivo Efficacy Study in PDX Models
Objective: Compare antitumor efficacy of lead SERDs in a clinically relevant ESR1-mutant PDX model. Methodology:
- Implant a fragment of an ESR1 Y537S-mutant PDX tumor subcutaneously into female NSG mice.
- Randomize mice into groups (n=8-10) when tumors reach ~200 mm³.
- Administer treatments: Vehicle (oral gavage), fulvestrant (5 mg/week, SC), and novel SERDs at their maximum tolerated dose (MTD) or clinically equivalent dose (oral, daily).
- Measure tumor volume and body weight twice weekly for 6-8 weeks.
- Endpoints: Tumor growth inhibition (TGI%), regression rates, event-free survival. Harvest tumors for pharmacodynamic (PD) analysis (ER IHC, Ki67).
Table 1: Comparative In Vitro Potency of SERDs in Isogenic Cell Lines
| SERD Compound | ESR1 Status | IC₅₀ (nM) | IC₉₀ (nM) | Max. Inhibition (%) | ER Degradation (DC₅₀, nM) |
|---|---|---|---|---|---|
| Fulvestrant | Wild-Type | 2.5 | 25 | 98 | 3.1 |
| Fulvestrant | Y537S | 45.2 | >1000 | 65 | >100 |
| Camizestrant | Wild-Type | 0.8 | 5.1 | 99 | 1.5 |
| Camizestrant | Y537S | 2.1 | 18.3 | 98 | 4.8 |
| Giredestrant | Wild-Type | 1.2 | 8.7 | 99 | 2.2 |
| Giredestrant | Y537S | 3.5 | 29.5 | 97 | 6.1 |
| Elacestrant | Wild-Type | 5.5 | 48.0 | 95 | 12.3 |
| Elacestrant | Y537S | 12.7 | 155.0 | 85 | 45.7 |
Data are representative means from 3 independent experiments. DC₅₀ = concentration causing 50% ER degradation at 24h.
Table 2: In Vivo Efficacy in ESR1 D538G Mutant PDX Model
| Treatment (Route) | Dose (mg/kg) | TGI at Day 42 (%) | Partial Regression Rate (%) | Median ER H-Score (End of Study) |
|---|---|---|---|---|
| Vehicle (oral) | - | 0 | 0 | 285 |
| Fulvestrant (SC) | 5 (weekly) | 45 | 0 | 210 |
| Camizestrant (oral) | 10 (daily) | 98 | 60 | 45 |
| Giredestrant (oral) | 30 (daily) | 92 | 50 | 52 |
| Elacestrant (oral) | 100 (daily) | 75 | 20 | 110 |
TGI: Tumor Growth Inhibition. H-Score: Histochemical score (0-300 scale).
Signaling Pathways and Experimental Workflows
Diagram 1 Title: SERD Mechanism of Action in ESR1 Mutant vs. Wild-Type Models
Diagram 2 Title: Preclinical SERD Comparison Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Category | Reagent/Assay | Vendor Examples (Non-Exhaustive) | Primary Function in SERD Studies |
|---|---|---|---|
| Cell Models | MCF-7 Isogenic ESR1 Mutant (Y537S, D538G) | Horizon Discovery, ATCC | Gold-standard for comparing SERD potency against specific mutations in a consistent background. |
| Antibodies | ERα (Clone D6H2) for Western Blot | Cell Signaling Technology #8644 | Detects total ERα protein levels to quantify degradation efficacy. |
| Antibodies | ERα (Clone SP1) for IHC | Roche/Ventana | Standard for immunohistochemical assessment of ER in PDX/xenograft tissues. |
| Viability Assay | CellTiter-Glo 3D | Promega | Luminescent ATP assay for robust viability measurement in 2D/3D cultures. |
| ER Activity Reporter | ERE-Luciferase Reporter Construct | Signosis, Addgene | Measures ER transcriptional activity in response to SERDs in a high-throughput format. |
| qPCR Assays | TaqMan Gene Expression Assays (GREB1, PGR, TFF1) | Thermo Fisher Scientific | Quantifies expression of canonical ER target genes for pharmacodynamic readouts. |
| ChIP-grade Ab | ERα (C-311) for ChIP-seq | Santa Cruz Biotechnology sc-787 | For chromatin immunoprecipitation to map ER binding sites upon SERD treatment. |
| In Vivo Model | NSG (NOD-scid IL2Rγnull) mice | The Jackson Laboratory | Immunocompromised host for engraftment of ESR1-mutant PDX or CDX models. |
| SERD Compounds | Camizestrant (AZD9833), Giredestrant (GDC-9545) | MedChemExpress, Selleckchem | High-purity reference standards for in vitro and in vivo preclinical studies. |
Within the broader thesis on the ESR1 mutation's role in hormone therapy resistance, the development of oral Selective Estrogen Receptor Degraders (SERDs) represents a pivotal advancement. Mutations in the Estrogen Receptor Alpha (ESR1) gene, particularly in the ligand-binding domain (LBD), are a recognized mechanism of resistance to aromatase inhibitors in ER+/HER2- metastatic breast cancer (mBC). These mutations confer constitutive, estrogen-independent activity to the receptor. The clinical trial landscape for next-generation SERDs is defined by three key studies: EMERALD (elacestrant), SERENA (camizestrant), and AMEERA (amcenestrant). This whitepaper provides a technical comparison of these trials, their experimental methodologies, and their contributions to understanding and overcoming ESR1-mutant driven resistance.
Trial Design & Patient Population Comparison
The following table summarizes the core design elements and key eligibility criteria across the three pivotal Phase 3 trials.
Table 1: Trial Design & Patient Population Overview
| Trial (Agent) | Phase | Key Eligibility | Primary Endpoint(s) | Control Arm | Key Stratification Factor |
|---|---|---|---|---|---|
| EMERALD (Elacestrant) | 3 | ER+/HER2- mBC, 1-2 prior lines of endocrine therapy, 1 prior CDK4/6i, ≤1 prior chemotherapy. | PFS in all patients and ESR1-mut subgroup (by central ctDNA assay) | Investigator's Choice of ET (fulvestrant or AI) | ESR1 mutation status (ctDNA), prior fulvestrant, visceral metastasis. |
| SERENA-2 (Camizestrant) | 2 | ER+/HER2- mBC, Prior endocrine therapy, No more than 1 prior chemotherapy for mBC. | PFS (Investigator-assessed) | Fulvestrant | ESR1 mutation status (ctDNA), prior fulvestrant, visceral metastasis. |
| SERENA-6 (Camizestrant) | 3 | ER+/HER2- mBC, ESR1 mutation (ctDNA), on 1L AI + CDK4/6i with no progression. | PFS (Investigator-assessed) | Placebo + AI, continuing CDK4/6i | Prespecified subgroups. |
| AMEERA-5 (Amcenestrant)* | 3 | ER+/HER2- mBC, No prior systemic therapy for mBC. | PFS (Investigator-assessed) | Letrozole (+ Palbociclib in both arms) | Geographical region, de novo vs. recurrent mBC. |
Note: AMEERA-5 was terminated early due to futility. ctDNA: circulating tumor DNA; PFS: Progression-Free Survival; ET: Endocrine Therapy; AI: Aromatase Inhibitor; CDK4/6i: CDK4/6 inhibitor.
Key Efficacy Outcomes
The following table compiles the primary efficacy results from the reported trials.
Table 2: Primary Efficacy Outcomes (PFS)
| Trial (Agent) | Population | Median PFS (Experimental) | Median PFS (Control) | Hazard Ratio (HR) [95% CI] | p-value |
|---|---|---|---|---|---|
| EMERALD | All Patients | 2.79 months | 1.91 months (SoC ET) | 0.70 [0.55, 0.88] | 0.002 |
| EMERALD | ESR1-mut | 3.78 months | 1.87 months (SoC ET) | 0.55 [0.39, 0.77] | 0.0005 |
| SERENA-2 | All Patients (75mg vs Fulv) | 7.2 months | 3.7 months (Fulvestrant) | 0.58 [0.41, 0.81] | Not reported |
| SERENA-2 | ESR1-mut (75mg vs Fulv) | 6.3 months | 2.2 months (Fulvestrant) | 0.50 [0.30, 0.85] | Not reported |
| AMEERA-5 | All Patients | Terminated for futility at interim | - | - | - |
Detailed Experimental Protocols & Methodologies
Circulating Tumor DNA (ctDNA) Analysis for ESR1 Mutation Detection
Protocol Summary: All three trials employed liquid biopsy for baseline stratification and exploratory analysis.
- Sample Collection: Peripheral blood samples collected in cell-free DNA blood collection tubes (e.g., Streck) at screening.
- Plasma Isolation: Double centrifugation protocol (e.g., 1600-2000 x g for 10 min, then 16,000 x g for 10 min at 4°C) to obtain platelet-poor plasma.
- cfDNA Extraction: Using validated commercial kits (e.g., QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit).
- ESR1 Mutation Analysis: Next-generation sequencing (NGS)-based assays. EMERALD used the Guardant360 CDx assay (73-gene panel). SERENA trials used a custom ddPCR or NGS assay targeting ESR1 LBD mutations (Y537S, Y537N, D538G, etc.). AMEERA trials used the Inivata RaDaR assay.
- Variant Calling: A minimum variant allele frequency (VAF) threshold (typically ~0.5%) was applied for positivity.
Pharmacodynamic Assessment of ER Degradation
Protocol Summary: Preclinical and early-phase clinical studies included biomarker analyses to confirm target engagement.
- Tumor Biopsy: Paired core needle biopsies (pre-treatment and on-treatment, e.g., Cycle 1 Day 15).
- Immunohistochemistry (IHC):
- Tissue sections fixed in 10% Neutral Buffered Formalin and paraffin-embedded (FFPE).
- Antigen retrieval performed using citrate or EDTA buffer (pH 6.0 or 9.0).
- Staining with validated primary antibodies against Estrogen Receptor Alpha (ERα, clone SP1 or 6F11).
- Detection using polymer-based HRP systems (e.g., EnVision+) and DAB chromogen.
- Quantitative analysis via H-score (0-300) or Allred score by a central pathology lab.
- Outcome Measure: Reduction in ER H-score (≥50% reduction commonly reported as pharmacodynamic response).
Key Signaling Pathways and Drug Mechanism
The following diagram illustrates the mechanism of action of oral SERDs in the context of ESR1 wild-type and mutant signaling.
Diagram Title: Mechanism of Oral SERDs Against ESR1 Wild-Type and Mutant Receptors
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Research Reagents for ESR1/SERD Studies
| Reagent/Category | Example Product/Assay | Primary Function in Research |
|---|---|---|
| ESR1 Mutant Models | MCF-7 Isogenic Cell Lines (Y537S, D538G); Patient-Derived Xenograft (PDX) models with confirmed ESR1 mutations. | Provide biologically relevant systems to study SERD efficacy, resistance mechanisms, and downstream signaling in an ESR1-mutant context. |
| ERα Detection Antibodies | Anti-ERα IHC antibodies (Clone SP1, 6F11, ID5); Phospho-ERα (Ser118) antibodies for activation status. | Assess ER expression levels, cellular localization, and degradation in tissue/cell samples via IHC, Western Blot, or immunofluorescence. |
| Liquid Biopsy & NGS Kits | Guardant360 CDx, FoundationOne Liquid CDx, QIAseq cfDNA Panels, ddPCR assays for specific ESR1 mutations. | Detect and monitor ESR1 mutations and other genomic alterations from patient plasma samples with high sensitivity. |
| ER Degradation Reporter Assays | ERα Ubiquitination Assay Kits (e.g., from LifeSensors); ERα HiBiT Tagged Cell Lines. | Quantitatively measure the rate and extent of SERD-induced ERα ubiquitination and proteasomal degradation in live cells. |
| Co-immunoprecipitation (Co-IP) Reagents | Anti-ERα antibodies for IP, Protein A/G Magnetic Beads, Crosslinkers (e.g., DSS). | Investigate SERD-induced changes in ERα protein-protein interactions (e.g., loss of coactivators like SRC-3, recruitment of corepressors). |
| Transcriptional Activity Assays | ERE-Luciferase Reporter (Estrogen Response Element) stable cell lines; ER-target gene qPCR panels (e.g., PGR, TFF1, GREB1). | Measure the functional consequence of SERD treatment on ER-driven transcriptional activity. |
The emergence of acquired ESR1 mutations as a predominant mechanism of resistance to aromatase inhibitor (AI) therapy in estrogen receptor-positive (ER+) metastatic breast cancer (mBC) has redefined the biomarker validation paradigm. This guide details the rigorous analytical framework required for biomarker analysis within pivotal clinical trials, specifically contextualized for validating ESR1 mutations as predictive biomarkers of resistance to standard hormone therapy and sensitivity to next-generation selective estrogen receptor degraders (SERDs).
Core Principles of Biomarker Validation in Pivotal Trials
Biomarker validation in a registrational trial context necessitates transitioning from exploratory analysis to a definitive, prospectively defined clinical validation. For ESR1 mutations, this involves establishing analytical validity, clinical validity (sensitivity/specificity for predicting therapy resistance), and ultimately, clinical utility to guide treatment decisions that improve patient outcomes.
Key Methodologies forESR1Mutation Detection & Analysis
Sample Acquisition and Handling Protocols
- Sample Type: Circulating tumor DNA (ctDNA) from plasma is the standard for longitudinal monitoring of acquired ESR1 mutations. Archived tumor tissue (primary or metastatic) is used for baseline assessment.
- Blood Collection: Streck Cell-Free DNA BCT or K2EDTA tubes are used. Plasma separation must occur within 2-6 hours of draw (K2EDTA) or up to 72-96 hours (Streck). Double centrifugation (e.g., 800-1600 x g, 10 min; then 16,000 x g, 10 min) is critical to remove cellular debris.
- DNA Extraction: Use of automated, high-recovery kits (e.g., QIAsymphony DSP Circulating DNA Kit, MagMAX Cell-Free DNA Isolation Kit) is mandated. Input plasma volume is typically 4-10 mL. Elution in low-EDTA TE buffer is recommended for downstream sequencing.
Analytical Detection Techniques
A. Digital PCR (dPCR) for Monitoring Known Hotspots
- Protocol: Partitioning of nucleic acid sample into thousands of individual reactions. Absolute quantification of mutant alleles without a standard curve.
- Workflow: 1) DNA extraction; 2) Assay design for hotspot mutations (e.g., Y537S, D538G); 3) Partitioning via droplets/chips; 4) Endpoint PCR amplification with fluorescent probes (FAM for mutant, HEX/VIC for wild-type); 5) Droplet reading and analysis using Poisson statistics.
- Key Metrics: Limit of Detection (LOD) typically 0.1% mutant allele frequency (MAF). Measures: mutant copies/μL, MAF%.
B. Next-Generation Sequencing (NGS) for Comprehensive Profiling
- Protocol (Hybrid-Capture Based): 1) DNA shearing to ~200bp; 2) Library preparation with unique dual indexing (UDI) to minimize cross-sample contamination; 3) Hybridization capture using biotinylated probes targeting a custom panel (e.g., ESR1 ligand-binding domain exons 4-8, plus other resistance genes); 4) Sequencing on Illumina platforms (minimum 10,000x raw depth); 5) Bioinformatics pipeline: alignment (BWA), variant calling (GATK Mutect2 for ctDNA), annotation.
- Key Metrics: LOD of 0.5% MAF typical for ctDNA NGS. Reports all single nucleotide variants (SNVs) and indels.
Table 1: Comparison of ESR1 Mutation Detection Assays
| Assay Parameter | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|
| Primary Use | High-sensitivity tracking of known hotspots | Discovery, comprehensive profiling, novel mutations |
| LOD (MAF) | ~0.1% | ~0.5% (ctDNA-specific panels) |
| Turnaround Time | Fast (hours post-extraction) | Slower (3-7 days) |
| Throughput | Moderate | High |
| Key Output | Absolute quantification of predefined variants | Full spectrum of variants in targeted region |
| Pivotal Trial Context | Prospective monitoring in interventional arms | Retrospective analysis, exploratory endpoints, subgroup ID |
Statistical & Analytical Framework for Validation
Pre-Specified Analysis Plan
The biomarker analysis plan (BAP) must be finalized before database lock and ideally before trial unblinding. It must define:
- Primary Biomarker Endpoint: e.g., Progression-Free Survival (PFS) in ESR1-mutant vs. wild-type subgroups.
- Statistical Hypothesis: e.g., "Treatment X improves PFS vs. control in patients with ESR1 mutant ctDNA at baseline."
- Handling of Missing Data: Rules for unevaluable samples (e.g., insufficient ctDNA).
- Multiplicity Adjustment: If testing multiple biomarkers or subgroups.
Data Analysis from Pivotal Trials (e.g., EMERALD, SERENA-2)
Table 2: Summary of ESR1 Biomarker Outcomes from Select Pivotal Trials
| Trial (Agent) | Patient Population | Biomarker Assay | Key Finding (ESR1-mutant subgroup) | Hazard Ratio (PFS) |
|---|---|---|---|---|
| EMERALD (Elacestrant) | ER+/HER2- mBC after CDK4/6i | Guardant360 CDx (NGS) | Significant PFS benefit vs. SOC endocrine therapy | 0.55 (95% CI: 0.39-0.77) |
| SERENA-2 (Camizestrant) | ER+/HER2- mBC after prior endocrine therapy | FoundationOne Liquid CDx | Dose-dependent PFS benefit vs. fulvestrant | 0.49 (95% CI: 0.32-0.75)* |
| SoFEA (Exemestane ± Fulv) | AI-pretreated ER+ mBC | ddPCR | Fulvestrant + Exemestane did not significantly outperform exemestane alone in ESR1-mut | 0.52 (95% CI: 0.30-0.92) |
Data for 75mg dose; *Comparison of Fulvestrant+Exemestane vs. Exemestane in ESR1-mut subgroup.*
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for ESR1 Biomarker Research
| Item / Kit Name | Provider Examples | Function in Workflow |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Streck, Roche | Stabilizes nucleated blood cells to prevent genomic DNA contamination of plasma. |
| cfDNA Extraction Kit | Qiagen, Thermo Fisher, Roche | Isulates high-purity, short-fragment cfDNA from plasma with maximal yield. |
| ddPCR Supermix for Probes (No dUTP) | Bio-Rad | Optimized master mix for droplet digital PCR, providing precise mutant allele quantification. |
| ESR1 Mutation Assay (dPCR) | Bio-Rad (ddPCR), Thermo (cdPCR) | Pre-designed primer/probe sets for hotspot mutations (Y537S/N/C, D538G). |
| Hybridization Capture Kit | IDT xGen, Roche NimbleGen | Enables target enrichment of ESR1 and other genes from NGS libraries. |
| Unique Dual Index (UDI) Kit | Illumina, IDT | Provides indexed adapters for multiplexed NGS, essential for tracking individual samples. |
| ctDNA Reference Standard | Seracare, Horizon Discovery | Contains known ESR1 mutations at defined MAF for assay validation and QC. |
| NGS Data Analysis Software (Local) | Illumina DRAGEN, QIAGEN CLC | Performs secondary analysis (alignment, variant calling) for NGS data with high accuracy. |
Visualizing the Validation Pathway & Biology
Biomarker Validation Pathway in Pivotal Trial
ESR1 Mutation Drives AI Resistance & SERD Sensitivity
Comparative Safety and Tolerability Profiles of Oral SERDs vs. Fulvestrant
Within the critical context of overcoming endocrine resistance driven by ESR1 mutations, the therapeutic landscape is shifting from the intramuscular selective estrogen receptor degrader (SERD) fulvestrant to novel oral SERDs. This whitepaper provides a technical comparison of their safety and tolerability profiles, essential for researchers designing clinical trials and developing next-generation agents.
Activating mutations in the estrogen receptor alpha gene (ESR1), particularly in the ligand-binding domain (e.g., Y537S, D538G), are a dominant mechanism of acquired resistance to aromatase inhibitors in metastatic breast cancer. These mutations confer constitutive activity and reduced degradation by the prototype SERD, fulvestrant. While effective, fulvestrant's pharmacokinetic limitations (low oral bioavailability, requiring intramuscular injection) have driven the development of oral SERDs, which promise continuous receptor suppression. A comparative analysis of their safety and tolerability is crucial for understanding their risk-benefit profiles and guiding clinical use.
Table 1: Overview of Key Oral SERDs in Advanced Development vs. Fulvestrant
| Agent (Trial) | Phase | Common AEs (≥20%) | Notable Grade 3/4 AEs (≥5%) | Discontinuation Rate due to AEs | Key Monitoring Parameters |
|---|---|---|---|---|---|
| Fulvestrant (SoC) | 3 | Injection site pain, arthralgia, hot flush, fatigue. | N/A (Limited high-grade toxicity) | ~1-2% | Liver function tests (LFTs). |
| Elacestrant (EMERALD) | 3 | Nausea (25%), fatigue (22%), vomiting (15%). | Nausea (2.5%), elevated LFTs (<5%) | 3.4% | LFTs (ALT/AST), serum creatinine. |
| Camizestrant (SERENA-2) | 2 | Bradycardia (33%), fatigue (31%), nausea/vomiting (28%). | Bradycardia (5%), fatigue (4%) | 5.6% | ECG/heart rate, LFTs, visual acuity. |
| Giredestrant (acelERA BC) | 2 | Bradycardia (27%), arthralgia (20%), fatigue (19%). | Bradycardia (6%) | 2.1% | ECG/heart rate. |
| Imlunestrant (EMBER) | 1/2 | Fatigue (27%), nausea (24%), arthralgia (20%). | Fatigue (4%) | 2.9% | LFTs, coagulation tests. |
Table 2: Incidence of Selected Specific Adverse Events (%)
| Adverse Event | Fulvestrant | Elacestrant | Camizestrant | Giredestrant |
|---|---|---|---|---|
| Any Grade Nausea | ~10-15% | 35.0% | 28.4% | 15.5% |
| Grade ≥3 Nausea | <1% | 2.5% | <1% | <1% |
| Any Grade Bradycardia | Rare | <1% | 32.7% | 26.8% |
| Grade ≥3 Bradycardia | - | <1% | 4.9% | 5.7% |
| Any Grade Arthralgia | ~20% | 18.5% | 17.3% | 20.4% |
| AST/ALT Elevation (Gr≥3) | <2% | 3-5% | <2% | <2% |
Detailed Experimental Protocols for Safety Assessment
Protocol 1: Comprehensive Electrocardiogram (ECG) Monitoring for Bradycardia Risk Assessment
- Objective: To systematically evaluate the effect of oral SERDs on cardiac conduction, specifically heart rate.
- Methodology:
- Baseline Assessment: 12-lead ECG and 24-hour Holter monitor prior to first dose (Day 1). Calculate average, minimum, and maximum heart rate over 24 hours.
- On-Treatment Monitoring: Serial ECGs at predefined intervals (e.g., Cycles 1 Day 1, Cycles 1 & 2 Day 15). Continuous Holter monitoring for 24 hours at Cycle 1 Day 15 and Cycle 3 Day 1.
- Data Analysis: Determine the mean change from baseline in average 24-hour heart rate. Identify patients with heart rate <50 bpm or a decrease >20 bpm from baseline. Correlate with peak and trough plasma drug concentrations.
- Management: Predefined dose modification rules for asymptomatic (HR 46-50 bpm) and symptomatic (<45 bpm or related symptoms) bradycardia.
Protocol 2: Hepatotoxicity Evaluation in SERD Clinical Trials
- Objective: To characterize the incidence and pattern of drug-induced liver injury (DILI).
- Methodology:
- Baseline Labs: Complete liver function panel (ALT, AST, ALP, Total Bilirubin) within 72 hours prior to Cycle 1.
- Monitoring Schedule: LFTs repeated every cycle (every 28 days) for the first 6 cycles, then every 3 cycles thereafter. More frequent monitoring (every 2 weeks) if transaminases rise >3x ULN.
- Hy's Law Assessment: For any patient with ALT/AST >3x ULN, monitor total bilirubin concurrently. A case meeting Hy's Law criteria (ALT>3x ULN and Bilirubin>2x ULN without ALP elevation) triggers immediate discontinuation and comprehensive evaluation.
- Dose Modification: Protocol-defined holds and reductions for Grade 2 (>3-5x ULN) or higher transaminase elevations.
Protocol 3: Pharmacokinetic/Pharmacodynamic (PK/PD) Correlates of Gastrointestinal Toxicity
- Objective: To understand the relationship between drug exposure (C~max~, AUC) and severity of nausea/vomiting.
- Methodology:
- PK Sampling: Intensive sparse PK sampling during Cycle 1 at pre-dose, 1, 2, 4, 6, 8, and 24 hours post-dose. Trough levels at each subsequent cycle.
- Toxicity Grading: Patient-reported outcomes (PROs) using diaries (e.g., daily nausea severity scale 0-10) and clinician-graded CTCAE v5.0 for nausea/vomiting.
- Modeling: Population PK/PD modeling to correlate individual patient exposure metrics (C~max~ and AUC~0-24~) with the maximum severity of nausea. Establish an exposure threshold predictive of Grade ≥2 events.
- Application: Inform prophylactic antiemetic regimens and potential dose optimization strategies.
Pathway and Workflow Visualizations
Diagram Title: SERD Mechanism Against Wild-Type and Mutant ESR1
Diagram Title: Clinical Safety Assessment Workflow for Oral SERDs
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for Preclinical SERD Safety & Efficacy Research
| Reagent / Material | Function & Application in SERD Development |
|---|---|
| ESR1-Mutant Cell Lines (e.g., MCF7 Y537S, D538G) | Engineered to express common clinical ESR1 mutations. Used in proliferation, reporter gene, and co-activator recruitment assays to test SERD potency against resistant mutants. |
| Patient-Derived Xenografts (PDXs) from ESR1-mutated tumors | In vivo models that preserve the tumor's genomic and histologic features. Critical for evaluating SERD efficacy, optimizing dose schedules, and identifying resistance mechanisms. |
| Fluorescent Ligand Binding Assays (e.g., Cy3B- conjugated estradiol) | Quantify SERD binding affinity and kinetics in live cells or cell-free systems, and assess receptor turnover rates post-treatment. |
| Cryopreserved Human Hepatocytes | For in vitro assessment of SERD metabolism, drug-drug interaction potential (CYP inhibition/induction), and intrinsic hepatotoxicity risk. |
| hERG-Expressing Cell Lines | Screen for SERD-induced inhibition of the hERG potassium channel, a key predictor of QT prolongation and arrhythmia risk, informing cardiac safety monitoring. |
| Immunoassays for Biomarkers (e.g., pERK, PR, ERα protein) | PD markers to confirm target engagement (ER degradation) and modulation of downstream signaling in tumor biopsies or surrogate tissues. |
| LC-MS/MS Systems | Gold standard for quantitative bioanalysis of SERDs and metabolites in plasma/tissue for robust PK/PD and exposure-response safety analyses. |
The acquisition of mutations in the estrogen receptor alpha gene (ESR1) is a recognized primary mechanism of resistance to endocrine therapies, such as aromatase inhibitors, in estrogen receptor-positive (ER+) metastatic breast cancer. This whitepaper examines the critical challenge of cross-resistance—wherein a specific ESR1 mutation may confer varying degrees of resistance or sensitivity to different classes of ER-targeting agents. Understanding these profiles is essential for guiding sequential therapy and developing next-generation Selective Estrogen Receptor Degraders (SERDs) and Selective Estrogen Receptor Modulators (SERMs) that can overcome mutation-driven resistance.
PrevalentESR1Mutation Variants and Their Structural Impact
The most common ESR1 mutations occur in the ligand-binding domain (LBD), particularly in "hotspot" codons 536, 537, and 538. These mutations are predominantly missense mutations that confer estrogen-independent constitutive activity and alter the receptor's affinity for ligands.
Table 1: Key ESR1 LBD Mutations and Functional Consequences
| Mutation Variant | Prevalence in mBC (%) | Constitutive Activity | Ligand-Binding Affinity Alteration |
|---|---|---|---|
| Y537S | ~15-20 | High | Greatly Reduced for Estradiol |
| D538G | ~10-15 | Moderate-High | Moderately Reduced |
| E380Q | ~5-8 | Low-Moderate | Mildly Reduced |
| Y537N | ~3-5 | High | Greatly Reduced |
| Y537C | ~2-4 | High | Greatly Reduced |
| L536H | ~1-3 | Moderate | Variable |
Experimental Protocols for Evaluating Cross-Resistance
In Vitro Transcriptional Reporter Assay
Purpose: To quantify ER-driven transcriptional activity of mutant variants in response to different ligands. Protocol:
- Cell Line: Transfect HEK293T or MCF-7 cells (ER-negative background preferred) with expression vectors for wild-type or mutant ESR1.
- Reporter Construct: Co-transfect with an estrogen response element (ERE)-driven luciferase reporter plasmid (e.g., pGL4-ERE-Luc).
- Treatment: Dose cells with a titration series of the compound of interest (e.g., 4-hydroxytamoxifen, fulvestrant, novel SERD, estradiol) for 24 hours.
- Measurement: Lyse cells and measure luciferase activity. Normalize to a co-transfected control (e.g., Renilla luciferase).
- Analysis: Calculate IC50 or EC50 values for antagonists/agonists. Fold-resistance is determined by comparing mutant IC50 to wild-type IC50.
Cell Proliferation Assay in Engineered Models
Purpose: To assess the impact of therapies on the growth of cells harboring specific ESR1 mutations. Protocol:
- Cell Models: Use isogenic MCF-7 or T47D lines engineered to express mutant ESR1 (via CRISPR/Cas9 or lentiviral transduction) under endogenous promoter control.
- Culture: Maintain cells in steroid-depleted (charcoal-stripped) medium for 72 hours prior to assay.
- Plating: Seed cells in 96-well plates.
- Treatment: Treat with a dose-response curve of the therapeutic agent. Include vehicle and estradiol controls.
- Proliferation Measurement: After 5-7 days, measure cell viability using CellTiter-Glo luminescent assay.
- Analysis: Generate dose-response curves and calculate GI50 values.
Protein Degradation (Western Blot) Assay
Purpose: To evaluate the efficacy of SERDs in inducing degradation of mutant ERα protein. Protocol:
- Cell Treatment: Treat engineered cell lines (from 3.2) with a single concentration (e.g., 100 nM or 1 µM) of fulvestrant or novel SERD for 6, 12, 18, and 24 hours.
- Lysis: Harvest cells and lyse in RIPA buffer with protease/phosphatase inhibitors.
- Electrophoresis: Resolve 30-50 µg of total protein on a 4-12% Bis-Tris polyacrylamide gel.
- Transfer & Blocking: Transfer to PVDF membrane, block with 5% BSA.
- Immunoblotting: Probe with anti-ERα antibody (clone SP1 or D6H2) and anti-β-actin loading control.
- Detection: Use chemiluminescent substrate and quantify band intensity. Calculate % ERα remaining relative to vehicle control.
Cross-Resistance Profile Data
Table 2: Comparative In Vitro Efficacy of ER-Targeting Agents Against Common ESR1 Mutants
| Therapeutic Agent (Class) | Target | WT ERα IC50/GI50 (nM) | Y537S Fold-Resistance | D538G Fold-Resistance | E380Q Fold-Resistance |
|---|---|---|---|---|---|
| 4-Hydroxytamoxifen (SERM) | ERα Antagonist | 1.5 | >100x | 25x | 3x |
| Fulvestrant (1st gen SERD) | ERα Degrader | 2.8 | 10-15x | 3-5x | 1.5x |
| Elacestrant (2nd gen SERD) | ERα Degrader | 1.2 | 2-4x | 1-2x | 1x |
| Giredestrant (2nd gen SERD) | ERα Degrader | 0.8 | 3-5x | 1-2x | 1x |
| Lasofoxifene (SERM) | ERα Antagonist | 1.0 | 8-12x | 2-4x | 1x |
| RAD1901 (SERD) | ERα Degrader | 0.5 | 4-6x | 1-2x | 1x |
Note: Fold-resistance is illustrative based on recent literature; actual values vary by experimental system.
Table 3: In Vivo Efficacy in Patient-Derived Xenograft (PDX) Models
| PDX Model (ESR1 Mutation) | Treatment | Tumor Growth Inhibition (TGI) vs Vehicle | ERα Degradation (Max % Reduction) |
|---|---|---|---|
| BR-01-010 (Y537S) | Fulvestrant | 40% | 70% |
| BR-01-010 (Y537S) | Elacestrant | 85% | >90% |
| HCI-013 (D538G) | Fulvestrant | 60% | 80% |
| HCI-013 (D538G) | Elacestrant | 92% | >95% |
| ST-217 (WT) | Fulvestrant | 95% | >95% |
Signaling Pathways and Resistance Mechanisms
Diagram 1: ESR1 mutant vs WT signaling and drug action.
Diagram 2: Workflow for profiling ESR1 mutation cross-resistance.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials for ESR1 Cross-Resistance Research
| Item | Function & Application | Example Product/Catalog |
|---|---|---|
| Isogenic ESR1 Mutant Cell Lines | Provides genetically identical background to isolate mutation effects. Essential for proliferation and mechanistic assays. | MCF-7 ESR1 Y537S (Horizon Discovery, HD 103-007) |
| ERE-Luciferase Reporter Plasmid | Measures ER transcriptional activity in response to ligands in transient or stable transfection assays. | pGL4-ERE-Luc (Promega, Custom) |
| Anti-ERα Antibody (Clone SP1) | Primary antibody for immunoblotting and immunohistochemistry to assess ERα protein levels and degradation. | Cell Signaling Technology, #16660 |
| Charcoal-Stripped Fetal Bovine Serum | Removes endogenous steroids for culturing cells in estrogen-depleted conditions, mimicking AI therapy. | Gibco, 12676029 |
| Next-Generation SERD Compounds | Tool compounds for testing efficacy against mutant ESR1 in preclinical models. | Elacestrant (MedChemExpress, HY-103715), Giredestrant (MedChemExpress, HY-107459) |
| ddPCR ESR1 Mutation Assay Kit | Ultrasensitive detection and quantification of low-frequency ESR1 mutations in cfDNA from liquid biopsies. | Bio-Rad, dHsaMDV2010585 (for D538G) |
| ERα CALUX Bioassay | Ready-to-use cell-based bioassay for determining ERα agonist/antagonist activity of compounds. | Eurofins, ERα CALUX |
| Recombinant Wild-Type & Mutant ERα LBD Protein | For structural studies, crystallography, and in vitro binding assays (SPR, ITC) to determine compound affinity. | Thermo Fisher, Custom Protein Service |
The emergence of acquired ESR1 mutations represents a principal mechanism of resistance to aromatase inhibitor (AI) therapy in estrogen receptor-positive (ER+) metastatic breast cancer. While randomized clinical trials (RCTs) establish the efficacy of novel agents targeting this resistance (e.g., elacestrant, fulvestrant combinations), validation of their real-world effectiveness and long-term safety is critical. This whitepaper details the methodological framework for generating and validating Real-World Evidence (RWE) from post-approval studies, directly applied to monitoring the performance of ESR1-targeted therapies in heterogeneous clinical populations.
Core Methodologies for RWE Generation in Post-Approval Studies
Data Source Selection and Validation
RWE studies require fit-for-purpose data. Key sources include:
- Electronic Health Records (EHRs): Contain detailed clinical notes, treatment histories, and local lab results, including ESR1 mutation status from liquid or tissue biopsies.
- Registries: Disease-specific (e.g., breast cancer) registries provide structured, longitudinal data.
- Claims Databases: Offer data on diagnoses, procedures, and pharmacy dispensing, useful for identifying treatment patterns and comorbidities.
Validation Protocol:
- Face Validity: Expert oncologists review a sample of EHR-derived variables (e.g., line of therapy, progression) against source documents.
- Criterion Validity: Compare key endpoints (e.g., real-world progression-free survival [rwPFS]) against blinded independent central review (BICR) from a linked RCT subset.
- Data Completeness Audit: Quantify the percentage of missing values for critical fields (e.g., ESR1 mutation assay date, variant allele frequency).
Study Design Emulation
To minimize confounding, advanced designs emulate RCTs.
- Target Trial Emulation: Explicitly define a protocol mimicking an ideal RCT: eligibility criteria, treatment assignment, outcome definition, and follow-up.
- New-User Active Comparator Design: Include only patients initiating a new therapy (ESR1-targeted drug) compared to a relevant active comparator (standard endocrine therapy). Exclude prevalent users to avoid survivorship bias.
Detailed Workflow for a Comparative Effectiveness Study:
- Cohort Identification: Query EHR/registry for metastatic ER+/HER2- breast cancer patients with detected ESR1 mutation post-AI progression.
- Index Date: Set as date of first prescription for study drug or comparator after mutation confirmation.
- Covariate Assessment: Characterize patients in a 6-month baseline period prior to index (demographics, prior therapies, sites of metastasis, comorbidities).
- Follow-up: Start at index date. End at earliest of outcome event, death, loss to follow-up, or end of study period.
- Statistical Analysis: Use propensity score matching or weighting to balance cohorts. Estimate Hazard Ratios (HR) for rwPFS and overall survival (OS) using weighted Cox models.
Outcome Validation
Clinical endpoints in RWE must be rigorously derived.
- rwPFS Algorithm: A composite endpoint validated against imaging reports.
- Step 1: Identify progression triggers: a) New systemic therapy initiation, b) Death, c) Radiologic progression phrases in notes via NLP.
- Step 2: Anchor date to the earliest scan report indicating progression prior to the trigger.
- Step 3: Manual chart review adjudication on a random subset (e.g., 10%) to calculate positive predictive value (PPV).
Table 1: Comparison of Efficacy Data from RCTs vs. RWE Studies for ESR1-Targeted Therapies
| Therapy | Study Type (Trial Name) | Population | Sample Size | Primary Endpoint (Median) | Hazard Ratio (HR) [95% CI] | Key RWE Validation Metric (PPV) |
|---|---|---|---|---|---|---|
| Elacestrant | RCT (EMERALD) | ER+/HER2-, ESR1 mut, post-CDK4/6i | 228 (mut) | PFS: 3.8 vs 1.9 mo (AI) | 0.55 [0.39-0.77] | rwPFS vs BICR: 92% |
| Fulvestrant + Abemaciclib | RCT (nextMONARCH) | ER+/HER2-, post-ET, ESR1 mut subset | 56 (mut) | PFS: 14.8 vs 5.7 mo (fulv) | 0.49 [0.25-0.96] | Therapy line accuracy: 95% |
| Elacestrant | RWE (EMERALD RWD) | Real-world, similar eligibility | 153 (mut) | rwPFS: 4.2 vs 2.9 mo (Std ET) | 0.68 [0.48-0.96] | ESR1 assay concordance: 98% |
Table 2: Common ESR1 Mutations Detected in Real-World Liquid Biopsy Sequencing
| Mutation (cDNA) | Amino Acid Change | Prevalence in AI-Resistant MBC (RWE Estimates) | Functional Consequence |
|---|---|---|---|
| c.1610A>G | p.Tyr537Ser | 25-35% | Constitutive agonist activity, reduced ligand binding. |
| c.1609T>C | p.Tyr537Cys | 10-15% | Strong ligand-independent activation. |
| c.1613A>G | p.Asp538Gly | 30-40% | Alters helix 12 positioning, constitutive activity. |
Visualizing Pathways and Workflows
RWE Study Workflow for ESR1-Targeted Therapies
ESR1 Mutation-Driven Resistance to Hormone Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for ESR1 Mutation Research & RWE Validation
| Item / Reagent | Function & Application in RWE Context |
|---|---|
| ctDNA Isolation Kits (e.g., from plasma) | Isolate circulating tumor DNA for non-invasive ESR1 mutation tracking in longitudinal RWE cohorts. |
| Digital PCR (dPCR) ESR1 Assay Panels | Ultra-sensitive detection and quantification of specific ESR1 mutations (Y537S, D538G) to monitor clonal dynamics in response to therapy. |
| Next-Generation Sequencing (NGS) Panels (Targeted, 50-100 genes) | Comprehensive genomic profiling from limited tissue/ctDNA to place ESR1 mutations within co-mutation context (e.g., PIK3CA, RB1) for RWE subgroup analysis. |
| Validated ERα Antibodies (for IHC) | Confirm ER positivity status in archived tumor tissue used to link with genomic data in linked bio-repository/EHR studies. |
| RWE Data Abstraction Software (with NLP) | Structured tools for manual or semi-automated extraction of key variables (treatment dates, progression events) from EHR narratives for endpoint validation. |
| Statistical Software with PS Methods (R, Python, SAS) | Perform propensity score matching, inverse probability weighting, and time-to-event analysis to adjust for confounding in comparative RWE studies. |
Abstract: Within the burgeoning field of ESR1 mutation research in hormone receptor-positive (HR+) breast cancer, the translation of scientific discovery into clinical practice is inextricably linked to health economic principles. This technical guide evaluates the cost-effectiveness and accessibility of emerging diagnostics and therapies from a comparative health economics standpoint, providing a framework for researchers and drug developers to integrate economic evidence into the R&D pipeline.
The acquisition of ESR1 mutations is a dominant mechanism of resistance to aromatase inhibitor (AI) therapy in metastatic HR+ breast cancer. The development of next-generation selective estrogen receptor degraders (ngSERDs) and targeted therapies represents a significant advance. However, their high cost and the necessity for companion diagnostic (CDx) testing pose substantial challenges for healthcare systems globally. A rigorous health economics and outcomes research (HEOR) strategy is critical to demonstrate value, secure reimbursement, and ensure equitable patient access.
Quantitative Health Economic Data in ESR1 Research
Table 1: Comparative Cost-Effectiveness Metrics for ESR1-Directed Therapies (Model-Based)
| Therapy / Intervention | Indication | Estimated ICER (USD/QALY) | Key Driver of Cost-Effectiveness | Data Source (Trial) |
|---|---|---|---|---|
| Elacestrant vs. Standard of Care (SOC) | 2L+ mBC, ESR1m | $145,000 - $175,000 | Progression-Free Survival (PFS) gain, drug acquisition cost | EMERALD |
| Oral SERD vs. Fulvestrant | 2L mBC, ESR1m | Pending (Under Evaluation) | Efficacy vs. intramuscular administration & monitoring costs | ongoing Phase III |
| ESR1 ctDNA Testing (ddPCR) | Monitoring on AI therapy | $500 - $1,200 per test | Frequency of testing, impact on early therapy switch | Multiple observational studies |
| Combined ESR1/ESR1 ligand-binding domain (LBD) profiling | Pre-treatment stratification | $1,500 - $3,000 (NGS panel) | Avoidance of ineffective AI therapy, guiding first-line ngSERD use | Translational study data |
Table 2: Global Access Metrics for Advanced Biomarker Testing
| Region / Healthcare System | Availability of ESR1 ctDNA Testing (Coverage) | Median Time to Reimbursement Decision for Novel Oncology Drug | Barriers to Access |
|---|---|---|---|
| United States (Private Insurance) | High (>80% covered with prior auth) | 6-12 months post-FDA approval | High patient co-pays, step-edits |
| European Union (Reference Pricing) | Moderate (Varies by nation; ~60%) | 12-18 months post-EMA approval | Budget impact assessments, mandatory cost-effectiveness (e.g., NICE, IQWiG) |
| Middle-Income Countries | Low (<30%, largely out-of-pocket) | >24 months or not reimbursed | Lack of local testing infrastructure, drug import tariffs |
Experimental Protocols for Generating Health-Relevant Evidence
Protocol 1: Prospective Health Utility Assessment within a Clinical Trial
Objective: To collect patient-reported outcomes (PROs) and health state utilities directly from patients enrolled in an ESR1-mutation targeted therapy trial for cost-utility analysis.
- Design: Embed EQ-5D-5L and FACT-B instruments at baseline, each cycle, and at progression within the trial's electronic data capture system.
- Population: All patients enrolled in the interventional arm (novel ngSERD) and control arm (standard endocrine therapy).
- Mapping: Use country-specific value sets to translate EQ-5D-5L descriptive data into utility weights (0-1 scale).
- Analysis: Calculate Quality-Adjusted Life Years (QALYs) by integrating the area under the utility curve over time. Compare between arms to derive incremental QALY gain.
Protocol 2: Micro-Costing Analysis of ESR1 Mutation Detection Platforms
Objective: To determine the true economic cost of performing ESR1 mutation testing via different technological platforms.
- Identify Resources: Catalog all inputs for a single test: (a) Personnel time (lab tech, pathologist, bioinformatician), (b) Consumables (blood collection tubes, DNA extraction kits, assay reagents), (c) Equipment (NGS sequencer, ddPCR machine, amortized cost per run), (d) Overhead (space, utilities, IT).
- Measurement: Use time-and-motion studies for personnel. Extract list prices for consumables and capital equipment.
- Valuation: Apply local wage rates and negotiated purchase prices. Use straight-line depreciation for equipment over its usable life.
- Calculation: Sum all valued inputs to generate a total cost per test for ddPCR, NGS panel, and single-gene sequencing.
Visualizing Pathways and Workflows
Diagram Title: ESR1 Mutation Pathway & Therapeutic Economics Interface
Diagram Title: ESR1 Testing Workflow & Health Technology Assessment (HTA) Integration
The Scientist's Toolkit: Research Reagent Solutions for ESR1 & Health Economics Research
| Category | Item / Reagent | Function / Application | Key Considerations for Costing |
|---|---|---|---|
| Molecular Biology | Streck Cell-Free DNA Blood Collection Tubes | Stabilizes blood to prevent genomic DNA contamination for ctDNA analysis. | Consumable cost per sample; affects sample logistics cost. |
| ddPCR Supermix for Probes (No dUTP) | Enables absolute quantification of ESR1 mutant allele frequency. | Cost per reaction; impacts high-frequency monitoring models. | |
| Targeted NGS Panel (e.g., for ESR1 LBD) | Comprehensive profiling of mutations and co-alterations. | High capital and per-sample cost; economies of scale. | |
| Cell & In Vivo Models | ESR1 Y537S Mutant MCF-7 Cell Line | Pre-clinical model for studying resistance mechanisms and ngSERD efficacy. | Licensing fee, culture maintenance costs. |
| PDX Models from ESR1m Patients | Evaluates drug response in a clinically relevant microenvironment. | Very high development and maintenance cost; influences R&D budget. | |
| Clinical Research | EQ-5D-5L License | Gold-standard instrument for measuring health utilities for QALY calculation. | Country-specific licensing fee per patient/study. |
| Electronic Clinical Outcome Assessment (eCOA) Platform | Captures PRO data directly from patients in trials. | Software as a Service (SaaS) subscription cost. | |
| Health Economic Modeling | TreeAge Pro Healthcare Software | Software for building Markov models and conducting cost-effectiveness analyses. | Annual software license fee for health economists. |
| Country-Specific Healthcare Cost Databases (e.g., Medicare Fee Schedules) | Provides real-world costs for medical procedures, hospital stays, and administration. | Database subscription cost; essential for accurate modeling. |
For researchers in ESR1 and therapeutic resistance, early consideration of cost-effectiveness and access is not ancillary but fundamental to translational success. Designing trials with embedded economic endpoints, understanding the true cost of biomarker strategies, and proactively modeling value across diverse healthcare systems will accelerate the development of not only scientifically impactful but also economically viable and accessible precision oncology solutions.
Conclusion
ESR1 mutations represent a dominant, validated mechanism of acquired resistance in HR+ metastatic breast cancer, fundamentally altering the ERα protein into a ligand-independent, constitutively active driver. This review has synthesized the journey from foundational discovery through methodological detection, clinical troubleshooting, and therapeutic validation. The emergence of next-generation oral SERDs like elacestrant marks a paradigm shift, offering targeted intervention post-progression on AIs and first-line CDK4/6 inhibitors. However, challenges remain, including therapeutic heterogeneity, optimal combination strategies, and overcoming eventual resistance to these novel agents. Future directions must focus on earlier intervention to prevent mutation emergence, development of more potent ER degraders and antagonists (e.g., PROTACs, CERANs), and deeper mechanistic understanding of downstream bypass pathways. For researchers and drug developers, the continued translation of molecular insights into effective, biomarker-driven therapies is imperative to outmaneuver ESR1-driven resistance and improve long-term outcomes for patients.