Harnessing AAV Vectors for CRISPR-Cas9 Delivery: A Comprehensive Guide for Cancer Therapy Development
This article provides a detailed exploration of Adeno-Associated Virus (AAV) vectors as delivery vehicles for CRISPR-Cas9 therapeutics in oncology, tailored for researchers and drug development professionals.
Harnessing AAV Vectors for CRISPR-Cas9 Delivery: A Comprehensive Guide for Cancer Therapy Development
Abstract
This article provides a detailed exploration of Adeno-Associated Virus (AAV) vectors as delivery vehicles for CRISPR-Cas9 therapeutics in oncology, tailored for researchers and drug development professionals. It begins by establishing the fundamental rationale for using AAVs, including their safety profile, serotype diversity, and capacity for stable gene expression. The core of the guide covers current methodologies, from vector design and payload engineering (e.g., SaCas9, compact editors) to preclinical in vivo delivery strategies. Critical challenges such as pre-existing immunity, off-target effects, and cargo size limitations are addressed with practical troubleshooting and optimization frameworks. Finally, the article evaluates AAV-CRISPR against alternative delivery platforms (LNPs, lentiviruses) and discusses the validation pathway from in vitro models to clinical trials. The synthesis offers a strategic roadmap for advancing AAV-CRISPR from bench to bedside in cancer treatment.
Why AAV? The Foundational Principles of Viral Vectors for CRISPR Cancer Therapy
Application Notes
CRISPR-Cas9 has transitioned from a basic gene-editing tool to a cornerstone of therapeutic development in oncology. Within the thesis framework of AAV vectors for therapeutic delivery, these notes detail critical applications. AAVs (Adeno-Associated Viruses) are the predominant in vivo delivery vehicle due to their low immunogenicity, persistent transgene expression, and serotype-specific tissue tropism, which can be engineered for targeted tumor delivery.
Key Therapeutic Strategies:
- Inactivation of Oncogenes: Direct targeting of gain-of-function mutations in genes like KRAS G12C/D/V, MYC, or EGFR.
- Restoration of Tumor Suppressors: Knock-in or homology-directed repair (HDR) to correct mutations in genes like TP53 or PTEN.
- Engineering Immune Cells: Ex vivo editing of T cells for CAR-T therapy (e.g., disrupting PD-1 to prevent exhaustion) or NK cells.
- Targeting Non-Coding Dependencies: Editing of regulatory elements or oncogenic non-coding RNAs.
- Synthetic Lethality: Knocking out genes that are essential only in the context of a specific cancer mutation.
Current Clinical Landscape: As of early 2024, over 50 clinical trials are investigating CRISPR-based therapies for cancer, with a significant portion utilizing viral vectors for delivery. The first ex vivo CRISPR-edited T cell therapies (e.g., for multiple myeloma) have received regulatory approval, marking a pivotal transition to clinical reality.
| Trial Phase | Target (Gene/Cell Type) | Delivery Method | Cancer Type | Key Metric (e.g., Response Rate) | NCT Number/Reference |
|---|---|---|---|---|---|
| Phase I/II | PD-1 (T cells) | Ex vivo electroporation | Non-small cell lung cancer | Objective Response Rate (ORR): ~40% | NCT02793856 |
| Phase I | NY-ESO-1 TCR + PD-1 KO (T cells) | Ex vivo electroporation | Multiple Myeloma, Sarcoma | Complete Response (CR): 60% in myeloma | NCT03399448 |
| Phase I | CD19 CAR + TCR & B2M KO (T cells) | Ex vivo electroporation | B-cell Malignancies | Overall Response (OR): 83% | NCT03166878 |
| Phase I/II | KRAS G12C | Lipid Nanoparticle (LNP) | Solid Tumors | Trial ongoing; preclinical data shows >70% editing in xenografts | NCT06004650 |
| Preclinical/IND-enabling | HPV Oncogenes E6/E7 | AAV (Intratumoral) | Cervical Cancer | >90% tumor regression in mouse models | (Recent literature) |
Protocols
Protocol 1: AAV Production for CRISPR-Cas9In VivoDelivery
Objective: To produce high-titer, recombinant AAV vectors serotype 9 (AAV9) or engineered capsid (e.g., AAV-PHP.eB) encoding SaCas9 (or a compact Cas9 variant) and a single guide RNA (sgRNA) targeting an oncogene.
Materials (Research Reagent Solutions):
| Item | Function |
|---|---|
| pAAV-CRISPR Vector (e.g., pAAV-SaCas9-sgRNA) | Plasmid containing CRISPR components under appropriate promoters (e.g., CBA for Cas9, U6 for sgRNA), flanked by AAV2 ITRs. |
| pHelper Plasmid (e.g., pHelper) | Provides adenoviral helper functions (E2A, E4, VA RNA) necessary for AAV replication. |
| pRep-Cap Plasmid (e.g., pAAV9/2) | Provides AAV replication (Rep) and serotype-specific capsid (Cap) proteins. Determines tissue tropism. |
| HEK293T Cells | Human embryonic kidney cell line expressing SV40 T-antigen, optimal for transfection and AAV production. |
| Polyethylenimine (PEI), linear, 40kDa | High-efficiency transfection reagent for co-delivery of three AAV plasmids. |
| Opti-MEM I Reduced Serum Medium | Serum-free medium for preparing DNA-PEI complexes. |
| Benzonase Nuclease | Digests unpackaged nucleic acids and cellular debris during purification. |
| Iodixanol Gradient (15%, 25%, 40%, 60%) | For ultracentrifugation-based purification of AAV particles based on buoyant density. |
| PBS-MK Buffer (PBS with 1mM MgCl₂, 2.5mM KCl) | Formulation buffer for final purified AAV vector storage. |
| qPCR Kit with ITR-specific primers/probe | For absolute quantification of viral genome titer (vg/mL). |
Method:
- Cell Seeding: Seed HEK293T cells in a cell factory or ten-layer stacker at 70% confluence in DMEM + 10% FBS.
- Transfection: For one cell factory, prepare a DNA mix of 750µg pAAV-CRISPR, 750µg pHelper, and 1000µg pRep-Cap in Opti-MEM. In a separate vessel, prepare PEI (1mg/mL) at a 3:1 PEI:total DNA ratio. Mix DNA and PEI solutions, vortex, incubate 15 min at RT, then add to cells.
- Harvest: 72 hours post-transfection, detach cells and pellet by centrifugation. Resuspend cell pellet in lysis buffer (150mM NaCl, 50mM Tris, pH 8.5) and perform 3-5 freeze-thaw cycles.
- Purification: Treat lysate with Benzonase (50U/mL) for 30 min at 37°C. Clarify by centrifugation. Load supernatant onto an iodixanol step gradient and centrifuge in a ultracentrifuge at 350,000 x g for 1.5 hours. Extract the opaque 40% iodixanol fraction containing AAV.
- Concentration & Buffer Exchange: Concentrate and exchange into PBS-MK using a 100kDa MWCO centrifugal filter.
- Titration: Determine genomic titer by quantitative PCR (qPCR) using primers against the AAV ITR region. Assess purity via SDS-PAGE.
Protocol 2:In VivoAssessment of AAV-CRISPR Efficacy in a Xenograft Model
Objective: To evaluate tumor growth inhibition following systemic or intratumoral delivery of AAV-CRISPR targeting a driver oncogene.
Materials: AAV-CRISPR vector (from Protocol 1, titer >1e13 vg/mL), immunodeficient NSG mice, human cancer cell line (e.g., HCT-116 colorectal), calipers, in vivo imaging system (IVIS) if using luciferase-tagged cells, tissue homogenizer, genomic DNA extraction kit, T7 Endonuclease I or next-generation sequencing (NGS) assay for indel analysis.
Method:
- Tumor Engraftment: Subcutaneously inject 5e6 luciferase-expressing HCT-116 cells into the flank of NSG mice.
- Randomization & Treatment: When tumors reach ~100mm³, randomize mice into cohorts (n=5-10). Treat via tail-vein injection (systemic; 1e11 vg/mouse) or direct intratumoral injection (5e10 vg/mouse) with AAV-CRISPR or AAV-control.
- Monitoring: Measure tumor volume (V = (L x W²)/2) and body weight bi-weekly for 4-6 weeks. Perform bioluminescent imaging weekly.
- Terminal Analysis: At endpoint, euthanize mice, excise tumors, and weigh. Split each tumor: portion for snap-freezing (molecular analysis), portion for formalin-fixation (histology/IHC).
- Editing Efficiency Analysis:
- Homogenize frozen tissue.
- Extract genomic DNA.
- PCR-amplify the on-target genomic region.
- Quantify indel percentage using T7E1 assay (digestion, gel electrophoresis) or, preferably, by NGS amplicon sequencing for accurate quantification and off-target assessment.
Diagrams
Within a thesis exploring AAV vectors for therapeutic CRISPR-Cas9 delivery in cancer, understanding the fundamental biology of Adeno-Associated Virus (AAV) is paramount. The choice of capsid serotype directly dictates in vivo tropism—determining which tissues are transduced—and thus the efficacy and safety of the gene therapy. This application note details the core principles of AAV tropism, compares key serotypes, and provides a rationale and protocol for in vivo delivery in preclinical cancer models.
Tropism and Serotype Comparison
AAV tropism is governed by the interaction between the viral capsid and specific cell surface receptors/co-receptors on target tissues. Different naturally occurring serotypes have evolved distinct capsid proteins, leading to varied receptor binding and transduction profiles.
Table 1: Key AAV Serotypes and Their Tropism in Cancer Research
| Serotype | Primary Receptors/Co-receptors | Notable Tissue Tropism | Advantages for Cancer Therapy | Reported Transduction Efficiency (Relative) in Common Models |
|---|---|---|---|---|
| AAV1 | N-linked sialic acid | Skeletal muscle, heart, CNS neurons | High muscle transduction; potential for targeting metastases. | Muscle: +++, Liver: +, Tumor (varies): +/++ |
| AAV2 | HSPG, αVβ5 integrin, FGFR1 | Liver, skeletal muscle, CNS, kidney | Well-characterized; extensive safety profile. | Liver: ++, Muscle: ++, Tumor (local): ++ |
| AAV5 | PDGFR, N-linked sialic acid | CNS astrocytes, photoreceptors, lung, pancreas | Efficient CNS glial cell targeting for brain tumors. | CNS: +++ (glia), Lung: ++, Liver: + |
| AAV6 | N- and O-linked sialic acid, EGFR | Heart, lung, skeletal muscle, liver | Efficient systemic and cardiac delivery. | Muscle: +++, Heart: +++, Tumor (varies): ++ |
| AAV8 | LamR (37/67 kDa), galactose | Liver, pancreas, heart, muscle, CNS | Superior hepatocyte transduction; ideal for liver-directed therapies. | Liver: +++++, Pancreas: +++, Muscle: ++ |
| AAV9 | N-linked galactose, LamR | Broad systemic: heart, liver, lung, CNS (crosses BBB) | Pan-tissue transduction; crosses blood-brain barrier for CNS tumors. | Heart: +++, Liver: ++++, CNS: +++, Tumor (broad): ++/+++ |
| AAV-DJ (Chimeric) | HSPG, lactosylceramide? | Broad: liver, heart, kidney, CNS | Engineered for enhanced in vitro & in vivo transduction across cell types. | Liver: ++++, Cultured Cells: +++++, Tumor (broad): +++ |
| AAVrh.10 | Unknown (similar to AAV9?) | Broad systemic, strong CNS, lung, retina | Efficient CNS and lung transduction; used in clinical trials for glioblastoma. | CNS: ++++, Lung: +++, Liver: ++ |
Note: ++++ denotes very high efficiency; + denotes low efficiency. Tumor transduction is highly model-dependent.
Rationale for In Vivo Delivery in Cancer Research
Direct in vivo delivery of AAV-CRISPR vectors offers significant advantages over ex vivo strategies for cancer:
- Targeting the Tumor Microenvironment (TME): Enables simultaneous genetic manipulation of cancer cells and stromal cells (e.g., fibroblasts, immune cells).
- Accessibility: AAVs can be administered systemically or locally to reach disseminated or surgically challenging tumors.
- Therapeutic Scope: Facilitates in situ gene editing for tumor suppressor reactivation, oncogene knockout, or engineering of immune cells in situ.
- Preclinical Modeling: More accurately recapitulates the complexity of tumor biology, immune interaction, and vector pharmacokinetics/pharmacodynamics.
Detailed Protocol: Systemic AAV-CRISPR Delivery in a Murine Xenograft Model
Objective: To systemically deliver an AAV9 vector encoding a CRISPR-Cas9 system to target a tumor-specific oncogene in a subcutaneous xenograft model.
A. Materials & Pre-Administration Setup
Research Reagent Solutions
| Item | Function | Example/Note |
|---|---|---|
| AAV Vector | Delivery vehicle for CRISPR machinery. | AAV9-CBh-Cas9-U6-sgRNA(Oncogene), purified, >1e13 vg/mL. |
| Sterile PBS (pH 7.4) | Diluent for the AAV vector to achieve desired dosing volume. | Nuclease-free, without Mg2+/Ca2+. |
| 1 mL Insulin Syringes (29G) | For precise intraperitoneal (IP) or intravenous (IV) injection in mice. | Low dead volume for accurate dosing. |
| Animal Warming Chamber | Dilates tail veins for easier IV injection. | Set to 37°C for 5-10 minutes. |
| Restrainer (for IV) | Secures mouse for tail vein injection. | Cylindrical rodent restrainer. |
| Cell Line & Matrigel | For establishing the tumor model. | Human cancer cell line of interest. |
| Anesthetic (e.g., Isoflurane) | For brief anesthesia during IV injection (optional but recommended). | Provides calm, precise administration. |
Animal Model Preparation: Inoculate immunodeficient mice (e.g., NSG) subcutaneously with 1-5x10^6 target cancer cells suspended in 50% Matrigel. Proceed with vector administration when tumors reach a palpable volume (~50-100 mm³).
B. Step-by-Step Procedure
- Vector Thawing & Preparation: Thaw AAV aliquot on ice. Dilute to the final working concentration in sterile, cold PBS. Gently mix by inversion. Keep on ice. Dose Example: 5e11 vector genomes (vg) per mouse in a 150 µL total volume.
- Mouse Restraint: For IV injection, place the mouse in the warming chamber for 5-10 minutes, then transfer to a suitable restrainer, exposing the tail.
- Administration (Intravenous - Tail Vein): a. Wipe the tail with an alcohol swab. b. Using a 29G insulin syringe, draw up the calculated dose volume. c. Identify one of the two lateral tail veins. Insert the needle bevel-up, parallel to the vein. d. Inject slowly (over ~30 seconds). A lack of resistance and visible clearing of the vein indicates proper delivery. e. Withdraw the needle and apply gentle pressure with gauze.
- Post-Injection Monitoring: Return the animal to its cage and monitor for acute distress. Tumors and tissues can be harvested at predetermined timepoints (e.g., 7, 14, 21 days post-injection) for analysis (editing efficiency, tumor growth, biodistribution).
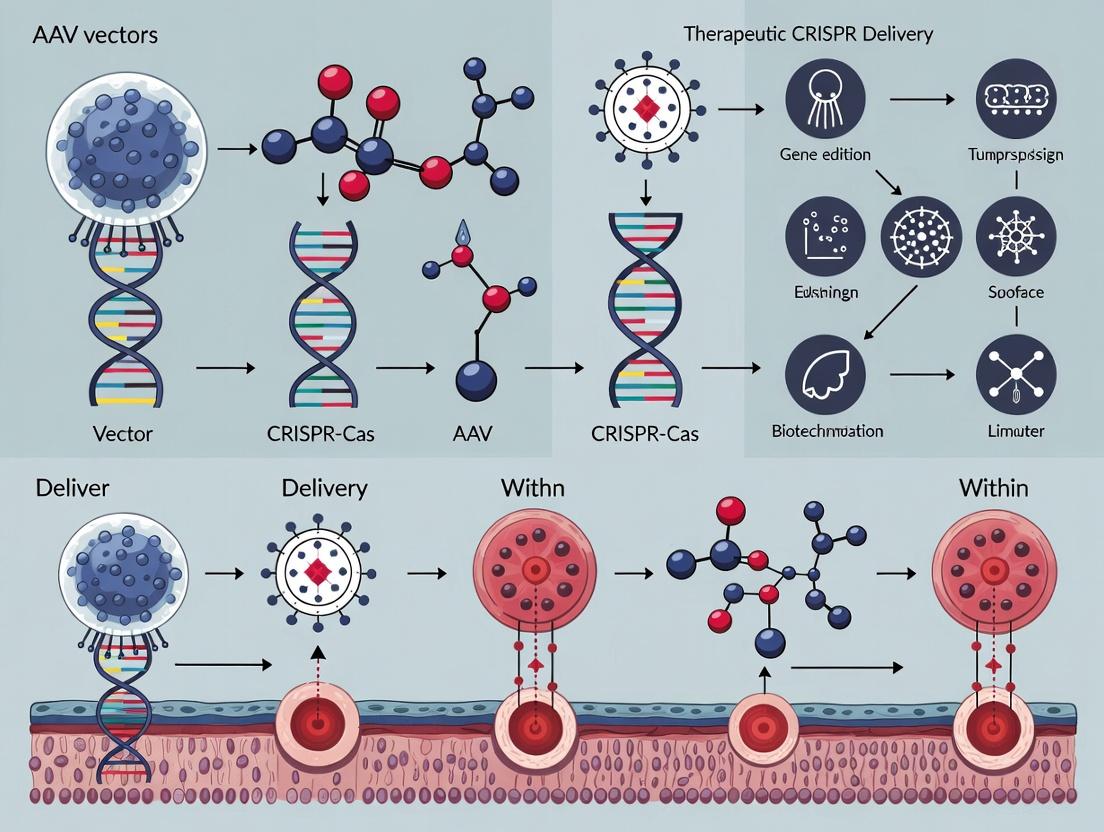
Visualization of Key Concepts
Diagram 1: AAV Serotype Determines In Vivo Tropism and Application
Diagram 2: Workflow: Systemic AAV-CRISPR Delivery for Tumor Editing
Adeno-Associated Virus (AAV) vectors have emerged as the leading platform for in vivo therapeutic gene delivery, particularly for CRISPR-based applications in oncology. Their utility is anchored in three pillars: the ability to sustain long-term transgene expression, a favorable safety profile with low pathogenicity, and a growing clinical track record. This application note details protocols and analyses supporting the use of AAVs within a thesis focused on CRISPR delivery for cancer research, providing researchers with actionable methodologies and current data.
Table 1: Comparison of AAV Serotypes for In Vivo Delivery to Common Cancer Model Tissues
| AAV Serotype | Primary Tissue Tropism | Reported Transduction Efficiency (Relative Units) | Time to Peak Expression (Days) | Expression Durability (Months) |
|---|---|---|---|---|
| AAV9 | Systemic, Broad (incl. CNS) | High | 7-14 | >12 (in rodents) |
| AAV8 | Liver, Muscle, Pancreas | Very High | 10-21 | >12 |
| AAV6 | Heart, Lung, Skeletal Muscle | Moderate-High | 5-10 | 6-12 |
| AAV5 | CNS, Retina, Lung | Moderate | 14-28 | >6 |
| AAV-DJ | Broad (Engineered) | Very High | 7-14 | >6 |
| AAVrh.10 | CNS, Retina | High | 14-21 | >9 |
Note: Efficiency and kinetics are model-dependent. Data compiled from recent pre-clinical studies (2022-2024).
Table 2: Clinical Trial Status of AAV-CRISPR Therapies in Oncology (as of 2024)
| Condition/Target | AAV Serotype | CRISPR Component | Phase | Key Safety Finding (Related to AAV) |
|---|---|---|---|---|
| HPV-related Cancers (Targeting E6/E7) | AAV-DJ | SaCas9 | I | Grade 1-2 liver enzyme elevation (dose-dependent) |
| Advanced Hematologic Malignancies | AAV6 | CRISPR-Cas9 Knockout | I/II | Mild cellular immune response to capsid |
| Solid Tumors (PD-1 knockout) | AAV9 | spCas9 | I | No dose-limiting toxicities attributed to vector |
Application Notes & Detailed Protocols
Protocol: Evaluating Long-Term Transgene Expression in a Murine Xenograft Model
Objective: To assess the durability of AAV-mediated CRISPR effector expression in tumor tissue. Materials: AAV9-CRISPR-sgRNA (targeting oncogene of interest), immunocompromised mice, luciferase-tagged cancer cell line, In Vivo Imaging System (IVIS), PCR reagents, IHC staining kit. Procedure:
- Tumor Engraftment: Subcutaneously inject 5x10^6 luciferase-positive tumor cells into the flank of mice (n=10 per group).
- AAV Administration: Once tumors reach ~100 mm³, administer 1x10^11 vg of AAV9-CRISPR via tail vein injection. Include a PBS control group.
- Longitudinal Monitoring:
- Tumor Growth: Measure tumor volume bi-weekly using calipers.
- In Vivo Imaging: Perform IVIS imaging weekly post-injection to monitor luciferase signal (correlates with tumor burden).
- Terminal Time Points: Euthanize cohorts at 1, 3, 6, and 9 months post-AAV injection.
- Tissue Analysis:
- Extract genomic DNA from harvested tumors. Perform PCR amplification of the target locus and subject to T7 Endonuclease I assay or next-generation sequencing to quantify indel frequency.
- Fix tumor sections for IHC staining against the CRISPR nuclease (e.g., anti-FLAG for tagged Cas9) to visualize protein persistence.
- Data Analysis: Plot indel frequency and nuclease protein expression against time to generate a durability curve. Compare tumor growth curves between treated and control groups.
Protocol: Assessing AAV Capsid Immunogenicity
Objective: To characterize humoral and cellular immune responses to AAV capsid, a key factor in pathogenicity and re-administration potential. Materials: Mouse serum samples (from Protocol 2.1), ELISA plates coated with empty AAV9 capsids, IFN-γ ELISpot kit, splenocytes, AAV capsid peptides. Procedure:
- Anti-Capsid Antibody Titer (ELISA):
- Collect serum at terminal time points.
- Coat ELISA plates with purified AAV9 capsids overnight.
- Add serial dilutions of mouse serum, followed by anti-mouse IgG-HRP.
- Develop with TMB substrate. Measure OD450. Report endpoint titers.
- Capsid-Specific T-Cell Response (ELISpot):
- At sacrifice, harvest spleens and isolate splenocytes.
- Seed 2x10^5 cells/well in an IFN-γ ELISpot plate.
- Stimulate cells with a pool of AAV9 capsid-derived MHC-I peptides.
- After 36-48h, develop the plate per manufacturer's instructions.
- Count spot-forming units (SFU) representing antigen-specific T-cells.
- Analysis: Correlate immune response data with expression longevity from Protocol 2.1. High neutralizing antibody titers or strong T-cell responses may correlate with diminished long-term expression.
Visualizations
AAV-CRISPR Long-Term Expression Workflow
AAV Immune Response Pathways
The Scientist's Toolkit: Essential Reagents for AAV-CRISPR Cancer Research
Table 3: Key Research Reagent Solutions
| Reagent/Material | Supplier Examples | Function in AAV-CRISPR Experiments |
|---|---|---|
| Purified AAV Serotypes | Vigene, Addgene | Pre-packaged AAVs of various serotypes for tropism screening and in vivo pilot studies. |
| AAV Genome Titer Kit (qPCR) | Thermo Fisher, Qiagen | Accurately quantifies vector genome (vg/mL) concentration, critical for dosing consistency. |
| T7 Endonuclease I / Surveyor Assay Kit | NEB, IDT | Detects CRISPR-induced indels at the target genomic locus with moderate throughput. |
| Anti-Capsid Neutralizing Antibody Assay | Progen, in-house | Measures serum antibodies that block AAV transduction, informing immunogenicity. |
| Next-Generation Sequencing Library Prep Kit for CRISPR | Illumina, Paragon Genomics | Enables deep sequencing of target loci for unbiased quantification of editing efficiency and spectrum. |
| Recombinant AAVR / HSPG Protein | Sino Biological | Used in in vitro binding assays to study AAV entry mechanisms and tropism. |
| Caspase-3/7 Apoptosis Assay | Promega | Assesses potential off-target cytotoxic effects of AAV-CRISPR delivery in non-target cells. |
Within the broader thesis on recombinant adeno-associated virus (AAV) vectors for therapeutic CRISPR-Cas delivery in oncology, three fundamental bottlenecks persist. These constraints—limited packaging capacity (~4.7 kb), pre-existing and therapy-induced immunogenicity, and scalable manufacturing hurdles—critically impact the efficacy, safety, and commercial viability of AAV-CRISPR cancer therapies. This document provides application notes and detailed protocols to address these challenges experimentally.
Challenge: Packaging Capacity
Application Notes
The CRISPR-Cas9 system, with its SpCas9 nuclease (~4.2 kb), sgRNA, and regulatory elements, easily exceeds AAV's payload limit. Strategies include using smaller Cas orthologs (e.g., SaCas9, ~3.2 kb) or split-inteln systems. The primary trade-off is between packaging efficiency and genome editing activity.
Table 1: Comparison of CRISPR-Cas Systems for AAV Packaging
| Cas Protein | Size (kb) | AAV Compatibility | Reported Editing Efficiency in Vivo | Key Limitations |
|---|---|---|---|---|
| SpCas9 | ~4.2 | Requires dual-AAV | 5-25% (liver) | Increased immunogenicity risk |
| SaCas9 | ~3.2 | Single-AAV with small promoter | 10-40% (liver) | PAM requirement (NNGRRT) |
| Cas12a (Cpf1) | ~3.9 | Often requires dual-AAV | 2-15% (liver) | Lower efficiency in some tissues |
| Ultracompact Cas (e.g., CasΦ) | ~2.0 | Single-AAV with large regulatory elements | Under investigation | Uncharacterized immunogenicity |
Protocol 1.1: Evaluating Dual-AAV Trans-Splicing System Efficiency
Objective: To quantify reconstitution efficiency of a large transgene split between two AAVs using the split-inteln system.
Materials:
- AAV-Pro1-Cas9N-intN (AAV serotype relevant to target tissue, e.g., AAV8 for liver)
- AAV-intC-Cas9C-Pro2-sgRNA-GOI (Matching serotype)
- Target cell line (e.g., HepG2)
- qPCR reagents, primers for junction region and reference gene.
- Western blot reagents, anti-Cas9 antibody.
Method:
- Cell Seeding & Transduction: Seed HepG2 cells in a 12-well plate. At 70% confluency, co-transduce with both AAVs at a 1:1 MOI ratio (e.g., 1e4 vg/cell each).
- Genomic DNA (gDNA) Isolation: At 72 hours post-transduction, isolate gDNA using a silica-column kit.
- qPCR for Junction DNA:
- Design a forward primer in the Cas9N segment and a reverse primer in the Cas9C segment, spanning the reconstituted inteln splice junction.
- Perform qPCR using SYBR Green. Normalize to a single-copy host gene (e.g., RPP30).
- Calculation:
% Reconstitution = (2^(-ΔCt_junction) ) * 100, where ΔCt = Ct(junction) - Ct(host gene).
- Protein Analysis: At 96 hours, lyse cells for western blot. Probe for full-length Cas9 protein.
- Functional Assay: Co-package a model sgRNA targeting a reporter gene (e.g., EGFP) and assess knockout via flow cytometry 7 days post-transduction.
Key Reagent Solutions:
- AAV Titration Kit (ddPCR-based): Essential for accurate vector genome (vg) quantification, crucial for determining MOI.
- Intein-Specific Antibodies: For detecting split fragments and reconstituted protein.
- QuickChange Mutagenesis Kit: For engineering inteln split sites into Cas9 plasmids.
Diagram Title: Dual-AAV Intein Reconstitution Workflow
Challenge: Immunogenicity
Application Notes
AAV capsids and CRISPR-Cas proteins can trigger host immune responses, leading to vector clearance, reduced transduction, and potential toxicity. This includes pre-existing neutralizing antibodies (NAbs) and cell-mediated immunity against Cas9. Monitoring is essential for preclinical studies.
Table 2: Immunogenicity Assessment Parameters & Methods
| Immune Component | Assay Method | Sample Type | Quantitative Readout | Threshold of Concern |
|---|---|---|---|---|
| Pre-existing AAV NAbs | Neutralization Assay | Serum | NT50 (50% neutralization titer) | NT50 > 1:5 |
| Anti-Cas9 Humoral Response | ELISA | Serum | End-point titer; μg/mL | Significant rise post-dose |
| Anti-Cas9 Cellular Response | IFN-γ ELISpot | PBMCs or Splenocytes | Spot-forming units (SFU) per 10^6 cells | >50 SFU/10^6 cells over baseline |
| Inflammatory Cytokines | Multiplex Luminex | Serum/Plasma | pg/mL of IL-6, TNF-α, IFN-γ | >2-fold increase vs. control |
Protocol 2.1: Mouse Serum Neutralization Assay for Pre-existing AAV Immunity
Objective: To determine the neutralizing antibody (NAb) titer in mouse serum against a specific AAV serotype.
Materials:
- Mouse serum samples (pre-dose).
- AAV-luciferase reporter vector (matching intended serotype).
- HEK293T cells.
- Luciferase assay kit.
- Cell culture medium.
Method:
- Serum Heat-Inactivation: Heat serum at 56°C for 30 minutes.
- Serial Dilution: Perform 2-fold serial dilutions of serum (e.g., 1:5 to 1:640) in culture medium.
- Virus-Serum Incubation: Mix a fixed amount of AAV-luciferase (e.g., MOI 1e4) with an equal volume of each serum dilution. Incubate at 37°C for 1 hour.
- Cell Infection: Add mixtures to HEK293T cells in a 96-well plate. Include controls: virus-only (no serum, max signal) and cell-only (no virus, background).
- Luciferase Readout: After 48 hours, lyse cells and measure luciferase activity.
- NT50 Calculation: Plot relative luminescence units (RLU) against serum dilution. Fit a 4-parameter logistic curve. The NT50 is the dilution that reduces luciferase signal by 50% compared to virus-only control.
Diagram Title: AAV Neutralization Assay Protocol Flow
Challenge: Manufacturing Hurdles
Application Notes
Scalable AAV production for CRISPR components faces issues with yield, empty/full capsid ratio, and potency consistency. The triple-transfection in HEK293 cells remains common but is difficult to scale. Baculovirus/Sf9 and HSV systems offer alternatives.
Table 3: Comparison of AAV Production Platforms for CRISPR Vectors
| Platform | Typified Yield (vg/L) | Empty/Full Ratio | Scalability | Key Challenge for CRISPR |
|---|---|---|---|---|
| HEK293 Transfection | 1e14 - 5e14 | Often high ( >10:1) | Moderate (Stirred-tank bioreactors) | Plasmid size affecting transfection efficiency |
| Baculovirus/Sf9 | 1e15 - 1e16 | Can be optimized to ~1:1 | High (Insect cell bioreactors) | Proper folding of mammalian Cas protein |
| HSV System | ~1e15 | Low | High | HSV contamination clearance |
Protocol 3.1: Analytical Ultracentrifugation (AUC) for Empty/Full Capsid Ratio
Objective: To determine the proportion of genome-containing (full) versus empty AAV capsids in a purified preparation.
Materials:
- Purified AAV-CRISPR sample.
- AUC compatible buffer (e.g., PBS pH 7.4).
- Analytical ultracentrifuge with UV/Vis optics.
- Double-sector centerpieces.
Method:
- Sample Preparation: Dilute AAV sample to an absorbance at 260 nm (A260) of ~0.5. Load ~400 μL into the sample sector of a centerpiece. Load matching buffer into the reference sector.
- Run Parameters: Use a rotor speed of 20,000 rpm at 20°C. Perform a radial scan at 260 nm (for DNA) and 230 nm or 280 nm (for protein) continuously.
- Data Analysis: Use software (e.g., SEDFIT) to model the sedimentation velocity data. The key signals are:
- ~60 Svedberg (S): Genome-containing (full) capsids (absorb at 260nm & 280nm).
- ~50 Svedberg (S): Empty capsids (absorb primarily at 280nm).
- Quantification: Integrate the areas under the peaks for the full and empty species from the c(s) distribution at 260nm. The ratio is proportional to the
Area_full / (Area_full + Area_empty).
The Scientist's Toolkit: Key Reagents & Materials
| Item | Function/Benefit | Example/Supplier |
|---|---|---|
| Reduced-Size Cas9 Expression Plasmids | Maximizes space for regulatory elements in single-AAV designs. | Addgene # plasmids for SaCas9. |
| Intein-Compatible Cloning Vectors | Facilitates split-Cas9 construct generation for dual-AAV systems. | Custom or commercial (e.g., Takara). |
| Anti-AAV Neutralizing Antibody ELISA Kits | High-throughput screening of patient sera for pre-existing immunity. | Progen, AAVance Biotech. |
| cGMP-Grade HEK293 Cell Lines | Essential for scalable, reproducible clinical vector production. | Thermo Fisher, ATCC. |
| AAX Helper-Free Expression System | Reliable, high-titer AAV production via transfection, reduces contamination risk. | Agilent Technologies. |
| iodixanol Gradient Medium | Ultracentrifugation medium for high-purity AAV purification from cell lysates. | OptiPrep (Sigma). |
| ddPCR AAV Titration Kits | Absolute quantification of vector genome titer without standards. | Bio-Rad. |
| Endotoxin Removal Resins | Critical for in vivo applications to reduce inflammatory responses. | Mustang E (Pall) or equivalent. |
Application Notes: Key Therapeutic Strategies and Quantitative Outcomes
Preclinical cancer research utilizing AAV-CRISPR pipelines focuses on three primary strategies: in vivo gene knockouts, targeted gene knock-ins, and transcriptional modulation. The following table summarizes recent representative studies and their quantitative outcomes.
Table 1: Preclinical Applications of AAV-CRISPR in Cancer Models
| Target Gene / Strategy | Cancer Model | AAV Serotype | Delivery Route | Key Quantitative Outcome | Reference (Example) |
|---|---|---|---|---|---|
| PD-1 Knockout | Murine Melanoma (B16) | AAV9 | Intravenous | ~60% editing in tumor-infiltrating lymphocytes; 80% tumor growth inhibition vs control | (2023, Mol. Ther.) |
| PLK1 Knockout | Hepatocellular Carcinoma (PDX) | AAV8 | Intratumoral | ~45% indels in tumor tissue; 70% reduction in tumor volume at day 21 | (2024, Hepatology) |
| KRASG12D Correction | Pancreatic Ductal Adenocarcinoma (GEMM) | AAVrh10 | Systemic (IV) | 8.5% correction efficiency in tumor cells; median survival extended from 45 to 68 days | (2023, Sci. Adv.) |
| CD19 CAR Knock-in | B-cell Leukemia (Xenograft) | AAV6 | Ex vivo (T cells) | ~35% knock-in efficiency; complete tumor regression in 5/7 mice | (2024, Blood) |
| dCas9-VP64 Activation (MHC-I) | Colon Carcinoma (MC38) | AAV-DJ | Intratumoral | 25-fold increase in H2-K1 mRNA; 50% increase in CD8+ T cell infiltration | (2023, Cell Rep.) |
| Dual gRNA: CTNNB1 & MYC | Glioblastoma (U87MG Xenograft) | AAV-PHP.eB | Intracranial | ~30% co-deletion efficiency; 90% reduction in bioluminescent signal | (2024, Nat. Commun.) |
Protocols
Protocol 2.1: In Vivo Knockout of Immune Checkpoint Gene in a Syngeneic Tumor Model
Objective: To assess the efficacy of AAV-CRISPR mediated PD-1 knockout in tumor-infiltrating lymphocytes (TILs) for melanoma immunotherapy.
Materials: See "The Scientist's Toolkit" below. Procedure:
- Tumor Inoculation: Inject 5x10^5 B16-F10 cells subcutaneously into the right flank of C57BL/6 mice (Day 0).
- AAV Preparation & Administration: When tumors reach ~50 mm³ (Day 7), administer 1x10^11 vg of AAV9-sgRNAhPD-1-SaCas9 (or spCas9) via tail vein injection. Include controls (AAV-GFP, PBS).
- Monitoring: Measure tumor dimensions with calipers every 2-3 days. Calculate volume: V = (length x width²)/2.
- Endpoint Analysis (Day 21): a. Euthanize mice, harvest tumors and spleens. b. Prepare single-cell suspensions using mechanical dissociation and a 70 µm strainer. c. Enrich TILs using a Percoll gradient centrifugation (40%/80%). d. Isolate genomic DNA from purified CD8+ T cells (e.g., using magnetic beads). e. Assess editing efficiency via T7 Endonuclease I assay or next-generation sequencing (NGS) of the target site. Calculate indel percentage. f. Analyze tumor-infiltrating immune populations by flow cytometry (CD45+, CD3+, CD8+, PD-1+).
Protocol 2.2: Targeted Gene Knock-in for CAR Expression via AAV-CRISPR
Objective: To integrate a CD19-CAR cassette into the TRAC locus of primary human T cells ex vivo.
Materials: See "The Scientist's Toolkit" below. Procedure:
- T Cell Activation: Isolate PBMCs from leukapheresis product. Activate CD3+ T cells with anti-CD3/CD28 beads (bead:cell ratio 3:1) in IL-2 (100 IU/mL) containing media for 48h.
- RNP Electroporation: Pre-complex 30 µg of spCas9 protein with 30 µg of TRAC-targeting sgRNA (chemical modification recommended) to form RNP. Electroporate 1x10^6 activated T cells with the RNP complex using a 4D-Nucleofector (program EO-115).
- AAV6 Transduction: Immediately post-electroporation, transduce cells with AAV6 donor vector (containing homology arms and CD19-CAR-P2A-GFP payload) at an MOI of 1x10^5 vg/cell. Centrifuge at 1000 x g for 90 min (spinoculation) at 32°C.
- Culture & Expansion: Maintain cells in IL-2/IL-15 media. Remove activation beads after 96h.
- Analysis (Day 7-10): a. Flow Cytometry: Assess CAR expression via GFP or anti-F(ab')2 staining. Calculate knock-in efficiency. b. Functional Assay: Co-culture CAR-T cells with CD19+ NALM-6 target cells at various E:T ratios. Measure cytotoxicity (e.g., luciferase-based assay) and cytokine (IFN-γ) secretion.
Visualizations
Diagram 1: Core AAV-CRISPR Preclinical Workflow (89 chars)
Diagram 2: AAV Delivery Routes for Cancer CRISPR (99 chars)
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for AAV-CRISPR Cancer Experiments
| Reagent/Material | Function/Purpose | Example Vendor/Catalog |
|---|---|---|
| AAV-Production System | Production of high-titer, clinical-grade vectors. | pAAV vector plasmids, AAVpro 293T cells (Takara), PEIpro transfection reagent. |
| CRISPR Nuclease Variants | Provides versatility in PAM requirements and size for AAV packaging. | spCas9 (3.2 kb), SaCas9 (3.1 kb), smaller Cas12f (1.5 kb). |
| Next-Generation Sequencing Kit | Quantifies on-target editing and off-target effects. | Illumina MiSeq, Amplicon-EZ service (GENEWIZ). |
| T7 Endonuclease I | Rapid, low-cost validation of indel formation. | NEB EnGen Mutation Detection Kit (NEB #E3321). |
| In Vivo Imaging System (IVIS) | Tracks tumor growth and metastasis longitudinally. | PerkinElmer IVIS Spectrum. |
| Multiparameter Flow Cytometer | Analyzes tumor immune microenvironment and cell surface markers. | BD Symphony A5, Antibody panels (BioLegend). |
| Electroporation System | Enables ex vivo RNP delivery for high-efficiency editing prior to AAV donor delivery. | Lonza 4D-Nucleofector X Unit. |
| Animal Models | Preclinical testing in immunocompetent or humanized contexts. | Syngeneic mice (C57BL/6), GEMMs, PDX/CDX models. |
Building the Vector: Methodologies for Engineering and Delivering AAV-CRISPR Payloads
The precise delivery of CRISPR-Cas9 components—Cas9 nuclease, guide RNA (gRNA), and a repair template for homology-directed repair (HDR)—is a central challenge in developing therapeutic applications for cancer. Adeno-associated virus (AAV) vectors are a leading delivery platform due to their excellent safety profile and ability to transduce dividing and non-dividing cells. However, the ~4.7 kb packaging capacity of AAV severely constrains the co-delivery of all necessary components. This document, framed within a thesis on AAV vectors for therapeutic CRISPR delivery in cancer research, details current strategies and protocols to overcome this limitation.
Strategies for AAV-CRISPR Payload Design
Dual-Vector/Split-Cas9 Systems
The most common strategy involves splitting the Cas9 coding sequence across two separate AAV vectors. The canonical S. pyogenes Cas9 (SpCas9) is ~4.2 kb, exceeding the AAV capacity when combined with essential regulatory elements. Split-intein systems are employed, where Cas9 is divided into N- and C-terminal fragments, each fused to split intein halves. Upon co-infection and translation, the inteins mediate a protein trans-splicing event to reconstitute a fully functional Cas9 nuclease.
Key Quantitative Data: Table 1: Comparison of Split-Cas9 Systems
| System | Cas9 Fragment Sizes | Reconstitution Efficiency * | Required AAV Vectors | Key Advantage |
|---|---|---|---|---|
| Intein (N/C) | ~2.1 kb each | 10-30% (in vivo) | 2 (Cas9 split) + 1 (gRNA) | Well-characterized, high-fidelity splicing |
| Intein (4-Part) | ~1.1 kb each | 1-10% (in vivo) | 4 (Cas9 split) | Enables delivery of larger nucleases (e.g., Cas12a) |
| Dual AAV (Overlap) | ~2.4 kb each | 0.5-5% (in vivo) | 2 (with overlapping homology) | No foreign splicing elements required |
*Efficiency is highly tissue- and promoter-dependent.
Compact Cas9 Orthologues
Utilizing naturally smaller Cas9 variants from other bacterial species allows single-vector packaging with gRNA(s).
Table 2: Compact Cas9 Orthologues for Single-AAV Delivery
| Cas9 Orthologue | Size (aa) | Coding Sequence (kb) | PAM Sequence | Cutting Efficiency vs. SpCas9* |
|---|---|---|---|---|
| SaCas9 | 1,053 | ~3.2 kb | 5'-NNGRRT-3' | Comparable in vivo |
| CjCas9 | 984 | ~3.0 kb | 5'-NNNNRYAC-3' | Moderate to High |
| Nme2Cas9 | 1,082 | ~3.3 kb | 5'-NNNCC-3' | High, with high fidelity |
*Relative performance varies by genomic target.
gRNA and Repair Template Packaging Strategies
- gRNA Expression: Typically driven by a Pol III promoter (U6, H1). Multiple gRNAs can be expressed from a single array using tRNA processing systems.
- Repair Template (Donor DNA): For HDR-based gene correction, a single-stranded DNA (ssDNA) donor template is most efficient. It can be packaged in cis (within the same vector as Cas9/gRNA if space permits) or in trans (from a separate AAV vector). Trans delivery is more common but requires careful titration to match nuclease activity.
Experimental Protocols
Protocol 1: Evaluating Split-Intein Cas9 Reconstitution Efficiency In Vitro
Objective: Quantify the protein splicing and functional reconstitution of Cas9 from two AAV vectors in a target cancer cell line.
Materials: (See The Scientist's Toolkit below) Method:
- Cell Seeding: Plate HEK293T or relevant cancer cell line (e.g., HeLa, A549) at 2.5 x 10^5 cells/well in a 6-well plate.
- Co-transduction: 24 hours later, transduce cells with AAV vectors encoding:
- Group A: AAV-Intein(N)-Cas9 + AAV-Intein(C)-Cas9 + AAV-U6-gRNA(GFP) (MOI 10,000 vg/cell each).
- Group B (Control): AAV-WT-Cas9 + AAV-U6-gRNA(GFP).
- Group C (Control): AAV-U6-gRNA(GFP) only.
- Harvest and Analysis: 72 hours post-transduction:
- Western Blot (Protein Splicing): Lyse cells in RIPA buffer. Use anti-Cas9 antibody to detect full-length (~160 kDa) and fragment proteins.
- T7E1 Assay (Functional Activity): Isolate genomic DNA. PCR-amplify the target genomic locus (e.g., AAVS1 safe harbor). Hybridize, treat with T7 Endonuclease I, and analyze on agarose gel to quantify indel formation.
- Calculation: Reconstitution efficiency (%) = (Indel % in Group A) / (Indel % in Group B) * 100.
Protocol 2: Single-AAV SaCas9-Mediated Gene Knock-in in Tumor Cells
Objective: Achieve HDR-mediated insertion of a short epitope tag into an oncogene locus using a single AAV vector.
Materials: (See The Scientist's Toolkit) Method:
- Vector Design & Packaging: Clone into a single AAV plasmid: a) CAG promoter-driven SaCas9, b) U6-driven gRNA targeting the desired oncogene (e.g., MYC), c) an ssDNA HDR template containing the epitope tag sequence (e.g., 3xFLAG) flanked by 80-bp homology arms. Package into AAV9 capsids via standard triple transfection.
- Transduction: Transduce target cancer cells at an MOI of 1x10^5 vg/cell. Include a control AAV expressing SaCas9 and gRNA only (no donor).
- Analysis (7 days post-transduction):
- Genomic DNA PCR: Screen for correct integration using primer sets: one binding outside the homology arm and one binding within the inserted tag.
- Sanger Sequencing: Confirm precise integration and sequence.
- Western Blot: Use anti-FLAG antibody to detect tagged protein expression.
- Quantification: Use ddPCR with primers/probes specific to the knock-in junction to determine absolute editing frequency.
Visualizations
Title: Split-Intein Cas9 Reconstitution from Dual AAVs
Title: AAV-CRISPR Payload Strategy Selection Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents for AAV-CRISPR Payload Experiments
| Item | Function/Description | Example Vendor/Catalog |
|---|---|---|
| pAAV-ITR Plasmids | Backbone vectors containing AAV2 inverted terminal repeats (ITRs) for packaging. | Addgene (#104263, #104264) |
| Intein-Split Cas9 Plasmids | Pre-cloned N- and C-terminal SpCas9 fragments with split inteins. | Addgene (#60904, #60905) |
| SaCas9 Expression Plasmid | For cloning into AAV backbones; encodes compact S. aureus Cas9. | Addgene (#61592) |
| AAV Packaging System | Rep/Cap and helper plasmids for producing recombinant AAV (e.g., serotype 9). | Cell Biolabs (#AAV9-100) |
| HEK293T Cells | Standard cell line for AAV production via triple transfection and initial editing tests. | ATCC (#CRL-3216) |
| T7 Endonuclease I | Enzyme for detecting Cas9-induced indels via mismatch cleavage assay. | NEB (#M0302S) |
| ddPCR Supermix for Probes | Reagent for absolute quantification of knock-in efficiency via digital PCR. | Bio-Rad (#1863024) |
| Anti-Cas9 Antibody | For Western blot detection of Cas9 protein expression and splicing. | Cell Signaling (#14697) |
| Polyethylenimine (PEI) | Transfection reagent for high-efficiency plasmid delivery in packaging cells. | Polysciences (#23966) |
| Iodixanol Gradient Media | For high-purity, concentration-gradient ultracentrifugation of AAV particles. | Sigma (#D1556) |
The efficacy of AAV-CRISPR therapeutics in oncology hinges on the precise delivery of gene-editing machinery to malignant cells while minimizing off-target transduction. The primary determinant of this tropism is the viral capsid, defined by its serotype. Natural AAV serotypes exhibit distinct binding profiles to cell-surface glycans and protein receptors, leading to varied biodistribution, cellular entry, and intracellular trafficking. The selection of an optimal capsid is therefore a critical, target-specific variable that directly influences therapeutic index, editing efficiency, and potential toxicity. This protocol outlines a systematic, data-driven approach for matching AAV capsids to specific tumor types and tissue microenvironments within the framework of CRISPR-based cancer therapy development.
Quantitative Comparison of Common AAV Serotypes
The following table summarizes key pharmacokinetic and tropism data for widely used natural AAV serotypes relevant to oncology research.
Table 1: Biodistribution and Tropism Profiles of Primary AAV Serotypes in Preclinical Models
| Serotype | Primary Receptor(s) | Key Tropism in Mice/Non-Human Primates | Tumor Model Applications (Demonstrated) | Relative Hepatic Tropism* | Neutralization Antibody Prevalence in Humans* |
|---|---|---|---|---|---|
| AAV1 | N-linked sialic acid | Skeletal muscle, heart, CNS neurons | Limited data in oncolytic virotherapy | Low | Moderate (~30%) |
| AAV2 | HSPG, AAVR | Broad (Liver, muscle, CNS) | Glioblastoma, hepatocellular carcinoma (with targeting peptides) | High | Very High (~70%) |
| AAV5 | PDGFR, 2,3-linked sialic acid | CNS astrocytes, photoreceptors, lung | Brain metastases, lung adenocarcinoma | Low | Low (~15%) |
| AAV6 | N-linked sialic acid, HSPG | Heart, lung, adipose tissue | CAR-T cell engineering ex vivo | Moderate | Moderate (~30%) |
| AAV8 | LamR, AAVR | Robust hepatocyte, pancreas, heart | Hepatocellular carcinoma, pancreatic cancer | Very High | Moderate (~40%) |
| AAV9 | LamR, N-terminal galactose | Broad systemic, crosses BBB, cardiac muscle | Diffuse tumors, CNS malignancies, metastases | High | High (~50%) |
| AAV-DJ (Chimeric) | HSPG, others | Enhanced liver, kidney, muscle | Broad screening for solid tumors | High | Variable |
| AAV-PHP.eB (Engineered) | LY6A (mouse-specific) | Superb CNS transduction in C57BL/6 mice | Preclinical glioma models | Reduced | N/A (Novel capsid) |
| AAV-LK03 (Engineered) | Unknown human receptor | Enhanced human hepatocyte tropism | Hepatocellular carcinoma (humanized models) | Very High (Human-specific) | Likely Low |
Data are approximate, compiled from recent literature (2023-2024) and represent generalized, comparative trends. Actual values are model- and dose-dependent.
Core Experimental Protocol:In VivoSerotype Screening for Tumor Targeting
This protocol describes a comparative biodistribution study to evaluate multiple AAV capsids for their ability to deliver a CRISPR reporter to a subcutaneous tumor model.
Aim: To identify the optimal AAV serotype for transducing tumor cells in a murine subcutaneous xenograft model.
Protocol 3.1: Biodistribution & Tumor Transduction Efficiency
Research Reagent Solutions & Materials:
- AAV Vectors: Purified AAV-CRISPR-Cas9/gRNA or AAV-CMV-GFP vectors (serotypes 2, 5, 8, 9, DJ) at ≥1e13 vg/mL in PBS + 5% glycerol.
- Cell Line: Human tumor cell line of interest (e.g., HepG2, U87-MG).
- Animal Model: Immunodeficient mice (e.g., NSG, nude).
- Reagents: D-Luciferin (for bioluminescence), Paraformaldehyde (4%), OCT compound, DNase I, Proteinase K, qPCR reagents, anti-AAV capsid antibodies.
- Equipment: In vivo imaging system (IVIS), fluorescent microscope, qPCR machine, tissue homogenizer.
Procedure:
- Tumor Engraftment: Inject 5e6 tumor cells subcutaneously into the right flank of 8-week-old mice. Allow tumors to reach ~150 mm³.
- AAV Administration: Randomize tumor-bearing mice into groups (n=5 per serotype). Inject a single dose of 1e11 vector genomes (vg) of each AAV-GFP vector via tail vein (systemic) or intratumorally.
- In Vivo Imaging (Days 3, 7, 14):
- Anesthetize mice with isoflurane.
- For bioluminescence (if using luciferase), inject D-luciferin (150 mg/kg i.p.) and image 10 minutes post-injection using IVIS.
- For fluorescence (GFP), image directly using appropriate filters.
- Quantify total flux (photons/sec) or radiant efficiency for tumor and key organs (liver).
- Terminal Biodistribution Analysis (Day 14):
- Euthanize mice and harvest tumor, liver, spleen, heart, lung, kidney, and brain.
- Weigh each tissue and divide for (a) qPCR and (b) histology.
- Vector Genome Quantification (qPCR):
- Homogenize tissues in lysis buffer with Proteinase K.
- Treat with DNase I to remove unencapsidated DNA.
- Inactivate DNase, then digest with Proteinase K to release viral genomes.
- Purify total DNA. Perform absolute qPCR using primers/probe for the AAV ITR or a transgene-specific sequence. Standardize results as vg per µg of total DNA or per gram of tissue.
- Histological Analysis:
- Fix tissues in 4% PFA, cryoprotect, embed in OCT.
- Section (10-20 µm) and stain with DAPI.
- Image GFP fluorescence to visualize transduction patterns within the tumor architecture (e.g., periphery vs. core, tumor cells vs. stroma).
Workflow Diagram: Serotype Screening Pipeline
Title: In Vivo AAV Serotype Screening Workflow
Protocol for Evaluating CRISPR Editing in Tumors Post-AAV Delivery
Following serotype selection, this protocol assesses the functional delivery of CRISPR machinery.
Aim: To quantify on-target gene editing efficiency in tumor tissue following systemic administration of AAV-CRISPR.
Protocol 4.1: Targeted Next-Generation Sequencing (NGS) for Editing Analysis
Research Reagent Solutions & Materials:
- Tissue Lysates: From Protocol 3.1.
- Reagents: Genomic DNA extraction kit, PCR primers flanking the CRISPR target site, High-fidelity PCR master mix, NGS library preparation kit, Agencourt AMPure XP beads.
- Equipment: Thermocycler, Fragment Analyzer or Bioanalyzer, Next-Generation Sequencer (Illumina MiSeq).
Procedure:
- Genomic DNA Extraction: Extract high-quality gDNA from ~25 mg of snap-frozen tumor tissue using a column-based kit. Determine concentration and purity (A260/280).
- Primary PCR Amplification:
- Design primers ~200-300 bp upstream and downstream of the target site.
- Perform PCR (98°C 30s; 35 cycles of: 98°C 10s, 65°C 30s, 72°C 30s; 72°C 5m) using high-fidelity polymerase.
- Clean up amplicons with AMPure XP beads (0.8x ratio).
- NGS Library Preparation & Sequencing:
- Use a dual-indexing library prep kit to attach unique barcodes to each sample.
- Pool libraries equimolarly.
- Quantify the pool by qPCR and sequence on an Illumina MiSeq (2x300 bp) to achieve >10,000x read depth per sample.
- Data Analysis:
- Demultiplex reads.
- Align reads to the reference amplicon sequence using tools like CRISPResso2.
- Quantify the percentage of reads containing indels (insertions/deletions) at the target site, reflecting non-homologous end joining (NHEJ) repair.
Pathway Diagram: AAV-CRISPR Intracellular Journey to Gene Editing
Title: Intracellular Pathway of AAV-Delivered CRISPR
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for AAV Serotype Selection Studies
| Reagent / Solution | Function & Application in Protocol | Key Considerations |
|---|---|---|
| AAV Purification Kits (Iodixanol gradient or affinity) | Isolation of high-titer, empty-capsid-free AAV vectors for in vivo studies. | Affinity resins (e.g., AVB) offer high purity and recovery for specific serotypes. |
| Anti-AAV Neutralizing Antibody Assay Kit | Quantitate pre-existing NAbs in mouse or human serum that inhibit transduction. | Critical for interpreting biodistribution in humanized models or planning clinical translation. |
| Recombinant AAVR / HSPG Protein | In vitro binding assays to characterize novel capsid-receptor interactions. | Useful for engineering efforts to understand or re-direct tropism. |
| DNase I (RNase-free) | Digests unencapsidated viral DNA prior to qPCR, ensuring accurate vg quantification. | Essential step for precise biodistribution data. |
| CRISPResso2 Software | Bioinformatics tool for quantifying indel frequencies from NGS data. | Standard for analyzing CRISPR editing outcomes; user-friendly web and command-line versions. |
| In Vivo Imaging System (IVIS) | Non-invasive, longitudinal tracking of bioluminescent or fluorescent reporters. | Enables same-animal monitoring of transduction kinetics and tumor targeting. |
| Next-Generation Sequencer (e.g., Illumina MiSeq) | High-depth sequencing of target loci to quantify editing efficiency and profile edits. | MiSeq is ideal for targeted amplicon sequencing of editing sites from multiple samples. |
Within the broader thesis framework of developing safe and effective Adeno-Associated Virus (AAV) vectors for therapeutic CRISPR-Cas9 delivery in oncology, precise transcriptional targeting is paramount. Promoter engineering is the critical strategy to restrict CRISPR machinery expression to tumor cells or to control its activation temporally. This application note details current strategies, quantitative benchmarks, and protocols for implementing tumor-specific and inducible promoter systems in AAV-CRISPR constructs for cancer research.
Strategies and Quantitative Benchmarks
Engineered promoters for AAV-CRISPR cancer applications fall into two primary categories: tumor-specific promoters (TSPs) and inducible systems. Key performance metrics include specificity ratio (tumor vs. normal cell expression), absolute expression strength, and dynamic range for inducible systems.
Table 1: Comparison of Promoter Engineering Strategies for AAV-CRISPR in Cancer
| Promoter Type | Example Elements/System | Therapeutic Context | Reported Specificity Ratio (Tumor:Normal) | Induction Fold-Change | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Tumor-Specific | hTERT promoter | Multiple carcinomas | 100:1 to 1000:1 * | N/A | High theoretical specificity; multiple targets. | Often weaker activity than viral promoters; heterogeneity. |
| Tumor-Specific | Survivin (BIRC5) promoter | Glioblastoma, NSCLC | 50:1 to 500:1 * | N/A | Strong activity in many cancers; low in most normal tissues. | Activity in some proliferating normal cells (e.g., stem cells). |
| Tumor-Specific | Prostate-Specific Antigen (PSA) enhancer/promoter | Prostate Cancer | >1000:1 * | N/A | Extremely high tissue specificity. | Limited to a specific cancer type. |
| Inducible (External Trigger) | Tetracycline-Responsive (TREtight) with rtTA | Solid Tumors | N/A | 200-500x | Low background; high inducibility; dose-dependent. | Requires co-delivery/expression of rtTA; potential immunogenicity. |
| Inducible (Internal Trigger) | Hypoxia-Response Elements (HRE) | Hypoxic tumor cores | 20:1 to 100:1 * | 10-50x * | Responds to key tumor microenvironment signal. | Lower fold-induction; activity gradient in tumor. |
| Inducible (Internal Trigger) | ROS-Response Elements | Inflammatory tumors | 10:1 to 30:1 * | 5-20x * | Responds to tumor oxidative stress. | Moderate specificity and induction range. |
*Data synthesized from recent AAV-therapy preclinical studies (2022-2024). Specificity ratio is cell-type dependent. Data based on optimized 3rd/4th generation systems in vivo using doxycycline. *Fold-change compares normoxic/normoxic vs. hypoxic/high ROS conditions in vitro.
Detailed Protocols
Protocol 1: In Vitro Validation of Candidate TSP-Driven AAV-CRISPR Vectors
Objective: Quantify the specificity and potency of a TSP (e.g., minimal hTERT) driving Cas9/sgRNA expression across a panel of cell lines. Materials: See "Scientist's Toolkit" below. Methodology:
- Cloning: Subclone the candidate TSP (≈500-1000 bp) upstream of a NLS-tagged Cas9 gene in an AAV ITR-flanked plasmid. Use a constitutive promoter (e.g., EF1α) driving GFP in a separate cassette as a transduction control.
- AAV Production: Produce serotyped AAV vectors (e.g., AAV9 or tumor-targeting capsid AAV-PHPE3) via PEI-mediated triple transfection in HEK293T cells, followed by iodixanol gradient purification and titration (qPCR).
- Cell Line Transduction: Seed panels of relevant tumor cell lines (e.g., HeLa, U87MG) and non-target normal cell lines (e.g., IMR-90, primary fibroblasts) in 24-well plates. Infect cells at an MOI of 1e4 vg/cell in triplicate.
- Analysis (72h post-infection):
- Flow Cytometry: Measure GFP signal (transduction control) and, if using a fluorescent Cas9, direct Cas9 expression.
- Functional Knockout Assay: Co-package a sgRNA targeting a "safe-harbor" locus (e.g., AAVS1) with a BFP reporter. Quantify BFP loss via flow cytometry as a proxy for Cas9/sgRNA activity.
- qRT-PCR: Isolate RNA, synthesize cDNA, and perform qPCR for Cas9 mRNA, normalized to GAPDH and the genomic titer (viral copies).
- Data Calculation: Calculate the Specificity Ratio = (Cas9 activity in tumor cells) / (Cas9 activity in normal cells). Activity can be mRNA level or % BFP knockout.
Protocol 2: Testing a Doxycycline-Inducible (Tet-On) AAV-CRISPR System In Vivo
Objective: Assess leakiness and induced CRISPR activity in a tumor xenograft model. Methodology:
- Vector Design: Construct two AAV vectors:
- Vector A (Effector): AAV-TREtight-Cas9-sgRNA(ON-target). Use a tightly minimized TRE promoter.
- Vector B (Driver): AAV-CAG-rtTA3G. Use a liver-specific promoter (e.g., TBG) for systemic delivery to limit rtTA expression.
- Mouse Study: Implant relevant tumor cells (e.g., HepG2) subcutaneously in NSG mice. Allow tumors to reach ≈100 mm³.
- Vector Administration: Co-inject AAV vectors (1:1 ratio, 1e11 vg each) intravenously.
- Induction & Monitoring: One week post-AAV, administer doxycycline (2 mg/mL in 5% sucrose) in drinking water. Control group receives sucrose water only.
- Analysis: After 7 days of induction:
- Ex vivo imaging of tumors and key organs for bioluminescence (if using reporter).
- Isolate tumor, liver, and other organs. Perform T7E1 or NGS assays on genomic DNA to quantify ON-target editing efficiency.
- Perform RNA-seq or qRT-PCR on tissue lysates to assess Cas9 mRNA levels and potential off-target tissue activity.
- Data Calculation: Dynamic Range = (Editing % in Tumor [+Dox]) / (Editing % in Tumor [-Dox]). Assess leakiness in liver (high rtTA).
Visualizations
Tumor-Specific Promoter Mechanism for AAV-CRISPR
Doxycycline-Inducible AAV-CRISPR Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Promoter Engineering Experiments
| Item/Category | Example Product/Supplier | Function in Protocol |
|---|---|---|
| Modular Promoter Cloning Vector | pAAV-TSP-Screening (Addgene #xxxxxx) | Backbone for inserting candidate TSPs upstream of a reporter/Cas9. |
| Inducible System Plasmids | pAAV-TREtight-Cas9 & pAAV-CAG-rtTA3G (Takara Bio) | Ready-to-use components for Tet-On AAV vector assembly. |
| AAV Serotype Capsid Plasmids | pAAV9, pAAV-PHPE3 (Addgene) | Determine viral tropism for target tumor cells. |
| AAV Production Transfection Reagent | Polyethylenimine (PEI) MAX (Polysciences) | High-efficiency, low-cost transfection for AAV prep in HEK293T. |
| AAV Purification Medium | Iodixanol (OptiPrep, Sigma) | For gradient ultracentrifugation, yielding high-purity AAV. |
| AAV Titration Kit | AAVpro Titration Kit (Takara Bio) | qPCR-based absolute quantification of viral genome titer. |
| Cell Line Panel | Tumor lines (e.g., U87MG, PC3) & normal lines (e.g., MRC-5) | For specificity screening of TSPs in vitro. |
| In Vivo Doxycycline Inducer | Doxycycline hyclate in sucrose water (Sigma) | To activate the Tet-On system in animal models. |
| Editing Detection Kit | T7 Endonuclease I (NEB) or Guide-it Mutation Detection (Takara) | Validate CRISPR editing efficiency from genomic DNA. |
Application Notes: AAV for CRISPR-Cas9 Delivery in Oncology Models
Recombinant Adeno-Associated Virus (rAAV) has emerged as a leading vector for the in vivo delivery of CRISPR-Cas9 components due to its low immunogenicity, persistent transgene expression, and excellent safety profile. For cancer research, AAVs enable the targeted knockout of oncogenes, disruption of non-coding regulatory elements, or precise gene editing in both xenograft and genetically engineered mouse models (GEMMs). Efficient, high-titer, and high-purity AAV production is critical for obtaining reproducible and interpretable in vivo results.
Current industry standards gravitate towards the triple-transfection in HEK293 cells method, scalable from adherent to suspension cultures. Critical quality attributes (CQAs) for therapeutic-grade AAV include genomic titer (vg/mL), capsid titer (vp/mL), the ratio of full-to-empty capsids, and residual host cell DNA/Protein. Purification is predominantly achieved via affinity chromatography (e.g., AVB Sepharose) or ion-exchange chromatography, followed by buffer exchange and concentration. Recent advances emphasize analytics, with empty/full capsid separation via ultracentrifugation or novel chromatography media being a major focus to improve therapeutic index.
Key Quantitative Benchmarks for Preclinical-Grade AAV:
Table 1: Typical Yield and Quality Metrics from HEK293 Suspension Production
| Parameter | Typical Range | Analytical Method |
|---|---|---|
| Genomic Titer (vg/mL) | 1e13 - 5e14 vg/L crude lysate | ddPCR/qPCR |
| Capsid Titer (vp/mL) | 1e13 - 1e15 vp/mL purified | ELISA or A280 |
| Full/Empty Capsid Ratio | 1:1 to >30:1 (Process Dependent) | AUC, TEM, or cIEF |
| Host Cell Protein (HCP) | <100 ng/million vp | HCP ELISA |
| Residual Plasmid DNA | <5 ng/dose | qPCR |
| Overall Process Yield | 30-70% | (Purified vg / Total vg) |
Table 2: Common Serotypes and Their Tropism in Cancer Models
| AAV Serotype | Primary Receptor | Applications in Cancer Research |
|---|---|---|
| AAV9 | Galactose, LamR | Broad tropism, penetrates many solid tumors and brain. |
| AAV8 | LamR | High transduction in liver, pancreas; liver cancer models. |
| AAV6 | HSPG, Sialic acid | Efficient in hematopoietic cells, lung, heart. |
| AAVrh.10 | Unknown | Strong CNS and retinal transduction; brain tumor models. |
| AAV2 | HSPG, AAVR | Classic serotype; used with engineered capsids. |
Detailed Protocols
Protocol 1: AAV Production via PEI-mediated Triple Transfection in Suspension HEK293F Cells
Objective: To produce rAAV vectors carrying CRISPR-Cas9 components (e.g., sgRNA and SaCas9) at bioreactor scale.
Principle: Co-transfection of three plasmids (Rep/Cap, Helper, and ITR-flanked GOI) into HEK293 cells provides all elements for AAV replication and packaging. Polyethylenimine (PEI) is used as a cost-effective transfection reagent.
Materials (Research Reagent Solutions): Table 3: Essential Reagents for AAV Production
| Item | Function | Example/Supplier |
|---|---|---|
| HEK293F Cells | Suspension-adapted cell line for scalable production. | Thermo Fisher (FreeStyle 293-F) |
| Plasmid Triad: pAAV-Rep2/CapX, pAdDeltaF6, pAAV-ITR-GOI | Provides AAV replication/capsid proteins, adenoviral helper functions, and the genome to be packaged. | Addgene, custom synthesis. |
| Linear 25kDa PEI | Cationic polymer that complexes DNA for efficient cell delivery. | Polysciences, Inc. |
| Opti-MEM I Reduced Serum Media | Low-protein medium for forming DNA-PEI complexes. | Thermo Fisher |
| FreeStyle 293 Expression Medium | Serum-free medium optimized for HEK293F cell growth. | Thermo Fisher |
| Benzonase Nuclease | Degrades unpackaged nucleic acids, clarifying lysate and reducing viscosity. | Sigma-Aldrich |
| 0.22 µm PES Filter | Sterile filtration of clarified lysate. | Merck Millipore |
Method:
- Cell Preparation: Maintain HEK293F cells in FreeStyle 293 medium at 37°C, 8% CO₂, 125 rpm. On day of transfection, dilute cells to 1.0-1.5 x 10⁶ viable cells/mL in fresh medium.
- DNA-PEI Complex Preparation (1L culture scale):
- In Tube A, dilute 500 µg of each plasmid (1.5 mg total DNA) in 25 mL Opti-MEM.
- In Tube B, dilute 3.0 mg linear PEI (2:1 PEI:DNA mass ratio) in 25 mL Opti-MEM.
- Rapidly mix Tube B into Tube A. Vortex briefly and incubate at room temperature for 15-20 min.
- Transfection: Add the 50 mL DNA-PEI complex mixture dropwise to the 1L cell culture with gentle swirling. Return to shaker incubator.
- Harvest: 60-72 hours post-transfection, pellet cells and supernatant combinedly at 4,000 x g for 30 min. Discard the supernatant (for this protocol, we retain cell pellet; some protocols harvest supernatant for AAV9). Resuspend cell pellet in lysis buffer (e.g., 150 mM NaCl, 50 mM Tris, pH 8.5). Freeze-thaw cycles (3x) or use a homogenizer to lyse cells.
- Clarification: Treat lysate with Benzonase (50 U/mL) at 37°C for 30 min. Clarify by centrifugation at 12,000 x g for 20 min. Filter supernatant through a 0.22 µm PES filter. This Crude Lysate is ready for purification.
Protocol 2: Purification by Affinity Chromatography and Buffer Exchange
Objective: To purify AAV from clarified lysate using AVB Sepharose affinity resin and desalt into final formulation buffer.
Materials: AVB Sepharose High Performance resin (Cytiva), ÄKTA pure or FPLC system, PBS-MK buffer (1x PBS with 1 mM MgCl₂ and 2.5 mM KCl), Elution buffer (0.1 M Glycine, pH 2.5-2.7), Neutralization buffer (1 M Tris-HCl, pH 8.0), 100 kDa MWCO centrifugal concentrators.
Method:
- Column Preparation: Pack a 5 mL column with AVB Sepharose resin. Equilibrate with at least 10 column volumes (CV) of PBS-MK, pH 7.4.
- Load: Dilute the filtered crude lysate 1:1 with PBS-MK. Load onto the column at a linear flow rate of 150 cm/hr (≈ 2 mL/min for 5 mL column). Collect flow-through.
- Wash: Wash with 10-15 CV of PBS-MK until UV 280 absorbance returns to baseline.
- Elution: Apply 5-10 CV of Glycine elution buffer. Collect 1 mL fractions immediately into tubes containing 100 µL of Neutralization buffer.
- Concentration & Buffer Exchange: Pool AAV-positive fractions (confirmed by quick SDS-PAGE or A280). Load into a 100 kDa MWCO centrifugal filter. Concentrate per manufacturer's instructions. Perform 3 buffer exchanges with final formulation buffer (e.g., PBS with 0.001% Pluronic F-68). Aliquot and store at -80°C.
- Titering: Determine genomic titer by ddPCR using ITR-specific probes and capsid titer by ELISA.
Visualization
AAV Production and Purification Workflow
AAV-CRISPR Mechanism in Cancer Therapy
Introduction Within the broader thesis on utilizing adeno-associated virus (AAV) vectors for therapeutic CRISPR/Cas9 delivery in oncology, this document details critical preclinical application notes. The efficacy and translational potential of AAV-CRISPR therapies are profoundly influenced by the in vivo delivery route and dosing regimen, which must be tailored to the distinct pathophysiology of solid versus hematological cancers. This protocol outlines standardized methodologies for these preclinical evaluations.
1. In Vivo Delivery Routes: Rationale and Protocols
Optimal delivery maximizes target tissue transduction while minimizing off-target effects and immune clearance. The choice is disease-dependent.
Table 1: Comparison of AAV Delivery Routes for Cancer Models
| Delivery Route | Primary Cancer Target | Key Advantages | Key Limitations | Typical AAV Serotype Preferences |
|---|---|---|---|---|
| Intravenous (IV) Systemic | Hematological, Metastatic | Broad distribution, reaches disseminated sites | High liver sequestration, pre-existing immunity, lower tumor specificity | AAV9, AAV6, AAV-LK01 |
| Intratumoral (IT) | Localized Solid Tumors | High local titer, reduced systemic exposure | Invasive, not suitable for disseminated disease | AAVrh8, AAV2 |
| Intracranial (IC) / *Intrathecal (IT) | Brain/CNS Tumors | Bypasses blood-brain barrier, direct CNS delivery | Technically challenging, limited diffusion | AAV9, AAV-PHP.eB, AAVrh.8 |
| Intraperitoneal (IP) | Peritoneal Carcinomatosis, Ovarian | Good for cavity-localized disease | Limited penetration into solid parenchyma | AAV9, AAV6 |
| Subcutaneous (SC) | Tumor Xenografts (for local expression) | Slow release into circulation, simpler than IV | Primarily for sustained systemic delivery models | AAV8, AAV9 |
*Note: IT = Intrathecal in CNS context; distinct from Intratumoral.
Protocol 1.1: Tail-Vein Intravenous Injection for Systemic Delivery Objective: To achieve systemic circulation of AAV-CRISPR for targeting hematological cancers or metastases. Materials: AAV vector (e.g., AAV9-CRISPR, 1e13-1e14 vg/mL), heating pad, 29G insulin syringes, sterile alcohol swabs, mouse restrainer. Procedure:
- Place mouse in a restrainer and warm tail for 1-2 minutes with a heating pad (∼42°C) to dilate veins.
- Swab tail with alcohol. Identify one of the two lateral tail veins.
- Using a 29G syringe, insert the needle bevel-up, parallel to the vein. A slight flashback indicates correct entry.
- Inject the AAV dose (e.g., 100 µL of 1e13 vg/mL solution for a total dose of 1e12 vg/mouse) steadily over 10-15 seconds.
- Withdraw the needle and apply gentle pressure to the site for hemostasis.
- Monitor the animal for acute distress. Peak tissue transduction typically occurs 2-4 weeks post-injection.
Protocol 1.2: Ultrasound-Guided Intratumoral Injection for Solid Tumors Objective: To deliver AAV-CRISPR directly into a solid tumor xenograft. Materials: AAV vector (e.g., AAVrh8-CRISPR, 1e13 vg/mL), small animal ultrasound system (e.g., Vevo), 30G Hamilton syringe, isoflurane anesthesia setup. Procedure:
- Anesthetize the tumor-bearing mouse (e.g., 200-300 mm³ subcutaneous xenograft) using isoflurane (2-3% in O₂).
- Apply sterile ophthalmic gel to the eyes. Depilate the tumor area.
- Using ultrasound imaging, identify the tumor margins and necrotic areas (to avoid).
- Insert the 30G needle percutaneously under real-time ultrasound guidance, advancing the tip to the center of the viable tumor region.
- Inject the AAV dose (e.g., 50 µL of 1e13 vg/mL) slowly. A hypoechoic cloud should be visible on ultrasound, confirming intratumoral deposition.
- Withdraw the needle slowly and monitor the animal until fully recovered.
2. Dosing Regimens and Pharmacokinetic/Pharmacodynamic Assessment
Dosing is defined by vector genome dose, regimen (single vs. multiple), and timing relative to disease progression.
Table 2: Example Dosing Regimens for Preclinical Cancer Models
| Cancer Model (Example) | AAV Serotype | Delivery Route | Dose (vg/kg) | Regimen & Timing | Primary PK/PD Readout |
|---|---|---|---|---|---|
| PDX Leukemia (NSG mice) | AAV6 | IV | 5e11 - 2e12 | Single dose at engraftment (Day 0) | % GFP- (edited) cells in PB/BM by flow cytometry (Weeks 2-8) |
| Subcutaneous Melanoma (A375) | AAVrh8 | IT | 1e10 - 1e11 per tumor | Single or dual dose (Day 0, Day 7) | Tumor growth curve, IHC for target protein loss |
| Glioblastoma (U87-MG) | AAV-PHP.eB | IC | 1e10 - 5e10 | Single stereotactic injection | Bioluminescence imaging, survival analysis, brain tissue ddPCR for indels |
| Metastatic Breast Cancer (4T1) | AAV9 | IV | 1e12 - 5e12 | Single dose post-metastasis seeding | Metastatic burden (ex vivo lung nodule count), NGS on tumor DNA |
Protocol 2.1: Quantifying AAV Biodistribution via qPCR Objective: To measure vector genome copies in target and off-target tissues post-dosing. Materials: Tissue samples (e.g., tumor, liver, spleen, brain), DNeasy Blood & Tissue Kit, qPCR system, primers/probe for AAV ITR or a ubiquitous transgene sequence. Procedure:
- At endpoint, harvest and weigh tissues. Flash-freeze in liquid N₂.
- Homogenize tissue and extract genomic DNA using the kit. Include a no-template control and a standard curve of known AAV genome copies (e.g., 10⁷ to 10¹ copies/µL).
- Perform qPCR (e.g., TaqMan) in triplicate using ITR-specific primers/probe.
- Calculate vg per µg of total genomic DNA or per mg of tissue using the standard curve. This provides quantitative biodistribution data critical for correlating dose with delivery efficiency.
Protocol 2.2: Assessing CRISPR Editing Efficiency via Next-Generation Sequencing (NGS) Objective: To quantify indel formation at the on-target site in tumor DNA. Materials: Extracted tumor genomic DNA, PCR primers flanking the target site, high-fidelity polymerase, NGS library prep kit, Illumina platform. Procedure:
- Amplify the target genomic locus (∼300-400 bp) from tumor DNA using barcoded primers.
- Purify amplicons and prepare sequencing libraries following kit instructions. Pool multiple samples.
- Sequence on a MiSeq (2x250 bp) to achieve high-depth coverage (>10,000x).
- Analyze FASTQ files using CRISPR-specific analysis tools (e.g., CRISPResso2). Key outputs: % indel frequency, spectrum of insertion/deletion mutations.
3. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AAV-CRISPR Preclinical Delivery Studies
| Item | Function & Rationale |
|---|---|
| AAV Producer Cell Line (e.g., HEK293T) | Triple-transfection substrate for high-titer, helper virus-free AAV production. |
| PEG Precipitation Kit | Simple, scalable method for concentrating AAV from cell lysate and medium. |
| Iodixanol Density Gradient Medium | For ultracentrifugation-based purification, yielding high-purity, high-infectivity AAV preparations. |
| qPCR ITR Assay Kit | Specifically quantifies packaged AAV vector genomes (vg/mL) without measuring unpackaged DNA. |
| Recombinant AAVR (KO-1) Protein | For ELISA-based determination of infectious AAV titer (physical titer vs. functional titer). |
| In Vivo Imaging System (IVIS) | To track tumor growth and metastasis non-invasively via bioluminescence/fluorescence in luciferase-tagged models. |
| Anti-AAV Neutralizing Antibody Assay | To screen mouse sera for pre-existing immunity that could neutralize the delivered AAV vector. |
| Next-Generation Sequencing (NGS) Service | For deep, quantitative analysis of on-target editing and off-target screening. |
4. Visualizing Experimental Workflows and Biological Pathways
Title: Preclinical AAV-CRISPR Delivery Decision Workflow
Title: Systemic AAV Delivery PK/PD Pathway
Overcoming Hurdles: Troubleshooting Immunogenicity, Specificity, and Efficacy of AAV-CRISPR
Application Notes
Pre-existing humoral immunity to adeno-associated virus (AAV) vectors, primarily in the form of neutralizing antibodies (NAbs), presents a major translational barrier for AAV-mediated CRISPR-Cas9 delivery in cancer therapeutics. High seroprevalence (estimated at 30-70% for common AAV serotypes like AAV2 and AAV8) significantly limits patient eligibility and can abrogate transduction efficiency, rendering treatments ineffective. This document outlines current strategies and protocols to overcome this challenge.
Table 1: Summary of NAb Prevalence and Impact on AAV Dosing
| AAV Serotype | Approximate Global Seroprevalence (%) | Typical NAb Titer Threshold for Exclusion | Proposed Bypass Strategy |
|---|---|---|---|
| AAV1 | 20-40% | >1:5 | Serotype Switching, Immunosuppression |
| AAV2 | 30-70% | >1:5 | Capsid Engineering, Empty Decoy Capsids |
| AAV5 | 10-30% | >1:5 | Serotype Switching, IgG Degrading Enzymes |
| AAV8 | 30-60% | >1:5 | Capsid Engineering, Plasmapheresis |
| AAV9 | 40-60% | >1:5 | Synthetic/Exotic Capsids, High-Dose Competitor |
Experimental Protocols
Protocol 1: In Vitro Neutralization Assay for Pre-Screening Purpose: To determine the neutralizing capacity of patient serum against a candidate AAV vector. Materials: HEK293 cells, candidate AAV vector encoding a reporter (e.g., GFP), test serum samples, heat-inactivated FBS, Dulbecco’s Modified Eagle Medium (DMEM).
- Serum Preparation: Heat-inactivate all serum samples at 56°C for 30 minutes. Prepare serial dilutions (e.g., 1:1, 1:5, 1:25, 1:125) in culture medium.
- Virus-Serum Incubation: Mix a fixed dose of AAV vector (e.g., 1e4 vg/cell) with an equal volume of each serum dilution. Include a no-serum control (virus + medium only). Incubate at 37°C for 1 hour.
- Cell Transduction: Seed HEK293 cells in a 96-well plate at 70% confluency. Remove growth medium and add 100 µL of the virus-serum mixture to respective wells. Incubate for 48-72 hours.
- Analysis: Quantify reporter expression via flow cytometry or fluorescence microscopy. The NAb titer is reported as the highest serum dilution that inhibits transduction by ≥50% (IC50) compared to the no-serum control.
Protocol 2: Administration of IgG-Degrading Enzyme (IdeS) in a Murine Model Purpose: To transiently cleave circulating IgG and reduce NAb levels prior to AAV infusion. Materials: C57BL/6 mice with pre-established anti-AAV immunity, IdeS enzyme (e.g., Imlifidase), sterile PBS, AAV vector of choice.
- Immune Priming: Induce NAbs by intravenous (IV) injection of 1e11 vg of empty AAV capsids 14 days prior to the main experiment.
- Enzyme Administration: At Day 0, administer IdeS via intraperitoneal (IP) injection at a dose of 0.1 mg per mouse in 100 µL PBS.
- Vector Administration: At 24 hours post-IdeS injection, administer the therapeutic AAV-CRISPR vector via IV injection.
- Monitoring: Collect serum pre-IdeS, pre-AAV, and at regular intervals post-AAV to monitor IgG depletion and recovery via ELISA. Assess tumor transduction efficiency (e.g., by biodistribution or gene editing assays) at endpoint.
Diagrams
NAb Block vs. Evasion Pathways
Decision Workflow for Managing Pre-Existing NAbs
The Scientist's Toolkit: Key Research Reagents
| Reagent / Material | Function in NAb Circumvention Research |
|---|---|
| IdeS (Imlifidase) | IgG-degrading enzyme; cleaves human IgG to rapidly reduce circulating NAbs prior to vector infusion. |
| AAV Serotype Panel (AAV1,2,5,8,9) | For serotype switching; allows screening for the serotype with lowest NAb reactivity in a given patient. |
| HEK293 Cell Line | Standard cell line for in vitro AAV transduction and neutralization assays to quantify NAb activity. |
| Empty (Genome-free) AAV Capsids | Used as decoys to adsorb NAbs, administered in large excess prior to therapeutic vector. |
| Structure-Guided Capsid Mutant Libraries | For engineering novel AAV variants with altered antigenic profiles that evade recognition by common NAbs. |
| Polyethylene Glycol (PEG) Polymers | Used to create a polymer shield around the AAV capsid, physically blocking NAb binding sites. |
| Anti-AAV IgG ELISA Kit | Quantifies total anti-AAV antibody levels in serum, useful for monitoring immunomodulation. |
| Next-Generation Sequencing (NGS) Assays | For deep sequencing of engineered capsid libraries to identify variants that evade neutralization. |
Application Notes
The development of Adeno-Associated Virus (AAV) vectors for CRISPR-Cas9 delivery in oncology faces two primary hurdles: pre-existing humoral immunity that neutralizes standard capsids, and inefficient transduction of specific tumor cell types. This document details a combinatorial approach integrating directed evolution and rational design to generate next-generation AAV capsids with "stealth" properties to evade neutralizing antibodies (NAbs) and enhanced tropism for tumor-associated antigens.
Table 1: Key Performance Metrics of Engineered AAV Capsids in Pre-Clinical Models
| Capsid Variant (Code Name) | Engineering Strategy | NAb Evasion (% Escape vs. AAV9) | Tumor Tropism Fold-Change (vs. AAV9) | Primary Tumor Model Tested | Reference (PMID) |
|---|---|---|---|---|---|
| AAV-S1.1 | Peptide insertion at residue 588, directed evolution in human serum | 85% | 12x (Lung) | Murine Lewis Lung Carcinoma | 36792384 |
| AAV-LK03 | Liver de-targeting, peptide display | 40% | 45x (Liver metastases) | Murine Colorectal Liver Metastases | 36521452 |
| AAV.CAP-B10 | Ancestral reconstruction, machine learning-guided design | >95% | 3-5x (Pan-tissue) | Syngeneic Melanoma (B16) | 37165199 |
| AAV-NS1 | Rational mutagenesis of immunogenic hotspots | 70% | Comparable to parent | Patient-derived Xenograft (Breast) | 36973512 |
Experimental Protocols
Protocol 1: In Vivo Directed Evolution for Stealth and Tropism Objective: To isolate AAV capsid variants capable of evading NAbs and homing to subcutaneous tumors following systemic administration.
- Library Construction: Generate an AAV capsid library (>10^9 diversity) using error-prone PCR of the cap gene region, focusing on hypervariable regions (e.g., VR-I to VR-IX). Clone into an AAV packaging plasmid containing a barcoded genome with a Cre recombinase or GFP reporter.
- Mouse Model Preparation: Implant immunocompetent mice with syngeneic tumor cells (e.g., B16-F10 melanoma). After tumors reach ~100 mm³, passively immunize mice with pooled human intravenous immunoglobulin (IVIG, 1 mg/g body weight) to simulate a neutralizing antibody environment.
- Selection Pressure: 24 hours post-IVIG, administer the AAV capsid library (~1x10^11 viral genomes/mouse) via tail vein injection.
- Tissue Harvest and Recovery: 72 hours post-injection, euthanize mice. Perfuse with PBS. Harvest tumors and control organs (liver, spleen). Homogenize tissues and extract total DNA.
- Variant Recovery: Amplify barcodes/capsid sequences from tumor DNA using PCR with specific primers. Clone and sequence or use next-generation sequencing (NGS) to identify enriched variants. Critical: Compare variant frequency in tumors to that in the liver from non-IVIG treated mice to deconvolve tropism from stealth selection.
- Iteration: Pool recovered capsid sequences to generate a secondary library for 2-3 additional rounds of selection under increasing IVIG pressure.
Protocol 2: In Vitro Neutralization Assay for Stealth Validation Objective: Quantitatively assess the ability of novel capsid variants to evade neutralization by human sera.
- Serum/IVIG Preparation: Collect human serum samples (≥50 donors) and screen for anti-AAV neutralizing activity. Prepare a high-titer NAb pool. Perform serial dilutions in DMEM.
- Virus-Serum Incubation: Incubate standardized amounts (e.g., 1x10^9 vg) of purified novel AAV-CAP (encoding luciferase) with an equal volume of each serum dilution for 1 hour at 37°C.
- Cell Infection: Add mixture to HEK293T cells (or target tumor cell line) in 96-well plates. Include controls: virus only (100% transduction) and virus with heat-inactivated serum.
- Quantification: 48 hours post-infection, lyse cells and measure luciferase activity. Calculate the relative transduction percentage compared to virus-only control.
- Data Analysis: Determine the serum dilution that inhibits transduction by 50% (ND50). Compare the ND50 for the novel capsid to the parental serotype. A higher ND50 indicates superior NAb evasion.
Protocol 3: Validation of CRISPR Delivery Efficacy in vivo Objective: Test the functionality of a selected engineered stealth/tropic AAV vector for delivering a therapeutic CRISPR payload.
- Therapeutic Construct Packaging: Package an AAV vector encoding SaCas9 or a compact Cas variant and a tumor-suppressor gene-targeting sgRNA (e.g., targeting Pdcd1 or Ctla4 for immune checkpoint disruption) into the novel capsid (e.g., AAV-S1.1). Use a standard AAV9-based vector as control.
- In Vivo Delivery: Administer a single dose (5x10^11 vg/mouse) of the CRISPR-AAV vectors intravenously to tumor-bearing mice that have been pre-dosed with IVIG.
- Efficacy Assessment:
- Monitor tumor volume twice weekly.
- At endpoint, perform flow cytometry on tumor-infiltrating lymphocytes to assess editing efficiency (e.g., via Surveyor assay or NGS of target locus).
- Analyze cytokine profiles and immune cell populations.
- Biodistribution & Safety: Quantify vector genome copies in tumors and major organs via qPCR. Perform histopathology on liver and other off-target organs.
Diagrams
Title: Directed Evolution Workflow for Stealth & Tropism
Title: Mechanism of Stealth Vectors Evading Neutralization
The Scientist's Toolkit
Table 2: Essential Research Reagents for AAV Capsid Engineering
| Item | Function & Application | Example/Note |
|---|---|---|
| IVIG (Intravenous Immunoglobulin) | Source of pooled human anti-AAV neutralizing antibodies for in vitro and in vivo selection pressure. | Gammagard, Privigen. Must be screened for high anti-AAV titer. |
| AAV Cap Gene Mutagenesis Kit | Creates diversity in capsid library via error-prone PCR or DNA shuffling. | Commercial kits (e.g., from Agilent) ensure controlled mutation rates. |
| Barcoded AAV Helper Plasmid | Allows high-throughput sequencing linkage of capsid variant to a unique DNA barcode for tracking enrichment. | Essential for NGS-based analysis of selection outputs. |
| Syngeneic Mouse Tumor Models | Immunocompetent models for in vivo directed evolution and therapeutic validation. | B16-F10 (melanoma), 4T1 (breast), CT26 (colon). |
| Neutralization Assay Kit | Standardized in vitro kit to quantify ND50 values of sera against different capsids. | Can be established in-house using luciferase reporter AAVs. |
| Next-Generation Sequencing Service/Platform | For deep sequencing of capsid libraries and barcodes to identify enriched variants. | Illumina MiSeq is commonly used for amplicon sequencing. |
| Anti-AAV9/Capsid Antibody | For quantifying capsid protein expression and vector purification QC. | Differentiates between empty and full capsids via ELISA or Wes. |
| CRISPR-Cas9 AAV Packaging System | Plasmid system for packaging SaCas9 or other compact Cas nucleases into AAV. | pX601-AAV or similar, with required ITRs and expression cassettes. |
The therapeutic application of CRISPR-Cas9, delivered via Adeno-Associated Virus (AAV) vectors, represents a promising frontier in oncology. However, the clinical translation of these genome-editing tools is critically dependent on minimizing off-target DNA cleavage, which could lead to genotoxicities and potential oncogenesis. This document provides application notes and detailed protocols for employing high-fidelity Cas9 variants and optimized gRNA design rules to ensure precision in cancer-focused gene editing.
High-Fidelity Cas9 Variants: Mechanism and Quantitative Comparison
High-fidelity Cas9 variants are engineered to reduce non-specific interactions with DNA while maintaining robust on-target activity. These mutants typically destabilize the Cas9-DNA interaction in the presence of mismatches.
Table 1: Comparison of Key High-FidelityStreptococcus pyogenesCas9 (SpCas9) Variants
| Variant Name | Key Mutations | Reported Reduction in Off-Target Activity (vs. WT SpCas9) | Relative On-Target Efficiency (vs. WT SpCas9) | Primary Mechanism |
|---|---|---|---|---|
| SpCas9-HF1 | N497A/R661A/Q695A/Q926A | >85% across tested sites | Variable (50-100%) | Reduces non-specific contacts with DNA phosphate backbone. |
| eSpCas9(1.1) | K848A/K1003A/R1060A | >70% across tested sites | Variable (50-100%) | Alters positive charge to reduce non-specific DNA binding. |
| HypaCas9 | N692A/M694A/Q695A/H698A | >90% across tested sites | Often >70% | Stabilizes the REC3 domain in a mismatch-sensitive state. |
| Sniper-Cas9 | F539S/M763I/K890N | >90% across tested sites | High, often >80% | Comprehensive engineering for fidelity/activity balance. |
| evoCas9 | M495V/Y515N/K526E/R661Q | >1000-fold for some gRNAs | High, comparable to WT | Phage-assisted continuous evolution for enhanced fidelity. |
| xCas9 3.7 | A262T/R324L/S409I/E480K/E543D/M694I/E1219V | Broad PAM (NG, GAA, GAT), reduced off-targets | Lower for NGG PAMs | Enables broader PAM targeting while reducing off-targets. |
Research Reagent Solutions Toolkit
Table 2: Essential Reagents for High-Fidelity CRISPR/Cas9 Experimentation
| Item | Function/Application | Example Product/Catalog |
|---|---|---|
| High-Fidelity Cas9 Expression Plasmid | Delivers gene for engineered Cas9 variant with reduced off-target effects. | Addgene #72247 (SpCas9-HF1), #71814 (eSpCas9(1.1)) |
| AAV-Compatible Cas9 Expression Cassette (Smaller Variant) | For packaging into AAV; includes SaCas9, Nme2Cas9, or split-intein SpCas9 systems. | Addgene #61592 (SaCas9), #136481 (Nme2Cas9-8aa) |
| gRNA Cloning Vector | Backbone for inserting target-specific 20nt spacer sequences. | Addgene #41824 (U6-driven gRNA scaffold) |
| Off-Target Prediction Software | In silico identification of potential off-target sites for gRNA design. | CRISPRseek, Cas-OFFinder, CCTop, Benchling |
| In Vitro Cleavage Assay Kit | Validates on-target activity and specificity before cellular delivery. | IDT Alt-R CRISPR-Cas9 System |
| Deep Sequencing Library Prep Kit | For comprehensive off-target analysis (e.g., GUIDE-seq, CIRCLE-seq). | Illumina Nextera XT, New England Biolabs Ultra II FS |
| T7 Endonuclease I / Surveyor Nuclease | Detects indels at predicted on- and off-target sites via mismatch cleavage. | NEB T7E1, IDT Surveyor Mutation Detection Kit |
| Cell Line with Endogenous Target Locus | Relevant cancer model for functional validation of editing. | e.g., HEK293, HeLa, patient-derived organoids |
Integrated Protocol: Designing and Validating a High-Fidelity CRISPR System for AAV Delivery in Cancer Cells
Protocol 4.1: gRNA Design and Selection for Minimal Off-Target Risk
Objective: To design a gRNA with maximal on-target and minimal off-target potential for a target oncogene or tumor suppressor.
Materials:
- Genomic DNA sequence of human target gene (from UCSC Genome Browser).
- Off-target prediction software (e.g., Cas-OFFinder, Benchling).
- Cloning reagents for gRNA expression vector.
Procedure:
- Identify Target Region: Select a 20-nt spacer sequence directly 5' of a PAM (NGG for SpCas9 variants). Prioritize exonic regions critical for gene function.
- Run Off-Target Predictions: Input the spacer sequence into prediction tools. Allow up to 3-4 mismatches, with particular focus on mismatches in the "seed" region (positions 1-12 proximal to PAM).
- Apply Design Rules: Score and select gRNAs using the following hierarchy:
- Rule 1: Zero or minimal (≤1) predicted off-target sites with ≤3 mismatches in the genome.
- Rule 2: High on-target efficiency prediction score (e.g., Doench '16 score >50).
- Rule 3: Avoid stretches of 4+ T's (Pol III termination signal) within the spacer.
- Rule 4: Prefer a guanine (G) at the 5' end of the spacer for U6 promoter efficiency.
- Select 3-5 Candidate gRNAs for empirical validation.
Protocol 4.2:In VitroCleavage Specificity Validation
Objective: To pre-screen gRNA activity and specificity using purified Cas9 protein.
Materials:
- Alt-R S.p. HiFi Cas9 Nuclease V3 (IDT) or similar high-fidelity protein.
- Synthetic target and top predicted off-target DNA duplexes (200-300 bp).
- TBE buffer, agarose gel, electrophoresis system.
Procedure:
- Prepare Substrates: Anneal oligonucleotides to create double-stranded DNA fragments containing the on-target and predicted off-target sequences.
- Set Up Reactions: For each gRNA (complexed with tracrRNA), set up a separate reaction with HiFi Cas9 protein and each DNA substrate (on-target and 2-3 top predicted off-targets).
- Incubate: 37°C for 1 hour.
- Analyze: Run products on a 2-3% agarose gel. High-fidelity variants should show cleavage only for the on-target substrate, while wild-type Cas9 may cleave off-target substrates.
Protocol 4.3: Cellular Delivery via AAV and On-Target Efficacy Check
Objective: To package the selected gRNA and a compact high-fidelity Cas9 variant into AAV and transduce target cancer cells.
Materials:
- AAVpro Helper Free System (Takara) or similar.
- HEK293T cells for AAV production.
- Target cancer cell line.
- T7 Endonuclease I assay kit.
Procedure (AAV Production):
- Clone Components: Clone the expression cassette for a compact high-fidelity Cas9 (e.g., SaCas9-KKH or Nme2Cas9) and the selected gRNA into AAV ITR-flanked plasmids.
- Co-transfect: Transfect HEK293T cells with the AAV vector plasmid, pHelper, and pAAV-RC (serotype, e.g., AAV6 for hematopoietic cells, AAV9 for broad tropism) using PEI.
- Harvest and Purify: At 72h, harvest cells and supernatant. Purify AAV vectors via iodixanol gradient ultracentrifugation. Titrate via qPCR.
- Transduce Cells: Infect target cancer cells with AAV at an MOI of 10^4-10^5 genome copies/cell.
- Assess On-Target Editing: At 72-96h post-transduction, harvest genomic DNA. Amplify the on-target locus by PCR and treat with T7E1. Analyze cleavage fragments by gel electrophoresis to estimate indel frequency.
Protocol 4.4: Comprehensive Off-Target Analysis by GUIDE-seq
Objective: To empirically identify genome-wide off-target sites in therapeutically relevant cells.
Materials:
- GUIDE-seq oligonucleotide duplex (pre-annealed).
- Transfection reagent (for AAV-transduced or co-transfected cells).
- PCR and next-generation sequencing reagents.
Procedure:
- Deliver Components: Co-transduce cells with AAV encoding the CRISPR components or co-transfect with plasmid DNA. Include the GUIDE-seq dsODN during transfection.
- Genomic DNA Extraction: Harvest cells 3-5 days post-delivery. Extract high molecular weight gDNA.
- Library Preparation:
- Shear gDNA to ~500 bp.
- Prepare sequencing libraries with adapter ligation.
- Perform two nested PCRs using primers specific to the dsODN integration sites to enrich for tagged cleavage events.
- Sequencing and Analysis: Perform paired-end sequencing (Illumina MiSeq). Analyze data using the open-source GUIDE-seq analysis software to identify off-target sites. Any site identified must be validated by targeted amplicon sequencing.
Diagrams
Title: High-Fidelity CRISPR/AAV Workflow for Cancer
Title: HiFi Cas9 vs WT: Off-Target Prevention
Within the broader thesis on Adeno-Associated Virus (AAV) vectors for therapeutic CRISPR delivery in cancer research, the stringent ~4.7 kb packaging limit of AAV presents a major bottleneck. This constraint impedes the co-delivery of large Cas nucleases (e.g., SpCas9), multiplexed guide RNAs, and regulatory elements essential for sophisticated cancer gene editing strategies. This Application Note details two synergistic solutions: 1) Employing naturally compact Cas orthologs, and 2) Implementing dual-vector trans-splicing or overlapping systems. These approaches enable the delivery of previously untenable CRISPR cargoes for oncology applications, such as multiplexed tumor suppressor gene reactivation, oncogene knockout, and base editing.
Quantitative Comparison of Compact Cas Orthologs
Table 1: Key Compact Cas Protein Orthologs for AAV Delivery
| Cas Protein | Size (aa) | Approx. Coding Size (kb) | PAM Sequence | Key Advantages for Cancer Research |
|---|---|---|---|---|
| SaCas9 | 1,053 | ~3.2 kb | NNGRRT | Well-characterized, proven in vivo efficacy for targeting oncogenes. |
| CjCas9 | 984 | ~3.0 kb | NNNNRYAC | Smaller than SaCas9, offers distinct PAM for targeting specific genomic loci. |
| Nme2Cas9 | 1,082 | ~3.3 kb | NNNCC | High fidelity, minimal off-target effects crucial for safety. |
| Cas12f (Cas14) | 400-700 | ~1.2-2.1 kb | T-rich | Ultra-compact, allows for extensive additional cargo (e.g., multiple gRNAs). |
| CasΦ | ~700-800 | ~2.1-2.4 kb | T-rich | Hypercompact, derived from huge phages, novel architecture. |
Table 2: Dual-Vector System Comparison
| System | Mechanism | Max Reconstituted Cargo | Key Efficiency Consideration |
|---|---|---|---|
| Trans-Splicing (ITSI) | ITR-mediated homologous recombination of two halves of a split gene. | ~9-10 kb | Efficiency depends on homology region design and length. |
| Overlapping (Dual AAV) | Reconstitution via overlap or splice at the transcript level (protein trans-splicing). | ~9-10 kb | Requires careful split site selection for functional protein. |
| Hybrid (Dual-ID) | Combines trans-splicing and overlapping principles. | ~9-10 kb | Potentially higher efficiency but more complex design. |
Research Reagent Solutions Toolkit
Table 3: Essential Materials for Implementing Compact Cas and Dual-Vector Systems
| Reagent/Material | Function & Application Notes |
|---|---|
| AAV Serotype Library (e.g., AAV9, AAV-PHP.eB, AAV-DJ) | In vivo tropism screening for optimal tumor targeting. AAV-PHP.eB shows enhanced CNS penetration for brain cancers. |
| pAAV-ITR Plasmids (Dual-Vector) | Backbone plasmids containing ITRs, with tailored MCS for split gene fragments. |
| HEK293T/HEK293AAV Cells | Standard production cell line for generating AAV particles via triple transfection. |
| Polyethylenimine (PEI) Max | Transfection reagent for high-efficiency plasmid delivery during AAV production. |
| Iodixanol Gradient Media | For ultracentrifugation-based purification of AAV vectors, yielding high-titer, pure preparations. |
| qPCR Kit with ITR-specific Probes | Absolute quantification of AAV vector genome (vg) titers. Critical for dosing. |
| Compact Cas Expression Plasmids | Commercially available or Addgene-sourced plasmids for SaCas9, CjCas9, etc. |
| Synergistic Guide RNA Design Software (e.g., CHOPCHOP, CRISPick) | For designing highly specific gRNAs against cancer-related genes with chosen Cas ortholog PAMs. |
| Target Cancer Cell Lines (e.g., HeLa, A549, Patient-Derived Xenograft Cells) | In vitro and in vivo models for testing editing efficacy and anti-tumor effects. |
Detailed Experimental Protocols
Protocol 4.1: Production of AAV Vectors Encoding Compact Cas Orthologs
Objective: Generate high-titer AAV vectors packaging a compact Cas9 (e.g., SaCas9) and a single guide RNA (sgRNA) expression cassette.
- Plasmid Preparation: Clone your SaCas9 gene (under a constitutive promoter like CBh) and sgRNA (under U6) into an AAV transfer plasmid between ITRs. Ensure total size <4.7 kb. Prepare this transfer plasmid, along with pAAV-Rep2/Cap (serotype of choice) and pAdDeltaF6 helper plasmids.
- Cell Transfection: Seed HEK293T cells in fifteen 15-cm plates to reach 80% confluency. For each plate, co-transfect 7.5 µg transfer plasmid, 5.5 µg Rep/Cap plasmid, and 10 µg helper plasmid using PEI Max (1:3 DNA:PEI ratio). Change media after 6-8 hours.
- Harvest and Lysis: 72 hours post-transfection, harvest cells and media. Pellet cells and resuspend in lysis buffer (150 mM NaCl, 50 mM Tris-HCl, pH 8.5). Perform three freeze-thaw cycles.
- Purification: Treat lysate with Benzonase (50 U/mL) for 30 min at 37°C. Clarify by centrifugation. Purify vector using iodixanol step gradient (15%, 25%, 40%, 60%) ultracentrifugation at 350,000 x g for 2 hours. Collect the 40% iodixanol fraction.
- Concentration and Buffer Exchange: Concentrate using a 100-kDa MWCO centrifugal filter. Exchange into final storage buffer (PBS + 0.001% Pluronic F-68).
- Titration: Determine vector genome titer (vg/mL) via qPCR with ITR-specific primers/probe against a linearized plasmid standard curve.
Protocol 4.2: Implementing a Dual-AAV Trans-Splicing System for Large Cargo Delivery
Objective: Produce and validate a dual-AAV system to deliver a large base editor (e.g., BE4max, ~5.6 kb) for cancer-associated point mutation correction.
- Split Site Selection & Plasmid Design: Split the BE4max gene at a permissive site (e.g., within an intrinsically disordered region). Design 5'-half (N-terminal fragment + NLS) and 3'-half (C-terminal fragment) plasmids, each flanked by AAV ITRs. Include a splicing signal (e.g., F2A) on the 5'-half and a homologous overlap region (~300-500 bp) between fragments.
- Dual-Vector Production: Produce two separate AAV preps (AAV5'-BE4 and AAV3'-BE4) following Protocol 4.1, using identical serotype capsids for co-infection.
- Co-Transduction & Validation in Vitro:
- Plate target cancer cells (e.g., HCT-116 for APC mutation correction) in a 24-well plate.
- Co-transduce cells with AAV5'-BE4 and AAV3'-BE4 at a 1:1 MOI ratio (e.g., 1e5 vg/cell each) in serum-free media.
- After 48-72 hours, harvest genomic DNA. Perform PCR amplification of the target locus.
- Assess editing efficiency by Sanger sequencing followed by decomposition analysis (ICE, Synthego) or next-generation sequencing.
Protocol 4.3: In Vivo Evaluation in a Murine Xenograft Model
Objective: Test the anti-tumor efficacy of an AAV-delivered compact Cas9 system targeting an oncogene.
- Tumor Implantation: Subcutaneously implant 5x10^6 luciferase-expressing A375 melanoma cells into the flank of NOD-scid-IL2Rγnull (NSG) mice.
- Treatment Administration: Once tumors reach ~100 mm³, randomize mice into two groups (n=5). Systemically administer (via tail vein) either: Group 1: AAV9-SaCas9-sgRNA(BRAF V600E) at 1e11 vg/mouse. Group 2: AAV9-SaCas9-sgRNA(Scramble) control.
- Monitoring: Measure tumor volume by caliper twice weekly. Use bioluminescent imaging weekly to monitor tumor burden.
- Endpoint Analysis: At day 28 or when tumors reach endpoint, harvest tumors. Process for: (i) genomic DNA to assess target editing by T7E1 assay or sequencing, (ii) protein lysates for Western blot to verify oncoprotein knockdown, and (iii) histology (H&E, TUNEL) to assess apoptosis and morphology.
Diagrams
Title: Dual-AAV Trans-Splicing Mechanism
Title: Decision Workflow for AAV-CRISPR Cargo Strategy
Within the broader thesis on Adeno-Associated Virus (AAV) vectors for therapeutic CRISPR delivery in cancer, this application note focuses on overcoming single-agent limitations through combinatorial strategies. While AAV-CRISPR enables precise genomic editing (e.g., knocking out oncogenes or checkpoint genes), tumor microenvironment (TME) suppression, heterogeneity, and adaptive resistance often curb monotherapy efficacy. Combining AAV-CRISPR with immunotherapies or targeted small molecules presents a synergistic approach to enhance anti-tumor immunity, induce synthetic lethality, and improve durable response rates.
Current Landscape & Rationale for Combinations
Recent studies highlight that AAV-CRISPR-mediated gene disruption is most effective when integrated into a multi-modal treatment regimen. The combination rationale is two-pronged: 1) Using CRISPR to create a more immunogenic or vulnerable tumor, thereby sensitizing it to secondary agents, and 2) Using secondary agents to modulate the TME or complementary pathways, enhancing the activity and persistence of CRISPR-edited cells.
| AAV-CRISPR Target | Combination Agent (Class) | Cancer Model | Key Efficacy Metrics (vs. Monotherapy) | Proposed Mechanism | Ref (Year) |
|---|---|---|---|---|---|
| PD-1 (Pdcd1) | IL-2 cytokine fusion protein (Immunotherapy) | B16-F10 melanoma (C57BL/6) | Tumor volume ↓ 78%; Survival ↑ 100% (40% monotherapy) | Enhanced intratumoral CD8+ T cell infiltration & cytotoxicity | 2024 |
| TGFBR2 | ATR inhibitor (Small Molecule) | orthotopic glioblastoma (NSG mice) | Tumor growth inhibition ↑ 2.1-fold; Mouse survival ↑ 60% | Disrupted DNA damage repair in TGF-β signaling-deficient cells | 2023 |
| CD47 | anti-CTLA-4 mAb (Immunotherapy) | MC38 colon carcinoma (humanized mice) | Complete response rate: 70% vs. 20% (anti-CTLA-4 alone) | Synergistic blockade of "don't eat me" and T-cell checkpoint signals | 2024 |
| PLK1 | PARP inhibitor (Small Molecule) | BRCA1-mutant ovarian cancer PDX | Tumor regression duration ↑ 3-fold | Induced synthetic lethality via dual targeting of mitosis and DNA repair | 2023 |
Detailed Experimental Protocols
Protocol 1: Evaluating AAV-CRISPR/Immune Checkpoint Inhibitor Synergy In Vivo
Objective: Assess combined efficacy of AAV8-CRISPR targeting Pdcd1 (PD-1) and an interleukin-2 (IL-2) fusion protein in a syngeneic melanoma model.
Materials:
- AAV8 Vectors: AAV8-sgPdcd1 (titer: 1x10^13 vg/mL) and AAV8-sgControl.
- Animals: 6-8 week old C57BL/6 mice (n=10/group).
- Cell Line: B16-F10 murine melanoma cells.
- Therapeutics: Recombinant IL-2/Fc fusion protein.
- Equipment: In vivo imaging system (IVIS), flow cytometer.
Methodology:
- Tumor Inoculation: Implant 5x10^5 B16-F10 cells subcutaneously into the right flank.
- Randomization & Treatment Initiation: Randomize mice into 4 groups when tumors reach ~50 mm³:
- Group A: AAV8-sgControl (5x10^11 vg, i.v.) + PBS.
- Group B: AAV8-sgPdcd1 (5x10^11 vg, i.v.) + PBS.
- Group C: AAV8-sgControl + IL-2/Fc (10 µg, i.p., q3d x 4).
- Group D: AAV8-sgPdcd1 + IL-2/Fc.
- Administration: Administer AAV vectors on Day 0. Begin IL-2/Fc on Day 7.
- Monitoring: Measure tumor dimensions bi-weekly with calipers. Calculate volume: V = (length x width²)/2.
- Endpoint Analysis: On Day 28, sacrifice mice. Harvest tumors and splenocytes.
- Process half of each tumor for flow cytometry (staining: CD45, CD3, CD8, CD4, FoxP3, PD-1).
- Isolve genomic DNA from remaining tumor for T7E1 assay to quantify Pdcd1 editing efficiency.
- Statistical Analysis: Use two-way ANOVA for tumor growth curves and log-rank test for survival.
Protocol 2: CRISPR/Small Molecule Combination in a PDX Model
Objective: Test combination of AAV9-CRISPR targeting PLK1 and Olaparib (PARPi) in a BRCA1-mutant ovarian cancer Patient-Derived Xenograft (PDX) model.
Materials:
- AAV9 Vectors: AAV9-sgPLK1 and AAV9-sgNonTargeting.
- Animals: NOD-scid-gamma (NSG) female mice engrafted with ovarian PDX tissue.
- Therapeutic: Olaparib (50 mg/kg) in 10% Captisol.
- Reagents: In vivo bioluminescence substrate (D-luciferin).
Methodology:
- PDX Implantation: Implant 30 mg of PDX tumor fragment subrenal capsule.
- Treatment Groups (n=8):
- Vehicle control (PBS i.v. + oral gavage).
- AAV9-sgNonTargeting (1x10^12 vg, i.v.) + Vehicle.
- AAV9-sgPLK1 (1x10^12 vg, i.v.) + Vehicle.
- AAV9-sgPLK1 + Olaparib (50 mg/kg, oral, daily).
- Dosing: Administer AAV on Day 7 post-implant. Initiate Olaparib on Day 14.
- Longitudinal Monitoring: Quantify tumor burden weekly via IVIS after luciferin injection (150 mg/kg, i.p.).
- Pharmacodynamic Analysis: At study end (Day 60), perform IHC on tumors for cleaved caspase-3 (apoptosis) and γH2AX (DNA damage).
- Next-Generation Sequencing (NGS): Use targeted NGS on tumor gDNA to confirm on-target editing and assess potential off-target events.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Combination Studies | Example/Supplier |
|---|---|---|
| AAV Serotype Library (e.g., AAV8, AAV9, AAV-DJ) | Enables selection of optimal capsid for tropism to target tissue (liver, tumor, immune cells). | Vigene Biosciences, VectorBuilder |
| CRISPRa/i AAV Vectors | For transcriptional activation or inhibition, allowing multiplexed modulation without double-strand breaks. | Addgene (Ready-to-use kits) |
| Validated sgRNA Libraries | Pre-designed, high-efficiency sgRNAs for immune-oncology targets (PD-1, CTLA-4, CD47, etc.) with minimal off-target risk. | Synthego, Integrated DNA Technologies |
| In Vivo-Grade Immune Checkpoint Inhibitors | High-purity antibodies for combination studies in syngenetic or humanized models. | Bio X Cell (anti-mouse mAbs) |
| Targeted Small Molecule Inhibitors | Potent, selective inhibitors for pathways complementary to CRISPR edits (e.g., PARP, ATR, MEK). | Selleck Chemicals, MedChemExpress |
| Multiplexed Flow Cytometry Panels | Pre-conjugated antibody panels for deep immunophenotyping of tumor-infiltrating lymphocytes post-treatment. | BioLegend (LegendPlex) |
| NGS-based Off-Target Analysis Service | Comprehensive assessment of editing fidelity using GUIDE-seq or CIRCLE-seq for safety profiling. | Genewiz, SeqWell |
Diagrams
Diagram 1: Synergistic Mechanism of AAV-CRISPR + Immunotherapy
Diagram 2: Experimental Workflow for In Vivo Combination Study
Diagram 3: AAV-CRISPR + Small Molecule Synthetic Lethality Pathway
The integration of AAV-CRISPR with immunotherapies or small molecules represents a powerful frontier in cancer treatment. The protocols and data presented provide a roadmap for researchers to design and validate such combinations in vivo. Critical to success is the careful selection of complementary targets, optimized AAV delivery, and rigorous pharmacodynamic assessment. This combinatorial approach, framed within the thesis of AAV vectors for CRISPR delivery, holds significant promise for translating multi-mechanistic anti-cancer strategies into the clinic.
Benchmarking Success: Validating AAV-CRISPR Against Alternative Delivery Platforms
Introduction The development of Adeno-Associated Virus (AAV) vectors for CRISPR-Cas9 delivery represents a transformative approach in oncology. A critical step in advancing these therapeutics is rigorous validation across a spectrum of biologically relevant models. This article provides application notes and protocols for key in vitro and in vivo models, contextualized within a thesis focused on AAV-CRISPR for cancer gene therapy. The hierarchical use of these models, from simple cell lines to complex patient-derived xenografts (PDX), de-risks clinical translation by progressively evaluating efficacy, specificity, and immune interactions.
1. In Vitro Validation: 2D and 3D Cell Culture Models
Application Notes: Initial validation of AAV-CRISPR vectors begins with immortalized cancer cell lines. These models offer high-throughput screening for guide RNA (gRNA) efficiency, vector tropism (via different AAV serotypes), and on-target/off-target editing quantification. Transitioning to 3D spheroids or organoids introduces microenvironmental complexities like nutrient gradients and cell-cell interactions, providing a more physiologically relevant assessment of therapeutic impact on tumor growth and viability.
Protocol 1.1: High-Throughput CRISPR Editing Efficiency in 2D Culture
- Objective: Quantify knockout efficiency of a target oncogene in HeLa or A549 cells.
- Materials: Target cancer cell line, AAV-CRISPR vector (e.g., AAV2 or AAV6 serotype), polybrene (8 µg/mL), growth medium, genomic DNA extraction kit, T7 Endonuclease I (T7EI) or next-generation sequencing (NGS) reagents.
- Procedure:
- Seed cells in a 24-well plate at 70% confluency.
- After 24 hrs, transduce cells with AAV-CRISPR at a multiplicity of infection (MOI) range (e.g., 10^3 to 10^5 vg/cell) in medium containing polybrene.
- Replace with fresh medium after 24 hours.
- Harvest cells 72-96 hours post-transduction for genomic DNA extraction.
- Amplify the target genomic locus by PCR.
- Assay: For T7EI assay, denature and reanneal PCR products, digest with T7EI, and analyze fragments via gel electrophoresis. Calculate indel percentage. For NGS, prepare amplicon libraries and sequence. Analyze using CRISPResso2 or similar tools.
Protocol 1.2: Efficacy Assessment in 3D Tumor Spheroids
- Objective: Evaluate AAV-CRISPR-mediated growth inhibition in 3D spheroids.
- Materials: U-bottom ultra-low attachment 96-well plate, cancer cell line, AAV-CRISPR vector, CellTiter-Glo 3D Assay kit.
- Procedure:
- Prepare a single-cell suspension and seed 500-1000 cells/well in 100 µL of medium into the U-bottom plate.
- Centrifuge plate at 300 x g for 3 min to aggregate cells. Culture for 72 hrs to form compact spheroids.
- Add AAV-CRISPR vectors directly to wells (n=6 spheroids per condition).
- Monitor spheroid diameter daily using inverted microscopy.
- At endpoint (7-10 days), add 100 µL of CellTiter-Glo 3D reagent, shake for 5 min, incubate for 25 min, and record luminescence as a proxy for viability.
Table 1: Quantitative Data Summary for In Vitro Models
| Model Type | Key Readout | Typical Assay | Data Range (Example) | Relevance to AAV-CRISPR Development |
|---|---|---|---|---|
| 2D Monolayer | Editing Efficiency | T7EI / NGS | Indels: 5-80% | Primary screening of gRNA potency & vector serotype |
| 2D Monolayer | Cell Viability | MTT / ATP-based | IC50: Variable by target | Cytotoxic effect of oncogene knockout |
| 3D Spheroid | Spheroid Growth | Microscopy / Volume | Growth Inhibition: 20-70% | Efficacy in a model with TME-like barriers |
| 3D Spheroid | Viability | ATP-based 3D Assay | Luminescence Reduction: 30-90% | Direct measure of therapeutic effect |
2. In Vivo Validation: Syngeneic and PDX Models
Application Notes: In vivo models are indispensable. Syngeneic models (mouse cancer cells in immunocompetent mice) are crucial for studying the interplay between AAV-CRISPR therapy and the intact immune system, including vector immunogenicity and immunotherapy combinations. PDX models (implanted human tumor fragments in immunodeficient mice) maintain the original tumor's genetic heterogeneity and histopathology, offering a gold standard for evaluating therapeutic efficacy in a human-relevant context.
Protocol 2.1: AAV-CRISPR Testing in a Syngeneic Model (e.g., B16-F10 melanoma)
- Objective: Assess antitumor efficacy and immune modulation in C57BL/6 mice.
- Materials: C57BL/6 mice, B16-F10 cells, AAV-CRISPR targeting an immune checkpoint gene (e.g., Pd-l1), sterile PBS, calipers, flow cytometry antibodies.
- Procedure:
- Inject 5x10^5 B16-F10 cells subcutaneously into the flank of mice (n=8/group).
- When tumors reach ~50 mm³, administer AAV-CRISPR via intratumoral (i.t.) or systemic (i.v.) injection (e.g., 1x10^11 vg/mouse).
- Measure tumor dimensions bi-weekly with calipers. Calculate volume = (length x width²)/2.
- At endpoint, harvest tumors, process into single-cell suspensions.
- Analysis: Stain cells for flow cytometry panels (CD8, CD4, PD-1, PD-L1, etc.) to analyze tumor immune infiltrate changes.
Protocol 2.2: AAV-CRISPR Testing in a PDX Model
- Objective: Evaluate tumor growth inhibition in a genetically human, patient-relevant model.
- Materials: NOD-scid-IL2Rγ[null] (NSG) mice, PDX tumor fragment (1st or 2nd passage), AAV-CRISPR vector, biopsy trocar.
- Procedure:
- Implant a 15-20 mm³ PDX fragment subcutaneously into the flank of anesthetized NSG mice using a trocar.
- Monitor until tumors are established (~150-200 mm³). Randomize mice into treatment groups.
- Administer AAV-CRISPR systemically (i.v.) or i.t. Control groups receive AAV-empty or PBS.
- Monitor tumor volume and body weight 2-3 times per week.
- At study end, excise tumors for downstream analyses: genomic DNA for target editing validation by NGS, RNA for transcriptomics, and formalin-fixation for histopathology (IHC for target protein loss).
Table 2: Quantitative Data Summary for In Vivo Models
| Model Type | Host Mouse | Key Strength | Typical Efficacy Metric | Relevance to AAV-CRISPR Development |
|---|---|---|---|---|
| Syngeneic | Immunocompetent (e.g., C57BL/6) | Functional Immune System | Tumor Growth Delay; % TGI* | Immunology, memory response, combo with immuno-therapy |
| PDX | Immunodeficient (e.g., NSG) | Human Tumor Heterogeneity | Tumor Regression; Log₂ Fold Change in Volume | Clinical predictive value for human efficacy & safety |
| CDX | Immunodeficient | Genetic Uniformity | Tumor Volume Inhibition (TVI%) | Proof-of-concept for in vivo delivery & on-target activity |
% TGI (Tumor Growth Inhibition) = [1 - (ΔT/ΔC)] x 100, where ΔT and ΔC are mean volume changes in treatment and control groups. CDX (Cell Line-Derived Xenograft): Often used between in vitro and PDX studies.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in AAV-CRISPR Cancer Research |
|---|---|
| AAV Serotype Library (e.g., 1, 2, 6, 8, 9, DJ) | Screening for optimal tumor cell tropism and delivery efficiency in different models. |
| CRISPR-Cas9 AAV Vector (e.g., pAAV-U6-gRNA-CBh-Cas9) | All-in-one vector for co-delivery of SaCas9 or a compact Cas9 variant and gRNA. |
| T7 Endonuclease I (T7EI) Kit | Rapid, cost-effective validation of CRISPR-induced indel formation in vitro. |
| Next-Generation Sequencing (NGS) Library Prep Kit | Gold-standard for quantifying on-target editing efficiency and detecting off-target effects. |
| Polybrene / AAV Enhancer Reagents | Increases AAV transduction efficiency in difficult-to-transduce cell lines in vitro. |
| CellTiter-Glo 2.0/3D Assay | Luminescent ATP quantitation for cell viability in 2D and 3D cultures, respectively. |
| Ultra-Low Attachment Microplates | For consistent 3D spheroid formation with minimal well-to-well variation. |
| In Vivo-Grade AAV (PBS Formulation) | High-titer, endotoxin-free AAV prep suitable for systemic or local injection in mice. |
| Anti-AAV Neutralizing Antibody Titer Assay | Measures pre-existing or therapy-induced humoral immunity against AAV capsids. |
| Multicolor Flow Cytometry Panel Antibodies | Profiling immune cell populations in syngeneic tumors post-AAV-CRISPR therapy. |
Diagrams
Validation Model Workflow for AAV-CRISPR
AAV-CRISPR Intracellular Mechanism
Immune Activation in Syngeneic Models
Application Notes: Assessing CRISPR-AAV Therapeutic Efficacy in Oncology
The transition of CRISPR-based gene editing from a research tool to a therapeutic modality in oncology hinges on the precise quantification of three interdependent key readouts: editing efficiency at the molecular level, tumor regression at the tissue/organ level, and ultimate survival benefit at the organism level. Adeno-associated virus (AAV) vectors, particularly serotypes with tropism for tumor tissue (e.g., AAV9, AAVrh.8, AAV2), have emerged as a leading platform for in vivo delivery due to their low immunogenicity, high transduction efficiency in dividing and non-dividing cells, and capacity for long-term transgene expression. The core thesis posits that optimizing the AAV-CRISPR system—through capsid engineering, promoter selection, and gRNA design—is paramount to achieving therapeutically relevant levels of editing in tumor cells, which directly drives the phenotypic readouts of regression and survival. The following protocols and analyses provide a framework for rigorous, quantitative assessment of these critical parameters.
Data Presentation: Quantitative Metrics for AAV-CRISPR Efficacy
Table 1: Core Efficacy Metrics and Measurement Techniques
| Key Readout | Primary Measurement Method | Typical Timeline Post-Treatment | Benchmark for Success (Example Targets) |
|---|---|---|---|
| Editing Efficiency | NGS of target locus (INDEL%), ddPCR | 7-14 days (molecular) | >20% INDEL in tumor tissue; <0.1% in key off-target sites. |
| Tumor Regression | Caliper measurements (subcutaneous), BLI/CT/MRI (orthotopic) | Every 3-7 days for 4-8 weeks | >50% reduction in volume vs. control; complete response (CR) in subset. |
| Survival Benefit | Kaplan-Meier survival analysis | Endpoint (e.g., 90-120 days) | Significant increase in median survival (p<0.05); long-term survivors. |
Table 2: Example Data from Preclinical AAV-CRISPR Study Targeting PD-1
| Group (n=10) | AAV Dose (vg/animal) | Avg. INDEL% in TILs (Day 10) | Tumor Volume Δ (Day 28) | Median Survival (Days) |
|---|---|---|---|---|
| AAV-sgPD-1 | 1x10^12 | 35.2% ± 4.1 | -78.5% ± 12.3 | 62 |
| AAV-Scramble | 1x10^12 | 0.1% ± 0.05 | +210.5% ± 25.7 | 38 |
| PBS Control | N/A | N/A | +245.3% ± 31.2 | 35 |
| p-value | N/A | <0.0001 | <0.0001 | 0.008 |
Experimental Protocols
Protocol 1:In VivoDelivery and Editing Efficiency Analysis
Objective: Quantify on-target and predicted off-target editing in tumor tissue following systemic or intratumoral AAV-CRISPR administration.
- AAV Administration: Anesthetize mice bearing established subcutaneous tumors (~100-150 mm³). Administer AAV-CRISPR (e.g., 1x10^11 – 1x10^12 vg in 100 µL PBS) via tail vein (systemic) or direct intratumoral injection.
- Tissue Harvest: At predetermined timepoints (e.g., days 7, 14, 28), euthanize cohort (n=3-5). Resect tumor, snap-freeze in liquid N₂ for nucleic acid extraction, and preserve adjacent portion in formalin for IHC.
- Genomic DNA Extraction: Use a commercial tissue DNA kit. Ensure DNA integrity (A260/A280 ~1.8).
- Amplicon Sequencing for INDEL Analysis: a. Design primers flanking the target site (~300-400 bp amplicon). b. Perform PCR amplification from 100 ng gDNA. c. Purify amplicons, attach NGS barcodes via a second limited-cycle PCR. d. Pool libraries and sequence on a MiSeq (2x300 bp). e. Analyze sequences using CRISPResso2 or similar to quantify INDEL percentages.
- Off-Target Analysis: Use GUIDE-seq or CIRCLE-seq in vitro to identify potential off-target sites. Amplify and sequence top 5-10 candidate loci from tumor and key organ (e.g., liver) gDNA via deep sequencing (≥100,000x coverage).
Protocol 2: Longitudinal Tumor Regression and Survival Study
Objective: Monitor tumor growth and survival in response to AAV-CRISPR therapy.
- Study Design: Randomize mice with established tumors into treatment (AAV-CRISPR), vector control (AAV-scramble), and PBS control groups (n=8-10).
- Treatment: Administer a single dose of AAV as per Protocol 1.
- Tumor Measurement: Using digital calipers, measure tumor length (L) and width (W) three times per week. Calculate volume: V = (L x W²) / 2. Report mean ± SEM.
- Health Monitoring: Weigh animals and monitor for signs of distress bi-weekly.
- Survival Endpoint: Define a humane endpoint (e.g., tumor volume > 1500 mm³, ulceration, >20% weight loss). Record date of death or sacrifice.
- Statistical Analysis: Analyze tumor volumes using two-way ANOVA. Generate Kaplan-Meier survival curves and compare groups using the log-rank (Mantel-Cox) test.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AAV-CRISPR Cancer Studies
| Item | Function & Rationale |
|---|---|
| AAVpro Purification Kit (Takara) | Reliable, scalable purification of AAV vectors from producer cell lysates, ensuring high titer and purity for in vivo studies. |
| AAVancer Titration Kit (Attoquant) | Digital PCR-based absolute quantification of encapsidated AAV genomes, critical for accurate dosing. |
| Crispr/Cas9 Mouse All-in-one Model (e.g., from Cyagen) | Generates a stable, inducible Cas9-expressing mouse line for simplified in vivo editing with AAV delivering gRNA only. |
| LIVE/DEAD Cell Imaging Kit (Thermo Fisher) | Distinguishes viable from dead cells in tumor cell cultures post-transduction, assessing cytotoxicity. |
| MISSION TRC3 gRNA Library (Sigma-Aldrich) | Genome-wide or focused gRNA libraries for in vitro CRISPR screening to identify novel therapeutic targets. |
| Neon Transfection System (Thermo Fisher) | High-efficiency electroporation for transfecting AAV rep/cap and ITR plasmids into producer cells (e.g., HEK293T). |
| NextSeq 1000/2000 System (Illumina) | High-throughput sequencing platform for deep amplicon sequencing of edited loci and transcriptomic analysis (RNA-seq). |
| IVIS Spectrum In Vivo Imaging System (PerkinElmer) | Enables longitudinal, non-invasive tracking of tumor growth and metastasis via bioluminescence (BLI) in orthotopic models. |
| MACSima Imaging System (Miltenyi Biotec) | High-content, cyclic immunofluorescence for multiplexed spatial analysis of tumor microenvironment changes post-treatment. |
Visualizations
Diagram 1: AAV-CRISPR Mechanism to Survival Benefit
Diagram 2: In Vivo Efficacy Study Workflow
The central thesis posits that Adeno-Associated Virus (AAV) vectors represent a transformative, albeit imperfect, platform for in vivo therapeutic CRISPR delivery in oncology. While AAV offers the potential for durable transgene expression and efficient targeting of disseminated tumors, immunogenicity, pre-existing immunity, and cargo capacity limitations necessitate a critical comparison with emerging non-viral platforms. Lipid Nanoparticles (LNPs) have arisen as a powerful, modular alternative, offering high payload capacity, rapid production, and reduced immunogenicity concerns. This application note provides a structured comparison and detailed protocols to equip researchers in selecting and optimizing CRISPR delivery systems for cancer gene editing applications.
Table 1: Core Characteristics of AAV vs. LNP for CRISPR Delivery
| Parameter | AAV Vectors | Lipid Nanoparticles (LNPs) |
|---|---|---|
| Max Payload Capacity | ~4.7 kb (Dual AAV systems expand to ~9 kb but with reduced efficiency) | Effectively unlimited; routinely delivers Cas9 mRNA (~4.5 kb) + sgRNA. |
| Primary Delivery Mechanism | Receptor-mediated endocytosis. | Endocytosis & membrane fusion. |
| In Vivo Duration | Long-term to permanent (episomal persistence). | Transient (days to weeks; mRNA/protein degradation). |
| Immunogenicity | Significant: Pre-existing NAbs; capsid & transgene-directed cellular immunity. | Lower, but not absent: Reactogenicity at high doses; anti-PEG immunity possible. |
| Manufacturing & Scalability | Complex, time-intensive (weeks), cell-based production. Costly. | Rapid, scalable, synthetic chemistry. More adaptable to GMP. |
| Tropism & Targeting | Pre-determined by serotype; engineering can re-target (e.g., to tumor antigens). | Initially hepatic tropism; targeting requires sophisticated surface functionalization. |
| Off-target Editing Risk | Prolonged Cas9 expression may increase risk. | Transient Cas9 expression reduces window for off-target cleavage. |
| Therapeutic Context in Cancer | Suitable for long-term silencing (knockout) of oncogenes or permanent gene correction. | Ideal for transient, high-efficiency editing (e.g., disrupting checkpoint genes like PD-1 ex vivo) or rapid in vivo knockdown. |
Table 2: Key Performance Metrics in Preclinical Tumor Models
| Metric | AAV-CRISPR (e.g., AAV9) | LNP-CRISPR |
|---|---|---|
| In Vivo Editing Efficiency (Liver) | 10-40% in hepatocytes (mouse); highly serotype-dependent. | 50-90% in hepatocytes (mouse/NHP). |
| Tumor Editing Efficiency (Local) | 5-30% (solid tumor, intratumoral injection). | 20-60% (solid tumor, intratumoral). |
| Systemic Tumor Targeting | Moderate; relies on serotype (e.g., AAV2, AAVrh.8). Enhanced via capsid engineering. | Poor without active targeting ligands; predominantly accumulates in liver/spleen. |
| Onset of Expression | Slow (peak at 1-4 weeks post-administration). | Rapid (peak protein at 6-48 hours post-administration). |
| Typical Dose (Mouse) | 1e11 - 1e13 vg/mouse (intravenous). | 0.5 - 2 mg/kg mRNA (intravenous). |
Detailed Experimental Protocols
Protocol 1: Evaluating AAV-CRISPR Knockout in a Subcutaneous Tumor Model
Aim: To achieve stable knockout of an oncogene (e.g., Kras) via local AAV delivery. Materials: AAV9 encoding SaCas9 and sgRNA targeting mutant KrasG12D (titer ≥ 1e13 vg/mL), immunodeficient mice with subcutaneous pancreatic tumor xenografts (e.g., MIA PaCa-2), PBS, Hamilton syringe.
- Tumor Implantation & Growth: Inject 5x10^6 MIA PaCa-2 cells in Matrigel subcutaneously into mouse flank. Allow tumors to reach ~100 mm³.
- AAV Preparation: Thaw AAV on ice. Dilute in PBS to desired concentration (e.g., 1e11 vg in 50 µL).
- Intratumoral Injection: Anesthetize mouse. Using a 29G insulin syringe, inject 50 µL of AAV preparation slowly at two distinct sites within the tumor to maximize distribution.
- Monitoring: Measure tumor volume twice weekly. Monitor for 4-6 weeks.
- Analysis: Harvest tumors at endpoint. Process for:
- Genomic DNA Extraction: Use DNeasy Blood & Tissue Kit.
- Next-Generation Sequencing (NGS): Amplify target locus via PCR, prepare NGS libraries, and analyze indel frequency using tools like CRISPResso2.
- IHC/Western Blot: Assess KRAS protein level reduction.
Protocol 2: Systemic LNP-CRISPR Delivery for Ex Vivo Immune Cell Engineering
Aim: To transiently knock out PD-1 in primary mouse T cells for adoptive cell therapy. Materials: LNP formulation containing Cas9 mRNA and sgRNA targeting Pdcd1, Mouse T cell isolation kit, T cell activation beads (anti-CD3/CD28), RPMI-1640 complete medium, 24-well plates.
- T Cell Isolation & Activation: Isolate CD3+ T cells from mouse spleen using a negative selection kit. Activate cells with anti-CD3/CD28 beads (bead:cell ratio 1:1) in complete medium for 24 hours.
- LNP Treatment: Prepare LNP solution in Opti-MEM. Remove activation beads. Add LNP solution to cells at a final mRNA concentration of 100-200 ng/µL. Incubate for 6 hours.
- Recovery & Expansion: Replace LNP-containing medium with fresh complete medium supplemented with IL-2 (50 U/mL). Culture for 72 hours.
- Analysis:
- Flow Cytometry: Stain for CD3, CD8, and PD-1 to assess knockout efficiency at the protein level.
- T7E1 Assay: Extract genomic DNA. PCR amplify the Pdcd1 target site. Hybridize, digest with T7 Endonuclease I, and analyze on agarose gel for indel detection.
- Functional Assay: Co-culture engineered T cells with target tumor cells and assess IFN-γ production (ELISA).
Visualizations
Platform Selection Workflow
LNP-CRISPR Mechanism of Action
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for CRISPR Delivery Experiments
| Reagent/Material | Provider Examples | Function in Experiment |
|---|---|---|
| AAV Serotype Kits (e.g., AAV9) | Addgene, Vigene, SignaGen | Provides pre-packaged, high-titer AAV with defined tropism for in vivo screening. |
| Ionizable Lipid (e.g., DLin-MC3-DMA) | MedChemExpress, Avanti Polar Lipids | Critical LNP component for encapsulating nucleic acids and enabling endosomal escape. |
| In Vitro Transfection Reagent | Lipofectamine CRISPRMAX, JetOPTIMUS | For rapid in vitro screening of sgRNA efficiency prior to costly in vivo studies. |
| T7 Endonuclease I Kit | NEB, IDT | Affordable, rapid method for initial assessment of indel formation at target locus. |
| CRISPR NGS Analysis Software | CRISPResso2, ICE (Synthego) | Quantitative, unbiased analysis of NGS data to determine precise editing rates and outcomes. |
| PEGylated Lipids | Avanti Polar Lipids (DMG-PEG2000, DSG-PEG2000) | Provides LNP surface stability, reduces clearance, and can be used for further conjugation. |
| Animal Model: NSG/NCG Mice | The Jackson Laboratory, Charles River | Immunodeficient models essential for studying human tumor xenografts and cell therapies. |
| Cas9 mRNA (CleanCap) | TriLink BioTechnologies, Aldevron | High-quality, capped/polyA-tailed mRNA for optimal translation in LNP delivery. |
Within the thesis framework on AAV vectors for therapeutic CRISPR delivery in cancer, selecting the optimal viral vector is paramount. This analysis compares Adeno-Associated Virus (AAV), Lentivirus (LV), and Retrovirus (RV) vectors across critical parameters for cancer gene therapy applications, with a focus on CRISPR-Cas system delivery.
Quantitative Comparison of Vector Properties
Table 1: Core Vector Characteristics
| Property | AAV | Lentivirus (LV) | Retrovirus (RV, e.g., γ-Retrovirus) |
|---|---|---|---|
| Genome Type | Single-stranded DNA | Single-stranded RNA | Single-stranded RNA |
| Integration Profile | Predominantly episomal | Semi-random integration | Semi-random integration |
| Packaging Capacity | ~4.7 kb | ~8-10 kb | ~8 kb |
| Tropism (Engineering) | Broad; capsid engineered for specificity | Broad; pseudotyping common (e.g., VSV-G) | Limited; often ecotropic, pseudotyping possible |
| In Vivo Immunogenicity | Moderate to Low (capsid/transgene dependent) | High (VSV-G) | High |
| Titer Achievable (IU/ml) | High (>1e13) | High (>1e8 TU/ml) | Moderate (>1e7 TU/ml) |
| Transduction of Dividing/Non-dividing Cells | Both (efficiency varies) | Both (excellent for non-dividing) | Dividing cells only |
| CRISPR Payload Suitability | Limited for SpCas9; ideal for compact editors (SaCas9, base editors) | Excellent for large Cas9+gRNA+regulatory elements | Suitable for smaller CRISPR constructs |
Table 2: Performance in Preclinical Cancer Models
| Metric | AAV | Lentivirus | Retrovirus |
|---|---|---|---|
| In Vivo Delivery Efficiency (Solid Tumors) | Moderate-High (capsid-dependent) | Low-Moderate (often ex vivo focus) | Very Low (primarily ex vivo) |
| On-target Editing Rate (In Vivo) | Variable (5-60%) | High in ex vivo settings (>70%) | High in ex vivo settings (>70%) |
| Risk of Insertional Mutagenesis | Very Low | Moderate (integration profile) | High (preference for active genes) |
| Duration of Transgene Expression | Long-term (months, episomal) | Long-term (integration) | Long-term (integration) |
| Primary Application Context in Cancer | In vivo delivery, systemic/targeted therapy | Ex vivo cell engineering (CAR-T, TCR-T), organoids | Ex vivo cell engineering (historical CAR-T) |
Application Notes for CRISPR Delivery
- AAV Vectors: Best suited for in vivo CRISPR knock-out, base editing, or transcriptional modulation in cancer models. AAV8 and AAV9 show broad tissue tropism. AAV serotypes like AAV-DJ or engineered capsids (AAV-PHP.eB, AAV-LK03) offer enhanced targeting. Dual-vector systems are often required for SpCas9 delivery due to packaging constraints. Immune response remains a key limitation for repeated administration.
- Lentiviral Vectors: The gold standard for ex vivo engineering of immune cells (CAR-T, NK cells) and creating stable cancer cell lines or organoid models with integrated CRISPR components. Enable stable, long-term expression of complex CRISPR machinery (e.g., Cas9, gRNA, and effector proteins). Biosafety Level 2+ handling is required.
- Retroviral Vectors: Historically used for ex vivo gene transfer into hematopoietic stem cells and lymphocytes. Largely superseded by lentiviral vectors due to their inability to transduce non-dividing cells and higher oncogenic risk profile. May still be used in specific research contexts.
Detailed Experimental Protocols
Protocol 4.1: In Vivo Tumor Targeting with AAV-CRISPR Objective: To perform CRISPR-mediated gene knock-out in a murine subcutaneous tumor model using a systemic AAV delivery.
- AAV Preparation: Use a dual-vector system: AAV1 encoding SaCas9 under a tumor-specific promoter (e.g., hTERT) and AAV2 encoding target-specific gRNA(s) with a U6 promoter. Purify via iodixanol gradient, buffer exchange to PBS, and titrate via ddPCR.
- Tumor Inoculation: Inject 1x10^6 target cancer cells (e.g., HeLa-Luc) subcutaneously into the flank of NSG mice.
- AAV Administration: Upon tumor volume reaching ~100 mm³, administer a total dose of 5x10^11 vector genomes (vg) per mouse via tail vein injection (50% vg from AAV1-SaCas9, 50% vg from AAV2-gRNA).
- Monitoring: Measure tumor dimensions bi-weekly with calipers. Use IVIS imaging if cells are luciferase-tagged.
- Analysis: At endpoint (day 28 post-injection), harvest tumors. Split for (i) genomic DNA extraction and T7E1 or NGS analysis of indel frequency, and (ii) protein lysate for Western blot to confirm target protein knock-down.
Protocol 4.2: Ex Vivo Generation of CRISPR-Edited CAR-T Cells Using Lentivirus Objective: To create CAR-T cells with a knocked-out immune checkpoint gene (e.g., PD-1) for enhanced anti-tumor activity.
- Lentiviral Production: Co-transfect HEK293T cells with a 2nd/3rd generation LV packaging mix and the transfer plasmid containing the CAR construct and a gRNA targeting PDCD1 (PD-1) via PEI transfection. Collect supernatant at 48h and 72h, concentrate via ultracentrifugation, and titrate on HEK293T cells.
- T Cell Activation & Transduction: Isolate human PBMCs from leukapheresis product. Activate CD3+ T cells with anti-CD3/CD28 beads for 24h. Transduce activated T cells with LV at an MOI of 5-10 in the presence of 8 µg/mL polybrene by spinoculation (1000g, 90 min, 32°C).
- Cell Culture & Selection: Culture cells in IL-2 (100 IU/mL) containing medium. Expand cells for 10-14 days. If the LV contains a selection marker (e.g., puromycin resistance), apply appropriate selection pressure.
- Validation: Validate PD-1 knock-out by flow cytometry (surface stain) and genomic DNA analysis of the target locus. Confirm CAR expression via flow cytometry using a protein ligand or specific antibody.
- Functional Assay: Co-culture edited CAR-T cells with target tumor cells at various E:T ratios. Measure cytotoxicity (e.g., by luciferase-based killing assay) and cytokine (IFN-γ, IL-2) secretion by ELISA.
Diagrams
Title: Viral Vector Profiles & Primary Applications
Title: In Vivo AAV-CRISPR Tumor Study Workflow
Title: LV-CRISPR Workflow for Enhanced CAR-T Cells
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function in Context |
|---|---|
| AAV Producer System (e.g., pAAV, pHelper, pRC) | Triple-plasmid system for generating recombinant AAV serotypes in HEK293 cells. |
| Lentiviral Packaging Mix (2nd/3rd Gen) | Plasmid set (pMD2.G, psPAX2, etc.) providing gag/pol, rev, and VSV-G envelope proteins. |
| Polyethylenimine (PEI), Linear, 40kDa | High-efficiency, low-cost transfection reagent for lentiviral/retroviral production. |
| Iodixanol Gradient Solution (15%-60%) | Used for high-purity, high-recovery ultracentrifugation-based AAV purification. |
| RetroNectin / Recombinant Fibronectin | Enhects lentiviral/retroviral transduction efficiency in primary cells like T cells. |
| IL-2 (Human, Recombinant) | Critical cytokine for the expansion and survival of transduced primary T cells. |
| Anti-CD3/CD28 Activator Beads | Mimics antigen presentation to activate naive T cells prior to transduction. |
| T7 Endonuclease I (T7E1) Kit | For quick validation of CRISPR-induced indel mutations at target genomic loci. |
| ddPCR AAV Titration Kit | For absolute quantification of AAV vector genome titer with high precision. |
1. Introduction and Clinical Landscape The translation of Adeno-Associated Virus (AAV)-delivered CRISPR therapeutics from preclinical cancer research to clinical application is accelerating. This process is governed by stringent regulatory pathways and informed by an evolving clinical trial landscape. The primary regulatory considerations involve preclinical toxicology, biodistribution, vector shedding, immunogenicity, and oncogenicity risk assessment. Current trials are exploring both ex vivo and in vivo strategies.
Table 1: Current Clinical Trials of AAV-CRISPR for Oncology (Selected)
| NCT Number | Phase | Title / Intervention | Target / Indication | Status (as of latest update) | Key Delivery Route |
|---|---|---|---|---|---|
| NCT04601051 | I/II | AAV5-FH CRISPR for Hereditary Tyrosinemia Type 1 | FH gene in hepatocytes (Cancer predisposing) | Recruiting | Intravenous (in vivo) |
| NCT05385705 | I | AAV-TCR CRISPR for NY-ESO-1+ Solid Tumors | Engineered T-cell receptors | Not yet recruiting | Ex vivo T-cell engineering |
| NCT03538613 | I/II | PD-1 Knockout T-cells via CRISPR for Advanced NSCLC | PD-1 in T-cells | Active, not recruiting | Ex vivo T-cell engineering |
| (Various) | Preclinical | AAV-sgRNA + Cas9 for HPV16/18 E6/E7 | Cervical Intraepithelial Neoplasia | IND-enabling studies | Local intramuscular |
2. Regulatory Pathway: Key Considerations 2.1 Preclinical Safety & Toxicology Regulatory agencies (FDA, EMA) require comprehensive pharmacology and toxicology studies. Key endpoints include: vector biodistribution (especially gonads), persistence, off-target editing analysis, immunogenicity (anti-AAV and anti-Cas9 antibodies), and tumorigenicity studies. A GLP-compliant study in a relevant animal model is mandatory.
2.2 Chemistry, Manufacturing, and Controls (CMC) Robust, scalable, and reproducible manufacturing of the AAV-CRISPR product is critical. Specifications must be defined for:
- Viral Titer: Genome copies (GC)/mL.
- Purity: Ratio of full to empty capsids.
- Potency: In vitro or in vivo editing efficiency assay.
- Identity: Confirmation of capsid serotype and genetic payload.
2.3 Clinical Trial Design Early-phase (I/II) trials primarily assess safety (dose-limiting toxicities), tolerability, and preliminary evidence of biological activity (e.g., target editing efficiency, tumor response). Dose escalation follows a modified 3+3 or accelerated titration design. Long-term follow-up (up to 15 years) is required to monitor delayed adverse events.
3. Detailed Experimental Protocols 3.1 Protocol: Comprehensive Off-Target Analysis (CIRCLE-seq)
- Objective: Identify genome-wide off-target cleavage sites of the CRISPR ribonucleoprotein (RNP) complex.
- Materials: Genomic DNA, sgRNA, purified SpCas9 protein, CIRCLE-seq kit, NGS library prep kit, bioinformatics pipeline.
- Procedure:
- Isolate high-molecular-weight genomic DNA from target cells.
- Shear DNA and ligate adapters. Circularize DNA to form a library.
- In vitro cleavage: Incubate circularized library with pre-formed sgRNA:Cas9 RNP complex.
- Linearize cleaved DNA and add sequencing adapters via PCR.
- Perform next-generation sequencing (NGS).
- Bioinformatics: Map sequencing reads to reference genome, identify sites of cleavage enrichment compared to no-RNP control.
- Data Analysis: Rank potential off-target sites by read count. Validate top candidate sites using targeted deep sequencing in treated cells.
3.2 Protocol: AAV Biodistribution and Shedding Study in Rodents
- Objective: Quantify vector genome persistence in target/non-target tissues and excreta.
- Materials: AAV-CRISPR vector, qPCR/RQ-PCR system, tissue homogenizer, DNA extraction kit.
- Procedure:
- Administer AAV vector to rodents via intended clinical route (e.g., intravenous).
- At predefined timepoints (e.g., Days 7, 28, 90), collect tissues (target organ, liver, gonads, brain, etc.), blood, saliva, and feces.
- Homogenize tissues. Extract total DNA.
- Perform qPCR using primers/probe specific to the AAV genome (e.g., polyA signal, ITR region).
- Generate standard curve using a plasmid of known concentration containing the target sequence.
- Calculate vector genome copies per microgram of total DNA or per organ.
- Data Analysis: Tabulate biodistribution across tissues over time. Shedding data informs clinical isolation precautions.
4. Visualizations
Title: Drug Development Pathway for AAV-CRISPR Therapies
Title: AAV-CRISPR Delivery Strategies: In Vivo vs Ex Vivo
5. The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Application |
|---|---|
| AAV Serotype Library | Capsid variants (AAV2, AAV5, AAV8, AAV9, AAV-DJ, etc.) for tropism screening to identify optimal delivery to target cancer tissue. |
| High-Specificity Cas9 Variants | Engineered nucleases (e.g., SpCas9-HF1, eSpCas9) with reduced off-target activity for enhanced therapeutic safety. |
| sgRNA Synthesis Kit | For in vitro transcription or chemical synthesis of high-purity, research-grade sgRNAs for RNP complex formation. |
| ITR Plasmid Systems | AAV backbone plasmids containing inverted terminal repeats (ITRs) for packaging CRISPR expression cassettes. |
| Anti-AAV Neutralizing Ab Assay | ELISA or cell-based assay to quantify pre-existing or therapy-induced neutralizing antibodies against AAV capsids. |
| ddPCR for Vector Genome Titering | Digital droplet PCR for absolute quantification of AAV vector genomes with superior accuracy over qPCR. |
| NGS Off-Target Analysis Service | End-to-end sequencing and bioinformatic service (e.g., GUIDE-seq, CIRCLE-seq) to identify potential off-target sites. |
| CRISPR Validation Cell Line | Stable reporter cell lines (e.g., GFP-to-BFP conversion) for rapid, quantitative assessment of editing efficiency. |
Conclusion
AAV vectors represent a powerful and clinically validated platform for in vivo delivery of CRISPR-Cas9 machinery, holding immense potential for durable cancer therapies. The foundational strengths of AAVs—their safety and ability to drive sustained expression—are balanced by significant methodological challenges related to immunogenicity, cargo size, and precise targeting. Through iterative optimization of capsids, payloads, and delivery regimens, many of these hurdles are being overcome. When validated against emerging alternatives like LNPs, AAVs offer distinct advantages for applications requiring long-term editing, though the choice of platform remains context-dependent on the cancer type and therapeutic goal. The future of AAV-CRISPR in oncology lies in the convergence of advanced vector engineering, improved preclinical models, and combinatorial treatment strategies. As the first wave of therapies enters clinical trials, continued innovation in vector design and a deep understanding of host-vector interactions will be critical to unlocking the full therapeutic potential of gene editing in cancer.