Liquid Biopsy in Cancer Monitoring: Advanced Techniques, Clinical Applications, and Future Directions for Research and Drug Development
This article provides a comprehensive overview of liquid biopsy technologies for cancer monitoring, tailored for researchers, scientists, and drug development professionals.
Liquid Biopsy in Cancer Monitoring: Advanced Techniques, Clinical Applications, and Future Directions for Research and Drug Development
Abstract
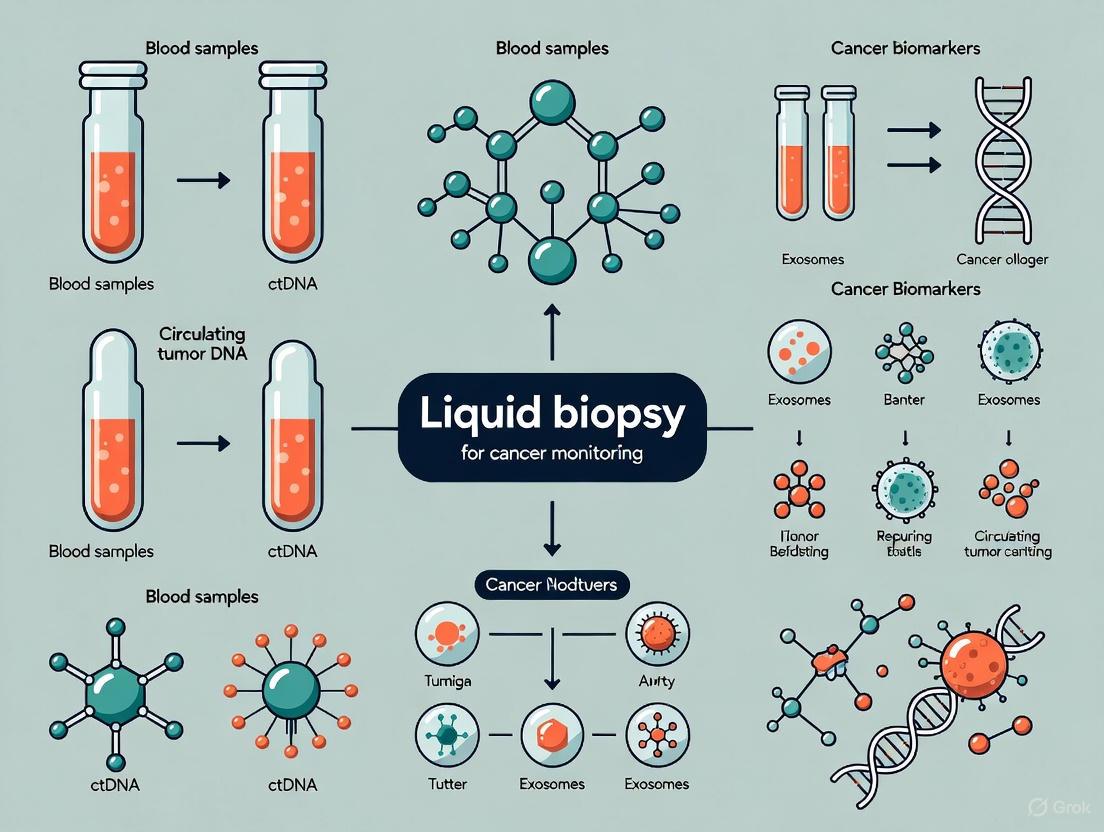
This article provides a comprehensive overview of liquid biopsy technologies for cancer monitoring, tailored for researchers, scientists, and drug development professionals. It explores the foundational biology of circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and other biomarkers. The scope encompasses current and emerging methodological approaches—including next-generation sequencing (NGS), digital PCR, and microfluidic isolation—along with their applications in therapy selection, minimal residual disease (MRD) detection, and tracking resistance. The content also addresses key challenges such as assay optimization, confounding factors like clonal hematopoiesis, and the critical validation frameworks necessary for clinical translation and comparative performance assessment against tissue biopsy.
The Foundation of Liquid Biopsy: Core Biomarkers and Biological Principles for Cancer Monitoring
Circulating Tumor DNA (ctDNA)
Core Characteristics and Biological Significance
Circulating tumor DNA (ctDNA) refers to small fragments of tumor-derived DNA circulating in the bloodstream, representing a subset of total cell-free DNA (cfDNA). These fragments are released into the circulation primarily through apoptosis and necrosis of tumor cells [1] [2]. ctDNA carries tumor-specific genetic and epigenetic alterations, including single nucleotide variants (SNVs), structural variants (SVs), copy number alterations, and methylation changes, providing a comprehensive molecular portrait of the tumor [1] [2]. A key advantage of ctDNA is its short half-life, estimated between 16 minutes to several hours, which enables real-time monitoring of tumor dynamics and treatment response [2]. The fraction of ctDNA in total cfDNA varies significantly with disease burden, ranging from below 0.1% in early-stage cancers to over 90% in advanced metastatic disease, creating substantial detection challenges particularly for minimal residual disease (MRD) assessment [1].
Current Detection Technologies and Methodologies
Advanced technologies have been developed to address the sensitivity challenges in ctDNA detection, particularly for low-frequency variants and MRD monitoring.
Table 1: Key Analytical Platforms for ctDNA Detection
| Technology Platform | Key Principle | Sensitivity Range | Primary Applications | Advantages | Limitations |
|---|---|---|---|---|---|
| ddPCR/BEAMing | Partitioning of DNA fragments for absolute quantification | ~0.01% VAF | Tracking known mutations, therapy monitoring | High sensitivity, absolute quantification, rapid turnaround | Limited to small number of pre-defined mutations |
| Structural Variant (SV) Assays | Detection of tumor-specific chromosomal rearrangements | <0.01% VAF (parts-per-million) | MRD, early-stage cancer detection | Ultra-high sensitivity, tumor-specific markers | Requires personalized assay design |
| Targeted NGS (CAPP-Seq, TEC-Seq) | Hybrid capture with error correction | 0.01%-0.1% VAF | Comprehensive mutation profiling, resistance monitoring | Broad genomic coverage, high specificity | Higher cost, complex bioinformatics |
| Magnetic Nano-electrode Systems | Electrochemical sensing with nanoparticle enrichment | Attomolar (10¯¹⁸ M) | Point-of-care applications, rapid detection | Extreme sensitivity, minimal processing | Still in development phase |
| PhasED-Seq | Detection of multiple phased variants on same DNA fragment | Ultra-high sensitivity (<0.0001%) | MRD, ultra-early recurrence | Exceptional sensitivity for very low ctDNA | Complex assay design |
Applications in Cancer Monitoring and Research
ctDNA analysis has transformed multiple aspects of cancer management through non-invasive liquid biopsy approaches. In treatment response monitoring, ctDNA levels provide a dynamic and quantitative measure of tumor burden, often demonstrating changes earlier than radiographic imaging [1] [2]. Studies in non-small cell lung cancer (NSCLC) and colorectal cancer have shown that ctDNA decline following therapy initiation accurately predicts radiographic response and improved survival outcomes [1]. For minimal residual disease (MRD) assessment, ctDNA detection after curative-intent surgery or completion of adjuvant therapy identifies patients at high risk of recurrence, often months to years before clinical manifestation [1] [2]. In breast cancer, SV-based ctDNA assays detected molecular recurrence more than one year before clinical evidence of disease [1]. Additionally, ctDNA enables noninvasive genotyping and therapy resistance monitoring, identifying emerging resistance mutations to targeted therapies (e.g., T790M in EGFR-mutant NSCLC) without repeated tissue biopsies [1]. Emerging applications include methylation profiling for tumor agnostic detection and fragmentomics analysis, which leverages ctDNA fragmentation patterns to distinguish tumor-derived DNA from normal cfDNA [1] [2].
Detailed Protocol: Structural Variant-Based ctDNA Detection for MRD
Principle: This tumor-informed approach identifies patient-specific structural variants (translocations, insertions, deletions) through baseline tumor tissue sequencing, then designs personalized hybrid-capture probes or multiplexed PCR panels to detect these rearrangements in plasma with ultra-high sensitivity [1].
Workflow:
- Tumor Tissue Sequencing: Perform whole-genome or whole-exome sequencing on baseline tumor tissue to identify tumor-specific structural variants with breakpoint sequences.
- Bioinformatic Analysis: Identify optimal SV targets (typically 1-16 variants) with unique breakpoint sequences not present in normal germline DNA.
- Panel Design: Design custom hybrid-capture baits or PCR primers flanking each breakpoint.
- Plasma Collection and Processing:
- Collect 10-20 mL blood in cell-free DNA collection tubes (e.g., Streck, PAXgene)
- Process within 6 hours of collection: centrifuge at 1600 × g for 10 min to separate plasma, then 16,000 × g for 10 min to remove residual cells
- Extract cfDNA using silica-membrane columns (QIAamp Circulating Nucleic Acid Kit)
- Quantify using fluorometry (Qubit dsDNA HS Assay)
- Library Preparation and Sequencing:
- Construct sequencing libraries with unique molecular identifiers (UMIs)
- Enrich for target regions using custom baits/primers
- Sequence to high depth (>100,000X) on Illumina platform
- Variant Calling and Quantification:
- Align sequences to reference genome
- Group reads by UMI to create consensus sequences
- Identify breakpoint-spanning reads
- Calculate variant allele frequency (VAF)
Quality Control:
- Input cfDNA: ≥10 ng recommended
- Spike-in synthetic controls for extraction efficiency monitoring
- Negative controls (healthy donor plasma) for background estimation
- Limit of detection: Establish using dilution series of tumor DNA in normal plasma
Figure 1: SV-based ctDNA MRD Detection Workflow
Circulating Tumor Cells (CTCs)
Core Characteristics and Biological Significance
Circulating tumor cells (CTCs) are intact cancer cells that detach from primary or metastatic tumors and enter the bloodstream, playing a crucial role in cancer metastasis [3] [4]. First identified in 1869, CTCs represent a rare population amidst billions of blood cells, with concentrations as low as 1 CTC per billion hematological cells in early-stage cancer [3]. These cells exhibit remarkable heterogeneity, encompassing epithelial, mesenchymal, and hybrid phenotypes resulting from epithelial-to-mesenchymal transition (EMT), which enhances their invasive capabilities and metastatic potential [3] [4]. CTCs can circulate as single cells or clusters (circulating tumor microemboli) and often display stem-like characteristics with self-renewal capacity [3]. Unlike ctDNA, CTCs provide comprehensive biological information including genomic, transcriptomic, proteomic, and functional data from viable tumor cells, offering unique insights into metastatic biology and therapeutic targets [3] [4].
Current Detection Technologies and Methodologies
CTC isolation and detection strategies leverage both biological and physical properties to overcome the challenge of extreme rarity in blood samples.
Table 2: CTC Isolation and Detection Platforms
| Technology Category | Specific Platforms/Methods | Isolation Principle | Recovery Efficiency | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Biological Properties-Based | CellSearch (FDA-approved) | Immunomagnetic enrichment (EpCAM) | Variable (40-90%) | Clinical validation, standardization | Misses EMT CTCs (EpCAM-negative) |
| MACS | Magnetic cell sorting | Moderate | High purity | Limited by antibody specificity | |
| FACS | Fluorescence-activated sorting | High | Single-cell resolution | Low throughput, equipment cost | |
| Physical Properties-Based | ISET (Rarecells) | Size-based filtration (8μm pores) | High | Marker-independent, preserves cell viability | May miss small CTCs |
| Parsortix | Size and deformability | Moderate | Downstream molecular analysis | Clogging potential | |
| Dean Flow Fractionation | Inertial focusing | High | High throughput | Complex microfluidics | |
| Microfluidic/Chip-Based | CTC-iChip | Inertial sorting + immunomagnetic | High | High recovery, marker-independent | Technical complexity |
| HB-Chip | Hemodynamic sorting | Moderate | Simple operation | Lower purity | |
| Functional Assays | EPISPOT assay | Protein secretion detection | Low | Viable CTC detection | Complex, low throughput |
Applications in Cancer Monitoring and Research
CTC enumeration and characterization provide valuable clinical insights across cancer types. As a prognostic biomarker, CTC counts consistently correlate with clinical outcomes. In metastatic breast, prostate, and colorectal cancers, elevated CTC counts (using CellSearch system) are associated with significantly reduced progression-free survival (PFS) and overall survival (OS) [3] [4]. For therapy monitoring, dynamic changes in CTC counts during treatment provide early indication of response or resistance, often preceding radiographic assessment [4]. In treatment selection, molecular characterization of CTCs can identify actionable targets and resistance mechanisms through protein expression analysis, fluorescence in situ hybridization (FISH), and next-generation sequencing [3]. Emerging applications include functional studies through in vitro CTC culture and CTC-derived xenograft (CDX) models, which enable drug sensitivity testing and investigation of metastasis mechanisms [4]. CTC clusters, while less frequent than single CTCs, demonstrate significantly enhanced metastatic potential and are associated with poorer patient outcomes [3].
Detailed Protocol: Integrated Microfluidic CTC Capture and Molecular Analysis
Principle: This protocol combines size-based enrichment with immunoaffinity capture for comprehensive CTC isolation, followed by molecular characterization using single-cell RNA sequencing.
Workflow:
- Blood Collection and Processing:
- Collect 10-15 mL peripheral blood in EDTA or CellSave tubes
- Process within 4-24 hours (depending on preservative)
- Initial centrifugation: 800 × g for 20 min with density gradient (Ficoll-Paque) to separate peripheral blood mononuclear cells (PBMCs)
Microfluidic CTC Enrichment:
- Prime microfluidic chip (e.g., CTC-iChip, Herringbone Chip) with PBS + 1% BSA
- Load PBMC fraction at controlled flow rate (1-2 mL/h)
- For immunomagnetic depletion: Incubate with CD45 magnetic beads to remove leukocytes
- Collect CTC-enriched fraction in collection buffer
CTC Identification and Enumeration:
- Cytocentrifugation onto glass slides
- Immunofluorescence staining:
- Epithelial markers: Pan-cytokeratin (CK 8,18,19) - Alexa Fluor 488
- Leukocyte marker: CD45 - Alexa Fluor 647 (exclusion)
- Nuclear stain: DAPI
- Microscopic analysis: Identify CTCs as CK+/DAPI+/CD45- cells
Single-Cell Isolation and Molecular Analysis:
- Manual picking or automated cell sorting (e.g., DEPArray, FACS)
- Single-cell whole transcriptome amplification (Smart-seq2 protocol)
- Library preparation and RNA sequencing (Illumina platform)
- Bioinformatic analysis for gene expression profiling and mutation detection
Alternative Workflow for Culture:
- Resuspend CTC-enriched fraction in CTC culture medium (RPMI-1640 + 10% FBS + growth factors)
- Plate in ultra-low attachment plates
- Monitor for CTC cluster formation and sphere growth
- Expand for drug sensitivity testing or CDX model generation
Quality Control:
- Blood processing: Maintain at room temperature, avoid refrigeration
- Spike-in controls: Add known number of tumor cells (e.g., SKBR3, MCF-7) to healthy donor blood for recovery assessment
- Purity assessment: Calculate ratio of CTCs to contaminating leukocytes
- Viability: >70% for successful culture attempts
Figure 2: Comprehensive CTC Analysis Workflow
Extracellular Vesicles (EVs)
Core Characteristics and Biological Significance
Extracellular vesicles (EVs) are heterogeneous, membrane-bound particles secreted by various cell types, playing crucial roles in intercellular communication through transfer of proteins, lipids, and nucleic acids [5]. According to MISEV2018 and MISEV2023 guidelines, EVs are broadly categorized by size and biogenesis into small extracellular vesicles (sEVs; <200 nm, including exosomes) and large extracellular vesicles (>200 nm, including microvesicles and apoptotic bodies) [5]. sEVs form through inward budding of the endosomal membrane, creating intraluminal vesicles within multivesicular bodies that subsequently fuse with the plasma membrane [5]. Microvesicles (200-1000 nm) generate through direct outward budding from the plasma membrane, while apoptotic bodies (1-5 μm) release during programmed cell death [5]. Tumor-derived EVs (tEVs) carry diverse biomolecules reflecting their parent cells, offering valuable insights into tumor presence and progression [5]. Key advantages of EV-based liquid biopsy include their higher concentration in bodily fluids compared to CTCs, exceptional biological stability even within harsh tumor microenvironments, and comprehensive molecular information surpassing circulating DNA [5].
Current Detection Technologies and Methodologies
EV isolation and characterization require specialized approaches to address challenges related to their small size, heterogeneity, and co-isolation with non-vesicular particles.
Table 3: EV Isolation and Analysis Techniques
| Isolation Method | Principle | Purity | Yield | Downstream Applications | Throughput |
|---|---|---|---|---|---|
| Ultracentrifugation | Sequential centrifugation forces | Moderate | High | Proteomics, RNA sequencing | Low |
| Size-Exclusion Chromatography | Size-based separation in columns | High | Moderate | Functional studies, biomarker discovery | Medium |
| Precipitation (ExoQuick) | Polymer-based aggregation | Low | High | RNA/protein analysis | High |
| Immunoaffinity Capture | Antibody-based (CD63, CD81, CD9) | High | Low | Subtype characterization, specific marker studies | Low |
| Microfluidic Devices | Immunoaffinity or size-based on chip | High | Moderate | Point-of-care applications | Medium |
| Asymmetric Flow FFF | Field-flow fractionation | High | Moderate | Size characterization, omics studies | Low |
Applications in Cancer Monitoring and Research
EV-based liquid biopsy demonstrates extensive potential applications in disease diagnosis, prognosis evaluation, and treatment monitoring [5]. For cancer diagnostics, EV biomarkers enable early detection across multiple cancer types. In hepatocellular carcinoma, elevated levels of Glypican-3 (GPC3) in circulating EVs serve as reliable indicators for early detection [5]. Microfluidic digital PCR platforms enable accurate quantification of tumor-derived sEVs across various tumor markers with exceptional sensitivity (detection limit: 10 copies) [5]. In therapeutic monitoring, EV cargo analysis provides dynamic insights into treatment response and resistance mechanisms. For disease subtyping, EV molecular profiles help classify cancer subtypes and monitor tumor evolution through serial liquid biopsies [5]. EVs also show promise in autoimmune diseases and infectious diseases through specific biomarker detection [5]. Beyond diagnostic applications, EVs are being explored as therapeutic agents in regenerative medicine and targeted drug delivery systems due to their natural biocompatibility and targeting capabilities [5].
Detailed Protocol: Ultracentrifugation-Based EV Isolation and RNA Profiling
Principle: This gold-standard method uses sequential centrifugation steps to isolate EVs based on size and density, followed by RNA extraction for downstream molecular analysis.
Workflow:
- Sample Collection and Pre-processing:
- Collect 10-20 mL blood in EDTA tubes
- Process within 1 hour: centrifuge at 1,600 × g for 15 min to obtain platelet-poor plasma
- Transfer supernatant to new tube, centrifuge at 16,000 × g for 20 min to remove apoptotic bodies and cell debris
- Aliquot and store at -80°C if not processing immediately
EV Isolation by Ultracentrifugation:
- Thaw plasma samples on ice if frozen
- Filter through 0.22 μm syringe filter
- Ultracentrifuge at 100,000 × g for 70 min at 4°C (Type 70 Ti rotor)
- Discard supernatant, resuspend pellet in 10 mL PBS (filtered through 0.22 μm)
- Repeat ultracentrifugation at 100,000 × g for 70 min
- Resuspend final EV pellet in 100-200 μL PBS for immediate use or store at -80°C
EV Characterization:
- Nanoparticle Tracking Analysis (NTA): Dilute EV sample 1:1000 in PBS, measure size distribution and concentration (NanoSight NS300)
- Transmission Electron Microscopy: Fix EVs in 2% paraformaldehyde, adsorb to formvar-carbon coated grids, negative stain with 1% uranyl acetate, image at 80 kV
- Western Blot: Detect EV markers (CD63, CD81, CD9, TSG101) and absence of negative markers (calnexin, GM130)
RNA Extraction and Analysis:
- Extract RNA using miRNeasy Micro Kit or equivalent
- Assess RNA quality and quantity using Bioanalyzer RNA Pico Chip
- For small RNA sequencing:
- Library preparation using NEBNext Small RNA Library Prep Kit
- Size selection for 15-50 nt fragments
- Sequence on Illumina platform (single-end 75 bp)
- For qRT-PCR:
- Reverse transcription using TaqMan MicroRNA Reverse Transcription Kit
- Pre-amplification if necessary
- qPCR with EV RNA-specific assays
Quality Control:
- Minimize freeze-thaw cycles to preserve EV integrity
- Include vesicle-free PBS as negative control throughout isolation
- Monitor protein contamination using BCA assay (typical EV preparation: protein/particle ratio ~100-500 fg/particle)
- Validate RNA quality: RIN >7.0 for mRNA analysis
Figure 3: EV Isolation and RNA Analysis Workflow
Cell-Free RNA (cfRNA)
Core Characteristics and Biological Significance
Cell-free RNA (cfRNA) comprises diverse RNA species circulating in bodily fluids, first discovered in plasma and serum in 1972 [6]. cfRNAs exist in multiple forms, including messenger RNA (mRNA), microRNA (miRNA), long non-coding RNA (lncRNA), circular RNA (circRNA), piwi-interacting RNA (piRNA), and small nuclear RNA (snRNA) [6]. These molecules are protected from degradation by RNases through various mechanisms, including encapsulation within extracellular vesicles, association with lipoprotein complexes, or binding to RNA-binding proteins like argonaute 2 (AGO2) [6]. Unlike cfDNA, cfRNA provides dynamic information about gene expression patterns and regulatory processes occurring in tumor cells [6]. A significant advantage of cfRNA is its high tissue specificity, which helps overcome the tissue-of-origin limitation in ctDNA analysis [6]. Studies have shown that cfRNAs in blood are more sensitive than cfDNAs in disease detection, and researchers can identify the tissue source of cfRNAs through bioinformatics algorithms [6].
Current Detection Technologies and Methodologies
cfRNA analysis requires specialized approaches to address challenges related to its instability and low abundance in circulation.
Table 4: cfRNA Detection and Analysis Platforms
| RNA Type | Detection Methods | Sensitivity | Primary Applications | Technical Considerations |
|---|---|---|---|---|
| mRNA | RNA-seq, qRT-PCR | Moderate | Gene expression profiling, fusion detection | Requires rapid processing, RNA stabilization |
| miRNA | miRNA-seq, qRT-PCR arrays | High | Diagnostic signatures, treatment monitoring | Stable in circulation, well-established protocols |
| lncRNA | RNA-seq, targeted panels | Variable | Cancer subtyping, prognostic stratification | Lower abundance, specific assay design |
| circRNA | RNase R treatment + RNA-seq, ddPCR | High | Drug resistance monitoring, stable biomarkers | Resistance to exonuclease degradation |
| piRNA | Small RNA-seq | Low | Germ cell tumors, emerging biomarkers | Limited knowledge of functions |
Applications in Cancer Monitoring and Research
cfRNA biomarkers demonstrate significant utility across multiple cancer applications. For early cancer detection, specific cfRNA signatures enable non-invasive identification of tumors. For instance, the SNORD3B-1 5' region with secondary structure demonstrates stable existence in plasma, with abundance serving as a biomarker for early diagnosis of liver cancer [6]. The S domain of srpRNA RN7SL1 shows reliable performance in hepatocellular carcinoma diagnosis and prognosis [6]. In therapy resistance monitoring, circRNAs have emerged as particularly valuable biomarkers due to their exceptional stability from covalently closed-loop structures [7]. Specific circRNAs including circHIPK3, circFOXO3, and circRNA100290 modulate cancer pathways and affect chemotherapy sensitivity [7]. For example, circRNA102231 is overexpressed in gefitinib-resistant NSCLC, functioning as a sponge for miR-130a-3p [7]. Similarly, circRNA CDR1as correlates with tamoxifen resistance in breast cancer through modulation of the miR-7/EGFR pathway [7]. Beyond oncology, cfRNA applications extend to prenatal screening, infectious diseases, and autoimmune disorders through analysis of expression patterns in plasma, saliva, urine, and other biofluids [6] [8].
Detailed Protocol: CircRNA Enrichment and Detection for Drug Resistance Monitoring
Principle: This protocol leverages circRNA resistance to exonuclease degradation to enrich for circular species, followed by precise quantification using droplet digital PCR for monitoring therapy resistance.
Workflow:
- Blood Collection and Plasma Separation:
- Collect 10 mL blood in PAXgene Blood RNA tubes
- Process within 4 hours: centrifuge at 1900 × g for 10 min at room temperature
- Transfer plasma to new tube, centrifuge at 16,000 × g for 10 min to remove debris
- Aliquot plasma and store at -80°C
RNA Extraction:
- Thaw plasma samples on ice
- Add 1 volume of Denaturing Solution (if needed for miRNA preservation)
- Extract total RNA using miRNeasy Serum/Plasma Kit
- Include MS2 bacteriophage RNA or synthetic spike-ins as extraction controls
- Elute in 14 μL nuclease-free water
- Quantify using Qubit RNA HS Assay
RNase R Treatment for CircRNA Enrichment:
- Set up reaction:
- 8 μL RNA extract
- 1 μL RNase R (20 U/μL)
- 1 μL 10× RNase R Reaction Buffer
- Incubate at 37°C for 15 min
- Purify using RNA Clean & Concentrator-5 kit
- Optional: Include no-RNase R control for comparison
- Set up reaction:
Reverse Transcription:
- Use SuperScript IV Reverse Transcriptase with random hexamers
- Include no-RT controls to assess DNA contamination
- Use circRNA-specific divergent primers for targeted reverse transcription
Droplet Digital PCR Quantification:
- Prepare reaction mix:
- 10 μL 2× ddPCR Supermix for Probes
- 1 μL 20× circRNA-specific assay (divergent primers/TaqMan probe)
- 4 μL cDNA template
- 5 μL nuclease-free water
- Generate droplets using QX200 Droplet Generator
- Perform PCR: 95°C for 10 min, then 40 cycles of 94°C for 30 s and 60°C for 60 s, 98°C for 10 min
- Read droplets using QX200 Droplet Reader
- Analyze using QuantaSoft software
- Prepare reaction mix:
Data Analysis:
- Calculate copies/μL based on Poisson distribution
- Normalize to spike-in controls or reference circRNAs
- Establish threshold for resistance detection based on clinical validation studies
Quality Control:
- RNA integrity: Assess using Bioanalyzer if sufficient material
- RNase R efficiency: Monitor by qPCR comparing linear vs. circular transcripts
- Limit of detection: Establish using synthetic circRNA standards
- Inter-assay variability: Include reference samples across runs
Figure 4: CircRNA Detection Workflow for Drug Resistance
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 5: Essential Research Reagents and Platforms for Circulating Biomarker Analysis
| Reagent/Platform | Supplier Examples | Primary Application | Key Features | Considerations |
|---|---|---|---|---|
| cfDNA Blood Collection Tubes | Streck, PAXgene, Roche | ctDNA stabilization | Preserves cfDNA for up to 7 days at room temperature | Compatibility with downstream assays |
| CTC Enrichment Kits | Menarini Silicon Biosystems, Miltenyi Biotec | CTC isolation | EpCAM-based or marker-independent | Cell viability preservation |
| EV Isolation Kits | System Biosciences, Thermo Fisher | EV purification | Polymer-based precipitation, antibody-based | Co-precipitation of contaminants |
| RNA Stabilization Reagents | Qiagen, Zymo Research | cfRNA preservation | RNase inhibition, RNA integrity maintenance | Compatibility with extraction methods |
| Unique Molecular Identifiers | Integrated DNA Technologies | NGS library preparation | Error correction, quantitative accuracy | Increased sequencing complexity |
| Digital PCR Systems | Bio-Rad, Thermo Fisher | Absolute quantification | High sensitivity, no standard curves | Limited multiplexing capability |
| Next-Generation Sequencers | Illumina, Pacific Biosciences | Comprehensive profiling | High throughput, multi-analyte capability | Bioinformatics infrastructure needs |
| Microfluidic Platforms | Fluxion Biosciences, BioFluidica | CTC/EV isolation | Integrated processing, automation | Throughput limitations |
Comparative Analysis and Integration Strategies
Table 6: Integrated Comparison of Circulating Biomarkers in Liquid Biopsy
| Parameter | ctDNA | CTCs | Extracellular Vesicles | cfRNA |
|---|---|---|---|---|
| Analytical Sensitivity | 0.01% VAF (targeted), <0.001% (SV-based) | 1-10 CTCs/mL blood | ~10 EV particles (dPCR) | Variable (miRNA: high, mRNA: moderate) |
| Tumor Representation | Tumor heterogeneity (via fragmentation) | Single-cell resolution, viable cells | Molecular cargo from parent cells | Active gene expression patterns |
| Stability in Circulation | Short half-life (minutes-hours) | Fragile, limited viability | High stability | Protected forms (EVs, protein complexes) |
| Information Content | Genetic and epigenetic alterations | Genomic, transcriptomic, proteomic, functional | Proteins, lipids, nucleic acids | Expression profiling, regulatory networks |
| Technical Challenges | Low abundance in early-stage, standardization | Extreme rarity, heterogeneity | Isolation purity, standardization | Instability, low abundance |
| Clinical Readiness | Advanced (FDA-approved assays) | Moderate (CellSearch approved) | Emerging (academic and commercial) | Emerging (growing validation) |
| Ideal Applications | MRD, therapy monitoring, resistance mutations | Prognostic stratification, functional studies, metastasis research | Early detection, subtyping, drug delivery | Therapy response, resistance mechanisms |
| Complementary Approach | Combined with fragmentomics | Combined with single-cell omics | Combined with cargo analysis | Combined with epigenetic profiling |
The future of liquid biopsy lies in integrated multi-analyte approaches that combine the strengths of different circulating biomarkers. Simultaneous analysis of ctDNA, CTCs, EVs, and cfRNA from a single blood sample provides complementary information that offers a more comprehensive understanding of tumor biology than any single analyte alone [2]. For instance, combining ctDNA mutation analysis with CTC functional characterization and EV RNA profiling can provide insights into genetic alterations, cellular phenotypes, and intercellular communication simultaneously. Such integrated approaches are particularly valuable for addressing tumor heterogeneity, monitoring evolving resistance mechanisms, and developing personalized treatment strategies based on a holistic view of the tumor ecosystem.
{=>}
The Biology of Tumor Shedding: Origins, Half-Life, and Dynamics in Circulation
Tumor shedding, the process by which cancerous lesions release cellular material into the circulation, is the fundamental biological principle underpinning liquid biopsy. The analysis of circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs) has emerged as a powerful, non-invasive approach for cancer monitoring, profiling, and detecting minimal residual disease [2] [9]. The utility of these analytes is dictated by their biology: their origins, the mechanisms of their release, their quantity in circulation, and their rapid clearance. A deep understanding of these dynamics is crucial for researchers and drug development professionals to accurately interpret liquid biopsy data, design effective clinical studies, and develop robust predictive biomarkers. This application note synthesizes current knowledge on the biology of tumor shedding, providing structured quantitative data, experimental protocols, and visual frameworks to guide research in this rapidly advancing field.
Core Biological Principles and Quantitative Parameters
The presence and concentration of tumor-derived material in the blood are governed by a set of biological processes and kinetic parameters. Key release mechanisms include apoptosis, necrosis, and active secretion, while the analyte half-life determines the time window for which it reflects the current tumor state [10]. The following sections and tables summarize the critical quantitative data and biological characteristics of ctDNA and CTCs.
Table 1: Characteristics and Release Mechanisms of Circulating Tumor Nucleic Acids and Cells
| Analyte | Primary Release Mechanisms | Typical Fragment Size/Characteristics | Key Release-Associated Proteins/Factors |
|---|---|---|---|
| Circulating Tumor DNA (ctDNA) | Apoptosis: Major source. Produces short, nucleosome-bound fragments [10].Necrosis: Results in longer, more random DNA fragments [10].Active secretion via extracellular vesicles (less characterized) [10]. | ~167 bp (DNA wrapped around one nucleosome plus linker), showing a ladder-like pattern on gel electrophoresis [10]. | Caspase-activated DNase (CAD) and other nucleases execute DNA fragmentation during apoptosis [10]. ERp5 protein identified as critical for shedding cell surface proteins like MICA, a potential model for other release mechanisms [11]. |
| Circulating Tumor Cells (CTCs) | Active invasion and intravasation into vasculature [12].Passive release from tumor margins, potentially enhanced by macrovascular infiltration in advanced disease [13]. | Whole, viable cells. Can circulate as single cells or clusters (homotypic or heterotypic with immune cells); clusters are associated with enhanced metastatic potential and can spike near end-of-life [13]. | EpCAM (used for CellSearch enrichment), Vimentin, N-cadherin [9]. |
Table 2: Kinetic and Quantitative Parameters of ctDNA and CTCs
| Parameter | ctDNA | CTCs |
|---|---|---|
| Half-Life in Circulation | ~16 minutes to several hours [2]. | ~1 to 2.5 hours [9]. |
| Represents | A snapshot of tumor cell death [2]. | A snapshot of viable, invasive cells [12]. |
| Shedding Probability (Modeled) | In lung cancer, ~0.014% of a tumor cell's DNA is shed per cell death (qd ≈ 1.4 × 10⁻⁴ haploid genome equivalents per cell death) [14]. | Not quantitatively modeled in the same way; release is stochastic and dynamic [12]. |
| Typical Abundance in Blood | Can range from <0.1% of total cell-free DNA in early-stage cancer to >90% in advanced disease [2]. | Extremely rare; approximately 1 CTC per 1-10 million leukocytes [9]. |
| Key Dynamic Behaviors | Levels correlate with tumor burden and cell turnover; rapid clearance allows for real-time monitoring of treatment response [2]. | Counts do not always correlate with primary tumor size; can show significant temporal fluctuations and perimortem spikes in clusters [12] [13]. |
Diagram 1: The Lifecycle of Tumor-Derived Analytes. This pathway outlines the journey of ctDNA and CTCs from their origin in the tumor, through their release into circulation, to their eventual clearance.
Experimental Protocols for Analyzing Shedding Dynamics
Robust experimental protocols are essential for investigating the dynamics of tumor shedding. Below are detailed methodologies for quantifying ctDNA shedding levels and for monitoring CTCs in vivo, which are critical for preclinical research.
Protocol: Quantifying Lesion-Specific ctDNA Shedding Using the Lesion Shedding Model (LSM)
The LSM is a computational framework that uses sequencing data from multiple lesions and a liquid biopsy to order lesions by their relative ctDNA shedding levels, helping to identify aggressively shedding lesions [15].
1. Sample Preparation and Input:
- Tissue Samples: Obtain whole-exome or genome sequencing (WES/WGS) data from multiple synchronous tumor lesions. Ensure high tumor purity; lesions with poor purity should be excluded [15].
- Liquid Biopsy: Sequence at least one blood plasma cfDNA sample collected most proximally to the lesion biopsies. Data should be formatted into a MAF (Mutation Annotation Format) file containing alteration information, including Variant Allele Frequency (VAF) or Cancer Cell Fraction (CCF) [15].
2. Hypothesis Blood Generation:
- For a given patient, subsample k lesions out of the total n lesions for computational tractability and to model missing lesions.
- For the selected k lesions, generate a "hypothesis blood" (HB) cfDNA profile. This is a mathematical mixture of the alterations from the k lesions, weighted by a hypothesis vector W = (w₁, w₂, ..., wₖ), where w represents the hypothesized relative shedding level for each lesion [15].
3. Target Function Optimization:
- Define a target function (a family of functions F) that measures the goodness-of-fit between the generated hypothesis blood (HB) and the actual observed cfDNA profile.
- Iteratively search for the optimal hypothesis vector W that minimizes the target function, thereby identifying the shedding levels that best explain the actual ctDNA data [15].
4. Consensus Shedding Network:
- Repeat the subsampling and optimization process many times (e.g., 1000 iterations) to ensure robustness.
- Aggregate the top hypothesis vectors from all iterations to calculate a consensus partial ordering of lesions from strongest to poorest shedders and construct a relative shedding level graph [15].
Key Application: This model is particularly useful for understanding which lesions contribute most to the ctDNA pool, which may have implications for targeting lesions responsible for progression or therapeutic resistance [15].
Protocol: In Vivo Monitoring of Circulating Tumor Cell Dynamics
Real-time monitoring of CTCs provides insights into their dynamic and fluctuating release, which is missed by single-time-point blood draws [12].
1. Animal Model Preparation:
- Inoculate immunodeficient mice with human tumor cell lines, preferably expressing fluorescent reporters (e.g., GFP) or luciferase for validation. Orthotopic inoculation (e.g., into the mammary gland for breast cancer) is preferred for modeling the native tumor microenvironment [12].
2. In Vivo Flow Cytometry Setup:
- Photoacoustic Flow Cytometry (PAFC): For detecting intrinsically pigmented cells (e.g., melanoma CTCs). Use a safe laser energy level (e.g., wavelength 1064 nm) focused on a peripheral blood vessel (e.g., mouse ear vessel, 50-250 µm diameter) [12].
- Fluorescence Flow Cytometry (FFC): For detecting fluorescently labeled cells. Use a continuous-wave laser (e.g., 488 nm for GFP) focused on the vessel. Set an amplitude threshold for positive signals (typically mean + 5 standard deviations of the autofluorescence background) [12].
3. Data Acquisition and Continuous Monitoring:
- Anesthetize the mouse and position it to allow stable laser alignment on the target blood vessel.
- Monitor the signal for extended periods (e.g., 60 minutes). Record the timestamp of every signal peak that crosses the set threshold, corresponding to a CTC or CTC cluster passing the detection point [12].
4. Data Analysis:
- CTC Rate Calculation: Divide the total monitoring time into short, consecutive intervals (e.g., 5 minutes). Calculate the CTC rate (cells per 5 min) for each interval to visualize dynamic fluctuations.
- Temporal Dynamics: Plot the CTC rate over time and correlate with primary tumor size measurements (e.g., caliper) and metastasis development (via bioluminescence imaging) at different time points (e.g., weekly) [12].
Key Finding: This protocol typically reveals that CTC counts are highly variable over time and do not always correlate with primary tumor size, with peaks often occurring during early disease stages [12].
Diagram 2: In Vivo CTC Monitoring Workflow. This protocol visualizes the steps for real-time, continuous monitoring of CTC dynamics in a preclinical model, revealing transient fluctuations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Tumor Shedding Studies
| Reagent/Material | Function/Application | Specific Examples/Notes |
|---|---|---|
| CellSearch System | FDA-cleared method for enumerating CTCs from human blood samples. Uses immunomagnetic enrichment based on EpCAM expression [9]. | Standardized for prognostic use in metastatic breast, colorectal, and prostate cancer. Critical for validating novel CTC detection methods [9]. |
| dPCR (digital PCR) | Absolute quantification of mutant allele frequencies in ctDNA without the need for standard curves. High sensitivity for tracking specific mutations [2]. | Ideal for tumor-informed monitoring of known mutations (e.g., in KRAS, EGFR, PIK3CA). Platforms include droplet digital PCR (ddPCR) [2]. |
| Next-Generation Sequencing (NGS) Panels | Comprehensive profiling of multiple genes and mutations from ctDNA. Allows for tumor-uninformed analysis and assessment of heterogeneity [2]. | Targeted panels (e.g., CAPP-Seq, TEC-Seq) offer deep sequencing for high sensitivity. Error-correction methods (e.g., Unique Molecular Identifiers - UMIs) are essential for low-frequency variant calling [2]. |
| Fluorescent Reporter Cell Lines | Enables tracking of tumor cells in vitro and in vivo. Essential for protocols involving in vivo flow cytometry and metastasis validation [12]. | Common reporters: GFP (for FFC), luciferase (for bioluminescence imaging of metastases). Allows for isolation and functional study of CTCs [12]. |
| Antibodies for Surface Marker Enrichment | Isolation and characterization of CTCs and CTC clusters based on cell surface antigen expression. | EpCAM: Common epithelial marker [9].CD44, CD24: Used for identifying cancer stem cell (CSC) subpopulations within CTCs [12]. |
| Nuclease Inhibitors | Preserve the integrity of cell-free nucleic acids in blood collection tubes by inhibiting DNases and RNases. | Critical for pre-analytical sample stabilization. Should be added to blood collection tubes or plasma processing reagents immediately after draw [10]. |
The biology of tumor shedding is complex, dynamic, and central to the application of liquid biopsy. Key characteristics such as the distinct origins and short half-lives of ctDNA and CTCs make them powerful, real-time biomarkers. However, challenges remain, including understanding the biological drivers of differential shedding between lesions and the clinical significance of transient CTC dynamics. As research continues to unravel these secrets, the integration of sophisticated mathematical models like the LSM and advanced detection protocols will be crucial for translating the biology of tumor shedding into improved cancer monitoring and drug development strategies.
Liquid biopsy represents a transformative approach in oncology, enabling the detection and analysis of cancer-derived biomarkers from bodily fluids such as blood, urine, or cerebrospinal fluid [16]. Unlike traditional tissue biopsies, which require invasive surgical procedures and provide only a static snapshot of a dynamic disease, liquid biopsy offers a minimally invasive, repeatable method for tracking cancer progression, detecting early-stage cancers, and monitoring therapeutic responses [17]. This technique primarily focuses on analyzing circulating tumor cells (CTCs), circulating tumor DNA (ctDNA), and other cancer-derived genetic materials that provide critical information on tumor heterogeneity, mutation profiles, and emerging drug resistance [9] [16].
The clinical significance of liquid biopsy is particularly evident in its ability to address fundamental limitations of tissue biopsy. Tissue biopsies are invasive, often limited to a single point in space and time, challenging to repeat, and may fail to reflect the full spectrum of tumor heterogeneity due to sampling bias [17]. In contrast, liquid biopsy captures contributions from multiple tumor sites—including primary and metastatic lesions—providing a more comprehensive molecular profile of the patient's disease [18] [19]. This capability is crucial for guiding personalized treatment strategies in advanced cancers where tumor heterogeneity significantly impacts therapeutic outcomes [20].
Key Advantages of Liquid Biopsy
Non-Invasiveness and Clinical Practicality
The minimally invasive nature of liquid biopsy, typically requiring only a blood draw, translates to substantial clinical benefits over conventional tissue biopsies [21]. This characteristic eliminates procedural risks associated with surgical biopsies, reduces patient discomfort, and enables higher compliance for repeated sampling, which is essential for longitudinal disease monitoring [22]. The simplicity of sample collection facilitates integration into routine clinical workflows, potentially allowing for decentralized testing through local phlebotomy services rather than specialized surgical facilities [17].
From a healthcare systems perspective, the non-invasive nature of liquid biopsy may lead to reduced costs associated with invasive procedures, hospital stays, and management of procedure-related complications [17]. Furthermore, the ability to obtain serial samples enables clinicians to monitor disease progression and treatment response more frequently, potentially identifying treatment failure or disease recurrence earlier than standard imaging modalities [9] [22].
Real-Time Monitoring and Dynamic Assessment
Liquid biopsy enables real-time tracking of tumor evolution, providing clinicians with dynamic information about treatment response and emerging resistance mechanisms [7] [16]. Unlike tissue biopsies, which offer a historical snapshot of the tumor genome at a single time point, liquid biopsy reflects the current molecular status of the disease, allowing for timely treatment adjustments [17].
The dynamic monitoring capability of liquid biopsy is particularly valuable for assessing minimal residual disease (MRD) after curative-intent therapy and detecting early recurrence before clinical or radiographic manifestation [16] [22]. Studies in triple-negative breast cancer (TNBC) have demonstrated that changes in CTC counts during systemic therapy can predict treatment response, with reductions in CTC levels correlating with improved progression-free survival [22]. Similarly, monitoring ctDNA levels can provide early evidence of therapeutic efficacy, often weeks to months before traditional imaging methods can detect changes in tumor burden [9] [21].
Comprehensive Capture of Tumor Heterogeneity
Tumor heterogeneity—encompassing genetic, epigenetic, and phenotypic diversity among cancer cells—represents a significant challenge in cancer treatment, contributing to mixed therapeutic responses and drug resistance [18] [19]. Liquid biopsy effectively addresses this challenge by capturing tumor-derived material released from multiple metastatic sites simultaneously, providing an integrated representation of the tumor's molecular landscape [18] [17].
Research comparing liquid biopsy with multi-region tissue sampling has demonstrated that liquid biopsy can detect spatial heterogeneity that might be missed by a single tissue biopsy [18]. A study analyzing 56 postmortem tissue samples from eight cancer patients found that liquid biopsy identified mutations across different metastatic sites, with overlapping mutation profiles between liquid and tissue biopsies ranging from 33% to 92% [18]. This comprehensive sampling is particularly important for identifying resistance mutations that may emerge in distinct tumor subclones under selective pressure of targeted therapies [7] [19].
Quantitative Comparison: Liquid Biopsy vs. Tissue Biopsy
Table 1: Comparative analysis of key performance metrics between liquid biopsy and tissue biopsy
| Parameter | Liquid Biopsy | Tissue Biopsy | Clinical Implications |
|---|---|---|---|
| Invasiveness | Minimally invasive (blood draw) [21] [16] | Invasive surgical procedure [17] [20] | Reduced procedural risks; improved patient compliance [22] |
| Sampling Frequency | High (repeatable at multiple timepoints) [9] [19] | Limited (difficult to repeat) [17] | Enables dynamic monitoring of treatment response [7] |
| Tumor Representation | Captures contributions from multiple tumor sites [18] [17] | Limited to sampled region [18] [19] | Better representation of heterogeneity [18] |
| Turnaround Time | Potentially faster (e.g., 3+ weeks earlier than tissue) [17] | Longer (requires surgical scheduling and processing) [20] | Earlier treatment decisions [17] |
| Detection of Resistance Mutations | Can identify emerging resistance mutations during treatment [7] [18] | May miss resistance mutations in unsampled regions [18] [19] | More adaptive treatment strategies [7] |
Table 2: Clinical performance of liquid biopsy in capturing tumor heterogeneity based on the study by Dissecting Tumor Heterogeneity by Liquid Biopsy [18]
| Patient | Total Mutations Detected in Tissue | Mutations Detected in Liquid Biopsy | Overlap Rate | Mutations Exclusive to Liquid Biopsy |
|---|---|---|---|---|
| Patient 1 | 8 | 7 | 75% | 2 |
| Patient 2 | 7 | 6 | 67% | 2 |
| Patient 3 | 4 | 5 | 80% | 2 |
| Patient 4 | 12 | 11 | 58% | 6 |
| Patient 5 | 10 | 9 | 60% | 4 |
| Patient 6 | 5 | 4 | 80% | 0 |
| Patient 7 | 6 | 7 | 67% | 2 |
| Overall | 52 | 49 | 69% (average) | 18 (35% of total) |
Liquid Biopsy Biomarkers and Their Clinical Applications
Circulating Tumor Cells (CTCs)
CTCs are cancer cells shed from primary or metastatic tumors into the bloodstream [9] [22]. These cells provide a comprehensive molecular resource as they contain intact DNA, RNA, proteins, and metabolites that reflect the tumor's biological state [21]. The detection and enumeration of CTCs have established prognostic value in multiple cancers, with higher counts correlating with reduced progression-free and overall survival [9] [22].
In breast cancer, particularly TNBC, the presence of ≥5 CTCs per 7.5 mL of blood is associated with significantly worse outcomes, and changes in CTC counts during treatment can predict therapeutic response [22]. Modern CTC isolation technologies, such as the Parsortix system and the CellSearch method (the only FDA-cleared system for CTC enumeration), enable not only counting but also molecular characterization of these cells through downstream analyses like immunofluorescence, FISH, and next-generation sequencing [9] [17].
Circulating Tumor DNA (ctDNA)
ctDNA consists of short DNA fragments (approximately 20-50 base pairs) released into the circulation through apoptosis or necrosis of tumor cells [9] [21]. Although ctDNA typically represents only 0.1-1.0% of total cell-free DNA, its short half-life (approximately 1-2.5 hours) makes it an excellent biomarker for real-time assessment of tumor burden [9].
The clinical utility of ctDNA includes detection of actionable mutations, monitoring of treatment response, identification of emerging resistance mechanisms, and assessment of MRD [9] [16]. In colorectal cancer, monitoring specific mutations (APC, KRAS, TP53, PIK3CA) in ctDNA has been shown to correlate with tumor burden and CEA concentration during therapy [9]. Additionally, ctDNA testing can capture the complete mutational landscape of heterogeneous tumors, overcoming the sampling bias inherent in single-site tissue biopsies [18] [21].
Novel Biomarkers: Circular RNAs and Extracellular Vesicles
Beyond CTCs and ctDNA, liquid biopsy encompasses several emerging biomarkers with significant clinical potential. Circular RNAs (circRNAs) represent a class of stable non-coding RNAs characterized by covalently closed-loop structures that confer resistance to exonuclease degradation [7]. Their remarkable stability in body fluids and association with drug resistance mechanisms—such as miRNA sponging, regulation of apoptosis, and epithelial-mesenchymal transition—make them promising biomarkers for therapeutic monitoring [7].
Extracellular vesicles (EVs), including exosomes, are membrane-bound particles released by cells that contain proteins, nucleic acids, and lipids reflective of their cell of origin [9] [21]. These vesicles play important roles in intercellular communication and tumor microenvironment modulation, carrying tumor-specific molecules that can be exploited for diagnostic and monitoring purposes [9].
Experimental Protocols for Liquid Biopsy Analysis
Protocol for CTC Isolation and Analysis Using the Parsortix System
Principle: CTCs are isolated based on their larger size and deformability compared to blood cells using a microfluidic mechanism [17].
Reagents and Equipment:
- EDTA or citrate blood collection tubes
- Parsortix system (ANGLE plc)
- Phosphate-buffered saline (PBS)
- Fixation buffer (4% formaldehyde)
- Permeabilization buffer (0.1% Triton X-100)
- Antibodies for immunofluorescence (e.g., anti-CK, anti-CD45)
- DAPI staining solution
- Microscope slides and mounting medium
Procedure:
- Collect 10-20 mL of peripheral blood into EDTA or citrate tubes.
- Process blood within 4-8 hours of collection; store at room temperature.
- Load blood sample into Parsortix instrument and run the separation program.
- Harvest captured cells onto a glass slide using the instrument's retrieval mechanism.
- Fix cells with 4% formaldehyde for 15 minutes at room temperature.
- Permeabilize with 0.1% Triton X-100 for 10 minutes if intracellular staining is required.
- Perform immunofluorescence staining using cytokeratin antibodies (epithelial marker) and CD45 antibodies (leukocyte marker) with DAPI for nuclear staining.
- Image slides using a fluorescence microscope and enumerate CTCs (CK+/CD45-/DAPI+).
- For molecular analysis, harvest cells into lysis buffer for nucleic acid extraction.
Downstream Applications:
- CTC enumeration for prognostic assessment
- Immunofluorescence for protein expression analysis
- Fluorescent in situ hybridization (FISH) for gene amplification detection
- Next-generation sequencing for mutation profiling
- Gene expression analysis using RT-PCR [17]
Protocol for ctDNA Analysis Using Next-Generation Sequencing
Principle: ctDNA is extracted from plasma and sequenced to identify tumor-specific mutations, with specialized methods to detect low variant allele frequencies [18].
Reagents and Equipment:
- Streck Cell-Free DNA Blood Collection Tubes or similar
- Plasma preparation tubes (EDTA)
- Centrifuge capable of 1600-3000 × g
- Commercial cfDNA extraction kit (e.g., QIAamp Circulating Nucleic Acid Kit)
- DNA quantification system (e.g., Qubit fluorometer)
- Library preparation kit for NGS
- Target enrichment system (hybridization-based or PCR-based)
- Next-generation sequencer
- Bioinformatics pipeline for variant calling
Procedure:
- Collect blood in cell-free DNA stabilization tubes (e.g., Streck tubes) to prevent genomic DNA contamination.
- Process samples within 6 hours of collection; centrifuge at 1600-3000 × g for 20 minutes to separate plasma.
- Transfer plasma to a fresh tube without disturbing the buffy coat and perform a second centrifugation at 16,000 × g for 10 minutes to remove remaining cells.
- Extract cfDNA using a commercial kit according to manufacturer's instructions.
- Quantify cfDNA using fluorometric methods; expect yields of 5-50 ng/mL plasma.
- Prepare sequencing libraries using protocols optimized for low-input DNA.
- Enrich for target regions (e.g., cancer gene panels) using hybridization capture or multiplex PCR.
- Sequence on an appropriate NGS platform with sufficient depth (typically >10,000x coverage).
- Analyze sequencing data using a bioinformatics pipeline designed for low-frequency variant detection.
Quality Control Considerations:
- Monitor fragment size distribution (ctDNA typically 160-180 bp)
- Include control samples to assess background error rates
- Set appropriate variant allele frequency thresholds (typically 0.1-0.5%)
- Filter out potential artifacts using duplicate removal and molecular barcode strategies [18]
Protocol for circRNA Detection from Plasma
Principle: circRNAs are isolated from plasma or exosomes and detected using reverse transcription-PCR or RNA sequencing with methods specific to their back-spliced junctions [7].
Reagents and Equipment:
- EDTA blood collection tubes
- RNase-free reagents and plasticware
- Centrifuge capable of 16,000 × g
- Total RNA extraction kit
- RNase R treatment (3-5 U/μg RNA)
- Reverse transcription kit
- PCR reagents or digital PCR system
- RNA sequencing library preparation kit
Procedure:
- Collect blood in EDTA tubes and process within 2 hours.
- Centrifuge at 1600-3000 × g for 20 minutes to separate plasma.
- Transfer plasma to a fresh tube and centrifuge at 16,000 × g for 10 minutes to remove vesicles and debris.
- Extract total RNA using a commercial kit with modifications for small RNAs.
- Treat RNA with RNase R (3-5 U/μg RNA) for 30 minutes at 37°C to degrade linear RNAs while preserving circRNAs.
- Perform reverse transcription using random hexamers or gene-specific primers.
- Detect circRNAs using:
- qRT-PCR: Design divergent primers that amplify across the back-splice junction
- Digital PCR: For absolute quantification of specific circRNAs
- RNA Sequencing: Prepare libraries from RNase R-treated RNA and sequence; identify circRNAs through back-splice junction detection algorithms
- Validate circRNA identity by Sanger sequencing of PCR products.
Applications:
- Detection of circRNAs associated with drug resistance (e.g., circHIPK3, circFOXO3)
- Monitoring of circRNA expression changes during therapy
- Correlation with treatment response and survival outcomes [7]
Visualizing Liquid Biopsy Workflows and Tumor Heterogeneity Capture
Diagram 1: Comprehensive workflow for liquid biopsy analysis from sample collection to clinical application
Diagram 2: Liquid biopsy captures comprehensive tumor heterogeneity compared to limited tissue sampling
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagent solutions for liquid biopsy applications
| Reagent/Material | Function | Application Examples | Considerations |
|---|---|---|---|
| Cell-Free DNA Blood Collection Tubes (e.g., Streck, PAXgene) | Stabilizes nucleated blood cells to prevent genomic DNA contamination | ctDNA analysis, especially when delayed processing is anticipated | Maintains sample integrity for up to 7 days at room temperature [18] |
| CTC Enrichment Systems (e.g., Parsortix, CellSearch) | Isolate rare circulating tumor cells from blood | CTC enumeration, molecular characterization, functional studies | Choice between epitope-dependent (CellSearch) and size-based (Parsortix) methods [9] [17] |
| RNase R | Degrades linear RNAs while preserving circular RNAs | circRNA detection and analysis from plasma or exosomes | Treatment conditions must be optimized for different sample types [7] |
| Next-Generation Sequencing Kits | Library preparation and target enrichment for mutation detection | ctDNA sequencing, CTC whole genome/transcriptome analysis | Ultra-sensitive protocols required for low VAF detection (0.1% or lower) [18] |
| Digital PCR Assays | Absolute quantification of rare mutations | Validation of NGS findings, monitoring specific mutations | Higher sensitivity than qPCR for rare variant detection [7] |
| Exosome Isolation Kits (e.g., precipitation, immunoaffinity-based) | Isolation of extracellular vesicles from biofluids | Exosomal RNA/protein analysis, biomarker discovery | Different methods yield exosomes with varying purity and recovery [9] |
Liquid biopsy represents a paradigm shift in cancer management, offering distinct advantages over traditional tissue biopsy through its non-invasive nature, capacity for real-time monitoring, and comprehensive capture of tumor heterogeneity. The integration of multiple analyte approaches—combining CTCs, ctDNA, and novel biomarkers like circRNAs—provides complementary molecular information that enhances our understanding of tumor dynamics and evolution [17] [20].
As liquid biopsy technologies continue to advance with improvements in sensitivity, standardization, and bioinformatics analysis, their role in clinical oncology is expected to expand significantly. Future applications may include population-based cancer screening, ultra-sensitive residual disease detection, and longitudinal adaptation of therapy based on evolving molecular profiles [7] [17]. The ongoing development of standardized protocols and analytical frameworks will be essential for realizing the full potential of liquid biopsy in precision oncology and improving outcomes for cancer patients across the disease spectrum.
Liquid biopsy is transforming oncology by providing a minimally invasive window into tumor biology. While blood plasma is the most common source, biofluids in closer anatomical proximity to tumors often contain higher concentrations of tumor-derived material, offering enhanced sensitivity for detecting cancer biomarkers [23] [24]. These "local" liquid biopsy sources—including urine, saliva, cerebrospinal fluid (CSF), and pleural effusions—enable more precise genomic analysis, early detection, and therapy monitoring while overcoming limitations of traditional tissue biopsies [25] [26]. The selection of an appropriate biofluid is critical and depends on the tumor location, the biomarker of interest, and the specific clinical application, ranging from early detection to monitoring minimal residual disease (MRD) [27]. This article provides a detailed overview of the applications, performance metrics, and standardized protocols for utilizing these alternative biofluids in cancer research and drug development.
The table below summarizes the key characteristics, dominant biomarkers, and clinical applications of the four primary non-blood biofluids.
Table 1: Comparative Analysis of Non-Blood Biofluid Sources for Liquid Biopsy
| Biofluid | Primary Cancer Applications | Key Biomarkers | Advantages | Limitations & Pre-analytical Considerations |
|---|---|---|---|---|
| Urine | Urological (Bladder, Prostate, Renal), also non-urological [24] | ctDNA, cfRNA, EVs [27] [28] | Fully non-invasive collection; Ideal for high-compliance repeated sampling; Low biological risk [24]. | Subject to variable dilution; Requires rapid stabilization to prevent enzymatic degradation of biomarkers; First-void urine often has highest biomarker concentration [23] [24]. |
| Saliva | Oral, Head and Neck, Lung, Pancreatic [29] [30] | Salivary cfDNA (ScfDNA), miRNAs, Proteins, EVs [23] [30] | 85% accuracy for non-oral cancers per meta-analysis [29]; Extremely low-cost and simple collection [29] [30]. | Rapid protein degradation requires additives; Composition varies with stimulation method; Contamination from oral microbes and food particles [29] [30]. |
| Cerebrospinal Fluid (CSF) | Brain Tumors, Leptomeningeal Carcinomatosis [23] [26] | ctDNA, CTCs [23] | Direct window to CNS; High tumor DNA fraction despite low total volume; Critical for assessing intrathecal therapy [23] [24]. | Invasive collection via lumbar puncture; Low total volume and biomarker concentration demands highly sensitive assays [23]. |
| Pleural Effusion | Lung, Breast, Thoracic Cancers [25] [26] | ctDNA, CTCs, miRNAs, EVs [25] | Very high ctDNA concentration & mutant allelic fraction; Outperforms plasma and cell blocks in genotyping sensitivity; Useful for targeted therapy selection [25] [26]. | Requires diagnostic thoracentesis; Distinguishing malignant from benign effusion is crucial; Sample processing must include centrifugation to remove cells and debris [25]. |
Biofluid-Specific Experimental Protocols
Urine Collection and cfDNA Analysis for Urological Cancers
Application: Non-invasive detection of TERT promoter mutations in bladder cancer [24].
Protocol:
- Collection: Collect 50-100 mL of first-void morning urine into a sterile container with an appropriate preservative (e.g., EDTA, proprietary nucleic acid stabilizers) to prevent degradation [23].
- Processing: Centrifuge at 2,000 × g for 10 minutes to pellet cells. Transfer the supernatant to a fresh tube and centrifuge at 16,000 × g for 20 minutes to remove residual debris and vesicles.
- cfDNA Isolation: Extract cfDNA from the clarified supernatant using a silica-membrane or magnetic bead-based kit optimized for low-abundance DNA from urine. Elute in a low volume (e.g., 20-50 µL) of Tris-EDTA buffer.
- Mutation Detection:
- For known variants (e.g., TERT C228T): Use highly sensitive methods like Droplet Digital PCR (ddPCR). Prepare a reaction mix with fluorescent probes for wild-type and mutant alleles, generate droplets, and perform PCR. Analyze on a droplet reader to determine the mutant allele concentration (copies/µL) [27].
- For unknown variants or comprehensive profiling: Use Targeted Next-Generation Sequencing (NGS). Prepare libraries from isolated cfDNA using a panel targeting cancer-associated genes (e.g., Uro-Amplicon Panel). Sequence on a platform like Illumina MiSeq and analyze data with bioinformatics tools (e.g., GATK, VarScan) for variant calling [23].
Saliva Collection and Biomarker Analysis for Oral Cancer Screening
Application: Early detection and monitoring of Oral Squamous Cell Carcinoma (OSCC) via multi-omics analysis [30] [28].
Protocol:
- Collection: Instruct donors not to eat, drink, or smoke for at least 90 minutes prior. Collect unstimulated whole saliva (5-10 mL) by passive drooling into a 50 mL conical tube placed on ice. For standardized collection, use the "Lashley Cup" for gland-specific saliva [30].
- Stabilization and Processing: Immediately add a protease inhibitor cocktail to the sample. Centrifuge at 2,600 × g for 15 minutes at 4°C to remove cells and debris. Aliquot the supernatant and store at -80°C.
- Biomarker Isolation and Analysis:
- DNA Methylation Analysis: Isolate salivary cell-free DNA (ScfDNA) using a commercial kit. Treat DNA with sodium bisulfite to convert unmethylated cytosines to uracils. Analyze using quantitative PCR (qPCR) or pyrosequencing for specific gene promoters (e.g., DAPK, MGMT) or employ a methylation-specific NGS panel [24] [28].
- miRNA Profiling: Extract total RNA, including small RNAs, from 200 µL of processed saliva. Synthesize cDNA and perform RT-qPCR using TaqMan assays for miRNAs of interest (e.g., miR-21, miR-184) [30]. For discovery, use miRNA sequencing.
- Proteomic Analysis: Concentrate proteins from saliva using centrifugal filters. Digest proteins with trypsin and analyze by LC-MS/MS (Liquid Chromatography with Tandem Mass Spectrometry) to identify and quantify cancer-associated proteins (e.g., CD44, IL-8) [31] [30].
Pleural Effusion Processing for ctDNA Genotyping in Lung Cancer
Application: Sensitive detection of EGFR mutations in cytology-negative Malignant Pleural Effusions (MPE) from NSCLC patients [25] [26].
Protocol:
- Collection: Collect pleural fluid during standard therapeutic thoracentesis in EDTA tubes to prevent clotting.
- Processing: Centrifuge the sample at 2,000 × g for 10 minutes to generate a cell pellet (for cytology/cell block) and cell-free supernatant. Transfer the supernatant to a new tube and perform a second, high-speed centrifugation at 16,000 × g for 20 minutes to remove any remaining cellular debris and platelets.
- cfDNA Isolation: Extract cfDNA from the double-centrifuged supernatant using a high-volume plasma cfDNA kit, given the typically high DNA yield. Quantify DNA using a fluorometer.
- Genotyping:
- For routine EGFR mutation testing: Use ddPCR with assays for common mutations (e.g., exon 19 deletions, L858R, T790M). This method offers high sensitivity and absolute quantification of mutant allelic frequency [27] [26].
- For comprehensive genomic profiling: Use NGS with a targeted amplicon-based lung cancer panel (e.g., covering EGFR, KRAS, ALK, etc.). Due to the high tumor fraction in MPE-cfDNA, NGS can reliably detect mutations and resistance mechanisms with high concordance to tissue [25] [26].
Diagram: Universal workflow for biofluid processing in liquid biopsy
The Scientist's Toolkit: Essential Reagent Solutions
Table 2: Key Research Reagents and Kits for Biofluid Analysis
| Reagent/Kits | Primary Function | Application Notes |
|---|---|---|
| cfDNA Isolation Kits (e.g., QIAamp Circulating Nucleic Acid Kit) | Isolation of high-quality, short-fragment cfDNA from biofluid supernatants. | Critical for removing PCR inhibitors; Kits optimized for plasma are generally applicable to urine, CSF, and pleural fluid supernatants. |
| RNA Stabilization Reagents (e.g., RNAlater) | Preservation of RNA integrity in saliva and urine during collection and storage. | Prevents degradation of labile miRNA and other RNA species by RNases; must be added immediately after sample collection. |
| Droplet Digital PCR (ddPCR) Supermixes | Absolute quantification of low-abundance mutations (e.g., EGFR, TERT) without standard curves. | Offers superior sensitivity and precision for detecting rare mutants in a high background of wild-type DNA; ideal for urine and pleural fluid. |
| Targeted NGS Panels (e.g., Illumina TSO 500 ctDNA) | Comprehensive profiling of cancer-associated genes from low-input cfDNA. | Enables detection of single nucleotide variants, indels, and fusions; requires library preparation kits compatible with fragmented DNA. |
| Protease Inhibitor Cocktails | Inhibition of proteases in saliva to prevent protein biomarker degradation. | Essential additive during saliva collection to maintain the integrity of the proteome for subsequent MS or immunoassay analysis. |
| Bisulfite Conversion Kits (e.g., EZ DNA Methylation Kit) | Chemical treatment of DNA for methylation analysis, converting unmethylated C to U. | Key first step for analyzing DNA methylation biomarkers in salivary or urinary cfDNA via PCR or NGS. |
Urine, saliva, CSF, and pleural effusions are powerful biofluid sources that complement and, in some contexts, surpass blood-based liquid biopsies. Their proximity to the tumor site results in higher biomarker concentrations, enabling more sensitive detection of driver mutations, therapy-resistant clones, and minimal residual disease [24] [26]. The ongoing standardization of collection protocols and analytical methods, as outlined in this article, is crucial for integrating these biofluids into robust and reproducible research workflows and clinical trials. As multi-omics approaches and sequencing technologies continue to advance, the strategic use of these localized liquid biopsies will undoubtedly accelerate the development of personalized cancer diagnostics and therapeutics.
Methodologies and Clinical Translation: From Isolation Technologies to Oncology Applications
Liquid biopsy has emerged as a transformative approach in oncology, enabling non-invasive cancer detection, prognosis, and therapy monitoring through the analysis of tumor-derived biomarkers in bodily fluids. Among these biomarkers, circulating tumor cells (CTCs) provide a complete molecular profile of the tumor, including DNA, RNA, and protein information [9]. However, CTCs are exceptionally rare, with approximately 1-10 CTCs present among millions of white blood cells and billions of red blood cells in just 1 milliliter of blood [32]. This extreme rarity presents a significant technological challenge, making efficient isolation and enrichment the critical first step for any subsequent analysis.
This Application Note provides a detailed technical overview of three principal methodologies for CTC isolation and enrichment: immunomagnetic capture, microfluidics, and size-based filtration. We focus on practical protocols, performance metrics, and reagent solutions to support researchers in implementing these techniques within the broader context of liquid biopsy for cancer monitoring.
Technical Comparison of Core Technologies
The table below summarizes the fundamental principles, advantages, and limitations of the three primary CTC isolation techniques.
Table 1: Comparison of Core CTC Isolation and Enrichment Techniques
| Technique | Fundamental Principle | Key Advantages | Major Limitations |
|---|---|---|---|
| Immunomagnetic Capture | Uses antibody-coated magnetic beads targeting surface antigens (e.g., EpCAM) on CTCs [32]. | High purity and specificity; amenability to automation (e.g., CellSearch system) [32] [9]. | Bias towards CTCs expressing the target antigen; potential loss of phenotypically heterogeneous or EpCAM-low CTCs [32]. |
| Microfluidics | Leverages microscale fluid dynamics and device structures to separate CTCs based on physical or affinity properties [33]. | High recovery rates and cell viability; low reagent consumption; integration with downstream analysis [33]. | Throughput limitations for processing large blood volumes; potential for channel clogging [34] [33]. |
| Size-Based Filtration | Separates CTCs from smaller hematological cells using physical filters with precise pore sizes (e.g., 5-10 μm) [33]. | Label-free, antigen-agnostic approach; preserves cell viability; simple and cost-effective [33]. | Reduced purity due to retained leukocytes of similar size; may miss CTCs that are small or highly deformable [33]. |
Detailed Experimental Protocols
Protocol: Immunomagnetic Negative Enrichment of CTCs
This protocol describes a negative selection method to isolate CTCs without relying on tumor-specific surface markers, thereby capturing a more heterogeneous population, including those undergoing epithelial-mesenchymal transition (EMT) [35].
Workflow Overview:
Materials & Reagents:
- Blood Sample: 7.5-10 mL of peripheral blood collected in EDTA or citrate tubes.
- Density Gradient Medium: Ficoll-Paque PREMIUM.
- Biotinylated Antibodies: Anti-CD45 (pan-leukocyte), anti-CD66b (granulocyte), anti-CD16 (monocyte) [35].
- Magnetic Beads: Streptavidin-coated magnetic beads.
- Enrichment Buffer: A specially formulated buffer that functions as a density gradient medium and a solvent for cell coating, enhancing the efficiency of immunomagnetic separation [35].
- Magnetic Separation Stand.
Procedure:
- PBMC Isolation:
- Layer 10 mL of blood carefully over 5 mL of density gradient medium in a 15 mL centrifuge tube.
- Centrifuge at 400 × g for 30-40 minutes at room temperature with the brake disengaged.
- Aspirate and transfer the peripheral blood mononuclear cell (PBMC) layer (a distinct buffy coat) to a new 15 mL tube.
Antibody Incubation and Magnetic Labeling:
- Wash the PBMCs twice with 10 mL of PBS containing 2% FBS.
- Resuspend the cell pellet in 1 mL of enrichment buffer.
- Add a cocktail of biotinylated antibodies (anti-CD45, anti-CD66b, anti-CD16) to the cell suspension. Incubate for 30 minutes on a rotator at 4°C.
- Wash the cells twice with 10 mL of enrichment buffer to remove unbound antibodies.
- Resuspend the cell pellet in 1 mL of enrichment buffer. Add streptavidin-coated magnetic beads and incubate for 15 minutes on a rotator at 4°C.
Magnetic Separation:
- Place the tube in a magnetic separation stand for 5-10 minutes.
- Carefully transfer the supernatant, which contains the unlabeled, enriched CTC population, to a new tube.
- Centrifuge the supernatant to collect the CTC pellet for downstream analysis.
Protocol: High-Throughput Microfluidic Enrichment via LPCTC-iChip
This advanced protocol processes large blood volumes from leukapheresis products (leukopaks) to achieve unprecedented CTC yields, enabling deep molecular profiling [34].
Workflow Overview:
Materials & Reagents:
- Leukopak: 100-150 mL diagnostic leukapheresis product.
- LPCTC-iChip System: Comprising a debulking chip and a MAGLENS (magnetic lens) chip [34].
- Biotinylated Antibodies: Anti-CD45, anti-CD66b, anti-CD16.
- Streptavidin Magnetic Beads.
- Peristaltic Pump capable of high-flow rates.
Procedure:
- Sample Preparation:
- Obtain a leukopak, which contains a mean of 5.3 ± 2.3 billion WBCs, from approximately 5.83 liters of processed patient blood [34].
- Filter the leukopak through a 42 µm filter to remove large aggregates and clots.
Antibody Incubation:
- Incubate the entire leukopak sample with a cocktail of biotinylated antibodies against CD45, CD66b, and CD16 for 30 minutes at room temperature.
Microfluidic Processing:
- Debulking Stage: Pump the sample through the inertial separation array (debulking chip) at a high flow rate (e.g., 10-20 mL/min) to remove red blood cells, platelets, and plasma.
- Magnetic Depletion Stage: Direct the nucleated cell output to the MAGLENS chip. This chip uses force-amplifying magnetic lenses to apply a strong magnetic field, deflecting and trapping antibody- and bead-labeled WBCs. The untagged CTCs flow through the device and are collected.
- The LPCTC-iChip technology can process an entire leukopak in hours, achieving a WBC depletion of >10,000-fold and yielding thousands of CTCs per patient [34].
Protocol: Size-Based Filtration Using Microsieves
This protocol offers a straightforward, label-free method for CTC enrichment based on the larger size and lower deformability of most tumor cells compared to blood cells [33].
Materials & Reagents:
- Blood Sample: 7.5-10 mL of peripheral blood.
- Microsieve Device: Silicon or polymer membrane with uniform pores (diameter 5-10 µm).
- Lysis Buffer: For optional red blood cell (RBC) lysis.
- Fixative: 4% Paraformaldehyde (PFA) for cell fixation.
- Permeabilization Buffer: 0.1% Triton X-100 in PBS.
- Staining Antibodies: Anti-cytokeratin (CK), anti-CD45, and DAPI.
Procedure:
- Sample Preparation (Optional):
- Lyse red blood cells using a commercial lysis buffer to reduce sample volume and cellular debris. Alternatively, use whole blood directly.
Filtration:
- Load the prepared blood sample onto the microsieve device.
- Apply a gentle vacuum or positive pressure to drive the sample through the membrane. CTCs and large leukocytes are retained on the membrane, while smaller blood cells pass through.
- Wash the membrane with PBS to remove non-specifically bound cells.
On-Device Staining and Analysis:
- Fix the cells on the membrane with 4% PFA for 15 minutes.
- Permeabilize the cells with 0.1% Triton X-100 for 10 minutes.
- Stain with anti-CK (for epithelial CTCs), anti-CD45 (to identify contaminating leukocytes), and DAPI (to label nuclei) for 1 hour.
- Image the membrane using fluorescence microscopy. CTCs are typically identified as CK+/CD45-/DAPI+ cells.
Performance Metrics and Data Analysis
Evaluating the performance of an isolation technique is crucial. The table below defines and summarizes target values for key performance metrics.
Table 2: Key Performance Metrics for CTC Enrichment Technologies
| Performance Metric | Definition & Calculation | Reported Performance Ranges |
|---|---|---|
| Capture/Recovery Rate | Percentage of spiked tumor cells successfully isolated. Formula: (Captured Tumor Cells / Spiked Tumor Cells) × 100% [32]. |
Immunomagnetic: >80% (CellSearch) [32].Microfluidics: ~86% (LPCTC-iChip) [34].Size-Based: ~80% for certain cell lines [33]. |
| Purity | Percentage of target CTCs among all captured cells. Formula: (Captured CTCs / (Captured CTCs + Captured WBCs)) × 100% [32]. |
Typically low for size-based filtration (<10%) due to leukocyte retention. Significantly higher for affinity-based methods. Negative enrichment microfluidics can achieve high purity via massive WBC depletion (>10⁴-fold) [34]. |
| Viability | Percentage of captured cells that remain viable for downstream culture. Formula: (Viable CTCs / (Viable + Apoptotic CTCs)) × 100% [32]. |
Label-free methods (size-based, some microfluidics) generally preserve higher viability. The LPCTC-iChip maintains cell viability for molecular analysis [34]. |
| Throughput | Volume of blood processed per unit time (mL/h). | Standard microchips: ~1-20 mL/h [33].High-Throughput Microfluidics (LPCTC-iChip): Processes entire leukopak (~100 mL) in hours [34]. |
| Cell Yield | Absolute number of CTCs isolated from a patient sample. | Standard 10mL blood draw: 0-10 CTCs in metastatic cancer [34].Leukapheresis + LPCTC-iChip: Mean of 10,057 CTCs per patient (range: 100 to 58,125) [34]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for CTC Enrichment
| Item | Function/Application | Example Specifications |
|---|---|---|
| Anti-EpCAM Magnetic Beads | Positive selection of epithelial CTCs in immunomagnetic assays. | Conjugated to magnetic microparticles; compatible with automated systems [32]. |
| CD45/CD66b/CD16 Antibody Cocktail | Negative depletion of hematopoietic cells (WBCs) for antigen-agnostic CTC capture. | Biotinylated for linkage to streptavidin beads; used in microfluidic and batch immunomagnetic protocols [34] [35]. |
| Specialized Enrichment Buffer | Enhances immunomagnetic separation efficiency by combining density gradient and cell coating properties [35]. | Optimized density and viscosity; contains reagents to minimize non-specific binding and cell aggregation. |
| Layer-by-Layer (LbL) Antibody Mesh | A physical filter functionalized with multiple layers of antibodies (e.g., anti-EpCAM) to increase capture efficiency and specificity [36]. | Gold-plated mesh with 20 µm pores; trilayered antibody network shown to improve clinical sample accuracy from 40% to 100% vs. single layer [36]. |
| Microfluidic Debulking Chip | Removes the bulk of RBCs, platelets, and plasma from large-volume samples like leukopaks prior to fine sorting [34]. | Contains inertial separation arrays; handles high flow rates and sample concentrations. |
| MAGLENS Microfluidic Chip | High-throughput depletion of magnetically labeled WBCs from pre-debulked samples [34]. | Incorporates "magnetic lenses" that amplify magnetic forces by 35-fold, enabling high-flow sorting. |
The isolation and enrichment of CTCs are foundational to realizing the potential of cell-based liquid biopsies. The protocols detailed herein—immunomagnetic capture, microfluidics, and size-based filtration—each offer distinct advantages and are suited to different research objectives. Immunomagnetic methods provide high specificity, size-based filtration is a simple and label-free approach, while advanced microfluidic technologies like the LPCTC-iChip are pushing the boundaries of CTC yield by processing liters of blood, thereby enabling comprehensive single-cell and molecular analyses. The choice of technique depends on the specific application, required throughput, and the need for downstream analysis of these rare but information-rich cells.
Liquid biopsy has emerged as a transformative paradigm in oncology, enabling non-invasive detection and monitoring of cancer through the analysis of circulating tumor-derived biomarkers, most notably circulating tumor DNA (ctDNA). The effective profiling of these biomarkers relies on sophisticated analytical detection platforms capable of identifying rare mutations within a high background of wild-type DNA. [37] [9]
The table below summarizes the core characteristics, advantages, and limitations of four key technologies used in liquid biopsy analysis.
Table 1: Comparison of Key Analytical Detection Platforms for Liquid Biopsy
| Platform | Core Principle | Key Applications in Liquid Biopsy | Sensitivity (Mutant Allele Frequency) | Major Advantages | Inherent Limitations |
|---|---|---|---|---|---|
| Next-Generation Sequencing (NGS) | Massively parallel sequencing of DNA fragments [37]. | - Genome-wide discovery of unknown variants [37]- Tumor agnostic screening [38]- Comprehensive genomic profiling [39] | < 1% [37] | - High-throughput & multiplexing capability [37]- Detects novel/unknown alterations [37]- Interrogates multiple alteration types (SNVs, CNAs, fusions) [38] | - Higher cost and longer turnaround time vs. PCR [38]- Requires complex bioinformatics [38]- Background sequencing error noise [1] |
| Digital PCR (dPCR) | Partitioning of sample into thousands of nanoreactors for absolute quantification via Poisson statistics [40]. | - Ultra-sensitive detection of known, specific mutations [40]- Treatment response monitoring [40]- MRD tracking [1] | < 0.1% [37] [40] | - Ultra-high sensitivity and specificity [40]- Absolute quantification without standard curves [40]- Robust and reproducible [40] | - Low-plex; limited to pre-defined known mutations [38] [40]- Cannot detect copy number alterations or fusions easily [38] |
| BEAMing | Beads, Emulsion, Amplification, and Magnetics; combines dPCR with flow cytometry [37] [40]. | - Extremely rare variant detection [37]- Early-stage cancer screening [37] | 0.02% [37] | - Exceptional sensitivity for single-molecule detection [37] [40]- Can be highly multiplexed [40] | - Complex, multi-step protocol [37]- Relatively expensive for routine clinical use [37] |
| CAPP-Seq | Cancer Personalized Profiling by deep Sequencing; uses optimized NGS library prep and bioinformatics [38]. | - Highly sensitive and specific targeted NGS [38]- MRD detection [38]- Therapy response monitoring [38] | ~0.1% [38] | - High sensitivity and specificity within NGS framework [38]- Cost-effective targeted approach [38]- Can detect SNVs and CNAs [38] | - Still an NGS-based method with associated cost and complexity [38]- Requires specialized bioinformatic probes and analysis [38] |
Detailed Methodologies and Experimental Protocols
Next-Generation Sequencing (NGS) for ctDNA Analysis
NGS enables comprehensive profiling of ctDNA by sequencing millions of DNA fragments in parallel, allowing for the detection of single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), and chromosomal rearrangements, even at low variant allele frequencies. [37] [38]
Table 2: Essential Research Reagents for NGS-based ctDNA Analysis
| Item/Category | Specific Examples | Function in the Workflow |
|---|---|---|
| Blood Collection Tube | Streck Cell-Free DNA BCT [39] | Stabilizes nucleated blood cells to prevent genomic DNA contamination of plasma cfDNA. |
| cfDNA Extraction Kit | QIAamp Circulating Nucleic Acid Kit [39] | Isolates and purifies cell-free DNA from plasma samples. |
| Library Prep Kit | TruSight Oncology ctDNA v2 [41] | Prepares DNA fragments for sequencing by adding adapters and sample indices. |
| Target Enrichment | Hybrid-capture probes or Amplicon-based panels [38] | Selectively enriches genomic regions of interest from the total cfDNA library. |
| Sequencing Platform | Illumina NovaSeq X Series [41] | Performs massively parallel sequencing of the prepared libraries. |
| Bioinformatics Tools | Variant callers, CAPP-Seq analyzer [38] | Aligns sequences to a reference genome and identifies somatic mutations. |
Protocol: Targeted NGS Workflow for ctDNA Detection
Sample Collection and Plasma Isolation: Collect peripheral blood (typically 10-20 mL) into Streck or similar cell-stabilizing tubes. [39] Invert gently to mix. Centrifuge using a two-step protocol: first at 1,600 × g for 10 minutes at 4°C to separate plasma from blood cells, then transfer the supernatant to a microcentrifuge tube and centrifuge at 16,000 × g for 10 minutes to remove any remaining cellular debris. [39] Aliquot plasma and store at -80°C if not processing immediately.
ctDNA Extraction and Quantification: Extract cfDNA from plasma (typically 1-5 mL) using the QIAamp Circulating Nucleic Acid Kit or equivalent, following the manufacturer's instructions. [39] Elute the DNA in a low-EDTA buffer or nuclease-free water. Quantify the extracted cfDNA using a fluorescence-based assay (e.g., Qubit dsDNA HS Assay) due to its sensitivity and specificity for double-stranded DNA over spectrophotometric methods.
NGS Library Preparation: Use 5-50 ng of cfDNA as input for library construction. Prepare sequencing libraries using a targeted kit such as the TruSight Oncology ctDNA v2 assay. [41] This involves:
- End-Repair and A-Tailing: Repair the fragment ends and add a single 'A' nucleotide to facilitate adapter ligation.
- Adapter Ligation: Ligate indexed sequencing adapters to the ctDNA fragments.
- Library Amplification: Perform a limited-cycle PCR to amplify the adapter-ligated library.
Target Enrichment: Enrich for specific genomic regions (e.g., a cancer gene panel) using hybrid-capture-based methods. Hybridize the library to biotinylated oligonucleotide probes designed against the target regions, then capture the probe-bound complexes using streptavidin-coated magnetic beads. Wash away non-specifically bound DNA and perform a post-capture PCR amplification to enrich the final library for the targets of interest.
Sequencing and Data Analysis: Pool the indexed libraries and sequence on a high-throughput platform like the Illumina NovaSeq X Series to achieve a minimum coverage of 10,000x, which is critical for detecting low-frequency variants. [41] For data analysis:
- Alignment: Align the raw sequencing reads to the human reference genome (e.g., GRCh37/hg19).
- Variant Calling: Use a specialized somatic variant caller (e.g., for SNVs, indels) that incorporates error-suppression models to distinguish true low-frequency mutations from sequencing artifacts.
- Annotation and Reporting: Annotate the filtered variants and report on actionable genomic alterations.
NGS ctDNA Analysis Workflow
Digital PCR for Ultra-Sensitive Mutation Detection
Digital PCR (dPCR) achieves ultra-sensitive absolute quantification of known mutations by partitioning a PCR reaction into thousands of nanoliter-scale reactions, such that each partition contains zero, one, or a few target molecules. [40] Following end-point PCR amplification, the fraction of positive partitions is counted, and the original target concentration is calculated using Poisson statistics. [40]
Protocol: Droplet Digital PCR (ddPCR) for Single-Nucleotide Variant (SNV) Quantification
Assay Design: Design and validate two probe-based assays: a mutant-specific probe (e.g., labeled with FAM fluorophore) and a wild-type-specific probe (e.g., labeled with HEX or VIC fluorophore).
Droplet Generation: In a microcentrifuge tube, combine 8 µL of ddPCR Supermix for Probes (no dUTP), 1 µL of the combined primer/probe assay, and 7 µL of the extracted ctDNA sample (up to 50 ng). Gently pipette the entire reaction mixture into a DG8 cartridge. Add 70 µL of droplet generation oil into the appropriate well. Place the cartridge into the droplet generator. This instrument partitions the 20 µL reaction into approximately 20,000 nanodroplets.
PCR Amplification: Carefully transfer the generated emulsion of droplets from the cartridge into a 96-well PCR plate. Seal the plate with a foil heat seal. Perform PCR amplification in a thermal cycler using optimized cycling conditions for the target sequence. A standard program includes: 10 minutes at 95°C (enzyme activation), followed by 40 cycles of 30 seconds at 94°C (denaturation) and 60 seconds at 55-60°C (annealing/extension), and a final signal stabilization step at 98°C for 10 minutes. Hold the plate at 4°C until ready for reading.
Droplet Reading and Data Analysis: Place the PCR plate into the droplet reader. The instrument aspirates the droplets from each well, streams them single file past a two-color optical detection system, and classifies each droplet as FAM-positive (mutant), HEX-positive (wild-type), positive for both, or negative. Analyze the data using the accompanying software. The concentration (copies/µL) of the mutant and wild-type sequences in the original sample is provided as an absolute value, from which the mutant allele frequency (MAF) can be calculated.
dPCR Mutation Detection Workflow
BEAMing Technology
BEAMing (Beads, Emulsion, Amplification, and Magnetics) is a highly sensitive technology that converts single DNA molecules into magnetic beads bearing thousands of copies of that DNA sequence, which can then be analyzed via flow cytometry. [37] [40]
Protocol: BEAMing Workflow for Rare Variant Detection
Template Annealing and Emulsion PCR: Dilute the ctDNA sample and mix it with magnetic beads coated with primers complementary to the target sequence, PCR reagents, and a water-in-oil emulsion mixture. The emulsion is vigorously vortexed to create millions of microreactors, each ideally containing a single bead and a single DNA molecule. The emulsion is then subjected to PCR amplification, resulting in beads that are covered with thousands of copies of the original DNA template.
Emulsion Breaking and Bead Recovery: After amplification, the emulsion is broken by adding an organic solvent (e.g., isopropanol) and centrifugation. The supernatant is removed, and the magnetic beads are collected using a magnet and washed.
Hybridization and Flow Cytometry: The amplified beads are incubated with fluorescently labeled oligonucleotide probes specific for the wild-type and mutant sequences. Each probe is labeled with a different fluorophore. The beads are then analyzed by flow cytometry. Beads that hybridize only to the mutant probe are counted as mutant, those that hybridize only to the wild-type probe are wild-type, and a small population may hybridize to both. The ratio of mutant beads to total beads provides the mutant allele frequency.
CAPP-Seq
CAPP-Seq is a targeted NGS methodology designed to optimize the sensitivity and specificity of ctDNA detection through informed selector design and specialized bioinformatics. [38]
Protocol: CAPP-Seq for Personalized Mutation Tracking
Selector Design: For a tumor-informed (personalized) approach, first sequence the tumor tissue (e.g., by whole-exome or whole-genome sequencing) to identify a set of somatic mutations (typically 10-20) specific to that patient's cancer. Design biotinylated DNA oligonucleotide "selectors" (hybrid-capture probes) that target these identified mutations and their immediate genomic context.
Library Preparation and Hybrid-Capture: Prepare NGS libraries from the patient's plasma-derived cfDNA. Hybridize these libraries to the custom-designed selector pool. This step enriches the sequencing library for DNA fragments containing the patient-specific tumor mutations.
Sequencing and Integrated Error-Suppression: Sequence the captured libraries to high depth. Use a dedicated bioinformatic pipeline that incorporates an error-suppression model. This model corrects for sequencing errors and PCR artifacts by leveraging features such as base quality scores, family sequencing (if unique molecular identifiers are used), and the specific sequence context, thereby significantly enhancing the signal-to-noise ratio for detecting true, low-frequency variants.
Research Applications in Cancer Monitoring
The described platforms are pivotal in advancing cancer research and personalized medicine through several key applications:
Minimal Residual Disease (MRD) and Relapse Monitoring: Ultrasensitive platforms like dPCR and tumor-informed NGS/CAPP-Seq can detect ctDNA from MRD long before clinical or radiographic recurrence becomes apparent. Studies show that ctDNA-positive status after curative-intent surgery or adjuvant therapy is a powerful predictor of imminent relapse and is associated with significantly worse disease-free and overall survival. [37] [1] [38]
Therapy Selection and Response Monitoring: Liquid biopsy enables non-invasive genotyping to identify actionable genomic alterations (e.g., EGFR, KRAS, BRAF mutations) that guide targeted therapy. [39] [38] The short half-life of ctDNA (16 min to 2.5 hours) allows for real-time monitoring of treatment efficacy, with a rapid decline in ctDNA levels often correlating with favorable response, and the emergence of new mutations indicating therapy resistance. [37] [1]
Early Detection and Screening: While challenges remain regarding sensitivity in very early-stage disease and specificity in healthy populations, technologies like CAPP-Seq, BEAMing, and methylation-based NGS assays are being actively investigated for multi-cancer early detection. [37] [41] The TRACERx study, for example, demonstrated that ctDNA could be detected in plasma up to six months before clinical diagnosis of relapse. [39]
Liquid biopsy has emerged as a transformative, minimally invasive approach for analyzing biomarkers in bodily fluids, revolutionizing cancer diagnosis, prognosis, and treatment monitoring [42]. This paradigm is particularly impactful in the context of therapy selection, enabling the identification of actionable mutations and prediction of response to immune checkpoint inhibitor (ICI) immunotherapy. By capturing tumor-derived components such as circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs) from blood, liquid biopsies provide a comprehensive view of tumor heterogeneity and dynamic changes under therapeutic pressure [27] [43]. For researchers and drug development professionals, these techniques facilitate real-time assessment of treatment efficacy, detection of resistance mechanisms, and informed decision-making for personalized treatment strategies, ultimately advancing precision medicine in oncology.
Actionable Mutation Detection via Liquid Biopsy
Key Analytes and Detection Platforms
The identification of actionable mutations relies on the isolation and analysis of specific tumor-derived components from liquid biopsy samples. The table below summarizes the primary analytes, their clinical significance, and technologies used for their detection.
Table 1: Key Liquid Biopsy Analytes for Actionable Mutation Detection
| Analyte | Description | Detection Technologies | Primary Applications in Therapy Selection |
|---|---|---|---|
| ctDNA | Cell-free DNA fragments shed by tumors into circulation [42] | ddPCR, NGS panels, WGS, MUTE-Seq [27] [44] | Detection of specific driver mutations (e.g., EGFR), monitoring resistance, MRD assessment |
| CTCs | Intact tumor cells circulating in peripheral blood [42] | Immunomagnetic enrichment, morphological analysis [27] | Morphological evaluation, chromosomal instability assessment, predicting taxane resistance [27] |
| Extracellular Vesicles (EVs) | Membrane-bound vesicles carrying proteins, nucleic acids [42] | Immunocapture, ultracentrifugation, nanoparticle tracking [42] | Analysis of surface markers, miRNA profiling, particularly in neuroblastoma [27] |
| cell-free RNA (cfRNA) | RNA transcripts released from tumor cells [27] | RNA-seq, targeted PCR, uRARE-seq [27] | Urine-based MRD assessment in bladder cancer, gene expression profiling [27] |
Comprehensive Protocol: Actionable Mutation Profiling from Plasma
Objective: To isolate and analyze ctDNA from patient blood samples for identification of actionable mutations guiding targeted therapy selection.
Materials and Reagents:
- Streck Cell-Free DNA Blood Collection Tubes or equivalent
- Plasma preparation tubes (PPT)
- QIAamp Circulating Nucleic Acid Kit (Qiagen) or similar ctDNA extraction kit
- Agilent High Sensitivity DNA Kit for Bioanalyzer quality control
- KAPA HyperPrep Kit (Roche) for library preparation
- IDT xGen Pan-Cancer Panel v2 or similar targeted NGS panel
- Illumina MiSeq or NextSeq sequencing platform
- Archer VariantPlex for structural variant detection (optional)
Experimental Workflow:
Sample Collection and Processing:
- Collect 10 mL peripheral blood into cell-free DNA preservation tubes.
- Process within 6 hours of collection: centrifuge at 1,600 × g for 20 min at 4°C to separate plasma.
- Transfer supernatant to fresh tube and centrifuge at 16,000 × g for 10 min to remove residual cells.
- Aliquot plasma and store at -80°C if not extracting immediately.
ctDNA Extraction and Quantification:
- Extract ctDNA from 2-4 mL plasma using validated extraction kits according to manufacturer protocols.
- Elute in 20-50 μL elution buffer.
- Quantify using fluorometric methods (Qubit dsDNA HS Assay).
- Assess fragment size distribution using Bioanalyzer or TapeStation.
Library Preparation and Sequencing:
- Convert 10-50 ng ctDNA to sequencing libraries using KAPA HyperPrep Kit.
- Hybridize with targeted pan-cancer panel (100-200 genes) for 16 hours.
- Capture with streptavidin beads, wash, and amplify with index primers.
- Pool libraries and sequence on Illumina platform (minimum 5,000x coverage).
Bioinformatic Analysis:
- Align reads to reference genome (hg38) using BWA-MEM or similar aligner.
- Call variants with MuTect2 for single nucleotide variants and Indels.
- Annotate variants with Oncotator or similar tools.
- Filter against population databases (gnomAD) and prioritize actionable alterations using OncoKB or similar knowledgebase.
Quality Control Considerations:
- Include negative controls (water) and positive controls (reference ctDNA) in each batch.
- Establish limit of detection (LOD) for variant allele frequency (VAF); typically 0.1-0.5% for most NGS panels.
- Monitor sequencing metrics: >80% on-target reads, >90% uniformity, mean coverage >5000x.
Predictive Biomarkers for ICI Response
Multidimensional Biomarker Framework
Predicting response to ICI therapy requires a multidimensional approach integrating biomarkers from various sources. The table below categorizes key predictive biomarkers and their clinical utility.
Table 2: Predictive Biomarkers for ICI Immunotherapy Response
| Biomarker Category | Specific Biomarkers | Detection Methods | Predictive Value and Clinical Utility |
|---|---|---|---|
| Tumor Cells-Derived | TMB, TNB, MSI, PD-L1 expression [44] | WES, NGS panels, IHC [44] | TMB-H (>10 mut/Mb) associated with improved response in multiple cancers; MSI-H predicts response to pembrolizumab [44] |
| Liquid Biopsy-Based | bTMB, ctDNA, CTCs, miRNAs [44] | ctDNA sequencing, CTC enumeration [44] | Baseline ctDNA levels prognostic for OS; ctDNA dynamics predict early response; CTC morphological features predict taxane resistance [27] |
| TIME-Derived | Immune cell densities, spatial relationships [45] | Multiplex IHC/IF, digital pathology, AI [45] [46] | PD-L1+ macrophages near tumor edge superior to bulk PD-L1 (AUC 0.98); CD8+ T-cell density and location predictive [45] |
| Gut Microbiome | Specific microbial signatures [44] | 16S rRNA sequencing, metagenomics [44] | Faecalibacterium and Bacteroidetes associated with response; microbiome modulation improves outcomes [44] |
Advanced Protocol: Predicting ICI Response Using Multi-Modal Liquid Biopsy
Objective: To integrate multiple liquid biopsy analytes for comprehensive prediction of response to ICI therapy.
Materials and Reagents:
- EDTA blood collection tubes for CTC analysis
- Streck Cell-Free DNA BCT tubes for ctDNA
- RosetteSep CTC Enrichment Cocktail (StemCell Technologies)
- CELLSEARCH CTC Kit or similar CTC enumeration system
- Qiagen miRNeasy Serum/Plasma Kit for miRNA isolation
- TaqMan Advanced miRNA cDNA Synthesis Kit
- FirePlex miRNA Assay (Abcam) for multiplex miRNA profiling
Experimental Workflow:
Sample Collection and Processing:
- Collect 20-30 mL blood total, splitting between EDTA (5 mL for CTCs) and Streck tubes (15 mL for ctDNA/miRNA).
- For CTC isolation: process EDTA tubes within 4 hours using density gradient centrifugation or microfluidic capture.
- For ctDNA/miRNA: process Streck tubes as in Protocol 2.1.
Multi-Analyte Analysis:
- bTMB Assessment: Isolate ctDNA and perform targeted NGS sequencing of 1-1.5 Mb genome. Calculate bTMB as mutations per megabase using validated algorithms.
- CTC Characterization: Enumerate CTCs using CELLSEARCH system. For morphological analysis, use imaging-based platforms to assess chromosomal instability (CTC-CIN) as predictor of taxane resistance [27].
- miRNA Profiling: Isolve miRNAs from 200 μL plasma using miRNeasy Kit. Prepare libraries and profile using FirePlex immunoassay focusing on immunomodulatory miRNAs (e.g., miR-21, miR-29, miR-155).
- Inflammatory Proteomics: Analyze 50 μL plasma using Olink Target 96 Immuno-Oncology Panel to quantify CXCL11 and other inflammatory proteins associated with immunotherapy toxicity [27].
Data Integration and Model Building:
- Normalize all biomarkers using z-scores or percentile transformation.
- Apply machine learning algorithms (random forest, logistic regression) to integrated biomarker data.
- Develop predictive score combining bTMB, CTC count, miRNA signature, and inflammatory proteins.
- Validate model using independent cohort with ROC analysis; target AUC >0.75 for clinical utility.
Quality Control Considerations:
- Standardize pre-analytical variables across collection sites.
- Use reference standards for each analyte type.
- Establish reproducibility through technical replicates.
Computational Approaches and AI Integration
Machine Learning Models for Response Prediction
Artificial intelligence, particularly machine learning (ML) and deep learning (DL), significantly enhances the predictive power of liquid biopsy data for ICI response prediction [46]. These computational approaches can integrate complex, multi-modal data to generate clinically actionable predictions.
Table 3: Computational Models for ICI Response Prediction
| Model Type | Specific Examples | Input Data | Performance and Applications |
|---|---|---|---|
| Supervised ML | SCORPIO, LORIS [47] | Clinical variables, genomic features, protein biomarkers | AUC 0.763, superior to single biomarkers; predicts progression-free survival [47] |
| Deep Learning | Deep convolutional neural networks (DCNN) [48] | H&E whole slide images, radiomic features | AUC 0.72 for predicting ICI response in melanoma; identifies histomorphologic features associated with survival [48] |
| Hybrid Models | QSP models with ML integration [44] | Pharmacokinetic data, tumor growth metrics, immune cell densities | Simulates dynamic interactions between tumor and immune system; predicts optimal dosing schedules [44] |
| Self-Supervised Learning | SSL for histology images [48] | Unlabeled H&E images, outcome data | Identifies novel tumor features (epithelioid histology, low tumor-stroma ratio) associated with survival [48] |
Implementation Protocol: AI-Driven Predictive Modeling
Objective: To develop and validate a machine learning model for predicting ICI response using integrated liquid biopsy and clinical data.
Computational Tools and Environment:
- Python 3.8+ with scikit-learn, TensorFlow, PyTorch libraries
- R 4.1+ with survival, randomForestSRC, glmnet packages
- High-performance computing cluster with GPU acceleration
- Data visualization tools (Tableau, R Shiny)
Methodological Workflow:
Data Preprocessing:
- Clean and normalize multi-omics data (ctDNA variant calls, miRNA counts, protein levels).
- Handle missing data using multiple imputation or k-nearest neighbors.
- Perform feature selection using variance filtering and correlation analysis.
Model Training:
- Partition data into training (70%), validation (15%), and test (15%) sets.
- Train multiple algorithms: random forest, gradient boosting, neural networks.
- Optimize hyperparameters using grid search with cross-validation.
- For survival outcomes, implement Cox proportional hazards models with regularization.
Model Validation:
- Assess performance using AUC, precision-recall curves, calibration plots.
- Perform internal validation via bootstrapping (1000 iterations).
- External validation on independent dataset from different institution.
- Evaluate clinical utility with decision curve analysis.
Model Interpretation:
- Compute feature importance using SHAP (SHapley Additive exPlanations) values.
- Generate partial dependence plots to visualize feature-response relationships.
- Develop simplified clinical scoring system based on top predictive features.
Implementation Considerations:
- Address class imbalance in responder/non-responder groups using SMOTE or weighted loss functions.
- Ensure reproducibility through version control (Git) and containerization (Docker).
- Develop clinician-friendly interface for model deployment in hospital settings.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Reagents and Platforms for Liquid Biopsy-Based Therapy Selection
| Category | Product/Platform | Manufacturer | Primary Research Application |
|---|---|---|---|
| ctDNA Isolation | QIAamp Circulating Nucleic Acid Kit | Qiagen | High-quality ctDNA extraction from plasma/serum |
| ctDNA Sequencing | AVENIO ctDNA Analysis Kits | Roche | Targeted NGS for liquid biopsy applications |
| CTC Enumeration | CELLSEARCH CTC System | Menarini Silicon Biosystems | Automated CTC capture and enumeration from whole blood |
| CTC Characterization | Parsortix System | Angle | Size-based isolation of CTCs for downstream molecular analysis |
| Extracellular Vesicle Isolation | exoRNeasy Serum/Plasma Kit | Qiagen | Simultaneous isolation of exosomes and other EVs |
| miRNA Profiling | TaqMan Advanced miRNA Assays | Thermo Fisher | Sensitive detection and quantification of miRNA biomarkers |
| Multiplex Proteomics | Olink Target 96/384 Panels | Olink | High-throughput protein biomarker quantification |
| Automated Library Prep | NeoGenomics ACCESS LP | NeoGenomics | Automated NGS library preparation for liquid biopsy samples |
| NGS Panels | Guardant360, FoundationOne Liquid CDx | Guardant Health, Foundation Medicine | Comprehensive genomic profiling from liquid biopsy |
| Bioinformatic Analysis | CLC Genomics Server | Qiagen | Integrated analysis of NGS data from liquid biopsies |
Visualizing Experimental Workflows and Signaling Pathways
Liquid Biopsy Analysis Workflow for Therapy Selection
Multi-Omics Integration for ICI Response Prediction
Liquid biopsy techniques have fundamentally transformed the approach to therapy selection in oncology, particularly for identifying actionable mutations and predicting response to ICI immunotherapy. The protocols and applications detailed in this document provide researchers and drug development professionals with comprehensive methodologies for implementing these cutting-edge approaches. As the field advances, key areas for future development include standardization of pre-analytical variables, validation of multi-modal predictive models across diverse populations, and integration of liquid biopsy with digital pathology and radiomics for comprehensive tumor profiling [46] [47]. The ongoing refinement of these approaches promises to further personalize cancer therapy, optimize treatment outcomes, and accelerate the development of novel therapeutic agents.
Monitoring Treatment Efficacy, Detecting MRD, and Tracking Emergent Resistance Mechanisms
Liquid biopsy has emerged as a transformative approach in clinical oncology, providing a minimally invasive method for diagnosing and monitoring cancer through the analysis of tumor-derived components in body fluids [9]. This technique stands in contrast to traditional tissue biopsies, which are invasive, difficult to serially obtain, and may not fully capture tumor heterogeneity [49]. By enabling real-time tracking of disease dynamics, liquid biopsy offers unprecedented opportunities for assessing treatment efficacy, detecting Minimal Residual Disease (MRD), and identifying the emergence of therapy resistance [50] [51].
The clinical significance of MRD detection is particularly profound in hematological malignancies and solid tumors. MRD refers to the small number of cancer cells that persist after treatment in patients who have achieved clinical remission [52]. These residual cells represent a latent reservoir of disease that can lead to relapse if not properly addressed. Accurate early detection of MRD allows clinicians to intervene before clinical recurrence becomes evident, potentially improving long-term survival outcomes [52]. Furthermore, liquid biopsy provides a powerful tool for uncovering the molecular mechanisms underlying treatment resistance, which often develops through dynamic interactions between tumors and their microenvironment [51].
Key Analytical Targets in Liquid Biopsy
Liquid biopsy encompasses several biologically significant components that serve as valuable biomarkers for cancer monitoring.
Circulating Tumor DNA (ctDNA)
Circulating tumor DNA (ctDNA) consists of fragmented DNA released into the circulation primarily through tumor cell apoptosis and necrosis [9]. It represents a small fraction (approximately 0.1-1.0%) of the total cell-free DNA (cfDNA) in blood [9]. ctDNA carries tumor-specific alterations including mutations, copy number variations, and epigenetic changes that reflect the tumor's genetic landscape. The short half-life of ctDNA (approximately 2 hours) makes it an excellent real-time biomarker for monitoring tumor dynamics and treatment response [9]. In non-small cell lung cancer (NSCLC), for example, ctDNA analysis enables rapid detection of resistance mechanisms in patients progressing on targeted therapies [50].
Circulating Tumor Cells (CTCs)
Circulating Tumor Cells (CTCs) are intact cells shed from primary or metastatic tumors that circulate in the peripheral blood [9]. While extremely rare (approximately 1 CTC per million leukocytes), CTCs play a crucial role in the metastatic cascade [9]. The presence and enumeration of CTCs have proven prognostic significance in multiple cancer types. Studies have demonstrated that higher CTC counts correlate with reduced progression-free survival and overall survival [9]. Technological advances in CTC isolation and analysis now enable not just enumeration but also molecular characterization and functional studies of these cells.
Additional Biomarkers
Beyond ctDNA and CTCs, several other components show promise in liquid biopsy applications. Extracellular vesicles (EVs), including exosomes, carry proteins, nucleic acids, and lipids from their parent cells and participate in intercellular communication [51]. Tumor-educated platelets (TEPs) incorporate tumor-derived biomolecules and reflect the RNA profiles of tumors they encounter [9]. Circulating free RNA (cfRNA), including microRNAs, offers insights into gene expression patterns and epigenetic regulation in tumors [49].
Liquid Biopsy Methodologies and Workflows
The implementation of liquid biopsy in research and clinical settings requires standardized methodologies for sample processing, analysis, and data interpretation.
Sample Collection and Processing
Proper sample collection and processing are critical for reliable liquid biopsy results. Blood samples collected in specialized tubes containing stabilizers prevent degradation of analytes. Plasma separation via centrifugation must typically occur within hours of collection. Processed samples can then be stored at -80°C until analysis. Different analytes require specific handling protocols; for example, ctDNA is stable in plasma, while CTCs require specialized preservatives to maintain cell viability and integrity [9].
Analytical Technologies for Liquid Biopsy
Multiple technological platforms are employed for detecting and analyzing liquid biopsy components, each with distinct strengths and applications.
Table 1: Comparison of Major MRD Detection Technologies
| Technology | Applicability | Sensitivity | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Next-Generation Sequencing (NGS) | >95% | 10⁻² - 10⁻⁶ | Comprehensive detection of multiple genetic alterations; broad applicability | Complex data analysis; high cost; not yet standardized [52] |
| Flow Cytometry | Almost 100% | 10⁻³ - 10⁻⁶ (increases with panel size) | Wide application range; relatively fast; can profile live cells | Lack of standardization; changes in immunophenotype; requires fresh cells [52] |
| qPCR/dPCR | ~40-50% | 10⁻⁴ - 10⁻⁶ | Highly standardized; lower cost; excellent sensitivity for known targets | Limited to predefined mutations; cannot detect novel alterations [52] |
Next-Generation Sequencing (NGS)
Next-generation sequencing (NGS) technologies enable comprehensive profiling of tumor-derived materials from liquid biopsies. NGS approaches for liquid biopsy include:
- Targeted panels: Focused sequencing of cancer-related genes for efficient mutation detection
- Whole exome/genome sequencing: Broad analysis of coding or entire genome
- Error-corrected sequencing: Methods using unique molecular identifiers to achieve high sensitivity
NGS provides unprecedented sensitivity (up to 10⁻⁶) for MRD detection and can monitor multiple genetic alterations simultaneously [52]. The technology is particularly valuable for tracking clonal evolution and emerging resistance mechanisms during treatment [50].
Polymerase Chain Reaction (PCR) Methods
Quantitative PCR (qPCR) and digital PCR (dPCR) offer highly sensitive detection of specific genetic alterations in ctDNA. These methods are ideal for monitoring known mutations during targeted therapy. For instance, EGFR mutation monitoring in NSCLC patients receiving tyrosine kinase inhibitors can be effectively performed using PCR-based approaches [50]. While these methods provide excellent sensitivity and are more accessible than NGS, they are limited to detecting predetermined mutations.
Flow Cytometry
Multiparameter flow cytometry is widely used for MRD detection in hematological malignancies by identifying aberrant immunophenotypes on tumor cells. Modern instruments with 6-8 color panels can achieve sensitivities of 10⁻⁴ to 10⁻⁶ [52]. The technology offers rapid turnaround times but requires expertise in panel design and data interpretation.
Workflow Visualization
The following diagram illustrates a generalized workflow for liquid biopsy analysis in cancer monitoring:
Application Note 1: MRD Detection in Hematologic Malignancies
Clinical Context and Significance
In hematological malignancies, including leukemia, lymphoma, and multiple myeloma, MRD detection plays an invaluable role in comprehensive clinical management, encompassing risk stratification, prognosis assessment, and recurrence monitoring [52]. Effective MRD detection facilitates improved treatment outcomes, long-term survival, and potential clinical cures. The presence of MRD after initial therapy represents the most important predictor of relapse in acute leukemias, with MRD-positive patients having significantly higher relapse rates and lower survival compared to MRD-negative counterparts [52].
Protocol: NGS-Based MRD Detection in Acute Leukemias
Principle: This protocol uses next-generation sequencing to identify and track clonal immunoglobulin (Ig) or T-cell receptor (TCR) gene rearrangements as unique markers of malignant cells.
Materials:
- Bone marrow aspirate or peripheral blood samples
- DNA extraction kit (e.g., QIAamp DNA Blood Mini Kit)
- PCR reagents and Ig/TCR primer sets
- NGS library preparation kit
- NGS platform (Illumina, Ion Torrent)
- Bioinformatics pipeline for clonotype identification and tracking
Procedure:
- Sample Collection: Collect 5-10 mL of bone marrow aspirate or peripheral blood in EDTA tubes. Process within 24 hours.
- DNA Extraction: Isolate genomic DNA using validated extraction methods. Quantify DNA concentration and assess quality.
- Library Preparation: Amplify Ig/TCR gene loci using multiplex PCR primers. Attach sequencing adapters and sample barcodes.
- Sequencing: Perform high-throughput sequencing with sufficient coverage (≥100,000 reads) to achieve desired sensitivity (10⁻⁵ to 10⁻⁶).
- Data Analysis:
- Identify dominant clonotype sequences in diagnostic samples
- Track these clonotypes in follow-up samples
- Calculate MRD levels based on clonotype frequency
- Interpretation: MRD positivity is typically defined as detection of malignant clonotype above the assay's validated sensitivity threshold.
Technical Notes: This approach requires a pre-treatment sample for clonotype identification. Sensitivity depends on sequencing depth and input DNA quantity.
Data Interpretation and Clinical Decision-Making
Table 2: MRD Detection in Hematologic Malignancies: Clinical Implications
| MRD Status | Relapse Risk | Clinical Implications | Therapeutic Considerations |
|---|---|---|---|
| Negative (<10⁻⁶) | Low (5-15% at 5 years) | Favorable prognosis | Consider treatment de-escalation, reduced duration of maintenance therapy |
| Positive (>10⁻⁴) | High (70-90% at 5 years) | Unfavorable prognosis | Intensify therapy, consider allogeneic stem cell transplantation, investigational approaches |
| Low Positive (10⁻⁵ to 10⁻⁶) | Intermediate (30-50% at 5 years) | Uncertain prognosis | Close monitoring, potential preemptive intervention |
Application Note 2: Tracking Resistance in Solid Tumors
Clinical Context and Significance
In solid tumors, liquid biopsy has proven particularly valuable for monitoring response to targeted therapies and detecting emerging resistance mechanisms. For example, in NSCLC patients receiving EGFR inhibitors, resistance invariably develops, often through secondary mutations like EGFR T790M or alternative pathway activation [50]. Liquid biopsy enables non-invasive serial monitoring to identify these resistance mechanisms, complementing or replacing repeat tissue biopsies and reducing patient burden from invasive procedures [50].
Protocol: ctDNA Analysis for Resistance Mutation Detection in NSCLC
Principle: This protocol uses targeted NGS to detect acquired resistance mutations in plasma ctDNA from NSCLC patients undergoing targeted therapy.
Materials:
- Blood collection tubes with ctDNA stabilizers (e.g., Streck, PAXgene)
- Plasma separation equipment
- ctDNA extraction kit
- Targeted NGS panel covering relevant resistance mutations
- NGS library preparation system
- Bioinformatics pipeline for variant calling
Procedure:
- Sample Collection: Draw 10 mL blood into ctDNA-stabilizing tubes. Invert gently 8-10 times. Store at room temperature if processing within 3 days.
- Plasma Preparation: Centrifuge within 72 hours at 1600-2000 × g for 20 minutes. Transfer supernatant to microcentrifuge tubes. Perform second centrifugation at 16,000 × g for 10 minutes.
- ctDNA Extraction: Use commercial ctDNA extraction kits following manufacturer's protocols. Elute in 20-50 μL buffer.
- Library Preparation: Use targeted NGS panels covering relevant genes (e.g., EGFR, ALK, ROS1, MET, KRAS). Include unique molecular identifiers to reduce errors.
- Sequencing: Sequence to high coverage (≥5000×) to detect low-frequency variants.
- Data Analysis:
- Align sequences to reference genome
- Call variants with allele frequency ≥0.5%
- Annotate resistance mutations with clinical significance
- Reporting: Document all resistance mutations with allele frequencies and evidence for clinical actionability.
Technical Notes: Establish a minimum variant allele frequency threshold based on validation studies. Consider confirmatory testing for critical treatment decisions.
Data Interpretation and Clinical Decision-Making
The emergence of resistance mutations in ctDNA typically precedes clinical or radiographic progression by several weeks to months, providing a window of opportunity for therapeutic intervention. Upon detection of resistance mechanisms, clinicians can consider switching to next-line targeted therapies, such as osimertinib for EGFR T790M-mediated resistance, or exploring combination strategies to overcome resistance [50].
Successful implementation of liquid biopsy workflows requires specific research reagents and resources optimized for various analytes and applications.
Table 3: Essential Research Reagent Solutions for Liquid Biopsy
| Reagent Category | Specific Examples | Primary Applications | Critical Function |
|---|---|---|---|
| Blood Collection Tubes with Stabilizers | Streck Cell-Free DNA BCT, PAXgene Blood cDNA Tube | ctDNA preservation, CTC stabilization | Prevent degradation of analytes, maintain cellular integrity during transport and storage |
| Nucleic Acid Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMax Cell-Free DNA Isolation Kit | ctDNA/ctDNA extraction, RNA isolation | Efficient recovery of low-concentration circulating nucleic acids, removal of inhibitors |
| Library Preparation Kits | AVENIO ctDNA kits, NEBNext Ultra II DNA Library Prep | NGS library construction, targeted sequencing | Preparation of sequencing libraries from low-input material, unique molecular identifiers |
| Targeted Sequencing Panels | AVENIO Oncology Panel, Oncomine Lung cfDNA Assay | Resistance mutation detection, MRD monitoring | Capture cancer-relevant genomic regions, optimized for low-input ctDNA applications |
| CTC Enrichment Systems | CellSearch System, Parsortix Technology | CTC enumeration, isolation for downstream analysis | Immunomagnetic or size-based enrichment of rare CTCs from whole blood |
Emerging Applications and Future Directions
The field of liquid biopsy continues to evolve rapidly, with several emerging applications showing significant promise. In small-cell lung cancer (SCLC), liquid biopsy is being explored for molecular subtyping based on transcriptional factor expression (ASCL1, NEUROD1, POU2F3, YAP1) and for assessing biomarkers predictive of immunotherapy response [49]. The analysis of extracellular vesicles (EVs) provides insights into tumor characteristics and the immune landscape, potentially guiding personalized strategies to enhance immune checkpoint inhibitor efficacy [51].
Future developments are likely to focus on integrating artificial intelligence to interpret complex liquid biopsy data, with potential applications in rare malignancies like blastic plasmacytoid dendritic cell neoplasm (BPDCN) [53]. The creation of organ-specific MRD assays and standardized protocols for global use represents another exciting frontier [53]. As these technologies mature, liquid biopsy is poised to become increasingly central in cancer management, enabling truly personalized, dynamic treatment approaches based on real-time assessment of tumor biology.
Navigating Technical Challenges and Optimizing Liquid Biopsy Assay Performance
Liquid biopsy, which involves the analysis of circulating tumor DNA (ctDNA) from blood and other bodily fluids, is revolutionizing cancer management by providing a minimally invasive method for diagnosis, monitoring treatment response, and detecting residual disease [9] [16]. The analytical phase of ctDNA testing has seen significant technological advances; however, the pre-analytical phase—encompassing sample collection, processing, and storage—remains a critical source of variability that can compromise the reliability and reproducibility of results [54]. ctDNA is a subset of cell-free DNA (cfDNA) and typically constitutes a small fraction (0.1% - 1.0%) of the total cfDNA in circulation, making it particularly vulnerable to pre-analytical artifacts [9]. Standardizing these initial procedures is therefore paramount to ensuring that liquid biopsy fulfills its potential in precision oncology [54] [16]. This Application Note details the critical pre-analytical variables and provides standardized protocols to safeguard ctDNA stability and integrity.
Critical Pre-Analytical Variables and Impact on ctDNA Analysis
The journey of a liquid biopsy sample from collection to analysis is intricate, with each step presenting opportunities for variation that can impact downstream results [54]. Key pre-analytical challenges include the selection of appropriate blood collection tubes, adherence to strict processing timelines, and the maintenance of controlled storage conditions.
Biological and Physiological Variables
Even before sample collection, numerous patient-specific factors can influence cfDNA/ctDNA characteristics. Acknowledging these variables is essential for proper study design and data interpretation. The table below summarizes major biological and physiological variables.
Table 1: Key Biological and Physiological Variables Affecting cfDNA/ctDNA
| Variable Category | Specific Factor | Impact on cfDNA/ctDNA | Key References |
|---|---|---|---|
| Demographic | Age | Significantly higher cfDNA levels in elderly individuals (over 60) | [54] |
| Gender | Higher cfDNA yields in women compared to men | [54] | |
| Living Habits | Exercise | Increases cfDNA levels associated with exercise-induced tissue injury | [54] |
| Diet | Changes in dietary composition can alter the types and amount of mitochondrial cfDNA | [54] | |
| Psychophysical State | Obesity | Induces inflammation, leading to higher cfDNA concentration | [54] |
| Stress & Emotion | Acute psychological stress and certain emotional states can increase circulating cell-free mitochondrial DNA (cf-mtDNA) | [54] | |
| Physiological Process | Pregnancy | cfDNA levels increase as gestation progresses, peaking before labor | [54] |
| Pathological Conditions | Cancer | cfDNA/ctDNA level often correlates with tumor size, growth rate, and cellular turnover | [54] [9] |
| Inflammation & Infection | Increased levels of cfDNA are associated with inflammatory states and infections | [54] | |
| Medical Interventions | Surgery | Can cause a spike in cfDNA levels, including donor-derived cfDNA in transplant patients | [54] [55] |
| Therapy | cfDNA/ctDNA content changes in response to therapy, allowing for treatment monitoring | [54] [55] |
Sample Collection and Handling
The choice of sample collection materials and initial handling procedures is a primary determinant of sample quality.
Table 2: Sample Collection Tube Types and Their Properties
| Tube Type | Additive | Mechanism of Action | Impact on cfDNA Stability | Recommended Use |
|---|---|---|---|---|
| K2EDTA | Ethylenediaminetetraacetic acid | Chelates calcium to inhibit coagulase and prevent clotting. | Prevents clot formation but does not stabilize nucleated blood cells, leading to genomic DNA contamination if processing is delayed (>6 hours) | Gold standard for well-controlled, rapid processing workflows; requires strict adherence to processing timelines [54] |
| Cell-Stabilizing Tubes | Proprietary reagents (e.g., formaldehyde releasers) | Cross-links nucleated blood cells to prevent cell lysis and release of genomic DNA. | Preserves the original cfDNA profile for several days at room temperature, allowing for extended transportation | Essential for multi-center trials or when central laboratory processing necessitates long transport times [54] |
The following workflow outlines the critical decision points and steps from sample collection to plasma isolation:
Sample Processing and Storage
Following collection, plasma processing must be performed with precision to isolate the cell-free fraction effectively. The recommended processing protocol is detailed below.
Table 3: Standardized Plasma Processing Protocol for cfDNA Analysis
| Processing Step | Parameter | Optimal Condition | Rationale & Impact of Deviation |
|---|---|---|---|
| Initial Centrifugation | Speed / RCF | 800 - 1,600 x g | Lower speed may fail to pellet cells; higher speed may lyse cells. |
| Temperature | 10 - 20°C (Room Temp) | Cold temperatures can promote cell lysis [54]. | |
| Duration | 10 - 20 minutes | Standardizes platelet yield in plasma. | |
| Intermediate Handling | Supernatant Transfer | Carefully aspirate supernatant without disturbing the cell pellet/buffy coat. | Disturbing the pellet contaminates plasma with genomic DNA from white blood cells. |
| Second Centrifugation | Speed / RCF | 16,000 x g | High speed is required to pellet remaining platelets and cellular debris. |
| Temperature | 10 - 20°C (Room Temp) | Maintains consistency. | |
| Duration | 10 - 20 minutes | Ensures complete pelleting of platelets. | |
| Final Plasma Handling | Aliquoting | Aliquot into low-DNA-binding tubes. | Prevents repeated freeze-thaw cycles and cfDNA loss due to adsorption. |
| Storage Temperature | ≤ -80°C | Long-term storage at -80°C preserves cfDNA integrity. Avoid -20°C for long-term storage. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful ctDNA analysis relies on a suite of specialized reagents and kits. The following table details key materials and their functions in the pre-analytical workflow.
Table 4: Essential Research Reagents and Materials for ctDNA Analysis
| Category | Item | Critical Function | Application Notes |
|---|---|---|---|
| Sample Collection | K₂EDTA Blood Collection Tubes | Prevents coagulation by chelating calcium. | Requires processing within 6 hours for optimal results [54]. |
| Cell-Stabilizing Blood Collection Tubes | Preserves nucleated blood cells, preventing genomic DNA release. | Enables room-temperature storage for up to 14 days, ideal for logistics-challenging studies [54]. | |
| Nucleic Acid Extraction | Silica-Membrane Column Kits | Selective binding and purification of cfDNA based on size and chemistry. | High specificity for short-fragment cfDNA; allows for automation. |
| Magnetic Bead-Based Kits | Paramagnetic bead technology to isolate cfDNA. | Amenable to high-throughput automation; efficient recovery of short fragments is kit-dependent. | |
| Quality Control | Fluorometric Assays (e.g., Qubit) | Fluorescent dye-based quantitation specific for DNA. | More accurate for low-concentration samples compared to UV absorbance. |
| Bioanalyzer / TapeStation | Microcapillary electrophoresis for sizing and integrity analysis. | Confirms the presence of the characteristic ~166 bp cfDNA peak and assesses fragment size distribution [54]. | |
| Downstream Analysis | Ultra-Sensitive NGS Library Prep Kits | Specialized enzymes and buffers for converting low-input cfDNA into sequencing libraries. | Designed to handle fragmented DNA and minimize biases; crucial for detecting low-frequency variants. |
The reliability of any liquid biopsy assay is fundamentally rooted in the quality of the pre-analytical phase. Variations in sample collection, processing timing, and storage conditions can introduce significant artifacts, leading to inaccurate results and hindering the comparability of data across studies [54]. The protocols and guidelines presented here provide a framework for standardizing these critical initial steps. By rigorously controlling for pre-analytical variables—from the selection of appropriate collection tubes to the meticulous processing and storage of plasma—researchers and clinicians can ensure the stability of ctDNA, maximize assay sensitivity, and fully leverage the transformative potential of liquid biopsy in cancer research and patient care [16] [55].
The accurate detection of circulating tumor DNA (ctDNA) is fundamentally challenged by low tumor shedding, particularly in early-stage disease and minimal residual disease (MRD) where ctDNA can represent less than 0.01% of total cell-free DNA (cfDNA) [1]. This low tumor fraction creates a significant technical barrier, as the signal from genuine tumor-derived fragments must be distinguished from an overwhelming background of wild-type DNA and sequencing artifacts [1] [2]. The biological basis for this challenge stems from several factors: the small size of early-stage tumors, variability in DNA release rates between cancer types, and the relatively short half-life of ctDNA (approximately 15 minutes to 2.5 hours) [56] [9]. Overcoming these limitations requires sophisticated technological approaches that enhance signal detection while minimizing background noise, enabling researchers to obtain meaningful data from increasingly dilute analyte samples.
Table 1: Key Challenges in Low ctDNA Fraction Detection
| Challenge | Impact on Detection | Typical Values in Early-Stage/MRD |
|---|---|---|
| Low Variant Allele Frequency (VAF) | Mutant alleles are rare relative to wild-type DNA | Often <0.01% VAF [1] |
| Limited Input Material | Reduced statistical power for variant calling | Sometimes single-digit mutant molecules [57] |
| Tumor Heterogeneity | Not all subclones may be represented | Variable based on cancer type and stage |
| Analytical Noise | Sequencing errors can mimic true mutations | Error rates can exceed true VAF [1] |
| Biological Background | Clonal hematopoiesis and other confounders | Increases false positive risk [2] |
Advanced Technological Approaches
Tumor-Informed versus Tumor-Agnostic Assays
The fundamental division in ctDNA detection strategies lies between tumor-informed and tumor-agnostic approaches, each with distinct advantages for low-shedding scenarios. Tumor-informed assays (e.g., Signatera, RaDaR, NeXT Personal) require prior sequencing of tumor tissue to identify patient-specific mutations that are then tracked in blood samples [57] [58]. This approach significantly enhances specificity by focusing on mutations known to be present in the patient's tumor, achieving sensitivities as high as 85-90% for MRD detection in early-stage breast cancer [57]. The NeXT Personal platform, for instance, can detect ctDNA down to 1 part per million, with the ChemoNEAR study demonstrating 100% sensitivity and specificity for MRD detection [57]. The primary limitations of tumor-informed approaches are longer turnaround times (typically 4-6 weeks) and the requirement for tumor tissue [58].
In contrast, tumor-agnostic assays (e.g., Guardant Reveal) utilize predefined mutation panels or epigenetic features without requiring prior tumor sequencing [57]. These assays identify cancer through cancer driver mutations, copy number aberrations, or cancer-derived methylation signals [57] [24]. While offering faster results (7-14 days) and not being limited by tissue availability, tumor-agnostic methods generally provide lower sensitivity in early-stage disease [58]. Recent advances in methylation-based patterns and fragmentomics are gradually closing this sensitivity gap, particularly for screening applications [24] [38].
Structural Variant and Phased Variant Approaches
Emerging technologies that focus on structural variants (SVs) and phased variants represent a promising direction for enhancing sensitivity. SV-based assays target tumor-specific chromosomal rearrangements (translocations, insertions, or deletions) with breakpoint sequences unique to the tumor, effectively eliminating concerns about background mutations from clonal hematopoiesis or sequencing artifacts [1]. In early-stage breast cancer, one SV-based ctDNA assay detected ctDNA in 96% (91/95) of participants at baseline with a median variant allele frequency of 0.15%, including 10% (9/91) with variant allele frequency of <0.01% [1].
Phased variant approaches, such as PhasED-seq (Phased Variant Enriched Detection Sequencing), provide additional sensitivity by targeting multiple single-nucleotide variants occurring on the same DNA fragment [1]. This method leverages the fact that while a single mutation on a fragment might be rare, the combination of multiple mutations on the same fragment is exponentially less likely to occur by chance or through technical artifacts, dramatically improving the signal-to-noise ratio in low-fraction scenarios.
Nanomaterial-Based Sensors and Fragmentomics
Nanomaterial-based electrochemical sensors represent a cutting-edge approach that bypasses some limitations of sequencing-based methods. These platforms utilize the high surface area and conductive properties of nanomaterials to transduce DNA-binding events into recordable electrical signals [1]. Magnetic nanoparticles coated with gold and conjugated with complementary DNA probes can capture and enrich target ctDNA fragments with attomolar limits of detection within 20 minutes [1]. Graphene or molybdenum disulfide (MoS₂) facilitates label-free sensing methods where ctDNA hybridization is detected through impedance changes or current-voltage characteristics [1]. Magnetic nano-electrode systems combine nucleic acid amplification via PCR with magnetic nanotechnology using superparamagnetic Fe₃O₄–Au core–shell particles, achieving detection sensitivities of three attomolar with a signal-to-noise ratio within 7 minutes of PCR [1].
Fragmentomics leverages the observation that tumor-derived cfDNA fragments have characteristic size distributions and end motifs that differ from normal cfDNA [2]. ctDNA fragments typically measure 90-150 base pairs, while DNA from non-tumor cells tends to be longer [1]. Library preparation methods that enrich for these shorter fragments can increase the fractional abundance of tumor-derived signals in sequencing libraries, improving the detection yield of low-frequency variants when combined with error-corrected next-generation sequencing [1]. This size-selection approach can reduce the required depth of sequencing, making MRD detection more efficient and cost-effective [1].
Table 2: Comparison of Advanced Detection Technologies for Low ctDNA Fractions
| Technology | Detection Principle | Limit of Detection | Advantages | Limitations |
|---|---|---|---|---|
| Tumor-Informed NGS (Signatera) | Patient-specific mutation tracking | ~0.001% VAF (single parts per million) [57] | High specificity, proven clinical utility | Long turnaround, requires tissue |
| Structural Variant Assays | Tumor-specific chromosomal rearrangements | <0.01% VAF [1] | Low background, avoids CHIP interference | Complex assay design |
| PhasED-Seq | Multiple mutations on same DNA fragment | Not specified (improves SNR) | Exponential signal enhancement | Computational complexity |
| Nanomaterial Sensors | Electrochemical detection of hybridization | Attomolar [1] | Rapid results, low cost | Early development, limited validation |
| Methylation Profiling | Cancer-specific methylation patterns | Varies by assay | Tumor-agnostic, tissue-of-origin data | Lower sensitivity in very low fraction |
| Fragmentomics | DNA size and end-motif patterns | Complements other methods | Orthogonal validation, cost-effective | Indirect detection method |
Experimental Protocols for Low Fraction ctDNA Analysis
Ultrasensitive ctDNA Workflow for MRD Detection
Purpose: To detect minimal residual disease in early-stage cancer patients with expected ctDNA fractions below 0.1%.
Sample Requirements: Collect 20-30 mL of blood into cell-free DNA blood collection tubes (e.g., Streck, Roche). Process within 6 hours of collection by double centrifugation (1,600 × g for 10 minutes, then 16,000 × g for 10 minutes) to isolate plasma. Store at -80°C if not extracting immediately [56] [2].
cfDNA Extraction: Use commercially available cfDNA extraction kits (QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit) following manufacturer protocols. Elute in 20-50 μL of elution buffer. Quantify using fluorometric methods (Qubit dsDNA HS Assay) and assess fragment size distribution (Bioanalyzer High Sensitivity DNA Kit or TapeStation) [2].
Library Preparation for Low Input: Employ library preparation methods specifically designed for short fragment enrichment. This includes bead-based or enzymatic size selection targeting fragments of 90-150 bp. Use unique molecular identifiers (UMIs) to tag individual DNA molecules before amplification to facilitate error correction [1] [2]. For tumor-informed approaches, hybrid-capture probes should be designed against 16-50 patient-specific variants identified through prior tumor sequencing [57].
Sequencing and Data Analysis: Sequence to high depth (typically 50,000-100,000x) using Illumina or similar platforms. Process data through a bioinformatics pipeline incorporating UMI-based error suppression, which involves grouping reads with the same UMI to generate consensus sequences that distinguish true mutations from PCR/sequencing errors [2]. For tumor-agnostic approaches, apply machine learning algorithms trained on fragmentation patterns or methylation profiles to distinguish cancer-derived signals [24] [38].
Protocol for ctDNA Fraction Enrichment via Size Selection
Rationale: Physical enrichment of ctDNA by size exclusion improves the signal-to-noise ratio by increasing the relative proportion of tumor-derived fragments in the sequencing library.
Procedure:
- Extract cfDNA as described in protocol 3.1.
- Prepare libraries using kits that preserve fragment size information (e.g., KAPA HyperPrep, ThruPLEX Tag-Seq).
- Perform double-sided size selection using magnetic beads (e.g., AMPure XP) with optimized bead-to-sample ratios:
- First selection: Use 0.45X ratio to remove fragments >250 bp
- Second selection: Use 0.95X ratio to retain fragments >100 bp
- Alternatively, use automated platforms (Pippin HT, BluePippin) with 2% agarose gel cassettes with size cutoffs of 100-250 bp.
- Proceed with target enrichment (for tumor-informed approaches) or direct sequencing (for whole-genome approaches).
- During bioinformatic analysis, apply additional in silico size filtering to include only fragments between 90-150 bp for variant calling [1].
Validation: Spike-in experiments using reference standards (Seraseq ctDNA Mutation Mix, Horizon HDx) demonstrate that this workflow can improve variant detection sensitivity by 3-5 fold in samples with ctDNA fractions below 0.5% [1].
Research Reagent Solutions
Table 3: Essential Research Reagents for Low ctDNA Studies
| Reagent/Category | Specific Examples | Function/Purpose | Considerations for Low Fraction |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, Roche Cell-Free DNA Collection Tubes | Preserve blood sample integrity | Prevent leukocyte lysis and background DNA release |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit | Isolate cfDNA from plasma | Maximize recovery of short fragments (90-150 bp) |
| Library Preparation | KAPA HyperPrep, ThruPLEX Tag-Seq, NEBNext Ultra II DNA | Prepare sequencing libraries | UMI incorporation, size selection capabilities |
| Target Enrichment | IDT xGen Lockdown Probes, Twist Custom Panels | Enrich for tumor-specific variants | High efficiency at low input amounts |
| Reference Standards | Seraseq ctDNA Mutation Mix, Horizon HDx | Assay validation and QC | Include variants at very low allelic fractions (0.01%-0.1%) |
| Size Selection | AMPure XP beads, Pippin HT systems | Enrich for ctDNA fragments | Optimized for 90-150 bp fragment recovery |
| Sequencing Platforms | Illumina NovaSeq, PacBio Revio, Oxford Nanopore | DNA sequencing | High depth, long reads for structural variants |
| Bioinformatic Tools | UMI error correction, fragment size analysis | Data analysis | Distinguish true variants from artifacts |
Clinical Validation and Applications
Analytical Validation Framework
Robust validation of ctDNA assays for low-shedding scenarios requires carefully designed experiments that establish key performance characteristics. Sensitivity and specificity should be determined using dilution series of reference standards with known variant allele frequencies, including points below 0.1% VAF [2]. The limit of detection (LOD) and limit of blank (LOB) must be established through replicate measurements (typically ≥20) at various input concentrations [2]. For tumor-informed assays, analytical validation should demonstrate consistent performance across different variant types (SNVs, indels, SVs) and genomic contexts [57].
Precision (repeatability and reproducibility) should be assessed by testing the same sample across multiple runs, operators, and instruments [2]. For MRD applications, where absolute ctDNA concentration may be more informative than mere detection, establishing a quantitative range through spike-in experiments is essential [57] [2]. Finally, the impact of pre-analytical variables (blood collection-to-processing time, shipping conditions, DNA extraction efficiency) should be systematically evaluated to define acceptable sample quality thresholds [2].
Clinical Utility in Treatment Monitoring and MRD
The most established application of low-fraction ctDNA analysis is in minimal residual disease detection and treatment response monitoring. Multiple studies have demonstrated that ctDNA dynamics during neoadjuvant therapy strongly correlate with pathological complete response and long-term outcomes [57]. In the I-SPY2 trial, persistent ctDNA positivity after neoadjuvant chemotherapy was significantly associated with lack of pathologic complete response (82% vs 52% non-pCR; odds ratio 4.33, P = 0.012), while early ctDNA clearance predicted improved outcomes in triple-negative breast cancer patients (P = 0.0002) [57].
For MRD detection post-surgery, ctDNA analysis provides a powerful prognostic tool. The ChemoNEAR study utilizing the NeXT Personal assay demonstrated that detection of ctDNA was associated with an increased risk of relapse (HR undefined, P <0.0001), decreased overall survival (P <0.0001), and provided a median lead time of 12.5 months before clinical recurrence [57]. Similar findings from the EBLIS study showed ctDNA detection preceded overt recurrence in 30 of 34 relapsed patients, with a lead time of up to 38 months (median 10.5 months) [57].
Overcoming the challenge of low tumor shedding requires a multifaceted approach combining advanced detection technologies, optimized experimental protocols, and rigorous validation frameworks. The field is rapidly evolving toward increasingly sensitive detection methods, with tumor-informed assays currently providing the highest sensitivity for MRD applications, while tumor-agnostic approaches based on methylation and fragmentomics show promise for screening applications [57] [24]. As these technologies mature, standardization of pre-analytical procedures, analytical validation approaches, and reporting standards will be essential for broader adoption in both research and clinical settings [2].
Future developments will likely focus on multi-modal approaches that combine mutation-based detection with epigenetic and fragmentomic features to further enhance sensitivity [24] [38]. The integration of machine learning algorithms to analyze complex multi-omic liquid biopsy data holds particular promise for improving discrimination between true low-frequency signals and background noise [38]. Additionally, the development of point-of-care electrochemical sensors could eventually enable rapid, cost-effective monitoring of treatment response [1]. As these technologies advance, they will increasingly enable researchers and clinicians to obtain meaningful molecular information from even the most challenging low-shedding scenarios, ultimately improving cancer detection, monitoring, and patient outcomes.
Distinguishing Tumor-Derived Variants from Clonal Hematopoiesis (CHIP) and Germline Mutations
Liquid biopsy, which involves genomic profiling of tumors using circulating biomarkers in bodily fluids, has emerged as a transformative technique in cancer management due to its minimal invasiveness and ability to capture tumor heterogeneity [9] [59]. However, the accurate interpretation of liquid biopsy results faces a significant challenge: distinguishing true tumor-derived variants from clonal hematopoiesis (CHIP) and germline mutations [59] [60]. Clonal hematopoiesis (CH) is an age-related process where hematopoietic stem cells acquire somatic mutations and expand clonally, while CHIP specifically refers to mutations in driver genes associated with hematological malignancies, detected at a variant allele frequency (VAF) of ≥2% in individuals without hematologic abnormalities [59]. These non-tumor derived mutations represent a source of biological background noise in cell-free DNA (cfDNA) analysis and, if misclassified, can lead to inappropriate therapeutic decisions [59] [60]. This Application Note provides detailed protocols and frameworks to address this critical diagnostic challenge, ensuring accurate variant interpretation in cancer research and drug development.
Technical Background and Definitions
Circulating tumor DNA (ctDNA) consists of fragmented DNA released from tumor cells into the bloodstream, typically representing only 0.1–1.0% of total cell-free DNA (cfDNA) in cancer patients [9]. The majority of cfDNA in plasma originates from hematopoietic cells: approximately 55% from white blood cells, 30% from erythroid progenitors, 10% from endothelial cells, and 1% from hepatocytes [59]. This hematopoietic origin explains why CH-derived mutations constitute a substantial confounding factor in liquid biopsy analysis.
Clonal Hematopoiesis of Indeterminate Potential (CHIP) is defined by the presence of somatic mutations in leukemia-associated genes in peripheral blood DNA, with a VAF ≥2%, in individuals without evidence of hematologic malignancy [59]. CHIP prevalence increases dramatically with age, affecting approximately 1% of individuals under 50, 10% of those over 65, and over 18% of those aged 90-108 [59]. The most commonly mutated genes in CHIP include epigenetic regulators DNMT3A, TET2, and ASXL1, followed by JAK2, PPM1D, TP53, and others also associated with hematological malignancies [59].
Incidental Germline Mutations are inherited variants present in all cells, including circulating white blood cells. When detected in cfDNA analysis without matched germline testing, these can be misinterpreted as tumor-derived somatic variants [60].
Quantitative Impact on Liquid Biopsy Analysis
Table 1: Performance Characteristics of Integrated Liquid Biopsy Approaches
| Analysis Method | Sensitivity for Tumor Variants | Specificity for Tumor Variants | CH Discrimination Capability | Germline Discrimination |
|---|---|---|---|---|
| Standard ctDNA NGS | Varies with ctDNA% (≥30% recommended for CNA detection) [61] | Moderate (confounded by CH) [59] | Limited without WBC sequencing [59] | Limited without WBC sequencing [60] |
| Caris Assure cNAS | 93.8% (for clinically actionable SNV/InDel) [60] | >99.9% (for SNV/InDel) [60] | Yes (via WBC sequencing) [60] | Yes (via WBC gDNA analysis) [60] |
| qcCHIP with permutation | Optimized per cohort characteristics [62] | Enhanced via cohort-specific filtering [62] | Yes (via bioinformatics filtering) [62] | Limited focus |
Table 2: Characteristic Features of Different Mutation Types in Liquid Biopsy
| Feature | Tumor-Derived Variants | CHIP Mutations | Germline Mutations |
|---|---|---|---|
| Typical VAF Range | Highly variable (0.1-50%+) depending on tumor burden [61] | Often 2-20% (following binomial distribution) [59] | ~50% or ~100% (heterozygous/homozygous) [60] |
| Commonly Affected Genes | Tumor-type specific (e.g., EGFR, KRAS, TP53 in solid tumors) [63] | DNMT3A, TET2, ASXL1, JAK2, PPM1D [59] | Cancer predisposition genes (e.g., BRCA1/2, TP53) [64] |
| Fragment Size Profile | Shorter fragments compared to non-tumor DNA [59] | Similar to wild-type hematopoietic DNA [59] | Similar to wild-type hematopoietic DNA [59] |
| Response to Therapy | Changes with tumor burden [61] | Generally stable over time [59] | Constant regardless of therapy [64] |
Experimental Protocols and Methodologies
Integrated Blood Collection and Processing for Comprehensive Mutation Discrimination
Principle: Simultaneous collection of plasma and white blood cells (WBCs) enables direct comparison of cfDNA variants with matched hematopoietic DNA, facilitating discrimination of CH and germline mutations [60].
Materials:
- Blood collection tubes (e.g., Streck Cell-Free DNA BCT or EDTA tubes)
- Centrifuge with temperature control
- DNA extraction kits for plasma and buffy coat
- Qubit fluorometer or equivalent for DNA quantification
- Agarose gel electrophoresis system
Procedure:
- Blood Collection and Processing:
- Collect whole blood into appropriate tubes (2×10 mL tubes recommended [60]).
- Process within 4-6 hours of collection for optimal cfDNA preservation.
- Centrifuge at 800-1600×g for 10 minutes at 4°C to separate plasma from cellular components.
- Transfer plasma to fresh tubes without disturbing the buffy coat layer.
- Centrifuge plasma a second time at 16,000×g for 10 minutes to remove residual cells.
- Isolate buffy coat for WBC genomic DNA extraction.
Nucleic Acid Extraction:
- Extract cfDNA from plasma using silica membrane or magnetic bead-based methods.
- Extract genomic DNA from WBCs using standard methods.
- Quantify DNA yield using fluorometric methods.
- Assess DNA quality via fragment analysis or agarose gel electrophoresis.
Library Preparation and Sequencing:
- Prepare sequencing libraries from both cfDNA and WBC gDNA.
- For comprehensive profiling, utilize whole exome sequencing (WES) or large gene panels (e.g., 23,000+ genes) [60].
- Achieve sufficient sequencing depth: ≥8,000x raw average coverage for clinically relevant genes in cfDNA, with matched WBC sequencing at ≥100x [60].
- Employ molecular barcoding to reduce sequencing artifacts and enable low-frequency variant detection.
Bioinformatics Analysis Pipeline for Variant Discrimination
Principle: Computational methods integrate multiple quality metrics and permutation-based optimization to distinguish tumor-derived variants from CH and germline mutations [62] [60].
Input Data Requirements:
- VCF files from cfDNA and matched WBC sequencing
- BAM files for visual validation
- Annotated variant files (e.g., using ANNOVAR)
Processing Steps:
- Variant Annotation and Filtering:
- Annotate variants with functional prediction scores
- Cross-reference with population databases (gnomAD, dbGaP)
- Check cancer-specific databases (COSMIC)
- Remove synonymous and common polymorphic variants
Technical Quality Control:
- Apply filters for strand bias (SOR < 3), read depth (DP > 20), and alternative allele depth (Alt_AD ≥ 3)
- For cfDNA variants, require supporting reads from both forward and reverse strands
CH-Specific Filtering:
- Remove variants present in matched WBC sequencing at similar VAF
- Filter out variants in CH-associated genes (DNMT3A, TET2, ASXL1, etc.) without strong tumor association
- Apply population-level frequency filters within the cohort
Germline Variant Identification:
- Identify variants present at ~50% or ~100% VAF in both cfDNA and WBC
- Compare with germline mutation databases
- Flag variants in cancer predisposition genes for confirmation testing
Permutation-Based Parameter Optimization (qcCHIP method):
- Randomly subset the cohort at different proportions (1/2, 1/3, ..., 1/10)
- Call CH variants in full cohort and subsets
- Calculate consistency metrics between full and subset calls
- Identify inflection points in consistency curves to determine optimal VAF and other parameter thresholds [62]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Mutation Discrimination Studies
| Category | Specific Product/Technology | Function in Experimental Workflow |
|---|---|---|
| Blood Collection & Preservation | Streck Cell-Free DNA BCT Tubes | Preserves cfDNA integrity and prevents WBC lysis during transport and storage |
| Nucleic Acid Extraction | QIAamp Circulating Nucleic Acid Kit (Qiagen) | Simultaneous extraction of cfDNA and viral nucleic acids from plasma |
| Nucleic Acid Extraction | MagMAX Cell-Free DNA Isolation Kit (Thermo Fisher) | High-efficiency cfDNA extraction using magnetic bead technology |
| DNA Quantification | Qubit dsDNA HS Assay Kit (Thermo Fisher) | Accurate quantification of low-concentration cfDNA samples |
| Library Preparation | AVENIO cfDNA Library Preparation Kit (Roche) | Optimized library construction from low-input cfDNA samples |
| Target Enrichment | xGen Pan-Cancer Panel (IDT) | Comprehensive coverage of cancer-related genes for targeted sequencing |
| Sequencing | Illumina NovaSeq X Series | Ultra-high-throughput sequencing for deep coverage applications |
| Bioinformatics | qcCHIP R Package [62] | Permutation-based parameter optimization for CH identification |
| Bioinformatics | ANNOVAR Software [62] | Functional annotation of genetic variants detected from sequencing |
| Reference Materials | Seraseq ctDNA Mutation Mix (LGC SeraCare) | Quantified reference materials for assay validation and quality control |
Data Interpretation and Quality Control
Critical Validation Metrics and Thresholds
Variant Allele Frequency Analysis:
- Tumor-derived variants typically show variable VAF (0.1-50%+) that may change with therapy [61]
- CH mutations generally demonstrate stable VAF (2-20%) over time, following binomial distribution patterns [59]
- Germline variants appear at approximately 50% (heterozygous) or 100% (homozygous) VAF in both cfDNA and WBC [60]
Fragment Size Analysis:
- Tumor-derived cfDNA fragments are shorter (~20-50 bp shorter) than those from hematopoietic cells [59]
- Implement size selection protocols to enrich for tumor-derived fragments when necessary
Cohort-Specific Optimization:
- For WES studies (100-200x depth), typical VAF cutoff is ≥0.02 [62]
- For ultra-deep sequencing (≥5000x depth), VAF cutoff can be reduced to 0.01 [62]
- Use permutation-based approaches to determine cohort-specific optimal parameters [62]
Troubleshooting Common Issues
Low ctDNA Fraction:
- When ctDNA% <2%, comprehensive biomarker assessment is limited [61]
- Consider repeating testing at later timepoints if disease progression occurs
- Utilize ctDNA prediction tools (e.g., ctDNA.org) to identify patients likely to have sufficient ctDNA% [61]
Persistent CH-Associated Variants:
- If CH variants remain after filtering, increase stringency of population-level frequency filters
- Implement manual review of variants in known CH genes
- Consider functional validation of uncertain variants
Discordant Tissue-Plasma Results:
- Investigate potential CH origin of plasma-specific variants
- Evaluate timing of sample collection relative to therapy
- Assess tumor heterogeneity and metastatic patterns
Accurate discrimination between tumor-derived variants, clonal hematopoiesis, and germline mutations is essential for proper interpretation of liquid biopsy results in cancer research and clinical applications. The integrated methodological approach presented here—combining matched WBC sequencing, sophisticated bioinformatics filtering, and cohort-specific parameter optimization—provides a robust framework for addressing this challenge. As liquid biopsy technologies continue to evolve and find expanded applications in cancer monitoring and drug development, these protocols will serve as critical tools for ensuring analytical accuracy and biological relevance in molecular profiling studies.
Liquid biopsy has emerged as a transformative tool in precision oncology, enabling non-invasive genomic profiling of tumors through the analysis of circulating tumor DNA (ctDNA). Despite its clinical potential, the analytical sensitivity of these assays, particularly for challenging genomic alterations such as copy number variations (CNVs), gene fusions, and low-frequency single-nucleotide variants/indels (SNV/Indels), remains a significant hurdle. This application note details the primary analytical challenges and presents validated experimental protocols and technological solutions designed to enhance detection sensitivity, thereby improving clinical utility for researchers and drug development professionals.
Performance Benchmarks for Sensitive Liquid Biopsy Assays
Current advanced assays have demonstrated markedly improved detection limits for key variant classes compared to earlier technologies. The following table summarizes performance benchmarks established in recent validation studies.
Table 1: Analytical Sensitivity Benchmarks for Key Variant Classes in Liquid Biopsy
| Variant Class | Reported 95% Limit of Detection (LOD) | Assay/Technology | Key Performance Findings |
|---|---|---|---|
| SNV/Indels | 0.15% VAF [65] [66] | Northstar Select (QCT technology) | 51% more pathogenic SNV/Indels identified compared to on-market assays; 91% of additional actionable variants found below 0.5% VAF [65]. |
| CNVs (Amplification) | 2.11 copies [65] [66] | Northstar Select (QCT technology) | 109% more CNVs detected versus on-market CGP assays [65]. |
| CNVs (Loss) | 1.80 copies [65] [66] | Northstar Select (QCT technology) | Sensitive detection of losses addressing a key challenge in liquid biopsy [65]. |
| Gene Fusions | 0.30% Tumor Fraction [65] [66] | Northstar Select (QCT technology) | Targeted sequencing approach for fusion detection in plasma [65]. |
| Microsatellite Instability (MSI-H) | 0.07% Tumor Fraction [65] [66] | Northstar Select (QCT technology) | High-sensitivity detection of MSI status from plasma [65]. |
| SNV/Indels (NSCLC context) | 0.2% VAF with >1400x mean depth [67] | 21-gene NGS panel (ddPCR validated) | >80% Positive Percentage Agreement (PPA) and >95% Negative Percentage Agreement (NPA) achieved in a 522-sample cohort [67]. |
Methodologies for Enhanced Detection Sensitivity
Protocol: Ultra-Sensitive Detection of SNVs/Indels at Low VAF
Principle: This protocol utilizes unique molecular identifiers (UMIs), ultra-deep sequencing, and matched white blood cell (WBC) sequencing to distinguish low-frequency somatic variants from sequencing artifacts and clonal hematopoiesis (CH)-derived variants [68] [69].
Procedure:
Sample Collection and Plasma Processing:
- Collect 20 mL of peripheral blood into Streck Cell-Free DNA BCT tubes or similar preservative tubes to prevent genomic DNA contamination from white blood cells [70] [71].
- Process with two-stage centrifugation: first at 1,000-1,600 RCF for 10 minutes at room temperature to isolate plasma, followed by a second centrifugation of the plasma at 12,000-20,000 RCF for 10 minutes to remove residual cellular debris [67] [71].
- Store the resulting cell-free plasma at -80°C if not extracting immediately [71].
cfDNA and WBC gDNA Co-Isolation:
- Extract cfDNA from 4-10 mL of plasma using a silica-membrane column kit (e.g., QIAamp Circulating Nucleic Acid Kit) which yields more ctDNA than magnetic bead-based methods [67] [71].
- In parallel, isolate genomic DNA (gDNA) from the buffy coat pellet to serve as a patient-matched normal sample [68] [69].
Library Preparation and Target Enrichment:
- Use a minimum of 20 ng of cfDNA for library preparation. For optimal low-VAF detection, inputs greater than 50 ng are recommended [67] [70].
- During library construction, incorporate UMIs to tag individual DNA molecules, enabling bioinformatic correction of PCR and sequencing errors [68] [69].
- Employ hybrid capture-based enrichment for target genes. Sequencing should be performed at a minimum mean depth of 20,000x on the cfDNA libraries. Sequence the matched WBC gDNA at a lower depth (~1,000x) [68].
Bioinformatic Analysis:
- Align sequences to the reference genome (e.g., GRCh37/hg19) using tools like BWA [67] [70].
- Perform UMI-aware variant calling with tools like Mutect2, and apply stringent filters (e.g., local depth >1000x) [67] [69].
- Critical Filtering Step: Subtract all variants detected in the matched WBC gDNA sample from the plasma cfDNA variant list. This removes germline polymorphisms and CH-derived variants, dramatically reducing false positives [68]. In one study, this method filtered out over 10,000 such variants [68].
Diagram 1: SNV/Indel detection workflow with matched normal.
Protocol: Sensitive CNV Detection in Liquid Biopsy
Principle: CNV detection in ctDNA is confounded by non-uniform fragmentation and background DNA. This protocol uses quantitative counting templates and robust bioinformatic normalization to distinguish focal amplifications and losses from chromosomal aneuploidies [65].
Procedure:
Wet-Lab Processing:
- Follow steps 1 and 2 from the SNV/Indel protocol for sample collection and DNA extraction.
- Utilize a targeted NGS panel designed with proprietary quantitative counting templates (QCT) or similar technology to minimize technical noise during library preparation and target capture [65].
- Sequence to a high depth (>20,000x) to generate sufficient data for copy number analysis.
Bioinformatic Analysis for CNVs:
- Calculate coverage depth across all targeted regions and normalize for GC content and mapability biases.
- Implement a specialized bioinformatic pipeline to differentiate focal CNV events from broad aneuploidies, as the former are more likely to be driver oncogenic events [65].
- Normalize coverage data against a reference set of non-cancer samples to account for technical variations.
- Call CNVs using a z-score-based approach or circular binary segmentation, setting a detection threshold of approximately 2.11 copies for gains and 1.80 copies for losses as demonstrated by validated assays [65] [66].
Protocol: Detection of Gene Fusions and MSI
Principle: Capturing tumor-derived RNA/DNA fragments spanning fusion breakpoints or exhibiting microsatellite instability in a high-noise background requires optimized wet-bench and computational methods.
Procedure for Fusions:
- Simultaneous DNA/RNA Extraction: Extract total nucleic acids from plasma. For RNA-based fusion detection, treat samples with proteinase K and DTT to lyse vesicles and inhibit RNases [69].
- Whole Transcriptome/Exome Sequencing: Convert RNA to cDNA and prepare libraries. Use hybrid capture panels baited for known fusion partners. For DNA-based fusion detection, ensure baits cover intronic regions where breakpoints occur [69].
- Bioinformatic Identification: Use tools like STAR for RNA alignment to identify chimeric transcripts. For DNA, analyze reads with soft-clips or mis-mates. Filter against WBC-derived sequencing data to remove false positives.
Procedure for MSI:
- Targeted Sequencing: Perform deep sequencing of a panel containing homopolymer repeat regions.
- Analysis of Instability: Compare the length distribution of microsatellite loci in the plasma cfDNA to a stable reference. A significant shift indicates MSI-H status, with advanced assays reporting detection down to 0.07% tumor fraction [65].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and their critical functions in sensitive liquid biopsy workflows.
Table 2: Essential Research Reagents for Sensitive Liquid Biopsy Analysis
| Reagent / Material | Function & Rationale | Example Products |
|---|---|---|
| Cell-Free DNA BCT Tubes | Preserves blood sample integrity by stabilizing nucleated blood cells, preventing lysis and release of wild-type gDNA during transport. Enables room-temperature storage for up to 7 days [67] [71]. | Streck cfDNA BCT, PAXgene Blood ccfDNA Tube (Qiagen), Roche cfDNA Tube [71]. |
| Silica-Membrane cfDNA Kits | Solid-phase extraction of cfDNA, providing higher yields than magnetic bead methods, which is critical for low-abundance targets [71]. | QIAamp Circulating Nucleic Acid Kit (Qiagen), Cobas ccfDNA Sample Preparation Kit [71]. |
| UMI Adapters | Tags individual DNA molecules with unique barcodes before PCR amplification, allowing bioinformatic consensus building to correct for sequencing errors and PCR duplicates [68] [69]. | KAPA HyperPrep with UDI, IDT for Illumina UDIs. |
| Hybrid-Capture Panels | Biotinylated probes used to enrich sequencing libraries for genes of interest, allowing for ultra-deep sequencing of targeted regions [65] [69]. | Panels covering 80+ genes (e.g., for CGP), Custom panels. |
| Matched Normal (WBC) DNA | Serves as a patient-specific reference to filter out germline variants and mutations from clonal hematopoiesis, drastically improving specificity [68]. | gDNA extracted from buffy coat. |
Overcoming the analytical hurdles in liquid biopsy requires an integrated approach spanning optimized pre-analytics, advanced molecular techniques, and sophisticated bioinformatics. The protocols and benchmarks detailed herein provide a framework for achieving the high sensitivity required for reliable detection of CNVs, fusions, and low-frequency variants. As these technologies continue to mature, they promise to deepen our understanding of tumor dynamics and enhance the development of personalized cancer therapies.
Assay Validation, Clinical Concordance, and Comparative Analysis in the Evolving Marketplace
Analytical validation is a critical process that determines whether a liquid biopsy assay performs as intended, assessing its performance limits and overall robustness by establishing key parameters such as the Limit of Detection (LOD), Limit of Quantification (LOQ), sensitivity, and specificity [72]. In the context of liquid biopsy for cancer monitoring, this validation ensures that circulating tumor DNA (ctDNA) assays can reliably detect and quantify the extremely low levels of tumor-derived material present in patient blood samples [9]. The importance of rigorous analytical validation has been recognized by international consortia including the Blood Profiling Atlas in Cancer (BloodPAC) and the International Society of Liquid Biopsy (ISLB), which work to establish standardized quality criteria for ctDNA analysis in oncology [73] [72].
Liquid biopsies offer a minimally invasive approach for cancer detection and monitoring, capturing tumor heterogeneity and enabling repeated sampling [24] [9]. However, the analytical challenges are significant—ctDNA often represents less than 0.1% of total cell-free DNA (cfDNA) in early-stage cancer, requiring exceptionally sensitive detection methods [65] [9]. Without comprehensive analytical validation, liquid biopsy tests may produce unreliable results that could lead to incorrect clinical decisions. This document provides detailed application notes and protocols for establishing analytical validation frameworks specifically designed for liquid biopsy assays in cancer research and drug development.
Key Validation Parameters and Definitions
Critical Performance Metrics
Limit of Detection (LOD) represents the lowest concentration of an analyte that can be reliably distinguished from zero with a defined level of confidence [74] [65]. In liquid biopsy applications, this typically refers to the lowest variant allele frequency (VAF) that can be detected with high confidence. The LOD is formally calculated as: LOD = mean blank value + [3.29 × (standard deviation)] for a 95% confidence level [74].
Limit of Quantification (LOQ) is defined as the lowest value that can not only be reliably detected but at which predefined goals for bias and imprecision are met [74]. For research applications, a common definition for LOQ is the lowest concentration at which assay imprecision is less than 20%, as indicated by the percent coefficient of variation (% CV = SD/mean × 100) [74].
Sensitivity refers to the ability of an assay to correctly identify true positive results, typically measured as the proportion of actual positives that are correctly detected. In liquid biopsy, this is crucial for identifying low-frequency variants present at minimal allele frequencies [65] [75].
Specificity describes the ability of an assay to correctly identify true negative results, measured as the proportion of actual negatives that are correctly identified. High specificity is essential to minimize false positives in cancer detection [65] [75].
Quantitative Performance Standards in Recent Liquid Biopsy Assays
Table 1: Analytical Performance of Recent Liquid Biopsy Assays
| Assay Name | LOD (SNV/Indels) | LOD (CNVs) | LOD (Fusions) | Specificity | Reference |
|---|---|---|---|---|---|
| Northstar Select | 0.15% VAF | 2.11 copies (amplification), 1.80 copies (loss) | 0.30% Tumor Fraction | >99.9999% (SNV/Indels) | [65] |
| PAN100 Panel | 0.3% VAF | Not specified | Not specified | >99.9% (Limit of Blank 0.00001%) | [75] |
| Not specified (DMMB assay example) | 11.9 µg/mL (calculated LOD) | Not applicable | Not applicable | Not specified | [74] |
Table 2: Performance Comparison Across ctDNA Assays in Clinical Validation
| Performance Measure | Northstar Select | On-market CGP Assays | Improvement |
|---|---|---|---|
| Pathogenic SNV/Indels Detected | 95% LOD at 0.15% VAF | LOD typically >0.2%-0.5% VAF | 51% more pathogenic SNV/indels |
| CNVs Detected | Sensitive down to 2.11 copies | Limited sensitivity in low tumor fraction | 109% more CNVs |
| Negative Reports | 11% | 20% | 45% fewer null reports |
| Actionable Variants Below 0.5% VAF | 91% of additional findings | Limited detection | Significantly enhanced |
Experimental Protocols for Validation
Protocol for Determining LOD and LOQ
Principle: This protocol establishes the lowest concentration of ctDNA that can be reliably detected (LOD) and quantified (LOQ) using serially diluted reference materials in a background of wild-type DNA [74] [65].
Materials:
- Seraseq ctDNA v2 Reference Materials or similar commercially available standards
- Wild-type DNA from healthy donors
- DNA quantification equipment (Qubit, TapeStation, or similar)
- Next-generation sequencing platform
- Bioinformatics analysis pipeline
Procedure:
- Prepare Contrived Samples: Create a dilution series of reference materials containing known mutations at variant allele frequencies ranging from 0.06% to 0.35% in a background of wild-type DNA [65].
- Extract and Process: Extract cfDNA from all samples using standardized methods and process through the entire assay workflow (library preparation, target capture, sequencing).
- Sequence and Analyze: Sequence all samples to appropriate depth (typically >10,000x coverage) and analyze using established bioinformatics pipelines.
- Calculate LOD: For each variant type (SNV, Indel, CNV, Fusion), determine the lowest VAF where 95% of expected variants are detected across replicate measurements (n≥20) [65].
- Establish LOQ: Calculate the coefficient of variation (% CV) at each dilution point and define LOQ as the lowest concentration where % CV remains below 20% [74].
- Statistical Analysis: Use probit regression analysis to determine the VAF at which 95% of variants are detected with 95% confidence.
Validation Criteria: The LOD must be demonstrated with at least 20 replicates at the claimed limit, with ≥95% detection rate. The LOQ must demonstrate ≤20% CV at the claimed limit [65].
Protocol for Establishing Sensitivity and Specificity
Principle: This protocol determines the true positive rate (sensitivity) and true negative rate (specificity) using well-characterized reference materials and clinical samples [65] [75].
Materials:
- Analytically valid reference standards with known mutations
- Clinical plasma samples with matched tumor tissue
- Samples from healthy donors for specificity determination
- Orthogonal validation method (ddPCR for SNVs/Indels)
Procedure:
- Sample Preparation: Assemble a sample set including reference materials, clinical samples with known mutation status, and healthy donor samples.
- Blinded Analysis: Process all samples through the liquid biopsy assay in a blinded manner.
- Orthogonal Confirmation: Validate a subset of results using orthogonal methods such as digital droplet PCR (ddPCR).
- Calculate Performance Metrics:
- Sensitivity = True Positives / (True Positives + False Negatives)
- Specificity = True Negatives / (True Negatives + False Positives)
- Positive Predictive Value (PPA) = True Positives / (True Positives + False Positives)
- Negative Predictive Value (NPA) = True Negatives / (True Negatives + False Negatives)
- Stratify by VAF: Calculate sensitivity separately for different VAF ranges (e.g., >0.5% VAF, 0.1-0.5% VAF) to understand performance characteristics across concentration ranges [65].
Validation Criteria: For clinical validation, positive percent agreement (PPA) with tissue biopsy should exceed 70% across variant types, with specificity >99% [75].
Protocol for Precision and Reproducibility Testing
Principle: This protocol establishes assay repeatability and reproducibility through intra-run, inter-run, and inter-operator testing [74].
Materials:
- Quality control materials at multiple concentrations (high, medium, low VAF)
- Multiple operators
- Multiple instrument lots/reagents when applicable
Procedure:
- Prepare QC Materials: Create quality control samples using reference materials or pooled patient samples at three different VAF levels (high, medium, near LOD).
- Intra-assay Precision: Process each QC sample in replicate (n≥5) within the same run.
- Inter-assay Precision: Process each QC sample across different runs (n≥5) on different days.
- Reproducibility: Include multiple operators and instrument/reagent lots when possible.
- Calculate Imprecision: Determine mean, standard deviation, and % CV for each level across all conditions.
- Establish QC Rules: Define acceptance criteria for ongoing quality control monitoring.
Validation Criteria: % CV should be <20% for samples above the LOQ, with no systematic differences between operators or reagent lots [74].
Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Liquid Biopsy Validation
| Reagent/Resource | Function | Example Products | Validation Role |
|---|---|---|---|
| Reference Standards | Provide known mutations at defined VAF for accuracy determination | Seraseq ctDNA v2, Horizon ctDNA | LOD/LOQ determination, sensitivity establishment |
| Healthy Donor Plasma | Provides wild-type background for specificity studies | Commercial pools, institutional collections | Specificity calculation, background estimation |
| cfDNA Extraction Kits | Isolve cell-free DNA from plasma samples | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit | Pre-analytical standardization |
| DNA Quantification Tools | Precisely measure DNA concentration and quality | Qubit dsDNA HS Assay, TapeStation, Fragment Analyzer | Input normalization, quality control |
| Library Preparation Kits | Prepare sequencing libraries from low-input cfDNA | KAPA HyperPrep, Illumina DNA Prep | Analytical phase standardization |
| Target Enrichment Panels | Capture cancer-associated genes | PAN100 panel, Northstar Select panel | Analytical sensitivity optimization |
| NGS Sequencing Platforms | Generate sequencing data for variant calling | Illumina NovaSeq, NextSeq, PacBio Sequel | Analytical performance establishment |
| Bioinformatics Pipelines | Analyze NGS data and call variants | Custom pipelines, commercially available software | Post-analytical validation |
Robust analytical validation is fundamental for generating reliable liquid biopsy data in cancer research and drug development. The frameworks presented here for establishing LOD, LOQ, sensitivity, and specificity provide a comprehensive approach to validating ctDNA assays. As the field advances, continued refinement of these protocols and adoption of standardized practices across laboratories will enhance reproducibility and accelerate the translation of liquid biopsy from research to clinical applications [73] [72].
The validation protocols outlined must be adapted to specific assay technologies and intended use cases. However, the fundamental principles of establishing detection limits, determining accuracy and precision, and implementing continuous quality control remain essential across platforms. By adhering to these rigorous validation standards, researchers can ensure that liquid biopsy assays generate reliable, reproducible data to support cancer monitoring and therapeutic development.
Liquid biopsy has emerged as a transformative tool in precision oncology, offering a minimally invasive alternative to traditional tissue biopsies for cancer genotyping and disease monitoring. These assays analyze circulating tumor DNA (ctDNA) and other biomarkers from blood, providing a real-time snapshot of tumor genomics. However, establishing the analytical validity and clinical utility of liquid biopsy requires rigorous concordance studies comparing it to tissue biopsy, the historical gold standard, and orthogonal methods like droplet digital PCR (ddPCR). This application note synthesizes recent evidence from such studies, providing detailed protocols and data to guide researchers and clinicians in validating and implementing these technologies.
Table 1: Key Biomarkers in Liquid Biopsy Concordance Studies
| Biomarker Class | Example Targets | Common Detection Technologies | Clinical Utility |
|---|---|---|---|
| Single Nucleotide Variants (SNVs) & Insertions/Deletions (Indels) | EGFR, KRAS, TP53, PIK3CA | NGS, ddPCR | Identifying actionable mutations for targeted therapy [27] [9] |
| Gene Fusions | ALK, ROS1, RET | NGS (Hybrid Capture) | Guiding treatment with specific kinase inhibitors [76] |
| Copy Number Variations (CNVs) | HER2 Amplification | ddPCR, NGS | Determining eligibility for anti-HER2 therapies [66] [77] |
| Microsatellite Instability (MSI) | MSI-High Status | NGS | Identifying patients for immunotherapy [66] [76] |
Concordance Between Liquid Biopsy and Tissue Biopsy
The agreement between liquid biopsy (using ctDNA) and tissue genotyping is a critical measure of clinical validity. Concordance is influenced by tumor type, burden, shedding, and heterogeneity.
Key Evidence and Quantitative Concordance
A landmark study in advanced breast cancer directly compared HER2 amplification status between tissue (IHC/FISH) and plasma (ddPCR) in 224 patients. The overall concordance was 66.96%, with sensitivity and specificity of 43.75% and 84.38%, respectively [77]. The study crucially demonstrated that concordance is dynamic and stage-dependent.
Table 2: Stage-Wise Concordance: Tissue vs. Liquid Biopsy (ddPCR) for HER2 in Breast Cancer [77]
| Cancer Stage | Sensitivity (PPA) | Specificity (NPA) | Key Interpretation |
|---|---|---|---|
| Stage III | 37.93% | 92.68% | Lower tumor burden limits ctDNA shedding, reducing sensitivity. |
| Stage IV | 41.67% | 86.44% | Increased tumor burden improves detection sensitivity. |
| Recurrent/Metastatic | 51.61% | 67.86% | Highest sensitivity; lower specificity may reflect emerging heterogeneity or new lesions not present in original tissue. |
| Overall Cohort (n=224) | 43.75% | 84.38% | Highlights the complementary value of both methods. |
The ROME trial in advanced solid tumors provided further insight, finding an overall 49% concordance for actionable alterations between tissue and liquid biopsy. Despite this modest agreement, the combined use of both modalities significantly increased the detection of actionable alterations and led to improved patient survival, underscoring their complementary roles in comprehensive genomic profiling [27].
Experimental Protocol: Validating Liquid Biopsy Against Tissue
This protocol outlines a standard method for conducting a head-to-head comparison study.
- 1. Patient Cohort Selection:
- Cohort: Enroll patients with histologically confirmed cancer (e.g., locally advanced or metastatic disease) who are scheduled for a tissue biopsy.
- Informed Consent: Obtain written informed consent as per institutional review board (IRB) guidelines.
- 2. Sample Collection:
- Tissue Biopsy: Collect tissue samples as per standard clinical practice (e.g., core needle biopsy). Process for FFPE and perform standard IHC/FISH or NGS testing.
- Blood Collection: Draw blood (typically 10-20 mL) into dedicated cell-free DNA blood collection tubes (e.g., PAXgene Blood ccfDNA Tubes or Streck Cell-Free DNA BCT) [77].
- 3. Plasma and cfDNA Processing:
- Plasma Separation: Centrifuge blood tubes within a specified time frame (e.g., 2 hours) at 1900 ×g for 15 minutes at room temperature. Transfer the supernatant and perform a second centrifugation at 1900 ×g for 10 minutes to obtain platelet-poor plasma. Aliquot and store at -80°C [77].
- cfDNA Extraction: Use commercial kits (e.g., QIAamp Circulating Nucleic Acid Kit) to extract cfDNA from 1-5 mL of plasma. Quantify and assess quality using a fluorometer.
- 4. Genomic Analysis:
- Liquid Biopsy: Analyze cfDNA using the technology under validation (e.g., NGS or ddPCR). For HER2 via ddPCR, see the dedicated protocol in Section 4.1.
- Tissue Biopsy: Analyze FFPE tissue DNA using the established standard (IHC/FISH for HER2; NGS for mutations).
- 5. Data Analysis:
- Calculate Positive Percent Agreement (PPA), Negative Percent Agreement (NPA), and Overall Percent Agreement (OAC) between liquid and tissue results.
- Use orthogonal methods (e.g., ddPCR for NGS findings) to confirm discrepant results and investigate biological causes like tumor heterogeneity.
Comparisons with Orthogonal Methods
Orthogonal methods are used to verify the results from a primary test, ensuring accuracy and reliability, especially for low-frequency variants.
ddPCR as an Orthodal Standard for NGS
Digital PCR is prized for its absolute quantification and high sensitivity, making it an ideal orthogonal method for validating NGS-based liquid biopsy assays. The TOMBOLA trial in bladder cancer provided a direct comparison, analyzing 1,282 plasma samples with both ddPCR and whole-genome sequencing (WGS). The study found an 82.9% overall concordance between the two ctDNA detection methods. Notably, ddPCR demonstrated higher sensitivity in samples with a low tumor fraction, with 12.9% of samples being positive only by ddPCR [27]. Both methods, however, showed comparable predictive power for recurrence-free survival.
Table 3: Analytical Performance of Select Liquid Biopsy Assays vs. Orthogonal Methods
| Assay / Technology | Variant Type | Claimed/Measured LOD95 | Orthogonal Validation & Key Findings |
|---|---|---|---|
| Northstar Select (smNGS) [66] [78] | SNV/Indels | 0.15% VAF | ddPCR: 98% concordance. Detected 51% more pathogenic SNV/Indels than on-market CGP assays, with 91% of additional findings below 0.5% VAF. |
| CNVs (Amplification) | 2.11 copies | - | |
| Hedera Profiling HP2 (NGS) [76] | SNV/Indels | - | Orthogonal methods: 94% concordance for ESMO Level I variants in clinical samples. |
| Fusions | - | Reference standards: 100% sensitivity and specificity at 0.5% AF. | |
| MUTE-Seq (CRISPR-based) [27] | SNV/Indels | Highly sensitive for low-frequency mutants | Used for MRD; demonstrated significant improvement in sensitivity for simultaneous mutant detection in NSCLC and pancreatic cancer. |
Experimental Protocol: Orthogonal Confirmation of NGS Findings by ddPCR
This protocol is used to verify specific variants (e.g., SNVs, CNVs) identified by NGS.
- 1. Assay Design:
- For the specific variant (e.g., an EGFR p.T790M mutation or HER2 amplification), design and order a validated ddPCR assay. This includes a fluorescent probe (e.g., FAM-labeled) for the mutant/target gene and a reference probe (e.g., HEX/VIC-labeled) for a wild-type/reference gene.
- 2. Reaction Setup:
- Prepare a 20-40 μL ddPCR reaction mixture containing:
- ddPCR Supermix for Probes (e.g., from Bio-Rad).
- Target Assay (FAM) and Reference Assay (HEX) at optimized concentrations.
- Approximately 5-20 ng of cfDNA extract.
- Prepare a 20-40 μL ddPCR reaction mixture containing:
- 3. Droplet Generation and PCR:
- Load the reaction mixture into a droplet generator (e.g., QX200 Droplet Generator, Bio-Rad) to create thousands of nanoliter-sized water-in-oil droplets.
- Transfer the emulsified sample to a 96-well PCR plate.
- Perform PCR amplification on a thermal cycler using manufacturer-recommended cycling conditions.
- 4. Droplet Reading and Analysis:
- Place the PCR plate in a droplet reader (e.g., QX200 Droplet Reader, Bio-Rad) which measures the fluorescence (FAM and HEX) in each droplet.
- Analyze the data using associated software (e.g., QuantaSoft, Bio-Rad). The software applies Poisson statistics to the count of positive and negative droplets to provide an absolute concentration (copies/μL) of the target and reference molecules. For CNVs, a ratio (e.g., HER2/Reference) is calculated.
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Liquid Biopsy Concordance Studies
| Item | Function/Application | Example Products/Brands |
|---|---|---|
| cfDNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA contamination and preserve cfDNA profile after blood draw. | PAXgene Blood ccfDNA Tubes (Qiagen), Streck Cell-Free DNA BCT [77] |
| cfDNA Extraction Kits | Isolate high-purity, short-fragment cfDNA from plasma samples for downstream molecular analysis. | QIAamp Circulating Nucleic Acid Kit (Qiagen) [77] |
| NGS Library Prep Kits | Prepare sequencing libraries from low-input cfDNA for comprehensive genomic profiling. | Kits tailored for hybrid capture or amplicon-based cfDNA sequencing (e.g., Northstar Select, Hedera HP2) [66] [76] |
| ddPCR Supermix & Assays | Enable absolute quantification and high-sensitivity detection of specific mutations or CNVs for orthogonal confirmation. | ddPCR Supermix for Probes (Bio-Rad), TaqMan Assays [77] |
| Reference Standards | Act as process controls for assay validation, calibration, and inter-laboratory comparison. | Commercially available synthetic or cell-line derived ctDNA standards with known variant allele frequencies [76] |
Workflow Visualization
The following diagram illustrates the integrated experimental workflow for conducting a concordance study, from sample collection to final data analysis.
Liquid biopsy has emerged as a transformative tool in precision oncology, offering a non-invasive method for genomic profiling of cancer through the analysis of circulating tumor DNA (ctDNA). This Application Note provides a detailed performance evaluation of three leading commercial liquid biopsy assays—Guardant360 CDx, FoundationOne Liquid CDx, and Tempus xF—within the broader context of liquid biopsy techniques for cancer monitoring research. Designed for researchers, scientists, and drug development professionals, this document synthesizes analytical validation data, clinical applications, and technical protocols to facilitate informed assay selection and implementation in research and development workflows. The data presented herein underscore the role of these assays in identifying therapeutic biomarkers, monitoring treatment resistance, and characterizing tumor heterogeneity through various analytical approaches, including fragmentomics analysis [79].
Results and Comparative Analysis
The three assays offer different coverages and technical characteristics, allowing researchers to select based on specific project requirements.
Table 1: Assay Overview and Genomic Coverage
| Assay Name | Total Genes | Variant Types Detected | Key Additional Features |
|---|---|---|---|
| Guardant360 CDx | 55 (Core CDx) [79] | SNVs, Indels, CNVs, Fusions [80] | FDA-approved companion diagnostic for multiple therapies; epigenomic capabilities via Guardant Infinity [81] |
| FoundationOne Liquid CDx | 309 (311 including non-exonic) [79] | SNVs, Indels, CNVs, Fusions | UV signature classification for tumors of cutaneous origin; EBV virus detection [82] [83] |
| Tempus xF | 105 [84] [85] | SNVs, Indels, CNVs, Rearrangements [85] | MSI-H status; bTMB (xF+ only) [84] |
| Tempus xF+ | 523 [84] | SNVs, Indels, CNGs, Rearrangements | Identifies variants potentially linked to clonal hematopoiesis (CH) [84] |
Analytical Performance Comparison
Analytical sensitivity and specificity are critical parameters for evaluating assay performance in detecting low-frequency variants in ctDNA.
Table 2: Analytical Performance Metrics by Variant Type
| Assay & Variant Type | VAF Sensitivity | Sensitivity (%) | Specificity (%) | Limit of Detection (LOD) |
|---|---|---|---|---|
| Guardant360 CDx | ||||
| HER2 Mutations (vs. tissue CTA) | - | 86.0-91.0 [86] | 100 [86] | - |
| Tempus xF (Chicago Lab) | ||||
| SNVs | ≥ 0.25% | 98.5 [84] | >99.9 [84] | 0.25% [84] |
| Indels | ≥ 0.5% | 98.5 [84] | >99.9 [84] | 0.50% [84] |
| CNVs | ≥ 0.5% | >99.9 [84] | 96.2 [84] | 0.50% [84] |
| Rearrangements | ≥ 1% | 94.4 [84] | >99.9 [84] | 1% [84] |
| Tempus xF+ (Chicago Lab) | ||||
| SNVs (Enhanced) | ≥ 0.2% | 98.3 [84] | >99.9 [84] | 0.2% [84] |
| Indels (Enhanced) | ≥ 0.25% | 95.5 [84] | >99.9 [84] | 0.25% [84] |
Key Clinical and Research Applications
- Therapy Selection and Companion Diagnostics: Guardant360 CDx is FDA-approved as a companion diagnostic for multiple targeted therapies in breast cancer (e.g., imlunestrant and elacestrant for
ESR1mutations) and NSCLC (e.g., trastuzumab deruxtecan forHER2mutations) [80] [86]. FoundationOne Liquid CDx can identify UV mutational signatures to classify cancers of cutaneous origin, which can inform diagnosis and treatment strategies [82]. - Monitoring Resistance and Recurrence: Tempus xF is clinically applied to track emerging resistance mutations during frontline targeted therapies, such as
ESR1mutations in breast cancer andEGFRresistance mutations in lung cancer [84]. The Guardant Reveal test, which leverages epigenomic features, has demonstrated utility in detecting molecular residual disease (MRD) in stage III colon cancer, identifying patients with poorer disease-free and overall survival [81]. - Fragmentomics for Phenotyping: Research indicates that fragmentomics patterns from targeted panels can infer cancer phenotypes. Normalized fragment read depth across all exons has shown strong predictive power for cancer type classification (AUROC up to 0.964), even with the smaller gene sets of commercial panels like Guardant360 CDx (55 genes) [79].
Experimental Protocols
Core Workflow for Targeted ctDNA NGS
The following diagram illustrates the generalized workflow common to the featured ctDNA assays, from sample collection to data analysis.
Detailed Methodologies
Sample Collection, Processing, and cfDNA Isolation
- Blood Collection and Plasma Separation: Collect whole blood in cell-stabilizing tubes (e.g., Streck Cell-Free DNA BCT). Process within a predefined window (e.g., up to 72 hours post-collection for Guardant360 CDx) [86]. Separate plasma through a double-centrifugation protocol (e.g., 1600 × g for 10 minutes at 4°C, followed by 16,000 × g for 10 minutes at 4°C) to remove cells and debris [85].
- cfDNA Extraction: Isolate cfDNA from the resulting plasma using silica membrane-based or magnetic bead-based commercial kits (e.g., QIAamp Circulating Nucleic Acid Kit from Qiagen or similar) according to the manufacturer's instructions. Quantify the extracted cfDNA using a fluorometric method (e.g., Qubit dsDNA HS Assay) [85].
Library Preparation and Sequencing
- Library Construction: Construct sequencing libraries from a defined input of cfDNA (e.g., 10-30 ng, as validated per assay). Steps include end-repair, adapter ligation, and the incorporation of unique molecular identifiers (UMIs) to tag original DNA molecules for error correction [85].
- Target Enrichment: Perform target enrichment using a hybrid-capture approach with biotinylated probes designed against the panel's gene targets. The Tempus xF assay, for instance, uses a 105-gene panel covering 270 kb [85]. Post-capture amplification is followed by quantification and normalization of the final libraries.
- Sequencing: Pool the libraries and sequence on a high-throughput NGS platform (e.g., Illumina NovaSeq 6000) to achieve a high unique median read depth, which is critical for detecting low-VAF variants. The Tempus xF validation achieved a unique median read depth of ~4,580x [85].
Bioinformatic Analysis and Variant Reporting
- Primary Analysis and Variant Calling: Perform base calling, demultiplexing, and alignment of sequencing reads to the human reference genome (e.g., GRCh37). UMI consensus sequences are generated to correct for amplification and sequencing errors. Variants (SNVs, Indels, CNVs, fusions) are called using specialized algorithms.
- Dynamic Filtering and Annotation: Implement a dynamic filtering method to reduce false positives. This critical step differentiates somatic tumor mutations from germline variants and mutations arising from clonal hematopoiesis (CH), especially in genes like
TP53,GNAS, andKRAS[85]. Foundational to this is the use of a matched normal sample (e.g., from buffy coat) when available. - Tumor Fraction and Complex Biomarker Estimation: Calculate the ctDNA tumor fraction (TF), which is the proportion of ctDNA in total cfDNA. For targeted panels, algorithms like the Off-Target Tumor Estimation Routine (OTTER) can estimate TF from off-target reads [85]. Complex biomarkers like blood Tumor Mutational Burden (bTMB) and Microsatellite Instability (MSI) status are also determined using validated computational methods [84].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item | Function/Application | Examples/Details |
|---|---|---|
| Cell-Free DNA BCT Tubes | Stabilizes blood cells to prevent genomic DNA contamination and preserve cfDNA profile during transport. | Streck Cell-Free DNA BCT tubes. |
| Nucleic Acid Extraction Kits | Isolation of high-quality, pure cfDNA from plasma samples. | QIAamp Circulating Nucleic Acid Kit (Qiagen). |
| Hybrid-Capture Probe Panels | Target enrichment for specific genomic regions of interest prior to sequencing. | Assay-specific panels (e.g., 55-gene for Guardant360 CDx, 105-gene for Tempus xF). |
| NGS Library Prep Kits | Preparation of cfDNA libraries for sequencing, including UMI incorporation. | Kits with UMI technology for error correction. |
| Bioinformatic Pipelines | Variant calling, filtering germline/CH variants, estimating TF and complex biomarkers. | OTTER algorithm for TF estimation; dynamic filtering methods [85]. |
| Orthogonal Validation Tools | Technical validation of NGS-identified variants. | Digital Droplet PCR (ddPCR) for hotspot mutations [85]. |
Discussion
The performance evaluation of Guardant360 CDx, FoundationOne Liquid CDx, and Tempus xF/xF+ reveals a landscape where assay selection is dictated by specific research objectives. Guardant360 CDx excels in clinical translation and companion diagnostic applications, particularly with its recent FDA approvals in breast cancer [80]. FoundationOne Liquid CDx offers extensive genomic coverage and specialized capabilities in viral and mutational signature detection [82] [83]. The Tempus xF/xF+ assays provide flexibility, with xF+ covering a very large gene set. A key research insight is that fragmentomics analysis, particularly normalized read depth metrics, can be successfully applied to the data generated by these targeted panels for cancer phenotyping, with minimal performance decrease even for smaller panels like Guardant360 CDx (55 genes) [79]. This underscores the potential for extracting additional layers of epigenetic information from standard targeted sequencing data.
A critical methodological consideration for all assays is the robust bioinformatic filtering of clonal hematopoiesis (CH)-derived variants, which can be misinterpreted as tumor-derived. The use of dynamic filtering methods and, where possible, a matched normal sample is essential for accurate variant interpretation [85]. Furthermore, the application of these assays is expanding beyond simple variant calling to include complex biomarkers like bTMB, MSI, and epigenomic modifications, as demonstrated by Guardant's MRD detection and tumor type classification in cancers of unknown primary [81].
Emerging High-Sensitivity Assays and the Impact of Lowering VAF Detection Limits
The field of liquid biopsy has been revolutionized by technological advancements that enable the detection of circulating tumor DNA (ctDNA) at increasingly lower variant allele frequencies (VAF). VAF measures the fraction of DNA molecules in a sample that carry a specific genomic alteration and serves as a critical indicator of tumor DNA burden in the blood. The drive toward higher sensitivity assays represents a paradigm shift in precision oncology, allowing for earlier cancer detection, improved therapy selection, and enhanced disease monitoring. This application note examines emerging high-sensitivity ctDNA assays and details the experimental protocols that enable robust detection of variants below 0.5% VAF, a threshold where conventional liquid biopsy assays typically demonstrate significant performance limitations [65] [87].
Lowering the limit of detection (LOD) for VAF is particularly crucial given that over 25% of somatic mutations in non-small cell lung cancer (NSCLC) are detected below 0.2% VAF, while most commercial assays until recently maintained an LOD above this level [65]. Furthermore, evidence confirms that variants detected at low VAF respond similarly to targeted therapies as those with higher signals, making accurate low-VAF detection essential for personalized care delivery [65]. This technical advance is especially beneficial for patients with low-shedding tumors or those with cancers where tissue sampling is challenging, such as central nervous system malignancies [88].
Performance Comparison of High-Sensitivity ctDNA Assays
Analytical Sensitivity Metrics
The table below summarizes the key performance characteristics of recently developed high-sensitivity ctDNA assays, demonstrating their enhanced capabilities for detecting low-frequency variants across different alteration types.
Table 1: Performance Metrics of Emerging High-Sensitivity ctDNA Assays
| Assay Name | Technology Platform | Gene Coverage | SNV/Indel LOD (VAF) | CNV LOD | Fusion LOD | MSI LOD |
|---|---|---|---|---|---|---|
| Northstar Select [65] [88] | Single-molecule NGS (smNGS) with QCT technology | 84 genes | 0.15% | 2.11 copies (amplification); 1.8 copies (loss) | 0.30% tumor fraction | 0.07% tumor fraction |
| LiquidHALLMARK [89] | Amplicon-based NGS with UMI | 80 genes | 0.1% | Empirically determined | 0.5% VAF | Empirically determined |
| HP2 [90] | Hybrid capture-based NGS | 32 genes | 0.5% (with 96.92% sensitivity) | Not specified | 0.5% (with 100% sensitivity) | Determined |
| Foundation Medicine Assays [91] | Hybrid capture-based NGS | Varies by test | Detection below published LOD demonstrated | Not specified | Not specified | Not specified |
Clinical Impact of Enhanced Sensitivity
The improved sensitivity of these next-generation assays directly translates to enhanced clinical utility. In a prospective head-to-head comparison study involving 182 patients with diverse solid tumors, Northstar Select demonstrated 51% more pathogenic SNV/Indels and 109% more copy number variants compared to six commercially available liquid biopsy assays [65] [88]. Notably, 91% of the additional clinically actionable variants detected by Northstar Select were found below 0.5% VAF, where other assays typically fail to reliably detect alterations [88]. This enhanced detection capability resulted in 45% fewer null reports (reports with no pathogenic or actionable results), significantly increasing the clinical utility of liquid biopsy testing [65].
Table 2: Clinical Performance in Prospective Studies
| Performance Metric | Northstar Select | Comparator Assays | Improvement |
|---|---|---|---|
| Pathogenic SNV/Indels Detected | 51% more | Baseline | 51% |
| Copy Number Variants Detected | 109% more | Baseline | 109% |
| Null Reports | 11% | 20% | 45% reduction |
| Actionable Variants <0.5% VAF | 91% of additional findings | Typically missed | Significant clinical impact |
| CNS Cancer Detection Rate | 87% | 27-55% | ~60% improvement |
Experimental Protocols for Ultrasensitive ctDNA Detection
Sample Collection and Pre-analytical Processing
Proper sample collection and processing are critical for maintaining ctDNA integrity and enabling low-VAF detection.
Blood Collection Protocol:
- Draw blood into cell-free DNA BCT tubes (e.g., Streck), which provide superior cfDNA stability compared to conventional EDTA tubes [92].
- Process samples within 24-96 hours of collection when using BCT tubes, as cfDNA remains stable within this window [92].
- Centrifuge at 300 × g for 20 minutes for initial plasma separation, followed by a secondary centrifugation at 5,000 × g for 10 minutes to completely remove residual cells [92].
- Aliquot plasma into low-bind tubes and store at -20°C or -80°C until extraction.
cfDNA Extraction Methods:
- The Zymo Quick cfDNA Serum and Plasma Kit demonstrates superior performance for manual extraction, providing higher yields and better preservation of low-VAF variants [92].
- For automated extraction, the QIAsymphony PAXcircDNASTA2400 protocol offers comparable results to manual methods with improved throughput [92].
- Optimal cfDNA input for library preparation typically ranges from ≥20 ng to 50 ng, with higher inputs improving sensitivity, particularly for variants below 0.5% VAF [87] [93].
Library Preparation and Target Enrichment
High-sensitivity assays employ specialized molecular techniques to minimize errors and enhance variant detection.
Single-Molecule NGS with QCT Technology (Northstar Select):
- Utilizes Quantitative Counting Templates that enable absolute molecular counting and dramatic noise reduction [65] [88].
- Implements a custom sequencing protocol optimized for ctDNA analysis, followed by advanced bioinformatic pipelines that further improve sensitivity, particularly for CNV detection [65].
- This technology achieves a five-fold better LOD for CNVs compared to first-generation liquid biopsies, enabling reliable detection of copy number losses, which most existing assays miss [88].
Amplicon-Based NGS with UMI (LiquidHALLMARK):
- Employs unique molecular identifiers introduced during target capture to enable error correction [89].
- Implements position-specific background error suppression through statistical modeling of noise inherent to samples and their processing [89].
- Demonstrates 99.38% sensitivity for point mutations and 95.83% sensitivity for insertions/deletions at 0.1% VAF, with specificity ≥99.9999% per base [89].
Hybrid Capture-Based NGS (Foundation Medicine):
- Leverages ultra-deep sequencing with optimized bioinformatic filters to distinguish true low-VAF variants from sequencing artifacts [91].
- Validated for clinical utility of variants below the published LOD, with studies showing similar response rates to targeted therapy for low-VAF alterations compared to the full biomarker-positive population [91].
Bioinformatic Analysis for Low-VAF Variant Calling
Advanced bioinformatic pipelines are essential for distinguishing true low-frequency variants from technical artifacts.
Key Steps in Variant Calling:
- Duplicate removal using molecular barcodes to eliminate PCR amplification biases.
- Position-specific error modeling to account for context-specific sequencing errors.
- Clonal hematopoiesis filtering using matched white blood cell DNA to distinguish true somatic variants from hematopoietic mutations [65].
- Statistical validation using binomial or Poisson models to confirm variant authenticity.
The following workflow diagram illustrates the complete process from sample collection to variant calling:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of high-sensitivity ctDNA detection requires carefully selected reagents and materials throughout the workflow.
Table 3: Essential Research Reagents for High-Sensitivity ctDNA Analysis
| Category | Specific Product/Technology | Function and Application |
|---|---|---|
| Blood Collection Tubes | Cell-Free DNA BCT Tubes (Streck) | Preserves cfDNA integrity by stabilizing nucleated blood cells, preventing genomic DNA contamination [92]. |
| cfDNA Extraction Kits | Zymo Quick cfDNA Serum and Plasma Kit | Provides high recovery of low-abundance cfDNA without carrier RNA interference [92]. |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit | Established manual method for cfDNA isolation with good yield and reproducibility [92]. |
| Automated Extraction | QIAsymphony PAXcircDNASTA2400 | Enables high-throughput, standardized cfDNA extraction with reduced manual handling [92]. |
| Library Preparation | Q5 High-Fidelity DNA Polymerase | Proofreading polymerase with low error rate for accurate amplification of low-VAF variants [92]. |
| Reference Materials | SEQC2 Reference Samples (Agilent) | Multi-cell line derived standards with known variants at various VAFs for assay validation [94]. |
| Orthogonal Validation | Digital Droplet PCR (ddPCR) | Absolute quantification for confirmation of NGS-detected low-VAF variants [65]. |
Critical Factors for Successful Low-VAF Detection
Technical Optimization Strategies
Achieving reliable detection of variants below 0.5% VAF requires attention to multiple technical parameters:
Input DNA and Sequencing Depth:
- Sensitivity increases significantly with higher cfDNA inputs (>20 ng recommended) [87].
- Sequencing depth >10,000x is typically required for confident detection of variants in the 0.1-0.5% VAF range [87].
- The on-target rate should exceed 50% to ensure efficient utilization of sequencing capacity [87].
Assay Design Considerations:
- Panel size should balance comprehensive genomic coverage with maintained sensitivity - smaller panels often provide better performance for low-VAF detection [65] [87].
- Amplicon-based approaches demonstrate advantages in on-target efficiency and sensitivity for SNVs/Indels at very low VAFs (<0.5%) [89].
- Hybrid capture-based methods offer more uniform coverage and better performance for detecting structural variants and copy number alterations [65] [91].
The relationship between VAF, detection sensitivity, and clinical utility follows a predictable pattern that can be visualized as follows:
Validation and Quality Control
Rigorous validation is essential for implementing high-sensitivity ctDNA assays in research and clinical settings:
Analytical Validation:
- Establish limit of detection using dilution series of reference materials with known variant concentrations [65] [89].
- Assess precision through replicate testing (both intra-run and inter-run) to determine reproducibility [93].
- Evaluate specificity using negative controls and wild-type samples to establish false-positive rates [65] [89].
Orthogonal Confirmation:
- Digital droplet PCR provides highly sensitive orthogonal validation, with studies demonstrating 98% concordance with Northstar Select results [88].
- Matched tissue-genotyping helps establish clinical sensitivity and specificity, though temporal and spatial heterogeneity may limit concordance [89].
- Reference materials such as the SEQC2 multi-cell line pools with known variants at various VAFs enable standardized performance assessment across platforms [94].
The ongoing development of high-sensitivity ctDNA assays with progressively lower VAF detection limits represents a significant advancement in liquid biopsy technology. The emergence of platforms capable of reliably detecting variants below 0.5% VAF, such as Northstar Select, LiquidHALLMARK, and enhanced Foundation Medicine assays, is already demonstrating tangible clinical benefits through identification of additional actionable alterations and reduction in null reports. Successful implementation requires meticulous attention to pre-analytical factors, optimized library preparation methodologies, and sophisticated bioinformatic analysis pipelines. As these technologies continue to evolve, they promise to further expand the utility of liquid biopsy in early cancer detection, minimal residual disease monitoring, and comprehensive genomic profiling for precision oncology applications.
Conclusion
Liquid biopsy has firmly established itself as an indispensable tool in precision oncology, moving beyond a complementary role to tissue biopsy towards enabling non-invasive, dynamic monitoring of cancer. The synthesis of foundational knowledge, refined methodologies, and robust validation underscores its power in tracking tumor evolution, detecting minimal residual disease, and uncovering resistance mechanisms. For researchers and drug developers, the future trajectory is clear: advancing multi-analyte and multi-omics approaches, integrating artificial intelligence for data interpretation, standardizing assays for early detection, and validating these tools in large-scale clinical trials. Overcoming remaining challenges in sensitivity and specificity will be paramount to fully realizing the potential of liquid biopsies in guiding drug development, personalizing therapy, and ultimately improving patient outcomes.
References
- 1. Monitoring and Assessment of Circulating Tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550271/]
- 2. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 3. Circulating tumor cells: overcoming challenges of detecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123222/]
- 4. Redefining cancer care: harnessing circulating tumor cells ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03883-y]
- 5. Extracellular vesicles in laboratory medicine: a review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631457/]
- 6. Proceedings of cell-free noncoding RNA biomarker studies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495990/]
- 7. Circular RNA-based liquid biopsy: a promising approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635984/]
- 8. Cell Free RNA Diagnostics Market Research 2025-2035 [https://www.globenewswire.com/news-release/2025/03/04/3036368/28124/en/Cell-Free-RNA-Diagnostics-Market-Research-2025-2035-Trends-Shaping-the-Market-and-Growth-Projections-by-Product-Type-Sample-Application-Technology-and-Geography-with-Profiles-of-th.html]
- 9. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 10. Circulating tumor nucleic acids: biology, release mechanisms ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01710-w]
- 11. Shedding secrets [https://www.fredhutch.org/en/news/center-news/2007/07/shedding-secrets.html]
- 12. Dynamic Fluctuation of Circulating Tumor Cells during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3980600/]
- 13. Macrovascular tumor infiltration and circulating tumor cell ... [https://www.nature.com/articles/s41591-025-03966-3]
- 14. A mathematical model of ctDNA shedding predicts tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7732186/]
- 15. Lesion Shedding Model: unraveling site-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10025438/]
- 16. Liquid biopsy in cancer management: Integrating ... [https://www.sciencedirect.com/science/article/pii/S2352551724000921]
- 17. How can liquid biopsies help capture the full spectrum of ... [https://www.oncology-central.com/how-can-liquid-biopsies-help-capture-the-full-spectrum-of-breast-cancer-heterogeneity/]
- 18. Dissecting Tumor Heterogeneity by Liquid Biopsy—A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347833/]
- 19. Tumor heterogeneity and the potential role of liquid biopsy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7896752/]
- 20. Patient Outcomes May Improve With Tailored Treatment ... [https://www.aacr.org/about-the-aacr/newsroom/news-releases/patient-outcomes-may-improve-with-tailored-treatment-guided-by-tissue-plus-liquid-biopsies-vs-individually/]
- 21. Non-invasive early-stage cancer detection - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11663200/]
- 22. Liquid biopsy in TNBC: significance in diagnostics ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1607960/full]
- 23. Beyond blood: Advancing the frontiers of liquid biopsy in oncology and personalized medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11007055/]
- 24. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 25. Diving into the Pleural Fluid: Liquid Biopsy for Metastatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8200094/]
- 26. Liquid Biopsy of Non-Plasma Body Fluids in Non-Small ... [https://www.mdpi.com/2073-4409/9/11/2486]
- 27. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 28. Updates of liquid biopsy in oral cancer and multiomics analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/34716963/]
- 29. Salivary biomarkers for cancer diagnosis: a meta-analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC7877992/]
- 30. Salivary biomarkers in cancer detection and management [https://www.frontierspartnerships.org/journals/acta-biochimica-polonica/articles/10.3389/abp.2025.14410/full]
- 31. A Comparative Proteomics Analysis of Five Body Fluids: Plasma, Urine, Cerebrospinal Fluid, Amniotic Fluid, and Saliva - PubMed [https://pubmed.ncbi.nlm.nih.gov/29781159/]
- 32. Immunomagnetic separation of circulating tumor cells with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7440929/]
- 33. Microfluidic devices to enrich and isolate circulating tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4664604/]
- 34. Tumor cell-based liquid biopsy using high-throughput ... [https://www.nature.com/articles/s41467-024-55140-x]
- 35. Design of buffer property for the new enrichment method ... [https://www.sciencedirect.com/science/article/pii/S2001037024004045]
- 36. LbL-Antibody Embedded Gold Mesh: An Effective Method ... [https://pubmed.ncbi.nlm.nih.gov/41244886/]
- 37. Next-generation sequencing in liquid : biopsy screening and... cancer [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-019-0220-8]
- 38. Circulating Tumor DNA as a Prognostic and Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564818/]
- 39. Real-World Data on Liquid Use in Non-Small Cell Lung... Biopsy [https://pmc.ncbi.nlm.nih.gov/articles/PMC9161665/]
- 40. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 41. Research | Cancer to Liquid tumor-derived... Biopsy NGS detect [https://www.illumina.com/areas-of-interest/cancer/research/applications/liquid-biopsy-research.html]
- 42. Liquid biopsy current techniques [https://www.sciencedirect.com/science/article/pii/B9780443274961000075]
- 43. Liquid Biopsies: A Revolution in Early Cancer Detection ... [https://www.aicr.org/resources/blog/liquid-biopsies-a-revolution-in-early-cancer-detection-and-monitoring/]
- 44. Frontiers | Biomarkers and computational models for predicting efficacy to tumor ICI immunotherapy [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1368749/full]
- 45. The current landscape of spatial biomarkers for prediction of response to immune checkpoint inhibition | npj Precision Oncology [https://www.nature.com/articles/s41698-024-00671-1]
- 46. Advancing precision medicine: the transformative role of artificial intelligence in immunogenomics, radiomics, and pathomics for biomarker discovery and immunotherapy optimization | Cancer Biology & Medicine [https://www.cancerbiomed.org/content/early/2025/01/02/j.issn.2095-3941.2024.0376]
- 47. Predictive models for immune checkpoint inhibitor ... [https://www.sciencedirect.com/science/article/pii/S1040842825003683]
- 48. Artificial Intelligence Algorithm Predicts Response to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351278/]
- 49. Liquid biopsy in diagnosis and monitoring of treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075280/]
- 50. Liquid Biopsy in Lung Cancer: Tracking Resistance to ... [https://pubmed.ncbi.nlm.nih.gov/41228269/]
- 51. Leveraging liquid biopsy to uncover resistance ... [https://www.sciencedirect.com/science/article/pii/S1936523325001767]
- 52. Minimal Residual Disease Detection: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079024/]
- 53. Leukemia specialists: How advances in measurable ... [https://www.mdanderson.org/cancerwise/leukemia-specialists--how-advances-in-measurable-residual-disease-MRD-are-improving-treatment.h00-159779601.html]
- 54. The impact of preanalytical variables on the analysis of cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11111958/]
- 55. Leveraging Liquid Biopsy to Improve Cancer Care | Blog [https://www.aacr.org/blog/2025/05/21/breakthroughs-in-the-blood-leveraging-liquid-biopsy-to-improve-cancer-care/]
- 56. Advances in CTC and ctDNA detection techniques [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02024-7]
- 57. Liquid clues: tracking early-stage breast cancer with ctDNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420329/]
- 58. Circulating Tumor DNA–Guided Risk Stratification in... - The ASCO Post [https://ascopost.com/issues/june-10-2025/circulating-tumor-dna-guided-risk-stratification-in-colorectal-cancer-evolving-evidence-and-future-utility/]
- 59. Clonal Hematopoiesis in Liquid Biopsy: From Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7463455/]
- 60. Caris Assure Blood-Based Profiling [https://www.carislifesciences.com/physicians/physician-tests/caris-assure/]
- 61. Prediction of plasma ctDNA fraction and prognostic ... [https://www.nature.com/articles/s41467-024-45475-w]
- 62. qcCHIP: an R package to identify clonal hematopoiesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466928/]
- 63. Efficacy of liquid biopsy for genetic mutations determination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11895383/]
- 64. prevalence, clinical utility and implications [https://pubmed.ncbi.nlm.nih.gov/38532104/]
- 65. Validation of a liquid biopsy assay with increased sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447423/]
- 66. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 67. Implementing liquid biopsy NGS in stage III/IV NSCLC [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-15227-0]
- 68. Tumor-Normal Matched Sequencing improves the ... [https://strandls.com/articles/tumor-normal-matched-sequencing-improves-the-accuracy-and-actionability-of-liquid-biopsies/]
- 69. Validation of an AI-enabled exome/transcriptome liquid ... [https://www.nature.com/articles/s41598-025-08986-0]
- 70. Mutational profiling using liquid biopsy to guide targeted ... [https://www.nature.com/articles/s41598-025-88094-1]
- 71. Improvement of the sensitivity of circulating tumor DNA-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332530/]
- 72. FDA-Reviewed Validation Protocols for Liquid Biopsy [https://www.bloodpac.org/publications/press-release-bloodpac-publishes-fda-reviewed-validation-protocols-for-liquid-biopsy]
- 73. International society of liquid biopsy (ISLB) perspective on ... [https://www.sciencedirect.com/science/article/pii/S2950195425000177]
- 74. Analytical Validation and Quality Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10264544/]
- 75. Development and Performance Validation of a ... [https://pubmed.ncbi.nlm.nih.gov/40888113/]
- 76. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://pubmed.ncbi.nlm.nih.gov/41015181/]
- 77. Liquid Biopsy and Tissue Biopsy Comparison with Digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8824896/]
- 78. BillionToOne's Northstar Select® Demonstrates Superior ... [https://www.billiontoone.com/news-media/billiontoones-northstar-select-r-demonstrates-superior-sensitivity-in-prospective-head-to-head-validation-study-publication]
- 79. Analysis of cfDNA fragmentomics metrics and commercial ... [https://www.nature.com/articles/s41467-025-64153-z]
- 80. FDA Clears Guardant360 CDx as Companion Diagnostic ... [https://www.onclive.com/view/fda-clears-guardant360-cdx-as-companion-diagnostic-for-imlunestrant-in-esr1-mutated-breast-cancer]
- 81. Press Releases [https://investors.guardanthealth.com/press-releases/press-releases/2025/Guardant-Health-and-Collaborators-to-Present-Over-19-Studies-Demonstrating-Role-of-Liquid-Biopsy-in-Advancing-Precision-Oncology-at-2025-ASCO-Annual-Meeting/default.aspx]
- 82. High-Specificity Detection of UV Mutational Signatures in ... [https://pubmed.ncbi.nlm.nih.gov/40846268/]
- 83. FoundationOne CDx and FoundationOne Heme Detect ... [https://www.sciencedirect.com/science/article/pii/S1525157825001679]
- 84. xF/xF+ [https://www.tempus.com/oncology/genomic-profiling/xf/?srsltid=AfmBOoqGn8-LKfcwv3q_lAkMbcxnMlbKDYNTmAOta-zG5RFNkyy4YWsd]
- 85. Validation of a liquid biopsy assay with molecular and ... [https://www.nature.com/articles/s41698-021-00202-2]
- 86. Analytical and Clinical Validation of the Plasma-Based ... [https://www.sciencedirect.com/science/article/pii/S1525157824003076]
- 87. Analytical evaluation of circulating tumor DNA sequencing ... [https://www.nature.com/articles/s41598-024-54361-w]
- 88. BillionToOne's Northstar Select® Demonstrates Superior ... [https://www.northstaronc.com/news/billiontoones-northstar-select-r-demonstrates-superior-sensitivity-in-prospective-head-to-head-validation-study-publication]
- 89. Analytical and clinical validation of an amplicon-based next ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0267389]
- 90. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 91. Demonstrating the Clinical Utility of Foundation Medicine's ... [https://www.foundationmedicine.com/blog/q3-research-recap-blog?utm_source=linkedin&utm_medium=organic-social&utm_campaign=q3-research-recap&utm_content=corporate]
- 92. Sensitive Quantification of Cell-Free Tumor DNA for Early ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.811291/full]
- 93. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 94. FDA-led consortium studies advance quality control of ... [https://pcm.amegroups.org/article/view/6609/html]