Master Protocols in Oncology: Revolutionizing Clinical Trial Design for Efficient Drug Development
This article provides a comprehensive overview of master protocol designs, a transformative approach for simultaneously evaluating multiple investigational drugs and/or cancer types within a single trial framework.
Master Protocols in Oncology: Revolutionizing Clinical Trial Design for Efficient Drug Development
Abstract
This article provides a comprehensive overview of master protocol designs, a transformative approach for simultaneously evaluating multiple investigational drugs and/or cancer types within a single trial framework. Tailored for researchers and drug development professionals, it explores the foundational concepts of basket, umbrella, and platform trials, their methodological application with real-world examples, and strategies to overcome operational and regulatory challenges. The content also benchmarks the performance and efficiency gains of master protocols against traditional designs, synthesizing key insights to guide future oncology clinical research towards more patient-centric and resource-effective models.
Understanding Master Protocols: A Foundational Shift from Traditional Oncology Trial Design
Master protocols represent a transformative approach in clinical research, designed to increase efficiency in modern drug development. A master protocol is defined as a single overarching protocol that coordinates multiple sub-studies to evaluate one or more investigational drugs in one or more disease subtypes within a unified trial structure [1]. This framework is particularly vital in oncology, where the rise of precision medicine and limited patient populations for specific genomic profiles make traditional, single-drug-single-disease trials increasingly impractical and inefficient [2]. By enabling the simultaneous assessment of multiple hypotheses, master protocols optimize the use of precious clinical trial resources and accelerate the drug development timeline.
The adoption of master protocols has gained significant regulatory recognition. In March 2022, the U.S. Food and Drug Administration (FDA) published official guidance on their use in oncology studies, providing crucial recommendations on design, safety, and regulatory aspects to support marketing authorization applications [3]. Similarly, the European Medicines Agency (EMA) has addressed these designs in its "Questions & Answers on Complex Clinical Trials" document, signaling broad regulatory acceptance of this innovative trial methodology [3].
Classification of Master Protocol Designs
Master protocols are generally categorized into three primary designs based on their structure and objectives: basket trials, umbrella trials, and platform trials. Each design addresses distinct research questions and offers unique advantages in clinical investigation.
Basket Trials
A basket trial tests a single investigational drug or drug combination across multiple different disease populations. These populations may be defined by various cancer types, disease stages, histologies, number of prior therapies, genetic or other biomarkers, or demographic characteristics [2] [1]. The fundamental principle is to evaluate whether a targeted therapy effective in one specific cancer type might also be effective in other cancer types sharing the same molecular alteration.
Umbrella Trials
An umbrella trial evaluates multiple investigational drugs or drug combinations within a single disease population. In this design, all investigational drugs or combinations are typically enrolled simultaneously without a rolling arm option [2]. These trials often stratify patients based on specific biomarker profiles within a single cancer type, assigning them to different targeted therapies matched to their tumor's molecular characteristics.
Platform Trials
A platform trial is a more flexible master protocol that allows for the addition of new treatment arms during the trial based on accumulated knowledge. This adaptive design can test several investigational therapies in potentially heterogeneous populations where new therapies are introduced over time through Intervention Specific Appendices (ISAs) [1] [4]. Platform trials may incorporate features of both basket and umbrella designs and typically employ adaptive methodologies to efficiently identify promising treatments while allowing less effective ones to be dropped.
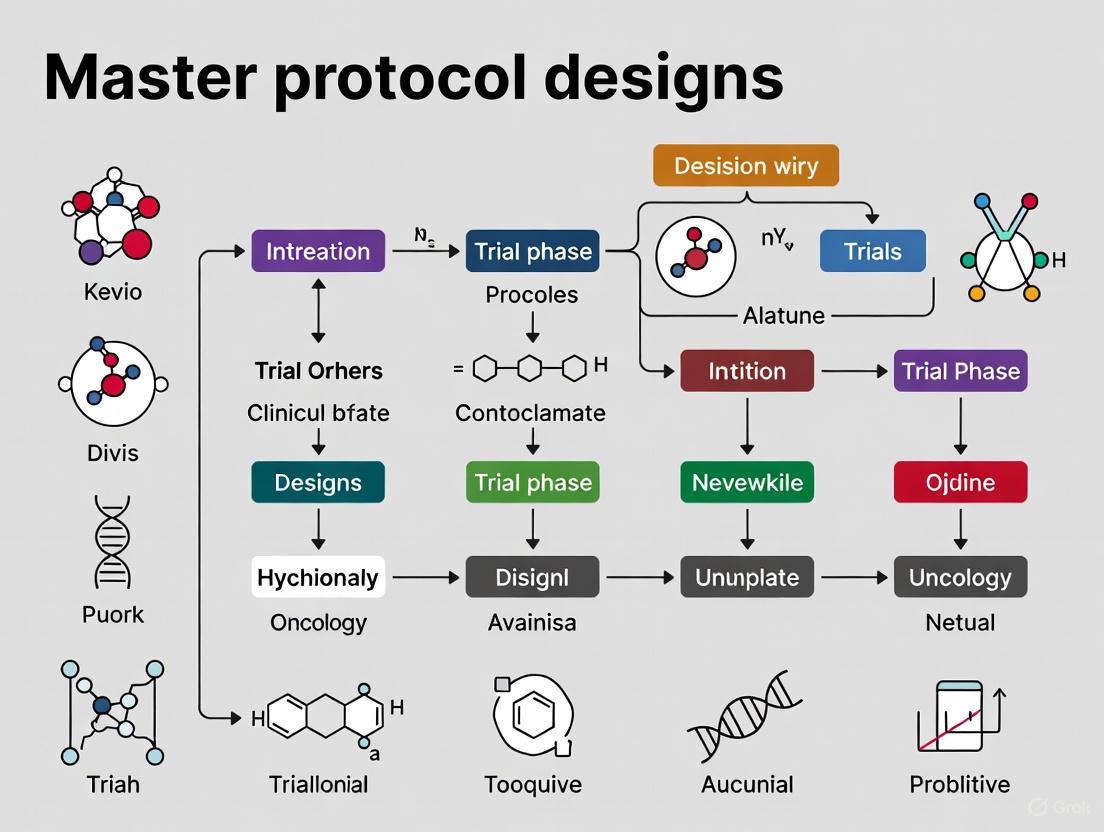
The following diagram illustrates the fundamental structure and patient flow of these three master protocol designs:
Diagram 1: Master Protocol Design Structures. Platform trials allow dynamic addition of arms over time (dashed line).
Current Usage and Statistical Characteristics
Adoption Across Organizations and Therapeutic Areas
Recent survey data from the American Statistical Association (ASA) Biopharmaceutical Section provides valuable insights into the current usage patterns of master protocols. According to the survey distributed to 37 organizations in 2021, 79% of respondents indicated that their organization had trials with master protocols in planning or implementation stages [2]. This high adoption rate reflects the growing acceptance of these efficient trial designs within the clinical research community.
The application of master protocols spans multiple therapeutic areas, with oncology representing the predominant field. The table below summarizes the key characteristics of master protocol usage based on the ASA survey data:
Table 1: Master Protocol Usage Characteristics Across Organizations
| Characteristic | Pharmaceutical Companies (n=25) | Academic/Non-Profit (n=6) | Total (n=31) |
|---|---|---|---|
| Disease Areas | |||
| ∟ Oncology | 21 (84%) | 5 (83%) | 26 (84%) |
| ∟ Infectious Disease | 8 (32%) | 1 (17%) | 9 (29%) |
| ∟ Neuroscience | 6 (24%) | 0 (0%) | 6 (19%) |
| ∟ Rare Disease | 3 (12%) | 1 (17%) | 4 (13%) |
| ∟ Immunology | 3 (12%) | 0 (0%) | 3 (10%) |
| Trial Types | |||
| ∟ Basket Trial | 19 (76%) | 5 (83%) | 24 (77%) |
| ∟ Umbrella Trial | 11 (44%) | 4 (67%) | 15 (48%) |
| ∟ Platform Trial | 18 (72%) | 5 (83%) | 23 (74%) |
| Development Phases | |||
| ∟ Phase I | 23 (92%) | 3 (50%) | 26 (84%) |
| ∟ Phase II | 15 (60%) | 3 (50%) | 18 (58%) |
| ∟ Phase I/II | 15 (60%) | 2 (33%) | 17 (55%) |
| ∟ Phase III | 5 (20%) | 1 (16%) | 6 (19%) |
| ∟ Phase II/III | 4 (16%) | 2 (33%) | 6 (19%) |
| Sponsorship | |||
| ∟ Solely Sponsored | 21 (84%) | 3 (50%) | 24 (77%) |
| ∟ Collaborative | 14 (56%) | 4 (67%) | 18 (58%) |
| Independent Monitoring | |||
| ∟ Use of IDMC | 6 (24%) | 4 (67%) | 10 (32%) |
Data Source: ASA BIOP Oncology Methods Scientific Working Group Master Protocol Sub-team Survey (2021) [2]
Statistical Features and Methodologies
Master protocols incorporate sophisticated statistical methodologies to maintain scientific integrity while evaluating multiple hypotheses. The ASA survey revealed that 72% of organizations reported using some form of randomization in their master protocols [2]. Additionally, various adaptive features are commonly employed, including sample size re-estimation (52%), adaptive randomization (44%), and arm dropping for futility (40%).
Multiplicity adjustment presents a significant statistical challenge in master protocols, with 60% of organizations reporting the use of methods to control for false positive findings across multiple comparisons [2]. Bayesian methods are increasingly utilized, particularly in platform trials, where they facilitate information borrowing across patient subgroups or treatment arms.
The following workflow illustrates the dynamic nature of platform trial operations and statistical monitoring:
Diagram 2: Platform Trial Operational Workflow with Dynamic ISA Integration
Implementation Framework and Experimental Protocols
Core Components and Regulatory Framework
Successful implementation of master protocols requires careful attention to several core components. The foundation is the master protocol document itself, which defines the general framework of the study including overall objectives, methodology, evaluation criteria, and analysis processes [3]. This document does not include indication- or product-specific details, which are instead detailed in independent sub-protocols or Intervention Specific Appendices (ISAs) for each targeted sub-study [4].
The regulatory landscape for master protocols has evolved significantly. The FDA's 2022 guidance on "Master Protocols: Efficient Clinical Trial Design Strategies to Expedite Development of Oncology Drugs and Biologics" provides crucial recommendations for sponsors utilizing these designs [3]. Similarly, the EMA's guidance on Complex Clinical Trials further legitimizes these approaches in the European regulatory context.
Essential Research Reagents and Methodologies
The implementation of master protocols in oncology requires specialized reagents and methodologies to support the complex biomarker-driven patient stratification and monitoring. The following table details key research reagent solutions essential for successful execution:
Table 2: Essential Research Reagent Solutions for Oncology Master Protocols
| Reagent/Material | Function | Application Context |
|---|---|---|
| Next-Generation Sequencing Panels | Comprehensive genomic profiling to identify biomarker-defined patient subgroups | Patient screening and stratification in basket and umbrella trials |
| Immunohistochemistry Assays | Protein-level biomarker detection and validation | Companion diagnostic development and patient selection |
| Liquid Biopsy Platforms | Non-invasive biomarker monitoring and resistance mechanism detection | Dynamic biomarker assessment in platform trials |
| Multiplex Immunoassays | Simultaneous measurement of multiple analytes in limited sample volumes | Pharmacodynamic biomarker evaluation and safety monitoring |
| Centralized Laboratory Services | Standardized biomarker testing across multiple clinical sites | Ensuring data consistency in multi-center master protocols |
| Data Transfer Specifications | Structured formats for biomarker data integration | Facilitating combination of complex biomarker data with clinical outcomes |
Statistical Analysis Plan Development
The Statistical Analysis Plan (SAP) for master protocols requires additional complexity for statistical inference, particularly when incorporating adaptive features, multiplicity adjustments, and Bayesian methods [1]. Development teams must maintain focus on the primary study objectives to prevent the SAP from becoming excessively extensive. The number of tables, figures, and listings can grow significantly in master protocols, making careful prioritization essential to manage reporting complexities [1].
For platform trials, the SAP must explicitly define rules for information borrowing between non-concurrent ISAs. Various quantitative strategies can be employed, including discounting patients enrolled before an ISA began, creating models for time trends, or implementing hierarchical borrowing techniques [4]. Each approach requires significant statistical expertise and extensive simulation studies during the design phase to understand operating characteristics.
Challenges and Best Practices
Implementation Challenges
Despite their efficiency benefits, master protocols present significant challenges across multiple domains. The ASA survey identified several key areas of difficulty, including operational execution, statistical design complexity, data management, and regulatory engagement [2].
Data management represents a particularly complex challenge, as master protocols generate large amounts of heterogeneous data requiring efficient integration and processing [1]. In basket trials, multiple indications may involve different endpoint definitions and response criteria across indications. Umbrella trials with multiple drugs lead to complex exposure and safety summaries, while platform trials continuously add new treatment arms, generating dynamic datasets that require real-time integration and analysis [1].
Safety monitoring in master protocols requires tailored strategies, as adverse events of special interest might need to be defined separately for each drug [1]. Additionally, biomarker data complexity presents challenges, as genomic data can be relatively large and complex, requiring intensive discussion with biomarker specialists to define rules for deriving biomarkers of interest and mapping raw data to standardized formats [1].
Strategic Recommendations for Success
Based on survey findings and industry experience, several best practices emerge for successful master protocol implementation:
Early Planning and Cross-Functional Alignment: Begin with comprehensive planning that engages all stakeholders, including statisticians, clinical operations, data management, and regulatory affairs [1]. Early discussion with safety and biomarker teams is particularly crucial.
CSR Strategy Definition: The strategy for Clinical Study Reports (separate CSR for each cohort versus single CSR) should be defined sufficiently early in the process to ensure consistent reporting standards [1].
Focused Objectives: Maintain clear focus on the key study objectives to prevent data overload and inefficiencies in reporting. Exploratory analyses can be planned in a second step after addressing primary endpoints [1].
Robust Simulation Studies: Conduct extensive simulation studies during the design phase to understand the operating characteristics of complex adaptive designs, particularly for platform trials [4].
Infrastructure Investment: Implement robust data management systems capable of handling evolving data structures and ensuring consistency across various cohorts in dynamic trial environments [1].
Multiple stakeholders, including regulatory agencies, academic institutions, and pharmaceutical companies, are called to work collaboratively to address these challenges and remove roadblocks for future usage of master protocol trials [2]. As these designs continue to evolve, their potential to transform oncology drug development remains substantial, offering more efficient pathways to bring promising therapies to patients in need.
Tumor heterogeneity presents a fundamental challenge in oncology, where cellular differences within and between tumors drive variations in treatment response and disease progression [5]. This biological complexity has catalyzed a paradigm shift from traditional "one-size-fits-all" clinical trials toward innovative master protocol frameworks that efficiently address molecular diversity [5]. Master protocols represent a transformative approach in precision medicine, utilizing a single, overarching design to evaluate multiple hypotheses simultaneously while standardizing trial procedures across different patient subpopulations [6] [5]. These designs have emerged as essential tools for accelerating targeted therapy development by matching the right treatments to the right patients based on specific molecular characteristics, thereby directly confronting the challenges posed by tumor heterogeneity.
Master Protocol Designs: Strategic Frameworks
Basket Trials: Targeting Pan-Cancer Molecular Alterations
Basket trials investigate a single targeted therapy across multiple cancer types that share a common molecular characteristic, such as a specific genetic mutation [6] [5]. This design operates on the principle of a proliferation-driven molecular phenotype, where the same molecular alteration drives cancer progression across different histological types [5]. The BRAF V600 trial exemplifies this approach, where vemurafenib demonstrated efficacy across various BRAF V600-mutant cancers, leading to the first FDA approval of an indication based on a cancer type-agnostic, biomarker-specific basket trial [6]. This design enables rapid clinical expansion of antitumor drugs across anatomical boundaries based on shared molecular drivers.
Experimental Protocol: Basket Trial Implementation
- Patient Screening: Implement high-throughput next-generation sequencing (NGS) panels to identify specific molecular alterations across cancer types [5]
- Centralized Biomarker Testing: Establish centralized molecular screening protocols with standardized operating procedures [6]
- Eligibility Assessment: Enroll patients based solely on molecular eligibility regardless of tumor histology [5]
- Response Evaluation: Utilize RECIST criteria with additional biomarker assessment including circulating tumor DNA (ctDNA) monitoring [7]
- Statistical Considerations: Employ Bayesian designs for efficient enrollment and endpoint assessment, particularly for rare mutations [6]
Umbrella Trials: Comprehensive Profiling for Single Disease Entities
Umbrella trials evaluate multiple targeted therapies within a single disease type, stratifying patients into biomarker-defined subgroups [6] [5]. The Lung-MAP trial represents a pioneering example, investigating multiple targeted agents for squamous cell lung cancer with biomarker-specific substudies [6]. This design acknowledges significant heterogeneity within a single cancer type and addresses it through parallel evaluation of multiple biomarker-guided therapies. Umbrella trials incorporate shared infrastructure for biomarker screening, data collection, and statistical analysis, significantly improving operational efficiency compared to multiple separate trials [6].
Table 1: Comparative Analysis of Master Protocol Designs
| Design Feature | Basket Trial | Umbrella Trial | Platform Trial |
|---|---|---|---|
| Patient Selection | Multiple diseases with common biomarker [5] | Single disease with multiple biomarkers [5] | Single disease with adaptive biomarkers [5] |
| Interventions | Single targeted therapy [6] | Multiple targeted therapies [6] | Multiple interventions with flexible addition/removal [6] |
| Statistical Approach | Histology-agnostic efficacy assessment [6] | Biomarker-stratified randomization [6] | Bayesian adaptive randomization with predictive probability [6] |
| Regulatory Path | Tumor-agnostic approval based on molecular alteration [6] | Indication-specific approval for biomarker-defined subgroups [6] | Graduation criteria for phase III progression [6] |
| Key Advantage | Identifies efficacy signals across tumor types [5] | Addresses intra-disease heterogeneity [5] | Continuously optimizes treatment strategies [5] |
Platform Trials: Adaptive Innovation in Oncology
Platform trials represent the most dynamic master protocol design, continuously evaluating multiple interventions for a disease with no predetermined stopping date and allowing for addition or removal of therapies based on interim analyses [6] [5]. The I-SPY 2 trial for high-risk breast cancer exemplifies this approach, using Bayesian adaptive randomization to preferentially assign patients to more promising treatments based on their molecular signature [6]. This design incorporates seamless phase II/III transitions, with interventions "graduating" when they demonstrate sufficient predictive probability of success in confirmatory trials [6]. Platform trials significantly enhance operational efficiency through shared control arms, infrastructure, and standardized procedures [6].
Diagram 1: Master Protocol Design Framework for Addressing Tumor Heterogeneity
Technological Enablers for Master Protocol Implementation
Advanced Genomic Profiling and Artificial Intelligence
Next-generation sequencing technologies form the foundation for master protocol implementation by enabling comprehensive molecular characterization of tumors [5]. The development of high-throughput NGS has facilitated simultaneous detection of diverse genomic alterations, including mutations, rearrangements, and copy number changes [5]. Artificial intelligence further enhances these capabilities, with tools like DeepHRD demonstrating three-fold improved accuracy in detecting homologous recombination deficiency compared to conventional genomic tests [8]. AI-driven platforms such as Prov-GigaPath and MSI-SEER are revolutionizing biomarker identification from histopathology images, expanding molecular profiling capabilities beyond traditional genomic approaches [8].
Experimental Protocol: Comprehensive Tumor Molecular Profiling
- Tissue Collection: Obtain fresh tumor biopsies or archival FFPE samples with appropriate quality control measures
- DNA/RNA Extraction: Use standardized kits (Qiagen, Illumina) with quality assessment via spectrophotometry and fragment analysis
- Sequencing Library Preparation: Employ targeted NGS panels (FoundationOne CDx, MSK-IMPACT) covering relevant cancer genes
- Bioinformatic Analysis: Implement pipelines for variant calling (GATK), copy number alteration assessment, and mutational signature analysis
- AI-Enhanced Pathology: Apply deep learning models (DeepHRD) to H&E slides for additional biomarker discovery [8]
- Data Integration: Combine genomic, transcriptomic, and digital pathology data for comprehensive molecular classification
Circulating Tumor DNA and Response Monitoring
Liquid biopsy approaches utilizing circulating tumor DNA (ctDNA) have emerged as powerful tools for dynamic monitoring of treatment response in master protocols [7]. ctDNA analysis enables real-time assessment of molecular response and emerging resistance mechanisms without repeated tissue biopsies. In 2025, early-phase clinical trials increasingly incorporate ctDNA testing to guide dose escalation and optimization decisions [7]. While ctDNA shows promise as a short-term biomarker for go/no-go decisions in trial development, correlation with long-term outcomes such as event-free survival and overall survival requires further validation [7].
Table 2: Advanced Research Reagent Solutions for Master Protocol Implementation
| Research Tool | Application | Key Features | Experimental Utility |
|---|---|---|---|
| Next-Generation Sequencing Panels (FoundationOne CDx, MSK-IMPACT) | Comprehensive genomic profiling [5] | 300-500 gene coverage, TMB, MSI status | Biomarker assignment for treatment arms |
| Digital Pathology Platforms (DeepHRD, Prov-GigaPath) | AI-based biomarker detection [8] | H&E slide analysis, transcriptomic imputation | Identifies patients for targeted therapies (PARP inhibitors) |
| Liquid Biopsy Assays (ctDNA monitoring) | Response assessment and resistance monitoring [7] | Tumor-informed and tumor-agnostic approaches | Early efficacy signals, dose optimization |
| Single-Cell Sequencing | Tumor microenvironment analysis [7] | Cell type resolution, spatial context | Identifies resistant cell populations and mechanisms |
| Multiplex Immunofluorescence | Immune contexture characterization | Simultaneous detection of 6+ markers | Predictive biomarker discovery for immunotherapies |
| Spatial Transcriptomics | Tumor heterogeneity mapping | Gene expression with tissue architecture | Regional biomarker distribution and clonal evolution |
Implementation Framework and Protocol Optimization
Operational Considerations for Master Protocol Execution
Successful implementation of master protocols requires sophisticated operational planning and infrastructure. The development of common data elements, standardized biomarker assessment protocols, and centralized imaging systems ensures consistency across participating sites [6]. Master protocols achieve significant efficiency gains through shared administrative, regulatory, and statistical infrastructure, substantially reducing the resources required compared to multiple independent trials [6]. The FDA has recognized the importance of these designs through specific guidance documents supporting basket and umbrella trials, facilitating regulatory alignment early in protocol development [6] [5].
Diagram 2: Integrated Molecular Profiling and Treatment Assignment Workflow
Future Directions: Evolving Precision Medicine Paradigms
The evolution of master protocols continues with emerging concepts of "Precision Pro," "Dynamic Precision," and "Intelligent Precision" shaping next-generation trial designs [5]. Precision Pro incorporates proteomics, metabolomics, and additional molecular layers beyond genomics to refine patient stratification. Dynamic Precision emphasizes real-time treatment adaptation based on evolving tumor characteristics, leveraging continuous monitoring technologies. Intelligent Precision integrates advanced artificial intelligence and machine learning for predictive biomarker discovery and treatment optimization [5]. These approaches will further enhance the ability of master protocols to address the complex challenges of tumor heterogeneity and accelerate targeted therapy development.
Experimental Protocol: Adaptive Therapy Modification Based on ctDNA Monitoring
- Baseline Assessment: Collect plasma for ctDNA analysis prior to treatment initiation
- Early Therapy Monitoring: Perform serial ctDNA assessment at cycles 2 and 3 of treatment
- Molecular Response Criteria: Define ctDNA reduction thresholds (e.g., >50% reduction) for continued therapy
- Emerging Resistance Detection: Monitor for new mutations indicative of resistance mechanisms
- Therapy Adaptation: Implement protocol-defined treatment modifications for molecular progression
- Correlative Analysis: Integrate ctDNA dynamics with radiographic assessment and symptom evaluation
Master protocol designs represent a transformative framework for addressing tumor heterogeneity and accelerating targeted therapy development in oncology. Through basket, umbrella, and platform trial structures, these approaches efficiently match emerging therapies with molecularly defined patient populations, overcoming limitations of traditional trial designs. Continued technological advances in molecular profiling, artificial intelligence, and response monitoring will further enhance the implementation and impact of master protocols, ultimately advancing precision medicine and improving outcomes for cancer patients.
The paradigm of oncology drug development has shifted significantly with the advent of precision medicine, moving away from a traditional "one-size-fits-all" approach toward strategies that tailor treatments based on individual patient biomarkers [9] [5]. This evolution has necessitated the development of innovative clinical trial designs that can efficiently evaluate multiple hypotheses within a single framework. Master protocols—comprising basket, umbrella, and platform trials—represent a transformative approach to clinical research that accelerates the development of targeted therapies by testing multiple drugs and/or multiple patient populations under a single, overarching protocol [9] [10]. These designs are particularly vital in oncology, where 91% of master protocol studies have been conducted, enabling researchers to address complex questions about biomarker-directed therapies more efficiently than traditional trial designs [11] [10].
Basket Trials: Design and Applications
Conceptual Framework and Definition
Basket trials are master protocol designs that evaluate a single targeted therapy across multiple disease populations—typically different cancer types—that share a common molecular alteration, such as a specific genetic mutation [9] [12] [13]. This design operates on the tissue-agnostic principle, hypothesizing that a drug targeting a specific molecular alteration will be effective regardless of the tumor's anatomical origin [11] [13]. The fundamental premise is that the shared molecular characteristic is a more important determinant of treatment response than the histology of the cancer itself.
In a basket trial, patients with various cancer types are grouped into a single cohort or "basket" based on the presence of a specific predictive biomarker. For instance, a trial might investigate a HER2-targeted therapy in patients with HER2-mutated cancers spanning breast, bladder, lung, and other tumor types [12]. This design enriches the study population by including only patients with markers that make them most likely to respond to the intervention, potentially providing earlier efficacy signals while collecting meaningful safety data [13].
Key Design Characteristics and Methodology
Basket trials are predominantly conducted in phase II settings (96%) and are frequently open-label (94%) without control groups (90%) [11]. The primary endpoint is typically objective response rate, and statistical design must account for potential heterogeneity in treatment effects across different tumor types [11].
The methodology involves a common screening protocol using standardized biomarker assays to identify eligible patients across multiple disease types. Patients who test positive for the target biomarker are enrolled regardless of their cancer histology. A key statistical challenge is determining whether to analyze results by pooling data across all cancer types or conducting histology-specific analyses [11]. While pooling increases statistical power, it risks masking differential treatment effects across tumor types.
Regulatory Precedents and Notable Examples
Basket trials have led to several landmark tissue-agnostic approvals by the U.S. Food and Drug Administration (FDA) [11] [13]. Key examples include:
- Larotrectinib: Approved in 2018 for solid tumors with NTRK gene fusions, based on a basket trial that enrolled patients across 17 different tumor types and demonstrated an 80% overall response rate [11].
- Pembrolizumab: Received the first tissue-agnostic indication in 2018 for microsatellite instability-high (MSI-H) or mismatch repair deficient (dMMR) solid tumors [11] [13].
- Dostarlimab: Approved in 2021 for MSI-high cancers based on basket trial evidence [11].
The European Organization for the Research and Treatment of Cancer (EORTC) CREATE trial of crizotinib represents another significant basket trial, evaluating the drug in multiple molecularly-defined cohorts [13].
Operational Implementation Protocol
Protocol Title: Basket Trial Design for Targeted Therapy Evaluation in Molecularly-Defined Populations
Screening Phase:
- Patient Identification: Identify potential candidates across multiple tumor-specific clinics
- Molecular Screening: Implement centralized biomarker testing using validated assays
- Eligibility Verification: Confirm presence of target molecular alteration through central laboratory review
Study Conduct:
- Enrollment: Register eligible patients to single-arm intervention cohort
- Treatment Administration: Implement standardized drug administration protocol across all sites
- Response Assessment: Conduct radiographic tumor assessments at predefined intervals (typically every 6-8 weeks) using RECIST criteria
- Safety Monitoring: Collect adverse event data according to CTCAE guidelines
Statistical Analysis Plan:
- Primary Endpoint: Objective response rate (ORR) assessed by independent review
- Sample Size Justification: Based on historical controls or minimal clinically meaningful effect size
- Interim Analysis: Preplanned interim analyses for futility or efficacy
- Subgroup Analysis: Pre-specified analysis by tumor histology to detect heterogeneity
Governance:
- Centralized IRB: Utilize single institutional review board for efficiency
- Study Steering Committee: Multidisciplinary oversight including disease-specific experts
- Data Monitoring Committee: Independent safety review
Umbrella Trials: Design and Applications
Conceptual Framework and Definition
Umbrella trials represent another master protocol approach characterized by evaluating multiple targeted therapies within a single disease entity, such as a specific cancer type, that is stratified into multiple subgroups based on different molecular alterations [9] [12] [14]. In this design, a single disease population is molecularly profiled, and patients are assigned to different treatment arms based on their specific biomarker profile [12]. The umbrella trial design follows the core principle of precision medicine by matching specific targeted therapies to the molecular drivers present in an individual patient's tumor.
Unlike basket trials that investigate one drug across multiple diseases, umbrella trials investigate multiple drugs within one disease [12]. This approach recognizes that what appears to be a single disease entity (e.g., lung cancer) actually comprises multiple molecular subtypes, each potentially requiring a different therapeutic approach. The design allows for the simultaneous evaluation of multiple biomarker-directed treatment strategies in a coordinated manner that would be logistically challenging to conduct as separate trials.
Key Design Characteristics and Methodology
Umbrella trials typically employ a common screening protocol with standardized biomarker assays to stratify patients with a single disease into multiple molecular subgroups [12] [14]. Each subgroup is then assigned to a specific targeted therapy matched to its molecular profile. The design may include both randomized and non-randomized elements, with some subtrials featuring randomization to control arms while others may be single-arm [14].
These trials are complex operationally, requiring robust biomarker screening infrastructure and clear assignment rules. A notable feature is the potential inclusion of an "all comers" subgroup for patients whose tumors lack any of the predefined biomarkers, who may be assigned to standard therapy or a non-matched investigational agent [14].
Notable Examples and Implementation
The plasmaMATCH trial exemplifies the umbrella design, evaluating five different therapies for advanced breast cancer stratified by molecular signatures [12]. The trial included:
- Group A (ESR1 mutations): Extended-dose fulvestrant
- Group B (HER2 mutations): Neratinib + fulvestrant (if estrogen receptor co-mutation)
- Group C (AKT mutations): AZD5364 + fulvestrant
- Group D (AKT activation): AZD5364 alone
- Group E (Triple-negative): Olaparib + AZD5364
Other notable umbrella trials include LUNG-MAP and NCI-MATCH, though the latter represents a hybrid design with characteristics of both basket and umbrella trials [14]. A systematic review identified 38 umbrella trials, with most (73.7%) conducted in early-phase settings and the vast majority (92.1%) in oncology [14].
Operational Implementation Protocol
Protocol Title: Umbrella Trial for Targeted Therapy Evaluation in Molecularly-Stratified Disease
Screening and Stratification Phase:
- Centralized Biomarker Testing: Implement high-throughput molecular profiling using next-generation sequencing panels
- Molecular Tumor Board: Establish multidisciplinary review for assignment recommendations
- Treatment Assignment Algorithm: Implement predefined rules matching biomarkers to corresponding targeted therapies
Study Conduct:
- Multi-Arm Structure: Establish parallel subtrials with protocol-specific procedures for each arm
- Randomization Schema: For subtrials with control arms, implement centralized randomization system
- Biomarker-Specific Endpoints: Define subgroup-specific primary endpoints with appropriate statistical powering
- Cross-Subtrial Safety Monitoring: Implement both subtrial-specific and cross-protocol safety oversight
Statistical Considerations:
- Sample Size Calculation: Determine sample size for each subtrial independently based on subtrial-specific hypotheses
- Error Rate Control: Consider appropriate multiple testing corrections for cross-subtrial analyses
- Interim Monitoring Plan: Define stopping rules for each subtrial independently
- Integrative Analysis: Plan for cross-subtrial analyses to evaluate overall trial performance and biomarker utility
Governance Structure:
- Overall Steering Committee: Coordinate cross-subtrial activities and resource allocation
- Subtrial-Specific Committees: Provide domain expertise for specific biomarker-therapy combinations
- Central Data Management: Implement unified data collection system with subtrial-specific modules
Platform Trials: Design and Applications
Conceptual Framework and Definition
Platform trials represent an adaptive master protocol design that compares multiple interventions against a common control group within a single, ongoing trial infrastructure that allows for interventions to be added or removed over time based on predefined decision rules [15] [10]. Unlike traditional trials with fixed design elements, platform trials are perpetual learning systems that evolve in response to accumulating data, creating a more efficient framework for evaluating therapeutic interventions [15].
These trials are characterized by their flexibility—new treatments can be introduced as they become available, and existing treatments can be dropped for futility or established as new standards of care based on interim analyses [15]. This adaptive approach allows the trial platform to respond more rapidly to emerging scientific information than traditional fixed-length trials, potentially accelerating the identification of effective treatments.
Key Design Characteristics and Methodology
The defining feature of platform trials is their flexible infrastructure that can accommodate multiple interventions entering and exiting the platform over time according to predefined rules [15]. Key methodological characteristics include:
- Common Control Arm: Multiple interventions share a common control group, increasing statistical efficiency
- Adaptive Features: Bayesian or frequentist statistical frameworks with prespecified rules for adding/dropping arms
- Interim Analyses: Regular statistical assessments of accumulating data to make adaptations
- Response-Adaptive Randomization: Potential to adjust randomization ratios to favor better-performing treatments
- Multi-Stage Design: Ability to make go/no-go decisions at multiple points throughout the trial
Platform trials typically employ Bayesian statistical methods because of their flexibility and principled framework for information borrowing, sequential analysis, and probabilistic interpretation of efficacy [15]. The design requires substantial upfront planning and sophisticated simulation to ensure proper operating characteristics.
Notable Examples and Implementation
The Randomized, Embedded, Multifactorial Adaptive Platform for Community Acquired Pneumonia (REMAP-CAP) represents a highly sophisticated platform trial that has evaluated multiple interventions for community-acquired pneumonia, including during the COVID-19 pandemic [15]. As of 2022, the trial had achieved approximately 24,500 patient randomizations across 66 interventions spanning 18 domains [15].
In oncology, platform trials are increasingly being implemented to efficiently evaluate multiple therapeutic strategies. A recent review identified 127 registered platform trials with a combined 823 arms, most started within the five years preceding 2022 [15]. These trials are particularly valuable in settings with considerable clinical equipoise around best practice that is likely to continue even in the presence of ongoing discoveries [15].
Operational Implementation Protocol
Protocol Title: Platform Trial with Adaptive Features for Multiple Intervention Evaluation
Core Infrastructure Establishment:
- Master Protocol Development: Create overarching protocol with shared procedures, data collection standards, and governance structure
- Statistical Framework: Define Bayesian or frequentist adaptive framework with decision rules
- Centralized Operations: Establish trial coordinating center with standardized operating procedures
- Data Systems: Implement flexible data management platform capable of accommodating new arms
Trial Conduct and Adaptation:
- Interim Analysis Schedule: Predefine timing and methodology for interim assessments
- Arm Addition Protocol: Establish scientific review process and statistical criteria for adding new interventions
- Dropping Rules: Define futility and efficacy thresholds for arm removal
- Randomization Adaptation: Plan for potential response-adaptive randomization adjustments
Statistical Design Elements:
- Simulation Plan: Conduct extensive simulation studies to evaluate operating characteristics under multiple scenarios
- Error Rate Control: Implement appropriate Bayesian or frequentist methods to control type I error
- Information Borrowing: Specify hierarchical models or other methods for borrowing information across subgroups or arms
- Decision Rules: Define precise probabilistic thresholds for all adaptation decisions
Governance and Oversight:
- Executive Committee: Provide overall trial leadership and resource allocation
- Independent Data Monitoring Committee: Review interim results and make adaptation recommendations
- Statistical Advisory Group: Provide specialized expertise on complex adaptive design issues
- Intervention-Specific Committees: Oversee scientific aspects of individual interventions
Comparative Analysis of Trial Designs
Structural and Methodological Comparison
The following table summarizes the key characteristics of basket, umbrella, and platform trials, highlighting their distinct approaches to clinical trial design in precision oncology:
Table 1: Comparative Analysis of Master Protocol Designs
| Characteristic | Basket Trial | Umbrella Trial | Platform Trial |
|---|---|---|---|
| Patient Population | Multiple diseases sharing common molecular alteration [9] [12] | Single disease stratified into molecular subgroups [9] [12] | Single disease or multiple diseases with flexible eligibility [15] |
| Intervention Strategy | Single targeted therapy [13] | Multiple targeted therapies (one per subgroup) [12] | Multiple interventions evaluated against common control [15] |
| Key Rationale | Tissue-agnostic drug development [11] [13] | Comprehensive evaluation of multiple therapies in molecularly-defined subsets [14] | Efficient, perpetual learning system [15] |
| Typical Phase | Phase II (96%) [11] | Early phase (73.7%) [14] | Phase III (47%) [10] |
| Control Group | Rarely used (10% have controls) [11] | More common, may be subtrial-specific [14] | Always includes common control arm [15] |
| Adaptive Features | Limited | Subtrial-specific adaptations possible [14] | Core feature - interventions enter/exit based on predefined rules [15] |
| Statistical Approach | Pooled or stratified analysis [11] | Typically frequentist, subtrial-specific [14] | Often Bayesian with information borrowing [15] |
| Primary Efficiency | Accelerates tissue-agnostic drug development [13] | Parallel evaluation of multiple biomarker-therapy combinations [14] | Shared infrastructure, common control, adaptive features [15] |
Quantitative Trial Landscape
Table 2: Quantitative Landscape of Master Protocol Trials Based on Systematic Reviews
| Parameter | Basket Trials | Umbrella Trials | Platform Trials |
|---|---|---|---|
| Percentage in Oncology | 91% [11] | 92.1% [14] | Majority [10] |
| Median Sample Size | 205 patients [11] | Variable by subtrial [14] | Typically large (e.g., REMAP-CAP: 24,500 randomizations) [15] |
| Average Number of Disease Types | 17 (range: 10-40) [11] | Single disease with multiple subgroups [12] | Flexible, can include multiple diseases or subgroups [15] |
| Randomization Prevalence | 10% [11] | More common than basket designs [14] | Universal [15] |
| Common Primary Endpoint | Objective Response Rate (ORR) [11] | Varies by subtrial [14] | Disease-specific primary outcomes [15] |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Core Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Master Protocol Implementation
| Reagent/Platform | Function | Application Notes |
|---|---|---|
| Next-Generation Sequencing Panels | High-throughput molecular profiling for biomarker identification [5] | Foundation for patient stratification; requires validation and standardization across sites |
| Digital Pathology Platforms | Quantitative assessment of protein expression and tissue morphology | Enables centralized biomarker assessment and quality control |
| Liquid Biopsy Assays | Non-invasive biomarker assessment via circulating tumor DNA [5] | Particularly valuable for serial monitoring in adaptive trials |
| Biobanking Infrastructure | Collection, processing, and storage of biospecimens | Critical for correlative studies and biomarker validation |
| Centralized Biomarker Validation | Standardized assessment of molecular targets across participating sites | Essential for trial integrity; minimizes inter-site variability |
| Statistical Analysis Software | Implementation of complex adaptive designs and Bayesian methods [15] | Requires specialized packages for platform trial simulation and conduct |
| Clinical Trial Management Systems | Coordination of complex multi-arm, multi-site trials | Must accommodate dynamic protocol amendments and adaptive features |
Methodological Considerations for Implementation
Biomarker Assay Validation: Prior to trial initiation, all biomarker assays require rigorous analytical validation establishing sensitivity, specificity, reproducibility, and precision [12]. Clinical cutpoints for biomarker positivity should be predefined based on biological rationale or previous data when available.
Statistical Simulation: For platform trials and complex adaptive designs, comprehensive simulation studies are mandatory to evaluate operating characteristics under various scenarios [15]. These simulations should assess type I error control, power, sample size requirements, and adaptation frequency.
Data Standardization: Implement common data elements across all trial arms and standardized data collection procedures to ensure compatibility and facilitate integrated analyses [15].
Basket, umbrella, and platform trials represent transformative approaches to clinical research that align with the fundamental principles of precision medicine. By moving beyond traditional "one-size-fits-all" trial designs, these master protocols enable more efficient evaluation of targeted therapies in molecularly-defined patient populations. Basket trials facilitate tissue-agnostic drug development by testing single targeted therapies across multiple diseases sharing common molecular alterations. Umbrella trials accelerate the comprehensive evaluation of multiple targeted therapies within a single disease stratified by molecular subtypes. Platform trials create perpetual learning systems that efficiently compare multiple interventions against a common control while adapting to accumulating evidence.
The successful implementation of these designs requires sophisticated infrastructure, including robust biomarker assessment platforms, specialized statistical expertise, and flexible operational systems. As precision medicine continues to evolve, these master protocol designs will play an increasingly vital role in accelerating the development of personalized cancer therapies and improving patient outcomes. Their growing adoption represents a paradigm shift in clinical research methodology, emphasizing efficiency, flexibility, and patient-centered therapeutic development.
In the evolving landscape of oncology clinical trials, master protocols have emerged as a transformative approach to streamline drug development. The U.S. Food and Drug Administration (FDA) defines a master protocol as "a protocol designed with multiple substudies, which may have different objectives and involve coordinated efforts to evaluate one or more medical products in one or more diseases or conditions within the overall study structure" [16]. The FDA's Oncology Center of Excellence (OCE) has recognized the growing importance of these innovative trial designs and includes them within its guidance agenda, reflecting their significance in modern clinical research [17]. This regulatory recognition provides a framework for researchers, scientists, and drug development professionals seeking to implement these efficient trial models, particularly in the complex field of oncology.
The December 2023 FDA draft guidance on "Master Protocols for Drug and Biological Product Development" offers non-binding recommendations on the design, analysis, and regulatory submission of these complex trials [18]. This guidance arrives at a critical juncture in drug development, addressing challenges posed by precision medicine and rare diseases where traditional single-drug, single-population trials have become increasingly inefficient. For oncology research specifically, master protocols enable simultaneous evaluation of multiple targeted therapies across different cancer subtypes, accelerating the development of personalized treatment approaches and maximizing the use of limited patient populations [16].
Master Protocol Typologies and Structural Framework
Master protocols encompass several distinct trial design categories, each with specific structural characteristics and applications in oncology research. Understanding these typologies is essential for selecting the appropriate framework for specific research objectives. The FDA guidance formally recognizes three primary types of master protocols, each serving different strategic purposes in clinical development [16].
Table: Master Protocol Typologies in Clinical Research
| Protocol Type | Primary Objective | Oncology Application Example | Key Structural Feature |
|---|---|---|---|
| Basket Trials | Evaluate a single medical product for multiple diseases or disease subtypes | Testing a targeted therapy (e.g., PI3K inhibitor) across different cancer types sharing a specific mutation | Single investigational product across multiple diseases |
| Umbrella Trials | Evaluate multiple medical products concurrently for a single disease | Testing different targeted therapies against different molecular alterations within a single cancer type | Multiple products within a single disease |
| Platform Trials | Assess multiple medical products for a disease in an ongoing manner | Adaptive design where treatments enter or leave the platform based on interim analyses | Flexible design with additions/removals of treatments |
The structural framework common to all master protocol designs involves a centralized infrastructure with shared components across substudies. This includes common control groups, standardized data collection methods, centralized imaging and laboratory assessment, unified statistical analysis plans, and coordinated regulatory oversight. The Clinical Electronic Structured Harmonised Protocol (CeSHarP) initiative, with its recently updated template in June 2025, provides an international standard for the content and electronic exchange of clinical trial protocol information, further supporting the implementation of master protocols [19]. This harmonized approach facilitates efficient review and assessment by regulators, sponsors, ethical oversight bodies, investigators, and other stakeholders involved in complex oncology trials.
Figure: Structural Framework of Master Protocol Designs
FDA Regulatory Considerations and Submission Pathways
Regulatory Submission Framework
Navigating the regulatory pathway for master protocols requires careful planning and early engagement with regulatory authorities. The FDA recommends submitting each master protocol as a new Investigational New Drug (IND) application, rather than attempting to modify existing INDs [16]. This approach provides a clean regulatory framework for evaluating the complex, multi-faceted nature of master protocols. Sponsors are strongly encouraged to request pre-IND meetings to discuss protocol design, statistical considerations, and submission details specific to their proposed master protocol. This early alignment is particularly valuable for oncology trials where molecular profiling, biomarker development, and patient stratification strategies add layers of complexity to the trial design.
The Oncology Center of Excellence (OCE) at FDA plays a pivotal role in reviewing master protocols for cancer therapies, providing specialized expertise in oncology drug development [17]. For ongoing protocol modifications, especially in platform trials where treatments may enter or exit the platform, the FDA guidance outlines specific procedures for protocol amendments. The guidance emphasizes the importance of a well-designed communication plan to ensure timely information sharing among all stakeholders, including sponsors, investigators, institutional review boards (IRBs), and regulatory agencies [16]. This transparent communication is essential for maintaining the scientific and regulatory integrity of these complex, evolving trials.
Documentation and Reporting Standards
Master protocols require comprehensive documentation that addresses both the overall master protocol structure and individual substudy specifications. The M11 Clinical Electronic Structured Harmonised Protocol (CeSHarP) template, updated in June 2025, provides an international standard for the content and electronic exchange of clinical trial protocol information [19]. This harmonized approach facilitates efficient review by regulators, sponsors, and ethical oversight bodies by standardizing headers, common text, and data fields across submissions.
Table: FDA Recommended Submission Elements for Master Protocols
| Submission Component | Key Requirements | Special Considerations for Oncology |
|---|---|---|
| Overall Protocol Structure | Master protocol design rationale and governance | Biomarker validation strategy and molecular testing approach |
| Substudy Specifications | Individual subprotocols with clear objectives | Biomarker-patient matching algorithms and stratification methods |
| Statistical Analysis Plan | Type I error control, power calculations, analysis populations | Adaptive design features, interim analysis timing, biomarker subgroup analyses |
| Investigator's Brochure | Comprehensive safety data for all investigational products | Unique safety profiles of targeted therapies and immunotherapies |
| Informed Consent Template | Clear explanation of complex trial structure | Germline testing implications and genetic counseling resources |
| Safety Monitoring Plan | Data Monitoring Committee (DMC) charter and operating procedures | Specialized safety monitoring for novel targeted therapies |
Regarding protocol deviations in master protocols, the FDA's January 2025 draft guidance defines "important protocol deviations" as those that might significantly affect the completeness, accuracy, and/or reliability of the study data or that might significantly affect a subject's rights, safety, or well-being [20]. The guidance recommends that sponsors "pre-specify which type of protocol deviations will be considered important" within the context of their specific master protocol. For oncology trials, this is particularly relevant for deviations related to biomarker testing accuracy, treatment allocation procedures, and endpoint assessment methodologies that are critical to interpreting trial results in molecularly-defined populations.
Implementation Protocols and Operational Considerations
Statistical Design and Analysis Methodology
The statistical methodology for master protocols requires sophisticated approaches to maintain scientific integrity while accommodating multiple treatments and potential adaptations. A key challenge reported by practitioners is the difficulty in evaluating the statistical properties of the master protocol and managing type I error rates across multiple sub-studies [16]. To address these issues, statisticians are developing new methodologies and adapting existing techniques to the unique requirements of master protocols.
For basket trials, which test a single targeted therapy across multiple tumor types defined by a common biomarker, Bayesian hierarchical models are often employed to borrow information across cancer types while preventing excessive borrowing when treatment effects differ. Umbrella trials, which evaluate multiple targeted therapies within a single cancer population stratified by molecular markers, typically utilize stratified randomization and require careful planning for biomarker assessment and allocation procedures. Platform trials, characterized by their adaptive nature, employ Bayesian response-adaptive randomization methods that allow treatment arms to be added or removed based on interim analyses, with some patients potentially being re-randomized to new arms as the trial evolves.
The FDA guidance emphasizes that randomization and blinding strategies require careful planning in master protocols [16]. The Agency recommends allocating more subjects to control arms to increase statistical power and considering adaptive randomization ratios for platform trials. All these statistical approaches must be pre-specified in the statistical analysis plan, including detailed simulations to understand operating characteristics under various scenarios.
Patient Recruitment and Informed Consent Protocols
Implementing effective patient recruitment and informed consent processes presents unique challenges in master protocols due to their complexity and evolving nature. The informed consent process must adequately communicate the trial's structure, including the possibility of multiple treatment options, complex randomization procedures, and for platform trials, the potential for new treatments to enter the trial over time [16]. The FDA recommends using a central Institutional Review Board (IRB) to review consent forms and ensuring that patients are informed about all potential treatment arms before randomization.
For oncology master protocols, the patient pathway typically begins with comprehensive molecular profiling of the patient's tumor to determine eligibility for specific substudies. The implementation of this screening process requires coordination between multiple stakeholders, including pathologists, molecular laboratories, bioinformaticians, and clinical investigators. A standardized approach to biomarker assessment is critical, particularly in basket trials where the same biomarker may be detected across different cancer types using various testing platforms.
Figure: Patient Pathway in Oncology Master Protocols
Safety Monitoring and Data Collection Procedures
Safety monitoring in master protocols requires specialized approaches to address the challenges of multiple investigational products and complex trial designs. The FDA recommends using a Data Monitoring Committee (DMC) or other independent entity to review accumulating safety and efficacy data across all treatment arms [16]. This centralized approach helps maintain trial integrity while ensuring patient safety across multiple investigational products, which is particularly important in oncology trials where novel targeted therapies and immunotherapies may have unique and evolving safety profiles.
Data collection procedures must be standardized across all substudies while allowing for product-specific assessments where necessary. Critical-to-quality factors—defined in the ICH E8(R1) Guidance as "attributes of a study whose integrity is fundamental to the protection of study participants, the reliability and interpretability of the study results, and the decisions made based on the study results"—should be identified and prioritized in the data collection plan [20]. For oncology master protocols, these typically include biomarker assessment accuracy, treatment administration compliance, endpoint evaluation consistency, and safety monitoring completeness.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing successful master protocols in oncology requires specialized reagents and materials to support the complex molecular profiling and analytical processes. The following toolkit outlines essential research reagent solutions and their applications in master protocol implementation.
Table: Research Reagent Solutions for Oncology Master Protocols
| Reagent/Material Category | Specific Examples | Application in Master Protocols |
|---|---|---|
| Next-Generation Sequencing (NGS) Panels | Comprehensive genomic profiling panels, whole exome sequencing, transcriptome sequencing | Molecular screening for basket and umbrella trials; identification of actionable alterations across multiple cancer types |
| Immunohistochemistry (IHC) Assays | PD-L1, MSH2, MSH6, MLH1, PMS2 antibodies; automated staining systems | Biomarker validation and patient stratification; companion diagnostic development |
| Circulating Tumor DNA (ctDNA) Kits | ctDNA extraction kits; digital PCR assays; NGS libraries for liquid biopsies | Longitudinal monitoring of treatment response; minimal residual disease detection; overcoming tissue limitations |
| Cell-Based Assays | Organoid culture systems; patient-derived xenograft models; high-throughput drug screening | Preclinical validation of targeted therapies; functional assessment of genomic alterations; drug combination testing |
| Multiplex Immunofluorescence Panels | Multi-color IHC panels; spatial transcriptomics platforms; automated image analysis systems | Tumor microenvironment characterization; immune cell profiling; biomarker discovery in limited tissue samples |
| Data Analysis Platforms | Bioinformatics pipelines; cloud-based data integration tools; clinical trial management systems | Molecular data integration; real-time eligibility assessment; biomarker-signature development |
These research reagents form the foundation for implementing master protocols in oncology, enabling the comprehensive molecular characterization necessary for patient allocation to appropriate substudies. The selection and validation of these reagents should be conducted following Good Laboratory Practice (GLP) standards and in accordance with any relevant FDA guidance on biomarker validation and companion diagnostic development. As master protocols continue to evolve, these reagent solutions will play an increasingly critical role in enabling efficient patient screening, accurate biomarker assessment, and comprehensive molecular monitoring throughout the trial lifecycle.
Implementing Master Protocols: Methodologies and Real-World Applications in Oncology
In the evolving landscape of precision oncology, master protocol designs have emerged as transformative approaches for efficient therapeutic development. Among these, basket trials represent a paradigm shift from traditional histology-based classification to a biomarker-driven methodology. A basket trial is defined as a master protocol study designed to test a single investigational drug or drug combination in different populations defined by disease stage, histology, number of prior therapies, genetic or other biomarkers, or demographic characteristics [11] [21]. This design is fundamentally histology-agnostic, enrolling patients based solely on shared molecular characteristics regardless of their cancer's tissue of origin [6] [5].
The conceptual foundation of basket trials stems from the understanding that many cancers share common proliferation-driven molecular phenotypes that transcend traditional histopathological classifications [5]. Advances in sequencing technologies have revealed recurrent alterations across cancer types, enabling the development of targeted therapies that act on distinct mechanisms of tumorigenesis common to multiple malignancies [11]. This recognition, coupled with the need to efficiently study rare molecular subsets, has propelled the adoption of basket designs in oncology drug development [22].
Basket trials are predominantly conducted within the phase II setting and are often open-label, single-arm studies designed to estimate high and durable objective responses [11]. They pose unique challenges to statistical design and interpretation, particularly regarding how to handle potential heterogeneity of treatment effects across different tumor types [11]. Despite these challenges, basket trials have demonstrated significant utility in accelerating the development of tissue-agnostic therapies, with several notable regulatory approvals based on their results [11] [23].
Quantitative Analysis of the ROAR Basket Trial
The Rare Oncology Agnostic Research (ROAR) trial represents a seminal example of a basket trial evaluating dabrafenib plus trametinib in patients with BRAF V600E-mutated rare cancers. This multicenter, open-label, single-arm, phase 2 basket trial investigated the combination therapy across eight rare cancer cohorts [23].
Primary Efficacy Endpoints
Table 1: Investigator-Assessed Objective Response Rate (ORR) by Cancer Cohort in the ROAR Trial [23]
| Cancer Cohort | Patient Number (n) | Objective Response Rate (ORR) | Complete Response (CR) | Partial Response (PR) |
|---|---|---|---|---|
| Anaplastic Thyroid Carcinoma (ATC) | 36 | 56% | 3% | 53% |
| Biliary Tract Cancer (BTC) | 43 | 53% | 2% | 51% |
| Gastrointestinal Stromal Tumor (GIST) | 1 | 0% | 0% | 0% |
| Adenocarcinoma of the Small Intestine (ASI) | 3 | 67% | 0% | 67% |
| Low-Grade Glioma (LGG) | 13 | 54% | 8% | 46% |
| High-Grade Glioma (HGG) | 45 | 33% | 7% | 27% |
| Hairy Cell Leukemia (HCL) | 55 | 89% | 44% | 45% |
| Multiple Myeloma (MM) | 19 | 50% | 0% | 50% |
Secondary Efficacy Endpoints
Table 2: Secondary Endpoints including Duration of Response (DoR), Progression-Free Survival (PFS), and Overall Survival (OS) [23]
| Cancer Cohort | Median DoR (months) | Median PFS (months) | Median OS (months) |
|---|---|---|---|
| Anaplastic Thyroid Carcinoma (ATC) | 14.4 | 6.7 | 14.5 |
| Biliary Tract Cancer (BTC) | 8.9 | 9.0 | 13.5 |
| Gastrointestinal Stromal Tumor (GIST) | Not reached | Not reached | Not reached |
| Adenocarcinoma of the Small Intestine (ASI) | 7.7 | Not evaluable | 21.8 |
| Low-Grade Glioma (LGG) | Not reached | 9.5 | Not evaluable |
| High-Grade Glioma (HGG) | 31.2 | 5.5 | 17.6 |
| Hairy Cell Leukemia (HCL) | Not reached | Not evaluable | Not evaluable |
| Multiple Myeloma (MM) | 11.1 | 6.3 | 33.9 |
Safety Profile
The ROAR trial demonstrated a consistent safety profile across cohorts. The most frequent (≥20% of patients) treatment-related adverse events were pyrexia (40.8%), fatigue (25.7%), chills (25.7%), nausea (23.8%), and rash (20.4%) [23]. Grade 3 or worse adverse events were reported in 53% of patients in the glioma cohorts, with the most common being fatigue (9%), decreased neutrophil count (9%), headache (5%), and neutropenia (5%) [24]. These findings were consistent with the known safety profile of dabrafenib plus trametinib in other approved indications [23].
Experimental Protocols and Methodologies
Core Basket Trial Protocol Structure
The successful implementation of a basket trial requires meticulous protocol development with specific considerations for histology-agnostic designs:
Patient Eligibility and Biomarker Screening:
- Inclusion of patients with advanced solid tumors or hematologic malignancies harboring the specific biomarker (BRAF V600E mutation) regardless of tumor histology [23]
- Centralized biomarker confirmation using validated assays (e.g., next-generation sequencing, immunohistochemistry, or PCR-based methods) [23] [25]
- ECOG performance status of 0-2 and adequate organ function [24]
- Prior therapy requirements may vary by cohort but typically include progression on standard treatments [23]
Treatment Administration:
- Dabrafenib 150 mg orally twice daily plus trametinib 2 mg orally once daily on a continuous dosing schedule [23] [24]
- Treatment continues until unacceptable toxicity, disease progression, or death [24]
- Dose modifications permitted for management of adverse events [23]
Assessment Schedule:
- Tumor assessments conducted every 8 weeks using appropriate radiographic criteria (RECIST 1.1 for solid tumors, Lugano criteria for lymphomas) [23]
- Additional disease-specific assessments as needed (e.g., RANO criteria for glioma) [24]
- Safety assessments performed at each visit, including vital signs, laboratory parameters, and physical examination [23]
Statistical Considerations:
- Primary endpoint: investigator-assessed objective response rate (ORR) [23]
- Sample size determination based on Simon's two-stage minimax design or Bayesian approaches to allow for early stopping for futility or efficacy [11]
- Intent-to-treat analysis for all enrolled patients who received at least one dose of study medication [23]
- Secondary endpoints: duration of response, progression-free survival, overall survival, and safety [24]
Biomarker Validation Protocol
Sample Collection and Processing:
- Collection of formalin-fixed paraffin-embedded (FFPE) tumor tissue blocks or slides from most recent available tumor biopsy [25]
- Alternatively, use of liquid biopsy approaches (circulating tumor DNA) when tissue is unavailable [25]
- Central laboratory processing with quality control metrics for tumor content and DNA integrity [23]
Mutation Detection Methods:
- Next-generation sequencing using validated panels covering BRAF V600E and other relevant mutations [22]
- Immunohistochemistry with VE1 antibody for BRAF V600E mutant protein detection [22]
- Reverse transcriptase-polymerase chain reaction (RT-PCR) as an alternative method [22]
- Orthogonal validation of positive results using a second method when possible [25]
Quality Assurance:
- Analytical validation of assay performance characteristics (sensitivity, specificity, reproducibility) [25]
- Regular proficiency testing and internal quality control measures [25]
- Documentation of assay validation for potential companion diagnostic development [25]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Basket Trial Implementation
| Reagent/Platform | Function | Application in BRAF V600E Trial |
|---|---|---|
| Next-Generation Sequencing Panels | Comprehensive genomic profiling to identify targetable mutations | Detection of BRAF V600E mutation and co-occurring genetic alterations [22] |
| IHC Anti-BRAF V600E (VE1) Antibody | Immunohistochemical detection of mutant BRAF protein | Rapid, cost-effective screening for BRAF V600E mutation status [22] |
| Digital PCR Platforms | Highly sensitive mutation detection and quantification | Monitoring treatment response via circulating tumor DNA [25] |
| Cell Line Panels | Preclinical models for drug sensitivity assessment | Validation of BRAF inhibitor efficacy across tumor types [22] |
| PDX Models (Patient-Derived Xenografts) | In vivo models maintaining tumor heterogeneity | Evaluating context-dependent responses to targeted therapy [22] |
Visualizing Basket Trial Workflows and Biological Mechanisms
Basket Trial Structure and Workflow
Basket Trial Structure and Workflow - This diagram illustrates the patient flow in a biomarker-driven basket trial, from screening through treatment and response assessment.
MAPK Pathway and Therapeutic Targeting
MAPK Pathway and Therapeutic Targeting - This diagram visualizes the MAPK signaling pathway and the mechanism of action of dabrafenib and trametinib in targeting BRAF V600E-mutant signaling.
Basket trials represent a transformative approach in oncology drug development, enabling efficient evaluation of targeted therapies across multiple tumor types based on shared molecular alterations. The ROAR trial with dabrafenib and trametinib exemplifies the successful application of this design, demonstrating clinically meaningful activity across diverse BRAF V600E-mutated rare cancers with a consistent safety profile [23]. This histology-agnostic, biomarker-specific approach has led to regulatory approvals that have fundamentally altered treatment paradigms for patients with rare malignancies [23] [22].
The implementation of basket trials requires careful consideration of statistical designs that account for potential heterogeneity of treatment effects across tumor types [11]. Furthermore, robust biomarker validation and standardized response assessment are critical for generating interpretable results [25]. As precision medicine continues to evolve, basket trials will play an increasingly important role in accelerating the development of targeted therapies, particularly for rare molecular subsets that transcend traditional histopathological classifications [5] [22].
Umbrella trials represent a transformative master protocol design in oncology clinical research, enabling the simultaneous evaluation of multiple targeted therapies within a single cancer type. Framed within the broader context of master protocols, which the U.S. Food and Drug Administration recognizes as "efficient clinical trial design strategies to expedite development of oncology drugs and biologics," umbrella trials specifically investigate multiple disease subsets defined by molecular markers within a single disease [21]. The Lung Cancer Master Protocol (Lung-MAP) stands as a pioneering example of this design, established as a precision medicine trial for patients with advanced non-small cell lung cancer (NSCLC) that uses genomic screening to match patients to investigational targeted treatments [26].
This approach fundamentally shifts the paradigm from histology-based to biomarker-driven cancer drug development. By leveraging a single infrastructure for patient screening, data collection, and regulatory coordination, umbrella trials like Lung-MAP accelerate therapeutic development while reducing operational costs and streamlining the identification of effective treatments for molecularly defined patient subgroups.
Lung-MAP: A Paradigm for Umbrella Trials
Evolution and Screening Enhancements
Since its initiation in 2014, Lung-MAP has continuously evolved to incorporate scientific advancements and practical clinical needs. The trial initially focused on patients with advanced squamous-cell NSCLC but expanded in 2019 (as Lung-MAP 2.0) to include all NSCLC subtypes [26]. The most recent iteration, Lung-MAP 3.0, implemented in 2025, significantly reformed the screening process by allowing the use of prior genomic testing results for sub-study assignment, eliminating the previous universal requirement for new biomarker testing on the Foundation Medicine platform [26].
This pragmatic enhancement dramatically improves the trial's accessibility, particularly for community-based sites where most patients receive care. As noted by the trial's principal investigator, Dr. Karen Reckamp, "Lung MAP 3.0 exemplifies the ability of the trial protocol platform to remain dynamic and evolve with the shifting standards for lung cancer diagnosis and treatment to meet the needs of a broader group of patients" [26]. This flexibility ensures that the trial population better reflects the real-world demographics of those diagnosed with advanced NSCLC.
Quantitative Trial Metrics
The scale and impact of Lung-MAP and similar trials are demonstrated through comprehensive clinical trial metrics collected across NCI-Designated Cancer Centers, as shown in the tables below.
Table 1: Clinical Trial Metrics by Study Source (Representative Fiscal Year)
| Study Source | Open Trials | Patients Accrued |
|---|---|---|
| Industry | 7,544 | 26,580 |
| Institutional | 7,375 | 195,477 |
| National Cooperative Group | 5,796 | 13,416 |
| External Peer Reviewed | 2,330 | 105,486 |
| Other/Unknown | 705 | 198,686 |
| Total | 23,750 | 539,645 |
Table 2: Clinical Trial Metrics by Phase (Representative Fiscal Year)
| Phase | Open Trials | Patients Accrued |
|---|---|---|
| I | 3,098 | 10,976 |
| I/II | 1,654 | 6,245 |
| II | 5,731 | 22,037 |
| II/III | 444 | 959 |
| III | 4,549 | 17,072 |
| 0 | 79 | 680 |
| IV | 128 | 720 |
| Pilot/Feasibility | 1,456 | 16,157 |
| N/A | 6,598 | 464,500 |
| Total | 23,750 | 539,645 |
Table 3: Clinical Trial Metrics by Primary Purpose (Representative Fiscal Year)
| Primary Purpose | Open Trials | Patients Accrued |
|---|---|---|
| Treatment (TRE) | 15,558 | 51,242 |
| Basic Science (BAS) | 2,412 | 65,147 |
| Other (OTH) | 2,802 | 150,043 |
| Diagnostic (DIA) | 823 | 12,076 |
| Supportive Care (SUP) | 1,051 | 14,287 |
| Prevention (PRE) | 439 | 28,132 |
| Screening (SCR) | 307 | 16,045 |
| Health Services Research (HSR) | 358 | 202,673 |
| Total | 23,750 | 539,645 |
These data illustrate the substantial infrastructure supporting complex trial designs like Lung-MAP within the National Clinical Trials Network, highlighting the significant patient participation required for their successful execution.
Key Methodologies and Experimental Protocols
Biomarker-Driven Patient Screening
The Lung-MAP protocol employs comprehensive genomic profiling to assign patients to biomarker-matched sub-studies. The process begins with the collection of tumor tissue or use of available archival tissue, with blood samples also collected for circulating tumor DNA (ctDNA) analysis in some cases [27]. For Lung-MAP 3.0, the protocol accepts results from more than 40 commercial and academic next-generation sequencing (NGS) platforms, reflecting the integration of standardized genomic testing into routine clinical practice [26].
The genomic analysis focuses on identifying specific actionable driver mutations that correspond to investigational targeted therapies available within the trial's sub-studies. The screening platform simultaneously tests for multiple genetic alterations, including but not limited to KRAS G12C, STK11, MET, RET, and NTRK, among others. This multi-target approach enables efficient allocation of patients to appropriate therapeutic arms based on their tumor's molecular profile rather than histologic subtype alone.
Pragmatic and Streamlined Data Collection
Recent innovations in master protocols emphasize pragmatic design elements to enhance efficiency and generalizability. The S2302 Pragmatica-Lung trial, a related initiative within the Lung-MAP framework, demonstrates this approach through dramatically reduced data collection requirements compared to traditional phase 3 trials [28]. Key streamlining features include:
- Limited data elements collected at fewer timepoints using fewer submission forms
- Focused adverse event tracking limited to serious, unexpected, treatment-related events
- Elimination of mandatory specimen collection or imaging scans beyond standard of care
- Minimal eligibility criteria to enhance patient representativeness
This pragmatic approach reduces operational burden on clinical sites, enabling broader participation across community and academic settings while maintaining rigorous safety and efficacy assessment for regulatory evaluation.
Statistical Framework and Interim Analysis
Umbrella trials employ sophisticated statistical frameworks to efficiently evaluate multiple therapeutic questions. The Lung-MAP protocol incorporates adaptive design elements with planned interim analyses for futility and efficacy assessments. For instance, the S2302 Pragmatica-Lung trial included two planned interim analyses, with the second analysis leading to early reporting of results when futility criteria were met [28].
The analysis utilizes the hazard ratio of overall survival as the primary endpoint, with propensity score methods to adjust for baseline confounding factors in emulated trials using real-world data [29]. This approach enables continuous evaluation of treatment effects across biomarker-defined subgroups while controlling for multiple comparisons and maintaining statistical power.
Workflow and Signaling Pathways
Lung-MAP Umbrella Trial Workflow
The following diagram illustrates the comprehensive patient journey through the Lung-MAP umbrella trial, from screening to treatment assignment and outcomes analysis:
Biomarker-Treatment Matching Logic
The core intelligence of the Lung-MAP umbrella trial lies in its biomarker-treatment matching algorithm, which directs patients to appropriate therapeutic sub-studies based on their molecular profile:
Data Analysis Pipeline
The computational framework for analyzing umbrella trial data integrates multiple data sources and analytical approaches to generate insights into treatment efficacy across biomarker-defined subgroups:
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Materials and Platforms for Umbrella Trial Implementation
| Category | Specific Examples | Function in Umbrella Trials |
|---|---|---|
| Genomic Profiling Platforms | Foundation Medicine CDx, Guardant360, Tempus xT, Caris Molecular Intelligence | Comprehensive biomarker detection and validation for patient stratification to appropriate therapeutic sub-studies [26] |
| Data Management Systems | Electronic Data Capture (EDC) systems, Clinical Data Management Systems (CDMS) | Centralized data collection, quality control, and integration across multiple therapeutic sub-studies within the master protocol [30] |
| Bioinformatics Tools | Trial Pathfinder computational framework, Shapley value analysis | Evaluation of eligibility criteria effects on trial populations and outcomes using real-world data [29] |
| Statistical Software | R, SAS, Python with specialized survival analysis packages | Advanced statistical analyses including propensity score weighting, hazard ratio estimation, and interim monitoring [29] |
| Specimen Collection Kits | Blood collection tubes (cfDNA), tumor tissue preservation systems | Standardized biospecimen acquisition for central biomarker testing and correlative studies [27] |
| Clinical Outcome Assessments | RECIST criteria, patient-reported outcome (PRO) instruments, adverse event grading systems (CTCAE) | Standardized efficacy and safety endpoint measurement across all therapeutic sub-studies [28] |
Application Notes and Implementation Protocols
Eligibility Criteria Optimization
The implementation of umbrella trials requires careful consideration of eligibility criteria to balance patient safety with generalizability. Research using the Trial Pathfinder computational framework demonstrates that many common eligibility criteria have minimal effect on trial hazard ratios while significantly limiting patient accrual [29]. Analysis of 10 completed aNSCLC trials revealed that, on average, only 30% of patients who received the trial drugs in real-world practice would have met the original trial eligibility criteria, yet the hazard ratio for the broader population was often comparable or more favorable [29].
A data-driven approach to eligibility optimization involves:
- Systematic evaluation of each criterion's impact on cohort size and hazard ratio using real-world data
- Prioritization of safety-critical exclusions while removing arbitrary restrictions
- Validation of broadened criteria against safety databases to ensure acceptable risk profiles
This methodology can more than double the pool of eligible patients while maintaining comparable treatment effects, addressing the critical challenge of low clinical trial enrollment that affects approximately 80% of trials [29].
Site Engagement and Patient Accrual Strategies
Successful umbrella trial implementation requires engagement of diverse clinical sites, particularly community-based practices where most cancer patients receive treatment. The Lung-MAP model achieves this through:
- Streamlined site activation processes reducing administrative burden
- Integrated genomic screening using existing testing platforms familiar to clinicians
- Pragmatic data collection aligned with routine clinical practice
- Centralized regulatory support managing multiple investigational products under single IND
These strategies enable participation across more than 900 clinical sites for Lung-MAP, facilitating rapid patient accrual that reflects real-world demographics, with recent trials achieving 22% non-White, 13% Black, and 15% rural participant representation [28].
Correlative Science Integration
Umbrella trials provide unique opportunities for integrated correlative science through systematic biospecimen collection. The Lung-MAP protocol incorporates:
- Longitudinal blood collection for circulating tumor DNA analysis
- Tissue banking for biomarker discovery and validation
- Digital pathology applications using artificial intelligence algorithms
- Patient-reported outcome tracking for quality-of-life assessment
These rich datasets enable exploratory analyses, such as the examination of co-mutation effects on targeted therapy efficacy, as demonstrated in the S1900E sub-study where STK11 co-mutations were associated with reduced efficacy of sotorasib in KRAS G12C-mutated NSCLC [27].
Umbrella trials like Lung-MAP represent a transformative approach to oncology drug development, efficiently addressing multiple clinical questions within a unified master protocol framework. By leveraging biomarker-driven patient stratification, pragmatic operational elements, and sophisticated statistical designs, these trials accelerate therapeutic development while enhancing the generalizability of results to real-world patient populations.
The continued evolution of umbrella trial designs, exemplified by Lung-MAP 3.0's expanded genomic screening options, demonstrates the adaptability of this approach to changing clinical practice and scientific understanding. As precision medicine advances, umbrella protocols provide an essential infrastructure for evaluating targeted therapy combinations, understanding resistance mechanisms, and ultimately improving outcomes for molecularly defined patient subgroups across cancer types.
The I-SPY 2 trial (Investigation of Serial studies to Predict Your Therapeutic Response with Imaging and Molecular Analysis 2) represents a transformative approach in oncology clinical research, serving as a pioneering adaptive platform trial designed to accelerate drug development for high-risk breast cancer patients [31]. This neoadjuvant trial functions as a master protocol under which multiple investigational treatments are simultaneously evaluated against a shared standard of care control arm, thereby creating a more efficient and personalized clinical development pathway [31] [32]. The trial specifically enrolls women with high-risk, stage II/III breast cancer, utilizing extensive biomarker testing and an adaptive design with intermediate endpoints to rapidly identify effective novel agents and corresponding biomarker signatures [31] [32].
The fundamental innovation of I-SPY 2 lies in its adaptive randomization methodology, which uses accumulating data to preferentially assign patients to treatments that are showing promise within their specific biomarker subtype [31]. This approach stands in stark contrast to traditional clinical trials that often require large patient numbers, extended follow-up periods, and fail to account for the molecular heterogeneity of breast cancer, ultimately resulting in a costly and inefficient drug development process [31]. By targeting rapid, focused development of promising agents and matching them to patient subtypes most likely to benefit, I-SPY 2 aims to bring more precise treatment options to breast cancer patients while minimizing exposure to ineffective therapies [31].
Core Methodology and Experimental Protocols
Trial Design and Structure
I-SPY 2 operates as an ongoing, multicenter, open-label, adaptive phase 2 platform trial with multiple experimental groups evaluating new agents combined with standard neoadjuvant therapy [31]. The trial employs a master protocol framework that allows for the continuous evaluation of multiple investigational regimens against a shared control arm, with the ability to add new agents as others graduate or are dropped for futility [31] [32]. This creates an efficient, perpetual testing environment that can rapidly adapt to emerging scientific evidence.
Table 1: Key Eligibility Criteria for I-SPY 2
| Criterion | Requirement |
|---|---|
| Disease Stage | Clinical stage II or III breast cancer |
| Tumor Size | ≥2.5 cm in diameter by imaging or physical exam |
| Age & Performance Status | >18 years with ECOG performance status 0-1 |
| Molecular Risk | MammaPrint High Risk for HR+HER2- disease [33] |
| Prior Therapy | No prior chemotherapy, radiation, or biologic therapy for current breast cancer |
All patients receive a standard neoadjuvant backbone of weekly paclitaxel for 12 weeks, followed by dose-dense doxorubicin and cyclophosphamide every 2-3 weeks for 4 cycles [31]. Patients with HER2-positive disease also receive trastuzumab during the paclitaxel phase, with pertuzumab added following its accelerated approval [31]. In experimental arms, investigational drugs are added to the standard paclitaxel regimen during the initial 12-week treatment phase.
Bayesian Adaptive Randomization Protocol
The statistical engine of I-SPY 2 utilizes Bayesian adaptive randomization to dynamically assign patients to treatment arms based on accumulating response data. The methodology operates through several key mechanisms. First, breast cancer is classified into 10 molecular subtypes based on hormone receptor status, HER2 status, and the 70-gene MammaPrint assay [31]. The algorithm continuously updates the probability of pathological complete response for each experimental treatment within each biomarker signature as patient outcome data accumulates. Patients are then randomized to available arms with probabilities proportional to the performance of each treatment within their specific biomarker subtype, preferentially assigning patients to treatments showing higher efficacy for their cancer subtype [31].
The adaptive process follows predefined decision rules: when an agent demonstrates a ≥85% Bayesian predictive probability of success in a future 300-patient phase 3 trial for any biomarker signature, it "graduates" from the platform [31]. Conversely, if this probability falls below 10% for all biomarker signatures, the agent is dropped from the trial for futility [31]. This continuous learning and adaptation system ensures that the trial efficiently identifies promising treatments while minimizing patient exposure to ineffective therapies.
Endpoint Assessment and Biomarker Evaluation
The primary endpoint for I-SPY 2 is pathological complete response, rigorously defined as the absence of invasive cancer in both the breast and lymph nodes at surgical resection following neoadjuvant therapy [31] [33]. This endpoint serves as a validated surrogate for long-term survival outcomes and enables more rapid evaluation of treatment efficacy compared to traditional time-to-event endpoints [31].
The trial incorporates comprehensive biomarker assessment through multiple modalities. Serial magnetic resonance imaging scans are obtained at enrollment, week 3, week 12, and before surgery to assess tumor volume changes and predict likelihood of pCR [31]. Multiple tumor biopsies are collected before, during, and after treatment for extensive molecular profiling, including gene expression analysis (e.g., MammaPrint, ImPrint classifier), protein signaling pathway assessment, and immune microenvironment characterization [31] [33] [34]. These biospecimens undergo centralized processing and analysis in CLIA-certified laboratories under Investigational Device Exemption from the FDA to ensure regulatory standards [33].
Key Analytical Frameworks and Signaling Pathways
Biomarker-Driven Patient Stratification
I-SPY 2 has pioneered the development and validation of several biomarker frameworks for therapeutic stratification. The ImPrint classifier is a 53-gene expression-based immune response predictor that identifies patients with hormone receptor-positive/HER2-negative breast cancer who are likely to respond to immunotherapy [33]. This FDA IDE-enabled assay demonstrated remarkable predictive capacity, with ImPrint+ HR+HER2- patients achieving a 75% pCR rate to IO-containing regimens compared to only 17% in ImPrint- patients [33].
The ecotype classification system represents another innovative approach, deconvoluting transcriptomic data into 10 multicellular organization systems within the tumor microenvironment [35]. Research has identified CE9 (a pro-inflammatory ecotype) as predictive of pCR across multiple treatment arms, while CE2 (a basal-enriched ecotype) specifically predicts response to durvalumab plus olaparib combination therapy [35].
Table 2: Performance of Predictive Biomarkers in I-SPY 2
| Biomarker | Patient Population | pCR Rate in Positive Patients | pCR Rate in Negative Patients | Odds Ratio |
|---|---|---|---|---|
| ImPrint+ | HR+HER2- to IO | 75% | 17% | 14.5 [33] |
| CE9 Ecotype | All-comers to Pembrolizumab | OR=2.07 | - | - [35] |
| CE2 Ecotype | All-comers to Durvalumab+Olaparib | OR=3.22 | - | - [35] |
| MP2 (MammaPrint) | HR+HER2- to IO | 56% | - | <7.5 [33] |
Protein Signaling Pathway Analysis
Functional protein pathway activation mapping using reverse phase protein array (RPPA) technology has provided critical insights into therapy resistance and sensitivity mechanisms [34]. This methodology involves laser capture microdissection of tumor tissue followed by quantitative expression analysis of 139 proteins and phosphoproteins to identify predictive signatures [34].
Key resistance biomarkers identified through this approach include elevated levels of cyclin D1, estrogen receptor alpha, and androgen receptor S650, which associate with global non-response across multiple therapy classes [34]. The HARPS (HER2 Activation Response Predictive Signature) framework has further enabled stratification of triple-negative breast cancer patients likely to respond to either HER2-targeted or immune checkpoint therapies based on underlying protein activation states [34].
I-SPY 2 Adaptive Platform Trial Workflow
Research Reagent Solutions and Essential Materials
The successful implementation of I-SPY 2's complex biomarker-driven methodology relies on a standardized toolkit of research reagents and analytical platforms. The following table details key reagents and their applications within the trial context.
Table 3: Essential Research Reagents and Platforms for Adaptive Platform Trials
| Reagent/Platform | Function/Application | Specifications |
|---|---|---|
| MammaPrint 70-Gene Assay | Molecular risk stratification using FFPE or fresh frozen tumor tissue | 70-gene signature, Agilent microarray platform, identifies High1/High2 risk categories [31] [33] |
| ImPrint Classifier | Immune response prediction for immunotherapy selection | 53-gene expression signature, FDA IDE-enabled, identifies IO-sensitive patients in HR+HER2- disease [33] |
| Reverse Phase Protein Array (RPPA) | Functional protein signaling pathway mapping | Quantitative analysis of 139 proteins/phosphoproteins, laser capture microdissected tissue [34] |
| Agilent 32K Gene Expression Arrays | Comprehensive transcriptomic profiling | Platform: Agilent 32K (Agendia32627DPv1.14SCFGplus), CLIA-certified laboratory [33] |
| Ecotype Classification Algorithm | Tumor microenvironment ecosystem analysis | Machine learning-based classification into 10 multicellular organization systems [35] |
Results and Clinical Implementation
Graduated Agents and Biomarker Signatures
The I-SPY 2 platform has demonstrated remarkable success in identifying promising therapeutic regimens for specific biomarker-defined populations. To date, seven agents have graduated from the trial, including neratinib, veliparib/carboplatin, MK2206, pertuzumab, T-DM1+pertuzumab, and pembrolizumab [31] [32]. Each graduation was supported by a specific biomarker signature predicting enhanced probability of response.
The trial has also efficiently identified agents unlikely to succeed, with several treatments dropped for futility when Bayesian probabilities fell below the prespecified threshold [31] [32]. This demonstrates the adaptive platform's utility not only in identifying successful treatments but also in rapidly terminating development of ineffective therapies, thereby conserving research resources and preventing patient exposure to unpromising treatments.
Clinical Translation and Regulatory Impact
The I-SPY 2 model has significantly influenced oncology drug development and regulatory science. The trial has established pCR as a validated surrogate endpoint in neoadjuvant breast cancer, enabling accelerated drug evaluation and approval [31]. Furthermore, the biomarker signatures identified through the trial have informed subsequent phase 3 trial designs and patient selection strategies, increasing the efficiency of confirmatory development programs [33].
The integration of novel biomarker assays like ImPrint into clinical decision-making represents a paradigm shift toward more personalized therapy selection [33]. The demonstration that specific HR+HER2- subsets (ImPrint+) achieve pCR rates exceeding 75% with immunotherapy challenges traditional subtype-based treatment boundaries and enables more precise allocation of potentially toxic therapies [33].
Multimodal Biomarker Integration Framework
Discussion and Future Directions
The I-SPY 2 adaptive platform trial represents a fundamental advancement in oncology clinical research methodology, demonstrating the feasibility and utility of master protocols with Bayesian adaptive randomization. By simultaneously evaluating multiple therapeutic agents against a shared control arm and using accumulating data to inform patient assignment, this model significantly accelerates the identification of effective treatments for biomarker-defined patient subsets [31].
Future iterations of the platform, including I-SPY 2.2, continue to refine this approach by incorporating more sophisticated biomarker-guided treatment assignment and expanding the repertoire of targeted and immunotherapeutic agents [33]. The integration of novel analytical frameworks such as carcinoma ecotyping and protein activation signatures provides increasingly granular understanding of therapy resistance and sensitivity mechanisms [34] [35].
The I-SPY model offers a blueprint for modern oncology drug development, potentially applicable across multiple cancer types. Its success in balancing statistical rigor with operational flexibility, while maintaining rigorous safety monitoring through an independent DSMB, demonstrates that adaptive platform trials can successfully navigate the complex regulatory landscape while bringing more effective treatments to patients in need [31] [32]. As precision medicine continues to evolve, the principles established by I-SPY 2 will undoubtedly inform the next generation of master protocol designs across oncology and beyond.
Master protocols represent a transformative approach in clinical research, enabling the coordinated and efficient evaluation of multiple investigational questions within a unified trial structure. Defined as protocols designed with multiple sub-studies to evaluate one or more investigational drugs or disease subtypes, they are primarily categorized into basket, umbrella, and platform trials [1]. While traditionally applied to pharmaceutical development, the conceptual framework of master protocols offers significant potential for accelerating the validation of complex therapeutic oncology devices such as the Magnetic Resonance-Linear Accelerator (MR-Linac) systems. The MR-Linac, which integrates real-time magnetic resonance imaging with a linear accelerator, exemplifies the type of innovative technology that can benefit from this efficient trial design paradigm [36]. This article explores the integration of master protocol principles with MR-Linac technology, providing detailed application notes and experimental protocols to guide researchers in this emerging field.
Master protocol trials are inherently complex due to their expansive scope and varied components. The three primary designs share a common goal of research efficiency but differ fundamentally in structure and application, as summarized in Table 1.
Table 1: Comparative Overview of Master Protocol Trial Designs
| Design Feature | Basket Trial | Umbrella Trial | Platform Trial |
|---|---|---|---|
| Core Concept | Tests a single investigational drug or drug combination in different disease populations [2] [1] | Evaluates multiple investigational drugs in a single disease population [2] [1] | Flexible design allowing arms to be dropped or added based on interim results [1] |
| Patient Stratification | Based on different cancers, disease stages, histologies, or biomarker status [1] | Typically based on specific molecular markers within a single cancer type [2] | Can adapt stratification criteria as trial progresses and new information emerges |
| Structural Flexibility | Limited - assesses one intervention across multiple baskets | Moderate - tests multiple drugs simultaneously but within fixed structure | High - enables continuous evolution of trial arms [1] |
| Primary Application Context | Often applied in oncology (84% of surveyed master protocols) [2] | Primarily used in oncology [2] | Emerging applications in infectious diseases, neuroscience, and rare diseases [2] |
A 2021 survey by the American Statistical Association Biopharmaceutical Section revealed that 79% of participating organizations had master protocols in planning or implementation, with the majority (54%) in oncology [2]. This demonstrates the growing acceptance of these efficient trial designs in modern drug development, particularly in precision oncology where patient populations are often limited.
MR-Linac Technology in Oncology: Technical Foundations
Magnetic resonance-guided radiotherapy (MRgRT) represents a paradigm shift in radiation oncology by enabling real-time visualization of tumors and surrounding tissues during treatment delivery. The two most established MR-Linac platforms are the Elekta Unity (1.5T MRI with 7 MV flattening filter-free linac) and the ViewRay MRIdian (0.35T MRI with linac) [36]. These systems provide continuous cine-MRI during treatment, allowing clinicians to visualize and track tumor motion in real-time, a capability particularly advantageous for lung cancers where respiratory-induced motion significantly affects target positioning [36].
The cornerstone of MRgRT is online adaptive radiotherapy (ART), which allows clinicians to modify treatment plans daily based on changes in tumor size, position, and surrounding anatomy observed via MR imaging [36]. This is achieved through online MR imaging, contouring based on the "anatomy of the day," and re-optimization while the patient remains on the treatment table. Clinical implementation of online ART has demonstrated the ability to reduce planning target volume margins and spare organs at risk more effectively than non-adaptive approaches [36].
Integrating Master Protocols with MR-Linac Clinical Development
Platform Trial Design for MR-Linac Application Optimization
The platform trial structure offers particular promise for evaluating multiple MR-Linac applications or treatment protocols within a unified framework. This design enables the efficient comparison of MRgRT against conventional radiotherapy techniques while simultaneously exploring different tumor types, fractionation schemes, or adaptive protocols.
Table 2: Clinical Outcomes of MR-Guided Adaptive Radiotherapy in Lung Cancer
| Study (Year) | Patient/Tumor Characteristics | Treatment Protocol | Key Clinical Outcomes |
|---|---|---|---|
| Finazzi et al. [36] | 25 patients with peripheral lung lesions | Stereotactic MR-guided adaptive radiation therapy (SMART) using gated breath-hold | PTV volumes reduced to 53.7% of ITV-based volumes from 4DCT; prescription dose coverage improved from 92.1% to 95.0% with adaptation |
| Regnery et al. [36] | 16 ultracentral lung tumors (ULT) | SMART with online ART in 91% of fractions | 2-year local progression rate of 7%; overall survival rate of 67% at median follow-up of 23.6 months |
| Single-Institution Retrospective [36] | 64 patients with 92 lung tumors (80.4% peripheral) | SMART for primary tumors and lung oligometastases | 1-year and 3-year local progression-free survival rates of 96.3% and 86.4% respectively without ≥grade 3 toxicity |
Experimental Protocol: SMART for Lung Tumors
The Stereotactic MR-guided Adaptive Radiation Therapy (SMART) approach represents a specific protocol successfully implemented for lung tumors [36]. The following detailed methodology outlines the key procedural steps:
Patient Selection and Staging: Enroll patients with either early-stage non-small cell lung cancer (NSCLC) unsuitable for surgery or patients with pulmonary oligometastases. Tumor centrality should be classified according to RTOG 0813 criteria, with ultracentral tumors (ULT) defined as those where the gross tumor volume directly abuts the proximal bronchial tree or trachea [36].
Simulation and Baseline Planning: Acquire a 4DCT simulation scan for initial assessment of tumor motion. Generate an internal target volume (ITV) based on the 4DCT dataset. Create an initial reference plan on the simulation CT, defining appropriate dose constraints for organs at risk (OARs) including spinal cord, esophagus, brachial plexus, and healthy lung tissue.
Daily Treatment Delivery with Online Adaptation: a. Patient Setup and Initial Imaging: Position the patient on the MR-Linac couch using appropriate immobilization devices. Acquire a volumetric MRI for assessment of the day's anatomy. b. Contour Adaptation: Adapt the target volume (GTV) and critical OAR contours to the daily MRI anatomy. AI-powered auto-contouring algorithms may be employed to expedite this process [36]. c. Plan Re-optimization: Generate a new treatment plan based on the adapted contours. For gated treatments, define the gating boundaries based on the real-time cine-MRI. d. Dose Evaluation and Approval: Evaluate the adapted plan using the same objectives and constraints as the reference plan. Ensure the adapted plan meets all clinical goals before proceeding. e. Treatment Delivery with Continuous Monitoring: Deliver the treatment while monitoring the tumor position in real-time using cine-MRI. Utilize automatic beam gating to ensure radiation is delivered only when the tumor is within the predefined target boundary [36].
Response Assessment and Follow-up: Schedule regular follow-up visits with functional imaging, such as diffusion-weighted MRI, to assess tumor response and identify potential radiation-induced changes.
Figure 1: SMART Workflow for Lung Tumors - This diagram illustrates the step-by-step protocol for Stereotactic MR-guided Adaptive Radiation Therapy, highlighting the cyclic nature of daily adaptation.
Implementation Framework and Research Toolkit
Key Research Reagent Solutions and Essential Materials
Table 3: Essential Research Materials and Tools for MR-Linac Master Protocol Implementation
| Item/Category | Function/Application | Implementation Notes |
|---|---|---|
| MR-Linac Systems | Delivery of radiation with simultaneous MR imaging for real-time adaptation | Elekta Unity (1.5T) or ViewRay MRIdian (0.35T); enables continuous cine-MRI during treatment [36] |
| AI-Powered Auto-Contouring Algorithms | Automated segmentation of targets and OARs on daily MRI | Reduces contouring time during online ART; requires validation for specific disease sites [36] |
| Data Management Platform | Integration and processing of large, complex datasets from multiple trial arms | Must handle dynamic dataset from platform trials with real-time integration capabilities [1] |
| Biomarker Data Specifications | Standardized processing of genomic and radiomic data | Early establishment of data transfer specifications is critical; requires collaboration with biomarker specialists [1] |
Statistical and Operational Considerations for Device-Focused Master Protocols
Implementing master protocols for therapeutic devices presents unique challenges distinct from pharmaceutical applications. Key considerations include:
Complex Statistical Analysis Plans: Account for adaptive features, multiplicity issues from multiple comparisons, and potential Bayesian methods. The number of tables, figures, and listings can grow significantly, requiring careful prioritization to prevent data overload [1].
Dynamic Data Management: Platform trials continuously add new treatment arms, generating a dynamic dataset that requires robust systems capable of handling evolving data structures and ensuring consistency across various cohorts [1].
Regulatory Engagement Strategy: Different regulatory agencies may have varying requirements for master protocol trials, particularly when the purpose is regulatory registration for devices. Early and frequent engagement is recommended [2].
Clinical Study Report Strategy: Decision on single versus multiple CSRs should be defined sufficiently early in the protocol development process, considering that each cohort may follow different timelines [1].
Figure 2: Platform Trial Structure for MR-Linac - This diagram visualizes a flexible platform trial design evaluating multiple MR-Linac applications simultaneously, with the capability to adapt arms based on interim analyses.
The integration of master protocol designs with therapeutic oncology devices like MR-Linac represents a promising frontier in clinical research methodology. This approach leverages the efficiency of coordinated trial structures to accelerate the validation of complex radiotherapy technologies that enable personalized, adaptive treatment. The framework presented herein provides researchers with practical application notes and detailed protocols to implement these innovative designs. As MRgRT technology continues to evolve, its integration with master protocols, functional imaging, radiomics, and AI-driven adaptive strategies is expected to expand its applications beyond current limitations, ultimately advancing precision oncology through more efficient clinical validation pathways.
Navigating Challenges and Optimizing Performance in Master Protocol Studies
Oncology clinical trials are pivotal for advancing cancer treatment, yet their operational complexity often hinders successful execution. Within the framework of master protocol designs—which evaluate multiple treatments, patient populations, or questions under a single protocol—efficient ecosystem coordination becomes even more critical. These sophisticated trial designs amplify common challenges, including patient recruitment, complex data management, and stringent regulatory adherence. This document provides detailed application notes and protocols to help researchers, scientists, and drug development professionals identify and overcome these operational hurdles. By integrating strategic planning, innovative technologies, and collaborative models, teams can enhance the integrity, efficiency, and overall success of oncology clinical trials.
The following table synthesizes key operational challenges in oncology clinical trials, derived from recent multicentric studies and industry analyses, and pairs them with evidence-based strategies for mitigation.
Table 1: Common Operational Barriers and Corresponding Mitigation Strategies
| Operational Barrier | Proposed Mitigation Strategy | Key Outcome / Impact |
|---|---|---|
| Patient Recruitment & Retention [37] [38] | Proactive referral network engagement (e.g., with gynecologists); Culturally relevant materials; Flexible visit scheduling [37] [38]. | Shortened recruitment period; Improved retention rates [37]. |
| Regulatory Delays [37] [38] | Early and proactive regulatory engagement; Centralized regulatory teams; Precise documentation [37] [38]. | Avoided delays of up to four months; Streamlined approval process [37]. |
| Complex Protocol Management [38] | Comprehensive site and investigator training; Feasibility-driven protocol simplification [38]. | Reduced protocol deviations; Smoother trial implementation [38]. |
| Data Management & Quality [37] [38] | Hybrid monitoring (remote & on-site); Advanced EDC & analytics; Centralized imaging review [37] [38]. | Upheld data integrity across sites; Enabled real-time oversight [37] [38]. |
| Vendor & Resource Management [37] [38] | Strategic mix of global and local vendors; Prudent negotiation; Robust financial planning and FSP models [37] [38]. | Cost optimization; On-budget trial completion [37] [38]. |
| Geographic & Diversity Disparities [39] [38] | Cultural competency training; Multiregional trial design inclusive of local contexts; DEI-integrated site selection [38] [40]. | Improved recruitment for rare cancers; Enhanced equity and generalizability [38] [40]. |
Experimental Protocols for Key Operational Areas
Protocol for Accelerated Patient Recruitment and Retention
Objective: To establish a systematic methodology for enhancing patient recruitment and minimizing loss-to-follow-up in oncology trials, particularly within complex master protocols.
Background: Slow enrollment and patient dropout significantly delay trial timelines and compromise data integrity. A multifaceted, patient-centric approach is required [37] [38].
Materials:
- Referral network database (e.g., specialist physicians, professional associations)
- Culturally adapted patient education materials
- Digital platform for patient engagement and scheduling
- Budget for travel reimbursement and incentives
Methodology:
- Pre-Site Activation:
- Conduct a feasibility assessment to identify sites with access to the target patient population and investigateur interest in the treatment paradigm [37].
- Integrate patient advocacy group feedback into protocol and consent form design.
- Referral Network Activation:
- Patient-Centric Enrollment:
- Retention and Follow-up:
Protocol for Integrated Data Management and Quality Assurance
Objective: To ensure data integrity and quality in oncology trials through a hybrid monitoring approach and advanced data capture technologies.
Background: The volume and complexity of data in oncology trials, including biomarker and imaging data, necessitate robust quality control systems to prevent inaccuracies that can jeopardize analysis [37] [38].
Materials:
- Electronic Data Capture (EDC) system
- Risk-Based Monitoring (RBM) platform
- Centralized imaging review system
- Independent Data Safety Monitoring Board (DSMB)
Methodology:
- System Interoperability:
- Hybrid Monitoring Plan:
- Combine centralized, remote source data verification with targeted, periodic on-site monitoring visits [37].
- Use a risk-based approach to focus monitoring resources on critical data points and high-risk sites.
- Endpoint Adjudication:
- Establish a centralized, blinded imaging core lab to consistently assess tumor response per RECIST criteria across all sites [37].
- Oversight and Review:
- Facilitate continuous communication with the independent DSMB, providing unblinded data for ongoing safety and efficacy reviews [37].
Visualization of Operational Workflows
Ecosystem Coordination for Master Protocols
Patient Stratification in Biomarker-Driven Trials
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Technologies for Modern Oncology Trials
| Item / Technology | Function / Application in Oncology Trials |
|---|---|
| Liquid Biopsy Kits (ctDNA) | For minimally invasive biomarker analysis, monitoring Minimal Residual Disease (MRD), and real-time patient stratification in adaptive trial designs [40]. |
| Electronic Data Capture (EDC) Systems | Centralized platforms for efficient and accurate collection and management of clinical trial data from multiple sites [38]. |
| EHR-to-EDC Automation Tools | Technology that automates data transfer from site-based Electronic Health Records to the trial's EDC, reducing site staff burden and improving data speed/accuracy [41]. |
| Validated Biomarker Assays (NGS, IHC) | Essential for analyzing tissue and blood samples to identify patient subgroups based on genetic mutations or protein expression, as required by master protocols [40]. |
| Interactive Web Response System (IWRS) | Manages patient randomization and drug inventory supply across the clinical trial network, integrated with the EDC for seamless data flow [37]. |
| Centralized Imaging Review Platform | Ensures consistent, unbiased assessment of tumor response per standardized criteria (e.g., RECIST) across all trial sites, upholding endpoint integrity [37]. |
| AI-Powered Pathological Assessment Tools | Leverages artificial intelligence to assist in the objective and rapid analysis of pathology samples, such as HER2 scoring, improving consistency [40]. |
The pursuit of scientific rigor in oncology clinical trials, particularly within master protocol frameworks, often leads to increasing design complexity. This complexity, while aimed at obtaining more precise and generalizable data, can paradoxically undermine the very studies it seeks to strengthen by creating significant barriers to patient recruitment and retention. Master protocols, which evaluate multiple therapies or disease subgroups within a single overarching structure, inherently introduce operational challenges that must be consciously balanced against their scientific ambitions. This application note examines this critical paradox and provides evidence-based protocols to optimize this balance, ensuring that complex designs do not compromise trial viability and that scientific innovation translates successfully into clinical practice.
Quantifying the Challenge: Data on Recruitment and Retention
Robust quantitative data is essential for understanding the current landscape of clinical trial efficiency and the impact of design complexity. The following tables synthesize recent findings on trial participation metrics and the primary barriers affecting recruitment and retention.
Table 1: Participant Engagement and Outcomes from Recent Oncology ECHO Programs [42]
| Program Characteristic | Program A | Program B | Program C | Program D | Aggregate (n=431) |
|---|---|---|---|---|---|
| Cancer Focus | Lung | Colorectal | Prostate | All | - |
| Primary Topic | Prevention | Screening | Screening | Caregiving | - |
| Program Length | 4 months | 7 months | 9 months | 7 months | - |
| Number of Sessions | 4 | 7 | 9 | 7 | 27 total |
| Unique Participants | 195 | 45 | 59 | 132 | 108 (Average) |
| Participants Planning to Use Information (within 1 month) | - | - | - | - | 59% |
| Mean Increase in Knowledge (5-point scale) | - | - | - | - | +0.84 |
| Mean Increase in Confidence (5-point scale) | - | - | - | - | +0.77 |
Table 2: Common Challenges and Impact on Oncology Trial Participation [43] [44]
| Challenge Category | Specific Challenge | Impact on Trial Participation |
|---|---|---|
| Logistical & Financial | Frequent travel requirements | Physical and emotional exhaustion for patients [43] |
| Financial strain (transportation, accommodation, missed work) | Creates prohibitive burden, especially for lower-income patients [43] | |
| Geographical barriers | Limits access for patients in rural or underserved areas [43] | |
| Clinical & Personal | Treatment side effects and burden | Difficulty staying engaged due to physical toll of treatment [43] |
| Lack of personalized support | Patients feel lost navigating the complex trial process [43] | |
| Communication & Design | Lack of clear communication | Patients feel uninformed and hesitant to continue [43] |
| Complex consent forms and unclear expectations | Discourages initial participation and ongoing engagement [44] | |
| Patient-unfriendly technologies | Raises privacy or safety concerns, acting as a barrier [44] |
Experimental Protocols for Optimized Trial Design
To address the challenges quantified above, the following protocols provide structured methodologies for integrating key stakeholder feedback and decentralized approaches into trial design.
Protocol 1: The Trifecta Collaborative Protocol Review
This protocol provides a framework for integrating feedback from patients, sites, and sponsors during the critical protocol design phase to preemptively identify and mitigate feasibility issues [45].
Methodology:
- Stakeholder Recruitment and Preparation:
- Patients: Recruit 8-12 participants representing the target disease population, ensuring diversity in disease stage, treatment history, and demographic background. Compensate them appropriately for their expertise and time [45]. Prepare simplified protocol materials for review.
- Sites: Identify 5-8 experienced research coordinators, clinical trial nurses, and principal investigators from both academic and community settings. Provide them with the full protocol and case report forms (CRFs).
- Sponsors: Assemble a cross-functional team including clinical science, regulatory, operations, and data management.
- Structured Feedback Sessions:
- Conduct separate, focused workshops with patient and site groups to foster open feedback.
- Use guided questionnaires targeting specific protocol elements: visit frequency and duration, procedural burden, clarity of instructions, consent form readability, and logistical requirements.
- Patient-Centric Questions: "How would the proposed visit schedule interact with your caregiving responsibilities?" "Are the potential side effects described in a way you can understand?" [45].
- Site-Centric Questions: "Are the data collection points sustainable with current staffing?" "Are the visit windows clinically realistic?" [45].
- Insight Integration and Protocol Refinement:
- Synthesize feedback into a structured report, highlighting points of convergence between patient and site perspectives.
- The sponsor team leads a protocol revision session, prioritizing changes that reduce burden without compromising scientific integrity (e.g., spacing consecutive-day visits, simplifying procedures, clarifying language) [45].
- Feedback Loop:
- Communicate back to patient and site reviewers how their input shaped the final protocol, closing the loop and building trust for future collaboration [45].
Protocol 2: Integrated Decentralized Clinical Trial (DCT) Feasibility Assessment
This protocol outlines a systematic approach for evaluating which trial procedures can be decentralized to reduce participant burden, a key strategy for improving retention [43] [44].
Methodology:
- Procedure Mapping and Burden Scoring:
- Create a comprehensive matrix of all procedures outlined in the schedule of assessments.
- For each procedure, score it (on a scale of 1-5) on two axes: a) Patient Burden (time, invasiveness, discomfort, travel requirement) and b) Site-Centric Complexity (need for specialized equipment, required personnel expertise, regulatory overhead) [46].
- Remote Feasibility Evaluation:
- For procedures with high patient burden scores (e.g., routine blood draws, patient-reported outcome surveys, vital signs monitoring), assess the feasibility of remote execution.
- Evaluate technologies and services for home-based care, including mobile phlebotomy services, electronic Clinical Outcome Assessment (eCOA) platforms, and wearable devices for remote monitoring [43].
- Validate that remote processes meet data integrity and regulatory standards.
- Hybrid Model Design:
- Design a hybrid trial model that strategically replaces specific high-burden, low-complexity site visits with remote alternatives.
- Clearly define which visits require in-person procedures (e.g., complex imaging, drug infusions) and which can be conducted virtually or via home health visits [43].
- Implementation and Support Plan:
- Develop a comprehensive support plan for decentralized elements, including:
- Technology Kits: Provision of necessary devices (e.g., tablets, wearables) to participants with limited access.
- Training: Clear instructions and 24/7 technical support for participants and site staff [43].
- Patient Concierge: Dedicated support for coordinating travel and accommodation for remaining essential site visits, further reducing logistical friction [43].
- Develop a comprehensive support plan for decentralized elements, including:
Visualizing Strategic Workflows
The following diagrams illustrate the core workflows and logical relationships for the protocols described above, providing a clear visual guide for implementation.
Figure 1: This workflow outlines the sequential and collaborative process of the Trifecta Collaborative Protocol Review, highlighting the distinct but complementary inputs from patients, sites, and sponsors [45].
Figure 2: This decision tree logic guides the assessment of which clinical trial procedures are suitable for decentralization, helping to systematically reduce patient burden without compromising data quality [43] [44].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successfully implementing complex master protocols requires not only strategic frameworks but also a suite of practical tools and technologies. The following table details key solutions for managing this complexity.
Table 3: Key Reagent Solutions for Modern Oncology Trials [40] [43] [44]
| Solution Category | Specific Tool/Technology | Function in Trial Execution |
|---|---|---|
| Biomarker & Monitoring | Circulating Tumor DNA (ctDNA) & Liquid Biopsies | Enables minimally invasive, real-time monitoring of minimal residual disease (MRD) and treatment response for dynamic patient stratification within master protocols [40]. |
| Data & Analytics | Artificial Intelligence (AI) Models | Assists in patient identification and trial matching to reduce screen failures; can automate tasks like biomarker assessment from images to increase site efficiency [40]. |
| Participant Support | Dedicated Patient Concierge & Navigator Services | Provides 24/7 personalized support for travel logistics, accommodation, and trial process navigation, directly mitigating key barriers to participation and retention [43]. |
| Trial Infrastructure | Decentralized Clinical Trial (DCT) Platforms | Integrates telemedicine, electronic consent (eConsent), home health visits, and wearable sensors to reduce the frequency and burden of site visits [43] [44]. |
| Participant Engagement | Patient-Friendly Materials & Social Media Campaigns | Uses clear, jargon-free language in consent forms and targeted media outreach to raise awareness, improve understanding, and support recruitment from diverse populations [44]. |
| Site Enablement | Clinical Trial Management System (CTMS) with Integrated Budgeting | Harmonizes the study calendar with financials from the Medicare Coverage Analysis (MCA) to streamline site activation, budgeting, and operational management [46]. |
The complexity paradox in oncology master protocols is not insurmountable. By consciously adopting a balanced, strategic approach that prioritizes operational feasibility and the human experience of trial participation, sponsors can design robust studies that are also executable. The quantitative data, structured protocols, visual workflows, and practical toolkit provided herein offer a roadmap for achieving this balance. Integrating stakeholder feedback proactively, leveraging technology to decentralize procedures, and providing dedicated participant support are no longer optional enhancements but essential components for the successful execution of the next generation of oncology clinical trials.
The development of novel oncology therapeutics is a complex, high-stakes endeavor. Two pillars have emerged as critical for de-risking this journey and accelerating the delivery of new treatments to patients: early and ongoing regulatory engagement and strategic participation in collaborative consortia. When executed within the framework of master protocol designs, these approaches provide a structured methodology for evaluating multiple questions in parallel, enhancing operational efficiency, and strengthening the evidence base for regulatory decision-making. This document outlines application notes and detailed protocols for implementing these best practices, providing researchers, scientists, and drug development professionals with actionable strategies for successful oncology clinical trials.
The Critical Role of Early and Ongoing Regulatory Engagement
Engaging with regulatory agencies early in the drug development process is not merely a procedural step but a strategic investment that can shape the entire development pathway. Proactive engagement aligns sponsor and regulator expectations, identifies potential issues before they become costly obstacles, and builds the collaborative relationship necessary for navigating complex review processes.
Quantitative Benefits of Early Regulatory Engagement
The following table summarizes key quantitative and strategic benefits of early regulatory engagement, as evidenced by industry practice and regulatory guidance.
Table 1: Value of Early Regulatory Engagement in Oncology Development
| Aspect | Impact of Early Engagement | Evidence/Mechanism |
|---|---|---|
| Program Timeline | Shortens NDA/BLA approval timeline from historical 33-36 months to significantly shorter periods [47] | Real-time reviews over secure portals and fast-track programs [47] |
| Development Cost | Avoids costly protocol revisions and major redesigns late in development [47] | Pre-IND meetings help reshape clinical trial design to meet efficacy endpoints early [47] |
| Regulatory Risk | Reduces risk of clinical hold and identifies unnecessary studies [48] | Obtaining agreement that FDA lacks substantive concerns with conducted and planned studies [48] |
| Approval Probability | Fosters better odds for approval when the time comes [47] | Continued conversations show engagement and build collaborative relationship with agencies [47] |
| Global Expansion | Facilitates simultaneous submission and review across international partners [47] | Mechanisms like FDA's Project Orbis streamline multinational approvals [47] |
Protocol: Strategic Framework for Early Regulatory Interactions
This protocol provides a detailed methodology for planning and executing effective early regulatory interactions throughout the drug development lifecycle.
2.2.1 Pre-Submission Phase (3-6 Months Before Regulatory Meeting)
- Objective: Establish comprehensive understanding of regulatory landscape and prepare robust briefing package.
- Procedure:
- Landscape Analysis: Conduct systematic review of relevant FDA guidance documents, including:
- Internal Alignment: Address fundamental development questions:
- Briefing Package Preparation: Develop concise data summaries (not detailed data sets) that:
2.2.2 Meeting Execution Phase
- Objective: Facilitate productive dialogue and obtain clear regulatory guidance.
- Procedure:
- Team Composition: Include regulatory affairs, clinical development, nonclinical, and CMC experts.
- Discussion Focus: Seek agreement on:
- Documentation: Designate dedicated note-taker to capture nuances and specific recommendations beyond official minutes.
2.2.3 Post-Meeting Integration Phase
- Objective: Implement feedback and maintain engagement momentum.
- Procedure:
- Response Development: Create detailed response letter addressing all agency questions and suggestions.
- Regulatory Roadmap Update: Integrate feedback into living regulatory strategy document including:
- Ongoing Engagement Plan: Schedule follow-up interactions and maintain regular updates to ensure ongoing compliance [47].
Workflow Visualization: Early Regulatory Engagement Process
The following diagram illustrates the continuous, iterative process of effective regulatory engagement:
Collaborative Consortia in Oncology Clinical Research
Oncology consortia represent a paradigm shift in how clinical research is conducted, bringing together multiple stakeholders to address complex scientific questions that individual organizations cannot solve alone. These collaborative networks are particularly valuable in the context of master protocols, where they provide the operational infrastructure and scientific expertise necessary for successful execution.
Landscape of Oncology Clinical Trial Consortia
The following table characterizes the major oncology consortia operating globally, their structural models, and specialized focuses.
Table 2: Global Oncology Early Phase Clinical Trial Consortia Landscape
| Consortium Name | Geographic Scope | Therapeutic Focus | Structural Model | Key Achievements |
|---|---|---|---|---|
| NCI Experimental Therapeutics Clinical Trials Networks | United States | Pan-cancer (multiple malignancies) | Government-funded [50] | Collaborative research, molecular tumor boards [50] |
| Academic GI Cancer Consortium (AGICC) | United States | Gastrointestinal cancers | Academic/Key Opinion Leader [51] | Rapid trial completion in GI cancers [51] |
| Academic Myeloma Consortium (AMyC) | United States | Multiple myeloma | Academic/Key Opinion Leader [51] | Identifies new drugs for myeloma [51] |
| Academic Thoracic Oncology Medical Investigators Consortium (ATOMIC) | United States | Thoracic cancers | Academic/Key Opinion Leader [51] | Adaptive clinical trial model for rapid drug development [51] |
| Private Oncology Networks | Multiple regions | Variable by network | Private research organization [50] | Streamlining trial conduct to improve timelines and cost efficiency [50] |
Protocol: Optimizing Consortium Participation for Master Protocol Execution
This protocol outlines a systematic approach for engaging with and leveraging collaborative consortia within master protocol frameworks.
3.2.1 Consortium Evaluation and Selection
- Objective: Identify consortium best aligned with scientific goals and operational requirements.
- Procedure:
- Strategic Fit Assessment:
- Operational Capability Evaluation:
- Governance and Intellectual Property Review:
- Analyze publication policies, authorship guidelines, and data sharing agreements
- Evaluate intellectual property frameworks and licensing arrangements
- Assess decision-making processes and sponsor representation in governance
3.2.2 Master Protocol Integration Within Consortium Framework
- Objective: Leverage consortium infrastructure for efficient master protocol implementation.
- Procedure:
- Scientific Steering Committee Establishment:
- Form multidisciplinary team including consortium representatives, sponsor scientists, and patient advocates
- Define decision-making authority and communication pathways
- Establish charter with clear objectives and operating procedures
- Operational Workflow Integration:
- Adaptive Governance Implementation:
- Establish protocol committee for ongoing evaluation of emerging data and protocol modifications
- Create data safety monitoring board with predefined stopping rules and futility analyses [52]
- Implement statistical analysis plan with pre-specified adaptive design elements
- Scientific Steering Committee Establishment:
3.2.3 Consortium Performance Management
- Objective: Ensure ongoing optimization of consortium performance and output.
- Procedure:
- Performance Metrics Monitoring:
- Track site activation timelines against predefined benchmarks
- Monitor screening efficiency and enrollment rates across all protocol sub-studies
- Evaluate data quality metrics (query rates, time to database lock)
- Collaborative Intelligence Gathering:
- Participate in consortium scientific meetings and working groups
- Access "soft intel" through discussions regarding possible regulatory changes [47]
- Share best practices and operational efficiencies across member institutions
- Value Assessment:
- Conduct periodic evaluation of consortium value against predetermined success criteria
- Assess publications, regulatory submissions, and other output metrics
- Evaluate patient engagement and experience across consortium sites
- Performance Metrics Monitoring:
Workflow Visualization: Consortium Operational Structure
The following diagram illustrates the integrated operational structure of a typical oncology research consortium:
Integrated Application in Master Protocol Designs
Master protocols (basket, umbrella, and platform trials) represent a transformative approach to oncology drug development that naturally aligns with both early regulatory engagement and consortium-based execution. The integration of these strategies creates a powerful framework for efficient clinical evaluation.
Regulatory Considerations for Master Protocols
Engaging regulators early is particularly crucial for master protocols due to their complexity and statistical considerations. Key focus areas include:
- Endpoint Selection: Alignment on appropriate endpoints for different sub-studies, considering the FDA's emphasis on overall survival as both an efficacy and safety endpoint [49]
- Statistical Considerations: Pre-specification of alpha spending functions, subgroup analysis plans, and handling of complex hypotheses [49]
- Adaptive Design Elements: Agreement on protocol modification triggers, interim analysis plans, and potential sample size re-estimation [52]
- Crossover and Subsequent Therapy: Transparent handling of intercurrent events, particularly in settings with potential for crossover [49]
Consortium-Enabled Operational Efficiencies in Master Protocols
Research consortia provide distinct advantages in master protocol execution through:
- Standardized Biomarker Platforms: Implementation of validated assays across network sites with centralized testing and quality control [52]
- Harmonized Data Collection: Establishment of common data elements across multiple sub-studies facilitating pooled analyses [50]
- Rapid Site Activation: Leverage of master contracts and centralized IRB reviews to accelerate study initiation [51]
- Shared Control Arms: Development of appropriately matched control populations that can be utilized across multiple experimental arms [53]
Successful implementation of early regulatory engagement and consortium participation requires specific tools and resources. The following table details essential components of the regulatory and consortium strategy toolkit.
Table 3: Essential Research Reagents and Resources for Regulatory-Consortium Strategy
| Tool/Resource | Function | Application Context |
|---|---|---|
| Regulatory Roadmap Template | Living document tracking planned interactions, milestones, and strategies for addressing challenges [47] | Early Regulatory Engagement |
| FDA OREEG Platform | Self-learning platform with educational resources for early-stage oncology companies [48] | Pre-IND Planning |
| Project Optimus Guidance | FDA guidance on dose optimization strategies balancing safety, tolerability and efficacy [54] | Early Phase Trial Design |
| Centralized IRB Platform | Streamlined ethical review process across multiple consortium sites [51] | Consortium Operations |
| Biomarker Validation Framework | Standards for assay validation, specimen handling, and quality control [52] | Master Protocol Implementation |
| Real-World Data Access | Curated real-world datasets for external control arms in single-arm trials [53] | Rare Cancers/Unmet Need |
| Molecular Tumor Board Platform | Multidisciplinary review platform for patient-specific biomarker-matched treatments [50] | Precision Medicine Trials |
| Common Data Elements Library | Standardized data definitions facilitating pooling and comparison across studies [52] | Data Harmonization |
| Risk-Based Monitoring Tools | Targeted monitoring approaches focusing on critical data and processes [52] | Quality Management |
| Statistical Analysis Plan Templates | Pre-specified analytical approaches including handling of complex scenarios [49] | Regulatory Submission Ready |
The integration of early regulatory engagement and collaborative consortia represents a powerful paradigm for modern oncology drug development, particularly within the context of master protocol designs. By proactively engaging regulators throughout the development process, sponsors can align on expectations, identify potential issues early, and build the collaborative relationships necessary for efficient review. Simultaneously, participation in research consortia provides the operational infrastructure, scientific expertise, and patient access necessary to execute complex master protocols efficiently. When implemented using the protocols and tools outlined in this document, these integrated strategies can significantly de-risk development programs, accelerate timelines, and ultimately enhance the delivery of innovative therapies to cancer patients.
Application Notes
The Imperative for Evolving Phase I Trial Designs
The 3+3 dose escalation design has been the cornerstone of oncology Phase I trials for decades, used in more than 95% of published studies. Its primary objective has been identifying the Maximum Tolerated Dose (MTD) under the paradigm that efficacy increases with dose, with toxicity being the primary limitation. However, this design faces significant challenges in the era of molecularly targeted agents and immunotherapies, where the therapeutic window may occur at doses significantly below the MTD and where the traditional dose-limiting toxicity (DLT) endpoint may not adequately capture the full biological activity profile. Approximately 25% of oncology agents approved by the FDA are ultimately labeled at a dose different from that identified in initial Phase I trials, indicating substantial limitations in current dose-optimization approaches. This discrepancy underscores the urgent need for more sophisticated frameworks that can integrate multiple endpoints to better identify the optimal biological dose rather than simply the MTD.
Quantitative Performance Comparison of Dose-Finding Methods
Statistical simulations and retrospective analyses consistently demonstrate the superior performance of model-based approaches like the Continual Reassessment Method (CRM) compared to traditional algorithm-based methods. The table below summarizes key comparative metrics based on published literature and trial data.
Table 1: Performance Comparison of 3+3 Design versus Model-Based Methods
| Performance Metric | 3+3 Design | Model-Based Methods (CRM) |
|---|---|---|
| Probability of Correct MTD Selection | ~20% lower than CRM across various scenarios [55] | Approximately 60% (though <60% for all methods in simulations) [55] |
| Median Number of Dose Levels Explored | 6 levels [55] | 10 levels [55] |
| Median Dose Ratio (Highest:Starting Dose) | 9 [55] | 30 [55] |
| Mean Number of Patients Exposed to Doses > MTD | 9 patients (approximately twice as high) [55] | 4 patients [55] |
| Flexibility for Expansion Cohorts | Limited [55] | High - can reassess risk of DLT with more data [55] |
| Adaptation to Patient Characteristics | Not available with standard design [55] | Possible through covariate-adjusted models [55] |
Integration with Master Protocol Frameworks
The evolution beyond 3+3 designs creates natural synergies with master protocol architectures, including basket, umbrella, and platform trials. These novel frameworks enable simultaneous evaluation of multiple therapeutics or therapeutic strategies within a single trial infrastructure against one or more disease types. Platform trials in particular leverage adaptive randomization and continuous learning to efficiently allocate patients to the most promising treatments based on accumulating data. The incorporation of model-based dose optimization within these master protocols allows for more efficient dose selection across multiple agents and biomarker-defined subgroups, substantially accelerating the drug development timeline while providing more robust dose justification for regulatory approval.
Experimental Protocols
Protocol 1: Continual Reassessment Method (CRM) Implementation
Objective
To determine the maximum tolerated dose (MTD) of a novel therapeutic agent using a model-based dose escalation approach that continuously updates the dose-toxicity relationship based on all accumulated patient data.
Materials and Reagents
Table 2: Research Reagent Solutions for CRM Implementation
| Item | Function | Specifications |
|---|---|---|
| Statistical Computing Environment | Model fitting and dose prediction | R, Python, or specialized clinical trial software (e.g., BOIN, EAST) |
| Prior Dose-Toxicity Model | Initial assumption of dose-toxicity relationship | Skeletons (prior probabilities of DLT at each dose); commonly: 0.05, 0.12, 0.25, 0.40, 0.55 [55] |
| Target DLT Rate | Definition of acceptable toxicity level | Typically 20-30%, determined by physician input [55] |
| Patient Safety Monitoring System | Tracking and reporting adverse events | Electronic data capture system with real-time reporting capabilities |
| Protocol Template | Structured protocol development | FDA/NIH Clinical Trial Protocol Template for Phase II and III IND/IDE Studies [56] |
Methodology
Preliminary Setup: Define dose levels, prior probabilities of DLT (skeleton), target DLT rate (typically 20-30%), and stopping rules. Establish a statistical model (commonly logistic or power model) relating dose to probability of DLT.
Initial Cohort: Treat the first patient or cohort at the predefined starting dose (often the lowest dose level or a dose based on preclinical data).
DLT Assessment: Evaluate patients for DLT during the first cycle (typically 21-28 days) using standardized criteria (e.g., CTCAE guidelines).
Model Reassessment: After DLT outcomes are observed, fit the statistical model to all accumulated data to estimate the probability of DLT at each dose level.
Dose Assignment for Next Patient: Allocate the next patient to the dose with estimated DLT probability closest to the target rate.
Iterative Process: Repeat steps 3-5 until a prespecified stopping rule is met (typically after a predetermined sample size or when MTD estimation reaches a specific precision).
MTD Determination: The recommended MTD is the dose level with estimated DLT probability closest to the target rate at trial completion.
Expansion Cohort: Utilize the continuously updated model to reassess DLT risk in expansion cohorts, incorporating additional patient data to refine the MTD estimate.
Figure 1: CRM Dose-Finding Workflow
Protocol 2: Master Protocol Integration with Adaptive Dose Optimization
Objective
To implement a model-based dose optimization strategy within a master protocol framework that enables simultaneous evaluation of multiple therapeutic agents or biomarker-defined patient populations.
Materials and Reagents
Table 3: Research Reagent Solutions for Master Protocol Implementation
| Item | Function | Specifications |
|---|---|---|
| Protocol Development Software | Structured protocol writing | Protocol Builder platforms with collaborative features [57] [58] |
| Electronic Protocol Template | Standardized protocol format | FDA/NIH Phase II/III IND/IDE template or institutional equivalents [56] |
| Centralized Randomization System | Patient allocation to biomarker-therapy matches | Interactive web response system (IWRS) |
| Biomarker Assessment Platform | Molecular profiling for patient stratification | Next-generation sequencing, immunohistochemistry, or flow cytometry |
| Data Monitoring Committee Charter | Oversight of adaptive trial conduct | Predefined charter outlining monitoring responsibilities |
Methodology
Protocol Development: Utilize structured protocol development tools (e.g., Protocol Builder) to create a comprehensive master protocol incorporating model-based dose optimization components. The protocol should include all elements required for efficient scientific and ethical review [57].
Biomarker Strategy: Define biomarker subgroups for targeted therapies using established assessment platforms. Incorporate these subgroups into the dose optimization model where appropriate.
Adaptive Dose-Finding Structure: Implement parallel CRM or Bayesian model-based designs for each therapeutic agent or combination being evaluated. For combination therapies, develop specialized designs that can optimize dosing for multiple agents simultaneously.
Randomization Framework: Establish an adaptive randomization system that allocates patients to optimal dose levels within their assigned treatment arm based on accumulating efficacy and toxicity data.
Interim Analysis Plan: Predefine interim analysis timepoints for dose optimization decisions, incorporating early efficacy endpoints alongside safety data where appropriate.
Expansion Cohort Strategy: Plan for biomarker-directed expansion cohorts at the optimized dose for each therapeutic agent, with predefined statistical thresholds for efficacy.
Integrated Informed Consent: Develop comprehensive consent documents that explain the adaptive nature of the trial using the Informed Consent Builder tools available in modern protocol development platforms [58].
Figure 2: Master Protocol Dose Optimization Architecture
Implementation Considerations
Regulatory Alignment and Protocol Development
Successful implementation of novel dose optimization frameworks requires careful attention to regulatory expectations and protocol standardization. Investigators should utilize established protocol templates such as the FDA/NIH Clinical Trial Protocol Template for Phase II and III IND/IDE studies to ensure comprehensive inclusion of all necessary elements [56]. Statistical sections must be written by the study team statistician, with clear specification of the model-based design, stopping rules, and operating characteristics. The protocol should explicitly address the NIH Policy on Sex as a Biological Variable and include detailed clinical management sections for handling adverse events, particularly for drug and biologic interventions.
Operational Requirements and Resource Allocation
Transitioning from traditional 3+3 designs to model-based approaches necessitates specialized statistical expertise and infrastructure. Research teams should ensure access to statistical support familiar with CRM and related methods, as well as appropriate computational resources for real-time dose assignment decisions. Collaborative protocol development platforms such as Protocol Builder can streamline the process through built-in compliance guidance, sample text, and collaborative features that facilitate communication between team members [57] [58]. These platforms also help maintain version control and track changes throughout the protocol development process.
Ethical Considerations and Safety Monitoring
While model-based designs potentially expose fewer patients to excessively toxic doses, they require careful safety monitoring plans. Protocols should include explicit statements that participant safety overrides protocol requirements, ensuring that treating physicians can provide whatever available treatment is considered best to protect participant safety and well-being. For device studies, additional sections describing post-trial transition plans, surgical implantation procedures, and device components/specifications must be included. Regular review by an independent Data and Safety Monitoring Board (DSMB) is essential for all adaptive trials incorporating novel dose-finding methodologies.
Benchmarking Master Protocols: Validating Efficiency Gains Against Traditional Trials
The rising complexity and cost of oncology clinical trials necessitate a paradigm shift toward more efficient research frameworks. Master protocol designs, which include umbrella, basket, and platform trials, have emerged as a powerful solution, enabling the simultaneous evaluation of multiple therapies, biomarkers, or patient populations within a single, unified infrastructure. The quantitative assessment of efficiency gains—spanning administrative, statistical, and regulatory domains—is critical for justifying their adoption and optimizing their implementation. This document provides application notes and detailed protocols for quantifying these efficiency gains, underpinned by current innovations in statistical methodology and operational strategy. Embracing these approaches is consistent with the foundational principles of R.A. Fisher, who championed the idea of asking multiple questions of nature within a single experiment [59].
Quantitative Assessment of Current Burdens and Efficiencies
A critical first step is to establish benchmarks for the burdens inherent in traditional trial designs and the potential efficiencies offered by master protocols. The data reveal a compelling case for change.
Table 1: Quantitative Burden of Traditional Oncology Trial Amendments
| Burden Category | Key Metric | Quantitative Impact | Source |
|---|---|---|---|
| Financial Burden | Percentage of trials requiring amendments | 76% (up from 57% in 2015) | [60] |
| Direct cost per amendment | $141,000 to $535,000 | [60] | |
| Trials requiring multiple amendments | Nearly 90% of oncology trials | [60] | |
| Timeline Burden | Average implementation time for an amendment | 260 days | [60] |
| Sites operating under different protocol versions | 215 days on average | [60] | |
| Operational Burden | Site-impacting amendments requiring budget renegotiation & system updates | 23% are potentially avoidable | [60] |
Table 2: Quantified Efficiency Gains from Innovative Designs & Strategies
| Efficiency Strategy | Quantitative Gain | Application in Master Protocols |
|---|---|---|
| Prognostic Covariate Adjustment | "Dramatically" improves statistical power compared to standard log-rank test | Increases statistical efficiency in randomized sub-studies with time-to-event endpoints [61]. |
| Factorial & Adaptive Designs | Enables addressing two or more questions with a single experiment | Core principle of master protocols; improves resource utilization and accelerates discovery [59]. |
| AI-Driven Site Selection | Identifies optimal sites for patient recruitment success | Streamlines study startup and improves enrollment efficiency in complex trial networks [62]. |
Protocol for Quantifying Administrative and Operational Efficiency
Application Notes
Administrative burden in clinical trials manifests as protocol amendments, lengthy site activation processes, and complex site management. A significant portion (an estimated 23%) of amendments are potentially avoidable, stemming from issues like poorly defined eligibility criteria or assessment schedules [60]. These amendments create a cascading effect of costs, timeline extensions, and operational disruptions. Quantifying the reduction of these burdens is essential for demonstrating the value of master protocols, which are designed with inherent flexibility to incorporate new questions without foundational changes.
Experimental Protocol: Tracking and Analyzing Amendment-Related Burdens
Objective: To systematically track, categorize, and quantify the administrative and operational burdens associated with protocol amendments within a clinical trial program, and to compare these metrics between traditional trials and trials using a master protocol framework.
Materials and Methods
- Data Sources: Clinical trial protocols, amendment records, contract values, internal review board (IRB) communication logs, site activation trackers, and electronic data capture (EDC) system change logs.
- Categorization Framework: Classify each amendment as:
- Key Metrics and Calculations:
- Amendment Frequency: (Total Number of Amendments per Trial) tracked over the trial lifecycle.
- Direct Cost Impact:
- Sum of IRB review fees, site contract renegotiation costs, and data management system update costs per amendment [60].
- Calculate the total direct cost attributable to amendments per trial.
- Timeline Impact:
- Measure the delay (in days) from amendment initiation to full implementation across all sites.
- Record the period sites operate under different protocol versions [60].
- Site Burden Score: Develop a composite score based on the number of systems impacted per amendment (e.g., EDC, CTMS, IxRS) and the required staff retraining hours.
Procedure
- Retrospective Baseline Establishment: Conduct a historical review of 5-10 completed traditional oncology trials to calculate baseline metrics for amendment frequency, cost, and timeline impact.
- Prospective Monitoring in Master Protocols: Implement a real-time tracking system for all amendments in active master protocols.
- Comparative Analysis: For each active master protocol, identify a matched traditional trial (by phase, oncology indication, and complexity) and compare the calculated metrics.
- Efficiency Quantification: Calculate the percentage reduction in amendment frequency, direct costs, and timeline delays in the master protocol versus the matched control.
Visualization of Workflow The following diagram illustrates the logical workflow for quantifying administrative efficiency, from data collection to final analysis.
Protocol for Enhancing Statistical Efficiency and Analysis
Application Notes
Statistical efficiency is the maximization of information gain from a given sample size or data source. Innovations such as Bayesian adaptive methods, factorial designs, and covariate adjustment for time-to-event endpoints are pivotal for boosting efficiency within master protocols [59] [61]. These approaches allow for dynamic decision-making, shared control arms, and more precise estimation of treatment effects, which directly reduces the required sample size and duration of a trial. The mindset required is one that prioritizes informative design over the rigid requirement of "high power" for every question, enabling the efficient exploration of multiple hypotheses [59].
Experimental Protocol: Implementing a Covariate-Adjusted Efficiency Analysis
Objective: To implement and validate a statistical method that increases power and precision in randomized oncology trials with time-to-event endpoints, thereby improving statistical efficiency within a master protocol.
Materials and Methods
- Research Reagent Solutions:
- Software: R or SAS statistical software.
- Data Set: De-identified patient-level data from a randomized trial with a primary time-to-event endpoint (e.g., Overall Survival, Progression-Free Survival).
- Prognostic Covariates: Pre-specified baseline measures strongly associated with the outcome (e.g., disease stage, number of prior therapies, specific genomic markers) as encouraged by FDA guidance [61].
- Statistical Method: An extension of Rosenbaum's exact testing method incorporating a variant of martingale residuals for right-censored data [61].
Procedure
- Data Preparation: Extract the time-to-event data, event indicator, treatment arm, and values for the pre-specified prognostic covariates for each patient.
- Model Fitting: Fit a Cox proportional hazards model to the data using the treatment arm and the prognostic covariates as independent variables.
- Residual Calculation: Compute the martingale residuals from the null Cox model (which excludes the treatment arm).
- Test Statistic Construction:
- Within the framework of a permutation test, create a test statistic that compares the treatment arms based on a weighted combination of the martingale residuals.
- This effectively tests the treatment effect after accounting for the prognostic information in the covariates.
- Power Comparison:
- Conduct a simulation study where data is repeatedly generated under a pre-defined treatment effect and covariate relationship.
- For each simulated dataset, perform both the proposed covariate-adjusted test and the standard log-rank test.
- Calculate the empirical power for each test as the proportion of simulations in which the null hypothesis of no treatment effect was rejected (p < 0.05).
- Efficiency Quantification: Report the percentage increase in power achieved by the covariate-adjusted method versus the standard log-rank test. Alternatively, calculate the reduction in sample size required by the adjusted method to achieve the same power as the unadjusted test.
Visualization of Analysis Workflow The diagram below outlines the key steps in this statistical efficiency protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Efficiency Analysis
| Item Name | Function/Benefit | Application Context |
|---|---|---|
| Prognostic Covariates | Baseline measures that increase statistical power by explaining outcome variability. | Covariate-adjusted analysis of time-to-event endpoints [61]. |
| Bayesian Adaptive Software | Enables real-time trial simulation and modification based on accumulating data. | Implementing adaptive randomization and sample size re-estimation in platform trials [59]. |
| AI for Site Selection | Analyzes historical and demographic data to identify high-performing sites. | Improving patient recruitment efficiency and streamlining study startup [62]. |
| Common Protocol Template | Drives consistency and simplifies technology setup and integration. | Reducing operational complexity and administrative burden in trial setup [62]. |
| Patient-Reported Outcome (PRO) Tools | Captures patient-centric data on treatment tolerability and quality of life. | Integrating patient-centric endpoints into early-phase dose-finding trials [63]. |
The rigorous quantification of efficiency gains in administrative, statistical, and regulatory domains provides a compelling evidence base for the widespread adoption of master protocol designs in oncology. By implementing the detailed protocols outlined in this document—tracking amendment burdens, employing advanced statistical methods like covariate-adjusted analyses, and leveraging tools from the research toolkit—sponsors and researchers can systematically demonstrate value, optimize resource allocation, and ultimately accelerate the delivery of new therapies to patients with cancer. The future of efficient oncology research lies in these integrated, adaptive, and quantitatively-driven approaches.
Within oncology clinical research, the escalating complexity of master protocol designs—including basket, umbrella, and platform trials—presents both unprecedented scientific opportunities and significant operational challenges. These sophisticated designs, while enabling efficient evaluation of multiple therapies or disease subtypes under a single protocol, inherently introduce complexity that directly impacts trial performance and cycle times. Recent data indicate that 76% of Phase I-IV trials now require protocol amendments, a substantial increase from 57% in 2015, with each amendment costing between $141,000 and $535,000 in direct expenses alone [60]. Furthermore, oncology trials demonstrate particularly high complexity, with 90% requiring at least one amendment [60]. This application note establishes comprehensive benchmarking frameworks and methodologies to quantify protocol complexity, predict its impact on cycle times, and implement evidence-based strategies for optimizing master protocol designs in oncology research.
Current State of Protocol Complexity and Cycle Time Metrics
Quantitative Benchmarking of Trial Performance
Table 1: Clinical Trial Performance Benchmarks Across Development Phases
| Metric Category | Phase I | Phase II | Phase III | Data Source |
|---|---|---|---|---|
| Average Duration | 16.0 months [64] | 36.2 months (Phase I/II) [64] | 39-40 months [64] | Tufts CSDD, Citeline Analysis |
| Success Rate | 60-70% (Phase I to II) [65] | 30-33% (Phase II to III) [65] | 50-57.8% (Phase III to Approval) [65] | Industry Benchmarks |
| Amendment Prevalence | 76% of all trials (Phase I-IV) [60] | - | - | Tufts CSDD 2024 |
| Amendment Cost | $141,000 - $535,000 per amendment [60] | - | - | Tufts CSDD 2024 |
Table 2: Operational Cycle Time Metrics and Industry Benchmarks
| Operational Metric | Industry Benchmark | Impact & Implications |
|---|---|---|
| Startup Phase Cycle Time | 24.8 weeks (pre-optimization) [66] | 45.6% reducible through systematic interventions [66] |
| IRB Submission to Approval | Highly variable [65] | Key startup metric indicating regulatory agility [65] |
| Contract to Enrollment | Highly variable [65] | Crucial indicator of recruitment readiness [65] |
| Protocol Amendment Implementation | 260 days average [60] | Sites operate under different protocol versions for 215 days average [60] |
The Complexity-Cycle Time Relationship
Evidence consistently demonstrates a direct correlation between protocol complexity and extended cycle times. Research on the Protocol Complexity Tool (PCT) revealed that total complexity scores showed statistically significant positive correlations with time-to-site activation (rho = 0.61; p = 0.005) and participant enrollment at 25% recruitment (rho = 0.59; p = 0.012) [67] [68]. Furthermore, analysis of over 16,000 clinical trials identified oncology as the therapeutic area with the most complex trials, with specific indications including prostate, colorectal, breast, and lung cancer contributing disproportionately to this complexity [69].
Diagram 1: Protocol Complexity Impact Cascade. This diagram illustrates how protocol complexity drives operational, regulatory, site, and patient burdens, ultimately impacting timeline, cost, and overall trial success.
Experimental Protocols for Complexity Assessment
Protocol Complexity Tool (PCT) Methodology
The Protocol Complexity Tool (PCT) provides a validated, quantitative framework for assessing trial complexity across five critical domains. Developed through a collaborative process with 20 cross-functional experts in clinical trial design and execution, the PCT employs 26 multiple-choice questions across five domains, each scored on a 3-point scale (0=low, 0.5=medium, 1=high complexity) [67] [68].
Table 3: PCT Domain Structure and Scoring Methodology
| Domain | Number of Questions | Key Assessment Areas | Scoring Calculation |
|---|---|---|---|
| Study Design | 6 | Endpoints, study type, design complexity, sub-studies | Domain Complexity Score (DCS) = Sum of question scores / Number of questions |
| Operational Execution | 5 | Site selection, data collection, monitoring complexity | Domain Complexity Score (DCS) = Sum of question scores / Number of questions |
| Regulatory Oversight | 5 | Geographic scope, regulatory requirements, safety reporting | Domain Complexity Score (DCS) = Sum of question scores / Number of questions |
| Site Burden | 5 | Staff training, resource requirements, pharmacy needs | Domain Complexity Score (DCS) = Sum of question scores / Number of questions |
| Patient Burden | 5 | Visit frequency, procedure complexity, travel requirements | Domain Complexity Score (DCS) = Sum of question scores / Number of questions |
| Total Complexity Score (TCS) | 26 questions across all domains | Overall protocol complexity | TCS = Sum of all 5 Domain Scores (range: 0-5) |
Implementation Protocol: PCT Assessment
Materials Required:
- PCT scoring template (tablet or paper-based)
- Finalized study protocol document
- Cross-functional assessment team
- Historical trial data for benchmarking
Step-by-Step Procedure:
Team Assembly: Convene a cross-functional assessment team including representatives from clinical operations, biostatistics, data management, regulatory affairs, and site management.
Protocol Review: Conduct a systematic review of the complete protocol document, focusing on design elements, procedures, and operational requirements.
Domain Scoring: For each of the 26 questions across the five domains, assign scores of 0 (low complexity), 0.5 (medium complexity), or 1 (high complexity) based on predefined criteria.
Calculation of Scores:
- Compute individual Domain Complexity Scores (DCS) by averaging question scores within each domain
- Calculate Total Complexity Score (TCS) by summing all five DCS values
- Record scores in the complexity assessment database
Benchmark Comparison: Compare TCS and individual domain scores against historical trials and therapeutic area benchmarks.
Complexity Reduction Workshop: Conduct a focused workshop to identify opportunities for complexity reduction in high-scoring domains while maintaining scientific integrity.
Post-Optimization Rescoring: Reassess complexity scores after protocol modifications to quantify improvement.
Validation Evidence: In validation studies, the PCT demonstrated significant utility, with 75% of assessed trials showing reduced complexity scores after PCT implementation, primarily in operational execution (50% of trials) and site burden (43.8% of trials) domains [67] [68].
Machine Learning Approaches for Cycle Time Prediction
Advanced machine learning methodologies, particularly survival analysis models, enable accurate prediction of clinical trial duration based on protocol features. The DeepSurv neural network model has demonstrated superior performance in predicting trial duration using the largest dataset in this domain, comprising 90,366 clinical trials involving 20,760 drugs [64].
Data Preprocessing Protocol:
Feature Extraction: Collect comprehensive trial features available before trial initiation, including:
- Trial design characteristics (phase, target accrual, endpoints)
- Drug properties (origin, medium, delivery route)
- Disease metrics (prevalence, DALY scores)
- Operational factors (regions, patient demographics)
Data Cleaning:
- Exclude trials with unknown start dates
- Compute duration for completed trials as difference between start and primary completion dates
- Treat ongoing trials as right-censored data
Feature Engineering:
- Apply one-hot encoding for multi-labeled categorical features
- Create interaction terms for key complexity drivers
- Normalize numerical features to standard distributions
Model Training Framework:
- Implement Cox Proportional Hazards model as baseline
- Train DeepSurv neural network architecture with appropriate hyperparameter tuning
- Validate models using time-dependent concordance indices and integrated Brier scores
- Calculate feature importance scores to identify key complexity drivers
Optimization Strategies for Master Protocols
Complexity Management Framework
Diagram 2: Multi-Dimensional Optimization Framework for Master Protocols. This diagram outlines the strategic, operational, and analytical approaches to managing complexity in master protocol designs.
Research Reagent Solutions: Complexity Assessment Toolkit
Table 4: Essential Research Reagents and Tools for Protocol Complexity Management
| Tool/Reagent | Function | Application in Master Protocols |
|---|---|---|
| Protocol Complexity Tool (PCT) | Quantitatively assesses protocol complexity across 5 domains | Standardized complexity scoring for basket, umbrella, and platform trials [67] [68] |
| Machine Learning Prediction Models | Predicts trial duration based on protocol features | Forecasting timelines for adaptive trial designs [64] |
| Clinical Trial Risk Tool | Assesses trial complexity from protocol text using NLP | Early-stage risk identification in master protocol development [69] |
| Amendment Management Framework | Categorizes and tracks protocol amendments | Distinguishing necessary vs. avoidable amendments in complex trials [60] |
| Stakeholder Engagement Platform | Facilitates cross-functional protocol review | Incorporating site, patient, and regulatory feedback pre-implementation [70] |
Systematic benchmarking of protocol complexity and cycle time metrics provides oncology drug development professionals with evidence-based frameworks for optimizing master protocol designs. The integration of structured assessment tools like the PCT, combined with machine learning forecasting models and strategic complexity reduction approaches, enables research teams to balance scientific ambition with operational feasibility. Implementation of these methodologies has demonstrated potential to reduce protocol complexity in 75% of trials and decrease startup cycle times by 45.6% [67] [66]. As master protocols continue to evolve in sophistication, maintaining rigorous focus on complexity management will be essential for accelerating oncology drug development without compromising scientific integrity or operational execution.
Within oncology clinical trials research, master protocol designs represent a transformative approach aimed at enhancing the efficiency of therapeutic evaluation. A core challenge in this domain is patient enrollment and retention, metrics critical to the timely and successful completion of clinical studies. This analysis provides a quantitative and methodological comparison of enrollment-to-completion rates between trials conducted under master protocols and those using traditional oncology protocols, contextualized within a broader thesis on advanced trial designs. The objective is to delineate the operational and statistical advantages of master protocols, supported by empirical data and detailed experimental frameworks for the research community.
Quantitative Performance Benchmarking
Data from recent studies, particularly from the Tufts Center for the Study of Drug Development (CSDD), highlight significant performance differentials between traditional oncology protocols and other trial types, underscoring the enrollment challenges in oncology [71] [72].
Table 1: Benchmarking Traditional Oncology vs. Non-Oncology Clinical Trials
| Performance & Design Metric | Phase II Oncology Trials | Phase II Non-Oncology Trials | Phase III Oncology Trials | Phase III Non-Oncology Trials |
|---|---|---|---|---|
| Patient Completion Rate [72] | 14% | 54% | Not Specified | Not Specified |
| Total Clinical Trial Duration (Days) [72] | 1,482 | 991 | 1,769 | 1,214 |
| Total Data Points per Protocol [72] | 3.1 million | 1.9 million | Not Specified | Not Specified |
| Average Number of Substantial Amendments [72] | 50-70% higher | Baseline | 50-70% higher | Baseline |
| Average Number of Protocol Deviations [72] | 121.8 | 75.8 | Not Specified | Not Specified |
Table 2: Protocol Design Complexity Metrics (Phase II & III Averages)
| Design Characteristic | Oncology Protocols | Non-Oncology Protocols |
|---|---|---|
| Total Endpoints [72] | 16.6 | 21.3 |
| Total Eligibility Criteria [72] | 29.8 | 31.2 |
| Number of Distinct Procedures [72] | 34.3 | 33.5 |
| Number of Investigative Sites & Countries [71] | Significantly Higher | Lower |
Oncology trials face profound enrollment challenges, with only 14% of screened patients enrolled and completing Phase II trials, compared to 54% in non-oncology trials [72]. This is compounded by longer cycle times and a higher volume of data collection. Furthermore, a meta-analysis of U.S. oncology trials found that 22% of patients did not enroll due to restrictive eligibility criteria, and 15% of eligible patients declined participation [73].
Master protocols are unified trial frameworks designed to evaluate multiple hypotheses simultaneously. They enhance efficiency by optimizing resource use and accelerating patient enrollment [1]. The three primary types are defined below, with their logical structures detailed in the accompanying diagrams.
Definition and Types
- Basket Trials: Investigate a single targeted therapy across multiple patient populations, which are defined by different cancer types or specific molecular biomarkers [1].
- Umbrella Trials: Evaluate multiple investigational drugs or combinations within a single disease population, which is often subdivided by genetic or other biomarkers [1].
- Platform Trials: Characterized by their adaptive nature, allowing for the dynamic addition of new treatment arms and the dropping of ineffective ones based on interim analyses [1].
Diagram 1: Logical structure of master protocol trial designs, including basket, umbrella, and platform trials [1].
Experimental Protocols and Methodologies
Traditional Site Management Workflow
The traditional model for clinical trial site management is linear and often protracted, contributing to enrollment delays [74].
Protocol Steps:
- Site Selection & Credentialing: Sites are pre-selected based on estimated enrollment potential and undergo a lengthy credentialing process [74].
- Contracting & IRB Approval: Contract negotiations and Institutional Review Board (IRB) approvals are completed. This process can take from 2 to 12 months per site [74].
- Site Initiation & Training: Following regulatory approval, sites are initiated, and staff are trained on the protocol.
- Patient Identification & Enrollment: Only after full initiation does the site begin to identify and enroll eligible patients. A significant challenge is that 20-30% of traditionally managed sites never enroll a single patient [74].
"Just-In-Time" (JIT) Patient-Focused Methodology
The JIT methodology inverts the traditional model to prioritize patient identification, thereby accelerating site activation and enrollment [74].
Protocol Steps:
- Advance Network & Training: Research-ready practices within a network are pre-trained on the JIT methodology and trial specifics.
- Patient Identification & Interest: Investigators pre-identify potential candidates using standard-of-care procedures. A patient's interest triggers the site activation process.
- Rapid Site Activation: A centralized administrative system targets completion of all site registration, contracting, and central IRB approval within 10 business days from the expression of patient interest [74].
- Formal Consent & Enrollment: The site is fully initiated just in time to formally consent and screen the identified patient.
Diagram 2: "Just-In-Time" patient-focused enrollment workflow, designed to rapidly activate sites upon patient identification [74].
Performance Outcomes: JIT vs. Traditional Methodology
A retrospective analysis of three cancer clinical trials demonstrated the efficacy of the JIT approach [74].
Table 3: JIT vs. Traditional Site Enrollment Outcomes
| Enrollment Metric | Just-In-Time (JIT) Sites | Traditional Sites |
|---|---|---|
| Mean Enrollment Rate (patients/site/month) [74] | Up to 2.75x higher | Baseline |
| Mean Patients Enrolled Per Site [74] | 1.82 | 1.78 |
| Percentage of Non-Enrolling Sites [74] | 7% (2/28) | 37% (19/52) |
The Scientist's Toolkit: Research Reagent Solutions
Successfully implementing complex trial designs like master protocols requires a suite of specialized tools and approaches.
Table 4: Essential Research Reagents & Solutions for Master Protocol Execution
| Research Solution | Function & Application |
|---|---|
| Central IRB | Streamlines and accelerates the ethical review process across multiple sites, crucial for JIT enrollment and master protocols [74]. |
| Centralized Administration System | Reduces site administrative workload by managing regulatory documents, contracts, and data, enabling rapid site activation [74]. |
| Biomarker Data Specifications | Protocols established early to ensure correct collection, transfer, and formatting of complex genomic and biomarker data for patient stratification [1]. |
| Adaptive Statistical Analysis Plan (SAP) | A pre-planned, flexible SAP that accounts for adaptive features, multiplicity, and complex Bayesian methods inherent in platform trials [1]. |
| Real-Time Data Management Systems | Robust platforms capable of integrating, processing, and cleaning large, dynamic datasets from multiple cohorts in near-real-time [1]. |
| Clinical Study Report (CSR) Strategy | A pre-defined plan for generating CSRs (e.g., one per cohort or a single comprehensive report) to manage reporting complexity [1]. |
Integrated Discussion
The quantitative data and methodological comparisons reveal a clear narrative: traditional oncology protocols are hampered by structural inefficiencies that lead to low enrollment-to-completion rates. The protracted timelines of traditional site management directly conflict with the narrow therapeutic windows in oncology care. Master protocols, supported by operational innovations like the JIT methodology, address these inefficiencies at a systemic level.
The JIT model's success—reducing non-enrolling sites from 37% to 7% [74]—demonstrates that aligning research procedures with patient and physician workflows is critical. This approach is conceptually synergistic with master protocols, which inherently create a more flexible and responsive trial infrastructure. By testing multiple therapies under a single protocol, master protocols increase the probability that a patient at a given site will be eligible for a sub-study, thereby improving site engagement and productivity.
While master protocols introduce complexities in data management, statistical analysis, and operational execution [1], the tools and methodologies detailed in this analysis provide a framework for managing these challenges. The continued evolution toward patient-centric, efficient trial designs is not merely an operational improvement but a scientific necessity for accelerating the development of new cancer therapies.
The development of innovative therapies for life-threatening malignancies has been fundamentally altered by the implementation of accelerated approval pathways. These regulatory mechanisms, established by the U.S. Food and Drug Administration (FDA), represent a paradigm shift from traditional approval processes that historically required Phase III trials demonstrating overall survival benefits [75]. The Accelerated Approval Program (AAP), codified in 21 CFR 314.510, permits approval based on surrogate endpoints reasonably likely to predict clinical benefit, such as progression-free survival (PFS) and overall response rate (ORR), rather than the gold standard of overall survival (OS) [75]. This approach acknowledges that cancer patients facing poor prognoses cannot wait for the completion of lengthy Phase III randomized trials when preliminary evidence suggests substantial therapeutic benefit.
Master protocol designs represent a complementary innovation in oncology drug development, enabling the simultaneous evaluation of multiple investigational drugs and/or cancer types within the same overall trial structure [21]. The FDA recommends that the recommended phase 2 dose (RP2D) should have been established for investigational drugs evaluated within such master protocols [21]. This framework provides an efficient clinical trial strategy to expedite the development of oncology drugs and biologics, particularly when combined with accelerated approval pathways.
This application note examines recent case studies of oncology therapies approved through accelerated pathways, detailing the quantitative evidence supporting their approval and providing experimental protocols for generating this evidence within the context of master trial designs.
Quantitative Evidence for Recent Accelerated Approvals
The following case studies from recent FDA approvals demonstrate the application of surrogate endpoints and the quantitative evidence required for accelerated approval in oncology.
Table 1: Recent FDA Accelerated Approvals in Oncology (July-September 2025)
| Drug (Brand Name) | Cancer Indication | Approval Date | Key Surrogate Endpoint(s) | Trial Design | Results |
|---|---|---|---|---|---|
| Dordaviprone (Modeyso) | H3 K27M-mutated diffuse midline glioma (DMG) | July-Sept 2025 | Overall Response Rate (ORR) | Single-arm trial in patients 1+ years with progression after prior therapy | [Data required for confirmatory trial] |
| Zongertinib (Hernexeos) | HER2-mutated non-small cell lung cancer (NSCLC) | July-Sept 2025 | ORR | Beamion LUNG-1 (first-in-human) in adults with unresectable/metastatic non-squamous NSCLC | Significant efficacy against broad HER2 mutations with favorable safety profile |
| Sunvozertinib (Zegfrovy) | EGFR exon 20 insertion-mutated NSCLC | July-Sept 2025 | ORR | Trial in adults with locally advanced/metastatic NSCLC progressing after chemotherapy | Activity against EGFR mutations including T790M resistance mutation |
| Imlunestrant (Inluriyo) | ESR1-mutated ER+/HER2- advanced breast cancer | July-Sept 2025 | PFS | Phase III EMBER-3 in adults progressing after endocrine therapy | Effectiveness alone and combined with abemaciclib |
| Linvoseltamab-gcpt (Lynozyfic) | Relapsed/refractory multiple myeloma | July-Sept 2025 | ORR | Trial in adults with ≥4 prior lines of therapy | Third BCMA-targeting bispecific T-cell engancer approved |
Table 2: Analysis of Surrogate Endpoints in Accelerated Approvals
| Surrogate Endpoint | Therapeutic Context | Correlation with Clinical Benefit | Regulatory Precedent |
|---|---|---|---|
| Progression-Free Survival (PFS) | Metastatic cancers with limited treatment options | Good correlation in metastatic disease settings | Palbociclib (Ibrance) in ER+/HER2- metastatic breast cancer [75] |
| Overall Response Rate (ORR) | Rare cancers and heavily pretreated populations | Valuable when traditional endpoints challenging | Ivosidenib (Tibsovo) in IDH1-mutated relapsed/refractory AML (30% ORR in Phase I) [75] |
| Duration of Response (DOR) | Targeted therapies in molecularly-defined subsets | Complements ORR by assessing response sustainability | Multiple biomarker-defined approvals in NSCLC and other solid tumors |
Master Protocol Framework for Accelerated Approval Trials
Master Protocol Design Principles
Master protocols represent an efficient clinical trial strategy for evaluating multiple investigational drugs and/or cancer subtypes within a unified trial structure. The FDA guidance on master protocols recommends that sponsors implement designs that simultaneously address multiple clinical questions, thereby accelerating drug development [21]. These protocols are particularly suited for accelerated approval pathways as they enable rapid evaluation of targeted therapies in molecularly-defined patient populations.
The fundamental structure of a master protocol for accelerated approval incorporates umbrella, basket, and platform trial designs that allow for:
- Evaluation of multiple targeted therapies against specific molecular alterations
- Efficient screening and allocation of patients to appropriate sub-studies
- Shared control arms and infrastructure to reduce operational costs
- Adaptive designs that allow for modification based on interim analyses
Master Protocol Workflow Implementation
Master Protocol Patient Allocation Workflow
This workflow illustrates the patient journey through a master protocol designed for accelerated approval. The process begins with comprehensive genomic profiling of the patient population, followed by biomarker assessment and molecular alteration detection. Patients are then allocated to specific treatment arms based on their molecular profile, with a shared endpoint of objective response rate suitable for accelerated approval.
Experimental Protocols for Accelerated Approval Evidence Generation
Protocol: Objective Response Rate Assessment in Solid Tumors
4.1.1 Purpose To standardize the assessment of Objective Response Rate (ORR) as a primary endpoint in clinical trials designed for accelerated approval, based on RECIST 1.1 criteria.
4.1.2 Materials and Reagents
- Contrast-enhanced CT or MRI imaging equipment
- RECIST 1.1 data collection forms
- Electronic case report forms (eCRFs)
- Central imaging review platform
- Tumor assessment software with volumetric capabilities
4.1.3 Procedure
- Baseline Tumor Assessment
- Perform contrast-enhanced CT or MRI of chest, abdomen, and pelvis within 28 days prior to treatment initiation
- Identify and measure all target lesions (maximum 5 total, 2 per organ)
- Document all non-target lesions
- Record measurements in eCRF with precise anatomical location
Treatment Phase Monitoring
- Schedule imaging assessments every 6-8 weeks during treatment period
- Maintain consistent imaging techniques and parameters across all assessments
- Document any changes in lesion measurements and appearance of new lesions
Response Categorization
- Complete Response (CR): Disappearance of all target and non-target lesions
- Partial Response (PR): ≥30% decrease in sum of diameters of target lesions
- Progressive Disease (PD): ≥20% increase in sum of diameters or appearance of new lesions
- Stable Disease (SD): Neither sufficient shrinkage for PR nor sufficient increase for PD
Independent Review
- Submit all imaging to blinded independent central review (BICR)
- Adjudicate discrepancies between investigator and central assessments
- Calculate confirmed ORR as proportion of patients achieving CR or PR
4.1.4 Data Analysis
- Calculate ORR with 95% confidence interval using exact binomial method
- Perform subgroup analyses based on molecular biomarkers
- Report duration of response using Kaplan-Meier methods
Protocol: Biomarker Validation for Patient Selection
4.2.1 Purpose To establish validated biomarker assays for patient selection in master protocols targeting specific molecular alterations.
4.2.2 Materials and Reagents
Table 3: Research Reagent Solutions for Biomarker Analysis
| Reagent/Equipment | Manufacturer/Catalog # | Function in Protocol |
|---|---|---|
| Next-generation sequencing panel | FoundationOne CDx or similar | Comprehensive genomic profiling for mutation detection |
| Immunohistochemistry antibodies | Various, target-specific | Protein expression analysis |
| PCR reagents for RT-PCR | ThermoFisher TaqMan | Rapid mutation detection in low DNA input samples |
| PD-L1 IHC companion diagnostic | Dako 22C3, Ventana SP142 | Immune checkpoint inhibitor selection |
| Circulating tumor DNA collection tubes | Streck cfDNA BCT | Liquid biopsy for genomic profiling |
| DNA/RNA extraction kits | Qiagen AllPrep | Nucleic acid isolation from FFPE tissue |
4.2.3 Procedure
- Sample Acquisition and Processing
- Obtain tumor tissue via core needle biopsy or surgical resection
- Process samples within 60 minutes of collection for optimal nucleic acid preservation
- Prepare formalin-fixed paraffin-embedded (FFPE) blocks with H&E staining for tumor content assessment
Nucleic Acid Extraction
- Extract DNA and RNA from FFPE sections with ≥20% tumor content
- Quantify nucleic acid concentration using fluorometric methods
- Assess quality metrics (DV200 for RNA, fragment size for DNA)
Molecular Analysis
- Perform next-generation sequencing using validated panels covering relevant biomarkers
- Establish variant calling thresholds with appropriate positive and negative controls
- Confirm actionable mutations with orthogonal methods when necessary
Companion Diagnostic Validation
- Establish analytical validation for companion diagnostic claims
- Determine positive/negative cutoffs using clinical samples
- Document sensitivity, specificity, and reproducibility metrics
Biomarker Analysis Workflow
This diagram illustrates the sequential process for biomarker analysis in master protocols, from sample collection through clinical reporting. The standardized workflow ensures reproducible molecular characterization for appropriate treatment assignment within the master protocol structure.
Confirmatory Evidence Generation Post-Approval
Protocol: Design of Confirmatory Trials for Verification of Clinical Benefit
Drugs approved via the AAP are subject to post-approval requirements to verify clinical benefit [75]. This conditional approval mechanism requires sponsors to submit protocols for confirmatory studies prior to full approval, ensuring continued evaluation of therapeutic efficacy through rigorous clinical investigation.
5.1.1 Confirmatory Trial Design Considerations
- Utilize overall survival (OS) or quality of life metrics as primary endpoints
- Implement randomized controlled designs when ethically feasible
- Incorporate patient-reported outcomes (PROs) to capture clinical benefit
- Establish hierarchical testing strategies for multiple endpoints
- Plan for interim analyses to potentially expedite full approval
5.1.2 Statistical Considerations
- Power calculations based on the magnitude of effect observed in the accelerated approval trial
- Alpha allocation between interim and final analyses
- Adjustments for cross-over and subsequent therapies
- Pre-specified subgroup analyses based on predictive biomarkers
Recent analyses of accelerated approvals in oncology reveal varying degrees of confirmatory trial success. In a cohort study evaluating 129 cancer drug-indication pairs granted accelerated approval from 2013 to 2023, among 46 indications with more than 5 years of follow-up, fewer than half (20/46, 43%) demonstrated a clinical benefit in confirmatory trials [75]. This outcome distribution underscores both the utility and limitations of surrogate endpoint-based approvals in predicting long-term clinical benefit.
Accelerated approval pathways, when integrated with master protocol designs, represent a powerful framework for expediting the development of promising oncology therapeutics. The case studies presented demonstrate how surrogate endpoints such as ORR and PFS can support regulatory approval when balanced against unmet medical needs in life-threatening malignancies.
The experimental protocols detailed provide standardized methodologies for generating the robust quantitative evidence required for accelerated approval, while maintaining scientific rigor through post-approval confirmatory trial requirements. As the field evolves, future refinements to AAPs may incorporate real-world evidence generation and adaptive trial designs to strengthen the evidentiary basis for regulatory decisions [75].
The integration of biomarker-driven patient selection and precision medicine approaches offers opportunities to enhance the predictive accuracy of surrogate endpoints while maintaining expedited access to transformative therapies for cancer patients with limited treatment options.
Conclusion
Master protocols represent a paradigm shift in oncology drug development, offering a robust, flexible, and efficient framework to match the complexity of modern cancer therapeutics. By consolidating multiple questions into a single infrastructure, these designs expedite the development of targeted treatments and devices, reduce resource burdens, and enhance patient centricity. The successful adoption of basket, umbrella, and platform trials, as evidenced by initiatives like Lung-MAP and I-SPY 2, demonstrates their tangible impact. Future directions will require continued ecosystem mobilization, wider adoption of novel dosage optimization strategies like those championed by Project Optimus, and the application of these designs to combination therapies and broader therapeutic areas. Embracing these efficient frameworks is crucial for delivering high-value innovations to cancer patients more rapidly.
References
- 1. Master Protocols in Oncology Trials [https://cytel.com/perspectives/master-protocols-in-oncology-trials/]
- 2. Current usage and challenges of master protocols—based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9577726/]
- 3. Master protocol: structuring pillar for clinical investigations. [https://www.multihealthgroup.com/en/master-protocol-the-cornerstone-of-clinical-trial-design/]
- 4. Platform Trials, Master Protocols, and Challenges in ... [https://cytel.com/perspectives/platform-trials-master-protocols-and-challenges-in-execution/]
- 5. New clinical trial design in precision medicine [https://www.nature.com/articles/s41392-024-01760-0]
- 6. Master Protocol Trial Design for Efficient and Rational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7073911/]
- 7. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 8. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 9. Novel Study Designs in Precision Medicine - Basket, Umbrella and Platform Trials - PubMed [https://pubmed.ncbi.nlm.nih.gov/34455953/]
- 10. Platform, Basket, and Umbrella Trial Designs - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK603602]
- 11. Basket Trials: Review of Current Practice and Innovations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10476732/]
- 12. An overview of precision oncology basket and umbrella trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7187272/]
- 13. Basket Clinical Trial Designs: The Key to Testing ... [https://acrpnet.org/2020/02/11/basket-clinical-trial-designs-the-key-to-testing-innovative-therapies-is-innovation-in-study-design-and-conduct]
- 14. Design and analysis of umbrella trials: Where do we stand? [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.1037439/full]
- 15. Platform trials: key features, when to use them and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318487/]
- 16. Master Protocols in Clinical Trials: The FDA's New Guidance [https://www.freyrsolutions.com/blog/master-protocols-in-clinical-trials-understanding-the-fdas-new-guidance]
- 17. Oncology Center of Excellence Guidance Documents [https://www.fda.gov/about-fda/oncology-center-excellence/oncology-center-excellence-guidance-documents]
- 18. Master Protocols for Drug and Biological Product ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/master-protocols-drug-and-biological-product-development]
- 19. M11 Template: Clinical Electronic Structured Harmonised ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m11-template-clinical-electronic-structured-harmonised-protocol-cesharp]
- 20. Clinical Trial Protocol Deviations: A New FDA Draft ... [https://www.ropesgray.com/en/insights/alerts/2025/01/clinical-trial-protocol-deviations-a-new-fda-draft-guidance-to-ring-in-the-new-year]
- 21. Master Protocols: Efficient Clinical Trial Design Strategies ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/master-protocols-efficient-clinical-trial-design-strategies-expedite-development-oncology-drugs-and]
- 22. Tumor-agnostic baskets to N-of-1 platform trials and real- ... [https://www.sciencedirect.com/science/article/abs/pii/S0305737224000215]
- 23. Dabrafenib plus trametinib in BRAFV600E-mutated rare ... [https://www.nature.com/articles/s41591-023-02321-8]
- 24. Dabrafenib plus trametinib in patients with BRAF ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/34838156/]
- 25. Biomarker-Driven Clinical Trials in Oncology [https://www.precisionformedicine.com/blog/biomarker-driven-clinical-trials-in-oncology-enrichment-stratification-all-comers-basket-when-to-use-what-and-why]
- 26. Lung-MAP 3.0 Expands Genomic Screening Options for ... [https://www.swog.org/news-events/news/2025/04/16/lung-map-30-expands-genomic-screening-options-patients]
- 27. Trial Results: ECOG-ACRIN and PrECOG Research at ASCO ... [https://blog-ecog-acrin.org/trial-results-ecog-acrin-and-precog-research-at-asco-2025/]
- 28. S2302 Pragmatica-Lung Reports Out at ASCO [https://www.swog.org/news-events/news/2025/06/06/s2302-pragmatica-lung-reports-out-asco]
- 29. Evaluating eligibility criteria of oncology trials using real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9007176/]
- 30. Clinical Data Visualizations | Tables Listings Figures (TLFs) [https://www.quanticate.com/visualizations]
- 31. I-SPY 2: a Neoadjuvant Adaptive Clinical Trial Designed to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7731787/]
- 32. Biomarkers Consortium - I-SPY TRIAL-2 (Investigation of ... [https://fnih.org/our-programs/biomarkers-consortium-i-spy-trial-2-investigation-of-serial-studies-to-predict-your-therapeutic-response-with-imaging-and-molecular-analysis-an-adaptive-breast-cancer-trial-design-in-the-setting/]
- 33. Immune Subtyping Identifies Patients With Hormone Receptor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12184982/]
- 34. Protein signaling and drug target activation signatures to ... [https://www.sciencedirect.com/science/article/pii/S2666379123005062]
- 35. Expression of carcinoma ecotypes in the tumor ... [https://www.nature.com/articles/s41598-025-28810-z]
- 36. Recent technical advancements and clinical applications of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259636/]
- 37. Overcoming Operational Challenges in Oncology ... [https://www.appliedclinicaltrialsonline.com/view/overcoming-operational-challenges-oncology-clinical-trials-lessons-multicentric-study-india]
- 38. Oncology Clinical Trials Operational Challenges [https://credevo.com/articles/2025/03/05/oncology-clinical-trials-key-operational-challenges-how-to-overcome-them/]
- 39. Barriers and facilitators to cancer clinical trial enrollment and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488194/]
- 40. ASCO 2025 Insights: Oncology Clinical Trends You Need ... [https://tfscro.com/resources/asco-2025-recap-oncology-clinical-trial-trends-cros-and-sponsors-need-to-know/]
- 41. Overcoming EHR-to-EDC Implementation Challenges in ... [https://theconferenceforum.org/webinars/overcoming-ehr-to-edc-implementation-challenges-in-oncology-trials]
- 42. A Quantitative Approach to Data Collection and Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12276416/]
- 43. Overcoming Retention Challenges in Oncology Trials [https://mdgroup.com/blog/from-burden-to-breakthrough-overcoming-retention-challenges-in-oncology-trials/]
- 44. Strategies to optimise patient engagement and retention in ... [https://www.clinicaltrialsarena.com/news/strategies-to-optimise-patient-engagement-and-retention-in-clinical-trials/]
- 45. The Trifecta of Protocol Review: Patients, Sites, and ... [https://theconferenceforum.org/editorial/the-trifecta-of-protocol-review-patients-sites-and-sponsors-building-better-studies]
- 46. Elevating Site Preparedness: Trends and Strategies for 2025 [https://www.wcgclinical.com/insights/elevating-site-preparedness-trends-and-strategies-for-2025/]
- 47. The Importance of Early and Ongoing Regulatory ... [https://www.worldwide.com/blog/2024/06/early-ongoing-regulatory-engagement-for-successful-clinical-trials/]
- 48. Oncology Regulatory Expertise and Early Guidance ... [https://www.fda.gov/about-fda/oncology-center-excellence/oncology-regulatory-expertise-and-early-guidance-oreeg]
- 49. FDA Draft Guidance on Overall Survival in Oncology Trials [https://www.precisionformedicine.com/blog/fda-draft-guidance-on-overall-survival-in-oncology-trials-what-sponsors-need-to-know]
- 50. Accelerating the Future of Oncology Drug Development [https://pubmed.ncbi.nlm.nih.gov/39808749/]
- 51. Oncology Consortia | Criterium CRO [https://www.criteriuminc.com/oncology-consortia/]
- 52. Ten Key Elements for Successful Operational Conduct of ... [https://www.linical.com/articles-research/ten-key-elements-for-successful-operational-conduct-of-oncology-clinical-trials?hsLang=en]
- 53. Real-World Evidence: Best Practices for Successful ... [https://acrpnet.org/2025/02/14/real-world-evidence-best-practices-for-successful-regulatory-engagements]
- 54. Global Regulatory Strategy for Oncology Programs [https://catalystcr.com/global-regulatory-strategy-to-guide-your-oncology-program/]
- 55. Statistical controversies in clinical research: requiem for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4551156/]
- 56. Clinical Trials e-Protocol Template/Tool - NIDCD - NIH [https://www.nidcd.nih.gov/research/clinical-studies/researchers-professionals/clinical-trials-e-protocol-template-tool]
- 57. Protocol Builder - UNC Research [https://research.unc.edu/systems/protocol-builder/]
- 58. Protocol Builder 2.0 with AI Assistant - Protocol Builder [https://protocolbuilderpro.com/]
- 59. Statistical innovations in clinical trial design with a focus on ... [https://www.sciencedirect.com/science/article/pii/S2274580725003346]
- 60. The Amendment Trap: Why 76% of Clinical Trials Face Six- ... [https://www.precisionformedicine.com/blog/the-amendment-trap-why-76-of-clinical-trials-face-six-figure-protocol-changes]
- 61. Strategies to boost statistical efficiency in randomized ... [https://pubmed.ncbi.nlm.nih.gov/40551565/]
- 62. New Predictions for 2025 [https://globalforum.diaglobal.org/issue/january-2025/additional-predictions-for-2025/]
- 63. From data to discovery: the impact of statistics in cancer ... [https://www.icr.ac.uk/about-us/icr-news/detail/from-data-to-discovery--the-impact-of-statistics-in-cancer-research]
- 64. Predicting clinical trial duration via statistical and machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12005917/]
- 65. Clinical Trial Velocity as a Signal for Predicting Drug ... [https://www.drugpatentwatch.com/blog/clinical-trial-velocity-as-a-signal-for-predicting-drug-approval-and-uptake/?srsltid=AfmBOopt-0FlwNPUf3cxd12NE3AHWaU8bKxVjR2urAi9rgAUiPB7S2Ks]
- 66. Streamlining and cycle time reduction of the startup phase of ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-4079-8]
- 67. Development of a protocol complexity tool - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395810/]
- 68. Development of a protocol complexity tool [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02652-9]
- 69. Oncology clinical trial complexity [https://clinicaltrialrisk.org/rct-complexity/oncology-trials/]
- 70. Navigating Complexity: Strategies to Accelerate Modern ... [https://www.appliedclinicaltrialsonline.com/view/navigating-complexity-strategies-accelerate-modern-clinical-trials]
- 71. Protocol Design and Performance Benchmarks by Phase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373886/]
- 72. Emerging Challenges in Oncology Trials: Enrollment ... [https://www.wcgclinical.com/insights/emerging-challenges-in-oncology-trials/]
- 73. The Challenge of Patient Enrollment in Clinical Trials [https://www.ncoda.org/news/the-challenge-of-patient-enrollment-in-clinical-trials/]
- 74. A Patient Focused Solution for Enrolling Clinical Trials in Rare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3754447/]
- 75. Accelerated Approval Pathways in Oncology: Balancing ... [https://www.linical.com/articles-research/accelerated-approval-pathways-in-oncology-balancing-speed-and-scientific-rigor?hsLang=en]