Molecular Techniques in Cancer Diagnostics: A Comprehensive Comparison for Precision Oncology
This article provides a systematic comparison of established and emerging molecular techniques for cancer diagnostics, tailored for researchers, scientists, and drug development professionals.
Molecular Techniques in Cancer Diagnostics: A Comprehensive Comparison for Precision Oncology
Abstract
This article provides a systematic comparison of established and emerging molecular techniques for cancer diagnostics, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of methods from PCR to Next-Generation Sequencing (NGS), details their specific applications in hereditary cancer testing, therapy selection, and minimal residual disease monitoring, and addresses key optimization challenges. A critical validation framework is presented to compare the analytical performance, clinical utility, and cost-effectiveness of these techniques, with an integrated analysis of how artificial intelligence is reshaping molecular diagnostics. The content synthesizes current evidence to guide technology selection, research direction, and clinical translation in the era of precision oncology.
The Molecular Toolkit: Core Principles and Technological Evolution in Cancer Diagnostics
The evolution of molecular diagnostics has fundamentally transformed cancer research and clinical practice, shifting the paradigm from traditional methods to advanced techniques capable of detecting biomarkers at the single-molecule level. This comparison guide objectively evaluates the performance of DNA-based and protein-based detection technologies, providing researchers with critical insights into their applications, limitations, and complementary roles in oncology. As liquid biopsy approaches gain prominence for non-invasive cancer detection, understanding the technical capabilities of these platforms becomes essential for advancing personalized medicine and improving patient outcomes through earlier detection and monitoring.
Performance Comparison of Molecular Detection Techniques
The table below summarizes the key performance characteristics of major molecular diagnostic techniques used in cancer research, highlighting their respective strengths and limitations.
Table 1: Performance Comparison of Cancer Diagnostic Techniques
| Technique | Biomarker Type | Sensitivity | Specificity | Variant Detection Limit | Key Applications | Major Limitations |
|---|---|---|---|---|---|---|
| Protein-based MCED [1] | Proteins/Antibodies | 100% (Overall); 100% (Stage I) | 97% (Overall) | N/A | Multi-cancer early detection, Tissue-of-origin identification | Limited to predefined protein panel; early validation stage |
| Digital PCR [2] | Nucleic Acids (DNA/RNA) | High for abundant mutations | High | 0.1% VAF | Circulating tumor DNA (ctDNA) detection, rare mutation identification | Limited multiplexing capability; sensitive to inhibitors |
| BEAMing [2] | Nucleic Acids (DNA) | Very High | Very High | 0.01% VAF | Ultra-sensitive ctDNA detection, rare variant quantification | Technically complex; labor-intensive; costly |
| qPCR [3] | Nucleic Acids (DNA/RNA) | Moderate | Moderate | 1-10% VAF | Gene expression analysis, mutation screening | Limited sensitivity for rare variants; requires calibration curves |
| Next-Generation Sequencing [3] | Nucleic Acids (DNA/RNA) | Variable (panel-dependent) | High | 1-5% VAF (standard); lower with deep sequencing | Comprehensive mutation profiling, biomarker discovery | Higher cost; complex data analysis; longer turnaround time |
Table 2: Tissue-of-Origin Accuracy of Protein-Based MCED Test [1]
| Cancer Type | Sample Size | Sensitivity | Specificity | TOO Accuracy |
|---|---|---|---|---|
| Breast | 61 | 100% | 96.6% | 98% |
| Lung | 43 | 100% | 97% | 98% |
| Colorectal | 13 | 100% | 100% | 98% |
| Ovarian | 13 | 100% | 100% | 98% |
| Pancreatic | 11 | 100% | 100% | 98% |
Experimental Protocols and Methodologies
Protein-Based Multi-Cancer Early Detection (MCED) Testing
Sample Preparation and Biomarker Panel [1]
- Sample Collection: Serum samples are procured from established biorepositories with documented informed consent and IRB approval. Samples from cancer patients with confirmed histological diagnosis prior to treatment and healthy controls are selected.
- Biomarker Analysis: A 16-parameter protein biomarker panel is analyzed, including:
- Extracellular Protein Kinase A (xPKA) activity quantified using MESACUP Protein Kinase Assay Kit
- Additional kinase activities measured with analogous assays
- Cancer-associated antibodies (IgG, IgM) quantified using standard ELISA protocols
- xPKA Activity Measurement: 108 μL serum samples are mixed with 12 μL activating buffer and incubated at room temperature for 30 minutes. Activated samples are combined with reaction buffer with/without protein kinase A inhibitor PKI. The mixture is incubated with immobilized peptide substrate for 30 minutes at 25°C with agitation. Peptide phosphorylation is detected using biotinylated phosphoserine antibodies followed by peroxidase-conjugated streptavidin with colorimetric TMB substrate detection.
Data Analysis and Classification [1]
- A supervised, rule-based classification framework is developed for cancer detection and tissue-of-origin assignment
- Initial pattern discovery utilizes quantitative biomarker distribution analysis through box plots and summary statistics
- Optimal threshold values for each biomarker are established where separation between groups is maximized
- Cancer-type-specific conditional rules are developed using if-then logic structures
- Cross-reactivity between cancer types is resolved through incorporation of additional biomarkers or fine-tuning threshold values
- Statistical analysis is performed using SAS Version 9.4 with cross-validation using 80-20 data splitting
Sample Partitioning
- The reaction mixture containing target nucleic acid, primers, and probes is segmented into numerous equally sized partitions
- Two primary methods are employed:
- Droplet Digital PCR: Reaction mixture is emulsified into thousands of water-in-oil droplets
- Microwell Arrays: Reaction mixture is distributed into plates containing tens of thousands of small wells
Amplification and Detection
- PCR amplification is performed within each partition
- Partitions with target DNA are differentiated from those without target based on fluorescence signal
- Target nucleic acid copy number per partition is determined using a Poisson model based on positive partitions and total partition count
- This binary approach (on/off) makes digital PCR more immune to factors affecting amplification efficiency compared to qPCR
Bead-Based Amplification
- Hundreds of millions of water-in-oil droplets are generated, each potentially containing a single target DNA molecule and a single magnetic bead
- Within each droplet, target DNA is amplified using PCR, resulting in thousands of copies attached to each bead
- Beads covered in amplified DNA are extracted from emulsion using magnetic separation techniques
Mutation Detection
- Beads are differentially stained with distinct fluorophores to identify mutant and wild-type DNA molecules
- Beads are counted using flow cytometry
- This approach achieves a limit of detection of 0.01%, an order of magnitude improvement over conventional digital PCR
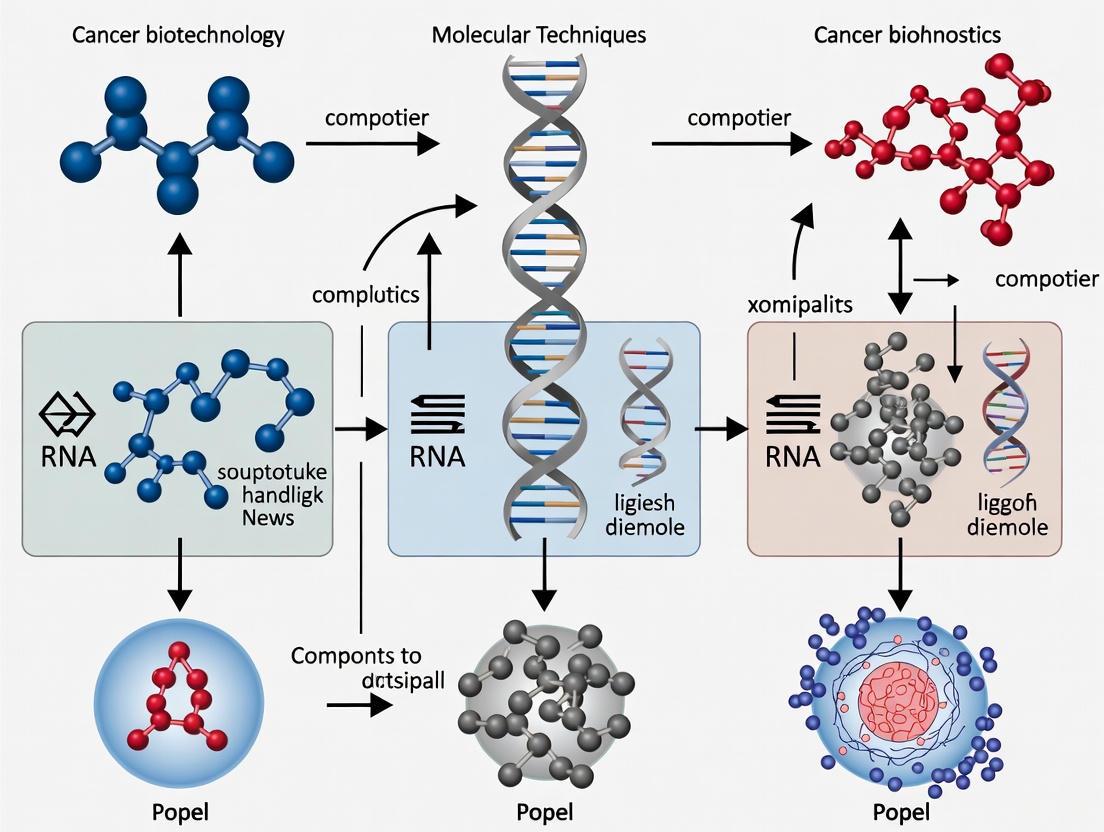
Visualization of Molecular Detection Workflows
Protein-Based MCED Test Workflow
Nucleic Acid Detection Techniques Comparison
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Molecular Cancer Diagnostics
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Protein Detection Reagents | MESACUP Protein Kinase Assay Kit [1] | Quantifies extracellular PKA activity in serum samples | Measures net xPKA activity with high reproducibility (3.7% CV) |
| Phosphoserine antibodies [1] | Detection of phosphorylated peptides in kinase assays | Used with peroxidase-conjugated streptavidin for colorimetric detection | |
| TMB substrate [1] | Colorimetric detection in ELISA-based protein assays | 60-minute incubation with acid stop solution; read at 450nm | |
| Nucleic Acid Amplification | PCR primers & probes [3] | Target-specific amplification in qPCR/digital PCR | Design critical for specificity; modified for real-time detection |
| Reverse transcriptase [3] | cDNA synthesis for RNA analysis in RT-PCR | Essential for analyzing gene expression biomarkers | |
| Sample Processing | Protein kinase inhibitors [1] | Specific inhibition in kinase activity assays | PKI inhibitor used at 0.5μM concentration for net activity calculation |
| Magnetic beads [2] | Nucleic acid capture in BEAMing technology | Enable single molecule to single bead conversion for ultra-sensitive detection | |
| Specialized Tools | SCOPE tool [4] | Targeted capture of DNA-binding proteins | Uses guide RNA and special amino acid (AbK) for UV-crosslinking |
| Mass spectrometry reagents [2] | Protein identification in novel tools | Used with SCOPE for identifying captured DNA-binding proteins |
Discussion and Future Perspectives
The comparison of molecular techniques reveals a complementary relationship between nucleic acid and protein-based approaches in cancer diagnostics. While DNA-based methods like digital PCR and BEAMing provide exceptional sensitivity for detecting rare mutations, protein-based MCED tests offer the advantage of direct functional relevance to cancer biology and robust early-stage detection [1] [2].
The emerging trend toward single-molecule detection sensitivity represents a significant advancement in molecular diagnostics [2]. These approaches overcome limitations of conventional techniques by detecting rare biomarkers that might be overlooked by ensemble averaging methods. The development of novel tools like SCOPE, which enables precise identification of DNA-binding proteins at specific genomic locations, further expands the toolkit available for cancer research [4].
For researchers and drug development professionals, the selection of appropriate diagnostic platforms should consider the specific application context. Nucleic acid techniques excel in tracking known mutations and monitoring treatment response, while protein-based approaches show promise in early detection across multiple cancer types where mutation profiles may not be predetermined. The integration of both approaches in complementary diagnostic strategies likely represents the future of comprehensive cancer detection and monitoring.
The invention of the Polymerase Chain Reaction (PCR) in 1986 revolutionized molecular biology by providing a means to exponentially amplify specific DNA sequences. [5] This foundational technique has since evolved through several generations, each enhancing quantitative capabilities and application scope. Second-generation quantitative PCR (qPCR), also known as real-time PCR, introduced fluorescence monitoring to enable nucleic acid quantification during amplification. [6] [5] Reverse Transcription PCR (RT-PCR) combines reverse transcription of RNA into complementary DNA (cDNA) with amplification, making it crucial for gene expression analysis and RNA virus detection. [6] The third generation, digital PCR (dPCR), provides absolute quantification by partitioning samples into thousands of individual reactions, representing the most significant recent advancement in PCR technology. [5] [7] Within cancer diagnostics, these techniques enable detection of genetic mutations, expression profiling, and monitoring of minimal residual disease through highly sensitive and specific molecular analysis.
Technology Comparison: Principles, Strengths, and Limitations
Core Principles and Workflows
Quantitative PCR (qPCR) monitors DNA amplification in real-time using fluorescent dyes or probes. The cycle at which fluorescence crosses a threshold (Cq or Ct value) is proportional to the initial target amount, quantified against a standard curve. [6] [8] RT-PCR begins with reverse transcription of RNA to cDNA followed by standard qPCR amplification, allowing quantification of RNA transcripts. [6] Digital PCR (dPCR) partitions a PCR reaction into thousands of nanoreactions, performs endpoint amplification, and applies Poisson statistics to the ratio of positive to negative partitions for absolute quantification without standard curves. [6] [5]
Comparative Performance Characteristics
Table 1: Technical comparison of PCR technologies for cancer research applications
| Parameter | qPCR | RT-PCR | dPCR |
|---|---|---|---|
| Quantification Method | Relative (requires standard curve) | Relative (requires standard curve) | Absolute (Poisson statistics) |
| Precision | ++ | ++ | +++ |
| Sensitivity | Detects down to <0.1% VAF [9] | Similar to qPCR | Superior for rare targets (<0.1%) [6] [8] |
| Dynamic Range | Large (up to 7-8 logs) [6] | Large | Limited by partition count [6] |
| Throughput | High (384-well format) [8] | High | Medium (up to 96 samples) [8] |
| Tolerance to Inhibitors | Moderate | Moderate | High [6] [8] |
| Multiplexing Capability | + | + | +++ [6] |
| Cost Considerations | Lower instrument and per-sample cost [8] | Similar to qPCR | Higher instrument cost, no standard curve needed [6] |
Table 2: Application suitability in cancer diagnostics research
| Application | Recommended Technology | Key Considerations |
|---|---|---|
| Gene Expression Profiling | qPCR/RT-PCR | High throughput, well-established protocols [9] |
| Rare Mutation Detection | dPCR | Superior sensitivity for variants <1% [6] [5] |
| Liquid Biopsy Analysis | dPCR | Excellent for low-abundance ctDNA [8] [10] |
| Copy Number Variation | qPCR/dPCR | dPCR offers absolute quantification [6] |
| Treatment Response Monitoring | qPCR/RT-PCR/dPCR | Choice depends on required sensitivity [11] |
| High-Throughput Screening | qPCR/RT-PCR | 384-well format, automation friendly [8] [9] |
Key Advantages and Limitations
qPCR/RT-PCR Advantages: Established gold standard with extensive validated protocols; superior throughput with 384-well formats; lower initial investment and operational costs; broad dynamic range suitable for most applications; capable of detecting fold changes greater than 2-fold. [6] [8] [9]
qPCR/RT-PCR Limitations: Requires standard curves for quantification; relatively lower precision for small fold differences (<2-fold); more susceptible to PCR inhibitors; limited sensitivity for very rare targets (<0.1%). [6] [12]
dPCR Advantages: Absolute quantification without standard curves; higher precision and reproducibility; superior sensitivity for rare targets; enhanced tolerance to inhibitors; better performance for complex samples. [6] [8] [5]
dPCR Limitations: Lower throughput; higher instrument costs; limited dynamic range requiring sample dilution for high concentrations; more expensive consumables. [6] [8] [12]
Experimental Data and Performance Benchmarks in Cancer Research
Sensitivity and Detection Limits
dPCR demonstrates superior sensitivity for low-abundance targets critical in cancer diagnostics. In studies comparing BCR-ABL1 monitoring for chronic myeloid leukemia, dPCR reliably quantified low-level transcript copies but required protocol adaptations to surpass qPCR sensitivity at very low levels (<0.1% BCR-ABL1IS). [11] For liquid biopsy applications, dPCR can detect mutant alleles in circulating tumor DNA (ctDNA) at frequencies as low as 0.001%, significantly below qPCR capabilities. [6] [5] This exceptional sensitivity enables earlier detection of residual disease and emerging treatment resistance.
Precision and Reproducibility
dPCR provides significantly improved precision, with much lower coefficients of variation compared to qPCR. [6] This enhanced reproducibility stems from dPCR's binary detection system and resistance to amplification efficiency variations. In copy number variation studies, dPCR can resolve differences below the twofold limit of qPCR, providing tighter confidence intervals with fewer replicates. [6] This precision is particularly valuable for longitudinal monitoring of cancer patients where small changes in biomarker levels have clinical significance.
Tolerance to Complex Samples
dPCR demonstrates superior performance with challenging sample types common in cancer research. Partitioning the reaction mixture dilutes inhibitors present in clinical samples like plasma, FFPE tissues, and liquid biopsies, maintaining amplification efficiency where qPCR would be compromised. [6] [8] This robustness makes dPCR particularly valuable for analyzing samples with high background DNA, such as detecting rare mutations in liquid biopsies where wild-type sequences vastly outnumber mutant alleles. [6]
Experimental Protocols for Cancer Research Applications
qPCR Protocol for Gene Expression Analysis in Tumor Tissues
Sample Preparation: Extract total RNA from fresh-frozen or FFPE tumor tissues using silica-membrane columns with DNase treatment. Assess RNA quality and concentration spectrophotometrically. [9]
Reverse Transcription: Convert 500ng-1μg total RNA to cDNA using reverse transcriptase with oligo(dT) and/or random hexamer primers in 20μL reaction volume. [6]
qPCR Setup: Prepare reactions with cDNA template, target-specific primers/probes, and qPCR master mix. Run samples in triplicate alongside standard curves and no-template controls. [6] [9]
Thermal Cycling: Initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 60°C for 1 minute on a real-time PCR instrument. [9]
Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method with normalization to reference genes. [6]
dPCR Protocol for Rare Mutation Detection in Liquid Biopsies
Cell-Free DNA Extraction: Isolate ctDNA from plasma using specialized circulating nucleic acid kits. Quantify using fluorometry. [5]
Assay Design: Design primer-probe sets to specifically detect mutant alleles while minimizing wild-type amplification. Include appropriate controls. [6]
Partitioning: Mix dPCR supermix, template DNA, and assays. Load onto dPCR plates for automated partitioning into nanoscale reactions. [8] [5]
Amplification: Perform endpoint PCR amplification with optimized cycling conditions for the partition system. [5]
Reading and Analysis: Count positive and negative partitions using fluorescence detection. Apply Poisson correction for absolute quantification of mutant alleles. [6] [5]
Technology Selection Guide for Cancer Research Applications
Decision Factors for Technology Selection
Choose qPCR/RT-PCR when: Processing large sample numbers requiring high throughput; conducting relative quantification with available standards; working with moderate to high abundance targets; operating with budget constraints; requiring established, validated protocols for regulated environments. [8] [9]
Choose dPCR when: Absolute quantification without standards is essential; detecting rare mutations or low-abundance targets (<1%); working with inhibitor-containing samples; requiring maximum precision and reproducibility; analyzing copy number variations with high precision. [6] [8] [10]
Essential Research Reagents and Materials
Table 3: Essential research reagents for PCR-based cancer diagnostics
| Reagent Category | Specific Examples | Function in Workflow |
|---|---|---|
| Nucleic Acid Extraction | Circulating nucleic acid kits, FFPE RNA/DNA kits, magnetic bead-based systems | Isolation of high-quality nucleic acids from clinical specimens [13] [9] |
| Reverse Transcriptase | Moloney murine leukemia virus (M-MLV), avian myeloblastosis virus (AMV) | cDNA synthesis from RNA templates for RT-PCR [6] |
| PCR Master Mixes | Hot-start polymerases, inhibitor-resistant enzymes, probe-based mixes | Provides core components for amplification with enhanced specificity [9] |
| Fluorescent Probes/Dyes | Hydrolysis probes (TaqMan), molecular beacons, intercalating dyes (SYBR Green) | Detection and quantification of amplified products [6] [5] |
| Reference Standards | Synthetic oligonucleotides, gBlocks, reference genes (GAPDH, ACTB) | Standard curves for qPCR, quality control, normalization [6] |
| Partitioning Reagents | Droplet generation oil, surfactants, nanowell chips | Creation of individual reaction chambers for dPCR [5] |
Future Perspectives and Emerging Trends
PCR technologies continue evolving to address emerging needs in cancer diagnostics. Microfluidic integration is enabling miniaturized dPCR systems with higher partition densities and reduced costs. [5] [7] Multiplexing capabilities are expanding with advanced probe chemistries allowing simultaneous quantification of multiple targets from limited samples. [6] [9] Artificial intelligence and machine vision applications are enhancing data analysis accuracy, particularly for dPCR partition classification. [7] The convergence of PCR with point-of-care testing through isothermal methods and portable systems promises to decentralize cancer molecular diagnostics. [12] [7] As cancer diagnostics increasingly relies on liquid biopsies and minimal residual disease monitoring, dPCR's exceptional sensitivity positions it as a cornerstone technology, while qPCR remains the workhorse for high-throughput applications requiring robust, cost-effective solutions. [6] [5] [9]
Next-Generation Sequencing (NGS) represents a paradigm shift in molecular analysis, enabling the simultaneous sequencing of millions to billions of DNA fragments in a single run [14] [15]. This massive parallelism, the core principle of NGS technology, has fundamentally transformed biomedical research and clinical diagnostics by providing unprecedented throughput, speed, and cost-efficiency compared to traditional Sanger sequencing [14] [16]. Often termed massively parallel sequencing, NGS has reduced the cost of genome sequencing by over 96%, making large-scale genomic studies and routine clinical application a practical reality [14]. The technology's versatility allows for comprehensive profiling across multiple molecular layers—including the genome, transcriptome, and epigenome—making it an indispensable tool in the era of precision medicine, particularly in oncology [17] [15].
The following diagram illustrates the core NGS workflow, from sample preparation to data analysis, highlighting the parallel processing of millions of DNA fragments.
Figure 1: The Core NGS Workflow. This process demonstrates the transformation of a biological sample into actionable genetic data through massive parallel sequencing.
NGS Versus Traditional Sequencing Methods
The transition from Sanger sequencing to NGS represents one of the most significant technological advancements in modern biology. While Sanger sequencing, developed in the 1970s, provides high accuracy for reading single DNA fragments, its low throughput makes large-scale projects like whole-genome sequencing prohibitively time-consuming and expensive [14] [16]. The Human Genome Project, which relied on Sanger sequencing, took over a decade and cost nearly $3 billion to complete [14]. In contrast, NGS can sequence an entire genome in days for under $1,000, demonstrating a dramatic improvement in efficiency and accessibility [14].
The table below provides a detailed comparison of these sequencing technologies across critical performance parameters.
Table 1: Performance Comparison: Sanger Sequencing vs. Next-Generation Sequencing
| Feature | Sanger Sequencing | Next-Generation Sequencing (NGS) |
|---|---|---|
| Throughput | Low (single fragment per reaction) | Ultra-high (millions to billions of fragments per run) [14] |
| Cost per Genome | High (billions for Human Genome Project) | Significantly lower (96% decrease, under $1,000) [14] |
| Speed | Slow (days for individual genes) | Rapid (whole genomes in days, targeted panels in hours) [14] |
| Accuracy | Very high (gold standard for validation) | High, with deep coverage providing robust variant detection [14] |
| Scalability | Limited to small regions or single genes | Highly scalable, from targeted panels to whole genomes [14] |
| Primary Clinical Utility | Ideal for sequencing single genes or validating specific mutations [16] | Detects a broad spectrum of mutations and structural variants; essential for comprehensive genomic profiling [16] [17] |
This comparative advantage makes NGS uniquely suited for comprehensive genomic profiling (CGP) in oncology, where it can simultaneously analyze hundreds of cancer-related genes to identify targetable mutations, resistance mechanisms, and biomarkers like tumor mutational burden (TMB) from a single, often limited, tissue sample [17] [18].
Experimental Protocols for NGS in Cancer Research
Implementing NGS in a research or diagnostic setting requires a rigorous, multi-stage process to ensure the generation of high-quality, reliable data. The following section details the standard protocols for key NGS applications in cancer genomics.
Protocol for Targeted Gene Panel Sequencing (e.g., for Solid Tumors)
Objective: To identify somatic mutations, copy number variations (CNVs), and gene fusions in a defined set of cancer-related genes from formalin-fixed, paraffin-embedded (FFPE) tumor tissue or liquid biopsy samples [17].
Step-by-Step Workflow:
- Nucleic Acid Extraction: Extract and quantify high-quality DNA from the tumor sample. For FFPE tissue, assess DNA fragmentation and degradation. For liquid biopsy, isolate cell-free DNA (cfDNA) from plasma [17].
- Library Preparation:
- Fragmentation: Use enzymatic or physical methods to shear DNA into fragments of 100-800 base pairs [14].
- Adapter Ligation: Attach platform-specific adapter sequences to both ends of each fragment. These adapters contain molecular barcodes (indexes) to allow for multiplexing—pooling multiple samples in a single sequencing run [14] [16].
- Target Enrichment: Hybridize the library to biotinylated RNA or DNA probes designed to capture exons of several hundred cancer-associated genes. Wash away non-hybridized fragments and elute the enriched target DNA. This step is crucial for focusing sequencing power on relevant genomic regions [14] [17].
- PCR Amplification: Amplify the enriched library to generate enough material for sequencing [14].
- Sequencing: Load the final library onto a sequencer (e.g., Illumina, Ion Torrent). The system performs clonal amplification (e.g., via bridge amplification on a flow cell) and sequencing-by-synthesis, generating millions of short reads [14] [16] [15].
- Data Analysis:
- Primary Analysis: Base calling and quality score (e.g., Q30, indicating 99.9% accuracy) assignment [14].
- Secondary Analysis: Align reads to a reference genome (e.g., GRCh38) and perform variant calling to identify SNPs, indels, and CNVs, generating a Variant Call Format (VCF) file [14].
- Tertiary Analysis & Interpretation: Annotate variants using databases (e.g., dbSNP, ClinVar), filter results, and classify variants according to guidelines (e.g., ACMG) into categories such as Pathogenic, Benign, or Variant of Uncertain Significance (VUS) [14].
Protocol for Whole-Genome Bisulfite Sequencing (WGBS) for Epigenomics
Objective: To generate a single-base resolution map of DNA methylation (5-methylcytosine, 5mC) across the entire genome [19].
Step-by-Step Workflow:
- DNA Extraction & Quality Control: Isolate genomic DNA and ensure high molecular weight and purity.
- Library Preparation & Bisulfite Conversion:
- Fragment DNA and prepare a standard NGS library with adapters.
- Treat the library with sodium bisulfite. This chemical conversion deaminates unmethylated cytosines to uracils (which are read as thymines during sequencing), while leaving methylated cytosines unchanged [19].
- Sequencing: Perform deep whole-genome sequencing on the converted library. This requires high coverage to confidently call methylation status.
- Data Analysis:
- Map the bisulfite-converted reads to a reference genome using specialized aligners that account for C-to-T conversions.
- Calculate the methylation percentage at each cytosine position by comparing the number of reads reporting a C (methylated) versus a T (unmethylated) [19].
Key NGS Applications in Cancer Diagnostics and Research
NGS has become the cornerstone of precision oncology, enabling a multi-faceted approach to understanding and treating cancer. Its applications span from comprehensive tissue analysis to non-invasive monitoring.
Comprehensive Genomic Profiling (CGP) in Tissue
CGP utilizes NGS to detect a wide range of alterations—including point mutations, indels, CNVs, gene fusions, and microsatellite instability (MSI)—across a large panel of genes in a single assay [17]. This approach is more efficient than sequential single-gene tests, conserving precious tissue samples and accelerating diagnostic turnaround times. CGP is critical for identifying actionable mutations that can be matched with targeted therapies, such as EGFR inhibitors in lung cancer or PARP inhibitors in BRCA-mutated cancers [16] [17]. It also enables the calculation of tumor mutational burden (TMB), a biomarker for response to immunotherapy [18].
Liquid Biopsy and Circulating Tumor DNA (ctDNA) Analysis
Liquid biopsy involves the sequencing of circulating tumor DNA (ctDNA)—fragmented DNA released by tumor cells into the bloodstream [17]. NGS-based liquid biopsy offers a non-invasive method for cancer detection, genotyping, and monitoring treatment response. Key applications include:
- Identifying Actionable Mutations: Detecting targetable mutations from blood, especially when tissue biopsy is unfeasible [17].
- Monitoring Treatment Response: Serial tracking of ctDNA levels and mutation profiles (e.g., variant allele frequency (VAF)) to assess therapy efficacy and detect the emergence of resistance mechanisms earlier than radiographic imaging [17].
- Minimal Residual Disease (MRD) Detection: Identifying molecular evidence of residual cancer after curative-intent treatment, predicting risk of relapse [16] [17].
The following diagram outlines the typical workflow for applying NGS in cancer research, from sample choice to clinical decision-making.
Figure 2: NGS Applications in Cancer Research and Clinical Decision-Making. This workflow shows how different sample types and NGS applications generate specific data types that inform clinical actions.
The Scientist's Toolkit: Essential Reagents and Platforms
Selecting the appropriate reagents and technologies is fundamental to successful NGS experimentation. The table below catalogs key solutions and their functions for NGS-based cancer genomics studies.
Table 2: Research Reagent Solutions for NGS-Based Cancer Genomics
| Category | Item | Function in the NGS Workflow |
|---|---|---|
| Library Preparation | Fragmentation Enzymes | Shears DNA into uniformly sized fragments for optimal sequencing [14]. |
| Adapter Oligos & Ligation Kits | Attaches platform-specific sequences to DNA fragments for binding and indexing [14] [16]. | |
| Hybridization Capture Probes | Enriches for target genomic regions (e.g., cancer gene panels) from a whole-genome library [14] [17]. | |
| Methylation-Specific Kits | Contains reagents for bisulfite conversion and library preparation for epigenomic studies [19]. | |
| Sequencing Platforms | Illumina (e.g., NovaSeq) | Uses sequencing-by-synthesis with reversible dye-terminators for high-throughput, accurate short-read sequencing [20] [15]. |
| Ion Torrent (e.g., Genexus) | Employs semiconductor sequencing detecting pH change during nucleotide incorporation; known for rapid turnaround [20] [15]. | |
| PacBio (HiFi) | Provides long-read sequencing with high accuracy (>99.9%), ideal for resolving complex structural variants and phasing [20] [15]. | |
| Oxford Nanopore (e.g., MinION) | Offers real-time, long-read sequencing by measuring electrical current changes as DNA passes through a nanopore [20] [15]. | |
| Bioinformatics Tools | Alignment Software (e.g., BWA) | Maps sequence reads to a reference genome to determine their genomic origin [14]. |
| Variant Callers (e.g., GATK) | Identifies mutations (SNPs, indels) by comparing the aligned sample sequence to the reference [14]. | |
| Annotation Databases (e.g., ClinVar, COSMIC) | Provides biological and clinical context for identified variants to aid interpretation [14] [17]. |
Next-Generation Sequencing has unequivocally established itself as the technological backbone of modern genomic medicine. Its ability to provide comprehensive, high-resolution insights into the genome, transcriptome, and epigenome from minimal sample input has made it particularly transformative for cancer research and diagnostics [14] [17] [18]. By enabling Comprehensive Genomic Profiling and non-invasive liquid biopsy monitoring, NGS guides therapeutic decisions, monitors treatment efficacy, and detects resistance, thereby fulfilling the core promise of precision oncology [16] [17].
While challenges related to data interpretation, standardization, and accessibility remain, ongoing advancements in sequencing chemistry, bioinformatics, and the integration of long-read technologies continue to push the boundaries [17] [15]. The future of NGS lies in its deeper integration with other 'omics' data and its evolution into a more accessible, automated tool that can deliver actionable insights for an ever-broader population of cancer patients, ultimately improving outcomes through molecularly driven care.
The tumor immune microenvironment (TIME) is a complex ecosystem comprising cancer cells, immune cells, stromal cells, and extracellular matrix components that collectively dictate tumor progression, therapeutic response, and patient outcomes [21]. Molecular imaging has emerged as an indispensable tool for visualizing and quantifying these dynamic interactions in vivo, providing non-invasive, real-time, and longitudinal insights that are transforming cancer diagnostics and therapeutic monitoring [22] [21]. By targeting specific biological processes within the TIME, imaging probes enable researchers and clinicians to move beyond anatomical assessment to functional and molecular characterization, paving the way for personalized medicine approaches in oncology [23] [24].
This guide provides a comprehensive comparison of three cornerstone molecular imaging modalities—Positron Emission Tomography (PET), Single-Photon Emission Computed Tomography (SPECT), and Magnetic Resonance Imaging (MRI)—for visualizing the TIME. We objectively evaluate their performance characteristics, present supporting experimental data, and detail methodologies for key applications, equipping researchers with the practical knowledge needed to select appropriate techniques for specific research questions in cancer immunology and drug development.
Comparative Analysis of Imaging Modalities
The following table summarizes the fundamental principles, strengths, and limitations of PET, SPECT, and MRI for probing the tumor immune microenvironment.
Table 1: Technical Comparison of Molecular Imaging Modalities for TIME Analysis
| Feature | PET | SPECT | MRI |
|---|---|---|---|
| Underlying Principle | Detects gamma rays from positron-emitting radiotracers [22] | Detects gamma rays from single-photon emitting radiotracers [21] | Utilizes magnetic fields and radio waves to image proton density/relaxation [22] [21] |
| Sensitivity | High (pM-nM range for tracers) [25] | Moderate (nM range) [25] | Low (μM-mM range) [21] |
| Spatial Resolution | Moderate (4–6 mm) [25] | Low (8–10 mm) [25] | High (μm-mm range) [21] |
| Tissue Penetration | Unlimited | Unlimited | Unlimited |
| Quantification Capability | Excellent (absolute quantification possible) | Good (semi-quantitative) | Variable (semi-quantitative) |
| Molecular Probe Types | Radiotracers (e.g., [¹⁸F], [¹¹C], [⁶⁸Ga]) [23] [26] | Radiotracers (e.g., [⁹⁹mTc], [¹¹¹In]) [21] | Paramagnetic/ superparamagnetic agents (e.g., Gd-, Fe-based) [24] [21] |
| Key Advantage | High sensitivity for tracking immune cell trafficking and receptor expression | Versatility for multi-probe imaging; wider tracer availability | Exceptional soft-tissue contrast and anatomical detail without ionizing radiation [21] |
| Primary Limitation | Limited anatomical context (requires CT/MRI fusion) [21] | Lower resolution and sensitivity vs. PET [21] | Low molecular sensitivity; longer acquisition times [21] |
| Representative Applications in TIME | Immunometabolism ([¹⁸F]FDG), T-cell activation ([⁸⁹Zr]CD8+ mAb) [22] | Imaging macrophage activity, vascular leakage | Visualizing immune cell infiltration via iron oxide nanoparticles [21] |
Targeted Molecular Probes and Their Applications
This section details specific molecular probes for key TIME components, comparing their performance across modalities with supporting experimental data.
Table 2: Comparison of Molecular Probes for Targeting TIME Components
| TIME Target / Process | Probe Name | Imaging Modality | Target / Mechanism | Key Experimental Findings & Performance Data |
|---|---|---|---|---|
| T-cell Infiltration | [⁸⁹Zr]CD8+ mAb | PET/CT | Binds to CD8+ T-cell surface markers | Non-invasive assessment of CD8+ tumor infiltration levels in patients undergoing immunotherapy for solid tumors [22]. |
| Immunometabolism | [¹⁸F]FDG | PET/CT | Marker of glucose metabolism (glycolysis) | High prognostic value in lymphoma; used with Deauville criteria [23]. AUCs >0.85 reported for predicting response to ICIs in HCC [25]. |
| Oxidative Stress | [¹⁸F]FSPG | PET | Substrate for system xc- (cystine-glutamate antiporter) | In animal models, changes in uptake preceded glycolytic changes ([¹⁸F]FDG) and tumor volume changes on CT [23]. |
| Cancer-Associated Fibroblasts (CAFs) | [⁶⁸Ga]FAPI-46 | PET/CT | Inhibits Fibroblast Activation Protein (FAP) on CAFs | Predictor of short overall survival in solid tumours [23]. In breast cancer NAC, uptake changes after 2 cycles predicted pathological complete response [23]. |
| Receptor Tyrosine Kinases (HER2) | [⁸⁹Zr]Trastuzumab | PET/CT | Binds to HER2 receptor | In the ZEPHIR trial (HER2+ breast cancer), HER2 PET/CT combined with early [¹⁸F]FDG metabolic response predicted T-DM1 treatment success [23]. |
| Extracellular Matrix (Collagen) | [⁶⁸Ga]Ga-CBP8 | PET/MRI | Binds to collagen deposits | Strong correlation between tumour collagen deposition and probe uptake in PDAC mice and patients, showing potential for monitoring chemotherapy response [21]. |
| Extracellular Matrix (Collagen) | EP-3533 | MRI | Gadolinium-based collagen-binding probe | Enhanced MRI signals indicating collagen deposition in LNCaP prostate tumors, validated histologically [21]. |
Experimental Protocols for Key Applications
Protocol 1: Assessing Treatment Response with [⁶⁸Ga]FAPI PET/CT in Breast Cancer
- Tracer: [⁶⁸Ga]FAPI-46 [23].
- Imaging Schedule: Baseline PET/CT scan prior to neoadjuvant chemotherapy (NAC), followed by a second scan after two cycles of NAC [23].
- Image Analysis: Quantify tracer uptake in tumors using standardized uptake values (SUVmax or SUVmean). Calculate the percentage change in SUV between baseline and follow-up scans.
- Outcome Correlation: A significant decrease in [⁶⁸Ga]FAPI uptake after two cycles was found to be predictive of achieving a pathological complete response (pCR) at surgery, allowing for early identification of responders [23].
Protocol 2: Visualizing Collagen Remodeling in the TME with [⁶⁸Ga]Ga-CBP8 PET/MRI
- Tracer: [⁶⁸Ga]Ga-CBP8, a collagen-binding peptide [21].
- Imaging Procedure: Perform simultaneous PET/MRI imaging. The MRI component provides high-resolution anatomical localization of the pancreas/tumor.
- Quantification: Draw volumes of interest (VOIs) around the tumor on fused PET/MRI images. Measure mean standardized uptake values (SUVmean) within the VOI.
- Validation: In murine models of pancreatic ductal adenocarcinoma (PDAC), a strong positive correlation was observed between PET signal and ex vivo histological quantification of collagen deposition (e.g., via Picrosirius Red staining). This protocol successfully detected FOLFIRINOX chemotherapy-induced collagen accumulation in a PDAC patient [21].
Protocol 3: Imaging CD8+ T-cell Infiltration with [⁸⁹Zr]CD8+ mAb PET/CT
- Tracer: [⁸⁹Zr]-labeled anti-CD8+ monoclonal antibody [22].
- Subject Preparation: Patients undergoing immune checkpoint inhibitor therapy for solid tumors.
- Image Acquisition: Whole-body PET/CT scans are acquired at a predetermined time point (e.g., 24-48 hours) post-injection to allow for tracer biodistribution and target binding.
- Data Analysis: The level of CD8+ T-cell infiltration is assessed non-invasively by quantifying tracer uptake in tumors and, potentially, in lymphoid organs. This data provides crucial insights for predicting and monitoring immunotherapy response [22].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for TIME Molecular Imaging
| Item / Reagent | Function / Application |
|---|---|
| Radiolabeled Precursors | Foundation for synthesizing PET and SPECT tracers (e.g., [¹⁸F]fluoride, [⁶⁸Ga]GaCl₃) [24]. |
| Chelators | Chemically link radioactive metals to targeting biomolecules (e.g., DOTA, NOTA for [⁶⁸Ga]) [24]. |
| Targeting Ligands | Provide specificity to molecular probes. Includes antibodies, peptides, aptamers, and small molecules [24]. |
| Contrast Agents | Enhance signal for MRI (e.g., Gadolinium-based) [24]. |
| Cell Tracking Agents | Label immune cells ex vivo for subsequent in vivo tracking (e.g., [⁸⁹Zr]Oxine, FeO nanoparticles) [21]. |
| Ex Vivo Validation Kits | Confirm imaging findings via IHC/IF staining for CD8, CD4, FoxP3, FAP, PD-L1, and collagen. |
Visualizing Experimental Workflows and Biological Pathways
The following diagrams illustrate a generalized workflow for probe development and a key immunometabolic pathway, respectively.
Diagram 1: Probe Development Workflow
Diagram 2: Key Immunometabolic Imaging Targets
Liquid biopsy represents a transformative approach in oncology, enabling the minimally invasive detection and monitoring of cancer through the analysis of tumor-derived components in bodily fluids [27]. Unlike traditional tissue biopsies, which can be invasive, difficult to repeat, and fail to capture tumor heterogeneity, liquid biopsies offer a dynamic snapshot of the tumor's genetic landscape through a simple blood draw [27] [28]. The concept centers on analyzing circulating biomarkers, with circulating tumor DNA (ctDNA) emerging as the most promising analyte due to technological advances in DNA analysis [28].
ctDNA consists of short DNA fragments shed into the bloodstream by tumor cells through apoptosis or necrosis [29]. It circulates as part of cell-free DNA (cfDNA) but constitutes only a small fraction (approximately 0.1% to 1.0%) of the total cfDNA in cancer patients, presenting significant detection challenges [27] [30]. The half-life of ctDNA is relatively short (approximately 1-2.5 hours), making it a dynamic biomarker capable of providing real-time information on tumor burden and treatment response [27]. The detection of tumor-specific alterations in ctDNA—including somatic mutations, copy number variations, epigenetic changes, and fragmentation patterns—enables cancer detection, molecular profiling, and monitoring [28] [29].
Molecular Techniques for ctDNA Analysis
Comparison of Detection Platforms
The analysis of ctDNA requires highly sensitive methods due to its low concentration in blood. Currently, two main technological approaches dominate the field: PCR-based methods and next-generation sequencing (NGS). Each offers distinct advantages and limitations for different clinical and research applications [28].
Table 1: Comparison of Major ctDNA Detection Platforms
| Technology | Key Variants | Sensitivity | Multiplexing Capacity | Primary Applications | Cost & Turnaround Time |
|---|---|---|---|---|---|
| PCR-Based | ddPCR, BEAMing | VAF 0.01%-0.1% | Low (1-few mutations) | Treatment monitoring, MRD detection | Lower cost, Rapid (hours-days) |
| NGS | Targeted Panels, WGS, WES | VAF 0.1%-1% (varies) | High (dozens-hundreds of genes) | Comprehensive profiling, biomarker discovery | Higher cost, Longer (days-weeks) |
| Emerging Methods | Methylation Analysis, Fragmentomics | Varies | Moderate to High | Early detection, cancer origin determination | Research phase, costs varying |
PCR-based platforms, particularly droplet digital PCR (ddPCR) and BEAMing (beads, emulsion, amplification, magnetics), provide exceptional sensitivity for detecting low-frequency mutations (as low as 0.01% variant allele frequency, VAF) [28]. These methods are ideal for tracking known mutations during treatment or monitoring for minimal residual disease (MRD) [30]. However, their utility is limited to assessing a small number of predefined mutations, restricting comprehensive genomic profiling [28].
NGS-based approaches enable broad genomic profiling through targeted panels, whole-exome sequencing (WES), or whole-genome sequencing (WGS) [28]. These methods can simultaneously assess hundreds of cancer-associated genes, capturing single nucleotide variants (SNVs), insertions/deletions (Indels), copy number variations (CNVs), and structural variants (SVs) [29]. While traditional NGS struggles with very low VAFs (<0.1%), advanced error-suppression techniques and unique molecular identifiers have significantly improved sensitivity [29].
Recent technological innovations include methylation analysis, which examines DNA methylation patterns to distinguish cancer-derived DNA, and fragmentomics, which leverages the observation that ctDNA fragments exhibit different size distributions and end motifs compared to non-cancer cfDNA [28]. Machine learning approaches integrating multiple analytical methods (genomic, epigenomic, fragmentomic) have demonstrated enhanced sensitivity for early cancer detection [28].
Workflow Diagrams for ctDNA Analysis
Figure 1: Overall Workflow for ctDNA Analysis
Figure 2: ddPCR Workflow for Targeted Mutation Detection
Figure 3: NGS Workflow for Comprehensive Genomic Profiling
Performance Comparison: Experimental Data and Protocols
Analytical Sensitivity Across Platforms
Recent comparative studies have systematically evaluated the performance of different ctDNA detection platforms. A 2024 comprehensive evaluation of nine ctDNA assays revealed significant variations in sensitivity, specificity, and reproducibility, particularly at lower DNA inputs and variant allele frequencies [29].
Table 2: Performance Metrics of ctDNA Detection Platforms Across Studies
| Study & Context | Technology | Sensitivity | Specificity | Key Findings | Limitations |
|---|---|---|---|---|---|
| Rectal Cancer (2025) [30] | ddPCR | 58.5% (pre-therapy) | High (not specified) | Higher detection in advanced stages; superior to NGS for localized cancer | Postoperative detection failed before most recurrences |
| NGS | 36.6% (pre-therapy) | High (not specified) | Lower detection rate vs. ddPCR (p=0.00075) | Less sensitive for MRD detection | |
| Melanoma Meta-analysis (2022) [31] | Various ctDNA assays | Pooled: 73% | Pooled: 94% | AUC 0.93 (92.87% accuracy vs. gold standard) | Sensitivity varied by country, sample source, method |
| 9-Assay Evaluation (2024) [29] | Multiple NGS assays | VAF 0.5%: ~95% (most assays) | Generally high (assay-dependent) | Sensitivity dropped substantially at VAF 0.1%; input amount critical | Inter-assay variability, especially at low VAF |
| Lung Adenocarcinoma (2021) [32] | Tissue NGS (benchmark) | 94.8% | Not specified | Detected significantly more clinically relevant alterations | Invasive procedure required |
| Plasma NGS | 52.6% (p<0.001) | Not specified | Useful when tissue unavailable | Low sensitivity limits standalone use |
A direct comparison between ddPCR and NGS in localized rectal cancer demonstrated that ddPCR detected ctDNA in 58.5% of pre-therapy plasma samples compared to 36.6% with NGS (p = 0.00075) [30]. This performance advantage was particularly evident in patients with higher clinical tumor stage and lymph node positivity [30]. The study employed a tumor-informed approach where mutations identified in tumor tissue NGS were subsequently tracked in plasma using custom ddPCR assays [30].
The 2024 multi-assay evaluation highlighted that most ctDNA assays achieved approximately 95% sensitivity for SNV detection at VAF ≥0.5% with adequate DNA input (>20ng) [29]. However, sensitivity substantially decreased at VAF 0.1%, with significant variability between platforms [29]. Assays with larger panel sizes (>1Mb) generally demonstrated lower sensitivity for low-frequency variants but provided more comprehensive genomic information [29].
Methodological Protocols
Sample Collection and Processing
Proper sample collection and processing are critical for reliable ctDNA analysis. The following protocols are adapted from recent studies [30] [29]:
- Blood Collection: 3 × 9 mL of blood collected into Streck Cell-Free DNA BCT or similar cfDNA preservation tubes [30]
- Processing: Plasma separation within 2-6 hours of collection by double centrifugation (e.g., 800 × g for 10 minutes, then 14,000 × g for 10 minutes) [29]
- Storage: Plasma stored at -80°C until cfDNA extraction [30]
- cfDNA Extraction: Automated extraction systems (e.g., QIAamp Circulating Nucleic Acid Kit, MagMax Cell-Free DNA Isolation Kit) following manufacturer protocols [29]
- Quality Control: cfDNA quantified using fluorometric methods (e.g., Qubit dsDNA HS Assay); fragment size distribution assessed (e.g., Bioanalyzer, TapeStation) [29]
- Input: 2-9 μL extracted cfDNA (approximately 10-50 ng total)
- Partitioning: Generation of approximately 20,000 droplets using droplet generator
- PCR Amplification: Endpoint PCR with mutation-specific probes (FAM-labeled) and reference probes (HEX/VIC-labeled)
- Thermal Cycling: 95°C for 10 minutes; 40 cycles of 94°C for 30 seconds and 55-60°C (assay-specific) for 60 seconds; 98°C for 10 minutes
- Detection: Droplet reading using droplet flow cytometer
- Analysis: Quantification of positive and negative droplets using vendor software; calculation of mutant copies/mL and variant allele frequency
- Input: 10-50 ng cfDNA (minimum recommended >20 ng)
- Library Preparation: End-repair, A-tailing, adapter ligation using commercial kits (e.g., Ion AmpliSeq Library Kit)
- Target Enrichment: Hybridization capture or amplicon-based (e.g., Ion AmpliSeq Cancer Hotspot Panel v2)
- Sequencing: NGS platform-specific (e.g., Illumina, Ion Torrent) to achieve minimum 5,000× deduplicated mean depth
- Variant Calling: Bioinformatic pipeline with unique molecular identifiers for error suppression; variant calling threshold typically 0.1-0.5% VAF
- Quality Metrics: On-target rate >50%, uniformity >80%, minimum coverage requirements met
Clinical Applications and Regulatory Status
Current Clinical Implementation
Liquid biopsy and ctDNA analysis have gained regulatory approval for specific clinical applications, particularly in therapy selection for advanced cancers. The FoundationOne Liquid CDx test received FDA approval as a companion diagnostic for multiple biomarkers, including:
- BRCA1/BRCA2 mutations in ovarian cancer for rucaparib treatment [33]
- ALK rearrangements in NSCLC for alectinib treatment [33]
- PIK3CA mutations in breast cancer for alpelisib treatment [33]
- BRCA1/BRCA2/ATM mutations in metastatic castration-resistant prostate cancer for olaparib treatment [33]
The FDA specifies that if these alterations are not detected in blood, tumor tissue testing should be performed to confirm negative results [33]. This reflects the recognized lower sensitivity of plasma-based testing compared to tissue analysis [32].
Beyond therapy selection, ctDNA analysis shows significant promise in multiple clinical domains:
- Minimal Residual Disease (MRD) Detection: Post-treatment ctDNA presence strongly predicts recurrence risk in colorectal cancer (up to 80-100% recurrence risk if ctDNA-positive) [30] [28]
- Treatment Response Monitoring: Dynamic changes in ctDNA levels often precede radiographic evidence of response or progression [27] [28]
- Early Cancer Detection: Multi-cancer early detection tests utilizing fragmentomics and methylation patterns are under investigation [28] [34]
Performance Across Cancer Types
The clinical utility of ctDNA analysis varies significantly by cancer type and stage. A meta-analysis of melanoma demonstrated 73% pooled sensitivity and 94% pooled specificity for ctDNA detection of BRAF mutations compared to tissue testing [31]. The area under the SROC curve was 0.93, indicating high diagnostic accuracy [31].
In lung adenocarcinoma, tissue-based NGS detected significantly more clinically relevant mutations (94.8% sensitivity) compared to plasma-based NGS (52.6% sensitivity, p<0.001) [32]. This performance gap was consistent across newly diagnosed and previously treated patients, suggesting tissue remains the preferred specimen when available [32].
Challenges and Research Gaps
Despite rapid advancement, ctDNA analysis faces several significant challenges that limit its widespread clinical implementation:
- Sensitivity Limitations: Current technologies struggle to detect very low VAFs (<0.1%), particularly in early-stage disease or low-shedding tumors [29]
- Preanalytical Variability: Differences in sample collection, processing, and storage significantly impact results [29]
- Inter-assay Discordance: Substantial variability exists between different ctDNA assays, especially for low-frequency variants [29] [32]
- Clonal Hematopoiesis: Age-related mutations in blood cells can confound ctDNA interpretation [29]
- Standardization Gaps: Lack of uniform protocols for sample processing, analysis, and interpretation [28] [29]
- Cost and Accessibility: NGS-based approaches remain expensive and technically demanding, limiting availability in resource-limited settings [28]
Essential Research Reagents and Tools
Table 3: Essential Research Reagents for ctDNA Analysis
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, CellSave Preservative Tubes | Preserves cfDNA integrity during transport/storage | Critical for preventing leukocyte lysis and background DNA release |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMax Cell-Free DNA Isolation Kit | Isolation of high-quality cfDNA from plasma | Automated systems preferred for reproducibility |
| DNA Quantification | Qubit dsDNA HS Assay, Bioanalyzer High Sensitivity DNA Kit | Accurate quantification and quality assessment | Fluorometric methods superior to spectrophotometry for cfDNA |
| ddPCR Reagents | Bio-Rad ddPCR Supermix, PrimePCR ddPCR Mutation Assays | Ultrasensitive detection of known mutations | Custom probes needed for rare mutations increase costs |
| NGS Library Prep | Illumina DNA Prep, Ion AmpliSeq Library Kit, KAPA HyperPrep | Preparation of sequencing libraries | Choice impacts coverage uniformity and GC bias |
| Target Enrichment | IDT xGen Pan-Cancer Panel, Thermo Fisher Oncomine Panels | Enrichment of cancer-relevant genomic regions | Hybridization capture vs. amplicon-based approaches |
| Bioinformatics Tools | GATK, MuTect2, VarScan, Conpair | Variant calling, quality control, contamination detection | Computational methods critical for low-VAF variant detection |
Liquid biopsy analysis of ctDNA represents a paradigm shift in cancer diagnostics, offering a minimally invasive approach to tumor genotyping, treatment monitoring, and recurrence detection. The comparative data clearly demonstrates a performance trade-off between PCR-based methods (higher sensitivity for known mutations) and NGS-based approaches (broader genomic coverage). As technological advancements continue to improve sensitivity and reduce costs, ctDNA analysis is poised to become increasingly integrated into routine cancer management. However, standardization of preanalytical procedures, validation of clinical utility across cancer types and stages, and resolution of bioinformatic challenges remain essential for widespread implementation. The ongoing development of multimodal approaches combining genomic, epigenomic, and fragmentomic analyses holds particular promise for enhancing the sensitivity and specificity of liquid biopsy applications in oncology.
From Bench to Bedside: Application-Driven Selection of Molecular Diagnostics in Clinical and Research Workflows
Hereditary cancer syndromes, such as those caused by pathogenic variants in the BRCA1/2 genes or the DNA mismatch repair (MMR) genes associated with Lynch syndrome (LS), account for a significant portion of cancer predisposition. Identifying these syndromes is crucial for implementing targeted cancer surveillance, risk-reducing strategies, and therapeutic interventions. Advances in molecular techniques have revolutionized diagnostic pathways, moving beyond family history-based models to incorporate tumor sequencing and multigene panels. This guide compares the current molecular techniques for diagnosing BRCA-related cancers and Lynch syndrome, focusing on their application in clinical and research settings. We provide a structured comparison of testing methodologies, their performance, and integrated clinical workflows to inform researchers, scientists, and drug development professionals.
Molecular Basis and Clinical Significance
BRCA1 and BRCA2 Syndromes
BRCA1 (BReast CAncer gene 1) and BRCA2 (BReast CAncer gene 2) are tumor suppressor genes that produce proteins critical for repairing damaged DNA. Harmful changes in these genes—pathogenic or likely pathogenic variants (PV)—significantly increase the lifetime risk of several cancers [35]. While traditionally associated with female breast and ovarian cancers, these mutations also confer markedly increased risks for male breast cancer, prostate cancer, and pancreatic cancer in carriers [36]. Notably, males represent half of all BRCA1/2 PV carriers, yet they undergo genetic testing at one-tenth the frequency of females, highlighting a significant gap in clinical identification [36].
Lynch Syndrome (Hereditary Non-Polyposis Colorectal Cancer)
Lynch syndrome is an autosomal dominant condition and the most frequent hereditary colorectal cancer (CRC) syndrome, accounting for 1–7% of all CRC cases [37] [38]. It is caused by germline mutations in MMR genes, primarily MLH1, MSH2, MSH6, PMS2, and EPCAM deletions. These mutations lead to microsatellite instability (MSI) and defective DNA repair, resulting in increased lifetime risks for colorectal, endometrial, gastric, ovarian, and other cancers [37] [38]. Timely molecular diagnosis is crucial for guiding endoscopic surveillance and risk-reducing interventions [38].
Comparative Analysis of Molecular Testing Techniques
Molecular diagnostics for hereditary cancer rely on various technologies, each with distinct strengths, limitations, and applications in research and clinical practice. The following table summarizes the primary techniques used for BRCA and Lynch syndrome identification.
Table 1: Comparison of Molecular Techniques for Hereditary Cancer Syndrome Identification
| Technique | Primary Application | Key Metrics/Performance | Advantages | Limitations |
|---|---|---|---|---|
| Next-Generation Sequencing (NGS) Multigene Panels [38] | Simultaneous analysis of multiple high- and moderate-penetrance cancer genes. | High sensitivity for point/small variants; Custom panels can cover 99% of target sequences [38]. | Cost-effective for multiple genes; higher sequencing depth than WES/WGS; focused analysis reduces incidental findings. | May not detect large copy number variations (CNVs) or large EPCAM deletions without specific design [38]. |
| Sanger Sequencing | Traditional method for single-gene testing. | High accuracy for confirming specific variants. | Low cost for a single gene; considered the gold standard. | Low throughput; not practical for analyzing multiple genes or large genes. |
| Tumor Analysis: Immunohistochemistry (IHC) [39] | Detects loss of MMR protein expression (MLH1, MSH2, MSH6, PMS2) in tumor tissue. | High negative predictive value; AUC ~0.82 for identifying MMR mutation carriers [39]. | Inexpensive; readily available in most pathology labs; pinpoints affected protein. | Does not identify the specific genetic alteration; can yield ambiguous results. |
| Tumor Analysis: Microsatellite Instability (MSI) Testing [39] | Detects hypermutability in microsatellite regions due to dMMR. | AUC ~0.77 for identifying MMR mutation carriers [39]. | Functional assay for dMMR; key biomarker for immunotherapy. | Requires paired normal tissue for optimal accuracy; does not identify the mutated gene. |
| Founder Mutation Panels [40] | Targeted testing for specific high-frequency variants in defined populations. | In Ashkenazi Jewish populations, 3 founder mutations account for most BRCA1/2 PVs [35]. | Fast and cost-effective for high-risk populations. | Will miss rare or population-specific variants; not for general population screening. |
Integrated Diagnostic Pathways and Prediction Models
Combining molecular tests with clinical criteria enhances the identification of mutation carriers. For Lynch syndrome, the integration of clinical prediction models with tumor testing has been systematically evaluated.
Table 2: Performance of Lynch Syndrome Identification Strategies [39]
| Identification Strategy | Area Under the Curve (AUC) | Clinical Utility |
|---|---|---|
| PREMM~1,2,6~ Model (Clinical/Family History Only) | 0.90 | Effective for initial risk stratification based on personal/family history. |
| Microsatellite Instability (MSI) Testing Alone | 0.77 | Good for functional assessment of dMMR but less discriminative alone. |
| Immunohistochemistry (IHC) Alone | 0.82 | Pinpoints protein loss; better performance than MSI alone. |
| PREMM~1,2,6~ + IHC | 0.94 | Excellent combined performance; recommended for integrated screening. |
| PREMM~1,2,6~ + MSI | 0.93 | Very good combined performance. |
| PREMM~1,2,6~ + IHC + MSI | 0.94 | No significant improvement over PREMM~1,2,6~ + IHC. |
For BRCA, testing indications have expanded beyond strong family history to include a personal history of specific cancers, such as male breast cancer, pancreatic cancer, and high-risk prostate cancer, as well as the presence of specific somatic tumor findings [36].
Detailed Experimental Protocols
This protocol outlines the targeted sequencing of a 9-gene panel for Lynch syndrome in a Uruguayan cohort, demonstrating a scalable in-house application.
- Step 1: Patient Selection and DNA Extraction: Recruit patients meeting clinical criteria for LS (e.g., Amsterdam II/Bethesda guidelines). Collect whole blood samples and extract genomic DNA using a commercial kit (e.g., QIAamp DNA Mini Kit). Verify DNA quality via 260/280 nm ratio and quantify using a fluorometric method (e.g., Qubit dsDNA HS Assay).
- Step 2: Custom Panel Design and Library Preparation: Design a custom AmpliSeq panel (e.g., using Ion AmpliSeq Designer) covering the coding sequences, splice junctions, and UTRs of target genes (
MLH1,MSH2,MSH6,PMS2,EPCAM,APC,MUTYH). For each patient, amplify 10 ng of genomic DNA via PCR using the custom primer pools. Construct barcoded libraries using a kit (e.g., Ion AmpliSeq Library Kit 2.0). - Step 3: Templating and Sequencing: Prepare sequencing templates using an ion emulsion PCR system (e.g., Ion Chef System). Sequence the libraries on a benchtop sequencer (e.g., Ion Torrent S5 System).
- Step 4: Data Analysis and Variant Interpretation: Map sequences to the human reference genome (e.g., hg19). Call and annotate variants. Prioritize variants based on allele frequency, in silico prediction tools (e.g., SIFT, PolyPhen), and existing pathogenicity databases. Classify variants according to the American College of Medical Genetics and Genomics (ACMG) guidelines.
This large-scale functional study used CRISPR/Cas9 to reclassify BRCA2 variants of uncertain significance (VUS), a major challenge in clinical genetics.
- Step 1: Variant Saturation: Use CRISPR/Cas9 gene editing to introduce approximately 7,000 different variants into a specific functional domain of the BRCA2 gene in a controlled cell line model.
- Step 2: Functional Selection: Subject the pools of variant-carrying cells to a growth-based assay that selects for cells with impaired BRCA2 function. Cells with pathogenic BRCA2 variants will survive this selection, while those with benign variants will not.
- Step 3: Sequencing and Enrichment Scoring: Extract genomic DNA from the selected cell populations and sequence the targeted BRCA2 region. Calculate a functional score for each variant based on its relative abundance before and after selection.
- Step 4: Variant Reclassification: Classify variants as "pathogenic/likely pathogenic" (low functional score) or "benign/likely benign" (high functional score). Submit validated data to expert panels (e.g., NIH's ClinVar) for official reclassification, impacting clinical care.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Research Reagents for Hereditary Cancer Genomics
| Reagent/Material Solution | Function | Example Product/Catalog Number |
|---|---|---|
| High-Quality DNA Extraction Kit | To obtain pure, high-molecular-weight genomic DNA from patient samples (blood, saliva). | QIAamp DNA Mini Kit (#51304) [38] |
| Targeted NGS Library Prep Kit | To amplify target genes and attach sequencing adapters and barcodes for multiplexing. | Ion AmpliSeq Library Kit 2.0 (#4475345) [38] |
| Ion Xpress Barcode Adapters | To individually index (barcode) each sample library for pooled sequencing. | Ion Xpress Barcode Adapters (#4474517) [38] |
| NGS Quantification Assay | To accurately quantify library concentration before sequencing. | Qubit 1X dsDNA HS Assay Kit (#Q33230) [38] |
| CRISPR/Cas9 System | For precise gene editing in functional studies of VUS. | CRISPR/Cas9 plasmids and reagents [41] |
Emerging Technologies and Future Directions
The field of hereditary cancer diagnostics is rapidly evolving. The development of cell-free RNA (cfRNA) blood tests shows promise for non-invasive detection of cancers and mechanisms of treatment resistance by analyzing messenger RNA signals from multiple tissues [42]. Furthermore, the distinction between precision cancer medicine (often genomics-guided stratified medicine) and true personalized cancer medicine (integrating multi-omics, pharmacogenomics, and patient-specific factors) is shaping clinical trial design and future biomarker discovery [43]. Efforts to reclassify variants of uncertain significance (VUS), as demonstrated by the BRCA2 functional study, are critical for reducing uncertainty in clinical management and disparities, particularly among understudied populations like Black women who have a higher frequency of VUS [41].
Companion diagnostics (CDx) are essential tools in modern oncology, providing the critical link between a specific therapeutic product and a patient's unique biomarker status. The U.S. Food and Drug Administration (FDA) defines these in vitro diagnostic devices as providing information that is critical for the safe and effective use of corresponding targeted therapies [44]. Their primary functions include identifying patients most likely to benefit from a particular treatment, identifying those at increased risk for serious side effects, and monitoring treatment response [44]. The success of this drug-diagnostic co-development model was established in 1998 with the parallel approval of trastuzumab (Herceptin) and the HercepTest for HER2-positive breast cancer, without which the targeted therapy might have been discarded due to insufficient activity in an unselected patient population [44]. This model has since become the standard for precision medicine, with the FDA having approved more than 78 drug/CDx combinations by early 2025 [45].
The molecular heterogeneity of cancer, particularly non-small cell lung cancer (NSCLC), necessitates precise biomarker testing to guide therapy selection. Biomarkers such as EGFR, ALK, BRAF, PD-L1, and MSI-H represent distinct molecular subtypes that predict response to specific targeted therapies and immunotherapies. The consistent upward trend in FDA approvals of new molecular entities linked to CDx assays—increasing from a mean of 3.5 annually (1998-2010) to 12.2 annually (2011-2024)—underscores the rapidly expanding role of companion diagnostics in oncology [45]. This guide provides a comprehensive comparison of CDx approaches for these five critical biomarkers, offering researchers and drug development professionals detailed experimental protocols, performance data, and technical insights to inform diagnostic development and clinical research strategies.
The following biomarkers guide treatment decisions across multiple cancer types, with particular significance in NSCLC:
- EGFR: Mutations in the epidermal growth factor receptor (EGFR) gene, particularly exon 19 deletions and L858R substitutions, drive a subset of NSCLC and are targeted by EGFR tyrosine kinase inhibitors (TKIs) [46].
- ALK: Gene rearrangements (fusions) involving the anaplastic lymphoma kinase (ALK) gene occur in approximately 3-5% of NSCLC patients and confer sensitivity to ALK inhibitors [47] [48]. ALK-positive patients often have a distinct clinical profile, frequently being younger, never-smokers or light smokers, and at higher risk of developing brain metastases [48].
- BRAF: The BRAF V600E mutation is a rare biomarker (1-2% prevalence in NSCLC) that results in constitutive activation of the MAPK pathway and is targeted by BRAF/MEK inhibitor combinations [46].
- PD-L1: Protein expression of programmed death-ligand 1 (PD-L1) on tumor and/or immune cells is used to predict response to immune checkpoint inhibitors, with cutoff values (e.g., ≥1%, ≥50%) varying by specific therapeutic agent and cancer type [49].
- MSI-H: Microsatellite instability-high (MSI-H) status, resulting from deficient DNA mismatch repair (dMMR), is a pan-cancer biomarker predicting response to immunotherapy across multiple solid tumor types, including colorectal cancer [50].
Table 1: Clinical Significance of Key Biomarkers in Targeted Therapy and Immunotherapy
| Biomarker | Alteration Type | Primary Cancer Types | Prevalence in NSCLC | Targeted Therapies |
|---|---|---|---|---|
| EGFR | Mutation | NSCLC, CRC | 24-60% (for specific EGFR alterations) [46] | Osimertinib, Gefitinib, Erlotinib |
| ALK | Rearrangement/Fusion | NSCLC | 3-13% [46] | Alectinib, Crizotinib, Lorlatinib |
| BRAF | V600E Mutation | NSCLC, Melanoma, CRC | 1-2% [46] | Dabrafenib + Trametinib, Vemurafenib |
| PD-L1 | Protein Expression | NSCLC, Melanoma, Urothelial Carcinoma | Varies by cutoff | Pembrolizumab, Atezolizumab, Durvalumab |
| MSI-H | Genomic Instability | CRC, Endometrial, Pan-Cancer | <5% (across all cancer types) | Pembrolizumab, Nivolumab ± Ipilimumab |
Comparison of Diagnostic Methodologies and Platforms
Multiple technology platforms are utilized for companion diagnostic testing, each with distinct advantages, limitations, and appropriate clinical contexts. The evolution of CDx technologies has progressed from predominantly immunohistochemistry (IHC) and in situ hybridization (ISH) methods to include polymerase chain reaction (PCR)-based platforms, which now represent the largest proportion of assays, and next-generation sequencing (NGS) [44].
Immunohistochemistry (IHC) detects protein expression using antibody-based staining and is widely used for PD-L1 and ALK testing. The Dako PD-L1 IHC 22C3 pharmDx (Agilent) is a prominent example, dominating the market with an estimated 50.4% share in 2025, largely due to its role as a companion diagnostic for pembrolizumab [51]. IHC offers the advantage of visualizing protein expression in the context of tissue architecture but is semi-quantitative and subject to interpretive variability.
Next-Generation Sequencing (NGS) enables massive parallel sequencing of DNA or RNA, allowing comprehensive genomic profiling of multiple genes simultaneously from limited tissue samples. NGS is particularly valuable for detecting a wide range of alterations, including mutations, fusions, and insertions/deletions. Foundation Medicine's CDx assays represent this category, with some approved as group CDx for multiple therapies [44].
PCR-based methods detect specific DNA sequences with high sensitivity and are commonly used for EGFR and BRAF mutation testing. The Idylla CDx MSI Test (Biocartis) exemplifies a fully automated, cartridge-based "sample-to-result" PCR system that can deliver results in less than 3 hours with minimal hands-on time [50].
Fluorescence In Situ Hybridization (FISH) detects gene rearrangements and amplifications using fluorescently labeled DNA probes and was historically the gold standard for ALK fusion detection, though it has largely been supplemented by IHC and NGS in many settings [47].
Table 2: Comparison of Companion Diagnostic Platforms and Technologies
| Technology Platform | Detects | Biomarker Examples | Key CDx Examples | Turnaround Time |
|---|---|---|---|---|
| Immunohistochemistry (IHC) | Protein Expression | PD-L1, ALK | Dako PD-L1 IHC 22C3 pharmDx, VENTANA PD-L1 (SP142) Assay [51] | 1-2 days |
| Next-Generation Sequencing (NGS) | Mutations, Fusions, CNAs, TMB | EGFR, ALK, BRAF, MSI-H | FoundationOne CDx, Guardant360 CDx | 7-14 days |
| PCR-based Methods | Mutations, MSI-H | EGFR, BRAF, MSI-H | Idylla CDx MSI Test [50], cobas EGFR Mutation Test v2 | 1-3 days |
| Fluorescence In Situ Hybridization (FISH) | Gene Rearrangements, Amplifications | ALK, ROS1 | Vysis ALK Break Apart FISH Probe | 3-5 days |
Analytical and Clinical Performance Data
Companion diagnostic validation requires robust demonstration of both analytical and clinical performance. For rare biomarkers, limited sample availability poses unique challenges, often necessitating regulatory flexibility in validation strategies. A review of FDA approvals for NSCLC CDx revealed that alternative sample sources (archival specimens, retrospective samples, commercially acquired specimens) were frequently used when clinical trial samples were limited—particularly for the rarest biomarkers (100% for biomarkers with 1-2% prevalence vs. 40% for more common biomarkers) [46].
Diagnostic Performance for Rare Biomarkers
Bridging studies are critical for CDx validation, especially when the pivotal clinical trial used different assays for patient selection. Analysis of these studies shows that sample sizes vary significantly based on biomarker prevalence. For the rarest biomarkers (ROS1, BRAF V600E), bridging studies included a median of only 67 positive samples (range: 25-167) and 119 negative samples (range: 114-135), whereas more common biomarkers (EGFR mutations, PD-L1) utilized substantially larger sample sizes (median 182.5 positive samples, range: 72-282) [46].
Recent advances in deep learning approaches show promise for improving rare biomarker detection. One study utilizing vision transformer models on H&E-stained whole slide images achieved ROC AUCs of 0.85 for ROS1 and 0.84 for ALK fusion prediction in NSCLC, despite limited positive sample sizes (306 ROS1-positive and 697 ALK-positive cases out of 33,014 patients) [47]. To address the challenge of limited ROS1-positive cases, researchers implemented a two-stage training strategy: first training the model to detect a composite biomarker (ROS1, ALK, and NTRK fusions), then fine-tuning it specifically for ROS1 prediction, which enhanced performance compared to direct training (ROC AUC of 0.86 vs. 0.83) [47].
Clinical Trial Data and Survival Outcomes
The critical importance of companion diagnostics is demonstrated by clinical trial data linking biomarker status to therapeutic outcomes:
ALK Testing and Alectinib: In the phase 3 ALEX trial, first-line alectinib demonstrated a clinically meaningful overall survival benefit compared to crizotinib in advanced ALK-positive NSCLC, with 50% of patients alive at 5 years—one of the longest survival rates reported for stage IV NSCLC [52]. For patients with CNS metastases who had received prior brain radiation, the median OS was 92.0 months with alectinib versus 39.5 months with crizotinib (HR, 0.62) [52].
MSI-H Testing and Immunotherapy: The CheckMate 8HW trial established the efficacy of nivolumab plus ipilimumab in patients with MSI-H/dMMR metastatic colorectal cancer, leading to FDA approval of the Idylla CDx MSI Test as a companion diagnostic [50]. This fully automated, cartridge-based test detects a panel of 7 monomorphic biomarkers indicative of MSI and delivers results in less than 3 hours with minimal hands-on time [50].
PD-L1 Quantitative Continuous Scoring: Research on computer vision systems for granular cell-level quantification of PD-L1 staining intensity has demonstrated potential improvements over subjective visual scoring. In an analysis of the MYSTIC trial, a Quantitative Continuous Scoring system (PD-L1 QCS-PMSTC) identified a biomarker-positive population with a similar hazard ratio (0.62) to visual scoring but with significantly increased prevalence (54.3% vs. 29.7%), potentially allowing more patients to be identified as candidates for immunotherapy [49].
Table 3: Clinical Trial Outcomes by Biomarker Status
| Biomarker | Therapy | Trial Name/Context | Survival Outcome | Comparator |
|---|---|---|---|---|
| ALK+ | Alectinib | ALEX (Phase 3), 1st line [52] | 50% OS at 5 years | Crizotinib (HR 0.78) |
| ALK+ with CNS mets | Alectinib | ALEX (Phase 3), prior brain radiation [52] | Median OS 92.0 months | Crizotinib: 39.5 months (HR 0.62) |
| PD-L1 QCS-PMSTC+ | Durvalumab | MYSTIC (Phase 3) [49] | HR 0.62 (CI 0.46-0.82) | Chemotherapy |
| MSI-H/dMMR CRC | Nivolumab + Ipilimumab | CheckMate 8HW (Phase 3) [50] | Significant PFS improvement | Chemotherapy |
Experimental Protocols and Methodologies
Deep Learning for Fusion Detection in NSCLC
Objective: To develop deep learning models using H&E-stained whole slide images (WSIs) to predict ALK and ROS1 fusions in NSCLC.
Dataset: 33,014 NSCLC patients, including 306 ROS1-fusion positive and 697 ALK-fusion positive cases [47].
Methodology:
- Feature Extraction: A vision transformer model (MoCo-V3) was trained in a self-supervised manner as a feature extractor.
- Model Architecture: Transformer-based models were trained to predict fusion presence using extracted features.
- Training Strategy: For ROS1 (limited positive samples), a two-stage specialized training procedure was implemented:
- Primary training on a composite "RAN" label (positive for any ROS1, ALK, or NTRK fusion)
- Fine-tuning specifically for ROS1 prediction with a reduced learning rate (10x smaller than direct training)
- Validation: Five-fold cross-validation followed by evaluation on a holdout dataset.
Key Parameters:
- Direct Training: Single-stage training for target biomarker prediction
- Train-Finetune: Initial training on RAN composite biomarker followed by fine-tuning
- Performance Metrics: ROC AUC, precision-recall curves
This approach achieved ROC AUCs of 0.85 for ROS1 and 0.84 for ALK on the holdout dataset, demonstrating the effectiveness of transfer learning for rare biomarker prediction [47].
Quantitative Continuous Scoring of PD-L1
Objective: To develop a computer vision system for granular cell-level quantification of PD-L1 staining intensity in digitized whole slide images.
Dataset: 768 WSIs from the MYSTIC trial (NCT02453282) [49].
Methodology:
- Image Analysis: Whole slide images of PD-L1 IHC-stained NSCLC specimens were processed using a computer vision system.
- Cell Segmentation: Tumor cells were identified and segmented within the digital images.
- Intensity Quantification: Membrane staining intensity (SI) was quantified for each tumor cell on a continuous scale.
- Biomarker Derivation: The PD-L1 QCS-PMSTC biomarker was defined as the percentage of tumor cells with medium to strong staining intensity (SI ≥40).
- Threshold Optimization: A cutoff of ≥0.575% was established to classify patients as biomarker-positive, maximizing the log-rank statistic while maintaining prevalence between 20-80%.
Validation Approach:
- Comparison to visual scoring (% tumor cells ≥50)
- Assessment of hazard ratios for durvalumab versus chemotherapy
- Evaluation of biomarker prevalence in the study population
This methodology resulted in a similar hazard ratio (0.62) to visual scoring but identified a substantially larger patient population likely to benefit from anti-PD-L1 treatment (54.3% vs. 29.7% with visual scoring) [49].
Diagnostic Workflows and Signaling Pathways
Companion Diagnostic Testing Workflow
The following diagram illustrates the generalized workflow for companion diagnostic testing in oncology, from sample collection through clinical decision-making:
Diagram 1: CDx Testing Workflow
Biomarker-Guided Therapeutic Pathways
The relationship between specific biomarker alterations and their corresponding targeted therapies follows distinct signaling pathways:
Diagram 2: Biomarker-Guided Therapy
Research Reagent Solutions and Essential Materials
The following table details key research reagents and materials essential for developing and implementing companion diagnostics for the featured biomarkers:
Table 4: Essential Research Reagents for Companion Diagnostic Development
| Reagent/Material | Function | Example Applications | Technical Notes |
|---|---|---|---|
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue Sections | Preserves tissue architecture and biomolecules for histological analysis | IHC, FISH, nucleic acid extraction | Section thickness (4-5μm) critical for optimal staining [47] |
| Primary Antibodies (Clone-Specific) | Binds specifically to target antigens in IHC | PD-L1 (22C3, SP142), ALK (D5F3) | Clone selection affects staining intensity and interpretation [51] |
| Fluorescently Labeled DNA Probes | Hybridizes to specific DNA sequences for FISH | ALK break-apart probes, ROS1 probes | Probe design crucial for specificity in fusion detection [47] |
| PCR Master Mixes | Amplifies target DNA sequences | EGFR, BRAF mutation detection | Contains polymerase, dNTPs, buffers for optimized amplification |
| Next-Generation Sequencing Panels | Targets specific genomic regions for parallel sequencing | Comprehensive genomic profiling | Coverage depth >500x recommended for variant detection |
| Cell Line Controls | Provides reference material for assay validation | Positive/negative controls for rare biomarkers | Essential for validating assays for rare biomarkers [46] |
Emerging Trends and Future Directions
The field of companion diagnostics continues to evolve with several emerging trends shaping future development. Liquid biopsy approaches are gaining prominence, with the first liquid biopsy CDx approved in 2016 for detecting EGFR mutations in NSCLC [44]. These plasma-based tests offer advantages including less invasive sample collection, faster turnaround times, and the ability to monitor treatment response over time [44].
Artificial intelligence and digital pathology are transforming biomarker quantification, particularly for traditionally subjective assessments like PD-L1 scoring. Automated image analysis systems can reduce inter-observer variability and enable more granular, continuous scoring approaches that may identify larger patient populations likely to respond to therapy [49]. The integration of AI with comprehensive genomic profiling represents a powerful approach to navigating the increasing complexity of cancer biomarkers and treatment options.
The regulatory landscape is also adapting to support these advancements. In April 2020, the FDA released guidance supporting broader "group claims" for companion diagnostics associated with multiple cancer medicines, aiming to decrease the need for physicians to order multiple tests and additional biopsies [44]. This approach enables greater flexibility for clinicians in choosing appropriate therapies based on a patient's biomarker status. However, as of early 2025, only five devices had been approved under this framework, indicating implementation challenges [44].
For rare biomarkers, regulatory flexibilities in validation strategies are becoming increasingly important. When clinical trial samples are limited, the use of alternative sample sources (archival specimens, retrospective samples, commercially acquired specimens) can facilitate CDx development and approval [46]. Establishing formal guidance on these flexibilities would support more streamlined processes for targeted therapies addressing unmet needs in small patient populations.
Minimal Residual Disease (MRD) refers to the small population of cancer cells that persist in a patient after treatment, often at levels undetectable by traditional morphological examination [53]. In hematological malignancies, MRD represents a latent reservoir of disease that can lead to relapse if not properly addressed [53]. The concept has since expanded to include solid tumors, where it is increasingly recognized as a pivotal biomarker for assessing relapse risk and optimizing therapeutic strategies [53] [54]. The clinical significance of MRD lies in its ability to detect residual disease at the molecular level before clinical or radiologic progression becomes apparent, allowing for earlier intervention and more personalized treatment approaches [54].
Accurate MRD detection provides critical prognostic information that surpasses traditional remission assessment. In acute myeloid leukemia (AML), for instance, studies have demonstrated a close relationship between detected MRD levels and both overall survival and progression-free survival [53]. The ability to identify patients at high and low risk of recurrence enables more precise treatment adjustments and risk stratification, potentially avoiding both undertreatment in high-risk patients and unnecessary toxicity in those with low or undetectable MRD [53]. As MRD detection technologies continue to evolve, they are progressively reshaping cancer management paradigms across both hematological malignancies and solid tumors.
Current MRD Detection Methodologies: A Technical Comparison
Multiple methodologies have been developed for MRD detection, each with distinct principles, sensitivity thresholds, and clinical applications. The selection of an appropriate technique depends on various factors, including cancer type, available tissue, required sensitivity, and clinical context [53].
Table 1: Comparison of Major MRD Detection Techniques
| Method | Applicability | Sensitivity | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Flow Cytometry (FCM) | Nearly 100% for hematologic malignancies [53] | 10−3 to 10−6 (depending on colors) [53] | Widely available, fast turnaround, relatively inexpensive [53] | Lack of standardization, changes in immunophenotype, requires fresh cells [53] |
| Quantitative PCR (qPCR) | ~40-50% [53] | 10−4 to 10−6 [53] | Highly sensitive for known targets, standardized, lower costs [53] | Limited to predefined targets, may miss emerging mutations [53] |
| Next-Generation Sequencing (NGS) | >95% [53] | 10−2 to 10−6 [53] | Comprehensive genomic coverage, detects novel mutations, broad applicability [53] | Higher cost, complex data analysis, longer turnaround time [53] |
| Digital PCR (dPCR) | Varies by target [3] | Can detect mutant allele frequencies <0.1% [3] | Absolute quantification, high sensitivity, robust against inhibitors [3] | Limited multiplexing capability, predefined targets required [3] |
The evolution of these technologies has progressively enhanced detection sensitivity. While traditional morphological methods could only detect 1 cancer cell in 20 (sensitivity of 5×10-2), modern techniques like NGS and dPCR can identify a single cancer cell among 10,000 to 1,000,000 normal cells [53] [3]. This dramatic improvement in sensitivity enables earlier detection of residual disease and more accurate assessment of treatment response. Each method occupies a specific niche in the MRD detection landscape, with the optimal choice dependent on the clinical question, available resources, and required performance characteristics.
Advanced ctDNA-Based MRD Detection Platforms
Circulating tumor DNA (ctDNA) analysis has emerged as a cornerstone of modern MRD assessment, particularly for solid tumors [54]. ctDNA represents a tumor-derived subset of cell-free DNA, with levels ranging from ≥5-10% in late-stage cancers to as low as ≤0.01-0.1% in early-stage cancers or post-surgical settings [54]. The extreme rarity of ctDNA in these contexts demands highly sensitive detection technologies, primarily utilizing droplet digital PCR (ddPCR) and next-generation sequencing (NGS) approaches [54].
Table 2: Comparison of ctDNA-Based MRD Detection Platforms
| Platform/Approach | Technology | Sensitivity (Limit of Detection) | Key Features | Best Applications |
|---|---|---|---|---|
| Tumor-Informed Approaches | ||||
| Signatera (Natera) | Amplicon-based targeted NGS [54] | 0.001-0.02% tumor fraction [54] | Patient-specific mutations, high specificity [54] | Longitudinal monitoring, therapy response assessment [54] |
| RaDaR (Inivata/NeoGenomics) | Amplicon-based targeted NGS [54] | 0.001-0.02% tumor fraction [54] | Tracks up to 48 tumor-specific variants [54] | Recurrence monitoring, residual disease detection [54] |
| MRDetect (Veracyte) | WGS-based with computational enhancement [54] | ~0.0001% tumor fraction [54] | Broad genomic coverage, AI-enhanced sensitivity [54] | Ultra-sensitive detection, heterogeneous tumors [54] |
| Tumor-Naïve Approaches | ||||
| Guardant Reveal (Guardant Health) | Hybrid capture-based NGS [54] | Varies by mutation | No prior tumor sequencing required [54] | Broad screening, when tissue unavailable [54] |
| InVisionFirst-Lung (Inivata) | Amplicon-based NGS [54] | 0.07-0.33% MAF [54] | 36-gene panel for lung cancer [54] | NSCLC management, recurrence risk stratification [54] |
The fundamental distinction in ctDNA-based MRD detection lies between tumor-informed and tumor-naïve (agnostic) approaches [54]. Tumor-informed methods require prior sequencing of tumor tissue to identify patient-specific mutations, which are then tracked in plasma using custom assays [54]. This approach offers high specificity by minimizing false positives from non-tumor sources like clonal hematopoiesis [54]. Conversely, tumor-naïve methods utilize predefined panels of recurrent cancer-associated alterations without requiring tumor tissue, offering faster turnaround times and broader applicability but potentially reduced sensitivity for patient-specific mutations [54].
The workflow diagram illustrates the procedural differences between these two main approaches. Tumor-informed methods begin with comprehensive tumor sequencing to identify patient-specific mutations, followed by custom assay design for longitudinal monitoring [54]. This process, while more complex and time-consuming, enables highly sensitive tracking of individual-specific mutations. Tumor-naïve approaches bypass the need for tissue sequencing, instead applying fixed panels of cancer-associated alterations directly to blood samples [54]. This offers practical advantages in settings where tumor tissue is unavailable or when rapid results are prioritized.
Experimental Protocols for MRD Detection
Tumor-Informed ctDNA Analysis Protocol
The tumor-informed approach represents the gold standard for sensitive MRD detection, with the Signatera assay being a prominent example. The methodology involves a multi-step process that begins with tumor whole exome sequencing (WES) to identify somatic mutations [54]. Bioinformatic analysis selects 16 patient-specific somatic single nucleotide variants (SNVs) that are then used to design a custom assay for tracking in plasma samples [54]. For each plasma sample, cell-free DNA is extracted and subjected to targeted PCR amplification of the selected mutations, followed by sequencing on an NGS platform [54]. A positive MRD call is typically made when ≥2 of the 16 tracked mutations are detected above background noise levels, with statistical confidence [54]. This approach achieves high sensitivity (down to 0.01% variant allele frequency) while maintaining specificity >99% due to the patient-specific nature of the tracked mutations [54].
Droplet Digital PCR (ddPCR) Protocol
Droplet digital PCR provides an alternative method for ultrasensitive MRD detection, particularly valuable for tracking known mutations. The protocol begins with plasma collection and cell-free DNA extraction using standardized kits [3]. The extracted DNA is then partitioned into approximately 20,000 nanoliter-sized droplets, effectively creating individual reaction chambers [3]. Each droplet undergoes PCR amplification with fluorescence-labeled probes specific to the mutant and wild-type sequences [3]. Following amplification, the droplets are analyzed in a flow cytometer to count the positive (mutant) and negative (wild-type) reactions [3]. The absolute concentration of mutant DNA molecules is calculated using Poisson statistics based on the ratio of positive to negative droplets [3]. This approach enables precise quantification of rare mutant alleles with sensitivity down to 0.001% mutant allele frequency, without requiring standard curves [3].
Next-Generation Sequencing-Based MRD Detection
NGS-based approaches for MRD detection leverage unique molecular identifiers (UMIs) and deep sequencing to achieve high sensitivity. The Safe-SeqS (Safe Sequencing System) protocol exemplifies this methodology [54]. Initially, each DNA molecule is tagged with a unique identifier during library preparation [54]. Following amplification and sequencing, bioinformatic analysis groups sequencing reads that share the same UMI, representing amplification products of a single original molecule [54]. A mutation is considered authentic if it is present in a specified percentage of molecules with different UMIs, effectively filtering out PCR and sequencing errors [54]. This approach typically requires deep sequencing coverage (≥10,000x) to reliably detect rare mutant alleles present at frequencies as low as 0.01% [54]. The main advantage of NGS-based methods is their ability to simultaneously track multiple mutations across various genomic regions, providing a more comprehensive assessment of residual disease [54].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for MRD Detection
| Category | Specific Product/Platform | Research Application | Key Features |
|---|---|---|---|
| NGS Platforms | Illumina NovaSeq Series [53] | High-throughput MRD sequencing | Enables deep sequencing for rare variant detection |
| Ion Torrent Genexus System [53] | Automated NGS for MRD | Integrated workflow from nucleic acids to report | |
| PCR Technologies | Bio-Rad QX600 Droplet Digital PCR [3] | Absolute quantification of MRD targets | Partitioned PCR for precise rare allele detection |
| Thermo Fisher QuantStudio dPCR [3] | Low-frequency variant detection | Microchip-based partitioning system | |
| Targeted Panels | ArcherDX PCM (Invitae) [54] | Tumor-informed MRD detection | Customizable target selection for patient-specific mutations |
| Oncomine cfDNA Assay (Thermo Fisher) [54] | Tumor-naïve MRD screening | Predesigned panels for common cancer mutations | |
| Bioinformatic Tools | C2-Intelligence (C2i Genomics) [54] | WGS-based MRD detection | AI-enhanced sensitivity for low tumor fraction |
| NeXT Personal (Personalis) [54] | Ultra-sensitive MRD monitoring | WGS-based approach with broad genomic coverage |
Successful MRD research requires not only sophisticated instrumentation but also specialized reagents and analytical tools. For ctDNA-based approaches, efficient extraction kits optimized for low-concentration cell-free DNA are essential, such as the QIAamp Circulating Nucleic Acid Kit or comparable systems [54]. For NGS-based MRD detection, library preparation kits incorporating unique molecular identifiers (UMIs) are critical for error suppression, with products from Illumina, Twist Bioscience, and IDT being widely utilized [54]. In the digital PCR domain, droplet generation oils and specialized probe chemistry from Bio-Rad or Thermo Fisher ensure optimal partitioning and detection efficiency [3]. Additionally, bioinformatic pipelines for variant calling, error correction, and clonal tracking represent indispensable software tools in the MRD researcher's arsenal, with platforms from C2i Genomics and Personalis offering integrated solutions [54].
Clinical Validation and Analytical Performance
The clinical utility of MRD detection methodologies depends on rigorous validation demonstrating both analytical and clinical performance. Key analytical metrics include sensitivity (limit of detection), specificity, precision, and linearity across the measuring interval [53] [54]. For MRD assays, the limit of detection is particularly critical, with optimal assays capable of detecting tumor fractions as low as 0.001% [54]. Specificity must be sufficiently high to distinguish true somatic mutations from artifacts arising from amplification errors, clonal hematopoiesis, or sample cross-contamination [54].
Clinical validation requires demonstrating prognostic significance across independent cohorts. In non-small cell lung cancer (NSCLC), multiple studies have confirmed that ctDNA-based MRD detection post-resection predicts recurrence with hazard ratios typically ranging from 5 to 15, significantly outperforming clinical-pathological factors alone [54]. Similarly, in hematological malignancies, MRD negativity has consistently correlated with prolonged progression-free and overall survival across multiple cancer types [53]. The emerging clinical evidence supports MRD as a robust surrogate endpoint for drug development and clinical trial stratification, potentially accelerating the approval of novel therapies [53] [54].
MRD detection technologies have revolutionized cancer management by enabling unprecedented sensitivity in monitoring treatment response and predicting clinical outcomes. The evolving landscape of MRD assessment is characterized by ongoing improvements in detection sensitivity, workflow efficiency, and clinical applicability. Future developments will likely focus on standardizing MRD assays across platforms, validating clinical utility in prospective interventional trials, and expanding applications to earlier cancer stages and additional tumor types [53] [54].
The integration of artificial intelligence and machine learning approaches represents a promising frontier for enhancing MRD detection sensitivity and specificity [55] [56]. AI algorithms can identify subtle patterns in complex sequencing data that might escape conventional analysis, potentially pushing detection limits below current thresholds [56]. Additionally, the combination of mutational analysis with epigenetic signatures such as DNA methylation patterns may provide orthogonal validation and further improve assay performance [54]. As these technologies mature and evidence accumulates, MRD assessment is poised to become an increasingly central component of cancer diagnostics, treatment selection, and therapeutic monitoring across the spectrum of malignant diseases.
Cancer diagnosis and treatment are undergoing a revolutionary transformation, moving from traditional histopathological classification toward molecular characterization. Two technological frontiers are driving this change: advanced molecular subtyping for Cancers of Unknown Primary (CUP) and liquid biopsy for multi-cancer early detection. CUP represents a significant diagnostic challenge, comprising 2-5% of all cancer cases characterized by metastatic disease without an identifiable primary tumor, leading to limited treatment options and poor prognosis with a median overall survival of 6-16 months depending on the subtype [57] [58]. Simultaneously, liquid biopsy technologies have emerged as promising tools for non-invasive cancer detection through analysis of circulating tumor biomarkers. This comprehensive analysis compares the technological foundations, clinical applications, and performance characteristics of these two approaches within the expanding toolkit of molecular cancer diagnostics, providing researchers and drug development professionals with critical insights for strategic decision-making.
Molecular Subtyping of Cancers of Unknown Primary (CUP)
Technological Foundations and Classification Approaches
Molecular subtyping of CUP aims to resolve the diagnostic enigma of these metastatic tumors through comprehensive biomarker profiling. The fundamental premise is that despite the absence of a detectable primary tumor, CUP metastases retain molecular signatures that can reveal their tissue of origin or identify actionable biomarkers.
Table 1: Molecular Classification Technologies for CUP
| Technology | Analytes | Primary Output | Therapeutic Guidance | Key Limitations |
|---|---|---|---|---|
| Immunohistochemistry (IHC) [58] | Protein expression | Lineage differentiation markers | Limited to known protein targets | Subjective interpretation; limited multiplexing |
| Gene Expression Profiling (GEP) [59] [58] | mRNA | Predicted tissue of origin | Site-specific therapy | Requires high-quality RNA |
| Comprehensive Genomic Profiling (CGP) [59] | DNA mutations, TMB, MSI | Actionable genomic alterations | Tissue-agnostic targeted therapy | Does not always identify tissue of origin |
| Epigenetic Profiling [59] | DNA methylation patterns | Methylation-based classification | Emerging for therapy selection | Complex bioinformatic requirements |
The clinical application of these technologies follows two distinct pathways: site-specific therapy based on predicted tissue of origin (primarily using GEP and IHC) and tissue-agnostic therapy based on specific molecular alterations (using CGP) [59]. The site-specific approach leverages the principle that CUP metastases may respond to treatments effective against their putative primary cancers, while the tissue-agnostic approach targets specific genomic alterations regardless of origin, such as high tumor mutational burden (TMB) or microsatellite instability (MSI) that may respond to immunotherapy [57].
Performance Characteristics and Clinical Validation
Recent meta-analyses and clinical trials provide robust quantitative data on the performance of molecularly directed therapies in CUP. A 2024 systematic review and meta-analysis of six studies encompassing 1,644 patients demonstrated that molecularly directed therapy (MDT) was associated with significantly improved overall survival (HR: 0.75, 95% CI: 0.62-0.91) and progression-free survival (HR: 0.79, 95% CI: 0.67-0.94) compared to empiric chemotherapy [59]. This evidence supports MDT as a potential new standard of care in CUP treatment.
Table 2: Clinical Trial Outcomes of Molecularly Directed Therapy in CUP
| Trial | Design | Molecular Technology | Key Survival Outcomes | Clinical Implications |
|---|---|---|---|---|
| CUPISCO (2024) [59] | Randomized Phase 2 | Comprehensive Genomic Profiling | PFS HR: 0.72 (95% CI: 0.56-0.92) | Benefit of tissue-agnostic approach |
| Fudan CUP-001 (2024) [59] | Randomized Controlled Trial | 90-gene expression assay | PFS HR: 0.68 (95% CI: 0.49-0.93) | Benefit of site-specific therapy |
| GEFCAPI 04 [58] | Phase III RCT | Molecular predictions of TOO | mOS 10.0 vs. 10.7 months (HR=0.92) | No significant benefit |
| Hayashi et al. [58] | Phase II Study | Comprehensive microarray GEP | mOS 9.8 vs. 12.5 months (HR=1.03) | No significant benefit |
Beyond predicting tissue of origin, molecular characterization has revealed that CUP tumors possess distinct biological features. A 2024 transcriptomic analysis demonstrated that CUP tumors are characterized by elevated expression of immune-related genes and pathways, high levels of tumor-infiltrating leukocytes (particularly CD8+ T cells), and increased circulating T cells compared to other metastatic cancers [57]. This distinct immunophenotype suggests a unique tumor microenvironment that may explain both the aggressive biology and potential responsiveness to immunotherapy in selected cases.
Figure 1: Molecular Subtyping Decision Pathway for CUP. The flowchart illustrates the diagnostic workflow from CUP presentation through molecular analysis technologies to therapeutic strategies.
Liquid Biopsy for Multi-Cancer Early Detection
Technological Platforms and Analytical Approaches
Liquid biopsy represents a paradigm shift in cancer detection through the analysis of circulating tumor-derived biomarkers in body fluids such as blood, saliva, or urine [60]. Unlike traditional tissue biopsies, liquid biopsies offer a non-invasive approach that can capture tumor heterogeneity and enable dynamic monitoring of disease evolution.
Table 3: Liquid Biopsy Platforms for Cancer Detection
| Technology Platform | Primary Analytes | Detection Principle | Cancer Applications | Stage of Development |
|---|---|---|---|---|
| ctDNA Mutation Analysis [61] | Circulating tumor DNA | Somatic mutations | Treatment monitoring, MRD | Clinical implementation |
| Methylation-Based MCED [62] [63] | DNA methylation patterns | Epigenetic signatures | Multi-cancer screening | Large-scale RCTs ongoing |
| Circulating Tumor Cells [61] | Whole tumor cells | Cell surface markers | Prognosis, functional studies | Research use |
| Extracellular Vesicles [61] | miRNAs, proteins | Cargo analysis | Early detection, monitoring | Preclinical/early clinical |
| Proteomic/Lipidomic [61] | Proteins, metabolites | Mass spectrometry | Companion diagnostics | Emerging |
The analytical sensitivity of liquid biopsy-based MCED tests is fundamentally constrained by both the volume of plasma sampled and the number of markers targeted [62]. This relationship explains why current MCED tests demonstrate higher sensitivity for later-stage cancers, which shed more ctDNA into circulation, compared to early-stage diseases where analyte concentration is substantially lower. Methylation-based MCED tests have gained significant traction in recent development pipelines due to their tissue-specific patterns and early detectability in carcinogenesis [62].
Performance Characteristics Across Cancer Types and Stages
The diagnostic performance of MCED tests varies considerably based on cancer type, stage, and biological characteristics. A recent prospective study of a methylation-based assay tested on more than 5,000 symptomatic patients demonstrated a sensitivity of 66.3%, specificity of 98.4%, and accurate tissue of origin identification in 85.2% of cases [61]. Sensitivity was observed to increase with cancer stage and patient age, reflecting the biological dynamics of tumor DNA shedding.
Table 4: Performance Characteristics of Liquid Biopsy Modalities
| Test Type | Cancer Types | Stage I Sensitivity | Stage IV Sensitivity | Specificity | TOO Accuracy |
|---|---|---|---|---|---|
| Methylation MCED [61] | Multiple (gynecological, lung, GI) | Not specified | Not specified | 98.4% | 85.2% |
| ctDNA CRC Screening [61] | Colorectal | 87.5% (I-III combined) | Not specified | ~90% | Not applicable |
| Proteomic Test [34] | Ovarian, others | Variable by cancer type | Variable by cancer type | >99% (some markers) | Not specified |
| miRNA Signatures [34] | Various | Under investigation | Under investigation | Developing | Emerging |
For colorectal cancer (CRC) screening in asymptomatic average-risk populations, a multimodal ctDNA blood-based test demonstrated 87.5% sensitivity for detecting stage I-III CRC, but only 13.2% sensitivity for advanced precancerous lesions [61]. This limitation in detecting precancerous lesions represents a significant challenge compared to colonoscopy, which can both detect and remove these lesions during the same procedure.
The clinical development pathway for MCED tests requires rigorous validation through large-scale randomized controlled trials with endpoints that demonstrate real clinical benefit, such as reduced late-stage cancer incidence or cancer-specific mortality, rather than just detection capability [62] [63]. Several such trials are currently underway, although whether the diagnostic performance of this first generation of MCED tests is sufficient to translate into clinical benefits remains to be determined [62].
Figure 2: Liquid Biopsy Analytical Workflow. The diagram illustrates the multi-step process from sample collection through analyte isolation and analysis to clinical application.
Comparative Analysis: Technological Integration and Future Directions
Complementary Diagnostic Applications
While molecular subtyping of CUP and liquid biopsy for early detection represent distinct applications of cancer diagnostics, they share common technological foundations in genomic analysis and are increasingly converging in clinical practice. Both approaches face the challenge of analyzing limited tumor material—metastatic biopsies in CUP and low-concentration circulating analytes in liquid biopsy—requiring highly sensitive detection methods.
Table 5: Comparison of Technical and Clinical Parameters
| Parameter | CUP Molecular Subtyping | Liquid Biopsy MCED |
|---|---|---|
| Sample Type | Tumor tissue (metastatic) | Blood/bodily fluids |
| Analytical Sensitivity | High (ample tumor content) | Variable (low ctDNA fraction) |
| Primary Clinical Goal | Identify treatment strategy | Early cancer detection |
| Evidence Level | Phase III RCT meta-analysis | Ongoing large-scale RCTs |
| Implementation Status | Clinical practice guideline | Investigational |
| Tissue of Origin | Essential for therapy selection | Secondary benefit |
| Major Technological Challenge | Tumor heterogeneity | Low analyte concentration |
Artificial intelligence is enhancing both fields through improved pattern recognition in complex datasets. For CUP, AI algorithms can integrate multimodal data from genomic, transcriptomic, and histopathological analyses to improve classification accuracy [56]. In liquid biopsy, AI enables the identification of subtle patterns in fragmentation profiles, methylation states, and genomic alterations that might escape conventional analysis [56].
Research Reagent Solutions and Essential Materials
Table 6: Essential Research Reagents and Platforms
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| NGS Library Prep Kits (KAPA mRNA HyperPrep) [57] | Nucleic acid library construction | Transcriptome sequencing for GEP |
| Hybridization Capture Panels (MedExomePlusV1) [57] | Target enrichment | Comprehensive genomic profiling |
| UMI Adapters (xGEN dual index) [57] | Error suppression | ctDNA mutation detection |
| Methylation Conversion Reagents | Bisulfite treatment | Epigenetic analysis for MCED |
| Immunohistochemistry Antibodies | Protein detection | Lineage determination in CUP |
| Single-cell Isolation Systems | Cell separation | CTC analysis and characterization |
The translational pathway for both technologies must address significant barriers, particularly in resource-limited settings. Developing countries face challenges in implementing advanced molecular diagnostics due to financial constraints, inadequate healthcare infrastructure, and limited technical expertise [64]. Future development should focus on creating more accessible platforms that maintain analytical performance while reducing cost and technical requirements.
Molecular subtyping of CUP and liquid biopsy for early detection represent complementary frontiers in cancer diagnostics, each addressing distinct clinical challenges through shared technological foundations. Molecular subtyping has reached clinical validation with demonstrated survival benefits in CUP patients, supporting its integration into standard practice guidelines. In contrast, liquid biopsy for MCED remains investigational, with ongoing trials determining whether its diagnostic performance translates into meaningful clinical benefits. Both technologies face ongoing challenges in sensitivity, standardization, and accessibility, particularly in resource-limited settings. The convergence of these approaches—potentially using liquid biopsy for initial detection followed by tissue-based molecular characterization for therapy guidance—represents the future of integrated cancer diagnostics. For researchers and drug development professionals, understanding the performance characteristics, technological requirements, and clinical validation status of these platforms is essential for strategic planning in diagnostic development and implementation.
The molecular landscape of cancer is characterized by profound complexity, driven by heterogeneous alterations across genomic, epigenomic, transcriptomic, and proteomic layers. Traditional single-omics approaches have provided valuable but fragmented insights, often failing to capture the interconnected biological networks that drive oncogenesis and therapeutic resistance [65]. The integration of multi-omics data represents a transformative paradigm in cancer research, enabling a systems-level understanding of tumor biology that can power more accurate diagnostics, prognostics, and targeted therapeutic interventions [66]. This approach recognizes that cancer phenotypes emerge from complex interactions across multiple molecular levels, and that combining complementary data types can reveal emergent properties invisible to single-analyte analyses.
The clinical imperative for multi-omics integration stems from the limitations of conventional biomarkers. Single biomarkers frequently lack the sensitivity and specificity required for early detection, patient stratification, or therapeutic monitoring [67] [68]. As noted in foundational biomarker research, "panels of biomarker analytes rather than single markers will be required to have sufficient sensitivity and specificity for the diagnosis or prognosis of cancer" [67]. Multi-omics profiling addresses this limitation by capturing synergistic information across biological layers, creating composite biomarkers with enhanced predictive power. Furthermore, the emergence of sophisticated computational methods, particularly machine learning and graph-based algorithms, has finally enabled researchers to navigate the analytical challenges posed by high-dimensional, heterogeneous omics datasets [69] [65].
Comparative Performance of Multi-Omics Integration Techniques
Analytical Approaches for Data Integration
Multi-omics integration strategies are broadly categorized into early, middle, and late integration based on when in the analytical process data fusion occurs [65]. Early integration concatenates features from different omics layers into a single matrix prior to analysis, while late integration performs separate analyses on each data type and merges the results. Middle integration, which uses statistical and machine learning models to consolidate data without simple concatenation, has emerged as the most powerful approach for capturing complex cross-omics relationships [65].
Recent computational advances have produced specialized frameworks for multi-omics analysis. Graph Neural Networks (GNNs) have demonstrated particular promise due to their ability to model biological systems as interconnected networks [69]. These architectures include Graph Convolutional Networks (GCNs), which operate on graph structures to capture neighborhood information; Graph Attention Networks (GATs), which incorporate attention mechanisms to weight the importance of different connections; and Graph Transformer Networks (GTNs), which handle long-range dependencies within biological networks [69]. Simultaneously, ensemble methods that combine multiple machine learning models have shown robust performance across diverse cancer types [70].
Quantitative Performance Comparison
Recent benchmarking studies provide compelling evidence for the superior performance of multi-omics integration compared to single-omics approaches. The table below summarizes key performance metrics across different integration methods and cancer types:
Table 1: Performance Comparison of Multi-Omics Integration Techniques
| Integration Method | Cancer Type | Omics Data Types | Key Performance Metrics | Reference |
|---|---|---|---|---|
| LASSO-MOGAT (Graph Attention) | Pan-cancer (31 types) | mRNA, miRNA, DNA methylation | Accuracy: 95.9% | [69] |
| MASE-GC (Autoencoder + Ensemble) | Gastric Cancer | Exon, mRNA, miRNA, DNA methylation | Accuracy: 0.981, F1-score: 0.988 | [70] |
| Multi-omics GCN | Pan-cancer | mRNA, miRNA, DNA methylation | Accuracy: ~94% (varies by architecture) | [69] |
| Proteomic risk analysis | 19 cancers | 1,463 plasma proteins | 29 protein-cancer associations with genetic support | [71] |
| Single-omics (DNA methylation only) | Pan-cancer | DNA methylation | Accuracy: 94.88% | [69] |
The performance advantage of multi-omics integration is consistently observed across cancer types and molecular classifications. For instance, in gastric cancer, the MASE-GC framework demonstrated a 15.2% improvement in accuracy compared to single-omics approaches [70]. Similarly, pan-cancer analyses revealed that integrating three omics data types (mRNA, miRNA, and DNA methylation) yielded a 1.02% accuracy improvement over two-omics integration and a 1.02-1.12% improvement over single-omics analyses [69]. These incremental gains, while seemingly modest, can be clinically significant when translated to population-scale screening and diagnostic applications.
Influence of Graph Structures on Model Performance
Beyond the integration algorithm itself, the construction of biological graphs significantly impacts model performance. Research comparing correlation-based graphs versus protein-protein interaction (PPI) networks has demonstrated that "correlation-based graph structures enhance the models' ability to identify shared cancer-specific signatures across patients" [69]. This advantage likely stems from the dynamic nature of correlation networks, which capture patient-specific molecular patterns, compared to static PPI networks that represent general biological knowledge.
Experimental Protocols and Methodological Frameworks
Graph Neural Network Protocol for Pan-Cancer Classification
A comprehensive benchmark study established a robust protocol for multi-omics cancer classification using graph neural networks [69]. The methodology comprises several critical stages:
Data Acquisition and Preprocessing: The analysis utilized 8,464 samples from 31 cancer types and normal tissue from TCGA, incorporating messenger RNA (mRNA), micro-RNA (miRNA), and DNA methylation data. Feature selection was performed using differential gene expression analysis and LASSO (Least Absolute Shrinkage and Selection Operator) regression to address high dimensionality [69].
Graph Construction: Two graph structures were investigated: (1) Correlation-based graphs using sample correlation matrices to capture patient similarity; (2) Knowledge-based graphs using protein-protein interaction networks from databases such as STRING to incorporate prior biological knowledge [69].
Model Architecture and Training: Three GNN architectures were implemented and compared: GCN, GAT, and GTN. The models were trained using a 70-15-15 train-validation-test split with five-fold cross-validation. The graph attention network employed in LASSO-MOGAT utilized attention mechanisms to compute neighborhood importance weights, enabling adaptive learning from complex graph structures [69].
Validation: Model performance was assessed using accuracy, precision, recall, and F1-score, with ablation studies conducted to evaluate the contribution of individual omics layers [69].
The following workflow diagram illustrates this experimental protocol:
Autoencoder and Ensemble Framework for Gastric Cancer Classification
The MASE-GC framework demonstrates an alternative approach combining deep feature extraction with ensemble learning [70]:
Data Preprocessing: The protocol incorporated exon expression, mRNA expression, miRNA expression, and DNA methylation data from the TCGA-STAD cohort. Preprocessing included filtering low-abundance features, K-nearest neighbor imputation for missing methylation values, min-max normalization, and differential feature screening using the LIMMA R package with a Benjamini-Hochberg adjusted p-value threshold of <0.001 [70].
Class Imbalance Handling: A hybrid SMOTE-Tomek algorithm addressed dataset imbalance by generating synthetic minority class samples while removing ambiguous boundary cases [70].
Multi-omics Integration: Modality-specific autoencoders extracted compact latent features from each omics layer, followed by weighted fusion to create integrated representations [70].
Ensemble Classification: A stacking ensemble incorporated five base learners (Support Vector Machine, Random Forest, Decision Tree, AdaBoost, and Convolutional Neural Network) with an XGBoost meta-classifier [70].
Validation: The model underwent internal validation on TCGA data and external validation on four independent cohorts (GSE62254, GSE15459, GSE84437, and ICGC), demonstrating robust generalizability [70].
Signaling Pathways and Biological Networks in Multi-Omics Integration
Cross-Omics Regulatory Networks
Multi-omics data integration reveals complex hierarchical relationships across molecular layers, with information flowing from genetic and epigenetic alterations through transcriptomic changes to proteomic and functional phenotypes. The following diagram illustrates key signaling pathways and their cross-omics interactions in cancer biology:
Key Pathway Insights from Multi-Omics Studies
Multi-omics approaches have elucidated several critical cancer pathways where interactions across molecular layers drive pathogenesis:
Immune Evasion Pathways: Multi-omics analyses of hematological malignancies revealed significant enrichment of proteins involved in adaptive immune response, including FC-receptor proteins (FCRL1, FCRL2, FCRL3, FCRL5, FCRLB) and TNF receptor family members (TNFRSF4, TNFRSF9, TNFRSF13B, TNFRSF13C) [71]. These networks connect genetic variants with protein-level immune checkpoint expression, explaining mechanisms of immune evasion.
Metabolic Reprogramming Networks: Integrated analyses have identified oncometabolites such as 2-hydroxyglutarate in IDH1/2-mutant gliomas, which create functional connections between genomic mutations, metabolic dysregulation, and epigenetic remodeling [66].
Growth Factor Signaling Cascades: Proteogenomic studies demonstrate discordance between mRNA expression and protein abundance in key growth factor pathways, highlighting the importance of post-transcriptional regulation in oncogenic signaling [65]. For instance, multi-omics classification models have identified IGFBP7 and IGFBP3 as key nodes connecting transcriptional regulation with protein-level activity in liver cancer [71].
Research Reagent Solutions and Computational Tools
Successful multi-omics research requires specialized reagents, databases, and computational tools. The following table catalogs essential resources for designing and implementing multi-omics studies:
Table 2: Essential Research Reagents and Computational Tools for Multi-Omics Studies
| Resource Category | Specific Tools/Reagents | Application/Function | Key Features |
|---|---|---|---|
| Multi-omics Databases | TCGA, ICGC, CPTAC, COSMIC, DepMap | Data source for multi-omics analysis | Curated cancer omics data with clinical annotations [65] |
| Proteomics Platforms | Olink Platform, LC-MS/MS, Reverse-phase protein arrays | Protein quantification | High-throughput measurement of protein abundance and modifications [66] [71] |
| Genomic/Epigenomic Tools | Whole genome bisulfite sequencing, Illumina Infinium Methylation arrays | DNA methylation analysis | Genome-wide profiling of epigenetic modifications [66] |
| Transcriptomic Technologies | RNA-Seq, miRNA-Seq, Microarrays | RNA expression profiling | Comprehensive characterization of coding and non-coding transcripts [66] |
| Graph Neural Network Tools | LASSO-MOGCN, LASSO-MOGAT, LASSO-MOGTN | Multi-omics data integration | Graph-based integration of heterogeneous omics data [69] |
| Ensemble Machine Learning Frameworks | MASE-GC, XGBoost, Random Forest | Classification and feature selection | Combines multiple models for improved prediction accuracy [70] |
| Pathway Analysis Resources | STRING, KEGG, DriverDBv4 | Biological network analysis | Contextualizes findings within established pathways [72] |
The integration of multi-omics data represents a paradigm shift in cancer research, moving beyond single-analyte approaches to embrace the complexity of biological systems. Experimental evidence consistently demonstrates that multi-omics integration outperforms single-omics analyses across diverse cancer types and clinical applications. Graph neural networks and ensemble methods have emerged as particularly powerful computational frameworks for capturing the complex relationships across genomic, transcriptomic, epigenomic, and proteomic layers.
The future of multi-omics integration will likely be shaped by several key developments. Single-cell multi-omics technologies are rapidly advancing, enabling researchers to deconvolute tumor heterogeneity and microenvironment interactions at unprecedented resolution [66]. Spatial multi-omics approaches add geographical context to molecular measurements, revealing how cellular neighborhoods influence cancer behavior [66]. From a computational perspective, the development of more interpretable AI models will be crucial for translating complex multi-omics signatures into clinically actionable insights. Finally, the integration of digital pathology and medical imaging data with molecular profiles promises to create truly comprehensive views of tumor biology, further blurring the boundaries between different data modalities in pursuit of more effective cancer diagnostics and therapeutics.
Navigating Technical Hurdles: Optimization Strategies for Sensitivity, Specificity, and Clinical Integration
The accuracy of molecular cancer diagnostics is fundamentally challenged by pre-analytical variables, which encompass all procedures from sample collection to data generation. These variables introduce significant uncertainty into biomarker measurements, potentially compromising diagnostic, prognostic, and predictive applications [73]. Among the most critical challenges are tumor sample heterogeneity—variation in the proportion of malignant cells within a specimen—and a host of other factors related to biospecimen handling [73]. The integrity of the sample is paramount, as it forms the foundational material upon which critical clinical and research decisions are based. This guide objectively compares the impact of these pre-analytical variables on different molecular analytical techniques, providing a structured overview of their effects and the relative robustness of various diagnostic approaches.
Quantitative Impact of Pre-analytical Variables on Molecular Analyses
Pre-analytical variables can systematically alter gene expression measurements, affecting the reliability of transcriptomics-based diagnostics. The following table summarizes the quantitative impact of specific single pre-analytical variables on gene expression values and the stability of within-sample Relative Expression Orderings (REOs) of gene pairs, based on an analysis of over 800 paired samples [73].
Table 1: Impact of Single Pre-analytical Variables on Gene Expression and REOs
| Pre-analytical Variable | Comparison (Case vs. Control) | Average Number of Genes with 2-Fold Change | Average REO Consistency Score | Average REO Consistency (Excluding 10% Closest-Expressing Pairs) |
|---|---|---|---|---|
| Sampling Methods | Biopsy vs. Surgical (Esophageal Cancer) | 3,286 | >86% | 89.90% |
| Tumor Sample Heterogeneity | Low vs. High Tumor Cell Proportion | 5,707 | 89.24% | 92.46% |
| Fixed Time Delays | 24-hour delay vs. 0-hour (Bone Marrow) | 2,113 | 88.94% | 92.27% |
| Fixed Time Delays | 48-hour delay vs. 0-hour (Bone Marrow) | 2,970 | 85.63% | 88.84% |
| Preservation Conditions | FFPE vs. Fresh-Frozen (Lung/Breast Cancer) | 5,009 (avg) | 86.42% (avg) | Information not specified |
| Preservation Conditions | FFPE vs. Fresh-Frozen (Lung/Breast Cancer) | 10,388 (avg) | 84.64% (avg) | Information not specified |
The data demonstrates that while pre-analytical conditions can induce large changes in quantitative gene expression (thousands of genes with twofold changes), the qualitative Relative Expression Ordering (REO) remains notably more stable, with consistency scores routinely exceeding 85% [73]. This robustness is further enhanced when gene pairs with nearly identical expression levels are excluded from the analysis.
Comparative Robustness of Analytical Techniques
Different molecular diagnostic techniques exhibit varying levels of susceptibility to pre-analytical challenges. The following table compares several prominent techniques based on their reported resilience to common sample quality issues.
Table 2: Comparative Robustness of Molecular Diagnostic Techniques to Pre-analytical Variables
| Analytical Technique | Key Measured Analytes | Reported Vulnerabilities & Strengths | Documented Impact |
|---|---|---|---|
| Gene Expression Profiling (Absolute Quantification) | mRNA levels | Highly vulnerable to sample degradation, fixation delays, and tumor heterogeneity [73]. | Thousands of differentially expressed genes reported due to pre-analytical variables [73]. |
| Relative Expression Ordering (REO) | Within-sample mRNA rank | Highly robust to sample degradation, fixation, and heterogeneity; maintains >85% consistency despite variables [73]. | REO-based signatures can overcome major limitations of absolute quantification for biomarker development [73]. |
| Liquid Biopsy | ctDNA, CTCs, Exosomes, miRNAs | Pre-analytical variables are a pivotal concern; can cause false positives/negatives and variability in tumor signal analysis [74]. | Standardized collection, processing, and storage protocols are critical for clinical utility [74]. |
| AI-Enhanced Digital Pathology | Whole Slide Images (WSI) | Can be trained to be robust to certain variations; performance is dependent on training data quality and diversity [56] [75]. | Successful AI integration can reduce radiologist workload by 54.5% and improve screening specificity [75]. |
| Multi-Omic AI Platforms | Proteins, Lipids, Metabolites (e.g., Gangliosides) | Combines multiple data types; machine learning can uncover disease signatures robust to noise in single analytes [76]. | Achieved AUC of 89-92% for early-stage ovarian cancer detection in symptomatic women, outperforming single markers like CA125 [76]. |
Detailed Experimental Protocols for Assessing Pre-analytical Variables
Understanding the experimental methodologies used to quantify the impact of pre-analytical variables is crucial for interpreting the data and designing robust studies.
Protocol for Evaluating Gene Expression and REO Robustness
The following methodology was used to generate the data in Table 1, based on the analysis of 18 datasets [73]:
- Sample Collection and Paired Study Design: Over 800 paired samples were collected from public databases (e.g., GEO, TCGA, SRA). For each pre-analytical variable (e.g., sampling method, preservation condition), a "case" sample (e.g., biopsy, FFPE) was compared to a paired "control" sample (e.g., surgical, fresh-frozen) from the same patient.
- Data Preprocessing: Gene expression data from oligonucleotide technology or Illumina-based sequencing technology were uniformly processed to ensure comparability.
- Differential Expression Analysis:
- Individual Level: The fold change (FC) for each gene was calculated between each paired case and control sample. Genes with FC > 2 were defined as differentially expressed.
- Population Level: Differentially expressed genes (DEGs) between case and control groups were identified using the
limmapackage with a False Discovery Rate (FDR) < 0.05 and FC > 2.
- REO Consistency Scoring:
- For each sample, all possible gene pairs (Gi, Gj) were defined by their REO (Gi > Gj or Gi < Gj).
- The Consistency Score between a paired case and control sample was calculated as N/(N+M), where N is the number of gene pairs with consistent REOs and M is the number with contradictory REOs.
- To enhance robustness, the analysis was repeated after excluding the 10% of gene pairs with the smallest absolute rank differences (closest expression levels) in the control sample.
Protocol for AI-Assisted Ultrasound Screening (HCC)
A retrospective, multicenter study evaluated four AI-assisted strategies for hepatocellular carcinoma (HCC) screening to improve accuracy and reduce radiologist workload [75]:
- Dataset: 21,934 liver ultrasound images from 11,960 patients were used. Models were trained on 17,913 images.
- AI Models:
- UniMatch: A deep learning model for detecting liver lesions.
- LivNet: A deep learning model for classifying detected lesions as benign or malignant, informing recall decisions.
- Human-AI Interaction Strategies: Four distinct strategies were tested for integrating AI into the screening workflow, ranging from fully automated AI assessment to AI as a triage tool or for second-reader functions. The optimal strategy (Strategy 4) used AI for initial detection and had radiologists evaluate negative cases in both detection and classification phases.
- Performance Metrics: Sensitivity, specificity, Area Under the Curve (AUC), radiologist workload (number of images requiring review), recall rate, and false positive rate were compared against the standard of care (radiologist-only assessment).
Visualizing Comparative Analysis and Workflows
REO Robustness Analysis Workflow
The diagram below illustrates the logical workflow for assessing the robustness of Relative Expression Orderings (REOs) against pre-analytical variables.
AI-Human Integration Strategy Comparison
This diagram outlines the four human-AI interaction strategies tested in the HCC screening study, with the optimal strategy (Strategy 4) highlighted.
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details essential reagents, materials, and tools referenced in the studies on pre-analytical variables and molecular techniques.
Table 3: Research Reagent Solutions for Pre-analytical and Analytical Workflows
| Item / Tool Name | Function / Application | Relevance to Pre-analytical Challenges |
|---|---|---|
| PAXgene Tissue System | Stabilizes RNA and proteins in tissue samples immediately upon collection. | Mitigates the effects of fixed time delays and preserves biomolecular integrity at room temperature [73]. |
| Liquid Chromatography Mass Spectrometry (LC-MS) | Analyzes complex mixtures of lipids, proteins, and metabolites from blood samples. | Core technology for multi-omic platforms; enables discovery of novel, stable biomarker classes like gangliosides [76]. |
| Cell-Free DNA BCT Tubes | Blood collection tubes that stabilize nucleated blood cells and prevent genomic DNA contamination of plasma. | Critical pre-analytical step in liquid biopsy to ensure accurate ctDNA analysis and minimize false positives [74]. |
| UniMatch Model | A deep learning model for detecting liver lesions in ultrasound images. | AI tool used to quantify and reduce the impact of operator dependency and workload in image-based screening [75]. |
| LivNet Model | A deep learning model for classifying liver lesions from ultrasound images. | AI tool that improves specificity in distinguishing benign from malignant lesions, reducing false recalls [75]. |
| Limma R Package | A statistical package for analyzing gene expression data, especially for identifying differentially expressed genes. | Key software tool for quantifying the impact of pre-analytical variables on transcriptomic data [73]. |
The detection of low-frequency genetic variants is a critical challenge in modern molecular diagnostics, especially in oncology for monitoring tumor heterogeneity, minimal residual disease, and emerging treatment-resistance mutations. The variant allele frequency (VAF) – the percentage of sequencing reads carrying a specific genetic variant – often defines the detection limit for these applications. While standard next-generation sequencing (NGS) and PCR-based methods have been widely adopted, their varying sensitivities and specificities create important trade-offs for researchers and clinicians. This guide provides an objective comparison of the technical performance of conventional PCR, digital PCR (dPCR), and NGS, synthesizing recent experimental data to inform method selection for cancer research and drug development.
Performance Comparison at a Glance
The following table summarizes the key technical characteristics and performance metrics of each method, based on current published studies.
Table 1: Technical Performance Comparison of PCR, dPCR, and NGS
| Feature | Conventional (q)PCR | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Key Principle | Relative quantification using standard curves | Absolute quantification by sample partitioning & Poisson statistics [77] | Massively parallel sequencing of DNA fragments |
| Theoretical Limit of Detection (LOD) for VAF | ~1-5% | <0.01% (1 in 10,000 alleles) [77] [78] | Standard: ~0.5-1%Ultrasensitive Methods: <0.1% [79] [80] |
| Demonstrated LOD in Recent Studies | Not a primary focus in reviewed literature | ~0.1% VAF [78] | 0.15% VAF for SNVs/Indels (Northstar Select assay) [80] |
| Quantification Type | Relative | Absolute (counts molecules) [77] | Relative (based on read counts) |
| Multiplexing Capability | Low to moderate | Moderate (e.g., multiplex drop-off assays) [81] [82] | High (can profile dozens to hundreds of genes simultaneously) [83] |
| Throughput | High | Moderate to High (increasing with automation) [77] | Very High |
| Best Application | High VAF detection, rapid target screening | Ultra-sensitive quantification of known, predefined variants [81] [77] | Discovery-based profiling, multi-gene analysis, detecting novel variants [81] [83] |
Detailed Experimental Evidence and Protocols
Recent comparative studies and validation papers provide critical data on how these technologies perform head-to-head in real-world research scenarios.
Direct Comparison of dPCR and Targeted NGS
A 2025 comparative study by Corné et al. directly evaluated the performance of multiplex dPCR and a targeted NGS assay for detecting ERBB2, ESR1, and PIK3CA mutations in plasma circulating cell-free DNA from 32 patients with metastatic breast cancer [81] [82].
- Experimental Protocol: The researchers analyzed a series of 32 cfDNA samples from patients with HR+ HER2- metastatic breast cancer. These samples had been previously tested using lab-developed multiplex dPCR assays. The same samples were then analyzed using the Plasma-SeqSensei (PSS) BC targeted NGS assay. The cfDNA input amounts ranged from 4.0 to 43 ng. The results from both techniques were directly compared for concordance and correlation [82].
- Key Findings: The study detected 44 mutations with an overall concordance of 95% (90/95) between the two methods. The correlation of VAF measurements was exceptionally high (R² = 0.9786). The study highlighted that both methods could reliably detect mutations at low VAFs (as low as 0.14%), though some discordances occurred in this very low VAF range. Notably, each method identified mutations missed by the other: NGS detected an additional PIK3CA mutation (p.P539R) later confirmed by a newly designed dPCR assay, while a multiplex drop-off dPCR system identified two ESR1 mutations also detected by NGS [81] [82].
- Conclusion: The targeted NGS assay performed comparably to multiplex dPCR for screening predefined mutations in liquid biopsies, offering a highly sensitive, ready-to-use solution for labs with NGS infrastructure [81].
Pushing the Limits of Detection with NGS
The demand for more sensitive NGS assays in liquid biopsy, particularly for low-shedding tumors, has driven the development of assays with lower limits of detection.
- Experimental Protocol: A 2025 study conducted analytical and clinical validation of Northstar Select, a plasma-based, comprehensive genomic profiling (CGP) assay covering 84 genes. The assay's performance was validated using 674 retrospective patient samples and prospectively compared to on-market CGP assays in 182 patients [80].
- Key Findings: Analytical validation demonstrated a 95% limit of detection of 0.15% VAF for single nucleotide variants and indels, which was confirmed by ddPCR. In the prospective head-to-head study, Northstar Select identified 51% more pathogenic SNVs/indels and 109% more copy number variations (CNVs) than the on-market comparators. Critically, 91% of the additional clinically actionable variants it found were detected below 0.5% VAF, leading to 45% fewer null reports (reports with no actionable findings) [80].
- Conclusion: This demonstrates that innovative NGS assays are closing the sensitivity gap with dPCR while retaining the advantage of broad, multi-variant class profiling, making them highly suitable for clinical CGP where tumor DNA shedding is low [80].
Ultrasensitive NGS Methodologies
Beyond standard NGS, specialized "consensus sequencing" methods are being developed to detect even rarer variants, pushing into the VAF range of 10⁻⁵ to 10⁻⁶ for specific applications [79]. These methods, such as Duplex Sequencing and Safe-SeqS, generate consensus sequences from multiple reads of the original DNA template to correct for errors introduced during PCR and sequencing. While not yet routine in clinical diagnostics, they represent the cutting edge of sensitivity for research applications like studying very early carcinogenesis [79].
Workflow and Decision Pathways
The following diagram illustrates the typical experimental workflows for dPCR and targeted NGS, highlighting key differences in process and output.
The Scientist's Toolkit: Key Research Reagents and Materials
Successful implementation of these sensitive assays relies on a suite of specialized reagents and tools. The following table lists essential components for the experiments cited in this guide.
Table 2: Essential Research Reagents and Kits for Sensitive Variant Detection
| Reagent / Kit Name | Function / Application | Key Feature / Purpose |
|---|---|---|
| QIAamp Circulating Nucleic Acid Kit (Qiagen) | Extraction of cell-free DNA (cfDNA) from plasma [83] | Optimized for obtaining high-quality, inhibitor-free cfDNA from low-concentration liquid biopsy samples. |
| Absolute Q DNA dPCR Master Mix (Applied Biosystems) | Master mix for digital PCR reactions [78] | Contains reagents essential for precise and sensitive dPCR, including polymerase, optimized buffer, and dNTPs. |
| Custom TaqMan Assay (Applied Biosystems) | Sequence-specific detection in dPCR [78] | Includes primers and fluorescent probes (FAM/VIC) designed to discriminate wild-type and mutant alleles with high specificity. |
| KAPA Hyper DNA Library Prep Kit (Roche) | Construction of sequencing-ready libraries for NGS [83] | Facilitates fragmentation, end-repair, A-tailing, and adapter ligation for Illumina sequencing platforms. |
| AmpliSeq Custom Panels (Thermo Fisher) | Targeted NGS library preparation [78] | Enables highly multiplexed PCR-based amplification of custom gene panels (e.g., for the UBA1 gene in VEXAS syndrome). |
| Plasma-SeqSensei PSS BC Assay (Sysmex Inostics) | Targeted NGS for breast cancer [82] | A ready-to-use, highly sensitive NGS panel optimized for detecting low-frequency variants in plasma ctDNA. |
The choice between dPCR and NGS for detecting low-frequency variants is not a matter of which technology is superior, but which is more appropriate for the specific research question.
- Digital PCR remains the gold standard for the absolute quantification of known, low-frequency variants (<0.1% VAF), offering unparalleled sensitivity and precision for focused applications like monitoring minimal residual disease or specific resistance mutations [77] [78].
- Next-Generation Sequencing provides a comprehensive, multi-genic view and is superior for discovery, profiling, and when the exact mutation is not known a priori. With the advent of highly sensitive assays (LOD ~0.15% VAF), NGS is increasingly capable of identifying actionable variants in samples with low ctDNA burden, making it a powerful tool for comprehensive genomic profiling in precision oncology [83] [80].
The future lies in the synergistic use of these technologies. For instance, using dPCR to validate and longitudinally monitor key mutations first identified by broad NGS screening. Furthermore, the integration of AI and machine learning with NGS data is poised to enhance the predictive value of the variants detected, further personalizing cancer diagnostics and treatment [56] [84]. As both technologies continue to evolve, their combined application will undoubtedly accelerate drug development and improve patient outcomes in oncology research.
In the field of cancer diagnostics research, the convergence of next-generation sequencing (NGS) technologies and advanced imaging has generated unprecedented volumes of complex data, presenting both extraordinary opportunities and formidable challenges. Molecular techniques now generate terabytes of data per project, requiring sophisticated bioinformatics pipelines and robust data management frameworks to extract meaningful biological insights [85] [15]. The versatility of NGS platforms has expanded the scope of genomics research, facilitating studies on rare genetic diseases, cancer genomics, microbiome analysis, and population genetics [15]. Simultaneously, AI-facilitated imaging diagnostics are transforming how we identify early-stage cancers through modalities including computed tomography, magnetic resonance imaging, and digital pathology [56]. This comparison guide examines the current landscape of data management and bioinformatics solutions for handling these complex NGS and imaging datasets within cancer research, providing researchers with objective performance comparisons and experimental protocols to inform their investigative workflows.
Next-Generation Sequencing Technologies: Performance Comparison
NGS Platform Specifications and Capabilities
The evolution of DNA sequencing technologies has progressed from first-generation Sanger sequencing to second-generation short-read platforms, and more recently to third-generation long-read technologies that sequence single molecules [15] [86]. As of 2025, the market features 37 sequencing instruments from 10 key companies, each with distinct strengths for specific cancer research applications [86]. The table below compares the core technical attributes of major sequencing platforms used in cancer genomics research:
Table 1: Comparison of Leading NGS Platforms for Cancer Research Applications
| Platform | Technology Type | Read Length | Accuracy | Key Strengths | Primary Cancer Applications |
|---|---|---|---|---|---|
| Illumina NovaSeq X | Short-read (SBS) | 36-300 bp | >Q30 (99.9%) | High throughput, low per-base cost | Whole genome sequencing, large cohort studies, tumor profiling [85] [87] |
| PacBio Revio (HiFi) | Long-read (SMRT) | 10-25 kb | Q30-Q40 (99.9-99.99%) | High accuracy long reads, epigenetic detection | Structural variant detection, haplotype phasing, fusion genes [86] |
| Oxford Nanopore (Q30 Duplex) | Long-read (Nanopore) | 10-30 kb | >Q30 (99.9%) | Real-time sequencing, ultra-long reads | Rapid diagnostics, metagenomics, full-length transcriptomics [86] |
| PacBio Onso System | Short-read (SBB) | 100-200 bp | High (Q30+) | Accuracy, cost-efficiency | Targeted sequencing, validation studies [86] |
Experimental Performance in Cancer Genomics
Recent studies have demonstrated how these sequencing technologies perform in specific cancer research contexts. For structural variant detection in complex cancer genomes, PacBio HiFi reads have shown superior performance compared to short-read approaches, with one study detecting over 90% of known structural variants in reference samples versus 65-75% with short-read technologies [86]. In liquid biopsy applications, Oxford Nanopore's duplex sequencing has enabled detection of circulating tumor DNA at variant allele frequencies as low as 0.1% while providing methylation data simultaneously [86].
For tumor mutational burden assessment, Illumina's short-read platforms remain the gold standard due to their high base-level accuracy and extensive validation in clinical settings, with error rates below 0.1% [87]. However, emerging data suggests that combining long-read and short-read approaches provides the most comprehensive view of cancer genomes, particularly for regions with high GC content or complex rearrangements [15].
Bioinformatics Tools for NGS Data Analysis
Comparative Performance of Variant Calling Algorithms
Variant calling from NGS data represents a critical bottleneck in cancer genomics, with accuracy being paramount for reliable mutation detection. Multiple studies have compared the performance of popular variant calling algorithms using reference samples with known mutation profiles:
Table 2: Performance Comparison of Bioinformatics Tools for NGS Data Analysis in Cancer Research
| Tool | Primary Function | Key Features | Accuracy in Cancer Samples | Computational Requirements |
|---|---|---|---|---|
| DeepVariant | Variant calling | Deep learning-based | >99.5% for SNVs in WGS | High (GPU recommended) [85] [88] |
| GATK | Variant calling | Broad Institute standard | 98.7% for SNVs with proper calibration | Moderate [85] |
| BLAST | Sequence alignment | Local alignment searches | Gold standard for small sequences | Low to moderate [88] |
| Bioconductor | Genomic analysis | R-based packages | Highly customizable for RNA-seq | Moderate to high [88] |
| Clustal Omega | Multiple sequence alignment | Progressive alignment | Limited for highly divergent sequences | Moderate [88] |
Specialized Cancer Genomics Workflows
In cancer research, specialized bioinformatics workflows have been developed to address tumor-specific challenges such as tumor heterogeneity and low tumor purity. Tools like Prov-GigaPath have demonstrated exceptional performance in analyzing whole-slide images and integrating pathological features with genomic data [56]. For multi-omics integration in cancer studies, platforms like Galaxy provide user-friendly interfaces that enable researchers without extensive programming expertise to build reproducible analytical pipelines [88].
Recent benchmarks of AI-driven tools for variant calling have shown that deep learning approaches like DeepVariant significantly outperform traditional statistical methods, particularly in detecting low-frequency variants in heterogeneous tumor samples [85]. In one controlled experiment using validated reference standards, DeepVariant achieved 99.65% sensitivity for single nucleotide variants at 50x coverage, compared to 98.2% for conventional callers [88].
Diagram 1: Standard NGS data analysis workflow in cancer research
Data Management Frameworks for Large-Scale Cancer Studies
FAIR Principles Implementation
Effective management of complex NGS and imaging datasets requires adherence to the FAIR Guiding Principles - ensuring data are Findable, Accessible, Interoperable, and Reusable [89] [90]. Implementation of these principles is particularly crucial in cancer research where data integration across multiple studies and institutions accelerates discovery. The FAIR principles emphasize machine-actionability, recognizing that computational systems must be able to find, access, interoperate, and reuse data with minimal human intervention given the volume and complexity of modern cancer datasets [90].
Findability requires that data and metadata are assigned persistent identifiers and are indexed in searchable resources. Accessibility involves standardizing communication protocols and ensuring metadata remains accessible even when data is restricted. Interoperability depends on using shared vocabularies and standards that enable data integration. Reusability requires rich metadata descriptions of context, usage licenses, and provenance [89].
Cloud Computing Infrastructure
The volume of data generated by NGS and multi-omics studies often exceeds terabytes per project, making cloud computing essential for modern cancer research [85]. Platforms like Amazon Web Services (AWS) and Google Cloud Genomics provide scalable infrastructure to store, process, and analyze this data efficiently [85]. Benefits include:
- Scalability: Handling datasets of virtually any size with elastic computing resources
- Global Collaboration: Enabling researchers from different institutions to collaborate on the same datasets in real-time
- Cost-Effectiveness: Allowing smaller labs to access advanced computational tools without significant infrastructure investments
- Security: Compliance with regulatory frameworks such as HIPAA and GDPR for sensitive genomic data [85]
Performance benchmarks show that optimized cloud-based pipelines can process whole genome sequencing data in 6-8 hours at a cost of approximately $25 per genome, making large-scale cancer genomics studies economically feasible [85].
AI and Machine Learning for Imaging Data Analysis in Cancer
Performance Comparison of AI-Based Imaging Tools
Artificial intelligence has revolutionized the analysis of medical images in cancer diagnostics, with deep learning algorithms now matching or exceeding human performance in specific tasks such as tumor detection and classification [56]. The table below compares leading AI technologies for cancer imaging analysis:
Table 3: Comparison of AI Technologies for Cancer Imaging Analysis
| AI Technology | Imaging Modality | Reported Performance | Key Applications |
|---|---|---|---|
| Prov-GigaPath | Digital pathology | AUC 0.96 for cancer subtyping | Whole-slide image analysis, prognosis prediction [56] |
| Owkin's Models | Multiple | 92% accuracy for therapy response | Predictive biomarker discovery, clinical trial optimization [56] |
| CHIEF | CT/MRI | 94% sensitivity for lesion detection | Tumor segmentation, radiomics feature extraction [56] |
| Deep Learning Radiomics | CT/PET | AUC 0.92 for metastasis prediction | Treatment response monitoring, survival prediction [56] |
Experimental Protocols for AI-Based Image Analysis
Standardized experimental protocols are essential for reproducible AI-based cancer image analysis. A typical workflow includes:
Data Acquisition and Annotation: Collecting high-quality digital pathology slides or radiographic images with expert annotations. For whole-slide images in pathology, scans are typically performed at 40x magnification [56].
Preprocessing and Augmentation: Applying normalization, stain normalization for pathology images, and data augmentation techniques to increase dataset diversity and model robustness.
Model Training: Implementing deep learning architectures (often convolutional neural networks) with appropriate regularization to prevent overfitting. Training typically uses 60-70% of the data.
Validation and Testing: Evaluating model performance on held-out datasets (15-20% for validation, 15-20% for testing) using metrics such as AUC, sensitivity, specificity, and F1-score.
In a recent study comparing pathologist and AI performance in breast cancer detection, the AI system achieved an AUC of 0.994, comparable to the pathologist average of 0.966, demonstrating the potential of AI to assist in diagnostic workflows [56].
Diagram 2: AI-powered medical image analysis workflow for cancer diagnostics
Multi-Omics Integration in Cancer Research
Bioinformatics Platforms for Multi-Omics Data
Multi-omics approaches that combine genomics, transcriptomics, proteomics, and metabolomics provide a comprehensive view of biological systems in cancer, linking genetic information with molecular function and phenotypic outcomes [85]. Several bioinformatics platforms specialize in integrating these diverse data types:
- Bioconductor: Provides over 2,000 R-based packages specifically designed for multi-omics integration, though it requires significant computational expertise [88]
- Galaxy: Offers a user-friendly, web-based interface with tools for multi-omics analysis, making it accessible to wet-lab researchers [88]
- KEGG: Specializes in pathway analysis and visualization, enabling researchers to map multi-omics data onto biological pathways [88]
In cancer research, multi-omics integration has been particularly valuable for dissecting the tumor microenvironment, revealing interactions between cancer cells and their surroundings that inform therapeutic strategies [85]. For example, combining genomic data on mutations with proteomic data on protein abundance has identified resistance mechanisms to targeted therapies in melanoma and lung cancer.
Experimental Protocol for Multi-Omics Studies
A standardized protocol for multi-omics studies in cancer research includes:
Sample Preparation: Processing matched samples for genomic, transcriptomic, proteomic, and metabolomic analyses from the same tumor specimen.
Data Generation:
- DNA sequencing (whole genome or exome)
- RNA sequencing (bulk or single-cell)
- Proteomic profiling (mass spectrometry-based)
- Metabolomic profiling (LC-MS or GC-MS)
Data Processing: Using specialized tools for each data type (e.g., DeepVariant for genomics, DESeq2 for transcriptomics, OpenMS for proteomics).
Integration Analysis: Employing multi-omics integration algorithms such as MOFA+ or mixOmics to identify cross-omic patterns.
Biological Validation: Testing key findings using functional experiments in model systems.
In a recent study of breast cancer subtypes, multi-omics integration identified novel subgroups with distinct clinical outcomes that were not apparent from genomic analysis alone, demonstrating the power of integrated approaches [85].
Essential Research Reagent Solutions
The following table details key research reagents and materials essential for experiments generating NGS and imaging data in cancer research:
Table 4: Essential Research Reagent Solutions for Cancer Genomics and Imaging
| Reagent/Material | Function | Application Context | Considerations |
|---|---|---|---|
| Q30+ Duplex Kit (ONT) | Library preparation for nanopore sequencing | Long-read sequencing, structural variant detection | Enables >Q30 accuracy with duplex reads [86] |
| HiFi SMRTbell Prep Kit (PacBio) | Library preparation for SMRT sequencing | High-fidelity long-read sequencing, epigenetics | Requires high molecular weight DNA [86] |
| TruSeq DNA PCR-Free (Illumina) | Library preparation for short-read sequencing | Whole genome sequencing, variant detection | Minimizes PCR bias [85] |
| Barcoded Antibodies (CITE-seq) | Protein surface marker detection | Single-cell multi-omics, tumor heterogeneity | Converts protein abundance to sequenceable tags [86] |
| Spatial Barcoding Reagents | Spatial transcriptomics | Tumor microenvironment mapping | Preserves spatial context in tissue sections [56] |
The landscape of data management and bioinformatics for NGS and imaging datasets in cancer research continues to evolve rapidly, driven by technological advancements and growing data volumes. The integration of AI and machine learning across the data analysis pipeline, from variant calling to image interpretation, is setting new standards for accuracy and efficiency [85] [56]. Emerging trends include the adoption of federated learning approaches to enable collaborative model training without sharing sensitive patient data, and the development of more sophisticated multi-omics integration tools that can handle temporal and spatial dimensions of tumor evolution [56].
For researchers navigating this complex landscape, the optimal strategy involves selecting sequencing technologies and analytical tools based on specific research questions rather than seeking a universal solution. Combining complementary technologies—such as using both short-read and long-read sequencing for comprehensive variant detection—often provides the most complete picture of cancer genomics [15] [86]. Similarly, implementing robust data management practices following FAIR principles from the beginning of a project ensures that valuable datasets remain accessible and reusable for future research, maximizing the return on research investments and accelerating progress in cancer diagnostics and treatment [89] [90].
The field of cancer diagnostics has undergone a revolutionary transformation with the advent of sophisticated molecular techniques. Next-generation sequencing (NGS), digital PCR, and quantitative PCR (qPCR) now provide unprecedented capabilities for detecting genetic alterations driving cancer progression [15]. While these technologies share the common goal of identifying clinically actionable variants, they differ significantly in their operational parameters, workflow requirements, and economic profiles. For researchers, scientists, and drug development professionals, selecting the appropriate technological platform requires careful consideration of multiple factors, including throughput needs, turnaround time constraints, and infrastructure capabilities [91]. This guide provides an objective comparison of current molecular techniques, focusing on their practical implementation in cancer research and diagnostic development. We present experimental data and analytical frameworks to inform strategic decisions regarding technology adoption and optimization within the context of modern oncology research programs.
Technology Comparison: NGS, HD-PCR, and qPCR
The selection of molecular diagnostic platforms involves trade-offs between discovery power, throughput, speed, and cost. Below we systematically compare the technical and operational characteristics of three predominant technologies in cancer diagnostics.
Table 1: Comparative Analysis of Molecular Detection Technologies
| Parameter | Next-Generation Sequencing (NGS) | High-Definition PCR (HD-PCR) | Quantitative PCR (qPCR) |
|---|---|---|---|
| Discovery Power | High; detects known and novel variants [91] | Limited to predefined targets | Low; detects only known sequences [91] |
| Multiplexing Capacity | Very High (100s-1000s of targets) [91] | Moderate (9-gene panel shown) [92] | Low (typically ≤ 20 targets) [91] |
| Typical Turnaround Time | 10-28 days (send-out) [92] | ~5 days (in-house) [92] | < 2 days (in-house) |
| Mutation Resolution | Single-nucleotide variants to large rearrangements [91] | Specific mutations and fusions [92] | Specific predefined variants |
| Throughput | High for multiple genes/samples [91] | Moderate | Low for multiple targets [91] |
| Best Application | Comprehensive genomic profiling, novel biomarker discovery | Rapid, focused panels for validated biomarkers | Validation studies, low-target clinical screening [91] |
Key Differentiators and Technology Selection
The choice between these technologies depends heavily on research objectives and operational constraints. NGS offers superior discovery power for identifying novel variants and comprehensive genomic profiling, making it ideal for exploratory research and biomarker discovery [91]. HD-PCR bridges the gap between comprehensive NGS and rapid qPCR, providing faster turnaround times for focused gene panels while maintaining clinical-grade accuracy [92]. qPCR remains valuable for high-volume testing of a limited number of established biomarkers where speed and cost-efficiency are paramount [91].
Workflow Integration and Operational Considerations
Implementing molecular diagnostics requires careful planning of laboratory workflows, with significant implications for resource allocation and operational efficiency.
Turnaround Time: A Critical Operational Metric
Turnaround time (TAT) significantly impacts clinical decision-making and research pacing. A comparative study of non-small cell lung cancer (NSCLC) testing demonstrated that in-house HD-PCR achieved an average TAT of 5.01 days, compared to 10.4 days for send-out NGS testing [92]. This >50% reduction in TAT enables more rapid therapeutic decisions and accelerates research timelines when testing focused gene panels.
Workflow Complexity and Infrastructure Requirements
NGS workflows typically involve multiple sophisticated steps including library preparation, sequencing, and complex bioinformatic analysis, requiring specialized expertise and infrastructure [15]. In contrast, PCR-based methods (both HD-PCR and qPCR) utilize more familiar workflows with accessible equipment already available in most laboratories, reducing implementation barriers [92] [91].
Economic Analysis: Cost Structures and Value Assessment
Understanding the economic implications of molecular diagnostic technologies requires analysis of both direct costs and broader healthcare economic impact.
Direct Cost Components and Infrastructure Investment
Molecular diagnostic platforms exhibit distinct cost structures. NGS requires significant capital investment in sequencing instrumentation and computing infrastructure for data analysis and storage [93]. Additionally, the requirement for advanced machines and sophisticated data systems creates substantial operational expenses that can be prohibitive for smaller laboratories [93]. PCR-based systems generally involve lower initial capital outlay and can be implemented with more modest computational infrastructure, making them more accessible to resource-constrained settings [91].
Healthcare Economic Impact and Value-Based Assessment
Beyond direct testing costs, molecular diagnostics impact overall healthcare expenditures through their influence on treatment decisions and resource utilization.
Table 2: Economic Impact of Molecular Testing Strategies
| Economic Factor | NGS Impact | PCR-Based Impact | Evidence |
|---|---|---|---|
| Total Healthcare Costs | Potential long-term savings through improved targeting | Reduced near-term costs vs. no testing | Multiplex RT-PCR reduced 6-month costs by $1,073 vs. no test [94] |
| Outpatient Service Utilization | Not specifically reported | Significant reduction in outpatient visits | 5.8% relative reduction in outpatient utilization with multiplex RT-PCR [94] |
| Therapeutic Optimization | Enables targeted therapy selection | Facilitates appropriate treatment | 40% increase in precision therapy use with NGS [93] |
| Diagnostic Revisions | Reduced need for repeat testing | Minimized diagnostic revisions | 30% decline in repeat invasive biopsies with NGS [93] |
The economic advantage of advanced molecular testing emerges clearly when considering total healthcare costs rather than just test price. Rapid, accurate diagnostics reduce unnecessary procedures, optimize treatment selection, and decrease long-term complications [94]. One study demonstrated that implementing syndromic multiplex RT-PCR testing for vaginitis significantly reduced mean total healthcare costs ($5,607 vs. $6,680) over six months compared to no diagnostic testing [94].
Experimental Protocols and Validation Frameworks
Robust validation of molecular diagnostics requires rigorous experimental design and benchmarking against established standards.
Structural Variant Detection Benchmarking
Accurate detection of structurally variant (SVs) such as gene fusions is critical in cancer diagnostics. A comprehensive benchmarking framework evaluated multiple SV callers (Delly, SvABA, Manta, Lumpy) using 476 cancer patient samples [95]. The study established an expert-reviewed SV call set of 1,303 tumor-specific SVs and developed a random-forest-based decision model that achieved over 90% accuracy (92-99.78%) across data types [95].
Experimental Protocol: SV Detection Validation
- Sample Preparation: Formalin-Fixed Paraffin-Embedded (FFPE) tumor tissue and matched peripheral blood samples from 476 cancer patients [95]
- Sequencing Method: Targeted NGS using custom panel covering clinically relevant SVs from 27 genes sequenced on MGISEQ platform (100bp paired-end reads) [95]
- Bioinformatic Processing: SOAPnuke for quality control, BWA for alignment to hg19, multiple SV callers applied [95]
- Validation Method: IGV visualization and expert review of soft-clip/split reads, breakpoint features; validation by IHC/FISH experiments [95]
- Statistical Analysis: Random-forest model with ten-fold cross-validation; metrics included accuracy, precision, recall, and F1 score [95]
NSCLC Mutation Detection Concordance Study
A rigorous comparison evaluated the performance of HD-PCR versus NGS for detecting clinically actionable mutations in non-small cell lung cancer [92].
Experimental Protocol: Method Concordance Assessment
- Sample Cohort: 58 retrospective FFPE specimens diagnosed with NSCLC [92]
- Testing Methods: ChromaCode HD-PCR NSCLC assay (9-gene panel) versus send-out NGS [92]
- Analyzed Targets: EGFR, BRAF, KRAS (G12C only), MET mutations and RNA fusions in RET, ROS1, ALK, NTRK1/2/3 [92]
- Outcome Measures: Concordance rate between platforms, turnaround time analysis [92]
- Results: 100% concordance observed between NGS and HD-PCR assays with all 5 positive cases accurately detected by both platforms [92]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of molecular diagnostics requires careful selection of reagents and platforms tailored to specific research needs.
Table 3: Essential Research Reagents and Platforms for Molecular Diagnostics
| Reagent/Solution | Function | Application Context |
|---|---|---|
| Custom Targeted Panels | Focused sequencing of clinically relevant genes | Cost-effective SV detection in clinical specimens [95] |
| FFPE DNA Extraction Kits | DNA isolation from archival clinical samples | Enables analysis of retrospective cohorts [95] |
| Multiplex RT-PCR Assays | Simultaneous detection of multiple pathogens | Syndromic testing for infectious causes of symptoms [94] |
| Bisulfite Conversion Kits | DNA modification for methylation studies | Epigenetic profiling in cancer research [96] |
| Bioinformatic Pipelines | Data analysis and variant calling | Structural variant detection from NGS data [95] |
| Digital PCR Systems | Absolute quantification of rare variants | High-sensitivity mutation detection [92] |
Implementation Strategies and Future Directions
Successful integration of molecular diagnostics requires strategic planning that aligns technological capabilities with research objectives and operational constraints.
Hybrid Testing Approaches
Many institutions implement complementary testing strategies that leverage the strengths of multiple platforms. A common approach utilizes rapid, in-house PCR-based testing for high-volume, time-sensitive applications while reserving comprehensive NGS profiling for complex cases or discovery research [92]. This hybrid model optimizes both responsiveness and discovery power while managing operational costs.
Emerging Trends and Innovation Frontiers
The molecular diagnostics landscape continues to evolve with several emerging trends:
- AI-Enhanced Diagnostics: Artificial intelligence approaches are demonstrating improved cost-effectiveness in various clinical applications, largely by minimizing unnecessary procedures and optimizing resource use [97]
- Liquid Biopsy Applications: Non-invasive circulating tumor DNA analysis enables real-time monitoring of treatment response and earlier detection of resistance mechanisms [93]
- Process Optimization: Workflow management platforms streamline molecular diagnostic operations through automation, error reduction, and improved resource utilization [98]
Molecular diagnostic technologies offer complementary capabilities for cancer research and diagnostic development. NGS provides unparalleled discovery power for comprehensive genomic profiling, while PCR-based methods deliver rapid, cost-effective testing for established biomarkers. The optimal technology selection depends on specific research objectives, throughput requirements, and operational constraints. As the field evolves, hybrid approaches that leverage the strengths of multiple platforms will likely dominate strategic implementation plans. By carefully considering workflow integration requirements, economic factors, and validation frameworks, researchers can effectively balance throughput, turnaround time, and accessibility to advance cancer diagnostics and therapeutic development.
In the field of cancer diagnostics, molecular techniques have revolutionized our ability to detect genetic alterations driving malignancy, opening the door to precision medicine and improved patient outcomes [3]. However, the transformative potential of these technologies can only be realized through rigorous standardization and quality control measures that ensure reproducible and reliable results across different laboratory settings. This guide objectively compares the performance of key molecular techniques—various polymerase chain reaction (PCR) methods and next-generation sequencing (NGS)—with a specific focus on the experimental protocols and quality metrics that underpin dependable inter-laboratory results.
Comparative Analysis of Key Molecular Techniques
The selection of an appropriate molecular diagnostic technique involves careful consideration of performance characteristics relative to clinical or research needs. The table below provides a structured comparison of key technologies based on their sensitivity, typical applications, and important technical considerations for standardization.
Table 1: Performance Comparison of Key Molecular Techniques in Cancer Diagnostics
| Technique | Key Strengths | Sensitivity | Common Cancer Diagnostic Applications | Standardization Considerations |
|---|---|---|---|---|
| Real-Time Quantitative PCR (qPCR) | Rapid, cost-effective, quantitative results [3] | Mutant Allele Frequency (MAF) >10% [3] | Gene duplication/deletion detection, gene expression analysis [3] | Requires internal controls, reference gene normalization [3] |
| Droplet Digital PCR (ddPCR) | Absolute quantification without standards, high sensitivity [3] | MAF <0.1% [3] | Circulating tumor DNA (ctDNA) analysis in liquid biopsies, PIK3CA mutation detection [3] | Capable of detecting rare mutations with 93.3% sensitivity, 100% specificity in breast cancer [3] |
| Reverse Transcriptase PCR (RT-PCR) | High sensitivity for RNA targets, can detect few cells per million [3] | 10 cancer cells per 3mL peripheral blood (spike-in experiment) [3] | Detection of circulating tumor cells, tissue-specific gene expression (e.g., melanoma, neuroblastoma) [3] | Used for low-density array analysis from FFPE samples with preamplification [99] |
| Next Generation Sequencing (NGS) | Comprehensive profiling, identifies unknown alterations, high multiplexing capability [3] | Varies by platform and depth of coverage | Identification of key genetic alterations driving malignancy (point mutations to structural variations) [3] | Requires careful bioinformatic standardization, variant calling thresholds |
Detailed Experimental Protocols for Assay Validation
Protocol 1: RNA Preamplification and Low-Density Array Analysis from FFPE Samples
Formalin-fixed paraffin-embedded (FFPE) tissues represent a valuable but challenging source of tumor samples. The following reproducible protocol has been validated for gene expression analysis from these samples [99]:
- RNA Extraction: Extract RNA from FFPE tissue sections using specialized kits designed to recover fragmented RNA. Assess RNA quality and quantity using appropriate methods.
- Reverse Transcription: Convert RNA to complementary DNA (cDNA) using reverse transcriptase with both random hexamers and oligo-dT primers to ensure comprehensive coverage.
- cDNA Preamplification: Utilize a commercial preamplification kit (e.g., TaqMan PreAmp Master Mix Kit) to amplify cDNA targets. This step is critical for generating sufficient material from low-yield, fragmented FFPE RNA.
- Low-Density Array Setup: Dilute preamplified cDNA according to manufacturer specifications and load into low-density array cards containing primer-probe sets for target genes (e.g., 96-gene panels).
- qPCR Amplification and Data Analysis: Run quantitative PCR using standardized cycling conditions. Analyze data using ∆∆Cq method with normalization to appropriate reference genes.
This complete workflow has been demonstrated to be a "powerful and reproducible approach for routine clinical purposes that can be performed even using poorer RNA quality samples" [99].
Protocol 2: Circulating Tumor DNA Analysis via ddPCR
Analysis of circulating tumor DNA in liquid biopsies requires exceptional sensitivity. The following protocol outlines a standardized approach for ddPCR analysis [3]:
- Plasma Separation: Collect blood in specialized tubes containing stabilizers. Process within specified timeframes (typically within 6 hours) with double centrifugation to isolate platelet-poor plasma.
- Cell-Free DNA Extraction: Extract cell-free DNA from plasma using validated kits optimized for low-concentration, short-fragment DNA. Elute in low-EDTA TE buffer or manufacturer-recommended solution.
- Droplet Generation: Combine extracted DNA with ddPCR supermix, primers, and probes for target mutations. Generate droplets using a droplet generator, ensuring proper formation and stability.
- PCR Amplification: Transfer droplets to a 96-well plate and seal securely. Perform PCR amplification with optimized thermal cycling conditions specific to the assay.
- Droplet Reading and Analysis: Read plate in a droplet reader. Analyze data using manufacturer's software with appropriate threshold settings. Report mutant allele frequency as copies/μL or fractional abundance.
This protocol has demonstrated high performance in clinical validation studies, achieving 93.3% sensitivity and 100% specificity for detecting PIK3CA mutations in breast cancer patients [3].
Visualization of Standardized Workflows
The following diagrams illustrate standardized workflows for the key experimental protocols described, highlighting critical quality control checkpoints.
Figure 1: Standardized FFPE RNA Analysis Workflow
Figure 2: Standardized ctDNA ddPCR Analysis Workflow
Essential Research Reagent Solutions
Successful implementation of standardized molecular techniques requires specific, high-quality reagents. The following table details essential materials and their functions in ensuring reproducible results.
Table 2: Essential Research Reagents for Molecular Cancer Diagnostics
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Specialized FFPE RNA Extraction Kits | Optimized recovery of fragmented RNA from archived tissue samples [99] | Critical for overcoming formalin-induced crosslinking and fragmentation in FFPE specimens |
| cDNA Preamplification Kits | Amplification of limited cDNA without distorting relative mRNA levels [99] | Enables multi-gene analysis from low-yield samples; essential for low-density arrays |
| Stabilized Blood Collection Tubes | Preservation of cell-free DNA profile by preventing white blood cell lysis [3] | Maintains original ctDNA concentration; critical for accurate liquid biopsy results |
| Droplet Digital PCR Supermix | Partitioning of nucleic acids into thousands of individual PCR reactions [3] | Enables absolute quantification and rare allele detection below 0.1% MAF |
| Multiplex PCR Assay Kits | Simultaneous amplification of multiple targets in single reaction [3] | Increases efficiency and conserves precious patient samples; reduces reagent costs |
| Reference Standard Materials | Calibration and quality control across laboratories and platforms | Enables method validation and inter-laboratory comparison of results |
The comparison of molecular techniques for cancer diagnostics reveals a critical balance between analytical sensitivity and standardization requirements. While NGS offers comprehensive genomic profiling and ddPCR provides exceptional sensitivity for liquid biopsy applications, all methods demand rigorous quality control measures to ensure reproducibility across laboratories. Standardized protocols for specimen processing, nucleic acid handling, and data analysis, coupled with appropriate quality control reagents, form the foundation of reliable molecular diagnostics. As these technologies continue to evolve and integrate into precision oncology, maintaining focus on standardization and quality control will be essential for delivering consistent, actionable results that ultimately improve patient outcomes.
Critical Performance Assessment: A Comparative Framework for Validating Molecular Diagnostic Techniques
The evolution of molecular diagnostics has fundamentally transformed the landscape of cancer detection and management, moving the field toward less invasive and more precise methodologies. Liquid biopsy, which involves the analysis of tumor-derived materials such as circulating tumor DNA (ctDNA) in blood and other biofluids, now serves as a critical tool for cancer diagnosis, prognosis, and monitoring of treatment response [28] [27]. The clinical utility of these tests hinges on their performance characteristics, which are determined by the underlying technology platform.
This guide provides a objective, data-driven comparison of the primary molecular techniques employed in liquid biopsy for cancer diagnostics: digital PCR (dPCR), next-generation sequencing (NGS), and emerging multimodal assays incorporating artificial intelligence (AI). We focus on the core performance metrics of analytical sensitivity, specificity, limit of detection (LOD), and turnaround time, which are paramount for researchers and drug development professionals selecting appropriate methodologies for their experimental and clinical goals.
The fundamental principle underlying liquid biopsy in oncology is the detection and analysis of circulating tumor DNA (ctDNA). ctDNA consists of short, fragmented DNA molecules released into the bloodstream by apoptotic or necrotic tumor cells. In cancer patients, ctDNA typically constitutes a small fraction (0.1% to 1.0%) of the total cell-free DNA (cfDNA) present in plasma, presenting a significant technical challenge for detection, particularly in early-stage disease or low-shedding tumors [28] [27]. The following diagram illustrates the general workflow from sample collection to data analysis.
Core Molecular Techniques
Digital PCR (dPCR)
Digital PCR represents the third generation of PCR technology, enabling absolute quantification of nucleic acids without the need for a standard curve. The core innovation of dPCR is the partitioning of a PCR reaction into thousands to millions of individual reactions, so that each partition contains either zero, one, or a few target molecules. Following end-point amplification, the fraction of positive partitions is counted, and the absolute concentration of the target is calculated using Poisson statistics [5]. This partitioning allows for the detection of rare mutations within a high background of wild-type DNA, making it exceptionally suitable for liquid biopsy applications [5]. Key commercial dPCR platforms include Bio-Rad's ddPCR, Thermo Fisher's QuantStudio, and Qiagen's QIAcuity systems [5].
Next-Generation Sequencing (NGS)
Next-generation sequencing encompasses a suite of high-throughput technologies that allow for the parallel sequencing of millions of DNA fragments. In contrast to dPCR's targeted approach, NGS can interrogate large genomic regions, the whole exome, or even the entire genome, providing a comprehensive view of the cancer genome. Common NGS approaches for liquid biopsy include tagged-amplicon deep sequencing (TAm-Seq), CAncer Personalized Profiling by deep Sequencing (CAPP-Seq), and targeted error correction sequencing (TEC-Seq) [28]. While NGS offers broad coverage, its sensitivity is highly dependent on sequencing depth, and the method can be susceptible to sequencing artifacts that must be computationally corrected [28].
Emerging Multimodal and AI-Enhanced Platforms
The field is rapidly advancing toward integrated platforms that combine multiple analytical dimensions. These include the analysis of genomic alterations, epigenomic features such as DNA methylation, and fragmentomics—the study of cfDNA fragmentation patterns [28]. Machine learning and deep learning models are increasingly applied to these complex, multi-modal datasets to improve classification accuracy. For example, the DELFI (DNA evaluation of fragments for early interception) method uses a machine learning model on genome-wide fragmentation profiles to detect cancer with a reported sensitivity of 91% [28]. AI-facilitated tools are also being deployed in imaging-based diagnostics, such as digital pathology and radiology, to enhance early cancer detection [56] [100].
Comparative Performance Metrics
The selection of a molecular technique is a trade-off between analytical performance, breadth of information, and practical considerations. The table below provides a direct comparison of the key performance metrics for dPCR, NGS, and AI-enhanced multimodal platforms.
Table 1: Head-to-Head Comparison of Key Metrics for Molecular Techniques in Cancer Diagnostics
| Metric | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) | AI-Enhanced Multimodal Platforms |
|---|---|---|---|
| Analytical Sensitivity | High (can detect mutant allele frequencies of ~0.1% or lower) [5] [28] | Moderate to High (Varies with sequencing depth; can reach 0.1%-1% with error-correction) [28] | Very High (Sensitivity of 91% reported for DELFI in cancer detection) [28] |
| Specificity | Very High (>99.7% reported for specific mutations) [101] | High (Specificity can be >99.5% with unique molecular identifiers) [28] [101] | High (e.g., SPOT-MAS specificity of 99.7% in pre-symptomatic cohorts) [101] |
| Limit of Detection (LOD) | Very low (Single molecule detection in a background of wild-type DNA) [5] | Low (Dependent on input DNA and read depth; requires higher input than dPCR) [28] | Not explicitly stated; inferred from high clinical sensitivity/specificity [28] [101] |
| Turnaround Time | Fast (~ 3 days from sample to result in community settings) [101] | Slower (Days to weeks due to complex library prep and bioinformatics) [28] | Variable (Highly dependent on data integration and computational analysis) [56] |
| Key Strength | Superior sensitivity/specificity for known, low-frequency variants; absolute quantification. | Unbiased discovery, broad genomic coverage, detection of novel variants. | Integration of multiple data types (genomic, fragmentomic, epigenetic) for enhanced performance. |
| Primary Limitation | Limited multiplexing; only detects pre-defined targets. | Higher cost, complex data analysis, longer turnaround time. | "Black box" nature of some AI models, data privacy concerns, requires massive datasets. |
Key Metrics Deep Dive
- Analytical Sensitivity and LOD: dPCR's unparalleled sensitivity for known targets stems from its partitioning step, which effectively enriches the target and reduces the background against which it must be detected, enabling a LOD at the single-molecule level [5]. While NGS can achieve similar sensitivity for known mutations with ultra-deep sequencing and error-correction methods, this comes at a significant cost. AI-enhanced platforms boost sensitivity by combining weak signals from multiple independent analytes (e.g., mutations, methylation, and fragmentation patterns) [28].
- Specificity: Specificity is a key strength of both dPCR and NGS. dPCR achieves high specificity through the use of fluorescently labeled, target-specific probes [5]. NGS ensures specificity via unique molecular identifiers (UMIs) that tag original DNA molecules to distinguish true variants from PCR and sequencing errors [28]. The high specificity of multimodal tests like SPOT-MAS demonstrates the power of complex feature analysis in minimizing false positives [101].
- Turnaround Time: dPCR offers a significant advantage in speed, with workflows that can be completed within a single day, making it suitable for rapid clinical decision-making [101]. NGS involves a multi-step process including library preparation, sequencing, and complex bioinformatic analysis, resulting in a turnaround time of several days to weeks [28]. The timeline for AI platforms is heavily influenced by the computational workload of integrating and processing diverse data streams [56].
Experimental Protocols and Reagent Solutions
To ensure the reproducibility of the high-performance metrics discussed, standardized experimental protocols and high-quality research reagents are essential. The following section outlines the detailed methodology for a core technique and lists critical reagent solutions.
Detailed Experimental Protocol: Droplet Digital PCR (ddPCR) for ctDNA Mutation Detection
This protocol is adapted from established dPCR methodologies for detecting a known somatic mutation (e.g., a KRAS G12D mutation) in plasma-derived ctDNA [5].
- Sample Collection and Plasma Separation: Collect whole blood into EDTA or specialized cell-stabilizing tubes (e.g., Streck). Process within 2-6 hours to prevent lysis of white blood cells. Centrifuge to separate plasma, followed by a second, high-speed centrifugation to remove residual cells.
- cfDNA Extraction: Extract cfDNA from plasma using a silica-membrane or magnetic bead-based kit optimized for low-concentration, short-fragment DNA. Elute in a low-EDTA buffer or nuclease-free water. Quantify using a fluorescence-based assay (e.g., Qubit).
- Reaction Mix Preparation: Prepare the ddPCR reaction mix containing:
- DNA template (typically 1-10 ng of cfDNA).
- Forward and reverse primers specific to the genomic region of interest.
- Two fluorescent probes: one labeled with FAM to detect the mutant allele and one labeled with HEX/VIC to detect the wild-type allele.
- ddPCR Supermix.
- Droplet Generation: Load the reaction mix and droplet generation oil into a droplet generator. This instrument partitions the 20 µL reaction into approximately 20,000 nanoliter-sized water-in-oil droplets.
- PCR Amplification: Transfer the emulsified sample to a 96-well PCR plate. Perform thermal cycling on a standard thermal cycler with the following profile:
- Enzyme activation: 95°C for 10 minutes.
- 40 cycles of: Denaturation (94°C for 30 seconds), Annealing/Extension (55-60°C for 60 seconds).
- Enzyme deactivation: 98°C for 10 minutes.
- Hold at 4°C.
- Droplet Reading: Place the plate in a droplet reader. This instrument flows droplets single-file past a two-color optical detection system that classifies each droplet as FAM-positive (mutant), HEX-positive (wild-type), positive for both, or negative.
- Data Analysis: Use the instrument's software to apply a fluorescence amplitude threshold and count the positive and negative droplets for each channel. The software automatically calculates the absolute concentration of mutant and wild-type DNA (in copies/µL) and the mutant allele frequency using Poisson statistics.
Essential Research Reagent Solutions
Table 2: Key Research Reagent Solutions for Liquid Biopsy Workflows
| Reagent / Solution | Function | Key Considerations |
|---|---|---|
| Cell-Free DNA Blood Collection Tubes | Stabilizes nucleated blood cells to prevent genomic DNA contamination during sample transport and storage. | Critical for preserving the integrity of the ctDNA profile. Tubes from Streck or CellSave are commonly used [27]. |
| cfDNA Extraction Kits | Isolation and purification of short-fragment cfDNA from plasma or other biofluids. | Kits should be optimized for low-input, low-concentration samples (e.g., Qiagen QIAamp Circulating Nucleic Acid Kit, Roche cobas cfDNA Sample Preparation Kit) [102]. |
| dPCR Supermix with Probe Chemistry | A master mix containing DNA polymerase, dNTPs, and optimized buffers for robust amplification within droplets or microchambers. | Must be formulated for droplet stability during thermal cycling. Probes (e.g., TaqMan) must be highly specific to minimize false positives [5]. |
| NGS Library Preparation Kits | Prepares cfDNA for sequencing by end-repairing, adding adapters, and amplifying the final library. | Kits designed for degraded, low-input DNA are essential. Includes reagents for attaching unique molecular identifiers (UMIs) to correct for amplification errors [28]. |
| Bisulfite Conversion Reagents | Chemically converts unmethylated cytosines to uracils, allowing for the discrimination of methylated DNA. | Key for DNA methylation-based assays. Can cause significant DNA degradation; bisulfite-free alternatives (e.g., EM-seq) are emerging [28] [102]. |
Technology Selection Workflow
Choosing the optimal molecular technique depends on the specific research question and practical constraints. The decision-making workflow below outlines the key considerations for researchers.
The molecular toolkit for cancer diagnostics is rich and varied, with each technology offering a distinct profile of advantages. Digital PCR stands out for applications requiring the utmost sensitivity and specificity for a known, predefined marker, such as monitoring minimal residual disease or tracking a specific resistance mutation. Next-generation sequencing is the undisputed choice for discovery and comprehensive genomic profiling, offering a broad view of the tumor genome at the cost of greater complexity and longer turnaround times. AI-enhanced multimodal platforms represent the cutting edge, leveraging the power of complex data integration to push the boundaries of early cancer detection and classification.
The optimal choice is not a question of which technology is universally "best," but which is the most fit-for-purpose for a given research or clinical objective. As these technologies continue to mature and converge, the future of cancer diagnostics lies in their intelligent and context-specific application, guided by a clear understanding of their fundamental performance characteristics as detailed in this comparison.
The advent of molecular diagnostics has revolutionized cancer research, offering unprecedented capabilities for detecting genetic variants that drive oncogenesis and therapy response. Among the most pivotal technologies in this domain are PCR-based methods, including the increasingly sophisticated digital PCR (dPCR), and next-generation sequencing (NGS). These techniques form the backbone of modern variant detection, yet they possess distinct operational principles, strengths, and limitations. The selection between PCR/dPCR and NGS is not a matter of identifying a superior technology, but rather of matching the tool to the specific research question based on key parameters such as the number of targets, required sensitivity, throughput, and available resources. This guide provides an objective comparison for researchers and drug development professionals, framing the discussion within the broader context of molecular techniques in cancer diagnostics. The decision matrix hinges primarily on the known or unknown nature of the target and the requisite detection sensitivity, positioning dPCR as the champion for ultrasensitive, targeted detection of known variants, while NGS offers a comprehensive, hypothesis-free approach for discovering novel alterations across the genome.
Core Principles and Technical Comparison
Fundamental Mechanisms of dPCR and NGS
Digital PCR (dPCR) operates on a simple yet powerful principle of limiting dilution and endpoint PCR. The sample is partitioned into thousands of individual reactions, resulting in partitions containing zero, one, or more target molecules. Following PCR amplification, each partition is analyzed for fluorescence. Partitions containing the target sequence fluoresce, while those without it remain dark. Using Poisson statistics, the absolute quantity of the target molecule in the original sample can be precisely calculated without the need for a standard curve [103]. This partitioning is the source of its exceptional sensitivity, as it effectively enriches rare alleles by separating them from the wild-type background.
Next-Generation Sequencing (NGS), in contrast, is a massively parallel sequencing technology. It requires a library preparation step where DNA samples are fragmented, and adapters are attached to both ends. The NGS platform then simultaneously sequences millions of these fragments in parallel, producing vast amounts of raw sequencing data. This data undergoes primary, secondary, and tertiary bioinformatics analyses to align sequences to a reference genome and identify variants [103]. The core strength of NGS lies in its untargeted nature and immense scalability, allowing for the detection of known and unknown mutations across many genes and samples simultaneously.
Comparative Strengths and Limitations
The table below summarizes the key characteristics of dPCR and NGS, providing a high-level overview for researchers.
Table 1: Core Characteristics of dPCR and NGS
| Feature | Digital PCR (dPCR) | Next-Generation Sequencing (NGS) |
|---|---|---|
| Detection Principle | Partitioning & endpoint fluorescence | Massively parallel sequencing |
| Target Requirement | Requires prior knowledge of target sequence | No prior sequence knowledge needed |
| Multiplexing Capacity | Limited (typically 4-6 plex, though emerging methods allow higher [104]) | Very high (hundreds to thousands of targets) |
| Sensitivity | Very high (can detect variants at <0.1% allele frequency [103] [105]) | Moderate to high (typically 1-2% allele frequency for common panels [103]) |
| Quantification | Absolute, without standards [103] | Relative, requires complex bioinformatics |
| Throughput | Low to medium (focus on sample number, not target number) | Very high (for both samples and targets) |
| Turnaround Time | Fast (hours from sample to result) | Longer (days due to library prep and analysis) |
| Cost per Sample | Low for few targets | Higher, but cost-effective for many targets |
| Data Complexity | Low; simple, interpretable data | High; requires specialized bioinformatics expertise |
| Ideal Application | Ultrasensitive detection/quantification of known variants | Comprehensive discovery of known/unknown variants |
Experimental Data and Performance Benchmarks
Direct Comparison in Cancer Detection
Recent comparative studies highlight the performance disparities between dPCR and NGS in real-world clinical research scenarios. A 2025 study on non-metastatic rectal cancer directly compared droplet digital PCR (ddPCR) and an NGS panel for detecting circulating tumor DNA (ctDNA) in patient plasma. In the development cohort, ddPCR demonstrated significantly higher detection rates, identifying ctDNA in 24 of 41 (58.5%) baseline plasma samples, whereas the NGS panel detected ctDNA in only 15 of 41 (36.6%) samples (p = 0.00075) [106] [107]. This underscores dPCR's superior analytical sensitivity for detecting low-abundance variants in a background of wild-type DNA, a common challenge in liquid biopsy applications.
Furthermore, the same study found that a positive ctDNA result, as detected by these methods, was associated with higher clinical tumor stage and lymph node positivity on MRI, affirming the biological and clinical relevance of the findings [106].
Performance in Assay Validation and Manufacturing
Beyond discovery and diagnostics, the robustness of quantitative data is critical in therapeutic development. A comparative study of qPCR and dPCR for CAR-T cell manufacturing validations revealed distinct performance differences. While qPCR showed a wider dynamic range (8 logs vs. 6 logs for dPCR) using synthetic gBlocks, dPCR proved superior in precision when analyzing actual biological samples. The complex absolute quantification in qPCR, which relies on serial dilution of standards, showed higher data variation (up to 20% difference in copy number ratio) and a lower correlation between genes linked in one construct (R² = 0.78 for qPCR vs. R² = 0.99 for dPCR) [108]. This makes dPCR a more reliable and less variable method for critical quality control assays in advanced therapy manufacturing.
Methodologies and Workflows
Detailed Experimental Protocol: dPCR for ctDNA Analysis
The high sensitivity of dPCR makes it ideal for detecting circulating tumor DNA (ctDNA). The following workflow outlines a typical protocol based on studies comparing dPCR and NGS [106] [107].
- Sample Collection and Processing: Collect patient blood in cell-stabilizing tubes (e.g., Streck). Process with a two-step centrifugation protocol: first at 1,600 × g for 10 minutes to isolate plasma, followed by 16,000 × g for 10 minutes to remove residual cellular debris. Aliquot and store plasma at -80°C until use [109].
- Cell-free DNA (cfDNA) Extraction: Extract cfDNA from plasma using a commercially available kit optimized for short-fragment DNA (e.g., QIAamp Circulating Nucleic Acid Kit). Elute the DNA in a low-EDTA buffer or nuclease-free water.
- Assay Design: Design hydrolysis (TaqMan) probes and primers specific to the mutation of interest, which was previously identified via NGS analysis of the primary tumor tissue.
- dPCR Reaction Setup: Prepare the dPCR reaction mix containing DNA template, forward and reverse primers, fluorescent probes for both mutant and wild-type alleles, and dPCR supermix. The total reaction volume varies by instrument.
- Partitioning and Amplification: Load the reaction mix into a dPCR instrument (e.g., Bio-Rad QX600 Droplet Digital PCR system, Qiagen QIAcuity). The instrument automatically partitions the sample into thousands of nanoscale reactions (droplets or nanowells). Perform PCR amplification with a standard thermal cycling protocol.
- Data Acquisition and Analysis: After amplification, the instrument reads the fluorescence in each partition. Partitions are classified as mutant-positive, wild-type-positive, double-positive, or negative. The software uses Poisson statistics to calculate the absolute concentration (copies/μL) and mutant allelic frequency of the target in the original sample.
Workflow for dPCR Variant Detection
Detailed Experimental Protocol: Targeted NGS for Tumor Mutational Profiling
NGS is employed for comprehensive genotyping. The following protocol is common for targeted panel sequencing from tumor samples or cfDNA.
- Sample Preparation: Extract high-quality genomic DNA from formalin-fixed paraffin-embedded (FFPE) tumor tissue or cfDNA from plasma as described in step 4.1. Quantify DNA using a fluorometric method (e.g., Qubit).
- Library Preparation: Fragment genomic DNA (if not using cfDNA) and perform end-repair and A-tailing. Ligate sequencing adapters containing unique dual indices (UDIs) to each sample to enable multiplexing. For targeted sequencing, hybridize the adapter-ligated library with biotinylated probes complementary to the regions of interest (e.g., a cancer hotspot panel).
- Target Enrichment: Capture the probe-bound targets using streptavidin-coated magnetic beads. Wash away non-hybridized fragments and amplify the captured library with a limited-cycle PCR.
- Library Quantification and Pooling: Precisely quantify the final libraries. dPCR is recognized as a highly accurate method for this purpose, ensuring optimal loading onto the sequencer and efficient use of sequencing capacity [103]. Normalize and pool libraries based on quantification data.
- Sequencing: Denature the pooled library and load it onto an NGS sequencer (e.g., Illumina MiSeq, NextSeq) for cluster generation and sequencing-by-synthesis, typically generating paired-end reads.
- Bioinformatic Analysis:
- Primary Analysis: Convert raw image data into nucleotide sequences (BCL to FASTQ).
- Secondary Analysis: Demultiplex samples based on indices. Align sequences to the human reference genome (e.g., hg38). Mark duplicate reads. Call variants (SNVs, indels) using specialized algorithms.
- Tertiary Analysis: Annotate variants, filter artifacts, and interpret pathological significance.
Workflow for Targeted NGS Sequencing
The Scientist's Toolkit: Key Reagent Solutions
Successful implementation of dPCR and NGS workflows relies on a suite of specialized reagents and tools. The following table details essential materials for the featured experiments.
Table 2: Key Research Reagent Solutions for Variant Detection
| Item | Function | Example Application |
|---|---|---|
| Cell-stabilizing Blood Collection Tubes | Prevents leukocyte lysis and preserves the integrity of cell-free DNA in blood samples during transport and storage. | Liquid biopsy; ctDNA analysis for both dPCR and NGS [109]. |
| cfDNA Extraction Kits | Optimized for isolation of short, fragmented DNA from plasma or other liquid biopsy sources. | Isolation of ctDNA template for dPCR or NGS library prep [106]. |
| dPCR Supermix | A PCR master mix formulated for optimal performance in partitioned reactions, often with enhanced resistance to inhibitors. | Ultrasensitive detection of known SNVs in ctDNA [105]. |
| TaqMan Assays | Sequence-specific fluorescent probes and primers for the absolute quantification of known mutant and wild-type alleles. | Target-specific detection in dPCR [106]. |
| NGS Library Prep Kits | Reagents for fragmenting DNA (if needed), end-repair, A-tailing, adapter ligation, and library amplification. | Preparing samples for sequencing on platforms like Illumina [103]. |
| Targeted Panels (Biotinylated Probes) | Probes designed to capture and enrich specific genomic regions (e.g., cancer genes) from a sequencing library. | Focused sequencing of clinically relevant genes [106]. |
| Universal Probe Systems (e.g., USE-PCR) | A novel approach using universal hydrolysis probes and color-coded primer tags to enable higher-order multiplexing on dPCR platforms. | Detecting up to 32 single nucleotide variants simultaneously in a single dPCR reaction [104]. |
Synergistic Applications and Future Directions
The most powerful research strategies often leverage the complementary strengths of both dPCR and NGS. A common paradigm in cancer research involves using NGS for discovery and dPCR for validation and longitudinal monitoring. For instance, in liquid biopsy analysis, NGS can provide a comprehensive profile of ctDNA, identifying cancer-related somatic mutations and fusion genes across a wide panel of genes. Once these specific biomarker candidates are identified, dPCR becomes the ideal tool for validating these findings and subsequently monitoring disease burden or tracking the emergence of resistance mutations during therapy over time [103]. This is due to dPCR's cost-effectiveness, rapid turnaround, and superior sensitivity for tracking small changes in a few known markers.
Future developments are focused on overcoming the inherent limitations of each technology. For dPCR, the primary challenge is limited multiplexing. Innovations like Universal Signal Encoding PCR (USE-PCR) are emerging to address this. USE-PCR combines universal hydrolysis probes with amplitude modulation and multispectral encoding, enabling the detection of up to 32 different targets in a single reaction with high accuracy (up to 97.6%), as demonstrated on multiple dPCR platforms [104]. For NGS, efforts continue to reduce costs, simplify workflows, and improve bioinformatics for better sensitivity and specificity, particularly for low-frequency variants. The ongoing integration of artificial intelligence in data analysis promises to further enhance the capabilities of both technologies, solidifying their roles as indispensable, complementary tools in cancer research and personalized medicine.
The paradigm of cancer diagnostics has been fundamentally reshaped by the advent of precision medicine, with molecular profiling becoming indispensable for treatment selection, response assessment, and resistance monitoring. Traditionally, tissue biopsy has served as the cornerstone of tumor diagnosis, providing a direct window into tumor morphology and genetics. However, the limitations of this invasive approach have catalyzed the emergence of liquid biopsy, a minimally invasive alternative that analyzes tumor-derived components from bodily fluids [110] [27]. This comparative analysis examines these two diagnostic modalities through the critical lenses of invasiveness, representativeness, and clinical utility, providing a framework for their integrated application in oncology research and drug development.
Fundamental Technical Comparison
Procedure and Sample Type
- Tissue Biopsy: Involves the physical removal of a tissue sample from a tumor site via surgical excision, core needle biopsy, or fine-needle aspiration. This procedure provides a direct physical specimen for pathological examination [27].
- Liquid Biopsy: Requires only a simple blood draw or collection of other bodily fluids such as urine or cerebrospinal fluid. It isolates and analyzes circulating tumor biomarkers, including circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and extracellular vesicles (EVs) [110] [27].
Key Biomarkers and Analytical Targets
- Tissue Biopsy: Enables comprehensive histological assessment including tumor type, grade, and stage, alongside molecular analysis of DNA, RNA, and protein biomarkers from a specific tumor region [27].
- Liquid Biopsy: Focuses on detecting and characterizing tumor-derived components shed into circulation:
- ctDNA: Short DNA fragments (approximately 20-50 base pairs) released by tumor cells through apoptosis or necrosis, typically representing 0.1-1.0% of total cell-free DNA [27] [111].
- CTCs: Intact tumor cells disseminated from primary and metastatic sites, found in extremely low abundance (approximately 1 CTC per 1 million leukocytes) with a short half-life of 1-2.5 hours in circulation [27].
- Tumor-Educated Platelets (TEPs): Platelets that have been altered by interactions with tumors, carrying tumor-derived biomolecules [110].
- Extracellular Vesicles (EVs): Membrane-bound particles carrying proteins, nucleic acids, and lipids from tumor cells [110].
Table 1: Comparative Analysis of Technical Characteristics
| Characteristic | Tissue Biopsy | Liquid Biopsy |
|---|---|---|
| Invasiveness | High (surgical procedure) | Minimal (blood draw) [27] |
| Sample Type | Tumor tissue | Blood, urine, CSF [110] |
| Primary Analytes | Tumor tissue (DNA, RNA, proteins) | ctDNA, CTCs, EVs [110] [27] |
| Tumor Fraction | High (near 100%) | Low (ctDNA: 0.1-1% of cfDNA) [27] |
| Turnaround Time | Days to weeks | Potentially hours to days [110] |
| Spatial Coverage | Single site/specific region | Represents multiple tumor sites [110] [111] |
Comparative Analysis of Key Parameters
Invasiveness and Safety Profile
The procedural risk profile differs substantially between these approaches. Tissue biopsies carry inherent risks including bleeding, infection, pain, and organ-specific complications such as pneumothorax in lung biopsies [111]. These procedures may require hospital visitation, specialized interventional radiology, and carry a small but significant risk of serious complications.
In contrast, liquid biopsies pose risks comparable to a standard blood draw—primarily minor discomfort and minimal bruising—making them substantially safer [27]. This safety profile enables repeated sampling for longitudinal monitoring without cumulative risk to patients.
Tumor Representativeness and Heterogeneity Capture
A critical distinction lies in how these modalities capture tumor biology:
- Tissue Biopsy: Provides a snapshot from a single anatomical location and timepoint, potentially missing spatial heterogeneity within primary tumors or between metastatic sites [112]. This limitation becomes particularly significant in cancers with high spatial heterogeneity.
- Liquid Biopsy: Offers a composite molecular profile representing multiple tumor deposits and subclones, potentially providing a more comprehensive view of clonal evolution and heterogeneity [111]. However, its representativeness depends on adequate shedding of tumor components into circulation, which varies by tumor type, burden, and location [111].
Temporal Dynamics and Monitoring Capabilities
The capacity for longitudinal assessment represents another key differentiator:
- Tissue Biopsy: Serial sampling is impractical due to invasiveness and cumulative risk, limiting temporal resolution for monitoring tumor evolution [110].
- Liquid Biopsy: Enables frequent serial monitoring of tumor dynamics, treatment response, and emergence of resistance mechanisms in near real-time [110] [113]. The short half-life of ctDNA (hours) facilitates rapid assessment of molecular changes [111].
Table 2: Clinical Applications and Limitations
| Parameter | Tissue Biopsy | Liquid Biopsy |
|---|---|---|
| Initial Diagnosis | Gold standard (provides histology) | Not sufficient for initial diagnosis [111] |
| Therapy Selection | Comprehensive genomic profiling | Targeted mutation detection [113] |
| Treatment Monitoring | Limited by invasiveness | Excellent for serial monitoring [110] [113] |
| MRD Detection | Insensitive | Emerging application [113] [114] |
| Early Detection | Not applicable | Potential for screening [114] |
| Tumor Heterogeneity | Limited to sampled site | Captures spatial heterogeneity [111] |
| False Negatives | Sampling error | Low tumor DNA shedding [111] |
Experimental Evidence and Clinical Validation
The ROME Trial: Integrated Diagnostic Approach
The phase II ROME trial provides compelling evidence supporting the complementary value of both modalities. This study enrolled 1,794 patients with advanced solid tumors and performed both tissue (FoundationOne CDx) and liquid (FoundationOne Liquid CDx) biopsies, with results reviewed by a molecular tumor board [112] [115].
Experimental Protocol
- Patient Population: Adults with advanced or metastatic solid tumors on second or third-line treatment
- Sample Collection: Paired tissue and blood samples collected from all participants
- Sequencing Methods: Centralized next-generation sequencing using FDA-approved platforms
- Analysis Method: Actionable alterations identified by molecular tumor board, with concordance defined as detection of the same significant alterations in both biopsy types [115]
Key Findings on Concordance and Outcomes
The trial revealed a concordance rate of only 49% between tissue and liquid biopsies for detecting actionable alterations, with 35% of alterations detected exclusively in tissue and 16% exclusively in liquid biopsies [115]. This discordance was attributed to:
- Differences in detection of molecular alterations (43.3%)
- Discordant high tumor mutational burden (35%)
- Microsatellite instability discrepancies (1%)
- Test failures (21%) [115]
Critically, patients with concordant findings receiving tailored therapy showed significantly improved outcomes:
- Median overall survival: 11.05 months vs. 7.7 months in standard-of-care (26% reduction in death risk)
- Median progression-free survival: 4.93 months vs. 2.8 months (45% reduction in progression risk) [112]
These findings demonstrate that integrated profiling enhances patient selection for targeted therapies, with concordant results potentially identifying patients most likely to benefit.
Technical Methodologies in Liquid Biopsy
ctDNA Detection Platforms
Multiple technological approaches have been developed for liquid biopsy analysis:
- PCR-Based Methods: Including droplet digital PCR (ddPCR), offering fast turnaround, lower cost, and high sensitivity for detecting specific mutations but limited multiplexing capability [111].
- Next-Generation Sequencing (NGS): Enabling broad genomic profiling, detection of novel variants, and assessment of complex biomarkers like tumor mutational burden and microsatellite instability [113] [111]. Targeted NGS panels achieve limits of detection down to 0.1% variant allele frequency [111].
Emerging Ultrasensitive Technologies
Novel approaches are pushing detection sensitivity boundaries:
- MUTE-Seq: An ultrasensitive method employing engineered FnCas9 to selectively eliminate wild-type DNA, enabling highly sensitive detection of low-frequency mutations for minimal residual disease monitoring [114].
- Fragmentomics Analysis: Leveraging patterns in cfDNA fragmentation to identify cancer signals with high accuracy, potentially enabling early detection [114].
Diagnostic Workflows and Analytical Pathways
The analytical processes for tissue and liquid biopsies differ significantly in their initial steps but converge toward similar molecular endpoints. The following diagram illustrates the core pathways for each approach, highlighting key decision points and analytical stages.
Biomarker Analysis Pathways in Liquid Biopsy
Liquid biopsy encompasses multiple analyte types, each requiring specialized isolation and analysis techniques. The following diagram outlines the primary biomarkers and their associated analytical pathways, from sample collection to clinical application.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms for Liquid Biopsy
| Reagent/Platform | Primary Function | Application Context |
|---|---|---|
| Streck Cell-Free DNA Blood Collection Tubes | Preserves blood cell integrity and prevents genomic DNA contamination during transport | Blood collection and stabilization [111] |
| EpCAM Antibodies | Immunomagnetic capture of circulating tumor cells | CTC isolation and enrichment [27] |
| FoundationOne Liquid CDx | Comprehensive genomic profiling of ctDNA using NGS | Identification of actionable alterations [112] [115] |
| Guardant360 CDx | Digital sequencing of ctDNA for mutation detection | Therapy selection and monitoring [111] |
| FnCas9 Enzymes (MUTE-Seq) | Ultrasensitive mutation detection through wild-type DNA depletion | MRD monitoring and low-frequency variant detection [114] |
| BEAMing Technology | Digital PCR-based detection of specific mutations | Quantitative mutation analysis [27] [113] |
| Ultracentrifugation Systems | Isolation of extracellular vesicles based on density | EV purification for downstream analysis [110] |
Tissue and liquid biopsies represent complementary rather than competing modalities in cancer diagnostics. Tissue biopsy remains indispensable for initial diagnosis, histological classification, and comprehensive genomic profiling. Meanwhile, liquid biopsy offers a minimally invasive approach for serial monitoring, assessment of heterogeneity, and detection of resistance mechanisms. The emerging paradigm, supported by clinical evidence from trials such as ROME, favors integrated diagnostic approaches that leverage the strengths of both modalities. For research and drug development, this synergy enables more precise patient stratification, dynamic response assessment, and accelerated therapeutic development. Future directions will focus on standardizing analytical methodologies, validating clinical utility across diverse cancer types, and incorporating multi-analyte approaches to fully realize the potential of both tissue and liquid biopsies in precision oncology.
The integration of artificial intelligence (AI) and machine learning (ML) is fundamentally transforming the landscape of cancer diagnostics, enabling unprecedented precision in both image analysis and biomarker discovery. These technologies are addressing critical limitations of traditional methods by detecting subtle patterns in complex datasets that escape human perception [56]. In modern oncology, AI encompasses a range of technologies including machine learning, deep learning, and natural language processing, which together can analyze multifaceted data from pathology reports, clinical records, genomic information, and medical images to generate clinically actionable insights [56]. The emergence of AI promises to bridge critical gaps in healthcare access, potentially helping to serve the 4.5 billion people currently lacking essential healthcare services by enhancing diagnostic efficiency and accuracy [116].
This comparison guide objectively evaluates the performance of AI-driven methodologies against conventional techniques across two foundational domains: automated image analysis in radiology and pathology, and predictive biomarker discovery in molecular oncology. By synthesizing current evidence and experimental data, we provide researchers, scientists, and drug development professionals with a rigorous assessment of how these technological paradigms compare in real-world clinical and research applications, framed within the broader context of molecular techniques in cancer diagnostics.
AI vs. Traditional Methods in Diagnostic Imaging
Performance Comparison in Clinical Practice
Table 1: Comparative Performance of AI vs. Traditional Methods in Cancer Imaging
| Diagnostic Metric | AI-Based Approaches | Traditional Methods | Clinical Evidence |
|---|---|---|---|
| Early Detection Sensitivity | Identifies subtle changes in scans; may detect cancer at earlier stages [117] | May miss subtle early signs; limited by human visual perception [117] | AI identified 64% of epilepsy brain lesions missed by radiologists [116] |
| Diagnostic Accuracy (AUC) | Potential to match or surpass human performance in task-specific applications [118] | Subject to inter-rater variability and human error [118] | AI model identified cancer risk in nodules with AUC of 0.87, outperforming clinical tests [117] |
| Analysis Speed | Rapid analysis of vast datasets; suitable for handling large volumes efficiently [117] | Requires more time for image analysis; potentially delayed diagnosis [117] | AI tool spotted brain lesions more quickly than doctors [116] |
| Tumor Characterization | Can characterize tumors at early stage; identifies nature and behavior [117] | Primarily focuses on detection; limited characterization information [117] | AI translates phenotypic nuances to genotype implications [118] |
| Workflow Integration | Can reduce time spent reviewing patients by up to 40% [116] | Manual processes dominate; time-consuming tumor delineation [118] | Digital patient platform Huma reduced readmission rates by 30% [116] |
The clinical implementation of AI in cancer imaging focuses on three main tasks: detection, characterization, and monitoring of tumors [118]. AI-based computer-aided detection (CADe) systems localize objects of interest in radiographs, reducing observational oversights and serving as an initial screen against errors of omission [118]. For characterization, AI enables precise segmentation, diagnosis, and staging of tumors, with capabilities extending to biological characterization through the emerging field of "imaging genomics" that correlates radiographic features with molecular signatures [118].
Experimental Protocol: AI-Assisted Mammography Interpretation
A 2024 retrospective study provides a robust experimental framework for evaluating AI implementation in clinical imaging workflows [119]. The study analyzed 2,061 screening examinations from 1,819 women with a mean age of 50.8 years.
Methodology:
- AI System: Commercial AI-CAD program (Lunit Insight MMG) providing abnormality scores (0-100%) per breast with heatmap visualization.
- Study Design: Alternating monthly implementation where radiologists either had access to or were blinded to AI-CAD results.
- Interpretation Protocol: Four radiologists interpreted mammograms with reference to prior studies when available.
- Reference Standard: Histopathological confirmation for cancer cases; stable findings on follow-up for at least 1 year for negative results.
- Statistical Analysis: Performance quantified by sensitivity, specificity, positive predictive value, negative predictive value, accuracy, area under the receiver-operating-characteristics curve, cancer detection rate, and recall rate.
Key Findings: Radiologists working with AI-CAD assistance showed the same sensitivity (76.5%) and similar specificity (92.3% vs 93.8%), AUC (0.844 vs 0.851), and recall rates (8.8% vs 7.4%) compared to standalone AI-CAD. However, without AI assistance, radiologists demonstrated lower specificity (91.9% vs 94.6%) and accuracy (91.5% vs 94.1%) alongside higher recall rates (8.6% vs 5.9%) compared to stand-alone AI-CAD [119].
AI-Driven Biomarker Discovery vs. Conventional Molecular Techniques
Comparative Analytical Approaches
Table 2: Comparison of Biomarker Discovery Methods
| Analytical Aspect | AI/ML-Driven Approaches | Conventional Molecular Techniques | Example Technologies |
|---|---|---|---|
| Throughput & Scale | Analyzes various data types from genomic sequences to proteomic profiles at system-wide level [120] | Typically focuses on single or limited biomarker analysis; lower throughput | MarkerPredict analyzes 3,670 target-neighbor pairs simultaneously [121] |
| Feature Identification | Identifies novel biomarker patterns through advanced feature selection techniques and algorithms [120] | Relies on predefined hypotheses and established biological knowledge | Random Forest and XGBoost ML models identify network topology features [121] |
| Multi-Modal Integration | Integrates network motifs with protein disorder data and other heterogeneous data types [121] | Limited capacity for integrating disparate data types in discovery phase | Combines topological information with protein annotations [121] |
| Validation Efficiency | LOOCV accuracy of 0.7-0.96 across different models and signaling networks [121] | Requires separate, often lengthy analytical and clinical validation phases | MarkerPredict uses leave-one-out-cross-validation during development [121] |
| Novelty Potential | Facilitates identification of novel biomarkers through system-level analysis [120] [121] | Primarily confirms or characterizes previously suspected biomarkers | Identified 2,084 potential predictive biomarkers, 426 classified by all calculations [121] |
AI and ML have become crucial tools for identifying biomarkers in healthcare engineering, with particular impact in precision oncology [120] [55]. These technologies enable researchers to analyze diverse data types - from genomic sequences to proteomic profiles - facilitating the identification of novel biomarkers that enhance understanding of cancer biology and pave the way for personalized medicine [120]. The analytical validity of biomarker assays is crucial, encompassing aspects such as sample handling, assay methods, and reliability of results [120].
Experimental Protocol: Predictive Biomarker Discovery with MarkerPredict
A 2025 study detailed the development of MarkerPredict, a hypothesis-generating framework that integrates network motifs and protein disorder to explore their contribution to predictive biomarker discovery [121].
Methodology:
- Training Data: Literature evidence-based positive and negative training sets of 880 target-interacting protein pairs total.
- Machine Learning Models: Random Forest and XGBoost algorithms trained on three signaling networks (Human Cancer Signaling Network, SIGNOR, ReactomeFI).
- Feature Analysis: Incorporated topological information from signaling networks and protein annotations, including comprehensive data from three IDP databases (DisProt, AlphaFold, IUPred).
- Classification Scope: Analyzed 3,670 target-neighbor pairs with 32 different models.
- Validation Approach: Leave-one-out-cross-validation, k-fold cross-validation, and validation with 70:30 splitting of training and test datasets.
- Output Metric: Biomarker Probability Score defined as a normalized summative rank of the models.
Key Findings: The framework achieved 0.7-0.96 LOOCV accuracy across different models [121]. The Biomarker Probability Score identified 2,084 potential predictive biomarkers for targeted cancer therapeutics, with 426 classified as biomarkers by all four calculations [121]. The study demonstrated that intrinsically disordered proteins are enriched in network triangles and are likely to be cancer biomarkers, with more than 86% of IDPs in all three networks being prognostic biomarkers [121].
Figure 1: MarkerPredict Workflow for Predictive Biomarker Discovery
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for AI-Enhanced Cancer Diagnostics
| Research Tool | Type/Platform | Primary Function | Application Context |
|---|---|---|---|
| Prov-GigaPath [56] [55] | Whole-slide foundation model | Provides whole-slide embeddings for digital pathology | Cancer detection imaging and pathology analysis |
| Owkin's Models [56] [55] | AI platform | Federated learning for multimodal data analysis | Drug discovery and biomarker identification |
| CHIEF [56] [55] | AI model | Cancer detection from imaging data | Diagnostic imaging interpretation |
| AlphaFold 3 [55] | Structure prediction AI | Predicts 3D protein structures and interactions | Forecasting treatment-relevant biomarkers |
| Paige Prostate Detect [55] | Clinical AI application | Improves prostate biopsy interpretation | Digital pathology and diagnostic support |
| MSI-SEER [55] | AI-powered diagnostic tool | Identifies microsatellite instability-high regions | Gastrointestinal cancer immunotherapy selection |
| Lunit Insight MMG [119] | Commercial AI-CAD program | Provides abnormality scores and heatmaps | Mammography interpretation assistance |
| HistoPathXplorer [55] | AI diagnostic tool | Tissue biomarker detection | Pathology and biomarker analysis |
| DeepHRD [55] | Deep learning tool | Detects homologous recombination deficiency | Identifying patients for PARP inhibitor therapy |
| MarkerPredict [121] | ML framework | Classifies predictive biomarkers using network data | Biomarker discovery for targeted cancer therapies |
Integrated Signaling Pathways in AI-Driven Biomarker Discovery
Figure 2: Network-Based Predictive Biomarker Discovery Pathway
The diagram illustrates the integrated signaling pathway approach that underpins modern AI-driven biomarker discovery. This framework leverages the relationship between intrinsically disordered proteins and their participation in network motifs with oncotherapeutic targets [121]. The working hypothesis is that protein disorder and protein position in signaling networks may contribute to the efficacy of predicting oncological biomarkers [121]. Three-nodal motifs typically represent parts of signaling pathways, and the enrichment of IDPs in these motifs suggests close regulatory connections that can be exploited for biomarker discovery [121].
The pathway begins with the identification of intrinsically disordered proteins and their participation in network motifs with target proteins. These relationships are processed through machine learning models that incorporate both topological features from signaling networks and protein disorder annotations. The output is a Biomarker Probability Score that enables ranking of potential biomarkers for further validation [121]. This approach has identified that triangles containing both IDP and target members exist with significantly larger frequency than would occur by random chance, and that unbalanced triangles are significantly overrepresented among these relationships [121].
The evidence synthesized in this comparison guide demonstrates that AI and ML technologies are not merely incremental improvements but represent a fundamental shift in cancer diagnostic capabilities. In imaging analysis, AI systems consistently match or surpass human performance in specific diagnostic tasks while offering significant improvements in efficiency and reproducibility [119] [118]. In biomarker discovery, ML approaches enable system-level analysis that identifies novel predictive patterns beyond the scope of conventional molecular techniques [120] [121].
Nevertheless, the most effective diagnostic paradigm appears to be a synergistic approach that leverages the strengths of both technological philosophies. AI excels at processing complex, high-dimensional data and identifying subtle patterns, while traditional methods provide established clinical validation and interpretability. The integration of AI tools into clinical workflows - as demonstrated in the mammography study where radiologists used AI-CAD assistance [119] - represents a pragmatic path forward that enhances human expertise rather than replacing it.
For researchers and drug development professionals, this evolving landscape presents both opportunities and challenges. The opportunity lies in leveraging AI-driven tools to accelerate discovery and personalize cancer diagnostics; the challenge resides in rigorously validating these tools, ensuring representative and diverse training data, and navigating the evolving regulatory landscape for AI-based medical devices. As these technologies continue to mature, they hold the potential to significantly advance precision oncology by making diagnostics more accurate, efficient, and broadly accessible.
The landscape of cancer diagnostics has been fundamentally reshaped by the advent of sophisticated molecular techniques, with next-generation sequencing (NGS) emerging as a pivotal technology. NGS represents a revolutionary leap in genomic technology, enabling the rapid sequencing of entire genomes or targeted genomic regions with unprecedented speed and accuracy [16]. Unlike traditional Sanger sequencing, which sequences DNA fragments individually, NGS utilizes massive parallel sequencing, processing millions of fragments simultaneously, significantly reducing both time and cost associated with comprehensive genomic analysis [16]. This technological advancement has facilitated the widespread integration of NGS into clinical settings, transforming the approach to cancer diagnosis and treatment through detailed genomic profiling of tumors [16].
The economic and regulatory considerations for adopting these advanced molecular techniques are complex and multifaceted. As clinical laboratories and healthcare institutions evaluate the implementation of NGS and related technologies, they must navigate intricate cost-benefit analyses, regulatory pathways for device approval, and strategies for securing clinical adoption and reimbursement. This guide provides a comparative analysis of these elements, offering researchers, scientists, and drug development professionals a structured framework for evaluating molecular diagnostic technologies within the broader context of cancer diagnostics research.
Comparative Analysis of Molecular Techniques
Technology Performance and Capabilities
Molecular techniques for cancer diagnostics vary significantly in their technical approaches, performance characteristics, and clinical applications. The following comparison outlines key technologies and their operational attributes:
Next-Generation Sequencing (NGS): NGS platforms provide comprehensive genomic profiling through massively parallel sequencing, enabling the identification of genetic mutations, structural variations, and other genomic alterations driving tumorigenesis [16]. Key methodologies include:
- Whole-Genome Sequencing (WGS): Analyzes the entire genome for comprehensive variant detection.
- Whole-Exome Sequencing (WES): Focuses on protein-coding regions, balancing cost and clinical yield.
- Targeted Panels: Sequences specific genes or regions of interest with enhanced depth and cost-efficiency for actionable mutations.
Targeted RNA-Sequencing: Specifically designed for detecting oncogenic fusions in cancer, with two primary methodological approaches:
- Amplicon-Based Assays: Amplifies specific target regions; generally faster and less complex but may miss novel or rare fusions [122].
- Hybridization-Capture-Based Assays: Uses probes to capture target sequences; demonstrates superior capability in identifying rare and novel oncogenic fusions missed by amplicon-based methods [122].
Traditional Sanger Sequencing: The historical gold standard, utilizing chain-terminating dideoxynucleotides (ddNTPs) during DNA synthesis followed by capillary electrophoresis [16]. While highly accurate for confirming specific mutations, its low throughput and inability to detect mutations in non-coding regions limit its utility in comprehensive cancer genomic profiling [16].
Table 1: Comparative Analysis of Sequencing Technologies
| Feature | Next-Generation Sequencing (NGS) | Sanger Sequencing |
|---|---|---|
| Cost-Effectiveness | Higher for large-scale projects | Lower for small-scale projects |
| Speed | Rapid sequencing of multiple targets | Time-consuming for multiple targets |
| Primary Applications | Whole-genome, whole-exome, and targeted sequencing | Ideal for sequencing single genes |
| Throughput | Processes millions of sequences simultaneously | Processes single sequences at a time |
| Data Output | Large amount of comprehensive genomic data | Limited data output |
| Clinical Utility | Detects mutations, structural variants, and fusion genes | Identifies specific known mutations |
Experimental Data and Performance Metrics
Recent studies provide quantitative comparisons of molecular technique performance. A single-institutional clinical experience with a testing algorithm for non-small-cell lung carcinoma (NSCLC) that utilized amplicon-based DNA/RNA sequencing, followed by reflex hybridization-capture-based RNA sequencing when initial testing was negative, demonstrated significant findings [122]. Among 1,211 NSCLC specimens tested, approximately 10% (120 cases) required reflex hybridization-capture-based RNA sequencing, which identified oncogenic fusions in 9 cases [122]. These included clinically actionable fusions involving ALK, BRAF, NRG1, NTRK3, ROS1, and RET—none of which were detected by the initial amplicon-based assay [122].
Analysis of the American Association for Cancer Research Project Genie database (version 15.1) comprising 20,900 NSCLC cases revealed that of the 1,081 cases harboring fusions, 893 (82.6%) could theoretically be detected by amplicon-based assays, indicating that approximately 17.4% of fusion-positive cases require more comprehensive methods like hybridization-capture-based RNA sequencing for detection [122]. This demonstrates the critical performance differences between methodological approaches and their direct impact on clinical sensitivity.
Table 2: Detection Rates of Fusion Genes by Sequencing Method in NSCLC
| Sequencing Method | Theoretical Detection Rate | Actual Detection in Clinical Series | Types of Fusions Identified |
|---|---|---|---|
| Amplicon-Based RNA Sequencing | 82.6% of known fusions (per database analysis) | 0/9 fusions in reflex-tested cases | None detected in reflex cohort |
| Hybridization-Capture-Based RNA Sequencing | Enhanced detection of rare/novel fusions | 9/9 fusions in reflex-tested cases | ALK, BRAF, NRG1, NTRK3, ROS1, RET |
| Reflex Testing Strategy | Comprehensive fusion detection | 120 cases tested (10% of total) | All clinically actionable fusions detected |
Experimental Protocols and Methodologies
Next-Generation Sequencing Workflow
The NGS process involves multiple critical steps, each requiring specific protocols and quality control measures to ensure accurate results [16]:
Sample Preparation and Library Construction:
- Nucleic Acid Extraction: Isolate high-quality DNA or RNA from tumor samples (fresh frozen or FFPE tissue).
- Quality Assessment: Evaluate nucleic acid quantity and quality using spectrophotometry (e.g., Nanodrop) and fluorometry (e.g., Qubit).
- Library Preparation: Fragment genomic DNA to appropriate size (approximately 300 bp) using physical, enzymatic, or chemical methods. Attach platform-specific adapters to fragment ends via ligation.
- Library Amplification: Amplify adapter-ligated fragments using polymerase chain reaction (PCR) to generate sufficient material for sequencing.
- Library Quality Control: Assess final library quality and quantity using methods such as quantitative PCR or bioanalyzer systems.
Sequencing Reaction:
- Cluster Generation: For Illumina platforms, immobilize library fragments on a flow cell and amplify to form clusters of identical sequences through bridge PCR.
- Sequencing-by-Synthesis: Utilize fluorescently labeled nucleotides incorporated into growing DNA strands, with imaging of fluorescence emission at each cycle to determine sequence.
- Signal Processing: Convert fluorescence signals into base calls with associated quality scores.
Data Analysis:
- Base Calling and Demultiplexing: Generate raw sequence data and assign reads to specific samples based on index sequences.
- Sequence Alignment: Map reads to reference genome using alignment algorithms (e.g., BWA, Bowtie).
- Variant Calling: Identify mutations, insertions/deletions, copy number variations, and structural variants using specialized software (e.g., GATK, VarScan).
- Variant Annotation and Interpretation: Annotate variants with biological and clinical information, filter for clinical relevance, and classify according to professional guidelines.
Targeted RNA-Sequencing Protocol for Fusion Detection
The experimental protocol for detecting oncogenic fusions in NSCLC using a reflex testing approach involves specific methodologies [122]:
Initial Testing - Amplicon-Based DNA/RNA Sequencing:
- Sample Requirements: Formalin-fixed paraffin-embedded (FFPE) tumor tissue sections with minimum tumor cellularity of 20%.
- Nucleic Acid Extraction: Co-extract DNA and RNA from the same FFPE section using commercial kits with DNase and RNase treatment steps.
- Targeted Amplification: For RNA analysis, convert to cDNA followed by PCR amplification using primers targeting known fusion hotspots in genes including ALK, ROS1, RET, NTRK, and others.
- Sequencing: Perform sequencing on appropriate NGS platform (e.g., Illumina MiSeq) with minimum coverage of 500x.
- Analysis: Use vendor-specific software for alignment and variant calling with established thresholds for fusion detection.
Reflex Testing - Hybridization-Capture-Based RNA Sequencing:
- Sample Selection: Apply to cases that are negative for oncogenic drivers in initial testing but have high clinical suspicion for fusions.
- Library Preparation: Use hybridization-based capture methods with probes designed to target full coding regions of relevant genes rather than specific breakpoints.
- Sequencing Parameters: Perform sequencing with increased depth (recommended >1000x) to enhance sensitivity for rare fusion events.
- Bioinformatic Analysis: Utilize multiple fusion detection algorithms (e.g., Arriba, STAR-Fusion, FusionCatcher) to identify both known and novel fusion events with high confidence.
- Validation: Confirm positive fusion results by an orthogonal method such as FISH or RT-PCR when sufficient sample is available.
Regulatory Pathways for Diagnostic Devices
FDA Regulatory Framework
Molecular diagnostic systems are regulated as medical devices by the U.S. Food and Drug Administration (FDA) under a risk-based classification system with three regulatory classes [123]. The pathway to market approval depends on the device's classification and intended use:
Class I Devices: Present minimal potential risk to users. Most are exempt from premarket notification requirements [123] [124]. Examples include simple specimen collection devices.
Class II Devices: Pose moderate risk and typically require Premarket Notification [510(k)] to demonstrate substantial equivalence to a legally marketed predicate device [123] [124]. Most NGS-based diagnostic systems fall into this category.
Class III Devices: Sustain or support life, are implanted, or present potential high risk, requiring Premarket Approval (PMA) to demonstrate safety and effectiveness through extensive scientific evidence [123] [124]. Companion diagnostics for high-risk applications may be classified as Class III.
Key Regulatory Pathways
The FDA provides multiple pathways for bringing medical devices to market, each with distinct requirements and considerations [123] [125]:
Premarket Notification [510(k)]:
- Purpose: Demonstrate substantial equivalence to a predicate device legally marketed in the U.S. [123].
- Process: Submit comparison to predicate device, detailed device descriptions, labeling, and performance data [124].
- Timeline: Typically processed within 30-90 days [125].
- Applicability: Most Class I and II devices, including many molecular diagnostics [123].
Premarket Approval (PMA):
- Purpose: Provide scientific evidence demonstrating reasonable assurance of device safety and effectiveness for Class III devices [123].
- Process: Requires extensive preclinical and clinical data, often from well-controlled clinical trials [124].
- Timeline: FDA review within 180 days, though the overall process may take years including data collection [125].
- Applicability: High-risk devices, including novel diagnostic platforms without predicates [123].
De Novo Classification:
- Purpose: Pathway for novel devices of low to moderate risk without predicates [123] [125].
- Process: Submit petition with detailed device information and evidence of safety and effectiveness [124].
- Timeline:
- Applicability: New types of molecular diagnostics with innovative technology but moderate risk profile [125].
Other Pathways:
- Humanitarian Device Exemption (HDE): For devices treating conditions affecting small populations (<4,000 patients annually in U.S.) with modified requirements for effectiveness evidence [123] [125].
- Custom Device Exemption: For devices created for individual patients with unique medical needs [125].
Quality System and Post-Market Requirements
Medical device manufacturers must comply with Quality System Regulations (QSR) throughout the device lifecycle [124]:
Quality Management System (QMS) Requirements:
- Design Controls: Establish and maintain procedures to control device design.
- Documentation Controls: Maintain Device Master Record (DMR) and Device History Record (DHR).
- Production and Process Controls: Implement Good Manufacturing Practices (GMP).
- Corrective and Preventive Actions (CAPA): Establish robust CAPA procedures.
- Management Responsibilities: Define organizational structure and responsibilities.
Post-Market Surveillance:
- Adverse Event Reporting: Monitor and report device-related adverse events.
- Post-Market Studies: Conduct additional studies if required as a condition of approval.
- Recalls and Corrections: Implement procedures for device recalls and corrections when necessary.
Economic Considerations and Reimbursement Strategies
Cost-Benefit Analysis of Molecular Techniques
The economic evaluation of molecular diagnostic techniques involves analyzing both direct costs and clinical benefits:
Direct Costs:
- Capital Equipment: NGS platforms represent significant capital investment ($100,000-$1,000,000+ depending on scale and capabilities).
- Consumables and Reagents: Cost per sample varies by methodology: targeted panels ($200-$500), whole exome sequencing ($500-$1,000), whole genome sequencing ($1,000-$3,000).
- Personnel Requirements: Bioinformaticians, molecular technologists, clinical laboratory geneticists.
- Infrastructure: IT infrastructure for data storage and analysis, laboratory space, quality control systems.
Clinical Benefits and Cost Offsets:
- Targeted Therapy Selection: Avoids costs of ineffective treatments; targeted therapies typically range from $5,000-$15,000 per month.
- Improved Outcomes: Earlier appropriate intervention may reduce downstream complications and hospitalizations.
- Efficient Diagnostic Pathways: Comprehensive testing reduces time to diagnosis compared to sequential single-gene tests.
Economic Value Proposition: Studies evaluating precision medicine interventions incorporating NGS have demonstrated improved overall survival compared to standard therapies alone, contributing to the value proposition despite higher initial testing costs [55]. The economic benefit is particularly evident in advanced cancers where inappropriate treatment imposes substantial clinical and financial costs.
Reimbursement Landscape and Strategies
Securing adequate reimbursement is critical for sustainable implementation of molecular diagnostic technologies:
Current Reimbursement Environment:
- CMS Coverage: Medicare coverage for NGS testing varies by jurisdiction and specific test indications.
- Private Payers: Coverage policies increasingly recognize the clinical utility of comprehensive genomic profiling, particularly in advanced cancers.
- Coding Systems: Utilize specific CPT codes for molecular pathology procedures, genomic sequencing procedures, and data analysis.
Reimbursement Strategy Development:
- Evidence Generation: Develop robust clinical utility evidence demonstrating improved health outcomes.
- Health Economic Analyses: Conduct cost-effectiveness studies comparing new technologies to standard approaches.
- Stakeholder Engagement: Collaborate with payers early in technology development to understand evidence requirements.
- Real-World Data Collection: Implement systems to collect real-world evidence on clinical utility and economic impact.
Adoption Barriers and Solutions: Key barriers to adoption identified across healthcare technologies include [126]:
- Workload Impact: Perceived increase in staff workload during implementation.
- Clinical Workflow Changes: Integration into existing clinical workflows and habits.
- Reimbursement Uncertainty: Unclear reimbursement pathways and levels.
Successful adoption strategies include [126]:
- Organizational Environment: Favorable institutional support and infrastructure.
- Tension for Change: Recognition of unmet clinical need creating impetus for change.
- Staff Engagement: Early and ongoing engagement of clinical staff in implementation planning.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Molecular Cancer Diagnostics
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from clinical specimens | Select based on sample type (FFPE, fresh frozen, liquid biopsy); critical input for all downstream analyses |
| Library Preparation Kits | Preparation of sequencing libraries from nucleic acids | Platform-specific kits (Illumina, Ion Torrent); target enrichment methods (hybridization-capture vs. amplicon-based) |
| Sequence Adapters and Indexes | Platform-specific oligonucleotides for sample multiplexing | Enable barcoding of samples for pooled sequencing; critical for sample tracking and identification |
| Hybridization Capture Probes | Target enrichment for specific genomic regions | Designed for genes of interest in cancer; impact sensitivity for fusion detection [122] |
| PCR Reagents | Amplification of target sequences | Enzymes with high fidelity critical for accurate variant detection; optimized buffers for GC-rich regions |
| Quality Control Assays | Assessment of nucleic acid and library quality | Fluorometric quantification (Qubit), fragment analysis (Bioanalyzer/TapeStation), qPCR for library quantification |
| Reference Standard Materials | Controls for assay validation and quality monitoring | Cell lines with known mutations, synthetic controls; essential for assay validation and proficiency testing |
| Bioinformatic Tools | Data analysis, variant calling, and interpretation | Open-source and commercial software for alignment (BWA), variant calling (GATK), fusion detection (Arriba, STAR-Fusion) |
The integration of advanced molecular techniques like NGS into cancer diagnostics represents a paradigm shift in precision oncology, offering unprecedented capabilities for comprehensive genomic profiling. The comparative analysis presented in this guide demonstrates significant differences in performance characteristics between methodological approaches, with hybridization-capture-based RNA sequencing showing particular value in detecting rare and novel oncogenic fusions that may be missed by amplicon-based methods [122].
Successful implementation of these technologies requires careful navigation of regulatory pathways, with the 510(k) route being most common for established technologies, while novel approaches may require De Novo classification or PMA depending on risk profile [123] [125]. Economic viability depends not only on the technical performance and cost structure of the testing methodology, but also on developing effective reimbursement strategies that demonstrate clinical value to healthcare systems [55].
As molecular technologies continue to evolve, researchers and diagnostic developers must maintain awareness of both the technical capabilities and the regulatory-economic landscape to successfully translate promising technologies into clinically adopted solutions that improve patient care in oncology.
Conclusion
The comparison of molecular techniques reveals a dynamic and complementary diagnostic ecosystem where no single technology is universally superior. The choice between PCR, NGS, liquid biopsy, and molecular imaging must be guided by the specific clinical or research question, weighing factors such as required sensitivity, the breadth of genomic interrogation, tissue availability, and cost. The integration of artificial intelligence is poised to revolutionize this field, enhancing the interpretation of complex datasets from NGS and digital pathology, and enabling the discovery of novel biomarkers. Future progress hinges on standardizing assays, validating them in large-scale clinical trials, and improving the accessibility of these sophisticated tools. For researchers and drug developers, this evolving landscape underscores the imperative to adopt a multi-modal, integrated diagnostic strategy to fully realize the promise of precision oncology, ultimately leading to more effective, personalized cancer therapies and improved patient outcomes.
References
- 1. A Protein-Based Blood Test for Multi-Cancer Diagnostics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561768/]
- 2. Analytical techniques for nucleic acid and protein detection ... [https://www.nature.com/articles/s12276-025-01453-w]
- 3. Molecular methods in cancer diagnostics: a short review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11100444/]
- 4. New tool enables and enhances protein investigations [https://www.news-medical.net/news/20251003/New-tool-enables-and-enhances-protein-investigations.aspx]
- 5. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 6. vs dPCR vs end-point qPCR PCR [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/pcr/digital-pcr/digital-pcr-vs-quantitative-pcr-vs-end-point-pcr]
- 7. A comprehensive review of methodological and ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975025002058]
- 8. vs qPCR : Choosing the Right dPCR ... | Technology Networks PCR [https://www.technologynetworks.com/analysis/articles/qpcr-vs-dpcr-choosing-the-right-pcr-technology-to-suit-your-experimental-needs-386507]
- 9. qPCR in Early Cancer Detection: Why It Still Leads the Pack [https://www.meridianbioscience.com/lifescience-blog/why-qpcr-still-leads-in-oncology/]
- 10. Digital PCR (dPCR) vs Real-Time PCR (qPCR) [https://firalismolecularprecision.com/2025/04/09/dpcr-qpcr-differences/]
- 11. - RT and qPCR -Digital RT : A PCR of Different Platforms... Comparison [https://pubmed.ncbi.nlm.nih.gov/27979961/]
- 12. Quantitative or digital PCR? A comparative analysis for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624001584]
- 13. Comparative Performance of Digital PCR and Real-Time RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474457/]
- 14. Next Generation Sequence Testing: Essential 2025 Guide [https://lifebit.ai/blog/next-generation-sequence-testing/]
- 15. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 16. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 17. Next-generation sequencing impact on cancer care [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1420190/full]
- 18. Benefits of NGS in Oncology [https://www.illumina.com/areas-of-interest/cancer/ngs-in-oncology.html]
- 19. A Comparative Overview of Epigenomic Profiling Methods [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.714687/full]
- 20. DNA Sequencing: How to Choose the Right Technology [https://frontlinegenomics.com/dna-sequencing-how-to-choose-the-right-technology/]
- 21. Molecular Imaging Probes Target Extracellular Matrix, ... [https://www.mdpi.com/1424-8247/17/12/1663]
- 22. Current status and future prospects of molecular imaging in ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1518555/full]
- 23. Novel molecular imaging approaches in oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12337909/]
- 24. Molecular imaging using (nano)probes - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03927d]
- 25. Advances and challenges in immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521690/]
- 26. Molecular PET imaging: Unlocking the secrets of cancer ... [https://www.sciencedirect.com/science/article/pii/S0006295225004678]
- 27. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 28. A Review of Circulating Tumor DNA (ctDNA) and the Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032849/]
- 29. Analytical evaluation of circulating tumor DNA sequencing ... [https://www.nature.com/articles/s41598-024-54361-w]
- 30. Performance Comparison of Droplet Digital PCR and Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062871/]
- 31. A Systematic Review and Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9581609/]
- 32. Comparison of solid tissue sequencing and liquid biopsy ... [https://pubmed.ncbi.nlm.nih.gov/34362997/]
- 33. FDA approves liquid biopsy NGS companion diagnostic ... [https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-liquid-biopsy-ngs-companion-diagnostic-test-multiple-cancers-and-biomarkers]
- 34. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 35. BRCA Gene Changes: Cancer Risk and Genetic Testing [https://www.cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet]
- 36. BRCA1, BRCA2 and Associated Cancer Risks ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12080741/]
- 37. Lynch syndrome and colorectal cancer: A review of current ... [https://pubmed.ncbi.nlm.nih.gov/40612862/]
- 38. Genetic characterization of Lynch syndrome germline ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1589765/full]
- 39. Comparison of the clinical prediction model PREMM>1,2,6 ... [https://mayoclinic.elsevierpure.com/en/publications/comparison-of-the-clinical-prediction-model-premmsub126sub-and-mo/]
- 40. Trends in the Utilization of BRCA1 and BRCA2 Testing After ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384781/]
- 41. BCRF-Supported Study Clarifies Risk Potential for ... [https://www.bcrf.org/blog/brca2-variants-of-uncertain-significance-2025/]
- 42. Stanford Medicine researchers develop RNA blood test to ... [https://med.stanford.edu/news/all-news/2025/04/rna-blood-test-cancer-detection.html]
- 43. Precision cancer medicine 2025: some concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439214/]
- 44. Companion diagnostics in targeted therapy | LabLeaders [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/companion-diagnostics-targeted-therapy.html]
- 45. An analysis of FDA drug approvals for oncological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507643/]
- 46. Companion Diagnostic FDA Review Flexibilities [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181087/]
- 47. Predicting ROS1 and ALK fusions in NSCLC from H&E ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12311174/]
- 48. Advancements in fighting lung cancer benefit ALK patients [https://diagnostics.roche.com/us/en/article-listing/lung-cancer-advancements-anaplastic-lymphoma-kinase-alk.html]
- 49. Enhanced patient selection with quantitative continuous ... [https://www.nature.com/articles/s41698-025-01107-0]
- 50. FDA Grants Premarket Approval to Idylla CDx MSI Test for ... [https://www.onclive.com/view/fda-grants-premarket-approval-to-idylla-cdx-msi-test-for-msi-h-crc]
- 51. PD-L1 Biomarker Testing Market Trends & Forecast 2025– ... [https://www.futuremarketinsights.com/reports/pd-l1-biomarker-testing-market]
- 52. First-Line Alectinib Yields Clinically Meaningful OS Benefit ... [https://www.onclive.com/view/first-line-alectinib-yields-clinically-meaningful-os-benefit-in-advanced-alk-nsclc]
- 53. Minimal Residual Disease Detection: Implications for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079024/]
- 54. A comprehensive overview of minimal residual disease in ... [https://www.nature.com/articles/s41698-025-00984-9]
- 55. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]
- 56. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 57. Exploring the molecular landscape of cancer of unknown ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11459033/]
- 58. Cancer of unknown primary: the hunt for its elusive tissue ... [https://www.nature.com/articles/s41416-025-03073-7]
- 59. Molecularly directed therapy in cancers of unknown primary [https://www.sciencedirect.com/science/article/abs/pii/S095980492500228X]
- 60. Liquid Biopsies: A Revolution in Early Cancer Detection ... [https://www.aicr.org/resources/blog/liquid-biopsies-a-revolution-in-early-cancer-detection-and-monitoring/]
- 61. Expanding screening through the use of liquid biopsy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12065791/]
- 62. Promises and pitfalls of multi-cancer early detection using ... [https://www.nature.com/articles/s41571-025-01033-x]
- 63. Review Liquid biopsy-based multi-cancer early detection [https://www.sciencedirect.com/science/article/pii/S2095927325006565]
- 64. Innovative laboratory techniques shaping cancer diagnosis ... [https://link.springer.com/article/10.1007/s12672-025-01877-w]
- 65. Machine learning for multi-omics data integration in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC8829812/]
- 66. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 67. Genomic and Proteomic Biomarkers for Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC2752479/]
- 68. Genomic and proteomic biomarkers for cancer: A multitude ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X09000262]
- 69. Analysis of Comparative - Multi Using Graph... Omics Integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC11928009/]
- 70. Frontiers | MASE-GC: a multi - omics autoencoder and stacking... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1704237/full]
- 71. Identifying proteomic risk factors for cancer using ... [https://www.nature.com/articles/s41467-024-48017-6]
- 72. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 73. Exploring the influence of pre-analytical variables on gene ... [https://www.nature.com/articles/s41598-025-88756-0]
- 74. Preanalytical variables and analytes in liquid biopsy ... [https://pubmed.ncbi.nlm.nih.gov/40884415/]
- 75. AI enhanced diagnostic accuracy and workload reduction ... [https://www.nature.com/articles/s41746-025-01892-9]
- 76. AOA Dx Demonstrates High Accuracy in AI-Powered Blood ... [https://aoadx.com/aacr2025/]
- 77. Digital PCR Breaks Into the Mainstream in 2025 - Vocal Media [https://vocal.media/feast/digital-pcr-breaks-into-the-mainstream-in-2025]
- 78. Monitoring Variant Allele Fraction in VEXAS Syndrome [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637854/]
- 79. Next-generation sequencing methodologies to detect low ... [https://www.sciencedirect.com/science/article/abs/pii/S1383574223000194]
- 80. Validation of a liquid biopsy assay with increased ... [https://www.sciencedirect.com/science/article/pii/S2950195425000384]
- 81. Comparative Performance of a Targeted Next-Generation ... [https://pubmed.ncbi.nlm.nih.gov/41072730/]
- 82. Comparative performance of a targeted next-generation ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157825002375]
- 83. Evaluating sensitivity of NGS-based mutation detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486888/]
- 84. A Review on Biomarker‐Enhanced Machine Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421415/]
- 85. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 86. A Primer on NGS Technologies and Their Specs (2025) [https://blog.latch.bio/p/a-primer-on-ngs-technologies-and]
- 87. Sequencing Quality Scores [https://www.illumina.com/science/technology/next-generation-sequencing/plan-experiments/quality-scores.html]
- 88. Top 10 Bioinformatics Tools in 2025: Features, Pros, Cons ... [https://www.cotocus.com/blog/top-10-bioinformatics-tools-in-2025-features-pros-cons-comparison/]
- 89. FAIR Principles [https://www.go-fair.org/fair-principles/]
- 90. The FAIR Guiding Principles for scientific data ... [https://www.nature.com/articles/sdata201618]
- 91. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 92. Evaluation of turnaround times and performance of in- ... [https://pubmed.ncbi.nlm.nih.gov/40328657/]
- 93. Next-Generation Cancer Diagnostics Market Size Worth ... [https://www.biospace.com/press-releases/next-generation-cancer-diagnostics-market-size-worth-usd-38-36-billion-by-2034]
- 94. Healthcare utilization and costs following molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11650384/]
- 95. A benchmarking framework for the accurate and cost-effective ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-04865-w]
- 96. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539629/]
- 97. Systematic review of cost effectiveness and budget impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12381244/]
- 98. Cost-Benefit Analysis of Workflow Management Software [https://www.highgear.com/blog/cost-benefit-analysis-of-workflow-management-software/]
- 99. Reliability and reproducibility of a RNA preamplification method for low-density array analysis from formalin-fixed paraffin-embedded breast cancer samples - PubMed [https://pubmed.ncbi.nlm.nih.gov/19430292/]
- 100. Current AI technologies in cancer diagnostics and treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128506/]
- 101. Cancer Diagnostics Market Size & Share Analysis [https://www.mordorintelligence.com/industry-reports/cancer-diagnostic-market]
- 102. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 103. dPCR and NGS: Better Together? [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/science-matters/pcr-solutions/dpcr-and-ngs]
- 104. Multiplexed, universal probe-based rare variant detection ... [https://www.nature.com/articles/s41598-025-08814-5]
- 105. Development of Multiplex Drop-Off Digital PCR Assays for ... [https://www.sciencedirect.com/science/article/pii/S1525157823000545]
- 106. Performance Comparison of Droplet Digital PCR and Next- ... [https://pubmed.ncbi.nlm.nih.gov/40346007/]
- 107. Performance Comparison of Droplet Digital PCR and Next- ... [https://researchportal.helsinki.fi/en/publications/performance-comparison-of-droplet-digital-pcr-and-next-generation]
- 108. A Comparative Study of qPCR and dPCR [https://www.sciencedirect.com/science/article/abs/pii/S1465324925004992]
- 109. Application of Digital Polymerase Chain Reaction (dPCR) in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940399/]
- 110. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 111. The 'Liquid' Biopsy [https://www.cap.org/member-resources/articles/the-liquid-biopsy]
- 112. Patient Outcomes May Improve With Tailored Treatment ... [https://www.aacr.org/about-the-aacr/newsroom/news-releases/patient-outcomes-may-improve-with-tailored-treatment-guided-by-tissue-plus-liquid-biopsies-vs-individually/]
- 113. Clinical applications of cell-free DNA-based liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S1936523325002505]
- 114. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 115. Survival Outcomes May Improve When Treatment Is ... [https://ascopost.com/news/april-2025/survival-outcomes-may-improve-when-treatment-is-guided-by-using-both-tissue-and-liquid-biopsies]
- 116. 7 ways AI is transforming healthcare [https://www.weforum.org/stories/2025/08/ai-transforming-global-health/]
- 117. AI vs. Traditional Methods in Cancer Diagnostics [https://oncobites.blog/2024/01/24/ai-vs-traditional-methods-in-cancer-diagnostics/]
- 118. Artificial intelligence in cancer imaging: Clinical challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6403009/]
- 119. Diagnostic performance with and without artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10825593/]
- 120. Machine learning in cancer prognostic and diagnostic ... [https://www.sciencedirect.com/science/article/pii/S2666053925001031]
- 121. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 122. Comparison of Targeted RNA-Sequencing Platforms for ... [https://www.sciencedirect.com/science/article/pii/S1525157825000649]
- 123. Step 3: Pathway to Approval [https://www.fda.gov/patients/device-development-process/step-3-pathway-approval]
- 124. The Complete Regulatory Pathway for Medical Devices: [https://synergbiopharma.com/regulatory-pathway-medical-devices/]
- 125. 7 FDA Pathways to Bring Your Medical Device to Market [https://www.greenlight.guru/blog/fda-pathways-medical-device-to-market]
- 126. Factors Impacting the Adoption and Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11634046/]