Navigating Analytical Validation for Cancer Biomarker Assays: A Fit-for-Purpose Roadmap from Bench to Bedside
This article provides a comprehensive guide to the analytical validation of cancer biomarker assays, a critical step for translating discoveries into reliable clinical and research tools.
Navigating Analytical Validation for Cancer Biomarker Assays: A Fit-for-Purpose Roadmap from Bench to Bedside
Abstract
This article provides a comprehensive guide to the analytical validation of cancer biomarker assays, a critical step for translating discoveries into reliable clinical and research tools. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles of validation, explores established and emerging methodological platforms like mass spectrometry and immunoassays, and addresses common troubleshooting challenges. A central theme is the 'fit-for-purpose' approach, which tailors validation stringency to the assay's intended use, from exploratory research to clinical decision-making. The content also synthesizes key performance parameters and regulatory considerations, offering a practical framework for developing robust, reproducible, and clinically impactful biomarker assays.
Laying the Groundwork: Principles and Purpose of Biomarker Validation
Analytical validation serves as the critical bridge between biomarker discovery and clinical application, providing the rigorous evidence that an assay reliably measures what it claims to measure. This comprehensive guide examines the foundational principles, key performance parameters, and experimental protocols that underpin robust analytical validation for cancer biomarker assays. We compare leading technological platforms—including immunoassays, mass spectrometry, and quantitative PCR—through structured data tables and experimental workflows. By establishing standardized frameworks for validation, the scientific community can ensure that biomarker data generated in research settings translates effectively to clinical decision-making, ultimately accelerating the development of precision oncology therapies.
The journey of a biomarker from initial discovery to clinical implementation follows a structured pipeline characterized by progressively increasing evidence requirements. Within this pathway, analytical validation constitutes the essential second phase, following discovery and preceding clinical validation [1]. This stage provides objective evidence that a biomarker assay consistently performs according to its specified technical parameters, establishing a foundation of reliability upon which all subsequent clinical interpretations will be built [2] [3].
The fit-for-purpose approach guides modern analytical validation, recognizing that the extent of validation should align with the biomarker's intended application and stage of development [3]. For biomarkers advancing toward clinical use, validation must demonstrate that the assay method accurately and precisely measures the analyte of interest in biologically relevant matrices [2]. This process stands distinct from clinical validation, which establishes the relationship between the biomarker measurement and clinical endpoints [3] [4]. Without rigorous analytical validation, even the most promising biomarker candidates risk generating irreproducible or misleading data, potentially derailing drug development programs and compromising patient care.
Core Principles and Framework of Analytical Validation
The V3 Framework: Verification, Analytical Validation, and Clinical Validation
A comprehensive framework for evaluating biomarker tests and Biometric Monitoring Technologies (BioMeTs) comprises three distinct but interconnected components: verification, analytical validation, and clinical validation (V3) [4]. Within this structure, analytical validation specifically "occurs at the intersection of engineering and clinical expertize" and focuses on evaluating "data processing algorithms that convert sample-level sensor measurements into physiological metrics" [4]. This stage typically occurs after technical verification of hardware components and before clinical validation in patient populations.
The fundamental question addressed during analytical validation is: "Does the assay accurately and reliably measure the biomarker in the intended biological matrix?" [2]. Answering this question requires systematic assessment of multiple performance characteristics under conditions that closely mimic the intended clinical or research use.
Key Performance Parameters in Analytical Validation
Table 1: Essential Performance Parameters for Analytical Validation
| Parameter | Definition | Experimental Approach |
|---|---|---|
| Precision | The closeness of agreement between independent test results obtained under stipulated conditions [2] | Repeated measurements of the same sample under specified conditions (within-run, between-day, between-laboratory) |
| Trueness | The closeness of agreement between the average value obtained from a large series of test results and an accepted reference value [2] | Comparison of measured values to reference materials or standardized methods |
| Limits of Quantification | The highest and lowest concentrations of analyte that can be reliably measured with acceptable precision and accuracy [2] [5] | Analysis of dilution series to determine the range where linearity, precision, and accuracy are maintained |
| Selectivity | The ability of the bioanalytical method to measure and differentiate the analytes in the presence of components that may be expected to be present [2] | Testing interference from related compounds, metabolites, or matrix components |
| Robustness | The ability of a method to remain unaffected by small variations in method parameters [2] | Deliberate variations in critical parameters (incubation times, temperatures, reagent lots) |
| Sample Stability | The chemical stability of an analyte in a given matrix under specific conditions for given time intervals [2] | Measurement of analyte recovery after exposure to different storage conditions |
The validation process must also establish additional parameters including dilutional linearity (ability to obtain reliable results after sample dilution), parallelism (comparable behavior in calibrators versus biological matrix), and recovery (detector response for analyte added to biological matrix compared to true concentration) [2].
Comparative Analysis of Analytical Platforms
Immunoassay Platforms
Immunoassays, particularly enzyme-linked immunosorbent assays (ELISAs), remain widely used for protein biomarker quantification due to their sensitivity, specificity, and relatively low implementation complexity [2] [6]. However, significant variability exists between commercial immunoassay kits, even when measuring the same analyte in identical samples.
Table 2: Comparison of Commercial ELISA Kits for Corticosterone Measurement
| ELISA Kit | Mean Corticosterone (ng/mL) | Standard Deviation | Significant Differences |
|---|---|---|---|
| Arbor Assays K014-H1 | 357.75 | ± 210.52 | Significantly higher than DRG-5186 and Enzo kits |
| DRG EIA-4164 | 183.48 | ± 108.02 | Significantly higher than DRG-5186 and Enzo kits |
| Enzo ADI-900-097 | 66.27 | ± 51.48 | No significant difference from DRG-5186 |
| DRG EIA-5186 | 40.25 | ± 39.81 | No significant difference from Enzo kit |
A comparative study of four commercial ELISA kits for corticosterone measurement revealed striking differences in absolute quantification, with the Arbor Assays kit reporting values approximately 9-fold higher than the DRG-5186 kit despite analyzing identical serum samples [6]. While correlation between kits remained high, these findings highlight that absolute concentration values cannot be directly compared across different immunoassay platforms without established standardization.
Mass Spectrometry-Based Platforms
Mass spectrometry (MS) offers advantages for biomarker verification and validation through its high specificity, multiplexing capability, and ability to distinguish between closely related molecular species [1] [7]. The transition from discovery to validation in MS-based proteomics typically involves moving from non-targeted "shotgun" approaches to targeted methods like multiple reaction monitoring (MRM) or selected reaction monitoring (SRM) [1].
Key considerations for analytical validation of MS-based biomarker assays include:
- Specificity: Demonstration that the assay measures the intended analyte without interference from isobaric compounds or matrix components [7]
- Dynamic range: The range of analyte concentrations over which the assay provides precise and accurate measurements, typically exceeding 3 orders of magnitude for MRM assays [1]
- Sample preparation robustness: Consistency of results across different sample preparation batches and operators [7]
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) platforms have demonstrated capability for quantitative measurement of proteins at low picogram per milliliter levels in human plasma/serum, making them suitable for validating candidate biomarkers initially identified in discovery proteomics [7].
Quantitative PCR Platforms
Quantitative PCR (qPCR) represents the gold standard for nucleic acid-based biomarker measurement, with applications including gene expression analysis, mutation detection, and viral load quantification [8] [5]. Analytical validation of qPCR assays requires establishing several key parameters.
Table 3: Essential Validation Parameters for qPCR Assays
| Parameter | Definition | Best Practices |
|---|---|---|
| Limit of Detection | The lowest amount of analyte that can be detected with stated probability [5] | Determined through serial dilution of standard material; distinct from limit of quantification |
| Limit of Quantification | The lowest amount of analyte that can be quantitatively determined with acceptable precision and accuracy [5] | The point at which Ct values maintain linearity with input template concentration |
| Precision | Agreement between independent test results under stipulated conditions [5] | Assessment of both repeatability (intra-assay) and reproducibility (inter-assay) |
| Dynamic Range | The range of template concentrations over which the assay provides reliable quantification | Typically determined through analysis of serial dilutions spanning 6-8 orders of magnitude |
Advanced statistical approaches for qPCR data analysis include weighted linear regression and mixed effects models, which have demonstrated superior performance compared to simple linear regression, particularly when applied to data preprocessed using the "taking-the-difference" approach [8].
Experimental Protocols for Key Validation Parameters
Protocol for Precision Assessment
Purpose: To determine the closeness of agreement between independent test results obtained under stipulated conditions [2].
Materials:
- Quality control samples at low, medium, and high concentrations within the assay dynamic range
- Appropriate biological matrix matching intended sample type
- Full complement of reagents, standards, and equipment specified in assay protocol
Procedure:
- Prepare quality control samples in appropriate matrix at three concentrations (low, medium, high)
- For within-run precision: Analyze each QC sample in replicates (n≥5) within a single assay run
- For between-run precision: Analyze each QC sample in duplicate across multiple independent runs (n≥5 runs over different days)
- For between-laboratory precision: Coordinate with collaborating laboratories to analyze identical QC samples using standardized protocols
Calculation: Calculate the mean, standard deviation (SD), and coefficient of variation (CV% = [SD/mean] × 100) for each QC level at each precision level. Acceptable precision is typically defined as CV% <15-20%, though more stringent criteria may apply for biomarkers with narrow therapeutic windows [2].
Protocol for Determination of Limits of Quantification
Purpose: To establish the lowest and highest concentrations of analyte that can be measured with acceptable precision and accuracy [2] [5].
Materials:
- Stock solution of analyte with known concentration
- Appropriate biological matrix (stripped or surrogate if necessary)
- Standard materials for calibration curve
Procedure:
- Prepare serial dilutions of the analyte in appropriate matrix covering the expected range
- Analyze each dilution in multiple replicates (n≥5) across independent runs
- For the lower limit of quantification (LLOQ): Identify the lowest concentration where CV% ≤20% and accuracy is within ±20% of nominal value
- For the upper limit of quantification (ULOQ): Identify the highest concentration where CV% ≤20% and accuracy is within ±20% of nominal value
- Confirm that the calibration curve demonstrates linearity (R² > 0.99) across the range from LLOQ to ULOQ
Documentation: Report the determined LLOQ and ULOQ values, along with supporting precision and accuracy data at these concentration levels. For qPCR assays, the limit of quantification represents "the lowest dilution that maintains linearity" between Ct values and template concentration [5].
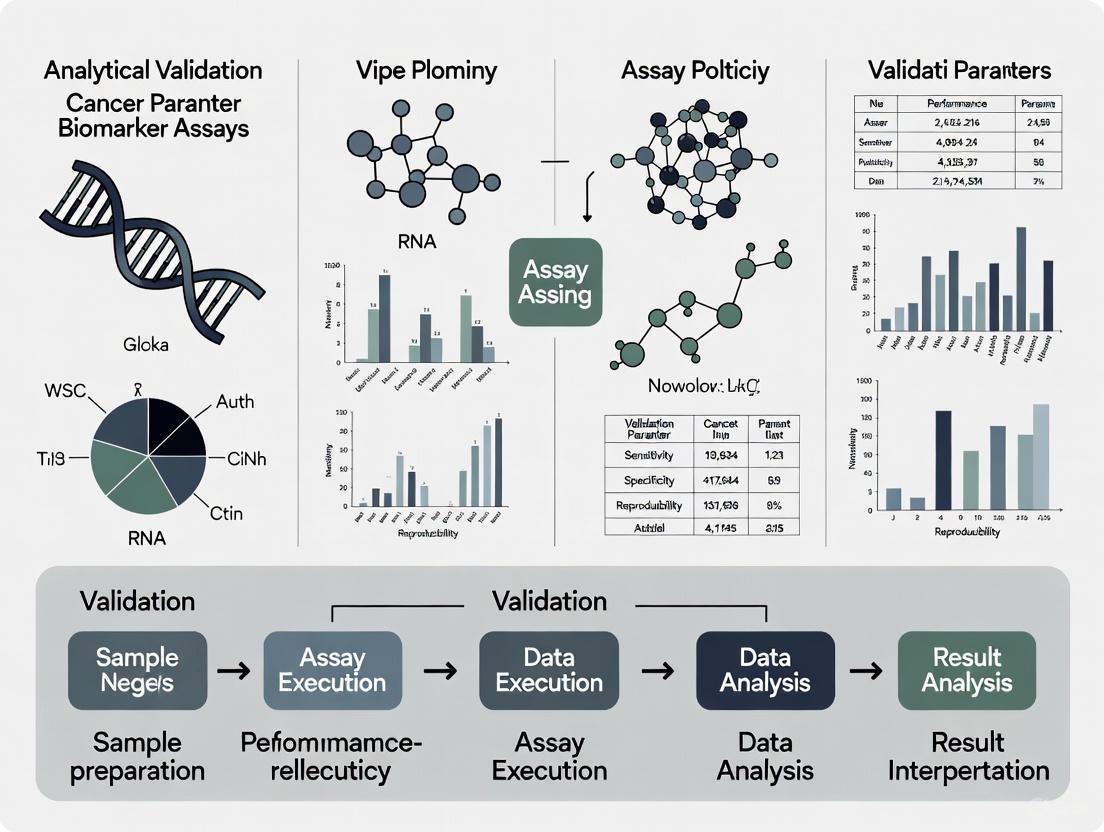
Visualizing the Analytical Validation Workflow
The following diagram illustrates the comprehensive workflow for analytical validation of biomarker assays, integrating multiple performance parameters into a systematic evaluation process:
Analytical Validation Parameter Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagents for Analytical Validation
| Reagent/Material | Function in Validation | Key Considerations |
|---|---|---|
| Reference Standards | Provide benchmark for accuracy assessment and calibration | Should be of highest available purity with documented provenance [2] |
| Quality Control Materials | Monitor assay performance across validation experiments | Should include low, medium, and high concentrations in appropriate matrix [6] |
| Biological Matrix | Evaluate assay performance in relevant sample type | Should match intended sample matrix (serum, plasma, tissue homogenate) [2] |
| Assay Diluents | Maintain analyte stability and matrix compatibility | Should be validated for absence of interference with assay performance [2] |
| Interference Compounds | Test assay selectivity against structurally similar compounds | Should include metabolites, related biomarkers, and common medications [2] |
Analytical validation represents the indispensable bridge between biomarker discovery and clinical utility, providing the evidentiary foundation that an assay generates reliable, reproducible data. As demonstrated through comparative analysis of major analytical platforms, each technology presents distinct advantages and validation considerations. Immunoassays offer practical implementation but may show significant inter-kit variability [6]. Mass spectrometry provides exceptional specificity but requires specialized expertise [1] [7]. Quantitative PCR delivers exceptional sensitivity for nucleic acid detection but demands rigorous statistical approaches for data analysis [8] [5].
The experimental protocols and frameworks presented herein provide researchers with practical guidance for implementing comprehensive analytical validation strategies. By adopting a fit-for-purpose approach that aligns validation rigor with intended application, the scientific community can advance robust biomarker assays along the development pipeline. Ultimately, rigorous analytical validation accelerates the translation of promising biomarkers from research discoveries to clinically impactful tools, strengthening the foundation of precision oncology and therapeutic development.
The development and integration of robust cancer biomarkers are fundamental to the advancement of precision oncology. However, the journey from biomarker discovery to clinical implementation is notoriously challenging, with an estimated success rate of only 0.1% for clinical translation [9]. A primary reason for this high attrition rate is not necessarily flawed science, but often poor choice of assay and inadequate method validation [10] [11]. To address this challenge, the fit-for-purpose paradigm has emerged as a practical and rigorous framework for biomarker method validation. This approach stipulates that the level of validation rigor should be commensurate with the intended use of the biomarker data and the associated regulatory requirements [10] [12] [13].
The core principle of fit-for-purpose validation is that the "purpose" or Context of Use (COU) is the primary driver for designing the validation process [12]. The COU defines the specific role of the biomarker in drug development or clinical decision-making, which can range from exploratory research to use as a companion diagnostic that dictates therapeutic choice. This paradigm fosters a flexible yet scientifically sound approach, allowing for iterative validation where the assay can be re-validated with increased rigor if its intended use evolves during the drug development process [12] [13]. Understanding this paradigm is essential for researchers, scientists, and drug development professionals aiming to efficiently translate biomarker science into clinically useful tools.
The Spectrum of Biomarker Applications and Corresponding Validation Requirements
Classifying Biomarker Assays and Their Context of Use
Biomarkers in oncology serve diverse functions, and their application dictates the necessary level of analytical validation. The American Association of Pharmaceutical Scientists (AAPS) and the US Clinical Ligand Society have identified five general classes of biomarker assays, each with distinct validation requirements [10]. A critical distinction lies between prognostic biomarkers, which provide information about the overall cancer course irrespective of therapy, and predictive biomarkers, which forecast response to a specific therapeutic intervention [14] [15]. Predictive biomarkers, such as EGFR mutations predicting response to gefitinib in lung cancer, are typically identified through an interaction test between treatment and biomarker in a randomized clinical trial [14].
The clinical application of a biomarker spans a wide spectrum. On one end are exploratory biomarkers used for internal decision-making in early research, which require a lower validation stringency. On the opposite end are companion diagnostics used to select patients for specific therapies, which demand the most rigorous validation, often culminating in FDA approval [12] [16]. For instance, the MI Cancer Seek test, an FDA-approved comprehensive molecular profiling assay, underwent extensive validation to achieve over 97% agreement with other FDA-approved diagnostics, a necessity for its role in guiding treatment [16]. The fit-for-purpose paradigm aligns the validation effort with this spectrum of application, ensuring resources are focused where they have the greatest impact on patient care and regulatory success.
A Framework for Fit-for-Purpose Validation
The process of fit-for-purpose biomarker method validation can be envisaged as progressing through discrete, iterative stages [10]. The initial stage involves defining the purpose and selecting the candidate assay, which is arguably the most critical step. Subsequent stages involve assembling reagents, writing the validation plan, the experimental phase of performance verification, and the final evaluation of fitness-for-purpose. The process continues with in-study validation to assess robustness in the clinical context and culminates in routine use with quality control monitoring. This phased approach, driven by continual improvement, ensures that the assay remains reliable for its intended application throughout its lifecycle.
The following diagram illustrates the logical relationship between a biomarker's clinical application and the corresponding validation rigor within the fit-for-purpose paradigm.
Experimental Protocols and Performance Standards for Biomarker Assays
Technical Validation Parameters Across Assay Categories
The specific performance parameters evaluated during biomarker method validation are directly determined by the assay's classification. Definitive quantitative assays, which use fully characterized reference standards to calculate absolute quantitative values, require the most comprehensive validation. In contrast, qualitative (categorical) assays, which rely on discrete scoring scales, have a different set of requirements [10]. The following table summarizes the consensus position on which key performance parameters should be investigated for each general class of biomarker assay.
Table 1: Key Performance Parameters for Biomarker Assay Validation by Category
| Performance Characteristic | Definitive Quantitative | Relative Quantitative | Quasi-Quantitative | Qualitative |
|---|---|---|---|---|
| Accuracy / Trueness (Bias) | + | + | ||
| Precision | + | + | + | |
| Reproducibility | + | |||
| Sensitivity | + (LLOQ) | + (LLOQ) | + | + |
| Specificity | + | + | + | + |
| Dilution Linearity | + | + | ||
| Parallelism | + | + | ||
| Assay Range | + (LLOQ–ULOQ) | + (LLOQ–ULOQ) | + |
Abbreviations: LLOQ = lower limit of quantitation; ULOQ = upper limit of quantitation [10].
For definitive quantitative assays (e.g., mass spectrometric analysis), the objective is to determine unknown concentrations as accurately as possible. Performance standards often adopt a default value of 25% for precision and accuracy (30% at the LLOQ), which is more flexible than the 15-20% standard for bioanalysis of small molecules [10]. A modern statistical approach endorsed by the Societe Francaise des Sciences et Techniques Pharmaceutiques (SFSTP) involves constructing an accuracy profile. This profile accounts for total error (bias and intermediate precision) and a pre-set acceptance limit, producing a β-expectation tolerance interval that visually displays the confidence interval for future measurements. This method allows researchers to determine the percentage of future values likely to fall within the pre-defined acceptance limit [10].
Experimental Protocol for a Definitive Quantitative Assay
A typical protocol for validating a definitive quantitative biomarker assay using the accuracy profile method involves the following steps [10]:
- Calibration Standards and Validation Samples (VS): Use 3-5 different concentrations of calibration standards and 3 different concentrations of VS (representing high, medium, and low points on the calibration curve).
- Replication: Run each calibration standard and VS in triplicate on 3 separate days to capture inter-day and intra-day variability.
- Data Analysis: Calculate the bias and intermediate precision for each concentration of the VS.
- Construct Accuracy Profile: Plot the β-expectation tolerance intervals (e.g., 95%) for each concentration level against the pre-defined acceptance limits.
- Evaluation: If the tolerance intervals for all concentrations fall entirely within the acceptance limits, the method is considered valid for its intended use. Parameters such as sensitivity, dynamic range, LLOQ, and ULOQ are derived directly from this profile.
For next-generation sequencing (NGS) assays like liquid biopsies, the experimental validation focuses on different parameters. The Hedera Profiling 2 (HP2) ctDNA test, for example, was validated using reference standards and a cohort of 137 clinical samples pre-characterized by orthogonal methods. In reference standards with variants at 0.5% allele frequency, the assay demonstrated a sensitivity of 96.92% and specificity of 99.67% for single-nucleotide variants and insertions/deletions, and 100% for fusions [17]. This highlights how the validation protocol is adapted to the technology and its intended clinical application.
Comparative Analysis of Validated Biomarker Assays
The fit-for-purpose paradigm is best understood through real-world examples. The following table provides a comparative analysis of several biomarker assays, highlighting how their validation strategies and performance data align with their specific Contexts of Use.
Table 2: Comparative Performance Data of Validated Biomarker Assays
| Assay Name | Technology / Platform | Intended Context of Use (COU) | Key Analytical Performance Data | Reference |
|---|---|---|---|---|
| Hedera Profiling 2 (HP2) | Hybrid capture NGS (Liquid Biopsy) | Detection of somatic alterations in ctDNA for precision oncology | SNVs/Indels (AF 0.5%): Sens: 96.92%, Spec: 99.67%Fusions: Sens: 100%Clinical Concordance: 94% for ESMO Level I variants | [17] |
| MI Cancer Seek | Whole Exome & Whole Transcriptome Sequencing | Comprehensive molecular profiling; FDA-approved companion diagnostic | Overall Concordance: >97% with other FDA-approved CDsMSI detection: Near-perfect accuracy in colorectal/endometrial cancerMinimal Input: 50 ng DNA from FFPE | [16] |
| Definitive Quantitative Assay (Theoretical) | Ligand Binding (e.g., ELISA) or Mass Spectrometry | Accurate concentration measurement for PK/PD or efficacy endpoints | Precision/Accuracy: ±25% (±30% at LLOQ)Validation Approach: Accuracy Profile with β-expectation tolerance intervals | [10] |
| OVA1 | Multi-marker panel (5 protein biomarkers) | Risk stratification for ovarian cancer; adjunct to clinical assessment | Purpose: Aids referral of high-risk women (Not a standalone screening tool) | [18] |
This comparison demonstrates that a decentralized liquid biopsy test (HP2) achieves high sensitivity and specificity for variant detection, suitable for molecular profiling. In contrast, an FDA-approved companion diagnostic (MI Cancer Seek) must demonstrate near-perfect concordance with existing standards. A general-purpose quantitative assay follows statistical validation principles, while a diagnostic aid (OVA1) is validated for a specific clinical triage role rather than standalone screening.
The Scientist's Toolkit: Essential Reagents and Materials
Successful biomarker development and validation rely on a foundation of critical reagents and materials. The following table details key components of the "Scientist's Toolkit," along with their essential functions and associated challenges.
Table 3: Key Research Reagent Solutions for Biomarker Assay Validation
| Tool / Reagent | Function in Development & Validation | Key Considerations & Challenges |
|---|---|---|
| Reference Standard / Calibrator | Serves as the basis for creating a calibration curve and assigning quantitative values to unknowns. | A major limitation is the lack of true reference standards for many biomarkers. Recombinant protein calibrators may differ from endogenous biomarkers, necessitating the use of endogenous quality controls for stability testing [12]. |
| Quality Control (QC) Samples | Used to monitor assay performance during both validation and routine sample analysis to ensure consistency and reliability. | Endogenous QCs are preferred over recombinant material for stability studies and in-study monitoring. During validation, QC results are evaluated against pre-set acceptance criteria (e.g., the 4:6:15 rule or confidence intervals) [10] [12]. |
| Validated Antibodies / Probes | For immunohistochemistry or ligand-binding assays, these are critical for the specific detection of the target biomarker. | Antibody sensitivity and specificity must be determined in the sample matrix (e.g., FFPE tissues), not just by Western blot. Optimal positive and negative controls (e.g., cell lines with/without target expression) are required for validation [11]. |
| Characterized Biospecimens | Used for assay development, validation, and as positive/negative controls. Include patient samples, cell lines, and synthetic reference standards. | Pre-analytical variables (collection, processing, storage) significantly impact results. Specimens should be well-characterized and relevant to the target population. Using "samples of convenience" is a major source of bias [12] [11] [9]. |
| Orthogonal Assay | A method based on different principles used to verify results from the primary biomarker assay. | Used in clinical validation to establish concordance. For example, the HP2 ctDNA assay was validated against pre-characterized clinical samples and other methods [17]. |
Navigating Pre-Analytical Variables and Workflow Considerations
A critical yet often overlooked aspect of biomarker validation is the management of pre-analytical variables. These are factors that affect the sample before it is analyzed and can have a profound impact on the integrity of the biomarker and the reliability of the results [12] [11]. For tissue-based biomarkers, such as those detected by immunohistochemistry, key pre-analytical variables include the time between tissue removal and fixation (warm ischemia), the type of fixative, and the length and conditions of fixation and paraffin-embedding [11]. For liquid biopsies, variables include the type of blood collection tube, time to plasma processing, and storage conditions [12].
These variables can be categorized as controllable or uncontrollable. Controllable variables, such as the matrix, specimen collection, processing, and transport procedures, should be standardized through detailed SOPs. For example, the choice of anticoagulant in blood collection tubes can affect the measurement of certain biomarkers like VEGF [12]. Uncontrollable variables, such as patient gender, age, or co-morbidities, cannot be standardized but must be documented and accounted for during data analysis and study design [12]. The following workflow diagram outlines key pre-analytical and analytical steps where these variables must be managed to ensure data integrity.
The fit-for-purpose paradigm provides a robust, practical, and logical framework for the validation of cancer biomarker assays. By tightly aligning the rigor of analytical validation with the biomarker's Context of Use, from exploratory research to companion diagnostics, this approach ensures scientific integrity while optimizing resource allocation. The successful implementation of this paradigm requires a deep understanding of the clinical and regulatory landscape, meticulous management of pre-analytical variables, and the application of appropriate statistical methods for performance verification. As precision oncology continues to evolve, driven by technologies like NGS and liquid biopsy, adherence to the principles of fit-for-purpose validation will be paramount in translating promising biomarkers from the research bench to the clinical bedside, ultimately improving patient care and outcomes.
The development and validation of biomarker assays are fundamental to advancing precision medicine, particularly in oncology. These assays provide critical data on disease detection, prognosis, and therapeutic response, enabling more personalized treatment approaches. Classification of these assays into definitive quantitative, relative quantitative, quasi-quantitative, and qualitative categories is essential for appropriate application in both research and clinical decision-making. This systematic framework ensures that the analytical performance of an assay aligns with its intended Context of Use (COU), a concise description of a biomarker's specified application in drug development [19].
The validation requirements for biomarker assays differ significantly from those for traditional pharmacokinetic (PK) assays, necessitating a fit-for-purpose approach that considers the specific biological and technical challenges of measuring endogenous biomarkers [19]. Unlike PK assays that measure well-characterized drug compounds, biomarker assays often lack reference materials identical to the endogenous analyte and must account for substantial biological variability and pre-analytical factors that can influence results [20] [19]. This comparison guide examines the performance characteristics, experimental methodologies, and applications of different biomarker assay classes to inform their appropriate selection and validation in cancer research.
Biomarker Assay Classification Framework
Biomarker assays can be categorized based on their quantitative output and the nature of the measurements they provide. This classification system ranges from assays that deliver exact concentration values to those that provide simple categorical results, with each category serving distinct purposes in biomarker development and application.
Categories of Biomarker Assays
Definitive Quantitative Assays: These assays measure the absolute quantity of an analyte using a calibration curve with reference standards that are structurally identical to the endogenous biomarker. They provide exact numerical concentrations in appropriate units (e.g., ng/mL, nM) and require the highest level of analytical validation [19].
Relative Quantitative Assays: These assays measure the quantity of an analyte relative to a reference material that may not be structurally identical to the endogenous biomarker. While they provide numerical results, these values are relative rather than absolute and require careful interpretation within the assay's specific parameters [19].
Quasi-Quantitative Assays: These assays provide approximate numerical estimates based on non-calibrated measurements or indirect relationships. The results are typically reported in arbitrary units rather than absolute concentrations and have more limited precision compared to fully quantitative methods [19].
Qualitative Assays: These assays classify samples into discrete categories (e.g., positive/negative, mutant/wild-type) without providing numerical values. They focus on determining the presence or absence of specific biomarkers or characteristics rather than measuring quantities [19] [21].
Table 1: Biomarker Assay Classification Framework
| Assay Category | Measurement Output | Reference Standard | Data Interpretation | Common Applications |
|---|---|---|---|---|
| Definitive Quantitative | Exact concentration with units | Identical to endogenous analyte | Direct quantitative comparison | Pharmacodynamic biomarkers, diagnostic applications |
| Relative Quantitative | Relative numerical value | Similar but not identical to analyte | Relative comparison between samples | Exploratory research, target engagement |
| Quasi-Quantitative | Approximate numerical value | Non-calibrated or indirect reference | Trend analysis within study | Screening assays, prioritization |
| Qualitative | Categorical classification | Qualitative controls | Binary or categorical assessment | Companion diagnostics, patient stratification |
Biomarker Assay Selection Workflow
Experimental Protocols for Biomarker Assay Comparison
Rigorous experimental protocols are essential for comparing biomarker assay performance across different categories. These protocols evaluate analytical parameters such as precision, accuracy, sensitivity, and reproducibility under conditions that mimic real-world applications.
Reference Sample Design for Assay Benchmarking
The experimental design for comparing biomarker assays requires carefully characterized reference materials that represent the biological and technical challenges encountered in actual study samples. A community-wide benchmarking study for DNA methylation assays utilized 32 reference samples including matched tumor/normal tissue pairs, drug-treated cell lines, titration series, and matched fresh-frozen/FFPE sample pairs to simulate diverse clinical scenarios [21]. This approach allows comprehensive evaluation of assay performance across different sample types and conditions relevant to cancer biomarker development.
For quantitative assays, establishing a calibration curve with appropriate reference standards is fundamental. However, for many biomarker assays, particularly those measuring protein biomarkers, reference materials may not be structurally identical to the endogenous analyte, necessitating additional validation steps such as parallelism assessments to demonstrate similarity between calibrators and endogenous analytes [19]. The experimental protocol must also account for pre-analytical variables including sample collection tubes, processing time, centrifugation conditions, and storage duration, as these factors contribute significantly to measurement variability [20].
Protocol for Quantitative Assay Validation
A standardized protocol for validating quantitative biomarker assays should include the following key steps:
Reference Material Characterization: Evaluate the similarity between reference standards and endogenous biomarkers through parallelism experiments where serial dilutions of biological samples are compared to the calibration curve [19].
Precision Profile Assessment: Determine within-run (repeatability) and between-run (intermediate precision) variability using quality control samples at multiple concentrations across different days [20].
Linearity of Dilution: Demonstrate that samples can be diluted to within the assay's quantitative range while maintaining proportional results [19].
Stability Studies: Evaluate analyte stability under various storage conditions (freeze-thaw cycles, benchtop stability, long-term storage) using actual study samples rather than only spiked standards [19].
Specificity and Selectivity: Assess interference from related molecules, matrix components, and common medications using samples from healthy donors and the target population [20].
Table 2: Key Experimental Parameters for Biomarker Assay Validation
| Validation Parameter | Definitive Quantitative | Relative Quantitative | Quasi-Quantitative | Qualitative |
|---|---|---|---|---|
| Accuracy/Recovery | 85-115% with spike-recovery | Relative accuracy assessment | Not required | Not applicable |
| Precision (CV) | <15-20% total CV | <20-25% total CV | <30% total CV | Positive/negative agreement |
| Calibration Curve | Required with authentic standard | Required with similar standard | Optional | Not applicable |
| Parallelism Assessment | Critical for endogenous analyte | Critical for endogenous analyte | Recommended | Not applicable |
| Stability | Comprehensive evaluation | Limited evaluation | Minimal evaluation | Sample integrity only |
| Reference Range | Established with population data | Study-specific controls | Not required | Cut-off determination |
Performance Comparison of Biomarker Assay Categories
Direct comparison of different assay categories reveals distinct performance characteristics that influence their suitability for specific applications in cancer biomarker research.
Quantitative Performance Metrics
In a comprehensive comparison of DNA methylation technologies, quantitative assays including amplicon bisulfite sequencing (AmpliconBS) and bisulfite pyrosequencing (Pyroseq) demonstrated superior all-around performance for biomarker development, providing precise measurements across the dynamic range with single-CpG resolution [21]. These methods showed high sensitivity in detecting methylation differences in low-input samples and effectively discriminated between cell types, making them suitable for both discovery and clinical applications.
A study comparing quantitative and qualitative MRI metrics in primary sclerosing cholangitis found that quantitative measurements of liver stiffness (determined by magnetic resonance elastography) and spleen volume had perfect and near-perfect agreement (intraclass correlation coefficients of 1.00 and 0.9996, respectively), while qualitative ANALI scores determined by radiologists showed only moderate inter-rater agreement (kappa = 0.42-0.57) [22]. Furthermore, as a continuous variable, liver stiffness was the single best predictor of hepatic decompensation (concordance score = 0.90), demonstrating the prognostic advantage of quantitative measurements in clinical applications.
Reproducibility Across Assay Categories
Reproducibility varies significantly across assay categories, with definitive quantitative assays generally demonstrating the highest inter-laboratory consistency when properly validated. In the DNA methylation benchmarking study, most quantitative assays showed good agreement across different laboratories, though some technology-specific differences were observed [21]. The study highlighted that assay sensitivity can be influenced by CpG density and genomic context, with some methods performing better in specific genomic regions.
For qualitative assays, performance is typically measured by positive and negative agreement rather than traditional precision metrics. These assays often demonstrate high reproducibility for categorical calls but may lack the granularity needed for monitoring subtle changes in biomarker levels over time [21]. The implementation of standardized protocols, automated procedures, and appropriate quality controls can significantly improve reproducibility across all assay categories [20].
Technical Considerations for Biomarker Assay Implementation
Successful implementation of biomarker assays in cancer research requires careful attention to technical factors that influence data quality and interpretation.
Pre-analytical Variables
Pre-analytical factors represent a significant source of variability in biomarker measurements, potentially accounting for up to 75% of errors in laboratory testing [20]. These factors include sample collection methods, choice of collection tubes, processing time, centrifugation conditions, and storage parameters. For example, the type of blood collection tube and its components (including gel activators) can markedly affect results, as can inadequate fill volume compromising sample-to-anticoagulant ratios [20].
Biological variability must also be considered during assay implementation. Factors such as age, sex, diet, time of day, comorbidities, medications, and menstrual cycle stage can all influence biomarker levels [20]. Understanding these sources of variability is essential for establishing appropriate reference ranges and interpreting results in the context of individual patient factors.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biomarker Assay Development
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| Reference Standards | Calibration and quality control | May differ from endogenous analyte in structure, folding, glycosylation [19] |
| Quality Control Materials | Monitoring assay performance | Should mimic study samples; may use pooled patient samples [20] |
| Collection Tubes | Sample acquisition and stabilization | Tube type and additives can affect results; consistency is critical [20] |
| Assay Antibodies | Detection and capture reagents | Specificity must be demonstrated; up to 50% of commercial antibodies may fail [20] |
| Matrix Materials | Diluent and background assessment | Should match study sample matrix; assess interference [19] |
| Enzymes and Conversion Reagents | Sample processing and modification | Batch-to-batch variability must be monitored [21] |
Regulatory and Validation Considerations
The fit-for-purpose approach to biomarker assay validation recognizes that the extent of validation should be appropriate for the intended context of use [19]. The 2025 FDA Bioanalytical Method Validation for Biomarkers guidance acknowledges that biomarker assays differ fundamentally from PK assays and require different validation strategies [19]. Unlike PK assays that typically use a fully characterized reference standard identical to the drug analyte, biomarker assays often rely on reference materials that may differ from the endogenous analyte in critical characteristics such as molecular structure, folding, truncation, and post-translational modifications [19].
This fundamental difference means that validation parameters for biomarker assays must focus on demonstrating performance with endogenous analytes rather than solely through spike-recovery experiments. Key assessments should include parallelism testing to evaluate similarity between calibrators and endogenous biomarkers, and use of endogenous quality controls that more adequately characterize assay performance with actual study samples [19].
The classification of biomarker assays into definitive quantitative, relative quantitative, quasi-quantitative, and qualitative categories provides a critical framework for selecting appropriate methodologies for specific research and clinical applications in oncology. Quantitative assays generally offer superior performance for monitoring disease progression and treatment response, while qualitative assays provide practical solutions for patient stratification and companion diagnostics. The emerging regulatory consensus emphasizes a fit-for-purpose validation approach that addresses the unique challenges of biomarker measurements, particularly the frequent lack of reference materials identical to endogenous analytes. As cancer biomarker research continues to evolve, this classification system and the associated validation strategies will support the development of robust, reproducible assays that generate reliable data for precision medicine applications.
Regulatory Landscape and Key Guidelines for Clinical Trial Assays
The regulatory landscape for clinical trial assays is dynamic, with recent updates emphasizing fit-for-purpose validation, the integration of advanced technologies like artificial intelligence (AI), and flexible approaches for novel biomarker development. These assays, which are critical for measuring biomarkers in drug development, are subject to guidance from various global health authorities, including the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the International Council for Harmonisation (ICH). A foundational understanding of Context of Use (COU) is paramount, as it defines the specific purpose an assay is intended to serve in the drug development process and directly dictates the extent and nature of its validation [19]. Unlike pharmacokinetic (PK) assays that measure drug concentrations, biomarker assays present unique challenges, often lacking a fully characterized reference standard identical to the endogenous analyte, which necessitates different validation strategies [19].
Recent regulatory activity has been significant. The FDA's finalization of the ICH E6(R3) guideline for Good Clinical Practice introduces more flexible, risk-based approaches to clinical trial conduct [23]. Furthermore, the start of 2025 saw the FDA release the Bioanalytical Method Validation for Biomarkers (BMVB) guidance, a pivotal document that officially recognizes the distinct nature of biomarker assay validation while creating some ambiguity by referencing ICH M10, a guideline developed for PK assays [24] [19]. Concurrently, professional societies are stepping forward to provide specialized guidance, such as the European Society for Medical Oncology's (ESMO) first framework for AI-based biomarkers in cancer, which categorizes these novel tools based on risk and required evidence levels [25]. These developments collectively shape the requirements for robust analytical validation of clinical trial assays, particularly in complex fields like cancer biomarker research.
Major Global Regulatory Guidelines
Navigating the requirements of various regulatory bodies is essential for the successful development and validation of clinical trial assays. The following table summarizes the key recent guidelines and their implications for assay development.
Table 1: Key Global Regulatory Guidelines for Clinical Trial Assays (2024-2025)
| Health Authority | Guideline Name | Status & Date | Key Focus & Impact on Assays |
|---|---|---|---|
| FDA (U.S.) | ICH E6(R3): Good Clinical Practice | Final (Sep 2025) [23] | Introduces flexible, risk-based approaches for trial conduct, impacting how assays are integrated and monitored within clinical trials. |
| FDA (U.S.) | Bioanalytical Method Validation for Biomarkers (BMVB) | Final (Jan 2025) [24] [19] | Recognizes differences from PK assays; recommends a fit-for-purpose approach and ICH M10 as a starting point, but requires justification for deviations. |
| EMA (EU) | Reflection Paper on Patient Experience Data | Draft (Sep 2025) [23] | Encourages inclusion of patient-reported data in medicine development, which may influence the development of companion diagnostics. |
| ESMO | Basic Requirements for AI-based Biomarkers in Oncology (EBAI) | Published (Nov 2025) [25] | Provides a validation framework for AI biomarkers, categorizing them by risk (Classes A-C) and defining required evidence for clinical use. |
| Friends of Cancer Research | Analysis on CDx for Rare Biomarkers | Published (2025) [26] | Characterizes regulatory flexibilities, such as use of alternative sample sources, for validating companion diagnostics for rare cancer biomarkers. |
Detailed Analysis of FDA Biomarker Guidance (BMVB)
The FDA's BMVB guidance, finalized in January 2025, marks a critical step by formally distinguishing biomarker validation from PK assay validation [19]. This guidance officially retires the relevant section of the 2018 FDA BMV guidance and establishes that a "fit-for-purpose" approach should be used to determine the appropriate extent of method validation [24] [19]. However, it has also sparked discussion within the bioanalytical community because it directs sponsors to ICH M10 as a starting point, despite ICH M10 explicitly stating it does not apply to biomarkers [24].
This creates a nuanced position for sponsors: while the principles of ICH M10 (e.g., assessing accuracy, precision, sensitivity) are relevant, the techniques to evaluate them must be adapted. For instance, unlike PK assays that use a well-defined drug reference standard, biomarker assays often rely on surrogate materials (e.g., recombinant proteins) that may not perfectly match the endogenous analyte's structure or modifications [19]. Therefore, key validation parameters like accuracy and parallelism must be assessed using samples containing the endogenous biomarker, rather than solely through spike-recovery of the reference standard [19]. The guidance ultimately requires sponsors to scientifically justify their chosen validation approach, particularly when it differs from the ICH M10 framework, in their method validation reports [19].
Emerging Guidance for AI-Based Biomarkers
The ESMO EBAI framework addresses the growing field of AI-based biomarkers, which use complex algorithms to analyze multidimensional data (e.g., histology slides) to predict disease features or treatment response [25]. This guidance establishes three risk-based categories:
- Class A (Low Risk): Automates tedious tasks (e.g., cell counting).
- Class B (Medium Risk): Acts as a surrogate biomarker for screening or enrichment within a population. It requires strong evidence of high sensitivity and specificity.
- Class C (High Risk): Comprises novel biomarkers without an established counterpart. This class is subdivided into C1 (prognostic) and C2 (predictive), with C2 requiring the highest level of evidence, ideally from randomized clinical trials [25].
For all classes, the framework emphasizes clarity on the ground truth (the gold standard for comparison), transparent reporting of performance against that standard, and demonstration of generalisability across different clinical settings and data sources [25].
Experimental Protocols and Validation Parameters
A robust analytical validation is the cornerstone of any clinical trial assay, ensuring the data generated is reliable and fit for its intended purpose. The specific protocols and acceptance criteria are driven by the assay's Context of Use (COU).
Core Validation Parameters and Methodologies
The following table outlines standard experimental protocols for key analytical validation parameters, drawing from established clinical and laboratory standards.
Table 2: Key Analytical Validation Parameters and Experimental Protocols
| Validation Parameter | Experimental Protocol Summary | Key Acceptance Criteria |
|---|---|---|
| Limit of Blank (LoB) & Limit of Detection (LoD) | Follows CLSI EP17-A2. Test blank and low-concentration samples over multiple days (e.g., 30 measurements each) to determine the lowest analyte level distinguishable from blank and reliably detected, respectively [27]. | LoD is typically set at a concentration where the signal-to-noise ratio is significantly distinguished. |
| Limit of Quantitation (LoQ) | Follows CLSI EP17-A2. Test serially diluted samples to find the lowest concentration measurable with defined precision (e.g., ≤20% coefficient of variation) [27]. | CV ≤ 20% at the LoQ concentration [27]. |
| Precision | Analyze multiple replicates of quality control samples at various concentrations (low, medium, high) within and across multiple runs/days [27]. | Pre-defined CV targets based on COU (e.g., <10% CV for high-sensitivity troponin at the 99th percentile URL) [27]. |
| Analytical Measurement Range (AMR) | Follows CLSI EP6-A. Perform linearity testing by serially diluting a high-concentration sample and plotting measured vs. expected values [27]. | High coefficient of determination (R²) demonstrating linearity across the claimed range. |
| Parallelism | Assessed by serially diluting patient samples containing the endogenous biomarker and comparing the dose-response curve to that of the calibrator [19]. | Demonstration that the diluted patient samples behave similarly to the standard curve, indicating no matrix interference. |
The workflow below illustrates the logical relationship and sequence of these key validation experiments.
Assessing Clinical Performance
Once analytical validation is established, clinical performance must be assessed. This involves determining the assay's diagnostic sensitivity, specificity, and predictive values in a relevant patient population. A study on high-sensitivity troponin I (hs-cTnI) assays provides a template for such an evaluation, comparing strategies like the Limit of Detection (LoD) strategy (offering 100% sensitivity but low positive predictive value) and the more balanced 0/2-hour algorithm [27]. For companion diagnostics, especially for rare biomarkers, regulatory flexibilities may be employed. A recent analysis of CDx for non-small cell lung cancer highlighted the use of alternative sample sources and bridging studies with smaller sample sizes to overcome the challenge of limited clinical specimens for the rarest biomarkers [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful development and validation of a clinical trial assay rely on a suite of critical reagents and materials. The selection and characterization of these components are vital for ensuring assay robustness and reproducibility.
Table 3: Essential Reagents and Materials for Biomarker Assay Development
| Tool / Reagent | Function & Importance |
|---|---|
| Reference Standard / Calibrator | Used to create the standard curve for quantitation. A major challenge is that these are often recombinant proteins or synthetic peptides that may not be identical to the endogenous biomarker, necessitating parallelism testing [19]. |
| Quality Control (QC) Samples | Materials with known analyte concentrations (often in a surrogate matrix) used to monitor assay precision and accuracy within and across runs [27]. |
| Characterized Biobanked Samples | Well-annotated clinical samples from patients and healthy donors. Crucial for determining clinical cut-offs, assessing specificity, and performing parallelism experiments with the endogenous biomarker [19] [27]. |
| Surrogate Matrix | A modified or artificial matrix (e.g., buffer, stripped serum) used to prepare calibrators and QCs when the native biological matrix interferes with the assay. Performance must be bridged to the native matrix [19]. |
| Critical Assay Reagents | Antibodies, primers, probes, enzymes, and other core components that define the assay's specificity and sensitivity. These require rigorous lot-to-lot testing [27]. |
Regulatory Pathways and Strategic Considerations
Navigating the regulatory landscape requires a strategic approach from assay developers and sponsors. The following diagram outlines a high-level decision-making pathway for validating a clinical trial assay, incorporating key regulatory considerations.
Key Strategic Implications
- Early Regulatory Interaction is Critical: For assays where the data will support a regulatory decision for drug approval or labeling, early consultation with agencies is strongly recommended. This is especially important for novel technologies or when validation presents unique challenges [19].
- Embrace Fit-for-Purpose and Flexibility: The
fit-for-purposeprinciple is now enshrined in FDA guidance [19]. Furthermore, regulatory flexibilities exist for challenging situations, such as developing companion diagnostics for rare biomarkers, where alternative sample types and smaller bridging studies may be acceptable [26]. - Discontinue "Qualification" in Favor of "Validation": To align with FDA terminology and avoid confusion with the separate process of "biomarker qualification," the term
"fit-for-purpose validation"or simply"validation"should be used for assays, discontinuing the use of "qualification" in this context [19].
The regulatory landscape for clinical trial assays in 2025 is characterized by a welcome recognition of their unique challenges, as seen in the FDA's new BMVB guidance and ESMO's framework for AI-based biomarkers. The core principles of fit-for-purpose validation, context of use, and scientific justification are more critical than ever. Success in this environment depends on a deep understanding of both the technical requirements for robust analytical validation and the strategic regulatory pathways available. As the field advances with more complex biomarkers and AI-driven tools, ongoing dialogue between industry and regulators will be essential to maintain scientific rigor while fostering innovation that ultimately benefits patient care.
Technology in Practice: Platforms and Workflows for Biomarker Quantification
Targeted proteomics represents a cornerstone of modern precision oncology, providing the quantitative accuracy and reproducibility essential for analytical validation of cancer biomarker assays. Unlike discovery-oriented "shotgun" approaches, targeted proteomics employs mass spectrometry to precisely monitor a pre-defined set of peptides, enabling highly sensitive and specific quantification of protein biomarkers. This focused strategy is indispensable for verifying biomarker candidates in complex biological matrices, a critical step in translating potential markers from research into clinical applications. The workflow's robustness hinges on a meticulously optimized sequence of steps—from sample digestion to liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis—each requiring stringent control to ensure data quality and reproducibility for drug development and clinical research [28].
This guide objectively compares the core methodologies and technological alternatives within the targeted proteomics workflow, framing them within the context of analytical validation for cancer biomarkers. We present supporting experimental data and detailed protocols to help researchers and scientists select the optimal strategies for their specific biomarker validation challenges.
Core Workflow of Targeted Proteomics
The foundational workflow of targeted proteomics is designed to transform complex protein samples into analytically tractable peptide measurements with high precision. The following diagram illustrates the logical sequence and key decision points in this multi-stage process.
Sample Preparation and Protein Digestion
The initial phase of sample preparation is critical, as it directly impacts the quality and reproducibility of all downstream data. Efficient sample preparation begins with protein extraction and solubilization from biological materials (e.g., cell cultures, tissue biopsies, or biofluids) using denaturing buffers, often containing urea or RIPA buffer, to ensure full protein accessibility [28]. For formalin-fixed paraffin-embedded (FFPE) tissues—a common clinical resource—novel AFA (Adaptive Focused Acoustics) technology has been shown to improve protein extraction efficiency and reproducibility compared to traditional bead-beating methods, mitigating issues related to variable yield and sample degradation [29].
Following extraction, proteins undergo reduction to cleave disulfide bonds (typically using dithiothreitol - DTT) and alkylation (e.g., with iodoacetamide) to prevent reformation, linearizing the proteins for enzymatic cleavage [28]. The core of sample preparation is protein digestion, most commonly using the serine protease trypsin, which cleaves peptide bonds C-terminal to lysine and arginine residues. This specificity yields peptides with predictable masses and charge states, simplifying subsequent LC-MS/MS analysis. Digestion protocols must be optimized to balance completeness (to avoid missed cleavages) with preventing over-digestion artifacts, often using controlled temperature and reaction time [28]. For complex or membrane protein samples, alternative enzymes like Lys-C may be employed to improve digestion efficiency [28].
Liquid Chromatography (LC) Separation
Following digestion, the complex peptide mixture must be separated before mass spectrometry analysis to reduce sample complexity and mitigate ion suppression effects. Liquid Chromatography is the workhorse for this separation, with reversed-phase chromatography being the most prevalent mode. Peptides are separated based on their hydrophobicity as an organic solvent gradient (typically acetonitrile) elutes them from a C18-coated column [28].
The choice of chromatographic scale involves a critical trade-off between sensitivity, throughput, and robustness, directly impacting assay performance in validation settings. The table below compares the performance characteristics of different LC flow rates, based on empirical benchmarking studies [30].
Table 1: Comparison of LC Flow Rates for Proteomic Analysis
| Flow Rate Scale | Typical Flow Rate | Column i.d. | Key Strengths | Ideal Application in Biomarker Validation |
|---|---|---|---|---|
| Nanoflow (nLC) | < 1 µL/min | 75-100 µm | Exceptional sensitivity, low sample consumption | Verification from sample-limited sources (e.g., microdissected tissue) |
| Capillary (capLC) | 1.5-5 µL/min | 150-300 µm | High sensitivity, excellent robustness & throughput | High-throughput candidate verification in large cohorts |
| Microflow (μLC) | 50-200 µL/min | 1-2.1 mm | High throughput & extreme robustness | Robust, reproducible quantification in clinical cohorts |
Recent studies demonstrate that capillary-flow LC (capLC) operating around 1.5 µL/min provides a robust and sensitive alternative, identifying approximately 2,600 proteins in 30-minute gradients and offering an optimal balance for high-throughput clinical samples [30]. Conversely, microflow LC (μLC) systems, running at higher flow rates (e.g., 50-200 µL/min), excel in throughput and robustness, making them suitable for analyzing large patient cohorts where thousands of samples must be processed with minimal downtime [30].
Mass Spectrometry Analysis: SRM and PRM
The mass spectrometry component is where targeted quantification occurs. In a typical LC-MS/MS experiment, peptides eluting from the LC column are ionized via electrospray ionization (ESI) and introduced into the mass spectrometer [28]. The instrument first performs a survey scan (MS1) to measure the mass-to-charge (m/z) ratios of intact peptide ions [28].
For targeted proteomics, two primary data acquisition techniques are employed:
- Selected Reaction Monitoring (SRM): This gold-standard method, often performed on triple quadrupole instruments, specifically monitors predefined precursor ion → fragment ion transitions for each target peptide. It offers exceptional sensitivity, dynamic range, and precision for quantifying a limited set of targets.
- Parallel Reaction Monitoring (PRM): A high-resolution targeted method performed on Orbitrap or time-of-flight (TOF) instruments. PRM acquires all fragment ions of a selected precursor simultaneously, providing high specificity and allowing retrospective data analysis without pre-defining specific transitions [28].
Both SRM and PRM provide superior quantitative accuracy for validating candidate biomarkers compared to discovery-oriented methods, as they focus the instrument's duty cycle on the most relevant ions, resulting in improved sensitivity, lower limits of quantification, and higher reproducibility.
Essential Research Reagents and Materials
The successful implementation of a targeted proteomics workflow depends on a suite of specialized reagents and materials. The following table details key components and their functions within the experimental pipeline.
Table 2: Research Reagent Solutions for Targeted Proteomics
| Item/Category | Specific Examples | Function in Workflow |
|---|---|---|
| Digestion Enzyme | Trypsin, Lys-C | Site-specific protein cleavage into analyzable peptides [28]. |
| Denaturant | Urea, RIPA Buffer | Unfolds proteins to make cleavage sites accessible [28]. |
| Reducing Agent | Dithiothreitol (DTT), Tris(2-carboxyethyl)phosphine (TCEP) | Breaks disulfide bonds to linearize proteins [28]. |
| Alkylating Agent | Iodoacetamide (IAA), Chloroacetamide (CAA) | Caps free thiols to prevent reformation of disulfide bonds [28]. |
| LC Column | C18 reversed-phase columns (varying i.d.) | Separates peptides based on hydrophobicity prior to MS injection [30]. |
| Internal Standards | Stable Isotope-Labeled Standard (SIS) Peptides | Enables precise quantification by correcting for variability in sample prep and MS ionization [31]. |
| Solid-Phase Extraction | C18 cartridges or tips | Desalts and concentrates peptide samples post-digestion [28]. |
Among these, stable isotope-labeled standard (SIS) peptides are particularly crucial for analytical validation. These synthetic peptides, identical to target peptides but with a heavy isotope label, are spiked into the sample at a known concentration before digestion. They correct for sample preparation losses and ionization variability, enabling highly accurate and precise quantification—a non-negotiable requirement for biomarker assay validation [31].
Analytical Validation in Cancer Biomarker Research
For a cancer biomarker assay to achieve clinical utility, it must undergo rigorous analytical validation to establish its performance characteristics. This process, guided by frameworks from organizations like the FDA and the NCI's Diagnostics Evaluation Branch (DEB), assesses key metrics including sensitivity, specificity, precision, and reproducibility [15]. The targeted proteomics workflow is uniquely positioned to meet these demands.
Validation begins with defining the assay's intended use and then systematically testing its performance. Key parameters include:
- Sensitivity and Specificity: Determining the lowest concentration of the biomarker that can be reliably detected (Limit of Detection, LOD) and quantified (Limit of Quantification, LOQ) with high specificity against a complex background [32].
- Precision and Reproducibility: Evaluating the assay's coefficient of variation (CV) across repeated measurements within runs (intra-assay) and between different runs, operators, and laboratories (inter-assay) [32].
- Linearity and Dynamic Range: Establishing that the quantitative response is linear across the expected physiological range of the biomarker [30].
The NCI's DEB supports this process through initiatives like the UH2/UH3 cooperative agreements, which fund projects focused on the analytical and clinical validation of biomarkers and assays for use in NCI-supported cancer trials [15]. This underscores the critical role of standardized, validated assays in translating proteomic discoveries into tools that can guide treatment decisions, such as companion diagnostics that link specific protein biomarkers to FDA-approved targeted therapies [32].
Mass spectrometry-based targeted proteomics, with its robust workflows from digestion to LC-MS/MS analysis, provides an indispensable platform for the analytical validation of cancer biomarker assays. The strategic selection of methodologies—from sample preparation techniques to the choice between LC flow rates and MS acquisition modes—directly impacts the sensitivity, throughput, and ultimate success of biomarker verification.
As the field advances, the integration of more robust capillary-flow LC systems, highly specific PRM acquisitions, and the mandatory use of stable isotope standards is setting a new standard for precision and reproducibility. By adhering to these rigorously validated workflows, researchers and drug development professionals can confidently generate the high-quality data necessary to bridge the gap between promising biomarker candidates and clinically actionable diagnostic tools, ultimately advancing the goals of precision oncology.
The analytical validation of cancer biomarker assays represents a critical frontier in molecular pathology and diagnostic research. For researchers and drug development professionals, selecting the appropriate immunoassay platform is not merely a technical choice but a fundamental decision that directly impacts data reliability, clinical translation, and therapeutic development. Immunoassay technologies have evolved substantially from their origins in radioimmunoassay to encompass a diverse toolkit for protein detection and quantification [33]. Within cancer biomarker research, the validation of assays requires careful consideration of multiple performance parameters including sensitivity, specificity, reproducibility, and analytical context.
This guide provides a comprehensive comparison of three major immunoassay platforms—ELISA, Immunohistochemistry (IHC), and emerging techniques—focusing on their technical principles, experimental methodologies, performance characteristics, and applications in cancer biomarker validation. Understanding the comparative strengths and limitations of each platform enables researchers to make informed decisions that align with their specific experimental requirements, whether for biomarker discovery, clinical validation, or therapeutic monitoring.
Technical Principles and Methodologies
Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA operates on the principle of detecting antigen-antibody interactions through enzyme-linked conjugates and chromogenic substrates that generate measurable color changes [34]. The core components include a solid-phase matrix (typically 96-well microplates), enzyme-labeled antibodies (conjugates), specific substrates, and wash buffers to remove unbound components [34]. The most common enzymes used for labeling are horseradish peroxidase (HRP) and alkaline phosphatase (AP), which react with substrates like tetramethylbenzidine (TMB) to produce quantifiable color signals measured spectrophotometrically at 450nm [34].
Several ELISA formats have been developed for different applications:
- Direct ELISA: Uses a single enzyme-linked antibody directly binding the antigen, offering simplicity but potentially lower sensitivity [33].
- Indirect ELISA: Employs an unlabeled primary antibody followed by an enzyme-linked secondary antibody, enhancing sensitivity through signal amplification [34].
- Sandwich ELISA: Requires two antibodies binding to different epitopes of the target antigen, offering high specificity and sensitivity, though it requires larger antigens with multiple epitopes [33].
- Competitive ELISA: Based on competition between sample antigens and labeled analogs for limited antibody binding sites, making it ideal for detecting small molecules or low-abundance targets [33].
Immunohistochemistry (IHC)
IHC combines immunological, histological, and biochemical principles to detect specific antigens within tissue sections while preserving morphological context [35]. The technique relies on monoclonal or polyclonal antibodies tagged with labels such as fluorescent compounds or enzymes that selectively bind to target antigens in biological tissues [35]. IHC can be performed through direct methods (labeled primary antibodies) or indirect methods (unlabeled primary antibodies with labeled secondary antibodies), with the latter providing enhanced sensitivity through signal amplification [35].
The critical distinction of IHC lies in its ability to provide spatial information about protein expression and distribution within the tissue architecture, allowing researchers to correlate biomarker expression with specific cell types, subcellular localization, and pathological features [36]. This spatial context is particularly valuable in cancer research for understanding tumor heterogeneity, tumor-microenvironment interactions, and compartment-specific biomarker expression.
Emerging and Hybrid Techniques
Innovative approaches are continually expanding the immunoassay toolbox:
- Histo-ELISA: This hybrid technique combines elements of conventional ELISA and standard ABC immunostaining to enable both quantification of target proteins and observation of related morphological changes concurrently [37]. It substitutes DAB with TMB peroxidase substrate and uses ELISA reader evaluation while maintaining tissue structure visualization.
- Digital ELISA: Emerging digital ELISA platforms offer significantly enhanced sensitivity, achieving up to 50-fold improvement over conventional ELISA through single-molecule detection methods [33].
- Bead-Based Immunoassays: These utilize antibody-coated beads distinguished by color, fluorescence, or size, enabling robust multiplexing capabilities for detecting multiple analytes within a single sample while maintaining high sensitivity and dynamic range [33].
- Novel Applications: Research continues to develop specialized assays such as simultaneous detection of p16 and Ki-67 biomarkers for cervical cancer screening, demonstrating the adaptability of ELISA platforms to specific clinical needs [38].
Performance Comparison and Experimental Data
Direct Performance Comparison
Table 1: Direct Comparison of Immunoassay Platforms for Cancer Biomarker Analysis
| Parameter | ELISA | IHC | Bead-Based Assays | Histo-ELISA |
|---|---|---|---|---|
| Quantification Capability | Fully quantitative [33] | Semi-quantitative at best [37] | Fully quantitative [33] | Fully quantitative with spatial context [37] |
| Sensitivity | High (picogram range) [36] | Medium [36] | High to ultra-high [33] | High, comparable to ELISA [37] |
| Multiplexing Capacity | Singleplex (typically) [33] | Limited multiplexing (up to 4 targets with fluorescence) [36] | High multiplexing (dozens of targets) [33] | Singleplex [37] |
| Spatial Context | No tissue morphology [37] | Preserves tissue morphology and spatial distribution [35] [36] | No tissue morphology | Preserves tissue morphology [37] |
| Throughput | High [36] | Low to medium | High [33] | Medium [37] |
| Reproducibility | Medium to high [33] | Medium (subject to interpretation variability) [35] | High [33] | High (low coefficient of variation) [37] |
| Dynamic Range | Medium (2-3 orders of magnitude) [33] | Limited | High (3-5 orders of magnitude) [33] | Comparable to ELISA [37] |
| Sample Requirements | Cell lysates, biological fluids (serum, plasma) [34] [36] | Tissue sections [35] | Small sample volumes (25-150μL) [33] | Tissue sections [37] |
Experimental Correlation Studies
Direct comparative studies between ELISA and IHC demonstrate complex relationships between these platforms. A 1999 study comparing ELISA and IHC for components of the plasminogen activation system in cancer lesions revealed Spearman correlation coefficients ranging from 0.41 to 0.78 across different biomarkers [39]. While higher IHC score categories consistently associated with increased median ELISA values, significant overlap of ELISA values between different IHC scoring classes indicated that these techniques are not directly interchangeable [39].
The correlation performance varied by cancer type, with stronger correlations observed in breast carcinoma lesions compared to melanoma lesions, highlighting the influence of tissue and biomarker characteristics on platform agreement [39]. This underscores the importance of context-specific validation when comparing data across different immunoassay platforms.
Application-Specific Performance
Table 2: Platform Selection Guide for Specific Research Applications
| Research Application | Recommended Platform | Key Advantages | Supporting Evidence |
|---|---|---|---|
| Biomarker Quantification in Biofluids | ELISA or Bead-Based Assays | High sensitivity, fully quantitative, high throughput | Detects and quantifies peptides, proteins, and hormones in biological fluids [34] [33] |
| Tumor Tissue Biomarker Localization | IHC | Spatial context, cell-specific information, correlation with histopathology | Visualizes marker distribution in tissues and tumor heterogeneity [35] [40] |
| Multiplex Biomarker Panels | Bead-Based Immunoassays | Simultaneous quantification of multiple analytes, conserved sample volume | Quantifies multiple protein biomarkers in one run [33] |
| Quantitative Tissue Biomarker Analysis | Histo-ELISA | Combines quantification with morphological preservation | Quantifies target proteins while observing morphological changes [37] |
| Low-Abundance Biomarker Detection | Digital ELISA | Ultra-high sensitivity (fg/mL range) | ~50-fold more sensitive than conventional ELISA [33] |
| Autoantibody Biomarker Discovery | Protein Microarrays | High-throughput profiling of autoantibody signatures | Identifies autoantibody panels for cancer detection [41] |
Experimental Protocols and Methodologies
Standard ELISA Protocol
The following diagram illustrates the fundamental steps and variations in ELISA experimental workflow:
The core protocol involves: (1) coating microplates with capture antibody; (2) blocking with protein buffers like BSA to prevent nonspecific binding; (3) sample incubation with target antigens; (4) detection with specific antibodies; (5) enzyme-conjugated secondary antibody incubation; (6) substrate addition for color development; and (7) spectrophotometric measurement at 450nm [34]. Critical optimization points include antibody concentration, incubation time and temperature, and washing stringency between steps.
For novel applications such as cervical cancer screening, specialized ELISA protocols have been developed for simultaneous detection of biomarkers like p16 and Ki-67. This involves custom capture antibodies, biotinylated secondary antibodies, streptavidin-HRP conjugation, and TMB substrate development, with validation across different sample collection media [38].
Standard IHC Protocol
The IHC workflow involves multiple critical steps that influence staining quality and interpretation:
Key methodological considerations include:
- Fixation: Choice of fixative (formalin, paraformaldehyde, or alcohol-based) significantly impacts antigen preservation and accessibility. Formaldehyde-based fixatives create methylene cross-links between proteins, preserving morphology but potentially masking epitopes without proper antigen retrieval [36].
- Antigen Retrieval: Essential for formalin-fixed tissues to reverse methylene cross-links that obscure epitopes. Methods include heat-induced epitope retrieval (HIER) or enzyme-based retrieval [35].
- Blocking: Critical step to prevent nonspecific antibody binding using serum, BSA, or commercial blocking buffers [36].
- Detection Systems: Chromogenic detection using enzymes like HRP with DAB substrate produces permanent stains, while fluorescence detection using fluorophore-conjugated antibodies enables multiplexing [36].
- Controls: Both positive and negative controls are essential for validation. Positive controls confirm protocol functionality, while negative controls assess background staining [35].
Histo-ELISA Protocol
The Histo-ELISA method bridges conventional IHC and ELISA: (1) Tissue sections are prepared and circled with a hydrophobic barrier; (2) Standard ABC immunostaining is performed with primary and biotinylated secondary antibodies; (3) Instead of DAB, TMB peroxidase substrate is applied; (4) Hydrolyzed substrate solution is transferred to microtiter plates; (5) Reaction is stopped with H₂SO₄ and measured at 450nm; (6) Sections are subsequently stained with H&E for morphological correlation [37]. This innovative approach enables precise quantification while maintaining tissue morphology observation.
Research Reagent Solutions
Table 3: Essential Research Reagents for Immunoassay Applications
| Reagent Category | Specific Examples | Function and Application | Technical Considerations |
|---|---|---|---|
| Solid Phase Matrices | 96-well microplates (polystyrene, polyvinyl) [34] | Immobilize antibodies or antigens for ELISA | High binding capacity plates maximize sensitivity |
| Detection Enzymes | Horseradish peroxidase (HRP), Alkaline phosphatase (AP) [34] | Enzyme-antibody conjugates for signal generation | HRP with TMB substrate is most common |
| Chromogenic Substrates | TMB (3,3',5,5'-tetramethylbenzidine), DAB (3,3'-diaminobenzidine) [34] [37] | Generate colorimetric signals for detection | TMB for ELISA/Histo-ELISA, DAB for IHC |
| Fixatives | Formalin, Paraformaldehyde (PFA), Methanol/Ethanol [36] | Preserve tissue architecture and antigen integrity | Choice affects antigen retrieval requirements |
| Blocking Agents | BSA, Goat serum, Commercial blocking buffers [36] [37] | Reduce nonspecific antibody binding | Serum from secondary antibody species is optimal |
| Antigen Retrieval Buffers | Citrate buffer, EDTA, Tris-EDTA [35] | Reverse formaldehyde-induced epitope masking | pH and buffer composition affect retrieval efficiency |
| Primary Antibodies | Monoclonal vs. polyclonal antibodies [35] | Specific recognition of target antigens | Monoclonal offer specificity, polyclonal offer sensitivity |
| Secondary Antibodies | Enzyme-conjugated or fluorophore-conjugated [36] | Bind primary antibodies for detection | Species-specific and cross-adsorbed for minimal background |
Applications in Cancer Biomarker Research
Diagnostic and Prognostic Applications
Immunoassay platforms serve critical roles in cancer diagnosis and prognosis. IHC is indispensable for tumor classification and subtyping based on protein expression patterns, with applications in identifying infectious agents in tissues when cultures cannot be obtained [35]. ELISA formats have been developed for specific cancer biomarkers, including novel assays for simultaneous detection of p16 and Ki-67 in cervical cancer screening, providing quantitative alternatives to qualitative IHC tests [38].
Autoantibody profiling using protein microarrays represents an emerging application, with research identifying novel autoantibody panels for detecting pancreatic ductal adenocarcinoma (PDAC) with high sensitivity and specificity (AUC = 85.0%) [41]. Such approaches leverage the early appearance of autoantibodies in cancer progression, enabling potentially earlier detection than conventional protein biomarkers.
Therapeutic Development and Monitoring
In drug development, IHC provides crucial pharmacodynamic biomarkers to assess target engagement and biological effects of therapeutic interventions [35]. The spatial context provided by IHC enables researchers to evaluate whether therapeutics reach their intended cellular targets and elicit expected molecular changes within the tumor microenvironment.
ELISA platforms facilitate therapeutic monitoring by quantifying soluble biomarkers in biofluids, offering non-invasive approaches to track treatment response and disease progression. The high throughput and quantitative nature of ELISA make it particularly suitable for longitudinal studies in clinical trials.
Biomarker Validation
The analytical validation of cancer biomarkers typically requires orthogonal verification across multiple platforms. While discovery phases may utilize high-throughput technologies like protein microarrays, validation often employs ELISA for precise quantification or IHC for spatial confirmation [41]. This multi-platform approach strengthens the rigor of biomarker validation and ensures that assay performance characteristics meet requirements for intended use.
Future Perspectives
The evolution of immunoassay technologies continues to address current limitations while expanding analytical capabilities. Integration of digital pathology and artificial intelligence with IHC enables automated interpretation of complex staining patterns, reducing subjectivity and improving reproducibility [35]. Multiplexed imaging techniques are advancing to allow comprehensive single-cell expression analysis within tissue contexts, providing unprecedented resolution of tumor heterogeneity [35].
Emerging technologies including digital ELISA platforms offer dramatically improved sensitivity for detecting low-abundance biomarkers, potentially enabling earlier cancer detection and monitoring of minimal residual disease [33]. Bead-based immunoassays with expanded multiplexing capabilities continue to evolve, allowing simultaneous quantification of dozens of biomarkers from minimal sample volumes [33].
The convergence of immunoassay technologies with other analytical methods, such as genomic and proteomic approaches, will further enhance comprehensive cancer biomarker validation. As these technologies advance, they will increasingly enable personalized cancer diagnosis, monitoring, and therapeutic selection based on detailed molecular profiling of individual tumors.
In the era of precision medicine, the accurate detection of genomic alterations has become a cornerstone of cancer diagnosis and treatment selection. Nucleic acid-based detection technologies, primarily Polymerase Chain Reaction (PCR) and Next-Generation Sequencing (NGS) panels, offer powerful means to identify these critical biomarkers. PCR methods, including quantitative PCR (qPCR) and droplet digital PCR (ddPCR), are renowned for their high sensitivity and rapid turnaround in detecting predefined mutations [42]. In contrast, NGS panels provide a comprehensive genomic profile by simultaneously interrogating numerous genes across multiple mutation types, all within a single assay [43]. The choice between these technologies carries significant implications for diagnostic yield, therapeutic decision-making, and healthcare resource utilization. This guide objectively compares their performance, supported by experimental data and detailed methodologies, within the critical framework of analytical validation for cancer biomarker assays.
Performance Comparison: Key Metrics and Experimental Data
Direct comparisons in clinical studies reveal significant differences in detection capabilities, turnaround times, and associated costs between PCR and NGS methodologies.
Detection Sensitivity and Diagnostic Yield
The sensitivity of a test refers to its ability to correctly identify true positive cases, a crucial metric for cancer biomarker detection where missing a mutation can lead to inappropriate therapy.
Table 1: Comparative Analytical Sensitivity and Diagnostic Yield
| Technology | Cancer Type / Application | Key Performance Findings | Citation |
|---|---|---|---|
| ddPCR | Localized Rectal Cancer | Detected ctDNA in 58.5% (24/41) of baseline plasma samples. | [44] |
| NGS Panel | Localized Rectal Cancer | Detected ctDNA in 36.6% (15/41) of baseline plasma samples (p=0.00075). | [44] |
| NGS | HPV-Associated Cancers | Demonstrated the greatest sensitivity for detecting circulating tumor HPV DNA, followed by ddPCR and then qPCR. | [45] |
| Targeted NGS Panel | Solid Tumors (61-gene panel) | Showed an analytical sensitivity of 98.23% and specificity of 99.99% for variant detection. | [43] |
A study on circulating tumor DNA (ctDNA) in localized rectal cancer provides a direct head-to-head comparison, demonstrating that the tumor-informed ddPCR assay detected a significantly higher proportion of patients with ctDNA than the tumor-uninformed NGS panel [44]. This highlights ddPCR's exceptional sensitivity for tracking known mutations. Meanwhile, a meta-analysis of HPV-associated cancers concluded that NGS-based testing was the most sensitive approach overall for detecting circulating tumor HPV DNA [45]. Furthermore, a validated 61-gene NGS panel for solid tumors demonstrated exceptionally high sensitivity and specificity, underscoring the robustness of well-validated NGS assays [43].
Turnaround Time and Cost Considerations
Operational metrics like turnaround time (TAT) and cost are critical for clinical implementation and patient management.
Table 2: Operational and Economic Comparison
| Metric | PCR-Based Methods | NGS Panels |
|---|---|---|
| Turnaround Time | Rapid (hours). RT-PCR assays for viruses can provide results in 1.5 hours [46]. | Longer (days). Targeted NGS can reduce TAT to 4 days [43], though external testing can take ~3 weeks [43]. |
| Testing Cost | Lower per-target cost. Operational costs for ddPCR are 5–8.5-fold lower than NGS [44]. | Higher initial cost, but potentially cost-saving. A model in NSCLC showed NGS was less expensive overall due to avoided suboptimal treatment [47]. |
| Multiplexing Capability | Limited. Traditionally focuses on single or a few targets. | High. Can simultaneously Interrogate dozens to hundreds of genes. |
PCR methods consistently offer faster results, which is vital for acute diagnostic situations. While the per-test cost of NGS is higher, a comprehensive cost-effectiveness analysis in metastatic non-small cell lung cancer (mNSCLC) revealed that NGS testing was associated with lower total per-patient costs ($8,866 for NGS vs. $18,246 for PCR strategies) [47]. These savings were driven by more rapid results, shorter time to appropriate therapy, and minimized use of ineffective treatments while awaiting test results [47].
Experimental Protocols and Validation Data
Robust analytical validation is fundamental to establishing the reliability of any clinical assay. The following protocols and results illustrate the rigorous processes behind PCR and NGS technologies.
PCR Assay Validation: A SARS-CoV-2 Model
While focused on a viral pathogen, the validation of this RT-PCR assay exemplifies the standard procedures for any PCR-based diagnostic.
- Assay Design: Researchers developed allele-specific primers and probes targeting nine signature mutations in the spike protein of SARS-CoV-2 variants (Omicron and Delta) [42].
- Clinical Validation: The assay was tested on 160 archived samples (75 positive, 85 negative). Results were compared to Whole Genome Sequencing (WGS) as the reference standard [42].
- Performance Metrics: The validated assay demonstrated high sensitivity and specificity in differentiating between the Omicron and Delta variants without requiring full genome sequencing [42]. This demonstrates the power of PCR for precise mutation detection.
NGS Panel Validation: A Solid Tumor Model
The development and validation of a targeted 61-gene oncopanel for solid tumors showcase the multi-step process for NGS.
- Assay Design & Wet-Lab: A hybridization-capture based target enrichment method was used on a panel targeting 61 cancer-associated genes. Libraries were prepared on an automated system and sequenced on a DNBSEQ-G50RS platform [43].
- Analytical Validation:
- Limit of Detection (LOD): The assay demonstrated 100% sensitivity for detecting variants at a Variant Allele Frequency (VAF) ≥ 3%. The minimum detectable VAF was determined to be 2.9% for both SNVs and INDELs [43].
- Precision: The assay showed 99.99% repeatability (intra-run precision) and 99.98% reproducibility (inter-run precision) [43].
- Accuracy: Using reference standards and clinical samples with known mutations, the assay achieved 98.23% sensitivity and 99.99% specificity [43].
- Clinical Concordance: When tested on 40 tumor samples, the panel identified 92 known variants with 100% concordance with orthogonal methods from external laboratories [43].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of PCR and NGS assays requires a suite of high-quality reagents and tools. The following table details key components used in the featured experiments.
Table 3: Essential Research Reagents for Nucleic Acid-Based Detection
| Reagent / Solution | Function in the Experiment | Example from Literature |
|---|---|---|
| Streck Cell Free DNA BCT Tubes | Stabilizes blood samples for cell-free DNA analysis, preventing white blood cell lysis and genomic DNA contamination. | Used for plasma collection in the rectal cancer ctDNA study [44]. |
| Ion AmpliSeq Cancer Hotspot Panel v2 | A targeted NGS panel for amplifying and sequencing hotspot regions of 50 oncogenes and tumor suppressor genes. | Used for identifying tumor mutations and ctDNA via NGS [44]. |
| One Step U* Mix & Enzyme Mix | An all-in-one master mix for reverse transcription and PCR amplification, streamlining reaction setup. | Used in the FMCA-based multiplex PCR for respiratory pathogens [46]. |
| Automated Nucleic Acid Extraction System | Standardizes and automates the purification of high-quality DNA/RNA from clinical samples, reducing manual error. | Used for nucleic acid extraction in both the respiratory pathogen and solid tumor NGS studies [46] [43]. |
| Sophia DDM Software | A bioinformatics platform that uses machine learning for variant calling, annotation, and clinical interpretation of NGS data. | Used for data analysis and visualization in the 61-gene oncopanel validation [43]. |
Technology Selection Workflow
The choice between PCR and NGS is not one of superiority but of appropriateness for a specific clinical or research question. The following diagram outlines a decision-making workflow based on key criteria.
Both PCR and NGS panels are indispensable tools in the molecular diagnostics arsenal, each with distinct strengths. PCR methods, particularly ddPCR, offer unmatched sensitivity and speed for monitoring specific, known mutations, making them ideal for minimal residual disease detection and tracking known resistance mechanisms [44]. NGS panels provide a broad, hypothesis-free approach for comprehensive genomic profiling, which is crucial for initial diagnosis, identifying unexpected therapeutic targets, and understanding tumor heterogeneity [43]. The choice between them must be guided by the clinical question, required sensitivity, and operational constraints. The trend in precision medicine is not to view them as competitors but as complementary technologies. A future-facing diagnostic pipeline may leverage NGS for initial comprehensive profiling, followed by ultrasensitive PCR assays for longitudinal monitoring of the specific mutations identified, thereby optimizing both breadth and depth for personalized patient management.
Liquid biopsy has emerged as a transformative approach in oncology, providing a non-invasive means to probe tumor dynamics through the analysis of circulating biomarkers such as circulating tumor DNA (ctDNA) and proteins [48] [49]. The analytical validation of assays that detect these biomarkers is a critical foundation for their reliable application in clinical practice and drug development. Validation ensures that tests are robust, sensitive, specific, and reproducible, meeting the stringent requirements for precision oncology [18] [50]. For ctDNA assays, key validation parameters often include sensitivity, specificity, and the limit of detection (LOD), particularly challenging due to the low fractional abundance of ctDNA in a high background of normal cell-free DNA [51] [50]. In contrast, protein biomarker assay validation grapples with the immense dynamic range and complexity of the plasma proteome, requiring technologies capable of high-plex quantification without sacrificing specificity or sensitivity [52] [18]. This guide provides a comparative analysis of current technologies and assays for ctDNA and protein analysis, detailing their performance metrics, underlying methodologies, and practical implementation to aid researchers in selecting and validating appropriate platforms for their specific research needs.
Comparative Performance of ctDNA and Protein Assays
The following tables summarize key performance characteristics and technologies for ctDNA and protein assays based on current literature and commercial platforms.
Table 1: Key Performance Metrics for ctDNA Detection Assays
| Assay/Technology | Reported Sensitivity | Reported Specificity | Key Applications | Defining Features & Limitations |
|---|---|---|---|---|
| TEC-Seq [51] [53] | 59% - 71% (Early-stage) | ~99% | Early cancer detection, mutation profiling | Ultra-sensitive sequencing; no prior tumor mutation knowledge needed. |
| dPCR/BEAMing [50] | High for known mutations | >99% [50] | Tracking specific mutations, therapy monitoring | Extremely sensitive for low-frequency variants; limited to few pre-defined mutations. |
| CAPP-Seq [50] | High (varies by tumor type) | >99% [50] | Comprehensive mutation profiling, MRD | Targeted NGS; cost-effective for wide genomic coverage. |
| Multi-Cancer Early Detection (MCED) [54] | 70.83% (Overall) | 99.71% | Multi-cancer screening, Tissue of Origin (TOO) | Analyzes methylation, fragmentomics; high specificity for population screening. |
Table 2: Key Performance Metrics and Technologies for Protein Biomarker Assays
| Technology | Plexity (Approx.) | Sensitivity (Typical) | Key Applications | Defining Features & Limitations |
|---|---|---|---|---|
| Mass Spectrometry (MS) [52] | Hundreds - Thousands | Variable (fg - pg range with optimization) | Biomarker discovery, proteome profiling | Unbiased discovery; high technical expertise required; complex data analysis. |
| Proximity Extension Assay (PEA) [52] | Thousands | High (fg/mL range) | High-plex biomarker validation, signature identification | High specificity and sensitivity in complex fluids; requires specialized instrumentation. |
| Aptamer-based Arrays [52] | Thousands | High (fg/mL - pg/mL range) | Large-scale clinical studies, biomarker panels | Very high plexity; stable reagents; potential for non-specific binding. |
| Reverse Phase Protein Arrays (RPPA) [52] | Hundreds | High | Signaling pathway analysis, phosphoproteomics | Functional proteomics; limited by antibody availability and quality. |
Experimental Protocols for Core Assay Types
Protocol for ctDNA Analysis Using Targeted NGS with Error Correction
The accurate detection of low-frequency mutations in ctDNA requires methods that mitigate sequencing errors. The following workflow is adapted from techniques like TEC-Seq and CAPP-Seq [51] [50] [53].
- Sample Collection & Plasma Preparation: Collect 10-20 mL of peripheral blood into cell-free DNA blood collection tubes (e.g., Streck). Process within a specified window (e.g., 2-5 days) [54]. Perform double centrifugation (e.g., 1600 × g followed by 16,000 × g) to isolate platelet-poor plasma.
- cfDNA Extraction: Extract cfDNA from 2-5 mL of plasma using commercial silica-membrane or magnetic bead-based kits. Quantify yield using fluorometry (e.g., Qubit).
- Library Preparation & Barcoding: Construct sequencing libraries from the extracted cfDNA. A critical step is the ligation of Unique Molecular Identifiers (UMIs), also known as molecular barcodes, to each original DNA fragment prior to PCR amplification [50].
- Target Capture & Sequencing: Use biotinylated probes to enrich for a predefined set of target genes (e.g., a pan-cancer panel or cancer-specific panel). Perform sequencing on a high-throughput platform (e.g., Illumina) to achieve high coverage (e.g., 10,000x).
- Bioinformatic Analysis & Error Correction:
- Sequence Alignment: Align sequences to the reference human genome.
- Consensus Building: Group reads originating from the same original DNA molecule using the UMIs. Generate a consensus sequence to eliminate PCR and sequencing errors that are not present in the majority of reads from the same molecule [50].
- Variant Calling: Identify somatic mutations by comparing against a matched normal DNA sample (e.g., from buffy coat) or a database of common polymorphisms.
Protocol for High-Plex Protein Analysis Using Proximity Extension Assay (PEA)
PEA combines the specificity of antibody-pair binding with DNA amplification for highly sensitive, multiplex protein quantification [52].
- Sample Preparation: Dilute plasma or serum samples in a suitable buffer to minimize matrix effects.
- Incubation with Proximity Probes: Incubate the sample with a library of matched antibody pairs, where each antibody is conjugated to a unique DNA oligonucleotide ("proximity probe").
- Dual Recognition and Hybridization: When two probes bind in close proximity to the same target protein, their DNA oligonucleotides can hybridize.
- Extension and Amplification: Add a DNA polymerase to extend one of the hybridized strands, creating a unique DNA barcode that is specific to the protein target. Amplify this barcode by PCR or isothermal amplification.
- Quantification and Identification: Quantify the amplified DNA barcodes using next-generation sequencing (NGS) or microfluidic quantitative PCR (e.g., BioMark HD system). The quantity of each specific DNA barcode is proportional to the concentration of the corresponding protein in the original sample.
Visualizing Analytical Workflows
The core workflows for ctDNA and protein analysis involve multi-step processes that transform a blood sample into quantifiable digital data. The following diagrams illustrate these pathways.
ctDNA Analysis Pathway from Blood to Variant Call
Proteomic Profiling via Proximity Extension Assay
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful assay validation and execution depend on a suite of reliable reagents and tools. The table below details essential components for setting up a liquid biopsy workflow.
Table 3: Essential Research Reagents and Tools for Liquid Biopsy Assays
| Reagent/Tool | Function | Key Considerations |
|---|---|---|
| cfDNA Blood Collection Tubes (e.g., Streck, PAXgene) | Stabilizes nucleated blood cells to prevent genomic DNA contamination and preserve cfDNA profile during transport [54]. | Critical for pre-analytical integrity; defines maximum hold time before processing. |
| cfDNA Extraction Kits (e.g., QIAamp, Circulating Nucleic Acid Kit) | Isolate and purify short-fragment cfDNA from plasma with high efficiency and reproducibility. | Key performance metrics: yield, purity, and removal of PCR inhibitors. |
| Unique Molecular Identifiers (UMIs) | Short random DNA barcodes ligated to each original DNA molecule to enable bioinformatic error correction [50]. | Fundamental for distinguishing true low-frequency variants from sequencing artifacts. |
| Targeted Hybrid Capture Panels | Biotinylated oligonucleotide probes designed to enrich for genomic regions of interest (e.g., cancer genes) prior to sequencing. | Panel design (size, content) dictates breadth of genomic Interrogation and cost. |
| Matched Antibody Pairs (for PEA) | Pairs of antibodies that bind non-overlapping epitopes on the same target protein, each conjugated to a unique DNA oligonucleotide [52]. | Antibody specificity is paramount for assay performance; commercial panels are available. |
| NGS Library Prep Kits | Prepare fragmented DNA for sequencing by adding platform-specific adapters. | Compatibility with low-input DNA and integration of UMI workflow are crucial. |
The Role of Recombinant Antibodies in Ensuring Specificity and Lot-to-Lot Consistency
In the field of cancer biomarker research, the reproducibility crisis fueled by unreliable biological reagents represents a significant barrier to clinical translation. It is estimated that $28.2 billion annually is lost to irreproducible preclinical research in the United States alone, with biological reagents being a major contributor [55]. Recombinant antibodies, generated through in vitro genetic manipulation rather than traditional animal-based systems, are emerging as critical tools to address these challenges by providing unprecedented specificity and lot-to-lot consistency, thereby enhancing the reliability of cancer biomarker analytical validation [56] [55].
What Are Recombinant Antibodies?
Recombinant antibodies are monoclonal antibodies produced by cloning antibody genes into expression vectors, which are then transfected into host cell lines for antibody expression [56] [57]. This method stands in contrast to traditional monoclonal antibodies produced via hybridoma systems or polyclonal antibodies purified from animal serum. The fundamental distinction lies in the defined genetic sequence that forms the foundation of recombinant antibodies, enabling precise control over production and manipulation [56] [58].
Key Production Workflow
The production of recombinant antibodies follows a systematic, genetically-engineered pipeline that ensures precision and consistency from inception to final product, as illustrated below.
This genetically-based manufacturing process eliminates the biological variability inherent in animal-based systems, establishing the foundation for superior performance characteristics essential for biomarker validation [58].
Comparative Analysis: Recombinant vs. Traditional Antibodies
The following table summarizes the critical differences between recombinant antibodies and traditional alternatives across parameters vital for robust cancer biomarker assay development.
| Characteristic | Recombinant Antibodies | Traditional Monoclonal Antibodies | Traditional Polyclonal Antibodies |
|---|---|---|---|
| Production Method | In vitro genetic manipulation in host cells [56] | Hybridoma generation via immunization [59] | Animal immunization with serum purification [59] |
| Lot-to-Lot Consistency | Highest (genetic sequence defined) [59] [57] | Variable (subject to genetic drift) [56] | Low (significant biological variability) [59] |
| Specificity | High (defined sequence, KO validation possible) [55] | Variable (dependent on epitope and validation) [59] | Variable (multiple epitopes, potential cross-reactivity) [59] |
| Scalability | High (amenable to large-scale production) [56] | Limited (dependent on hybridoma stability) [56] | Limited (multiple animal immunizations) |
| Animal Use | Avoided (animal-free manufacturing) [56] | Required (hybridomas or ascites production) [56] | Required (serum collection from immunized hosts) [56] |
| Engineering Potential | High (isotype switching, species switching, formatting) [56] [60] | Low (difficult to modify once produced) | None (complex mixture of antibodies) |
Experimental Evidence: Performance in Biomarker Assay Applications
Enhanced Sensitivity through Fc Engineering
Proprietary Fc engineering technology has demonstrated significant improvements in recombinant antibody performance. In western blot analyses, engineered recombinant rabbit monoclonal antibodies against Parkin and OCT4 showed an approximately two-fold sensitivity enhancement over wild-type parental antibodies, enabling detection of low-abundance targets critical for cancer biomarker research [60].
Experimental Protocol:
- Cell Lines: SH-SY5Y (for Parkin) and NTERA-2 (for OCT4)
- Antibody Concentrations: Parkin (1 µg/ml), OCT4 (0.5 µg/ml)
- Methods: Western blot analysis performed on whole cell extracts
- Validation: siRNA-mediated knockdown confirmed specificity of both targets [60]
Application Coverage and Signal Enhancement
Engineered recombinant antibodies demonstrate superior performance across multiple applications essential for comprehensive biomarker validation, as quantified below.
| Application | Performance Metric | Traditional Antibodies | Recombinant Antibodies |
|---|---|---|---|
| Western Blotting | Signal intensity (fold enhancement) | Baseline | ~2.0-fold increase [60] |
| Immunocytochemistry | Signal-to-noise ratio | Baseline | ~1.5-fold increase [60] |
| Flow Cytometry | Detection sensitivity | Limited for low-abundance targets | Enhanced detection of intracellular targets [60] |
| Immunohistochemistry | Specificity in FFPE tissues | Variable based on clone | Reliable performance with minimal background [60] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of recombinant antibodies in cancer biomarker validation requires specific reagent systems and validation approaches, as detailed in the following table.
| Reagent/Tool | Function in Biomarker Validation | Key Features |
|---|---|---|
| Recombinant Rabbit Monoclonals | Primary detection for IHC, WB, FC [58] | High specificity, picomolar affinity, suitable for "difficult" immunogens [57] |
| Knockout Validation Cell Lines | Specificity confirmation [55] | Isogenic cell lines with target gene knockout serving as true negative controls [55] |
| Lyophilized Recombinant Antibodies | Stable reagent storage and shipping [57] | Ambient temperature stability, reduced shipping costs, pre-aliquoted formats [57] |
| Engineered Fc Region Antibodies | Enhanced detection sensitivity [60] | Proprietary Fc modifications that improve signal without altering antigen binding [60] |
| Biophysical QC Tools (LC-MS, HPLC) | Molecular identity confirmation [55] | Purity, aggregation, and sequence identity assessment for lot-to-lot consistency [55] |
Recombinant Antibodies in Cancer Biomarker Analytical Validation
The analytical validation of cancer biomarker assays requires demonstrating that a test consistently and accurately measures the intended biomarker, establishing analytical validity as a foundation for clinical utility [61]. Recombinant antibodies contribute significantly to this process through several key attributes that directly address regulatory requirements for biomarker assays used in drug development and clinical trials [62] [63].
Addressing Biomarker Validation Spheres
The development and implementation of predictive biomarkers in oncology follows a structured pathway where recombinant antibodies play increasingly important roles at multiple stages, as illustrated in the validation workflow below.
For companion diagnostics (CDx), recombinant antibodies provide the consistency required for regulatory approval, while for laboratory developed tests (LDTs), they facilitate the indirect clinical validation necessary to demonstrate equivalence to clinical trial assays [63].
Ensuring Reproducibility in Long-Term Studies
The defined genetic sequence of recombinant antibodies ensures that the same antibody can be produced indefinitely, eliminating concerns about cell line drift or hybridoma instability that plague traditional monoclonal antibodies [56] [59]. This characteristic is particularly valuable for long-term cancer studies or when validating biomarkers across multiple sample sets, as it guarantees reagent consistency throughout the project lifecycle [58].
Recombinant antibodies represent a transformative technology for cancer biomarker research, directly addressing the reproducibility challenges that have hampered translational progress. Through their defined genetic sequence, exceptional lot-to-lot consistency, and engineerability, these reagents provide the reliability necessary for robust analytical validation of biomarker assays. As the field moves toward more precise biomarker-driven therapeutic approaches, recombinant antibodies will play an increasingly critical role in ensuring that biomarker tests meet the stringent requirements for clinical implementation, ultimately supporting more accurate cancer diagnosis, prognosis, and treatment selection.
Overcoming Hurdles: Common Pitfalls and Strategies for Robust Assays
The integration of biomarker testing into oncology has revolutionized cancer treatment, enabling personalized therapy based on the unique molecular profile of each patient's tumor [64]. However, the effectiveness of these advanced assays is often limited by the quality and quantity of tumor tissue available for analysis [65]. Samples from clinical trials frequently exhibit significant degradation and low nucleic acid recovery, complicating every step from extraction to data analysis [65]. This challenge is particularly pronounced in small biopsies, such as those obtained via core needle procedures, which may yield only trace amounts of usable nucleic acids [65]. Within the framework of analytical validation, which ensures that biomarker tests are accurate, reliable, and reproducible, sample limitations represent a critical bottleneck. This guide objectively compares current strategies and technologies designed to maximize information yield from minimal sample input, providing researchers and drug development professionals with data-driven insights for navigating these fundamental constraints.
Comparative Analysis of Strategic Approaches
The following table summarizes the core strategies for handling low-input and challenging samples, comparing their core principles, technological requirements, and key performance metrics as evidenced by current research.
Table 1: Strategic Comparison for Low-Input and Challenging Matrices
| Strategic Approach | Core Principle | Key Technologies/ Methods | Reported Performance & Data | Primary Application in Validation |
|---|---|---|---|---|
| Workflow Innovation & Automated Extraction [65] | Standardizing and automating protocols to maximize nucleic acid yield and quality from suboptimal samples. | Dual extraction techniques; automated, standardized protocols; robust quality control (QC). | Marked improvements in sample quality and sequencing success rates; reduces incidence of insufficient samples. | Ensuring input sample quality and consistency for downstream assays. |
| Comprehensive Genomic Profiling [64] [65] | Using broad sequencing approaches to extract maximum molecular information from a single, limited test. | Whole Exome Sequencing (WES); Whole Transcriptome Sequencing (WTS); expansive targeted NGS panels. | Detects a wide spectrum of genetic alterations (mutations, amplifications, translocations) and emerging biomarkers from minimal input. | Comprehensive profiling for therapy selection and biomarker discovery when tissue is scarce. |
| Advanced Imaging & Radiomics [66] [67] | Extracting high-dimensional, quantitative data from medical images as non-invasive or complementary biomarkers. | Quantitative High-Definition Microvessel Imaging (qHDMI); MRI Radiomics; contrast-free ultrasound. | qHDMI differentiates choroidal melanoma from nevus with statistical significance (e.g., vessel segments, p=0.003) [66]; Radiomic feature repeatability (ICC 0.30-0.99) varies with sequence [67]. | Technical validation of imaging biomarkers; providing prognostic/predictive data when tissue is unavailable. |
| Liquid Biopsies & Circulating Biomarkers [68] | Interrogating tumor-derived material from peripheral blood as a non-invasive alternative to tissue biopsies. | Circulating Tumor DNA (ctDNA) analysis; exosome isolation; microRNA (miRNA) profiling. | Shows promising potential for early cancer detection and monitoring; challenges include low ctDNA concentration and need for clinical standardization [68]. | Enabling repeated monitoring of disease burden and treatment response; useful when tissue biopsy is infeasible. |
Detailed Experimental Protocols and Methodologies
Protocol for Quantitative High-Definition Microvessel Imaging (qHDMI)
This contrast-free ultrasound-based technique visualizes and quantifies tumor microvasculature, providing objective biomarkers for differentiating malignant lesions [66].
- Step 1: Image Acquisition. A research ultrasound platform (e.g., Verasonics Vantage 128 scanner with a L22vXLF linear array transducer) is used. Participants are scanned transcutaneously over the eyelid. The lesion is identified using B-mode ultrasound, followed by ultrafast imaging via 3-angle coherent plane-wave compounding at a high frame rate (1000 Hz) for one second without any contrast agent [66].
- Step 2: Microvasculature Image Generation. The raw data is processed offline. A series of clutter filtering, denoising, and vessel enhancement techniques are applied to generate the high-definition microvessel images [66].
- Step 3: Region of Interest (ROI) Definition and Vessel Skeletonization. An ROI is defined on the B-mode image to encapsulate the tumor. The HDMI image within the ROI is converted to a binary image, and the full skeleton of the microvessel network is constructed [66].
- Step 4: Quantitative Biomarker Extraction. Morphological parameters are automatically quantified from the skeletonized network. Key biomarkers include [66]:
- Vessel Density (VD): The proportion of vessel area with blood flow over the total ROI area.
- Number of Vessel Segments (NV) & Branch Points (NB): Counts of discrete vessel segments and points where three or more segments connect.
- Vessel Tortuosity (τ): The ratio of the actual vessel path length to the linear distance between its endpoints.
- Microvessel Fractal Dimension (mvFD): A unit-less measure of the structural complexity of the vascular network.
Protocol for Enhanced Nucleic Acid Extraction from FFPE Samples
This protocol outlines steps to improve the quantity and quality of nucleic acids recovered from formalin-fixed paraffin-embedded (FFPE) samples, which are often degraded [65].
- Step 1: Standardized Tissue Sectioning. Precisely cut FFPE tissue sections of consistent thickness to minimize pre-analytical variability.
- Step 2: Dedeparaffinization and Lysis. Use standardized, automated protocols to remove paraffin and lyse the tissue completely. This ensures uniform exposure of cells to extraction reagents.
- Step 3: Dual Nucleic Acid Extraction. Employ a dual extraction technique that simultaneously recovers both DNA and RNA from a single sample aliquot. This maximizes the utility of a limited sample by providing material for multiple types of genomic analyses [65].
- Step 4: Rigorous Quality Control (QC). Quantify the yield using fluorescence-based assays (e.g., Qubit) which are more accurate for degraded samples than absorbance. Qualitatively assess the integrity of the nucleic acids using methods like the DNA Integrity Number (DIN) or RNA Integrity Number (RIN), or by PCR/sequencing-based QC assays. This step is critical to exclude unreliable data and ensure only high-confidence variants are reported [65].
Strategic Framework and Workflow Integration
The following diagram illustrates the logical relationship and integration of the different strategic approaches for addressing sample limitations, from sample acquisition to clinical insight.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful navigation of sample limitations requires a suite of specialized reagents and tools. The following table details key items essential for experiments in this field.
Table 2: Key Research Reagent Solutions for Low-Input Biomarker Analysis
| Item / Reagent | Function / Application | Specific Use Case & Consideration |
|---|---|---|
| Automated Nucleic Acid Extraction Systems | Standardized, high-efficiency recovery of DNA and RNA from limited or challenging matrices like FFPE. | Dual extraction protocols for simultaneous DNA/RNA recovery maximize data from a single sample aliquot [65]. |
| Broad-Panel NGS Kits | Targeted sequencing for detecting a wide array of genetic alterations (SNVs, fusions, CNVs) from low-yield samples. | Panels should cover relevant oncogenes (e.g., EGFR, ALK, HER2, NTRK) and tumor suppressors to guide therapy when tissue is scarce [64] [65]. |
| Ultrafast Ultrasound Research Platform | Enables acquisition of high-frame-rate data required for contrast-free microvascular imaging techniques like qHDMI. | Systems like the Verasonics Vantage allow for custom sequence design and raw RF data capture for advanced processing [66]. |
| Specialized Buffers for FFPE De-crosslinking | Reverses formalin-induced crosslinks in nucleic acids, which is critical for improving sequencing library quality from archived tissues. | Reduces sequencing artifacts and improves the mapping rate and coverage uniformity, especially for older archival samples. |
| Single-Pixel Imaging (SPI) Modulation Matrices | Used in computational imaging to optimize sampling efficiency and image reconstruction quality under low-light or low-sampling conditions. | Matrices like the Convolutional Matrix (CM) adaptively optimize sampling, improving feature capture and reducing redundancy [69]. |
In the precision-driven field of cancer biomarker research, the accuracy of data generated from ligand binding assays (LBAs) such as ELISA is paramount. Two of the most pervasive analytical challenges that threaten this accuracy are cross-reactivity and matrix interferences. Cross-reactivity occurs when an antibody binds to non-target proteins or analytes with structural similarities to the intended target, potentially leading to false positive signals or an overestimation of the analyte concentration [70] [71]. Matrix interference, often considered the single most important challenge in LBAs, refers to the effect of components within a biological sample (e.g., serum, plasma) that alter the true value of the result for an analyte [20] [70]. Within the hospital clinical chemistry laboratory, it is estimated that the pre-analytical phase, where many such interferences originate, is responsible for up to 75% of errors [20]. For researchers and scientists in drug development, navigating these challenges is not merely a technical exercise but a fundamental requirement for generating reliable, reproducible, and clinically actionable data. This guide objectively compares the performance of various technological and methodological approaches in mitigating these specific threats to assay integrity.
Cross-Reactivity: Mechanisms and Platform Comparison
Cross-reactivity poses a fundamental threat to immunoassay specificity. The scale of this problem is significant; one evaluation of 11,000 affinity-purified antibodies found that approximately 95% bound to "non-target" proteins in Western blot analyses, indicating widespread cross-reactivity [70] [71]. The mechanisms and vulnerabilities differ substantially between assay formats.
Mechanisms of Cross-Reactivity
- Sample-Driven Cross-Reactivity: Predominantly affects single-antibody assay formats (e.g., direct detection arrays). In this scenario, cross-reacting proteins or interferents in the sample matrix bind directly to immobilized capture agents, generating a false signal that is indistinguishable from specific binding [71].
- Reagent-Driven Cross-Reactivity: A unique challenge in multiplexed sandwich assays (MSAs). Here, a detection antibody intended for one analyte may erroneously bind to a different capture antibody within the multiplexed panel. This creates a "cross-talk" between assays, leading to false positives that are particularly difficult to identify because the signal is generated through a complete, but incorrect, sandwich complex [71].
Technology Performance Comparison
The following table compares how different immunoassay platforms address the challenge of cross-reactivity.
Table 1: Platform Comparison for Managing Cross-Reactivity
| Assay Format | Mechanism of Cross-Reactivity | Key Strengths | Key Limitations | Best Use Cases |
|---|---|---|---|---|
| Single-Antibody Array | Sample-driven | Requires only one antibody per target; easier to scale to high-plex (1000+ targets) [71]. | Highly vulnerable to false positives from sample matrix; limited specificity verification [71]. | Initial, high-volume biomarker discovery screening. |
| Traditional Sandwich ELISA (Single-plex) | Requires two simultaneous spurious bindings for a false positive [71]. | High inherent specificity; well-understood and established protocol [72] [71]. | Low-plex only; requires carefully matched antibody pairs [72]. | Targeted, quantitative analysis of a single analyte. |
| Multiplexed Sandwich Assay (Bead or Planar Array) | Reagent-driven (cross-talk) [71]. | Conserves precious sample volume; generates multi-analyte data from a single run [73]. | Specificity validation is complex; vulnerable to reagent cross-talk; scaling beyond ~50 targets is challenging [73] [71]. | Pathway analysis or profiling a defined set of biomarkers. |
| Proximity Ligation/Extension Assays (PLA/PEA) | Molecular recognition of specific binding events [71]. | Extremely high specificity; digitally discriminates true binding from cross-reactivity; attomolar to zeptomolar sensitivity [71]. | Complex reagent design and workflow; higher cost per sample. | Ultra-sensitive quantification of critical low-abundance biomarkers. |
Matrix interference encompasses a wide range of pre-analytical and analytical variables that can compromise assay accuracy. Sources include heterophilic antibodies, binding proteins, lipids (lipemia), hemolyzed hemoglobin, drug metabolites, and concomitant therapies [70]. The impact can manifest as poor spike-and-recovery, a lack of parallelism in serial dilutions, or inconsistent results between sample batches.
Experimental Protocols for Evaluating Matrix Interference
To ensure data quality, the following experimental protocols are essential during assay development and validation:
- Parallelism/Linearity-of-Dilution: Prepare serial dilutions of a sample containing the endogenous analyte in the intended matrix. The observed concentration, when plotted against the dilution factor, should produce a linear response that is parallel to the calibration curve. Non-parallelism indicates significant matrix interference [70].
- Spike-and-Recovery: Spike a known quantity of purified recombinant standard into the sample matrix and measure the recovered concentration. The recovery percentage is calculated as
(Observed Concentration / Expected Concentration) * 100. Acceptable recovery (typically 80-120%) confirms that the matrix does not interfere with the antigen-antibody interaction [70] [72]. - Determination of Minimum Required Dilution (MRD): Perform spike-and-recovery experiments at a series of sample dilutions. The MRD is defined as the lowest dilution factor at which acceptable recovery is achieved, effectively minimizing matrix effects while maintaining sufficient assay sensitivity [70] [73].
Comparative Analysis of Interference Mitigation Approaches
Different technological and methodological strategies offer varying levels of effectiveness against matrix interference.
Table 2: Comparison of Matrix Interference Mitigation Strategies
| Strategy | Methodology | Effectiveness | Trade-offs & Considerations |
|---|---|---|---|
| Sample Dilution | Diluting the sample in assay buffer to reduce concentration of interferents [70]. | Simple, widely applicable, and often effective. | Reduces the concentration of the target analyte, potentially compromising sensitivity [70]. |
| Alternative Blocking Buffers | Using non-mammalian protein blockers (e.g., salmon serum) or protein-free solutions to prevent non-specific binding [72]. | Can significantly reduce specific interferents like heterophilic antibodies. | Requires empirical testing; optimal blocker is system-dependent [72]. |
| Platform Flow-Through Kinetics | Using microfluidic systems to minimize contact time between sample/reagents and the solid phase [70]. | Highly effective; favors high-affinity specific interactions while minimizing low-affinity interference [70]. | Requires specialized instrumentation (e.g., Gyrolab). Platform may have limited assay multiplexing capacity. |
| Automation & Miniaturization | Using automated liquid handling and nano-/micro-scale assay volumes [70]. | Improves precision, reduces pipetting errors and sample/reagent consumption. | High initial investment; requires method adaptation and validation for miniaturized format [70]. |
The following diagram illustrates the decision-making workflow for troubleshooting and mitigating matrix interference based on experimental findings.
The Scientist's Toolkit: Essential Reagents and Materials
Successful management of cross-reactivity and interference relies on a foundation of high-quality reagents and conscientious experimental design. The following table details key components of this toolkit.
Table 3: Research Reagent Solutions for Ensuring Specificity
| Item / Reagent | Function & Role in Ensuring Specificity | Key Selection Criteria & Considerations |
|---|---|---|
| High-Quality Antibodies | Form the core of the assay's specificity. Capture and detect the target analyte. [72] | Specificity: Prefer monoclonal for capture. Affinity: High affinity (low Kd) withstands washes. Validation: Seek antibodies validated for your specific application (e.g., ELISA) [70] [72]. |
| Matched Antibody Pairs | Critical for sandwich immunoassays to ensure two distinct antibodies recognize different epitopes on the same target without steric hindrance [72]. | Verify the pair is certified for use together. Ensure capture and detection antibodies are raised in different species if using a secondary detection system [72]. |
| Matrix-Appropriate Blocking Buffers | Block unused binding sites on the solid phase to minimize non-specific binding of sample components [72]. | Standard blockers: BSA or casein. If cross-reactivity persists, test non-mammalian options (e.g., fish serum) or commercial protein-free blockers [72]. |
| Surfactant-Containing Wash Buffers | Remove unbound reagents and loosely attached interferents during wash steps [72]. | A concentration of 0.05% (v/v) Tween 20 in PBS or TBS is common. Harshness can be adjusted but may disrupt specific binding if too stringent [72]. |
| Well-Characterized Reference Standard | Serves as the benchmark for constructing the calibration curve, enabling accurate quantitation of the target in unknown samples [72]. | Should be a highly purified form of the analyte (e.g., recombinant). Concentration must be accurately determined. Matrix composition should be well-defined [72]. |
In the critical pursuit of analytical validity for cancer biomarker assays, a proactive and systematic approach to cross-reactivity and matrix interference is non-negotiable. As the data demonstrates, no single platform or strategy offers a perfect solution; each presents a unique set of trade-offs between specificity, sensitivity, multiplexing capability, and workflow efficiency. The optimal path forward relies on a fit-for-purpose mindset [20] [3], where the intended use of the data guides the selection of technology and the rigor of validation. By leveraging a combination of rigorous experimental protocols—including parallelism and spike-and-recovery tests—and modern technological solutions such as flow-through systems and proximity assays, scientists can generate the high-fidelity data essential for driving confident decisions in drug development and, ultimately, advancing personalized cancer care.
Reproducibility is a fundamental requirement in scientific research, with a recent survey finding that 90% of respondents believe there is a significant reproducibility crisis in science [74]. Batch effects and reagent variability represent paramount factors contributing to irreproducibility, potentially resulting in retracted articles, discredited research findings, and substantial economic losses [74]. In the specific context of cancer biomarker assays, these technical variations introduce unacceptable uncertainty into analytical validation, potentially compromising clinical decision-making for personalized treatment approaches.
Batch effects are technical variations irrelevant to study factors of interest that are introduced into high-throughput data due to variations in experimental conditions over time, use of different laboratories or instruments, or different analysis pipelines [74]. These effects are notoriously common in omics data and can introduce noise that dilutes biological signals, reduces statistical power, or generates misleading results [74]. When integrated into cancer biomarker research, these variables can significantly impact the reliability of assays intended for diagnosis, prognosis, and therapeutic monitoring.
Reagent variability, particularly lot-to-lot variance (LTLV), presents another critical challenge for biomarker assay reproducibility. Immunoassays—widely used in clinical practice and modern biomedical research—are plagued by LTLV, which negatively affects assay accuracy, precision, and specificity [75]. This variance can arise from fluctuations in raw material quality and deviations in manufacturing processes, with estimates suggesting that 70% of an immunoassay's performance is attributed to raw materials, while the remaining 30% depends on production processes [75]. For cancer biomarker validation, this variability introduces substantial challenges in maintaining consistent analytical performance over time.
This comparison guide objectively evaluates current methodologies for managing these critical variables, providing researchers with experimental data and protocols to enhance the reproducibility of their cancer biomarker assays.
Batch effects can emerge at every step of a high-throughput study, with specific manifestations across different analytical platforms. The table below summarizes the primary sources of batch effects across experimental workflows:
Table 1: Major Sources of Batch Effects in Cancer Biomarker Research
| Source Category | Specific Examples | Affected Omics Types | Impact on Biomarkers |
|---|---|---|---|
| Study Design | Flawed or confounded design; Minor treatment effect size | Common across all types | Reduces ability to distinguish biological signals from batch effects |
| Sample Processing | Centrifugal force variations; Storage temperature and duration | Proteomics, Metabolomics, Transcriptomics | Alters mRNA, protein, and metabolite stability |
| Instrumentation | Different scanners (PET/CT); Platform models | Radiomics, Genomics, Transcriptomics | Affects texture parameters, sequencing depth, and signal quantification |
| Reagent Lots | Different antibody batches; Enzyme activity variations | Immunoassays, Proteomics | Impacts sensitivity, specificity, and quantitation accuracy |
| Personnel & Timing | Different operators; Processing across multiple days | All types | Introduces systematic technical variations |
Documented Impacts on Cancer Biomarker Research
The profound negative impacts of batch effects are well-documented in oncology research. In clinical trials, batch effects introduced by a change in RNA-extraction solution resulted in shifted gene expression profiles, leading to incorrect classification outcomes for 162 patients, 28 of whom received incorrect or unnecessary chemotherapy regimens [74]. Similarly, in cross-species studies, apparent differences between human and mouse gene expression were initially attributed to biological factors but were later shown to derive primarily from batch effects related to different data generation timepoints separated by three years [74].
The challenges are particularly pronounced in emerging technologies. Single-cell RNA sequencing (scRNA-seq), which provides unprecedented resolution for exploring tumor heterogeneity, suffers from higher technical variations compared to bulk RNA-seq, with lower RNA input, higher dropout rates, and increased cell-to-cell variations [74]. These factors make batch effects more severe in single-cell data, complicating the identification of rare cell populations that might serve as crucial biomarkers for cancer progression [74] [76].
Comparative Analysis of Batch Effect Correction Methods
Multiple computational and experimental approaches have been developed to address batch effects in cancer biomarker research. These methods range from experimental design-based approaches to computational corrections applied during data analysis. The selection of an appropriate method depends on the specific omics platform, study design, and the nature of the batch effects present.
Performance Comparison of Statistical Correction Methods
A recent comparative analysis of batch correction methods for FDG PET/CT radiogenomic data in lung cancer patients provides valuable experimental insights into method performance [77]. This study evaluated three correction approaches: phantom correction (a conventional method that unifies parameters from different instruments based on value ratios), ComBat (an empirical Bayes framework), and Limma (a linear modeling-based approach). The researchers assessed performance using multiple metrics including principal component analysis (PCA), the k-nearest neighbor batch effect test (kBET), and silhouette scores.
Table 2: Performance Comparison of Batch Effect Correction Methods in Radiogenomic Data
| Correction Method | kBET Rejection Rate | Silhouette Score | Association with TP53 Mutations | Key Advantages | Limitations |
|---|---|---|---|---|---|
| Uncorrected Data | High | Low | Limited significant associations | No data transformation required | Strong batch effects mask biological signals |
| Phantom Correction | Lower than uncorrected | Lower than uncorrected | Moderate associations | Physical standardization | Limited effectiveness for complex batch effects |
| ComBat Method | Low | Low | More significant associations | Handles multiple batch types | May over-correct and remove biological signal |
| Limma Method | Low | Low | More significant associations | Linear model framework; Flexible covariate inclusion | Assumes linear batch effects |
The study demonstrated that both ComBat and Limma methods effectively reduced batch effects, with no significant difference between their performance metrics [77]. Notably, after applying these correction methods, more texture features exhibited significant associations with TP53 mutations—a critical cancer biomarker—than in phantom-corrected or uncorrected data [77]. This finding highlights how effective batch effect correction can enhance the discovery and validation of biologically relevant biomarkers in cancer research.
Reagent Variability: Challenges and Mitigation Strategies
Reagent variability, particularly lot-to-lot variance (LTLV), presents a formidable challenge in maintaining consistency in cancer biomarker assays. LTLV can arise from several factors, including variations in the quality, stability, and manufacturing processes of key reagents [75]. In immunoassays—a cornerstone technology for cancer biomarker detection—these variations significantly impact the accuracy, precision, and overall performance of assays [75].
The clinical consequences of undetected LTLV can be severe. Documented cases include:
- HbA1c testing: A change in reagent lot led to an average increase in patient results of 0.5%, potentially causing incorrect diabetes diagnoses and inappropriate medication initiation [78].
- PSA testing: Falsely elevated PSA results due to LTLV caused undue concern for post-prostatectomy patients, as such results would suggest cancer recurrence [78].
- IGF-1 testing: Discrepancies went unnoticed despite evaluation procedures, requiring clinician reports of unusually large numbers of discrepant results to identify the problem [78].
Critical Reagents Contributing to Variability
Understanding the specific reagents that contribute most significantly to variability enables more targeted quality control approaches. The following table summarizes key reagents and their potential impacts on assay performance:
Table 3: Key Reagent Sources of Lot-to-Lot Variability in Biomarker Assays
| Reagent Type | Specifications Leading to LTLV | Impact on Assay Performance | Quality Assessment Methods |
|---|---|---|---|
| Antibodies | Unclear appearance; Low concentration; High aggregation; Low purity | Reduced specificity; High background; Signal leap | SDS-PAGE; SEC-HPLC; CE-SDS; Activity testing |
| Enzymes (HRP, ALP) | Inconsistent enzymatic activity; Purity variations | Altered reaction kinetics; Sensitivity drift | Activity unit measurement; Purity verification |
| Antigens/Calibrators | Aggregate formation; Improper storage buffer; Truncated synthetic peptides | Standard curve shifts; Accuracy degradation | Purity analysis; Stability testing |
| Solid Phases | Inhomogeneous magnetic beads; Unclean containers | Binding capacity variations; Increased background | Microscopic inspection; Consistency testing |
Research has demonstrated that even minor impurities in critical reagents can substantially impact assay performance. For instance, when a monoclonal antibody for CTX-III was transitioned from hybridoma to recombinant production with identical amino acid sequences, the recombinant antibody showed substantially lower sensitivity and maximal signals despite adequate purity (98.7%) by SEC-HPLC [75]. Further analysis revealed nearly 13% impurity by CE-SDS, primarily consisting of a single light chain, two heavy chains with one light chain (2H1L), two heavy chains (2H), and nonglycosylated IgG [75]. This case highlights the importance of implementing multiple orthogonal methods for evaluating critical reagent quality.
Experimental Protocols for Managing Technical Variability
Protocol for Evaluating New Reagent Lots
The clinical laboratory standard for evaluating new reagent lots involves a systematic comparison process using patient samples [78]. The protocol includes:
Establish Acceptance Criteria: Determine critical differences based on medical needs or biological variation requirements rather than arbitrary percentages. The Clinical and Laboratory Standards Institute (CLSI) recommends choosing criteria based on the updated Milan criteria for defining analytical performance specifications [78].
Sample Selection: Collect 20-40 native patient samples spanning the analytical measurement range of the assay. Avoid using only internal quality control (IQC) or external quality assurance (EQA) materials due to commutability issues [78].
Testing Procedure: Analyze all samples in duplicate with both current and new reagent lots in the same run, using the same instrument and operator to minimize additional variables.
Statistical Analysis: Perform regression analysis (Passing-Bablok or Deming) and Bland-Altman plots to assess systematic and proportional differences.
Decision Making: Accept the new lot if differences fall within predetermined acceptance criteria. If not, contact the manufacturer and continue using the current lot until resolution.
This protocol emphasizes the use of patient samples rather than quality control materials alone, as evidence demonstrates significant differences between IQC material and patient serum in 40.9% of reagent lot change events [78].
Protocol for Batch Effect Assessment and Correction in Omics Data
For omics data (genomics, transcriptomics, proteomics), the following protocol provides a standardized approach for batch effect management:
Experimental Design: Implement blocking strategies by including samples from different experimental groups in each batch. Randomize processing order to avoid confounding biological and technical effects [74].
Quality Control: Perform pre-correction visualization using Principal Component Analysis (PCA) and hierarchical clustering to identify batch-associated clustering.
Batch Effect Quantification: Apply quantitative metrics including:
Batch Effect Correction: Select an appropriate correction method based on data type:
Post-Correction Validation: Verify that correction preserves biological signals by testing known biological relationships and assessing positive controls.
Visualization of Batch Effect Management Workflow
The following diagram illustrates a comprehensive workflow for managing batch effects and reagent variability in cancer biomarker studies:
Batch Effect Management Workflow
Implementing robust practices for managing batch effects and reagent variability requires specific tools and resources. The following table summarizes key solutions for maintaining reproducibility in cancer biomarker research:
Table 4: Essential Research Reagent Solutions for Reproducible Biomarker Assays
| Tool Category | Specific Examples | Function in Managing Variability | Application Context |
|---|---|---|---|
| Quality Assessment Platforms | SEC-HPLC; CE-SDS; SDS-PAGE | Evaluate critical quality attributes of antibodies and proteins | Pre-use verification of critical reagents |
| Reference Materials | WHO International Standards; Master Calibrators | Provide standardization across laboratories and platforms | Assay calibration and harmonization |
| Batch Correction Software | ComBat; Limma; sva package in R | Statistical adjustment for technical variations | Post-hoc correction of omics data |
| Stability Monitoring Systems | Real-time stability chambers; Temperature loggers | Track reagent storage conditions and shelf life | Preventive quality assurance |
| Data Visualization Tools | PCA; Hierarchical clustering; kBET | Identify and quantify batch effects in multivariate data | Quality control of large datasets |
Achieving reproducibility in cancer biomarker research requires a systematic, multi-faceted approach to managing batch effects and reagent variability. The comparative analysis presented in this guide demonstrates that statistical correction methods like ComBat and Limma can effectively reduce batch effects in complex data types, while rigorous reagent evaluation protocols using patient samples are essential for managing lot-to-lot variation.
As the field advances toward increasingly complex multi-omics approaches and liquid biopsy applications [18] [49], the principles of robust analytical validation become even more critical. By implementing the standardized protocols, quality control measures, and correction strategies outlined in this guide, researchers can significantly enhance the reliability and reproducibility of cancer biomarker assays, ultimately supporting more accurate diagnosis, prognosis, and treatment selection in oncology.
The accurate detection of low-abundance biomarkers is a cornerstone of modern precision oncology, directly influencing early cancer diagnosis, treatment selection, and patient outcomes. Sensitivity—the ability of an assay to detect the smallest possible amount of a target biomarker—is often the critical differentiator between early intervention and missed diagnostic opportunities [79]. In clinical settings, highly sensitive immunoassays can identify biomarkers at the earliest stages of disease, enabling timely therapeutic intervention and significantly improving survival rates [79] [80]. The challenge intensifies with biomarkers such as circulating tumor DNA (ctDNA), which exist in minute quantities amidst a complex background of biological molecules in biofluids [80] [18].
The field of biomarker detection is undergoing rapid transformation, driven by innovations in signal amplification, molecular technologies, and biosensor design. This guide objectively compares the performance of current and emerging techniques, providing researchers and drug development professionals with experimental data and protocols to inform their assay development strategies. From optimized immunoassays to next-generation sequencing (NGS) and innovative enrichment techniques like sonobiopsy, we examine the methodologies pushing the boundaries of detection sensitivity in cancer biomarker research.
Fundamental Principles for Optimizing Assay Sensitivity
Optimizing sensitivity requires a multifaceted approach that begins with reagent selection and assay design. Two foundational properties profoundly impact assay performance: antibody affinity and specificity.
Antibody Affinity and Specificity: Antibody affinity refers to the strength of interaction between an antibody and its specific antigen. High-affinity antibodies bind more tightly to their targets, which is crucial for capturing low-abundance biomarkers and preventing dissociation during wash steps [79]. This strong binding ensures that even minute quantities of antigen are effectively captured, leading to a detectable signal. Equally important is antibody specificity—the precision with which an antibody recognizes its intended target without cross-reacting with other molecules [79]. Poor specificity can lead to false positives from cross-reactivity, compromising assay accuracy. Achieving an optimal balance is essential; an antibody with high affinity but poor specificity may bind non-target molecules, while a highly specific antibody with low affinity might miss low-concentration targets [79].
Signal Amplification Systems: Signal amplification techniques enhance the detectable signal generated from the binding event, making minimal antigen quantities measurable. Common amplification methods include:
- Enzyme-Linked Amplification: Used extensively in ELISA formats, enzymes like horseradish peroxidase (HRP) or alkaline phosphatase (AP) catalyze reactions that produce colorimetric, fluorescent, or chemiluminescent signals [79].
- Chemiluminescence: This method involves chemical reactions that produce light, measured by a luminometer. It typically offers higher sensitivity than colorimetric methods due to more intense signal production [79].
- Fluorescence-Based Detection: Fluorophores conjugated to antibodies emit light at specific wavelengths when excited. This approach provides high sensitivity and enables multiplexing but requires specialized detection equipment [79].
- Nanoparticle-Based Amplification: Nanoparticles (e.g., gold nanoparticles or quantum dots) conjugated to antibodies offer ultra-high sensitivity and stability, making them ideal for point-of-care diagnostics [79].
The following diagram illustrates the core decision-making workflow for developing a highly sensitive detection assay, integrating these key considerations:
Established and Emerging Detection Technologies
Advanced Immunoassay Platforms
Microfluidic-Enhanced Lateral Flow Immunoassays (LFIA): Traditional LFIAs are valued for rapid results and ease of use but often suffer from limited sensitivity. Recent innovations integrate LFIAs with microfluidic chips to precisely control fluid dynamics, significantly enhancing performance. One optimized microfluidic biosensor for C-Reactive Protein (CRP) detection demonstrated a measurable range of 1–70 μg/mL by implementing a one-step detection system that eliminates separate buffer solution requirements [81]. This approach minimizes non-specific binding by restricting the nitrocellulose (NC) pad to just the detection test line, improving sensitivity while reducing reagent use and fabrication complexity [81]. The platform successfully employed both gold nanoparticles for visual detection (1–10 μg/mL) and fluorescent labels for expanded quantitative range (1–70 μg/mL), showcasing how detection label choice impacts assay capabilities [81].
Experimental Protocol: Microfluidic LFIA with Fluorescent Detection
- Device Fabrication: Microfluidic chips are designed with channels leading to a pre-blocked nitrocellulose detection zone. The conjugate pad is eliminated by directly applying and drying fluorescently-labeled antibodies (e.g., from Proteintech) within the microchannel [81].
- Assay Procedure: Apply the sample (serum/plasma) to the inlet. Capillary action drives the fluid through the channel, where it rehydrates and mixes with the detection antibodies. The complex migrates to the test line containing capture antibodies. Fluid flow is precisely controlled by channel geometry without external buffers [81].
- Signal Measurement: After a 15-minute incubation, quantify fluorescence intensity at the test line using a 16-bit CCD imaging system (e.g., Olympus). CRP concentration correlates directly with fluorescence intensity [81].
- Key Optimization: A dual-blocking approach using BSA and casein significantly reduces background noise. Pre-blocking the NC pad streamlines the process to a single step [81].
Molecular and Sequencing-Based Approaches
Comprehensive Molecular Profiling with NGS: Next-generation sequencing technologies have revolutionized cancer biomarker detection by enabling comprehensive molecular profiling from minimal tissue inputs. The MI Cancer Seek assay exemplifies this advancement, utilizing simultaneous whole exome and whole transcriptome sequencing from a single total nucleic acid extraction [32] [82]. This FDA-approved test requires only 50 ng of DNA input from formalin-fixed paraffin-embedded (FFPE) tissue with minimum 20% tumor content and achieves an average sequencing depth of 230× for the whole exome, 1,000× for 720 clinically relevant genes, and 1,500× for 228 reportable genes [32]. RNA is sequenced to a minimum of 1.37 million total mapped reads, providing both genomic and transcriptomic information from a single, small sample [32].
The assay demonstrates exceptional clinical performance, with >97% negative and positive percent agreement compared to other FDA-approved companion diagnostics for biomarkers including PIK3CA alterations in breast cancer, BRAF V600E mutations in colorectal cancer and melanoma, and EGFR mutations in non-small cell lung cancer [32] [82]. It also accurately identifies microsatellite instability (MSI) status, a key predictor of immunotherapy response [82].
Liquid Biopsy and Circulating Biomarkers: Liquid biopsy represents a paradigm shift in non-invasive cancer detection by analyzing circulating biomarkers such as ctDNA, circulating tumor cells (CTCs), and exosomes in blood [80] [18]. However, the extreme scarcity of these biomarkers in early-stage disease remains a significant challenge. Digital droplet PCR (ddPCR) and optimized NGS protocols have enhanced detection sensitivity, but intrinsic limitations persist due to low biomarker concentration and an inability to localize the anatomical origin of the disease [83].
Innovative Enrichment and Sensing Technologies
Sonobiopsy for Biomarker Enrichment: Sonobiopsy addresses fundamental limitations of conventional liquid biopsy by integrating focused ultrasound (FUS) to locally enrich circulating biomarkers from ultrasound-targeted disease regions [83]. This technique uses various FUS modalities—including thermal ablation, histotripsy, and FUS combined with microbubbles—to disrupt cell and vessel barriers in a controlled manner, facilitating the release of biomarkers into circulation immediately before blood collection [83]. The approach provides three unique advantages: (1) enrichment of circulating biomarkers from the target tissue, (2) spatial targeting with millimeter resolution to localize the biomarker source, and (3) temporal control to account for the short half-lives of circulating biomarkers (e.g., cfDNA half-life of 16 minutes to 2.5 hours) [83].
In preclinical studies, sonobiopsy with FUS and microbubbles enhanced the detection of brain cancer-derived biomarkers like EGFRvIII mutation in ctDNA by over 4-fold compared to conventional liquid biopsy [83]. Clinical translation is underway, with demonstrated safety in patients with Alzheimer's disease, amyotrophic lateral sclerosis, and glioblastoma [83].
Molecularly Imprinted Polymer (MIP) Biosensors: MIP-based biosensors offer an alternative to antibody-based detection by creating artificial recognition sites complementary to target biomarker shapes and functional groups. These sensors demonstrate remarkable sensitivity and selectivity for cancer biomarkers including CEA, AFP, CA 125, PSA, and CA 15-3 [84]. When combined with electrochemical, optical, or mass-sensitive transducers, MIP biosensors achieve low limits of detection (LOD) suitable for clinical applications, with advantages including high stability, reusability, and cost-effectiveness compared to biological recognition elements [84].
Comparative Performance Analysis of Detection Techniques
Table 1: Comparison of Sensitivity and Performance Characteristics Across Detection Platforms
| Technology | Detection Principle | Key Biomarkers Detected | Sensitivity/LOD | Sample Requirements | Multiplexing Capability |
|---|---|---|---|---|---|
| Microfluidic LFIA [81] | Immunoassay with fluorescent detection | CRP | 1 μg/mL (full range 1-70 μg/mL) | Low volume serum/plasma | Limited |
| MI Cancer Seek NGS [32] [82] | Whole exome & transcriptome sequencing | PIK3CA, BRAF V600E, EGFR, MSI, TMB | 50 ng DNA input; >97% agreement with FDA CDx | FFPE tissue (50 ng, 20% tumor) | High (20,859 genes) |
| Sonobiopsy-Enhanced Liquid Biopsy [83] | Ultrasound-enabled biomarker enrichment | ctDNA, proteins, EVs | 4-fold increase in EGFRvIII ctDNA detection | Blood post-FUS treatment | Medium |
| MIP-Based Biosensors [84] | Synthetic polymer recognition | CEA, AFP, CA 125, PSA | Variable (sub-nanogram levels demonstrated) | Serum, minimal processing | Low to Medium |
Table 2: Analysis of Technical Requirements and Implementation Challenges
| Technology | Equipment Needs | Assay Time | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Microfluidic LFIA [81] | Microfluidic chip, fluorescence reader | <20 minutes | Simplified workflow, cost-effective, POC suitability | Limited multiplexing, requires optimization for each biomarker |
| MI Cancer Seek NGS [32] [82] | NGS platform, bioinformatics infrastructure | Several days | Comprehensive profiling, high multiplexing, FDA-approved CDx | High cost, complex data analysis, tissue requirement |
| Sonobiopsy-Enhanced Liquid Biopsy [83] | Focused ultrasound system, standard liquid biopsy platforms | Hours (including FUS treatment) | Spatially targeted, enhances sensitivity of downstream assays | Requires specialized ultrasound equipment, clinical translation ongoing |
| MIP-Based Biosensors [84] | Electrochemical or optical reader | Minutes to hours | High stability, reusable, cost-effective | Complex polymer optimization, potential non-specific binding |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Sensitive Biomarker Detection Assays
| Reagent/Material | Function | Application Examples | Considerations for Sensitivity Optimization |
|---|---|---|---|
| High-Affinity Antibodies [79] | Specific biomarker recognition | Immunoassays, LFIA, microfluidics | Affinity screening essential; recombinant antibodies offer better batch-to-batch consistency |
| Signal Amplification Labels (Enzymes, nanoparticles, fluorophores) [79] [81] | Signal generation and amplification | HRP/AP for colorimetric/chemiluminescent assays; gold nanoparticles; quantum dots | Choice impacts sensitivity: chemiluminescent > fluorescent > colorimetric |
| Blocking Agents (BSA, casein, PEG) [81] | Minimize non-specific binding | Microfluidic assays, LFIA, ELISA | Dual-blocking approaches (e.g., BSA + casein) can significantly reduce background noise |
| Microfluidic Chip Components (NC membranes, channel substrates) [81] | Controlled fluid movement and reaction | Microfluidic LFIA, POC devices | Pre-blocking NC pads eliminates buffer addition steps, simplifying workflow |
| NGS Library Prep Kits [32] | Nucleic acid preparation for sequencing | Whole exome/transcriptome sequencing | Simultaneous DNA/RNA extraction maximizes tissue utilization from limited samples |
| Molecularly Imprinted Polymers [84] | Synthetic biomarker recognition | Biosensors for CEA, AFP, PSA | Offer antibody-like specificity with enhanced stability and lower cost |
| FUS Microbubbles/Nanodroplets [83] | Ultrasound cavitation nuclei | Sonobiopsy for biomarker enrichment | Lower acoustic pressure requirements for tissue barrier disruption |
Integrated Workflow and Future Perspectives
The following diagram illustrates how advanced techniques like sonobiopsy are integrated with established detection methods to create highly sensitive diagnostic workflows:
The field of sensitive biomarker detection is advancing toward multi-modal approaches that combine enrichment strategies with sophisticated detection technologies. Artificial intelligence and machine learning are increasingly employed to identify subtle patterns in complex datasets, enhancing diagnostic accuracy beyond what conventional analysis achieves [18]. Multi-cancer early detection (MCED) tests like the Galleri test, which analyzes ctDNA to detect over 50 cancer types simultaneously, represent the next frontier in population-scale screening [18].
For researchers optimizing sensitivity in biomarker assays, the integration of complementary technologies appears most promising—using techniques like sonobiopsy to enrich biomarker availability before applying ultra-sensitive detection platforms such as advanced NGS or multiplex immunoassays. As these technologies mature and validation frameworks standardize, the detection of low-abundance biomarkers will continue to transform from a technical challenge to a routine clinical capability, ultimately enabling earlier cancer diagnosis and more personalized therapeutic interventions.
Pre-analytical variables—encompassing sample collection, processing, and storage conditions—represent a critical frontier in the analytical validation of cancer biomarker assays. For researchers and drug development professionals, inconsistent handling during these initial stages can alter the molecular integrity of biospecimens, leading to unreliable data, failed validation studies, and ultimately, compromised clinical decisions [85]. This guide objectively compares the effects of different pre-analytical conditions on various biomarker types, providing a synthesized overview of supporting experimental data to inform robust biospecimen protocols.
Comparative Analysis of Pre-Analytical Variable Impacts
The effects of pre-analytical variables are highly dependent on the specific biomarker type and analytical platform. The tables below summarize key experimental findings on how different variables influence biomarker stability and measurement.
Table 1: Impact of Pre-Analytical Variables on Different Biomarker Types
| Pre-Analytical Variable | Biomarker Type | Key Experimental Findings | Magnitude of Effect |
|---|---|---|---|
| Cold Ischemic Time (Delay to Fixation) | Phosphoproteins [85] | Marked degradation and altered detection in tissue specimens. | Effect is protein-specific; ≤1 hour is often critical for phosphoproteins [85]. |
| Immunohistochemistry (IHC) Targets [85] | Altered antigen detection, impacting diagnostic accuracy (e.g., ER/PR status in breast cancer). | ≤12 hours often recommended, but optimal time is biomarker-dependent [85]. | |
| Sample Storage Temperature | Metabolites & Proteins [86] | 15 out of 193 serum analytes were significantly affected by sub-optimal storage. | Glutamate/glutamine ratio >0.20 identified as an indicator of -20°C storage [86]. |
| Serum Tumor Markers (e.g., CA 15-3) [87] | Measured concentrations increased after long-term storage. | ~15% increase over 10 years of storage, leading to biased association estimates [87]. | |
| Tumor Sample Heterogeneity | Gene Expression [88] | Thousands of genes showed a >2-fold change in expression when tumor cell proportion was low. | Average of 5,707 genes with 2-fold change; REO consistency remained high at 89.24% [88]. |
| Preservation Method (FFPE vs. Fresh-Frozen) | Gene Expression [88] | Significant differences in quantitative gene expression measurements. | Thousands of genes with 2-fold changes; REO consistency around 82-86% [88]. |
| Next-Generation Sequencing [85] | Delay to fixation, formalin time, and pH can alter variant calls and microsatellite instability signals. | Number of nucleotide variants identified is affected by pre-analytical factors [85]. |
Table 2: Impact of Pre-Analical Variables on Gene Expression Robustness [88]
| Pre-Analytical Variable | Average Number of Genes with 2-Fold Change | Average REO Consistency Score | Consistency After Excluding 10% Closest Pairs |
|---|---|---|---|
| Sampling Method (Biopsy vs. Surgery) | 3,286 | 86% | 89.90% |
| Tumor Heterogeneity (Low vs. High Purity) | 5,707 | 89.24% | 92.46% |
| Fixation Delay (48h vs. 0h) | 2,970 | 85.63% | 88.84% |
| Preservation (FFPE vs. Fresh-Frozen) | Data not specified in excerpt | ~82-86% | Data not specified in excerpt |
Experimental Protocols for Key Pre-Analical Studies
- Objective: To document metabolites and proteins in serum affected by long-term storage at -20°C versus -80°C.
- Sample Type: Non-fasting serum samples from 16 individuals with type 1 diabetes (split-aliquots).
- Experimental Design: Matched paired samples from the same individual were stored for a median of 4.2 years at either -20°C or -80°C without prior freeze-thaw cycles.
- Analytical Platforms:
- Liquid Chromatography Tandem Mass Spectrometry (LC-MS/MS): Quantified 269 analytes (122 metabolites and ratios, 147 tryptic peptides).
- Luminex Platform: Quantified 31 protein concentrations.
- Statistical Analysis:
- Pairwise Comparison: Paired t-test or Wilcoxon signed-rank test to quantify the significance of differences between storage conditions for each analyte.
- Effect Size Score: ( Sd = \mud / \sigmad ), where ( \mud ) is the mean difference and ( \sigma_d ) is the standard deviation of the difference.
- Discriminatory Power: Receiver Operating Characteristics (ROC) analysis to evaluate each analyte's ability to classify storage temperature.
- Objective: To assess the effect of ten pre-analytical variables on gene expression measurements and Relative Expression Orderings (REOs).
- Data Collection: Analyzed 18 public datasets containing over 800 paired samples from the same patient, where one sample was exposed to a suboptimal condition (case) and the other was a high-quality control.
- Variables Tested: Sampling methods, tumor heterogeneity, fixation delays, preservation conditions, degradation levels, RNA extraction kits, amplification kits, RNA quantity, measuring platforms, and laboratory sites.
- Differential Expression Analysis:
- Fold Change (FC): Calculated for each gene between paired case and control samples (( FC = \frac{exper(B)}{exper(A)} )).
- Differentially Expressed Genes (DEGs): Defined as genes with FC > 2.
- REO Consistency Analysis:
- Gene Pairs: The relative order (Gi > Gj or Gi < Gj) of all possible gene pairs was compared between paired samples.
- Consistency Score: Calculated as ( \frac{N}{N+M} ), where N is the number of gene pairs with consistent REOs and M is the number with reversed REOs.
Research Reagent Solutions for Pre-Analytical Stabilization
Table 3: Essential Materials for Biospecimen Research
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Formalin, Buffered | Tissue fixation for histopathology and FFPE block creation. | pH and buffer composition are critical to minimize biomolecule degradation [85]. |
| RNAlater or Similar RNA Stabilization Solution | Preserves RNA integrity in tissues and cells by inhibiting RNases. | Crucial for maintaining accurate gene expression profiles when immediate freezing is not possible [88]. |
| PAXgene Blood RNA Tubes | Stabilizes intracellular RNA in whole blood for transcriptomic studies. | Standardizes the pre-analytical phase for blood-based biomarkers [88]. |
| Luminex Bead-Based Assay Kits | Multiplexed quantification of proteins in serum/plasma. | Used to evaluate the stability of protein biomarkers under different storage conditions [86]. |
| LC-MS/MS Kits for Metabolomics | Targeted quantification of small molecule metabolites. | Enables assessment of metabolite stability in serum/plasma under varying pre-analytical conditions [86]. |
| FDA-Approved IHC Assays (e.g., Dako 22C3, Ventana SP142) | Standardized detection of protein biomarkers (e.g., PD-L1) in FFPE tissue. | Used to evaluate impact of cold ischemia and fixation on critical immunotherapy biomarkers [85]. |
Visualizing Pre-Analytical Workflows and Impacts
The following diagrams, generated using Graphviz, illustrate the experimental workflow for a stability study and the comparative robustness of different biomarker measurements.
Experimental Workflow for Stability Study
Robustness of Biomarker Types
The journey from biospecimen collection to data generation is fraught with variables that can significantly impact the analytical validity of cancer biomarker assays. The experimental data synthesized herein demonstrates that while absolute quantification of biomarkers (e.g., gene expression levels, specific protein concentrations) is highly susceptible to variations in collection, stabilization, and storage, alternative approaches like Relative Expression Orderings (REOs) may offer greater robustness [88]. For serum-based studies, storage at -80°C is strongly preferred over -20°C for long-term preservation of many metabolites and proteins [86]. Ultimately, standardizing and validating pre-analytical protocols against intended endpoint assays is not merely a best practice but a fundamental requirement for generating reliable, reproducible data that can confidently inform drug development and clinical decision-making [85] [14].
Proving Performance: Validation Parameters and Technology Benchmarking
The successful clinical translation of cancer biomarkers is critically dependent on robust analytical validation, which confirms that an assay reliably measures the intended biomarker with sufficient precision, accuracy, and reproducibility for its specific intended use [89] [90]. In the field of precision oncology, where biomarkers guide critical treatment decisions, establishing key performance parameters is not merely a regulatory formality but a fundamental requirement for ensuring patient safety and therapeutic efficacy [91] [9]. The "fit-for-purpose" approach to validation has gained prominence, emphasizing that the level of validation rigor should be commensurate with the intended clinical application of the biomarker [90]. This paradigm promotes flexible yet scientifically rigorous method development, acknowledging that biomarkers serve different functions across the drug development continuum—from early pharmacodynamic markers to definitive diagnostic tests [89].
The validation journey is complex, with only approximately 0.1% of potentially clinically relevant cancer biomarkers described in literature progressing to routine clinical use [92] [9]. This high attrition rate underscores the critical importance of establishing robust performance parameters early in development. The international standard for analytical method validation is "the confirmation by examination and the provision of objective evidence that the particular requirements for a specific intended use are fulfilled" [89] [90]. This definition anchors validation efforts to the biomarker's specific clinical context, ensuring that performance parameters are clinically relevant rather than merely technically achievable.
Defining Key Performance Parameters
Core Definitions and Relationships
The analytical validation of cancer biomarker assays rests on four fundamental performance parameters: accuracy, precision, sensitivity, and specificity. Each parameter provides distinct yet complementary information about assay performance, collectively forming a comprehensive picture of analytical capability [14] [89].
Accuracy represents the closeness of agreement between a measured value and the true value of the analyte. It is typically expressed as percent deviation from the nominal concentration and reflects the total error in the method, encompassing both systematic and random error components [90]. In practice, accuracy is determined by analyzing samples with known concentrations (validation samples) and calculating the mean percentage deviation from the expected value [89].
Precision describes the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions. Precision is usually expressed as the coefficient of variation (%CV) and can be examined at three levels: repeatability (within-run precision), intermediate precision (within-laboratory variations), and reproducibility (between-laboratory precision) [89] [90].
Sensitivity encompasses two related concepts: analytical sensitivity refers to the lowest concentration of an analyte that can be reliably distinguished from zero, often defined as the lower limit of quantitation (LLOQ), while clinical sensitivity represents the proportion of individuals with the target condition who test positive (true positive rate) [14].
Specificity also has dual aspects: analytical specificity refers to the ability of the assay to measure the analyte unequivocally in the presence of interfering substances, while clinical specificity represents the proportion of individuals without the target condition who test negative (true negative rate) [14].
Performance Metrics for Biomarker Evaluation
Beyond the core parameters, several derived metrics are essential for comprehensive biomarker evaluation:
- Positive Predictive Value (PPV): The proportion of test-positive patients who actually have the disease
- Negative Predictive Value (NPV): The proportion of test-negative patients who truly do not have the disease
- Receiver Operating Characteristic (ROC) Curve: A plot of sensitivity versus 1-specificity across all possible threshold values
- Area Under the Curve (AUC): A measure of overall discriminatory power, ranging from 0.5 (no discrimination) to 1.0 (perfect discrimination) [14]
These metrics are particularly important for clinical validation, where the correlation between the biomarker result and clinical outcomes is established [14] [93].
Performance Standards Across Assay Categories
Fit-for-Purpose Validation Framework
The American Association of Pharmaceutical Scientists (AAPS) and the US Clinical Ligand Society have established five general classes of biomarker assays, each with distinct validation requirements [89] [90]. This classification recognizes that different technologies and clinical applications demand tailored validation approaches, moving beyond a one-size-fits-all model.
Table 1: Biomarker Assay Categories and Validation Focus
| Assay Category | Description | Key Validation Parameters |
|---|---|---|
| Definitive Quantitative | Uses calibrators and regression model to calculate absolute quantitative values; reference standard fully characterized and representative of biomarker | Accuracy, precision, sensitivity, specificity, dynamic range, LLOQ, ULOQ |
| Relative Quantitative | Uses response-concentration calibration with reference standards not fully representative of biomarker | Precision, sensitivity, specificity, dynamic range (relative values) |
| Quasi-Quantitative | No calibration standard; continuous response expressed in terms of sample characteristics | Precision, specificity, sensitivity, dynamic range |
| Qualitative (Categorical) | Ordinal (discrete scoring scales) or nominal (yes/no situations) | Precision, specificity, sensitivity (as categorical classifications) |
Acceptance Criteria for Quantitative Assays
For definitive quantitative biomarker methods, recognized performance standards have been established, though more flexibility is generally allowed compared to small molecule bioanalysis [90]. During pre-study validation, each assay is typically evaluated on a case-by-case basis, with 25% being the default value for precision and accuracy (30% at the LLOQ) [90]. These criteria may be tightened or relaxed based on the biological variability of the biomarker and its intended clinical use.
The Societe Francaise des Sciences et Techniques Pharmaceutiques (SFSTP) has advocated for an "accuracy profile" approach that accounts for total error (bias and intermediate precision) along with pre-set acceptance limits defined by the user [90]. This method produces a β-expectation tolerance interval that displays the confidence interval for future measurements, allowing researchers to visually check what percentage of future values are likely to fall within pre-defined acceptance limits.
Experimental Protocols for Parameter Establishment
Protocol for Establishing Accuracy and Precision
A standardized approach for determining accuracy and precision involves repeated analyses of validation samples at multiple concentrations spanning the expected range of the assay:
Sample Preparation: Prepare validation samples (VS) at a minimum of three concentrations (low, medium, high) representing the calibration range, plus LLOQ and ULOQ samples.
Experimental Design: Analyze each VS in triplicate on at least three separate days to capture within-run and between-run variability.
Data Analysis:
- Calculate mean measured concentration for each VS level
- Determine accuracy as (mean measured concentration/nominal concentration) × 100%
- Calculate precision as %CV for within-run and between-run measurements
- For biomarker assays, ≤25% deviation for accuracy and ≤25% CV for precision are generally acceptable, except at LLOQ where ≤30% may be permitted [90]
Total Error Assessment: Combine random and systematic error components to evaluate whether the method meets the predefined acceptance limits for its intended purpose [90].
Protocol for Determining Sensitivity and Specificity
The establishment of clinical sensitivity and specificity follows a different pathway centered on clinical sample analysis:
Sample Cohort Selection: Implement a Prospective-Specimen-Collection, Retrospective-Blinded-Evaluation (PRoBE) design, where specimens are collected prospectively from a cohort representing the target population before outcome ascertainment [94].
Blinded Analysis: After outcome status is determined, randomly select case patients and control subjects from the cohort and assay their specimens in a fashion blinded to case-control status.
Statistical Analysis:
- Calculate sensitivity as (True Positives / [True Positives + False Negatives]) × 100
- Calculate specificity as (True Negatives / [True Negatives + False Positives]) × 100
- Generate ROC curves by plotting sensitivity versus 1-specificity across all possible threshold values
- Determine AUC as a measure of overall discriminatory power [14]
Validation: Establish performance in an independent sample set to verify initial findings and minimize overfitting.
Analytical Workflow Visualization
Biomarker Validation Workflow with Key Parameters
Technology Comparison and Performance Data
Analytical Platforms for Biomarker Validation
Different technology platforms offer varying strengths for biomarker validation, with selection dependent on the required sensitivity, specificity, throughput, and multiplexing capability:
Table 2: Technology Platform Comparison for Biomarker Analysis
| Technology Platform | Sensitivity | Multiplexing Capability | Dynamic Range | Best Applications |
|---|---|---|---|---|
| ELISA | Moderate | Low (single-plex) | Moderate (~2 logs) | High-abundance proteins; confirmation studies |
| Meso Scale Discovery (MSD) | High (up to 100x ELISA) | Medium (10-plex typically) | Broad | Cytokines; low-abundance biomarkers |
| LC-MS/MS | High | Medium (multiplexed) | Broad | Small molecules; metabolomics; proteomics |
| Multiplex Bead Arrays | Moderate | High (up to 50-plex) | Moderate | Biomarker panels; exploratory studies |
Advanced technologies like MSD and LC-MS/MS often provide superior performance compared to traditional ELISA. MSD utilizes electrochemiluminescence detection, providing up to 100 times greater sensitivity than traditional ELISA and a broader dynamic range [92]. LC-MS/MS similarly surpasses ELISA in sensitivity, making it particularly valuable for detecting low-abundance species [92].
Economic Considerations in Technology Selection
Cost-effectiveness is a practical consideration in biomarker validation, particularly when evaluating multiple candidates:
- Measuring four inflammatory biomarkers (IL-1β, IL-6, TNF-α and IFN-γ) using individual ELISAs costs approximately $61.53 per sample
- Using MSD's multiplex assay reduces the cost to $19.20 per sample, representing a saving of $42.33 per sample [92]
- These economic advantages, combined with technical superiority, make advanced multiplexing platforms increasingly attractive for comprehensive biomarker validation
The Researcher's Toolkit: Essential Reagents and Materials
Successful biomarker validation requires careful selection of reagents and materials to ensure robust, reproducible results:
Table 3: Essential Research Reagent Solutions for Biomarker Validation
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Reference Standards | Calibrate assays; determine accuracy | Should be fully characterized and representative of endogenous biomarker when possible |
| Quality Control Materials | Monitor assay performance over time | Should represent low, medium, and high concentrations spanning clinical range |
| Capture and Detection Antibodies | Specifically bind target analyte | Critical for immunoassay specificity; require rigorous cross-reactivity testing |
| Matrix Materials | Diluent for standards and samples | Should match patient sample matrix as closely as possible; assess interference |
| Assay Buffers | Maintain optimal assay conditions | Must preserve biomarker integrity and antibody binding characteristics |
For LBAs, which represent the archetypical quantitative assay for endogenous protein biomarkers, the availability of appropriate reference standards is particularly challenging [90]. Since most biomarker ligands are endogenous substances already present in patient samples, an analyte-free matrix for use during validation studies is difficult to obtain. This limitation often places biomarker LBAs in the category of relative quantitation methods rather than definitive quantitative assays [90].
The establishment of key performance parameters—accuracy, precision, sensitivity, and specificity—forms the foundation of credible cancer biomarker assays. The "fit-for-purpose" approach provides a flexible yet rigorous framework for validation, recognizing that different clinical contexts demand different levels of evidence [89] [90]. As biomarker technologies continue to evolve, with advanced platforms like MSD and LC-MS/MS offering improved sensitivity and multiplexing capabilities, the fundamental requirement for robust analytical validation remains constant [92].
The remarkably low success rate of biomarker translation (approximately 0.1%) highlights the critical importance of establishing robust performance parameters early in development [92] [9]. By implementing systematic validation protocols, selecting appropriate technology platforms, and utilizing high-quality reagents, researchers can significantly enhance the reliability and clinical utility of cancer biomarker assays. This rigorous approach to analytical validation ultimately accelerates the translation of promising biomarkers from discovery to clinical practice, advancing the field of precision oncology and improving patient outcomes.
In the field of cancer biomarker research, the reliability of quantitative data is paramount for making critical decisions in drug development and clinical diagnostics. The Analytical Measurement Range (AMR), also known as the reportable range, defines the span of analyte concentrations that an method can accurately and reliably measure without modification [95]. For researchers and scientists validating biomarker assays, establishing a robust AMR is an indispensable component of method validation, ensuring that results fall within a range where precision, accuracy, and linearity are maintained [96]. The AMR is bounded by two critical parameters: the Lower Limit of Quantification (LLOQ) and the Upper Limit of Quantification (ULOQ), which represent the lowest and highest concentrations that can be quantitatively determined with acceptable precision and accuracy [97] [95]. Together with linearity—the ability of a method to obtain results directly proportional to analyte concentration within the AMR—these parameters form the foundation for generating trustworthy analytical data in preclinical and clinical studies [98] [96].
The "fit-for-purpose" approach to biomarker method validation, now widely adopted in anticancer drug development, emphasizes that the rigor of AMR validation should be aligned with the intended application of the biomarker [10]. For definitive quantitative assays used in clinical trials, stringent characterization of the AMR is required to meet regulatory standards and ensure the quality of every aspect of the trial [10].
Core Components of the Analytical Measurement Range
Lower Limit of Quantification (LLOQ)
The LLOQ is the lowest concentration of an analyte that can be quantitatively determined with stated acceptance criteria for precision and accuracy [99]. According to industry standards, at the LLOQ, the analyte response should be identifiable, discrete, and reproducible with a precision of ≤20% coefficient of variation (CV) and accuracy of 80-120% [10] [99]. The LLOQ is particularly crucial in cancer biomarker research when measuring low-abundance analytes, such as circulating proteins or drugs in pharmacokinetic studies.
Calculation Approaches for LLOQ: Multiple approaches exist for determining LLOQ, each with specific applications and considerations:
- Signal-to-Noise Ratio: LLOQ corresponds to the analyte concentration that produces a signal at least 5 times higher than the background noise [99]. This approach is commonly used in chromatographic methods.
- Standard Deviation and Slope Method: LLOQ can be calculated as (y~blank~ + 10σ)/b, where y~blank~ is the background signal, σ is the standard deviation of the response, and b is the slope of the calibration curve [99].
- Biological Matrix-Based Approach: For biomarker assays, LLOQ is typically determined as the lowest standard with a %backfit of 75-125% and %CV <20-30%, with a positive mean signal intensity difference from the negative control [97].
Upper Limit of Quantification (ULOQ)
The ULOQ represents the highest concentration of an analyte that can be reliably quantified with stated accuracy and precision requirements [97] [95]. At the ULOQ, precision should be within 15% CV and accuracy within 85-115% of the nominal concentration [99]. In practice, the ULOQ is often defined as the highest calibration standard that demonstrates a %backfit of 80-120%, a %CV of <30%, and a positive mean signal intensity difference between it and the negative control [97].
Linearity
Linearity refers to the ability of an analytical method to produce results that are directly proportional to the concentration of analyte in the sample within the AMR [98] [96]. It is assessed by measuring samples at various concentrations across the claimed range and statistically evaluating the relationship between measured and expected values. A linearity-of-dilution experiment provides information about the precision of results for samples tested at different dilution levels in a chosen matrix [98]. Good linearity over a wide range of dilutions provides flexibility to assay samples with different analyte levels, enabling high-concentration samples to be diluted into the AMR [98].
Table 1: Key Performance Criteria for LLOQ and ULOQ
| Parameter | Definition | Acceptance Criteria | Common Calculation Methods |
|---|---|---|---|
| LLOQ | Lowest concentration measurable with acceptable accuracy and precision | Precision ≤20% CV; Accuracy 80-120% [10] [99] | Signal-to-noise ratio (5:1) [99]; Standard deviation/slope method [99]; Biological matrix-based approach [97] |
| ULOQ | Highest concentration measurable with acceptable accuracy and precision | Precision ≤15% CV; Accuracy 85-115% [99] | Highest standard with %backfit 80-120% and %CV <30% [97] |
| Linearity | Ability to obtain results proportional to analyte concentration | R² ≥ 0.975 [100]; Visual linearity across range [96] | Linear regression analysis; Visual inspection of plotted data [96] |
Experimental Protocols for Determining AMR Parameters
Protocol for Establishing LLOQ and ULOQ
A standardized approach for determining LLOQ and ULOQ involves analyzing multiple replicates of calibration standards at varying concentrations. The following protocol is adapted from validated bioanalytical methods used in cancer research:
Preparation of Calibration Standards: Prepare a minimum of 6-8 calibration standards spanning the expected concentration range, preferably in the same biological matrix as study samples [101] [100]. For example, in validating an LC-MS/MS method for CDK4/6 inhibitors, researchers used eight calibration working dilutions from 0.10 to 25.0 µM for abemaciclib [101].
Sample Analysis: Analyze each calibration standard with appropriate replication (typically 5-6 replicates) across multiple runs [10] [100]. In the MyProstateScore 2.0 validation, eight replicates of each concentration were run from pre-amplification through qPCR [100].
Data Analysis: Calculate the precision (%CV) and accuracy (% deviation from nominal concentration) for each calibration standard. The LLOQ is identified as the lowest concentration where CV ≤20% and accuracy is within 80-120%. The ULOQ is the highest concentration meeting CV ≤15% and accuracy within 85-115% [99].
Confirmation: Verify LLOQ and ULOQ using quality control samples (QC-LLOQ and QC-H) in subsequent validation runs [101].
Protocol for Linearity Assessment
The linearity of dilution experiment evaluates whether a method provides proportional responses across the AMR:
Sample Preparation: Prepare a high-concentration sample and serially dilute it to create at least 5 concentration levels spanning the claimed AMR [96]. Use the appropriate sample matrix to maintain consistency.
Analysis and Plotting: Analyze each dilution level in replicate and plot measured values against expected values [96]. The National Committee for Clinical Laboratory Standards (NCCLS) recommends a minimum of 4-5 different levels or concentrations [96].
Statistical Evaluation: Evaluate linearity through linear regression analysis, calculating the coefficient of determination (R²). For qPCR-based methods such as MyProstateScore 2.0, R² ≥ 0.975 with PCR efficiencies of 97-105% indicates acceptable linearity [100].
Visual Assessment: Manually draw the best straight line through the linear portion of the data or use computer-generated "best fit" linear regression statistics [96].
Diagram 1: Workflow for determining analytical measurement range
Comparative Analysis of AMR Across Technologies
Different analytical platforms demonstrate distinct performance characteristics for LLOQ, ULOQ, and linearity in cancer biomarker research. The selection of an appropriate technology depends on the required sensitivity, dynamic range, and specific application of the biomarker assay.
Table 2: Technology Comparison for AMR Parameters in Biomarker Assays
| Technology Platform | Typical LLOQ | Typical ULOQ | Linear Range | Applications in Cancer Research |
|---|---|---|---|---|
| Multiplex Immunoassays [102] | pg/mL range | ng/mL range | 3-4 log dynamic range | Verification of protein biomarker candidates; measuring cytokine panels |
| LC-MS/MS [101] | µM to nM range (compound-dependent) | µM range (compound-dependent) | 2-3 orders of magnitude | Quantifying small molecule drugs (e.g., CDK4/6 inhibitors) and metabolites in plasma |
| qPCR-based Methods [100] | 40-160 copies/reaction (LOD) | 10^6^-10^7^ copies/reaction | 5-6 log dynamic range | Gene expression biomarkers; urinary biomarkers for prostate cancer detection |
| Planar Antibody Arrays [102] | Variable; depends on detection method | Variable; depends on detection method | Limited data | Discovery-phase protein biomarker screening |
The AMR performance can vary significantly between these platforms. Multiplex immunoassays typically offer a wide dynamic range (pg/mL to ng/mL) suitable for measuring circulating protein biomarkers [102]. In contrast, LC-MS/MS methods provide excellent specificity for small molecule quantification but may have a narrower linear range (2-3 orders of magnitude) [101]. qPCR-based approaches, such as that used in MyProstateScore 2.0, demonstrate an extensive linear range spanning 5-6 orders of magnitude, which is particularly valuable for measuring nucleic acid biomarkers that can vary widely in concentration between samples [100].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for AMR Validation
| Reagent/Material | Function in AMR Validation | Examples/Specifications |
|---|---|---|
| Reference Standards | Fully characterized analyte for calibration curve preparation | Purified recombinant proteins [98]; Certified reference materials [10] |
| Biological Matrix | Mimics patient sample composition for validation studies | Charcoal-stripped serum/plasma [98]; Artificial urine [100] |
| Quality Control Materials | Monitor assay performance during validation | QC-LLOQ, QC-L, QC-M, QC-H samples [101] |
| Sample Collection Tubes | Maintain analyte stability during collection | Specific anticoagulants for plasma; protease inhibitors for protein stability [102] |
| Detection Reagents | Generate measurable signal proportional to analyte | Enzyme-conjugated antibodies [102]; Fluorescent probes for qPCR [100] |
| Calibrator Diluent | Appropriate medium for serial dilution of standards | Matrix-matched to minimize background [98] |
Addressing Technical Challenges in AMR Establishment
Matrix Effects and Interference
Biological sample matrices can significantly impact assay performance and the determined AMR. Components in serum, plasma, or urine may interfere with analyte detection, leading to inaccurate quantification [98] [102]. To address this:
- Conduct spike-and-recovery experiments by adding known amounts of analyte into the natural sample matrix and comparing recovery to identical spikes in standard diluent [98].
- Assess potential interference from substances commonly found in samples. For example, in the MyProstateScore 2.0 validation, 12 potential interfering substances were tested, with only whole blood affecting performance [100].
- Optimize standard diluent to match sample matrix composition, which may involve adding carrier proteins like BSA or adjusting pH [98].
Sample Dilution and Parallelism
When analyte concentrations exceed the ULOQ, samples require dilution to bring them within the AMR. However, dilution can introduce inaccuracies if the sample matrix affects detectability differently than the standard diluent [98].
- Perform linearity-of-dilution experiments to validate that samples can be accurately diluted [98].
- Ensure parallelism between the standard curve and serial dilutions of sample to confirm consistent analyte detection across concentrations [10].
- Use the appropriate dilution factor to bring samples into the central portion of the AMR rather than near the limits of quantification [98].
Diagram 2: Approach for addressing technical challenges in AMR validation
Regulatory and Practical Considerations
Fit-for-Purpose Validation Approach
The "fit-for-purpose" approach to biomarker method validation recognizes that the extent of AMR characterization should be aligned with the intended application of the biomarker [10]. This framework acknowledges that biomarkers used in different contexts—from early discovery to clinical decision-making—require different levels of validation rigor. The American Association of Pharmaceutical Scientists (AAPS) has identified five general classes of biomarker assays, each with different recommended validation parameters [10]:
- Definitive quantitative assays require full validation of AMR parameters as they are used to measure absolute quantitative values for unknowns.
- Relative quantitative assays may have more flexible AMR requirements as they use reference standards not fully representative of the biomarker.
- Quasi-quantitative assays without calibration standards have different performance considerations for their measurable range.
Documentation and Reporting Standards
When reporting assay data, it is conventional to include values for ULOQ, LLOQ, and the determined AMR [97]. Data falling outside these limits should be reported as >ULOQ,
- Detailed methodology for determining LLOQ and ULOQ
- Statistical analysis of linearity including correlation coefficients and confidence intervals
- Results from interference studies and matrix effect evaluations
- Protocols for sample dilution and re-assay when values fall outside the AMR
The precise definition of the Analytical Measurement Range through LLOQ, ULOQ, and linearity assessment is a critical component of method validation in cancer biomarker research. As demonstrated across various analytical platforms, establishing a robust AMR ensures the generation of reliable, reproducible data that can confidently inform drug development decisions and clinical applications. The experimental protocols and technical considerations outlined provide researchers with a framework for comprehensive AMR validation aligned with both scientific rigor and the practical realities of biomarker implementation. By adopting a fit-for-purpose approach that matches validation stringency to application context, scientists can efficiently characterize the performance of their analytical methods while meeting the evolving standards of cancer biomarker research.
The accurate quantification of protein biomarkers is fundamental to advancing cancer research, drug development, and ultimately, precision medicine. Within this realm, two primary analytical techniques dominate: immunoassays and mass spectrometry (MS). Immunoassays, such as ELISA, are long-established gold standards, prized for their convenience and high sensitivity [103]. Mass spectrometry, particularly liquid chromatography-tandem mass spectrometry (LC-MS/MS), has emerged as a powerful quantitative tool that can overcome several limitations inherent to antibody-based methods [104]. For researchers and scientists engaged in the analytical validation of cancer biomarker assays, understanding the comparative performance, advantages, and limitations of these platforms is critical for selecting the optimal method for a given application. This guide provides an objective, data-driven comparison of these two technologies, framing the discussion within the context of assay validation for clinical and research use.
Head-to-Head Performance Comparison
Direct comparative studies provide the most insightful data for platform evaluation. A landmark study in Alzheimer's disease research, which shares analytical challenges with cancer biomarker validation, directly compared immunoassay and mass spectrometry for quantifying phosphorylated tau (p-tau) proteins in cerebrospinal fluid.
Table 1: Diagnostic Performance Comparison for Detecting Amyloid-PET Positivity (Adapted from [105] [106])
| Biomarker | Technology | Area Under the Curve (AUC) | Key Comparative Finding |
|---|---|---|---|
| p-tau217 | Immunoassay | ~0.95* | Highly comparable performance, effect sizes, and associations with PET biomarkers. |
| p-tau217 | Mass Spectrometry | ~0.95* | |
| p-tau181 | Immunoassay | Higher | Immunoassays demonstrated slightly superior diagnostic performance. |
| p-tau181 | Antibody-Free Mass Spectrometry | Lower | |
| p-tau231 | Immunoassay | Higher | Immunoassays demonstrated slightly superior diagnostic performance. |
| p-tau231 | Antibody-Free Mass Spectrometry | Lower |
*AUC values are approximate representations from the study's ROC analyses.
The core finding was that while p-tau217 measurements were highly comparable between the two platforms, immunoassays for p-tau181 and p-tau231 showed slightly superior diagnostic performance compared to the antibody-free mass spectrometry method used in the study [105] [106]. This highlights that performance can be biomarker-specific, and a one-size-fits-all approach is not applicable.
Beyond individual biomarkers, the utility of each platform is demonstrated in large-scale clinical validation studies. For multi-cancer early detection (MCED), an AI-empowered test measuring seven protein tumor markers with immunoassays achieved an AUC of 0.829 in a cohort of over 15,000 participants, demonstrating robust clinical performance [107]. Conversely, a mass spectrometry-based pipeline for pancreatic cancer discovered a novel 4-protein biomarker panel (APOE, ITIH3, APOA1, APOL1) that, when combined with the traditional CA19-9 marker, achieved a 95% sensitivity and 94.1% specificity, significantly outperforming CA19-9 alone [108].
Immunoassay Workflow and Principles
Immunoassays rely on the specific binding of an antibody to its target antigen. The most common format in protein biomarker research is the sandwich ELISA, which uses a capture antibody immobilized on a solid phase and a detection antibody that binds to a different epitope of the target protein. The detection antibody is conjugated to a reporter enzyme or label that generates a measurable signal, allowing for quantification.
Diagram: Sandwich Immunoassay Workflow
A key innovation is the mass spectrometric immunoassay, which combines the specificity of immunoaffinity enrichment with the detection power of MS. In this hybrid approach, target proteins are first captured from a complex sample using antibody-conjugated beads. After washing, the captured proteins are digested into peptides and analyzed by MALDI-TOF MS or LC-MS/MS, using a synthetic peptide as an internal standard for quantification [103]. This method merges the high specificity of immunoassays with the multiplexing capability and interference resistance of MS.
Mass Spectrometry Workflow and Principles
Mass spectrometry identifies and quantifies molecules based on their mass-to-charge ratio. A typical targeted proteomics workflow for protein biomarkers involves multiple steps to convert proteins into measurable peptides.
Diagram: Targeted MS Proteomics Workflow
Detailed LC-MS/MS Protocol for Phosphorylated Tau [105] [106]:
- Sample Preparation: 250 µL of cerebrospinal fluid is spiked with stable isotope-labeled peptide internal standards. Proteins are precipitated using perchloric acid, leaving tau in solution. The supernatant is purified using solid-phase extraction (SPE).
- Digestion: The sample is digested with trypsin overnight at 37°C to generate peptides.
- Liquid Chromatography (LC): Tryptic peptides are separated by liquid chromatography to reduce sample complexity before entering the mass spectrometer.
- Mass Spectrometry Analysis: Analysis is performed using a high-resolution Orbitrap mass spectrometer in Parallel Reaction Monitoring (PRM) mode. The method monitors specific precursor ions (the target peptides) and fragments them to measure multiple product ions for precise identification and quantification.
- Data Analysis: Quantification is achieved by comparing the peak areas of the endogenous "light" peptides to their corresponding stable isotope-labeled "heavy" internal standards, allowing for absolute quantification.
This workflow is equally applicable to cancer biomarkers. For example, in acute myeloid leukemia (AML), MS-based workflows are used for deep proteomic and metabolomic profiling to uncover disease-associated molecular signatures and therapeutic vulnerabilities [109].
Advantages, Limitations, and Clinical Utility
Table 2: Core Characteristics of Immunoassays and Mass Spectrometry
| Feature | Immunoassays | Mass Spectrometry |
|---|---|---|
| Principle | Antibody-Antigen Binding | Mass-to-Charge Ratio Measurement |
| Multiplexing | Limited (typically <10-plex) | High (dozens to hundreds) [110] |
| Throughput | Very High | Moderate |
| Specificity | High (dependent on antibody quality) | Very High (avoids antibody cross-reactivity) [104] |
| Development Time | Sherter (if commercial kits exist) | Longer |
| Absolute Quantification | Possible with standards | Native capability with SIS standards |
| Sample Volume | Low | Can be higher (e.g., 250-300 µL for CSF) [106] |
| Detect Post-Translational Modifications | Limited (requires specific antibody) | Excellent (discovery and targeted) [109] |
| Instrument Cost | Lower | High |
| Per-Sample Cost | Lower (at low plex) | Can be higher |
A significant advantage of MS is its ability to avoid antibody-related interferences. For example, in thyroid cancer monitoring, immunoassays for thyroglobulin can be compromised by anti-thyroglobulin antibodies in patient serum, leading to falsely low results. Targeted LC-MS/MS assays bypass this interference, providing reliable quantification [104]. Furthermore, MS panels can be easily modified and expanded as new biomarkers are discovered, offering greater flexibility than developing new immunoassays [108] [110].
The choice between platforms often depends on the clinical or research context. Immunoassays are well-suited for high-throughput, routine measurement of single or a few well-established biomarkers. Mass spectrometry excels in discovery research, validating novel biomarkers, multiplexed quantification, and in situations where immunoassays are known to fail, such as with problematic antibodies or required high specificity for specific protein variants [104] [109].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Biomarker Assays
| Reagent / Material | Function in Immunoassays | Function in Mass Spectrometry |
|---|---|---|
| Capture & Detection Antibodies | Bind specifically to target protein for isolation and signal generation. | Used primarily in hybrid immunoaffinity-MS methods for initial enrichment [110]. |
| Stable Isotope-Labeled Standards (SIS) | Not typically used. | Crucial for absolute quantification; corrects for sample prep and ionization variability [104]. |
| Trypsin / Lys-C | Not typically used. | Proteolytic enzyme that digests proteins into peptides for MS analysis. |
| Solid-Phase Extraction (SPE) Plates | For sample cleanup. | For desalting and concentrating peptide mixtures before LC-MS/MS. |
| LC Columns (C18) | Not applicable. | Separates peptides based on hydrophobicity prior to ionization. |
| MALDI Matrix (e.g., CHCA, DHB) | Not applicable. | Absorbs laser energy to facilitate soft ionization of analytes for MALDI-TOF analysis [103] [111]. |
Both immunoassays and mass spectrometry are indispensable tools in the portfolio of cancer researchers and drug developers. The decision to use one over the other is not a matter of declaring a universal winner but requires a strategic choice based on the specific application. Immunoassays remain the best choice for high-throughput, cost-effective analysis of single or a few established biomarkers where high-quality antibodies are available. Mass spectrometry is superior for discovery-phase research, multiplexed quantification of dozens of proteins, detecting post-translational modifications, and in scenarios where antibody-based assays suffer from interferences or do not exist. As the field moves toward greater precision, the combination of both technologies—using immunoaffinity enrichment for sample preparation prior to MS analysis—often provides the most specific and reliable results, pushing the boundaries of analytical validation in cancer biomarker research.
The management of Non-Small Cell Lung Cancer (NSCLC) has been revolutionized by precision medicine, where targeted therapies are directed against specific molecular drivers. Next-generation sequencing (NGS) panels enable comprehensive genomic profiling to identify these actionable mutations simultaneously. This case study examines the validation of a multi-gene NGS panel within the broader context of analytical validation for cancer biomarker assays, providing objective performance comparisons against alternative testing methodologies and platforms.
Performance Comparison of NGS Testing Approaches
Data from recent validation studies demonstrate the performance characteristics of different NGS testing strategies for NSCLC. The following tables summarize key metrics across specimen types, gene panels, and technologies.
Table 1: Comparative Performance of Tissue vs. Cytology Specimens for NGS Panel Testing
| Performance Metric | Cytology Specimens | Tissue (FFPE) Specimens | Clinical Implications |
|---|---|---|---|
| Success Rate of Gene Analysis | 98.4% (95% CI, 95.9–99.6%) [112] | Conventional rates: 72.0–90.0% [112] | Higher success rate minimizes test failures and avoids re-biopsies. |
| Positive Concordance Rate | 97.3% (95% CI, 90.7–99.7%) with other CDx kits [112] | Not reported in study | Ensures reliability and inter-platform consistency for clinical decision-making. |
| Median Nucleic Acid Yield | DNA: 546.0 ng; RNA: 426.5 ng [112] | Varies; often lower due to fixation [112] | Sufficient yield reduces the risk of insufficient sample quantity. |
| Nucleic Acid Quality | DNA Integrity Number: 9.2; RNA Quality: 4.7 [112] | Generally lower due to formalin fixation [112] | Higher quality improves library preparation efficiency and data quality. |
| VAF Correlation | Pearson coefficient: 0.815 vs. FFPE [112] | Reference standard | High correlation ensures accurate mutation allele measurement for therapy selection. |
Table 2: Analytical Performance Metrics of Validated NGS Panels
| Panel (Study) | Sensitivity | Specificity | Limit of Detection (LOD) | Key Genes Covered |
|---|---|---|---|---|
| LCCP (cPANEL Trial) [112] | Implied by 97.3% concordance | Implied by 97.3% concordance | EGFR exon19 del: 0.14%; L858R: 0.20%; T790M: 0.48% [112] | EGFR, BRAF, KRAS, ERBB2, ALK, ROS1, MET, RET [112] |
| TTSH-Oncopanel (61 genes) [43] | 98.23% (for unique variants) | 99.99% | 2.9% VAF for SNVs and INDELs [43] | KRAS, EGFR, ERBB2, PIK3CA, TP53, BRCA1 [43] |
| 101-test (ctDNA) [113] | SNVs: 98.3%; InDels: 100%; Fusions: 100% | 99.99% | 0.38% for SNVs; 0.33% for InDels and Fusions [113] | 101 cancer-related genes including EGFR, ALK, ROS1, MET, RET, NTRK [113] |
| nNGMv2 Panel (26 genes) [114] | Robust detection down to 6.25 ng DNA input | Specific detection confirmed | Identified all but two MET variants (found with adjusted filter) [114] | ALK, BRAF, EGFR, ERBB2, KRAS, MET, NTRK1/2/3, RET, ROS1, TP53 [114] |
Table 3: Turnaround Time and Operational Efficiency
| Parameter | In-House TTSH-Oncopanel [43] | Outsourced NGS [43] | nNGMv2 ArcherDX Panel [114] |
|---|---|---|---|
| Average Turnaround Time | 4 days [43] | ~3 weeks [43] | Successful in 98.9% of samples (N=90) [114] |
| DNA Input Requirements | ≥50 ng [43] | Varies by external provider | Successful with input as low as 6.25 ng [114] |
| Primary Advantage | Faster clinical decision-making [43] | Access to specialized expertise | Cost-effective; fast protocol; high success rate on routine samples [114] |
Experimental Protocols and Methodologies
Specimen Collection and Processing
Cytology Specimen Protocol (cPANEL Trial):
- Collection: Specimens were obtained via transbronchial brushing, needle aspiration washing, or pleural effusion [112].
- Preservation: Immediately placed in a non-formalin, ammonium sulfate-based nucleic acid stabilizer (GM tube) to inhibit nuclease activity [112].
- Storage and Transport: Refrigerated without centrifugation or freezing and shipped to the testing facility [112].
- Nucleic Acid Extraction: DNA and RNA were co-purified using the Maxwell RSC Blood DNA and simplyRNA Cells Kits (Promega) [112].
FFPE Tissue Specimen Protocol (Multi-center Study):
- Macrodissection: Tumor areas were marked on H&E-stained slides and microdissected from unstained serial sections to enrich tumor content [114].
- DNA Extraction: Genomic DNA was isolated using kits such as the QIAamp DNA FFPE tissue kit (Qiagen) or Maxwell RSC FFPE Plus DNA Kit (Promega) [113] [114].
- Quality Control: DNA concentration was measured by fluorometry (e.g., Qubit), and quality was assessed via TapeStation or similar systems to determine DNA Integrity Number (DIN) [112] [114].
Library Preparation and Sequencing
Two primary target enrichment methods were employed across the studies:
Anchored Multiplex PCR (ArcherDX):
- Technology: Utilizes gene-specific primers and adaptor primers for efficient amplification from low-quality/quantity DNA [114].
- Workflow: Library preparation with the ArcherDX VariantPlex panel, followed by sequencing on Illumina or similar platforms [114].
- Analysis: Data processed through the Archer Analysis pipeline, using hg19 as reference [114].
Hybrid Capture-Based Method (101-test):
- Technology: Uses biotinylated oligonucleotide probes to capture target regions from a fragmented DNA library [113].
- Workflow: Libraries were prepared from 20-80 ng of cell-free DNA, followed by capture-based targeting of 101 genes, and sequenced on Illumina NextSeq or NovaSeq platforms [113].
- Analysis: A customized bioinformatics pipeline was used for variant calling and annotation [113].
Analytical Validation Experiments
Limit of Detection (LOD) Determination:
- Method: Serial dilution studies using commercially available reference standards (e.g., HD701) or cell line DNA with known mutations [43] [113].
- Procedure: DNA is diluted to varying variant allele frequencies (VAFs) and tested with the NGS panel [43].
- Analysis: The LOD is defined as the lowest VAF at which 95% of positive samples are reliably detected (LoD₉₅) [113]. The LCCP panel demonstrated an LOD as low as 0.14% for specific EGFR mutations [112].
Precision and Reproducibility:
- Repeatability (Intra-run): Multiple replicates of the same sample are processed within a single sequencing run [43].
- Reproducibility (Inter-run): The same sample is tested across different runs, operators, or instruments [43].
- Metrics: The TTSH-Oncopanel showed 99.99% repeatability and 99.98% reproducibility [43].
Concordance Analysis:
- Method: Results from the candidate NGS panel are compared to an orthogonal method, such as digital droplet PCR (ddPCR), breakpoint PCR, or a previously validated test [113] [114].
- Sample Sets: Typically use a set of clinical samples with known mutation status [115].
- Calculation: Positive Percent Agreement (sensitivity) and Negative Percent Agreement (specificity) are calculated [113].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Kits for NGS Panel Validation
| Reagent/Kits | Primary Function | Specific Examples |
|---|---|---|
| Nucleic Acid Stabilizer | Preserves DNA/RNA in cytology samples by inhibiting nucleases. | GM tube (ammonium sulfate-based stabilizer) [112] |
| DNA/RNA Extraction Kits | Isolate high-quality nucleic acids from diverse sample types. | Maxwell RSC FFPE Plus DNA Kit (Promega); QIAamp DNA FFPE tissue kit (Qiagen); simplyRNA Cells Kits (Promega) [112] [114] |
| Target Enrichment & Library Prep Kits | Prepare sequencing libraries from extracted nucleic acids. | ArcherDX VariantPlex; Sophia Genetics Library Kit; Hybrid Capture-based kits [43] [113] [114] |
| Reference Standards | Act as positive controls for assay validation and LOD studies. | Horizon HD701; SeraCare ctDNA v2 Reference Materials [43] [113] |
| Quantification & QC Assays | Accurately measure nucleic acid concentration and quality. | Qubit dsDNA HS Assay Kit (Thermo Fisher); TapeStation (Agilent) [112] [114] |
| Bioinformatics Pipelines | Analyze raw NGS data for variant calling and annotation. | Archer Analysis; Sophia DDM; Custom pipelines using Burrows-Wheeler Aligner, Vardict [113] [114] |
Discussion and Clinical Implications
The validation of multi-gene NGS panels is critical for implementing precision oncology for NSCLC patients. The data presented demonstrates that well-validated panels, whether using tissue or cytology specimens, provide high success rates, sensitivity, and specificity required for clinical use [112] [43] [113].
A key advancement is the demonstrated utility of cytology specimens preserved in nucleic acid stabilizers, which can yield higher success rates and nucleic acid quality compared to traditional FFPE tissue [112]. This is significant for clinical practice, as cytology samples are often obtained through less invasive procedures.
Furthermore, the development of in-house NGS panels can drastically reduce turnaround time from weeks to just a few days, facilitating quicker therapeutic decisions [43]. However, this requires substantial initial investment in validation and infrastructure.
For laboratories developing their own tests, adhering to guidelines for indirect clinical validation is essential, particularly for Laboratory Developed Tests (LDTs) [115]. The framework involves demonstrating high accuracy against a comparator assay and using properly validated reference materials to ensure clinical relevance.
The consistent detection of actionable mutations across different panels and platforms underscores the reliability of NGS technology in identifying patients eligible for targeted therapies. The high concordance between ctDNA and tissue testing further supports the use of liquid biopsies as a complementary approach when tissue is insufficient [113].
In conclusion, the rigorous analytical and clinical validation of NGS panels, as detailed in this case study, provides the necessary foundation for their reliable integration into clinical pathways, ultimately guiding personalized treatment decisions and improving outcomes for NSCLC patients.
The Role of Stable Isotope-Labeled Standards (SIS) in Accurate Quantification
In the era of precision oncology, the accurate quantification of protein cancer biomarkers has become indispensable for early detection, risk classification, and treatment monitoring. These biomarkers, objectively measured as indicators of normal biological or pathogenic processes, provide crucial insights for clinical decision-making [3]. However, the journey from biomarker discovery to clinical implementation is fraught with analytical challenges, primarily concerning the precision, accuracy, and reproducibility of quantitative measurements across complex biological matrices. It is within this challenging landscape that Stable Isotope-Labeled Standards (SIS) have emerged as transformative tools, enabling researchers to achieve the rigorous analytical validation required for clinical application.
Mass spectrometry-based targeted proteomics, particularly liquid chromatography-tandem mass spectrometry (LC-MS/MS), has become a powerful platform for cancer biomarker quantification, often overcoming limitations associated with traditional immunoassays [116]. The core strength of these MS-based methodologies hinges on the strategic implementation of SIS, which serve as molecular mirrors of target analytes but are distinguished by their mass. These standards, incorporating non-radioactive heavy isotopes such as ^13^C, ^15^N, ^18^O, or ^2^H (deuterium), are added in known quantities to samples, allowing them to track and compensate for analytical variability throughout the complex sample preparation and analysis workflow [117]. This article provides a comprehensive comparison of SIS implementation strategies, supported by experimental data, to guide researchers in optimizing these critical reagents for robust cancer biomarker assays.
SIS in Context: Core Functions and Strategic Importance
Stable Isotope-Labeled Standards are not merely convenient additives; they perform multiple essential functions that collectively ensure data reliability. Their primary role is to normalize for analytical variability that occurs during sample processing, ionization efficiency changes in the mass spectrometer, and matrix effects where other substances in the sample interfere with analyte detection [117] [118]. By providing a parallel internal reference that co-elutes with the native analyte but is distinguishable by mass, SIS enable correction for these uncontrollable factors, thereby significantly improving the sensitivity and accuracy of the final measurement [117].
This capability is particularly critical in the context of clinical cancer biomarkers, where proteins of interest often exist at low concentrations amidst a complex background of high-abundance proteins in blood or other biofluids. The fit-for-purpose validation approach, now widely adopted for biomarker assays, recognizes that the stringency of analytical validation should be aligned with the intended use of the biomarker, from exploratory research to clinical decision-making [90]. Within this framework, SIS provide the foundational robustness that allows assays to progress through the biomarker development pipeline—from discovery and verification to clinical validation [1].
Table 1: Key Functions of Stable Isotope-Labeled Standards in Quantitative Proteomics
| Function | Mechanism | Impact on Assay Performance |
|---|---|---|
| Quantitative Normalization | Accounts for variability in sample preparation, extraction efficiency, and instrument performance | Improves accuracy and precision of concentration measurements |
| Matrix Effect Correction | Compensates for ion suppression/enhancement from co-eluting substances in complex samples | Enhances specificity and reliability in biological matrices |
| Compensation for Sample Losses | Tracks analyte degradation or adsorption during processing | Ensures measurements reflect true original concentrations |
| Calibration Reference | Serves as internal standard for instrument calibration | Improves reproducibility across batches and instruments |
Comparative Analysis of SIS Formats and Experimental Performance
Not all stable isotope-labeled standards are created equal. Researchers have developed multiple SIS formats, each with distinct advantages and limitations for specific applications in cancer biomarker quantification. The choice of standard format can significantly influence the accuracy and reliability of the final results, particularly when addressing specific challenges such as enzymatic digestion efficiency or variable sample preparation recovery.
SIS Peptides vs. Extended SIS Peptides for Digestion Efficiency Tracking
A critical application of SIS in protein quantification involves accounting for variability in tryptic digestion, a fundamental step in bottom-up proteomics. A seminal comparative study examined this challenge during the quantification of human osteopontin (hOPN), a cancer biomarker elevated in various malignancies. Researchers compared a standard SIS peptide (GDSVVYGLR) against an extended SIS peptide (TYDGRGDSVVYGLRSKSKKF) containing the signature peptide sequence within a larger context [119].
The experimental protocol involved immunocapture of hOPN from plasma using specific antibodies, followed by trypsin digestion to generate the signature peptide. Both SIS formats were evaluated under varying trypsin activity conditions (20-180% of normal levels) to simulate digestion variability. The results demonstrated a striking advantage for the extended SIP: when trypsin activity was varied, the use of the extended SIL peptide as an internal standard limited quantification variability to within ±30% of the normalized response. In contrast, when the standard SIL peptide was used, the variability ranged dramatically from -67.4% to +50.6% [119]. This study provides compelling evidence that extended SIS peptides more effectively correct for digestion inefficiencies, a crucial consideration for assays requiring high precision.
SIS in Method Comparison Studies Across Technology Platforms
The performance of SIS-assisted assays can also be evaluated by comparing different proteomic technology platforms. A comprehensive comparison of proteomic technologies for blood-based detection of colorectal cancer provided insightful data on this front [120]. The study compared proximity extension assays (PEA), LC/MRM-MS, quantibody microarrays (QMA), and immunome full-length functional protein arrays (IpA) using samples from 56 colorectal cancer patients and 99 controls.
Table 2: Technology Platform Comparison with SIS-Based LC/MRM-MS
| Technology Platform | Correlation with LC/MRM-MS (SIS) | Exemplary Biomarker Performance (AUC) | Key Findings |
|---|---|---|---|
| LC/MRM-MS (SIS) | Reference | IGFBP2, MMP9: AUC ~0.60 | Robust quantification with good precision |
| Proximity Extension Assay (PEA) | Good (≥0.6 for 4/9 proteins) | TR: AUC 0.74; SPARC: AUC 0.66 | Similar performance to LC/MRM-MS for specific biomarkers |
| Quantibody Microarray (QMA) | Moderate (0.69 for GDF15 only) | GDF15: AUC 0.63 | Lower concordance and diagnostic performance |
| Immunome Protein Array (IpA) | Poor correlation | All biomarkers: AUC <0.60 | Significantly inferior performance for quantification |
The findings revealed that technologies incorporating SIS principles (LC/MRM-MS) or similar normalization strategies (PEA) demonstrated superior correlation and diagnostic performance compared to array-based technologies without robust internal standardization [120]. This highlights the indispensable role of effective internal standardization, whether through SIS or alternative mechanisms, in achieving reliable biomarker quantification.
Experimental Workflows and Protocol Design
Implementing SIS in cancer biomarker assays requires meticulous protocol design and optimization. The following section outlines detailed methodologies for key experiments cited in this review, providing researchers with practical guidance for incorporating SIS into their quantitative workflows.
General Workflow for SIS-Based Protein Quantification
The typical workflow for quantifying protein biomarkers using SIS involves multiple critical steps from sample collection to data analysis, with the SIS integrated at specific points to control for variability. The following diagram illustrates this process, highlighting where different types of SIS are introduced to account for technical variations:
This workflow demonstrates two primary points of SIS introduction: (A) SIS proteins added before digestion account for variability in protein recovery and enzymatic cleavage efficiency; (B) SIS peptides added after digestion correct for variability in subsequent processing steps and analytical instrumentation [116].
Detailed Protocol: Evaluating Extended vs. Standard SIS Peptides
Based on the study by Morse Faria et al. comparing standard and extended SIS peptides for hOPN quantification [119], the following detailed protocol can be implemented:
Step 1: Sample Preparation
- Collect plasma samples in appropriate anticoagulant tubes
- Perform immunocapture of target protein (hOPN) using specific antibodies
- Include surrogate matrix (e.g., immunocapture buffer) for validation standards
Step 2: SIS Addition and Digestion
- Divide samples into two sets:
- Set A: Add extended SIL peptide (TYDGRGDSVVYGLRSKSKSKKF)
- Set B: Add standard SIL peptide (GDSVVYGLR)
- Add trypsin at varying activities (20-180% of normal) to simulate digestion variability
- Incubate at 37°C for predetermined optimal digestion time
Step 3: LC-MS/MS Analysis
- Use capillary microflow LC system (e.g., Waters IonKey/MS)
- Set flow rate to 2.5 μL/min
- Employ reverse-phase chromatography with appropriate gradient
- Monitor signature peptide transition (GDSVVYGLR) and corresponding SIS transitions
Step 4: Data Analysis
- Calculate peak area ratios (native peptide/SIS)
- Normalize responses across different trypsin activities
- Compare variability between Set A and Set B
This protocol specifically addresses the critical challenge of accounting for digestion variability, which is often a major source of inaccuracy in protein quantification assays.
Protocol for Metabolic Labeling for RNA Modification Quantification
While this review focuses primarily on protein biomarkers, the principles of SIS application extend to other molecular classes. For RNA modification quantification, a metabolic labeling approach can be employed as described in search results [121]:
Step 1: SILIS Production
- Grow microorganisms (E. coli or S. cerevisiae) in isotopically labeled media
- For E. coli: Use M9 media with ^13^C~6~-glucose and ^15^N-NH~4~Cl as sole carbon and nitrogen sources
- For S. cerevisiae: Use Silantes ^13^C media supplemented with ^13^C~6~-glucose and CD~3~ methionine
- Harvest cells at early stationary phase (OD~600~ = 2.2 for E. coli, 3.5 for yeast)
Step 2: RNA Isolation and Purification
- Isolate total RNA using TRI-Reagent and chloroform extraction
- Precipitate with isopropanol at -20°C overnight
- Wash RNA pellet with 70% ethanol and dissolve in nuclease-free water
- Further purify large RNA and tRNA fractions as needed
Step 3: Sample Preparation and Analysis
- Digest RNA to nucleosides using appropriate enzymes
- Mix known amounts of SILIS with experimental samples
- Analyze via LC-MS/MS with multiple reaction monitoring (MRM)
- Quantify using heavy/light peak area ratios
This approach enables absolute quantification of modified nucleosides, demonstrating the versatility of stable isotope standards across different biomarker classes.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of SIS-based quantification assays requires careful selection of reagents and materials. The following table details essential research reagent solutions and their specific functions in SIS workflows for cancer biomarker validation:
Table 3: Essential Research Reagent Solutions for SIS-Based Assays
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Stable Isotope-Labeled Peptides | Internal standards for protein quantification; normalize for MS variability | Select proteotypic peptides with optimal ionization; consider extended formats for digestion control |
| Stable Isotope-Labeled Proteins | Internal standards accounting for pre-digestion variability | Ideal but often challenging to produce; required for complete process control |
| Trypsin (Sequencing Grade) | Protein digestion to generate measurable peptides | Quality critical for reproducibility; activity must be standardized |
| Immunoaffinity reagents | Target enrichment from complex matrices | Antibodies, aptamers, or other capture agents for specific biomarker isolation |
| Stable Isotope-Labeled Nucleosides | Internal standards for RNA modification quantification | Metabolic labeling in microorganisms provides comprehensive SILIS |
| Depletion/Enrichment Columns | Remove high-abundance proteins | Critical for plasma/serum analysis; improves detection of low-abundance biomarkers |
| LC-MS/MS Grade Solvents | Mobile phase for chromatographic separation | Ensure minimal background interference and consistent ionization |
| Quality Control Materials | Verify assay performance across runs | Pooled patient samples, commercial QC materials, or synthetic standards |
Implementation in Clinical Validation: Regulatory and Practical Considerations
The transition of SIS-based assays from research tools to clinically validated methods requires careful attention to regulatory guidelines and practical implementation considerations. The fit-for-purpose validation approach recognizes that the extent of validation should be commensurate with the intended application of the biomarker [90]. For biomarkers progressing toward clinical decision-making, more rigorous validation is essential.
The Clinical & Laboratory Standards Institute (CLSI) provides specific guidance documents relevant to SIS-based methods, including "C50-A: Mass Spectrometry in the Clinical Laboratory: General Principles and Guidance," "C62-A: Liquid Chromatography-Mass Spectrometry Methods," and "C64: Quantitative Measurement of Proteins and Peptides by Mass Spectrometry" [116]. These guidelines establish performance standards for key validation parameters, including:
- Accuracy and precision (typically within ±25% for biomarkers, ±15% for PK studies)
- Analytical sensitivity (Lower Limit of Quantification)
- Dynamic range (reporting range)
- Specificity and selectivity
- Stability under various storage and processing conditions
The following diagram illustrates the key stages in the clinical validation and implementation pathway for SIS-based biomarker assays, highlighting the iterative nature of this process:
For Laboratory Developed Tests (LDTs), which currently include most targeted proteomics assays, laboratories must establish rigorous quality assurance programs including internal quality control, external quality assessment, and proficiency testing [116]. The implementation of SIS plays a crucial role in meeting these requirements by providing built-in quality control through the continuous monitoring of standard performance across analytical runs.
Stable Isotope-Labeled Standards have revolutionized accurate quantification in cancer biomarker research, providing the analytical rigor necessary to advance promising biomarkers from discovery to clinical application. The comparative data presented in this review demonstrates that the strategic selection of SIS format—whether conventional peptides, extended peptides, or full-length proteins—significantly impacts assay performance, particularly in addressing specific challenges such as digestion variability or matrix effects.
As the field moves toward increasingly complex multi-analyte biomarker panels for cancer detection and monitoring, the role of SIS will only grow in importance. Future developments will likely focus on expanding the availability of SIS for novel biomarker candidates, standardizing SIS implementation across laboratories, and further optimizing SIS design for maximum correction capability. By providing a comprehensive comparison of SIS performance and detailed experimental protocols, this guide equips researchers with the knowledge needed to implement these powerful tools effectively, ultimately contributing to the development of more reliable cancer diagnostics and more personalized patient care.
Conclusion
The successful analytical validation of a cancer biomarker assay is a multifaceted, iterative process that is foundational to the advancement of precision oncology. By adopting a fit-for-purpose mindset, researchers can ensure that validation efforts are both rigorous and appropriately scaled, efficiently navigating the path from exploratory research to clinical application. Future progress hinges on the continued integration of more sensitive and specific technologies, the standardization of reagents and methodologies, and the adoption of multi-parameter or multi-biomarker approaches that better reflect the complex biology of cancer. Ultimately, robust analytical validation is the critical link that ensures biomarker data is reliable, empowering clinicians to make informed treatment decisions and accelerating the development of new, life-saving therapies.
References
- 1. Mass spectrometry based biomarker discovery, verification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528535/]
- 2. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 3. Validation of Analytical Methods for Biomarkers Employed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2744124/]
- 4. Verification, analytical validation, and clinical validation (V3) [https://www.nature.com/articles/s41746-020-0260-4]
- 5. Quantitative PCR validation for research scientists: Part 2 of 2 [https://virologyresearchservices.com/2023/01/13/quantitative-pcr-validation-for-research-scientists-part-2-of-2/]
- 6. Comparison of commercial ELISA assays for quantification ... [https://www.nature.com/articles/s41598-017-06006-4]
- 7. Tutorial: best practices and considerations for mass ... [https://www.nature.com/articles/s41596-021-00566-6]
- 8. Comparison of Analytic Methods for Quantitative Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4642823/]
- 9. Cancer biomarker discovery and validation - Goossens [https://tcr.amegroups.org/article/view/4536/html]
- 10. Fit-for-purpose biomarker method validation for application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2990602/]
- 11. Revisiting the technical validation of tumour biomarker assays [https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-41]
- 12. Best practices for the development and fit-for-purpose ... [https://aapsopen.springeropen.com/articles/10.1186/s41120-021-00050-1]
- 13. Fit-for-Purpose Method Development and Validation ... [https://link.springer.com/article/10.1007/s11095-005-9045-3]
- 14. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 15. Diagnostics Evaluation Branch (DEB) - NCI [https://dctd.cancer.gov/programs/cdp/organization/deb]
- 16. FDA-Approved MI Cancer Seek Test Enhances Tumor ... [https://www.oncotarget.com/news/pr/fda-approved-mi-cancer-seek-test-enhances-tumor-profiling-for-precision-oncology/]
- 17. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 18. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 19. Why is Biomarker Assay Validation Different from that of ... [https://link.springer.com/article/10.1208/s12248-025-01135-5]
- 20. Exploring technical aspects of biomarker assays - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK513094/]
- 21. Quantitative comparison of DNA methylation assays for ... [https://www.nature.com/articles/nbt.3605]
- 22. Comparative Performance of Quantitative and Qualitative ... [https://www.sciencedirect.com/science/article/pii/S277257232200005X]
- 23. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 24. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 25. The first ESMO guidance for AI-based biomarkers [https://dailyreporter.esmo.org/spotlight/the-first-esmo-guidance-for-ai-based-biomarkers]
- 26. Regulatory Flexibilities for Rare Cancer Biomarker ... [https://friendsofcancerresearch.org/news/new-analysis-describes-flexibility-associated-with-companion-diagnostic-development-for-rare-cancer-biomarkers/]
- 27. Clinical performance validation and four diagnostic ... [https://www.nature.com/articles/s41598-025-99273-5]
- 28. Bottom-Up Proteomics: Principles, Workflow, and Analysis [https://www.technologynetworks.com/analysis/articles/deconvoluting-the-proteome-principles-and-advances-in-bottom-up-proteomics-406583]
- 29. ASMS 2025 [https://www2.covaris.com/ASMS2025]
- 30. High-Performance Proteomics Using Nano‑, Capillary‑ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12501992/]
- 31. Mass-spectrometry based metabolomics - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105183/]
- 32. Clinical and analytical validation of MI Cancer Seek ® , a ... [https://www.oncotarget.com/article/28761/text/]
- 33. Types Of Immunoassay - And When To Use Them [https://www.quanterix.com/immunoassay-technologies-past-present-and-future/]
- 34. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 35. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467?utm_source=chatgpt.com]
- 36. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 37. Histo-ELISA technique for quantification and localization of ... [https://www.nature.com/articles/s41598-020-76950-1]
- 38. A novel in-house ELISA assay for the simultaneous ... [https://www.sciencedirect.com/science/article/abs/pii/S002217592500198X]
- 39. Comparison of immunohistochemistry with immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2362713/]
- 40. Flow Cytometry vs. IHC vs. ELISA: How to Choose the ... [https://www.linkedin.com/pulse/flow-cytometry-vs-ihc-elisa-how-choose-right-immunophenotyping-y8zaf]
- 41. Identification and validation of a novel autoantibody ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1494446/full]
- 42. Development and validation of novel RT-PCR assay for ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325000933]
- 43. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 44. Performance Comparison of Droplet Digital PCR and Next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062871/]
- 45. Comparing the Diagnostic Performance of Quantitative ... [https://www.sciencedirect.com/science/article/pii/S1525157823002921]
- 46. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 47. Cost of genetic testing, delayed care, and suboptimal ... [https://pubmed.ncbi.nlm.nih.gov/38391239/]
- 48. Liquid biopsy – a narrative review with an update on current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 49. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 50. Circulating tumor DNA to monitor treatment response in ... [https://www.nature.com/articles/s41698-025-00876-y]
- 51. Exploring Circulating Tumor DNA (CtDNA) and Its Role in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10516512/]
- 52. Proteomics technologies for cancer liquid biopsies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8845389/]
- 53. Clinical utility of various liquid biopsy samples for the early ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1594100/full]
- 54. Prospective validation study: a non-invasive circulating tumor ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03929-y]
- 55. How high-quality antibodies keep your research moving [https://www.abcam.com/en-us/stories/articles/antibody-quality-matters]
- 56. What is a Recombinant Antibody? [https://www.cellsignal.com/about-us/our-approach-process/what-is-recombinant?srsltid=AfmBOopdBd8Zbcch3ObOv-PdNAsPPZSsUvoLAdtCA-QMBAikfTeZ1Pij]
- 57. Recombinant Antibody Technology [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/immunohistochemistry/zoomab-recombinantmab?srsltid=AfmBOoraLxKYjb-TNvkFOfRAERZS3tzq5G6LyWDBowuhv1y9q3yt35fG]
- 58. The Complete Guide to Recombinant Antibody Production [https://www.neobiotechnologies.com/resources/recombinant-antibody-production/?srsltid=AfmBOordHak7r4E8qU-B3K3AJQwNAFdVXVWw-84VmQaCLxLuh3oYevt-]
- 59. Recombinant Antibodies [https://www.thermofisher.com/us/en/home/life-science/antibodies/recombinant-antibodies.html]
- 60. Recombinant antibodies: Genetic engineering and beyond [https://www.thermofisher.com/blog/behindthebench/recombinant-antibodies-genetic-engineering-and-beyond/]
- 61. Review Biomarker validation and testing [https://www.sciencedirect.com/science/article/pii/S1574789114002439]
- 62. Analytical comparability study of recombinant monoclonal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5973765/]
- 63. Indirect clinical validation for predictive biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488805/]
- 64. Cancer Biomarkers - Emerging Trends and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7616034/]
- 65. Navigating the Challenges of Biomarker Testing in Oncology [https://patientworthy.com/2025/10/23/navigating-the-challenges-of-biomarker-testing-in-oncology-innovations-for-low-yield-samples/]
- 66. Quantitative Biomarkers Derived from a Novel, Contrast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10814019/]
- 67. Image Contrast, Image Pre-Processing, and T 1 Mapping ... [https://www.mdpi.com/2072-6694/13/2/240]
- 68. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 69. Data-driven optimization of modulation matrices for low- ... [https://www.sciencedirect.com/science/article/abs/pii/S0030399225011466]
- 70. Solutions to immunoassay interference, cross reactivity and ... [https://www.gyrosproteintechnologies.com/spinblog/immunoassay-interference-crossreactivity-challenges]
- 71. Cross-reactivity in antibody microarrays and multiplexed ... [https://www.sciencedirect.com/science/article/abs/pii/S1367593113002317]
- 72. Factors Affecting Signal Generation in ELISA [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/factors-affecting-ELISA-signal.html]
- 73. Recommendations for Use and Fit-for-Purpose Validation ... [https://link.springer.com/article/10.1208/s12248-015-9820-y]
- 74. Assessing and mitigating batch effects in large-scale omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447944/]
- 75. Lot-to-Lot Variance in Immunoassays—Causes, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10252387/]
- 76. Optimising your single-cell experiment: Where does ... [https://frontlinegenomics.com/optimising-your-single-cell-experiment-where-does-variation-come-from/]
- 77. Comparative analysis of batch correction methods for FDG ... [https://www.nature.com/articles/s41598-023-45296-9]
- 78. Lot-to-Lot Variation - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6223607/]
- 79. Optimizing Sensitivity in Antibody-Based Immunoassays [https://www.genscript.com/optimizing-sensitivity-in-antibody-based-immunoassays.html]
- 80. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 81. Optimized Microfluidic Biosensor for Sensitive C-Reactive ... [https://www.mdpi.com/2079-6374/15/4/214]
- 82. FDA-approved MI cancer seek test enhances tumour ... [https://ecancer.org/en/news/26894-fda-approved-mi-cancer-seek-test-enhances-tumour-profiling-for-precision-oncology]
- 83. Sonobiopsy for sensitive and spatially targeted molecular ... [https://www.nature.com/articles/s44384-025-00014-9]
- 84. Sensitive and selective detection of cancer biomarkers with ... [https://www.sciencedirect.com/science/article/pii/S2666831925000463]
- 85. Understanding Preanalytical Variables and their Effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6004232/]
- 86. Effect of serum sample storage temperature on ... [https://www.nature.com/articles/s41598-022-08429-0]
- 87. The impact of sample storage time on estimates of association ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3131186/]
- 88. Exploring the influence of pre-analytical variables on gene ... [https://www.nature.com/articles/s41598-025-88756-0]
- 89. Fit-for-purpose biomarker method validation in anticancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644610002606]
- 90. Fit-for-purpose biomarker method validation for application ... [https://www.nature.com/articles/6605910]
- 91. Cancer Biomarkers and Precision Oncology: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11571259/]
- 92. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 93. The Biomarker Toolkit — an evidence-based guideline to ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-03075-3]
- 94. Pivotal Evaluation of the Accuracy of a Biomarker Used for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2567415/]
- 95. Understanding Analytical Measurement Range [https://www.thetechplaybook.co/blog/understanding-analytical-measurement-range]
- 96. The Linearity or Reportable Range Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson26.html]
- 97. An Explanation of Sensitivity and the LLD, LLOQ, and ... [https://www.quansysbio.com/support/explanation-of-sensitivity-lld-lloq-and-uloq/]
- 98. Spike and Recovery and Linearity of Dilution Assessment [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/spike-recovery-linearity-assessment.html]
- 99. Limit of Quantitation - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/limit-of-quantitation]
- 100. Analytical Validation of MyProstateScore 2.0 [https://www.mdpi.com/2075-4418/15/7/923]
- 101. Validation of an LC-MS/MS Method for the Simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030624/]
- 102. Multiplex assays for biomarker research and clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248403/]
- 103. MALDI-TOF mass spectrometric immunoassay of multiple ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025000360]
- 104. Recent developments in mass-spectrometry-based targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10826105/]
- 105. with mass spectrometry-derived p-tau quantification for the ... [https://pubmed.ncbi.nlm.nih.gov/38185677/]
- 106. Comparison of immunoassay- with mass spectrometry-derived ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-023-00689-2]
- 107. A large-scale, multi-centre validation study of an AI ... [https://www.nature.com/articles/s41698-025-01105-2]
- 108. A new panel of pancreatic cancer biomarkers discovered ... [https://www.nature.com/articles/bjc2017365]
- 109. Harnessing Mass Spectrometry for Biomarker Discovery in ... [https://blog.crownbio.com/biomarker-and-mass-spectrometry-aml]
- 110. Targeted Mass Spectrometry Enables Multiplexed ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.765898/full]
- 111. Detection of Protein and Metabolites in Cancer Analyses by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606767/]
- 112. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512683/]
- 113. Analytical and clinical validation of a NGS panel in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11464656/]
- 114. Development, testing and validation of a targeted NGS ... [https://www.por-journal.com/journals/pathology-and-oncology-research/articles/10.3389/pore.2024.1611590/full]
- 115. Indirect clinical validation for predictive biomarkers in ... [https://link.springer.com/article/10.1007/s00428-025-04169-4]
- 116. Recent developments in mass-spectrometry-based targeted ... [https://clinicalproteomicsjournal.biomedcentral.com/articles/10.1186/s12014-024-09452-1]
- 117. What can stable isotope internal standards do? [https://www.musechem.com/blog/what-can-stable-isotope-internal-standards-do/?srsltid=AfmBOooUEbFyS908psc69GkfzQ4dT_5VvGJoZCDsMHUvkIBTm_wQFytY]
- 118. Mitigating analyte to stable isotope labelled internal ... [https://www.sciencedirect.com/science/article/pii/S2667145X22000104]
- 119. Comparison of a stable isotope labeled (SIL) peptide and ... [https://pubmed.ncbi.nlm.nih.gov/26279007/]
- 120. Comparison of Proteomic Technologies for Blood-Based ... [https://www.mdpi.com/1422-0067/22/3/1189]
- 121. Production and Application of Stable Isotope-Labeled Internal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6356711/]