Next-Generation Sequencing in Cancer Genomics: Comprehensive Protocols from Foundational Principles to Clinical Applications
This article provides a comprehensive examination of next-generation sequencing (NGS) protocols and their transformative impact on cancer genomics.
Next-Generation Sequencing in Cancer Genomics: Comprehensive Protocols from Foundational Principles to Clinical Applications
Abstract
This article provides a comprehensive examination of next-generation sequencing (NGS) protocols and their transformative impact on cancer genomics. Covering foundational principles, methodological approaches, troubleshooting strategies, and validation frameworks, we detail how NGS enables comprehensive genomic profiling for precision oncology. The content explores diverse sequencing platforms, library preparation techniques, and analytical pipelines for detecting somatic mutations, structural variants, and biomarkers relevant to therapeutic decision-making. Special emphasis is placed on practical implementation challenges, including sample quality considerations, bioinformatics requirements, and clinical validation pathways. With insights into emerging trends like liquid biopsies and single-cell sequencing, this resource serves as an essential guide for researchers and drug development professionals advancing molecularly-driven cancer care.
Foundations of NGS in Cancer Genomics: From Historical Context to Core Principles
The evolution of DNA sequencing technologies from the Sanger method to massively parallel sequencing (Next-Generation Sequencing, NGS) represents a transformative shift in biomedical research, particularly in cancer genomics. This technological revolution has enabled researchers to move from analyzing single genes to comprehensively characterizing entire cancer genomes, transcriptomes, and epigenomes with unprecedented speed and resolution. Sanger sequencing, developed in 1977, established the foundational principles of sequencing technology and remains the gold standard for accuracy in validating specific genetic variants [1]. However, the emergence of NGS platforms has addressed the critical limitations of throughput and scalability, making large-scale projects like The Cancer Genome Atlas (TCGA) feasible and revolutionizing our understanding of cancer biology [2] [3].
In clinical oncology, NGS has become indispensable for identifying somatic mutations, fusion genes, copy number alterations, and other molecular features that drive tumorigenesis. These insights facilitate molecular tumor subtyping, prognostication, and selection of targeted therapies. The ability to detect rare cancer-associated variants in complex tumor samples has positioned NGS as a cornerstone of precision oncology, enabling therapeutic decisions based on the unique genetic profile of individual tumors [4]. This article provides a comprehensive technical overview of sequencing technologies, their applications in cancer research, and detailed protocols for implementing these methods in genomic studies.
Technological Principles and Comparison
Sanger Sequencing: The Foundational Method
Sanger sequencing operates on the principle of chain termination using dideoxynucleotide triphosphates (ddNTPs). These modified nucleotides lack the 3'-hydroxyl group necessary for phosphodiester bond formation, causing DNA polymerase to terminate synthesis when incorporated into a growing DNA strand. The process involves four main steps: (1) DNA template preparation, (2) chain termination PCR with fluorescently-labeled ddNTPs, (3) fragment separation by capillary electrophoresis, and (4) detection via laser-induced fluorescence to generate a chromatogram [1].
The key advantage of Sanger sequencing is its exceptional accuracy and long read lengths (up to 1000 bp), making it ideal for confirming mutations identified through NGS and for sequencing small genomic regions. However, its low throughput and limited sensitivity for detecting variants in heterogeneous samples (typically >20% allele frequency) restrict its utility in comprehensive cancer genomic profiling [1].
Massively Parallel Sequencing: High-Throughput Paradigm
NGS technologies employ a fundamentally different approach characterized by parallel sequencing of millions of DNA fragments. While platform-specific implementations vary, all NGS methods share common principles: (1) library preparation through DNA fragmentation and adapter ligation, (2) clonal amplification of fragments (except for single-molecule platforms), (3) cyclic sequencing through synthesis or ligation, and (4) imaging-based detection [5]. This massively parallel approach enables sequencing of entire human genomes in days at a fraction of the cost of Sanger sequencing, with sufficient depth to detect low-frequency somatic mutations in tumor samples.
Comparative Analysis of Sequencing Platforms
Table 1: Technical comparison of sequencing platforms and their applications in cancer genomics
| Characteristic | Sanger Sequencing | Next-Generation Sequencing |
|---|---|---|
| Principle | Chain termination with ddNTPs [1] | Massively parallel sequencing [5] |
| Throughput | Low (single fragment per reaction) [1] | High (millions of fragments simultaneously) [5] |
| Read Length | Long (600-1000 bp) [1] | Short to long (50-300 bp for Illumina; >10 kb for PacBio) |
| Cost per Mb | High for large volumes [1] | Significantly lower [1] |
| Variant Sensitivity | ~20% allele frequency [1] | 1-5% allele frequency with sufficient depth |
| Primary Cancer Applications | Mutation validation, targeted gene sequencing [1] | Whole genome/exome sequencing, transcriptomics, fusion detection, biomarker discovery [5] [4] |
Table 2: NGS enrichment methods for targeted sequencing in cancer research
| Enrichment Method | Principle | Advantages | Limitations | Cancer Applications |
|---|---|---|---|---|
| Hybridization-Based Capture | Solution-based hybridization with biotinylated probes to target regions [5] | High uniformity, flexible target design, cost-effective for large regions | Requires more input DNA, longer protocol | Comprehensive cancer panels, whole exome sequencing [4] |
| Amplicon-Based (e.g., Microdroplet PCR) | PCR amplification of target regions within water-in-oil emulsions [5] | Fast protocol, low DNA input, robust performance | Limited multiplexing capability, lower uniformity | Targeted mutation profiling, circulating tumor DNA analysis |
Applications in Cancer Genomics
Mutation Detection in Heterogeneous Disorders
NGS has proven particularly valuable for diagnosing genetically heterogeneous cancers where multiple genes can contribute to similar phenotypes. In congenital muscular dystrophy research, which presents diagnostic challenges due to phenotypic variability, targeted NGS panels covering 321 exons across 12 genes demonstrated superior diagnostic yield compared to sequential Sanger sequencing. Both hybridization-based and microdroplet PCR enrichment methods showed excellent sensitivity and specificity for mutation detection, though Sanger sequencing fill-in was still required for regions with high GC content or repetitive sequences [5].
Fusion Gene Detection in Solid Tumors
The detection of oncogenic fusion genes, such as NTRK fusions, exemplifies the clinical importance of NGS in cancer diagnosis and treatment selection. RNA-based hybrid-capture NGS has demonstrated high sensitivity for identifying both known and novel NTRK fusions across diverse tumor types, with a prevalence of 0.35% in a real-world cohort of 19,591 solid tumors. Tumor types with the highest NTRK fusion prevalence included glioblastoma (1.91%), small intestine tumors (1.32%), and head and neck tumors (0.95%) [4]. The comprehensive nature of NGS-based fusion detection directly impacts therapeutic decisions, as NTRK fusions are clinically actionable biomarkers with FDA-approved targeted therapies (larotrectinib, entrectinib, repotrectinib) showing high response rates [4].
NGS Fusion Detection Workflow
Biomarker Discovery and Validation
NGS enables the discovery of novel cancer biomarkers through integrated analysis of multiple molecular datasets. In hepatocellular carcinoma (HCC), comprehensive profiling of cleavage and polyadenylation specificity factors (CPSFs) using NGS data from TCGA revealed that CPSF1, CPSF3, CPSF4, and CPSF6 show significant transcriptional upregulation in tumors, with overexpression correlated with advanced disease progression and poor prognosis [3]. Functional validation using reverse transcription-quantitative PCR and cell proliferation assays confirmed the oncogenic roles of CPSF3 and CPSF7, demonstrating how NGS-driven discovery can identify novel therapeutic targets [3].
Similarly, in glioblastoma, integrated CRISPR/Cas9 screens with NGS analysis identified RBBP6 as an essential regulator of glioblastoma stem cells through CPSF3-dependent alternative polyadenylation, revealing a novel therapeutic vulnerability [6]. These examples illustrate how NGS facilitates the transition from biomarker discovery to functional validation and therapeutic development.
Experimental Protocols
DNA Hybrid-Capture Targeted Sequencing for Mutation Detection
Application Note: This protocol is adapted from methods used for congenital muscular dystrophy gene panel sequencing [5] and comprehensive genomic profiling for fusion detection [4], optimized for detecting somatic mutations in cancer samples.
Materials and Reagents:
- Input DNA: 50-200ng from FFPE tissue or fresh frozen tumor samples
- Hybridization capture reagents: Biotinylated oligonucleotide probes targeting cancer-related genes
- Library preparation kit: Fragmentation enzymes, end repair, A-tailing, and ligation reagents
- Sequencing platform: Illumina, Ion Torrent, or similar NGS systems
- Bioinformatics tools: BWA-MEM for alignment, GATK for variant calling, VarScan for somatic mutation detection
Procedure:
- DNA Shearing and Quality Control: Fragment genomic DNA to 150-300bp using acoustic shearing or enzymatic fragmentation. Assess DNA quality and quantity using fluorometric methods.
- Library Preparation: Perform end repair, 3' adenylation, and adapter ligation using dual-indexed adapters to enable sample multiplexing.
- Hybrid Capture: Denature library DNA and hybridize with biotinylated probes for 16-24 hours. Capture probe-bound fragments using streptavidin-coated magnetic beads.
- Post-Capture Amplification: Perform 10-12 cycles of PCR to amplify captured libraries.
- Sequencing: Pool libraries at equimolar concentrations and sequence on appropriate NGS platform (minimum 150bp paired-end reads, 500x coverage for tumor samples).
- Data Analysis: Align sequences to reference genome, perform quality control metrics, and call variants using validated bioinformatics pipelines.
Quality Control Considerations:
- Minimum sequencing depth: 500x for tumor samples
- Minimum unique molecular coverage: 100x
- Include positive and negative control samples in each run
- Verify detection sensitivity for variants at 5% allele frequency
RNA Sequencing for Fusion Gene Detection
Application Note: This protocol describes RNA-based hybrid-capture sequencing for detecting oncogenic fusions, adapted from the methodology used for NTRK fusion detection [4].
Materials and Reagents:
- Input RNA: 50-100ng total RNA from FFPE tissue (DV200 > 30%)
- RNA library preparation kit: Including rRNA depletion or poly-A selection reagents
- Hybridization capture reagents: Biotinylated probes targeting fusion partners
- TruSight Oncology 500 or similar comprehensive assay
- Bioinformatics tools: STAR for alignment, Arriba, STAR-Fusion, or Manta for fusion detection
Procedure:
- RNA Extraction and QC: Extract total RNA from tumor tissue. Assess RNA integrity using fragment analyzer or similar system.
- rRNA Depletion: Remove ribosomal RNA using sequence-specific probes.
- Library Preparation: Fragment RNA, synthesize cDNA, and add dual-indexed adapters.
- Hybrid Capture: Hybridize with bait set covering known and potential fusion partners (e.g., full coding regions of NTRK1/2/3).
- Sequencing: Sequence libraries with minimum 100M reads per sample (2x100bp).
- Fusion Calling: Identify fusion transcripts using multiple algorithms with manual review of supporting reads.
Validation:
- Confirm novel fusions by orthogonal methods (RT-PCR, FISH)
- Compare with IHC for protein expression when antibodies available
- Assess functional impact of fusions through pathway analysis
Cancer NGS Analysis Pipeline
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential research reagents and computational tools for cancer NGS studies
| Category | Specific Product/Platform | Application in Cancer NGS | Key Features |
|---|---|---|---|
| Library Prep Kits | Illumina TruSight Oncology 500 [4] | Comprehensive genomic profiling | Detects SNVs, indels, fusions, TMB, MSI from FFPE |
| Target Enrichment | Hybrid-capture baits (NimbleGen, IDT) [5] | Targeted sequencing | Customizable content, high uniformity |
| Bioinformatics Tools | cBioPortal [3] | Genomic alteration analysis | Interactive exploration of cancer genomics data |
| Bioinformatics Tools | GSCALite [3] | Cancer pathway analysis | Functional analysis of genes in cancer signaling |
| Expression Databases | UALCAN [3] | Gene expression analysis | CPTAC and TCGA data analysis portal |
| Survival Analysis | Kaplan-Meier Plotter [3] | Prognostic biomarker validation | Correlation of gene expression with patient survival |
| Immune Infiltration | TIMER [3] | Tumor immunology | Immune cell infiltration estimation |
| Validation Tools | Sanger Sequencing [1] | NGS variant confirmation | High accuracy for individual variants |
The evolution from Sanger to massively parallel sequencing has fundamentally transformed cancer research and clinical oncology. NGS technologies now enable comprehensive molecular profiling of tumors, revealing the complex genetic alterations that drive cancer progression and treatment resistance. The applications described—from detecting mutations in heterogeneous tumors to identifying actionable gene fusions and novel biomarkers—demonstrate the indispensable role of NGS in advancing precision oncology.
As sequencing technologies continue to evolve, with reductions in cost and improvements in accuracy and throughput, their integration into routine clinical practice will expand. Future developments in single-cell sequencing, long-read technologies, and multi-omics integration will further enhance our ability to decipher cancer complexity, ultimately leading to more effective personalized cancer therapies and improved patient outcomes.
Next-Generation Sequencing (NGS) has fundamentally transformed oncology research and clinical practice by enabling comprehensive genomic profiling of tumors at unprecedented resolution and scale [7]. This technology allows researchers to simultaneously sequence millions of DNA fragments, providing unparalleled insights into genetic variations, gene expression patterns, and epigenetic modifications that drive carcinogenesis [8]. In contrast to traditional Sanger sequencing, which processes single DNA fragments sequentially, NGS employs massively parallel sequencing architecture, making it possible to interrogate hundreds to thousands of genes in a single assay [7]. This capability is particularly valuable for deciphering the complex genomic landscape of cancer, a disease characterized by diverse and interacting molecular alterations spanning single nucleotide variations, copy number alterations, chromosomal rearrangements, and gene fusions [9].
The implementation of NGS in cancer research has accelerated the development of precision oncology approaches, where treatments are increasingly tailored to the specific molecular profile of a patient's tumor [7]. The core NGS workflow encompasses multiple interconnected stages, each with critical technical considerations that collectively determine the success and reliability of genomic analyses. This application note provides a detailed examination of these workflow components, with specific emphasis on protocols and methodological considerations essential for cancer genomics research.
Core NGS Workflow: From Sample to Insight
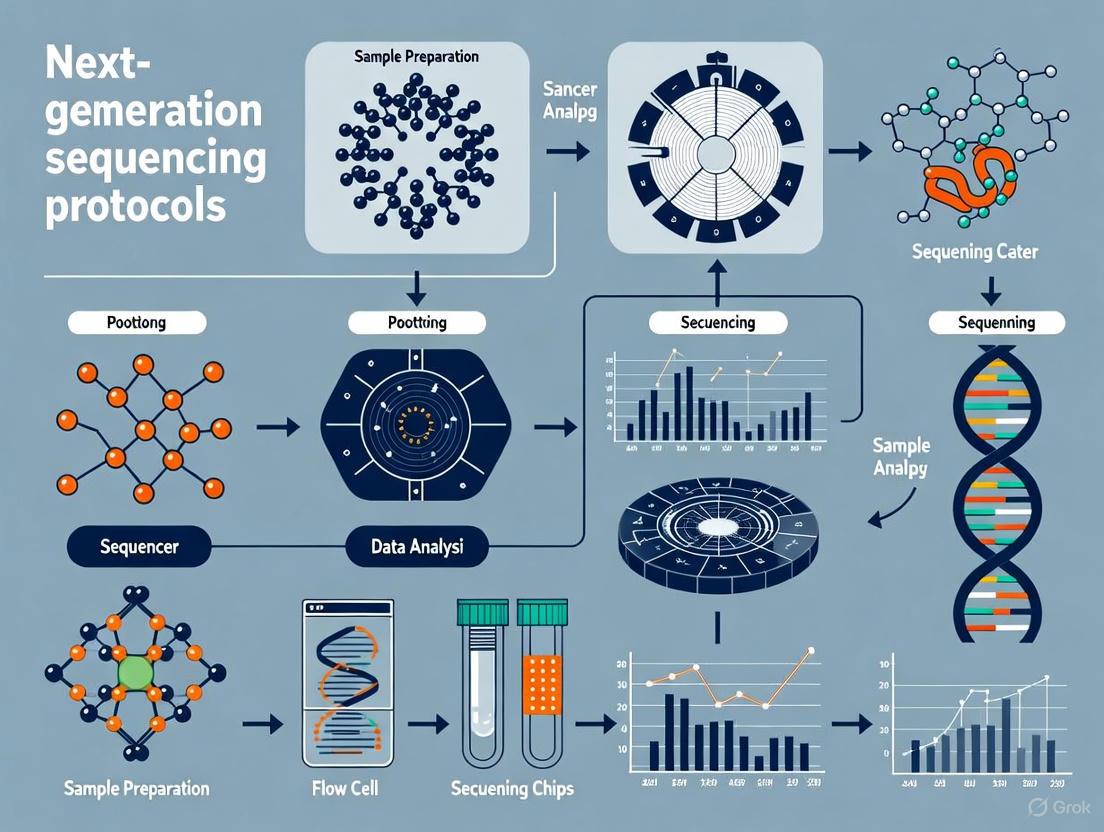
The following diagram illustrates the complete NGS workflow, from sample preparation through final data analysis, highlighting key decision points and processes specific to cancer genomics research.
Sample Preparation: Critical First Steps
Nucleic Acid Extraction and Quality Control
The initial and perhaps most critical phase of the NGS workflow begins with the extraction of high-quality nucleic acids from biological samples [10]. In cancer genomics, sample types range from fresh frozen tissues and cell lines to more challenging specimens like Formalin-Fixed Paraffin-Embedded (FFPE) tissue blocks and liquid biopsies [11]. The quality of extracted nucleic acids profoundly influences all subsequent steps, making rigorous quality control (QC) essential.
Protocol: DNA Extraction from FFPE Tissue Sections [11] [12]
- Sample Preparation: Cut 2-5 sections of 5-10µm thickness from FFPE blocks containing at least 20% tumor tissue (verified by pathological review).
- Deparaffinization: Incubate sections with xylene or a commercial deparaffinization solution, followed by ethanol washes.
- Proteinase K Digestion: Digest tissue overnight at 56°C with proteinase K in appropriate buffer to reverse formalin cross-links.
- Nucleic Acid Purification: Use silica-column or magnetic bead-based purification systems specifically validated for FFPE samples.
- DNase Treatment: For RNA extraction, include DNase digestion to remove genomic DNA contamination.
- Quantification and QC:
- Quantify DNA using fluorometric methods (Qubit dsDNA HS Assay) rather than spectrophotometry [12].
- Assess DNA integrity via Fragment Analyzer, TapeStation, or Bioanalyzer. For FFPE-derived DNA, a DV200 value >50-70% is generally acceptable [11].
- Verify purity using A260/A280 and A260/A230 ratios (ideal values: 1.8-2.0).
Sample Quality Requirements for NGS [12]
| Sample Type | Minimum Quantity | Quality Metrics | Storage/Shipment |
|---|---|---|---|
| Genomic DNA (Blood/Tissue) | 100 ng (WGS)50 ng (Targeted) | A260/A280: 1.8-2.0A260/A230: 2.0-2.2DNA Integrity Number (DIN) >7 | -20°C or belowDry ice shipment |
| FFPE DNA | 50-100 ng | DV200 >50%Fragment size: 200-1000 bp | Room temperatureProtect from moisture |
| Total RNA | 100 ng (Standard RNA-seq)1 ng (Ultra-low Input) | RIN >7DV200 >70% for FFPE | -80°CRNase-free conditions |
| Cell-Free DNA | 1-50 ng (depending on panel) | Fragment size: ~160-180 bp | -80°CAvoid freeze-thaw cycles |
Library Preparation: Converting Nucleic Acids to Sequencable Formats
Library preparation transforms extracted nucleic acids into formats compatible with NGS platforms through fragmentation, adapter ligation, and optional indexing steps [10]. The choice of library preparation method depends on the experimental goals, sample type, and available resources.
Protocol: Library Preparation Using Hybridization Capture [11]
DNA Fragmentation:
- Fragment 10-1000 ng genomic DNA to 150-300 bp fragments using acoustic shearing (Covaris) or enzymatic fragmentation (tn5 transposase).
- For FFPE-derived DNA, additional fragmentation may be unnecessary due to inherent degradation.
End Repair and A-Tailing:
- Convert fragmented DNA to blunt ends using end repair enzyme mix (30 minutes at 20-25°C).
- Add adenine nucleotide to 3' ends using A-tailing enzyme (30 minutes at 37°C).
Adapter Ligation:
- Ligate platform-specific adapters containing sequencing motifs and dual-index barcodes to enable sample multiplexing (15-60 minutes at 20-25°C).
- Clean up ligation reactions using magnetic beads to remove excess adapters.
Library Amplification:
Target Enrichment:
- Hybridize amplified libraries with biotinylated oligonucleotide probes targeting specific genomic regions (16-24 hours at 65°C).
- Capture probe-bound fragments using streptavidin-coated magnetic beads.
- Wash to remove non-specific binding and perform post-capture amplification (4-10 PCR cycles).
Final Library QC:
- Quantify using fluorometric methods (Qubit).
- Assess size distribution using Fragment Analyzer, TapeStation, or Bioanalyzer.
- Validate library molarity via qPCR using library quantification kits.
Comparison of Target Enrichment Methods [11]
| Parameter | Amplicon-Based | Hybridization Capture |
|---|---|---|
| Input DNA | 1-100 ng | 10-1000 ng |
| Workflow Duration | 6-8 hours | 2-3 days |
| On-Target Rate | >90% | 50-80% |
| Uniformity | Lower (amplicon-specific bias) | Higher (Fold-80 penalty: 1.5-3) |
| Target Region Flexibility | Limited to predefined amplicons | Flexible; suitable for large targets |
| Ability to Detect CNVs | Limited | Good |
| Cost | Lower | Higher |
| Optimal Use Cases | Hotspot mutation screening, small panels | Whole exome sequencing, large panels |
Sequencing Platforms and Data Generation
The selection of an appropriate sequencing platform represents a critical decision point in experimental design, with significant implications for data quality, throughput, and analytical approaches [7].
Comparative Analysis of NGS Platforms [14] [7]
| Platform | Technology | Read Length | Throughput per Run | Error Profile | Optimal Cancer Applications |
|---|---|---|---|---|---|
| Illumina NovaSeq | Fluorescent reversible terminators | 50-300 bp (paired-end) | 8000 Gb | Substitution errors (0.1-0.5%) | Whole genome sequencing, large cohort studies |
| Illumina MiSeq | Fluorescent reversible terminators | 25-300 bp (paired-end) | 15 Gb | Substitution errors (0.1-0.5%) | Targeted panels, validation studies |
| Ion Torrent PGM | Semiconductor sequencing | 200-400 bp | 2 Gb | Homopolymer errors | Rapid mutation profiling, small panels |
| PacBio Revio | Single Molecule Real-Time (SMRT) | 10-50 kb | 360 Gb | Random errors (~5-15%) | Structural variant detection, fusion genes |
| Oxford Nanopore | Nanopore sensing | Up to 4 Mb | 100-200 Gb | Random errors (~5-20%) | Real-time sequencing, isoform detection |
Data Analysis: From Raw Sequences to Biological Insights
The transformation of raw sequencing data into biologically meaningful information requires a multi-stage analytical approach with specialized computational tools at each step [8].
Quality Control Metrics for Targeted Sequencing
Rigorous quality assessment at multiple stages of the analytical pipeline is essential for generating reliable, interpretable results [13].
Key NGS Quality Metrics and Interpretation [13]
| Metric | Definition | Optimal Range | Clinical Significance |
|---|---|---|---|
| Depth of Coverage | Number of times a base is sequenced | >100X for somatic variants>500X for liquid biopsies | Ensures detection sensitivity for low-frequency variants |
| On-Target Rate | Percentage of reads mapping to target regions | 50-80% (hybridization capture)>90% (amplicon) | Measures enrichment efficiency; impacts cost and sensitivity |
| Uniformity | Evenness of coverage across targets (Fold-80 penalty) | 1.5-3.0 | Affects ability to detect variants in poorly covered regions |
| Duplicate Rate | Percentage of PCR/optical duplicates | <10-20% (depending on application) | High rates indicate limited library complexity or over-amplification |
| GC Bias | Deviation from expected GC distribution | <10% deviation | Impacts detection in GC-rich or AT-rich regions |
Protocol: Somatic Variant Calling from Tumor-Normal Pairs
Data Preprocessing:
- Quality control: Run FastQC on raw FASTQ files to assess per-base quality scores, GC content, and adapter contamination.
- Adapter trimming: Use Trimmomatic or Cutadapt to remove adapter sequences and low-quality bases.
Alignment to Reference Genome:
- Align trimmed reads to reference genome (GRCh38) using BWA-MEM or STAR (for RNA-seq).
- Convert SAM to BAM format, sort by coordinate, and mark duplicates using Picard Tools.
Variant Calling:
- For DNA sequencing: Use MuTect2 (GATK) for SNVs/indels, Control-FREEC for CNVs, and Manta for structural variants.
- For RNA sequencing: Use STAR-Fusion for gene fusions and RSEM for expression quantification.
Variant Annotation and Prioritization:
- Annotate variants using ANNOVAR or VEP with databases including COSMIC, ClinVar, gnomAD, and dbNSFP.
- Filter variants based on population frequency (<1% in control populations), functional impact (missense, nonsense, splice-site), and clinical relevance (OncoKB, CIViC).
Essential Research Reagents and Solutions
Successful implementation of NGS workflows requires carefully selected reagents and materials optimized for each procedural step.
Essential Research Reagents for NGS in Cancer Genomics
| Reagent Category | Specific Products | Function | Technical Considerations |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA FFPE Kit, AllPrep DNA/RNA Kit, Qubit dsDNA HS Assay | Isolation and quantification of nucleic acids from various sample types | FFPE-specific kits address cross-linking; fluorometric quantification preferred over spectrophotometry [11] [12] |
| Library Preparation | KAPA HyperPlus Kit, Illumina Nextera Flex, IDT xGen cfDNA Library Prep | Fragmentation, adapter ligation, and amplification for sequencing | PCR cycles should be minimized to reduce duplicates and bias; molecular barcodes enable duplicate removal [11] [13] |
| Target Enrichment | Illumina AmpliSeq Cancer Hotspot Panel, IDT xGen Pan-Cancer Panel, Roche NimbleGen SeqCap EZ | Selection of genomic regions of interest | Amplicon-based: rapid, low input; Hybridization capture: better uniformity, larger targets [11] |
| Sequencing Reagents | Illumina SBS Chemistry, Ion Torrent Semiconductor Sequencing Kits, PacBio SMRTbell | Nucleotide incorporation and signal detection during sequencing | Platform-specific; determine read length, error profiles, and throughput capabilities [14] [7] |
| Bioinformatics Tools | BWA, GATK, ANNOVAR, Franklin by Genoox, TumorSecTM | Data analysis, variant calling, and interpretation | Automated pipelines (TumorSecTM) standardize analysis; population-specific databases improve accuracy [8] [11] |
The comprehensive NGS workflow outlined in this application note provides a robust framework for implementing next-generation sequencing in cancer genomics research. Each component—from sample preparation through data analysis—requires careful consideration and optimization to generate clinically actionable insights. As NGS technologies continue to evolve, with emerging approaches including single-cell sequencing, spatial transcriptomics, and artificial intelligence-enhanced analysis, the fundamental workflow principles described here will remain essential for generating reliable, reproducible genomic data to advance precision oncology [7]. The integration of standardized protocols, rigorous quality control measures, and appropriate bioinformatics approaches enables researchers to fully leverage the transformative potential of NGS in deciphering the molecular complexity of cancer.
Cancer is fundamentally a genetic disease driven by the accumulation of molecular alterations that disrupt normal cellular functions, leading to uncontrolled proliferation and metastasis. Next-generation sequencing (NGS) has revolutionized our ability to detect and characterize these alterations with unprecedented resolution and scale, moving beyond single-gene analyses to comprehensive genomic profiling [9] [15]. The complex genomic landscape of cancer is primarily shaped by four key types of genetic alterations: single nucleotide variants (SNVs), copy number variations (CNVs), gene fusions, and various biomarkers that predict therapy response [16] [17]. These alterations activate oncogenic pathways, inactivate tumor suppressors, and create dependencies that can be therapeutically targeted, forming the foundation of precision oncology.
The clinical utility of comprehensive genomic profiling lies in its ability to identify targetable mutations across diverse cancer types simultaneously, providing a more efficient and tissue-saving approach compared to serial single-gene tests [17]. Large-scale genomic studies of advanced solid tumors have demonstrated that over 90% of patients harbor therapeutically actionable alterations, with approximately 29% possessing biomarkers linked to FDA-approved therapies and another 28% having alterations eligible for off-label targeted treatments [16]. This wealth of genomic information, when interpreted through structured frameworks like the Association for Molecular Pathology (AMP) variant classification system, enables clinicians to match patients with appropriate targeted therapies and immunotherapies based on the molecular characteristics of their tumors rather than solely on histology [18].
Characterization of Major Genetic Alterations
Single Nucleotide Variants (SNVs) and Small Insertions/Deletions (Indels)
Single nucleotide variants (SNVs) represent the most frequent class of somatic mutations in cancer, occurring when a single nucleotide base is substituted for another [16]. Small insertions or deletions (indels), typically involving fewer than 50 base pairs, constitute another common mutation type [17]. These alterations can have profound functional consequences depending on their location and nature. Missense mutations result in amino acid substitutions that may alter protein function, nonsense mutations create premature stop codons leading to truncated proteins, and splice site variants can disrupt normal RNA processing [9]. Frameshift mutations caused by indels that alter the reading frame often produce completely aberrant protein products.
Oncogenic SNVs frequently occur in critical signaling pathways that regulate cell growth, differentiation, and survival. For example, mutations in the KRAS gene are found in approximately 10.7% of solid tumors and drive constitutive activation of the MAPK signaling pathway, promoting uncontrolled cellular proliferation [18]. Similarly, EGFR mutations in lung cancer and BRAF V600E mutations in melanoma and other cancers serve as oncogenic drivers that can be targeted with specific kinase inhibitors [9] [15]. Other clinically significant SNVs include PIK3CA mutations in breast and endometrial cancers, IDH1/2 mutations in gliomas and acute myeloid leukemia, and TP53 mutations across numerous cancer types [17].
The clinical detection of SNVs and indels requires sensitive methods capable of identifying low-frequency variants in heterogeneous tumor samples. NGS technologies can reliably detect variants with variant allele frequencies (VAF) as low as 2-5%, with some optimized assays pushing detection limits below 1% [18] [16]. This sensitivity is crucial for identifying subclonal populations that may drive therapy resistance and for analyzing samples with low tumor purity.
Copy Number Variations (CNVs)
Copy number variations (CNVs) are genomic alterations that result in an abnormal number of copies of a particular DNA segment, ranging from small regions to entire chromosomes [16]. In cancer, CNVs primarily manifest as amplifications of oncogenes or deletions of tumor suppressor genes. Gene amplifications can lead to protein overexpression and constitutive activation of oncogenic signaling pathways, while homozygous deletions often result in complete loss of tumor suppressor function [17].
Therapeutically significant CNVs include HER2 (ERBB2) amplifications in breast and gastric cancers, which predict response to HER2-targeted therapies like trastuzumab and ado-trastuzumab emtansine [19]. MYC amplifications occur in various aggressive malignancies including Burkitt lymphoma and neuroblastoma, while MDM2 amplifications are found in sarcomas and other solid tumors and can be targeted with MDM2 inhibitors [16]. CDKN2A deletions, which remove a critical cell cycle regulator, are common in glioblastoma, pancreatic cancer, and melanoma [17].
CNV detection by NGS relies on measuring sequencing depth relative to a reference genome, with specialized bioinformatics tools like CNVkit used to identify regions with statistically significant deviations from normal copy number [18]. The threshold for defining amplifications varies by laboratory but typically requires an average copy number ≥5, while homozygous deletions are identified by complete absence of coverage in tumor samples despite adequate overall sequencing depth [18].
Gene Fusions and Structural Variants
Gene fusions are hybrid genes created by structural chromosomal rearrangements such as translocations, inversions, or deletions that bring together portions of two separate genes [16]. These events can produce chimeric proteins with novel oncogenic functions or place proto-oncogenes under the control of strong promoter elements, leading to their constitutive expression [9]. NGS technologies, particularly RNA sequencing, have dramatically improved the detection of known and novel gene fusions compared to traditional methods like fluorescence in situ hybridization (FISH) [17].
Therapeutically targetable fusions include EML4-ALK in non-small cell lung cancer, FGFR2 and FGFR3 fusions in various solid tumors, and NTRK fusions across multiple cancer types, which respond to specific TRK inhibitors [16] [17]. In prostate cancer, gene fusions are particularly common, with TMPRSS2-ERG fusions occurring in approximately 42% of cases [16]. Other clinically significant fusions include ROS1 fusions in lung cancer and RET fusions in thyroid and lung cancers, both of which have approved targeted therapies [17].
Detection methods for gene fusions have evolved significantly with NGS. DNA-based sequencing can identify breakpoints at the genomic level, while RNA sequencing provides direct evidence of expressed fusion transcripts and can detect fusions regardless of the specific genomic breakpoint location [16]. Various computational tools like LUMPY are employed to identify structural variants from sequencing data, with read counts ≥3 typically interpreted as positive results for structure variation detection [18].
Emerging Biomarkers for Therapy Selection
Beyond specific mutations, several genomic biomarkers provide crucial information for therapy selection, particularly for immunotherapy. Tumor Mutational Burden (TMB) measures the total number of mutations per megabase of DNA and serves as a proxy for neoantigen load, with high TMB (TMB-H) predicting improved response to immune checkpoint inhibitors across multiple cancer types [16] [17]. Microsatellite Instability (MSI) results from defective DNA mismatch repair and creates a hypermutated phenotype that is highly responsive to immunotherapy [18]. PD-L1 expression, while often measured by immunohistochemistry, can also be assessed genomically through PD-L1 (CD274) amplifications, which are enriched in metastatic triple-negative breast cancer and associated with immunotherapy response [20].
Additional emerging biomarkers include HRD (Homologous Recombination Deficiency) scores, which predict sensitivity to PARP inhibitors and platinum-based chemotherapy in ovarian, breast, and prostate cancers [17]. Alterations in DNA damage response (DDR) genes including BRCA1, BRCA2, ATM, and ATRX are also associated with treatment response and prognosis [20]. The comprehensive assessment of these biomarkers through NGS panels enables a more complete understanding of tumor immunobiology and therapeutic vulnerabilities.
Table 1: Key Genetic Alterations in Cancer and Their Clinical Applications
| Alteration Type | Key Examples | Primary Detection Methods | Therapeutic Implications |
|---|---|---|---|
| SNVs/Indels | KRAS (10.7%), EGFR (2.7%), BRAF (1.7%) [18] | NGS, Sanger sequencing | EGFR inhibitors (e.g., osimertinib), BRAF inhibitors (e.g., vemurafenib) |
| CNVs | HER2 amplification, CDKN2A deletion [17] | NGS, FISH, microarray | HER2-targeted therapies (e.g., trastuzumab), CDK4/6 inhibitors |
| Gene Fusions | EML4-ALK, TMPRSS2-ERG (42% in prostate cancer) [16] | RNA-seq, DNA-seq, FISH | ALK inhibitors (e.g., crizotinib), NTRK inhibitors (e.g., larotrectinib) |
| Immunotherapy Biomarkers | TMB-H, MSI-H, PD-L1 amplification [17] [20] | NGS, immunohistochemistry | Immune checkpoint inhibitors (e.g., pembrolizumab) |
Experimental Protocols for Genetic Alteration Detection
Sample Preparation and Quality Control
Robust sample preparation is foundational to successful NGS-based detection of genetic alterations in cancer. The process begins with formalin-fixed paraffin-embedded (FFPE) tumor specimens, which are the most common sample type in clinical oncology, though fresh frozen tissues and liquid biopsy samples are also suitable [18]. Pathological review of hematoxylin and eosin (H&E) stained slides is essential to assess tumor content, with specimens containing ≥25% tumor nuclei generally recommended for optimal performance [17]. Areas of viable tumor are marked for manual macrodissection or microdissection to enrich tumor content and minimize contamination from normal stromal cells.
Nucleic acid extraction typically utilizes the QIAamp DNA FFPE Tissue Kit (Qiagen) or similar systems designed to handle cross-linked, fragmented DNA from archival specimens [18]. For fusion detection, RNA extraction is performed using systems like the ReliaPrep FFPE gDNA Miniprep System (Promega) [20]. DNA and RNA concentration and quality are assessed using fluorometric methods (Qubit dsDNA HS Assay) and spectrophotometry (NanoDrop), with additional fragment size analysis performed via bioanalyzer systems (Agilent 2100 Bioanalyzer) [18] [20]. Minimum quality thresholds typically include DNA quantity ≥20 ng, A260/A280 ratio between 1.7-2.2, and DNA fragment size >250 bp for FFPE samples [18].
For liquid biopsy applications, cell-free DNA (cfDNA) is extracted from plasma samples using specialized kits that efficiently recover short, fragmented DNA. The fraction of circulating tumor DNA (ctDNA) can be estimated through various methods, with higher fractions generally correlating with improved detection sensitivity for somatic mutations [19].
Library Preparation and Target Enrichment
Library preparation converts extracted nucleic acids into sequencing-compatible formats by fragmenting DNA (if not already fragmented), repairing ends, phosphorylating 5' ends, adding A-tails to 3' ends, and ligating platform-specific adapters [9]. For FFPE-derived DNA, additional steps may be required to repair damage caused by formalin fixation, such as deamination of cytosine bases. Adapter-ligated libraries are then amplified using PCR with primers complementary to the adapter sequences [9].
Target enrichment is crucial for focused cancer panels and can be achieved through either hybrid capture or amplicon-based approaches. Hybrid capture methods using kits such as the Agilent SureSelectXT Target Enrichment System employ biotinylated oligonucleotide baits complementary to targeted genomic regions to pull down sequences of interest from the whole-genome library [18]. This approach provides uniform coverage, handles degraded samples effectively, and enables the inclusion of large genomic regions for assessing TMB and CNVs. Amplicon-based methods use PCR primers designed to flank target regions and are highly efficient for small genomic intervals but may struggle with GC-rich regions and typically require higher DNA input [15].
For comprehensive genomic profiling, integrated DNA and RNA sequencing approaches are increasingly employed. The TruSight Oncology 500 assay (Illumina) simultaneously profiles 523 cancer-related genes from both DNA and RNA in a single workflow, detecting SNVs, indels, CNVs, fusions, and immunotherapy biomarkers like TMB and MSI [17]. Similarly, the OncoExTra assay provides whole exome and whole transcriptome data from tumor-normal pairs, offering exceptionally broad coverage for discovery applications [16].
Sequencing and Data Analysis
Sequencing is typically performed on Illumina platforms (NextSeq 550Dx, NovaSeq X) using sequencing-by-synthesis chemistry, though Ion Torrent, Pacific Biosciences, and Oxford Nanopore technologies are also used in specific contexts [18] [21]. The required sequencing depth varies by application, with targeted panels often sequenced to 500-1000x mean coverage to ensure adequate sensitivity for low-frequency variants, while whole exome sequencing typically achieves 100-200x coverage [18] [16]. For the SNUBH Pan-Cancer v2.0 Panel, an average mean depth of 677.8x is maintained, with at least 80% of targeted bases required to reach 100x coverage for a sample to pass quality thresholds [18].
Bioinformatic analysis begins with base calling and demultiplexing, followed by alignment to the reference genome (GRCh37/hg19 or GRCh38/hg38) using tools like BWA (Burrows-Wheeler Aligner) [20]. Variant calling employs specialized algorithms: Mutect2 is commonly used for SNV and indel detection, CNVkit for copy number analysis, and LUMPY for structural variant identification [18]. For tumor-normal paired samples, additional steps distinguish somatic from germline variants. Variant annotation using tools like SnpEff provides functional predictions and databases like ClinVar and COSMIC help prioritize clinically relevant mutations [18].
Variant filtering and prioritization are critical steps that consider variant allele frequency (with thresholds typically ≥2% for SNVs/indels), functional impact (prioritizing nonsense, splice-site, and missense mutations in cancer genes), and presence in population databases (excluding common polymorphisms) [18]. The final step involves clinical interpretation and classification according to guidelines from the Association for Molecular Pathology (AMP), which categorizes variants into four tiers: Tier I (strong clinical significance), Tier II (potential clinical significance), Tier III (unknown significance), and Tier IV (benign or likely benign) [18].
Table 2: Comparison of NGS Approaches for Detecting Genetic Alterations in Cancer
| Parameter | Targeted Panels | Whole Exome Sequencing | Whole Transcriptome Sequencing |
|---|---|---|---|
| Genomic Coverage | 50-500 genes | ~20,000 genes (exons) | All expressed genes |
| Primary Applications | Routine clinical testing, therapy selection | Discovery research, novel gene identification | Fusion detection, expression profiling, immune context |
| SNV/Indel Detection | Excellent for targeted regions | Comprehensive across exomes | Limited to expressed variants |
| CNV Detection | Good for known cancer genes | Comprehensive but requires specialized analysis | Indirect via expression levels |
| Fusion Detection | Limited without RNA component | Limited | Excellent for known and novel fusions |
| TMB Assessment | Possible with sufficient gene content | Gold standard | Not applicable |
| Turnaround Time | 1-2 weeks | 2-4 weeks | 2-3 weeks |
| Cost | $$ | $$$ | $$ |
Clinical Applications and Therapeutic Implications
Matching Genetic Alterations to Targeted Therapies
The primary clinical application of comprehensive genomic profiling is to identify targetable genetic alterations that can be matched with specific therapies. Real-world data from tertiary hospitals demonstrates that approximately 13.7% of patients with Tier I variants (strong clinical significance) receive NGS-informed therapy, with response rates varying by cancer type [18]. In one study of 32 patients with measurable lesions who received NGS-based therapy, 12 (37.5%) achieved partial response and 11 (34.4%) achieved stable disease, with a median treatment duration of 6.4 months [18].
Therapeutic matching follows established guidelines such as the AMP tier system and ESCAT (ESMO Scale for Clinical Actionability of Molecular Targets) framework [18]. Level I alterations have validated clinical utility supported by professional guidelines or FDA approval, such as EGFR mutations in NSCLC treated with osimertinib, BRAF V600E mutations treated with vemurafenib/dabrafenib, and NTRK fusions treated with larotrectinib or entrectinib [16] [15]. Level II alterations show promising efficacy in clinical trials or off-label use, such as HER2 amplifications in colorectal cancer treated with HER2-targeted therapies or MET exon 14 skipping mutations treated with MET inhibitors [16].
The therapeutic actionability rate of genomic alterations is remarkably high. Comprehensive genomic profiling of over 10,000 advanced solid tumors revealed that 92.0% of samples harbored therapeutically actionable alterations, with 29.2% containing biomarkers associated with on-label FDA-approved therapies and 28.0% having alterations eligible for off-label targeted treatments [16]. Similarly, a study of 1,000 Indian cancer patients found that 80% had genetic alterations with therapeutic implications, with CGP revealing a greater number of druggable genes (47%) than did small panels (14%) [17].
Biomarkers for Immunotherapy Response
Genomic biomarkers play an increasingly important role in predicting response to immune checkpoint inhibitors (ICIs). Tumor mutational burden (TMB) has emerged as a quantitative biomarker that measures the total number of mutations per megabase of DNA, with high TMB (TMB-H) generally defined as ≥10 mutations/Mb [17]. TMB-H tumors are thought to generate more neoantigens that make them visible to the immune system, thus increasing the likelihood of response to ICIs [16]. In one cohort, TMB-H was observed in 16% of patients, leading to immunotherapy initiation [17].
Microsatellite instability (MSI) results from defective DNA mismatch repair and creates a hypermutated phenotype that is highly immunogenic [18]. MSI-high (MSI-H) status, detected in approximately 3-5% of all solid tumors, is a pan-cancer biomarker for pembrolizumab approval regardless of tumor origin [16]. MSI status can be determined through multiple methods, including fragment analysis of five mononucleotide repeat markers (BAT-26, BAT-25, D5S346, D17S250, and D2S123) according to the Revised Bethesda Guidelines or through NGS-based approaches that compare microsatellite regions in tumor versus normal DNA [18].
Additional genomic features influencing immunotherapy response include PD-L1 (CD274) amplifications, which are enriched in metastatic triple-negative breast cancer and associated with improved ICI response [20]. Alterations in DNA damage response (DDR) pathways, particularly in homologous recombination repair genes like BRCA1, BRCA2, and ATM, are associated with increased TMB and enhanced immunogenicity [20]. Interestingly, specific mutational signatures such as the APOBEC mutation signature have also been correlated with improved immunotherapy outcomes in certain cancer types [20].
Monitoring Treatment Resistance and Disease Evolution
NGS technologies enable dynamic monitoring of cancer genomes throughout treatment, revealing mechanisms of resistance and disease evolution. Liquid biopsy approaches that sequence circulating tumor DNA (ctDNA) from blood samples provide a non-invasive method for monitoring treatment response, detecting minimal residual disease (MRD), and identifying emerging resistance mutations [19]. For example, in EGFR-mutant lung cancer treated with EGFR inhibitors, serial ctDNA analysis can detect the emergence of resistance mutations such as T790M, C797S, and MET amplifications weeks to months before radiographic progression [15].
The fragmentomic analysis of cell-free DNA has emerged as a promising approach to overcome the limitation of low ctDNA concentration in early-stage cancers [19]. This method exploits differences in DNA fragmentation patterns between tumor-derived and normal cell-free DNA, providing an orthogonal approach to mutation-based liquid biopsy. Studies have demonstrated that fragmentomic features can significantly enhance the sensitivity of liquid biopsy for early cancer detection, particularly when combined with mutation analysis [19].
Longitudinal genomic profiling also reveals clonal evolution patterns under therapeutic pressure. Multi-region sequencing of primary and metastatic tumors has demonstrated substantial spatial heterogeneity, while sequential sampling reveals temporal heterogeneity as treatment-resistant subclones expand under selective pressure [17]. Understanding these evolutionary trajectories is crucial for designing combination therapies that prevent or overcome resistance by simultaneously targeting multiple vulnerabilities.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Cancer Genomics Studies
| Reagent/Material | Manufacturer/Provider | Function in Experimental Workflow |
|---|---|---|
| QIAamp DNA FFPE Tissue Kit | Qiagen | Extraction of high-quality DNA from formalin-fixed paraffin-embedded tissue specimens |
| ReliaPrep FFPE gDNA Miniprep System | Promega | Extraction of DNA from challenging FFPE samples with improved yield |
| Agilent SureSelectXT Target Enrichment System | Agilent Technologies | Hybrid capture-based enrichment of target genomic regions for sequencing |
| TruSight Oncology 500 Assay | Illumina | Comprehensive genomic profiling of 523 cancer-related genes from DNA and RNA |
| NEBNext Ultra DNA Library Prep Kit | New England Biolabs | Preparation of sequencing libraries with high efficiency and low bias |
| Illumina NextSeq 550Dx System | Illumina | High-throughput sequencing platform for clinical genomic applications |
| Agilent 2100 Bioanalyzer | Agilent Technologies | Quality control and fragment size analysis of nucleic acids and libraries |
| Integrated DNA Technologies Pan-Cancer Panel | IDT | Customizable hybrid capture panel targeting 1,021 cancer-related genes |
Visualizing Genetic Alterations and Their Clinical Translation Pathways
The following diagram illustrates the pathway from genetic alteration detection to clinical application, highlighting key decision points in therapeutic matching:
Detection to Therapy Pathway
The NGS experimental workflow encompasses multiple coordinated wet-lab and computational steps as shown below:
NGS Experimental Workflow
Next-Generation Sequencing (NGS) has fundamentally transformed the landscape of cancer research and clinical oncology by enabling comprehensive genomic profiling of tumors. This technology facilitates a paradigm shift from traditional histopathology-based classification to molecularly-driven personalized cancer care [7]. By simultaneously interrogating millions of DNA fragments, NGS provides unprecedented insights into the genetic alterations driving tumorigenesis, enabling researchers and clinicians to identify actionable mutations, guide targeted therapy selection, and monitor treatment response [9]. The integration of NGS into oncology research has been accelerated by a deepening understanding of cancer genomics and a growing arsenal of targeted therapeutics, making it an indispensable tool for advancing precision oncology initiatives [22].
NGS technologies have displaced traditional Sanger sequencing due to their massively parallel sequencing architecture, which provides significantly higher throughput, greater sensitivity for detecting low-frequency variants, and the ability to comprehensively detect diverse genomic alterations including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), gene fusions, and structural variants from a single assay [7]. The continued evolution of NGS platforms and analytical approaches has positioned this technology as the foundation for modern cancer genomics research and clinical applications, from basic discovery to translational research and clinical trials [23].
NGS Methodologies and Technical Approaches
Core NGS Workflow and Platform Selection
The NGS workflow comprises three major components: sample preparation, sequencing, and data analysis [24]. The process begins with extracting genomic DNA from patient samples, followed by library generation that creates random DNA fragments of a specific size range with platform-specific adapters [24]. For targeted approaches, an enrichment step isolates genes or regions of interest through multiplexed PCR-based methods or oligonucleotide hybridization-based methods [24]. The sequenced samples undergo massive parallel sequencing, after which the resulting sequence reads are processed through computational pipelines for base calling, read alignment, variant calling, and variant annotation [24].
Selecting an appropriate NGS method depends on the research objectives, desired genomic information, and available sample types [23]. The major NGS approaches include:
Whole Genome Sequencing (WGS): Provides the most comprehensive analysis of entire genomes, valuable for discovering novel genomic alterations and characterizing novel tumor types [23]. However, WGS requires high sample input, generates complex data, and may not be practical for limited or degraded samples [23].
Exome Sequencing: Focuses on the protein-coding regions of the genome (approximately 1-2%), where most known disease-causing mutations reside [24]. This approach generates data at higher coverage depth than WGS, providing more confidence in detecting low allele frequency somatic variants [23].
Targeted Sequencing Panels: Interrogate predefined sets of genes, variants, or biomarkers relevant to cancer pathways [23]. This is the most widely used NGS method in oncology research due to lower input requirements, compatibility with compromised samples like FFPE tissue, higher sequencing depth, and more manageable data analysis [24] [23].
RNA Sequencing: Facilitates transcriptome analysis to detect gene expression changes, fusion transcripts, and alternative splicing events [9] [23].
Table 1: Comparison of Major NGS Approaches in Cancer Research
| NGS Method | Genomic Coverage | Recommended Applications | Sample Requirements | Advantages | Limitations |
|---|---|---|---|---|---|
| Whole Genome Sequencing | Entire genome | Discovery research, novel alteration identification, comprehensive profiling | High-quality, high-molecular weight DNA (typically 1μg) [23] | Most comprehensive, detects all variant types across genome | High cost, large data storage, complex analysis, not suitable for degraded samples |
| Exome Sequencing | Protein-coding regions (1-2% of genome) | Identifying coding variants, focused discovery | Moderate input requirements (typically 500 ng) [23] | Balances comprehensiveness with practicality, higher depth than WGS | Misses non-coding variants, uneven coverage, not recommended for FFPE [23] |
| Targeted Sequencing Panels | Selected genes/regions | Routine research, clinical trials, biomarker validation | Low input (minimum 10 ng), compatible with FFPE and degraded samples [23] | High depth, cost-effective, manageable data, ideal for limited samples | Limited to predefined targets, cannot discover novel genes outside panel |
| RNA Sequencing | Transcriptome | Gene expression, fusion detection, splicing analysis | Total RNA (500 ng–2 μg for whole transcriptome) [23] | Detects expressed variants, fusion transcripts, expression levels | RNA stability challenges, complex data normalization |
Sample Considerations for Optimal NGS Results
Sample quality and preparation critically impact NGS success. Different sample types present unique challenges and requirements for optimal sequencing results:
FFPE Tissue: The most common sample type in oncology research, but fixation causes cross-linking, strand breaks, and nucleic acid fragmentation [23]. DNA from FFPE is typically low molecular weight with fragments <300 bp, resulting in variable library yields and potential reduced data accuracy without proper methods [23]. Targeted amplicon sequencing is most reliable for FFPE due to compatibility with short fragments [23].
Fresh-Frozen Tissue: Provides the highest quality nucleic acids compatible with all NGS methods [23].
Liquid Biopsies: Utilize cell-free DNA (cfDNA) from blood or other fluids, with tumor DNA representing only a small fraction of total cfDNA [23]. This requires specialized ultra-deep targeted sequencing to sufficiently cover tumor DNA [23]. cfDNA consists of very short fragments that degrade rapidly, necessitating optimized collection, processing, and storage conditions [23].
Fine-Needle Aspirates and Core-Needle Biopsies: Limited samples best analyzed with targeted sequencing due to low input requirements [23]. Quality depends on cytopreparation method, with fresh or frozen samples preferred over formalin-fixed [23].
Tumor content is another critical consideration, with typical minimum requirements of 10-20% to avoid false-negative results [23]. Tumor enrichment techniques include macrodissection or pathologist-guided selection of cancer cell-rich areas [23].
Diagram 1: Comprehensive NGS Workflow for Cancer Research. This diagram illustrates the key steps in the NGS process, from sample collection through interpretation, highlighting critical decision points and methodology options.
Key Research Applications in Precision Oncology
Comprehensive Genomic Profiling for Actionable Alterations
NGS enables comprehensive genomic profiling that identifies actionable mutations across multiple cancer types, facilitating personalized treatment approaches. Research demonstrates that approximately 62.3% of tumor samples harbor actionable biomarkers identifiable through NGS, with tissue-agnostic biomarkers present in 8.4% of cases across diverse cancer types [25]. The clinical actionability of these findings is substantial, with real-world studies showing that 26.0% of patients harbor Tier I variants (strong clinical significance) and 86.8% carry Tier II variants (potential clinical significance) according to Association for Molecular Pathology classification [18].
In clinical implementation studies, NGS-based therapy led to measurable benefits, with 37.5% of patients achieving partial response and 34.4% achieving stable disease [18]. The median treatment duration was 6.4 months, demonstrating the meaningful clinical impact of NGS-guided treatment selection [18]. The prevalence of actionable alterations varies by cancer type, with highest rates observed in central nervous system tumors (83.6%), lung cancer (81.2%), and breast cancer (79.0%) [25].
Table 2: Prevalence of Actionable Biomarkers Across Major Cancer Types
| Cancer Type | Prevalence of Actionable Alterations | Most Common Actionable Alterations | Tumor-Agnostic Biomarker Prevalence |
|---|---|---|---|
| Central Nervous System Tumors | 83.6% [25] | IDH1/2, BRAF V600E, TERT promoter [22] | 8.4% across 26 cancer types [25] |
| Lung Cancer | 81.2% [25] | EGFR, ALK, ROS1, RET, KRAS [26] | 16.8% [25] |
| Breast Cancer | 79.0% [25] | PIK3CA, BRCA1/2, ERBB2, AKT/PTEN pathway [26] | Information not specified in search results |
| Colorectal Cancer | Information not specified in search results | KRAS, NRAS, BRAF, MSI-H [25] | 8.4% across 26 cancer types [25] |
| Prostate Cancer | Information not specified in search results | BRCA1/2, HRD, PTEN [25] | 8.4% across 26 cancer types [25] |
| Ovarian Cancer | Information not specified in search results | BRCA1/2, HRD [25] | 8.4% across 26 cancer types [25] |
Tumor-Agnostic Biomarker Discovery
NGS has been instrumental in identifying and validating tumor-agnostic biomarkers that enable treatment decisions based on molecular characteristics rather than tissue of origin [22]. Key tissue-agnostic biomarkers include:
NTRK Fusions: Occur in diverse cancer types including gastrointestinal cancers, gynecological, thyroid, lung, and pediatric malignancies [22]. First-generation TRK inhibitors like Larotrectinib demonstrate impressive efficacy with overall response rates of 79% across multiple trials [22].
RET Fusions: Present in less than 5% of all cancer patients, found in thyroid, lung, and breast cancers [22]. Selective RET inhibitors like Selpercatinib and Pralsetinib show pan-cancer efficacy with response rates of 43.9-57% in non-NSCLC or thyroid carcinomas [22].
Microsatellite Instability-High (MSI-H): Found in multiple cancer types including endometrial (5.9%), gastric (4.7%), and cancer of unknown primary (4%) [25]. MSI-H tumors show significantly higher tumor mutational burden compared to microsatellite stable tumors (median TMB 23.0 vs 5.15) [25].
High Tumor Mutational Burden (TMB-H): Defined as ≥10 mutations/megabase, found in 6.6% of samples across cancer types, with highest proportions in lung (15.4%), endometrial (11.8%), and esophageal (11.1%) cancers [25].
Homologous Recombination Deficiency (HRD): Observed in 34.9% of samples across cancer types, present in approximately 50% of breast, colon, lung, ovarian, and gastric tumors [25]. HRD-positive tumors exhibit significantly higher TMB compared to HRD-negative tumors [25].
Diagram 2: Tumor-Agnostic Biomarkers and Matched Therapies. This diagram illustrates key tissue-agnostic biomarkers detectable by NGS and their corresponding targeted therapeutic approaches.
Experimental Protocols for NGS Implementation
DNA Extraction and Library Preparation Protocol
Sample Requirements and Quality Control:
- Obtain FFPE tissue sections, fresh-frozen tissue, or liquid biopsy samples [23] [18]
- For FFPE samples: Use a sufficient number of slides (typically 5-10 sections of 5-10μm thickness) to meet input requirements [23]
- Ensure tumor content ≥20% through macro-dissection or pathologist review [23]
- Extract DNA using specialized kits (e.g., QIAamp DNA FFPE Tissue kit for FFPE samples) [18]
- Quantify DNA concentration using fluorescence-based methods (e.g., Qubit dsDNA HS Assay) rather than UV absorbance [23]
- Assess DNA purity (A260/A280 ratio between 1.7-2.2) and fragment size [18]
- Minimum input: 20 ng DNA for hybrid capture methods; 10 ng for targeted amplicon sequencing [23] [18]
Library Preparation Steps:
- Fragmentation: Fragment genomic DNA to 300 bp using physical, enzymatic, or chemical methods [9]
- Adapter Ligation: Attach platform-specific adapters to both ends of DNA fragments [9] [24]
- Barcoding: Add unique molecular barcodes to enable sample multiplexing [24]
- Library Amplification: Amplify library using PCR with adapter-specific primers [24]
- Quality Control: Assess library quantity and quality using quantitative PCR and fragment analysis (e.g., Agilent 2100 Bioanalyzer) [9] [18]
- Target Enrichment: For targeted panels, use hybridization capture (e.g., Agilent SureSelectXT) or multiplex PCR approaches to enrich for genes of interest [24] [18]
Sequencing and Data Analysis Protocol
Sequencing Execution:
- Select appropriate sequencing platform based on required read length, throughput, and application [7]
- For targeted panels, sequence on platforms such as Illumina NextSeq 550Dx with recommended coverage >500x for somatic variant detection [18]
- Include both positive and negative controls in each sequencing run [27]
Bioinformatic Analysis Pipeline:
- Base Calling: Convert raw signal data to nucleotide sequences using platform-specific software [24]
- Read Alignment: Map sequence reads to reference genome (e.g., hg19) using aligners like BWA [7]
- Variant Calling:
- Variant Annotation: Annotate variants using SnpEff and filter against population databases (e.g., gnomAD) [18]
- Specialized Biomarker Analysis:
Quality Assurance Measures:
- Implement quality control at each analysis step, monitoring metrics including coverage uniformity, mapping rates, and duplicate reads [27]
- Validate variant calls using orthogonal methods when necessary [24]
- Classify variants according to established guidelines (e.g., AMP/ASCO/CAP standards) [18]
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for NGS in Cancer Genomics
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA from various sample types | QIAamp DNA FFPE Tissue kit, specialized kits for different sample matrices [18] |
| Library Preparation Kits | Fragment processing, adapter ligation, library amplification | Illumina library prep kits, Agilent SureSelectXT for hybrid capture [18] |
| Target Enrichment Systems | Selection of genomic regions of interest | Multiplex PCR approaches, hybridization capture baits (e.g., for 544-gene panels) [18] |
| Sequencing Platforms | Massive parallel sequencing of prepared libraries | Illumina NextSeq 550Dx, platform-specific flow cells and reagents [18] |
| Quality Control Tools | Assessment of nucleic acid and library quality | Qubit dsDNA HS Assay, Agilent 2100 Bioanalyzer, quantitative PCR [23] [18] |
| Bioinformatics Software | Data analysis, variant calling, interpretation | BWA alignment, Mutect2 variant calling, CNVkit, SnpEff annotation [18] |
| Reference Standards | Process validation and quality assurance | Cell line-derived controls, synthetic spike-in controls for variant detection [27] |
NGS technologies have become the cornerstone of precision oncology research, providing comprehensive genomic profiling that enables personalized cancer treatment strategies. The applications span from basic cancer biology research to clinical trial design and implementation, with demonstrated utility in identifying actionable alterations, guiding targeted therapy, and discovering novel biomarkers. The continued refinement of NGS methodologies, analytical pipelines, and quality management systems will further enhance the capabilities of cancer researchers and clinicians to deliver on the promise of precision oncology.
As NGS technologies evolve and integrate with emerging approaches like single-cell sequencing, spatial transcriptomics, and artificial intelligence, their transformative impact on cancer research and patient care will continue to accelerate. The standardized protocols and analytical frameworks presented here provide a foundation for rigorous implementation of NGS in precision oncology research initiatives.
The comprehensive molecular characterization of human cancers has been revolutionized by large-scale, collaborative genomics initiatives. The Cancer Genome Atlas (TCGA) and the International Cancer Genome Consortium (ICGC) represent two landmark programs that have systematically cataloged genomic alterations across thousands of tumors, creating foundational resources for cancer research [28] [29]. These initiatives emerged in the mid-2000s, leveraging advances in next-generation sequencing (NGS) technologies to generate multi-dimensional datasets encompassing genomic, epigenomic, transcriptomic, and proteomic data [30] [31]. The primary objective of these programs was to create a comprehensive map of cancer genomic abnormalities, enabling researchers to identify novel cancer drivers, understand molecular subtypes, and discover potential therapeutic targets.
The scale of these projects is unprecedented in biomedical research. TCGA molecularly characterized over 20,000 primary cancer and matched normal samples spanning 33 cancer types, generating over 2.5 petabytes of publicly available data [28]. Similarly, the ICGC originally aimed to define the genomes of 25,000 primary untreated cancers, with subsequent initiatives expanding this scope [29]. These programs have transitioned cancer research from a single-gene to a systems biology approach, facilitating the discovery of complex molecular interactions and networks that drive oncogenesis. The lasting impact of these resources continues to grow as researchers worldwide utilize these datasets to address fundamental questions in cancer biology and therapeutic development.
The Cancer Genome Atlas (TCGA) Program
The Cancer Genome Atlas (TCGA) was launched in 2006 as a joint effort between the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) [28]. This landmark program employed a coordinated team science approach to comprehensively characterize the molecular landscape of tumors through multiple analytical platforms. TCGA began with a three-year pilot project focusing on glioblastoma multiforme (GBM), lung squamous cell carcinoma (LUSC), and ovarian serous cystadenocarcinoma (OV), which demonstrated the feasibility and value of large-scale cancer genomics [30]. The success of this pilot phase led to the full-scale project from 2009 to 2015, ultimately encompassing 33 different cancer types from 11,160 patients [30].
A key innovation of TCGA was its systematic approach to sample acquisition and data generation. The program established standardized protocols for sample collection, nucleic acid extraction, and molecular analysis to ensure data consistency across participating institutions [28]. Each tumor underwent comprehensive molecular profiling, including whole-exome sequencing, DNA methylation analysis, transcriptomic sequencing (RNA-seq), and in some cases, whole-genome sequencing and proteomic analysis. This multi-platform approach enabled researchers to examine multiple layers of molecular regulation and their interactions in cancer development and progression.
To maximize the research utility of TCGA data, significant efforts were made to curate high-quality clinical information alongside molecular profiles. The TCGA Pan-Cancer Clinical Data Resource (TCGA-CDR) was developed to provide standardized clinical outcome endpoints across all TCGA cancer types [30]. This resource includes four major clinical outcome endpoints: overall survival (OS), disease-specific survival (DSS), disease-free interval (DFI), and progression-free interval (PFI). The TCGA-CDR addresses challenges in clinical data integration arising from the democratized nature of original data collection, providing researchers with carefully curated clinical correlates for genomic findings.
The clinical utility of TCGA data is enhanced through the Genomic Data Commons (GDC), which serves as a unified repository for these datasets [32]. Launched in 2016 and recently upgraded to GDC 2.0, this platform provides researchers with web-based tools for data analysis and visualization directly within the portal, eliminating the need for extensive bioinformatics expertise or specialized analysis tools [32]. The GDC represents a critical evolution in data sharing, making TCGA data accessible to a broader research community and enabling real-time exploration of complex genomic datasets.
Table 1: Key Molecular Data Types in TCGA
| Data Type | Description | Primary Applications |
|---|---|---|
| Whole-Exome Sequencing | Sequencing of protein-coding regions | Identification of somatic mutations in genes |
| RNA Sequencing | Transcriptome profiling | Gene expression analysis, fusion gene detection |
| DNA Methylation Array | Epigenomic profiling | Analysis of promoter methylation and gene silencing |
| Copy Number Variation | Genomic copy number analysis | Identification of amplifications and deletions |
| Clinical Data | Patient outcomes and treatment history | Clinical-genomic correlation studies |
Analytical Methods and Computational Tools
TCGA employed sophisticated computational pipelines for data processing and variant calling. For mutation detection, multiple algorithms were utilized including VarScan and SomaticSniper for somatic single nucleotide variants (SNVs), Pindel for insertion/deletion detection, and specialized tools for copy number alteration (CNA) and structural variation (SV) identification [33]. The alignment of sequencing data to reference genomes and subsequent variant calling followed stringent quality control measures to ensure data reliability.
The analytical approaches developed for TCGA data addressed several unique challenges in cancer genomics. Normalization procedures were implemented to correct for GC content bias and mapping biases inherent in NGS data [33]. For copy number analysis, methods such as GC-based coverage normalization and correction for mapping bias were applied to unique read depth calculations [33]. The integration of multiple data types required specialized statistical methods and visualization tools, leading to the development of resources like the Integrative Genomics Viewer (IGV) for exploring large genomic datasets [33].
International Cancer Genome Consortium (ICGC)
Consortium Structure and Global Collaboration
The International Cancer Genome Consortium (ICGC) was established in 2008 as a global initiative to coordinate large-scale cancer genome studies across multiple countries and institutions [29] [31]. Unlike TCGA's primarily U.S.-focused effort, ICGC was designed as a federated network of research programs following common standards for data generation and sharing. This international approach enabled the characterization of cancer genomes across diverse populations and healthcare systems, capturing a broader spectrum of genomic variation and cancer subtypes.
The original ICGC initiative, known as the 25k Project, aimed to comprehensively analyze 25,000 primary untreated cancers across 50 different cancer types [29]. To date, this effort has produced more than 20,000 tumor genomes for 26 cancer types, with participating countries including Canada, United Kingdom, Germany, Japan, China, and Australia, among others [29]. The distributed nature of ICGC required sophisticated informatics infrastructure for data harmonization, with central portals facilitating data access while raw data remained stored at contributing institutions. This model demonstrated the feasibility of international collaboration in big data cancer research while respecting national data governance policies.
Key Initiatives: PCAWG and ARGO
The Pan-Cancer Analysis of Whole Genomes (PCAWG) project represents a landmark achievement of the ICGC. Commencing in 2013, this international collaboration analyzed more than 2,600 whole-cancer genomes from ICGC and TCGA [29] [31]. Unlike previous efforts focused primarily on protein-coding regions, PCAWG comprehensively explored somatic and germline variations in both coding and non-coding regions, with specific emphasis on cis-regulatory sites, non-coding RNAs, and large-scale structural alterations. The project published a suite of 23 papers in Nature and affiliated journals in February 2020, reporting major advances in understanding cancer driver mutations, structural variations, and mutational processes [31].
Building on these achievements, ICGC has evolved into its next phase known as ICGC ARGO (Accelerating Research in Genomic Oncology) [34]. This initiative aims to analyze specimens from 100,000 cancer patients with high-quality clinical data to address outstanding questions in cancer genomics and treatment. As of recent data releases, ICGC ARGO has reached significant milestones with over 5,500 donors available in the data platform and more than 63,000 committed donors representing 20 tumor types [34]. The ARGO platform emphasizes uniform analysis of specimens with comprehensive clinical annotation, enabling researchers to correlate genomic findings with detailed treatment responses and patient outcomes.
Table 2: ICGC Initiative Overview
| Initiative | Primary Focus | Key Achievements |
|---|---|---|
| 25k Project | Comprehensive analysis of 25,000 primary untreated cancers | >20,000 tumor genomes for 26 cancer types [29] |
| PCAWG | Whole-genome analysis of 2,600+ cancers | 23 companion papers; non-coding driver mutations [31] |
| ICGC ARGO | Clinical translation with 100,000 cancer patients | 5,528 donors in current release; 20 tumor types [34] |
Data Generation and Harmonization
ICGC implemented rigorous technical standards for data generation across participating centers. The PCAWG project alone collected genome data from 2,834 donors, with 2,658 passing stringent quality assurance measures [31]. Mean read coverage was approximately 39× for normal samples and bimodal (38×/60×) for tumor samples, ensuring sufficient depth for variant detection [31]. To address computational challenges in processing nearly 5,800 whole genomes, the consortium utilized cloud computing to distribute alignment and variant calling across 13 data centers on 3 continents [31].
Variant calling in ICGC employed multiple complementary approaches to maximize sensitivity and specificity. For the PCAWG project, three established pipelines were used to call somatic single-nucleotide variations (SNVs), small insertions and deletions (indels), copy-number alterations (CNAs), and structural variants (SVs) [31]. The consensus approach significantly improved calling accuracy, particularly for variants with low allele fractions originating from tumor subclones. Benchmarking against validation datasets demonstrated 95% sensitivity and 95% precision for SNVs, with lower but substantial accuracy for more challenging variant types like indels (60% sensitivity, 91% precision) [31].
Next-Generation Sequencing Methodologies
Core NGS Technologies and Platform Comparisons
Next-generation sequencing technologies form the methodological foundation for modern cancer genomics initiatives. NGS represents a revolutionary leap from traditional Sanger sequencing, enabling massive parallel sequencing of millions of DNA fragments simultaneously [9]. This technological advancement has dramatically reduced the time and cost associated with comprehensive genomic analysis, making large-scale projects like TCGA and ICGC feasible. The core principle of NGS involves fragmenting genomic DNA, attaching universal adapters, amplifying individual fragments, and simultaneously sequencing millions of these clusters through cyclic synthesis with fluorescently labeled nucleotides.
Several NGS platforms have been utilized in cancer genomics research, each with distinct strengths and applications. The Illumina platform, used extensively in TCGA and ICGC, employs bridge amplification on flow cells and fluorescent nucleotide detection [9]. Other technologies include Ion Torrent, which detects hydrogen ions released during DNA polymerization, and Pacific Biosciences, which implements single-molecule real-time (SMRT) sequencing for longer read lengths [9]. The choice of platform depends on research objectives, with considerations including read length, throughput, error rates, and cost per sample.
Table 3: Comparison of Sequencing Technologies
| Feature | Next-Generation Sequencing | Sanger Sequencing |
|---|---|---|
| Cost-effectiveness | Higher for large-scale projects | Lower for small-scale projects [9] |
| Speed | Rapid sequencing of multiple samples | Time-consuming for large volumes [9] |
| Application | Whole-genome, exome, transcriptome | Ideal for sequencing single genes [9] |
| Throughput | Millions of sequences simultaneously | Single sequence at a time [9] |
| Data output | Large amount of data (gigabases) | Limited data output [9] |
Library Preparation and Target Enrichment
Library preparation is a critical first step in NGS workflows, significantly impacting data quality and completeness. The process begins with nucleic acid extraction and quality assessment, followed by fragmentation to appropriate sizes (typically 300 bp) [9]. Following fragmentation, adapter sequences are ligated to DNA fragments, enabling attachment to sequencing surfaces and serving as priming sites for amplification and sequencing. For targeted sequencing approaches commonly used in clinical applications, hybrid capture methods using biotinylated probes selectively enrich genomic regions of interest [18].
In clinical NGS implementation, such as described in the Seoul National University Bundang Hospital (SNUBH) study, specific quality thresholds are maintained throughout library preparation. The SNUBH protocol requires at least 20 ng of DNA with A260/A280 ratio between 1.7 and 2.2, with library size and concentration cutoffs of 250-400 bp and 2 nM, respectively [18]. For targeted panels like the SNUBH Pan-Cancer v2.0 (544 genes), minimum coverage of 80% at 100× is required, with average mean depth of 677.8× across the cohort [18]. These stringent quality control measures ensure reliable variant detection, particularly for low-frequency mutations in heterogeneous tumor samples.
Analytical Pipelines for Variant Detection
The analysis of NGS data requires sophisticated computational pipelines to transform raw sequencing reads into biologically meaningful variants. Following sequencing, raw data undergoes primary analysis including base calling and quality scoring, followed by alignment to reference genomes using tools like BWA or Bowtie [33]. Post-alignment processing includes removal of PCR duplicates, base quality recalibration, and local realignment around indels to reduce false positives [33].
For somatic variant detection in cancer genomes, specialized algorithms have been developed to address tumor-specific challenges such as tumor purity, subclonal populations, and copy number alterations. VarScan employs heuristic approaches and Fisher's exact test to identify somatic mutations, making it suitable for data sets with varying coverage depths [33]. SomaticSniper uses Bayesian theory to calculate the probability of differing genotypes in tumor and normal samples [33]. For structural variant detection, tools like BreakDancer and Lumpy identify large-scale genomic rearrangements from paired-end sequencing data [33] [18]. The integration of multiple calling algorithms, as demonstrated in the PCAWG project, significantly improves variant detection accuracy across different mutation types and allelic fractions.
Experimental Protocols for Cancer Genomics
DNA Extraction and Quality Control from FFPE Samples
Formalin-fixed paraffin-embedded (FFPE) tissue specimens represent the most common source material for clinical cancer genomics studies. The protocol for DNA extraction from FFPE samples begins with manual microdissection of representative tumor areas with sufficient tumor cellularity. The QIAamp DNA FFPE Tissue kit (Qiagen) is commonly used for DNA extraction, providing high-quality DNA despite cross-linking induced by formalin fixation [18]. Following extraction, DNA concentration is quantified using fluorometric methods such as the Qubit dsDNA HS Assay kit on the Qubit 3.0 Fluorometer, which provides more accurate quantification than spectrophotometric methods for degraded FFPE DNA [18].
Quality control assessment includes evaluation of DNA purity using NanoDrop Spectrophotometer, with acceptable A260/A280 ratios between 1.7 and 2.2 indicating minimal protein or solvent contamination [18]. For FFPE-derived DNA, additional quality metrics such as fragment size distribution using tape station analysis may be performed to assess DNA degradation. The minimum input requirement for library preparation is typically 20 ng of DNA, though higher inputs (50-200 ng) are preferred for degraded samples to ensure adequate library complexity and coverage uniformity.
Targeted Sequencing Library Preparation
The following protocol details library preparation for targeted sequencing using hybrid capture, as implemented in the SNUBH Pan-Cancer v2.0 panel [18]:
DNA Shearing: Fragment 50-200 ng of genomic DNA to 300 bp using ultrasonication or enzymatic fragmentation methods.
End Repair and A-tailing: Convert fragmented DNA to blunt ends using a combination of T4 DNA polymerase, Klenow fragment, and T4 polynucleotide kinase. Subsequently, add a single A-base to the 3' ends using Klenow exo- to facilitate adapter ligation.
Adapter Ligation: Ligate Illumina-compatible sequencing adapters containing unique dual indexes to the A-tailed fragments using T4 DNA ligase.
Library Amplification: Amplify adapter-ligated DNA using 4-8 cycles of PCR with high-fidelity DNA polymerase to enrich for properly ligated fragments.
Hybrid Capture: Incubate amplified libraries with biotinylated RNA probes (SureSelectXT Target Enrichment System, Agilent Technologies) targeting 544 cancer-related genes. Use streptavidin-coated magnetic beads to capture probe-bound fragments.
Post-Capture Amplification: Amplify captured libraries with 10-12 cycles of PCR to generate sufficient material for sequencing.
Library Quantification and Quality Control: Assess final library concentration using qPCR and size distribution using Agilent 2100 Bioanalyzer with High Sensitivity DNA Kit. Libraries should show a predominant peak at 250-400 bp with minimal adapter dimer contamination.
Sequencing and Data Analysis
Sequencing is performed on Illumina platforms such as NextSeq 550Dx using 2×150 bp paired-end runs to ensure sufficient coverage of target regions [18]. The following bioinformatic pipeline is implemented for data analysis:
Demultiplexing: Assign reads to specific samples based on unique dual indexes using bcl2fastq or similar tools.
Read Alignment: Map sequencing reads to the reference genome (hg19) using BWA-MEM or similar aligners.
Duplicate Marking: Identify and mark PCR duplicates using Picard Tools to prevent false positive variant calls.
Variant Calling:
- SNVs/Indels: Use Mutect2 for somatic single nucleotide variants and small insertions/deletions with minimum variant allele frequency threshold of 2% [18].
- Copy Number Variants: Apply CNVkit to identify copy number alterations, with average copy number ≥5 considered amplification [18].
- Gene Fusions: Detect using LUMPY, with read counts ≥3 interpreted as positive results [18].
Variant Annotation: Annotate identified variants using SnpEff with functional predictions and population frequency databases.
Microsatellite Instability and Tumor Mutational Burden:
Visualization of NGS Data Analysis Workflow
NGS Data Analysis Workflow: This diagram illustrates the comprehensive workflow from sample preparation through clinical reporting for cancer genomic analysis using next-generation sequencing technologies, as implemented in large-scale initiatives and clinical studies [9] [18].
Essential Research Reagent Solutions
Table 4: Essential Research Reagents for Cancer Genomics
| Reagent/Kit | Manufacturer | Primary Function | Application Notes |
|---|---|---|---|
| QIAamp DNA FFPE Kit | Qiagen | DNA extraction from FFPE tissues | Optimized for cross-linked DNA; requires proteinase K digestion [18] |
| SureSelectXT Target Enrichment | Agilent Technologies | Hybrid capture for targeted sequencing | Custom pan-cancer panels (e.g., 544 genes); includes biotinylated RNA baits [18] |
| Illumina Sequencing Kits | Illumina | Cluster generation and sequencing | Platform-specific (NextSeq 500/550/2000); includes flow cells and SBS reagents [18] |
| Qubit dsDNA HS Assay | Thermo Fisher Scientific | Fluorometric DNA quantification | Specific for double-stranded DNA; more accurate than spectrophotometry for FFPE DNA [18] |
| Agilent High Sensitivity DNA Kit | Agilent Technologies | Library quality assessment | Chip-based analysis for size distribution (250-400 bp ideal) [18] |
Clinical Implementation and Impact
Real-World Clinical Utility of NGS Profiling
The translation of cancer genomics from research to clinical practice is demonstrated in real-world studies such as the SNUBH experience, where NGS testing was implemented for 990 patients with advanced solid tumors [18]. Using the Association for Molecular Pathology (AMP) variant classification system, 26.0% of patients harbored tier I variants (strong clinical significance), and 86.8% carried tier II variants (potential clinical significance) [18]. The most frequently altered genes in tier I were KRAS (10.7%), EGFR (2.7%), and BRAF (1.7%), reflecting both common oncogenic drivers and potentially actionable therapeutic targets.
A critical measure of clinical utility is the implementation of genomically-matched therapies based on NGS findings. In the SNUBH cohort, 13.7% of patients with tier I variants received NGS-based therapy, with varying rates across cancer types: thyroid cancer (28.6%), skin cancer (25.0%), gynecologic cancer (10.8%), and lung cancer (10.7%) [18]. Among 32 patients with measurable lesions who received NGS-guided treatment, 12 (37.5%) achieved partial response and 11 (34.4%) achieved stable disease, demonstrating meaningful clinical benefit. The median treatment duration was 6.4 months, with overall survival not reached during follow-up, suggesting improved outcomes for molecularly selected patients [18].
Analytical Validation and Quality Assurance
Robust analytical validation is essential for clinical implementation of NGS testing. The PCAWG project established rigorous benchmarking approaches, where multiple variant calling pipelines were evaluated against validation datasets generated by deep sequencing of custom bait sets [31]. For somatic SNV detection, core pipelines demonstrated individual sensitivity of 80-90%, with precision exceeding 95% [31]. The consensus approach across multiple callers improved sensitivity to 95% while maintaining 95% precision, highlighting the value of complementary algorithms for comprehensive variant detection.
Quality metrics for clinical NGS testing include minimum coverage thresholds, with the SNUBH protocol requiring at least 80% of target bases covered at 100×, achieving average mean depth of 677.8× across the cohort [18]. For variant calling, minimum variant allele frequency thresholds of 2% were implemented to detect mutations in heterogeneous tumor samples [18]. Additional quality parameters include minimum DNA input (20 ng), library concentration (2 nM), and size distribution (250-400 bp), with failure rates of approximately 2.3% primarily due to insufficient tissue specimen or failed DNA extraction [18].
The TCGA and ICGC initiatives have fundamentally transformed cancer research by providing comprehensive molecular landscapes across thousands of tumors. These programs have established standardized approaches for genomic analysis, data sharing, and clinical annotation that continue to serve as models for collaborative science. The transition to subsequent phases like ICGC ARGO demonstrates the ongoing commitment to translating genomic discoveries into clinical applications, with ambitious goals of analyzing 100,000 cancer patients with detailed clinical data [34].
The lasting impact of these initiatives extends beyond their specific genomic findings to the creation of infrastructure and resources that continue to enable new discoveries. The Genomic Data Commons provides unified access to these datasets with increasingly sophisticated analysis tools, supporting a global community of researchers [32]. As NGS technologies evolve toward single-cell sequencing, liquid biopsies, and multi-omics integration, the foundational principles established by TCGA and ICGC—standardization, data sharing, and collaborative science—will continue to guide the next generation of cancer genomics research.
NGS Methodologies and Clinical Applications: Implementing Precision Oncology Protocols
Next-generation sequencing (NGS) has revolutionized cancer genomics research by enabling the comprehensive detection of somatic mutations, structural variants, and expression alterations driving oncogenesis [35]. Selecting the appropriate sequencing platform is paramount for generating clinically actionable insights, as each technology presents distinct trade-offs in accuracy, throughput, read length, and cost [36]. This Application Note provides a structured comparison of predominant short-read platforms—Illumina and Ion Torrent—alongside emerging third-generation long-read technologies from Pacific Biosciences (PacBio) and Oxford Nanopore Technologies (ONT) [37] [38]. We focus on their applicability within cancer research protocols, offering detailed methodologies and data-driven guidance for researchers and drug development professionals engaged in precision oncology.
The core distinction between platforms lies in their underlying sequencing biochemistry and detection methods, which directly influence their performance in genomics applications [35] [36].
Illumina employs sequencing-by-synthesis with fluorescently-labeled, reversibly-terminated nucleotides. Clusters of identical DNA fragments are generated on a flow cell via bridge amplification. As each nucleotide is incorporated, a camera captures the fluorescent signal, enabling base identification [35]. This technology is known for its high accuracy.
Ion Torrent utilizes semiconductor technology, detecting hydrogen ions released during nucleotide incorporation. This method directly translates chemical signals into digital information without needing optics, cameras, or fluorescent dyes [35] [39]. DNA is amplified via emulsion PCR on microscopic beads, which are then deposited into semiconductor chip wells [35].
Third-Generation/Long-Read Technologies sequence single DNA molecules in real time without amplification. PacBio's Single Molecule Real-Time (SMRT) sequencing observes DNA synthesis in real time within zero-mode waveguides [38]. Oxford Nanopore's technology threads DNA strands through protein nanopores, detecting changes in ionic current as bases pass through [38].
The table below summarizes the key specifications of these platforms for direct comparison.
Table 1: Key Specifications of Major Sequencing Platforms
| Feature | Illumina | Ion Torrent | PacBio (HiFi) | Oxford Nanopore |
|---|---|---|---|---|
| Technology | Fluorescent SBS | Semiconductor detection | SMRT sequencing | Nanopore detection |
| Read Length | Up to 2x300 bp (paired-end) [35] | Up to 600 bp (single-end) [35] | 10-25 kb [38] | Tens of kb, up to >100 kb [37] |
| Typical Accuracy | >99.9% (Q30) [35] [40] | ~99% (higher indel errors) [35] | >99.9% (Q30) [38] | Simplex: ~Q20 (99%); Duplex: >Q30 (99.9%) [38] |
| Throughput Range | Millions to billions of reads [35] | Millions to tens of millions of reads [35] | Moderate to High [37] | Moderate to High [38] |
| Primary Error Mode | Substitution | Insertion/Deletion (homopolymers) [35] | Random (corrected in HiFi) | Insertion/Deletion |
| Run Time | ~4-48 hours [41] | A few hours to ~1 day [35] | Hours to days | Minutes to days |
| Key Cancer Application | SNV/indel detection, panels, RNA-seq | Targeted panels, rapid turnaround | SV detection, phasing, fusion genes | SV detection, epigenetics, rapid diagnostics |
Application in Cancer Genomics
Each sequencing platform offers distinct advantages for specific cancer genomics applications:
- Illumina is the gold standard for detecting single nucleotide variants (SNVs) and small insertions/deletions (indels) due to its high base-level accuracy [35] [40]. Its high throughput and availability of paired-end sequencing make it ideal for whole-genome sequencing (WGS), whole-exome sequencing (WES), large gene panels, and transcriptome profiling (RNA-seq) to identify differentially expressed genes and gene fusions [41].
- Ion Torrent excels in focused, rapid diagnostic applications. Its speed and simpler workflow are beneficial for targeted gene panels (e.g., for hotspot mutation screening in solid tumors) [35] [42]. However, its higher error rate in homopolymer regions requires careful bioinformatics validation for clinical reporting [35].
- Third-Generation Sequencing addresses critical limitations of short-read technologies in oncology. Long reads are indispensable for resolving complex structural variants, mapping chromosomal rearrangements, phasing haplotypes (e.g., in loss of heterozygosity studies), identifying complex gene fusions, and detecting epigenetic modifications like methylation natively [37] [38]. PacBio's high-fidelity (HiFi) reads provide accuracy for variant calling, while ONT's real-time capability allows for ultra-rapid pathogen identification in immunocompromised patients [38].
Experimental Protocols
Protocol 1: Illumina-Based Whole Exome Sequencing for Somatic Variant Discovery
Principle: This protocol uses hybrid capture to enrich protein-coding regions from tumor and matched normal DNA, followed by Illumina sequencing to identify tumor-specific SNVs and indels with high confidence [35] [41].
Materials:
- DNA Samples: High-quality genomic DNA (≥100 ng) from tumor and matched normal tissue.
- Library Prep Kit: Illumina DNA Prep kit or equivalent.
- Exome Enrichment Kit: IDT xGen Exome Research Panel or similar.
- Sequencing Platform: Illumina NovaSeq X, NextSeq 1000/2000, or MiSeq [41].
- Bioinformatics Tools: DRAGEN Bio-IT Platform, GATK, MuTect2.
Procedure:
- Library Preparation: Fragment genomic DNA to 200-300 bp. Perform end-repair, A-tailing, and adapter ligation using the Illumina DNA Prep kit. Clean up libraries using SPRI beads.
- Exome Capture: Hybridize library to biotinylated exome capture baits. Wash away non-specific fragments and elute the captured DNA.
- Library Amplification: Perform PCR amplification of the enriched library. Validate library quality and quantity using Agilent Bioanalyzer and qPCR.
- Sequencing: Pool libraries and load onto the Illumina flow cell. Sequence using a 2x150 bp paired-end run on a NovaSeq X Plus to achieve >100x coverage.
- Data Analysis:
- Align FASTQ data to a reference genome (e.g., GRCh38) using DRAGEN or BWA-MEM.
- Call somatic variants (SNVs/indels) using DRAGEN or MuTect2, with the matched normal as a control.
- Annotate variants using databases like COSMIC and ClinVar.
Protocol 2: Long-Read Sequencing for Structural Variant Detection
Principle: This protocol leverages PacBio HiFi or ONT duplex sequencing to generate long, accurate reads capable of spanning large structural variants (SVs), complex rearrangements, and repetitive regions often missed by short-read technologies [37] [38].
Materials:
- DNA Samples: High-molecular-weight (HMW) gDNA (≥1 μg, average fragment size >30 kb).
- Library Prep Kit: PacBio SMRTbell Prep Kit or ONT Ligation Sequencing Kit.
- QC Instrument: Pulsed-field gel electrophoresis or Fragment Analyzer.
- Sequencing Platform: PacBio Revio or Sequel IIe / ONT PromethION.
- Bioinformatics Tools: PBSV or Sniffles for SV calling, minimap2 for alignment.
Procedure:
- DNA QC and Size Selection: Assess DNA integrity and fragment size using pulsed-field gel electrophoresis. A key quality control requirement is an average fragment size >30 kb [37].
- Library Preparation:
- For PacBio: Repair DNA and ligate SMRTbell adapters to create circular templates.
- For ONT: Repair DNA, ligate sequencing adapters.
- Sequencing:
- PacBio HiFi: Load library onto the SMRT cell. Sequence on a Revio system to generate HiFi reads via Circular Consensus Sequencing (CCS).
- ONT Duplex: Load library onto a PromethION flow cell. Perform duplex sequencing with Kit14 for >Q30 accuracy.
- Data Analysis:
- For HiFi data, generate CCS reads. For ONT, perform basecalling with Dorado.
- Align long reads to the reference genome using minimap2.
- Call SVs (deletions, duplications, inversions, translocations) using specialized tools (PBSV, Sniffles).
- Phase variants and analyze methylation (from ONT data).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for NGS Workflows in Cancer Research
| Item | Function | Example Use Case |
|---|---|---|
| Hieff NGS Library Prep Kit | Prepares DNA fragments for sequencing by adding platform-specific adapters. | Standard library construction for Illumina or ONT platforms [37]. |
| IDT xGen Exome Research Panel | Set of biotinylated probes for enriching exonic regions from a genomic library. | Focusing sequencing power on coding regions for efficient mutation discovery [41]. |
| PacBio SMRTbell Prep Kit | Creates circularized DNA templates necessary for PacBio HiFi sequencing. | Generating long, accurate reads for structural variant detection [38]. |
| ONT Ligation Sequencing Kit | Prepares DNA libraries for nanopore sequencing by ligating motor protein adapters. | Enabling real-time, long-read sequencing on MinION or PromethION platforms [38]. |
| SPRI Beads | Magnetic beads for size-selective purification and clean-up of DNA fragments. | Post-reaction clean-up and size selection during library preparation. |
| Agilent Bioanalyzer DNA Kit | Microfluidics-based analysis for quantifying and qualifying DNA library fragment size. | Quality control check of the final library before sequencing [37]. |
Within cancer genomics research, next-generation sequencing (NGS) has become an indispensable tool for elucidating the molecular drivers of tumorigenesis and guiding personalized treatment strategies [43]. The accuracy and reliability of NGS data are fundamentally dependent on the initial steps of sample preparation, particularly library construction and target enrichment [9] [10]. These processes convert extracted nucleic acids into a format compatible with sequencing platforms and selectively enrich for genomic regions of interest, thereby optimizing data quality and cost-efficiency [44]. This application note provides a detailed comparison of DNA and RNA library preparation methodologies, outlines key target enrichment approaches, and presents standardized protocols tailored for cancer genomics applications, providing researchers with practical guidance for implementing these critical techniques.
DNA vs. RNA Library Preparation: Core Strategies and Workflows
Library preparation is a pivotal first step in the NGS workflow, requiring different strategies for DNA and RNA to address their distinct biological characteristics and research objectives [10].
DNA Sequencing Library Preparation
The foundational steps for preparing a DNA sequencing library involve fragmenting the genomic DNA and attaching platform-specific adapter sequences. The general workflow is as follows [9] [10]:
- Fragmentation: Double-stranded DNA is fragmented to a desired size (e.g., 200–500 bp) using physical (e.g., sonication), enzymatic (e.g., fragmentase), or chemical methods.
- End-Repair and A-Tailing: The fragmented DNA undergoes end-repair to generate blunt ends, followed by the addition of a single 'A' nucleotide to the 3' ends. This facilitates the ligation of adapters that have a complementary 'T' overhang.
- Adapter Ligation: Sequencing adapters, which may include sample-indexing barcodes for multiplexing, are ligated to the A-tailed fragments.
- Library Amplification and Clean-up: The adapter-ligated fragments are PCR-amplified to enrich for properly constructed library molecules, followed by purification to remove contaminants and size selection to achieve a library of uniform fragment size.
RNA Sequencing Library Preparation
RNA library preparation requires an initial reverse transcription step to convert RNA into more stable complementary DNA (cDNA), and the specific protocol varies depending on the RNA species of interest [9] [10].
- RNA Fragmentation: RNA is typically fragmented to overcome issues related to secondary structures.
- Reverse Transcription: The fragmented RNA is reverse-transcribed into first-strand cDNA using reverse transcriptase and primers. For mRNA sequencing, oligo(dT) primers can be used to selectively target polyadenylated transcripts.
- Second-Strand Synthesis: The RNA template is degraded, and a second DNA strand is synthesized to create double-stranded cDNA.
- Library Construction: The resulting double-stranded cDNA then enters a workflow similar to DNA library preparation, involving end-repair, A-tailing, adapter ligation, and PCR amplification.
Table 1: Key Differences Between DNA and RNA Library Preparation Workflows
| Feature | DNA Sequencing | RNA Sequencing (RNA-Seq) |
|---|---|---|
| Starting Material | Genomic DNA | Total RNA or mRNA |
| Key Conversion Step | Not applicable | Reverse transcription of RNA to cDNA [10] |
| Primary Application in Cancer | Identifying mutations, structural variants, copy number alterations [9] | Analyzing gene expression, fusion genes, alternative splicing [43] |
| Common Enrichment Method | Hybridization capture or amplicon-based [10] | Often poly-A selection for mRNA or rRNA depletion for total RNA [45] |
Target Enrichment Approaches in Cancer Genomics
Targeted sequencing allows for deep sequencing of specific genomic regions of interest, making it cost-effective for analyzing cancer-related genes. The two primary methods are hybridization capture and amplicon sequencing [10].
Hybridization Capture
This method involves solution-based hybridization of the sequencing library to biotinylated probes complementary to the target regions, followed by pull-down with streptavidin-coated magnetic beads [44] [10].
- Workflow: A prepared sequencing library is denatured and hybridized with the probe library. The probe-target hybrids are captured on beads, washed stringently to remove off-target fragments, and then eluted and amplified.
- Advantages: High specificity and uniformity of coverage; capacity for very large target sizes (e.g., whole exome); capacity for discovering novel variants.
- Disadvantages: Requires more steps and longer hands-on time; typically requires more input DNA.
Amplicon Sequencing
This approach uses polymerase chain reaction (PCR) with primers designed to flank the target regions, thereby selectively amplifying them [10].
- Workflow: Target-specific primers, which may also include partial adapter sequences, are used to amplify the regions of interest from the genomic DNA. The amplicons are then further processed into a sequencing library.
- Advantages: Fast and simple workflow; suitable for low-input DNA; high on-target rate.
- Disadvantages: Primers may introduce bias and can struggle with high-GC content regions; limited capability for detecting structural variants or novel fusions.
Table 2: Comparison of Target Enrichment Methods for Cancer Panels
| Parameter | Hybridization Capture | Amplicon Sequencing |
|---|---|---|
| Principle | Solution-based hybridization to biotinylated probes [44] | Multiplex PCR amplification [10] |
| Best For | Large gene panels (e.g., whole exome), discovery of novel variants | Small to medium panels, low-input samples, somatic variant detection |
| Hands-on Time | Longer (~2 days) | Shorter (~1 day) |
| Uniformity | High | Can be lower due to PCR bias |
| Variant Detection | SNVs, Indels, CNVs, Fusions | Primarily SNVs, small Indels |
Detailed Protocols for Key Experiments
Protocol 1: Standard DNA Library Preparation for Hybridization Capture
This protocol is optimized for formalin-fixed, paraffin-embedded (FFPE) or fresh-frozen tumor samples and is compatible with downstream hybridization-based target enrichment [9] [46].
Materials:
- Input: 100–500 ng of genomic DNA (quantity depends on kit and sample quality)
- DNA Library Prep Kit (e.g., KAPA HyperPrep, Illumina TruSeq DNA Nano)
- Magnetic beads (e.g., SPRIselect) for clean-up
- Thermocycler
- Bioanalyzer or TapeStation for quality control
Procedure:
- DNA Fragmentation and Quality Control: Fragment gDNA to a target size of 250–300 bp using Covaris sonication or an enzymatic fragmentase. Verify the fragment size distribution using a Bioanalyzer.
- End-Repair and A-Tailing: Combine fragmented DNA with end-repair and A-tailing enzyme mix. Incubate as per manufacturer's instructions (typically 30 minutes at 20°C for end-repair, followed by 30 minutes at 65°C for A-tailing).
- Adapter Ligation: Add unique dual-indexed adapters to the A-tailed DNA fragments. Use a 10:1 molar excess of adapter to insert DNA. Incubate for 15–30 minutes at 20°C.
- Post-Ligation Clean-up: Purify the ligation reaction using magnetic beads at a 0.8–1.0x ratio to remove excess adapters and retain the desired fragment sizes.
- Library Amplification (Optional): If required, perform a limited-cycle (4–10 cycles) PCR to amplify the adapter-ligated library. Use a high-fidelity polymerase to minimize bias.
- Final Library Purification and QC: Perform a final bead-based clean-up. Quantify the library using fluorometry (e.g., Qubit) and assess the size profile and quality using a Bioanalyzer. The library is now ready for target enrichment or sequencing.
Protocol 2: Stranded RNA Sequencing Library Preparation
This protocol is designed for transcriptome analysis from tumor RNA, preserving strand information to accurately determine the origin of transcripts [45] [10].
Materials:
- Input: 100 ng – 1 µg of total RNA with RIN (RNA Integrity Number) > 7
- Stranded RNA-Seq Kit (e.g., Illumina TruSeq Stranded Total RNA, SMARTer Stranded RNA-Seq)
- rRNA Depletion Kit (e.g., Illumina Ribo-Zero) or mRNA Selection Beads (e.g., oligo(dT))
- Magnetic beads
- Thermocycler
Procedure:
- rRNA Depletion or mRNA Enrichment: Treat total RNA with an rRNA depletion probe set or use oligo(dT) magnetic beads to isolate poly-A containing mRNA.
- RNA Fragmentation and Priming: Elute the enriched mRNA and fragment it using divalent cations at elevated temperature (e.g., 94°C for 5–8 minutes) to generate fragments of ~200 bp.
- First-Strand cDNA Synthesis: Reverse-transcribe the fragmented RNA using random hexamers and reverse transcriptase. The protocol incorporates dUTP in place of dTTP in the second-strand synthesis mix, which is key for strand marking.
- Second-Strand cDNA Synthesis: Synthesize the second strand using DNA Polymerase I. The incorporation of dUTP quenches this strand during subsequent amplification.
- Library Construction: Proceed with standard library construction steps: end-repair, A-tailing, and adapter ligation.
- Strand Selection and Amplification: Prior to PCR, treat the double-stranded library with Uracil-Specific Excision Reagent (USER) enzyme, which degrades the dUTP-containing second strand. The PCR then amplifies only the first strand, preserving strand orientation.
- Final Library QC: Purify the final library with beads and quantify. Validate the library size (~280 bp) and absence of adapter dimers on a Bioanalyzer.
The Scientist's Toolkit: Research Reagent Solutions
Selecting the appropriate reagents and kits is critical for successful NGS library preparation. The table below summarizes key solutions and their applications in cancer genomics research [44] [45] [46].
Table 3: Essential Research Reagents for NGS Library and Target Enrichment Preparation
| Product Type | Example Kits/Systems | Key Function | Considerations for Cancer Genomics |
|---|---|---|---|
| DNA Library Prep | Illumina TruSeq Nano, KAPA HyperPrep, NEBNext Ultra II | Fragments DNA, adds adapters, and amplifies the library. | Input DNA flexibility is crucial for FFPE samples. Kits with lower input requirements (e.g., 10-100 ng) are advantageous [46]. |
| RNA Library Prep | Illumina TruSeq Stranded mRNA, SMARTer Stranded RNA-Seq | Depletes rRNA, converts RNA to cDNA, and constructs a strand-specific library. | Strand specificity is vital for accurately annotating overlapping transcripts and fusion genes [45]. |
| Hybridization Capture | Illumina TruSeq Custom Panels, Agilent SureSelect XT | Enriches for target regions using biotinylated DNA or RNA probes. | Ideal for large, custom cancer panels; allows for uniform coverage across exons [44] [10]. |
| Amplicon Sequencing | Illumina TruSight Tumor Panels, Thermo Fisher Oncomine | Uses multiplex PCR to amplify a predefined set of cancer-related genes. | Fast turnaround and high sensitivity for mutation detection in low tumor purity samples [10]. |
| Automation Systems | Agilent Bravo, Hamilton NGS STAR | Automates liquid handling in library prep and target enrichment. | Improves reproducibility and throughput for processing large sample batches in clinical research settings [44]. |
Next-generation sequencing (NGS) has revolutionized cancer genomics research by enabling massive parallel sequencing of DNA fragments, significantly reducing time and cost compared to traditional Sanger sequencing [9]. This technological advancement provides unprecedented insights into the genomic landscape of tumors, facilitating the discovery of therapeutic targets and personalized treatment strategies. In clinical oncology, three primary NGS approaches are utilized: whole genome sequencing (WGS), whole exome sequencing (WES), and targeted panel sequencing. Each method offers distinct advantages and limitations in terms of genomic coverage, analytical depth, clinical actionability, and cost-effectiveness, making them suitable for different research and clinical applications.
The selection of an appropriate NGS approach depends on multiple factors, including research objectives, clinical context, bioinformatics capabilities, and budgetary constraints. Targeted panels focus on curated gene sets with clinical relevance, WES covers all protein-coding regions (~1% of the genome), and WGS interrogates the entire genome, including non-coding regions. Understanding the technical specifications, performance characteristics, and implementation requirements of each platform is essential for optimizing genomic research in oncology and translating findings into clinically actionable insights.
Comparative Analysis of NGS Approaches
Technical Specifications and Performance Metrics
Table 1: Comparative Technical Specifications of NGS Approaches
| Parameter | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|---|
| Sequencing Region | Selected genes (dozens to hundreds) | Whole exome (~30 million base pairs) | Whole genome (~3 billion base pairs) [47] |
| Protein-Coding Region Coverage | ~2% (selected genes only) | ~85% of known pathogenic variants [48] | ~100% |
| Typical Sequencing Depth | >500X [47] | 50-150X [47] | >30X [47] |
| Data Output Volume | Lowest | 5-10 GB [47] | >90 GB [47] |
| Detectable Variant Types | SNPs, InDels, CNV, Fusion [47] | SNPs, InDels, CNV, Fusion [47] | SNPs, InDels, CNV, Fusion, Structural Variants [47] |
| Non-Coding Region Detection | No | Limited | Comprehensive |
Table 2: Clinical and Practical Considerations in NGS Approach Selection
| Consideration | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|---|
| Cost-Effectiveness | Highest for focused applications | Moderate | Highest [48] |
| Turnaround Time | Shortest (e.g., median 29 days in BALLETT study [49]) | Moderate | Longest |
| Actionability Rate | 21% (small panels) to 81% (CGP) [49] | Moderate | Potentially highest but with interpretation challenges |
| Data Interpretation Burden | Lowest | Moderate | Highest (~3 million variants/sample [48]) |
| Ideal Use Case | Routine clinical testing for known biomarkers | Hypothesis-free exploration of coding regions | Comprehensive discovery including non-coding regions |
Clinical Performance and Actionability
Recent real-world evidence demonstrates the significant clinical impact of comprehensive genomic profiling (CGP). The Belgian BALLETT study, which utilized a 523-gene CGP panel across 12 hospitals, demonstrated the feasibility of decentralized CGP implementation with a 93% success rate and median turnaround time of 29 days [49]. Critically, this approach identified actionable genomic markers in 81% of patients, substantially higher than the 21% actionability rate using nationally reimbursed small panels [49]. Similarly, a South Korean study of 990 patients with advanced solid tumors using a 544-gene panel found that 26.0% of patients harbored tier I variants (strong clinical significance), and 86.8% carried tier II variants (potential clinical significance) [18].
The BALLETT study further reported that a national molecular tumor board recommended treatments for 69% of patients based on CGP results, with 23% ultimately receiving matched therapies [49]. In the South Korean cohort, 13.7% of patients with tier I variants received NGS-based therapy, with the highest rates observed in thyroid cancer (28.6%), skin cancer (25.0%), gynecologic cancer (10.8%), and lung cancer (10.7%) [18]. Among 32 patients with measurable lesions who received NGS-based therapy, 12 (37.5%) achieved partial response and 11 (34.4%) achieved stable disease, demonstrating meaningful clinical benefit [18].
Decision Framework for NGS Platform Selection
Experimental Protocols and Workflows
Sample Preparation and Library Construction
The initial phase of any NGS workflow requires meticulous sample preparation to ensure high-quality results. The process begins with nucleic acid extraction from tumor samples, typically formalin-fixed paraffin-embedded (FFPE) tissue specimens [18]. DNA quality and quantity are assessed using fluorometric methods such as Qubit dsDNA HS Assay, with purity verification via spectrophotometry (A260/A280 ratio between 1.7-2.2) [18]. A minimum of 20ng DNA is typically required for library preparation, though optimal results are obtained with higher inputs [18].
For comprehensive genomic profiling using hybridization capture methods, DNA fragmentation is performed to achieve fragment sizes of approximately 300 base pairs [9]. Library construction involves attaching adapter sequences to DNA fragments, which enables binding to sequencing flow cells and subsequent amplification [9]. The BALLETT study implemented a fully standardized CGP methodology across nine Belgian NGS laboratories using a 523-gene panel, demonstrating that decentralized sequencing with rigorous standardization can achieve a 93% success rate despite variability in local operational factors [49].
NGS Library Preparation Workflow
Sequencing and Data Analysis Protocols
Sequencing is typically performed on platforms such as Illumina NextSeq 550Dx with a minimum depth of coverage varying by application: >500X for targeted panels, 50-150X for WES, and >30X for WGS [47] [18]. The SNUBH Pan-Cancer v2.0 panel implementation achieved an average mean depth of 677.8X, with samples failing if they had less than 80% of bases covered at 100X [18].
Bioinformatics analysis begins with quality control of raw sequencing data using tools like FastQC [47]. Reads are aligned to a reference genome (hg19) using aligners such as BWA [47] [9]. Variant calling employs specialized tools: Mutect2 for single nucleotide variants (SNVs) and small insertions/deletions (indels), CNVkit for copy number variations, and LUMPY for gene fusions [18]. For tumor mutational burden (TMB) calculation, the number of eligible variants within the panel size is normalized to mutations per megabase, excluding variants with population frequency >1% or those classified as benign in ClinVar [18]. Microsatellite instability (MSI) status is determined using tools like mSINGS, which compares microsatellite regions in tumor versus normal samples [18].
Table 3: Key Research Reagent Solutions for Comprehensive Genomic Profiling
| Reagent/Category | Function | Example Products |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA from FFPE tissues | QIAamp DNA FFPE Tissue kit (Qiagen) [18] |
| DNA Quantification Assays | Accurate measurement of DNA concentration and quality | Qubit dsDNA HS Assay kit (Invitrogen) [18] |
| Library Preparation Kits | Fragmentation, adapter ligation, and target enrichment | Agilent SureSelectXT Target Enrichment Kit [18] |
| Hybridization Capture Probes | Selective enrichment of target genomic regions | Illumina TruSight Oncology Comprehensive [50] |
| Sequencing Consumables | Cluster generation and sequencing reactions | Illumina sequencing reagents (Flow Cells, Buffer Kits) |
| Quality Control Tools | Assessment of library size, quantity, and adapter removal | Agilent 2100 Bioanalyzer with High Sensitivity DNA Kit [18] |
Implementation in Cancer Genomics Research
Clinical Validation and Quality Assurance
Successful implementation of comprehensive genomic profiling in clinical and research settings requires rigorous quality control measures and validation protocols. The BALLETT study established that CGP success rates vary by tumor type, with lowest success rates observed in uveal melanoma (72%) and gastric cancer (74%), likely due to limited biopsy material [49]. Turnaround time from sample acquisition to molecular tumor board report averaged 29 days, with significant variability between institutions (range 18-45 days) [49].
Quality metrics for hybridization capture probes include on-target rate (percentage of sequencing data aligning to target regions), coverage uniformity, and duplication rate [47]. High-performing probes demonstrate excellent specificity, sensitivity, uniformity, and reproducibility [47]. For clinical reporting, variants are classified according to established guidelines such as the Association for Molecular Pathology (AMP) tiers: Tier I (variants of strong clinical significance), Tier II (variants of potential clinical significance), Tier III (variants of unknown significance), and Tier IV (benign or likely benign variants) [18].
Biomarker Detection and Therapeutic Matching
Comprehensive genomic profiling enables simultaneous assessment of multiple biomarker classes beyond simple mutation detection. The BALLETT study identified 1957 pathogenic or likely pathogenic SNVs/indels, 80 gene fusions, and 182 amplifications across 276 different genes in 756 patients [49]. The most frequently altered genes were TP53 (46% of patients), KRAS (13%), APC (9%), PIK3CA (11%), and TERT (8%) [49]. Additionally, 16% of patients exhibited high tumor mutational burden (TMB-high), particularly in lung cancer, melanoma, and urothelial carcinomas [49].
Genomically-matched therapy recommendations require integration of molecular findings with clinical context. In the BALLETT study, the national molecular tumor board provided treatment recommendations for 69% of patients, with 23% ultimately receiving matched therapies [49]. Barriers to implementation included drug access, patient performance status, and clinical trial eligibility [49]. The continuous evolution of knowledge bases and biomarker-therapy associations necessitates regular reanalysis of genomic data, as demonstrated by findings that 23% of positive WES results involve genes discovered within the previous two years [48].
Comprehensive genomic profiling through targeted panels, whole exome sequencing, and whole genome sequencing has fundamentally transformed cancer genomics research and precision oncology. Each approach offers distinct advantages, with targeted panels providing cost-effective focused analysis for clinical applications, WES offering a balance between coverage and cost for hypothesis-generating research, and WGS delivering the most comprehensive variant detection for discovery science. Real-world evidence demonstrates that comprehensive genomic profiling identifies actionable biomarkers in most patients with advanced cancer, enabling matched targeted therapies that improve clinical outcomes.
Successful implementation requires standardized protocols, robust bioinformatics pipelines, and interdisciplinary collaboration through molecular tumor boards. As sequencing technologies continue to evolve and costs decrease, the integration of comprehensive genomic profiling into routine cancer research and clinical care will continue to expand, further advancing personalized cancer medicine and therapeutic development.
Next-generation sequencing (NGS) has revolutionized cancer genomics research, enabling comprehensive molecular profiling that guides precision oncology. The application of liquid biopsy for circulating tumor DNA (ctDNA) analysis represents a particularly transformative approach for detecting minimal residual disease (MRD)—the presence of cancer-derived molecular evidence after curative-intent treatment when no tumor is radiologically visible [51] [52]. In solid tumors like non-small cell lung cancer (NSCLC), colorectal cancer, and breast cancer, MRD assessment via ctDNA monitoring provides a highly sensitive biomarker for predicting recurrence and guiding adjuvant therapy decisions [51] [53] [52].
This protocol details the application of NGS-based ctDNA analysis for MRD monitoring, framed within the broader context of cancer genomics research. The core principle leverages the detection of tumor-specific genetic alterations in blood plasma, often at variant allele frequencies as low as 0.001%-0.1%, requiring ultra-sensitive detection platforms [51] [53]. When implemented within rigorous research frameworks, these protocols enable molecular relapse detection with lead times of 3-8 months before radiographic confirmation, creating critical windows for therapeutic intervention [52].
Technology Platforms for ctDNA-Based MRD Detection
The selection of appropriate detection technology is paramount for MRD assessment, as ctDNA can constitute ≤0.01–0.1% of total cell-free DNA (cfDNA) in early-stage cancers or post-treatment settings [51] [53]. MRD detection assays primarily utilize digital PCR (dPCR) and NGS methods, each with distinct advantages and limitations for research applications.
Key Analytical Platforms
Table 1: Comparison of Major MRD Detection Technologies
| Technology | Sensitivity (LoD) | Key Advantages | Limitations | Primary Applications |
|---|---|---|---|---|
| Tumor-Informed NGS (Signatera, RaDaR) | 0.001%-0.02% VAF [51] | High specificity; tracks patient-specific mutations; reduces false positives from CHIP [51] | Requires tumor tissue; longer turnaround; higher cost [51] | Longitudinal MRD monitoring; recurrence risk stratification [51] [52] |
| Tumor-Naïve NGS (Guardant Reveal, InVisionFirst-Lung) | 0.07%-0.33% VAF [51] | No tumor tissue required; faster turnaround; lower cost [51] | Lower sensitivity; may miss patient-specific mutations [51] | Broad screening applications; when tissue is unavailable [51] |
| ddPCR | ~0.001% VAF [51] [54] | Absolute quantification; high sensitivity for known mutations [51] | Limited to predefined mutations; low multiplex capability [51] | Tracking specific known mutations; validation of NGS findings [54] |
| Structural Variant-Based Assays | 0.0011%-0.01% VAF [53] | High specificity from unique chromosomal rearrangements; avoids PCR errors [53] | Requires specialized bioinformatics; limited for tumors without SVs [53] | Early-stage breast cancer; karyotypically complex tumors [53] |
| Phased Variant Sequencing (PhasED-Seq) | <0.0001% tumor fraction [51] [53] | Ultra-sensitive detection; multiple SNVs on same DNA fragment [53] | Complex methodology; computational intensity [51] | Ultra-early recurrence detection; very low tumor fraction scenarios [51] |
Emerging Detection Technologies
Novel approaches are pushing sensitivity boundaries further. Electrochemical biosensors utilizing nanomaterials (e.g., magnetic nano-electrode systems) achieve attomolar sensitivity with rapid results within 20 minutes [53]. Fragmentomics approaches exploit the size difference between ctDNA (90-150 bp) and non-tumor cfDNA, enriching for shorter fragments to improve detection of low-frequency variants [53]. The MUTE-Seq method presented at AACR 2025 uses engineered FnCas9 to selectively eliminate wild-type DNA, significantly enhancing sensitivity for low-frequency mutation detection [54].
Experimental Workflow for MRD Assessment
The complete MRD assessment workflow extends from sample collection through data analysis, with rigorous quality control at each stage to ensure reliable results for research applications.
Figure 1: Complete workflow for ctDNA-based MRD detection, spanning pre-analytical, analytical, and post-analytical phases with critical quality control checkpoints.
Pre-Analytical Phase
Blood Collection and Processing
- Collection Tubes: Use Streck Cell-Free DNA Blood Collection Tubes or K₂EDTA tubes with processing within 2-4 hours of collection [52].
- Plasma Separation: Perform double centrifugation: initial at 1,600×g for 10 minutes at 4°C, followed by supernatant centrifugation at 16,000×g for 10 minutes to remove residual cells [53] [52].
- Plasma Storage: Store at -80°C in multiple aliquots to avoid freeze-thaw cycles.
cfDNA Extraction and QC
- Extraction Kits: Use QIAamp Circulating Nucleic Acid Kit (Qiagen) or similar, with elution volumes of 20-50 μL to maximize concentration.
- Quality Assessment: Quantify using Qubit dsDNA HS Assay and assess fragment size distribution using Agilent 2100 Bioanalyzer with High Sensitivity DNA Kit [18]. Expected cfDNA peak: 160-170bp; mononucleosomal ctDNA peak: 90-150bp [53].
- Minimum Input: 10-30ng cfDNA required for library preparation, though higher inputs (up to 50ng) improve sensitivity [52].
Analytical Phase: Library Preparation and Sequencing
Library Construction
Two primary approaches dominate MRD research applications:
Tumor-Informed Approach
- Tumor Sequencing: Perform whole-exome sequencing (WES) or large panel NGS (e.g., 544-gene panel) on tumor tissue to identify 16-50 patient-specific somatic variants [51] [18].
- Custom Panel Design: Create patient-specific multiplex PCR panel targeting identified variants.
- Plasma Analysis: Track these variants in serial plasma samples using ultra-deep sequencing (>50,000× coverage) [51].
Tumor-Naïve Approach
- Fixed Panel Design: Use predefined panels of recurrent cancer-associated mutations (e.g., 425-gene NGS panel) [51] [52].
- Hybrid Capture: Employ Agilent SureSelectXT Target Enrichment with biotinylated probes for hybridization-based capture [18].
- Amplification: Use unique molecular identifiers (UMIs) to enable error correction and distinguish true variants from PCR/sequencing artifacts [51] [53].
Sequencing Parameters
- Sequencing Depth: Minimum 20,000× read depth, with >50,000× recommended for high-sensitivity applications [51] [52].
- Platforms: Illumina NextSeq 550Dx or NovaSeq X for high-throughput applications; Ion Torrent for rapid turnaround [9] [21].
- Coverage: >80% of targets at 0.1× mean depth as quality threshold [18].
Post-Analytical Phase: Data Analysis and Interpretation
Bioinformatics Processing
- Alignment: Map reads to reference genome (hg19/GRCh38) using BWA-MEM or similar aligner [9] [15].
- Variant Calling: Use MuTect2 for SNVs/indels, CNVkit for copy number variations, and LUMPY for structural variants [18].
- Error Suppression: Apply UMI-based consensus calling and bioinformatic filters to remove artifacts from clonal hematopoiesis (CHIP) [51] [53].
MRD Positivity Criteria
- Statistical Threshold: Variant allele frequency (VAF) significantly above limit of detection (LOD) with p<0.001 [51].
- Multi-Marker Approach: Detection of ≥2 tumor-specific variants in tumor-informed approach increases specificity [51].
- Longitudinal Trend: Consecutive positive results strengthen MRD confirmation [52].
Research Reagent Solutions
Table 2: Essential Research Reagents for ctDNA MRD Analysis
| Reagent Category | Specific Products | Research Application | Key Considerations |
|---|---|---|---|
| Blood Collection Tubes | Streck Cell-Free DNA BCT, K₂EDTA tubes | Plasma preservation for ctDNA analysis | Streck tubes: stability up to 7 days at room temp; EDTA: process within 2-4h [52] |
| cfDNA Extraction Kits | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA Isolation Kit | Isolation of high-quality cfDNA from plasma | Maximize yield from limited input; minimize contamination [52] |
| Library Prep Kits | Illumina TruSeq DNA PCR-Free, Agilent SureSelectXT | NGS library construction from low-input cfDNA | UMI incorporation essential for error correction [53] [18] |
| Target Enrichment | Agilent SureSelectXT (hybrid capture), IDT xGen (amplicon) | Enrichment of tumor-specific variants | Hybrid capture: broader coverage; amplicon: higher sensitivity for known variants [51] [18] |
| Quality Control Assays | Agilent 2100 Bioanalyzer, Qubit dsDNA HS Assay, qPCR | Quantification and qualification of nucleic acids | Fragment size analysis critical for ctDNA enrichment [53] [18] |
| Reference Materials | Seraseq ctDNA Reference Materials, Horizon Multiplex I cfDNA | Assay validation and quality control | Enable standardization across batches and laboratories [52] |
Clinical Validation and Performance Assessment
Robust validation is essential before implementing MRD assays in research settings. Key performance metrics must be established using appropriate reference materials and statistical approaches.
Table 3: Performance Metrics for MRD Assay Validation
| Performance Parameter | Target Specification | Validation Approach |
|---|---|---|
| Analytical Sensitivity | 90-95% detection at 0.01% VAF [51] [52] | Dilution series of reference material with known VAF |
| Analytical Specificity | >99% for variant calling [51] | Analysis of healthy donor plasmas (n≥50) |
| Limit of Detection (LOD) | 0.001%-0.1% VAF depending on technology [51] [53] | Probit analysis of dilution series; 95% detection rate |
| Precision | CV <15% for ctDNA quantification [52] | Replicate analysis across operators, days, and instruments |
| Dynamic Range | 0.001% to 10% VAF [51] | Linear regression of expected vs. observed VAF |
| Input Material QC | 10-50ng cfDNA input; DV200 >30% [52] | Correlation between input quality and assay success |
Clinical Correlation Studies
For research applications, MRD assays should demonstrate:
- Lead Time: ctDNA positivity 88-200 days (median 3-6 months) before radiographic recurrence [52].
- Positive Predictive Value: >90% for recurrence in NSCLC and colorectal cancer studies [52].
- Negative Predictive Value: 96-100% for recurrence-free survival across multiple cancer types [51] [52] [54].
Implementation Considerations for Research Studies
Timing of Sampling
Critical timepoints for MRD assessment in therapeutic studies include:
- Pre-treatment: Baseline genetic characterization and variant identification [52].
- Post-treatment: 3-8 weeks after completion of curative-intent therapy (surgery, chemoradiation) [51] [52].
- Longitudinal Monitoring: Every 3-6 months for 2-3 years, then annually [52].
Analytical Challenges and Solutions
- Clonal Hematopoiesis: Bioinformatic filtering of CHIP-associated mutations (e.g., DNMT3A, TET2, ASXL1) [51].
- Low Tumor Fraction: Utilize phased variant approaches (PhasED-Seq) or fragmentomics to enhance detection sensitivity [53].
- Spatial Heterogeneity: Combine tissue and liquid biopsy approaches where possible; the ROME trial showed only 49% concordance but improved outcomes when both were used [54].
Liquid biopsy protocols for ctDNA-based MRD monitoring represent a powerful application of NGS technologies in cancer genomics research. The integration of tumor-informed and tumor-naïve approaches, combined with ultra-sensitive detection methods and rigorous bioinformatic analysis, enables unprecedented capability to detect molecular residual disease long before clinical recurrence. As these technologies continue to evolve toward even greater sensitivity and standardization, they promise to transform cancer management through early intervention opportunities and personalized adjuvant therapy strategies. Research implementation requires careful attention to pre-analytical variables, appropriate technology selection, and robust validation—all essential for generating reliable, actionable data in both basic science and clinical translation contexts.
In the context of cancer genomics, understanding the active genetic drivers of malignancy is paramount. While DNA sequencing reveals the genetic potential of a tumor, RNA sequencing (RNA-Seq) bridges the critical "DNA to protein divide" by capturing the expressed mutational landscape [55]. It provides a functional readout of the tumor's transcriptional activity, making it indispensable for detecting key oncogenic events like gene fusions and for quantitative expression profiling of cancer-related genes. The integration of RNA-Seq into next-generation sequencing (NGS) protocols offers a more robust framework for somatic mutation detection, ultimately advancing precision medicine by ensuring clinical decisions are based on actionable, expressed genetic targets [55].
This application note details standardized protocols for leveraging RNA-Seq in cancer research, specifically for the detection of gene fusions and differential expression analysis, framed within a comprehensive NGS workflow for oncology.
Key Applications in Oncology
RNA-Seq has moved beyond a research tool and is now critical in clinical oncology for its ability to resolve complex genetic subtypes.
- Fusion Gene Detection: RNA-Seq is a powerful, unbiased method for discovering novel and known fusion genes, which are common oncogenic drivers in cancers such as leukemia and sarcoma. A 2025 study on B-cell acute lymphoblastic leukemia (B-ALL) demonstrated that RNA-Seq successfully identified fusion genes in 68% (41/60) of patients who had previously been unclassifiable using standard diagnostic methods alone [56]. This led to the reclassification of 72% (43/60) of "B-other" ALL patients into 11 distinct molecular subtypes, such as
DUX4rearranged andPAX5alt, enabling improved risk stratification [56]. - Expression Profiling for Subtyping and Biomarker Discovery: Gene expression profiling (GEP) via RNA-Seq allows for the molecular subclassification of tumors based on their transcriptional signatures. The same B-ALL study utilized GEP to assign patients to specific subtypes, including
BCR::ABL1-like, by comparing their expression data to established reference cohorts [56]. Furthermore, expression profiling is fundamental for confirming the overexpression of oncogenes or the silencing of tumor suppressors identified in DNA-seq assays, thereby validating their potential clinical relevance [55].
Experimental Protocol: A Step-by-Step Guide
Sample Preparation and Library Construction
The process begins with the extraction of high-quality RNA from tumor samples (e.g., bone marrow, frozen tissue).
- RNA Extraction and QC: Extract total RNA using a commercial kit (e.g., Zymo Research Direct-zol RNA MiniPrep). Assess RNA integrity (RIN ≥6 is recommended) and concentration using systems like Agilent TapeStation and Qubit fluorometer. Samples should have a high percentage of target cells (>60% leukaemic cells as assessed by flow cytometry) [56].
- Library Preparation: Use a stranded mRNA sequencing kit (e.g., Illumina TruSeq stranded mRNA kit) with an input of 500–700 ng of total RNA [56]. This protocol typically involves:
- mRNA Enrichment: Poly-A selection to capture mRNA.
- Fragmentation: Chemical or enzymatic fragmentation of RNA to a target size of ~300 bp.
- cDNA Synthesis: Reverse transcription of RNA into double-stranded cDNA.
- Adapter Ligation: Attachment of platform-specific sequencing adapters to the cDNA fragments.
- Library QC and Sequencing: Quantify the final library and check its quality. Sequencing is performed on a platform such as the Illumina NextSeq 550, using a 2x75 bp paired-end run to provide sufficient read length for accurate alignment and fusion detection [56].
Bioinformatics Analysis Workflow
The following workflow outlines the primary steps for data analysis, from raw sequencing reads to biological interpretation.
Detailed Methodologies for Core Applications
Fusion Gene Detection Protocol
- Alignment: Map quality-controlled reads to a reference genome (e.g., GRCh38) using a splice-aware aligner such as STAR [56].
- Fusion Calling: Utilize a multi-algorithm approach to maximize sensitivity. The Fusion InPipe algorithm or similar pipelines can be employed [56]. A conservative strategy involves:
- Initial Calling: Run multiple fusion callers (e.g., Arriba, STAR-Fusion).
- Filtering: Retain fusions identified by three or more algorithms to reduce false positives. Manually inspect fusion events involving known leukemia-associated genes that may be missed by automated filters [56].
- Visual Validation: Verify supporting reads using a genome browser (e.g., New Genome Browser).
- Experimental Validation: Confirm in-frame and other high-confidence fusions using RT-qPCR with custom-designed probes and primers [56].
Expression Profiling and Differential Expression Analysis
- Read Quantification: Calculate read counts per gene using the aligned BAM files and an annotation file (e.g., Gencode v34) with tools like HTSeq [56].
- Normalization and Batch Correction: Normalize raw counts to account for sequencing depth and library composition. Use the median-of-ratios method in DESeq2 or the TMM method in edgeR [57]. Correct for technical batch effects (from library preparation, sequencing run) using R packages like
limma[56]. - Differential Expression and Subtyping: Perform differential expression analysis between sample groups (e.g., tumor vs. normal, different subtypes) with DESeq2 [56]. For molecular subtyping, compare the sample's gene expression profile (GEP) to a well-characterized reference cohort (e.g., from St. Jude Children's Research Hospital) using dimensionality reduction techniques like t-SNE [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 1: Key research reagents, tools, and software for RNA-Seq analysis in cancer genomics.
| Category | Item/Reagent | Function/Benefit |
|---|---|---|
| Wet-Lab Reagents | TruSeq Stranded mRNA Kit (Illumina) | Library prep with strand specificity [56]. |
| Direct-zol RNA MiniPrep (Zymo Research) | High-quality total RNA extraction [56]. | |
| Agilent TapeStation D1000 ScreenTape | Assess RNA Integrity Number (RIN) [56]. | |
| Bioinformatics Tools | STAR Aligner | Splice-aware alignment for accurate RNA-Seq mapping [56]. |
| Fusion InPipe / Multiple Callers | Sensitive and specific fusion gene detection [56]. | |
| HTSeq | Generation of raw gene-level count matrices [56]. | |
| DESeq2 / edgeR | Statistical analysis for differential gene expression [57] [56]. | |
| Reference Data | GRCh38 Human Genome | Standard reference for alignment and annotation. |
| Gencode Annotations | Comprehensive gene annotation for quantification [56]. | |
| St. Jude Cloud / Public Cohorts | Reference gene expression profiles for subtyping [56]. |
Data Interpretation and Integration
Successful integration of RNA-Seq data into a cancer genomics workflow requires careful interpretation.
- Validation and Prioritization: Fusions and overexpressed genes should be prioritized based on their known oncogenic roles and functional potential (e.g., in-frame vs. out-of-frame fusions) [56]. Orthogonal validation of key findings using RT-qPCR or other methods is a critical step before clinical application [56].
- Combining DNA and RNA Evidence: Integrate RNA-Seq findings with DNA-based NGS panels. This helps distinguish between expressed, potentially actionable mutations and silent DNA variants that may not contribute to the tumor phenotype, thereby improving the strength of clinical predictions [55].
- Normalization Considerations: Be aware that no single normalization method is perfect for all comparisons. Counts per Million (CPM) and Transcripts per Million (TPM) are useful for visualization and within-sample comparisons but are not recommended for differential expression analysis between samples. For that purpose, methods like the median-of-ratios (DESeq2) and TMM (edgeR), which account for library composition, are more appropriate [57].
Table 2: Common normalization methods for RNA-Seq expression data.
| Method | Sequencing Depth Correction | Gene Length Correction | Library Composition Correction | Suitable for DE Analysis? |
|---|---|---|---|---|
| CPM | Yes | No | No | No |
| FPKM/RPKM | Yes | Yes | No | No |
| TPM | Yes | Yes | Partial | No |
| Median-of-Ratios (DESeq2) | Yes | No | Yes | Yes |
| TMM (edgeR) | Yes | No | Yes | Yes |
Next-generation sequencing (NGS) has revolutionized oncology by enabling comprehensive genomic profiling of tumors, facilitating the development of personalized cancer treatment plans [9]. The bioinformatics pipeline that transforms raw sequencing data into clinically actionable information is a critical component of this process. This pipeline encompasses a structured workflow designed to process and analyze biological data, particularly genomic and transcriptomic data, for clinical applications in cancer research and treatment [58]. In clinical oncology, these pipelines are indispensable for identifying driver mutations, detecting hereditary cancer syndromes, monitoring minimal residual disease, and guiding immunotherapy decisions [9]. The complexity and critical nature of these analyses demand robust, standardized bioinformatics practices to ensure accuracy, reproducibility, and clinical utility in molecularly driven cancer care.
Pipeline Architecture and Core Components
A clinical bioinformatics pipeline for cancer genomics consists of multiple interconnected phases that systematically process and interpret raw sequencing data. The overall workflow can be conceptualized in three primary stages: primary, secondary, and tertiary analysis [59].
Table 1: Core Components of a Clinical Bioinformatics Pipeline for Cancer Genomics
| Pipeline Stage | Key Inputs | Main Processes | Key Outputs |
|---|---|---|---|
| Primary Analysis | DNA/RNA from tumor samples (often FFPE tissue) | DNA extraction, library preparation, sequence generation, preliminary QC | Raw sequence data (BCL files) |
| Secondary Analysis | Raw sequence data (BCL/FASTQ) | Alignment to reference genome, variant calling, data QC | Aligned reads (BAM), variant calls (VCF) |
| Tertiary Analysis | Variant calls (VCF) | Annotation, filtering, prioritization, classification | Annotated variants, clinical reports |
The initial data acquisition phase involves collecting raw data from NGS platforms such as Illumina, PacBio, or Oxford Nanopore [58]. For cancer testing, this typically uses DNA extracted from formalin-fixed paraffin-embedded (FFPE) tumor specimens, with careful quality control to ensure sufficient DNA quantity (minimum 20 ng) and purity (A260/A280 ratio between 1.7-2.2) [18]. Library preparation utilizes hybrid capture methods for target enrichment, with the resulting libraries undergoing quality assessment for size (250-400 bp) and concentration before sequencing [18].
The subsequent bioinformatic processing begins with demultiplexing of raw sequencing output (conversion from BCL to FASTQ format), followed by alignment of sequencing reads to a reference genome (hg19 or hg38) to create BAM files [60] [18]. Current recommendations advocate adopting the hg38 genome build as a standard reference [60]. Variant calling then identifies multiple variant types, with the following recommended analyses for comprehensive cancer genomic profiling:
- Single nucleotide variants (SNVs) and small insertions/deletions (indels)
- Copy number variants (CNVs)
- Structural variants (SVs) including insertions, inversions, translocations
- Short tandem repeats (STRs)
- Loss of heterozygosity (LOH) regions
- Mitochondrial SNVs and indels [60]
Additional optional analyses with significant clinical utility in oncology include microsatellite instability (MSI) for identifying DNA mismatch repair defects, homologous recombination deficiency (HRD) for predicting PARP inhibitor response, and tumor mutational burden (TMB) for guiding immunotherapy decisions [60].
Figure 1: Core bioinformatics pipeline workflow showing primary, secondary, and tertiary analysis stages.
Variant Calling Methodologies
Traditional and AI-Based Variant Calling Approaches
Variant calling represents a crucial analytical step that identifies genetic alterations in tumor samples. Traditionally, this process has relied on statistical methods, but the advent of artificial intelligence (AI) has introduced a new generation of tools with improved accuracy, efficiency, and scalability [61]. Conventional statistical approaches analyze aligned sequencing reads to detect genetic variations, which are recorded in variant call format (VCF) files, followed by refinement steps to remove false positives [61]. Traditional tools mentioned in the literature include GATK's Mutect2 for detecting single nucleotide variants (SNVs) and small insertions/deletions (indels), CNVkit for identifying copy number variations, and LUMPY for detecting structural variants such as gene fusions [18].
AI-based variant calling represents a transformative advancement, leveraging machine learning (ML) and deep learning (DL) algorithms trained on large-scale genomic datasets to identify subtle patterns and reduce false-positive and false-negative rates [61]. These approaches are particularly valuable in complex genomic regions where conventional methods often struggle.
Table 2: Comparison of Variant Calling Tools and Technologies
| Tool Name | Underlying Technology | Primary Applications | Strengths | Limitations |
|---|---|---|---|---|
| DeepVariant | Deep learning (CNN) | Short-read and long-read data (PacBio HiFi, Oxford Nanopore) | High accuracy, automatically produces filtered variants | High computational cost |
| DeepTrio | Deep learning (CNN) | Family trio analysis | Enhanced accuracy in challenging regions, improved de novo mutation detection | Designed specifically for trio analysis |
| DNAscope | Machine learning | Short-read and long-read data | Computational efficiency, high SNP and InDel accuracy | Does not leverage deep learning architectures |
| Clair/Clair3 | Deep learning (CNN) | Short-read and long-read data | Better performance at lower coverages, fast runtime | Earlier versions inaccurate for multi-allelic variants |
| GATK | Statistical methods | Germline and somatic variant discovery | Well-established, widely validated | Rule-based approach may miss complex variants |
| SAMtools | Statistical methods | Variant calling from aligned reads | Lightweight, fast processing | Less accurate for complex variant types |
Experimental Protocol: Variant Calling Implementation
For researchers implementing variant calling in cancer genomics, the following detailed protocol provides a robust framework:
Sample Quality Control and Sequencing
- Extract genomic DNA from FFPE tumor tissue using a QIAamp DNA FFPE Tissue kit or equivalent [18].
- Assess DNA concentration using Qubit dsDNA HS Assay kit and purity using NanoDrop Spectrophotometer (target A260/A280 ratio: 1.7-2.2) [18].
- Perform library preparation using hybrid capture method (e.g., Agilent SureSelectXT Target Enrichment System) with at least 20 ng input DNA [18].
- Sequence libraries on appropriate NGS platform (e.g., Illumina NextSeq 550Dx) with target mean coverage >500x for tumor samples [18].
Bioinformatic Processing
- Convert raw BCL files to FASTQ format using appropriate demultiplexing tools (e.g., Illumina bcl2fastq).
- Perform quality control on FASTQ files using FastQC to assess base quality scores, adapter contamination, and GC content.
- Align reads to reference genome (hg19 or hg38) using aligners such as BWA-MEM or STAR.
- Process BAM files to mark duplicates, perform base quality score recalibration, and conduct post-alignment QC.
Variant Calling Implementation
- For SNVs and indels, use Mutect2 with minimum variant allele frequency (VAF) threshold of 2% [18].
- For copy number variations, apply CNVkit with average copy number ≥5 considered as amplification [18].
- For structural variants and fusions, implement LUMPY with read counts ≥3 interpreted as positive results [18].
- Consider supplementing traditional callers with AI-based tools like DeepVariant or DNAscope for improved accuracy, particularly in challenging genomic regions [61].
Validation and Quality Metrics
- Validate pipeline performance using standard truth sets such as GIAB for germline variants and SEQC2 for somatic variant calling [60].
- Supplement with recall testing of real human samples previously tested using validated methods [60].
- Verify sample identity through fingerprinting and genetically inferred identification markers such as sex and relatedness [60].
- Ensure data integrity using file hashing throughout the pipeline [60].
Variant Annotation and Functional Prediction
Annotation Frameworks and Databases
Variant annotation constitutes the initial phase of tertiary analysis, where genomic variants are enriched with biological and clinical context to enable prioritization and interpretation [59]. This process involves appending variants with information about their predicted gene-level impact according to standardized nomenclature and contextual information utilized in subsequent analysis steps [59]. A key recommendation for clinical production is the implementation of automated quality assurance that is handled partially or fully within the analysis pipeline [60].
The annotation process typically employs multiple bioinformatics tools and databases to comprehensively characterize variants:
- Functional Impact Prediction: Tools like SnpEff and VEP (Variant Effect Predictor) annotate variants with their predicted functional consequences on genes and proteins, including categories such as missense, nonsense, frameshift, and splice-site variants [58].
- Population Frequency Databases: Annotation with population allele frequencies from databases such as gnomAD helps filter common polymorphisms unlikely to contribute to disease.
- Cancer-Specific Databases: Integration with cancer genomics resources like COSMIC (Catalogue of Somatic Mutations in Cancer) provides information on recurrence of mutations in cancer cohorts.
- Clinical Significance Databases: Annotation with clinical interpretations from ClinVar and OncoKB helps identify clinically actionable variants.
- Functional Domain Annotation: Tools like InterProScan and hmmscan identify functional protein domains and motifs affected by variants [62].
For clinical cancer genomics, the Association for Molecular Pathology (AMP) variant classification system provides a standardized framework for categorizing variants based on their clinical significance [18]. This system includes:
- Tier I: Variants of strong clinical significance (FDA-approved drugs, professional guidelines)
- Tier II: Variants of potential clinical significance (investigational therapies)
- Tier III: Variants of unknown clinical significance
- Tier IV: Benign or likely benign variants [18]
Experimental Protocol: Automated Annotation Pipeline
Implementation of Annotation Workflow
- Install and configure annotation tools such as ANNOVAR, SnpEff, or VEP, ensuring access to required database versions [58].
- For comprehensive functional annotation, implement InterProScan to identify protein domains, gene ontology terms, and pathway information [62].
- For hypothetical proteins or variants of unknown significance, perform additional analysis using hmmscan and RPS-BLAST to identify distant homologs and functional domains [62].
- Incorporate cancer-specific annotations from dedicated resources such as CIViC, OncoKB, and COSMIC to identify therapeutic implications.
Customization for Cancer Genomics
- Configure filtering parameters to prioritize oncogenic variants based on AMP/ASCO/CAP guidelines [18] [59].
- Implement tumor-specific annotation including mutation signatures, mutational burden calculation, and microsatellite instability status [18].
- For TMB calculation, establish criteria counting eligible missense mutations while excluding variants with population frequency >1% in East Asian or gnomAD databases, pathogenic/likely pathogenic mutations in ClinVar, variants with allele frequency <2%, and variants below depth 200 [18].
- For MSI detection, utilize tools such as mSINGs or similar algorithms optimized for NGS data [18].
Validation and Quality Assurance
- Establish standardized protocols for annotation consistency across different samples and batches [60].
- Implement version control for all databases and software tools to ensure reproducibility [60].
- Conduct regular updates of annotation databases to incorporate the latest clinical and functional evidence [58].
Figure 2: Variant annotation and prioritization workflow showing key steps from functional annotation to clinical reporting.
Clinical Interpretation and Reporting
Interpretation Framework and Clinical Integration
The final stage of the bioinformatics pipeline involves interpreting prioritized variants in the context of the specific cancer type and patient clinical picture to generate actionable reports. This process requires integrating evidence from multiple sources to determine clinical actionability and appropriate therapeutic strategies [59]. A real-world study of NGS implementation in a tertiary hospital demonstrated that among patients with Tier I variants (strong clinical significance), 13.7% received NGS-based therapy, with the highest rates in thyroid cancer (28.6%), skin cancer (25.0%), gynecologic cancer (10.8%), and lung cancer (10.7%) [18]. Of patients with measurable lesions who received NGS-based therapy, 37.5% achieved partial response and 34.4% achieved stable disease, demonstrating the clinical utility of comprehensive genomic profiling [18].
Critical considerations for clinical interpretation include:
- Phenotype Integration: Detailed phenotype information is essential for accurate variant interpretation. This can be captured through clinic notes, structured forms, or automated extraction from electronic medical records using natural language processing (NLP) algorithms [59].
- Actionability Assessment: Variants must be evaluated for therapeutic implications based on levels of evidence, including FDA-approved drugs, clinical trial eligibility, and preclinical evidence.
- Germline-Somatic Differentiation: Determining whether a potentially pathogenic variant is of germline or somatic origin has significant implications for treatment and genetic counseling.
- Reporting Standards: Clinical reports should clearly communicate variant classification, evidence supporting the interpretation, and therapeutic recommendations in a format accessible to oncologists.
Experimental Protocol: Clinical Interpretation and Reporting
Pre-Analytical Considerations
- Develop detailed test requisition forms that capture essential clinical information, including cancer type, stage, prior treatments, and family history [59].
- Establish clear policies for secondary and incidental findings, including which genes will be analyzed and reported beyond the primary indication [59].
- Implement informed consent processes that address the scope of analysis, potential findings, and data usage [59].
Interpretation Process
- Initiate interpretation with review of clinical context and primary phenotypes to guide analysis [59].
- Apply variant classification guidelines (AMP/ASCO/CAP) to categorize variants based on clinical significance [18] [59].
- Assess therapeutic actionability using structured frameworks that consider levels of evidence from professional guidelines, clinical trials, and preclinical studies.
- Differentiate between somatic driver alterations, passenger mutations, and potentially germline variants requiring additional confirmation.
Report Generation and Communication
- Structure clinical reports to include patient and specimen information, test methods, genomic findings, clinical interpretation, and therapeutic implications.
- Use clear language to describe variant significance, associated evidence, and treatment recommendations.
- For actionable findings, provide specific drug recommendations, clinical trial options, and additional testing considerations (e.g., germline confirmation).
- Implement multidisciplinary review for complex cases or unexpected findings to ensure comprehensive interpretation.
Post-Reporting Considerations
- Establish processes for result communication and integration into patient management decisions.
- Implement systems for results reanalysis as new evidence emerges, particularly for variants of uncertain significance [59].
- Maintain documentation of interpretation rationale and evidence sources for quality assurance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Computational Tools for Cancer Genomics Pipelines
| Category | Specific Tools/Reagents | Function/Purpose |
|---|---|---|
| Sample Preparation | QIAamp DNA FFPE Tissue Kit (Qiagen) | DNA extraction from archival tumor samples [18] |
| Agilent SureSelectXT Target Enrichment System | Library preparation and target capture [18] | |
| Sequencing Platforms | Illumina NextSeq 550Dx | High-throughput sequencing for pan-cancer panels [18] |
| Illumina NovaSeq X | Ultra-high-throughput for large-scale projects [21] | |
| Oxford Nanopore Technologies | Long-read sequencing for complex genomic regions [21] | |
| Variant Calling Tools | GATK (Mutect2) | SNV and indel detection [18] |
| DeepVariant | AI-based variant calling with high accuracy [61] [21] | |
| CNVkit | Copy number variant detection [18] | |
| LUMPY | Structural variant and fusion detection [18] | |
| Annotation Resources | SnpEff/VEP | Functional consequence prediction [18] [58] |
| InterProScan | Protein domain and functional site identification [62] | |
| ClinVar | Clinical variant interpretations [58] | |
| COSMIC | Catalog of somatic mutations in cancer [58] | |
| Workflow Management | Nextflow/Snakemake | Pipeline orchestration and reproducibility [58] |
| Docker/Singularity | Containerization for software environment consistency [60] | |
| Visualization Tools | IGV (Integrative Genomics Viewer) | Visual exploration of genomic data [58] |
Emerging Trends and Future Directions
The field of clinical bioinformatics is rapidly evolving, with several emerging technologies poised to enhance cancer genomic analysis. Artificial intelligence and machine learning are being increasingly integrated into pipelines for predictive analytics and pattern recognition, with tools like DeepVariant demonstrating superior accuracy in variant calling [61] [21] [58]. The integration of multi-omics approaches—combining genomics with transcriptomics, proteomics, metabolomics, and epigenomics—provides a more comprehensive view of biological systems and tumor biology [21]. Single-cell sequencing and spatial transcriptomics are advancing resolution to individual cells within tissues, revealing tumor heterogeneity and microenvironment interactions [9] [21]. Cloud computing platforms have become essential for scalable data storage and analysis, enabling global collaboration while maintaining security compliance with regulations such as HIPAA and GDPR [21]. Long-read sequencing technologies from PacBio and Oxford Nanopore are improving the detection of complex structural variants and epigenetic modifications [21]. These advancements are collectively driving the field toward more automated, real-time, and personalized bioinformatics pipelines that will further enhance precision oncology approaches [58].
Troubleshooting NGS Workflows: Overcoming Technical and Analytical Challenges
Next-generation sequencing (NGS) has revolutionized cancer genomics, yet the quality of sequencing data is profoundly influenced by the quality of the starting sample. Formalin-fixed paraffin-embedded (FFPE) tissues and low-input samples present significant challenges due to nucleic acid degradation and limited quantity. This application note details optimized protocols to overcome these hurdles, ensuring reliable data for research and drug development.
Sample Quality Assessment and Pre-Analytical Variables
Assessing RNA Integrity in FFPE Samples
The RNA Integrity Number (RIN) is not considered appropriate for FFPE samples due to widespread rRNA degradation. Instead, the DV200 index (the percentage of RNA fragments longer than 200 nucleotides) is a reliable predictor of successful library construction [63]. FFPE samples can be categorized as follows [64]:
- High-quality: DV200 > 70%
- Medium-quality: DV200 50% - 70%
- Low-quality: DV200 30% - 50%
- Heavily degraded (often excluded): DV200 < 30%
One study on oral squamous cell carcinoma (OSCC) FFPE samples stored for 1-2 years reported average DV200 values within the 30%-50% range, yet successfully generated sequencing data with optimized protocols [64].
Optimizing Pre-Analytical Conditions for FFPE Tissues
RNA integrity in FFPE specimens is heavily influenced by pre-analytical factors. A 2024 study established optimal preparation conditions to maximize RNA quality [63]:
- Ischemia Time: Tissue ischemia should be kept at 4°C for < 48 hours or at 25°C for a short time (0.5 hours).
- Fixation Time: 48-hour fixation at 25°C is recommended. Prolonged fixation (e.g., 72 hours) contributes to RNA fragmentation.
- Sampling Method: Sampling from FFPE scrolls is preferable to sections. The outermost layer of paraffin exposed to air should be cut away before collecting 5 μm thick scrolls for RNA extraction [63].
Table 1: Impact of FFPE Sample Storage Time on RNA Yield and Quality
| Storage Duration | Number of Samples | Average RNA Concentration | DV200 Index | Sufficient for Library Prep? |
|---|---|---|---|---|
| 1 year | 13 | > 130 ng/μL | 30% - 50% | Yes [64] |
| 2 years | 7 | > 130 ng/μL | 30% - 50% | Yes [64] |
Optimized Nucleic Acid Extraction and Library Construction
RNA Extraction from FFPE Tissues
For FFPE tissues, using six 8 μm thick slices from a remounted paraffin block provides sufficient RNA yield without compromising quality [64]. The study found no significant difference in RNA quantity or quality when comparing four versus six slices, or when using remounted versus non-remounted blocks. The extraction process involves deparaffinization, lysis with proteinase K, and RNA purification. The extracted RNA should be stored at -80°C until library preparation [64].
Library Preparation Method Comparison for FFPE RNA-Seq
The choice of library preparation method is critical for successfully sequencing degraded RNA from FFPE samples. A comparative study of two common methods on OSCC FFPE samples with low-quality RNA (DV200 30-50%) yielded clear results [64]:
- Exome Capture Method: This two-stage method first prepares a cDNA library, then performs target enrichment via hybridization. It used 100 ng of input RNA and significantly outperformed rRNA depletion in final library output concentration (p < 0.001) and the amount of usable sequencing data generated.
- rRNA Depletion Method: This method removes ribosomal RNAs from the total RNA before library preparation. It required a higher 750 ng of input RNA and proved less effective for low-quality FFPE samples.
Table 2: Comparison of RNA Library Prep Methods for Low-Quality FFPE Samples
| Method | Input RNA | Procedure | Performance for Low-Quality FFPE RNA |
|---|---|---|---|
| Exome Capture | 100 ng | 1. cDNA library prep2. Target enrichment by hybridization | Superior library output and sequencing data [64] |
| rRNA Depletion | 750 ng | Removal of rRNA followed by library prep | Inferior to exome capture for this sample type [64] |
Library Preparation for Low-Input and Degraded DNA
For samples with very low DNA quantity or high degradation (e.g., from FFPE blocks, ancient DNA, or ChIP assays), specialized kits are required. These kits employ unique chemistries to handle single-stranded DNA (ssDNA) and low-input double-stranded DNA (dsDNA), which are common in damaged samples.
- xGen ssDNA & Low-Input DNA Library Prep Kit: This kit uses Adaptase technology to simultaneously perform tailing and ligation in a template-independent manner, generating libraries from inputs as low as 10 picograms and from fragments ≥40 bp. It is compatible with both ssDNA and dsDNA, preserving input fragmentation patterns for precise mapping [65].
- NGS Low Input DNA Library Prep Kit: This kit is designed for DNA inputs from 1 ng to 400 ng and features a fast 1.5-hour protocol. Its unique chemistry for DNA end-polishing and ligation results in even coverage and low GC bias. A key advantage is the requirement for fewer magnetic beads during cleanup steps, reducing costs by over 50% [66].
The workflow for handling single-stranded and degraded DNA, as exemplified by the xGen kit, can be summarized as follows:
Technical Solutions and Reagent Selection
Specialized reagent kits are fundamental for managing the complexities of FFPE and low-input samples. The table below lists key solutions and their applications.
Table 3: Research Reagent Solutions for FFPE and Low-Input NGS
| Product Name | Sample Type | Input Range | Key Technology / Advantage | Compatible Platform |
|---|---|---|---|---|
| xGen ssDNA & Low-Input DNA Library Prep Kit [65] | Degraded DNA, ssDNA, dsDNA mixtures | 10 pg - 250 ng | Adaptase technology for ssDNA/dsDNA; minimal sequence bias | Illumina |
| NGS Low Input DNA Library Prep Kit [66] | Low input DNA | 1 ng - 400 ng | 1.5-hour protocol; low bead usage for cost savings | Illumina, MGI |
| PureLink FFPE RNA Isolation Kit [64] | FFPE Tissue | 4-6 slices (8 µm) | Optimized for deparaffinization and lysis | N/A (Extraction) |
| NEBNext Ultra II Directional RNA Library Prep Kit [64] | Total RNA (including FFPE) | 5 ng - 1 µg (rRNA depletion) | dUTP method for strand specificity | Illumina |
| xGen NGS Hybridization Capture Kit [64] | cDNA libraries | Varies | Target enrichment for exome capture | Illumina |
| Tecan NGS Library Prep Reagents [67] | DNA/RNA, broad types | From 10 pg | Optimized for automated workflows on Tecan systems | Illumina |
Protocol Implementation and Automation
Automation of NGS library preparation significantly enhances reproducibility and throughput for FFPE and low-input protocols. Platforms like the Tecan DreamPrep NGS can process up to 96 DNA libraries in a single run in less than 4 hours, minimizing hands-on time and the risk of human error [67]. These automated systems are often open platforms, verified to work with various commercial library prep kits from manufacturers like Illumina and New England Biolabs, providing flexibility for different research applications and sample types [67].
The decision-making process for optimizing an NGS workflow for challenging samples involves several key steps, from initial quality control to final data output:
Obtaining robust NGS data from FFPE and low-input samples is achievable through meticulous attention to pre-analytical variables, rigorous quality control, and the selection of specialized extraction and library preparation protocols. Key to success is the use of the DV200 metric for RNA quality assessment, the application of exome capture for degraded RNA, and the implementation of innovative technologies like Adaptase for low-input and damaged DNA. By integrating these optimized wet-lab protocols with automated platforms, researchers can reliably unlock the vast potential of these challenging yet invaluable sample types in cancer genomics research.
Tumor heterogeneity represents a fundamental challenge in modern cancer research and therapy. It refers to the existence of distinct cellular subpopulations (subclones) within a single tumor, each possessing unique genetic and phenotypic characteristics [68]. This diversity arises through a process of clonal evolution, driven by genetic instability, selective pressures from the microenvironment, and therapeutic interventions [68] [69]. The presence of multiple subclones directly impacts clinical outcomes by fostering therapy resistance, enabling immune evasion, and promoting metastatic progression [68] [69].
Next-generation sequencing (NGS) technologies have revolutionized our ability to dissect this complexity by providing high-resolution genomic data. However, the accurate detection and characterization of subclones requires sophisticated computational approaches that can distinguish meaningful biological signals from technical artifacts and interpret the complex mixture of cells within tumor samples [70] [69]. This application note explores cutting-edge computational methods for subclone detection, their integration with experimental protocols, and their critical role in advancing precision oncology.
Key Computational Methods for Subclone Detection
Advanced computational methods have been developed to reconstruct tumor subclonal architecture using various data types, from bulk to single-cell and spatial omics. The table below summarizes the features of two prominent approaches, Clonalscope and Tumoroscope.
Table 1: Comparison of Computational Methods for Subclone Detection
| Method | Primary Data Input | Core Algorithm | Subclone Features Detected | Spatial Resolution |
|---|---|---|---|---|
| Clonalscope [71] | Copy number alterations from scRNA-seq, scATAC-seq, Spatial Transcriptomics | Nested Chinese Restaurant Process | Genetically distinct subclones with differential CNV profiles | Yes, on spatial transcriptomics spots |
| Tumoroscope [72] | Somatic point mutations from bulk DNA-seq, Spatial Transcriptomics, H&E images | Probabilistic graphical model | Clones with distinct point mutation profiles, spatially localized | Yes, near single-cell resolution |
Technical Principles and Applications
Clonalscope implements a Nested Chinese Restaurant Process to identify tumor subclones de novo based on DNA copy number alteration (CNA) profiles derived from single-cell or spatial omics data [71]. This Bayesian non-parametric approach efficiently clusters cells into subpopulations with distinct CNA patterns without requiring pre-specification of the number of clusters. A significant advantage is its ability to incorporate prior information from matched bulk DNA sequencing data, which enhances subclone detection accuracy and improves the labeling of malignant cells [71]. Applied to single-cell RNA sequencing and single-cell ATAC sequencing data from gastrointestinal tumors, Clonalscope has successfully identified genetically distinct subclones and validated their association with differential differentiation levels, drug resistance, and survival-associated gene expression [71].
In contrast, Tumoroscope addresses the critical challenge of deconvoluting clone proportions within spatial transcriptomics spots using a probabilistic framework that integrates pathological images, whole exome sequencing, and spatial transcriptomics data [72]. Its core innovation lies in mathematically modeling each spatial transcriptomics spot as a mixture of clones previously reconstructed from bulk DNA sequencing, then estimating clone proportions per spot using mutation coverage (alternative and total read counts) and prior cell count information from H&E images [72]. This approach has revealed spatially segregated subclones with distinct phenotypes in prostate and breast cancers, identifying patterns of clone colocalization and mutual exclusion while inferring clone-specific gene expression profiles [72].
Experimental Protocols for Subclone Detection
Integrated Workflow for Spatial Subclone Detection
The following diagram illustrates the comprehensive experimental workflow for subclone detection integrating multiple data types, as implemented in methods like Tumoroscope:
Protocol Steps and Data Integration
Step 1: Tissue Processing and Multi-Modal Data Generation Begin with collecting fresh tumor tissue samples from resection or biopsy. Split the sample into three portions: (1) fix one portion in formalin and embed in paraffin (FFPE) for H&E staining and histopathological assessment; (2) snap-freeze another portion for bulk DNA extraction; (3) preserve the final portion in optimal cutting temperature (OCT) compound for spatial transcriptomics using platforms like 10x Genomics Visium [72]. For H&E-stained sections, use digital pathology tools (e.g., QuPath) to annotate cancer cell-containing regions and estimate cell counts within each spatial transcriptomics spot, providing crucial priors for computational deconvolution [72].
Step 2: Bulk DNA Sequencing and Clone Reconstruction Extract high-quality DNA from frozen tumor tissue using validated kits (e.g., DNeasy Blood & Tissue Kit). Prepare whole-exome or whole-genome sequencing libraries following manufacturer protocols (e.g., Illumina DNA Prep) and sequence on appropriate platforms (e.g., NextSeq 2000) to achieve minimum 80-100x coverage [73] [72]. Process raw sequencing data through a standardized bioinformatics pipeline: perform somatic variant calling using tools like Vardict [72], infer allele-specific copy number alterations with FalconX [72], and reconstruct clone genotypes and phylogenetic trees using methods such as Canopy [72]. The output is a genotype matrix of somatic mutations across identified clones.
Step 3: Spatial Transcriptomics and Data Integration Generate spatial transcriptomics data from OCT-embedded tissue sections according to platform-specific protocols (e.g., 10x Genomics Visium). After standard gene expression quantification, extract mutation coverage information by counting alternative and total reads for each somatic mutation identified in bulk DNA sequencing at each spatial spot [72]. This step is technically challenging as spatial transcriptomics primarily captures mRNA, but sufficient DNA-based mutation signals can be obtained from nascent pre-mRNA.
Step 4: Computational Deconvolution and Spatial Mapping Integrate all processed data inputs—cell counts per spot (from H&E), clone genotypes and frequencies (from bulk DNA-seq), and mutation coverage (from spatial transcriptomics)—into the probabilistic deconvolution model (Tumoroscope) or copy-number-based method (Clonalscope) [71] [72]. Execute the computational framework using appropriate parameters to estimate the proportion of each clone in every spatial spot. Validate results through cross-validation and comparison with independent single-cell datasets where available.
Essential Research Reagents and Tools
Successful implementation of subclone detection workflows requires specialized reagents and computational tools. The following table catalogizes key solutions for generating and analyzing subclone data.
Table 2: Research Reagent Solutions for Subclone Detection Studies
| Category | Product/Resource | Primary Function | Application Context |
|---|---|---|---|
| Sequencing Kits | Illumina DNA Prep | Library preparation for whole-genome sequencing | Bulk DNA sequencing for clone reconstruction [73] |
| Spatial Omics | 10x Genomics Visium | Spatial gene expression profiling | Mapping transcriptomes in tissue context [72] |
| Digital Pathology | QuPath | Image analysis for cell quantification | Estimating cell counts in H&E images [72] |
| Variant Caller | Vardict | Somatic mutation detection | Identifying point mutations from bulk DNA-seq [72] |
| CNV Analysis | FalconX | Allele-specific copy number estimation | Inferring copy number alterations from bulk DNA-seq [72] |
| Clone Reconstruction | Canopy | Clonal tree reconstruction | Building phylogenetic models from bulk sequencing [72] |
Analytical Framework and Data Interpretation
Clone Deconvolution Principles
The core computational challenge in subclone detection involves accurately estimating the proportion of each clone in mixed samples. Tumoroscope addresses this through a Binomial probability model that predicts the expected ratio of alternative to total reads for each mutation in every spot, based on clone genotypes and their proportions [72]. This approach maintains robustness against gene expression fluctuations by focusing on read count ratios rather than absolute expression values.
Performance validation demonstrates that deconvolution accuracy strongly correlates with sequencing depth. Studies show that increasing the average spot coverage from 18 (very low) to 110 (high) reads significantly reduces the Mean Average Error (MAE) in clone proportion estimation from approximately 0.15 to 0.02 [72]. This relationship underscores the importance of sufficient sequencing depth for reliable subclone detection. The method also exhibits robustness to noise in input cell counts, particularly when cell numbers are treated as priors rather than fixed values, enabling adaptation to imperfect histological estimates [72].
Spatial Heterogeneity Analysis
Beyond mere proportion estimation, computational approaches enable comprehensive spatial heterogeneity analysis. Clonalscope implements algorithms to identify spatially segregated subclones with distinct differentiation levels and differential expression of clinically relevant genes associated with drug resistance and survival [71]. Similarly, Tumoroscope reconstructs detailed spatial distribution maps that reveal patterns of clone colocalization and mutual exclusion within tumor tissues [72].
These spatial patterns provide critical insights into clonal dynamics and evolutionary relationships. For example, the discovery of subclones localized to specific microenvironments suggests adaptive specialization, while mutually exclusive distributions may indicate competitive interactions between subpopulations [72] [68]. Such findings have profound clinical implications, as spatially restricted therapy-resistant subclones might escape detection in single-region biopsies but drive eventual treatment failure.
Computational approaches for subclone detection represent essential tools in the era of precision oncology. Methods like Clonalscope and Tumoroscope demonstrate how integrated analysis of multi-modal data—combining bulk sequencing, single-cell technologies, spatial omics, and digital pathology—can resolve the complex spatial and genomic architecture of tumors with unprecedented resolution [71] [72]. As these technologies mature, they are poised to transform clinical practice by enabling identification of resistant subclones before treatment failure, guiding combination therapies that target multiple subpopulations simultaneously, and uncovering novel therapeutic targets within the tumor evolutionary landscape.
The ongoing integration of artificial intelligence and machine learning with multi-omics data will further refine subclone detection capabilities [74] [68]. Additionally, the development of standardized analytical frameworks and benchmarking datasets will be crucial for clinical translation. As NGS technologies continue to advance and computational methods become more sophisticated, the comprehensive characterization of tumor heterogeneity will increasingly guide therapeutic decisions, ultimately improving outcomes for cancer patients.
The reliable detection of low-frequency variants is a critical challenge in cancer genomics, with implications for understanding tumor heterogeneity, monitoring minimal residual disease (MRD), and guiding targeted therapy decisions [75] [76]. Next-generation sequencing (NGS) enables comprehensive mutation profiling, but its utility is often limited by error rates that obscure true low-abundance mutations [75]. In oncology research, distinguishing bona fide somatic mutations from sequencing artifacts is particularly difficult when variant allele frequencies (VAFs) drop below 1% [77] [76]. This application note details integrated experimental and bioinformatic techniques to enhance sensitivity for rare mutation detection in cancer genomic studies, enabling reliable variant calling at frequencies as low as 0.0015% under optimized conditions [76].
Technical Approaches for Enhanced Sensitivity
Template Preparation and Library Construction
The initial stages of NGS workflow introduce significant artifacts that impact variant detection sensitivity. Template preparation methods must be optimized to minimize errors while preserving authentic low-frequency variants [75].
DNA Repair for Challenging Samples: Formalin-fixed, paraffin-embedded (FFPE) tissue specimens, while invaluable for cancer research, contain damaged DNA that increases false positive variant calls. Enzymatic repair mixes specifically designed for FFPE-derived DNA can significantly improve data quality. Studies demonstrate that FFPE DNA repair increases mean target coverage by 20-50% across samples with varying damage levels (mild, moderate, and severe) and maintains coverage exceeding 500x with only 50 ng of input DNA [77]. This repair process facilitates reliable detection of variants with VAFs as low as 3% even in severely compromised samples [77].
PCR Enzyme Selection: The choice of DNA polymerase profoundly impacts error rates during amplification. Proofreading enzymes significantly reduce PCR-induced transitions (particularly G>A and C>T errors), which constitute the majority of substitution errors in NGS data [76]. This optimization is crucial for detecting low-level single nucleotide variants (SNVs), as the prevalent transition versus transversion bias (3.57:1) directly affects site-specific detection limits [76].
Hybridization-Based Enrichment: For FFPE and other fragmented DNA samples, hybridization-based target enrichment outperforms amplicon-based approaches due to better tolerance for DNA fragmentation, greater uniformity of coverage, fewer false positives, and superior variant detection resulting from reduced PCR cycles [77].
Advanced Sequencing Methodologies
Single-Cell DNA-RNA Sequencing: Single-cell DNA-RNA sequencing (SDR-seq) enables simultaneous profiling of up to 480 genomic DNA loci and genes in thousands of single cells, allowing accurate determination of variant zygosity alongside associated gene expression changes [78]. This approach confidently links precise genotypes to transcriptional phenotypes at single-cell resolution, revealing subpopulations of cells with elevated mutational burdens and distinct expression profiles in B-cell lymphoma [78]. Fixation conditions significantly impact data quality, with glyoxal providing superior RNA target detection and UMI coverage compared to paraformaldehyde [78].
Targeted RNA-Seq for Expressed Variant Detection: Targeted RNA sequencing complements DNA-based mutation detection by confirming which variants are functionally expressed [55]. This approach bridges the "DNA to protein divide" in precision oncology, prioritizing clinically relevant mutations. When analyzing targeted RNA-seq data, stringent false positive rate control is essential, achieved through parameters such as VAF ≥2%, total read depth ≥20, and alternative allele depth ≥2 [55]. This methodology uniquely identifies pathologically relevant variants missed by DNA-seq alone [55].
Read Length Optimization: The choice of sequencing read length represents a trade-off between cost, throughput, and detection performance. For viral pathogen detection, 75 bp reads demonstrate 99% sensitivity median, increasing to 100% with 150-300 bp reads [79]. Bacterial pathogen detection benefits more substantially from longer reads, with sensitivity medians of 87% (75 bp), 95% (150 bp), and 97% (300 bp) [79]. In outbreak scenarios requiring rapid response, 75 bp reads represent a cost-effective option for viral detection, enabling more samples to be sequenced with streamlined workflows [79].
Table 1: Comparison of Sensitivity Enhancement Techniques
| Technique | Mechanism | Optimal Application | Achievable Sensitivity | Key Limitations |
|---|---|---|---|---|
| FFPE DNA Repair | Enzyme mix repairs deamination, nicks, gaps, oxidized bases | Archival tissue samples, fragmented DNA | VAF ~3% in severely damaged samples [77] | Cannot restore completely degraded sequences |
| Proofreading PCR Enzymes | Reduces polymerase incorporation errors | Low-input samples, MRD detection | VAF ~0.0015% for JAK2 mutations [76] | Higher cost, potential bias for specific sequences |
| Hybridization Capture | Superior fragmented DNA tolerance, reduced PCR cycles | FFPE samples, copy number analysis | >99.6% variant concordance across damage levels [77] | More complex workflow, longer hands-on time |
| Single-Cell DNA-RNA Seq | Links genotype to phenotype in individual cells | Tumor heterogeneity, clonal evolution | Detection of rare subpopulations in primary lymphoma [78] | High cost, specialized equipment required |
| Targeted RNA-Seq | Confirms expressed variants | Therapy selection, neoantigen verification | Identifies clinically actionable expressed mutations [55] | Limited to expressed genes, tissue-specific expression |
Bioinformatic Enhancements
Bioinformatic processing significantly impacts low-frequency variant detection through rigorous error correction and filtering strategies.
Unique Molecular Identifiers (UMIs): Incorporating UMIs during library preparation enables bioinformatic correction of PCR and sequencing errors [80]. Each original molecule receives a unique barcode before amplification, allowing duplicate reads originating from the same molecule to be identified and collapsed into a consensus sequence. This process distinguishes true biological variants from amplification artifacts, dramatically improving detection confidence for low-frequency variants [80].
Read Trimming and Quality Control: Stringent read trimming and quality filtering are essential preprocessing steps. Adapter sequences and low-quality bases must be removed using tools such as Trimmomatic, Cutadapt, or BBDuk [81]. A minimum read length of 50-75 base pairs is recommended, with reads below Phred quality score of 20 (Q20) typically removed [79] [81]. FastQC provides comprehensive quality assessment both before and after trimming [81] [80].
Variant Calling Parameters: Specialized variant calling pipelines for low-frequency mutations require adjusted parameters. For research applications detecting very low VAFs (0.01-0.0015%), parameters must be optimized to balance sensitivity and specificity [76]. Multi-caller approaches combining VarDict, Mutect2, and LoFreq, followed by ensemble filtering, improve detection reliability [55].
Experimental Protocols
Protocol: FFPE DNA Repair and Hybridization-Based Library Preparation
This protocol enables reliable mutation detection from challenging FFPE-derived DNA samples [77].
Materials:
- SureSeq FFPE DNA Repair Mix (OGT)
- SureSeq NGS Library Preparation Kit
- Covaris S220 focused-ultrasonicator
- Agilent TapeStation for DNA quality assessment
- Custom hybridization panel (e.g., 8.7 kb cancer hot-spot panel)
Procedure:
- DNA Quality Assessment: Determine DNA Integrity Number (DIN) using Agilent TapeStation. Typical DIN values: mild damage (6.6), moderate damage (3.2), severe damage (1.9) [77].
- DNA Shearing: Fragment 10-200 ng DNA using Covaris S220 to achieve 150-800 bp fragments.
- DNA Repair: Treat sheared DNA with FFPE Repair Mix according to manufacturer's instructions.
- Library Preparation: Prepare sequencing library using SureSeq NGS Library Preparation Kit with repaired DNA.
- Library Quantification: Assess pre-capture library yields; repaired samples should show increased peak height at ~200 bp compared to untreated controls.
- Target Enrichment: Perform hybridization capture using custom panel (16-24 hours).
- Sequencing: Sequence on Illumina MiSeq using v2 300 cycles kit.
Quality Control Metrics:
- Pre-capture library yield increase after repair
- Mean target coverage >1000x at 100 ng input, >500x at 50 ng input [77]
- Uniformity of coverage across targeted regions
Protocol: Single-Cell DNA-RNA Sequencing (SDR-seq)
This protocol enables simultaneous DNA and RNA variant detection at single-cell resolution [78].
Materials:
- Mission Bio Tapestri platform
- Custom poly(dT) primers with UMIs and sample barcodes
- Glyoxal fixative
- Proteinase K
- Barcoding beads with cell barcode oligonucleotides
Procedure:
- Cell Preparation: Dissociate tissue into single-cell suspension.
- Fixation: Fix cells with glyoxal (superior to PFA for RNA detection).
- In Situ Reverse Transcription: Perform RT with custom poly(dT) primers adding UMIs, sample barcodes, and capture sequences.
- Droplet Generation: Load cells onto Tapestri platform for first droplet generation.
- Cell Lysis: Lyse cells within droplets and treat with Proteinase K.
- Target Amplification: Mix with reverse primers for gDNA/RNA targets during second droplet generation with barcoding beads.
- Multiplexed PCR: Amplify both gDNA and RNA targets within droplets.
- Library Preparation: Generate separate NGS libraries for gDNA (full-length) and RNA (transcript + barcode information).
Quality Control Metrics:
- >95% of reads per cell mapping to correct sample barcode [78]
- >80% gDNA target detection in >80% of cells [78]
- Minimal cross-contamination (<0.16% gDNA, 0.8-1.6% RNA) [78]
Table 2: Performance Metrics of Enhanced NGS Methods
| Method | Input Requirements | Coverage Depth | VAF Detection Limit | Variant Concordance |
|---|---|---|---|---|
| Standard NGS | 50-100 ng high-quality DNA | ~500x | ~1-5% | Varies with error rate [75] |
| FFPE-Optimized with Repair | 10-200 ng FFPE DNA | >1000x (100 ng), >500x (50 ng) [77] | ~3% | 99.6% across damage levels [77] |
| UMI-Mediated Sequencing | Varies with application | Varies | 0.1-1% | Improved by error correction [80] |
| Ultra-Sensitive NGS (Optimized) | Varies | >10,000x | 0.0015% (JAK2) [76] | Validated by ddPCR [76] |
| Single-Cell DNA-RNA Seq | Thousands of single cells | Per-cell coverage | Zygosity determination [78] | Links genotype to phenotype [78] |
Workflow Visualization
Integrated DNA-RNA Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Sensitive Mutation Detection
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| DNA Repair Kits | SureSeq FFPE DNA Repair Mix (OGT) | Repairs deamination, nicks, gaps, oxidized bases in FFPE DNA [77] |
| NGS Library Prep | SureSeq NGS Library Preparation Kit | Construction of sequencing libraries from low-input/damaged samples [77] |
| Hybridization Panels | Agilent Clear-seq, Roche Comprehensive Cancer Panels | Target enrichment; longer probes (120 bp) vs. shorter probes (70-100 bp) impact coverage [55] |
| Single-Cell Platforms | Mission Bio Tapestri | Simultaneous DNA+RNA profiling at single-cell level [78] |
| Polymerases | Proofreading enzymes | Reduces PCR-induced errors; critical for low-VAF detection [76] |
| Targeted RNA Panels | Afirma Xpression Atlas (593 genes) | Detects expressed mutations; bridges DNA-to-protein divide [55] |
| Quality Control | Agilent TapeStation, FastQC | Assesses DNA quality (DIN), sequencing data quality [77] [81] |
| UMI Adapters | Various commercial systems | Molecular barcoding for error correction [80] |
Enhanced sensitivity for low-frequency variant detection requires integrated optimization across sample preparation, sequencing methodology, and bioinformatic analysis. Key strategies include enzymatic DNA repair for compromised samples, proofreading polymerases to reduce amplification errors, UMIs for bioinformatic error correction, single-cell approaches to resolve heterogeneity, and combined DNA-RNA sequencing to distinguish expressed mutations. Through implementation of these techniques, researchers can reliably detect rare variants down to 0.0015% VAF, enabling advanced applications in cancer genomics including MRD monitoring, therapy resistance detection, and comprehensive tumor heterogeneity characterization [78] [77] [76].
Next-generation sequencing (NGS) has revolutionized cancer genomics research, enabling comprehensive molecular profiling of tumors to guide precision oncology. The integration of NGS into clinical practice represents a paradigm shift from traditional single-gene testing to massively parallel genomic analysis, facilitating the identification of actionable mutations, biomarkers, and therapeutic targets [9]. However, the implementation of NGS in research and clinical settings presents substantial bioinformatics challenges related to the management and interpretation of vast genomic datasets. The convergence of massive data volumes, complex computational requirements, and the need for standardized analytical frameworks constitutes a critical bottleneck in realizing the full potential of NGS for cancer research and drug development [82] [83]. This application note addresses these interconnected challenges within the context of establishing robust NGS protocols for cancer genomics, providing actionable frameworks for researchers and scientists engaged in oncogenomics and therapeutic development.
Core Bioinformatics Challenges in NGS
Data Storage and Management
The massive data volumes generated by NGS platforms present unprecedented storage and management challenges for cancer genomics initiatives. Table 1 quantifies the typical data output from contemporary NGS platforms used in cancer research.
Table 1: Data Output Metrics of Common NGS Platforms in Cancer Genomics
| Platform/Sequencing Type | Typical Data Output per Run | Common Applications in Cancer Research |
|---|---|---|
| Illumina NextSeq 2000 | ~360 GB (High-output flow cell) | Whole exome sequencing, large gene panels, transcriptomics [73] |
| Illumina MiSeq | ~15 GB (V3 chemistry) | Targeted gene panels, validation sequencing [73] |
| Whole Genome Sequencing (WGS) | ~90-100 GB per sample | Comprehensive genomic profiling, structural variant discovery [9] |
| Whole Exome Sequencing (WES) | ~5-7 GB per sample | Coding variant discovery, tumor-normal paired analysis [9] |
| Targeted Gene Panel (500 genes) | ~1-3 GB per sample | High-depth somatic variant detection, clinical profiling [18] |
Effective data management extends beyond storage capacity to encompass data security, accessibility, and sharing compliance. The National Institutes of Health (NIH) mandates stringent data security controls for genomic data managed in trusted partner environments like the Genomic Data Commons (GDC) and dbGaP. Researchers accessing controlled genomic data must comply with NIST 800-171 cybersecurity requirements, which encompass 18 control families including access control, audit accountability, system integrity, and media protection [84]. Implementation often requires secure research enclaves (SREs) with associated infrastructure costs, presenting both technical and budgetary considerations for research organizations [84].
Computational Resource Requirements
NGS data analysis demands substantial computational infrastructure, typically involving high-performance computing (HPC) clusters or cloud computing environments. The bioinformatics workflow for cancer genomics—from raw sequence data to variant calling—requires specialized computational resources:
- Processing Power: Multi-core processors for parallelized task execution during sequence alignment and variant calling.
- Memory (RAM): High-memory nodes (≥ 64 GB RAM) for processing large reference genomes and handling complex alignment algorithms.
- Persistent Storage: Scalable storage systems capable of handling terabytes to petabytes of data with high input/output performance [83].
Cloud-based solutions like the Cancer Genomics Cloud (CGC) resources provide alternative computational infrastructure, offering scalable analysis environments with access to large reference datasets like The Cancer Genome Atlas (TCGA) [85] [86]. These platforms provide over 800 bioinformatic tools and workflows, enabling researchers without local HPC resources to perform sophisticated genomic analyses [85].
Pipeline Standardization and Validation
The complexity of NGS bioinformatics pipelines introduces significant challenges for standardization, validation, and reproducibility in cancer research. The Association for Molecular Pathology (AMP) and the College of American Pathologists (CAP) have jointly recommended guidelines for bioinformatics pipeline validation to ensure analytical accuracy and clinical reliability [87]. Key standardization challenges include:
- Variant Calling Consistency: Different algorithms may yield discordant results for complex variants such as insertions-deletions (indels) and structural variants [83].
- Pipeline Upgrades and Version Control: Systematic management of pipeline versions and components using frameworks like git and mercurial is essential for reproducibility [83].
- Quality Control Metrics: Implementation of predetermined quality control checkpoints across the entire workflow, from initial sample evaluation to final variant reporting [82].
Laboratory accreditation requirements from CAP include 18 specific checklist items for NGS processes, covering documentation, validation, quality assurance, confirmatory testing, variant interpretation, and data storage [82]. Adherence to these standards is particularly crucial for clinical applications of cancer genomic data.
Experimental Protocols for NGS Bioinformatics
Protocol: Validation of NGS Bioinformatics Pipelines
This protocol outlines the key steps for validating bioinformatics pipelines for cancer NGS data analysis, based on joint recommendations from AMP and CAP [87].
1. Pre-Validation Requirements
- Define the intended use of the NGS assay and variant types to be detected (SNVs, indels, CNVs, fusions).
- Document all pipeline components, including software versions, reference genomes, and database builds.
- Establish validation samples with known variants, using cell lines or previously characterized patient specimens.
2. Determination of Performance Characteristics
- Accuracy: Compare variant calls from the pipeline to a validated orthogonal method or reference material. Recommended minimum of 50 samples with various variant types [82].
- Precision: Assess repeatability (same conditions) and reproducibility (changed conditions) using a minimum of three positive samples for each variant type.
- Analytical Sensitivity/Specificity: Calculate positive and negative agreement compared to a gold standard method, considering depth of coverage and read quality [82].
- Variant Calling Evaluation: Specifically assess performance for phased variants and complex haplotypes, which are challenging for many algorithms [83].
3. Validation Execution and Documentation
- Execute the pipeline on the validation samples using locked parameters and settings.
- Document all command-line parameters and software configurations.
- Establish an exception log to track and address pipeline errors or unexpected behaviors.
- Implement semantic versioning for the pipeline and all components [83].
4. Post-Validation Monitoring
- Establish ongoing quality control metrics for routine monitoring of pipeline performance.
- Implement procedures for controlled pipeline upgrades with appropriate revalidation.
- Maintain comprehensive documentation for traceability and accreditation requirements.
Protocol: Implementation of NGS Quality Management System
Quality management is essential for generating reliable and reproducible cancer genomic data. This protocol outlines a framework for implementing a comprehensive quality management system for NGS workflows [82].
1. Quality Documentation System
- Develop Standard Operating Procedures (SOPs) for all NGS workflow steps.
- Implement Technical Notes (TN) as quality records for each sample, documenting critical parameters and potential deviations.
- Establish a Quality Management System (QMS) with a three-tier hierarchy: policies, SOPs, and records.
2. Quality Control Checkpoints
- Sample Preparation: Assess DNA/RNA quality (e.g., Qubit quantification, NanoDrop purity, RNA Integrity Number).
- Library Construction: Evaluate library size and concentration (e.g., Bioanalyzer profile).
- Sequencing: Monitor quality metrics (e.g., Q-scores, cluster density, error rates).
- Data Analysis: Implement QC thresholds (e.g., minimum coverage, uniformity, mapping rates).
3. Proficiency Testing and Continuous Improvement
- Participate in external proficiency testing programs when available.
- Perform regular internal competency assessments using reference materials.
- Implement a failure mode and effects analysis (FMEA) to identify and address potential workflow failures.
Workflow Visualization
NGS Workflow with Quality Gates
Bioinformatics Pipeline Architecture
The Scientist's Toolkit
Table 2: Essential Bioinformatics Tools for Cancer NGS Analysis
| Tool/Resource Name | Type | Primary Function in Cancer NGS |
|---|---|---|
| GATK (Genome Analysis Toolkit) | Variant Discovery | Somatic variant calling, base quality score recalibration [82] |
| Mutect2 | Variant Caller | Detection of somatic SNVs and small indels [18] |
| CNVkit | Copy Number Analysis | Identification of copy number variations from targeted sequencing [18] |
| LUMPY | Structural Variant Caller | Detection of gene fusions and large structural variants [18] |
| cBioPortal | Data Analysis Portal | Interactive exploration of cancer genomics datasets [88] |
| COSMIC | Database | Comprehensive resource of somatic mutations in cancer [88] |
| UCSC Xena | Data Analysis Platform | Multi-omic and clinical/phenotype data visualization [88] |
| SnpEff | Variant Annotation | Functional annotation of genetic variants [18] |
Table 3: Key Online Resources for Pan-Cancer Analysis
| Resource | Data Content | Application in Cancer Research |
|---|---|---|
| TCGA (The Cancer Genome Atlas) | Multi-omics data for 33 cancer types | Reference dataset for cancer genomic alterations [88] |
| ICGC (International Cancer Genome Consortium) | Genomic data from 50+ tumor types | International collaboration for pan-cancer analysis [88] |
| CPTAC (Clinical Proteomic Tumor Analysis Consortium) | Proteogenomic data for 10+ cancers | Integration of proteomic and genomic data [88] |
| Genomic Data Commons (GDC) | NCI's genomic data repository | Unified data sharing and analysis platform [86] |
| Cancer Genomics Cloud (CGC) | Cloud-based analysis platform | Secure computational environment with 800+ tools [85] |
The integration of robust bioinformatics solutions is paramount for harnessing the full potential of NGS in cancer genomics research. Addressing the interconnected challenges of data storage, computational resources, and pipeline standardization requires systematic approaches to quality management, validation, and infrastructure planning. The implementation of standardized protocols, comprehensive quality control checkpoints, and validated bioinformatics pipelines ensures the generation of reliable, reproducible genomic data essential for both research and clinical applications.
Emerging methodologies such as single-cell sequencing and liquid biopsies promise to further enhance the precision of cancer diagnostics and treatment monitoring, while simultaneously intensifying bioinformatics challenges related to data complexity and volume [9]. Future developments in computational genomics will likely focus on enhanced cloud-based solutions, artificial intelligence-driven variant interpretation, and more sophisticated integrative analysis of multi-omics data. The continued collaboration between researchers, bioinformaticians, and clinicians remains essential for advancing NGS applications in oncology and ultimately improving patient outcomes through precision cancer medicine.
In the field of cancer genomics research, next-generation sequencing (NGS) has emerged as a pivotal technology, transforming the approach to cancer diagnosis and treatment by enabling detailed genomic profiling of tumors [9]. The technology's ability to identify genetic alterations that drive cancer progression facilitates the development of personalized treatment plans, significantly improving patient outcomes [9]. However, the implementation of NGS in research settings presents a fundamental challenge: the need to balance data quality, governed by parameters of sequencing depth and coverage, against inevitable budget constraints. This application note provides a structured framework for researchers and drug development professionals to optimize this balance, ensuring maximal scientific return on investment in cancer genomics studies.
Defining Core Metrics: Depth and Coverage
A critical first step in designing a cost-effective NGS experiment is to understand the distinct meanings of sequencing depth and coverage, terms often used interchangeably but that provide different insights into data quality [89].
- Sequencing Depth: Also known as read depth, this refers to the number of times a specific nucleotide in the genome is read during the sequencing process [89]. It is expressed as an average multiple (e.g., 100x) and is a key determinant of variant-calling accuracy. Higher depth is particularly crucial for detecting subclonal populations in heterogeneous tumor samples [89].
- Sequencing Coverage: This metric describes the proportion of the target genome (whole genome, exome, or a targeted panel) that has been sequenced at least once [89]. It is typically expressed as a percentage (e.g., 95% coverage) and indicates the completeness of the data. Gaps in coverage can lead to missed variants, which is especially problematic in cancer gene panels where missing a driver mutation could alter clinical interpretation [89].
The relationship between these two parameters is foundational to experimental design. In theory, increasing sequencing depth can also improve coverage, as more reads increase the likelihood of covering all genomic regions. However, due to technical biases in library preparation or sequencing, certain regions (e.g., those with high GC content or repetitive elements) may remain underrepresented regardless of depth [89]. A well-designed NGS project must therefore aim for a balance: sufficient depth to detect variants confidently and comprehensive coverage to ensure the entire target region is represented.
The Fundamental Trade-off: Data Quality vs. Resource Allocation
The core trade-off in NGS experimental design, under a fixed budget, lies between the number of samples sequenced (sample size, N) and the amount of sequencing performed per sample (depth of coverage, λ). Deeper sequencing per sample provides more confident variant calls but is more expensive, thereby reducing the number of samples that can be included in the study under a fixed budget. Conversely, sequencing more samples at a lower depth increases the statistical power for population-level analyses but reduces the power to detect variants within each individual sample [90].
Theoretical and empirical studies have demonstrated that the power to detect rare variant associations does not increase monotonically with sample size when the total sequencing resource (e.g., total gigabases sequenced) is fixed. Instead, power follows a sawtooth pattern, with a maximum achieved at a medium depth of coverage where the power to call heterozygous variants, R(λ), is suboptimal but not minimal [90]. This counterintuitive finding highlights that maximizing data quality per sample is not always the optimal strategy for study power. The optimal depth is the point where the cost of a further increase in depth, in terms of samples excluded from the study, outweighs the benefit in improved variant-calling accuracy.
Table 1: Key Definitions for NGS Cost-Benefit Optimization
| Term | Definition | Impact on Data Quality | Relationship to Cost |
|---|---|---|---|
| Sequencing Depth (Read Depth) | The number of times a specific nucleotide is read during sequencing [89]. | Higher depth increases confidence in variant calls and enables detection of low-frequency variants [89]. | Directly proportional; higher depth requires more sequencing reads, increasing cost per sample. |
| Sequencing Coverage | The percentage of the target genomic region sequenced at least once [89]. | Higher coverage ensures comprehensive assessment of the region of interest and prevents missed variants. | Influenced by depth and library quality; achieving high coverage in difficult regions can be costly. |
| Variant Calling Power | The probability of correctly identifying a true genetic variant. | A function of sequencing depth, especially for heterogeneous samples like tumors [89]. | A primary benefit of increased spending on depth. |
| Total Bases Sequenced | The total gigabases (Gb) of sequence data generated for a study. | The fundamental unit of sequencing resource that is partitioned between samples and depth [90]. | Directly determines the total cost of the sequencing effort. |
Quantitative Framework for Optimization
Cost and Power Modeling
To operationalize the trade-off between sample size and sequencing depth, a model must be established that links budget constraints to statistical power. The first step is to define the cost structure. Two primary cost regimes are prevalent:
- Cost Proportional to Total Bases: In this model, relevant for whole-genome sequencing, the total cost is directly proportional to the total amount of base pairs sequenced across all samples (T). Here, the average depth (λ) is determined by the number of samples (N) and the total resource: λ = T / N [90].
- Fixed Cost Per Sample: This model, more common in exome or targeted sequencing, approximates the cost as a fixed amount per sample, largely independent of depth within a certain range. The budget then directly determines the total number of samples that can be sequenced [90].
For the first regime, the key is to find the sample size N that maximizes power, given that increasing N reduces the depth λ = T / N per sample. The power to detect a carrier of a rare variant is a function of depth, R(λ), which typically follows a sigmoid curve, increasing sharply from a minimum depth threshold before plateauing [90]. The statistical power for a case-control association study using a collapsing method (for rare variants) can be calculated based on the binomial distribution of observed carriers, with probability p ≈ F₁R(λ) in cases, where F₁ is the compound carrier frequency of causal variants [90]. Online tools like OPERA are available to perform these calculations under flexible assumptions [90].
Recommended Depth and Coverage for Cancer Genomics Applications
The optimal depth and coverage are not universal but are dictated by the specific research application and the type of variants of interest. The following table provides benchmark values for common applications in cancer genomics, synthesized from current literature and practices.
Table 2: Recommended Sequencing Parameters for Cancer Genomics Applications
| Application | Recommended Depth | Recommended Coverage | Rationale and Technical Notes |
|---|---|---|---|
| Whole Genome Sequencing (WGS) - Germline | 30x - 50x | > 95% | Balances cost and ability to detect most single nucleotide variants (SNVs) and small indels across the genome [91]. |
| Whole Exome Sequencing (WES) | 100x - 150x | > 98% | Higher depth is required to confidently call variants in the protein-coding exome, which constitutes ~1-2% of the genome. |
| Tumor Somatic Variant Detection | 100x (Normal) & 200x+ (Tumor) | > 98% | High depth in the tumor sample is critical for detecting low-frequency somatic mutations present in a subclonal population [9]. |
| Liquid Biopsy (ctDNA) | 5,000x - 30,000x | > 99% | Ultra-deep sequencing is mandatory to detect and quantify extremely low levels of circulating tumor DNA (ctDNA) against a background of wild-type DNA [92]. |
| RNA-Seq (Transcriptomics) | 20-50 million reads/sample | N/A | Adequate for differential expression analysis. Deeper sequencing (50-100M reads) may be needed for isoform discovery or lowly expressed genes. |
Protocol for Determining Optimal Design Given a Fixed Budget
This protocol provides a step-by-step methodology for determining the optimal number of samples and sequencing depth.
Step 1: Define Study Objectives and Variant Types Clearly outline the primary goal. Are you identifying common germline polymorphisms, rare germline variants, or low-frequency somatic mutations? This will define the required depth per sample [89]. For instance, detecting a somatic variant present in 10% of tumor cells requires significantly higher depth than calling a germline heterozygous variant.
Step 2: Establish the Total Sequencing Budget and Cost Model Determine the total financial resource available. Then, work with your sequencing provider or core facility to establish the cost model: is it primarily based on total Gb sequenced (WGS) or a per-sample fee (exome/targeted)?
Step 3: Calculate the Power vs. Sample Size Curve Using a power calculator like OPERA or custom scripts, model the statistical power for a range of sample sizes (N) [90]. For a fixed total budget (T), this will automatically determine the depth (λ = T / N) and the corresponding variant-calling sensitivity R(λ) for each N.
Step 4: Identify the Optimal Point on the Curve The optimal design is the sample size N (and its corresponding depth λ) that provides the highest statistical power for your primary objective from Step 1. As per theoretical findings, this often corresponds to a medium depth of coverage, not the maximum possible depth [90].
Step 5: Incorporate Contingency and Practical Considerations Allocate a portion of the budget (e.g., 5-10%) for contingency to handle unexpected issues such as sample failure, need for repeat sequencing, or discovery of interesting findings that require validation [93]. Factor in sample quality, as low-quality DNA/RNA may require higher depth to achieve confident calls.
Experimental Protocols and Workflows
Comprehensive Workflow for Cost-Optimized NGS in Cancer Research
The following diagram illustrates the end-to-end workflow, from sample preparation to data analysis, highlighting key decision points for cost-benefit optimization.
Diagram 1: An integrated workflow for cost-effective NGS in cancer genomics, highlighting the critical strategic planning phase.
Protocol for Tumor-Normal Pair Sequencing with Optimal Pseudo-Depth
This protocol is designed for robust somatic variant discovery while making efficient use of sequencing resources.
Objective: To identify somatic mutations in a tumor sample by sequencing a matched normal sample from the same patient to filter out germline variants.
Materials and Reagents:
- Tumor Tissue: FFPE blocks or fresh frozen tissue.
- Matched Normal Tissue: Blood, saliva, or adjacent healthy tissue.
- DNA Extraction Kit: e.g., QIAamp DNA FFPE Tissue Kit or equivalent.
- NGS Library Prep Kit: e.g., Illumina DNA Prep or KAPA HyperPrep Kit.
- Target Enrichment Kit (if applicable): e.g., IDT xGen Pan-Cancer Panel, Illumina TruSight Oncology 500.
- Sequencing Platform: e.g., Illumina NovaSeq X, Illumina NextSeq 550.
Procedure:
- Nucleic Acid Extraction: Extract high-quality DNA from both tumor and normal samples. Quantify using fluorometry (e.g., Qubit) and assess quality/fragment size (e.g., Bioanalyzer/TapeStation). Note: For FFPE samples, assess DNA degradation and factor this into depth requirements.
- Library Preparation: Prepare sequencing libraries according to the manufacturer's protocol. This typically involves DNA fragmentation, end-repair, A-tailing, and adapter ligation. Use dual-indexing adapters to enable multiplexing of multiple samples in a single sequencing run, which is a key cost-saving strategy [92].
- Target Enrichment (for Panel Sequencing): For targeted panels, perform hybrid capture-based enrichment using biotinylated probes complementary to the target regions. This step pulls down the sequences of interest, allowing for deeper sequencing of relevant genes without the cost of whole-genome sequencing.
- Library QC and Pooling: Quantify the final libraries using qPCR for accurate molarity. Pool libraries at equimolar concentrations for multiplexed sequencing.
- Sequencing: Load the pooled library onto the sequencer. Sequence the normal sample to a minimum of 100x and the tumor sample to a minimum of 200x (for tissue) or much higher for liquid biopsies (cf. Table 2). The higher depth in the tumor is necessary to achieve power to detect subclonal mutations.
Bioinformatic Analysis:
- Alignment: Align sequencing reads to a reference genome (e.g., GRCh38) using tools like BWA-MEM or STAR.
- Variant Calling: Use specialized callers for somatic variants. For example:
- Mutect2 (from GATK) for SNVs and small indels.
- ASCAT or Sequenza for copy number alterations.
- Manta or Delly for structural variants.
- Annotation and Filtering: Annotate variants using databases like dbSNP, gnomAD, COSMIC, and ClinVar. Filter against the matched normal to remove germline polymorphisms.
The Scientist's Toolkit: Essential Research Reagent Solutions
The selection of reagents and kits is critical for the success and reproducibility of NGS experiments. The following table details key solutions used in modern cancer genomics workflows.
Table 3: Key Research Reagent Solutions for NGS in Cancer Genomics
| Product Category/Example | Primary Function | Application Context |
|---|---|---|
| QIAGEN QIAseq Hyb Panels [91] | Hybrid capture-based target enrichment using a single-tube reaction. | Targeted sequencing for oncology; allows deep sequencing of cancer-associated genes from low-input DNA, including FFPE. |
| Illumina DNA Prep [92] | Library preparation for whole-genome and whole-exome sequencing. | A flexible, high-throughput library prep method for generating sequencing-ready libraries from genomic DNA. |
| IDT for Illumina DNA/RNA UD Indexes | Provides unique dual indexes for sample multiplexing. | Allows massive multiplexing of samples on Illumina sequencers, dramatically reducing per-sample sequencing costs [92]. |
| PacBio HiFi Reads | Long-read, high-fidelity sequencing. | Ideal for resolving complex genomic regions, detecting structural variants, and phasing mutations in cancer genomes, complementing short-read data. |
| Oxford Nanopore Ligation Sequencing Kits | Long-read, real-time sequencing. | Enables direct detection of base modifications (epigenetics) and sequencing of very long DNA fragments, useful for complex rearrangement analysis. |
| Bio-Rad SEQuoia RiboDepletion Kit | Removal of ribosomal RNA (rRNA) from RNA samples. | Critical for RNA-Seq workflows to enrich for mRNA and other non-ribosomal RNAs, improving the efficiency of transcriptome sequencing. |
Optimizing the balance between sequencing depth, coverage, and budget is not a one-size-fits-all calculation but a deliberate, strategic process fundamental to the success of cancer genomics research. As this application note outlines, the most cost-effective design often involves a medium depth of coverage that maximizes statistical power for a fixed budget, rather than simply pursuing the highest possible data quality per sample [90]. By rigorously defining study objectives, understanding the distinct roles of depth and coverage [89], leveraging quantitative power models, and implementing the detailed protocols and workflows provided, researchers can design robust and financially sustainable NGS studies. This disciplined approach ensures that precious resources are allocated to generate the most scientifically impactful data, accelerating progress in personalized oncology and drug development.
Next-generation sequencing (NGS) has revolutionized cancer genomics, enabling comprehensive molecular profiling of tumors. However, the analytical sensitivity of these methods makes them susceptible to technical artifacts that can compromise data integrity and lead to erroneous biological conclusions. Two of the most significant challenges are false positives (erroneous variant calls) and batch effects (technical variations introduced during experimental processing) [94] [95]. In cancer genomics, where detecting low-frequency variants is critical for understanding tumor heterogeneity and evolution, these artifacts can have profound consequences, potentially leading to incorrect therapeutic assignments or flawed cancer predisposition findings [96] [97].
Batch effects are notoriously common technical variations unrelated to study objectives that can be introduced due to variations in experimental conditions over time, using data from different labs or machines, or employing different analysis pipelines [94] [95]. These effects are observed across all omics data types, including genomics, transcriptomics, proteomics, and metabolomics. The fundamental cause can be partially attributed to the basic assumptions of data representation in omics data, where the relationship between instrument readout and true analyte concentration may fluctuate across different experimental conditions [94] [95]. The profound negative impact of these artifacts is exemplified by a clinical trial study where a change in RNA-extraction solution introduced batch effects that resulted in incorrect classification outcomes for 162 patients, 28 of whom received incorrect or unnecessary chemotherapy regimens [94] [95].
Origins and Impact of Batch Effects
The occurrence of batch effects can be traced back to diverse origins and can emerge at every step of a high-throughput study. Understanding these sources is crucial for developing effective mitigation strategies. Some sources are common across numerous omics types, while others are exclusive to particular fields [94] [95].
Table: Major Sources of Batch Effects in NGS Workflows
| Stage | Source | Impact on Data |
|---|---|---|
| Study Design | Flawed or confounded design; Minor treatment effect size | Systematic differences between batches; Difficulty distinguishing signals from noise [94] [95] |
| Sample Preparation | Protocol procedures; Sample storage conditions | Significant changes in mRNA, proteins, and metabolites [94] [95] |
| Library Preparation | Different technicians; Enzyme efficiency; Reagent lots | Variation in library complexity and coverage uniformity [98] |
| Sequencing | Different instruments; Flow cell variation; Index misassignment | Platform-specific systematic errors; Sample cross-contamination [99] [98] |
| Data Analysis | Different variant callers; Bioinformatics pipelines | Inconsistent variant identification; Variable sensitivity/specificity [96] |
In transcriptomics, batch effects can stem from multiple sources including sample preparation variability, sequencing platform differences, library prep artifacts, reagent batch effects, and environmental conditions [98]. For single-cell RNA-seq, additional challenges include higher technical variations, lower RNA input, higher dropout rates, and a higher proportion of zero counts compared to bulk RNA-seq [94] [95]. In metabolomics and proteomics, batch correction typically relies on QC samples and internal standards spiked into every run, whereas transcriptomics correction depends more on statistical modeling due to the lack of physical standards [98].
False Positives and Index Misassignment
False positives in NGS data can arise from multiple sources, with index misassignment (also called index hopping) representing a particularly challenging problem in amplicon sequencing studies [99]. This phenomenon occurs when sequences are assigned to the wrong sample during multiplexed sequencing and can be disastrous for clinical diagnoses depending heavily on scarce mutations and/or rare microbes [99].
The rate of index misassignment varies significantly between sequencing platforms. Comparative studies using mock microbial communities have demonstrated that the DNBSEQ-G400 platform shows a significantly lower fraction (0.08%) of potential false positive reads compared to the NovaSeq 6000 platform (5.68%) [99]. This differential rate has substantial consequences for diversity analyses, as unexpected operational taxonomic units (OTUs) were almost two orders of magnitude higher for the NovaSeq platform, significantly inflating alpha diversity estimates for simple microbial communities and underestimating complexity in diverse communities [99].
A critical challenge is that routine quality control processes and standard bioinformatic algorithms cannot remove these false positives because they are high-quality reads, not sequencing errors [99]. This limitation underscores the importance of preventive experimental design and appropriate platform selection, especially when studying rare variants or low-abundance taxa.
Experimental Design Strategies for Artifact Prevention
Strategic Study Design and Sample Processing
The most effective approach to managing technical artifacts is to prevent them through careful experimental design. This proactive strategy is more reliable than attempting to correct artifacts computationally after data generation [98]. Several key principles should guide experimental planning:
Randomization and Balancing: Biological groups and experimental conditions should be randomized across processing batches to avoid confounding technical and biological variation. Never process all samples of one condition together; instead, ensure each batch contains representatives from all experimental groups [98]. This balanced distribution allows statistical methods to separate biological signals from technical noise more effectively.
Replication Strategies: Include at least two replicates per group per batch to enable more robust statistical modeling of batch effects [98]. Technical replicates across batches are particularly valuable for assessing variability and validating correction methods. For large-scale studies, incorporate reference samples or control materials in each batch to monitor technical variation.
Standardization and Controls: Use consistent reagents, protocols, and personnel throughout the study whenever possible. When reagent changes are unavoidable, document lot numbers carefully and plan for bridging experiments to quantify the impact [98]. Implement multiple types of controls, including positive controls with known variants, negative controls without template, and blank controls to identify contamination sources [99].
For NGS-based cancer testing, pre-analytical sample assessment is crucial. Solid tumor samples require microscopic review by a certified pathologist to ensure sufficient non-necrotic tumor content and accurate tumor cell fraction estimation, which is critical for interpreting mutant allele frequencies and copy number alterations [97]. Macrodissection or microdissection may be necessary to enrich tumor fraction and increase sensitivity for detecting somatic variants.
Platform Selection and Library Preparation
The choice of sequencing platform and library preparation method significantly influences the susceptibility to technical artifacts:
Platform Considerations: For studies focusing on rare variants or low-abundance biological signals, select platforms with demonstrated low index misassignment rates [99]. When combining data from multiple platforms, include overlapping samples to quantify and correct for platform-specific biases.
Library Preparation Methods: Two major approaches are used for targeted NGS—hybrid capture-based and amplification-based methods [97]. Hybrid capture methods use longer probes that can tolerate several mismatches without interfering with hybridization, circumventing issues of allele dropout that can occur in amplification-based assays [97]. However, amplification-based methods may be more efficient for low-input samples. The choice depends on the specific application, target regions, and sample types.
Unique Dual Indexing: Employ unique dual indexing strategies to minimize the impact of index hopping. This approach allows definitive identification of misassigned reads, as both indexes must incorrectly match for misassignment to occur undetected.
Computational Correction Methods
Batch Effect Correction Algorithms
When batch effects cannot be prevented through experimental design, computational correction methods are essential. Multiple batch effect correction algorithms (BECAs) have been developed, each with distinct strengths and limitations:
Table: Comparison of Batch Effect Correction Algorithms
| Method | Primary Application | Strengths | Limitations |
|---|---|---|---|
| ComBat | Bulk RNA-seq, Microarrays | Adjusts known batch effects using empirical Bayes; widely used and simple [100] [98] | Requires known batch info; may not handle nonlinear effects [98] |
| limma removeBatchEffect | Bulk RNA-seq | Efficient linear modeling; integrates with differential expression workflows [100] [98] | Assumes known, additive batch effect; less flexible [98] |
| SVA | Bulk RNA-seq | Captures hidden batch effects; suitable when batch labels are unknown [98] | Risk of removing biological signal; requires careful modeling [98] |
| Harmony | scRNA-seq, Multi-omics | Fast and scalable; preserves biological variation while correcting batches [101] [102] | Limited native visualization tools [102] |
| Seurat Integration | scRNA-seq | High biological fidelity; comprehensive workflow with clustering and DE tools [102] | Computationally intensive for large datasets [102] |
| BBKNN | scRNA-seq | Computationally efficient; integrates seamlessly with Scanpy [102] | Less effective for non-linear batch effects [102] |
The performance of these methods varies depending on the data type and specific context. For radiogenomic data from FDG PET/CT images of lung cancer patients, both ComBat and Limma methods provided effective correction of batch effects, revealing more significant associations between texture features and TP53 mutations than phantom-corrected data [100]. In proteomics, recent evidence suggests that protein-level batch effect correction is more robust than correction at the precursor or peptide level, with the MaxLFQ-Ratio combination showing superior prediction performance in large-scale plasma samples from type 2 diabetes patients [101].
Validation of Correction Quality
Assessing the success of batch effect correction is crucial to avoid overcorrection that might remove biological signal or undercorrection that leaves technical artifacts. Multiple validation strategies should be employed:
Visual Assessment: Dimensionality reduction techniques such as PCA (Principal Component Analysis) and UMAP (Uniform Manifold Approximation and Projection) provide visual assessment of batch effect correction [100] [98]. Before correction, samples often cluster by batch rather than biological condition; successful correction should result in grouping by biological identity.
Quantitative Metrics: Several statistical metrics have been developed to quantitatively assess batch correction quality:
- kBET (k-nearest neighbor Batch Effect Test): Statistical test that assesses whether the proportion of cells from different batches in a local neighborhood deviates from the expected proportion [100] [102].
- LISI (Local Inverse Simpson's Index): Quantifies both batch mixing (Batch LISI) and cell type separation (Cell Type LISI) [102].
- ASW (Average Silhouette Width): Measures clustering tightness and separation [98].
- ARI (Adjusted Rand Index): Measures similarity between two data clusterings [98].
These metrics provide complementary information about different aspects of correction quality and should be used in combination for comprehensive validation.
Detailed Experimental Protocols
Protocol for Validating NGS Panel Performance
For clinical NGS testing in oncology, rigorous validation is essential to establish assay performance characteristics. The following protocol is adapted from joint consensus recommendations from the Association of Molecular Pathology and College of American Pathologists [97]:
Pre-validation Phase (Familiarization and Optimization)
- Panel Content Selection: Define intended use, including sample types (primary tumors, residual disease monitoring) and diagnostic information to be evaluated.
- Reference Materials: Acquire well-characterized reference cell lines and DNA samples with known variants across different variant types (SNVs, indels, CNAs, fusions).
- Pilot Testing: Conduct preliminary runs to optimize library preparation, sequencing conditions, and bioinformatics parameters.
- Error Assessment: Identify potential sources of errors throughout the analytical process and address through test design.
Validation Phase
- Sample Selection: Use a minimum of 20-30 samples with known variants for each variant type (SNVs, indels, CNAs, fusions).
- Performance Establishment:
- Determine positive percentage agreement and positive predictive value for each variant type.
- Establish limit of detection for different variant types using dilution series.
- Verify minimal depth of coverage requirements (typically >250x for somatic variants).
- Assess reproducibility through inter-run and intra-run replicates.
- Bioinformatics Validation: Validate all components of the analysis pipeline, including alignment, variant calling, filtering, and annotation.
- Quality Control Metrics: Establish thresholds for quality metrics including coverage uniformity, base quality, duplication rates, and contamination checks.
Ongoing Quality Monitoring
- Control Materials: Include reference control materials in each sequencing run to monitor assay performance over time.
- Key Performance Indicators: Track metrics such as sequencing output, coverage uniformity, and variant calling consistency.
- Re-validation: Re-validate the assay when making significant changes to any component of the testing process.
Protocol for Assessing Index Misassignment Rates
To evaluate and monitor index misassignment in amplicon sequencing studies, implement the following protocol [99]:
Control Design:
- Prepare customized mock communities with known composition.
- Include biological replicates of the same mock community in the same sequencing run.
Sequencing:
- Sequence the same mock community samples on different platforms for comparison.
- Use unique dual indexes for all samples.
Analysis:
- Process sequencing data through standard bioinformatics pipeline (quality filtering, OTU clustering/denoising).
- Identify unexpected taxa/OTUs not present in the known mock community composition.
- Calculate the rate of unexpected OTUs as a percentage of total reads.
Interpretation:
- Compare rates between platforms and between runs.
- Establish acceptable thresholds based on study requirements for rare variant detection.
- Implement platform-specific strategies to minimize impacts (e.g., increased replication for platforms with higher misassignment rates).
Integrated Workflow for Addressing Technical Artifacts in NGS Studies
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Research Reagent Solutions for Artifact Mitigation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Reference Cell Lines | Well-characterized controls with known variants for validation | Essential for establishing assay performance; should cover variant types of interest [97] |
| Universal Reference Materials | Multi-omics reference materials for cross-batch normalization | Enables ratio-based correction methods; particularly valuable in proteomics [101] |
| Unique Dual Indexes | Molecular barcodes for sample multiplexing | Minimizes index hopping; allows detection of misassigned reads [99] |
| Mock Communities | Synthetic communities with known composition | Critical for assessing false positive rates and index misassignment [99] |
| QC Samples | Quality control samples for monitoring technical variation | Should be included in every batch; enables drift correction [101] |
| Hybrid Capture Probes | Target-enrichment reagents for NGS | Longer probes tolerate mismatches better than PCR primers, reducing allele dropout [97] |
Addressing technical artifacts in NGS-based cancer genomics requires a comprehensive approach integrating careful experimental design, appropriate platform selection, and validated computational correction methods. Batch effects and false positives represent significant challenges that can compromise data integrity and lead to erroneous biological conclusions, particularly in clinical settings where treatment decisions may be influenced by molecular findings [96] [94]. The strategies outlined in this document provide a framework for minimizing these artifacts throughout the entire research workflow, from initial study design to final data interpretation.
Successful artifact mitigation requires acknowledging that these technical variations are inevitable in large-scale omics studies and implementing systematic approaches to address them. By combining preventive experimental strategies with rigorous computational corrections and comprehensive validation, researchers can enhance the reliability and reproducibility of their genomic findings, ultimately advancing our understanding of cancer biology and improving patient care through more accurate molecular profiling.
Validation and Comparative Analysis: Establishing Clinical-Grade NGS Assays
The implementation of Next-Generation Sequencing (NGS) in clinical oncology represents a paradigm shift from traditional single-gene testing to comprehensive genomic profiling. This transition demands rigorous validation frameworks to ensure that results are accurate, precise, and reproducible, as they directly impact patient diagnosis, treatment selection, and clinical outcomes [15]. Clinical validation establishes the performance characteristics of an assay by defining its analytical sensitivity and specificity for detecting various variant types, and confirming its clinical utility to guide therapeutic decisions [97] [103]. For cancer genomics, this process is particularly complex due to the diversity of genomic alterations driving malignancy, including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), and gene fusions [97]. This document outlines standardized protocols and application notes for establishing validation frameworks that meet regulatory standards and ensure reliable implementation of NGS in clinical cancer research and diagnostics.
Foundational Principles of Assay Validation
Key Performance Metrics
Clinical validation of NGS assays requires demonstration of several interlinked performance characteristics through carefully designed experiments. Accuracy measures how close test results are to the true value, typically established by comparison to orthogonal methods or reference materials with known variants [104] [105]. Precision encompasses both repeatability (same operator, same setup) and reproducibility (different operators, instruments, laboratories) of measurements over time [97] [106]. Reproducibility between laboratories is especially critical for multicenter studies and clinical trials, ensuring consistent results regardless of testing location [106].
The limit of detection (LOD) defines the lowest variant allele frequency (VAF) at which a variant can be reliably detected, which is crucial for identifying subclonal populations in heterogeneous tumor samples [97]. Analytical sensitivity refers to the probability that the test will correctly detect a variant when present (true positive rate), while specificity indicates the probability that the test will correctly return a negative result when the variant is absent (true negative rate) [104].
Regulatory and Guidelines Framework
Clinical NGS assays should adhere to established professional guidelines, such as those from the Association of Molecular Pathology (AMP) and College of American Pathologists (CAP), which provide standards for test validation, quality control, and variant interpretation [97]. Compliance with In Vitro Diagnostic Regulation (IVDR) in the European Union and quality management systems such as ISO 13485 is essential for diagnostic applications [107]. Furthermore, data security and patient privacy must be maintained in accordance with GDPR and HIPAA requirements when handling genomic data [107].
Experimental Protocols for Establishing Validation Frameworks
Analytical Validation Study Design
A robust validation study should employ a combination of reference standards and clinical specimens to establish comprehensive performance characteristics across all variant types [97] [103].
Table 1: Recommended Sample Sizes for Analytical Validation Studies
| Variant Type | Minimum Number of Positive Samples | Minimum Number of Negative Samples | Recommended Reference Materials |
|---|---|---|---|
| SNVs | 10-15 | 3-5 | Genome in a Bottle, Seraseq |
| Indels | 10-15 (various lengths) | 3-5 | Seraseq, Horizon Dx |
| CNVs | 5-8 (both gains and losses) | 3-5 | Cell line mixtures, Coriell samples |
| Gene Fusions | 5-10 (various partners) | 3-5 | Cell lines with known rearrangements |
Reference Material Preparation and Dilution Series
Purpose: To establish analytical sensitivity, specificity, and limit of detection across variant types using samples with known truth sets.
Materials:
- Commercially available reference standards (e.g., Seraseq, Horizon Dx)
- DNA from cell lines with characterized variants (e.g., NCI-60 panel)
- Matched normal DNA from the same donor or cell line
- Qubit dsDNA HS Assay Kit (Invitrogen)
- Agilent TapeStation 4200 with High Sensitivity D1000 reagents
Procedure:
- Extract DNA from reference materials and cell lines using validated methods (e.g., QIAamp DNA FFPE Tissue Kit for formalin-fixed samples)
- Quantify DNA concentration using fluorometric methods (Qubit) and assess quality through spectrophotometry (NanoDrop) and fragment analysis (TapeStation)
- For limit of detection studies, create dilution series of tumor DNA in matched normal DNA to simulate varying tumor purity (e.g., 50%, 25%, 10%, 5%, 1%)
- For each dilution point, prepare three independent replicates to assess reproducibility
- Process all samples through the entire NGS workflow, including library preparation, target enrichment, and sequencing
- Analyze data using established bioinformatics pipelines to calculate sensitivity, specificity, and precision at each dilution level
Orthogonal Confirmation Using Clinical Specimens
Purpose: To validate NGS findings against established clinical testing methods using real-world patient samples.
Materials:
- Archived FFPE tumor samples with existing clinical test results
- Orthogonal testing platforms (Sanger sequencing, PCR-based methods, FISH, IHC)
- Nucleic acid extraction kits appropriate for sample type
- Library preparation reagents (e.g., Agilent SureSelectXT, Illumina TruSeq)
Procedure:
- Select 50-100 clinical samples representing various tumor types and sample qualities
- Ensure samples have been previously characterized by validated clinical tests for relevant biomarkers
- Perform nucleic acid extraction, quantifying both yield and quality
- Process samples through the NGS workflow alongside appropriate controls
- Analyze sequencing data and compare variant calls with prior clinical testing results
- Resolve discrepancies through additional testing or review to establish true positives/false positives
Table 2: Example Performance Metrics from a Validated Pan-Cancer Panel
| Performance Characteristic | SNVs/Indels | CNVs | Fusions | MSI Status |
|---|---|---|---|---|
| Sensitivity | 96.92% | 97.0% | 100% | 100% |
| Specificity | 99.67% | 97.8% | 91.3% | 94% |
| Limit of Detection (VAF) | 0.5% | 20% tumor content | 5% tumor content | 20% tumor content |
| Concordance with Orthogonal Methods | 94% (ESMO Level I variants) | 97.8% | 91.3% | 94% |
Reproducibility Assessment Across Sites
Purpose: To evaluate inter-laboratory reproducibility, essential for multicenter studies and clinical trials.
Materials:
- Aliquots of the same reference standards distributed to multiple testing sites
- Standardized protocols for library preparation, sequencing, and analysis
- Centralized data collection and analysis platform
Procedure:
- Prepare large batches of reference standards and distribute identical aliquots to participating laboratories
- Provide detailed testing protocols but allow each site to use their established NGS platforms and reagents
- Process samples in each laboratory following the provided protocol
- Analyze data both locally and through a centralized bioinformatics pipeline
- Compare variant calls across sites to calculate inter-laboratory reproducibility
- A recent study demonstrated that targeted NGS approaches show high inter-laboratory reproducibility, with minimal variation between independent facilities when sufficient read depth is maintained [106]
Bioinformatics Validation and Quality Control
Pipeline Verification
Bioinformatics pipelines require separate validation to ensure accurate variant calling, annotation, and interpretation.
Data Analysis Protocols:
- Alignment: Map sequencing reads to the reference genome (hg19 or hg38) using optimized aligners (BWA, STAR) [103]
- Variant Calling: Utilize established algorithms for different variant types:
- Annotation: Annotate variants using SnpEff and clinical databases [18]
- Filtering: Implement stringent filters based on depth (≥200x), allele frequency (≥2%), and quality scores [18]
Validation Metrics:
- Precision and recall for each variant type compared to known variants in reference standards
- Concordance with orthogonal methods for clinical samples
- Reproducibility across different computing environments
Quality Control Thresholds
Establish and monitor QC metrics throughout the NGS workflow:
- DNA/RNA quality: DV200 > 30% for FFPE samples, RIN > 7 for RNA [103]
- Library concentration: ≥ 2nM [18]
- Sequencing depth: Mean coverage ≥500x for targeted panels, ≥100x for whole exome [103]
- Uniformity: >80% of targets at ≥100x coverage [18]
- Duplication rate: <20% for DNA, <50% for RNA [103]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for NGS Validation Studies
| Category | Specific Products | Application | Quality Control Parameters |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA FFPE Tissue Kit, AllPrep DNA/RNA Mini Kit | Isolation of nucleic acids from various sample types | DNA: A260/A280 1.7-2.2, DV200 > 30%\nRNA: RIN > 7.0 |
| Library Preparation | Agilent SureSelectXT, Illumina TruSeq stranded mRNA | Library construction for DNA and RNA sequencing | Library size: 250-400 bp, Concentration: ≥2nM |
| Target Enrichment | SureSelect Human All Exon V7, Pan-cancer gene panels | Hybrid capture-based enrichment of target regions | Coverage uniformity: >80% at 100x |
| Reference Standards | Seraseq, Horizon Dx, Coriell cell lines | Analytical validation, LOD studies | Known variant VAF, Tumor purity |
| Sequencing Platforms | Illumina NovaSeq 6000, PacBio Sequel II | DNA and RNA sequencing | Q30 > 90%, PF > 80% |
| Analysis Tools | BWA, GATK, Strelka2, CNVkit, SnpEff | Sequence alignment, variant calling, annotation | Concordance with reference standards |
Clinical Implementation and Real-World Performance
Clinical Validation in Patient Cohorts
Large-scale clinical validation studies demonstrate the real-world performance of NGS assays. A study of 990 patients with advanced solid tumors using a 544-gene panel found that 26.0% harbored Tier I variants (strong clinical significance), and 86.8% carried Tier II variants (potential clinical significance) [18]. Among patients with Tier I variants, 13.7% received NGS-informed therapy, with 37.5% achieving partial response and 34.4% achieving stable disease [18]. For liquid biopsy applications, a multicenter validation of a 32-gene ctDNA panel demonstrated 96.92% sensitivity and 99.67% specificity for SNVs/Indels at 0.5% allele frequency, with 100% sensitivity for fusion detection [104].
Integrated RNA and DNA Sequencing
Combining RNA-seq with whole exome sequencing (WES) significantly enhances detection of clinically relevant alterations, particularly for gene fusions and expression-based biomarkers [103]. A validation study of 2230 clinical tumor samples demonstrated that integrated RNA-DNA sequencing enabled detection of actionable alterations in 98% of cases, recovering variants missed by DNA-only testing and revealing complex genomic rearrangements [103]. The validation framework for combined assays should include:
- Analytical validation using custom reference samples containing known variants
- Orthogonal testing in patient samples compared to established methods
- Clinical utility assessment in real-world cases to demonstrate improved detection of actionable alterations
Establishing rigorous clinical validation frameworks for NGS assays in cancer genomics requires a systematic, evidence-based approach that addresses analytical and clinical performance across all variant types. The protocols outlined herein provide a roadmap for demonstrating accuracy, precision, and reproducibility through well-designed experiments using reference standards, clinical samples, and orthogonal methods. As NGS technologies evolve and integrate multi-omic approaches, validation frameworks must similarly advance to ensure reliable clinical implementation. Standardization of these processes across laboratories will facilitate broader adoption of comprehensive genomic profiling in precision oncology, ultimately improving patient care through more accurate diagnosis and targeted treatment selection.
Within cancer genomics research, the accurate detection of genomic alterations is fundamental for diagnosis, prognosis, and guiding targeted therapies. Next-generation sequencing (NGS) has emerged as a powerful, high-throughput technology capable of interrogating multiple genes simultaneously. However, the integration of NGS into clinical and research workflows requires rigorous benchmarking against established orthogonal methods such as Polymerase Chain Reaction (PCR) and Fluorescence In Situ Hybridization (FISH) [108] [109]. This application note provides a detailed, structured comparison of these technologies, supported by quantitative data and experimental protocols, to guide researchers and drug development professionals in validating and implementing NGS for cancer genomics.
Performance Benchmarking: Quantitative Comparison of NGS, PCR, and FISH
A direct comparison of key performance metrics is essential for evaluating the strengths and limitations of each technology. The table below summarizes the capabilities of NGS, PCR, and FISH based on published studies.
Table 1: Key Performance Metrics of NGS, PCR, and FISH in Cancer Genomics
| Feature | Next-Generation Sequencing (NGS) | PCR-Based Methods | Fluorescence In Situ Hybridization (FISH) |
|---|---|---|---|
| Detection Scope | Comprehensive; discovers known and novel variants across many targets simultaneously [92]. | Targeted; detects specific pre-defined mutations or fusions [110] [109]. | Targeted; primarily detects chromosomal rearrangements, amplifications, and deletions [111]. |
| Sensitivity | High; demonstrated 85% sensitivity for malignancy in biliary brushings, surpassing FISH (76%) when combined with cytology [108]. | Very High; RT-PCR for ALK fusions showed 100% sensitivity compared to FISH [109]. | Moderate to High; 67-76% sensitivity in direct comparisons with NGS and PCR [108] [109]. |
| Specificity | High; specificities often exceed 94% [109]. | High; can achieve >99% specificity for well-characterized targets [110]. | High; specificities of 98% have been reported [108]. |
| Throughput | Very High; processes millions of sequences in parallel, suitable for large gene panels, whole exome, or whole genome sequencing [92]. | Moderate to High; suitable for multiplexing several targets, but limited by primer design [110]. | Low; typically analyzes one to a few targets per assay [111]. |
| Ability to Detect Novel Variants | Yes; hypothesis-free approach can identify novel fusions and mutations [112]. | No; limited to detecting variants for which specific primers are designed [110]. | Limited; can suggest a rearrangement but cannot identify novel fusion partners without specific probes [111]. |
| Tumor Cell Viability Requirement | No; detects nucleic acids from both viable and non-viable cells [113]. | No; similar to NGS, it cannot distinguish between viable and non-viable organisms [113]. | Yes; requires intact, viable cells for nucleus preservation [111]. |
Experimental Protocols for Orthogonal Method Comparison
The following section outlines standardized protocols for conducting a validation study comparing NGS to PCR and FISH.
Sample Preparation and DNA Extraction
Objective: To ensure consistent, high-quality input material for all three platforms. Materials:
- FFPE Tissue Sections: Sections of 5-10 µm thickness from patient tumor samples.
- DNA Extraction Kit: A commercially available kit designed for FFPE tissue (e.g., QIAamp DNA FFPE Tissue Kit).
- Nucleic Acid Quantitation Instrument: Fluorometer or spectrophotometer [114].
- Nucleic Acid Quality Analyzer: Bioanalyzer or TapeStation to assess DNA integrity [114].
Protocol:
- Macrodissection: Review a Hematoxylin and Eosin (H&E) stained slide to identify regions of high tumor purity. Mark these areas on the corresponding unstained FFPE slides.
- DNA Extraction: Follow the manufacturer's instructions for the DNA extraction kit. Include a deparaffinization step if required.
- DNA Quantification and Quality Control: Quantify the purified DNA using a fluorometric method. Assess DNA integrity via the DNA Integrity Number (DIN) or similar metric. Only proceed with samples meeting pre-defined quality thresholds (e.g., DIN > 4 and concentration > 2 ng/µL).
NGS Library Preparation and Sequencing
Objective: To prepare sequencing libraries for targeted cancer gene panels. Materials:
- Targeted Gene Panel Kit: e.g., Illumina TruSight Oncology or similar panel.
- Library Prep Reagents: Enzymes for end-repair, A-tailing, and adapter ligation.
- Index Adapters: For sample multiplexing.
- Thermocycler [114].
- Benchtop Sequencer: e.g., Illumina MiSeq, NextSeq 2000, or Complete Genomics DNBSEQ-G400 [114] [115].
Protocol:
- Library Preparation: Fragment genomic DNA to an average size of 200-300 bp. Perform end-repair, A-tailing, and ligate indexed Illumina-compatible adapters to the fragments.
- Target Enrichment: Hybridize the adapter-ligated library to biotinylated probes targeting the genes of interest. Capture the probe-bound fragments using streptavidin-coated magnetic beads.
- Library Amplification: Perform a limited-cycle PCR to amplify the enriched library.
- Library QC and Normalization: Quantify the final library and pool equimolar amounts of each sample for sequencing.
- Sequencing: Load the pooled library onto the sequencer and perform a paired-end run according to the manufacturer's instructions.
Orthogonal Validation Using RT-PCR and FISH
Objective: To validate key genetic alterations identified by NGS using orthogonal methods.
A. Validation of Fusion Genes by RT-PCR Materials:
- RT-PCR Kit: One-step RT-PCR kit with reverse transcriptase and DNA polymerase.
- Gene-Specific Primers: Primers designed to span the specific fusion breakpoint identified by NGS.
- Real-Time PCR Instrument.
Protocol:
- Reverse Transcription: Convert RNA extracted from the FFPE sample into cDNA.
- PCR Amplification: Set up reactions with gene-specific primers and cDNA template.
- Amplification and Detection: Run the real-time PCR protocol. A sample is considered positive if amplification occurs at or before a pre-defined cycle threshold (Ct) [109].
- Resolution of Discordance: In cases of discordance between NGS and RT-PCR (e.g., NGS-positive/RT-PCR-negative), confirm the result using RNA sequencing to detect the full-length transcript of the fusion gene [109].
B. Validation of Gene Amplifications by FISH Materials:
- FISH Probe Set: Commercially available break-apart or locus-specific probes for the target gene (e.g., UroVysion for chromosomal abnormalities) [108].
- Hybridization System.
Protocol:
- Slide Preparation: Prepare 4-5 µm FFPE tissue sections and bake them overnight.
- Pretreatment and Denaturation: Deparaffinize slides, perform a pretreatment to allow probe access, and denature the DNA.
- Hybridization: Apply the denatured FISH probe to the slide and incubate overnight in a humidified chamber to allow for hybridization.
- Post-Hybridization Wash and Counterstain: Wash slides to remove unbound probe and counterstain with DAPI.
- Signal Enumeration: Visualize signals using a fluorescence microscope. Score a pre-defined number of tumor cell nuclei (e.g., 50-100) for the FISH signal pattern. A sample is considered positive if the percentage of cells with the abnormal signal pattern exceeds the validated cutoff (e.g., >15% for some ALK assays) [109].
Visualizing the Benchmarking Workflow
The following diagram illustrates the logical workflow for benchmarking NGS against orthogonal methods, from sample preparation to data interpretation.
Figure 1: Benchmarking and Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful experimentation relies on a suite of reliable reagents and instruments. The table below details key materials for the experiments described.
Table 2: Essential Research Reagents and Equipment
| Item | Function/Application | Example Products / Notes |
|---|---|---|
| FFPE DNA Extraction Kit | Isolation of high-quality, amplifiable DNA from archived formalin-fixed, paraffin-embedded (FFPE) tissue samples. | QIAamp DNA FFPE Tissue Kit (QIAGEN) [109]. |
| Targeted NGS Panel | A predesigned set of probes for enriching and sequencing a specific set of cancer-related genes, enabling focused analysis. | Illumina TruSight Oncology, Comprehensive Cancer Panels. |
| NGS Library Prep Kit | A set of reagents to fragment DNA and attach platform-specific adapters and indices for sequencing. | Illumina DNA Prep kits. |
| RT-PCR Assay Kit | Validated reagents and primers for the sensitive and quantitative detection of specific RNA transcripts or fusion genes. | ALK RGQ RT-PCR Kit (QIAGEN) [109]. |
| FISH Probe Set | Fluorescently labeled DNA probes designed to bind to specific chromosomal loci for visualizing gene rearrangements or copy number changes. | Vysis ALK Break Apart FISH Probe (Abbott) [109]. |
| Nucleic Acid Quantitation Instrument | Accurate quantification of DNA/RNA concentration, critical for normalizing input material for NGS and PCR. | Fluorometer (e.g., Qubit, Thermo Fisher) [114]. |
| Nucleic Acid Quality Analyzer | Assessment of DNA/RNA integrity, a crucial quality control step, particularly for FFPE-derived material. | Bioanalyzer (Agilent) or TapeStation (Agilent) [114]. |
| Benchtop Sequencer | Instrument for performing NGS runs; benchtop systems offer a balance of throughput and accessibility for many labs. | Illumina iSeq 100, NextSeq 2000; Complete Genomics DNBSEQ-G400 [114] [115]. |
Benchmarking studies consistently demonstrate that NGS offers a comprehensive and highly sensitive platform for genomic profiling in cancer research, often outperforming or complementing targeted methods like PCR and FISH [108] [109]. While PCR remains the gold standard for ultra-sensitive detection of specific mutations and FISH for visualizing structural variations in a cellular context, NGS provides a unifying technology that can streamline testing and uncover novel biomarkers. The protocols and data presented herein provide a framework for researchers to rigorously validate NGS implementations, thereby strengthening the molecular foundation for drug discovery and clinical development.
Next-generation sequencing (NGS) has fundamentally transformed the landscape of clinical oncology by enabling comprehensive genomic profiling of tumors. This technology facilitates the delivery of precision medicine by identifying tumor-specific genomic alterations that can be targeted with matched therapies [9]. While the benefits of NGS-guided approaches in early-stage cancer are well-established, their impact in advanced, metastatic, or relapsed settings continues to be defined [116]. This application note synthesizes recent real-world evidence and randomized controlled trial (RCT) data to evaluate the clinical efficacy, implementation protocols, and practical considerations of NGS-guided therapies in advanced cancers, providing researchers and drug development professionals with a clear framework for clinical study design and analysis.
Clinical Outcomes from NGS-Guided Therapy
Efficacy and Survival Outcomes
Recent high-quality evidence from a systematic review and meta-analysis of 30 RCTs (enrolling 7,393 patients) demonstrates the significant benefit of NGS-guided matched targeted therapies (MTTs), particularly when combined with standard of care (SOC) treatments [116]. The analysis, which included patients with eight different advanced cancer types whose disease had progressed after at least one prior systemic therapy, showed that MTTs were associated with a 30-40% reduction in the risk of disease progression or death (Hazard Ratio for PFS ~0.6-0.7) [116].
Table 1: Summary of Efficacy Outcomes from NGS-Guided Therapy Studies
| Study Type | Patient Population | Key Efficacy Findings | Overall Survival | Reference |
|---|---|---|---|---|
| Meta-analysis of 30 RCTs | 7,393 patients with various advanced solid and haematological tumors | 30-40% risk reduction in disease progression; PFS benefit most pronounced in MTT + SOC combination | No consistent OS benefit with MTT monotherapy; OS improvement with MTT+SOC (prostate/urothelial cancer) | [116] |
| Real-World Study (SNUBH) | 990 patients with advanced solid tumors (82.5% Stage IV) | 37.5% partial response rate; 34.4% stable disease rate in patients with measurable lesions | Median OS not reached; median treatment duration: 6.4 months | [18] |
| Real-World Study (K-MASTER) | Multiple cancer cohorts (e.g., 225 colorectal cancer patients) | High concordance with orthogonal methods; sensitivity/specificity varied by gene (e.g., KRAS: 87.4%/79.3%) | Clinical outcomes inferred from accurate biomarker detection | [117] |
The survival benefits, however, were more tumor-specific. The meta-analysis found that combining MTTs with SOC resulted in improved overall survival (OS), with particularly notable benefits in patients with prostate and urothelial cancers. For patients with breast and ovarian cancer, the MTT and SOC combination conferred a progression-free survival (PFS) gain without a corresponding OS improvement [116].
Supporting these clinical trial findings, a real-world study of 990 patients with advanced solid tumors demonstrated that NGS-based therapy resulted in a 37.5% partial response rate and a 34.4% stable disease rate among patients with measurable lesions [18]. The median treatment duration was 6.4 months, indicating sustained disease control in this heavily pre-treated population [18].
Actionable Mutations and Treatment Rates
The real-world implementation evidence reveals both the promise and challenges of NGS-guided therapy. In the study at Seoul National University Bundang Hospital (SNUBH), 26.0% of patients harbored Tier I variants (variants of strong clinical significance), and 86.8% carried Tier II variants (variants of potential clinical significance) using the Association for Molecular Pathology classification system [18].
Despite this high rate of actionable mutations, only 13.7% of patients with Tier I variants subsequently received NGS-guided therapy [18]. The rate of implementation varied significantly by cancer type, being highest in thyroid cancer (28.6%), skin cancer (25.0%), gynecologic cancer (10.8%), and lung cancer (10.7%) [18]. This discrepancy between actionable mutation identification and treatment implementation highlights the significant barriers that remain in translating genomic findings into clinical practice, including drug access, performance status, and comorbidities.
Analytical Validation and Methodological Considerations
NGS Performance Versus Orthogonal Methods
The analytical validity of NGS testing is crucial for its reliable clinical application. The K-MASTER project, a Korean national precision medicine initiative, conducted extensive comparisons between NGS panel results and established orthogonal methods across multiple cancer types [117].
Table 2: Analytical Performance of NGS Versus Orthogonal Methods in the K-MASTER Cohort
| Cancer Type | Genetic Alteration | Sensitivity (%) | Specificity (%) | Concordance Notes |
|---|---|---|---|---|
| Colorectal Cancer (n=225) | KRAS mutation | 87.4 | 79.3 | Discordant cases resolved by ddPCR |
| Colorectal Cancer (n=197) | NRAS mutation | 88.9 | 98.9 | High positive predictive value |
| Colorectal Cancer | BRAF mutation | 77.8 | 100.0 | Perfect specificity |
| NSCLC (n=109) | EGFR mutation | 86.2 | 97.5 | Platform-dependent variability |
| NSCLC | ALK fusion | 100.0 | 100.0 | Perfect concordance |
| NSCLC | ROS1 fusion | 33.3 (1/3) | 100.0 | Limited positive cases |
| Breast Cancer (n=260) | ERBB2 amplification | 53.7 | 99.4 | Compared to IHC/ISH |
| Gastric Cancer (n=64) | ERBB2 amplification | 62.5 | 98.2 | Compared to IHC/ISH |
The results showed a high overall agreement rate between NGS and orthogonal methods, though the degree of concordance varied for specific genetic alterations [117]. The relatively lower sensitivity for ERBB2 amplification detection in breast and gastric cancers highlights both the technical challenges in detecting copy number variations and the biological complexities of gene amplification assessment compared to immunohistochemistry and in situ hybridization [117].
Sample Quality and Pre-Analytical Variables
The reliability of NGS testing depends heavily on sample quality and processing conditions. Formalin-fixed, paraffin-embedded (FFPE) specimens, the most common sample type in clinical practice, show detectable but generally negligible effects on NGS data quality compared to fresh-frozen tissue [118].
A comprehensive comparison of paired FFPE and frozen lung adenocarcinoma specimens revealed that FFPE samples had smaller library insert sizes, greater coverage variability, and an increase in C>T transitions—particularly at CpG dinucleotides—suggesting interplay between DNA methylation and formalin-induced changes [118]. Despite these differences, the error rate, library complexity, enrichment performance, and coverage statistics were not significantly different between sample types [118]. The high concordance of >99.99% in base calls between paired samples demonstrates that FFPE samples can be a reliable substrate for clinical NGS testing when proper quality control measures are implemented [118].
Experimental Protocols for Clinical NGS Implementation
Sample Preparation and Quality Control
Robust sample preparation is foundational to successful clinical NGS implementation. The following protocol outlines the key steps based on established methodologies from recent real-world studies [18]:
- DNA Extraction from FFPE Tissue: Use manual microdissection to select representative tumor areas with sufficient tumor cellularity. Extract genomic DNA using the QIAamp DNA FFPE Tissue kit (Qiagen) or similar systems designed for cross-linked samples [18].
- DNA Quantification and Quality Control: Quantify DNA concentration using the Qubit dsDNA HS Assay kit on the Qubit 3.0 Fluorometer. Assess DNA purity with NanoDrop Spectrophotometer, requiring an A260/A280 ratio between 1.7 and 2.2 for optimal library preparation [18].
- Library Preparation: Use a hybrid capture method for DNA library preparation and target enrichment according to Illumina's standard protocol with an Agilent SureSelectXT Target Enrichment Kit. The recommended input is at least 20 ng of high-quality DNA [18].
- Library Validation: Assess average library size and quantity using an Agilent 2100 Bioanalyzer system with an Agilent High Sensitivity DNA Kit. The typical acceptable size range is 250–400 bp with a minimum concentration of 2 nM [18].
Sequencing and Data Analysis Parameters
The analytical phase requires careful parameter selection to ensure reliable variant detection:
- Sequencing Platform and Coverage: Sequence samples on established platforms such as the Illumina NextSeq 550Dx. Achieve an average mean depth of at least 650×, with less than 80% of 100x coverage considered a sequencing failure [18].
- Variant Calling: Align reads to the human reference genome hg19. Use Mutect2 for detecting single nucleotide variants (SNVs) and small insertion/deletions (INDELs), with a recommended variant allele frequency (VAF) threshold of ≥2% for clinical reporting. Annotate identified variants using SnpEff [18].
- Copy Number Variation and Fusion Detection: Identify copy number variations (CNVs) using CNVkit, considering an average copy number ≥5 as a gain (amplification). Detect gene fusions using LUMPY, with read counts ≥3 interpreted as positive results for structural variations [18].
- Variant Classification and Reporting: Classify all genetic alterations into tiers according to the Association for Molecular Pathology guidelines, focusing clinical reporting on Tier I (strong clinical significance) and Tier II (potential clinical significance) variants [18].
Visualization of Clinical NGS Implementation Workflow
The following diagram illustrates the complete pathway from sample collection to clinical decision-making in NGS-guided therapy:
Diagram 1: Clinical NGS Implementation and Decision Pathway
This workflow outlines the sequential steps from patient identification through outcome assessment, highlighting key quality control checkpoints and decision nodes in the NGS-guided therapy process.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Clinical NGS Studies
| Category | Specific Product/Platform | Function in NGS Workflow | Key Specifications |
|---|---|---|---|
| DNA Extraction | QIAamp DNA FFPE Tissue Kit (Qiagen) | DNA extraction from formalin-fixed tissue | Optimized for cross-linked, fragmented DNA |
| DNA Quantification | Qubit dsDNA HS Assay (Invitrogen) | Fluorometric DNA quantification | Selective for double-stranded DNA |
| Library Preparation | Agilent SureSelectXT Target Enrichment | Hybrid capture-based library prep | Enriches for target genes of interest |
| Library Validation | Agilent 2100 Bioanalyzer | Library size and quality assessment | Fragment analysis via electrophoresis |
| Sequencing Platform | Illumina NextSeq 550Dx | High-throughput sequencing | Clinical-grade system for diagnostic use |
| Variant Calling | Mutect2 (Broad Institute) | SNV and INDEL detection | Optimized for somatic variant calling |
| Copy Number Analysis | CNVkit | Copy number variation detection | Targeted sequencing data compatible |
| Fusion Detection | LUMPY | Structural variant identification | Integrates multiple SV signals |
| Variant Annotation | SnpEff | Functional effect prediction | Annotates coding and non-coding variants |
The accumulation of real-world evidence and meta-analyses of randomized trials provides compelling data that NGS-guided therapy significantly improves progression-free survival in patients with advanced cancers, particularly when targeted agents are combined with standard of care treatments [116] [18]. The successful implementation of these approaches requires rigorous attention to pre-analytical variables, analytical validation, and careful interpretation of genomic findings within molecular tumor boards [118] [117]. While challenges remain in translating actionable mutations into delivered therapies, the continued refinement of NGS technologies, bioinformatic pipelines, and clinical decision support systems promises to further enhance the precision oncology paradigm, ultimately improving outcomes for cancer patients.
Within the framework of next-generation sequencing (NGS) protocols for cancer genomics research, rigorous analytical validation is paramount to ensure reliable clinical and research outcomes. The foundational parameters of analytical sensitivity (the ability to detect true positives), analytical specificity (the ability to avoid false positives), and limit of detection (the lowest quantity reliably detected) form the cornerstone of assay performance assessment [119]. For NGS applications in oncology, these parameters must be evaluated across diverse variant types—including single nucleotide variants (SNVs), insertions and deletions (indels), copy number alterations (CNAs), and gene fusions—each presenting unique technical challenges [97]. This document outlines standardized protocols and application notes for validating these critical parameters in targeted NGS panels for cancer genomic profiling.
Performance Benchmarks in Cancer Genomics
The performance requirements for NGS assays vary significantly based on intended use, from liquid biopsy-based multi-cancer early detection to tumor tissue sequencing for therapeutic guidance. The table below summarizes performance characteristics from established NGS applications.
Table 1: Performance Characteristics of NGS-Based Oncology Tests
| Test / Application | Reported Sensitivity | Reported Specificity | Key Performance Notes | Citation |
|---|---|---|---|---|
| Multi-Cancer Early Detection (Galleri) | 51.5% (all cancers, all stages); 76.3% (12 deadly cancers) | 99.6% | Sensitivity is stage-dependent: 39% Stage I to 92% Stage IV for key cancers. | [120] [121] |
| Liquid Biopsy for Lung Cancer (MAPs Method) | 98.5% | 98.9% | Orthogonally validated against ddPCR; sensitive down to 0.1% allele frequency. | [122] |
| Tumor Tissue NGS (SNUBH Panel) | N/A | N/A | 26% of patients harbored Tier I (strong clinical significance) variants. | [18] |
Experimental Protocols for Parameter Validation
Determining Analytical Sensitivity and Specificity
Principle: Analytical sensitivity and specificity are calculated by comparing NGS results to a reference method across a set of known positive and negative samples [119] [122]. The formulas are defined as:
- Sensitivity = Number of True Positives / (Number of True Positives + Number of False Negatives)
- Specificity = Number of True Negatives / (Number of True Negatives + Number of False Positives) [119]
Materials:
- DNA from well-characterized reference cell lines (e.g., Coriell Institute) with known variants.
- Clinical samples or tumor tissue with orthogonal validation data (e.g., from ddPCR) [97] [122].
- Targeted NGS sequencing platform (e.g., Illumina NextSeq 550Dx) [18].
- Bioinformatic pipeline for variant calling (e.g., Mutect2 for SNVs/indels, CNVkit for copy number variations) [18].
Procedure:
- Sample Selection: Assemble a validation set that includes samples with known positive variants (True Positives) and samples confirmed negative for those variants (True Negatives). The set should encompass the variant types the assay is designed to detect (SNVs, indels, CNAs, fusions) [97].
- NGS Testing: Process all samples through the entire NGS workflow, from nucleic acid extraction to library preparation and sequencing [97] [18].
- Data Analysis: Analyze sequencing data using the established bioinformatics pipeline.
- Result Comparison: Compare NGS results to the known reference truth data for each sample.
- Calculation: Classify results as True Positive (TP), False Negative (FN), True Negative (TN), and False Positive (FP). Calculate sensitivity and specificity using the formulas above [119].
Establishing the Limit of Detection (LOD)
Principle: The LOD is the lowest variant allele frequency (VAF) or concentration at which a variant can be reliably detected in a defined percentage of replicates (e.g., 95%) [97] [122].
Materials:
- Tumor cell line DNA with a known variant.
- Genomic DNA from a normal cell line.
- Digital PCR (dPCR) system for precise quantification of input DNA VAF [122].
Procedure:
- Sample Dilution: Create a dilution series of the tumor DNA (positive for the target variant) into the normal (wild-type) DNA. Use dPCR to accurately determine the VAF for each dilution point (e.g., 5%, 2%, 1%, 0.5%, 0.1%) [122].
- Replicate Testing: Process a sufficient number of replicates (e.g., n=20-30) at each dilution level through the NGS assay.
- Data Analysis: For each dilution level, calculate the detection rate (number of positive replicates / total number of replicates).
- LOD Determination: The LOD is the lowest VAF at which the variant is detected in ≥95% of replicates [97].
Workflow Visualization
The following diagram illustrates the core analytical validation workflow for an NGS assay in cancer genomics.
Figure 1: A workflow diagram for the analytical validation of an NGS assay, showing the key stages from planning to reporting.
The wet-lab process for a targeted NGS assay, crucial for generating the data used in validation, involves several key steps as depicted below.
Figure 2: The core wet-lab workflow for a targeted NGS assay, from sample input to data generation.
The Scientist's Toolkit
Successful implementation and validation of an NGS assay for cancer genomics requires specific reagents and tools. The following table details essential components.
Table 2: Key Research Reagent Solutions for NGS Assay Validation
| Reagent / Material | Function in Validation | Examples / Specifications |
|---|---|---|
| Reference Cell Lines | Provide samples with known, defined variants to act as positive controls and for LOD studies. | Commercially available cell lines from repositories like ATCC or Coriell. |
| Targeted Enrichment Kit | Isolates and amplifies genomic regions of interest for sequencing. | Hybrid capture-based (e.g., Agilent SureSelectXT) or amplicon-based (e.g., Illumina AmpliSeq) panels [97] [18]. |
| NGS Library Prep Kit | Prepares fragmented DNA for sequencing by adding platform-specific adapters. | Illumina Stranded mRNA Prep, or other kits compatible with the chosen sequencer [123]. |
| Orthogonal Validation Platform | Provides a reference method for confirming NGS results and determining true positives/negatives. | ddPCR [122] or qPCR [124]. |
| Bioinformatics Software | Analyzes raw sequencing data for variant calling, classification, and reporting. | Mutect2 (for SNVs/indels), CNVkit (for CNAs), LUMPY (for fusions) [18]. |
Next-generation sequencing (NGS) has revolutionized cancer genomics by enabling comprehensive molecular profiling of tumors, guiding precision oncology, and facilitating biomarker discovery [9] [7]. The analytical sensitivity and specificity of NGS-based assays are fundamentally dependent on rigorous quality control (QC) metrics throughout the workflow. In clinical cancer research, where the accurate detection of low-frequency somatic variants can determine therapeutic decisions, monitoring sequencing depth, coverage uniformity, and established QC thresholds becomes paramount [125] [126]. This application note provides detailed protocols and frameworks for implementing these critical quality control measures in cancer genomics research.
Core Quality Control Metrics
Sequencing Depth and Coverage
Sequencing depth, also referred to as sequencing coverage, describes the average number of reads that align to a given reference base position [127] [128]. It is a primary determinant of variant-calling confidence, especially for detecting subclonal populations in heterogeneous tumor samples [126].
The required depth varies significantly by application (Table 1). The Lander/Waterman equation (C = LN / G) is fundamental for calculating projected coverage, where C is coverage, L is read length, N is the number of reads, and G is the haploid genome length [127].
Table 1: Recommended Sequencing Coverage for Common NGS Applications in Cancer Research
| Sequencing Method | Recommended Coverage | Key Considerations in Cancer Context |
|---|---|---|
| Whole Genome Sequencing (WGS) | 30× to 50× for human [127] | Requires higher depth (≥80x) for somatic variant calling; sufficient for structural variants. |
| Whole-Exome Sequencing (WES) | 100× [127] | Standard for germline; often increased to 150-200x for somatic mutation detection in tumors. |
| Targeted Gene Panels | 500× - 1000×+ [125] [18] | Essential for confidently identifying low-frequency somatic variants (e.g., <5% VAF). |
| RNA-Seq | Usually measured in millions of reads [127] | 50-100 million reads per sample often required to detect rare transcripts and fusion genes. |
For liquid biopsy applications, where cell-free DNA fragments are short and variant allele frequencies can be extremely low (<<1%), sequencing depths often exceed 10,000x to achieve the necessary statistical power for detection [7].
Coverage Uniformity
Coverage uniformity measures the evenness of read distribution across the genome or target regions [128]. In cancer genomics, poor uniformity can lead to "dropouts" in critical genes or exons, potentially missing actionable mutations.
The Inter-Quartile Range (IQR) is a key metric for evaluating uniformity, defined as the difference in sequencing coverage between the 75th and 25th percentiles. A lower IQR indicates more uniform coverage across the dataset [127]. Hybridization capture-based panels are particularly prone to coverage biases due to varying probe efficiencies [125].
Key QC Thresholds and Data Analysis Metrics
Robust bioinformatic pipelines are required to calculate post-sequencing QC metrics. The following thresholds are considered minimum standards for high-quality data in cancer research:
- Mean Mapped Read Depth: Must meet or exceed the minimum depth determined by the experimental design and variant-calling requirements (see Table 1) [127].
- On-Target Rate: For hybrid-capture panels, >70% of reads should align to the targeted regions. A low rate indicates inefficient capture.
- Duplicate Read Rate: <20% for whole-genome sequencing; can be higher for capture-based assays but should be monitored closely.
- Uniformity: >80% of target bases should be covered at ≥20% of the mean depth [127] [128].
- Quality Scores (Q30): >80% of bases should have a base quality score of 30 or higher (indicating a 1 in 1000 error probability).
Experimental Protocols for Quality Control
Protocol: Pre-Sequencing Library QC
Objective: To ensure library quality and quantity before sequencing, maximizing the success of the run.
- Quantification: Precisely quantify the final library using fluorometric methods (e.g., Qubit dsDNA HS Assay). Verify DNA purity using a spectrophotometer (e.g., NanoDrop), accepting A260/A280 ratios between 1.7 and 2.2 [18].
- Fragment Size Analysis: Determine the average library fragment size using an instrument like the Agilent 2100 Bioanalyzer with a High Sensitivity DNA Kit. The typical target size for Illumina libraries is 250–400 bp [18].
- Quality Threshold: Proceed with sequencing only if the library concentration is ≥2 nM and the size distribution profile shows a clear, single peak without adapter dimer contamination [18].
Protocol: Calculating and Validating Sequencing Depth
Objective: To project the required sequencing output and confirm sufficient depth post-alignment.
Pre-Sequencing Calculation:
- Use the Lander/Waterman equation: C = LN / G.
- For a 100 Mb target (e.g., large panel), 300 million 150bp reads would yield: (150 * 300,000,000) / 100,000,000 = 450x coverage.
- Adjust the number of samples batched together on a flow cell to achieve the desired per-sample depth, as the total data output is fixed [126].
Post-Alignment Validation:
- Using alignment files (BAM), calculate mean depth with tools like
samtools depth. - Generate a coverage histogram to visualize the distribution of read depths across all bases [127].
- Confirm that ≥95% of target bases are covered at the minimum required depth for your study (e.g., 100x for a panel).
- Using alignment files (BAM), calculate mean depth with tools like
Protocol: Evaluating Somatic Variant Calling Sensitivity
Objective: To establish the limit of detection (LOD) for low-frequency variants, critical for cancer applications.
- Use Reference Standards: Sequence commercially available matched tumor-normal cell lines with known somatic variants (e.g., Genome in a Bottle HG008 reference material) [129].
- Titrate Data: Downsample the sequencing data from high-depth runs (e.g., 1000x) to various lower depths (e.g., 500x, 250x, 100x).
- Analyze Sensitivity: At each depth level, call variants and calculate the sensitivity (percentage of known variants detected) and precision. Plot sensitivity against variant allele frequency (VAF).
- Define LOD: Establish the minimum VAF that can be reliably detected at a given sequencing depth and set this as the LOD for your assay [125] [126].
Workflow Visualization
The following diagram illustrates the integrated quality control workflow for an NGS experiment in cancer genomics, from sample preparation to final data analysis.
Figure 1: NGS Quality Control Workflow for Cancer Genomics. This workflow outlines the critical QC checkpoints from library preparation to final analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for NGS QC in Cancer Genomics
| Item | Function | Example Product/Category |
|---|---|---|
| FFPE DNA/RNA Extraction Kits | Isols high-quality nucleic acids from archived clinical tumor samples. | QIAamp DNA FFPE Tissue Kit [18], Concert FFPE DNA kit [125] |
| Library Prep Kits | Fragments DNA and attaches platform-specific adapters. | Agilent SureSelectXT [18], Illumina DNA Prep |
| Target Enrichment Panels | Hybridization-based capture of genes of interest for targeted sequencing. | Custom-designed panels (e.g., HRR/HRD panels [125]), Comprehensive cancer panels (e.g., 544-gene panel [18]) |
| Unique Molecular Identifiers (UMIs) | Short random nucleotide tags to correct for PCR duplicates and sequencing errors, crucial for low-VAF detection. | Commercially incorporated in many library prep kits [126] |
| Quantification & QC Instruments | Accurately measure nucleic acid concentration and library fragment size. | Qubit Fluorometer, Agilent Bioanalyzer/TapeStation [18] |
| Matched Tumor-Normal Reference Standards | Benchmarked materials for validating somatic variant calling accuracy and sensitivity. | Genome in a Bottle (GIAB) HG008 cell line [129] |
Implementing rigorous quality control protocols for monitoring sequencing depth, coverage uniformity, and established QC thresholds is non-negotiable in modern cancer genomics research. The frameworks and protocols detailed herein provide a roadmap for researchers to ensure data integrity, maximize variant detection sensitivity, and generate clinically actionable insights from NGS data. As technologies evolve with the adoption of long-read sequencing and liquid biopsies, these foundational QC principles will remain critical for the advancement of precision oncology.
The implementation of next-generation sequencing (NGS) in clinical cancer genomics requires adherence to a complex regulatory landscape designed to ensure test accuracy, reliability, and clinical utility. In the United States, this landscape is primarily governed by two parallel yet complementary pathways: laboratory quality standards under the Clinical Laboratory Improvement Amendments (CLIA) and accreditation from the College of American Pathologists (CAP), and market authorization for tests and instruments through the Food and Drug Administration (FDA) [130] [131]. For researchers and drug development professionals, understanding the distinctions, applications, and intersections of these frameworks is crucial for developing clinically applicable NGS protocols, especially with significant regulatory updates taking effect in January 2025 [132] [133].
CLIA establishes federal quality standards for all laboratory testing performed on human specimens, focusing on the analytical validity of tests—their accuracy, precision, and reliability [130]. CAP accreditation is a more stringent, voluntary program that often complements CLIA certification, with a particular emphasis on pathology and detailed laboratory operations [130]. In contrast, the FDA regulates test kits and instruments as medical devices, focusing on their safety and effectiveness when used as directed by the manufacturer [130] [131]. The convergence of these frameworks ensures that NGS-based genomic profiling can be reliably translated into clinical decision-making for precision oncology.
Comparative Analysis of Regulatory Pathways
CLIA Certification & CAP Accreditation
CLIA Certification is a federal mandate established in 1988. Laboratories obtain a CLIA certificate by demonstrating to the Centers for Medicare & Medicaid Services (CMS) that they meet standards for personnel qualifications, quality control procedures, and analytical performance [130]. This certification is legally required for clinical laboratories in the U.S. to report patient results and is valid for two years. CLIA-certified labs are permitted to perform Laboratory Developed Procedures (LDPs), which are tests designed, validated, and used within a single laboratory [131]. The key strength of the CLIA framework is its flexibility, allowing labs to rapidly adapt and validate new biomarkers and NGS panels without seeking new pre-market approvals, a critical feature in the fast-evolving field of cancer genomics [131].
CAP Accreditation represents a higher "gold standard" of excellence. The inspection process is more detailed and is conducted by practicing laboratory professionals [130]. CAP standards often exceed CLIA requirements, particularly in areas like specimen handling, test validation, and pathology review. Laboratories with dual CLIA certification and CAP accreditation are recognized as operating at the highest level of clinical quality, which is why many leading molecular profiling companies and academic centers maintain both [130].
Table 1: Key Characteristics of CLIA and CAP
| Feature | CLIA Certification | CAP Accreditation |
|---|---|---|
| Nature | Federal law (mandatory) | Voluntary, peer-reviewed program |
| Oversight Body | Centers for Medicare & Medicaid Services (CMS) | College of American Pathologists |
| Primary Focus | Analytical validity, quality control, personnel | Comprehensive lab quality, pathology standards, patient care |
| Inspection Cycle | Every two years | Every two years |
| Value for NGS | Enables clinical reporting of LDPs | Demonstrates excellence and rigor in complex testing |
FDA Approval Pathways
The FDA regulates medical devices, including test kits and instruments, through pathways that require demonstration of clinical validity—the test's ability to accurately identify a clinical condition or predisposition [131]. For NGS tests, the primary authorization pathways are 510(k) clearance (for substantial equivalence to a predicate device) and Premarket Approval (PMA) for higher-risk Class III devices. A critical designation within oncology is the Companion Diagnostic (CDx), a test that is essential for the safe and effective use of a corresponding therapeutic product [134] [135].
The FDA's oversight has expanded to include some NGS-based tests, particularly those marketed as CDx. Recent examples include the MI Cancer Seek test from Caris Life Sciences, which received FDA approval as a CDx combining whole exome and whole transcriptome sequencing [134] [136], and Thermo Fisher's Oncomine Dx Express Test, approved for decentralized, rapid NGS testing in non-small cell lung cancer [135]. The fundamental regulatory conflict in this space stems from the FDA's view of LDPs as medical devices subject to their authority, while laboratories argue that LDPs are professional medical services best overseen under modernized CLIA standards [131].
2025 Regulatory Updates
Significant regulatory changes took effect in January 2025, impacting both proficiency testing and personnel qualifications.
Proficiency Testing (PT) Changes: CLIA regulations have been updated with 29 new regulated analytes and the deletion of five others [132]. A key change for oncology is the new requirement for laboratories to enroll in PT for conventional troponin I and T; high-sensitivity troponin assays, while not CLIA-regulated, will still require PT enrollment under CAP Accreditation Programs [132]. Furthermore, the performance criteria for hemoglobin A1c have been updated, with CMS setting a ±8% performance range and CAP applying a stricter ±6% accuracy threshold [132] [133]. In transfusion medicine, the performance criteria for unexpected antibody detection has been raised to 100% accuracy [132].
Personnel and Consultant Qualifications: The 2024 CLIA Final Rule revised qualification standards. Nursing degrees no longer automatically qualify as equivalent to biological science degrees for high-complexity testing, though new equivalency pathways are available [133]. Similarly, qualifications for Technical Consultants (TCs) now place greater emphasis on specific education and professional experience [133]. "Grandfathering" provisions allow personnel who met previous qualifications to continue in their roles.
Table 2: Summary of Key 2025 CLIA Regulatory Changes
| Area of Change | Specific Update | Impact on NGS Labs |
|---|---|---|
| Regulated Analytes | Addition of 29 new analytes, deletion of 5 [132] | Labs must review and update their PT programs to ensure all regulated analytes for which they test are covered. |
| Troponin Testing | Conventional troponin I and T are now regulated [132] | PT enrollment is required for conventional troponin assays. |
| Hemoglobin A1c | CMS performance criteria: ±8%; CAP: ±6% [133] | Labs must ensure their methods meet the relevant performance criteria for their accreditation. |
| Personnel | Updated qualifications for high-complexity testing personnel and Technical Consultants [133] | Labs must verify that new hires meet updated educational and experiential requirements. |
Experimental Protocols for Regulatory Compliance
Protocol: Analytical Validation of an NGS Panel under CLIA/CAP
This protocol outlines the key steps for analytically validating a targeted NGS panel for solid tumor profiling, consistent with CLIA/CAP standards and recent regulatory updates.
1. Sample Preparation and Library Construction
- Input Material: Use 50 ng of total nucleic acids isolated from Formalin-Fixed Paraffin-Embedded (FFPE) tumor tissue specimens, mirroring the input requirements of FDA-approved tests like MI Cancer Seek [134] [136].
- Nucleic Acid Extraction: Extract DNA and RNA simultaneously to conserve precious tumor samples. Assess quantity and quality using fluorometry and fragment analyzers.
- Library Preparation: Fragment the genomic DNA to a target size of 300 bp. Attach platform-specific adapter sequences via ligation. For targeted panels, use hybridization-based capture with biotinylated probes to enrich for the genes of interest. Amplify the final library via PCR and validate its quality using quantitative PCR or capillary electrophoresis [9].
2. Sequencing and Data Analysis
- Sequencing Reaction: Load the library onto the NGS platform (e.g., Illumina, Ion Torrent). Perform cluster generation and utilize sequencing-by-synthesis chemistry with fluorescently labeled nucleotides or semiconductor-based detection [9]. Aim for a minimum average coverage of 500x for the targeted regions to ensure high confidence in variant calling.
- Data Analysis Pipeline:
- Primary Analysis: Convert raw signal data (e.g., .bcl files) to base calls and generate FASTQ files.
- Secondary Analysis: Align reads to a reference genome (e.g., GRCh38) using a validated aligner (e.g., BWA). Call variants (SNVs, indels, CNAs) using approved bioinformatics algorithms. For RNA sequencing, also perform transcript alignment and gene expression quantification.
- Tertiary Analysis: Annotate variants using curated knowledge bases (e.g., ClinVar, COSMIC). Filter and prioritize variants based on quality metrics and clinical relevance. Generate a final clinical report [9].
3. Analytical Validation Metrics Establish performance metrics for the entire NGS workflow against known reference samples or orthogonal methods:
- Accuracy/Concordance: Demonstrate >97% positive and negative percent agreement with other FDA-approved assays for key biomarkers like PIK3CA, EGFR, and BRAF mutations, as well as for TMB and MSI [134] [136].
- Precision: Show ≥99% repeatability (within-run) and reproducibility (between-run, between-operator, between-instrument) [134].
- Analytical Sensitivity: Determine the limit of detection (LoD) for variant allele frequency, typically between 2-5% for somatic mutations.
- Analytical Specificity: Demonstrate ≥99% specificity to minimize false positives [134] [136].
- Reportable Range: Validate the entire NGS workflow from the extraction step through final reporting.
Protocol: Bridging LDP Validation to FDA Submission
For laboratories considering transitioning a Laboratory Developed Procedure (LDP) to an FDA-approved kit, the following bridging studies are essential.
1. Comparative Analytical Validation
- Conduct a method comparison study directly pitting the LDP against the predicate or to-be-approved IVD test.
- Use a set of well-characterized clinical FFPE samples spanning the assay's intended scope. The sample cohort should include a range of tumor types, variant types (SNVs, indels, CNAs, fusions), and variant allele frequencies.
- Establish success criteria prior to the study, such as ≥97% overall percent agreement for variant detection and ≥99% agreement for critical companion diagnostic biomarkers [134].
2. Clinical Validation for Companion Diagnostic Claims
- If the test is intended as a CDx, a clinical study must link the test result to a therapeutic outcome.
- Enroll patients from the intended-use population. Compare the test's ability to identify responders and non-responders to the targeted therapy against the clinical outcome.
- The study should be designed to meet the regulatory standards for the specific drug's labeling, often requiring a demonstration of statistical significance for improved outcomes in biomarker-positive patients [134] [135].
Visual Workflows and Signaling Pathways
The following diagrams illustrate the core regulatory pathways and NGS experimental workflow, providing a clear visual reference for researchers.
Diagram 1: U.S. Regulatory Pathways for NGS Tests. This chart illustrates the parallel paths of laboratory services (LDPs) governed by CLIA/CAP versus medical devices regulated by the FDA.
Diagram 2: NGS Workflow for Tumor Genomic Profiling. This flowchart outlines the key steps from sample to clinical report, highlighting critical quality control checkpoints required for CLIA/CAP compliance.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for NGS-based Cancer Genomics
| Item | Function/Description | Application in Protocol |
|---|---|---|
| FFPE Tumor Tissue Sections | Archival clinical samples; source of tumor DNA/RNA. Requires specialized extraction for fragmented, cross-linked nucleic acids. | The primary input material for solid tumor profiling; validation must account for its variable quality [134] [136]. |
| Total Nucleic Acid Extraction Kits | Reagents for simultaneous co-extraction of DNA and RNA from a single sample. | Conserves limited tissue, enabling comprehensive DNA and RNA analysis from one specimen [136]. |
| Hybridization Capture Probes | Biotinylated oligonucleotides designed to target specific genomic regions (e.g., 228-gene panel, whole exome). | Enriches sequences of interest before sequencing, making large-scale sequencing efficient and cost-effective [9]. |
| NGS Library Prep Kits | Reagents for fragmenting DNA, repairing ends, adding adapters, and amplifying the final library. | Prepares the nucleic acid sample for the sequencing platform; critical for achieving high complexity and low bias [9]. |
| Reference Standard Materials | Genetically characterized cell lines or synthetic controls with known mutations. | Serves as a positive control for validating assay accuracy, precision, and limit of detection during analytical validation. |
| Bioinformatics Pipelines | Software for sequence alignment, variant calling, and annotation. | Transforms raw sequencing data into interpretable genetic variants; must be rigorously validated [9]. |
Navigating the regulatory environment for NGS in cancer genomics demands a strategic approach that balances innovation with compliance. The CLIA/CAP and FDA pathways, while distinct, collectively ensure that genomic tests are analytically robust and clinically meaningful. For researchers, the optimal strategy involves building NGS protocols on a foundation of rigorous CLIA/CAP compliance, which provides the flexibility needed for research and development. When the goal is widespread commercial distribution of a test kit or a specific companion diagnostic claim, engaging with the FDA approval pathways becomes necessary. The recent 2025 updates to CLIA regulations further emphasize the need for laboratories to stay current with proficiency testing and personnel standards. By integrating these regulatory considerations into the earliest stages of experimental design, scientists and drug developers can accelerate the translation of genomic discoveries into validated clinical applications that reliably inform patient care.
Conclusion
Next-generation sequencing has fundamentally transformed cancer genomics, providing unprecedented capabilities for comprehensive molecular profiling that directly informs therapeutic decision-making. The integration of NGS into clinical oncology requires robust protocols spanning technical execution, bioinformatics analysis, and clinical interpretation. While challenges remain in standardization, cost management, and data interpretation, the demonstrated improvement in progression-free survival with NGS-guided therapy underscores its clinical value. Future directions will focus on integrating multi-omics data, advancing liquid biopsy applications for dynamic monitoring, implementing artificial intelligence for enhanced variant interpretation, and expanding accessibility to diverse healthcare settings. As sequencing technologies continue to evolve toward single-molecule and single-cell resolutions, NGS will increasingly become the cornerstone of precision oncology, enabling more nuanced molecular classifications and personalized treatment strategies that improve patient outcomes across cancer types.
References
- 1. : Principle, Steps, Applications, Diagram Sanger Sequencing [https://microbenotes.com/sanger-sequencing/]
- 2. A computational framework for extracting biological ... [https://www.nature.com/articles/s41598-025-91781-8]
- 3. Molecular and Clinical Oncology [https://www.spandidos-publications.com/10.3892/mco.2025.2855]
- 4. RNA hybrid-capture next-generation sequencing has high ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1550706/full]
- 5. Assessment of target enrichment platforms using massively ... parallel [https://pubmed.ncbi.nlm.nih.gov/22426012/]
- 6. RBBP6 maintains glioblastoma stem cells through CPSF3- ... [https://www.nature.com/articles/s41421-024-00654-3]
- 7. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 8. Next generation DNA Sequencing data analysis and its ... [https://www.sciencedirect.com/science/article/abs/pii/S034403382500473X]
- 9. Next-generation sequencing in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 10. Sample Preparation for NGS – A Comprehensive Guide [https://frontlinegenomics.com/sample-preparation-for-ngs-a-comprehensive-guide/]
- 11. A Feasibility Study of NGS-Based Variant Analysis of FFPE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384127/]
- 12. Next Generation Sequencing Sample Submission Guidelines [https://www.genewiz.com/public/resources/sample-submission-guidelines/next-generation-sequencing-sample-submission-guidelines]
- 13. Making the Most of Your NGS Data: Understanding Metrics ... [https://sequencing.roche.com/us/en/article-listing/metrics-for-target-enriched-ngs.html]
- 14. An NGS Workflow Blueprint for DNA Sequencing Data and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4827795/]
- 15. Next-Generation Sequencing: A Review of Its ... [https://www.mdpi.com/2075-4418/15/19/2425]
- 16. Comprehensive genomic profiling of over 10000 advanced ... [https://www.oncotarget.com/article/28757/text/]
- 17. Comprehensive genomic profiling reveals a unique ... [https://www.nature.com/articles/s41598-025-94762-z]
- 18. Clinical implementation of next-generation sequencing ... [https://www.nature.com/articles/s41598-024-84909-9]
- 19. Emerging biomarkers for early cancer detection and diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359849/]
- 20. The evolving landscape of genetic biomarkers for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1522262/full]
- 21. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 22. Next-Generation Sequencing in Oncology—A Guiding ... [https://www.mdpi.com/1422-0067/26/7/3123]
- 23. NGS Basics for Cancer Research [https://www.thermofisher.com/us/en/home/life-science/sequencing/sequencing-learning-center/next-generation-sequencing-information/cancer-research/basics.html]
- 24. ACMG clinical laboratory standards for next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4098820/]
- 25. High clinical actionability of a pan-cancer tissue-based ... [https://www.nature.com/articles/s41698-025-01126-x]
- 26. NGS Streamlines Biomarker Testing in Solid Tumors [https://www.oncnursingnews.com/view/ngs-streamlines-biomarker-testing-in-solid-tumors]
- 27. The Next Generation Sequencing Quality Initiative [https://www.cdc.gov/lab-quality/php/ngs-quality-initiative/index.html]
- 28. The Cancer Genome Atlas Program (TCGA) - NCI [https://www.cancer.gov/ccg/research/genome-sequencing/tcga]
- 29. ICGC Initiatives [https://www.icgc-argo.org/page/65/icgc-initiatives-]
- 30. An Integrated TCGA Pan-Cancer Clinical Data Resource to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6066282/]
- 31. Pan-cancer analysis of whole genomes [https://www.nature.com/articles/s41586-020-1969-6]
- 32. Genomic Data Commons 2.0: A Valuable Tool for Cancer ... [https://ncifrederick.cancer.gov/about/theposter/content/genomic-data-commons-20-a-valuable-tool-for-cancer-researchersm]
- 33. Analysis of next-generation genomic data in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC2953747/]
- 34. ICGC ARGO - Home [http://www.icgc-argo.org/]
- 35. Comparing NGS Platforms: Ion Torrent vs. Illumina [https://www.biotechveritas.com/blog/ngs]
- 36. DNA Sequencing: How to Choose the Right Technology [https://frontlinegenomics.com/dna-sequencing-how-to-choose-the-right-technology/]
- 37. Decoding the Power of Third-Generation Sequencing - Yeasen [https://www.yeasenbio.com/blogs/ngs/decoding-the-power-of-third-generation-sequencing-applications-beyond-ngs]
- 38. A Primer on NGS Technologies and Their Specs (2025) [https://blog.latch.bio/p/a-primer-on-ngs-technologies-and]
- 39. Ion Torrent Next-Generation Sequencing Technology [https://www.thermofisher.com/us/en/home/life-science/sequencing/next-generation-sequencing/ion-torrent-next-generation-sequencing-technology.html]
- 40. Ultima Genomics UG 100 platform vs. Illumina NovaSeq X ... [https://www.illumina.com/science/genomics-research/articles/ultima-ug-100-vs-illumina-novaseq-x-wgs-data.html]
- 41. Sequencing Platforms | Illumina NGS platforms [https://www.illumina.com/systems/sequencing-platforms.html]
- 42. Ion Torrent NGS Instruments - Sequencing [https://www.thermofisher.com/us/en/home/life-science/sequencing/next-generation-sequencing/ion-torrent-next-generation-sequencing-workflow/ion-torrent-next-generation-sequencing-run-sequence.html]
- 43. Editorial: Next generation sequencing and cancer [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1675753/full]
- 44. A study on the global Library Preparation and Target ... [https://www.linkedin.com/pulse/astudy-onthe-global-library-preparation-target-enrichment-next-sxpgf]
- 45. Comparison of library preparation methods reveals their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4213505/]
- 46. a systematic comparison of DNA library preparation kits for ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-016-2757-4]
- 47. WGS vs. WES vs. Targeted Sequencing Panels [https://www.cd-genomics.com/resource-wgs-vs-wes-vs-targeted-panels.html]
- 48. Panels, WES, or WGS: Which is Best for Rare Disease ... [https://3billion.io/blog/which-is-the-best-ngs-approach-for-rare-disease-diagnosis-panels-wes-or-wgs]
- 49. A nationwide comprehensive genomic profiling and ... [https://www.nature.com/articles/s41698-025-00858-0]
- 50. Illumina Comprehensive Genomic Profiling Test for Cancer ... [https://www.illumina.com/company/news-center/press-releases/2025/586da3e1-460e-4a24-a018-0d82b7e35c01.html]
- 51. A comprehensive overview of minimal residual disease in ... [https://www.nature.com/articles/s41698-025-00984-9]
- 52. Liquid biopsy for minimal residual disease and monitoring ... [https://www.explorationpub.com/Journals/em/Article/1001349]
- 53. Monitoring and Assessment of Circulating Tumor DNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550271/]
- 54. Cancer in a Drop: Liquid biopsy insights from AACR 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223554/]
- 55. Augmenting precision medicine via targeted RNA-Seq ... [https://www.nature.com/articles/s41698-025-00993-8]
- 56. RNA‐sequencing: A reliable tool to unveil transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078890/]
- 57. a practical guide to RNA sequencing data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599993/]
- 58. Clinical Bioinformatics Pipeline [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/clinical-bioinformatics-pipeline]
- 59. Best practices for the interpretation and reporting of clinical ... [https://www.nature.com/articles/s41525-022-00295-z]
- 60. Recommendations for bioinformatics in clinical practice [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01543-4]
- 61. Artificial intelligence in variant calling: a review [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1574359/full]
- 62. AnnotaPipeline: An integrated tool to annotate eukaryotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9723129/]
- 63. Optimization of FFPE preparation and identification of gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10830353/]
- 64. Optimizing RNA extraction and library preparation from oral ... [https://bmrat.org/index.php/BMRAT/article/view/840]
- 65. xGen ssDNA & Low-Input DNA Library Prep Kit | IDT [https://www.idtdna.com/pages/products/next-generation-sequencing/workflow/xgen-ngs-library-preparation/dna-library-preparation/ssdna-low-input-dna-library-prep-kit]
- 66. NGS Low Input DNA Library Prep Kit - 1.5-hour Protocol [https://biodynami.com/product/ngs-low-input-dna-library-prep-kit/?srsltid=AfmBOopXw0wd84UdhIuSdgpMM7MMh4xPbYV6_1c1zgJXqR12fgX5yfYt]
- 67. Automated NGS library preparation - Genomics [https://lifesciences.tecan.com/applications_and_solutions/genomics/ngs_sample_preparation]
- 68. Advances in tumor subclone formation and mechanisms of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06486-3]
- 69. Characterization of cancer genomic heterogeneity by next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6333046/]
- 70. Tumour heterogeneity articles within Nature Methods [https://www.nature.com/subjects/tumour-heterogeneity/nmeth]
- 71. Cancer subclone detection based on DNA copy number in ... [https://pubmed.ncbi.nlm.nih.gov/40954304/]
- 72. Integrative spatial and genomic analysis of tumor ... [https://www.nature.com/articles/s41467-024-53374-3]
- 73. - Next (NGS) | CCR Generation Sequencing Genomics [https://genomics.ccr.cancer.gov/technologies/ngs/]
- 74. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 75. Methods to improve the accuracy of next-generation sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC9895957/]
- 76. An optimized targeted Next-Generation Sequencing ... [https://www.sciencedirect.com/science/article/pii/S2214753517302115]
- 77. Greater confidence in calling low-frequency variants [https://www.ogt.com/us/resources/ngs-resources-and-support/ngs-resources/greater-confidence-in-calling-low-frequency-variants-from-as-little-as-10ng-of-severely-formalin-compromised-dna/]
- 78. Functional phenotyping of genomic variants using joint ... [https://www.nature.com/articles/s41592-025-02805-0]
- 79. analysis of read length impact on cost and performance | BMC ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10778-1]
- 80. NGS Data Analysis for Illumina Platform—Overview and ... [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/next-generation-sequencing/ngs-data-analysis-illumina.html]
- 81. A General Guide on NGS Data Analysis [https://bioinfo.cd-genomics.com/resource-ngs-data-analysis.html]
- 82. Standardization and quality management in next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5025460/]
- 83. Next-Generation Sequencing Bioinformatics Pipelines [https://myadlm.org/cln/articles/2020/march/next-generation-sequencing-bioinformatics-pipelines]
- 84. NIH Data Management and Access Requirements for Sharing ... [https://researchservices.upenn.edu/nih-data-management-and-access-requirements-for-sharing-genomic-data/]
- 85. Tools & Resources [https://www.cancergenomicscloud.org/tools-and-resources]
- 86. Computational Genomics Research - NCI [https://www.cancer.gov/ccg/research/computational-genomics]
- 87. Standards and Guidelines for Validating Next-Generation ... [https://www.sciencedirect.com/science/article/pii/S1525157817303732]
- 88. Bioinformatics tools and resources for cancer and application [https://pmc.ncbi.nlm.nih.gov/articles/PMC11374212/]
- 89. Sequencing Depth vs. Coverage: Key Metrics in NGS ... [https://3billion.io/blog/sequencing-depth-vs-coverage]
- 90. Coverage tradeoffs and power estimation in the design of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3129526/]
- 91. Next Generation Sequencing Market Size & Forecast, 2025 ... [https://www.coherentmarketinsights.com/market-insight/next-generation-sequencing-market-158]
- 92. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 93. Maximizing Impact: Strategies for Budget Allocation Efficiency [https://cassandra.app/resources/maximizing-impact-strategies-for-budget-allocation-efficiency]
- 94. Assessing and mitigating batch effects in large-scale omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11447944/]
- 95. Assessing and mitigating batch effects in large-scale omics ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 96. Substantial batch effects in TCGA exome sequences ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6686424/]
- 97. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 98. Why You Must Correct Batch Effects in Transcriptomics Data? [https://www.metwarebio.com/transcriptomics-batch-effect-correction/]
- 99. Sequencing introduced false positive rare taxa lead to biased ... [https://environmentalmicrobiome.biomedcentral.com/articles/10.1186/s40793-022-00436-y]
- 100. Comparative analysis of batch correction methods for FDG ... [https://www.nature.com/articles/s41598-023-45296-9]
- 101. Protein-level batch-effect correction enhances robustness ... [https://www.nature.com/articles/s41467-025-64718-y]
- 102. Batch effect correction and normalization of scRNA-Seq data [https://www.nygen.io/resources/blog/batch-effect-normalization-techniques-scrna-seq]
- 103. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 104. Analytical Validation of a Pan-Cancer NGS Assay for In- ... [https://www.sciencedirect.com/science/article/pii/S152515782500220X]
- 105. Clinical Validation of Whole Genome Sequencing for ... [https://www.sciencedirect.com/science/article/pii/S1525157821001203]
- 106. Reproducibility of next-generation-sequencing-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10562171/]
- 107. How NGS Automation Improves Library Preparation ... [https://www.euformatics.com/blog-post/how-ngs-automation-improves-library-preparation-efficiency-and-accuracy]
- 108. Next-Generation Sequencing and Fluorescence in Situ ... [https://www.sciencedirect.com/science/article/pii/S1525157815002226]
- 109. Performance of a RT-PCR Assay in Comparison to FISH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5575602/]
- 110. PCR-based diagnostics for infectious diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC7106425/]
- 111. Fluorescence in situ hybridization: uses and limitations [https://pubmed.ncbi.nlm.nih.gov/11071355/]
- 112. Next generation DNA sequencing data analysis and its ... [https://pubmed.ncbi.nlm.nih.gov/41177096/]
- 113. Limitations of PCR Only [https://pathnostics.com/limitations-of-pcr-only/]
- 114. Cost of NGS | Comparisons and budget guidance [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/ngs-cost.html]
- 115. Next-Generation Sequencing Costs: The Sub $100 Genome [https://www.completegenomics.com/next-generation-sequencing-costs/]
- 116. Clinical Impact of Next-Generation Sequencing-Guided ... [https://pubmed.ncbi.nlm.nih.gov/41101085/]
- 117. Comparison of the Data of a Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8756135/]
- 118. Comparison of Clinical Targeted Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4912568/]
- 119. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 120. Galleri Test Sensitivity & Specificity | Galleri® for HCPs [https://www.galleri.com/hcp/galleri-test-performance]
- 121. Sensitive and specific multi-cancer detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8274402/]
- 122. Sensitivity, specificity, and accuracy of a liquid biopsy ... [https://www.nature.com/articles/s41598-021-89592-8]
- 123. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 124. Next generation sequencing reveals limitation of qPCR ... [https://pubmed.ncbi.nlm.nih.gov/33738553/]
- 125. A Differential Depth Sequencing Method, SPRE‐Seq, for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552348/]
- 126. Sequencing depth vs. sequencing batching [https://www.ogt.com/us/resources/ngs-resources-and-support/ngs-resources/sequencing-depth-vs-sequencing-batching/]
- 127. Sequencing Coverage for NGS Experiments [https://www.illumina.com/science/technology/next-generation-sequencing/plan-experiments/coverage.html]
- 128. Sequencing 101: Sequencing coverage [https://www.pacb.com/blog/sequencing-101-sequencing-coverage/]
- 129. Development and extensive sequencing of a broadly ... [https://www.nature.com/articles/s41597-025-05438-2]
- 130. CLIA and CAP: What You Need to Know [https://www.foregenomics.com/blog/clia-cap?srsltid=AfmBOor1_3ijilEAEzBjYGUmqM166uz15WdoGs98bb32N5BSnyNmuHwv]
- 131. Understanding Implications of the Proposed FDA Regulation ... [https://www.personalizedmedonc.com/articles/understanding-implications-of-the-proposed-fda-regulation-of-laboratory-developed-tests]
- 132. Get Ready for the PT CLIA Changes:… [https://www.cap.org/calendar/webinars/get-ready-for-the-pt-clia-changes-stay-ahead-stay-compliant]
- 133. 2025 Changes to Point-of-Care Testing Regulatory ... [https://myadlm.org/education/point-of-care-testing-professional-certification/the-point/articles/2025/may]
- 134. FDA-Approved MI Cancer Seek Test Enhances Tumor ... [https://www.oncotarget.com/news/pr/fda-approved-mi-cancer-seek-test-enhances-tumor-profiling-for-precision-oncology/]
- 135. FDA approves companion diagnostic for lung cancer [https://myadlm.org/cln/articles/2025/septemberoctober/fda-approves-companion-diagnostic-for-lung-cancer]
- 136. Press Release [https://www.carislifesciences.com/about/news-and-media/caris-life-sciences-demonstrates-scientific-rigor-with-clinical-validation-of-fda-approved-mi-cancer-seek/]