PDX vs. Organoid Models: A Comparative Analysis of Predictive Value in Oncology Drug Development
This article provides a comprehensive comparative analysis of Patient-Derived Xenograft (PDX) and Patient-Derived Organoid (PDO) models, two transformative technologies in preclinical oncology research.
PDX vs. Organoid Models: A Comparative Analysis of Predictive Value in Oncology Drug Development
Abstract
This article provides a comprehensive comparative analysis of Patient-Derived Xenograft (PDX) and Patient-Derived Organoid (PDO) models, two transformative technologies in preclinical oncology research. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles, methodological applications, and optimization strategies for both platforms. We critically evaluate their capacity to predict clinical drug response, examining evidence from multiple cancer types including gastrointestinal, ovarian, and prostate cancers. The analysis synthesizes current data on model fidelity, throughput, cost, and clinical correlation, offering a strategic framework for model selection to enhance the predictive power and efficiency of cancer drug discovery and personalized medicine approaches.
Understanding PDX and Organoid Models: Core Principles and Tumor Biology Preservation
Model Fundamentals and Establishment
Patient-Derived Xenograft (PDX) Models are established by implanting fresh fragments of human patient tumors directly into immunocompromised mice [1] [2]. These models serve as in vivo surrogates, allowing the study of tumor behavior within a living organism. The process involves several key steps: tumor tissue is acquired from surgery or biopsy, cut into small pieces, and then implanted into mice, typically subcutaneously, orthotopically (into the corresponding mouse organ), or under the renal capsule [1] [3]. To prevent rejection of the human tissue, highly immunodeficient mouse strains such as NOD-SCID or NSG mice are used [1] [3]. The engrafted tumors are then passaged in mice to expand the model [1].
Organoids, or Patient-Derived Organoids (PDOs), are three-dimensional (3D) in vitro systems grown from stem cells or tumor cells in a lab dish [4] [5]. They are designed to self-organize and recapitulate the structure and function of the original tissue [4]. Establishment involves digesting a patient tumor sample into small fragments or single cells, which are then embedded in an extracellular matrix (like Matrigel) and fed with a specialized culture medium containing growth factors necessary for stem cell survival and proliferation [6] [4]. This process allows the cells to grow and form 3D structures that mimic key aspects of the original tumor [5].
Comparative Strengths and Limitations
The choice between PDX and organoid models is guided by their distinct advantages and drawbacks, which are summarized in the table below.
Table 1: Strengths and Limitations of PDX and Organoid Models
| Feature | Patient-Derived Xenograft (PDX) | Patient-Derived Organoid (PDO) |
|---|---|---|
| Physiological Context | In vivo; preserves some tumor-stroma interactions and allows study of systemic drug effects like pharmacokinetics [1] [7]. | In vitro; largely lacks a complete tumor microenvironment (e.g., functional blood vessels, immune system) though co-culture methods are improving this [3] [8]. |
| Predictive Value | High; demonstrates strong correlation with patient clinical responses, making them a gold standard for preclinical drug testing [2] [7]. | High; shows a 68% Positive Predictive Value (PPV) and 78% Negative Predictive Value (NPV) for therapy response in colorectal cancer [6]. |
| Tumor Heterogeneity | Retains the intratumor heterogeneity and spatial architecture of the original patient tumor [1]. | Retains tumor cell heterogeneity but may lose some spatial context and select for certain cell populations over time [4] [8]. |
| Throughput & Scalability | Low to medium; time-consuming (months) and expensive to establish and maintain, limiting high-throughput screening [3]. | High; can be established and expanded in 1-2 weeks, suitable for high-throughput drug screening and biobanking [6] [8]. |
| Technical & Cost Considerations | High cost due to animal maintenance; requires specialized facilities for immunodeficient mice; low engraftment rate for some cancer types [2] [3]. | Cost-effective; more affordable than PDX; technically less demanding but requires optimization of culture media for different cancer types [8]. |
| Human Microenvironment | Lacks a human immune system (unless using humanized mice), and mouse stroma eventually replaces human stroma [1] [3]. | Enables co-culture with patient-specific immune cells to study immunotherapy and reconstruct human tumor-immune interactions [8] [9]. |
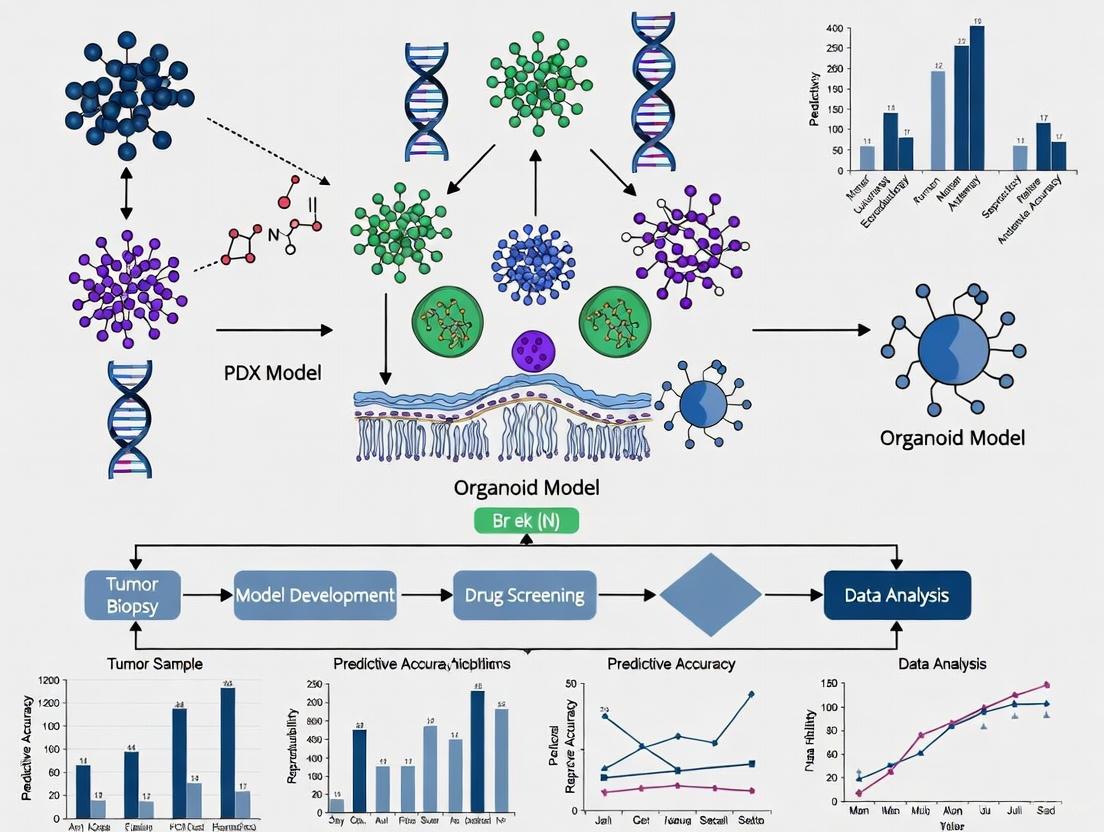
Experimental Workflows
The processes for establishing and utilizing these models differ significantly. The following diagrams outline the core workflows.
Diagram: PDX Establishment and Application Workflow
Diagram: Organoid Establishment and Application Workflow
Quantitative Predictive Performance Data
A critical measure of a model's value is its ability to accurately predict patient responses. The table below summarizes performance data for organoid models from a systematic review in colorectal cancer.
Table 2: Predictive Performance of Colorectal Cancer Organoids in Therapy Response [6]
| Therapy Category | Predictive Metric | Performance Value |
|---|---|---|
| Chemotherapy, Targeted Drugs, & Radiotherapy | Positive Predictive Value (PPV) | 68% |
| Negative Predictive Value (NPV) | 78% | |
| Illustrative Drug: 5-Fluorouracil (5-FU) | Organoid Response predicts Patient Non-response | High Accuracy (Specificity >95% in one study [6]) |
For PDX models, while specific NPV/PPV values are not provided in the search results, multiple studies confirm a high degree of correlation between drug responses in PDX models and the clinical outcomes of the donor patients, solidifying their role in preclinical drug development [2] [7].
Essential Research Reagents and Materials
Successful establishment and experimentation with these models rely on a suite of specialized reagents.
Table 3: Key Reagent Solutions for PDX and Organoid Research
| Reagent / Material | Function in Research | Model Application |
|---|---|---|
| Immunodeficient Mice (e.g., NSG, NOG) | Host for human tumor tissue implantation; prevents graft rejection. | PDX |
| Extracellular Matrix (e.g., Matrigel) | Provides a 3D scaffold that supports cell growth, polarization, and organization. | Organoid |
| Specialized Culture Media | Chemically defined medium containing niche factors (e.g., WNT, R-spondin) for stem cell maintenance. | Organoid |
| Tumor Dissociation Kits | Enzymatic blends (e.g., collagenase) for breaking down solid tumor tissue into cells/fragments. | PDX & Organoid |
| Cryopreservation Media | Allows long-term storage and biobanking of established PDX tumors or organoid lines. | PDX & Organoid |
PDX and organoid models are complementary tools that address different research needs. PDX models are the premier in vivo system for studying tumors in a whole-body context, making them indispensable for late-stage preclinical validation of drug efficacy, resistance mechanisms, and metastatic processes [1] [7]. In contrast, organoids are a powerful high-throughput in vitro platform ideal for large-scale drug screening, personalized therapy prediction, and genetic manipulation, all within a clinically relevant timeline [6] [8] [9].
The future of cancer modeling lies in the convergence of these systems. Emerging approaches include using PDX-derived organoids to expand limited PDX material and creating more complex humanized PDX models by engrafting a human immune system to effectively evaluate immunotherapy [3]. As both technologies evolve, they will continue to enhance the predictive power of cancer research and accelerate the development of novel therapeutics.
The Critical Role of Cancer Stem Cells in Maintaining Tumor Heterogeneity
Tumor heterogeneity remains a significant challenge in oncology, driving disease progression, metastasis, and therapeutic resistance. Cancer stem cells (CSCs) are now recognized as pivotal contributors to this heterogeneity through their self-renewal and differentiation capacities. This review examines how patient-derived xenograft (PDX) and organoid models uniquely capture CSC-driven heterogeneity and their predictive value in preclinical research. We provide a comparative analysis of these models' abilities to maintain CSC populations, preserve tumor architecture, and predict clinical drug responses. The integration of these advanced models represents a transformative approach for drug development and personalized cancer therapy, enabling more accurate simulation of patient-specific tumor biology and treatment outcomes.
Tumor heterogeneity presents a fundamental obstacle in cancer treatment, contributing to variable therapeutic responses and eventual treatment failure. This diversity within tumors arises from genetic, epigenetic, and microenvironmental variations, with cancer stem cells (CSCs) serving as key regulators through their capacity for self-renewal and differentiation into multiple cell lineages [10]. CSCs not only initiate and maintain tumors but also drive metastasis and confer resistance to conventional therapies, making them critical targets for therapeutic development.
The emergence of sophisticated preclinical models has revolutionized our ability to study CSC biology and tumor heterogeneity. Patient-derived xenografts (PDXs), established by transplanting human tumor fragments into immunodeficient mice, preserve the original tumor's stromal components and cellular diversity [11] [12]. Conversely, patient-derived organoids (PDOs) are three-dimensional (3D) in vitro cultures that self-organize from stem cells—including CSCs—to recapitulate the structural and functional characteristics of original tumors [13] [10]. Both models offer distinct advantages for investigating CSC maintenance and functionality within heterogeneous tumor populations.
This review provides a comprehensive comparison of PDX and organoid models in their capacity to maintain tumor heterogeneity through CSC preservation. We evaluate their applications in drug screening, personalized medicine, and preclinical validation, highlighting how each model system captures different aspects of CSC biology. Understanding the strengths and limitations of these platforms is essential for advancing cancer research and developing more effective, heterogeneity-informed treatment strategies.
Fundamentals of Cancer Stem Cells and Tumor Heterogeneity
Biological Mechanisms of Cancer Stem Cells
CSCs constitute a small subpopulation within tumors that possess stem cell-like properties, including self-renewal capability, multipotency, and enhanced survival mechanisms. These cells drive tumor initiation, progression, and recurrence by generating diverse daughter cells through asymmetric division [10]. The CSC hypothesis posits that hierarchical organization exists within tumors, with CSCs at the apex maintaining the heterogeneous cellular composition of the malignancy.
CSCs reside in specialized microenvironmental niches that regulate their behavior through complex signaling networks. Key pathways involved in CSC maintenance include Wnt/β-catenin, Notch, Hedgehog, and EGFR-RAS-RAF-MAPK cascades [13] [12]. These pathways not only control CSC self-renewal and differentiation but also contribute to therapeutic resistance mechanisms. CSCs demonstrate enhanced DNA repair capacity, increased expression of drug efflux transporters, and resistance to apoptosis, making them particularly resilient to conventional chemotherapy and radiotherapy [14].
Technical Approaches for CSC Identification and Isolation
Several methodologies enable the identification and isolation of CSCs for experimental study:
- Cell Surface Marker Expression: Specific markers vary by cancer type but commonly include CD44, CD133, CD24, and epithelial-specific antigen (ESA) [10]. These markers facilitate CSC isolation via fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting for downstream applications.
- Functional Assays: The gold standard for CSC validation includes sphere-forming assays under non-adherent conditions, in vivo limiting dilution transplantation assays, and dye exclusion assays demonstrating side population phenotype via Hoechst 33342 efflux [14].
- Transcriptional Profiling: Detection of stemness-associated transcription factors such as OCT4, SOX2, NANOG, and MYC provides additional confirmation of CSC identity [10].
The successful maintenance of these CSC properties in experimental models is crucial for preserving tumor heterogeneity in preclinical studies.
Comparative Analysis of PDX and Organoid Models
Model Establishment and Technical Specifications
Table 1: Establishment Protocols and Success Rates for PDX and Organoid Models
| Parameter | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Source Material | Surgical specimens, biopsy fragments | Surgical specimens, biopsies, malignant effusions, circulating tumor cells |
| Establishment Time | 3-6 months | 2-8 weeks |
| Success Rate | Variable (15-80%, tumor-type dependent) | 70-90% for certain carcinomas [15] |
| Key Culture Components | Immunodeficient mice, Matrigel | Defined medium with growth factors (EGF, Noggin, R-spondin), extracellular matrix (Matrigel) [13] |
| Cost Considerations | High (animal maintenance, personnel) | Moderate (culture reagents, matrix) |
| Throughput Capacity | Low to moderate | High to very high |
Fidelity in Preserving Tumor Heterogeneity
Table 2: Model Performance in Capturing Tumor Heterogeneity and CSC Properties
| Feature | PDX Models | Organoid Models |
|---|---|---|
| Genetic Stability | High fidelity maintained over early passages, potential for mouse stromal replacement over time | High short-term genetic stability, clonal selection possible in long-term culture [13] |
| CSC Maintenance | Preserves native CSC niche and hierarchy | Maintains self-renewing capacity through culture conditions supporting stemness [10] |
| Cellular Heterogeneity | Recapitulates original tumor cellular diversity | Maintains intra-tumoral heterogeneity, though stromal components may be lost [11] |
| Microenvironment | Intact human stroma initially, gradually replaced by mouse stroma | Limited native microenvironment, requires co-culture systems for immune/stromal cells [13] |
| Histopathological Concordance | High architectural similarity to original tumor | Maintains histologic features but may lack organizational context [15] |
PDX models demonstrate superior preservation of the tumor microenvironment, including stromal components and vascular networks, which are crucial for maintaining CSC niches. A comparative study of ovarian clear cell carcinoma models found that PDX and PDTO models were able to recapitulate patient tumor heterogeneity, while cell lines failed to maintain this diversity [11]. This preservation extends to molecular characteristics, with PDXs maintaining genomic stability across passages when carefully managed.
Organoid models excel in maintaining epithelial heterogeneity and CSC functionality through specialized culture conditions. Lung cancer organoids derived from malignant serous effusions have demonstrated success rates exceeding 80% while faithfully reflecting the original sample's pathologic and genomic features [15]. These models can capture spatial and temporal heterogeneity, making them valuable for studying clonal evolution and CSC dynamics in response to therapeutic pressures.
Predictive Value in Drug Development and Personalized Medicine
Table 3: Predictive Performance in Preclinical and Clinical Applications
| Application | PDX Models | Organoid Models |
|---|---|---|
| Drug Screening | Moderate throughput, strong clinical correlation | High throughput, emerging clinical validation [15] [12] |
| Clinical Response Prediction | High concordance (85-90%) for certain cancer types | Promising results (80-90% concordance) in multiple studies [15] [11] |
| Therapeutic Timeline | Too slow for real-time clinical decisions (months) | Potentially clinically actionable timeframe (weeks) [15] |
| Personalized Medicine Applications | Limited by establishment time and cost | Promising for biobanking and individualized therapy testing [13] |
PDX models have established a strong track record in predicting clinical responses, particularly for targeted therapies. Their preservation of tumor-stroma interactions enables more accurate modeling of drug penetration and metabolism. However, the extended timeline for PDX establishment (3-6 months) often precludes their use in guiding first-line therapy decisions for individual patients.
Organoid models offer accelerated testing timelines compatible with clinical decision-making. A landmark study on lung cancer organoids demonstrated that LCO-based drug sensitivity tests (LCO-DSTs) accurately predict clinical response to both chemotherapy and targeted therapy in patients with advanced lung cancer [15]. Similarly, colorectal cancer organoids have shown high concordance with patient responses to standard chemotherapies like 5-FU and FOLFOX [12]. The scalability of organoid platforms enables high-throughput drug screening while maintaining patient-specific heterogeneity.
Experimental Protocols for CSC and Heterogeneity Analysis
Organoid Establishment from Patient Tumors
Sample Processing and Initiation:
- Sample Collection: Obtain tumor tissue via surgical resection, core needle biopsy, or malignant effusion (pleural, ascitic, or pericardial fluid) [15] [14]. Process within 1-2 hours of collection for optimal viability.
- Mechanical Dissociation: Mince tissue into 1-3 mm³ fragments using sterile surgical scissors or scalpels in cold Advanced DMEM/F12 medium.
- Enzymatic Digestion: Incubate tissue fragments with collagenase/hyaluronidase solution (e.g., Tumor Dissociation Kit, Miltenyi Biotec) at 37°C with agitation for 30 minutes to 2 hours based on tissue density [11] [14].
- Cell Separation: Pass digested suspension through 70-100 μm cell strainers to obtain single cells and small clusters. Centrifuge at 300-500 × g for 5 minutes and resuspend in organoid basal medium.
Organoid Culture and Maintenance:
- Matrix Embedding: Mix cell pellet with extracellular matrix (Matrigel, BME, or Geltrex) at appropriate dilution (typically 1:1 to 1:3 ratio). Plate 10-50 μL drops in pre-warmed culture plates and polymerize at 37°C for 20-30 minutes [14].
- Medium Formulation: Overlay with organoid culture medium containing essential supplements:
- Base Medium: Advanced DMEM/F12 with HEPES and GlutaMAX
- Growth Factors: EGF (50 ng/mL), FGF-10 (20 ng/mL), FGF-basic (1-10 ng/mL)
- Pathway Modulators: R-spondin (Wnt agonist), Noggin (BMP inhibitor), A-83-01 (TGF-β inhibitor)
- Additional Supplements: B27, N-Acetylcysteine, Nicotinamide, Prostaglandin E2
- ROCK Inhibitor: Y-27632 (10 μM) for initial 2-3 days to prevent anoikis [11] [14]
- Passaging: Dissociate mature organoids (7-21 days) using mechanical disruption or enzymatic treatment with TrypLE Express. Replate dissociated cells in fresh matrix at appropriate dilution (typically 1:3 to 1:10 split ratio).
PDX Establishment and Propagation
Initial Implantation:
- Sample Preparation: Process fresh tumor tissue within 1 hour of resection. Minimally dissect into 2-4 mm³ fragments in cold, serum-free medium preserving tissue architecture.
- Host Selection: Utilize immunocompromised mouse strains (NSG, NOG, or nude mice) aged 6-8 weeks. Anesthetize animals following institutional guidelines.
- Surgical Implantation: For subcutaneous models, create small dorsal incision and insert single tumor fragment into flank pocket. For orthotopic models, implant directly into corresponding organ of origin [11].
- Post-operative Care: Monitor animals for tumor growth, general health, and potential complications according to ethical guidelines.
Model Propagation and Cryopreservation:
- Passage Timing: Harvest tumors at 1000-1500 mm³ volume (typically 2-6 months post-implantation) to maintain exponential growth phase.
- Fragment Preparation: Aseptically process harvested tumor, removing necrotic areas. Prepare fragments as for initial implantation.
- Serial Passage: Implant prepared fragments into new host animals (typically 3-5 mice per line) to maintain model.
- Biobanking: Cryopreserve early passage fragments in DMSO/FBS solution using controlled-rate freezing for long-term storage in liquid nitrogen [11].
CSC Functional Assays in Model Systems
Sphere Formation Assay:
- Single-Cell Preparation: Dissociate PDX tumors or organoids to single-cell suspension using enzymatic digestion and mechanical disruption.
- Culture Conditions: Plate 500-10,000 viable cells/mL in ultra-low attachment plates with serum-free medium supplemented with EGF, bFGF, and B27.
- Quantification: Count spheres >50 μm after 7-21 days using inverted microscopy. Calculate sphere-forming efficiency as (number of spheres/number of cells seeded) × 100% [14].
In Vivo Limiting Dilution Assay:
- Cell Preparation: Generate single-cell suspensions from PDX or organoid models with confirmed viability >90%.
- Cell Dilutions: Prepare serial dilutions (e.g., 10,000, 1,000, 100, 10 cells) in PBS:Matrigel mixture (1:1).
- Implantation: Inject each dilution subcutaneously into immunocompromised mice (5-10 animals per dilution).
- Tumor Incidence Monitoring: Palpate weekly for 8-16 weeks for tumor formation. Calculate CSC frequency using extreme limiting dilution analysis (ELDA) software [10].
Drug Response Assays:
- Treatment Planning: Plate organoids or PDX-derived cells in 96-well format. Include viability controls and reference compounds.
- Compound Exposure: Add serially diluted therapeutics (typically 5-8 concentrations) after 24-72 hours of culture. Include vehicle controls.
- Endpoint Analysis: Assess viability after 5-7 days using CellTiter-Glo 3D or similar ATP-based assays. Calculate IC₅₀ values and generate dose-response curves [15] [11].
- Heterogeneity Assessment: Analyze single-cell responses via flow cytometry, imaging, or single-cell RNA sequencing to evaluate effects on CSC subpopulations.
Research Reagent Solutions for CSC and Heterogeneity Studies
Table 4: Essential Research Reagents for CSC and Tumor Heterogeneity Investigations
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Extracellular Matrices | Matrigel, BME, Cultrex, synthetic PEG hydrogels | 3D structural support for organoid growth and CSC niche maintenance [13] |
| Stem Cell Media Supplements | B27, N2, N-Acetylcysteine, Recombinant EGF, FGF, R-spondin, Noggin | Creation of stem cell-supportive culture conditions for CSC maintenance [13] [14] |
| Cell Dissociation Reagents | Collagenase/Hyaluronidase, TrypLE, Accutase, Dispase | Tissue processing and organoid passaging while preserving cell viability [11] [14] |
| CSC Marker Antibodies | Anti-CD44, Anti-CD133, Anti-CD24, Anti-ESA | Identification and isolation of CSC populations via FACS or immunofluorescence |
| Pathway Inhibitors | Y-27632 (ROCK inhibitor), A-83-01 (TGF-β inhibitor), LGK974 (Porcupine inhibitor) | Modulation of signaling pathways critical for CSC self-renewal and differentiation [11] [14] |
| Viability Assays | CellTiter-Glo 3D, MTS, CCK-8, Live-Dead staining | Assessment of treatment responses and CSC survival in heterogeneous cultures [15] [13] |
Signaling Pathways in Cancer Stem Cell Maintenance
Figure 1: Key signaling pathways regulating cancer stem cell maintenance and function. These pathways represent critical therapeutic targets for eliminating CSCs and overcoming tumor heterogeneity. The Wnt/β-catenin pathway promotes self-renewal and proliferation, while Notch signaling balances self-renewal with differentiation decisions. Hedgehog signaling influences both self-renewal and epithelial-mesenchymal transition (EMT), a process linked to metastatic potential. EGFR-RAS signaling drives proliferation and contributes to therapy resistance, while TGF-β-SMAD signaling regulates EMT and therapeutic resistance programs [13] [12] [10]. Successful CSC-targeted therapies must address these interconnected pathways to effectively combat tumor heterogeneity.
Future Perspectives and Concluding Remarks
The integration of PDX and organoid models represents a powerful approach for advancing CSC research and addressing tumor heterogeneity in drug development. While each model offers distinct advantages, their complementary applications provide a more comprehensive understanding of CSC biology. PDX models maintain physiological microenvironmental contexts crucial for CSC regulation, while organoid platforms enable scalable experimentation and rapid clinical translation.
Future directions in this field include the development of more sophisticated microenvironmental reconstitution in organoid systems through co-culture with immune cells, fibroblasts, and vascular components [13]. Additionally, the integration of multi-omics technologies with functional drug testing in these models will enhance our understanding of heterogeneity-driven treatment resistance. The emerging "Organoid Plus and Minus" framework, which combines technological augmentation with culture system refinement, shows promise for improving screening accuracy and physiological relevance [16].
Advanced engineering approaches such as microfluidic organ-on-chip platforms that incorporate fluid flow, mechanical forces, and multi-tissue interfaces offer exciting opportunities to model CSC niches more accurately [12]. These systems can potentially bridge the gap between simplified organoid cultures and complex in vivo PDX models. Furthermore, the application of artificial intelligence and machine learning to analyze heterogeneity patterns and predict drug responses across model systems will accelerate therapeutic discovery [16].
As these technologies evolve, standardization of culture protocols, validation across diverse cancer types, and establishment of large-scale biobanks will be critical for broader implementation. The ongoing refinement of PDX and organoid models promises to enhance their predictive value in clinical translation, ultimately enabling more effective targeting of CSCs and overcoming tumor heterogeneity in cancer treatment.
In conclusion, both PDX and organoid models provide invaluable tools for studying the critical role of CSCs in maintaining tumor heterogeneity. Their continued development and integration into drug discovery pipelines will facilitate the creation of more effective therapeutic strategies that address the fundamental challenges of cancer heterogeneity, moving us closer to personalized medicine approaches that can overcome treatment resistance and improve patient outcomes.
Patient-derived xenograft (PDX) and patient-derived organoid (PDO) models are foundational tools in precision oncology, enabling the study of tumor biology and the prediction of patient responses to therapy. A model's utility in both basic research and clinical decision-making hinges on its ability to faithfully recapitulate the histopathological and genomic complexity of the original patient tumor. This guide provides an objective, data-driven comparison of PDX and PDO models, evaluating their performance in retaining key tumor characteristics and their application in predictive drug response studies. The analysis is framed within the context of a broader thesis comparing the predictive value of these avatar models, providing researchers and drug development professionals with a clear overview of their respective strengths and limitations.
At a Glance: Comparing PDX and PDO Model Fidelity
The following table summarizes the core characteristics of PDX and PDO models, providing a high-level comparison of their performance in retaining original tumor features.
Table 1: Core Characteristics of PDX and PDO Models
| Characteristic | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Fundamental Principle | Implantation of human tumor tissue into immunocompromised mice [17] [7] | 3D in vitro culture of patient tumor cells in defined matrices [17] [18] |
| Histopathological Architecture | Retains original histological architecture and stromal components [7] [19] | Recapitulates key architectural and molecular features [20] [18] |
| Cellular Heterogeneity | Preserves clonal diversity and tumor heterogeneity [21] [22] | Maintains cellular heterogeneity of the original tumor [20] [23] |
| Tumor Microenvironment (TME) | Retains human tumor stroma and interacts with mouse host components; lacks human adaptive immune system [17] [21] | Lacks native vascular and complex stromal complexity; can be co-cultured with immune cells [17] [18] |
| Ethical & Financial Burden | High (extensive animal use, time-consuming, costly) [17] [24] | Lower (in vitro culture, amenable to high-throughput screening) [17] [24] |
| Key Limitation | Mouse-specific evolution and genetic drift over passages [17] [22] | Inability to model tumor-stroma and immune interactions natively [17] [18] |
Quantitative Fidelity Assessment: A Meta-Analysis Perspective
A recent systematic review and meta-analysis directly compared the performance of PDX and PDO models in predicting patient responses to anti-cancer therapy. The study analyzed 411 patient-model pairs (267 PDX, 144 PDO) from solid tumors. The quantitative findings are summarized below.
Table 2: Predictive Performance of PDX and PDO Models from Meta-Analysis
| Performance Metric | PDX Models | PDO Models | Overall Concordance |
|---|---|---|---|
| Overall Response Concordance | No significant difference from PDO | No significant difference from PDX | 70% [17] [24] |
| Sensitivity & Specificity | Comparable to PDO [24] | Comparable to PDX [24] | Not Specified |
| Predictive Value (PPV/NPV) | Comparable to PDO [24] | Comparable to PDX [24] | Not Specified |
| Association with Patient PFS | Association found only in low bias-risk pairs [17] | Patients with responding PDOs had prolonged PFS [17] | Not Applicable |
This comprehensive analysis suggests that PDOs perform similarly to PDX models in predicting matched-patient treatment response, while offering advantages in scalability and reduced ethical burden [17] [24].
Experimental Protocols for Model Establishment and Validation
To critically assess the data generated from these models, it is essential to understand their establishment and the rigorous validation processes required to confirm their fidelity.
Protocol for PDX Model Establishment
The following workflow outlines the typical process for creating and validating a PDX model, as demonstrated in studies on breast and pediatric solid tumors [19] [22].
Key Experimental Steps [19] [22]:
- Sample Collection & Preparation: Fresh tumor specimens are obtained from patients with informed consent. The tissue is transported in storage solution on ice, rinsed, and minced into small fragments (∼3–4 mm) under sterile conditions.
- Implantation: Tumor fragments are surgically implanted into immunocompromised mice (e.g., NOD-SCID or NSG strains). Implantation can be orthotopic (e.g., mammary fat pad for breast cancer) or subcutaneous.
- Monitoring and Passaging: Mice are monitored for tumor engraftment and growth. Upon reaching a predefined volume (e.g., 1000-1500 mm³), the tumor is harvested. A portion is cryopreserved for biobanking, and other fragments are serially passaged into new mice to expand the model, creating subsequent generations (G1, G2, etc.).
- Validation: Critical steps to confirm model fidelity include:
- Histopathology (H&E staining): To confirm retention of the original tumor's histological architecture.
- Immunohistochemistry (IHC): To validate the expression of key biomarkers (e.g., ER, PR, HER2 for breast cancer).
- Short Tandem Repeat (STR) Profiling: A DNA fingerprinting technique to genetically match the PDX tumor to the patient's original sample. Concordance rates are typically high, reported at 81.1%–100% in recent studies [19] [22].
- RNA Sequencing / RT-PCR: To confirm the presence of driver genetic alterations, such as fusion genes, with high fidelity (e.g., 92.6% retention in sarcoma PDXs) [22].
Protocol for PDO Model Establishment
The establishment of PDOs, particularly for challenging cancers like renal cell carcinoma (RCC) and brain tumors, involves a distinct in vitro process [20] [18].
Key Experimental Steps [20] [18]:
- Tissue Processing: Patient tumor samples are processed rapidly to maintain viability. The tissue is dissociated mechanically and/or enzymatically to create a cell suspension or small cell clusters.
- 3D Culture: The dissociated cells are embedded in an extracellular matrix substitute (e.g., Matrigel, Geltrex), which provides a scaffold for 3D growth.
- Defined Culture Media: The embedded cells are cultured in a specialized, defined medium. The composition of this medium is critical and often needs to be optimized for specific cancer subtypes to support the growth of tumor cells while suppressing the outgrowth of normal cells. For example, RCC organoids may require specific growth factor combinations [18].
- Expansion and Maintenance: Organoids are allowed to grow and are periodically passaged by mechanically breaking them up and re-embedding the fragments into new matrix.
- Validation: Similar to PDX, PDOs are rigorously validated using:
- Histology and IHC: To demonstrate recapitulation of tumor morphology and protein marker expression.
- Genomic/Transcriptomic Analysis: Whole-exome sequencing, RNA sequencing, and single-cell RNA sequencing (scRNA-seq) are used to confirm that organoids retain the molecular features, heterogeneity, and gene expression profiles of the parent tumor [20] [23].
The Scientist's Toolkit: Essential Research Reagents
The successful establishment and application of PDX and PDO models rely on a suite of specialized reagents and materials. The following table details key solutions used in the featured experiments.
Table 3: Essential Reagents for PDX and PDO Research
| Research Reagent | Function | Application Context |
|---|---|---|
| Immunocompromised Mice (e.g., NOD-SCID, NSG) | In vivo hosts that allow engraftment and growth of human tumor tissue without immune rejection. | PDX Model Establishment [19] [22] |
| Extracellular Matrix (e.g., Matrigel, Geltrex) | Provides a 3D scaffold that supports cell polarization, self-organization, and survival of organoids. | PDO Model Establishment [20] [18] |
| Defined Culture Media & Growth Factors | A chemically defined cocktail of nutrients, hormones, and growth factors that selectively supports the growth of tumor epithelial cells. | PDO Model Establishment & Maintenance [18] |
| Short Tandem Repeat (STR) Profiling Kit | A molecular biology tool that amplifies specific genomic loci to create a DNA "fingerprint" for authenticating human origin and matching models to patient samples. | PDX & PDO Model Validation [19] [22] |
| EnVision FLEX Mini Kit (Dako) | A standardized immunohistochemistry (IHC) detection system used to visualize specific protein biomarkers (e.g., ER, HER2) in formalin-fixed tumor sections. | Histopathological Validation [19] |
Analysis of Histopathological and Genomic Retention
Performance Across Tumor Types
The success and fidelity of these models can vary significantly depending on the cancer type and subtype.
- PDX Engraftment Efficiency: A study establishing a pediatric solid tumor PDX biobank reported an overall success rate of 44.35% across 124 samples. Engraftment was notably higher for sarcomas (e.g., osteosarcoma, Ewing sarcoma) at >55%, while central nervous system (CNS) tumors had lower success rates, reflecting their unique microenvironmental requirements [22]. For treatment-resistant HR+/HER2- breast cancer, the median time for a palpable G0 PDX was 100 days, highlighting the slow growth of some subtypes [19].
- PDO Culture Success and Challenges: The establishment efficiency of PDOs is highly subtype-dependent. While protocols for cancers like colorectal and breast have been optimized, modeling renal cell carcinoma (RCC) presents specific hurdles. Clear cell RCC (ccRCC) organoids are more readily established, whereas papillary and particularly chromophobe RCC (chRCC) prove much more difficult due to molecular features that impair proliferative capacity and structural integrity in vitro [18].
Limitations and Drift
A critical consideration for both platforms is their potential deviation from the original tumor over time.
- Genetic Drift in PDX: While PDX models show high initial concordance, serial passaging can lead to changes. Second-generation PDX tumors often show faster growth, suggesting a selective adaptation to the murine host [22]. Sporadic discrepancies, such as the emergence of new fusion genes or the outgrowth of murine lymphoproliferative cells, have been observed, underscoring the necessity for ongoing molecular validation [19] [22].
- Phenotypic Instability in PDO: PDOs can experience "phenotypic drift" in long-term culture, where the cellular composition and molecular characteristics may gradually shift away from the original tumor. Furthermore, the absence of a native tumor microenvironment (TME)—including blood vessels, cancer-associated fibroblasts, and immune cells—remains a fundamental limitation for studying therapies that target these components, such as immunotherapies and anti-angiogenic drugs [17] [18]. Advanced co-culture systems are being developed to bridge this gap.
Overcoming the Limitations of Traditional 2D Cell Lines and CDX Models
For decades, cancer research has relied on traditional two-dimensional (2D) cell cultures and cell line-derived xenograft (CDX) models for drug discovery. However, their limited clinical predictive power has constrained progress. This guide compares two advanced, patient-derived models—Patient-Derived Xenografts (PDX) and Patient-Derived Organoids (PDO)—that are overcoming these limitations by better preserving the biological complexity of human tumors.
The table below provides a high-level comparison of the key characteristics of 2D, CDX, PDX, and PDO models to help researchers select the appropriate tool for their investigations [25] [26].
| Feature | Traditional 2D Cell Lines / CDX | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|---|
| Basis of Model | Immortalized, clonal cell lines [27] | Tumor tissue implanted directly into mice [1] | Tumor cells cultured as 3D structures in vitro [25] |
| Tumor Microenvironment | Poor; lacks stromal and immune components [1] | High; retains human stroma initially, replaced by mouse cells over time [1] | Moderate; can include some epithelial components, but lacks vascular and immune systems [17] |
| Intratumor Heterogeneity | Low (clonal) [28] | High (preserves patient tumor heterogeneity) [28] | Moderate to High (preserves cellular heterogeneity) [25] |
| Clinical Predictive Value | Low; high attrition rates in drug development [1] | High; demonstrated significant concordance with patient responses [17] [1] | High; performance similar to PDX in predicting patient response [17] |
| Throughput & Scalability | High (for 2D); Moderate (for CDX) | Low; time-consuming and resource-intensive [25] | High; amenable to high-throughput drug screening [17] [26] |
| Timeline & Cost | Low cost, rapid results | Long timeline (months), high cost [25] | Moderate timeline (weeks), lower cost than PDX [17] [25] |
| Key Advantages | Cost-effective, scalable, standardized | Retains in vivo biology and tumor architecture, gold standard for preclinical studies [1] | Cost-effective, high-throughput, retains patient-specific genetics, ethical advantages [17] |
| Primary Limitations | Genomically simplified, poor clinical translation [27] [1] | Low engraftment rates for some cancers, use of immunocompromised hosts, ethical concerns [25] | Lacks full tumor microenvironment, cannot model immune therapies or pharmacokinetics [17] |
Quantitative Predictive Performance Data
A systematic review and meta-analysis directly comparing the predictive accuracy of PDX and PDO models provides critical performance metrics. The analysis, which included 411 patient-model pairs (267 PDX, 144 PDO) from solid tumors, found that the overall concordance in treatment response between patients and matched models was 70%, with no significant differences in performance between PDX and PDO models [17].
The table below summarizes the detailed performance characteristics [17]:
| Metric | PDX Performance | PDO Performance | Notes |
|---|---|---|---|
| Overall Concordance | ~70% | ~70% | No statistically significant difference found between models [17]. |
| Sensitivity & Specificity | Comparable to PDO | Comparable to PDX | Values were comparable between the two model types [17]. |
| Positive Predictive Value (PPV) | Comparable to PDO | Comparable to PDX | PPV for organoid-informed treatment in colorectal cancer was 68% [29]. |
| Negative Predictive Value (NPV) | Comparable to PDO | Comparable to PDX | NPV for organoid-informed treatment in colorectal cancer was 78% [29]. |
| Association with Patient Survival | Significant | Significant | Patients whose matched PDOs responded to therapy had prolonged progression-free survival (PFS). For PDX, this association was strong in studies with low risk of bias [17]. |
Experimental Workflows and Protocols
PDX Model Establishment and Drug Trials
The following diagram illustrates the multi-generational process of establishing and utilizing PDX models for drug testing.
Key Methodological Steps for PDX Models [1]:
- Sample Acquisition and Implantation: Fresh tumor tissues from surgical resections or biopsies are collected and cut into small fragments (approx. 2-3 mm³). These fragments are implanted into immunocompromised mice (e.g., NOD-SCID, NSG) via subcutaneous, orthotopic, or renal capsule routes.
- Engraftment and Passage: Engrafted tumors are grown to a volume of 1-2 cm³, constituting the first generation (P0 or F1). The tumor is then harvested, divided, and re-implanted into new mice to create subsequent generations (P1, P2, etc.). The time for establishment varies from weeks to months.
- Characterization: PDX models must be validated to confirm they retain the histological architecture and molecular features (e.g., via DNA/RNA sequencing, IHC) of the original patient tumor.
- Drug Efficacy Studies: cohorts of mice bearing specific PDX models are treated with vehicle control or the investigational drug(s). Drug response is typically monitored by measuring tumor volume over time. A key advantage is the ability to create "Mouse Clinical Trials" or "Patient-Derived Clinical Trials" by testing a single drug across a large panel of different PDX models to mimic population-level response variability [1].
PDO Culture and High-Throughput Screening
The workflow for establishing and using PDOs for drug screening is outlined below.
Key Methodological Steps for PDO Models [25] [10]:
- Tissue Processing: Patient tumor samples are minced and digested with enzymes (e.g., collagenase) to create a single-cell suspension or small cell clusters.
- 3D Culture Setup: The cell suspension is mixed with a basement membrane extract (BME) like Matrigel, which provides a 3D scaffold. This mixture is plated and allowed to solidify.
- Defined Culture Medium: Organoids are cultured in a specialized, defined medium that varies by tumor type. Key additives often include:
- Growth Factors: EGF (Epidermal Growth Factor) to promote proliferation.
- Wnt Agonists: R-spondin to support stem cell function.
- BMP Inhibitors: Noggin to prevent differentiation.
- Other Pathway Modulators: such as A83-01 (a TGF-β inhibitor).
- Drug Screening: Expanded organoids are dissociated and re-plated in 384-well plates for high-throughput screening. After treatment with compound libraries, viability is measured using assays like ATP-based CellTiter-Glo. A sensitivity threshold (e.g., IC50) is applied to classify tumors as sensitive or resistant [29].
The Scientist's Toolkit: Essential Research Reagents
The table below details key reagents and their functions essential for establishing and maintaining PDX and PDO models.
| Reagent / Material | Function in PDX Models | Function in PDO Models |
|---|---|---|
| Immunocompromised Mice (e.g., NOD-SCID, NSG) | Essential in vivo host; prevents rejection of human tumor implant [1]. | Not Applicable |
| Basement Membrane Extract (BME/Matrigel) | Not typically used for initial implantation. | Critical 3D scaffold that provides structural support and mimics the extracellular matrix [25]. |
| R-spondin | Not a standard reagent. | Key growth factor in culture medium; agonist of Wnt signaling crucial for stem cell maintenance [10]. |
| Noggin | Not a standard reagent. | Key growth factor; inhibits BMP signaling to prevent differentiation of stem/progenitor cells [10]. |
| EGF (Epidermal Growth Factor) | Not a standard reagent. | Promotes cell proliferation and survival in the organoid culture medium [10]. |
| A83-01 (TGF-β Inhibitor) | Not a standard reagent. | Added to culture medium to inhibit TGF-β signaling, which can otherwise suppress growth and induce differentiation [25]. |
PDX and PDO models have moved beyond the limitations of traditional 2D and CDX systems, offering a more physiologically relevant and clinically predictive platform for oncology research. The choice between them is not a matter of which is universally better, but which is more appropriate for the specific research question.
- PDX models are the preferred choice for studying complex in vivo interactions, including tumor-stroma crosstalk, metastasis, and pharmacokinetics/pharmacodynamics (PK/PD), and for the final, most clinically relevant validation of therapeutic efficacy prior to human trials [1] [26].
- PDO models excel in applications requiring scale and speed, such as high-throughput drug screening, personalized medicine approaches, and genetic manipulation, offering a more ethical and cost-effective system [17] [30].
An integrated approach, using PDOs for large-scale initial screening followed by validation of top hits in PDX models, leverages the strengths of both platforms and represents a powerful strategy for accelerating the development of novel cancer therapeutics.
Patient-derived models have revolutionized cancer research by providing more physiologically relevant tools for studying tumor biology and treatment response. The two most prominent models in modern oncology are patient-derived xenografts (PDX), which involve transplanting human tumor tissue into immunocompromised mice, and patient-derived organoids (PDO), which are three-dimensional in vitro cultures derived from patient tumors [17] [11]. Both models have significantly advanced beyond traditional two-dimensional cell lines, which lack the structural architecture and cellular diversity of human tumors [31] [32]. This guide provides a comprehensive comparison of PDX and PDO models across the research spectrum, from fundamental biological investigation to clinical treatment personalization, empowering researchers to select the optimal model for their specific applications.
Model Foundations and Technical Specifications
Fundamental Characteristics and Working Principles
Patient-Derived Xenografts (PDX) are established by directly implanting fresh human tumor fragments into immunocompromised mouse hosts. These models maintain much of the original tumor's histological architecture and cellular heterogeneity while interacting with mouse stromal components [17]. PDX models require extensive use of animals, typically employing highly immunocompromised strains like NOD-SCID-IL2Rγnull (NSG) mice to improve engraftment rates [33]. The in vivo environment allows for preservation of some tumor-stroma interactions and provides a system for studying metastasis and systemic drug effects [7] [34].
Patient-Derived Organoids (PDO) are generated by embedding dissociated tumor cells in a basement membrane matrix and culturing them in specialized media containing growth factors and signaling pathway inhibitors [11] [8]. This approach recapitulates key architectural and molecular features of the original tumor in a three-dimensional in vitro system that can be rapidly expanded and maintained long-term [8]. However, PDO models typically lack the vascular and stromal complexity of in vivo systems, limiting their application for studying tumor-microenvironment interactions unless co-culture systems are implemented [17] [35].
Comparative Technical Specifications
Table 1: Technical comparison between PDX and PDO models
| Parameter | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Foundation | In vivo implantation in immunocompromised mice | 3D in vitro culture in extracellular matrix |
| Time to Establishment | 3-6 months | 2-8 weeks |
| Success Rates | Variable (10-80%) depending on cancer type | Generally higher across tumor types |
| Cost Considerations | High (animal maintenance, ethical costs) | Moderate (specialized media, matrices) |
| Scalability | Low to moderate | High (amenable to HTS) |
| Throughput | Low | High |
| Genetic Stability | Maintained over early passages | Generally high with defined protocols |
| Tumor Microenvironment | Partial (mouse stroma, human tumor) | Limited (can be enhanced with co-cultures) |
| Key Advantages | Preserves tumor architecture, in vivo context | Scalable, cost-effective, high clinical predictivity |
| Primary Limitations | Time-consuming, expensive, ethical considerations | Limited microenvironment, may miss systemic effects |
Predictive Performance and Validation
Concordance with Clinical Responses
Recent meta-analyses have systematically evaluated the predictive accuracy of both models. A comprehensive assessment of 411 patient-model pairs (267 PDX, 144 PDO) across solid tumors demonstrated 70% overall concordance in treatment response between patients and matched models, with no statistically significant differences between PDX and PDO models [17]. Sensitivity, specificity, positive predictive value, and negative predictive value were all comparable between the two platforms, suggesting similar capability for predicting both responsive and non-responsive clinical scenarios.
Evidence from specific cancer types reinforces these findings. In ovarian clear cell carcinoma, both PDX and PDO models accurately recapitulated the patient's clinical resistance to carboplatin, doxorubicin, and gemcitabine, while traditional 2D cell lines showed sensitivity to these same agents [11]. Similarly, in prostate cancer, PDX models and their derived organoids maintained transcriptomic and genomic similarity to primary tumors and demonstrated differential drug sensitivities that aligned with clinical expectations [34].
Survival Correlation and Clinical Relevance
The association between model responses and patient outcomes provides critical validation for both platforms. Patients whose matched PDOs responded to therapy showed significantly prolonged progression-free survival in clinical follow-up [17]. For PDX models, this association held true only when analyses were restricted to patient-model pairs with low risk of bias after rigorous quality assessment, highlighting the importance of methodological standardization in predictive modeling.
Table 2: Predictive performance metrics across cancer types
| Cancer Type | Model | Concordance with Patient Response | Key Findings | Reference |
|---|---|---|---|---|
| Multiple Solid Tumors | PDX | 70% overall | Predictive accuracy similar between platforms | [17] |
| Multiple Solid Tumors | PDO | 70% overall | Association with patient PFS established | [17] |
| Ovarian Clear Cell | PDX | High | Recapitulated clinical resistance to carboplatin/doxorubicin/gemcitabine | [11] |
| Ovarian Clear Cell | PDO | High | Identified HDAC inhibitor belinostat as potentially effective | [11] |
| Prostate Cancer | PDX | High | Androgen-dependent responses mirrored clinical behavior | [34] |
| Gastric Cancer | Both | High | Models informed personalized treatment strategies | [33] |
Experimental Workflows and Methodologies
Model Establishment and Validation Protocols
PDX Establishment Protocol:
- Tumor Processing: Fresh tumor tissue is collected sterilely and cut into 3-5 mm³ fragments in cold preservation medium
- Implantation: Fragments are implanted subcutaneously (typically scapular region) or orthotopically into anesthetized immunocompromised mice
- Monitoring: Tumor growth is measured twice weekly until reaching 800-1000 mm³
- Passaging: Tumors are harvested, with portions used for analysis and serial transplantation into new mouse cohorts
- Validation: Histological comparison (H&E staining), genomic verification (DNA fingerprinting), and molecular characterization confirm fidelity to original tumor [11] [34]
PDO Establishment Protocol:
- Tissue Dissociation: Tumor tissue is dissociated using enzymatic kits (e.g., Tumor Dissociation Kit, Miltenyi Biotec) and mechanical disruption
- Matrix Embedding: Cells are resuspended in basement membrane extract (e.g., Matrigel) and plated as domes
- Specialized Media Culture: Cultures are maintained in organoid basal medium supplemented with niche factors (B27, N-acetylcysteine, EGF, FGF, ROCK inhibitor Y27632)
- Expansion: Organoids are passaged every 1-3 weeks through mechanical/ enzymatic dissociation and re-embedding
- Validation: Morphological assessment, lineage markers by immunofluorescence, and genomic profiling verify representation of original tumor [11] [8]
Drug Screening Methodologies
PDX Drug Testing Workflow:
- Cohort Design: Mice bearing passage 3-5 PDX tumors are randomized into treatment groups when tumors reach 150-200 mm³
- Dosing Regimen: Compounds are administered via clinically relevant routes (oral gavage, intraperitoneal injection) at mouse-equivalent doses of human treatments
- Response Monitoring: Tumor volumes and mouse weights are tracked 2-3 times weekly
- Endpoint Analysis: Tumors are harvested for molecular and histological analysis when control tumors reach endpoint volume [34] [33]
PDO Drug Screening Workflow:
- Platform Preparation: Organoids are dissociated into single cells or small clusters and seeded in 384-well plates
- Compound Exposure: Libraries of FDA-approved or investigational compounds are transferred via automated liquid handling
- Viability Assessment: Cell viability is quantified after 5-7 days using ATP-based, resazurin, or imaging-based assays
- Dose-Response Analysis: Multi-concentration testing generates IC₅₀ values and response classifications [11] [35]
Research Applications Across the Discovery-Clinical Spectrum
Basic Cancer Biology Applications
Both PDX and PDO models have become indispensable tools for investigating fundamental cancer processes. PDX models excel in studying tumor-stroma interactions, metastatic cascades, and systemic signaling due to their preserved tissue architecture and in vivo context [7] [34]. The mouse microenvironment, while not human, provides physiological cues that influence tumor behavior and evolution. Researchers have leveraged PDX models to map clonal evolution during treatment and identify microenvironment-driven resistance mechanisms.
PDO platforms offer distinct advantages for deconstructing tumor-intrinsic signaling pathways, mapping heterogeneity, and performing genetic screens [8]. The tractability of organoid systems enables precise manipulation of signaling pathways through media supplementation with growth factors and small molecule inhibitors. PDO biobanks representing molecularly annotated tumors have proven valuable for associating genetic alterations with phenotypic behaviors and identifying subtype-specific vulnerabilities.
Preclinical Drug Development Applications
In drug discovery, PDX models serve as the gold standard for in vivo efficacy assessment prior to clinical trials [7] [33]. Their conservation of tumor heterogeneity and pathophysiology provides critical insights into compound pharmacokinetics, pharmacodynamics, and therapeutic indices. PDX trials—where cohorts of models representing molecular subtypes are treated with investigational agents—help stratify patient populations most likely to respond and identify potential resistance mechanisms.
PDO systems enable unprecedented scalability in drug screening, with platforms routinely testing hundreds of compounds across large organoid panels [8] [35]. This high-throughput capacity is particularly valuable for combination therapy discovery, where testing thousands of drug pairs would be prohibitively expensive in vivo. PDO screens have successfully identified novel therapeutic candidates, including a bispecific antibody triggering EGFR degradation specifically in LGR5+ cancer stem cells, later validated in matched PDX models [35].
Functional Precision Medicine Applications
The most transformative application of both platforms lies in functional precision medicine, where models guide individual patient treatment decisions. Multiple studies have demonstrated that ex vivo drug sensitivity testing in PDOs can predict clinical response with high accuracy [11] [36]. The faster turnaround time of PDO screens (2-4 weeks versus 3-6 months for PDX) makes them more feasible for clinical decision support, particularly in advanced disease where treatment choices are time-sensitive.
PDX models still play important roles in addressing specific clinical questions, particularly for immunotherapies and complex microenvironment interactions not recapitulated in PDO cultures [33]. Humanized PDX models—where immunodeficient mice are engrafted with human immune systems—enable evaluation of checkpoint inhibitors and other immunomodulatory agents. For targeted therapies where microenvironment influence is less critical, PDOs provide a more scalable and cost-effective predictive tool.
Table 3: Application-specific recommendations and considerations
| Research Application | Recommended Model | Key Advantages | Important Limitations |
|---|---|---|---|
| Targeted Therapy Screening | PDO | High-throughput capacity, genetic annotation | May miss paracrine signaling effects |
| Immunotherapy Assessment | Humanized PDX | Functional human immune system | Technically challenging, variable reconstitution |
| Metastasis Studies | PDX | Preserved invasion and colonization programs | Mouse stroma may not fully mimic human niche |
| Tumor Heterogeneity Analysis | Both | Maintain parental tumor diversity | Selection pressures may alter representation |
| Functional Precision Medicine | PDO (primary), PDX (validation) | Clinical turnaround (PDO), in vivo validation (PDX) | Establishment failure for some tumor types |
| Mechanistic Pathway Studies | PDO | Genetic manipulation, signaling dissection | Lack of systemic regulation |
| Co-clinical Trials | PDX | Parallel treatment with patients | Time and resource intensive |
Essential Research Reagents and Solutions
Successful implementation of PDX and PDO platforms requires specialized reagents and materials. The following table details key solutions used in model establishment and maintenance.
Table 4: Essential research reagents and solutions for PDX and PDO workflows
| Reagent Category | Specific Examples | Function | Model Application |
|---|---|---|---|
| Immunocompromised Mice | NOD-scid-IL2Rγnull (NSG), NOG | Host organisms for PDX engraftment | PDX |
| Basement Membrane Matrix | Matrigel, BME-2 | 3D scaffold for organoid growth | PDO |
| Dissociation Reagents | Tumor Dissociation Kit (Miltenyi), collagenase | Tissue processing into single cells | Both |
| Specialized Media Supplements | B27, N-acetylcysteine, nicotinamide | Support stem cell maintenance | PDO |
| Growth Factors | EGF, FGF-10, FGF-basic, Noggin | Mimic niche signaling pathways | PDO |
| Signaling Inhibitors | A-83-01 (TGF-β inhibitor), Y27632 (ROCK inhibitor) | Prevent differentiation and apoptosis | PDO |
| Validation Reagents | Species-specific antibodies, PCR panels | Confirm human origin and contamination | Both |
| Cryopreservation Media | DMSO/FBS solutions | Long-term model biobanking | Both |
Integrated Workflows and Future Directions
The complementary strengths of PDX and PDO models have inspired integrated workflows that leverage both platforms throughout the drug discovery pipeline. A common strategy employs PDO screens for high-throughput compound identification followed by PDX models for in vivo validation of prioritized hits [35]. This approach balances efficiency with physiological relevance, accelerating the development of promising therapeutic candidates.
Emerging technologies are addressing current limitations of both platforms. For PDO models, microfluidic organ-on-chip systems and co-culture methods are incorporating immune cells, fibroblasts, and endothelial cells to better mimic tumor microenvironment complexities [8] [36]. For PDX models, humanized mouse strains with improved human immune system reconstitution are enabling more accurate evaluation of immunotherapies [33]. Both model systems are increasingly being paired with computational approaches, including machine learning algorithms that predict drug response based on molecular features combined with functional data.
The evolution of these platforms continues to enhance their translational impact. As biobanks expand to encompass broader tumor diversity and protocols standardize across laboratories, PDX and PDO models will play increasingly central roles in bridging basic cancer biology with personalized clinical care, ultimately improving outcomes for cancer patients through more precise and effective therapeutic strategies.
Practical Implementation: Establishment Protocols and Translational Applications in Drug Discovery
In the evolving landscape of precision oncology, patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as indispensable "patient avatar" systems for preclinical research and therapeutic prediction. These models represent a paradigm shift from genomics-based medicine toward functional precision medicine, which evaluates therapeutic efficacy by directly treating living patient tumors ex vivo to better predict patient-specific responses [36]. While both model types aim to bridge the gap between traditional preclinical models and human clinical response, they offer distinct advantages and limitations in terms of predictive accuracy, establishment complexity, cost, and ethical considerations [17] [26].
A recent comprehensive meta-analysis comparing these avatar systems revealed no significant difference in overall predictive performance, with both models demonstrating approximately 70% concordance with patient treatment responses [17]. This comparative guide provides an objective, data-driven analysis of PDX and PDO model establishment, from initial tissue acquisition through functional assay implementation, empowering researchers to select the most appropriate model system for their specific research applications.
Model Establishment: Comparative Workflows
Tissue Acquisition and Sample Preparation
The initial phase of model establishment requires careful consideration of sample source and preparation techniques, which vary significantly between PDX and PDO approaches.
PDX Models typically utilize surgically resected tumor fragments, preferably within 2 hours of resection to maintain tissue viability [36]. Both primary and metastatic tumor sites can serve as source material, with the transplantation success rate heavily influenced by tumor type and grade [7] [36].
PDO Models offer more diverse sampling options, including:
- Surgical specimens from endoscopic biopsies or resection specimens [14]
- Minimally invasive sources such as pleural effusions, bronchoalveolar lavage fluid, ascites, urine, and peripheral blood [14]
- Existing models including PDX tissues or established cell lines [14]
The preparation of PDO samples involves meticulous mechanical disruption using scalpels, followed by enzymatic digestion with collagenase/hyaluronidase and TrypLE Express enzymes appropriate for the specific tumor type [14]. For digestions exceeding 2 hours, adding a ROCK inhibitor (10 µM) improves growth efficiency by enhancing cell survival [14].
Table: Sample Acquisition and Preparation Requirements
| Parameter | PDX Models | PDO Models |
|---|---|---|
| Primary Sample Sources | Surgical resection fragments [36] | Surgical specimens, body fluids, existing models [14] |
| Time to Processing | <2 hours preferred [36] | 4 hours from sample to culture [37] |
| Preparation Methods | Minced tissue fragments [36] | Mechanical chopping, enzymatic digestion [14] [37] |
| Critical Reagents | Storage media for transport [36] | Collagenase/hyaluronidase, TrypLE Express, ROCK inhibitor [14] |
| Sample Volume Requirements | Millimeter-scale tissue fragments [36] | Small biopsies (1-3 mm³) or milliliter-scale fluids [14] [37] |
Core Establishment Protocols
The fundamental divergence in model establishment occurs after sample preparation, with PDX models requiring in vivo engraftment and PDO models utilizing three-dimensional in vitro culture systems.
PDX Establishment Protocol
The establishment of PDX models involves implanting prepared tumor tissue into immunocompromised mice, which can be achieved through several methodological approaches:
- Host Selection: Immunocompromised mice (e.g., NSG, nude strains) serve as hosts to prevent graft rejection [7].
- Implantation Methods:
- Monitoring and Passaging: Tumor growth is monitored regularly, with successful engraftments serially passaged to expand model numbers [38].
The successful construction rate of PDX models varies significantly by cancer type and is influenced by factors such as tumor grade, aggressiveness, and stromal content [7] [36].
PDO Establishment Protocol
The establishment of PDO models centers on creating a supportive three-dimensional environment that promotes stem cell maintenance and self-organization:
- Extracellular Matrix (ECM) Embedding: The digested cell pellets or tissue fragments are resuspended in a gelatinous protein mixture such as Matrigel, BME, or Geltrex [14] [37]. These hydrogels provide crucial growth factors and structural support for three-dimensional development.
- Plating Technique: The cell-ECM mixture is plated as small drops (10-20 μL) onto multi-well plates, typically using 98-, 48-, or 24-well formats [14]. The plates are inverted during incubation at 37°C for 15-30 minutes to prevent cell settling and promote hemispherical 3D structure formation.
- Culture Initiation: After ECM solidification, organoid-specific culture medium is added, and plates are maintained at 37°C with 5% CO₂ [37]. The liquid feed is renewed every few days, with organoids typically developing within approximately 2 weeks [37].
The PDO establishment process from tissue receipt to culture incubation takes approximately 4 hours of active processing time [37].
Model Expansion and Maintenance
Long-term model propagation requires specialized techniques for both PDX and PDO systems.
PDX Maintenance relies on serial passaging in mice, where established tumors are harvested and re-implanted into new host animals. The Mayo Clinic Brain Tumor PDX National Resource and similar facilities provide standardized protocols for these processes, including in vitro culture techniques for specific PDX lines [38].
PDO Expansion utilizes a subculture process called "passaging":
- Matrix Dissolution: The Matrigel surrounding organoids is dissolved using specific buffers [37].
- Organoid Dissociation: Organoids are broken apart either mechanically (pipetting through narrow openings) or chemically using enzyme solutions [37].
- Re-plating: The resulting cell clusters are centrifuged, resuspended in fresh Matrigel, and cultured as in the initial establishment [37].
This passaging process can be repeated multiple times, generating substantial material for research applications. For large-scale needs, semi-automated bioprocess technology has been developed to produce standardized PDOs with reduced batch-to-batch variability [37].
Functional Assays and Predictive Value Assessment
Drug Treatment and Response Assessment
The ultimate validation of both PDX and PDO models lies in their ability to accurately predict patient responses to therapeutic agents.
Treatment Protocol Design requires careful attention to dosing strategies. For PDX models, when multiple doses are tested, the closest murine equivalent of the clinical dose should be selected using established conversion methods [17]. For both models, the route of administration should mirror the clinical approach whenever possible [17].
Response Assessment methodologies differ between models:
- PDX Response: Typically measured by tumor volume reduction in vivo, often using caliper measurements or imaging [17]
- PDO Response: Assessed through viability assays (e.g., CellTiter-Glo), morphology changes, or functional readouts in vitro [8]
The meta-analysis of 411 patient-model pairs demonstrated that patients whose matched PDOs responded to therapy had significantly prolonged progression-free survival [17]. For PDX models, this association was statistically significant only when analyses were restricted to patient-model pairs with low risk of bias [17].
Predictive Performance Metrics
The comprehensive meta-analysis of 267 PDX and 144 PDO pairs from solid tumors treated with identical anti-cancer agents as matched patients provides robust comparative data on model predictive performance [17].
Table: Predictive Performance Metrics from Meta-Analysis
| Performance Metric | PDX Models | PDO Models | Statistical Significance |
|---|---|---|---|
| Overall Concordance | 70% | 70% | Not significant [17] |
| Sensitivity | Comparable | Comparable | Not significant [17] |
| Specificity | Comparable | Comparable | Not significant [17] |
| Positive Predictive Value | Comparable | Comparable | Not significant [17] |
| Negative Predictive Value | Comparable | Comparable | Not significant [17] |
| Association with Patient PFS | Significant only in low-bias pairs [17] | Significant association [17] | - |
Technical Considerations and Quality Control
Quality Assessment and Validation
Robust quality control measures are essential for ensuring model fidelity and predictive reliability. A standardized risk of bias assessment tool adapted from the Newcastle-Ottawa scale has been developed for this purpose, encompassing six key criteria [17]:
- Selection Bias Assessment: Evaluation of whether the paper included treatment responses from all PDX or PDO-matched patient pairs from the modeling project
- Origin Validation: Verification that models were successfully validated to originate from matching human tissue through DNA, RNA, protein-based assays, or histology
- Outcome Objectivity: Determination of whether patient response was assessed using RECIST criteria and model response data was obtained objectively
- Follow-up Adequacy: Assessment of whether patient follow-up was sufficiently long for meaningful survival evaluation (≥6 months or until earlier death)
- Reporting Sufficiency: Evaluation of comprehensive reporting including matching administration routes, dosing regimens, and previous treatment lines
- Technical Replicates: Verification that at least n=3 replicates were used for PDX or PDO experiments
Patient-model pairs meeting ≥4 of these criteria are classified as high reliability (low risk of bias), while those meeting ≤3 criteria are considered low reliability (high risk of bias) [17].
The Research Toolkit: Essential Reagents and Materials
Successful model establishment and maintenance require specific, specialized reagents and materials that constitute the essential research toolkit for both PDX and PDO workflows.
Table: Essential Research Reagent Solutions for Model Establishment
| Reagent/Material | Function | Application |
|---|---|---|
| Matrigel/BME/Geltrex | Extracellular matrix hydrogel providing structural support and growth factors for 3D development [14] [37] | PDO Establishment |
| Collagenase/Hyaluronidase | Enzyme cocktail for tissue digestion and cell cluster isolation [14] | PDO Sample Preparation |
| TrypLE Express | Enzyme solution for further dissociation of cell clusters [14] | PDO Sample Preparation |
| ROCK Inhibitor (Y-27632) | Enhances cell survival during digestion and early culture stages [14] | PDO Establishment |
| Organoid Culture Media | Specialized media containing nutrients and growth factors (e.g., R-spondins, Noggin) [39] | PDO Maintenance |
| Immunocompromised Mice | Host organisms for PDX engraftment and propagation [7] | PDX Establishment |
| Cryopreservation Media | Specialized solutions for long-term model storage and biobanking [14] | Both Models |
The establishment of PDX and PDO models from tissue acquisition through functional assays represents a sophisticated technological pipeline for advancing precision oncology. The comparative analysis reveals that both models demonstrate equivalent predictive accuracy for treatment response, with approximately 70% concordance with patient outcomes [17].
The selection between PDX and PDO models should be guided by specific research requirements:
- PDX models offer a more physiologically relevant microenvironment and are preferred for studying complex tumor-stroma interactions, angiogenesis, and therapies requiring an intact immune system (though limited to murine immunity) [26].
- PDO models excel in high-throughput drug screening applications due to faster establishment timelines, lower costs, reduced ethical complexity, and superior scalability [17] [26] [8].
For comprehensive precision oncology programs, these models can serve complementary roles—with PDOs enabling rapid initial drug screening and PDXs providing validated in vivo confirmation of promising therapeutic candidates. This integrated approach maximizes both efficiency and clinical relevance in the development of personalized cancer treatments.
In the pursuit of effective cancer therapeutics, researchers rely on preclinical models that faithfully recapitulate human tumor biology. For decades, the field has been divided between traditional two-dimensional (2D) cell lines, which offer high-throughput capability but low clinical relevance, and patient-derived xenograft (PDX) models, which provide high clinical fidelity but are resource-intensive and low-throughput [40]. This dichotomy has created a significant gap in the drug discovery pipeline, necessitating a model that combines the scalability of in vitro systems with the predictive power of in vivo models. Enter patient-derived xenograft-derived organoids (PDXOs)—a hybrid technology that is rapidly bridging this critical divide. PDXOs are three-dimensional (3D) in vitro models generated from patient-derived xenografts, effectively combining the strengths of both parent platforms [35] [41]. This comparative analysis examines the predictive value of PDXOs against established PDX and patient-derived organoid (PDO) models, providing researchers with a scientific framework for model selection in preclinical oncology research.
Model Fundamentals: PDX, PDO, and the Emergence of PDXO
Defining the Core Preclinical Platforms
Patient-Derived Xenografts (PDXs) are established by directly implanting fragments of patient tumor tissue into immunodeficient mice. These models are considered the gold standard for in vivo preclinical research because they maintain key features of the original tumor, including its 3D architecture, genetic profile, and heterogeneity [42] [7]. PDXs are particularly valued for their ability to preserve the stromal component and tumor microenvironment (TME) during early passages, though this human stroma is gradually replaced by mouse cells over time [42] [43]. Their primary applications include late-stage drug validation, biomarker discovery, and co-clinical trials [42].
Patient-Derived Organoids (PDOs) are 3D in vitro structures grown from patient tumor stem cells using specialized matrices and cytokine protocols. First pioneered for intestinal tissue by Sato et al. in 2009, organoid technology enables long-term expansion while preserving the genetic and phenotypic characteristics of the original tumor [40] [44]. PDOs excel in high-throughput drug screening and genetic manipulation but often lack the complete tumor microenvironment, particularly native immune and stromal cells [35] [40].
PDX-Derived Organoids (PDXOs) represent a synergistic innovation, generated by establishing organoid cultures from previously characterized PDX tumors [35] [41]. This hybrid approach leverages the proven clinical relevance of PDX models while enabling the scalability and flexibility of 3D in vitro systems [45]. PDXOs effectively serve as patient surrogates for large-scale drug screens, with published data confirming >90% correlation in drug response profiles with their matched PDX models [35].
Comparative Model Workflows and Relationships
The diagram below illustrates the typical workflow for establishing and utilizing PDX, PDO, and PDXO models in cancer research, highlighting their interrelationships and primary applications.
Comparative Analysis: Model Strengths, Limitations, and Predictive Value
Quantitative Comparison of Key Model Characteristics
Table 1: Direct comparison of key technical and performance metrics across preclinical platforms.
| Characteristic | PDX Models | PDO Models | PDXO Models |
|---|---|---|---|
| Clinical Predictive Accuracy | ~85% correlation with patient response [41] | High correlation in drug response profiles [43] | >90% correlation with matched PDX response [35] |
| Time to Establish/Expand | 3-6 months for tumor growth [42] | 2-8 weeks for establishment [40] | 2-4 weeks from existing PDX [45] |
| Cost Considerations | High (animal maintenance, imaging) [40] | Moderate (matrices, growth factors) [40] | Moderate (similar to PDO, minus animal costs) [35] |
| Throughput Capacity | Low (individual drug testing) [35] | High (HTS compatible) [40] | High (HTS compatible) [41] |
| Tumor Microenvironment | Human stroma replaced by mouse cells over time [42] | Lacks native TME; requires co-culture [35] | Lacks native TME; requires co-culture [35] |
| Genetic Fidelity | High initially; clonal selection occurs [43] | Maintains genetic features long-term [35] | Retains PDX genetic profile [45] |
| Success Rate/Engraftment | Variable (27.4% for breast cancer) [42] | Depends on tumor type and epithelial origin [35] | Higher than direct PDO for some cancers [45] |
Advantages and Limitations in Research Applications
PDX Models remain unparalleled for late-stage validation studies where the complete in vivo context is essential. They provide critical insights into drug pharmacokinetics, metastasis, and systemic effects that cannot be replicated in vitro [42] [7]. However, their utility is limited by several factors: the gradual replacement of human stroma with mouse cells alters the tumor microenvironment; they are unsuitable for immunooncology studies in standard immunodeficient hosts; and their time-intensive nature (3-6 months for tumor development) precludes rapid decision-making [42] [43]. Furthermore, PDX models exhibit selection bias where only the most aggressive tumor subclones successfully engraft, potentially misrepresenting the original tumor heterogeneity [43].
PDO Models offer exceptional scalability for drug discovery, enabling high-throughput screening of hundreds or thousands of compounds [40]. They maintain genomic stability over long-term culture and are highly amenable to genetic manipulation using CRISPR-Cas9 or other technologies [40] [44]. Their primary limitation lies in their incomplete tumor microenvironment, particularly the lack of native immune cells, stromal components, and vascular networks [35]. Additionally, PDO establishment is generally restricted to epithelial-derived tumors, and the variable composition of extracellular matrix materials like Matrigel can introduce experimental inconsistencies [35] [44].
PDXO Models effectively bridge these platforms by combining the clinical relevance of PDX with the practicality of organoid culture [35] [41]. They provide a biologically equivalent alternative to PDX models for high-throughput applications, significantly reducing timelines and costs associated with in vivo studies [35]. PDXOs are particularly valuable for population-wide studies as they enable the expansion of PDO collections from existing PDX biobanks, capturing broader tumor heterogeneity [35]. Like PDOs, they face challenges in recreating the complete tumor microenvironment, though this limitation is increasingly addressed through advanced co-culture systems with immune cells [35] [44].
Experimental Design: Protocols and Methodologies
Establishing PDXO Cultures from PDX Tumors
The generation of PDXOs requires careful execution of several critical steps to ensure the resulting organoids faithfully represent the original PDX tumor. The following protocol has been adapted from established methodologies used in both academic and CRO settings [35] [45]:
PDX Tumor Harvesting: Euthanize the mouse bearing the PDX tumor when it reaches approximately 1,000-1,500 mm³ in volume. Aseptically resect the tumor and place it in cold (4°C) phosphate-buffered saline (PBS) or advanced DMEM/F12 medium supplemented with antibiotics.
Tissue Processing and Digestion: Mince the tumor tissue into small fragments (<1 mm³) using sterile surgical blades. Transfer the fragments to a digestion solution containing collagenase (1-2 mg/mL) and dispase (1-2 mg/mL) in advanced DMEM/F12. Incubate with gentle agitation at 37°C for 30-60 minutes until a single-cell suspension is achieved.
Cell Separation and Seeding: Pellet the cells by centrifugation (300-500 × g for 5 minutes). Resuspend the cell pellet in a basement membrane matrix such as Matrigel. Plate the cell-Matrigel suspension as domes in pre-warmed tissue culture plates and allow polymerization at 37°C for 20-30 minutes.
Organoid Culture Maintenance: Overlay the polymerized domes with complete organoid growth medium, typically containing essential additives like Noggin, R-spondin, EGF, Wnt3A, and B27 supplement, with exact formulations varying by tumor type [44]. Refresh the medium every 2-3 days and monitor organoid formation and growth.
Passaging and Expansion: Passage organoids every 7-14 days by mechanical disruption and enzymatic digestion. For long-term storage, cryopreserve organoids in freezing medium containing 10% DMSO and fetal bovine serum.
Key Research Reagents for PDXO Development
Table 2: Essential reagents and materials required for establishing and maintaining PDXO cultures.
| Reagent Category | Specific Examples | Function in PDXO Culture |
|---|---|---|
| Extracellular Matrices | Matrigel, Synthetic hydrogels (e.g., GelMA) | Provides 3D scaffolding for organoid growth; influences cell signaling and differentiation [44] |
| Digestive Enzymes | Collagenase, Dispase, Trypsin-EDTA | Breaks down tumor tissue into single cells or small clusters for organoid initiation [45] |
| Growth Factors & Cytokines | EGF, Noggin, R-spondin, Wnt3A, FGF10 | Promotes stem cell maintenance and proliferation; formulation varies by tumor type [35] [44] |
| Basal Media | Advanced DMEM/F12 | Nutrient foundation for organoid growth medium [45] |
| Media Supplements | B27, N2, N-Acetylcysteine | Provides essential nutrients, antioxidants, and survival factors [44] |
| Platform-Specific Additives | A83-01 (TGF-β inhibitor), Y-27632 (ROCK inhibitor) | Enhances cell survival and prevents anoikis during passaging [45] |
Research Applications: From Basic Science to Clinical Translation
Functional Screens and Therapeutic Discovery
PDXO models have demonstrated particular utility in high-throughput and high-content drug screening applications. In a landmark study by Herpers et al., PDOs were used in combination with high-content imaging (HCI) to functionally evaluate complex drug responses, screening over 500 phenotypic parameters [35]. This approach identified a bispecific antibody that triggers EGFR degradation specifically in LGR5+ cancer stem cells while minimizing toxicity to healthy colon stem cells. The findings were subsequently validated in matched in vivo PDOX and PDX models, demonstrating the power of PDXOs as a primary screening tool with results that translate to more complex in vivo systems [35].
The diagram below illustrates this integrated screening workflow that connects in vitro PDXO screening with in vivo validation.
Immunotherapy Applications and Co-culture Systems
A significant advancement in organoid technology involves the development of immune co-culture systems that better model the tumor-immune interactions critical for immunotherapy response [44]. These systems can be broadly categorized into two approaches:
Innate Immune Microenvironment Models utilize tumor tissue-derived organoids that naturally retain tumor-infiltrating lymphocytes (TILs) and other immune components from the original tumor. For example, Neal et al. developed a tumor tissue-derived organoid model using a liquid-gas interface that maintained functional TILs and replicated PD-1/PD-L1 immune checkpoint function [44]. Similarly, Voabil et al. established a platform using 1 mm³ tumor fragments that, when treated with PD-1 inhibitors, showed response patterns correlating with clinical outcomes in high TMB tumors like melanoma and NSCLC [44].
Immune Reconstitution Models involve co-culturing established tumor organoids with autologous or allogeneic immune cells. Dijkstra et al. demonstrated that autologous TILs could be expanded and co-cultured with matched tumor organoids to successfully predict clinical response to PD-1 blockade [44]. These co-culture systems are becoming increasingly sophisticated, incorporating not only T cells but also natural killer (NK) cells, macrophages, and dendritic cells to more comprehensively model the immune landscape of tumors [44].
PDX-derived organoids represent a significant evolution in preclinical cancer modeling, effectively bridging the historical gap between high-throughput in vitro systems and clinically relevant in vivo platforms. By combining the genetic fidelity and clinical predictive power of PDX models with the scalability and versatility of 3D organoid cultures, PDXOs offer researchers a powerful tool for accelerating drug discovery and advancing personalized medicine approaches [35] [41].
The future of PDXO technology will likely focus on addressing current limitations, particularly the recreation of a more complete tumor microenvironment. Emerging strategies include the development of more sophisticated co-culture systems incorporating multiple immune cell types, cancer-associated fibroblasts, and vascular components [44]. The integration of microfluidic organ-on-chip technologies will enable more dynamic interactions between tumor organoids and stromal elements, better mimicking the in vivo niche [44]. Furthermore, the standardization of defined, synthetic matrices will reduce batch-to-batch variability and improve experimental reproducibility [44].
As these technologies mature, PDXO biobanks capturing diverse cancer subtypes and resistance profiles will become increasingly valuable resources for both basic research and drug development. When integrated with complementary in vivo PDX models, PDXOs provide a comprehensive platform system that maximizes predictive confidence while optimizing resource utilization across the drug discovery pipeline [35]. For researchers and drug development professionals, this integrated approach represents a strategically advantageous path forward in the challenging landscape of oncology therapeutics development.
The pursuit of effective cancer therapeutics relies heavily on predictive preclinical models that can accurately mirror patient-specific tumor biology. For decades, patient-derived xenograft (PDX) models have been considered the gold standard in cancer research, involving the implantation of human tumor tissue into immunocompromised mice to preserve tumor architecture and heterogeneity [24] [17]. While these models provide an in vivo context for studying tumor behavior and drug response, they face significant limitations including lengthy establishment times (often exceeding six months), high costs, ethical complexities surrounding animal use, and limited suitability for high-throughput applications [24] [17] [14].
In parallel, patient-derived organoids (PDOs) have emerged as a transformative three-dimensional (3D) in vitro model system that recapitulates key aspects of the original tumor. These self-organizing microtissues are derived from patient tumor samples and cultured in defined matrices with specific growth factors that maintain the tumor's genomic, epigenetic, and metabolic profiles [46] [47]. The fundamental distinction between these platforms lies in their practical application: while PDX models offer complex in vivo biology, PDOs provide unprecedented scalability for systematic drug screening against large compound libraries, positioning them as indispensable tools for modern drug discovery pipelines [48] [47].
Comparative Predictive Performance: PDX vs. PDO Models
A comprehensive 2025 meta-analysis directly compared the predictive accuracy of PDX and PDO models across 411 patient-model pairs (267 PDX, 144 PDO) from solid tumors, providing the most robust comparative data available to date [24] [17]. The findings demonstrate remarkable equivalence between these platforms in forecasting patient treatment responses.
Table 1: Predictive Performance Metrics of PDX vs. PDO Models
| Performance Metric | PDX Models | PDO Models | Statistical Significance |
|---|---|---|---|
| Overall Concordance | 70% | 70% | Not significant |
| Sensitivity | Comparable | Comparable | Not significant |
| Specificity | Comparable | Comparable | Not significant |
| Positive Predictive Value | Comparable | Comparable | Not significant |
| Negative Predictive Value | Comparable | Comparable | Not significant |
| Progression-Free Survival Correlation | Present only in low bias-risk pairs | Significantly prolonged when PDO responded | More robust for PDOs |
The meta-analysis revealed that patients whose matched PDOs responded to therapy had significantly prolonged progression-free survival, whereas this association for PDX models was only maintained when analyses were restricted to patient-model pairs with low risk of bias after applying rigorous assessment metrics [17]. This suggests that while both models offer predictive value, PDOs may provide more consistent correlation with clinical outcomes when standardized protocols are implemented.
Technical Scalability for High-Throughput Screening
The infrastructure requirements and throughput capabilities differ substantially between PDX and PDO models, with significant implications for drug screening applications.
Table 2: Scalability Comparison for High-Throughput Drug Screening
| Parameter | PDX Models | PDO Models | Implications for Drug Screening |
|---|---|---|---|
| Establishment Time | 4-8 months | 2-4 weeks | PDOs enable rapid turnaround from patient to results |
| Cost per Model | High ($5,000-$10,000) | Moderate ($500-$2,000) | PDOs allow broader compound testing within budget constraints |
| Throughput Capacity | Low (10-20 compounds/model) | High (100-1,000+ compounds/model) | PDOs compatible with large compound libraries |
| Automation Potential | Limited | High | PDOs amenable to robotic liquid handling and automated imaging |
| Format Compatibility | Not applicable | 96-, 384-, 1536-well plates | PDOs enable miniaturization and reduced reagent consumption |
| Replication Capacity | Low (n=3-5 typical) | High (n=10-100+ technical replicates) | PDOs provide robust statistical power |
The scalability advantages of organoid systems are further enhanced through advanced culturing systems and microfluidic technologies that enable precise control over the microenvironment, significantly increasing throughput while maintaining physiological relevance [46]. These systems facilitate the testing of extensive compound libraries across multiple patient-derived organoid lines in a timeframe and at a cost structure incompatible with PDX methodologies.
Experimental Workflows for High-Throughput Organoid Screening
Organoid Establishment and Culture
The workhorse of high-throughput organoid screening begins with robust establishment and culture protocols:
Sample Acquisition and Processing: Tumor tissues are obtained through surgical resection, biopsy procedures, or from bodily fluids such as pleural effusions, ascites, or blood (for circulating tumor cells) [14] [47]. Samples undergo mechanical disintegration followed by enzymatic digestion using collagenase/hyaluronidase cocktails and TrypLE Express, typically with agitation over 1-6 hours depending on tumor type [46] [14]. The resulting cell suspensions are filtered (70-100μm filters) and centrifuged to obtain single cells or small clusters, with viability and density assessed before proceeding.
3D Culture Establishment: The cell pellet is resuspended in extracellular matrix (ECM) substitutes such as Matrigel, Basement Membrane Extract (BME), or Geltrex at densities ranging from 100-10,000 cells per μL depending on application [46] [14]. The cell-ECM suspension is plated as micro-droplets (10-20μL) in multiwell plates (96-, 384-, or 1536-well formats), solidified through brief incubation (15-30 minutes at 37°C), and overlaid with organoid-specific culture media containing essential growth factors and small molecule inhibitors tailored to the tumor type [46].
High-Throughput Screening Protocol
The integration of organoids into high-throughput screening pipelines involves several critical steps:
Assay Setup: Mature organoids (typically 14-21 days post-establishment) are harvested through enzymatic dissociation into single cells or small clusters, counted, and dispensed into miniaturized formats using automated liquid handling systems [46] [49]. The CTG-3D patient-derived organoid platform exemplifies this approach, seeding 384-well plates at densities optimized for specific tumor types [49].
Compound Treatment and Incubation: Compound libraries are transferred via non-contact dispensers capable of nanoliter-scale accuracy, with each treatment typically performed in 3-6 technical replicates and multiple concentration points (e.g., 1nM-100μM) [50]. Plates are incubated for 3-7 days to allow compound response, with timing optimized based on organoid doubling rates.
Endpoint Analysis: Viability is assessed through ATP-based assays (CellTiter-Glo 3D), caspase activation, or high-content imaging systems that quantify organoid size, morphology, and composition [46] [49]. Advanced platforms like DRUG-seq merge compound screening with bulk transcriptomics, generating mechanistic resolution of drug action by detecting expression changes in over 13,000 genes from as few as 1,000 cells per well [49].
Essential Research Reagents and Solutions
Successful implementation of high-throughput organoid screening requires carefully selected reagents and systems:
Table 3: Essential Research Reagents for Organoid Screening
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| ECM Substitutes | Matrigel, BME, Geltrex, Collagen | 3D structural support mimicking native microenvironment | Lot-to-lot variability; tumor-type specific optimization required |
| Digestion Enzymes | Collagenase/Hyaluronidase, TrypLE, Accutase | Tissue dissociation and organoid passaging | Concentration and timing critical for viability and yield |
| Growth Supplements | EGF, Noggin, R-Spondin, FGF, Wnt3a | Maintenance of stemness and proliferation | Specific cocktails required for different cancer types |
| Small Molecule Inhibitors | A83-01 (TGF-β inhibitor), SB202190 (p38 MAPK inhibitor) | Inhibition of differentiation and senescence | Concentration optimization essential to avoid off-target effects |
| Detection Reagents | CellTiter-Glo 3D, Caspase-Glo, Cytotoxicity dyes | Viability and apoptosis assessment | 3D-optimized protocols required for reagent penetration |
| Specialized Media | Intestinal Organoid Media, Prostate Cancer Media | Tissue-specific culture support | Commercial formulations available but often require customization |
Advanced Applications and Integrated Technologies
The integration of organoid screening with cutting-edge technologies has substantially expanded its applications in drug discovery. Microfluidic systems and 3D printing technologies enable precise control over organoid size and distribution, addressing critical variability challenges that previously complicated high-throughput screening outcomes [46]. These systems facilitate the creation of standardized, uniform organoid arrays compatible with automated imaging and analysis platforms.
The emergence of transcriptomic-level screening through methods like DRUG-seq represents a paradigm shift beyond conventional viability-based assessment. This approach enables the classification of compounds by mechanism of action (MoA) through comparison with large public perturbation datasets (e.g., iLINCS - Library of Integrated Network-Based Cellular Signatures), providing rich mechanistic insight alongside efficacy data [49]. When coupled with AI and machine learning platforms, these multidimensional datasets can predict responses to unscreened compounds and even inform the design of novel chemical entities with desired transcriptomic profiles [51] [49].
For immune-oncology applications, co-culture systems incorporating immune cells with tumor organoids enable the evaluation of immunomodulatory agents, though this remains technically challenging in high-throughput formats [14]. Similarly, assembloid systems that combine multiple organoid types offer opportunities for studying tumor-stromal interactions and metastatic processes in controlled settings [48].
The comparative analysis of PDX and PDO models reveals complementary strengths with distinct applications in drug discovery. While PDX models retain value for studying in vivo tumor behavior and complex microenvironmental interactions, PDO platforms offer unmatched scalability, cost-efficiency, and throughput capacity for systematic compound screening. The equivalent predictive accuracy demonstrated in recent meta-analyses, coupled with reduced ethical concerns and faster turnaround times, positions organoid technology as the premier platform for high-throughput drug screening against extensive compound libraries [24] [17].
The future trajectory of organoid screening points toward increased automation, standardization, and integration with computational approaches. The development of standardized operating procedures (SOPs) and quality control metrics will enhance reproducibility across laboratories [46]. Meanwhile, the convergence of organoid technology with AI-driven analysis and multi-omics readouts promises to establish a new paradigm in drug discovery—one where compound screening simultaneously elucidates mechanisms of action, predicts clinical responsiveness, and guides lead optimization strategies [49]. As these technologies mature, organoid-based screening is poised to become an indispensable component of the drug development pipeline, accelerating the delivery of effective therapeutics to cancer patients.
In the field of oncology, a staggering 96% of drug candidates fail during clinical trials, often due to inadequate preclinical models that fail to accurately predict human responses [52]. This high failure rate delays life-saving treatments and escalates development costs, creating an urgent need for more reliable predictive tools. Patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as the two most widely studied patient "avatar" systems in precision oncology, offering a more direct bridge between laboratory research and clinical application [17]. These models are transforming approaches to personalized cancer treatment by allowing researchers to test drug efficacy on living representations of an individual patient's tumor before administering treatments to the patient themselves.
The fundamental premise of these avatar models is their derivation directly from patient tumor tissue, preserving key biological characteristics of the original cancer. PDX models involve implanting fresh human tumor tissue into immunocompromised mice, where the tumor retains much of its histological architecture and cellular heterogeneity while interacting with host stromal components [17]. In contrast, PDO models are generated by culturing patient tumor cells as three-dimensional organoids in vitro using defined culture media supported by growth factors and extracellular matrix components [17]. Both platforms serve as living biobanks that maintain the genetic and phenotypic diversity of human cancers, enabling more accurate prediction of treatment responses and resistance patterns.
Comparative Analysis: PDX vs. PDO Model Characteristics
Fundamental Model Attributes and Technical Considerations
The selection between PDX and PDO platforms involves careful consideration of their respective strengths and limitations across multiple parameters, from physiological relevance to practical implementation factors.
Table 1: Fundamental Characteristics of PDX and PDO Models
| Characteristic | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Model Definition | Human tumor tissue implanted into immunocompromised mice [17] | 3D in vitro cultures from patient tumor cells in defined matrices [17] [16] |
| Tumor Microenvironment | Retains human stromal components initially; replaced by mouse stroma over time [17] | Lacks native vascular and immune components; can be co-cultured with added elements [17] [53] |
| Physiological Complexity | High; preserves tissue architecture and cell heterogeneity [7] [54] | Moderate; maintains cellular heterogeneity but simplified microenvironment [16] [8] |
| Throughput Capability | Low to moderate; limited by mouse housing and handling [17] | High; amenable to 96/384-well formats for drug screening [17] [16] |
| Establishment Timeline | 3-6 months for expansion and drug testing [17] [54] | 2-4 weeks from biopsy to drug screening [55] [8] |
| Success Rate | Variable (30-70%) depending on cancer type [54] | Generally higher for gastrointestinal cancers [55] |
| Cost Considerations | High (animal maintenance, imaging) [17] | Lower per model; higher throughput reduces cost per data point [17] [8] |
| Ethical Considerations | Significant animal use [17] | Minimal ethical concerns [17] [16] |
| Immunotherapy Applications | Possible with humanized mouse models [56] | Limited; requires co-culture with immune cells [17] [8] |
Predictive Performance Metrics from Clinical Studies
Recent meta-analyses have provided quantitative insights into the clinical predictive performance of both avatar systems. A systematic review and meta-analysis of studies using PDX or PDO from solid tumors treated with identical anti-cancer agents as matched patients identified 411 patient-model pairs (267 PDX, 144 PDO) [17]. The findings revealed that the overall concordance in treatment response between patients and their matched models was 70%, with no statistically significant differences between PDX and PDO platforms [17]. Sensitivity, specificity, positive predictive value, and negative predictive value were also comparable between the two model types.
Notably, patients whose matched PDOs responded to therapy showed significantly prolonged progression-free survival, while for PDX models, this association held only when analyses were restricted to patient-model pairs with low risk of bias after applying rigorous assessment metrics [17]. This suggests that with standardized protocols, both platforms can effectively stratify patients based on likely treatment outcomes.
Figure 1: Experimental workflow for PDX and PDO model generation and drug testing, demonstrating parallel paths with similar predictive concordance.
Experimental Protocols and Methodologies
PDX Model Establishment and Drug Testing Protocol
The development of PDX models requires meticulous technical execution across multiple phases from tissue acquisition to drug response evaluation:
Tissue Acquisition and Processing: Fresh tumor samples are obtained from surgical resections or biopsies, maintained in cold preservation media, and processed within hours of collection. Tissue is minced into 1-3 mm³ fragments under sterile conditions [7] [54].
Implantation Techniques: Tissue fragments are implanted subcutaneously into immunodeficient mice (e.g., NSG, NOG strains) using trocar insertion or surgical orthotopic implantation for site-specific models. The mammary fat pad is used for breast cancer models to better mimic the native microenvironment [17].
Engraftment and Expansion: Successful engraftment typically occurs within 3-6 months, with tumor growth monitored through caliper measurements. Upon reaching 1000-1500 mm³, tumors are harvested and passaged into subsequent mouse cohorts to establish stable model lines [54].
Model Validation: Histological validation through H&E staining confirms retention of original tumor architecture. Genomic characterization via whole-genome sequencing, RNA sequencing, and proteomics analyses verifies molecular fidelity to the patient tumor [56] [57].
Drug Treatment Studies: Mice bearing passage 3-5 tumors are randomized into treatment groups when tumors reach 100-200 mm³. Drugs are administered via routes matching clinical practice (oral, intraperitoneal, intravenous) at human-equivalent doses calculated through established conversion methods [17] [56]. Treatment response is assessed through tumor volume measurements, with criteria such as tumor growth inhibition percentage or regression defining sensitivity versus resistance.
PDO Generation and High-Throughput Screening Protocol
PDO cultures offer a more streamlined approach while maintaining critical tumor characteristics:
Tissue Dissociation and Processing: Patient tumor tissue undergoes enzymatic digestion (collagenase, dispase) to generate single-cell suspensions or small cell clusters. Mechanical disruption may supplement enzymatic digestion for particularly robust tissues [16] [8].
3D Matrix Embedding: Cells are resuspended in defined, growth factor-reduced extracellular matrix substitutes (e.g., Matrigel, synthetic hydrogels) and plated as domes in multi-well plates. After matrix polymerization, organoid culture medium specific to the tumor type is added [16] [53].
Culture Maintenance: Organoids are cultured in specialized media containing necessary niche factors (e.g., Wnt agonists, R-spondin, Noggin for gastrointestinal tumors). Media formulations are increasingly refined through "minus" strategies that reduce non-physiological component concentrations [16]. Passaging occurs every 1-3 weeks via mechanical or enzymatic disruption.
Drug Sensitivity Testing: Established organoids are dissociated and replated in 384-well formats for high-throughput screening. Varying concentrations of therapeutic agents are applied, with viability assessed after 5-7 days using ATP-based or resazurin reduction assays [55] [8]. Dose-response curves are generated to calculate IC₅₀ values or area under the curve (AUC) metrics.
Response Interpretation and Clinical Correlation: Drug sensitivity thresholds are established based on validation studies comparing organoid response to patient clinical outcomes. For colorectal cancer organoids, responses to 5-fluorouracil and oxaliplatin have demonstrated significant correlation with patient progression-free survival [55].
Technological Innovations and Integration with Advanced Platforms
Computational Integration and AI-Enhanced Prediction
The integration of artificial intelligence with avatar models represents a transformative advancement in predictive accuracy. The PharmaFormer platform exemplifies this approach, utilizing a custom Transformer architecture and transfer learning strategy to predict clinical drug responses [55]. This system is initially pre-trained on extensive gene expression and drug sensitivity data from over 900 cancer cell lines, then fine-tuned with limited organoid pharmacogenomic data to dramatically improve prediction accuracy for specific tumor types [55].
In validation studies, PharmaFormer demonstrated superior performance compared to classical machine learning algorithms, achieving a Pearson correlation coefficient of 0.742 versus 0.477 for Support Vector Machines and 0.375 for Multi-Layer Perceptrons [55]. When applied to TCGA colon cancer data, the organoid-fine-tuned model showed substantially improved hazard ratio predictions for 5-fluorouracil (increasing from 2.50 to 3.91) and oxaliplatin (increasing from 1.95 to 4.49) compared to the pre-trained model [55].
The "Organoid Plus and Minus" Framework
A strategic framework termed "Organoid Plus and Minus" is being employed to address limitations in traditional organoid models through both internal optimization and external enhancement [16]. The "Minus" approach focuses on rational simplification, including:
- Reduced Growth Factor Media: Formulations without R-spondin, Wnt3A, and EGF that preserve intratumoral heterogeneity while improving predictive validity [16].
- Defined Biomaterials: Engineered scaffolds that replace biologically variable matrices like Matrigel, providing greater control and reproducibility [16] [53].
The complementary "Plus" strategy enhances functionality through technological integration:
- Microfluidic Integration: Organ-on-a-chip platforms that introduce fluid shear stress, mechanical strain, and nutrient gradients to better mimic physiological conditions [16] [53].
- Vascularization Strategies: Incorporation of endothelial cells to create perfusable networks that address diffusion limitations in larger organoids [16].
- Immune Co-culture Systems: Introduction of autologous immune cells to model tumor-immune interactions and immunotherapy responses [8].
Humanized PDX Models for Immunotherapy Applications
For PDX platforms, the development of humanized models has created unprecedented opportunities for immuno-oncology research. These models are generated by transplanting human hematopoietic stem cells or peripheral blood mononuclear cells into immunodeficient mice before or alongside tumor implantation [56]. The resulting chimeric immune systems enable evaluation of immunomodulatory agents, including:
- Immune checkpoint inhibitors (anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies)
- CAR-T cell therapies and other adoptive cell transfers
- Antibody-drug conjugates (ADCs) that rely on target antigen expression and internalization [56]
These humanized PDX models are particularly valuable for studying the mechanisms of action and resistance to ADCs, which represent one of the fastest-growing classes of oncology therapeutics with more than 350 candidates in development [56].
Essential Research Reagents and Materials
Successful implementation of PDX and PDO methodologies requires specific reagent systems and technical resources. The following table details key solutions and their applications in avatar model research.
Table 2: Essential Research Reagent Solutions for Avatar Model Development
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Extracellular Matrices | Matrigel, synthetic PEG-based hydrogels, collagen-based scaffolds | Provide 3D support structure for organoid growth; influence differentiation and proliferation [16] [53] |
| Specialized Media Formulations | IntestiCult, STEMdiff, customized low-growth factor media | Support stem cell maintenance and lineage-specific differentiation; increasingly defined to reduce batch variability [16] |
| Enzymatic Dissociation Kits | Collagenase/Dispase blends, TrypLE, Accutase | Gentle tissue dissociation preserving cell viability and surface receptors [16] [8] |
| Cryopreservation Media | CryoStor, Bambanker, DMSO-based formulations | Long-term storage of established PDX/PDO lines for biobanking [57] |
| Cell Viability Assays | CellTiter-Glo, resazurin reduction, Calcein-AM | High-throughput assessment of drug response in screening campaigns [55] [8] |
| Immunodeficient Mouse Strains | NSG, NOG, NRG mice | Host organisms for PDX engraftment with varying levels of immune deficiency [7] [54] |
| Humanization Systems | CD34+ hematopoietic stem cells, PBMC reconstitution kits | Creation of humanized PDX models for immunotherapy studies [56] |
Figure 2: Technological innovations addressing limitations in patient-derived avatar models, showing solution pathways across multiple challenge domains.
PDX and PDO models have established themselves as invaluable tools in the precision oncology arsenal, with comparable predictive accuracy of approximately 70% concordance with patient responses according to recent meta-analyses [17]. The choice between these platforms depends heavily on specific research objectives, with PDX models offering superior microenvironmental context for studying stromal interactions and certain therapeutic classes like antibody-drug conjugates [56], while PDO platforms provide unmatched throughput and scalability for drug screening and biomarker discovery [16].
Looking forward, several trends are shaping the evolution of patient avatar technologies. The regulatory landscape is shifting, with the FDA announcing plans to phase out traditional animal testing in favor of advanced human-model systems like organoids and organ-on-a-chip platforms for drug safety evaluation [16]. This policy change will accelerate adoption of these technologies across the pharmaceutical industry. The integration of multi-omics data with high-content imaging and AI-driven analysis is creating increasingly sophisticated digital twins of patient tumors, enabling in silico prediction of treatment responses and resistance evolution [55] [52].
For clinical implementation, the most promising path lies in strategic hybrid approaches that leverage the complementary strengths of both platforms. Early drug screening and biomarker discovery can be efficiently conducted in PDO systems, with lead candidates and combination therapies validated in PDX models that provide crucial in vivo context [56]. As these technologies continue to mature and standardize, patient-derived avatars are poised to transform oncology drug development from a process with 96% failure rates to one with precision-guided success, ultimately delivering more effective treatments to cancer patients based on the unique characteristics of their individual diseases.
In the era of precision medicine, the development of effective cancer therapies relies heavily on preclinical models that faithfully recapitulate the complexity of human tumors. For decades, cancer research has utilized traditional two-dimensional (2D) cell lines and patient-derived xenograft (PDX) models, but each approach has significant limitations. While 2D cell lines are easy to manipulate and cost-effective, they lack the three-dimensional architecture and cellular heterogeneity of original tumors, leading to poor clinical predictive power [11]. PDX models, which involve transplanting patient tumor tissue into immunodeficient mice, better maintain tumor heterogeneity but are limited by long establishment times, high costs, low success rates for some cancer types, and the inability to model human immune responses [58] [59].
The emergence of patient-derived organoids (PDOs) has expanded the repertoire of relevant models. These self-organizing three-dimensional structures grown from patient tumor samples maintain key aspects of the original tumor's histo-architecture, genetic diversity, and cellular heterogeneity [43] [60]. PDOs can be established more rapidly than PDXs and are amenable to medium- to high-throughput drug screening, making them particularly valuable for personalized medicine approaches [59] [61]. This review presents a comparative analysis of PDX and PDO models through specific case studies in gastrointestinal, ovarian, and prostate cancers, evaluating their predictive value for therapeutic response and their applications in cancer research and drug development.
Comparative Advantages and Limitations
Table 1: Characteristics of Patient-Derived Xenograft (PDX) and Organoid (PDO) Models
| Characteristic | PDX Models | PDO Models |
|---|---|---|
| Model type | In vivo | Ex vivo |
| Patient recapitulation | Yes | Yes |
| Tumor microenvironment | Yes (from mouse host) | Limited or none |
| Maintenance of immune response | No (unless humanized) | No |
| Scalability | Medium | High |
| Establishment time | Slow (several months) | Relatively fast (weeks) |
| Cost | High | Relatively low |
| Success rate | Variable by cancer type | Generally high |
| High-throughput screening | Not suitable | Highly suitable |
| Genetic manipulation | Challenging | Amenable |
| Ethical considerations | Animal use | Minimal |
Experimental Workflow for Model Establishment
The following diagram illustrates the parallel workflows for establishing PDX and PDO models from patient tumor samples:
Diagram 1: Workflow for establishing PDX and PDO models from patient tumor samples.
Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for PDX and PDO Research
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Extracellular Matrix | Matrigel, Basement Membrane Extract (BME), Geltrex | Provides 3D scaffold for organoid growth and differentiation |
| Digestive Enzymes | Collagenase/Hyaluronidase, TrypLE Express | Dissociates tumor tissue into single cells or small clusters |
| Growth Factors & Inhibitors | EGF, FGF, B27, Noggin, R-spondin, A83-01, Y27632 | Supports stem cell maintenance and organoid growth |
| Specialized Media | Advanced DMEM/F12, Organoid Basal Medium | Base medium formulation for organoid culture |
| Immunodeficient Mice | NOD-scid, NSG strains | Host animals for PDX establishment and propagation |
| Cryopreservation Solutions | DMSO/FBS mixtures | Long-term storage of PDX and PDO models |
Case Study 1: Gastrointestinal Cancers
Esophageal Cancer Models and Drug Response Prediction
Gastrointestinal cancers, particularly esophageal cancers including esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC), present significant therapeutic challenges with poor prognosis for advanced disease. Research utilizing both PDX and PDO models has demonstrated their utility in predicting therapy response and understanding resistance mechanisms.
In ESCC, PDO models have shown remarkable accuracy in recapitulating patient responses to chemotherapy. Kijima et al. established PDOs from tumor and adjacent normal mucosa biopsies of ESCC patients with a success rate of 68.75% (11/16) [61] [62]. When these PDOs were treated with 5-fluorouracil (5-FU), resistance was associated with tumor-like organ formation and a treatment-resistant cell population characterized by high CD44 expression and enhanced autophagy capacity [61] [62]. This finding not only demonstrated the predictive value of PDOs but also identified potential mechanisms of chemoresistance that could be targeted in combination therapies.
For EAC, Li et al. established long-term expansion PDOs from resection tissues using a glandular-preferred protocol with additional Wnt3A in the culture medium [61] [62]. Drug sensitivity testing of 24 anticancer compounds in these PDOs revealed that responses to targeted agents aligned with molecular status, such as TP53 and EGFR mutations, while resistance to chemotherapeutic drugs (5-fluorouracil, epirubicin, and cisplatin) mirrored patient responses [61] [62]. In another study, EAC PDOs carrying ERBB2 amplification showed specific response to the HER2-targeted agent mubritinib, while wild-type organoids were non-responsive, highlighting the potential for PDOs to guide targeted therapy selection [61].
PDX models of esophageal cancer have also demonstrated significant value in preclinical research. Zou et al. established 25 PDX models from 188 fresh endoscopic biopsy tissues of ESCC patients, with the resulting models retaining histologic and genomic characteristics of the original tumors [62]. Importantly, tumor growth inhibition in 5 xenografts exposed to paclitaxel and platinum-based chemotherapy correlated well with the clinical responses of the corresponding patients [62]. Similarly, Zhu et al. reported one of the largest ESCC PDX cohorts consisting of 61 models and identified EGFR as a potential predictive biomarker for cetuximab response [62].
Quantitative Comparison of Model Performance
Table 3: Performance Metrics of GI Cancer PDX and PDO Models
| Study | Cancer Type | Model | Success Rate | Predictive Accuracy | Key Findings |
|---|---|---|---|---|---|
| Kijima et al. | ESCC | PDO | 68.75% (11/16) | High for 5-FU response | CD44+ cells with high autophagy capacity associated with resistance |
| Li et al. | EAC | PDO | 31.25% (10/32) | Consistent with patient response | Drug sensitivity aligned with molecular status (TP53, EGFR) |
| Vlachogiannis et al. | GI Cancers | PDO | 70% | 100% sensitivity, 93% specificity | Living biobank predicted response to chemo/targeted therapy |
| Zou et al. | ESCC | PDX | 13.3% (25/188) | Correlated with clinical response | TGI in xenografts correlated with patient response to paclitaxel/platinum |
| Dodbiba et al. | EC/GEJ | PDX | 38% (21/55) | Variable (2/7 models correlated) | Highlighted heterogeneity in predictive capacity |
Case Study 2: Ovarian Cancer
Recapitulating Clinical Drug Resistance in OCCC Models
Ovarian cancer, particularly ovarian clear cell carcinoma (OCCC), is characterized by inherent resistance to platinum-based chemotherapy, contributing to its poor prognosis. A comprehensive study directly compared multiple models derived from the same OCCC patient, including 4 cell lines, 2 PDOs, and 1 PDX, providing unique insights into their respective capacities to recapitulate clinical drug responses [11].
In this comparative analysis, the patient was refractory to carboplatin, doxorubicin, and gemcitabine. While traditional 2D cell lines derived from the same tumor showed sensitivity to these chemotherapeutic agents, both PDX and PDO models accurately displayed resistance patterns consistent with the patient's clinical response [11]. Transcriptomic analysis further validated these findings, with PDX and PDO models clustering separately from the 2D cell lines and more closely representing the original tumor characteristics [11].
The study also demonstrated the utility of PDOs for identifying alternative treatment options. When the OCCC PDOs were screened against drugs not previously used in the patient's clinical management, the HDAC inhibitor belinostat was identified as a potentially effective treatment [11]. This finding highlights how functional drug testing using PDOs can guide therapeutic decisions for patients with resistant disease, potentially improving outcomes through drug repurposing.
Modeling Tumor Heterogeneity and Microenvironment
Ovarian cancer exhibits significant heterogeneity, with evidence suggesting different cells of origin including the ovarian surface epithelium (OSE) and fallopian tube (FT) epithelium. Organoid models have enabled direct comparison of these potential origins, revealing biological and therapeutic differences with clinical implications [60].
Using organoids derived from both OSE and FT tissues with introduced HGSOC-associated mutations through CRISPR-Cas9 gene editing, researchers confirmed that both epithelia can give rise to epithelial tumors with high-grade pathology [60]. However, tumors of fallopian tube origin demonstrated stronger tumorigenic potential and proliferative properties, along with greater sensitivity to paclitaxel and niraparib compared to those of OSE origin [60]. These findings suggest that determining the cell of origin in HGSOC could have prognostic and therapeutic implications, highlighting how organoid models can advance our understanding of ovarian cancer biology.
For modeling the tumor microenvironment, PDX-derived organoids (PDXOs) offer a unique advantage by incorporating some stromal elements. Chen et al. established PDXO models from ovarian cancer tissues transplanted into mice, creating models that better recapitulate aspects of the tumor microenvironment while maintaining the advantages of organoid systems for drug screening applications [60].
Case Study 3: Prostate Cancer
Modeling Advanced Disease and Treatment Resistance
Prostate cancer progression from androgen-sensitive to castration-resistant disease represents a major therapeutic challenge. PDX and PDO models have proven invaluable for studying this transition and screening potential therapies. A notable example is the LuCaP PDX cohort, which includes models representing both adenocarcinoma and neuroendocrine lineages of metastatic castration-resistant prostate cancer (mCRPC) [63].
Using 20 models from this cohort, researchers systematically optimized prostate organoid culture conditions, enabling the establishment of a biobank of PDX-derived organoids that preserved the genomic heterogeneity of the original PDXs [63]. Molecular characterization confirmed that lineage markers and transcriptomes were maintained between PDXs and their derived organoids. Critically, the dependence on androgen receptor (AR) signaling was preserved in adenocarcinoma organoids, replicating a fundamental characteristic of CRPC that is essential for clinically relevant drug testing [63].
Drug sensitivity testing in this biobank demonstrated genotype-dependent responses, with maximum cytotoxicity to the PARP inhibitor olaparib observed in BRCA2-deficient organoids, mirroring responses seen in patients with similar genetic alterations [63]. This finding validates the utility of these models for preclinical drug testing and biomarker identification, particularly for targeted therapies like PARP inhibitors that require specific genetic contexts for efficacy.
Androgen-Dependent Models and Drug Screening Platforms
The PNPCa model, an androgen-dependent PDX derived from a treatment-naïve soft tissue metastasis, provides a unique resource for studying early-stage prostate cancer biology and therapy responses [64]. This model harbors BRCA2 and CHD1 somatic mutations and exhibits microsatellite instability-high (MSI-H) status, a genomic feature present in approximately 3% of advanced prostate cancers that had not been previously modeled in vivo [64].
Organoids derived from the PNPCa PDX, along with additional metastatic PDX models (BM18, LAPC9), were used in a medium-throughput drug screen of FDA-approved compounds [64]. This platform revealed differential drug sensitivities across models representing different disease stages and molecular subtypes. Multikinase inhibitors including ponatinib, sunitinib, and sorafenib demonstrated broad effectiveness on all PDX- and patient-derived organoids from advanced cases with acquired resistance to standard-of-care agents [64]. This proof-of-concept study established a preclinical tool for screening responses to both standard therapies and repurposed compounds, potentially accelerating therapeutic development.
The comprehensive analysis of PDX and PDO models across gastrointestinal, ovarian, and prostate cancers demonstrates that both platforms offer significant advantages over traditional 2D cell lines for preclinical cancer research and drug development. Each model system has distinct strengths that make it suitable for specific applications.
PDO models excel in scenarios requiring rapid turnaround, such as functional precision medicine approaches where treatment decisions need to be made within clinically relevant timeframes. Their compatibility with medium- to high-throughput drug screening enables comprehensive testing of therapeutic options, including combination therapies. The ability to cryopreserve and biobank PDOs facilitates the creation of living libraries representing diverse cancer subtypes and genomic alterations, providing valuable resources for both basic and translational research [43] [61] [63].
PDX models remain invaluable for studying tumor-stroma interactions, metastatic processes, and therapeutic responses in an in vivo context. The development of humanized PDX models with reconstituted immune components holds particular promise for immuno-oncology research, enabling evaluation of immunotherapies that require functional immune responses [58] [59]. PDX models also provide critical validation for therapeutic candidates identified through in vitro PDO screens, establishing a comprehensive pipeline from initial discovery to preclinical validation.
Future directions for the field include further technical optimization to improve establishment success rates, particularly for rare cancer subtypes; standardization of culture conditions to enhance reproducibility across laboratories; and the development of more complex models that incorporate immune cells, fibroblasts, and vascular components to better mimic the tumor microenvironment. The integration of multi-omics technologies with functional drug testing in these models will further enhance their predictive power and utility for guiding personalized cancer therapy.
As these complementary models continue to evolve and improve, they will play increasingly important roles in bridging the gap between basic cancer research and clinical application, ultimately accelerating the development of more effective and personalized cancer treatments.
Navigating Challenges: Model Limitations and Strategic Optimization Approaches
In the pursuit of precision oncology, Patient-Derived Xenograft (PDX) models and Patient-Derived Organoid (PDO) models have emerged as foundational tools. A central thesis in comparative oncology research is that these models offer complementary strengths and weaknesses, primarily characterized by a fundamental trade-off: PDX models offer superior tumor microenvironment complexity at the cost of significant time and financial investment, whereas PDO models provide unmatched scalability and speed but lack a complete native microenvironment [43] [26]. This guide provides an objective comparison for researchers and drug development professionals, synthesizing current experimental data and methodologies to inform model selection.
Quantitative Model Comparison: PDX vs. PDO
The following table synthesizes key comparative data from recent meta-analyses and research publications, providing a quantitative overview of the performance and limitations of both models.
Table 1: Direct Comparison of PDX and PDO Model Characteristics and Performance
| Characteristic | Patient-Derived Xenograft (PDX) | Patient-Derived Organoid (PDO) |
|---|---|---|
| Predictive Concordance with Patient Response | ~70% (based on meta-analysis of 267 pairs) [24] | ~70% (based on meta-analysis of 144 pairs) [24] |
| Typical Establishment Time | Several months [43] [26] | Weeks [43] [26] |
| Relative Cost & Throughput | Low-throughput, high cost per model [24] [65] | High-throughput, lower cost, amenable to large-scale drug screening [24] [26] |
| Tumor Microenvironment (TME) | More complex, includes in vivo mouse stromal components [27] [26] | Lacks a complete native TME (e.g., vascular, immune components) [44] [26] |
| Key Microenvironment Limitation | Gradual replacement of human stroma with mouse cells; lacks functional human immune system for immunotherapy testing [43] | Requires sophisticated co-culture systems to introduce immune and other stromal cells [44] |
| Genetic Fidelity | High, but can undergo clonal selection and dynamic genetic alterations over time [43] | High, maintains aspects of tumor structure and genetic heterogeneity [43] |
| Primary Strengths | In vivo systemic context, models metastasis, preserves tumor architecture [27] | Speed, cost-effectiveness, scalability, biobanking, genetic fidelity [43] [30] |
Experimental Protocols & Methodologies
Understanding the foundational workflows for generating and utilizing these models is critical for assessing their limitations and applications.
PDX Model Generation and Drug Testing Workflow
The PDX workflow is a multi-step process that directly links clinical and preclinical research, but its lengthy timeline is a major constraint [43] [66].
Key Experimental Steps:
- Tumor Implantation: Fresh patient tumor tissue is surgically implanted into an immunodeficient mouse (e.g., NSG mouse) [27] [66].
- Engraftment and Expansion (P0): The initial implant is allowed to grow, which can take several months. This first-generation model is termed passage 0 (P0) [43].
- Propagation and Biobanking (P1+): The P0 tumor is excised and fragmented to implant into a new cohort of mice (P1). This process creates a stable, expandable model line that can be cryopreserved [67] [66].
- Therapeutic Study: Cohort groups are established from propagated models. After tumor establishment, mice are randomized into treatment and control groups. Tumor volume is tracked over weeks to assess drug efficacy [27].
- Endpoint Analysis: Tumors are harvested for downstream genomic, transcriptomic, and histopathological analysis to correlate response with molecular features [66].
PDO Generation and High-Throughput Screening
The PDO workflow is designed for efficiency and scalability, directly addressing the time and cost constraints of PDX models, though it requires active engineering of the microenvironment [43] [44].
Key Experimental Steps:
- Tissue Processing: Patient tumor samples are digested enzymatically and mechanically into a single-cell suspension or small fragments [44] [68].
- 3D Embedding: The cell suspension is mixed with a basement membrane extract (e.g., Matrigel) and plated. The matrix provides a 3D scaffold that supports self-organization [44] [68].
- Defined Culture: Organoids are cultured in a specialized medium containing a cocktail of growth factors (e.g., Wnt, R-spondin, Noggin) tailored to the tumor type to promote stem cell maintenance and growth [44].
- Expansion and Biobanking: Organoids are passaged every 1-3 weeks by mechanical or enzymatic dissociation and re-embedded, allowing for massive expansion and cryopreservation in biobanks [43] [30].
- Microenvironment Engineering (Critical Step): To address the native TME lack, autologous immune cells (e.g., TILs) can be added back into the culture to create immune-organoid co-cultures for immunotherapy testing [44].
- High-Throughput Screening: Organoids can be dissociated and seeded into 384-well plates for automated, high-throughput drug screening. Cell viability is typically measured using assays like CellTiter-Glo after 5-7 days of drug exposure [43] [30].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of PDX and PDO models relies on a suite of specialized reagents and materials. The table below details key solutions for these experimental workflows.
Table 2: Essential Research Reagents and Materials for PDX and PDO Models
| Reagent/Material | Function in Model System | Specific Examples & Applications |
|---|---|---|
| Immunodeficient Mice | Provides an in vivo host for PDX tumor engraftment without immune rejection. | NSG (NOD-scid-gamma) mice are the gold standard, offering a high engraftment success rate [67]. |
| Defined Growth Factors | Promotes the growth and maintenance of stem cells within PDO cultures. | Wnt3A, R-spondin, and Noggin are essential for growing gastrointestinal organoids [44]. |
| Extracellular Matrix (ECM) | Provides a 3D scaffold that supports cell polarization and self-organization in PDOs. | Matrigel is widely used but has batch variability. Synthetic hydrogels (e.g., GelMA) are emerging alternatives [44] [68]. |
| Cryopreservation Media | Enables long-term storage and biobanking of both PDX tumor fragments and PDOs. | Typically contains DMSO and serum alternatives to maintain cell viability during freeze-thaw cycles [43]. |
| Cytokines for Co-culture | Used to activate and maintain immune cells in PDO-immune co-culture systems. | IL-2 is critical for the survival and function of T cells in immune-organoid co-cultures [44]. |
The comparative analysis affirms that the choice between PDX and PDO is not about identifying a superior model, but about selecting the right tool for the research question and stage.
- PDX models are indispensable for studies requiring a systemic, in vivo context, such as evaluating metastasis, pharmacokinetics, and therapies targeting the native stromal niche. Their use is justified despite the cost and time when the biological question necessitates a whole-organism physiology [27] [26].
- PDO models excel in applications demanding speed and scale, including high-throughput drug screening, rapid biomarker discovery, and personalized medicine approaches where treatment decisions are time-sensitive. Their microenvironment limitations are being actively addressed through advanced co-culture and organ-on-chip technologies [44] [30].
Future directions point toward the integrated use of both models—using PDOs for initial high-throughput screening to triage candidates, followed by validation in a select set of clinically relevant PDX models—creating a powerful, iterative pipeline for accelerating oncology drug development [24].
Success Rate Variations Across Cancer Types and Establishment Protocols
The following table summarizes the core performance metrics of Patient-Derived Xenograft (PDX) and Patient-Derived Organoid (PDO) models based on current research.
| Performance Metric | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Overall Predictive Concordance with Patient Response | ~70% (no significant difference from PDO) [69] [24] | ~70% (no significant difference from PDX) [69] [24] |
| Typical Model Establishment Time | Several months; can stabilize to 40-50 days with passages [1] | Rapid expansion possible; high-throughput screening enabled [8] [14] |
| Key Advantages | Retains original tumor architecture & heterogeneity; provides an in vivo platform [7] [1] | High success rate; cost-effective; preserves genetic stability; amenable to gene editing [8] [14] |
| Major Limitations | Low success rate for some tumors; high cost; ethical concerns; long cultivation cycles [7] [1] | Lacks complex vascular and stromal components of the in vivo microenvironment [8] [24] |
Cancer-Type Specific Success Rates and Challenges
The successful establishment of patient-derived models is highly dependent on the cancer type and its intrinsic biological properties.
Success Rates in Preclinical Modeling
Table 1.1: Model Establishment Rates and Considerations by Cancer Type
| Cancer Type | PDX Establishment Considerations | PDO Establishment Considerations |
|---|---|---|
| Glioblastoma (GBM) & Aggressive Cancers | Higher establishment rate correlated with tumor grade and aggressiveness [36]. | Easier ex vivo maintenance for aggressive cancers, resulting in higher establishment rates [36]. |
| Lower-Grade Tumors | Poses significant challenges for reproducible ex vivo maintenance, leading to lower establishment rates [36]. | Lower establishment rates compared to aggressive cancers; modeling complexity varies [14]. |
| Ovarian Clear Cell Carcinoma (OCCC) | Availability is limited; one study reported establishment from a single patient sample [11]. | Successfully established from a patient tumor, recapitulating patient's drug resistance profile [11]. |
| Pancreatic, Colorectal, & Other Cancers | Successfully modeled for drug screening and biomarker discovery [1]. Protocols require optimization for each cancer type [14]. | Successfully established for numerous cancers (e.g., colorectal, prostate, gastric); protocols require tumor-specific optimization [14] [44]. |
Detailed Establishment Protocols
The reliability of any model is fundamentally linked to the robustness of its establishment protocol. Below are the standardized workflows for generating PDX and PDO models.
Patient-Derived Xenograft (PDX) Workflow
Protocol Steps:
- Sampling: Obtain fresh tumor tissue from primary or metastatic sites via surgical resection or biopsy [1].
- Processing: The tumor tissue is cut into small fragments (e.g., 4mm³) while maintaining the tissue structure [1] [11].
- Implantation: Fragments are implanted into an immunocompromised mouse host. Common methods include:
- Engraftment & Growth: The host mouse is monitored for tumor growth. Successful engraftment that reaches a predefined volume (e.g., 1-2 cm³) is designated the first generation (F0) [1].
- Harvesting & Passaging: The F0 tumor is harvested, segmented, and re-implanted into new mice to generate subsequent generations (F1, F2, etc.). This process stabilizes the model and expands the tissue bank [1].
- Cryopreservation: Residual tumor fragments can be cryopreserved in media containing DMSO and fetal bovine serum for long-term storage and future use [11].
Patient-Derived Organoid (PDO) Workflow
Protocol Steps:
- Sampling: Tumor tissue can be obtained from surgical resection or via less invasive methods such as malignant ascites, pleural effusions, or urine [14].
- Digestion: The sample is broken down using mechanical disruption (pipetting, cutting) and enzymatic digestion with a cocktail of enzymes like collagenase/hyaluronidase and TrypLE Express to obtain single cells or small cell clusters [14].
- Filtration & Washing: The digested cell suspension is passed through a strainer (70µm or 100µm) to remove debris and obtain a uniform cell population, followed by centrifugation [14].
- Embedding in ECM: The cell pellet is resuspended and mixed with an Extracellular Matrix (ECM) such as Matrigel, Basement Membrane Extract (BME), or Geltrex, which provides a 3D scaffold for growth [14].
- Plating & Culture: Small drops of the cell-ECM mixture are plated and solidified. Pre-warmed organoid culture medium is added. This medium is critical and is supplemented with a tailored cocktail of growth factors (e.g., Wnt3A, Noggin, R-spondin, EGF, B27), which varies by cancer type to support stem cell expansion and inhibit non-tumor cell growth [14] [44].
- Expansion & Passaging: Organoids are allowed to grow and can be mechanically or enzymatically broken down and re-plated to passage and expand the culture over the long term [14].
Comparative Experimental Data on Predictive Performance
A direct comparison of model predictions against actual patient outcomes is the ultimate validation of their clinical relevance.
Key Comparative Study Findings
Table 3.1: Predictive Performance Metrics from Meta-Analysis and Direct Comparisons
| Study Model/Type | Experimental Design | Key Finding on Predictive Value | Clinical Correlation |
|---|---|---|---|
| Meta-Analysis (411 patient-model pairs) [69] [24] | Systematic review & meta-analysis of studies using PDX or PDO treated with identical agents as the patient. | Overall response concordance was 70%, with no significant difference between PDX and PDO. Sensitivity, specificity, PPV, and NPV were also comparable. | Patients whose matched PDO responded to therapy had prolonged progression-free survival (PFS). For PDX, prolonged PFS was observed only in analyses restricted to low risk-of-bias pairs. |
| Ovarian Clear Cell Carcinoma (OCCC) Case Study [11] | Comprehensive comparison of 7 models (4 cell lines, 2 PDO, 1 PDX) from the same patient. | Cell lines were sensitive to carboplatin, doxorubicin, and gemcitabine. In contrast, PDX and PDO displayed resistance to all three drugs. | The patient was clinically refractory to these three drugs. Only the PDX and PDO models accurately recapitulated the patient's drug resistance. |
| PDO Clinical Utility [11] | Using the OCCC PDO model to test the HDAC inhibitor Belinostat, a drug not used in the patient's prior treatment. | Identified Belinostat as a potential effective treatment based on PDO response. | Suggests PDO's potential for guiding new therapeutic choices after standard therapies have failed. |
The Scientist's Toolkit: Essential Research Reagents
The successful establishment and maintenance of PDX and PDO models rely on a suite of specialized reagents and materials.
Table 4.1: Key Reagents for Patient-Derived Model Research
| Reagent/Material | Function | Common Examples & Notes |
|---|---|---|
| Extracellular Matrix (ECM) | Provides a 3D scaffold that supports cell polarization, proliferation, and organization, mimicking the in vivo basement membrane. | Matrigel, BME, Geltrex. Batch-to-batch variability is a concern; synthetic hydrogels (e.g., GelMA) are emerging alternatives [14] [44]. |
| Specialized Culture Media | Provides nutrients and specific signaling molecules to promote the growth and maintenance of tumor stem/progenitor cells. | Advanced DMEM/F12 base, supplemented with B27, N-Acetylcysteine, and critical growth factors like EGF, FGF-10, Wnt3A, Noggin, and R-spondin [14] [11]. |
| Enzymatic Digestion Cocktail | Breaks down the tough extracellular matrix of tumor tissue to isolate viable single cells or small clusters for culture. | Collagenase/Hyaluronidase blend and TrypLE Express (a recombinant trypsin substitute) are commonly used [14]. |
| Small Molecule Inhibitors | Added to the culture medium to suppress the growth of non-tumor cells (e.g., fibroblasts) and inhibit unwanted differentiation or apoptosis. | A-83-01 (TGF-β inhibitor), Y-27632 (ROCK inhibitor), and SB202190 (p38 MAPK inhibitor) [14] [11]. |
| Immunocompromised Mice | Serves as the in vivo host for PDX models, allowing the engraftment and growth of human tumor tissue without immune rejection. | Nude, SCID, NOD-SCID, and NSG mice. The degree of immunodeficiency required can vary with tumor type [1]. |
Patient-derived models have revolutionized cancer research by providing more physiologically relevant platforms for drug development and personalized medicine. The two most prominent systems—Patient-Derived Xenografts (PDX) and Patient-Derived Organoids (PDO)—each present unique advantages and challenges, with their predictive accuracy heavily dependent on optimized culture conditions [17] [70]. The extracellular matrix (ECM) and specific growth factor cocktails play pivotal roles in determining the success of model establishment and maintenance of tumor fidelity [59]. This guide provides a comparative analysis of how these critical components influence model performance, offering researchers evidence-based protocols to enhance predictive value in preclinical applications.
Systematic evaluation reveals that both PDX and PDO models demonstrate approximately 70% overall concordance with patient treatment responses, showing no statistically significant difference in predictive accuracy between the two platforms [17]. However, their operational characteristics, including establishment success rates, time requirements, and associated costs, differ substantially, making the optimization of culture parameters essential for maximizing research outcomes.
Model Fundamentals and Comparative Framework
Defining PDX and PDO Models
Patient-Derived Xenografts (PDX) are established through the transplantation of fresh human tumor tissue directly into immunocompromised mice [71]. The model retains key aspects of the tumor's three-dimensional architecture and stromal components through interaction with the mouse microenvironment, though this stromal compartment gradually becomes murine in character over successive passages [17] [71].
Patient-Derived Organoids (PDO) are three-dimensional in vitro structures derived from patient tumor tissue or cancer stem cells that self-organize in defined culture media supported by ECM substrates [59]. While lacking the complete tumor microenvironment found in PDX, PDO models effectively recapitulate histological architecture and maintain genetic profiles of original tumors while offering superior scalability [17] [8].
Key Comparative Metrics
The following table summarizes core performance characteristics across major cancer types, highlighting how establishment success varies by tumor origin:
Table 1: Model Establishment and Operational Characteristics
| Cancer Type | PDX P0 Engraftment Rate | PDO Establishment Success | PDX Timeline (months) | PDO Timeline (weeks) |
|---|---|---|---|---|
| Pancreatic | 59-62% [72] | Information missing | 2-4 [71] | 2-4 [59] |
| Duodenal/Ampullary | 86% [72] | Information missing | 2-4 [71] | 2-4 [59] |
| Biliary | 35% [72] | Information missing | 2-4 [71] | 2-4 [59] |
| Colorectal | Information missing | ~70% [59] | 2-4 [71] | 2-4 [59] |
| Breast | Information missing | Information missing | 2-4 [71] | 2-4 [59] |
Table 2: Predictive Performance and Applications
| Parameter | PDX Performance | PDO Performance |
|---|---|---|
| Overall Response Concordance | 70% [17] | 70% [17] |
| Sensitivity/Specificity | Comparable [17] | Comparable [17] |
| PFS Prediction | Association with low bias risk only [17] | Strong association [17] |
| Immunotherapy Applications | Limited (humanized models required) [43] [71] | Limited (immune co-culture required) [17] [8] |
| High-Throughput Capacity | Low [43] [70] | High [17] [59] |
Experimental Methodology for Model Establishment
PDX Development Protocol
The successful establishment of PDX models requires careful attention to tissue processing, host selection, and implantation techniques:
Tissue Acquisition and Preparation: Surgically resected tumor samples should be placed in cold solution containing Fetal Bovine Serum (FBS) and penicillin/streptomycin immediately after resection [71]. Tissue is then cut into 3-5 mm³ pieces under sterile conditions, preserving viability by minimizing processing time [71].
Host Selection and Implantation: NOD/SCID/IL2rγnull (NSG) mice demonstrate 95-100% engraftment efficacy for difficult-to-transplant tumors, superior to other immunocompromised strains [71]. Both subcutaneous (flank) and orthotopic (tissue-of-origin) implantation sites are used, with orthotopic placement potentially providing a more relevant microenvironment despite technical challenges [71] [72].
Monitoring and Passage: Tumor growth is monitored twice weekly using vernier calipers, measuring both length and width [71]. Initial engraftment typically requires 2-4 months, with successful models reaching 1-2 cm³ before passage to subsequent generations (F1, F2, F3, etc.) [71]. The third generation (F3) is typically used for drug treatment studies once model stability is confirmed [71].
Diagram 1: PDX Establishment Workflow
PDO Culture Protocol
Organoid establishment relies on precisely defined matrix and media components to maintain tumor cell viability and proliferation:
Sample Processing and Digestion: Tumor samples are mechanically dissociated followed by enzymatic digestion using collagenase/hyaluronidase and TrypLE Express [59]. For samples requiring extended digestion (>2 hours), addition of 10µM ROCK inhibitor (Y-27632) improves growth efficiency by preventing anoikis [59]. The resulting cell clusters (2-10 cells) are filtered through 70-100µm strainers to achieve appropriate size distribution.
ECM Embedding and Culture: Processed cells are resuspended in basement membrane extract (BME), Matrigel, or Geltrex [59]. The cell-ECM suspension is plated as 10-20µL drops in pre-warmed plates and solidified at 37°C for 15-30 minutes [59]. Following polymerization, specialized organoid medium containing essential growth factors is added [59].
Growth Factor Supplementation: PDO media requires precise formulation including Wnt pathway agonists (e.g., R-spondin), epidermal growth factor (EGF), and transforming growth factor-β inhibitors (e.g., Noggin) [59]. These components maintain stemness and promote epithelial proliferation while inhibiting differentiation [59].
Diagram 2: PDO Establishment Workflow
Impact of Culture Components on Model Fidelity
Extracellular Matrix Optimization
The ECM serves as more than a simple scaffold—it provides critical biochemical and biophysical cues that direct cell behavior, proliferation, and differentiation:
PDX Microenvironment Dynamics: Initial PDX passages retain human cancer-associated fibroblasts (CAFs), endothelial cells, and tumor-associated macrophages within their native extracellular matrix composed of collagen, laminin, and fibronectin [71]. However, serial passaging results in gradual replacement of human stromal components with murine equivalents, potentially altering drug distribution and response profiles [43] [71].
PDO Matrix Specifications: For organoid cultures, Matrigel remains the most widely utilized ECM substrate, though BME and Geltrex offer alternatives with varying protein compositions and polymerization properties [59]. The optimal ECM concentration balances support for 3D structure with nutrient diffusion requirements, typically at 50-80% dilution in cold medium before polymerization [59]. Emerging synthetic ECM alternatives promise better batch-to-batch consistency for standardized drug screening applications.
Growth Factor Requirements
Precise growth factor supplementation dictates long-term culture success and maintenance of tumor cell populations:
Wnt Pathway Activation: R-spondin represents a critical component for gastrointestinal cancer organoids, activating Wnt signaling essential for stem cell maintenance [59]. Optimal concentrations vary by tumor type, with colorectal models typically requiring higher levels than pancreatic or breast cancer organoids.
Growth and Inhibition Balance: Epidermal growth factor (EGF) promotes epithelial proliferation across most cancer types at concentrations ranging 25-100 ng/mL [59]. Simultaneously, Noggin (a BMP pathway inhibitor) prevents differentiation and maintains precursor cell populations at 50-100 ng/mL [59]. Additional supplements including FGF-10, N-acetylcysteine, and B27 enhance viability for specific cancer subtypes.
Diagram 3: Key Signaling Pathways in Culture Conditions
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for PDX and PDO Models
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| ECM Substrates | Matrigel, BME, Geltrex | 3D structural support for organoids | Varying protein concentrations; batch variability concerns [59] |
| Enzymatic Digestion | Collagenase/Hyaluronidase, TrypLE | Tissue dissociation | Concentration and timing varies by tumor type [59] |
| Growth Factors | R-spondin, EGF, Noggin, FGF | Maintain stemness and proliferation | Essential for long-term culture; concentration optimization required [59] |
| ROCK Inhibitor | Y-27632 | Prevents anoikis | Critical during initial establishment and passage [59] |
| Mouse Strains | NSG, NOD/SCID | Immunocompromised hosts | NSG offers highest engraftment rates [71] |
| Media Supplements | B27, N-acetylcysteine | Enhanced viability | Particularly important for gastrointestinal organoids [59] |
The optimization of culture conditions—specifically extracellular matrix composition and growth factor supplementation—profoundly impacts the predictive value of both PDX and PDO cancer models. While both platforms demonstrate equivalent accuracy in forecasting patient treatment responses (70% concordance) [17], their practical implementation differs significantly in terms of temporal requirements, financial investment, and technical expertise.
PDX models maintain superior tumor microenvironment integrity initially but gradually undergo murine stromal replacement, potentially compromising their translational relevance in prolonged studies [43] [71]. PDO systems, while lacking complete microenvironment complexity, offer unprecedented scalability and experimental flexibility for high-throughput drug screening applications [17] [59]. The research reagent toolkit provided herein offers practical guidance for implementing these optimized protocols, enabling researchers to select and refine the most appropriate model system for their specific therapeutic questions. As these technologies continue to evolve, further standardization of culture components will enhance reproducibility and accelerate the translation of preclinical findings to clinical applications.
The rising demand for more predictive and translational preclinical models in oncology has positioned patient-derived xenografts (PDXs) and patient-derived organoids (PDOs) at the forefront of cancer research. While each model offers distinct advantages, a growing body of evidence suggests that their integrated use as matched pairs creates a powerful synergistic platform that surpasses the capabilities of either model in isolation. PDX models, established by implanting human tumor tissues into immunocompromised mice, preserve the histological architecture, cellular heterogeneity, and stromal components of the original tumor, providing an invaluable in vivo context for drug evaluation [7] [24]. Conversely, PDO models—three-dimensional in vitro cultures derived from patient tumors—maintain key molecular features while offering superior scalability, cost-effectiveness, and suitability for high-throughput screening [16] [73]. The creation of matched PDX-PDO pairs from the same patient tumor represents an innovative approach that leverages the complementary strengths of both systems, enabling researchers to bridge the gap between high-throughput in vitro discovery and physiologically relevant in vivo validation [74] [75].
Recent meta-analyses have demonstrated that both PDX and PDO models show comparable predictive accuracy for patient treatment responses, with overall concordance rates of approximately 70% [24] [17]. However, their combined use addresses individual limitations: PDX models are costly, time-consuming, and low-throughput, while PDO models lack the full tumor microenvironment and systemic context [61] [74]. By establishing paired models, researchers can perform initial high-throughput drug screening in PDOs followed by validation of lead compounds in matched PDX models, creating a more efficient and predictive workflow for drug development and personalized medicine approaches [74] [75].
Comparative Analysis of PDX and PDO Models
Characteristics and Applications
Table 1: Key Characteristics of PDX and PDO Models
| Characteristic | PDX Models | PDO Models |
|---|---|---|
| Model Type | In vivo | Ex vivo |
| Patient Recapitulation | Yes, maintains histopathology and heterogeneity [7] | Yes, preserves molecular and phenotypic features [16] |
| Tumor Microenvironment | Yes (from host, but human immune components absent) [7] [61] | Limited, few or no native stromal/immune cells [61] |
| Throughput | Low to medium [74] | High [16] [74] |
| Establishment Time | Several months [61] | Several weeks [61] |
| Cost | High [24] [17] | Relatively low [24] [17] |
| Scalability | Medium [61] | High [16] [61] |
| Genetic Stability | High through early passages [7] | Generally high, though subclonal mutations may occur in prolonged culture [16] |
| Key Applications | Preclinical therapeutic validation, co-clinical trials [7] | High-throughput drug screening, personalized therapy prediction [16] [73] |
Predictive Performance Metrics
Table 2: Predictive Performance of PDX and PDO Models
| Performance Metric | PDX Models | PDO Models |
|---|---|---|
| Overall Concordance with Patient Response | 70% (based on meta-analysis of 267 pairs) [24] [17] | 70% (based on meta-analysis of 144 pairs) [24] [17] |
| Sensitivity | Comparable to PDOs [24] [17] | Comparable to PDXs [24] [17] |
| Specificity | Comparable to PDOs [24] [17] | Comparable to PDXs [24] [17] |
| Association with Patient Survival | Predictive when using low risk-of-bias pairs [24] [17] | Patients with responsive PDOs had prolonged progression-free survival [24] [17] |
| Drug Response Prediction | Recapitulates patient responses to chemotherapy and targeted therapies [7] | High predictive accuracy for chemotherapy and targeted agents [16] [61] |
Establishing Matched PDX-PDO Pairs: Methodological Framework
Workflow for Model Generation
The creation of matched PDX-PDO pairs requires a coordinated workflow that begins with patient tumor tissue acquisition and branches into parallel development of both model types. This integrated approach ensures that both models share a common origin, enabling direct comparison and complementary use throughout the research process.
Detailed Protocol for PDX-Derived Organoid Generation
The conversion of existing PDX models into organoids (PDXOs) provides a strategic approach to rapidly build matched pairs. This method leverages established PDX biobanks while overcoming the throughput limitations of in vivo models [74] [75]. The following protocol outlines key steps for generating PDXOs:
PDX Tumor Harvest: Collect fresh PDX tumors from mice when they reach 200-800 mm³ volume. Remove adjacent non-tumor tissues, necrosis, and calcified areas under sterile conditions [75].
Tissue Processing: Mince the tumor tissue into small fragments (approximately 2-4 mm³) using scalpels or surgical scissors. Digest the fragments with Collagenase B (1-2 mg/mL) in PBS for 20-60 minutes at 37°C with gentle agitation [74] [75].
Cell Strainer Filtration: Pass the digested tissue suspension through a 100 μm cell strainer to remove debris and undigested fragments. Wash the flow-through with cold PBS and centrifuge at 300-500 × g for 5 minutes [74].
Matrix Embedding: Resuspend the cell clusters in pre-cooled Basement Membrane Extract (BME) or Matrigel solution. Plate the suspension as solid droplets in culture plates and allow them to solidify at 37°C for 20-30 minutes [75].
Organoid Culture: Add appropriate organoid culture medium supplemented with tissue-specific growth factors. Refresh the medium every 2-3 days and monitor organoid growth using light microscopy [74] [75].
Passaging and Expansion: Passage organoids every 7-14 days by disrupting the BME droplets mechanically and enzymatically (using trypsin). Re-embed the organoid fragments in fresh BME for continued expansion [75].
Cryopreservation: Cryopreserve organoids in freezing medium containing 10 μM Y-27632 (ROCK inhibitor) for long-term storage in liquid nitrogen [74].
Essential Research Reagents and Materials
Table 3: Key Reagents for Establishing Matched PDX-PDO Pairs
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Basement Membrane Extract (BME)/Matrigel | Provides 3D extracellular matrix support for organoid growth and polarization [16] [75] | Used as scaffold for PDO and PDXO culture; enables proper 3D architecture formation [74] [75] |
| Collagenase B | Enzymatic digestion of tumor tissues into smaller cell aggregates and clusters [74] | Processing PDX tissues for organoid generation; helps maintain cell-cell contacts while dissociating matrix [75] |
| Y-27632 (ROCK inhibitor) | Prevents anoikis (cell death after detachment); enhances survival of dissociated cells [75] | Added to culture medium during passaging and cryopreservation of organoids [74] |
| Tissue-Specific Growth Factor Cocktails | Supports expansion of tissue-specific stem/progenitor cells; maintains lineage identity [16] [61] | Formulations vary by cancer type (e.g., Wnt agonists for colorectal, EGF for gastrointestinal) [61] |
| Immunocompromised Mice | Host organisms for PDX engraftment; lack immune rejection of human tissues [7] [75] | Balb/c nude or NSG mice commonly used for PDX establishment and maintenance [75] |
Research Applications of Matched PDX-PDO Pairs
High-Throughput Drug Screening and Validation
The combined use of matched PDX-PDO pairs creates an efficient screening pipeline that leverages the strengths of both systems. PDOs enable rapid, cost-effective screening of large compound libraries, while matched PDXs provide physiological context for validating lead compounds [74]. This approach is particularly valuable for "matrix" screening strategies that simultaneously evaluate multiple compounds across numerous models to identify both effective agents and responsive patient populations [74]. Research has demonstrated that PDXOs maintain similar drug response profiles to their parental PDXs, with high concordance in IC50 values for standard chemotherapeutic and targeted agents [74]. This biological equivalence enables researchers to use PDXOs for initial high-throughput screening followed by confirmation in a subset of matched PDX models, significantly accelerating the drug discovery process while reducing costs and animal use [74] [17].
Personalized Medicine and Co-Clinical Trials
Matched PDX-PDO pairs serve as powerful "avatar" models for functional precision medicine, allowing clinicians to test therapeutic options for individual patients outside the body [61] [36]. In this approach, tumor tissues from patients are used to establish both PDX and PDO models, which are then exposed to the same therapies being considered for the patient. The models' responses inform treatment selection, potentially improving outcomes. A landmark study by Vlachogiannis et al. demonstrated that PDOs could predict patient responses with 100% sensitivity and 93% specificity [61]. Similarly, PDX models have been used in co-clinical trials where mice bearing patient-derived tumors are treated in parallel with the corresponding patients, creating a feedback loop that enhances understanding of treatment responses and resistance mechanisms [7] [36]. The integration of both models provides complementary information—PDOs offer rapid turnaround for urgent clinical decisions, while PDXs provide additional physiological context for interpreting results.
Biological and Translational Studies
Beyond direct drug screening, matched PDX-PDO pairs enable sophisticated studies of tumor biology and therapeutic resistance. The paired models allow researchers to investigate fundamental cancer processes such as tumor heterogeneity, clonal evolution, and metastasis in both in vitro and in vivo contexts [16] [73]. PDXOs can be genetically engineered using CRISPR-Cas9 to introduce specific mutations or reporter genes, then re-implanted into mice to study their impact on tumor behavior [16]. This seamless transition between in vitro manipulation and in vivo validation accelerates functional genomics studies. Additionally, the paired model system facilitates investigation of the tumor microenvironment's role in drug response by comparing results from the stroma-deficient PDOs with the stroma-containing PDXs, helping to distinguish cell-autonomous from microenvironment-dependent drug resistance mechanisms [7] [73].
Current Challenges and Future Directions
Technical and Biological Limitations
Despite their significant potential, the implementation of matched PDX-PDO pairs faces several challenges. Establishment success rates vary considerably across cancer types, with particularly low efficiency for some malignancies such as esophageal cancer, where organoid establishment rates can be as low as 31-68% [61]. The absence of a fully functional human immune system in both models limits their utility for immuno-oncology studies, though emerging approaches such as PDO-immune cell co-cultures and humanized PDX models are addressing this gap [16] [74]. Genetic drift remains a concern, particularly during extended culture, where subclonal mutations may alter drug response profiles [16]. Additionally, the high costs and specialized expertise required for maintaining both model systems present practical barriers to widespread adoption [24] [36].
Technological Innovations and Framework Integration
Future advances in matched PDX-PDO methodologies will likely focus on enhancing physiological relevance and standardization. The "Organoid Plus and Minus" framework proposes complementary strategies: technological augmentation to increase complexity ("Plus") and culture system refinement to improve reproducibility ("Minus") [16]. Low-growth factor media formulations that reduce dependence on exogenous cytokines show promise for maintaining more physiological signaling environments [16]. Defined, tunable biomaterials are being developed to replace poorly characterized matrices like Matrigel, enabling better control over the mechanical and biochemical microenvironment [16]. Integration with microfluidic organ-on-a-chip platforms provides precise control over nutrient and growth factor gradients, while advanced imaging technologies enable real-time monitoring of drug responses [16]. These innovations, combined with standardized biobanking practices and multi-omics characterization, will further establish matched PDX-PDO pairs as indispensable tools in translational oncology research.
The strategic integration of matched PDX-PDO pairs represents a paradigm shift in preclinical cancer modeling, effectively combining the high-throughput capabilities of in vitro systems with the physiological relevance of in vivo models. This complementary approach enables researchers to overcome the individual limitations of each model while leveraging their respective strengths for more efficient and predictive drug development. As technological innovations continue to enhance the sophistication and accessibility of both platforms, their coordinated use is poised to accelerate the translation of basic cancer discoveries into effective personalized therapies, ultimately advancing the field of precision oncology. The systematic implementation of matched PDX-PDO pairs offers a powerful framework for bridging the critical gap between preclinical findings and clinical success in cancer drug development.
In the evolving landscape of preclinical cancer research, patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as transformative tools that more accurately recapitulate human tumor biology compared to traditional cell lines. However, maintaining the genomic stability and phenotypic fidelity of these models across serial passages presents significant technical challenges that can compromise their predictive validity and translational relevance. Quality control measures are therefore paramount to ensure these complex biological models retain key characteristics of the original patient tumors throughout their experimental lifespan. The fundamental importance of robust quality control is underscored by meta-analyses revealing an overall 70% concordance in treatment response between patients and matched models, with no significant differences between PDX and PDO platforms [17]. This comparative guide examines the methodologies, metrics, and practical approaches for preserving model integrity in both PDX and PDO systems, providing researchers with a structured framework for quality assurance in preclinical studies.
Comparative Performance Metrics: PDX vs. PDO Models
Understanding the relative strengths and limitations of PDX and PDO models requires systematic evaluation across multiple quality parameters. The table below summarizes key comparative metrics based on current research findings:
Table 1: Comparative Quality Metrics for PDX and PDO Models
| Quality Parameter | PDX Models | PDO Models | Key Supporting Evidence |
|---|---|---|---|
| Overall Predictive Concordance | 70% with matched patients [17] | 70% with matched patients [17] | No significant difference in predictive accuracy between platforms [17] |
| Genomic Stability Assessment | Exome sequencing shows high concordance with original tumors (>24/25 allelic alterations preserved) [76] | RNA profiling demonstrates molecular similarity to native tissue [77] | PDOs maintain critical genomic features of matched PDX tumors [76] |
| Phenotypic Preservation | Retains histological architecture and cellular heterogeneity [1] | Recapitulates microarchitecture and physiology of tissue of origin [77] | Organoids retain original tissue's properties for months to years [77] |
| Passage-related Drift | Mouse-specific evolution occurs beyond passage 5 [17] | Media composition influences differentiation status [76] | WNT in culture media affects organoid phenotypes through population selection [76] |
| Stromal Components | Retains human tumor stroma initially, replaced by mouse stroma over time [1] | Lacks vascular and stromal complexity [17] | PDO limitation precludes study of immunotherapeutics and anti-angiogenic agents [17] |
These quantitative comparisons highlight important considerations for model selection based on research objectives. PDX models generally demonstrate superior preservation of tumor microenvironmental elements, particularly in early passages, while PDO platforms offer greater scalability and avoidance of species-specific artifacts. Both platforms show equivalent performance in predicting patient treatment responses when proper quality control measures are implemented [17].
Essential Methodologies for Quality Assessment
Genomic Stability Monitoring Protocols
Maintaining genomic integrity across passages requires regular molecular characterization. The following protocols represent best practices for genomic quality control:
DNA-Based Authentification Method:
- Procedure: Extract genomic DNA from model samples at early and late passages (recommended at every 3-5 passages). Perform short tandem repeat (STR) profiling or single nucleotide polymorphism (SNP) genotyping and compare to original patient tissue.
- Quality Threshold: ≥80% match with original profile confirms maintained identity [1].
- Technical Replicates: Perform in triplicate to ensure consistency.
Whole Exome Sequencing (WES) Protocol:
- Procedure: Conduct WES on model samples at critical passages (P1, P3, P5, P10, then every 10 passages). Compare variant calls to original tumor using established bioinformatics pipelines.
- Validation Standard: PDX models should maintain >90% of original tumor mutations across passages [76]. One study demonstrated 24 of 25 allelic alterations matched between PDX and PXO models [76].
- Data Analysis: Focus on driver mutations and copy number variations in cancer-relevant genes.
Phenotypic Consistency Evaluation
Preserving morphological and functional characteristics requires multidimensional assessment:
Histopathological Validation Workflow:
- Sample Preparation: Fix model samples in formalin and embed in paraffin using standard protocols. Section at 4-5μm thickness.
- Staining Protocol: Perform hematoxylin and eosin (H&E) staining and tissue-specific immunohistochemistry (IHC) for markers such as cytokeratin 19 for pancreatic models [76].
- Assessment Criteria: Compare architectural features (gland formation, cribriform patterns) to original tumor. PDX models should recapitulate spatial structure and intratumor heterogeneity [1].
Differentiation Status Monitoring:
- Procedure: Analyze expression of differentiation markers (e.g., GATA6 in pancreatic models) via qRT-PCR or Western blot at regular passages.
- Critical Parameter: Culture conditions significantly impact differentiation. Studies show WNT-containing media can alter GATA6 expression in pancreatic organoids [76].
- Documentation: Maintain detailed records of morphological changes across passages.
The Scientist's Toolkit: Essential Research Reagents
Implementing robust quality control requires specific reagents and materials. The following table details essential solutions for maintaining model fidelity:
Table 2: Essential Research Reagents for Quality Control
| Reagent Category | Specific Examples | Function in Quality Control | Application Notes |
|---|---|---|---|
| Extracellular Matrices | Engelbreth-Holm-Swarm (EHS) murine sarcoma ECM (e.g., Matrigel) [78] | Provides 3D structural support for organoid growth | Batch-to-batch variation requires validation; final concentration 10-18 mg/ml [78] |
| Stem Cell Niche Factors | Wnt-3a, R-spondin, Noggin, EGF [77] [78] | Maintains stemness and enables long-term culture | Concentrations vary by tissue type; WNT presence influences differentiation [76] |
| Differentiation Modulators | FGF family members (FGF7, FGF10), HGF, nicotinamide [77] | Promotes tissue-specific morphogenesis and self-renewal | Essential for lung organoid development [77] |
| Passaging Enzymes | Collagenase, Dispase, Trypsin-EDTA [78] | Enables dissociation and replating while maintaining viability | Mechanical dissociation alternative for sensitive models |
| Cryopreservation Solutions | DMSO-containing medium with serum alternatives [78] | Long-term storage while maintaining viability and functionality | Standardized freezing protocols ensure recovery consistency |
Experimental Workflows for Quality Monitoring
Implementing systematic quality control requires standardized operational procedures. The following diagrams illustrate key workflows for maintaining model integrity across passages.
PDX Model Quality Control Pathway
PDX Quality Control Workflow: This pathway systematically evaluates both genomic and phenotypic integrity at each passage to identify drift and maintain model fidelity.
Organoid Culture Quality Assurance
Organoid Quality Assurance Process: This workflow emphasizes regular assessment of morphology, differentiation status, and functionality, with particular attention to media composition effects on model behavior.
Impact of Culture Conditions on Model Stability
The stability of both PDX and PDO models is profoundly influenced by specific culture conditions and technical handling. Understanding these factors is essential for maintaining quality across passages:
Media Composition Effects: Organoid differentiation status is significantly affected by media formulations. Studies demonstrate that WNT-containing media can alter GATA6 expression levels in pancreatic organoids compared to WNT-free conditions [76]. This has functional consequences, as organoids maintained in WNT-free pancreatic tumor organoid media (PTOM) showed different growth rates and morphological features [76].
Passage-related Evolution: PDX models undergo gradual murine-specific stromal replacement, with human stroma typically replaced by mouse stroma beyond passage 5 [17] [1]. This transition can affect drug response profiles, particularly for therapeutics targeting human-specific stromal interactions. Regular monitoring of human-mouse cell ratios is recommended.
Matrix Considerations: Organoid culture requires extracellular matrix components that introduce batch-to-batch variability. Matrigel, derived from Engelbreth-Holm-Swarm murine sarcoma, is commonly used but lacks defined composition [78]. Systematic testing of new lots is essential before implementation in long-term studies.
Ensuring genomic stability and phenotypic consistency across passages in PDX and PDO models requires a multifaceted approach integrating regular molecular validation, morphological assessment, and environmental standardization. While both platforms demonstrate equivalent predictive accuracy for treatment response [17], they present distinct technical challenges that necessitate tailored quality control strategies. PDX models demand vigilant monitoring of species crossover and stromal composition changes, whereas PDO systems require precise control of culture conditions that influence differentiation states. By implementing the comprehensive quality framework outlined in this guide—including standardized protocols, essential reagent management, and systematic workflow monitoring—researchers can maximize the translational relevance of these advanced preclinical models throughout their experimental lifespan, ultimately enhancing the reliability of drug development and precision oncology initiatives.
Evidence-Based Validation: Comparative Analysis of Clinical Predictive Power
In the pursuit of precision oncology, researchers rely on preclinical avatar models to predict patient responses to therapy. Among the most prominent tools are Patient-Derived Xenografts (PDX) and Patient-Derived Organoids (PDO). PDX models are established by transplanting fresh human tumor tissue into immunocompromised mice, providing an in vivo system that preserves tumor architecture and heterogeneity [1]. PDOs are 3D in vitro structures cultured from patient tumor cells, which maintain key aspects of the original tumor's histo-architecture and genetic diversity [43]. Understanding the relative strengths and limitations of these models is crucial for their appropriate application in both basic research and clinical decision-making. This guide provides a direct comparison of their performance in predicting patient outcomes, supported by experimental data and methodological details.
Predictive Performance: Quantitative Analysis
A 2025 systematic review and meta-analysis directly compared the predictive accuracy of PDX and PDO models from solid tumors treated with identical anti-cancer agents as their matched patient [69]. This comprehensive analysis, which included 411 patient-model pairs (267 PDX and 144 PDO), provides the most current head-to-head comparison of these technologies.
Table 1: Overall Predictive Concordance of PDX and PDO Models
| Metric | PDX Models | PDO Models | Overall Combined |
|---|---|---|---|
| Overall Concordance | ~70% (from 267 pairs) | ~70% (from 144 pairs) | 70% |
| Sensitivity | Comparable to PDO | Comparable to PDX | No significant difference |
| Specificity | Comparable to PDO | Comparable to PDX | No significant difference |
| Positive Predictive Value | Comparable to PDO | Comparable to PDX | No significant difference |
| Negative Predictive Value | Comparable to PDO | Comparable to PDX | No significant difference |
| Association with Patient Survival | Present only in low risk-of-bias pairs | Present (prolonged PFS in responders) | N/A |
The analysis concluded that there were no significant differences in predictive accuracy between PDX and PDO models across all measured metrics [69]. This fundamental equivalence in performance occurs despite their very different biological environments and technical requirements.
Table 2: Technical and Practical Characteristics of PDX vs. PDO Models
| Characteristic | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Model Definition | Tumor tissues implanted into immunocompromised mice [1] | Miniature 3D in vitro structures from patient tumor samples [43] |
| Tumor Microenvironment | More complex, includes mouse stromal components [1] | Lacks a complete tumor microenvironment [26] |
| Experimental Timeline | Several months [43] | Shorter, enables more rapid testing [26] |
| Cost & Throughput | Lower throughput, higher cost [79] [69] | High-throughput drug screening possible [43] [26] |
| Key Advantages | Preserves tumor architecture and heterogeneity; enables in vivo drug PK/PD studies [1] | Maintains tumor structure and genetic diversity; amenable to long-term expansion and cryopreservation [43] |
| Key Limitations | Time-consuming, costly, mouse stromal cells replace human components [43] | Lack tumor microenvironment, may not fully capture systemic effects [26] |
| Ideal Use Case | Comprehensive in vivo efficacy studies, co-clinical trials [7] | High-throughput drug screening, biobanking, personalized treatment planning [43] [26] |
Experimental Protocols for Model Establishment and Validation
PDX Model Establishment Protocol
The standard workflow for creating PDX models involves specific reagents and a multi-step process [1]:
- Tumor Acquisition: Fresh tumor tissue is obtained from patient biopsies or surgical resections and maintained in a sterile, cold preservation medium.
- Tissue Processing: The sample is cut into small fragments (typically 2-3 mm³) using surgical tools.
- Implantation: Tumor fragments are implanted into immunocompromised mice. Common implantation sites include:
- Subcutaneous (most common)
- Orthotopic (into the organ/tissue of origin)
- Renal capsule
- Intrafat pad
- Engraftment and Passage: Mice are monitored for tumor growth. Upon reaching a predefined volume (e.g., 1-2 cm³), the tumor is harvested and re-implanted into new mice to expand the model (passaging).
- Cryopreservation: Tumor fragments from early passages can be cryopreserved in freezing medium containing DMSO to create a renewable resource.
PDO Model Establishment Protocol
The general protocol for generating PDOs includes the following key steps [43] [80]:
- Tissue Dissociation: Patient tumor tissue is minced and enzymatically digested into a single-cell suspension or small cell clusters.
- Matrix Embedding: The cell suspension is mixed with a basement membrane extract (e.g., Matrigel) which provides a 3D scaffold for growth.
- Culture: The matrix-embedded cells are plated and submerged in a specialized culture medium containing a cocktail of growth factors (e.g., Wnt, R-spondin, Noggin) necessary for stem cell maintenance and organoid growth.
- Expansion and Passaging: Established organoids are enzymatically or mechanically broken up and re-embedded in fresh matrix for expansion.
- Biobanking: Organoids can be cryopreserved in freezing medium for long-term storage in liquid nitrogen, enabling the creation of large-scale living biobanks.
The following diagram illustrates the parallel workflows for establishing and applying these two critical models.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful establishment and experimentation with PDX and PDO models require a suite of specialized reagents and tools.
Table 3: Key Reagent Solutions for PDX and PDO Research
| Reagent / Material | Function | Application |
|---|---|---|
| Immunocompromised Mice (e.g., NOD-SCID, NSG) | Provide an in vivo environment without graft rejection. | PDX Model Establishment [1] |
| Basement Membrane Extract (e.g., Matrigel) | Acts as a 3D scaffold to support complex organoid structure. | PDO 3D Culture [80] |
| Specialized Growth Media | Contains precise growth factor cocktails (Wnt, R-spondin, Noggin) for stem cell maintenance. | PDO Culture & Expansion [43] |
| Tissue Dissociation Enzymes (e.g., Collagenase, Trypsin) | Break down the extracellular matrix to create single-cell suspensions or small clusters. | Initial Processing for PDO & PDX [43] [1] |
| Cryopreservation Medium (with DMSO) | Protects cells from ice crystal formation during freezing for long-term storage. | Biobanking of PDO & PDX Tumors [43] [1] |
Emerging Technologies and Future Directions
The field of preclinical modeling is being enhanced by the integration of advanced technologies. Machine learning is now being applied to drug response data from patient-derived cell cultures to impute or predict the efficacy of a wider range of drugs, thereby increasing the informational output from screening campaigns [79]. Furthermore, organ-on-a-chip systems and the integration of functional biomaterials are being developed to create more sophisticated PDO co-culture environments that better capture tumor–stroma–immune interactions, potentially overcoming the current limitation of PDOs lacking a complete tumor microenvironment [81] [80].
Direct comparative evidence indicates that PDX and PDO models demonstrate statistically equivalent overall concordance with patient treatment responses, approximately 70% [69]. The choice between these models, therefore, is not one of superior predictive power but of strategic application. PDX models offer a more physiologically relevant in vivo system for studying complex systemic interactions and pharmacokinetics, while PDO models provide a rapid, scalable, and cost-effective platform for high-throughput drug screening and personalized therapy selection [43] [26]. Researchers and drug developers should base their model selection on the specific research question, available resources, and desired throughput, with a growing trend towards using these models as complementary rather than competing tools in the precision oncology pipeline.
In the pursuit of precision oncology, patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as pivotal tools for predicting therapeutic efficacy. These biomimetic avatars bridge the critical gap between traditional preclinical models and human clinical response, enabling more personalized treatment strategies [17] [82]. However, their widespread clinical integration necessitates rigorous, quantitative validation of their predictive performance. For researchers and drug development professionals, understanding the comparative predictive accuracy—quantified through sensitivity, specificity, and concordance metrics—is essential for model selection and translational research design.
This guide provides a structured comparison of PDX and PDO models based on recent meta-analyses and experimental studies. We synthesize quantitative performance data, detail standardized methodological protocols, and visualize key workflows to support evidence-based decision-making in preclinical oncology research.
Quantitative Comparison of Predictive Performance
A direct comparative meta-analysis of studies involving solid tumors revealed that both PDX and PDO models demonstrate statistically comparable performance in predicting patient-specific drug responses [17].
Table 1: Overall Predictive Performance of PDX and PDO Models
| Metric | Overall Value (PDX & PDO Combined) | PDX-Specific Performance | PDO-Specific Performance | Statistical Significance (P-value) |
|---|---|---|---|---|
| Overall Concordance | 70% | Comparable to overall | Comparable to overall | Not Significant |
| Sensitivity | Comparable | Comparable | Comparable | Not Significant |
| Specificity | Comparable | Comparable | Comparable | Not Significant |
| Positive Predictive Value (PPV) | Comparable | Comparable | Comparable | Not Significant |
| Negative Predictive Value (NPV) | Comparable | Comparable | Comparable | Not Significant |
| Association with Patient PFS | N/A | Held only in low-bias pairs | Strong association demonstrated | N/A |
Table 2: Performance in Colorectal Cancer (CRC) Specific PDO Studies
| Metric | Reported Value in CRC PDOs | Clinical Context |
|---|---|---|
| Positive Predictive Value (PPV) | 68% | Organoid-informed treatment selection |
| Negative Predictive Value (NPV) | 78% | Organoid-informed treatment selection |
The data indicates that the primary differentiators for model selection are not based on predictive power but on practical and ethical considerations. PDOs offer a compelling advantage with lower financial and ethical burdens, faster establishment times, and suitability for higher-throughput screening compared to PDX models [17] [8].
Experimental Protocols for Model Validation
The reliable quantification of predictive accuracy depends on rigorously standardized experimental protocols. The following methodologies are critical for generating high-quality, comparable data.
Systematic Review and Meta-Analysis Protocol
The comparative performance data in Section 2 was derived from a comprehensive systematic review and meta-analysis conducted according to PRISMA guidelines [17].
- Search Strategy: A systematic search of MEDLINE and EMBASE databases was performed for the period from January 1, 2002, to December 10, 2022, yielding over 30,000 initial results. The review protocol was prospectively registered with PROSPERO (ID: CRD42023387229) [17].
- Inclusion/Exclusion Criteria: Studies were included if they involved PDX or PDO models from human solid tumors treated with systemic therapies, with reported response data for both the model and the matched patient to the identical agent(s). Liquid tumors, models derived through an intermediate step, and studies involving only immunotherapies or hormone therapies were excluded [17].
- Data Extraction and Harmonization: Treatment response in models was recorded as defined by the original authors. Patient response was preferentially assessed using RECIST v1.1 criteria. For PDX models tested with multiple doses, the closest murine equivalent of the clinical dose was selected for analysis to ensure translational relevance [17].
- Risk of Bias Assessment: A critical step involved applying a standardized quality assessment tool adapted from the Newcastle-Ottawa scale. This tool evaluated selection bias, model validation, outcome ascertainment, follow-up length, reporting sufficiency, and the use of technical replicates. Patient-model pairs were classified as high-reliability (low risk of bias) if they met at least 4 out of 6 criteria [17].
In Vitro Drug Sensitivity Testing in PDOs
A common protocol for assessing drug response in PDOs, particularly for digestive system cancers, involves the following steps [6] [83]:
- Organoid Establishment: Patient tumor tissue from biopsy or surgical resection is mechanically and enzymatically digested into single cells or small clusters.
- 3D Culture: The tumor cells are embedded in a supportive extracellular matrix (e.g., Matrigel) and cultured in specialized media containing growth factors tailored to the tissue of origin.
- Drug Exposure: Organoids are exposed to a range of concentrations of the anti-cancer drug(s) of interest. Commonly tested therapies for CRC, for example, include 5-fluorouracil (5-FU), oxaliplatin, irinotecan, and their combinations (FOLFOX, FOLFIRI) [6].
- Response Readout: Viability is measured after a defined period (e.g., 5-7 days) using assays such as ATP-based cell viability assays (CellTiter-Glo) or organoid morphology-based imaging. A threshold for sensitivity/resistance (e.g., IC50) is applied to classify the response.
In Vivo Drug Efficacy Testing in PDX Models
The typical workflow for a PDX drug trial, as used in studies that contributed to the meta-analysis, is as follows [84]:
- Model Generation: Immunocompromised mice are implanted with patient tumor tissue fragments.
- Treatment Cohorts: Once tumors are established and reach a predetermined volume, mice are randomized into treatment or control groups. The treatment group receives the candidate drug, while the control group receives a vehicle.
- Dosing and Monitoring: The drug is administered via a route and at a dose equivalent to the human clinical dose. Tumor volumes and mouse body weights are measured regularly over 2-3 weeks.
- Endpoint Analysis: Tumor growth inhibition is calculated by comparing the tumor volumes (or volume changes) in the treatment group versus the control group at the end of the study. Multiple measures of tumor growth, such as final volume, area under the growth curve, and regression analysis, can be used for a more robust classification of response [84].
Diagram Title: Workflow for Validating PDX and PDO Predictive Accuracy
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful establishment and drug testing of PDX and PDO models rely on a suite of specialized reagents and platforms.
Table 3: Essential Research Reagents and Solutions for Model Establishment and Screening
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| Matrigel / Geltrex | Provides a 3D extracellular matrix scaffold for organoid growth and polarization. | Used for embedding dissociated tumor cells to establish PDO cultures [6] [83]. |
| Defined Growth Media | Chemically defined media supplemented with tissue-specific growth factors (e.g., EGF, Noggin, R-spondin). | Supports the long-term expansion and maintenance of PDOs while preserving original tumor characteristics [6] [83]. |
| Immunodeficient Mice | Host organisms that allow the engraftment and growth of human-derived tumor tissues without immune rejection. | Essential for establishing and propagating PDX models (e.g., NSG, NOG strains) [85] [84]. |
| Cell Viability Assays | Biochemical assays (e.g., ATP-based luminescence) to quantify cell viability and drug sensitivity in a high-throughput manner. | Used for screening drug responses in PDO plates to determine IC50 values [6]. |
| AI-Powered Analysis Platforms | Software for automated image analysis, organoid classification, and drug response prediction. | Platforms like SiQ-3D and OrBITS automate the analysis of organoid drug screening data, enhancing reproducibility and throughput [83]. |
The quantitative evidence demonstrates that PDX and PDO models possess comparable predictive accuracy for clinical drug response, with overall concordance rates around 70%. The choice between these powerful models should therefore be guided by specific research objectives: PDX models may be preferable for studying in vivo tumor-stroma interactions, while PDOs offer a scalable, ethical, and cost-effective platform for high-throughput drug screening and personalized therapy prediction. As the field evolves, the integration of standardized protocols, advanced biomaterials, and artificial intelligence will further enhance the reliability and clinical translation of both models, solidifying their role in advancing precision oncology.
In the era of precision oncology, patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as transformative tools for drug development and therapeutic prediction. These models aim to bridge the translational gap between traditional laboratory models and human clinical trials by preserving critical characteristics of original patient tumors [1]. However, despite their widespread adoption and demonstrated utility, discordant cases where model predictions diverge from actual clinical outcomes present significant scientific and clinical challenges. Understanding the sources and implications of these discrepancies is essential for improving model fidelity and translational accuracy.
The fundamental premise underlying these advanced models is their ability to recapitulate human tumor biology with greater fidelity than traditional cell lines. PDX models, established by transplanting patient tumor fragments into immunodeficient mice, maintain key aspects of tumor heterogeneity and microenvironmental interactions [71]. PDOs, which are three-dimensional structures derived from patient tumor cells and cultured in vitro, preserve histological architecture and molecular features of the original tumors while offering greater scalability and throughput [6]. Yet both approaches face inherent limitations that can contribute to predictive failures when their results are applied to clinical decision-making.
Model-Specific Limitations and Failure Mechanisms
Patient-Derived Xenograft Limitations
PDX models, while valuable, suffer from several technological constraints that can compromise their predictive value. A critical limitation stems from the immune system mismatch in conventional PDX models, which require immunocompromised mouse hosts to prevent graft rejection. This absence of a functional human immune system fundamentally alters tumor biology and precludes accurate evaluation of immunotherapies, which now constitute a cornerstone of cancer treatment [43] [1]. Additionally, the stromal replacement phenomenon occurs over successive passages, where human stromal components are gradually replaced by murine counterparts, potentially modifying tumor-stromal interactions that influence drug response [43].
The practical constraints of PDX models also impact their predictive reliability. The extended timeframe required for PDX establishment (typically 2-4 months for initial engraftment, with additional time needed for drug studies) often exceeds clinically relevant windows for treatment decisions in aggressive malignancies [43] [71]. Furthermore, clonal selection pressures during engraftment and passage can distort original tumor heterogeneity, as only subsets of tumor cells successfully proliferate in the murine host [43]. Genetic analyses of PDX models have demonstrated that they may capture only a fraction of the mutation spectrum present in original patient tumors, with potential emergence of additional mutations during culture [43].
Patient-Derived Organoid Limitations
While organoid technology offers significant advantages for high-throughput applications, PDO models face their own distinct set of challenges. The most significant limitation is the absence of tumor microenvironment, including vascular networks, immune cells, and stromal components that profoundly influence tumor behavior and therapeutic response [86] [35]. This deficiency is particularly problematic for evaluating therapies that target microenvironmental interactions or depend on immune effector functions.
Technical constraints also impact organoid predictive validity. The restricted tumor spectrum currently limits organoid establishment primarily to epithelial-derived solid tumors, with variable success rates across different cancer types [35]. Additionally, the culture-induced adaptations may select for cellular subpopulations with enhanced in vitro survival capabilities, potentially skewing representation of original tumor heterogeneity [11]. The artificial Matrigel environment and optimized growth factor cocktails create conditions that differ substantially from the in vivo milieu, potentially altering cellular behavior and drug sensitivity profiles.
Table 1: Key Limitations of PDX and PDO Models Contributing to Clinical Discordance
| Limitation Category | PDX Models | PDO Models |
|---|---|---|
| Microenvironment | Progressive murine stromal replacement; Lack of functional human immune system | Absence of vascular, immune, and stromal components; Artificial extracellular matrix |
| Technical Constraints | Extended establishment time (2-6 months); High cost; Variable engraftment rates | Limited to epithelial tumors; Culture-induced adaptations; Variable establishment success |
| Tumor Representation | Clonal selection during engraftment; Genetic drift during passages | Selection for in vitro survival subpopulations; Potential loss of original heterogeneity |
| Drug Testing Limitations | Altered drug pharmacokinetics in mice; Inability to test immunotherapies in standard models | Absence of pharmacokinetic considerations; Lack of immune-mediated effects |
Case Studies of Model-Clinical Outcome Discordance
The SELECT Trial: A Paradigm of Predictive Failure
The Selenium and Vitamin E Cancer Prevention Trial (SELECT) represents a landmark case of discordance between preclinical predictions and clinical outcomes. Extensive epidemiological and preclinical data had suggested that both selenium and vitamin E were protective against prostate cancer, with numerous in vitro studies demonstrating anti-proliferative, pro-apoptotic, and antioxidant mechanisms in advanced prostate cancer cell lines [86]. However, the SELECT trial, a phase III clinical trial enrolling 35,533 men, found that not only did these antioxidants fail to reduce prostate cancer incidence, but vitamin E was associated with a statistically significant 17% increased risk of the disease [86].
This dramatic failure of prediction was subsequently attributed to fundamental limitations in the preclinical models employed. The traditional two-dimensional cell line models used for these studies were derived from advanced cancers and failed to model the early carcinogenesis processes relevant to prevention [86]. Additionally, these models lacked the physiological cell-matrix interactions and tissue architecture that influence cellular behavior and drug response. When researchers later utilized three-dimensional organoid cultures that better recapitulated in vivo prostate biology, the SELECT trial results were successfully replicated, with vitamin E showing no protective effect and potentially enhancing proliferation in certain contexts [86]. This case underscores the critical importance of selecting models with appropriate biological context for the research question being addressed.
Ovarian Clear Cell Carcinoma: Divergent Drug Responses Across Platforms
A comprehensive comparative analysis of multiple models derived from the same ovarian clear cell carcinoma (OCCC) patient provided striking evidence of how model selection can dramatically influence therapeutic predictions [11]. In this study, researchers established seven distinct models from a single patient tumor: four conventional cell lines, two PDOs, and one PDX. When these models were tested against the same chemotherapeutic agents the patient had received clinically (carboplatin, doxorubicin, and gemcitabine), the results revealed profound discordance.
The patient had demonstrated clinical resistance to all three agents. Similarly, both the PDX and PDO models displayed resistance profiles that mirrored the patient's clinical outcome. In stark contrast, the conventional 2D cell lines derived from the same tumor showed significant sensitivity to these same chemotherapeutic agents [11]. Transcriptomic analysis confirmed that the PDX and PDO models clustered together and with the original patient tumor, while the cell lines showed distinct expression profiles. This case illustrates how more advanced models that preserve tissue architecture and heterogeneity can provide superior clinical prediction compared to traditional reductionist approaches, while also highlighting how different models from the same tumor can yield contradictory results.
Statistical Insufficiency: The Number Matters
Beyond biological considerations, statistical design factors significantly contribute to discordant predictions. A sophisticated analysis of preclinical experimental designs in glioblastoma PDX models demonstrated that the number of distinct PDX lines utilized profoundly impacts result reproducibility and predictive accuracy [87]. Researchers empirically evaluated statistical power for designs utilizing varying numbers of PDX lines (1-20) and animals per line (1-10).
The findings revealed that experiments using only a single PDX line required substantial subsampling (6-9 mice per treatment group) to detect clinically relevant survival differences of 100-135 days. In contrast, designs incorporating multiple PDX lines achieved superior statistical power with far fewer animals per line [87]. For instance, a design using 10 PDX lines had >80% power to detect a 135-day survival difference with just one mouse per PDX per treatment. This research highlights how underpowered preclinical studies utilizing insufficient model diversity represent a major source of discordance with clinical outcomes, where patient populations inherently encompass substantial inter-tumor heterogeneity.
Table 2: Documented Cases of Model-Clinical Outcome Discordance
| Clinical Context | Preclinical Prediction | Clinical Reality | Identified Causes of Discordance |
|---|---|---|---|
| SELECT Prevention Trial [86] | Selenium and vitamin E reduce prostate cancer risk | No reduction; Vitamin E increased risk | Advanced disease models unsuitable for prevention studies; Lack of physiological context in 2D models |
| OCCC Chemotherapy [11] | 2D cell lines predicted sensitivity to carboplatin, doxorubicin, gemcitabine | Patient refractory to all three agents | Loss of tumor heterogeneity in 2D cultures; Absence of microenvironmental influences |
| PDX Predictive Accuracy [87] | Underpowered single-PDX studies show strong treatment effects | Heterogeneous patient responses in clinic | Insufficient representation of tumor heterogeneity; Inadequate experimental design |
Methodological Approaches for Discordance Analysis
Experimental Workflows for Model Validation
Establishing robust methodologies for comparing model predictions with clinical outcomes requires systematic approaches. For therapeutic response validation, the following workflow has demonstrated utility:
Tumor Collection and Processing: Fresh tumor tissues from surgical resection or biopsies are processed within strict time constraints (typically <1 hour from resection to preservation or processing) to maintain viability [11]. Tissues are divided for parallel model development, molecular characterization, and histopathological analysis.
Parallel Model Establishment: Both PDX and PDO models are established simultaneously from the same tumor sample. For PDX, tumor fragments (3-5 mm³) are implanted subcutaneously or orthotopically into immunocompromised mice (e.g., NSG or NOD-SCID strains) [71]. For PDOs, tumor tissues undergo enzymatic and mechanical dissociation before embedding in extracellular matrix (e.g., Matrigel) with specialized media formulations supporting stem cell growth [6] [11].
Molecular Characterization: Comprehensive genomic, transcriptomic, and proteomic profiling establishes baseline similarity between models and originating tumor. This includes whole-exome sequencing, RNA sequencing, and immunohistochemical validation of key protein markers [11].
Therapeutic Testing: Models are exposed to identical drug regimens used in the corresponding clinical setting, employing clinically relevant dosing schedules and concentrations. Multiple endpoints are assessed, including viability metrics (CellTiter-Glo for PDOs), volumetric measurements (caliper measurements for PDX), and histological analysis [6] [11].
Correlation Analysis: Model responses are quantitatively compared with clinical outcomes (radiographic response, progression-free survival, overall survival) using statistical methods ranging from correlation coefficients to supervised machine learning approaches [6].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for Model-Clinical Correlation Studies
| Reagent Category | Specific Examples | Function in Discordance Analysis |
|---|---|---|
| Extracellular Matrix | Matrigel, Geltrex, Cultrex BME, synthetic hydrogels | Provides 3D scaffolding for organoid growth; Influences cell signaling and drug penetration |
| Specialized Media Formulations | Advanced DMEM/F12 with B27, N-Acetylcysteine, growth factors (EGF, FGF), inhibitors (A83-01, Y27632) | Supports stem cell maintenance and proliferation; Modulates differentiation states |
| Immunodeficient Mouse Strains | NOD-SCID, NSG, NOG, nude mice | Hosts for PDX engraftment; Variable levels of immunodeficiency affect engraftment success |
| Cell Dissociation Reagents | Collagenase, Dispase, Trypsin-EDTA, Tumor Dissociation Kits | Tissue processing to single cells or fragments; Impacts cell viability and establishment efficiency |
| Viability Assays | CellTiter-Glo, ATP-based assays, resazurin reduction, caspase activity | Quantifies therapeutic response; Different assays may yield varying sensitivity estimates |
Strategies for Improving Model Predictive Value
Integrated Model Systems
Recognizing the complementary strengths and limitations of individual model systems, researchers are increasingly developing integrated approaches. PDX-derived organoids (PDXOs) represent one such hybrid model, combining the in vivo selection and maintenance of tumor heterogeneity afforded by PDX models with the scalability and throughput advantages of organoid systems [35]. Studies have demonstrated remarkable biological equivalency between PDX models and organoids derived from them, with >90% correlation in drug response profiles [35]. This approach enables initial in vivo passage to stabilize tumor ecosystems followed by large-scale in vitro drug screening.
The incorporation of humanized microenvironments represents another promising strategy. For PDOs, this includes co-culture systems with immune cells, cancer-associated fibroblasts, and endothelial cells to better mimic tumor-stromal interactions [35]. For PDX models, humanized mice engrafted with human immune systems (humanized PDX or Hu-PDX) enable evaluation of immunotherapies and immune-mediated mechanisms of response and resistance [1] [71]. These advanced systems more faithfully recapitulate the complex cellular ecosystems of human tumors while maintaining experimental tractability.
Analytical and Statistical Improvements
Enhanced analytical approaches are equally critical for improving predictive accuracy. Multi-omics integration—combining genomic, transcriptomic, proteomic, and metabolomic datasets from both models and patient tumors—enables more comprehensive molecular matching and identification of discordance-associated features [1]. Computational methods for cross-species analysis help distinguish human-specific from mouse-specific signals in PDX models, clarifying which molecular networks remain intact versus those perturbed by the xenogeneic environment.
Robust experimental design that adequately captures tumor heterogeneity is essential. Rather than relying on single models, field-leading approaches now employ panels of models representing molecularly defined subtypes, with statistical power calculations guiding model numbers and replicates [87]. The "1 × 1 × 1" approach (one mouse per model per treatment) enables screening across hundreds of models, while "2 × 1 × 1" or "3 × 1 × 1" designs provide greater reliability for confirmatory studies [71]. Standardized response metrics and reporting standards facilitate cross-study comparisons and meta-analyses that can identify consistent patterns of prediction success and failure across diverse model systems.
Discordance between model systems and clinical outcomes represents neither model failure nor clinical irrelevance, but rather reveals fundamental biological complexities that demand more sophisticated approaches. The cases and analyses presented demonstrate that predictive accuracy depends on multiple interconnected factors: biological fidelity (preservation of tumor heterogeneity and microenvironment), technical optimization (establishment efficiency, culture conditions), and analytical rigor (appropriate experimental design, quantitative assessment).
Moving forward, the field must abandon the notion of a single "perfect" model and instead embrace context-specific model selection, acknowledging that different research questions and clinical applications may require distinct model systems. For drug discovery targeting cell-autonomous mechanisms, screened PDO panels may offer optimal efficiency and predictive value. For therapies targeting tumor-stromal interactions or requiring complex pharmacokinetic-pharmacodynamic relationships, PDX models remain essential. For immunotherapies, only humanized PDX models currently provide physiologically relevant systems.
Ultimately, the systematic investigation of discordant cases provides the most valuable insights for model improvement. By understanding when and why models fail to predict clinical outcomes, researchers can develop increasingly sophisticated systems that bridge the translational gap, accelerating the development of effective cancer therapies while sparing patients from ineffective treatments based on misleading preclinical predictions.
Patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as transformative tools in preclinical cancer research, offering more physiologically relevant platforms for studying tumor biology and drug response than traditional 2D cell lines. These models are particularly valuable for investigating biomarker-driven responses to targeted therapies, especially in cancers featuring EGFR and HER2 alterations. As precision oncology advances, understanding the relative strengths and limitations of these model systems becomes crucial for designing effective research strategies and translating findings to clinical applications. This guide provides a comparative analysis of PDX and organoid models, focusing on their utility in predicting responses to therapies targeting key molecular features like EGFR and HER2, complete with experimental protocols, visualization of signaling pathways, and essential research reagents.
Model Comparison: PDX vs. Organoid Systems
Fundamental Characteristics and Applications
Patient-derived xenografts (PDXs) are established by directly transplanting patient tumor fragments into immunodeficient mice, allowing the tumor to grow in an in vivo environment. In contrast, patient-derived organoids (PDOs) are 3D miniature structures derived from patient tumor cells and grown in a specialized matrix in vitro, where they self-organize to recapitulate key aspects of the original tumor architecture [88] [89].
Table 1: Core Characteristics of PDX and Organoid Models
| Feature | PDX Models | Organoid Models |
|---|---|---|
| Genetic/epigenetic alterations | Similar to original tumor [88] | Similar to original tumor [88] |
| Pathohistological characteristics | Similar to original tumor [88] | Similar to original tumor [88] |
| Response to anti-cancer drugs | Closely correlated with clinical data [88] | Similar to original tumor [88] |
| Tumor microenvironment | Human stroma replaced by murine counterparts [88] | Limited native microenvironment; can be co-cultured with immune/stromal cells [89] |
| Throughput for drug screening | Low to medium (weeks to months) [90] | High (days to weeks) [30] [89] |
| Success rate of establishment | Varies by cancer type (35-86%) [72] | Generally high; can be established from small biopsies [91] |
| Scalability | Limited by mouse housing and costs [92] | Highly scalable for high-throughput screening [30] [89] |
| Personalized medicine applications | Used for co-clinical trials and biomarker discovery [88] [93] | Suitable for rapid treatment selection and personalized therapy prediction [30] [89] |
Predictive Performance for Biomarker-Driven Therapies
Both model systems demonstrate significant value in predicting responses to therapies targeting molecular features. PDX models have shown strong correlation between drug susceptibility and clinical outcomes in patients from whom the models were derived [88]. For instance, in HER2-positive breast cancer, PDX models have been instrumental in understanding mechanisms of resistance to HER2-targeted therapies like trastuzumab and lapatinib [94]. Organoid models similarly maintain the molecular features of parent tumors and have demonstrated high accuracy in predicting clinical drug responses, with studies reporting sensitivity of 82.35-100% and specificity of 69.23-93% across various cancer types including lung, breast, and gastrointestinal cancers [89].
Table 2: Engraftment and Predictive Performance by Cancer Type
| Cancer Type | PDX P0 Engraftment Rate | PDX/Organoid Predictive Accuracy | Key Biomarkers Studied |
|---|---|---|---|
| Pancreatic ductal adenocarcinoma | 62% (105/169) [72] | Activated KRAS-MAPK pathway independent of KRAS status [72] | KRAS, EGFR, BRAF [72] |
| Duodenal/Ampullary | 86% (25/29) [72] | Information not specified in search results | Information not specified in search results |
| Bile duct | 35% (17/48) [72] | Information not specified in search results | Information not specified in search results |
| Breast cancer | 25-40% in NOD-SCID mice [88] | 82.35% sensitivity, 69.23% specificity in organoids [89] | HER2, EGFR [94] [95] |
| Non-small cell lung cancer | 25-40% in NOD-SCID mice [88] | 84.0% sensitivity, 82.8% specificity in organoids [89] | EGFR [89] |
| Cutaneous melanoma | 25-40% in NOD-SCID mice [88] | Information not specified in search results | Information not specified in search results |
Experimental Protocols for Model Establishment and Analysis
PDX Model Generation and Drug Testing
Protocol 1: Establishing PDX Models from Surgical Specimens
- Sample Collection: Obtain fresh tumor tissue from surgical resections under sterile conditions, ideally within 1-2 hours of resection [72].
- Tissue Processing: Mince tumor tissue into 2-3 mm³ fragments in cold PBS or DMEM medium supplemented with antibiotics.
- Implantation: Implant fragments subcutaneously into immunodeficient mice (NOD-SCID, NSG, or NOG strains) using a trocar, or orthotopically via surgical procedures [88] [72].
- Monitoring: Palpate implantation sites regularly for tumor growth. Initial (P0) tumors typically appear within 2-8 weeks, depending on cancer type [72].
- Passaging: Once tumors reach 1.0-1.5 cm in diameter, harvest, mince, and reimplant into new recipient mice for expansion and experiments [88].
Protocol 2: Drug Efficacy Studies in PDX Models
- Randomization: When PDX tumors reach 100-200 mm³, randomize mice into treatment and control groups (n=5-8 per group).
- Dosing: Administer therapeutic agents at clinically relevant doses and schedules via appropriate routes (oral gavage, intraperitoneal, or intravenous injection) [90] [93].
- Monitoring: Measure tumor dimensions 2-3 times weekly using calipers. Calculate tumor volume using the formula: V = (length × width²)/2.
- Endpoint Analysis: At study endpoint, collect tumors for molecular analysis (e.g., genomic profiling, immunohistochemistry, RNA sequencing) [90] [72].
Organoid Establishment and High-Throughput Screening
Protocol 3: Deriving Patient-Derived Organoid Cultures
- Tissue Processing: Mechanically mince and enzymatically digest tumor tissue using collagenase/dispase solutions to create single-cell suspensions or small cell clusters [89] [91].
- Matrix Embedding: Resuspend cell pellets in ECM substitute (e.g., Matrigel, synthetic hydrogels) and plate as droplets in pre-warmed culture plates. Polymerize at 37°C for 20-30 minutes [89].
- Culture Medium: Overlay with specialized medium containing tissue-specific growth factors and small molecules:
- Essential Components: B27 and N-2 supplements, growth factors (EGF, FGF, Wnt-3A, R-Spondin-1, Noggin), and pathway inhibitors (Y-27632, A83-01) depending on cancer type [89].
- Maintenance: Culture at 37°C with 5% CO₂, with medium changes every 2-3 days, and passage every 1-2 weeks using mechanical disruption or enzymatic digestion [89] [91].
Protocol 4: Drug Sensitivity Testing in Organoid Models
- Organoid Harvesting: Dissociate organoids to single cells or small clusters (approximately 10-20 cells) using enzymatic or mechanical methods.
- Plating: Seed organoid fragments in 96-well or 384-well plates pre-coated with ECM at optimized densities.
- Drug Treatment: After 24-48 hours, add serial dilutions of therapeutic compounds. Include positive and negative controls.
- Viability Assessment: After 5-7 days, measure viability using ATP-based (CellTiter-Glo) or resazurin-based assays. Calculate IC₅₀ values using non-linear regression analysis [89].
EGFR/HER2 Heterodimer Analysis
Protocol 5: Studying Receptor Interactions and Signaling
- Receptor Labeling: For simultaneous detection of EGFR and HER2, use specific labeling with quantum dot nanoparticles (QDs) of different sizes [94]:
- Label EGFR with biotinylated EGF followed by streptavidin-conjugated QD655 (red fluorescence, 14-18 nm)
- Block free binding sites with streptavidin and biotin
- Label HER2 with biotinylated anti-HER2 Affibody followed by streptavidin-conjugated QD565 (yellow fluorescence, 12 nm)
- Fixation: Use two-step fixation (3% formaldehyde for 5 minutes, followed by 3% formaldehyde with 0.2% glutaraldehyde for 5 minutes) to preserve membrane structures [94].
- Imaging: Analyze using correlative fluorescence and liquid phase electron microscopy to determine receptor distribution and density at single-molecule resolution [94].
- Data Analysis: Quantify receptor surface density and clustering patterns in different membrane regions and cellular subpopulations.
Diagram 1: EGFR/HER2 Heterodimer Formation and Signaling Dynamics. The asymmetric dimer formation relies primarily on the HER2 dimerization arm, leading to prolonged signaling and reduced receptor endocytosis, enhancing oncogenic effects [95].
Research Reagent Solutions for PDX and Organoid Research
Essential Materials and Their Applications
Table 3: Key Research Reagents for Model Establishment and Analysis
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| ECM Substitutes | Matrigel, Synthetic hydrogels (e.g., GelMA) | Provides 3D structural support for organoid growth | Matrigel shows batch variability; synthetic hydrogels offer better reproducibility [89] |
| Growth Factors & Cytokines | EGF, FGF, Wnt-3A, R-Spondin-1, Noggin, HGF | Promotes stemness and proliferation in organoid cultures | Specific combinations required for different cancer types [89] |
| Pathway Inhibitors | Y-27632 (ROCK inhibitor), A83-01 (TGF-β inhibitor), SB202190 (p38 MAPK inhibitor) | Enhances cell survival and inhibits differentiation | Y-27632 particularly important during initial establishment and passaging [89] |
| Immunodeficient Mouse Strains | NOD-SCID, NSG, NOG mice | Hosts for PDX engraftment | NSG and NOG with complete lack of T, B, and NK cell activity show higher engraftment rates [88] |
| Cell Culture Supplements | B27, N-2 | Serum-free supplements providing essential nutrients | Standard component for most organoid media formulations [89] |
| Labeling Reagents | Biotinylated EGF, Anti-HER2 Affibody, Quantum Dots (QD565, QD655) | Specific receptor labeling for imaging studies | Enables single-molecule detection of EGFR and HER2 [94] |
Advanced Applications and Integration with Novel Technologies
Incorporation with Artificial Intelligence and High-Throughput Platforms
The integration of PDX and organoid models with advanced computational approaches represents the cutting edge of cancer research. Machine learning frameworks, particularly pan-cancer pan-treatment (PCPT) models, have been developed to predict treatment outcomes across multiple cancer types using PDX data [90]. These models utilize genomic features (gene expression, copy number variations, mutations) combined with cancer type and treatment information as input features, achieving promising prediction accuracy for treatment responses [90].
For organoid models, automation and AI integration are addressing challenges of reproducibility and scalability. Advanced platforms now combine automation and AI to produce more reliable organoid models with reduced variability, eliminating human bias and standardizing protocols [30]. These developments are crucial for the creation of "assay-ready, validated models" that have undergone rigorous testing to confirm they accurately mimic biological processes [30].
Modeling the Tumor Microenvironment and Immunotherapy Responses
Recent advancements in both model systems have focused on better recapitulating the tumor microenvironment, particularly for immunotherapy applications. Organoid technology has evolved to include co-culture models with immune cells, enabling the study of complex tumor-immune interactions and evaluation of immunotherapies such as immune checkpoint inhibitors, CAR-T therapies, and oncolytic viruses [89]. These immune-enhanced organoid models provide a powerful platform for assessing personalized immunotherapy strategies and studying immune evasion mechanisms.
PDX models face limitations in immuno-oncology research due to their immunocompromised nature, though humanized PDX models with engrafted human immune cells are being developed to overcome this challenge. For organoids, current efforts focus on incorporating adult tissue-specific immune compartments, vascularization, and multiple cell types to create more physiologically relevant models [30] [89].
Diagram 2: Decision Framework for Selecting PDX vs. Organoid Models. The choice between model systems depends on research objectives, with opportunities for integrated approaches that leverage the strengths of both platforms.
PDX and organoid models each offer distinct advantages for studying biomarker-driven responses in cancer research, particularly for EGFR, HER2, and other molecular features. PDX models provide an in vivo context that preserves tumor architecture and stromal interactions, albeit with eventual murine stromal replacement, making them valuable for preclinical validation studies. Organoid models excel in scalability, throughput, and preservation of human tumor biology, enabling rapid personalized therapy screening and extensive drug discovery applications. The complementary use of both systems, enhanced by emerging technologies like artificial intelligence, microfluidic platforms, and advanced imaging, will continue to advance our understanding of cancer biology and accelerate the development of targeted therapies. As these models evolve with improved microenvironment recapitulation and standardization, their predictive power in clinical translation will further strengthen, ultimately enabling more effective personalized cancer treatments.
In the evolving landscape of precision oncology, patient-derived xenograft (PDX) and patient-derived organoid (PDO) models have emerged as transformative tools that bridge the gap between conventional preclinical models and human clinical response. While traditional two-dimensional cell cultures and genetically engineered mouse models have contributed substantially to cancer biology, they often fail to recapitulate the complexity and heterogeneity of human tumors, contributing to the high failure rates in oncology drug development [96]. Both PDX and PDO models preserve key characteristics of original patient tumors, including histopathological architecture, genetic profiles, and cellular heterogeneity, making them invaluable for drug development and personalized treatment strategies [97] [98].
The critical distinction between these platforms lies in their operational frameworks: PDX models involve implanting human tumor tissue into immunocompromised mice, maintaining tumor-stroma interactions and in vivo biology, while PDO models are three-dimensional in vitro cultures that derive from patient tumor cells and self-organize into structures mimicking the original tissue [96] [4]. This fundamental difference drives significant variations in throughput, timelines, resource allocation, and specific applications. A recent meta-analysis of 411 patient-model pairs demonstrated that overall concordance in treatment response between patients and matched models was 70%, with no significant differences in predictive accuracy between PDX and PDO platforms [17]. This comparable performance raises important questions about how to strategically deploy each model type within research and drug development pipelines to maximize scientific insight while responsibly managing finite resources.
Quantitative Comparison: Operational Metrics and Performance
Direct comparison of PDX and PDO models across standardized metrics reveals distinct operational profiles that inform their strategic application in research and drug development. The tables below synthesize quantitative data from multiple studies to facilitate evidence-based decision-making.
Table 1: Operational and Resource Metrics for PDX and PDO Models
| Metric | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Establishment Time | 4-8 months [97] | 1-3 weeks [97] [14] |
| Engraftment/Success Rate | Highly variable: 9%-85% depending on cancer type and source [98] | Generally higher and more consistent across cancer types [97] |
| Cost Considerations | High (specialized mice, housing, long-term maintenance) [17] [97] | Significantly lower (plasticware, media components) [17] [97] |
| Throughput Potential | Low to moderate (limited by mouse housing space and time) [97] | High (amenable to 96/384-well formats) [97] [14] |
| Scalability | Low (requires significant animal resources) [97] | High (can bank and expand models extensively) [97] [14] |
| Ethical Considerations | Significant (extensive animal use) [17] | Minimal (in vitro system) [17] |
| Cryopreservation/ Biobanking | Challenging with low reanimation efficiency [97] | Highly efficient with successful recovery [97] [14] |
Table 2: Functional Performance Characteristics of PDX and PDO Models
| Characteristic | Patient-Derived Xenografts (PDX) | Patient-Derived Organoids (PDO) |
|---|---|---|
| Predictive Concordance | 70% overall (meta-analysis) [17] | 70% overall (meta-analysis) [17] |
| Tumor Microenvironment | Retains human stroma initially, replaced by mouse stroma over time [96] [97] | Primarily epithelial; requires co-culture for immune/stromal components [97] [14] |
| Immunotherapy Applications | Limited in standard form; requires humanized mice [97] | Can be co-cultured with immune cells for immuno-oncology studies [97] [14] |
| Genetic Stability | High through early passages; mouse stromal overgrowth later [96] | High genetic stability during long-term culture [4] [14] |
| Clinical Translation Timeline | Too slow for real-time treatment guidance in most cases [97] | Potentially suitable for real-time therapeutic guidance [98] |
Experimental Design and Methodological Considerations
The strategic selection between PDX and PDO platforms requires understanding their foundational methodologies and the types of experimental questions each can most effectively address.
PDX Model Establishment and Workflow
PDX establishment begins with implanting freshly collected patient tumor fragments or single-cell suspensions into immunocompromised mice, typically using subcutaneous or orthotopic sites [96] [97]. The process involves several critical stages:
Sample Preparation: Tumor tissues are minimally processed, cut into 1-3 mm³ fragments, or digested into single-cell suspensions using collagenase/hyaluronidase enzymes [98] [99].
Implantation: Samples are implanted into recipient mice (typically NSG or similar immunodeficient strains) using surgical procedures for orthotopic placement or injection for subcutaneous models [97] [99].
Engraftment Monitoring: Tumors are monitored for growth over several months, with successful engraftment rates varying significantly by cancer type [98].
Propagation: Established models can be serially passaged in mice, with early passages (P1-P3) considered most representative of original tumors before mouse stromal replacement occurs [96].
Diagram 1: PDX Model Establishment Workflow. The process requires 4-8 months for initial model development, creating significant timeline constraints for research applications.
PDO Model Establishment and Workflow
PDO generation employs a more streamlined approach that enables rapid model development:
Sample Acquisition: Tumor tissues can be obtained through surgical resection, biopsies, or from malignant body fluids (pleural effusions, ascites) [14].
Tissue Processing: Samples are minced and digested using enzyme cocktails (collagenase, trypsin) to create single-cell suspensions or small cell clusters [14].
3D Culture: Processed cells are embedded in extracellular matrix substitutes (Matrigel, BME) and cultured with specialized media containing niche-specific growth factors [4] [14].
Expansion and Banking: Organoids are typically visible within 1-3 weeks and can be passaged every 2-4 weeks, with efficient cryopreservation enabling stable biobanking [14].
Diagram 2: PDO Model Establishment Workflow. The significantly shorter timeline (1-3 weeks) enables rapid model generation suitable for functional precision medicine applications.
Key Signaling Pathways in Model Development
Both PDX and PDO models depend on carefully regulated signaling environments to maintain tumor characteristics. For PDO cultures, specific pathway activation is essential:
Diagram 3: Key Signaling Pathways in PDO Culture. Successful organoid culture requires precise modulation of core signaling pathways to maintain cancer stem cells and appropriate differentiation.
Research Reagent Solutions and Essential Materials
The experimental workflows for PDX and PDO models require specialized reagents and materials that contribute significantly to their operational costs and technical feasibility.
Table 3: Essential Research Reagents for PDX and PDO Models
| Reagent Category | Specific Examples | Function | Model Application |
|---|---|---|---|
| Extracellular Matrix | Matrigel, BME, Geltrex | Provides 3D structural support for cell growth | Essential for PDO; not required for PDX [14] |
| Digestion Enzymes | Collagenase, Hyaluronidase, TrypLE | Dissociates tumor tissue into single cells or small clusters | Used in both PDX and PDO establishment [14] [99] |
| Specialized Media | Stem cell media with growth factors (EGF, Noggin, R-spondin) | Supports stem cell maintenance and proliferation | Critical for PDO culture; not required for PDX [4] [14] |
| Mouse Strains | NSG, NOG, NRG | Provides immunocompromised host for human tumor engraftment | Essential for PDX; not required for PDO [97] [99] |
| Cryopreservation Media | DMSO-containing solutions | Enables long-term storage of cells and tissues | Used for both models; higher efficiency with PDO [14] [99] |
Strategic Implementation and Decision Framework
The comparable predictive performance but divergent operational characteristics of PDX and PDO models present a strategic landscape for research planning. The meta-analysis finding of 70% concordance for both platforms suggests that model selection should be driven by specific research questions, resource constraints, and timeline requirements rather than assumed superiority of either platform [17].
Resource Allocation Optimization
Strategic resource allocation requires matching model capabilities to research objectives:
PDX models justify their substantial resource investment (typically $2,000-$5,000 per model considering specialized mice and long-term housing) for studies requiring in vivo context, such as assessing drug pharmacokinetics, metastasis, and therapies targeting tumor-stroma interactions [96] [97]. The demonstrated association between PDX treatment response and patient progression-free survival further supports their value in late-stage preclinical validation [17].
PDO models provide cost-effective solutions (typically $200-$500 per model considering reagents and plasticware) for high-throughput drug screening, mechanistic studies, and real-time precision medicine applications [17] [98]. Their scalability enables the creation of extensive biobanks representing tumor heterogeneity at a fraction of PDX costs.
Integrated Approaches and Emerging Solutions
Hybrid approaches are emerging to leverage the strengths of both platforms:
PDX-derived organoids (PDxO) combine the in vivo relevance of PDX with the throughput advantages of organoid culture, enabling in vitro screening with subsequent in vivo validation [98].
Patient-derived cell xenografts (PDCX) utilize cryopreserved primary cancer cells instead of tissue fragments, improving standardization and reducing procedural variability while maintaining in vivo context [99].
These integrated approaches exemplify the evolving toolkit for cancer researchers seeking to balance biological fidelity with practical constraints.
The cost-benefit analysis between PDX and PDO models reveals a complementary rather than competitive relationship. PDX models provide irreplaceable in vivo context for studies requiring full biological complexity, despite their substantial resource demands and extended timelines. PDO models offer unprecedented throughput and scalability for drug screening and functional precision medicine, with limitations in microenvironmental representation.
The comparable predictive accuracy of both platforms [17] suggests that operational considerations—throughput requirements, timeline constraints, resource availability, and specific research questions—should drive model selection rather than assumed predictive superiority. Strategic resource allocation increasingly favors PDO models for initial high-throughput screening and mechanistic studies, with PDX models reserved for subsequent in vivo validation of prioritized therapeutic candidates. This integrated approach maximizes the distinctive advantages of each platform while acknowledging their respective constraints, ultimately accelerating oncology drug development and advancing personalized cancer treatment.
Conclusion
The comparative analysis reveals that PDX and organoid models offer complementary rather than competing value in preclinical oncology. PDX models remain the gold standard for in vivo validation, providing crucial systemic context and maintaining high clinical predictive accuracy. Meanwhile, organoids excel in high-throughput applications, offering unprecedented scalability for drug screening while preserving key tumor characteristics. The emerging practice of using matched PDX-organoid pairs represents a powerful paradigm, leveraging the strengths of both platforms. Future directions should focus on standardizing protocols across cancer types, incorporating immune components, and expanding biobanks to better capture population heterogeneity. As functional precision medicine advances, the strategic integration of these models will be crucial for accelerating drug development and improving patient outcomes through more predictive preclinical modeling.
References
- 1. Patient-derived xenograft models in cancer therapy [https://www.nature.com/articles/s41392-023-01419-2]
- 2. Patient Derived Xenograft Models: An Emerging Platform ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4167608/]
- 3. Patient-Derived Xenograft Models of Breast Cancer and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6628218/]
- 4. Organoids: The current status and biomedical applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC10192887/]
- 5. Human organoids: model systems for human biology and ... [https://www.nature.com/articles/s41580-020-0259-3]
- 6. predictive value of organoids in colorectal cancer [https://www.nature.com/articles/s41598-023-45297-8]
- 7. Patient-derived xenograft models: Current status ... [https://www.sciencedirect.com/science/article/pii/S2352304225000091]
- 8. Organoid models in oncology: advancing precision cancer ... [https://www.cancerbiomed.org/content/early/2025/07/24/j.issn.2095-3941.2025.0127]
- 9. Patient-derived organoids in precision cancer medicine [https://www.sciencedirect.com/science/article/pii/S266663402400343X]
- 10. The role of organoids in cancer research [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-023-00433-y]
- 11. Comparative analysis of response to treatments and ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-023-02809-8]
- 12. Organoids and organs-on-chips: insights into predicting the ... [https://www.nature.com/articles/s41420-023-01354-9]
- 13. Patient-derived tumor organoids: a new avenue for ... [https://www.nature.com/articles/s12276-024-01272-5]
- 14. Modeling methods of different tumor organoids and their ... [https://www.oaepublish.com/articles/cdr.2025.34]
- 15. Using patient-derived organoids to predict locally ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9975107/]
- 16. Iteration of Tumor Organoids in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566727/]
- 17. Comparative analysis of patient-derived organoids and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12363698/]
- 18. Renal cell carcinoma organoids for precision medicine [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06949-7]
- 19. Patient derived xenograft models of hormone receptor ... [https://www.nature.com/articles/s41598-025-22361-z]
- 20. Individualized patient tumor organoids faithfully preserve ... [https://www.sciencedirect.com/science/article/pii/S1934590925000025]
- 21. Patient-derived xenograft models: a revolution in colorectal ... [https://ecancer.org/en/news/27273-patient-derived-xenograft-models-a-revolution-in-colorectal-cancer-research]
- 22. Establishing a pediatric solid tumor PDX biobank for precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351738/]
- 23. Individualized patient tumor organoids faithfully preserve ... [https://pubmed.ncbi.nlm.nih.gov/39938519/]
- 24. Comparative analysis of patient-derived organoids and ... [https://www.medrxiv.org/content/10.1101/2025.08.10.25333051v1.full-text]
- 25. Tumor organoids: A review of culture methods, applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574996/]
- 26. The use of patient-derived xenografts and ... [https://www.sciencedirect.com/science/article/pii/S0753332224016366]
- 27. PDX models are back – and they're exposing what cell ... [https://www.drugtargetreview.com/article/187056/pdx-models-are-back-and-theyre-exposing-what-cell-lines-missed/]
- 28. Why PDX Models Are Essential for Radiopharmaceutical ... [https://blog.championsoncology.com/blog/using-well-characterized-pdx-models-to-guide-radiopharma-development]
- 29. Systematic review: predictive value of organoids in colorectal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10593775/]
- 30. 2025 Trends: Organoids [https://www.genengnews.com/topics/genome-editing/2025-trends-organoids/]
- 31. 2D and 3D cell cultures – a comparison of different types of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6040128/]
- 32. A hitchhiker's guide to cancer models - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9588514/]
- 33. Xenograft and organoid in developing precision medicine for... models [https://www.spandidos-publications.com/10.3892/ijo.2024.5629]
- 34. Patient-derived xenografts and organoids therapy response in... model [https://www.nature.com/articles/s41467-021-21300-6?error=cookies_not_supported&code=7cb5e5ad-934a-42ba-a126-df14c48a96cb]
- 35. PDOs, PDXOs, PDOXs or PDXs? Selecting the Best Model to... [https://blog.crownbio.com/pdos-pdxos-pdoxs-or-pdxs-selecting-the-best-model-to-progress-your-patient-centric-research]
- 36. Opportunities and challenges for patient-derived models of ... [https://www.nature.com/articles/s41698-025-00832-w]
- 37. How to grow patient-derived organoids (PDOs) [https://www.moleculardevices.com/lab-notes/3d-biology/how-to-grow-patient-derived-organoids]
- 38. Translational Neuro-Oncology: Jann N. Sarkaria - Protocols [https://www.mayo.edu/research/labs/translational-neuro-oncology/mayo-clinic-brain-tumor-patient-derived-xenograft-national-resource/protocols]
- 39. Successful Start: Tips for Establishing Organoids [https://bitesizebio.com/45452/successful-start-tips-for-establishing-organoids/]
- 40. Research Progress, Challenges, and Breakthroughs of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8635113/]
- 41. PDX Organoid models | PDXO | CRO [https://www.oncodesign-services.com/oncology/tumor-models/pdx-models/pdx-organoid/]
- 42. Challenges and Prospects of Patient-Derived Xenografts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10486659/]
- 43. Patient-Derived Xenograft vs. Organoids: A Preliminary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7593921/]
- 44. Breakthroughs and challenges of organoid models for ... [https://www.nature.com/articles/s41420-025-02505-w]
- 45. PDX Derived Organoids (PDXOs) [https://www.championsoncology.com/ex-vivo-models]
- 46. High-throughput solutions in tumor organoids - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11811636/]
- 47. Cancer patient-derived organoids: Novel models for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12320244/]
- 48. Organoids in high-throughput and high-content screenings [https://www.frontiersin.org/journals/chemical-engineering/articles/10.3389/fceng.2023.1120348/full]
- 49. SITC 2025 Poster 148: DRUG-seq in CTG3D Organoid ... [https://www.championsoncology.com/posters/2025/drug-seq-ctg3d-organoids-148?hsLang=en]
- 50. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 51. High Throughput Screening Market Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/high-throughput-screening-market]
- 52. Accelerating precision oncology with advanced tumor avatars [https://eqtgroup.com/thinq/library-of-hope/accelerating-precision-oncology-with-advanced-tumor-avatars]
- 53. Organoids as predictive platforms: advancing disease ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592500834X]
- 54. PDX models: a new tool for colorectal cancer research [https://www.drugtargetreview.com/news/190758/pdx-models-a-new-tool-for-colorectal-cancer-research/]
- 55. PharmaFormer predicts clinical drug responses through ... [https://www.nature.com/articles/s41698-025-01082-6]
- 56. The role of patient-derived xenograft models (PDX) in ... [https://blog.crownbio.com/the-role-of-patient-derived-xenograft-models-pdx-in-antibody-drug-conjugate-development]
- 57. Patient Derived Xenograft/PDX Models Report 2025 [https://finance.yahoo.com/news/patient-derived-xenograft-pdx-models-101600614.html]
- 58. New Therapeutic Perspectives in Prostate Cancer: Patient- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10604340/]
- 59. Modeling methods of different tumor organoids and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366422/]
- 60. Exploration of organoids in ovarian cancer - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11437877/]
- 61. Promising preclinical patient-derived organoid (PDO) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10702130/]
- 62. Promising preclinical patient-derived organoid (PDO) and ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-023-11434-9]
- 63. A PDX/Organoid Biobank of Advanced Prostate Cancers ... [https://pubmed.ncbi.nlm.nih.gov/29748182/]
- 64. Patient-derived xenografts and organoids model therapy ... [https://www.nature.com/articles/s41467-021-21300-6]
- 65. United States PDX Models Market Key Restraints [https://www.linkedin.com/pulse/united-states-pdx-models-market-key-restraints-oy9hc/]
- 66. Sourcing Better PDX Models with a Streamlined “Clinic-to- ... [https://startresearch.com/sourcing-better-pdx-models-with-a-streamlined-clinic-to-bench-pipeline/]
- 67. Patient-derived Xenograft (PDX) Models [https://www.datainsightsmarket.com/reports/patient-derived-xenograft-pdx-models-582161]
- 68. Trends and challenges in organoid modeling and expansion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11608026/]
- 69. Comparative analysis of patient-derived organoids and ... [https://pubmed.ncbi.nlm.nih.gov/40832408/]
- 70. Opportunities and challenges of patient-derived models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8851816/]
- 71. Patient-derived xenograft (PDX) models, applications and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-022-03405-8]
- 72. Patient-derived tumor xenograft and organoid models ... [https://www.nature.com/articles/s41598-021-90049-1]
- 73. Organoid models in oncology: advancing precision cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418270/]
- 74. A living biobank of matched pairs of patient-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9815646/]
- 75. Creating Matched In vivo/In vitro Patient-Derived Model ... [https://www.jove.com/t/61382/creating-matched-vivoin-vitro-patient-derived-model-pairs-pdx-pdx]
- 76. PDX-derived organoids model in vivo drug response and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7710298/]
- 77. Primary human organoids models: Current progress and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10029057/]
- 78. ATCC Organoid Culture Guide [https://www.atcc.org/resources/culture-guides/organoid-culture-guide]
- 79. Establishing predictive machine learning models for drug ... [https://www.nature.com/articles/s41698-025-00937-2]
- 80. Advances in precision oncology using patient-derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518345/]
- 81. Predictive Validity: the Key to Improving Success in Drug ... [https://emulatebio.com/predictive-validity-the-key-to-improving-the-drug-development-process/]
- 82. Stem Cells and Organoids: A Paradigm Shift in Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299584/]
- 83. The application of organoids in treatment decision-making ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02429-0]
- 84. Improved drug-screening tests of candidate anti-cancer drugs ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0324141]
- 85. Advances in the application of patient-derived xenograft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159603/]
- 86. Organoids Increase the Predictive Value of in vitro Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6391333/]
- 87. Experimental design of preclinical experiments: number ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8643474/]
- 88. Applications of patient-derived tumor xenograft models and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6947974/]
- 89. Breakthroughs and challenges of organoid models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059183/]
- 90. A pan-cancer, pan-treatment model for predicting drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12408900/]
- 91. Beyond animal models: how organoids could transform ... [https://www.nature.com/articles/d42473-025-00219-2]
- 92. Patient Derived Xenograft/PDX Models Report 2025 [https://uk.finance.yahoo.com/news/patient-derived-xenograft-pdx-models-101600358.html]
- 93. AACR: Predictivity of Genomate Validated in PDX Models [https://www.genomate.health/publication/predictivity-of-genomate-drug-ranking-validated-in-pdx-models]
- 94. EGFR Expression in HER2-Driven Breast Cancer Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC7729501/]
- 95. Structure and dynamics of the EGFR/HER2 heterodimer [https://www.nature.com/articles/s41421-023-00523-5]
- 96. Patient-derived xenograft models in cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10097874/]
- 97. Patient-derived organoids (PDOs) and PDO ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11256726/]
- 98. A human breast cancer-derived xenograft and organoid ... [https://www.nature.com/articles/s43018-022-00337-6]
- 99. Establishment and Its Utility of a Patient-Derived Cell ... [https://www.mdpi.com/2073-4409/14/5/325]