Predicting Immunotherapy Success: A 2024 Guide to Biomarker Discovery and Clinical Validation
This comprehensive review synthesizes current research on biomarkers for predicting response to immunotherapy.
Predicting Immunotherapy Success: A 2024 Guide to Biomarker Discovery and Clinical Validation
Abstract
This comprehensive review synthesizes current research on biomarkers for predicting response to immunotherapy. We explore foundational concepts like PD-L1, TMB, and the tumor microenvironment, then detail advanced multi-omic and spatial methodologies for biomarker discovery. The article addresses critical challenges in standardization and data integration, and evaluates comparative performance and clinical validation pathways for emerging biomarkers. Aimed at researchers and drug development professionals, this guide provides actionable insights for translating biomarker science into robust predictive tools for personalized immuno-oncology.
Immunotherapy Biomarker Fundamentals: From PD-L1 to the Next Generation
Immune checkpoint inhibitors (ICIs) have transformed cancer therapy, yet significant heterogeneity in patient response remains a central challenge. Within the broader thesis on biomarker identification for immunotherapy response prediction, this document outlines application notes and experimental protocols to systematically dissect the tumor microenvironment (TME) and host factors contributing to ICI response variability.
Table 1: Major Determinants of Heterogeneous ICI Response
| Factor Category | Specific Biomarker/Feature | Association with Response (Approx. Prevalence in Non-Responders) | Key Supporting References |
|---|---|---|---|
| Tumor-Intrinsic | Low Tumor Mutational Burden (TMB) | <10 mutations/Mb in ~60-70% of non-responders | Hellmann et al., 2018; Marabelle et al., 2020 |
| Deficient Mismatch Repair (dMMR)/MSI-H | Present in <5% of most solid tumors, but high response rate | Le et al., 2017 | |
| Low PD-L1 Expression (TPS <1%) | Observed in ~40-50% of non-responders across cancers | Garon et al., 2015 | |
| Tumor Microenvironment | Exclusion of CD8+ T-cells | Present in ~30-40% of "immune-cold" tumors | Herbst et al., 2014 |
| Immunosuppressive Cell Infiltrate (Tregs, M2 Macrophages) | High density correlates with resistance in multiple studies | Tumeh et al., 2014 | |
| Deficient Antigen Presentation (Low MHC-I) | Found in ~15-30% of resistant cases | Zaretsky et al., 2016 | |
| Host Factors | Gut Microbiome Dysbiosis | Specific taxa absent in ~70% of non-responders in some studies | Gopalakrishnan et al., 2018 |
| Systemic Inflammation (High NLR, CRP) | Elevated NLR (>3) in ~60% of non-responders | Diem et al., 2017 |
Detailed Experimental Protocols
Protocol 1: Multiplex Immunofluorescence (mIF) for TME Phenotyping
Objective: To spatially quantify immune cell subsets, their activation states, and checkpoints within the TME from formalin-fixed, paraffin-embedded (FFPE) tumor sections.
Workflow:
- Sectioning & Baking: Cut 4-5 µm FFPE sections onto charged slides. Bake at 60°C for 1 hour.
- Deparaffinization & Antigen Retrieval: Deparaffinize in xylene and rehydrate through graded ethanol. Perform heat-induced epitope retrieval (HIER) in EDTA buffer (pH 9.0) for 20 min at 97°C.
- Multiplexed Antibody Staining Cycle (Iterative):
- Block endogenous peroxidase and proteins.
- Incubate with primary antibody (e.g., anti-CD8) for 1 hour at RT.
- Incubate with HRP-conjugated secondary polymer for 10 min.
- Apply tyramide signal amplification (TSA) fluorophore (e.g., Opal 520) for 10 min.
- Strip antibody complex via microwave HIER to prepare for next cycle.
- Sequential Cycling: Repeat Step 3 for additional markers (e.g., CD68, PD-1, PD-L1, PanCK, FoxP3, Ki67). Include DAPI in the final step.
- Imaging & Analysis: Scan slides using a multispectral imaging system (e.g., Vectra/Polaris). Use image analysis software (e.g., inForm, HALO) to perform cell segmentation, phenotyping, and spatial analysis (e.g., distance of CD8+ cells to tumor margin).
Protocol 2: Gene Expression Profiling for Immune Signatures
Objective: To quantify predefined gene expression signatures indicative of immune activity and suppression from tumor RNA.
Workflow:
- RNA Extraction: Isolate total RNA from FFPE core biopsies or sections using a kit optimized for degraded RNA (e.g., Qiagen RNeasy FFPE Kit). Assess RNA integrity (DV200).
- Library Preparation & Sequencing: For low-input RNA, use a targeted immune-oncology panel (e.g., PanCancer IO 360 Panel) or perform whole transcriptome sequencing. Convert RNA to cDNA and prepare libraries per manufacturer's protocol.
- Data Analysis:
- Align reads to the reference genome.
- Generate normalized gene expression counts (e.g., TPM, FPKM).
- Score samples against published signatures (e.g., IFN-γ signature, T-cell-inflamed GEP, chemokine expression profile) using single-sample gene set enrichment analysis (ssGSEA) or z-score aggregation.
- Correlate signature scores with clinical response data.
Visualizations
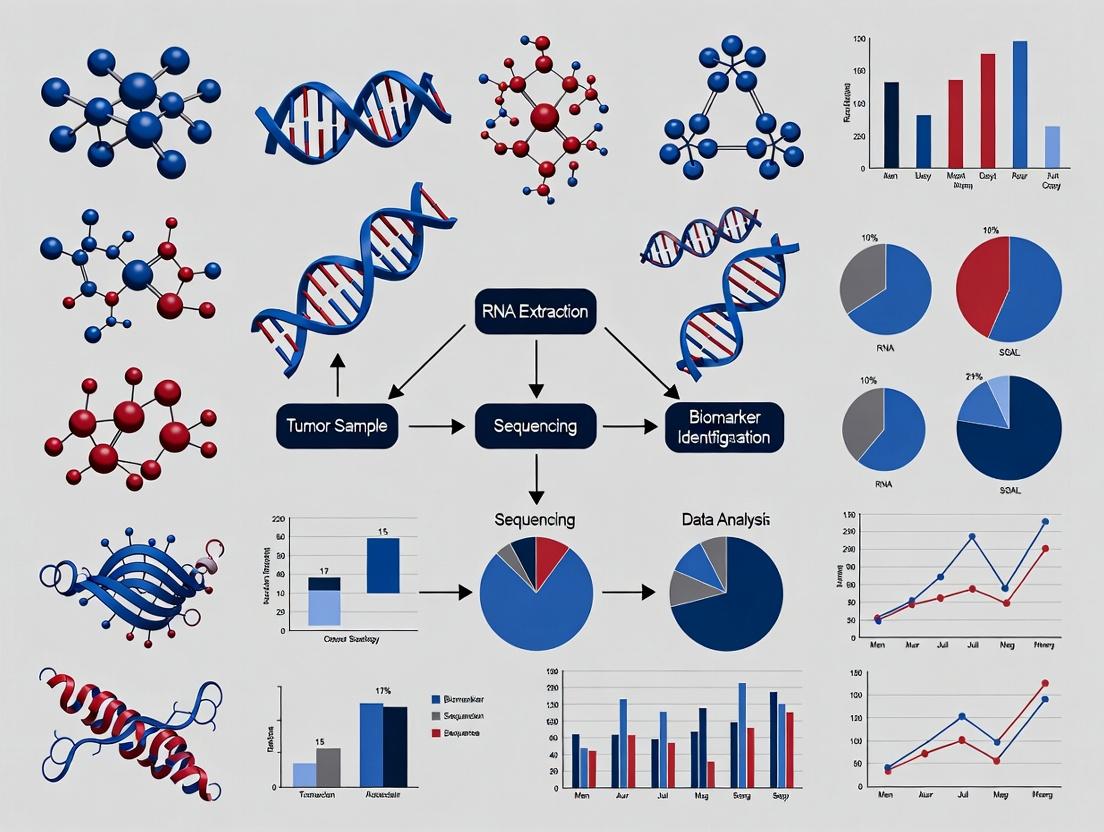
Title: Determinants of ICI Response and Resistance
Title: Integrated Biomarker Discovery Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Kits for ICI Response Research
| Item | Function/Benefit | Example Product/Catalog |
|---|---|---|
| Validated FFPE IHC/mIF Antibodies | Ensure specificity and reproducibility for key targets (PD-L1, CD8, FoxP3, etc.) in multiplex panels. | Akoya Biosciences OPAL reagents; Cell Signaling Technology mAb |
| Multiplex IHC/mIF Staining Platform | Enables simultaneous detection of 6+ markers on one tissue section with spatial context. | Akoya Phenocycler/PhenoImager; Lunaphore COMET |
| RNA Isolation Kit (FFPE optimized) | Efficiently extracts fragmented RNA from precious archived tumor samples. | Qiagen RNeasy FFPE Kit (#73504) |
| Targeted IO Gene Expression Panel | Focused NGS panel for comprehensive immune profiling from low-quality RNA. | NanoString PanCancer IO 360 Panel |
| Single-Cell RNA-Seq Solution | Unbiased dissection of cellular heterogeneity in the TME at single-cell resolution. | 10x Genomics Chromium Single Cell Immune Profiling |
| Cytokine/Chemokine Multiplex Assay | Quantifies dozens of soluble immune factors in patient serum/plasma. | Luminex xMAP Technology Assays |
| Digital Pathology Analysis Software | Quantitative, high-throughput analysis of whole-slide images for cell phenotypes. | Indica Labs HALO; Visiopharm |
| Organoid/Co-culture Media | Supports ex vivo culture of patient-derived tumor fragments with immune cells. | STEMCELL Technologies Immune Cell Media |
Application Notes
These established biomarkers are integral to selecting patients for immune checkpoint inhibitor (ICI) therapy across numerous cancer types. Their predictive utility stems from their ability to characterize distinct tumor-immune phenotypes: adaptive immune resistance (PD-L1), tumor immunogenicity (TMB), and genomic instability leading to neoantigen presentation (MSI-H/dMMR). In the context of biomarker identification for immunotherapy response prediction research, these serve as foundational benchmarks against which novel biomarkers must be validated.
Table 1: Key Biomarkers, Assays, and Clinical Applications
| Biomarker | Common Assay Methods | Scoring/Cut-off Criteria | Primary Predictive Utility | FDA-Approved Indications (Examples) |
|---|---|---|---|---|
| PD-L1 Expression | IHC (e.g., 22C3, 28-8, SP142, SP263 clones) | Tumor Proportion Score (TPS), Combined Positive Score (CPS), Immune Cell (IC) Score. Cut-offs vary (e.g., TPS ≥1%, ≥50%; CPS ≥10). | Predicts response to anti-PD-1/PD-L1 monotherapy in selected cancers (e.g., NSCLC, gastric). | NSCLC (pembrolizumab), Gastric cancer (pembrolizumab), UC (atezolizumab). |
| Tumor Mutational Burden (TMB) | NGS (Whole Exome Sequencing or targeted NGS panels ≥1 Mb) | Reported as mutations/megabase (mut/Mb). High TMB (TMB-H) often defined as ≥10 mut/Mb (varies by assay/tumor type). | Pan-cancer predictor of response to anti-PD-1/PD-L1 therapy, especially in low PD-L1 expression contexts. | Any solid tumor with TMB-H ≥10 mut/Mb (pembrolizumab). |
| MSI-H/dMMR Status | PCR (fragment analysis of microsatellites) or IHC (loss of MMR proteins: MLH1, PMS2, MSH2, MSH6) or NGS. | MSI-H: Instability in ≥2/5 mononucleotide markers. dMMR: Loss of nuclear expression in ≥1 MMR protein. | High predictive biomarker for response to anti-PD-1 therapy across tumor types. | Any solid tumor with MSI-H/dMMR (pembrolizumab, dostarlimab). |
Table 2: Comparative Characteristics of Biomarkers
| Characteristic | PD-L1 | TMB | MSI-H/dMMR |
|---|---|---|---|
| Biological Basis | Adaptive immune resistance at the tumor-immune interface. | Proxy for tumor neoantigen burden. | Consequence of defective DNA repair, leading to hypermutation. |
| Spatial Heterogeneity | High (intra- and inter-tumoral). | Moderate (assessed via bulk sequencing). | Generally homogeneous within tumor. |
| Temporal Stability | Dynamic (changes with therapy/immune pressure). | Relatively stable. | Stable (germline or somatic event). |
| Prevalence in Solid Tumors | Variable (~15-60% depending on cancer). | ~13-20% across tumors (≥10 mut/Mb). | ~2-4% across tumors; high in CRC, endometrial. |
Experimental Protocols
Protocol 1: PD-L1 Immunohistochemistry (IHC) and Scoring (22C3 pharmDx assay example)
- Objective: To qualitatively and quantitatively detect PD-L1 protein expression in formalin-fixed, paraffin-embedded (FFPE) NSCLC tissue sections.
- Reagents & Equipment: FFPE tissue sections, PD-L1 IHC 22C3 pharmDx kit, autostainer, antigen retrieval solution, wash buffer, hematoxylin counterstain, coverslips.
- Procedure:
- Cut 4-5 μm sections from FFPE block and mount on slides.
- Bake slides at 60°C for 1 hour, then deparaffinize and rehydrate.
- Perform heat-induced epitope retrieval using recommended retrieval solution.
- Cool slides, then place on autostainer.
- Apply peroxidase block for 5 minutes to quench endogenous peroxidase.
- Apply primary anti-PD-L1 antibody (clone 22C3) for 60 minutes at room temperature.
- Apply labeled polymer-HRP secondary reagent for 30 minutes.
- Apply DAB+ chromogen for 10 minutes to visualize staining.
- Counterstain with hematoxylin, dehydrate, clear, and mount.
- Scoring (TPS):
- Assess only viable tumor cells with partial or complete membrane staining.
- Calculate TPS = (Number of PD-L1 staining tumor cells / Total number of viable tumor cells) x 100%.
- Score entire tumor area present on the slide.
Protocol 2: Tumor Mutational Burden (TMB) Assessment by Targeted NGS
- Objective: To estimate TMB from FFPE tumor DNA using a targeted NGS panel covering ≥1 Mb of genome.
- Reagents & Equipment: FFPE tumor and matched normal DNA, targeted NGS panel (e.g., ~1.1 Mb), library prep kit, sequencer, bioinformatics pipeline.
- Procedure:
- DNA Extraction: Extract high-quality DNA from FFPE tumor and matched normal tissue.
- Library Preparation: Fragment DNA, perform end-repair, adapter ligation, and PCR amplification using panel-specific probes for hybrid capture.
- Sequencing: Pool libraries and sequence on an NGS platform to achieve high uniform coverage (e.g., >500x).
- Bioinformatics Analysis:
- Align sequences to reference genome.
- Call somatic variants (SNVs, indels) in tumor vs. normal.
- Filter out known germline polymorphisms (using population databases) and driver mutations.
- Apply panel-specific calibration to account for panel size and gene content.
- TMB Calculation: TMB (mut/Mb) = (Total number of synonymous and non-synonymous somatic mutations / Size of the coding region of the targeted panel in Mb).
Protocol 3: Microsatellite Instability (MSI) Testing by PCR Fragment Analysis
- Objective: To detect MSI status by analyzing length alterations in microsatellite markers.
- Reagents & Equipment: FFPE tumor and normal DNA, fluorescently-labeled primers for 5 mononucleotide markers (e.g., BAT-25, BAT-26, NR-21, NR-24, MONO-27), PCR master mix, capillary electrophoresis sequencer.
- Procedure:
- Amplify each marker separately via PCR using fluorescent primers.
- Pool PCR products and perform capillary electrophoresis.
- Analyze fragment peaks for each marker in tumor and matched normal DNA.
- Interpretation: A marker is scored as unstable if novel peaks (size shifts) are present in the tumor DNA compared to the normal control. MSI-H status is assigned if ≥2/5 markers show instability.
Visualizations
Title: PD-1/PD-L1 Checkpoint Blockade Mechanism
Title: Biomarker Development Pipeline with Benchmarks
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function / Application |
|---|---|
| FFPE Tissue Sections | The standard biospecimen for retrospective biomarker studies, enabling IHC and DNA/RNA extraction. |
| Validated IHC Antibody Clones | Essential for specific, reproducible detection of proteins like PD-L1 (clones 22C3, SP142) and MMR proteins (MLH1, MSH2, etc.). |
| Targeted NGS Panels | Comprehensive gene panels (e.g., >1 Mb) for concurrent assessment of TMB, MSI, and specific mutations from limited FFPE DNA. |
| Matched Normal DNA | Critical for distinguishing somatic tumor mutations (for TMB) from germline polymorphisms during NGS analysis. |
| Microsatellite Instability PCR Kit | Standardized, multiplexed assays containing fluorescently-labeled primers for consensus mononucleotide markers. |
| Capillary Electrophoresis System | For high-resolution fragment analysis of PCR products, essential for MSI determination and other genotyping applications. |
| Certified Digital Pathology Software | For quantitative, reproducible scoring of IHC assays (e.g., PD-L1 TPS) and analysis of spatial tumor-immune interactions. |
| Bioinformatics Pipeline (TMB/MSI) | Validated software for processing NGS data, calling mutations, filtering artifacts, and calculating final biomarker scores. |
Application Notes for Biomarker Identification in Immunotherapy Response Prediction
The characterization of the Tumor Immune Microenvironment (TIME) is a cornerstone of biomarker discovery for predicting response to immune checkpoint inhibitors (ICIs). Three critical, interlinked components—CD8+ T-cell infiltration, the phenotype and abundance of myeloid cells, and the presence of Tertiary Lymphoid Structures (TLS)—provide quantitative and spatial data predictive of clinical outcomes. Integrating these elements into a composite biomarker profile allows for stratification of patients into "hot" (immune-inflamed), "immune-excluded," and "cold" (immune-desert) tumor phenotypes, which correlate strongly with ICI efficacy.
Key Quantitative Findings: Recent meta-analyses and clinical trial correlative studies underscore the prognostic value of these features. The data below summarizes critical thresholds and associations.
Table 1: Quantitative Biomarker Associations with Anti-PD-1/PD-L1 Response
| TIME Component | Metric | Predictive Cut-off/State | Association with Response (Odds Ratio/HR) | Key References |
|---|---|---|---|---|
| CD8+ T-cells | Infiltrating Density (cells/mm²) | > 250 cells/mm² at invasive margin | OR: 4.7 (95% CI: 2.5–8.9) for objective response | Herbst et al., Nature 2014 |
| Spatial Location | Intra-tumoral > Stromal | HR for OS: 0.47 (0.29–0.77) | Tumeh et al., Nature 2014 | |
| Myeloid Cells | M2/M1 Macrophage Ratio | Ratio > 2.0 in tumor core | OR for non-response: 3.2 (1.8–5.6) | DeNardo et al., Cancer Discov 2021 |
| Myeloid-Derived Suppressor Cells (MDSCs) | >10% of CD45+ cells in blood | HR for PFS: 2.1 (1.3–3.4) | Weber et al., Clin Cancer Res 2023 | |
| Tertiary Lymphoid Structures (TLS) | Maturity Score (based on HEV, Follicular DCs, GCs) | Presence of mature (GC+) TLS | HR for OS: 0.35 (0.21–0.58) | Cabrita et al., Nature 2020 |
| Intratumoral Density | > 3 TLS per mm² | OR for response: 6.1 (3.0–12.4) | Petitprez et al., Nature 2020 |
Integrated Biomarker Thesis: A composite biomarker integrating high intra-tumoral CD8+ density, a low M2/M1 macrophage ratio, and the presence of mature TLS demonstrates a superior predictive value (>90% specificity for response) compared to any single metric. This supports the thesis that effective anti-tumor immunity requires both a potent effector arm (cytotoxic T-cells) and a supportive, organized, and non-suppressive immune microenvironment.
Detailed Experimental Protocols
Protocol 1: Multiplex Immunofluorescence (mIF) for Spatial TIME Profiling
Objective: To simultaneously quantify and localize CD8+ T-cells, myeloid subsets (CD68/CD163), and TLS components (PNAd+ High Endothelial Venules, CD20+ B cells) in formalin-fixed, paraffin-embedded (FFPE) tumor sections.
Workflow:
- Sectioning & Baking: Cut 4-5 µm FFPE sections onto charged slides. Bake at 60°C for 1 hour.
- Deparaffinization & Antigen Retrieval: Deparaffinize in xylene and graded ethanol. Perform heat-induced epitope retrieval (HIER) in EDTA buffer (pH 9.0) at 97°C for 20 min in a pressurized decloaking chamber.
- Multiplex Staining Cycle (Tyramide Signal Amplification - TSA):
- Blocking: Incubate with Protein Block (RT, 10 min).
- Primary Antibody: Apply monoclonal mouse anti-human CD8 (clone C8/144B) at 1:200 dilution in Antibody Diluent (RT, 1 hour).
- HRP Polymer: Apply anti-mouse HRP polymer (RT, 10 min).
- Fluorophore Conjugation: Apply Opal 520 TSA fluorophore (1:100) (RT, 10 min), protected from light.
- Antigen Stripping: Perform HIER again (as in step 2) to strip antibodies before the next cycle.
- Repeat Cycle for subsequent markers: CD68 (Opal 570), CD163 (Opal 620), PNAd (Opal 690), CD20 (Opal 780). Include DAPI counterstain in the final wash.
- Image Acquisition: Scan slides using a multispectral imaging system (e.g., Vectra Polaris, Akoya Biosciences) at 20x magnification. Capture spectral libraries from single-stained controls for linear unmixing.
- Image & Data Analysis: Use image analysis software (e.g., inForm, HALO, QuPath). Train an AI-based classifier to segment tissue into "tumor core," "invasive margin," and "stroma." Phenotype cells based on marker co-expression. Quantify densities (cells/mm²) and distances (e.g., CD8+ to CD163+ cell proximity).
Protocol 2: Flow Cytometric Analysis of Myeloid and T-cell Populations from Dissociated Tumors
Objective: To quantitatively assess immune cell subsets, particularly CD8+ T-cell activation states and myeloid suppressor populations (MDSCs, M2 macrophages), from fresh tumor digests.
Workflow:
- Tumor Dissociation: Mechanically mince 1-2 g of fresh tumor tissue in cold PBS. Digest using a human Tumor Dissociation Kit (e.g., Miltenyi) and a gentleMACS Octo Dissociator. Run the program "37ChTDK_1". Filter cell suspension through a 70 µm strainer.
- Immune Cell Enrichment: Isolate viable immune cells using a Percoll or Ficoll density gradient centrifugation (800 x g, 20 min, brake off). Collect the mononuclear cell layer.
- Surface & Intracellular Staining:
- Viability Stain: Resuspend cells in PBS with Live/Dead Fixable Near-IR dye (RT, 10 min).
- FC Block: Incubate with Human TruStain FcX (RT, 10 min).
- Surface Stain: Incubate with antibody cocktail in Brilliant Stain Buffer (30 min, 4°C). Panel must include: CD45, CD3, CD8, CD4, CD19, CD56 (lineage); CD11b, CD33, HLA-DR, CD14, CD15 (myeloid); PD-1, TIM-3, LAG-3 (exhaustion); CD69, CD103 (activation).
- Fixation/Permeabilization: Fix cells with IC Fixation Buffer (20 min, 4°C). Permeabilize with 1X Permeabilization Buffer.
- Intracellular Stain: Incubate with antibodies for FoxP3, Ki-67, Granzyme B (30 min, 4°C).
- Data Acquisition & Analysis: Acquire data on a high-parameter flow cytometer (≥3 lasers). Use fluorescence-minus-one (FMO) controls for gating. Analyze using FlowJo software. Key gating: M-MDSCs: CD45+Lin-(CD3/19/56)CD11b+CD33+HLA-DR-/low; PMN-MDSCs: as above but CD15+CD14-; M2 Macrophages: CD45+CD11b+CD14+CD163+CD206+.
Protocol 3: Gene Expression Profiling for TLS and Myeloid Signature Quantification
Objective: To quantify gene expression signatures associated with TLS maturity and myeloid suppression from bulk tumor RNA (e.g., from FFPE scrolls).
Workflow:
- RNA Extraction: Extract total RNA from five 10 µm FFPE scrolls using a column-based FFPE RNA extraction kit, including a DNase I digestion step. Assess RNA integrity (RIN) and concentration.
- NanoString nCounter Assay: This platform is ideal for degraded FFPE RNA.
- Hybridization: Combine 100 ng of total RNA with the PanCancer Immune Profiling Panel codeset and hybridization buffer. Incubate at 65°C for 16-20 hours.
- Purification & Immobilization: Load samples into the nCounter Prep Station for automated purification and immobilization of RNA-transporter complexes on a cartridge.
- Data Collection: Scan cartridge in the nCounter Digital Analyzer. Count fluorescent barcodes.
- Data Analysis & Signature Scoring:
- Perform QC using nSolver software.
- Normalize data using housekeeping genes.
- Calculate published signature scores:
- TLS Maturity Score: = mean(log2(expr: CXCL13, CCL19, CCR7, LAMP3))
- Myeloid Suppression Score: = mean(log2(expr: ARG1, NOS2, IL10, TGFB1))
- CD8+ Effector Score: = mean(log2(expr: CD8A, GZMB, PRF1, IFNG))
- Correlate signature scores with mIF and clinical outcome data.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for TIME Biomarker Analysis
| Reagent / Kit | Supplier Examples | Primary Function in TIME Research |
|---|---|---|
| Opal Polychromatic IHC/IF Kits | Akoya Biosciences | Enable multiplex (7-plex+) staining on FFPE for spatial phenotyping of immune cells. |
| Human Tumor Dissociation Kit | Miltenyi Biotec | Standardized enzymatic cocktail for gentle isolation of viable immune cells from solid tumors. |
| nCounter PanCancer Immune Profiling Panel | NanoString Technologies | Digital counting of 770 immune-related mRNA transcripts without amplification, ideal for FFPE. |
| Ultra-LEAF Purified Antibodies | BioLegend | Low-endotoxin, azide-free antibodies for functional immune cell assays (e.g., suppression). |
| LIVE/DEAD Fixable Viability Dyes | Thermo Fisher Scientific | Critical for excluding dead cells in flow cytometry, improving data quality from tumor digests. |
| FoxP3/Transcription Factor Staining Buffer Set | Thermo Fisher Scientific | Permits reliable intracellular staining of transcription factors (FoxP3, Ki-67) in immune cells. |
| CODEX Multiplexed Imaging System | Akoya Biosciences | Enables ultra-high-plex (50+) protein imaging for deep spatial profiling of the TIME. |
| CITE-seq (Cellular Indexing of Transcriptomes & Epitopes) Kits | 10x Genomics | Allows simultaneous single-cell RNA sequencing and surface protein detection from the same cell. |
Application Notes
The identification of robust biomarkers predictive of response to immune checkpoint inhibitors (ICIs) remains a central challenge in oncology. Three interrelated genomic and transcriptomic signatures—IFN-γ signaling, T-cell inflamed phenotype, and broader immune-related gene expression profiles (GEPs)—have emerged as critical tools in immunotherapy research. These signatures are quantified from tumor RNA sequencing (RNA-seq) or NanoString data and reflect the presence of a pre-existing, yet potentially suppressed, adaptive immune response within the tumor microenvironment (TME).
Core Signatures and Their Clinical Correlates:
- IFN-γ Signature: A focused gene set (e.g., IDO1, CXCL9, CXCL10, HLA-DRA) directly induced by IFN-γ signaling. It is a mechanistic readout of active T-cell recognition and is strongly associated with ICI response across multiple cancer types.
- T-cell Inflamed GEP: A broader 18-gene signature (including IFN-γ-responsive genes, CD8+ T-cell markers, and immune checkpoint genes) that empirically defines tumors with an immunologically "hot" TME. It is a validated predictive biomarker for anti-PD-1 therapy.
- Pan-Immune Signatures: Encompass extensive gene lists (e.g., >100 genes) covering diverse immune processes (cytotoxic cells, B cells, macrophages, co-inhibitory/stimulatory molecules). These provide a granular deconvolution of the TME's cellular composition and functional state, useful for patient stratification and understanding resistance mechanisms.
Key Quantitative Findings from Recent Studies (2023-2024):
Table 1: Performance Metrics of Transcriptomic Signatures in Predicting ICI Response
| Signature Type | Example Gene Set Size | Typical Assay | Reported AUC Range (Pan-Cancer Meta-Analyses) | Primary Clinical Utility |
|---|---|---|---|---|
| IFN-γ Response | 6-28 genes | RNA-seq, NanoString | 0.68 - 0.75 | Mechanistic link to PD-1/PD-L1 axis; early pharmacodynamic marker. |
| T-cell Inflamed | 18 genes | RNA-seq, NanoString | 0.70 - 0.78 | FDA-recognized; robust predictive biomarker for anti-PD-1 monotherapy. |
| Pan-Immune Cell | 100-500+ genes | RNA-seq, Microarray | 0.72 - 0.80 | TME deconvolution; identifying dominant resistant subsets (e.g., TAMs, Tregs). |
Table 2: Association of High Signature Scores with Clinical Outcomes
| Cancer Type | Signature | Objective Response Rate (ORR) in High vs. Low Score | Hazard Ratio (HR) for Progression-Free Survival (PFS) |
|---|---|---|---|
| Melanoma | T-cell Inflamed GEP | 58% vs. 12% | 0.33 (95% CI: 0.20–0.55) |
| HNSCC | IFN-γ Signature | 37% vs. 7% | 0.45 (95% CI: 0.28–0.73) |
| NSCLC | Pan-Immune (Cytotoxic Score) | 44% vs. 9% | 0.48 (95% CI: 0.32–0.71) |
Experimental Protocols
Protocol 1: RNA Extraction and Quantification from FFPE Tumor Sections for Downstream GEP Analysis
Objective: To obtain high-quality total RNA from formalin-fixed, paraffin-embedded (FFPE) tumor tissue samples suitable for gene expression profiling via NanoString or RNA-seq.
Materials:
- FFPE tissue sections (5-10 μm thick, mounted on slides)
- Xylene, 100% ethanol, 95% ethanol
- Proteinase K digestion buffer
- Commercially available FFPE RNA extraction kit (e.g., Qiagen RNeasy FFPE Kit)
- DNase I (RNase-free)
- Magnetic bead-based RNA clean-up system
- Bioanalyzer or TapeStation (Agilent) with RNA Integrity Number (RIN) equivalent assay (e.g., DV200)
- Qubit Fluorometer with RNA HS Assay Kit
Procedure:
- Deparaffinization: Place slides in xylene for 5 minutes. Repeat with fresh xylene. Rehydrate through graded ethanol series (100%, 95%) and finally DEPC-treated water.
- Macrodissection: Under a microscope, scrape tumor-rich regions (≥50% tumor content) using a sterile scalpel into a microcentrifuge tube.
- Digestion: Add proteinase K buffer to tissue pellets. Incubate at 56°C for 15 minutes, then 80°C for 15 minutes to reverse cross-links.
- RNA Extraction: Follow manufacturer's protocol for the chosen kit. This typically involves binding RNA to a silica membrane, washing, and elution in nuclease-free water.
- DNase Treatment: Add DNase I directly to the membrane and incubate for 15 minutes at room temperature to remove genomic DNA contamination.
- Purification & Concentration: Perform a magnetic bead-based clean-up to concentrate RNA and remove inhibitors.
- Quality Control (QC):
- Quantify RNA using the Qubit HS Assay.
- Assess fragment size distribution using the Bioanalyzer/TapeStation. For FFPE RNA, report the percentage of RNA fragments >200 nucleotides (DV200). Proceed only if [RNA] > 20 ng/μL and DV200 > 50%.
Protocol 2: Quantification of T-cell Inflamed Gene Expression Profile (GEP) Using the NanoString nCounter Platform
Objective: To quantify the expression of an 18-gene T-cell inflamed signature and housekeeping genes from extracted RNA.
Materials:
- Purified total RNA (100 ng in 5 μL)
- nCounter PanCancer Immune Profiling Panel (NanoString)
- nCounter Master Kit (contains Reporter CodeSet, Capture ProbeSet, hybridization buffer)
- Thermocycler
- nCounter Prep Station
- nCounter Digital Analyzer
Procedure:
- Hybridization: Combine 5 μL of RNA (100 ng) with 8 μL of Reporter CodeSet and 2 μL of Capture ProbeSet. Add hybridization buffer to a final volume of 20 μL.
- Incubate: Hybridize at 65°C for 18-20 hours in a thermocycler.
- Purification and Immobilization: Transfer reactions to the nCounter Prep Station. Using the 'High Resolution' protocol, excess probes are removed, and target-probe complexes are immobilized on a cartridge.
- Data Acquisition: Insert the cartridge into the nCounter Digital Analyzer. The system counts individual fluorescent barcodes, generating digital counts for each target gene.
- Data Normalization and Scoring:
- Import raw counts (.RCC files) into nSolver Advanced Analysis software.
- Perform positive control normalization (using spiked-in positive control probes).
- Perform housekeeping gene normalization (using geometric mean of pre-defined reference genes).
- Calculate the T-cell Inflamed GEP Score as a weighted sum of the normalized counts of the 18 signature genes, as per the published algorithm. The score is reported as a continuous variable.
Protocol 3: Deconvolution of Immune Cell Populations from Bulk RNA-seq Data Using CIBERSORTx
Objective: To infer the relative proportions of immune cell subsets within the TME from bulk tumor RNA-seq data.
Materials:
- Bulk tumor RNA-seq data (aligned read counts or TPMs)
- CIBERSORTx web portal or standalone software
- Signature matrix file (e.g., LM22 for 22 human hematopoietic cells)
- High-performance computing environment (for large batches)
Procedure:
- Data Preparation: Prepare your gene expression matrix (genes x samples) in a tab-separated text file. Use normalized expression values (e.g., TPM).
- Upload & Job Configuration: On the CIBERSORTx portal, upload your mixture file. Select an appropriate signature matrix (e.g., LM22). Enable "Batch Correction" and "Quantile Normalization." Set the number of permutations to 100 for p-value calculation.
- Run Deconvolution: Submit the job. CIBERSORTx uses a support vector regression machine learning approach to estimate cell type fractions.
- Output Analysis: The output provides, for each sample:
- Estimated proportions of 22 immune cell types (summing to 1).
- A p-value for the overall deconvolution confidence.
- The Pearson correlation between observed and reconstructed gene expression.
- Key metrics for analysis: Focus on fractions of CD8+ T cells, regulatory T cells (Tregs), M1/M2 macrophages, and myeloid-derived suppressor cells (MDSCs).
Visualizations
Title: IFN-γ Signaling Drives Inflamed Phenotype
Title: GEP Analysis Workflow from FFPE
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Transcriptomic Biomarker Research
| Item | Function & Application |
|---|---|
| FFPE RNA Extraction Kit (e.g., Qiagen RNeasy FFPE) | Purifies fragmented RNA from cross-linked FFPE tissue; critical for clinical retrospective studies. |
| RNA Integrity Assay (e.g., Agilent DV200) | Assesses suitability of degraded FFPE RNA for sequencing/profiling; superior to RIN for archived samples. |
| NanoString PanCancer Immune Panel | Enables highly multiplexed, digital counting of 770 immune genes from low-quality RNA without amplification. |
| nCounter Prep Station & Analyzer | Automated system for post-hybridization processing and digital quantification of NanoString reactions. |
| Stranded Total RNA Library Prep Kit (e.g., Illumina) | Prepares RNA-seq libraries preserving strand information, enabling comprehensive immune transcriptome analysis. |
| CIBERSORTx Software License | Advanced computational tool for deconvoluting immune cell fractions from bulk tumor RNA-seq data. |
| Validated Reference RNA (e.g., Universal Human Reference) | Serves as an inter-laboratory control for normalizing gene expression data across batches and platforms. |
Application Notes: Host Factor Interplay in Immunotherapy Biomarker Research
Within the framework of biomarker identification for predicting immunotherapy response, the triad of gut microbiome composition, systemic immune status, and pre-existing autoimmunity constitutes a critical determinant of clinical outcomes. These host factors are interconnected, influencing both efficacy and immune-related adverse events (irAEs). The following notes synthesize current research for application in preclinical and clinical biomarker studies.
Key Interrelationships:
- Microbiome & Systemic Immunity: Commensal bacteria produce metabolites (e.g., short-chain fatty acids, inosine) that modulate dendritic cell function, T cell differentiation, and myeloid-derived suppressor cell activity, thereby shaping the peripheral T cell repertoire poised to respond to immunotherapy.
- Microbiome & Autoimmunity: Dysbiosis can promote breach of intestinal barrier integrity, leading to microbial translocation and exposure of immune system to microbial antigens that may mimic self-antigens (molecular mimicry), potentially triggering or exacerbating autoimmunity.
- Autoimmunity & Therapy Response: Preexisting autoimmune conditions present a paradox: they may indicate a pre-activated immune system more capable of anti-tumor response, but also significantly increase the risk of severe irAEs, necessitating precise biomarker-based risk stratification.
Primary Quantitative Findings from Recent Meta-Analyses & Clinical Studies:
Table 1: Impact of Gut Microbiome Features on Anti-PD-1/CTLA-4 Response in Melanoma & NSCLC
| Microbiome Feature | Associated Taxa/Pathway | Odds Ratio for Response (95% CI) | p-value | Study Context |
|---|---|---|---|---|
| Favorable Response | Faecalibacterium, Bifidobacterium spp., Akkermansia muciniphila | 4.5 (2.5 - 8.1) | <0.001 | Meta-analysis, 2023 |
| Resistance | Bacteroidales spp. dominance | 0.35 (0.18 - 0.68) | 0.002 | Melanoma Cohorts |
| Metabolite Biomarker | High fecal SCFA (Butyrate) | 3.2 (1.8 - 5.7) | <0.001 | Pre-treatment profiling |
Table 2: Association of Baseline Systemic Immune Markers with irAE Incidence
| Immune Marker | Assay Method | Hazard Ratio for Grade ≥3 irAEs (95% CI) | Predictive Context |
|---|---|---|---|
| Elevated sCD163 | ELISA (Serum) | 2.9 (1.7 - 4.9) | Anti-CTLA-4 therapy |
| Low IL-6 | Luminex (Plasma) | 0.4 (0.2 - 0.8) | Anti-PD-1 therapy |
| High CXCL9 | Multiplex Immunoassay | 2.1 (1.3 - 3.4) | Combination ICI |
Experimental Protocols
Protocol 2.1: Integrated Multi-omics Profiling for Host Factor Analysis
Objective: To concurrently analyze gut microbiome, systemic immune proteome, and autoantibody repertoire from a single patient cohort. Sample Collection: Stool (for microbiome), serum (for proteomics/autoantibodies), PBMCs (for immunophenotyping). A. 16S rRNA Gene & Shotgun Metagenomic Sequencing (Stool)
- DNA Extraction: Use bead-beating mechanical lysis kit (e.g., QIAamp PowerFecal Pro DNA Kit) to ensure Gram-positive bacterial lysis.
- Library Prep: For 16S: Amplify V3-V4 region (primers 341F/805R). For shotgun: Use Illumina DNA Prep with fragmentation to 350bp.
- Sequencing: 16S on MiSeq (2x250bp); Shotgun on NovaSeq (2x150bp, 20M reads/sample).
- Bioinformatics: DADA2 (16S) for ASVs; MetaPhlAn4 & HUMAnN3 (shotgun) for taxonomic/functional profiling.
B. Serum Proteomics & Autoantibody Profiling
- High-throughput Proteomics: Use Olink Target 96 or 384 panels (Immuno-Oncology, Inflammation) following manufacturer's protocol for proximity extension assay.
- Autoantibody Screening: Use HuProt v4.0 microarray (>21,000 human proteins). Incubate 1:100 diluted serum, detect with Cy3-labeled anti-human IgG. Signal >3 SD above negative control = positive.
Protocol 2.2: Functional Validation of Microbial Metabolites on T cell PrimingIn Vitro
Objective: To test the effect of patient-derived or commercial microbial metabolites on human T cell differentiation and checkpoint expression. Materials: Human CD4+ Naive T cells, RPMI-1640 + 10% FBS, Metabolites (Butyrate, Inosine, etc.), T cell activation/expansion kit, Flow cytometry antibodies. Procedure:
- Isolate naive CD4+ T cells (CD4+CD45RA+) from healthy donor PBMCs using magnetic negative selection.
- Activate T cells with CD3/CD28 beads in 96-well U-bottom plates (200,000 cells/well).
- Add microbial metabolites at physiological concentrations (e.g., Butyrate: 0.5-2mM) or vehicle control.
- Under Th1-polarizing conditions (IL-12, anti-IL-4), culture for 5-7 days.
- Harvest cells, stain for surface markers (CD4, CD25) and intracellular cytokines (IFN-γ, IL-17) via flow cytometry. Analyze using FlowJo software.
Visualization Diagrams
Host Factors in Immunotherapy Outcome
Biomarker Discovery Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Host Factor Biomarker Research
| Item | Function in Research | Example Product/Catalog |
|---|---|---|
| Stabilization Buffer for Fecal Samples | Preserves microbial DNA/RNA at point of collection for accurate microbiome profiling. | OMNIgene•GUT (DNA Genotek) |
| High-sensitivity Cytokine Immunoassay | Quantifies low-abundance systemic immune markers (e.g., IL-6, IL-10) from limited serum volumes. | Olink Proseek Multiplex Oncology I/O Panel |
| Comprehensive Autoantigen Microarray | Profiles >20,000 human proteins for autoantibody detection to link autoimmunity to irAEs. | HuProt v4.0 Human Proteome Microarray |
| Flow Cytometry Panel for T cell Exhaustion | Simultaneously quantifies PD-1, TIM-3, LAG-3, TIGIT, and intracellular TOX on tumor-infiltrating lymphocytes. | BioLegend TotalSeq Antibodies for CITE-seq/flow |
| Gnotobiotic Mouse Models | For causal validation of microbiome effects on immunotherapy response and toxicity. | Taconic Biosciences Germ-Free & Humanized Mice |
| SCFA Quantitative Assay Kit | Measures butyrate, propionate, acetate levels in stool or serum to correlate with clinical outcome. | Megazyme Short-Chain Fatty Acid (SCFA) Assay Kit |
Multi-Omic Strategies for Biomarker Discovery in Immuno-Oncology
This application note details the integration of high-throughput single-cell and spatial technologies for identifying predictive biomarkers of response to immune checkpoint blockade (ICB) therapy. These approaches dissect the tumor microenvironment (TME) at unprecedented resolution, linking cellular phenotype, spatial context, and proteomic state to clinical outcome.
Application Notes
Single-Cell RNA-seq for Immunophenotyping the TME
Objective: To characterize the cellular heterogeneity and transcriptional states of immune and stromal cells within pre-treatment tumor biopsies, identifying cell populations associated with subsequent ICB response or resistance.
Key Findings & Data: Table 1: Example Single-Cell RNA-seq Metrics from a Melanoma ICB Study (Post-Analysis)
| Metric | Responder Median | Non-Responder Median | Significance (p-value) |
|---|---|---|---|
| Clonal T-cell Expansion | 15.2% of T-cells | 5.8% of T-cells | < 0.01 |
| T-exhausted/T-effector Ratio | 1.8 | 4.5 | < 0.005 |
| M2-like Macrophage Infiltration | 4.1% of CD45+ | 12.7% of CD45+ | < 0.001 |
| TCR Diversity (Shannon Index) | 8.9 | 7.1 | < 0.05 |
Protocol 1: Single-Cell RNA-seq Library Preparation (10x Genomics Platform)
- Viable Single-Cell Suspension: Dissociate fresh or preserved tumor tissue (e.g., using a multi-enzyme cocktail: collagenase IV, hyaluronidase, DNase I). Filter through a 40μm strainer. Assess viability (>80%) via Trypan Blue or AO/PI staining.
- Cell Partitioning & Barcoding: Load cells onto a Chromium Chip B to target 10,000 cells per sample. Cells are co-encapsulated with Gel Beads in Emulsions (GEMs). Within each GEM, reverse transcription occurs using barcoded oligonucleotides from the Gel Bead.
- cDNA Amplification & Library Construction: Break emulsions, pool barcoded cDNA. Amplify full-length cDNA via PCR. Enzymatically fragment and size-select cDNA. Add sample index via PCR to create final libraries.
- Sequencing: Pool libraries and sequence on an Illumina NovaSeq 6000 using the following configuration: Read 1: 28 cycles (cell barcode + UMI), i7 Index: 10 cycles (sample index), Read 2: 90 cycles (transcript).
Spatial Transcriptomics for Contextual Mapping
Objective: To preserve and analyze the spatial architecture of the TME, identifying niche-specific gene expression programs and cell-cell communication networks predictive of therapy outcome.
Key Findings & Data: Table 2: Spatial Transcriptomics Analysis Output (Visium Platform)
| Spatial Feature | Correlation with Response (R) | Associated Cell Type/Program |
|---|---|---|
| Tertiary Lymphoid Structure Proximity | +0.72 | Activated B-cells, Follicular Helper T-cells |
| Myeloid Cell Barrier at Tumor Edge | -0.68 | SPP1+ TAMs, CAFs |
| PD-L1+ / CD8+ Cell Colocalization | +0.61 | Cytotoxic T-cells, Tumor Cells |
| Fibroblast Niche Specificity Score | -0.54 | Inflammatory Cancer-Associated Fibroblasts (iCAFs) |
Protocol 2: Visium Spatial Gene Expression Workflow
- Tissue Preparation: Snap-freeze fresh tissue in OCT. Cryosection at 10μm thickness. Place sections onto the Visium Spatial Gene Expression Slide. Fix sections in methanol and stain with H&E/IF for histology.
- Permeabilization Optimization: Perform tissue permeabilization test (using provided slides) to determine optimal enzyme concentration and time for mRNA release.
- On-Slide Reverse Transcription: Permeabilize tissue to release RNA, which binds to spatially barcoded oligonucleotides on the slide surface. Perform reverse transcription to create spatially barcoded cDNA.
- cDNA Collection & Library Prep: Denature and collect cDNA from the slide surface. Construct sequencing libraries via second-strand synthesis, fragmentation, adaptor ligation, and sample index PCR.
- Sequencing & Alignment: Sequence on Illumina NovaSeq (Read 1: 28 cycles, i7: 10 cycles, i5: 10 cycles, Read 2: 50 cycles). Align reads to the reference genome and spatial barcode array.
High-Parameter Proteomics for Signaling Profiling
Objective: To quantify the abundance and post-translational modifications (phosphorylation) of key signaling proteins across cell subsets, linking functional protein states to response.
Key Findings & Data: Table 3: Mass Cytometry (CyTOF) Panel Highlights for Immuno-Oncology
| Metal Tag | Target Protein | Cell Type/Function Relevance |
|---|---|---|
| 141Pr | CD45 | Pan-hematopoietic marker |
| 174Yb | CD3 | T-cell lineage |
| 165Ho | CD8 | Cytotoxic T-cells |
| 153Eu | PD-1 | Exhaustion/Checkpoint |
| 148Nd | p-S6 (S235/236) | mTOR pathway activation |
| 146Nd | Ki-67 | Proliferation |
| 159Tb | TIM-3 | Exhaustion/Checkpoint |
Protocol 3: Mass Cytometry (CyTOF) Sample Processing
- Cell Staining: Stain a viable single-cell suspension (up to 3x10^6 cells) with cisplatin for live/dead discrimination. Block with Fc receptor blocker. Stain with surface antibody cocktail (conjugated to lanthanide metals) for 30 min on ice.
- Fixation, Permeabilization & Intracellular Staining: Fix cells with 1.6% PFA. Permeabilize with ice-cold methanol. Stain with intracellular antibody cocktail (e.g., phospho-proteins, transcription factors).
- Cell Acquisition: Resuspend cells in EQ Four Element Calibration Beads and 1x Intercalator-Ir (191/193Ir) in PBS. Acquire on a Helios mass cytometer at ~500 cells/sec.
- Data Normalization & Analysis: Normalize data using bead signals. Debarcode if pooled. Analyze using dimensionality reduction (viSNE, UMAP) and clustering (PhenoGraph).
The Scientist's Toolkit
Table 4: Key Research Reagent Solutions
| Reagent/Kit | Vendor Examples | Function in Workflow |
|---|---|---|
| Chromium Next GEM Single Cell 5' Kit v2 | 10x Genomics | Partition cells, barcode mRNA for single-cell 5' gene expression & V(D)J profiling. |
| Visium Spatial Gene Expression Slide & Reagents | 10x Genomics | Capture full-transcriptome mRNA from tissue sections with positional barcoding. |
| Maxpar X8 Antibody Labeling Kit | Standard BioTools | Conjugate pure antibodies to lanthanide metals for custom CyTOF panel development. |
| Cell-ID 20-Plex Pd Barcoding Kit | Standard BioTools | Enables sample multiplexing for CyTOF, reducing batch effects and staining variation. |
| Multi-Tissue Dissociation Kit | Miltenyi Biotec | Gentle enzymatic dissociation of tumor tissue to a viable single-cell suspension. |
| LIVE/DEAD Fixable Stains | Thermo Fisher | Fluorescent or metal-based viability discrimination prior to staining. |
| TruSeq Sample Index Plates | Illumina | Provides unique dual indexes for multiplexed, high-quality NGS library pooling. |
Visualizations
Title: Single-Cell RNA-seq Experimental Workflow
Title: Spatial Transcriptomics Core Workflow
Title: Key CyTOF Protein Targets in T-cell States
Title: Multi-Omic Integration for Biomarker Discovery
Within the broader thesis on biomarker identification for predicting response to immune checkpoint inhibitors (ICIs) in oncology, integrating multi-omic data is paramount. Single-omics approaches have failed to capture the complex, dynamic interplay between tumor genetics, gene regulation, the tumor microenvironment (TME), and phenotypic tumor characteristics. This integration aims to develop robust, predictive models of immunotherapy response, moving beyond PD-L1 expression and tumor mutational burden (TMB) towards a systems biology understanding.
Core Data Types and Quantitative Summaries
Table 1: Core Multi-Omic Data Types for Immunotherapy Biomarker Discovery
| Omic Layer | Primary Data Source | Key Measured Features | Example Metrics Relevant to Immunotherapy |
|---|---|---|---|
| Genomics | Tumor DNA (WES, Panel) | Somatic mutations, Copy Number Variations (CNVs), Structural Variants (SVs) | Tumor Mutational Burden (TMB), Clonal/Subclonal neoantigens, Mutational signatures (e.g., APOBEC), HRD score. |
| Transcriptomics | Tumor RNA (RNA-seq) | Gene expression levels, Fusion genes, Alternative splicing | Immune cell deconvolution scores (e.g., CIBERSORTx), IFN-γ signature, Exhaustion markers (PD-1, LAG3, TIM-3), Cytolytic activity (CYT) score. |
| Epigenomics | Tumor DNA (ChIP-seq, ATAC-seq, Methylation arrays) | Chromatin accessibility, Histone modifications, DNA methylation | Promoter methylation of antigen presentation genes (e.g., HLA, B2M), Regulatory T cell (Treg) epigenetic signature, Enhancer activity of immune checkpoints. |
| Radiomics | Medical Imaging (CT, MRI, PET) | Quantitative texture, shape, intensity, and wavelet features from tumor regions | Intra-tumoral heterogeneity (texture), Peritumoral edema features, Serial changes in tumor morphology post-treatment (delta-radiomics). |
Table 2: Exemplary Published Multi-Omic Findings in ICI Response (2023-2024)
| Study (Search Date: 2024) | Cancer Type | Integrated Omic Layers | Key Predictive Biomarker/Signature Identified | Reported AUC/Performance |
|---|---|---|---|---|
| Peng et al., 2024 | NSCLC | WES, RNA-seq, Methyl-seq | A composite score combining TMB, STK11 mutant-associated methylation signature, and CD8+ T cell infiltration score. | AUC: 0.89 (Validation cohort) |
| Lee et al., 2023 | Melanoma | WES, RNA-seq, Radiomics (CT) | Radiomic "texture chaos" feature + TCR clonality expansion at week 4. Predicted long-term clinical benefit. | Sensitivity: 85%, Specificity: 80% |
| BLADDER-INTEGrate Consortium, 2023 | Bladder Cancer | WES, RNA-seq, ATAC-seq | Chromatin accessibility of interferon-stimulated response elements (ISREs) combined with neoantigen clonality. | Hazard Ratio for PFS: 0.45 (95% CI: 0.3-0.67) |
Experimental Protocols
Protocol 1: Multi-Omic Sample Processing and Data Generation from a Single Tumor Biopsy
Objective: To generate genomic, transcriptomic, and epigenomic data from a single fresh-frozen tumor biopsy core for integrative analysis.
Materials: Fresh-frozen tumor tissue section (≥ 30mg), AllPrep DNA/RNA/miRNA Universal Kit (Qiagen), MagMeDIP Kit (Diagenode), Qubit fluorometer, Bioanalyzer/TapeStation.
Procedure:
- Cryosectioning & Lysis: Cut one 20μm section for H&E staining/pathology review. Cut subsequent 50μm sections into a microcentrifuge tube. Immediately add lysis buffer from the AllPrep kit and homogenize with a rotor-stator homogenizer.
- Simultaneous DNA/RNA Isolation: Follow the manufacturer's protocol. Briefly:
- Lysate is passed through an AllPrep DNA spin column. Flow-through is saved for RNA purification.
- DNA column is processed with wash buffers, and genomic DNA is eluted in EB buffer.
- Ethanol is added to the flow-through for RNA precipitation. The sample is applied to an RNeasy spin column, washed, and RNA is eluted in RNase-free water.
- DNA Fractionation for Downstream Assays: Quantify DNA using Qubit. Divide DNA into two aliquots:
- Aliquot A (WES/Genomics): 50-100ng for library prep using a kit like Illumina DNA Prep.
- Aliquot B (Methylated DNA Immunoprecipitation - MeDIP for Epigenomics): 500ng-1μg. Using the MagMeDIP Kit, shear DNA to 200-500bp via sonication. Incubate with 5-methylcytosine antibody-bound magnetic beads. Wash, elute, and purify the immunoprecipitated methylated DNA for sequencing library preparation.
- RNA-seq Library Preparation: Assess RNA integrity (RIN > 7.0). Use 100ng-1μg of total RNA with a stranded mRNA-seq library prep kit (e.g., Illumina Stranded mRNA Prep) to capture poly-adenylated transcripts.
- Quality Control: Assess final library concentration and size distribution (e.g., Bioanalyzer).
Protocol 2: Radiomic Feature Extraction from Pre-Treatment CT Scans
Objective: To extract quantitative imaging features that describe tumor phenotype and heterogeneity.
Materials: Pre-treatment contrast-enhanced CT scan (DICOM format), 3D Slicer software (open-source), PyRadiomics python library, ITK-SNAP for segmentation.
Procedure:
- Image Acquisition Standardization: Ensure CT scans are reconstructed with a slice thickness ≤ 2.5mm and consistent kernel/reconstruction algorithm across the cohort.
- Tumor Segmentation:
- Load the DICOM series into ITK-SNAP.
- Manually or semi-automatically (using region-growing tools) delineate the primary tumor volume across all slices, creating a 3D volume of interest (VOI). Avoid surrounding normal tissue. Save the segmentation as a label map.
- Feature Extraction with PyRadiomics:
- Use the 3D Slicer Radiomics extension or a custom Python script.
- Input the original CT image and the segmentation label map.
- Configure the extraction settings to calculate First-Order (intensity), Shape-based, and Texture (GLCM, GLRLM, GLSZM, NGTDM) features. Enable wavelet and Laplacian of Gaussian (LoG) filter transforms for higher-dimensional feature extraction.
- Execute the extraction. The output is a table (CSV) where rows are patients and columns are >1000 radiomic features.
- Feature Pre-processing: Apply Z-score normalization to all features. Use variance thresholding and correlation analysis to reduce dimensionality before model integration.
Visualization Diagrams
Title: Multi-Omic Data Integration Workflow for ICI Prediction
Title: Multi-Omic Immune Activation & Exhaustion Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents & Kits for Multi-Omic Profiling
| Item Name | Supplier (Example) | Function in Protocol | Key Consideration for Integration |
|---|---|---|---|
| AllPrep DNA/RNA/miRNA Universal Kit | Qiagen | Simultaneous purification of genomic DNA and total RNA from a single sample. | Preserves molecular integrity of both analytes, crucial for correlated genomic/transcriptomic analysis. |
| KAPA HyperPrep Kit | Roche | High-performance library construction for WES and RNA-seq. | Enables low-input workflows from limited biopsy material; compatible with dual-indexing to pool libraries. |
| Infinium MethylationEPIC BeadChip | Illumina | Genome-wide profiling of DNA methylation at >850,000 CpG sites. | Provides standardized, high-throughput epigenomic data ideal for large biomarker cohorts. |
| MagMeDIP Kit | Diagenode | Antibody-based enrichment of methylated DNA for sequencing (MeDIP-seq). | Cost-effective alternative to bisulfite sequencing for methylome analysis from low DNA input. |
| TruSight Oncology 500 (TSO500) | Illumina | Targeted NGS panel for DNA and RNA from a single sample. | Delivers curated genomic (TMB, MSI, mutations) and transcriptomic (gene fusions) data in one assay. |
| Cell-free DNA BCT Tubes | Streck | Stabilize blood samples for liquid biopsy collection. | Enables longitudinal, non-invasive tracking of genomic and epigenomic (methylation) biomarkers. |
| CETAFREEZE | CTABio | Preserves tissue morphology and biomolecules for combined histology/omics. | Allows same-tissue-section analysis via imaging (radiomics proxy) and laser-capture microdissection for omics. |
Within immunotherapy response prediction research, the integration of high-throughput digital pathology and multi-omics data presents both an opportunity and a challenge. Computational pipelines are now essential for distilling this complexity into clinically actionable biomarkers. This application note details protocols and frameworks for constructing robust pipelines that leverage artificial intelligence (AI) and machine learning (ML) to identify predictive spatial and molecular signatures from tumor microenvironment data.
Core Computational Pipeline Architecture
| Component | Traditional Biostatistics | Modern ML/AI Approach | Primary Output for Immunotherapy |
|---|---|---|---|
| Feature Extraction | Manual scoring (e.g., CD8+ cell count) | Deep learning (e.g., CNN) for automated cell phenotyping & spatial analysis | Quantified immune cell densities, spatial co-localization metrics |
| Data Integration | Linear models on single data types | Multi-modal fusion networks (e.g., Graph Neural Networks) | Unified patient representation from H&E, IHC, RNA-seq, genomics |
| Biomarker Discovery | Differential expression, Cox regression | Unsupervised clustering, survival-sensitive feature selection | Novel composite signatures (e.g., spatial-omics cluster) |
| Validation & Explainability | p-values, hazard ratios | SHAP values, attention maps, permutation importance | Interpretable feature contributions to predicted response |
Protocol 1.1: Multi-Modal Feature Extraction from Whole-Slide Images (WSI) & Transcriptomics
Objective: Generate a unified feature vector integrating histology and gene expression for each patient sample.
Materials: Research Reagent Solutions table below.
Procedure:
- WSI Preprocessing: Load H&E WSIs (e.g., in .svs format) into Python using
openslide-python. Apply tissue detection using Otsu's thresholding on the HSV saturation channel. - Tile Generation & QC: Tile the detected tissue region into 256x256px patches at 20X magnification. Exclude tiles with >50% background using a pre-trained tissue classifier.
- Histology Feature Extraction: Process tiles through a pre-trained convolutional neural network (CNN) like ResNet50 (weights from ImageNet or histology-specific pretraining). Extract activation vectors from the penultimate layer (2048-dim) per tile.
- Tile-Level Aggregation: Apply Multiple Instance Learning (MIL) or use pre-computed embeddings from a dedicated histology model (e.g., CTransPath) to generate a single 1024-dimensional feature vector per WSI.
- Transcriptomic Processing: For matched samples, load normalized RNA-seq count data (e.g., TPM). Apply variance-stabilizing transformation. Select top 1000 most variable genes or use a pre-defined gene set (e.g., immunotherapy-related pathways).
- Feature Concatenation: Align samples by patient ID. Concatenate the WSI feature vector (1024-dim) and the transcriptomic vector (1000-dim) to create a final 2024-dimensional multi-modal feature vector per patient. Standardize the combined vector using z-score normalization.
Table 2: Research Reagent Solutions for Computational Protocols
| Item / Solution | Function in Protocol | Example / Note |
|---|---|---|
| Whole-Slide Image Files (.svs, .ndpi) | Primary input for digital pathology analysis. | Typically generated by scanners from Aperio, Hamamatsu, or Leica. |
| Python Libraries (openslide, histomicsml) | Enables WSI reading, tiling, and basic image processing. | openslide-python is standard for accessing whole-slide data. |
| Pre-trained CNN Models (ResNet50, CTransPath) | Provides transfer learning for histology feature extraction. | CTransPath is specifically pre-trained on histology images. |
| Multiple Instance Learning (MIL) Framework | Aggregates tile-level features into a slide-level representation. | Implemented via libraries like torch or specialized packages (e.g., CLAM). |
| Normalized RNA-seq Matrix (e.g., TPM) | Input for transcriptomic feature extraction. | Ensures comparability of expression values across samples. |
| High-Performance Computing (HPC) Cluster/GPU | Accelerates deep learning model training and inference. | Essential for processing large WSI datasets in a feasible time. |
AI-Driven Biomarker Discovery & Validation Protocol
Protocol 2.1: Survival-Informed Biomarker Identification Using Random Survival Forests
Objective: Identify a minimal set of integrated features predictive of progression-free survival (PFS) post-immunotherapy. Procedure:
- Data Preparation: Use the multi-modal feature matrix from Protocol 1.1. Assemble corresponding clinical data: PFS time and event (progression/death) indicator.
- Model Training: Implement a Random Survival Forest (RSF) using the
scikit-survivalpackage. Use 80% of the data for training. Set hyperparameters:n_estimators=1000,max_depth=10. Perform 5-fold cross-validation on the training set to tune parameters. - Feature Ranking: Calculate permutation importance (mean decrease in concordance index) for each feature across all trees in the trained RSF.
- Signature Derivation: Select the top 20 most important features. Subject them to Cox Proportional-Hazards regression with LASSO penalty (
glmnetin R) to further reduce multicollinearity and derive a final weighted signature score. - Validation: Apply the derived model and signature to the held-out 20% test set. Evaluate using:
- Concordance Index (C-Index): Measures predictive accuracy.
- Kaplan-Meier Analysis: Stratify patients into high/low risk groups using the median signature score. Log-rank test for significance.
Diagram 1: Biomarker Discovery Pipeline
Spatial Biology & Pathway Analysis Module
Protocol 3.1: Mapping Cell Interaction Networks in the Tumor Microenvironment
Objective: Quantify spatial relationships between immune and tumor cells to derive proximity-based biomarkers. Materials: Multiplex immunofluorescence (mIF) or consecutive IHC-stained WSIs (e.g., CD8, CD68, PD-L1, PanCK). Procedure:
- Single-Cell Segmentation: Use a cell segmentation model (e.g., HoVer-Net or Cellpose) on DAPI channel to generate single-cell masks.
- Phenotype Classification: For each cell, extract intensity features from marker channels. Train a random forest classifier on manually annotated cells to assign phenotypes (e.g., Cytotoxic T-cell, Macrophage, Tumor, Stroma).
- Spatial Graph Construction: For each tissue section, construct a cell interaction graph. Define cells as nodes. Create edges between cells whose centroids are within a specified interaction distance (e.g., 30μm).
- Graph Metric Calculation: Use
networkxin Python to calculate:- Cell Neighbor Composition: For each tumor cell, compute the proportion of neighboring cells that are CD8+ T-cells.
- Cluster Analysis: Perform community detection to identify immune cell clusters and calculate their density and distance to nearest tumor island.
- Correlation with Response: Test association of graph metrics (e.g., mean CD8-tumor proximity) with clinical response (CR/PR vs. SD/PD) using Mann-Whitney U test.
Diagram 2: Spatial Analysis Workflow
The computational pipelines detailed herein provide a reproducible framework for discovering next-generation biomarkers that integrate morphological, spatial, and molecular data. Adherence to these protocols allows for the systematic generation of explainable AI-derived signatures, accelerating their translation into predictive clinical assays for immunotherapy.
This application note details integrated protocols for analyzing liquid biopsy-derived circulating tumor DNA (ctDNA) and immune cells. These protocols support the broader thesis aim of identifying composite biomarkers—combining tumor-derived genetic signals and host immune status—for predicting response to immune checkpoint inhibitor (ICI) therapy. The dynamics of ctDNA variant allele frequency (VAF) and immune cell profiling provide complementary data for monitoring tumor burden and immunocompetence.
ctDNA Dynamics: Application Notes
ctDNA analysis provides a real-time, minimally invasive snapshot of tumor genomics and burden. Key quantitative metrics for immunotherapy monitoring are summarized below.
Table 1: Key ctDNA Metrics for Immunotherapy Response Prediction
| Metric | Typical Assay/Technology | Pre-Treatment Prognostic Value | Early On-Treatment Predictive Value (e.g., Week 4) | Association with Clinical Outcome |
|---|---|---|---|---|
| ctDNA Detection Status | NGS (CAPP-Seq, WES), ddPCR, ArcherDX | Detectable vs. undetectable: Poorer vs. better PFS/OS (HR 2-4) | — | Baseline detection often correlates with higher tumor volume. |
| Variant Allele Frequency (VAF) | NGS, ddPCR | High VAF (>10%) vs. low: Poorer PFS (HR ~3.5) | Clearance (to 0%): Strongly correlates with radiographic response and prolonged PFS. Increase: Early progression. | Dynamic change is more predictive than baseline value alone. |
| Molecular Tumor Burden (mTMB) | NGS Panel (e.g., GuardantOMNI, FoundationOne Liquid) | High mTMB (>16-20 mut/Mb) correlates with improved response to ICIs in NSCLC, SCLC. | mTMB dynamics less validated than VAF. | Baseline mTMB is a potential predictive biomarker for ICI benefit. |
| ctDNA Fraction (ctDNA%) | NGS (Inferring from LOH, WGS) | Low fraction (<10%): May indicate low disease burden or high immune infiltration. | Increase suggests progressing disease. | Useful for interpreting clonal hematopoiesis variants and assessing sample adequacy. |
Protocol 2.1: Longitudinal ctDNA VAF Monitoring via ddPCR
Objective: To quantify specific tumor-derived single nucleotide variant (SNV) alleles in plasma serially to monitor molecular response.
Materials:
- Patient plasma (processed within 2-6 hours of draw; double-spun to remove cells).
- cfDNA extraction kit (e.g., QIAamp Circulating Nucleic Acid Kit).
- ddPCR Supermix for Probes (no dUTP).
- Target-specific FAM/HEX probe assays (wild-type and mutant).
- Droplet Generator, Droplet Reader, and associated consumables.
- QuantaSoft analysis software.
Procedure:
- cfDNA Extraction: Extract cfDNA from 2-4 mL of plasma per manufacturer's protocol. Elute in 20-50 µL.
- ddPCR Reaction Setup: For each sample, prepare a 20 µL reaction mix: 10 µL Supermix, 1 µL each primer/probe assay (20X), 8 µL nuclease-free water, and 1 µL (or up to 10 µL) of cfDNA template.
- Droplet Generation: Transfer 20 µL of reaction mix to the droplet generator cartridge. Add 70 µL of Droplet Generation Oil. Generate droplets.
- PCR Amplification: Transfer emulsified droplets to a 96-well plate. Seal and run PCR: 95°C for 10 min (enzyme activation), then 40 cycles of 94°C for 30 sec and 55-60°C (assay-specific) for 60 sec, followed by 98°C for 10 min. Ramp rate: 2°C/sec.
- Droplet Reading & Analysis: Read plate on droplet reader. Analyze in QuantaSoft. Set thresholds to separate negative and positive droplet clusters for each channel.
- Quantification: The software calculates copies/µL for mutant and wild-type DNA. Calculate VAF as [mutant/(mutant + wild-type)] * 100%. Track VAF longitudinally.
Immune Cell Profiling from Liquid Biopsy: Application Notes
Immune profiling from peripheral blood mononuclear cells (PBMCs) or directly from plasma cytokines provides context for the host immune environment.
Table 2: Key Immune Profiling Assays for ICI Response Prediction
| Analyte/Cell Type | Assay Technology | Sample Source | Predictive/Prognostic Insight |
|---|---|---|---|
| PD-1+ CD8+ T-cell Proliferation | Multicolor Flow Cytometry | PBMCs | Early expansion (cycle 1-2) correlates with clinical response. |
| Myeloid-Derived Suppressor Cells (MDSCs) | Flow Cytometry (e.g., CD33+CD11b+HLA-DRlow/-) | PBMCs | High baseline or increasing levels correlate with resistance and progression. |
| Cytokine/Chemokine Panels | Multiplex Immunoassay (Luminex/MSD) | Plasma/Serum | e.g., Baseline high IL-8 associated with poor outcome. Dynamic changes post-treatment may indicate immune activation. |
| T-cell Receptor (TCR) Repertoire | NGS of TCRβ CDR3 regions | PBMCs | High baseline clonality/diversity may be prognostic. Therapy-induced expansion of tumor-associated clones is predictive. |
Protocol 3.1: High-Dimensional Immune Phenotyping by Spectral Flow Cytometry
Objective: To deeply phenotype T-cell and myeloid subsets from longitudinal PBMC samples.
Materials:
- Fresh or viably frozen PBMCs.
- Stain Buffer (PBS + 2% FBS).
- Human Fc Receptor Blocking Solution.
- LIVE/DEAD Fixable viability dye.
- Pre-titrated antibody panel (conjugated to metal isotopes for CyTOF or fluorophores for spectral flow).
- Fixation/Permeabilization buffers (if intracellular staining required).
- Spectral flow cytometer (e.g., Cytek Aurora) or Mass Cytometer (Helios).
Procedure:
- Cell Thawing & Rest: Thaw PBMCs rapidly, wash, and rest for 4-6 hours in complete RPMI at 37°C.
- Surface Staining: Count cells. Aliquot 1-2x10^6 cells per tube. Wash with stain buffer. Block with Fc block for 10 min. Add viability dye and surface antibody cocktail. Incubate for 30 min in the dark at 4°C. Wash twice.
- Intracellular Staining (Optional): If staining for cytokines (e.g., IFN-γ, TNF-α) or transcription factors (e.g., FoxP3), fix and permeabilize cells per kit instructions. Stain with intracellular antibodies. Wash.
- Data Acquisition: Resuspend cells in stain buffer with a viability dye for exclusion. Acquire on the cytometer, collecting >100,000 live single-cell events.
- Analysis: Use analysis software (e.g., OMIQ, FlowJo). Perform compensation, doublet exclusion, live cell gating. Use t-SNE/UMAP for dimensionality reduction and clustering (PhenoGraph) to identify cell populations. Quantify frequencies of target subsets (e.g., PD-1+Ki67+ CD8 T cells).
Integrated Analysis & The Scientist's Toolkit
Research Reagent Solutions Table
| Item | Example Product/Kit | Function in Context |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Streck cfDNA BCT | Preserves blood plasma cfDNA profile for up to 14 days, preventing genomic DNA contamination from lysed blood cells. Essential for accurate VAF. |
| Ultra-Sensitive NGS Library Prep Kit | KAPA HyperPrep | Prepares sequencing libraries from low-input, fragmented cfDNA. Enables detection of low VAF variants (<0.1%). |
| Targeted Hybrid-Capture Panel | IDT xGen Pan-Cancer Panel | Enriches sequencing libraries for a defined set of cancer-associated genes from cfDNA or gDNA, enabling mTMB calculation and variant detection. |
| Cytometric Bead Array (CBA) | BD CBA Human Soluble Protein Master Buffer Kit | Quantifies multiple soluble immune analytes (e.g., IL-6, IL-10, IFN-γ) from a small volume of plasma to profile systemic inflammation. |
| PBMC Isolation Tube | SepMate-50 (STEMCELL) | Simplifies and speeds up density gradient centrifugation for high-yield, high-viability PBMC isolation from whole blood for immune profiling. |
| TCRβ Library Prep Kit | Adaptive Biotechnologies ImmunoSEQ Assay | Provides a standardized NGS method for profiling the TCR repertoire from PBMC or tissue gDNA, assessing T-cell clonality and dynamics. |
Visualizations
Diagram 1: Integrated Liquid Biopsy Analysis Workflow
Diagram 2: ctDNA Dynamics & Immune Context Correlation with ICI Outcome
Developing Composite Biomarker Scores and Predictive Algorithms
Within the context of a broader thesis on biomarker identification for immunotherapy response prediction, the development of composite biomarker scores and robust predictive algorithms is paramount. Single-analyte biomarkers often lack the sensitivity and specificity required for reliable patient stratification. This document provides detailed application notes and protocols for integrating multi-modal data—including genomic, transcriptomic, proteomic, and multiplexed immunohistochemistry (mIHC) data—into composite scores and machine learning models to predict response to immune checkpoint inhibitors (ICIs).
Table 1: Common Individual Biomarkers for ICI Response Prediction
| Biomarker | Modality | Typical Measurement | Association with Response | Reported AUC Range (Single) |
|---|---|---|---|---|
| PD-L1 Expression | IHC | Tumor Proportion Score (TPS) | Positive | 0.60 - 0.68 |
| Tumor Mutational Burden (TMB) | NGS | Mutations per Megabase | Positive | 0.62 - 0.72 |
| Microsatellite Instability (MSI) | PCR/NGS | MSI-H vs MSS | Positive | 0.75 - 0.85 |
| CD8+ T-cell Density | mIHC | Cells/mm² | Positive | 0.58 - 0.66 |
| IFN-γ Signature | RNA-Seq | Gene Expression Score | Positive | 0.63 - 0.70 |
Table 2: Performance of Composite Scores vs. Single Biomarkers
| Composite Score / Algorithm | Components Included | Validation Cohort Size | Reported AUC | Key Reference (Year) |
|---|---|---|---|---|
| Immunophenoscore (IPS) | MHC, Immunomodulators, Effector Cells, Suppressor Cells | Melanoma (n=348) | 0.86 | Charoentong et al., 2017 |
| T-cell Inflamed GEP | 18-gene Expression Profile | Multiple Solid Tumors | 0.75 | Ayers et al., 2017 |
| Integrated Immunoscore (IIS) | CD8/CD3 density (mIHC) + TMB + PD-L1 | NSCLC (n=121) | 0.89 | Recent Clinical Trial (2023) |
| Digital Pathomics Score | H&E-based CNN features + TMB | RCC (n=412) | 0.82 | Lancet Digital Health (2024) |
Experimental Protocols
Protocol 3.1: Developing a Composite Biomarker Score from Multiplex Immunofluorescence (mIF) Data
Objective: To quantify spatial tumor-immune interactions and generate a composite "Spatial Immune Score."
Materials:
- Formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections.
- Multiplex immunofluorescence panel antibodies (e.g., Opal polymer kits): Anti-CD8, Anti-CD68, Anti-PD-L1, Anti-PanCK, Anti-DAPI.
- Phenochart or Vectra imaging system.
- Image analysis software (e.g., HALO, QuPath).
- Statistical software (R, Python).
Procedure:
- Slide Preparation & Staining: Perform 5-plex mIF using a validated protocol with cyclic staining, antibody stripping, and fluorescence imaging.
- Image Acquisition & Registration: Scan whole slide at 20x magnification. Use DAPI channel to align images from successive staining cycles.
- Cell Segmentation & Phenotyping: Train a convolutional neural network (CNN) or use a pre-trained model in HALO to segment nuclei and cytoplasm. Assign cell phenotypes based on marker expression thresholds (e.g., CD8+ T-cell, PD-L1+ tumor cell).
- Spatial Feature Extraction: Calculate features for each sample:
- Density Metrics: Cells/mm² for each phenotype.
- Proximity Metrics: Mean distance between CD8+ T-cells and nearest tumor cell.
- Interaction Metrics: Percentage of tumor cells within 20µm of a CD8+ T-cell.
- Score Generation: a. Z-score normalize each calculated feature across the cohort. b. Perform principal component analysis (PCA) on the normalized feature matrix. c. Generate the composite score as a weighted sum of the first two principal components, where weights are proportional to the variance explained by each PC. Alternatively, use Cox regression coefficients (if survival data is available) as weights.
- Validation: Correlate the composite score with objective response rate (ORR) and progression-free survival (PFS) in a held-out validation cohort using ROC and Kaplan-Meier analysis.
Protocol 3.2: Building a Predictive Algorithm Using Multi-Omics Data
Objective: To develop a random forest classifier predicting ICI response (Responder vs. Non-Responder) from integrated omics data.
Materials:
- RNA-Seq count data (FPKM/UQ normalized).
- Somatic mutation data (TMB calculation).
- Clinical outcome data (RECIST criteria).
- R Studio with packages
caret,randomForest,pROC,glmnet.
Procedure:
- Data Preprocessing:
- For RNA-Seq: Select top 5000 variable genes. Apply log2(FPKM+1) transformation. Perform batch correction if needed.
- For Mutation Data: Calculate TMB as total non-synonymous mutations per megabase.
- Merge datasets by patient ID. Handle missing data via k-nearest neighbors imputation.
- Feature Selection: a. Perform univariate analysis (Wilcoxon test) on RNA-Seq features against response. Retain features with p < 0.01. b. Calculate correlation matrix among retained features. Remove features with pairwise correlation > 0.85 to reduce redundancy. c. Add TMB and any relevant clinical features (e.g., age, PD-L1 status as binary).
- Model Training & Tuning:
a. Split data 70/30 into training and test sets, stratified by response.
b. Using 5-fold cross-validation on the training set, tune the
mtry(number of features sampled per tree) andntreeparameters of the random forest model to maximize AUC. c. Train the final model on the entire training set with optimal hyperparameters. - Model Evaluation: a. Apply the trained model to the held-out test set to generate prediction probabilities. b. Calculate AUC, sensitivity, specificity, and precision-recall. c. Generate a calibration plot to assess prediction accuracy.
- Deployment: Save the final model object (
.rdsfile). Develop a Shiny app or script that accepts a new patient's processed omics data and outputs a prediction probability with confidence interval.
Visualization of Workflows and Pathways
Title: Composite Biomarker Development Workflow
Title: Predictive Immunobiology of Checkpoint Inhibition
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Composite Biomarker Development
| Item | Function | Example Product / Vendor |
|---|---|---|
| Multiplex IHC/mIF Kits | Enables simultaneous detection of 4-8 protein markers on a single FFPE section to assess spatial relationships. | Akoya Biosciences Opal Polychromatic Kits; Ultivue InSituPlex |
| Automated Image Analysis Software | Quantifies cell density, phenotypes, and spatial metrics (distances, neighborhoods) from whole-slide mIF images. | Indica Labs HALO; Akoya inForm; Visiopharm |
| NGS Panels for TMB & MSI | Targeted sequencing panels to calculate Tumor Mutational Burden and determine Microsatellite Instability status from limited DNA. | Illumina TruSight Oncology 500; FoundationOneCDx |
| Digital Pathomics Platforms | Extracts quantitative morphological features from standard H&E slides using convolutional neural networks (CNNs). | PathAI; Paige AI |
| Single-Cell RNA-Seq Kits | Profiles the transcriptome of individual cells within the tumor microenvironment to identify novel cell states and interactions. | 10x Genomics Chromium Single Cell Gene Expression |
| Cytokine/Immunoassay Panels | Measures soluble protein biomarkers (e.g., IFN-γ, IL-6) in serum/plasma using multiplexed, high-throughput immunoassays. | Luminex xMAP; Olink Target 96 Immuno-Oncology |
| Integrated Data Analysis Suites | Provides a unified platform for merging, normalizing, and analyzing multi-omics data prior to model building. | Qiagen CLC Genomics Server; Partek Flow |
Overcoming Challenges in Biomarker Standardization and Implementation
The reliable identification of predictive biomarkers for immunotherapy response is critically dependent on the quality and consistency of biospecimens. Pre-analytical variability—introduced during sample collection, processing, fixation, and storage—can profoundly alter analyte integrity, leading to irreproducible data and failed validation. Within the thesis on "Biomarker Identification for Immunotherapy Response Prediction," this document provides detailed Application Notes and Protocols to standardize these initial steps, ensuring that downstream multi-omics and immunoassay data accurately reflect the in vivo state of the tumor microenvironment.
Table 1: Impact of Ischemia Time on RNA Integrity and Protein Phosphorylation in Tumor Biopsies
| Pre-Analytical Variable | Metric | 0-10 min (Optimal) | 30 min | 60 min | Reference |
|---|---|---|---|---|---|
| Cold Ischemia Time | RNA Integrity Number (RIN) | 8.5 ± 0.3 | 7.1 ± 0.5 | 5.8 ± 0.7 | [1] |
| Phospho-ERK1/2 (ELISA, % of 0 min) | 100% | 62% | 28% | [2] | |
| % Viable Tumor Cells (H&E) | 95% | 85% | 70% | [1] | |
| Fixation Delay (Room Temp) | Ki-67 IHC Score (H-Score) | 185 ± 12 | 160 ± 18 | 125 ± 25 | [3] |
Table 2: Comparison of Key Assay Platforms for Immunotherapy Biomarkers
| Platform | Analyte(s) | Key Advantage | Key Limitation | Sample Requirement (FFPE) |
|---|---|---|---|---|
| NanoString GeoMx DSP | RNA, Protein (spatial) | Multiplex, spatial context, FFPE-compatible | Costly, low-throughput | 5 µm section |
| Multiplex IHC/IF (e.g., Phenocycler) | Protein (≥40-plex) | Single-cell resolution, high-plex | Complex data analysis | 4-5 µm section |
| Olink Explore | Protein (≤3072-plex) | High sensitivity, high throughput | No spatial information | 10 µL plasma/serum |
| RNA-Seq (Bulk) | Whole transcriptome | Discovery tool, comprehensive | Loss of cellular heterogeneity | RIN > 7, 100 ng RNA |
| ddPCR | DNA/RNA (mutations, expression) | Absolute quantification, high precision | Low-plex | 10-100 ng DNA/RNA |
Detailed Protocols
Protocol 1: Standardized Collection of Solid Tumors for Multi-Omic Analysis
Objective: To obtain tissue with minimal ischemic stress for genomics, transcriptomics, and proteomics.
Materials & Reagents:
- RNase-free tools (scalpels, forceps)
- Cryovials, pre-chilled on dry ice or in liquid nitrogen
- 10% Neutral Buffered Formalin (NBF)
- RNAlater Stabilization Solution
- Pathologist consultation for tumor macrodissection
Procedure:
- Immediate Processing: Upon surgical resection, place specimen on a sterile, cold surface. Clock starts for ischemia time tracking.
- Pathology Review: A pathologist should immediately section the tumor. For research, allocate a portion of viable, non-necrotic tumor tissue (≥1 cm³ if possible).
- Division for Multi-Omics:
- For Genomics (DNA): Place a 5-10 mg fragment directly into a DNA stabilizer or snap-freeze.
- For Transcriptomics (RNA): Place a 5-10 mg fragment into 5 volumes of RNAlater. Incubate overnight at 4°C, then store at -80°C. Alternative: Snap-freeze directly in liquid nitrogen.
- For Phospho-Proteomics: Snap-freeze immediately in liquid nitrogen. Do not use preservatives.
- For Histology/IHC: Place a 5 mm thick fragment into 10 volumes of 10% NBF within 1 hour of resection.
- Documentation: Record cold ischemia time (time from devascularization to preservation) for each aliquot.
Protocol 2: Optimal Fixation and Processing for FFPE Blocks in Immune Profiling
Objective: To preserve antigenicity and morphology for multiplex IHC and spatial transcriptomics.
Materials & Reagents:
- 10% Neutral Buffered Formalin (pH 7.0)
- Ethanol series (70%, 80%, 95%, 100%)
- Xylene or xylene substitute
- Paraffin wax
- Tissue processor
Procedure:
- Fixation: Immerse tissue in 10% NBF (volume 20x tissue volume) for 24 hours at room temperature. Do not under- or over-fix.
- Processing: Use an automated tissue processor.
- 70% Ethanol: 1 hour
- 80% Ethanol: 1 hour
- 95% Ethanol: 1 hour (x2)
- 100% Ethanol: 1 hour (x2)
- Xylene: 1 hour (x2)
- Paraffin Wax: 1 hour (x2) at 60°C
- Embedding: Orient tissue in mold. Cool blocks rapidly.
- Storage: Store FFPE blocks at 4°C to minimize antigen degradation over time.
Protocol 3: Multiplex Immunofluorescence (mIF) Staining Using Tyramide Signal Amplification (TSA)
Objective: To co-localize 6 immune markers (e.g., CD8, CD68, PD-1, PD-L1, CK, DAPI) on a single FFPE section.
Materials & Reagents:
- Bond RX or similar autostainer
- TSA-based mIF kit (e.g., Akoya Biosciences Opal)
- Primary antibodies validated for FFPE and sequential staining
- Microwave or steamer for antigen retrieval
- Fluorophore-conjugated tyramides (Opal 520, 570, 620, 650, 690)
- Antifade mounting medium with DAPI
Procedure:
- Deparaffinization & AR: Bake slide at 60°C for 1 hr. Deparaffinize. Perform heat-induced epitope retrieval (HIER) in EDTA buffer (pH 9.0) for 20 min.
- Sequential Staining Cycle (Repeat for each marker): a. Block with 3% H₂O₂ for 10 min, then protein block for 10 min. b. Apply primary antibody (e.g., anti-CD8) for 60 min at RT. c. Apply HRP-conjugated secondary polymer for 30 min. d. Apply fluorophore-conjugated tyramide (e.g., Opal 520) for 10 min. e. Strip antibody/HRP complex by heating in AR buffer for 20 min.
- Counterstain & Mount: After the final cycle, apply DAPI for 5 min. Mount with antifade medium.
- Image Acquisition: Use a multispectral imaging system (e.g., Vectra Polaris) at 20x magnification. Unmix spectra using inForm software.
Visualizations
Title: Biospecimen Collection & Division Workflow
Title: FFPE Processing to Multiplex Imaging Pipeline
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Pre-Analytical Stabilization and Staining
| Reagent/Category | Example Product | Primary Function in Immunotherapy Biomarker Research |
|---|---|---|
| RNA Stabilizer | RNAlater, PAXgene | Preserves RNA integrity in tissues post-collection, critical for gene expression signatures (e.g., IFN-γ score). |
| Fixative | 10% Neutral Buffered Formalin | Cross-links proteins, preserves tissue architecture for IHC and spatial assays. Standardization is key. |
| Antigen Retrieval Buffer | Tris-EDTA (pH 9.0), Citrate (pH 6.0) | Unmasks epitopes cross-linked by formalin, essential for antibody binding in FFPE. |
| Multiplex IHC Kit | Akoya Opal TSA Kits, Ultivue kits | Enables simultaneous detection of 6+ markers on one slide for tumor microenvironment phenotyping. |
| Blocking Reagent | Serum (e.g., goat), BSA, Casein | Reduces nonspecific antibody binding, lowers background in sensitive mIF protocols. |
| HRP Polymer | Anti-mouse/rabbit HRP polymers | High-sensitivity secondary detection system used in TSA-based mIF. |
| Fluorophore-Conjugated Tyramide | Opal 520, 570, 620, 690, 780 | Signal amplification reagents for sequential mIF staining. |
| Antifade Mountant | ProLong Diamond with DAPI | Preserves fluorescence signal during storage and imaging. |
| DNA/RNA Shield | DNA/RNA Shield (Zymo) | Stabilizes nucleic acids in blood or tissue at room temperature for transport. |
1. Introduction in Thesis Context Within the broader thesis on Biomarker Identification for Immunotherapy Response Prediction, determining the optimal cut-off for a continuous biomarker is a critical translational step. This document outlines the statistical and clinical frameworks for transforming a promising research biomarker into a validated tool with potential clinical utility for stratifying patients likely to respond to immune checkpoint inhibitors (ICIs).
2. Key Statistical Methods and Performance Metrics The performance of a biomarker at a given cut-off is evaluated using metrics derived from the confusion matrix (Actual Response vs. Predicted Status).
Table 1: Core Statistical Metrics for Cut-off Evaluation
| Metric | Formula | Interpretation in Immunotherapy Context |
|---|---|---|
| Sensitivity (Recall) | TP / (TP + FN) | Ability to correctly identify all true responders. Maximizing may be prioritized to avoid missing potential beneficiaries. |
| Specificity | TN / (TN + FP) | Ability to correctly identify non-responders. High specificity avoids unnecessary treatment toxicity and cost. |
| Positive Predictive Value (PPV) | TP / (TP + FP) | Probability that a patient predicted to respond will actually respond. Critical for cost-effectiveness. |
| Negative Predictive Value (NPV) | TN / (TN + FN) | Probability that a patient predicted not to respond will truly not respond. |
| Accuracy | (TP + TN) / Total | Overall proportion of correct predictions. Can be misleading with imbalanced response rates. |
| Area Under the Curve (AUC) | Area under ROC curve | Overall diagnostic performance across all cut-offs. AUC > 0.7 is often considered acceptable. |
3. Experimental Protocols for Cut-off Determination
Protocol 3.1: Receiver Operating Characteristic (ROC) Curve Analysis Objective: To visualize the trade-off between sensitivity and specificity across all possible cut-offs and identify candidate optimal thresholds. Materials: Pre-validated biomarker measurement data (e.g., PD-L1 IHC H-score, tumor mutational burden [TMB] score) with corresponding ground-truth clinical response data (e.g., RECIST v1.1) for a training cohort. Procedure:
- For each unique biomarker value in the dataset, treat it as a potential cut-off.
- Calculate the corresponding sensitivity (True Positive Rate) and 1-specificity (False Positive Rate) against the clinical response gold standard.
- Plot sensitivity (y-axis) against 1-specificity (x-axis) for all cut-offs to generate the ROC curve.
- Calculate the Youden Index (J = Sensitivity + Specificity - 1) for each cut-off.
- Identify the cut-off(s) with the maximum Youden Index as statistically optimal for balanced sensitivity/specificity.
- Alternatively, identify cut-offs that meet pre-specified clinical requirements (e.g., sensitivity ≥ 90%).
Protocol 3.2: Clinical Utility Focused Determination via Decision Curve Analysis (DCA) Objective: To evaluate the net benefit of using the biomarker across different probability thresholds, incorporating clinical consequences. Materials: Biomarker and response data, along with validated clinical outcome data (e.g., overall survival). Procedure:
- Define a range of threshold probabilities (Pt) representing the minimum probability of response at which a clinician would recommend immunotherapy.
- For each Pt, calculate the Net Benefit of using the biomarker model versus "treat all" and "treat none" strategies using the formula: Net Benefit = (TP / N) - (FP / N) * (Pt / (1 - Pt)) where N is the total number of patients.
- Plot Net Benefit (y-axis) against Threshold Probability (x-axis) for each strategy.
- The optimal clinical cut-off is the one derived from the model that provides the highest net benefit across a plausible range of Pt, informed by clinical judgment on risk/benefit trade-offs.
4. The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biomarker Threshold Studies
| Item | Function & Relevance |
|---|---|
| Validated Clinical-Grade IHC Assay Kits (e.g., PD-L1 22C3, SP142) | Standardized detection of protein biomarkers on tumor tissue. Essential for generating reproducible quantitative data (e.g., Tumor Proportion Score) for cut-off analysis. |
| Next-Generation Sequencing (NGS) Panels (≥ 1 Mb) | For quantifying tumor mutational burden (TMB) and genomic biomarkers. Panel size and bioinformatics pipelines must be consistent to define TMB cut-offs (e.g., 10 mut/Mb). |
| Multiplex Immunofluorescence (mIF) Platforms | Enable simultaneous quantification of multiple cell phenotypes (e.g., CD8+ T cells, PD-L1+ cells) in the tumor microenvironment. Used to define composite biomarker scores. |
| Digital Pathology & Image Analysis Software | Allows objective, quantitative analysis of IHC or mIF staining (H-score, cell density, spatial analysis), reducing subjectivity in continuous biomarker measurement. |
| Standardized Clinical Response Criteria (RECIST v1.1, iRECIST) | Provide the essential ground truth ("gold standard") for defining responder vs. non-responder status, against which biomarker predictions are evaluated. |
5. Visualizations
Title: Threshold Optimization Workflow
Title: ROC Curve & Threshold Trade-off
Title: Decision Curve Analysis Logic
Within biomarker identification for immunotherapy response prediction, tumor heterogeneity presents a significant challenge. Spatial heterogeneity refers to genomic and immunophenotypic differences across distinct geographical regions of a tumor, while temporal heterogeneity describes genomic evolution and microenvironmental changes over time, often under therapeutic pressure. This document provides application notes and protocols for characterizing this heterogeneity to inform robust biomarker strategies.
Quantitative Data on Tumor Heterogeneity
Table 1: Comparison of Genomic Discordance in Single vs. Multi-Region Sampling
| Metric | Single-Site Biopsy | Multi-Region Biopsy (≥3 regions) | Key Study |
|---|---|---|---|
| Detection of Clonal Mutations | 100% (by definition) | 100% | Gerlinger et al., NEJM 2012 |
| Detection of Subclonal Mutations | 22-35% | 63-69% | Gerlinger et al., NEJM 2012 |
| Predicted Therapeutic Target Capture | 30-50% | 75-90% | Morris et al., Nat Rev Clin Oncol 2016 |
| Discordance in TMB Classification | N/A | 20-40% of cases | Chan et al., Cancer Cell 2019 |
| PD-L1 Expression Discordance (IC Score) | N/A | 15-45% of cases (Δ≥10%) | McLaughlin et al., JAMA Oncol 2016 |
Table 2: Impact of Biopsy Strategy on Predictive Biomarker Assessment
| Biomarker | Risk of Misclassification (Single-Site) | Recommended Sampling Strategy | Evidence Level |
|---|---|---|---|
| Tumor Mutational Burden (TMB) | High (Spatial heterogeneity of neoantigens) | Multi-region (3-5 sites) or liquid biopsy complement | IB |
| PD-L1 IHC (IC/TC) | Moderate-High (Focal expression patterns) | Multi-region (2-3 sites) with consensus scoring | IB |
| Microsatellite Instability (MSI) | Low (Truncal mutation) | Single-site usually sufficient | IA |
| Oncogenic Drivers (e.g., EGFR) | Low (Truncal in most cancers) | Single-site usually sufficient | IA |
| Immune Phenotype (e.g., CD8+ T-cell density) | Very High (Immune deserts/excluded) | Multi-region mandatory for spatial mapping | IIB |
Experimental Protocols
Protocol 1: Multi-Region Tumor Sampling for Genomic and Transcriptomic Analysis
Objective: To comprehensively profile spatial intratumor heterogeneity (ITH) from a primary tumor resection specimen.
Materials:
- Fresh or OCT-embedded frozen tumor tissue from ≥5 geographically distinct regions.
- PAXgene Tissue Fixative and Stabilizer (for simultaneous morphology and nucleic acid preservation).
- Hematoxylin and Eosin (H&E) staining reagents.
- Laser Capture Microdissection (LCM) system (optional, for stromal/epithelial separation).
Procedure:
- Macrodissection & Annotation: Immediately after resection, photograph the intact specimen. Serially slice the tumor at 3-5 mm intervals. From each slice, sample ≥5 regions (core diameter ≥1 mm) from the tumor center, peripheral invasive front, and intermediate zones. Record spatial coordinates.
- Histopathological Validation: A mirror section from each region is fixed in formalin, paraffin-embedded (FFPE), and H&E stained. A certified pathologist confirms tumor cellularity (>20%) and annotates necrosis, stromal content, and immune infiltrates.
- Nucleic Acid Extraction: For each macro-dissected region, split tissue for DNA/RNA co-extraction (using AllPrep DNA/RNA Mini Kit) and for FFPE. Quantify DNA/RNA yield (Qubit). Assess integrity (RNA Integrity Number, RIN >7 for frozen; DV200 >30% for FFPE).
- Library Preparation & Sequencing:
- DNA: Prepare whole-exome sequencing (WES) libraries (≥150x mean coverage) using a kit like Kapa HyperPrep. Include a matched normal sample (blood or adjacent normal tissue).
- RNA: Prepare stranded RNA-seq libraries (≥50 million paired-end reads) using Illumina TruSeq Stranded mRNA kit.
- Bioinformatic Analysis: Align sequences (BWA for DNA, STAR for RNA). Call somatic variants (MuTect2). Infer clonal architecture (PyClone, SciClone). Calculate ITH metrics (mathletic diversity index). Perform consensus clustering on RNA-seq data for immune phenotype classification.
Protocol 2: Longitudinal Liquid Biopsy Complement to Tissue Biopsy
Objective: To monitor temporal heterogeneity and clonal dynamics during immunotherapy.
Materials:
- Patient plasma collection tubes (cfDNA BCT Streck tubes).
- Cell-free DNA (cfDNA) extraction kit (QIAamp Circulating Nucleic Acid Kit).
- Digital PCR or NGS-based assay for variant detection (e.g., Guardant360, FoundationOne Liquid).
Procedure:
- Baseline Sampling: Collect 2x10 mL blood in Streck tubes concurrently with tumor biopsy (single or multi-region). Process within 6 hours.
- Longitudinal Sampling: Schedule draws at pre-treatment (C1D1), early on-treatment (C2D1, C3D1), and at progression.
- cfDNA Isolation: Centrifuge blood at 1600xg for 20 min. Isolate cfDNA from 4-8 mL plasma per kit instructions. Elute in low-EDTA TE buffer.
- Analysis:
- Targeted NGS: Prepare libraries using a 70+ gene pan-cancer panel. Sequence to high depth (>10,000x). Call variants and calculate variant allele frequency (VAF).
- Data Integration: Compare baseline tissue-derived mutations with cfDNA mutations. Track VAF dynamics over time. Emergence of new clones at progression indicates temporal evolution.
- Correlation with Response: Associate clonal dynamics (clearing of founder clones, rise of resistant subclones) with radiographic response (RECIST v1.1) and survival (PFS, OS).
Diagrams
Diagram 1: Multi-Region Biopsy Workflow for Spatial Heterogeneity
Title: Multi-Region Biopsy to Profile Spatial Heterogeneity
Diagram 2: Integrated Strategy for Spatial & Temporal Heterogeneity
Title: Integrated Spatial & Temporal Biomarker Strategy
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Heterogeneity Studies
| Item | Function & Application | Example Product/Catalog # |
|---|---|---|
| PAXgene Tissue System | Simultaneous fixation and stabilization of RNA/DNA/proteins; preserves histomorphology for multi-omics from same block. | PreAnalytix PAXgene Tissue System |
| AllPrep DNA/RNA/miRNA Universal Kit | Co-isolation of genomic DNA, total RNA, and microRNA from a single tumor tissue sample. | Qiagen 80224 |
| Streck cfDNA BCT Blood Collection Tube | Stabilizes nucleated blood cells to prevent genomic DNA contamination of plasma cfDNA for liquid biopsies. | Streck 230386 |
| QIAamp Circulating Nucleic Acid Kit | Optimized spin-column purification of cell-free DNA from human plasma/serum. | Qiagen 55114 |
| Kapa HyperPrep Kit | Robust, high-yield library construction for low-input and degraded DNA (FFPE, cfDNA) for WES. | Roche 07962363001 |
| TruSeq Stranded mRNA Library Prep Kit | Generation of stranded RNA-seq libraries for gene expression and immune deconvolution. | Illumina 20020595 |
| Multiplex IHC/IF Antibody Panels | Simultaneous imaging of multiple immune markers (CD8, PD-1, PD-L1, FoxP3, CK) on a single slide to map microenvironment. | Akoya Biosciences OPAL 7-Color Kit |
| Human Pan-Cancer Cell-Free DNA Panel | Targeted NGS panel for detecting mutations, indels, CNVs, and fusions in cfDNA; used for longitudinal tracking. | Guardant360 Panel |
Within biomarker discovery for immunotherapy (e.g., anti-PD-1/PD-L1, anti-CTLA-4), a critical bottleneck is the integration of disparate, high-dimensional datasets. Effective harmonization of genomic, transcriptomic, proteomic, and digital pathology data from heterogeneous clinical cohorts is essential to build robust, generalizable predictive models. This protocol outlines a standardized framework for achieving semantic and technical interoperability to enable meta-analyses and cross-cohort validation.
The primary challenges in cohort harmonization are summarized in the table below.
Table 1: Key Data Heterogeneity Challenges in Immunotherapy Cohorts
| Challenge Category | Specific Issue | Typical Impact/Variance |
|---|---|---|
| Clinical Data | RECIST criteria vs. irRECIST vs. iRECIST | 15-20% discrepancy in response classification |
| Genomic Data | Different sequencing panels (e.g., MSK-IMPACT vs. FoundationOne) | Gene coverage varies from 300 to 500+ genes; TMB calculation methods differ |
| Transcriptomic Data | Platform differences (RNA-seq vs. microarray) and batch effects | Inter-platform correlation: r = 0.6-0.8 for comparable signatures |
| Tissue Imaging | H&E slide scanning magnification (20x vs. 40x) and stain variation | Algorithm performance can drop by 10-30% without normalization |
| Sample Metadata | Inconsistent annotation (e.g., "prior therapy" definitions) | Up to 30% of samples may be excluded due to ambiguous metadata |
Core Harmonization Protocol
This protocol is structured into three phases: Pre-integration Curation, Technical Normalization, and Semantic Mapping.
Phase 1: Pre-integration Curation & Cohort Definition Objective: To establish a unified cohort definition and quality control (QC) baseline.
- Define Core Clinical Variables: Establish a minimum data dictionary (e.g., using CDISC standards) for immunotherapy studies. Mandatory fields must include:
Treatment (Drug, Line),Response (using harmonized criteria),Overall Survival (OS),Progression-Free Survival (PFS),Primary Cancer Type,Baseline Demographics. - Sample QC: Apply uniform QC thresholds.
- For genomic data: Minimum read depth >100x, tumor purity >20%.
- For RNA-seq: Minimum of 20 million reads per sample, RIN >7.
- For digital pathology: Exclude slides with >50% tissue fold or tear.
- Cohort Querying: Use a standardized SQL-like syntax to create cohorts across databases. Example:
SELECT sample_id WHERE treatment = 'pembrolizumab' AND line_of_therapy = 1 AND has_rnaseq = TRUE AND has_wsi = TRUE.
Phase 2: Technical Normalization & Batch Correction Objective: To remove non-biological technical variation from molecular data.
- Genomic Variant Harmonization:
- Map all variants to GRCh38. Use a tool like
vcfannoto annotate against common databases (ClinVar, dbSNP, gnomAD). - For Tumor Mutational Burden (TMB): Standardize calculation to
total nonsynonymous mutations / size of targeted coding region (in Mb). Report separately for panel and whole-exome sequencing.
- Map all variants to GRCh38. Use a tool like
- Transcriptomic Data Harmonization:
- For RNA-seq to RNA-seq integration: Perform Counts Per Million (CPM) or Transcripts Per Million (TPM) normalization, followed by ComBat-Seq (for count data) or ComBat (for normalized log-expression) to adjust for batch and study effects.
- For Signature Scoring: Use a single-sample scoring method (e.g., singscore, GSVA) to calculate enrichment scores for immune gene signatures (e.g., IFN-gamma response, T-cell inflamed signature) across all cohorts uniformly.
- Digital Pathology Normalization:
- Apply stain normalization (e.g., Macenko method) to all H&E whole slide images (WSIs) using a reference slide from a central lab.
- Use a standardized tumor segmentation model (e.g., Hover-Net) to generate consistent cell phenotype maps ( tumor, lymphocyte, stroma).
Phase 3: Semantic Mapping & Linked Data Model Objective: To create a FAIR (Findable, Accessible, Interoperable, Reusable) data resource.
- Ontology Mapping: Map all free-text clinical and pathologic terms to controlled vocabularies.
- Use NCIt for cancer types, drug names, and procedures.
- Use Uberon for anatomical sites.
- Use LOINC for lab test identifiers.
- Create a Unified Data Model: Implement a graph-based or relational schema that links all data types via a unique
subject_idandsample_id. - Federated Query Interface: Deploy a platform (e.g., based on Gen3 or OHDSI/OMOP) that allows researchers to query aggregated, harmonized metadata across cohorts without transferring raw data, compliant with data use agreements.
Experimental Validation Protocol
Title: Cross-Cohort Validation of a Hypothetical Biomarker Signature Objective: To test the robustness of a T-cell inflammation signature derived from Cohort A in an independent, harmonized Cohort B.
- Input: Harmonized RNA-seq expression matrices from Cohort A (discovery, n=300) and Cohort B (validation, n=150), both treated with anti-PD-1.
- Signature Definition: In Cohort A, perform differential expression between responders (R) and non-responders (NR). Define a 50-gene T-cell inflammation signature.
- Scoring: Apply the single-sample GSEA (ssGSEA) algorithm identically to both Cohort A and the harmonized Cohort B data to generate a continuous signature score for each patient.
- Statistical Analysis:
- In Cohort A, determine the optimal score cutoff via maximally selected rank statistics.
- Apply this exact cutoff to Cohort B.
- Evaluate performance using:
- Logistic regression for response prediction (OR, p-value).
- Kaplan-Meier analysis and Cox proportional hazards model for PFS (HR, p-value).
- Output: A report comparing the signature's predictive performance (AUC, HR) across the two harmonized cohorts, demonstrating generalizability.
Pathway and Workflow Visualization
Diagram 1: Data Harmonization Workflow
Diagram 2: Immunotherapy Biomarker Integration Network
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Data Harmonization in Immunotherapy Research
| Tool/Resource Name | Type | Primary Function in Harmonization |
|---|---|---|
| Gen3 Data Platform | Software Framework | Provides a FAIR data commons architecture for managing, curating, and sharing heterogeneous cohort data with fine-grained access control. |
| BioContainers | Computational Tool | Offers Docker/Singularity containers for standardized, reproducible execution of bioinformatics tools (e.g., alignment, variant calling) across different compute environments. |
| Ensembl VEP | Bioinformatics Tool | Standardizes genomic variant annotation (consequences, frequencies) against a consistent reference, crucial for harmonizing mutations from different panels. |
| HarmonizR | R Package | Implements the ComBat algorithm and other methods for batch effect adjustment of gene expression and proteomic data across multiple studies. |
| Cytokit / HALO | Image Analysis Software | Enables standardized, high-throughput quantification of cell types and spatial relationships in multiplex immunofluorescence or H&E tissue images. |
| OHDSI OMOP CDM | Data Model | A standardized, common data model for observational health data, allowing systematic analysis of harmonized clinical variables across global cohorts. |
| ImmPort | Data Repository | A public repository of immunology-related datasets, often with already-curated metadata, serving as a reference for data structure and ontologies. |
Regulatory and Reimbursement Hurdles for Novel Biomarker Tests
Within the broader thesis on biomarker identification for immunotherapy response prediction, translating a candidate biomarker into a clinically validated and widely adopted diagnostic test presents formidable regulatory and reimbursement challenges. This document outlines these hurdles and provides detailed application notes and protocols for navigating the evidence generation required for regulatory clearance and payer coverage.
Current Regulatory Landscape: FDA and EMA Pathways
The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have distinct but converging frameworks for biomarker test approval. The choice of pathway depends on the test's risk classification and intended use.
Table 1: Key Regulatory Pathways for Biomarker Tests
| Agency | Pathway | Description | Typical Timeline | Key Evidence Required |
|---|---|---|---|---|
| FDA (U.S.) | De Novo Classification | For novel, low-to-moderate risk devices with no predicate. | 6-12 months (after submission) | Analytical & Clinical Validation, Clinical Utility data. |
| FDA (U.S.) | 510(k) Clearance | For tests substantially equivalent to a legally marketed predicate. | 3-7 months | Analytical & Clinical Validation demonstrating equivalence. |
| FDA (U.S.) | Pre-Market Approval (PMA) | For high-risk (Class III) tests. | 6-12 months (intensive review) | Rigorous Clinical Trial data proving safety and effectiveness. |
| EMA (EU) | IVDR (Class C/D) | In Vitro Diagnostic Regulation for high-performance tests. | ~12-18 months (Notified Body review) | Performance Evaluation Report (Analytical & Clinical), Post-Market surveillance plan. |
Core Reimbursement Hurdles: U.S. Payer Requirements
Securing payment from U.S. payers like Medicare (via CMS) and private insurers is critical for test adoption. Payers evaluate tests based on specific, stringent criteria.
Table 2: U.S. Payer Evidence Requirements for Coverage
| Payer | Evidence Domain | Specific Requirements | Common Gaps for Novel Biomarkers |
|---|---|---|---|
| CMS (Medicare) | Analytical Validity | Test accuracy, precision, reproducibility, and reliability. | Lack of standardization across labs. |
| CMS (Medicare) | Clinical Validity | Strong association between test result and clinical outcome (e.g., PFS, OS). | Retrospective data only; small cohort sizes. |
| CMS (Medicare) | Clinical Utility | Evidence that using the test improves patient management and net health outcomes. | Lack of prospective interventional trial data. |
| Private Payers | Economic Impact | Cost-effectiveness analysis demonstrating savings or value. | High test cost without clear offset in other care costs. |
Application Notes: Building a Evidence Generation Protocol
Application Note 001: Protocol for a Pivotal Clinical Utility Study
Objective: To generate Level 1 evidence for clinical utility, satisfying both regulatory (FDA PMA) and reimbursement (CMS) requirements for a novel predictive biomarker test in non-small cell lung cancer (NSCLC) immunotherapy.
Design: Prospective, randomized, controlled, multi-center trial. Primary Endpoint: Overall survival (OS) in biomarker-selected arm vs. standard of care. Secondary Endpoints: Progression-free survival (PFS), objective response rate (ORR), cost per quality-adjusted life year (QALY).
Protocol Workflow:
- Patient Screening: Enroll metastatic NSCLC patients eligible for first-line immunotherapy.
- Biomarker Testing: Perform the novel multi-analyte assay (e.g., RNA-seq signature) in a CLIA-certified, CAP-accredited central lab.
- Randomization: Stratify patients based on biomarker status (High vs. Low Score).
- Intervention Arm (Biomarker-High): Receive immunotherapy + standard chemotherapy.
- Control Arm (All Comers): Receive standard of care (immunotherapy +/- chemotherapy per physician choice).
- Blinded Outcome Assessment: Independent radiology review of RECIST v1.1 criteria.
- Health Economics Data Collection: Capture resource utilization, adverse events, and patient-reported outcomes (PROs) for cost-effectiveness modeling.
Diagram 1: Pivotal Clinical Utility Trial Workflow
Application Note 002: Protocol for Analytical Validation per CLSI Guidelines
Objective: To establish the analytical validity of a novel immunohistochemistry (IHC)-based companion diagnostic, a prerequisite for FDA submission.
Key Experiments & Metrics:
- Precision: Repeatability (within-run) and Reproducibility (between-day, between-operator, between-site).
- Accuracy: Comparison to a validated orthogonal method (e.g., RNA in situ hybridization).
- Analytical Specificity: Assessment of cross-reactivity with similar antigens.
- Robustness: Testing under deliberate, small variations in pre-analytical conditions (fixation time, antigen retrieval).
Protocol: Inter-Site Reproducibility (CLSI EP15-A3)
- Sample Set: Select 20 patient tissue sections with a range of biomarker expression (negative, low, medium, high).
- Site Selection: Three independent testing laboratories.
- Blinded Testing: Each site performs the IHC assay according to the locked-down protocol on three separate days.
- Scoring: All slides are scored by three certified pathologists using the pre-defined scoring algorithm.
- Statistical Analysis: Calculate intra-class correlation coefficient (ICC) and concordance rates. Target ICC > 0.90 for continuous scores; > 95% concordance for positive/negative calls.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Biomarker Assay Development
| Reagent/Material | Function/Application | Key Considerations for Regulatory Submission |
|---|---|---|
| Recombinant Antibodies (RUO vs. IVD) | Detection of protein biomarkers via IHC, IF, or immunoassay. | For CDx development, antibodies must be sourced as IVD-grade or extensively re-validated for analytical performance. |
| PCR Assay Kits (qPCR/ddPCR) | Quantification of DNA or RNA biomarkers (e.g., tumor mutational burden). | Requires strict validation of limit of detection (LoD), precision, and inhibition resistance. |
| Next-Generation Sequencing (NGS) Panels | Multi-analyte profiling of mutations, expression, and signatures. | Bioinformatics pipeline lock-down and validation is as critical as wet-lab reagents. |
| Cell Line-Derived Reference Standards | Positive controls for assay development and calibration. | Must be well-characterized, stable, and traceable. Genomic DNA or formalin-fixed cell pellets are common. |
| Formalin-Fixed, Paraffin-Embedded (FFPE) Tissue Reference Sets | For validating assays on clinically relevant sample matrices. | Should represent a range of biomarker expression, tumor types, and tissue qualities. Procurement requires appropriate IRB consent. |
Navigating the Evidence-to-Payment Pathway
The journey from biomarker discovery to reimbursed test requires parallel planning for regulatory and payer needs.
Diagram 2: Evidence Generation to Reimbursement Pathway
Validating and Benchmarking Biomarkers: From Bench to Bedside
Application Notes
Within a thesis on biomarker identification for predicting immunotherapy response, a rigorous, phased validation strategy is paramount. Immunotherapy biomarkers, such as PD-L1 expression, tumor mutational burden (TMB), or novel gene expression signatures, must transition from research observations to tools that reliably inform clinical decisions. This document outlines the three core validation phases with specific application notes for the immunotherapy context.
Phase 1: Analytical Validation This phase establishes that the test itself reliably measures the biomarker. For immunotherapy, this is complex due to biomarker heterogeneity. Key considerations include:
- Assay Platform: Distinctions between immunohistochemistry (IHC), next-generation sequencing (NGS), or RNA-seq must be defined.
- Pre-Analytical Variables: Tissue fixation time, biopsy site, and sample age critically impact results for biomarkers like PD-L1.
- Precision and Accuracy: Demonstrating repeatability across operators, instruments, and laboratories is essential for trial reproducibility.
Phase 2: Clinical Validation This phase evaluates the statistical strength of the association between the biomarker and the clinical endpoint. For immunotherapy response prediction:
- Clinical Sensitivity/Specificity: The biomarker's ability to correctly identify responders (sensitivity) and non-responders (specificity) must be quantified.
- Association with Endpoints: Correlation with objective response rate (ORR), progression-free survival (PFS), and overall survival (OS) in well-defined cohorts is required.
- Confounding Factors: Analyses must account for variables like performance status, prior therapies, and tumor type.
Phase 3: Clinical Utility Validation The highest bar, demonstrating that using the biomarker to guide treatment improves patient outcomes compared to standard care.
- Clinical Trial Design: Requires prospective, often randomized, trials where treatment assignment is based on biomarker status.
- Net Benefit Assessment: Measures if biomarker-guided therapy leads to superior efficacy (e.g., longer OS) or reduced toxicity (avoiding ineffective therapy) without undue harm.
- Health Economic Impact: Assessment of cost-effectiveness of biomarker testing in the clinical pathway.
Protocols
Protocol 1: Analytical Validation of an Immunohistochemistry (IHC) Assay for PD-L1 Expression
Objective: To establish the analytical precision and reproducibility of a PD-L1 IHC assay in non-small cell lung cancer (NSCLC) tissue sections.
Materials:
- Formalin-fixed, paraffin-embedded (FFPE) NSCLC tissue microarrays (TMAs) with known PD-L1 expression levels (0%, 1-49%, ≥50% Tumor Proportion Score).
- Validated anti-PD-L1 primary antibody and compatible detection kit.
- Automated IHC stainer.
- Light microscope with digital slide scanner.
Procedure:
- Assay Run: Perform the IHC staining procedure across three separate runs (days), using the same protocol, by two trained technologists.
- Slide Scoring: Three pathologists, blinded to each other's scores and run details, independently assess the TPS for each core.
- Data Analysis:
- Calculate intra-observer concordance (same pathologist, different days).
- Calculate inter-observer concordance between pathologists using intraclass correlation coefficient (ICC).
- Calculate inter-run reproducibility by comparing scores from the same tissue across different runs.
Key Metrics Table: Analytical Performance of PD-L1 IHC Assay
| Metric | Target Acceptance Criterion | Example Result (Hypothetical Data) |
|---|---|---|
| Intra-observer Concordance (ICC) | >0.90 | 0.95 |
| Inter-observer Concordance (ICC) | >0.80 | 0.87 |
| Inter-run Reproducibility (% Agreement ±5% TPS) | >95% | 98% |
| Limit of Detection (LoD) | Consistent staining at 1% TPS | Achieved |
Protocol 2: Clinical Validation of a TMB Assay via NGS
Objective: To validate the association between tumor mutational burden (TMB) as measured by a targeted NGS panel and objective response to anti-PD-1 therapy in melanoma.
Materials:
- FFPE tumor samples and matched normal blood from a retrospective cohort of melanoma patients treated with anti-PD-1.
- DNA extraction kits.
- Targeted NGS panel (e.g., ~1.1 Mb).
- NGS sequencing platform.
- Clinical data: ORR, PFS.
Procedure:
- Sequencing & Bioinformatic Analysis: Extract DNA, perform NGS. Call somatic variants. Calculate TMB as mutations per megabase (mut/Mb).
- Threshold Determination: Using a training cohort, determine the optimal TMB cut-off (e.g., using ROC analysis against ORR).
- Statistical Analysis: In a validation cohort, apply the cut-off. Compare ORR and PFS between TMB-high and TMB-low groups using Fisher's exact test and Kaplan-Meier analysis with log-rank test.
Key Metrics Table: Clinical Performance of TMB Assay
| Metric | TMB-High Cohort (≥10 mut/Mb) | TMB-Low Cohort (<10 mut/Mb) | P-value |
|---|---|---|---|
| Number of Patients (n) | 45 | 55 | - |
| Objective Response Rate (ORR) | 60% | 18% | <0.001 |
| Median PFS | 15.2 months | 4.1 months | <0.001 |
| Hazard Ratio (HR) for PFS | 0.38 (95% CI: 0.24-0.60) | - | <0.001 |
Protocol 3: Prospective Clinical Utility Trial Design
Objective: To assess the clinical utility of a novel biomarker signature for guiding first-line therapy in advanced NSCLC.
Design: Prospective, randomized, controlled trial.
Procedure:
- Patient Screening: All newly diagnosed advanced NSCLC patients undergo tumor biopsy for biomarker testing (Signature X).
- Randomization: Patients are randomized 1:1.
- Arm A (Biomarker-Guided): Signature X-positive patients receive immunotherapy combo; Signature X-negative patients receive chemotherapy.
- Arm B (Standard of Care): All patients receive standard chemo-immunotherapy combo, blinded to biomarker status.
- Endpoint Analysis: The primary endpoint is overall survival (OS) in the biomarker-positive subgroup between Arm A and Arm B. A significant improvement in OS in Arm A demonstrates clinical utility.
Visualizations
Diagram Title: Three Phases of Biomarker Validation
Diagram Title: NGS Workflow for Immunotherapy Biomarkers
Diagram Title: PD-1/PD-L1 Pathway & Therapeutic Blockade
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Immunotherapy Biomarker Research |
|---|---|
| Validated FFPE-Reactive Antibodies (e.g., anti-PD-L1, CD8) | For precise spatial detection of protein biomarkers via IHC, critical for analytical validation. |
| Targeted NGS Panels (e.g., TMB, Immune Repertoire) | For simultaneous, quantitative assessment of genomic biomarkers (TMB, mutations) from limited FFPE DNA. |
| RNA Stabilization & Extraction Kits (for FFPE) | To obtain high-quality RNA from archival tissues for gene expression signature development (e.g., interferon-gamma signatures). |
| Multiplex Immunofluorescence (mIF) Kits | To characterize the tumor immune microenvironment (CD8, PD-L1, FoxP3, etc.) in situ on a single slide, enabling complex biomarker discovery. |
| Digital PCR Assays | For ultra-sensitive and absolute quantification of low-frequency biomarkers (e.g., circulating tumor DNA for minimal residual disease). |
| Immune Cell Deconvolution Bioinformatics Tools | To estimate immune cell type abundances from bulk RNA-seq data, a key computational method for biomarker signature development. |
Application Notes
The development of immune checkpoint inhibitors (ICIs) has revolutionized oncology, yet robust predictive biomarkers remain a critical unmet need. This document, framed within a thesis on biomarker identification for immunotherapy response prediction, evaluates the analytical and clinical performance of single biomarkers against composite biomarker signatures.
Single biomarkers, such as PD-L1 immunohistochemistry (IHC) or Tumor Mutational Burden (TMB), offer simplicity but are limited by biological complexity, spatial heterogeneity, and dynamic regulation. Composite biomarkers, which integrate multiple data types (e.g., genomic, transcriptomic, proteomic), aim to capture the multifaceted nature of the tumor-immune interaction, potentially offering superior predictive power for durable clinical benefit (DCB).
Key comparative metrics include sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and the area under the receiver operating characteristic curve (AUC-ROC). Early evidence suggests composite biomarkers consistently outperform single agents in AUC-ROC across multiple cancer types, though often at the cost of increased assay complexity and reduced accessibility.
Table 1: Head-to-Head Performance of Single vs. Composite Biomarkers in Predicting ICI Response (Non-Small Cell Lung Cancer Example)
| Biomarker | Assay Type | AUC-ROC (95% CI) | Sensitivity (%) | Specificity (%) | Clinical Utility & Limitations |
|---|---|---|---|---|---|
| PD-L1 IHC (TPS ≥50%) | Single (Protein) | 0.62 (0.58-0.66) | 45 | 79 | Standardized, approved companion diagnostic. Limited by heterogeneity and temporal dynamics. |
| TMB (≥10 mut/Mb) | Single (Genomic) | 0.68 (0.64-0.72) | 52 | 81 | Captures tumor neoantigen burden. Cutoff variability, platform dependency, cost. |
| Composite Gene Expression Profile (GEP) | Composite (RNA) | 0.75 (0.71-0.79) | 70 | 75 | Quantifies inflamed tumor microenvironment. Requires high-quality RNA, lacks universal signature. |
| Integrated Score (TMB + GEP + CD8 IHC) | Composite (Multi-omics) | 0.82 (0.78-0.85) | 78 | 80 | Highest predictive power. Complex, not standardized, high cost, computational burden. |
Experimental Protocols
Protocol 1: Evaluating a Single Biomarker (PD-L1 by IHC)
Objective: To quantify PD-L1 protein expression in formalin-fixed, paraffin-embedded (FFPE) tumor tissue using IHC. Materials: See "The Scientist's Toolkit" below. Procedure:
- Sectioning: Cut 4-5 µm sections from FFPE tissue blocks and mount on charged slides.
- Deparaffinization & Rehydration: Bake slides at 60°C for 1 hour. Deparaffinize in xylene (3 x 5 min) and rehydrate through graded ethanol (100%, 95%, 70%) to distilled water.
- Antigen Retrieval: Perform heat-induced epitope retrieval (HIER) in EDTA buffer (pH 9.0) using a pressure cooker or decloaking chamber for 15-20 min. Cool slides for 30 min.
- Peroxidase Blocking: Incubate with 3% hydrogen peroxide solution for 10 min to block endogenous peroxidase activity. Rinse with wash buffer (TBST).
- Protein Block & Primary Antibody: Apply protein block for 10 min. Incubate with validated anti-PD-L1 primary antibody (e.g., clone 22C3, 28-8, or SP142) for 60 min at room temperature.
- Detection: Apply labeled polymer-HRP secondary antibody for 30 min. Visualize using DAB chromogen for 5-10 min. Counterstain with hematoxylin, dehydrate, and mount.
- Scoring: Evaluate by a certified pathologist using the approved scoring algorithm (e.g., Tumor Proportion Score (TPS) for NSCLC).
Protocol 2: Developing a Composite Biomarker Signature
Objective: To develop a composite RNA-based gene expression profile predictive of ICI response. Materials: See "The Scientist's Toolkit" below. Procedure:
- Cohort Selection & RNA Extraction: Select a retrospective cohort of ICI-treated patients with documented response (Responders vs. Non-Responders). Isolve total RNA from FFPE tumor sections using a silica-membrane column kit with DNase I treatment. Assess RNA quality (DV200 > 30%).
- Library Preparation & Sequencing: Convert 10-100 ng of RNA to cDNA. Prepare sequencing libraries using a pan-cancer immune profiling panel (e.g., targeting 395+ immune-related genes). Perform hybridization capture and sequence on a high-throughput platform (150 bp paired-end).
- Bioinformatic Analysis: a. Alignment & Quantification: Align reads to the human reference genome (GRCh38) using a splice-aware aligner (e.g., STAR). Quantify gene-level counts. b. Differential Expression: Perform normalized counts (e.g., using DESeq2 or edgeR) to identify genes differentially expressed between Responders and Non-Responders (FDR < 0.05, |log2FC| > 1). c. Signature Building: Apply machine learning (e.g., LASSO regression) on the training set to select a minimal gene set predictive of response. Weigh genes to create a single continuous score.
- Validation: Lock the algorithm. Validate the composite score's performance (AUC-ROC, PPV, NPV) in an independent, held-out validation cohort using pre-specified cutpoints.
Visualizations
Title: Single vs. Composite Biomarker Development Workflow
Title: Key Signaling Pathways Informing Biomarker Selection
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for Biomarker Studies
| Item | Function & Application | Example/Notes |
|---|---|---|
| FFPE Tissue Sections | Archival patient samples for IHC and nucleic acid extraction. | Ensure appropriate ethical approvals and linked clinical outcome data. |
| Validated PD-L1 IHC Antibody Clones | Specific detection of PD-L1 protein for single biomarker analysis. | Clones 22C3 (Dako), 28-8 (Dako), SP142 (Ventana). Use with matched platform. |
| Automated IHC Stainer | Standardized, high-throughput staining for reproducibility. | Dako Autostainer, Ventana BenchMark series. |
| RNA/DNA Co-extraction Kit | Simultaneous isolation of high-quality nucleic acids from FFPE. | Qiagen AllPrep DNA/RNA FFPE Kit. Critical for multi-omics workflows. |
| Targeted RNA-seq Panel | Focused profiling of immune-related gene expression. | NanoString PanCancer IO 360 Panel, HTG EdgeSeq Oncology Panel. |
| Whole Exome Sequencing Kit | Comprehensive genomic analysis for TMB calculation. | Illumina TruSeq DNA Exome, Agilent SureSelect Human All Exon. |
| Multiplex IHC/IF Detection Kit | Spatial profiling of multiple protein markers in one tissue section. | Akoya Biosciences Opal Polychromatic IF, Cell DIVE. |
| Bioinformatics Pipeline Software | For alignment, quantification, and analysis of NGS data. | CLC Genomics Server, Partek Flow, custom R/Python scripts. |
| Reference Control Materials | Assay calibration and inter-laboratory standardization. | Cell line-derived FFPE pellets with known biomarker status. |
Within biomarker identification for immunotherapy response prediction, a central debate hinges on the utility of pan-cancer versus tissue-specific biomarkers. Pan-cancer biomarkers, often derived from fundamental immunological or genetic processes, promise broad applicability across cancer types. In contrast, tissue-specific biomarkers arise from the unique biology of the tumor microenvironment (TME) and cellular origin of a given cancer. This application note details their distinct contexts of use, supporting clinical evidence, and experimental protocols for their evaluation.
Context of Use: Comparative Analysis
| Aspect | Pan-Cancer Biomarkers | Tissue-Specific Biomarkers |
|---|---|---|
| Definition | Molecular features predictive of immunotherapy response across multiple, histologically distinct cancer types. | Molecular features predictive of response within a specific cancer type or tissue of origin. |
| Biological Basis | Fundamental immune processes: e.g., T-cell infiltration, interferon-gamma signaling, DNA damage repair. | Tissue-specific TME, unique oncogenic drivers, and organ-specific antigen presentation. |
| Primary Context of Use | Initial patient stratification for agnostic clinical trials; companion diagnostics for tumor-agnostic therapies. | Refinement of patient stratification within a specific cancer type; companion diagnostics for tissue-indicated therapies. |
| Key Examples | Tumor Mutational Burden (TMB), Microsatellite Instability-High (MSI-H), PD-L1 expression (in some contexts). | Intratumoral CD8+ T-cell density (melanoma), EGFR mutations (NSCLC), BRCA mutations (ovarian/breast). |
| Regulatory Path | Often pursued under the FDA's "site-agnostic" or "basket trial" frameworks. | Traditional, tissue-specific drug approval pathways. |
| Limitations | May overlook nuanced, tissue-specific biology leading to variable predictive value. | Limited generalizability; may not inform on rare cancers. |
| Biomarker | Type | Key Trial(s) & Year | Cancer Types | Outcome (e.g., ORR) | FDA Status |
|---|---|---|---|---|---|
| MSI-H/dMMR | Pan-Cancer | KEYNOTE-158 (2020), et al. | >15 types (e.g., colorectal, endometrial) | ~34-40% ORR with pembrolizumab | Approved (2017) |
| High TMB (≥10 mut/Mb) | Pan-Cancer | KEYNOTE-158 (2020) | Multiple solid tumors | 29% ORR vs. 6% in low-TMB | Approved (2020) |
| PD-L1 Expression (CPS≥10) | Tissue-Specific/Pan | KEYNOTE-059 (Gastric, 2017), KEYNOTE-048 (HNSCC, 2019) | Gastric, HNSCC, others | Varies by cancer (e.g., 22% in gastric) | Approved for specific indications |
| Tumor-Infiltrating Lymphocytes (TILs) | Tissue-Specific | Pooled Melanoma Trials (2019) | Melanoma | High TILs correlate with improved PFS/OS | Clinical use, not standard diagnostic |
| EGFR mutations | Tissue-Specific | FLAURA (2018) - for targeted therapy; influences immunotherapy resistance | NSCLC | Negative predictor for ICI response | Standard of care for TKI use |
Detailed Experimental Protocols
Protocol 1: Pan-Cancer Biomarker Assessment via Tumor Mutational Burden (TMB) Calculation
Objective: To determine the total number of somatic mutations per megabase (mut/Mb) from whole-exome sequencing (WES) or targeted NGS panel data. Workflow:
- Sample Preparation: Extract DNA from matched tumor and normal (e.g., blood) formalin-fixed, paraffin-embedded (FFPE) tissue. Quality control (QC): DNA integrity number (DIN) >4.0.
- Sequencing: Perform WES (preferred) or large targeted NGS panel (>1 Mb) on tumor and normal samples. Recommended coverage: >100x for tumor, >60x for normal.
- Bioinformatic Pipeline: a. Alignment: Map reads to a reference genome (e.g., GRCh38) using BWA-MEM. b. Variant Calling: Call somatic variants (SNVs, indels) using paired tumor-normal callers (e.g., Mutect2, VarScan2). c. Filtering: Remove known germline polymorphisms (dbSNP, gnomAD), synonymous mutations, and variants in hypermutated or HLA regions. d. TMB Calculation: (Total number of filtered somatic mutations / Size of targeted genomic region in Mb). For WES, typically use ~35-50 Mb coding region.
- Validation: Compare against a validated reference standard (e.g., cell lines with known TMB). Report in mut/Mb. Clinical threshold often set at ≥10 mut/Mb.
Protocol 2: Tissue-Specific Biomarker Assessment via Multiplex Immunofluorescence (mIF)
Objective: To spatially quantify specific immune cell populations (e.g., CD8+ PD-1+ cells) within the tumor microenvironment of a specific cancer type. Workflow:
- Slide Preparation: Cut 4-5 μm sections from FFPE tumor blocks. Bake, deparaffinize, and rehydrate.
- Antigen Retrieval: Use a high-pH retrieval buffer (e.g., Tris-EDTA) in a pressure cooker for 15 minutes.
- Multiplex Staining Cycle (Iterative): a. Blocking: Incubate with protein block (e.g., 10% normal goat serum) for 30 minutes. b. Primary Antibody Incubation: Apply antibody (e.g., anti-CD8, clone C8/144B) for 1 hour at room temperature. c. Tyramide Signal Amplification (TSA): Apply appropriate HRP-conjugated secondary antibody, then fluorescently labeled TSA reagent (e.g., Opal 520) for 10 minutes. d. Antigen Stripping: Heat slides in retrieval buffer to remove antibodies, leaving fluorescent epitope tags intact. e. Repeat steps a-d for each marker (e.g., PD-1, CD68, Pan-CK, DAPI).
- Image Acquisition & Analysis: Scan slides using a multispectral microscope (e.g., Vectra/Polaris). Use image analysis software (inForm, QuPath) to perform: a. Tissue segmentation (tumor vs. stroma). b. Cell segmentation and phenotyping based on marker co-expression. c. Calculate densities (cells/mm²) and spatial metrics (e.g., distance of CD8+ cells to tumor cells).
Pathway and Workflow Visualizations
Title: Pan vs. Tissue Biomarker Pathways
Title: TMB Calculation Workflow
Title: mIF Staining & Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Reagent/Material | Function/Description | Example Supplier/Catalog |
|---|---|---|
| High-Quality FFPE DNA Kit | Extracts PCR-amplifiable DNA from challenging FFPE samples for NGS. | Qiagen GeneRead DNA FFPE Kit |
| Comprehensive NGS Panel | Targeted sequencing panel covering >1 Mb for reliable TMB calculation. | Illumina TruSight Oncology 500 |
| Validated mIF Antibody Panel | Antibodies optimized for sequential TSA-based multiplex IHC. | Akoya Biosciences Opal Polychromatic Kits |
| Multispectral Imaging System | Microscope capable of spectral unmixing for high-plex fluorescence imaging. | Akoya Vectra/Polaris, Zeiss Axioscan |
| Spatial Biology Analysis Software | Software for cell segmentation, phenotyping, and spatial analysis. | Akoya inForm, QuPath, Visiopharm |
| Reference Standard (Cell Lines) | Genomic DNA from cell lines with certified TMB values for assay validation. | Horizon Discovery HDx Reference Standards |
| Tumor Microenvironment Atlas | Annotated, multi-omics reference data for specific cancer types. | The Cancer Genome Atlas (TCGA), CancerSEA |
Real-World Evidence (RWE) and Post-Market Surveillance for Biomarker Performance
The identification of predictive biomarkers (e.g., PD-L1, TMB, MSI) is central to personalizing immunotherapy. While clinical trials establish initial efficacy, the real-world performance of these biomarkers across diverse populations, clinical settings, and long-term use requires rigorous post-market surveillance. Real-World Evidence (RWE) derived from electronic health records (EHRs), registries, and genomic databases is critical for validating, refining, or identifying new biomarkers for immunotherapy response and safety.
Application Notes
Note 1: RWE for Biomarker Performance Validation
- Purpose: To assess the real-world predictive power of a biomarker (e.g., PD-L1 TPS ≥50%) for anti-PD-1 therapy outcomes in non-small cell lung cancer (NSCLC) outside of trial constraints.
- Data Sources: Linkage of oncology EHR data with a structured biomarker registry.
- Key Metrics: Real-world overall response rate (rwORR), real-world progression-free survival (rwPFS), and overall survival (OS) stratified by biomarker status.
- Considerations: Confounding by indication, variability in assay/platform, and data completeness are major challenges requiring robust statistical adjustment.
Note 2: Surveillance for Emergent Resistance Biomarkers
- Purpose: To identify genomic or clinical features associated with acquired resistance to immunotherapy using longitudinal RWD.
- Data Sources: Repeat liquid or tissue biopsy genomic data paired with clinical progression timelines in a real-world cohort.
- Outcome: Generation of hypotheses on resistance mechanisms (e.g., emergence of new mutations, changes in T-cell clonality) for further prospective study.
Note 3: Post-Market Safety Signal Detection for Biomarker-Defined Subgroups
- Purpose: To monitor incidence rates of immune-related adverse events (irAEs) in patients selected by a specific biomarker profile.
- Data Sources: Pharmacovigilance databases (e.g., FDA Adverse Event Reporting System - FAERS) augmented with biomarker information from linked claims or EHRs.
- Action: Disproportionality analysis (e.g., reporting odds ratio) to detect safety signals potentially unique to a biomarker-positive population.
Table 1: Comparative Performance of PD-L1 as a Predictive Biomarker in NSCLC: Clinical Trial vs. Real-World Evidence
| Metric | Clinical Trial (KEYNOTE-024) | Real-World Evidence (Example Meta-Analysis) | Notes |
|---|---|---|---|
| Population | PD-L1 TPS ≥50%, no EGFR/ALK, PS 0-1 | PD-L1 TPS ≥50%, mixed comorbidities, incl. PS >1 | RWE includes broader, less-selected patients. |
| Treatment | Pembrolizumab vs. Platinum Chemo | Pembrolizumab monotherapy (1L) | RWE is observational, no randomized control. |
| Sample Size | ~ 305 patients | ~ 2,150 patients (pooled) | RWE can achieve larger sample sizes. |
| Median PFS | 10.3 vs. 6.0 months | 7.2 - 8.5 months | Real-world PFS often shorter due to assessment frequency. |
| Median OS | 30.0 vs. 14.2 months | 18.5 - 22.0 months | OS benefit remains clear but attenuated in RWE. |
| irAE Rate | 29.4% (Grade 3-5) | 22-27% (Grade 3-5) | Rates can vary based on real-world management. |
Table 2: Common RWE Data Sources for Immunotherapy Biomarker Surveillance
| Data Source Type | Examples | Key Biomarker Data Strengths | Primary Limitations |
|---|---|---|---|
| Integrated Health Systems | Flatiron Health, OPTUM | Curated EHR with treatment/outcome linkage; some genomic data. | Potential selection bias; incomplete biomarker testing. |
| Cancer Registries | SEER, NCDB | Population-level outcomes, expanding biomarker fields. | Limited treatment detail and longitudinal follow-up. |
| Genomic Databases | Guardant INFORM, Foundation INSIGHT | Large-scale genomic profiling data. | Clinical outcome data may be less granular. |
| Pharmacovigilance DB | FAERS, EudraVigilance | Global safety signal capture. | Underreporting, lack of denominator, sparse biomarker data. |
Experimental Protocols
Protocol 1: Retrospective Cohort Study for Real-World Biomarker Validation
Title: Assessing Real-World Effectiveness of TMB-H in Predicting ICI Response. Objective: To evaluate the association between tissue Tumor Mutational Burden (tTMB) ≥10 mut/Mb and real-world outcomes in patients receiving immune checkpoint inhibitors (ICIs).
Methodology:
- Cohort Definition: Identify patients in the linked EHR-genomic database diagnosed with advanced solid tumors who received ICI as any line of therapy and had tTMB testing via a targeted NGS panel (e.g., MSK-IMPACT, FoundationOne CDx).
- Exposure Definition: Define exposure as tTMB-H (≥10 mut/Mb) vs. tTMB-L (<10 mut/Mb).
- Outcome Assessment:
- rwPFS: Define progression as the earliest of: (a) radiologist's statement of progression in imaging report, (b) new systemic therapy initiation, or (c) death. Calculate from ICI start date.
- OS: Calculate from ICI start date to death from any cause.
- Covariate Adjustment: Extract data on age, sex, performance status, tumor type, line of therapy, and comorbid conditions. Use propensity score matching or multivariable Cox regression to adjust for confounding.
- Statistical Analysis: Generate Kaplan-Meier curves for rwPFS and OS. Compare groups using stratified log-rank test. Calculate adjusted hazard ratios (HR) with 95% confidence intervals.
Protocol 2: Signal Refinement for Biomarker-Associated Adverse Event
Title: Disproportionality Analysis for Myocarditis in PD-1 Inhibitor Patients with Concurrent Autoimmune Biomarkers. Objective: To investigate if presence of pre-existing autoimmune serology (e.g., ANA, anti-TPO) is associated with increased reporting of myocarditis in patients on PD-1 inhibitors.
Methodology:
- Data Source: Hospital-based pharmacovigilance database with linked rheumatology lab data.
- Case Identification: Identify all reports of myocarditis (MedDRA Preferred Term) in patients prescribed nivolumab or pembrolizumab.
- Biomarker Status: Ascertain autoantibody test results within 6 months prior to ICI initiation. Define biomarker-positive (any positive titer) vs. negative.
- Control Reports: For the same drug cohort, identify reports of other, unrelated irAEs (e.g., colitis, rash) as controls.
- Analysis: Construct a 2x2 contingency table. Calculate the Reporting Odds Ratio (ROR) and its 95% CI. A signal is considered if the lower bound of the 95% CI > 1.0 and a minimum case threshold is met.
Visualization: Diagrams via Graphviz
Diagram 1: RWE Generation Workflow for Biomarker Surveillance
Diagram 2: Biomarker Performance Validation Logic
The Scientist's Toolkit: Research Reagent & Data Solutions
Table 3: Essential Resources for RWE Biomarker Studies
| Item / Solution | Function / Purpose | Example (for illustration) |
|---|---|---|
| Linked EHR-Genomic Database | Provides the core RWD, linking clinical phenotypes (treatment, outcomes) with biomarker genotypes. | Flatiron Health-Foundation Medicine Clinico-Genomic Database. |
| Biomarker-Specific Data Model | Standardized ontology (e.g., OMOP CDM) to structure variables like assay type, result, unit, and specimen date. | OHDSI OMOP Common Data Model with oncology extensions. |
| NGS-Based Assay | To uniformly assess genomic biomarkers (TMB, MSI, specific mutations) from archival tissue or liquid biopsy. | FoundationOne CDx (tissue), Guardant360 CDx (liquid). |
| Immunohistochemistry Assay | To assess protein expression biomarkers (e.g., PD-L1) with validated scoring protocols. | PD-L1 IHC 22C3 pharmDx (Agilent) with TPS scoring. |
| Data Linkage Software | Secure, HIPAA-compliant software to deterministically or probabilistically link patient records across data sources. | Datavant software tools. |
| Statistical Analysis Package | For advanced survival analysis, propensity score modeling, and disproportionality analysis. | R (survival, MatchIt, PhViD packages) or SAS. |
| Biomarker Registry Platform | A prospective, systematic database to capture biomarker test results and indications in real-time. | Institutional REDCap-based biomarker registry. |
Application Notes
Current State of Predictive Biomarkers in Immunotherapy
The integration of biomarkers into standard clinical practice for immunotherapy, particularly immune checkpoint inhibitors (ICIs), has evolved rapidly. The primary goal is to stratify patients into likely responders and non-responders to maximize therapeutic benefit and minimize toxicity and cost. Several biomarkers have transitioned from research to clinical use, while others remain investigational.
Table 1: Clinically Validated and Emerging Immunotherapy Biomarkers
| Biomarker | Assay/Platform | Clinical Context | Predictive Performance (Approx. Metrics) | Current Guideline Status |
|---|---|---|---|---|
| PD-L1 IHC | 22C3 pharmDx (Agilent), SP142/263 (Ventana) | NSCLC, HNSCC, UC | CPS ≥10 in HNSCC: ORR ~25-30% vs <10%: ~15%. TPS ≥50% in NSCLC: improved OS. | NCCN/ASCO guideline-recommended for multiple cancers. |
| Tumor Mutational Burden (TMB) | WES; FoundationOne CDx, MSK-IMPACT (NGS panels) | Pan-cancer, especially NSCLC, melanoma | High TMB (≥10 mut/Mb): Improved PFS/OS in subsets. FDA-approved for pembrolizumab use in TMB-H solid tumors. | FDA-approved companion diagnostic; inclusion in some NCCN guidelines. |
| Microsatellite Instability (MSI) | PCR (BAT-25/26); IHC (MMR proteins); NGS | Colorectal, endometrial, pan-cancer | MSI-H: High response rates (~40-50%) to ICIs across tumor types. | FDA-approved as agnostic biomarker for pembrolizumab; standard-of-care. |
| Gene Expression Profiling (GEP) | Nanostring PanCancer IO360, RNA-seq | Melanoma, RCC, NSCLC | Inflamed GEP signature correlates with response (AUC ~0.65-0.75 in trials). | Investigational; used in clinical trials for patient stratification. |
| Tumor-Infiltrating Lymphocytes (TILs) | Multiplex IHC/IF (CD8, CD3, FOXP3); H&E scoring | Melanoma, breast cancer | High CD8+ density: associated with improved response and survival. | Not yet standard-of-care; active research area. |
Key Challenges in Guideline Integration
- Technical Validation: Standardization of pre-analytical variables (tissue fixation, timing), assay protocols, and scoring systems across labs is critical.
- Clinical Utility: Prospective validation in randomized controlled trials is required to prove that biomarker-directed therapy improves patient outcomes over standard care.
- Dynamic Nature of Biomarkers: Biomarker status (e.g., PD-L1) can change with disease progression or prior therapy, necessitating re-biopsy strategies.
- Multiplexing and Complexity: The future lies in composite biomarkers integrating genomic, transcriptomic, and proteomic data, requiring sophisticated bioinformatics and clear clinical cut-offs.
Experimental Protocols
Protocol 1: Quantitative PD-L1 Immunohistochemistry (IHC) and Scoring (22C3 pharmDx on NSCLC)
Objective: To determine the PD-L1 Tumor Proportion Score (TPS) in formalin-fixed, paraffin-embedded (FFPE) non-small cell lung cancer (NSCLC) tissue sections.
Materials:
- FFPE tissue sections (4 µm thickness)
- PD-L1 IHC 22C3 pharmDx kit (Agilent, SK006)
- Autostainer (e.g., Dako Link 48)
- Positive and negative control slides
- Light microscope
Procedure:
- Baking & Deparaffinization: Bake slides at 60°C for 1 hour. Deparaffinize in xylene and rehydrate through graded alcohols.
- Antigen Retrieval: Use EnVision FLEX Target Retrieval Solution (High pH, 50x) in a preheated retrieval chamber (97°C) for 20 minutes.
- Peroxidase Blocking: Apply endogenous enzyme block for 5 minutes.
- Primary Antibody Incubation: Apply anti-PD-L1 monoclonal antibody (clone 22C3) for 30 minutes at room temperature.
- Visualization: Apply labeled polymer-HRP anti-mouse secondary for 30 minutes, followed by DAB+ chromogen for 10 minutes.
- Counterstaining: Counterstain with hematoxylin, then dehydrate and mount.
- Scoring (TPS): Assess the percentage of viable tumor cells with partial or complete membrane staining at any intensity. TPS = (Number of PD-L1 staining tumor cells / Total number of viable tumor cells) x 100%. Score only viable tumor cell membranes; exclude necrotic areas, stromal cells, and lymphocytes.
Protocol 2: Tumor Mutational Burden (TMB) Assessment via Targeted NGS Panel
Objective: To calculate TMB (mutations per megabase) from DNA extracted from tumor and matched normal FFPE samples using a targeted sequencing panel.
Materials:
- DNA from FFPE tumor and matched normal (≥50 ng)
- Targeted NGS panel (e.g., Illumina TSO500, ~1.5 Mb)
- Next-generation sequencer (Illumina NovaSeq)
- Bioinformatics pipeline (e.g., Illumina DRAGEN TMB, bcbio)
Procedure:
- DNA QC: Quantify DNA using fluorometry (Qubit). Assess fragment size (TapeStation).
- Library Preparation: Perform hybrid capture-based library preparation per kit instructions, incorporating unique dual indices.
- Sequencing: Sequence to a minimum mean coverage of 500x for tumor and 200x for normal samples.
- Bioinformatic Analysis:
- Alignment: Map reads to a reference genome (hg38) using an aligner (e.g., BWA-MEM).
- Variant Calling: Call somatic SNVs and small indels using a caller (e.g., Strelka2, Mutect2) against the matched normal.
- Filtering: Remove known germline variants (using population databases like gnomAD), synonymous variants, and variants in known germline or blacklisted regions.
- TMB Calculation: TMB = (Total number of passing somatic, coding mutations) / (Size of the coding capture panel in Mb). Report as mutations per megabase (mut/Mb).
Visualization: Diagrams
Title: Biomarker Development Pipeline to Guidelines
Title: Multi-Omics Biomarker Data Integration Workflow
Title: PD-1/PD-L1 Checkpoint Blockade Mechanism
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Immunotherapy Biomarker Research
| Item / Solution | Function / Application | Example Product/Catalog |
|---|---|---|
| Validated IHC Antibody Clones | Detect protein biomarkers (PD-L1, CD8, etc.) on FFPE tissue with high specificity for clinical-grade assays. | PD-L1 Clone 22C3 (Agilent, SK006); CD8 (C8/144B, Dako M7103) |
| Multiplex Immunofluorescence (mIF) Kits | Enable simultaneous detection of 6+ biomarkers on a single tissue section to study spatial relationships and immune contexture. | Akoya Biosciences OPAL 7-Color Kit; Ultivue InSituPlex |
| Targeted NGS Panels for TMB/IO | Harmonized wet-lab and bioinformatic solution for assessing TMB, MSI, and somatic variants from limited FFPE DNA. | Illumina TruSight Oncology 500; FoundationOne CDx |
| Gene Expression Panels | Profile immune and tumor gene signatures from low-quality RNA derived from FFPE samples. | NanoString nCounter PanCancer IO360 Panel; HTG EdgeSeq Immuno-Oncology Assay |
| Digital Spatial Profiling (DSP) Technology | Combine high-plex RNA/protein analysis with spatial resolution from user-defined regions of interest (e.g., tumor vs. stroma). | NanoString GeoMx Digital Spatial Profiler |
| Single-Cell RNA-seq Kits | Profile transcriptomes of individual cells from tumor dissociates to discover novel cell states predictive of response. | 10x Genomics Chromium Single Cell 5' Immune Profiling |
| Cytometry by Time-of-Flight (CyTOF) Antibodies | Perform ultra-high parameter (40+) proteomic phenotyping of immune cells with minimal signal overlap. | Standard BioTools Maxpar Direct Immune Profiling Assay |
Conclusion
The field of biomarker identification for immunotherapy response is rapidly evolving beyond single-analyte assays toward integrated, multi-modal models. Foundational markers like PD-L1 and TMB provide a critical baseline, but their limitations underscore the need for the sophisticated methodologies and multi-omic integration detailed here. Success requires rigorous troubleshooting of technical and analytical variability, followed by robust comparative validation in diverse clinical contexts. Future progress hinges on collaborative frameworks for data sharing, the development of standardized, dynamic (e.g., ctDNA-based) monitoring tools, and the design of biomarker-stratified clinical trials. Ultimately, the convergence of advanced technologies, computational biology, and clinical validation will be essential to realize the promise of truly personalized immunotherapy, improving patient outcomes and optimizing healthcare resource utilization.