Prognostic vs Predictive Biomarkers: A Comprehensive Framework for Clinical Utility Assessment in Drug Development
This article provides a systematic guide for researchers, scientists, and drug development professionals on evaluating the clinical utility of prognostic and predictive biomarkers.
Prognostic vs Predictive Biomarkers: A Comprehensive Framework for Clinical Utility Assessment in Drug Development
Abstract
This article provides a systematic guide for researchers, scientists, and drug development professionals on evaluating the clinical utility of prognostic and predictive biomarkers. It covers foundational definitions, methodological approaches for development and application, strategies to overcome common implementation challenges, and robust validation frameworks. By integrating insights from recent advances in multi-omics, artificial intelligence, and clinical trial design, this review offers actionable methodologies to bridge the gap between biomarker discovery and clinical implementation, ultimately supporting more efficient and personalized therapeutic development.
Demystifying Biomarker Fundamentals: From Core Definitions to Clinical Context
In the era of personalized medicine, biomarkers have become indispensable tools for refining diagnosis, prognostication, and treatment selection. A clear understanding of the distinct roles played by different classes of biomarkers is fundamental to their correct application in both drug development and clinical practice. Two categories, prognostic and predictive biomarkers, are particularly crucial, yet their concepts are frequently conflated. A prognostic biomarker is defined as "a biomarker used to identify likelihood of a clinical event, disease recurrence or progression in patients who have the disease or medical condition of interest" [1]. In essence, it provides information about the natural history of the disease, independent of any specific therapy. In contrast, a predictive biomarker is "used to identify individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a medical product or an environmental agent" [2]. It informs on the likelihood of response to a specific therapeutic intervention.
The clinical utility of a biomarker—the extent to which it improves patient outcomes and healthcare decision-making—is the ultimate measure of its value [3] [4]. This guide provides a detailed, objective comparison of prognostic and predictive biomarkers, underpinned by foundational definitions, experimental data, and methodological protocols, to serve researchers, scientists, and drug development professionals.
Core Conceptual Differences and Direct Comparison
The fundamental distinction lies in the clinical question each biomarker type answers. A prognostic biomarker addresses "What is the likely course of my patient's disease?", while a predictive biomarker addresses "Will this specific treatment work for my patient?" [5]. This difference dictates their application; prognostic markers are used for patient stratification and counseling about disease outcomes, whereas predictive markers are used for treatment selection [6] [2].
Table 1: Core Conceptual Comparison of Prognostic and Predictive Biomarkers
| Feature | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Core Question | What is the likely disease outcome? | Will this specific treatment be effective? |
| Clinical Utility | Stratifies patients by risk of future events (e.g., recurrence, death) [1]. | Identifies patients most likely to benefit from a specific therapy [2]. |
| Effect of Biomarker | The association between the biomarker and outcome is present without reference to different interventions [1]. | Acts as an effect modifier; the biomarker status changes the effect of the therapy [6] [2]. |
| Interpretation Context | Interpretation is relative to the natural history of the disease or a standard background therapy. | Interpretation is always relative to a specific therapeutic intervention and a control. |
| Typical Study Design for Validation | Often identified from observational data in a defined patient cohort [1]. | Generally requires a comparison of treatment to control in patients with and without the biomarker, ideally from randomized trials [6] [2]. |
Illustrative Examples in Oncology
The following examples, summarized in the table below, clarify these concepts in a concrete context.
Table 2: Exemplary Biomarkers in Oncology
| Biomarker | Type | Clinical Context | Utility and Interpretation |
|---|---|---|---|
| Chromosome 17p deletion / TP53 mutation [1] | Prognostic | Chronic Lymphocytic Leukaemia (CLL) | Assesses likelihood of death, indicating a more aggressive disease course. |
| Gleason Score [1] | Prognostic | Prostate Cancer | Assesses likelihood of cancer progression based on tumor differentiation. |
| BRCA1/2 mutations | Dual | Breast Cancer | Prognostic: Evaluates likelihood of a second breast cancer [1].Predictive: Identifies likely responders to PARP inhibitors in platinum-sensitive ovarian cancer [2]. |
| HER2/neu amplification [7] [5] | Predictive | Breast Cancer | Identifies patients who are likely to respond to HER2-targeted therapies like Trastuzumab. |
| EGFR mutations [5] | Predictive | Non-Small Cell Lung Cancer (NSCLC) | Identifies patients likely to respond to EGFR tyrosine kinase inhibitors. |
| BRAF V600E mutation [6] | Predictive | Melanoma | Identifies patients with late-stage melanoma who are candidates for BRAF inhibitor therapy (e.g., vemurafenib). |
Methodological Frameworks for Biomarker Assessment
Experimental Design for Distinguishing Prognostic from Predictive Effects
A common point of confusion arises because a biomarker can be both prognostic and predictive. Isolating a purely predictive effect requires a specific study design that includes a control group not receiving the investigational therapy. As the FDA-NIH Biomarker Working Group explains, demonstrating that biomarker-positive patients have a better outcome on an experimental therapy does not, by itself, establish a predictive effect. The same survival difference could be due to the biomarker's prognostic ability [6]. A predictive effect is established by a significant treatment-by-biomarker interaction, where the difference in outcome between the experimental and control therapies is greater in the biomarker-positive group than in the biomarker-negative group [6] [2].
Phased Approach for Evaluating Clinical Utility
Establishing that a biomarker is statistically associated with an outcome is only the first step. Proving its clinical utility—that its use actually improves patient management and health outcomes—requires a phased approach [3] [8]. These phases progress from early discovery to confirmation of real-world effectiveness.
Table 3: Phases of Biomarker Development and Assessment
| Phase | Primary Objective | Key Methodological Considerations |
|---|---|---|
| 1. Discovery [8] | To identify a biomarker associated with pathology or a biological process. | Focus on biological plausibility and initial measurement reliability. Often uses "predictor-finding" studies. |
| 2. Translation [8] | To determine if the biomarker can separate diseased from non-diseased, or high-risk from low-risk patients. | Evaluation of diagnostic accuracy (sensitivity, specificity, AUC). Requires a clear reference standard. |
| 3. Single-Center Clinical Utility [8] | To assess if the biomarker is useful in clinical practice at a single site. | Evaluation of impact on clinical decision-making and patient outcomes (e.g., via biomarker-strategy RCTs [3]). |
| 4. Multi-Center Validation & Cost-Effectiveness [8] | To confirm utility across multiple centers and assess economic impact. | Large-scale studies to ensure generalizability. Formal cost-effectiveness analysis is conducted [4]. |
Determining Clinical Utility and Cut-Points
The gold standard for measuring the health impact of a biomarker strategy is a randomized controlled trial where participants are randomized to a management strategy that uses the biomarker result versus one that does not [3]. This design directly measures whether biomarker-informed care leads to better outcomes, such as reduced hospitalizations or improved quality-adjusted life-years (QALYs) [3].
Furthermore, selecting the optimal cut-point for a continuous biomarker can be guided by clinical utility rather than just statistical accuracy. Methods are being developed that incorporate the clinical consequences of test results, integrating diagnostic accuracy (sensitivity, specificity) with the outcomes of clinical decisions (e.g., maximizing total clinical utility or balancing positive and negative utility) [9].
The Scientist's Toolkit: Essential Reagents and Materials
The transition of a biomarker from a research concept to a validated diagnostic, especially a companion diagnostic, demands rigorous standardization of reagents and protocols [7].
Table 4: Essential Research Reagent Solutions for Biomarker Development
| Reagent/Material | Function in Biomarker Assay Development | Critical Considerations |
|---|---|---|
| Validated Primary Antibodies (for IHC) [7] | Specifically binds to the target protein analyte in tissue sections. | Requires extensive validation for specificity and sensitivity in the specific assay platform (e.g., FFPE tissues). Changes in antibody lot or vendor may require re-validation. |
| Cell Line Controls [7] | Serves as a reference standard for assay performance and reproducibility across runs. | Must be prepared to give consistent protein expression levels. Ideally, multiple controls spanning the assay's dynamic range (e.g., negative, low-positive, high-positive) are used. |
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue | The standard substrate for retrospective and diagnostic tissue-based biomarker studies. | Pre-analytical variables (cold ischemia time, fixation duration, processing) significantly impact results, especially for phospho-proteins and labile biomarkers [7]. |
| Automated Staining Platforms | Performs the immunoassay (IHC) under tightly controlled, reproducible conditions. | Automation minimizes protocol "tweaking" and operator-to-operator variability, which is critical for quantitative or semi-quantitative assays [7]. |
| Digital Whole Slide Imaging (WSI) & Analysis Software | Enables quantitative, objective analysis of biomarker expression (e.g., H-score, percentage of positive cells). | Moves interpretation beyond subjective "eyeballing." Algorithms must be validated against clinical outcomes to ensure their scoring is clinically relevant [7]. |
The precise distinction between prognostic and predictive biomarkers is not merely academic; it is a foundational prerequisite for their valid development and application in clinical trials and patient care. Prognostic biomarkers illuminate the disease trajectory, while predictive biomarkers guide the therapeutic journey. The future of biomarker development lies in robust methodological frameworks that progress from discovery to the unequivocal demonstration of clinical utility through well-designed trials. As the field advances towards increasingly personalized medicine, the rigorous standards exemplified by companion diagnostics—treating assays as precise quantitative tools rather than qualitative stains—will become the benchmark for all biomarker development [7].
In the evolving landscape of precision medicine, the precise differentiation between outcome indicators and treatment response predictors represents a fundamental requirement for effective drug development and clinical trial design. These distinct categories of biomarkers serve different purposes, require different validation approaches, and inform different clinical decisions. Outcome indicators, more formally known as prognostic biomarkers, provide information about a patient's overall disease course, including natural progression and long-term outcomes, regardless of specific therapeutic interventions. In contrast, treatment response predictors, or predictive biomarkers, identify patients who are more likely to respond favorably to a particular treatment, enabling therapy selection tailored to individual biological characteristics [10].
The clinical utility of this distinction extends beyond academic classification to practical implementation across therapeutic areas. In oncology, for example, biomarkers guide therapy selection for numerous cancer types, while in psychiatry, they are increasingly employed to optimize antidepressant selection. The critical importance of this differentiation lies in its direct impact on clinical decision-making, clinical trial optimization, drug development efficiency, and ultimately, patient outcomes. Misclassification or conflation of these biomarker types can lead to flawed trial designs, inappropriate treatment decisions, and failed drug development programs. This guide provides a structured comparison of these biomarker categories, supported by experimental data and methodological details to inform researchers, scientists, and drug development professionals.
Comparative Analysis: Prognostic versus Predictive Biomarkers
Table 1: Fundamental Characteristics of Prognostic and Predictive Biomarkers
| Characteristic | Prognostic Biomarkers | Predictive Biomarkers |
|---|---|---|
| Primary Function | Provide information about disease course and long-term outcomes | Identify likelihood of response to specific treatments |
| Clinical Utility | Stratify patients by disease aggressiveness, inform monitoring intensity | Guide therapy selection, optimize treatment benefit-risk ratio |
| Measurement Timing | Often measured at baseline or diagnosis | Typically assessed pretreatment |
| Decision Impact | Informs "what will happen" to the patient | Informs "which treatment will work" |
| Representative Examples | S100B in melanoma, LDH in multiple cancers [10] | PD-L1 in NSCLC, MSI-H/dMMR status in colorectal cancer [10] |
Table 2: Clinical Application and Evidence Requirements
| Parameter | Prognostic Biomarkers | Predictive Biomarkers |
|---|---|---|
| Evidence Standard | Association with outcomes across treatment types | Specific interaction with particular therapeutic intervention |
| Trial Design | Often evaluated in observational studies or untreated arms | Require randomized controlled trials with treatment interaction analysis |
| Validation Approach | Consistent association with disease outcomes across populations | Demonstrated differential treatment effect between biomarker-positive and negative groups |
| Regulatory Consideration | May inform patient stratification or subgroup identification | Often required for companion diagnostic approval |
Methodological Approaches: Experimental Protocols for Biomarker Validation
Neuroimaging Biomarkers for Antidepressant Response Prediction
Recent research has established protocols for developing neuroimaging-based predictive biomarkers for antidepressant treatment response, with demonstrated cross-trial generalizability. In a prognostic study examining major depressive disorder (MDD) outcomes, researchers implemented a standardized methodology across two large multisite studies [11].
Experimental Protocol:
- Study Design: Prognostic study using data from EMBARC (US) and CANBIND-1 (Canadian) randomized clinical trials
- Participants: 363 adult MDD patients (225 from EMBARC, 138 from CANBIND-1; mean age 36.6±13.1 years; 64.7% female)
- Interventions: Sertraline (EMBARC) and escitalopram (CANBIND-1) administration
- Data Collection: Structural and functional resting-state MRI at baseline, clinical and demographic data, depression severity scores at baseline and week 2
- Predictor Variables: Clinical features (age, sex, employment, baseline depression severity, anhedonia scores, BMI) and neuroimaging features (functional connectivity of dorsal anterior cingulate cortex [dACC] and rostral anterior cingulate cortex [rACC])
- Outcome Measures: Treatment response defined as ≥50% reduction in depression severity at 8 weeks
- Analytical Approach: Elastic net logistic regressions with regularization; performance assessed using balanced classification accuracy and area under the curve (AUC)
- Validation Method: Cross-trial generalizability testing (training on one trial, testing on the other)
Key Findings: The best-performing models combining clinical features and dACC functional connectivity demonstrated substantial cross-trial generalizability (AUC = 0.62-0.67). The addition of neuroimaging features significantly improved prediction performance compared to clinical features alone. Early-treatment (week 2) depression severity scores provided the best generalization performance, comparable to within-trial performance [11].
Machine Learning Framework for Treatment Selection in Depression
The AID-ME study developed an artificial intelligence model to personalize treatment selection in major depressive disorder, representing an advanced approach to predictive biomarker implementation [12].
Experimental Protocol:
- Data Source: 22 clinical trials with 9042 adults with moderate to severe MDD
- Predictor Variables: Clinical and demographic variables routinely collectible in practice
- Outcome Measure: Remission across multiple pharmacological treatments
- Model Architecture: Deep learning model predicting probabilities of remission for 10 treatments
- Validation Approach: Held-out test-set validation, hypothetical and actual improvement testing, bias assessment
- Performance Metrics: AUC, population remission rate improvement, drug ranking variation
Key Findings: The model demonstrated an AUC of 0.65 on the held-out test-set, significantly outperforming a null model. It increased population remission rate in testing and showed significant variation in drug rankings across patient profiles without amplifying harmful biases [12].
Multi-Omics Biomarker Development in Prostate Cancer
A comprehensive approach to biomarker development in prostate cancer illustrates the integration of prognostic and predictive elements through multi-omics analysis [13].
Experimental Protocol:
- Data Sources: TCGA-PRAD bulk RNA sequencing datasets, single-cell RNA sequencing data (GSE206962), clinical cohorts from DKFZ and GEO repositories
- Analytical Methods: FindAllMarkers, Dseq2 R package, ssGSEA, WGCNA at single-cell and bulk transcriptome scales
- Machine Learning Framework: 14 algorithms with 162 algorithmic combinations to develop consensus immune and prognostic-related signatures (IPRS)
- Validation Approach: Systematic validation in training and test cohorts, multivariate nomogram construction
- Additional Assessments: Multi-omics analyses (genomic, single-cell transcriptomic, bulk transcriptomic), immunotherapy response evaluation, drug selection relevance
Key Findings: Identification of 91 genes associated with prognosis in the tumor microenvironment, with 15 connected to biochemical recurrence. The consensus IPRS demonstrated potential value in prognosis prediction and clinical relevance, with significant differences in biological functions, immune infiltration, and genomic mutations observed among different risk groups [13].
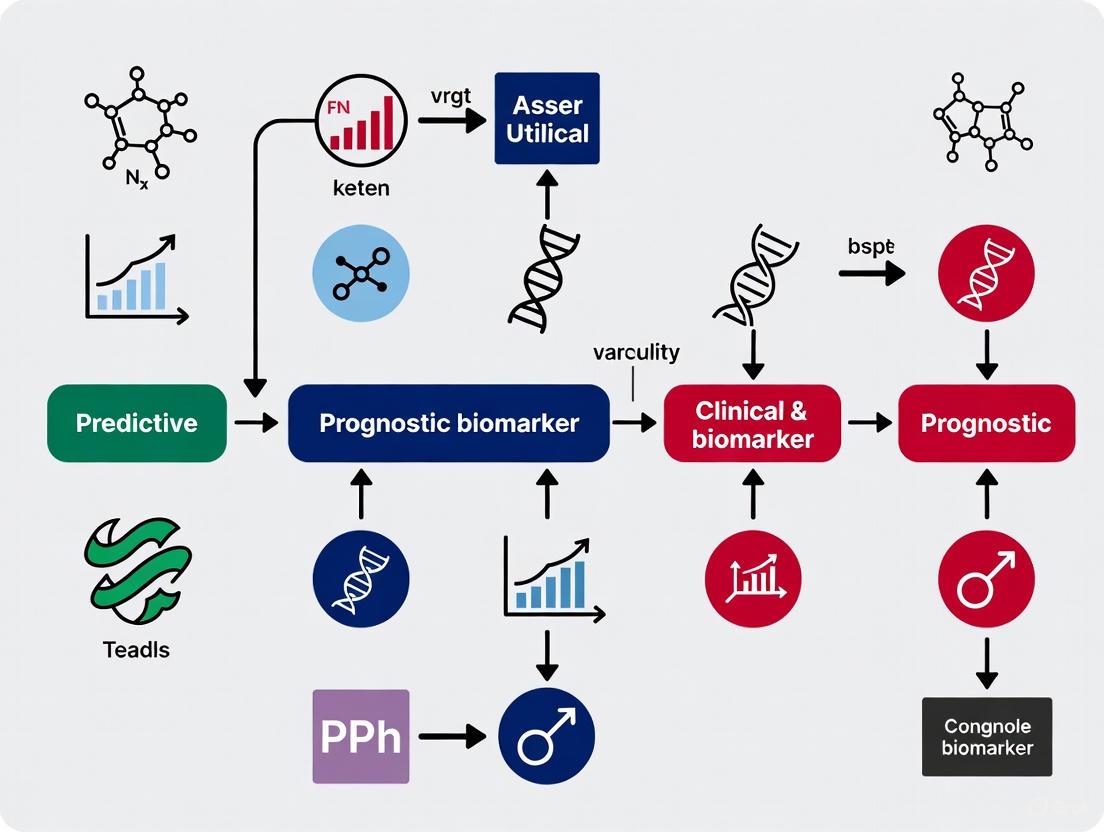
Visualizing Biomarker Pathways and Relationships
Biomarker Clinical Application Pathways
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Biomarker Research
| Tool/Platform | Primary Function | Application Examples |
|---|---|---|
| fMRIPrep | Standardized functional MRI data preprocessing | Neuroimaging biomarker development for antidepressant response prediction [11] |
| Weighted Gene Co-expression Network Analysis (WGCNA) | Identification of gene co-expression patterns | Prostate cancer prognostic signature development [13] |
| Single-cell RNA sequencing | Resolution of cellular heterogeneity within tumor microenvironment | Characterization of prostate cancer tumor microenvironment [13] |
| Liquid biopsy platforms | Non-invasive detection of circulating tumor DNA (ctDNA) | Early cancer detection, monitoring treatment response [14] [15] |
| Elastic net regularization | Variable selection and regularization in predictive modeling | Prediction of antidepressant treatment response [11] |
| Deep learning architectures | Complex pattern recognition across multiple treatments | Differential treatment benefit prediction for depression [12] |
| Next-generation sequencing (NGS) | Comprehensive genomic profiling | Mutation detection, fusion identification, copy number alteration analysis [14] |
| Multi-omics integration platforms | Combined analysis of genomic, transcriptomic, proteomic data | Improved biomarker precision for immunotherapy response [10] |
Clinical Implementation and Validation Frameworks
The translation of biomarkers from research discoveries to clinically applicable tools requires rigorous validation frameworks. For predictive biomarkers, this typically involves demonstration of a significant treatment-by-biomarker interaction in randomized controlled trials. The example of PD-L1 as a predictive biomarker for immunotherapy response in non-small cell lung cancer illustrates this validation process, where the KEYNOTE-024 trial showed that patients with PD-L1 expression ≥50% experienced significantly improved outcomes with pembrolizumab versus chemotherapy (median overall survival: 30.0 months vs. 14.2 months; HR: 0.63; 95% CI: 0.47-0.86) [10].
For prognostic biomarkers, validation requires consistent association with clinical outcomes across multiple patient populations and study designs. The incorporation of lactate dehydrogenase (LDH) into the American Joint Committee on Cancer (AJCC) staging for melanoma exemplifies this process, where elevated LDH levels consistently demonstrate association with poor prognosis across multiple studies [10]. The emerging field of multi-omics biomarkers represents a promising approach to overcoming the limitations of single-analyte biomarkers, with studies demonstrating approximately 15% improvement in predictive accuracy when integrating genomic, transcriptomic, and proteomic data through machine learning models [10].
The critical distinction between outcome indicators and treatment response predictors carries significant implications for drug development strategy and clinical trial design. Prognostic biomarkers enable enrichment of trials with patients at higher risk of disease progression, potentially reducing sample size requirements and study duration for outcomes-driven trials. Predictive biomarkers facilitate targeted drug development by identifying patient subgroups most likely to benefit from specific therapeutic interventions, potentially increasing trial success rates and supporting personalized medicine approaches. As biomarker science continues to evolve, the integration of multi-omics approaches, advanced analytics, and standardized validation frameworks will further enhance our ability to develop biomarkers that accurately inform both prognosis and treatment selection across therapeutic areas.
In the pursuit of efficient and meaningful drug development, the precise use of biomarkers, surrogate endpoints, and clinical endpoints is critical for evaluating therapeutic interventions. These concepts form a hierarchy of measurement, with each level serving a distinct purpose in clinical research and regulatory decision-making. A biomarker is a defined characteristic that is measured as an indicator of normal biological processes, pathogenic processes, or responses to an exposure or intervention [16]. Biomarkers encompass a wide range of measurements, including molecular, histologic, radiographic, or physiologic characteristics [16]. The Biomarkers, EndpointS, and other Tools (BEST) resource categorizes biomarkers into seven primary types: susceptibility/risk, diagnostic, monitoring, prognostic, predictive, pharmacodynamic/response, and safety biomarkers [16].
A surrogate endpoint is a specific type of biomarker intended to substitute for a clinical endpoint [17]. It is defined as "a biomarker intended to substitute for a clinical endpoint," where a clinical endpoint is "a characteristic or variable that reflects how a patient feels, functions, or survives" [17]. The use of a surrogate endpoint is fundamentally an exercise in extrapolation, where changes induced by a therapy on the surrogate are expected to reflect changes in a clinically meaningful outcome [18] [19]. In contrast, a clinical endpoint (also known as a clinically meaningful endpoint or true endpoint) provides a direct assessment of a patient's health status, measuring how a patient feels, functions, or survives [19]. These endpoints represent outcomes that matter most to patients, such as overall survival, reduction in pain, or improved physical function.
Hierarchical Relationship and Distinctions
The Conceptual Hierarchy
The relationship between biomarkers, surrogate endpoints, and clinical endpoints is inherently hierarchical. All surrogate endpoints are biomarkers, but not all biomarkers qualify as surrogate endpoints [17]. This hierarchy exists because a surrogate endpoint must undergo a rigorous validation process to ensure that treatment effects on the surrogate reliably predict clinical benefit [19]. A widely accepted four-level hierarchy for endpoints categorizes them as follows [19]:
- Level 1: A true clinical efficacy measure (e.g., overall survival, how a patient feels/functions/survives).
- Level 2: A validated surrogate endpoint for a specific disease setting and class of interventions.
- Level 3: A non-validated surrogate established as "reasonably likely to predict clinical benefit."
- Level 4: A correlate that is a measure of biological activity but not established to be at a higher level.
This structured approach helps clinical researchers and regulators appropriately interpret trial results based on the type of endpoint used.
Distinguishing Prognostic and Predictive Biomarkers
Within biomarker classification, understanding the distinction between prognostic and predictive biomarkers is essential for personalized medicine. A prognostic biomarker provides information about the likely natural history of a disease irrespective of therapy [6] [20]. It offers insight into the overall disease outcome, such as the risk of recurrence or progression. In contrast, a predictive biomarker indicates the likelihood of benefit from a specific therapeutic intervention [6] [20]. It helps identify which patients are most likely to respond to a particular treatment.
To visualize the fundamental hierarchical relationship between these core concepts and the distinction between prognostic and predictive biomarkers, the following diagram provides a clear structural overview:
A single biomarker can sometimes serve both prognostic and predictive functions. For example, HER2 overexpression in breast cancer initially identified patients with poorer prognosis (prognostic) but now primarily guides treatment with HER2-targeted therapies (predictive) [20]. Similarly, β-HCG and α-fetoprotein in male germ cell tumors help monitor for recurrence (prognostic) and guide decisions about adjuvant chemotherapy (predictive) [20].
Comparative Characteristics Table
The table below summarizes the key characteristics of clinical endpoints, surrogate endpoints, and general biomarkers:
Table 1: Key Characteristics of Endpoints in Clinical Research
| Characteristic | Clinical Endpoint | Surrogate Endpoint | General Biomarker |
|---|---|---|---|
| Definition | Direct measure of how a patient feels, functions, or survives [17] [19] | Biomarker intended to substitute for a clinical endpoint [17] | Measured indicator of biological processes, pathogenesis, or treatment response [16] |
| Primary Role | Direct assessment of treatment benefit | Predict clinical benefit; accelerate drug development [21] | Diagnosis, prognosis, monitoring, safety assessment [16] |
| Validation Requirements | Content validity; reliability; sensitivity to intervention [19] | Analytical validation; clinical validation; surrogate relationship evaluation [22] | Analytical validity; clinical validity for intended use [23] |
| Examples | Overall survival, stroke incidence, pain relief [19] | Blood pressure (for stroke risk), LDL-C (for cardiovascular events) [21] [22] | PSA levels, tumor grade, genetic mutations [17] [20] |
| Level in Hierarchy | Level 1 [19] | Level 2 (validated) or Level 3 (reasonably likely) [19] | Level 4 (or lower levels if validated as surrogate) [19] |
| Regulatory Acceptance | Gold standard for definitive trials [19] | Accepted when validated; basis for ~45% of new drug approvals (2010-2012) [21] | Varies by context of use and validation level |
Validation Frameworks and Methodologies
Validating Surrogate Endpoints
For a biomarker to be accepted as a surrogate endpoint, it must undergo rigorous evaluation. The validation process includes analytical validation (assessing assay sensitivity and specificity), clinical validation (demonstrating ability to detect or predict disease), and assessment of clinical utility [22]. The International Conference on Harmonisation guidelines propose evaluating three levels of association for surrogate endpoints: (1) biological plausibility, (2) individual-level association (predicting disease course in individual patients), and (3) study-level association (predicting treatment effects on the final outcome based on effects on the surrogate) [24].
Statistical methods for validating surrogate endpoints often involve meta-analytic approaches using data from multiple historical randomized controlled trials [24] [18]. The Daniels and Hughes method uses a bivariate meta-analysis to evaluate the association pattern between treatment effects on the surrogate and final outcomes [24]. A zero-intercept random-effects linear regression model can be applied to historical trial data to establish whether the surrogate endpoint reliably predicts effects on the clinical outcome [18].
Criteria for Surrogate Endpoint Validation
Several statistical and biological criteria should be satisfied for a surrogate endpoint to be considered valid:
Statistical Criteria:
- Acceptable sample size multiplier: The sample size needed for predicting treatment effect on the true endpoint via the surrogate should be practically feasible [18].
- Prediction separation score >1: Indicates that the effect of treatment on the surrogate is informative for the effect on the true endpoint [18].
- Slope (λ₁) ≠ 0: Establishes association between treatment effects on surrogate and final outcome [24].
- Conditional variance (ψ²) approaching zero: Suggests the true effect on the final outcome can be well-predicted from the effect on the surrogate [24].
- Intercept (λ₀) = 0: Ensures that no treatment effect on the surrogate implies no effect on the final outcome [24].
Biological/Clinical Criteria:
FDA Biomarker Qualification Process
The FDA's Biomarker Qualification Program employs a structured, collaborative approach to qualify biomarkers for use in drug development. This formal regulatory process ensures that a biomarker can be relied upon for a specific interpretation and application within a stated Context of Use (COU) [16]. The qualification process involves three stages:
- Stage 1: Letter of Intent - Initial submission describing the biomarker, proposed COU, and unmet drug development need [16].
- Stage 2: Qualification Plan - Detailed proposal for biomarker development to support qualification for the proposed COU [16].
- Stage 3: Full Qualification Package - Comprehensive compilation of supporting evidence for FDA's qualification decision [16].
Upon successful qualification, the biomarker may be used in any CDER drug development program within the qualified COU to support regulatory approval of new drugs [16].
Applications, Challenges, and Research Tools
Advantages and Applications
The appropriate use of biomarkers and surrogate endpoints offers significant advantages in drug development:
- Efficiency: Surrogate endpoints are often cheaper, easier, and quicker to measure than clinical endpoints [17]. For example, blood pressure measurement is far more efficient than long-term stroke mortality data collection [17].
- Smaller sample sizes: Clinical trials using surrogate endpoints typically require fewer participants [17]. A blood pressure trial might need only 100-200 patients, whereas a stroke prevention trial would require thousands [17].
- Earlier measurement: Surrogate endpoints can be assessed much sooner than long-term clinical outcomes [17], potentially accelerating drug development.
- Ethical considerations: In some cases, using biomarkers avoids ethical problems associated with waiting for clinical endpoints to manifest [17]. For example, in paracetamol overdose, plasma paracetamol concentration guides treatment decisions without waiting for actual liver damage [17].
- Personalized medicine: Predictive biomarkers enable selection of patients most likely to benefit from specific targeted therapies, particularly in oncology [23] [20].
Limitations and Cautions
Despite their advantages, significant challenges and limitations exist:
- Pathophysiological complexity: Surrogate endpoints are most reliable when disease pathophysiology and intervention mechanism are thoroughly understood [17]. Without this understanding, pitfalls await.
- Historical failures: Several biomarkers have failed as surrogates despite strong biological rationale. For example:
- Context dependence: A surrogate endpoint validated for one class of interventions may not apply to another, even within the same disease area [24].
- Statistical issues: Using surrogate endpoints as entry criteria can introduce heterogeneous variance and regression to the mean, potentially reducing study power [17].
- Safety detection: Smaller sample sizes in trials using surrogate endpoints may be insufficient to detect rare but serious adverse effects [17].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents and Platforms for Biomarker Research
| Tool/Category | Specific Examples | Primary Research Function |
|---|---|---|
| Genomic Platforms | Array-based hybridization assays; Next-generation DNA sequencing [23] | Identification of molecular targets; development of prognostic/predictive biomarkers |
| Gene-Expression Classifiers | Oncotype DX (21-gene assay) [23] | Prognostic stratification; prediction of recurrence risk |
| Immunohistochemical Tests | Estrogen receptor status; HER2 amplification status [23] [20] | Predictive biomarker assessment for treatment selection |
| Laboratory Assays | Serum TSH; INR with warfarin; autoantibodies; C. difficile toxin [17] | Diagnostic, monitoring, and safety biomarkers |
| Imaging Technologies | MRI scans (e.g., white dots for multiple sclerosis lesions) [17] | Radiographic biomarkers for diagnosis and disease monitoring |
| Physiological Measurements | Blood pressure; FEV1; peak expiratory flow rate [17] | Physiological biomarkers for disease status and treatment response |
Biomarkers, surrogate endpoints, and clinical endpoints form an essential hierarchy in clinical research and drug development. While biomarkers serve broad purposes across diagnosis, prognosis, and monitoring, surrogate endpoints represent a specific subclass of biomarkers that undergo rigorous validation to substitute for clinical endpoints. The distinction between prognostic biomarkers (informing likely disease course) and predictive biomarkers (identifying patients likely to respond to specific treatments) is particularly crucial for advancing personalized medicine. Despite the efficiency gains offered by surrogate endpoints, their validation requires comprehensive evidence that treatment effects on the surrogate reliably predict meaningful clinical benefits. As biomarker science evolves with new genomic technologies and analytical methods, these tools will continue to transform drug development, enabling more targeted therapies and refined treatment selection for individual patients.
In the era of precision medicine, biomarkers are indispensable tools that provide an objectively measured indicator of normal biological processes, pathogenic processes, or pharmacological responses to therapeutic interventions [25]. The clinical utility of biomarkers is primarily categorized into two distinct functions: prognostic and predictive. Prognostic biomarkers provide information about the patient's overall cancer outcome regardless of therapy, identifying the likelihood of a clinical event, disease recurrence, or progression in patients who have the disease or medical condition of interest [6] [26]. In contrast, predictive biomarkers identify individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a medical product or environmental agent, providing information on the effect of a therapeutic intervention [6] [26].
The distinction between these biomarker types has profound clinical implications. For example, in breast cancer, estrogen receptor (ER) and progesterone receptor (PR) expression serve as both prognostic and predictive biomarkers—patients with ER+/PR+ tumors have better survival (prognostic) and are more likely to benefit from endocrine therapy (predictive) [26]. Similarly, HER2/neu amplification in breast cancer indicates a more aggressive tumor (prognostic) and predicts response to trastuzumab treatment (predictive) [26]. Understanding this distinction is critical for proper patient stratification and treatment selection in clinical practice.
Performance Comparison of Multi-Level Biomarker Data
Cancer Subgroup Classification Accuracy
Advanced technologies now enable the measurement of molecular data at various levels of gene expression, including genomic, transcriptomic, and translational levels [27]. However, information carried by one level of gene expression is not similar to another, as evidenced by the low correlation observed between different molecular levels such as transcriptome and proteome data [28]. This fundamental insight has driven interest in integrated multi-omics approaches for precision medicine applications.
Table 1: Performance Comparison of Single vs. Multi-Omic Data in Cancer Subgroup Classification
| Cancer Type | Transcriptome Only | miRNA Only | Methylation Only | Proteome Only | Integrated Multi-Omic |
|---|---|---|---|---|---|
| Breast Cancer | >90% accuracy [28] | Data available [27] | Data available [27] | >90% accuracy [28] | Comprehensive analysis [27] |
| Multiple Cancers (9 types) | High accuracy in most cancers [28] | Performance varies [27] | Performance varies [27] | High accuracy in most cancers [28] | Potential performance improvement [28] |
Research demonstrates that for many cancers, even a single molecular level can predict corresponding cancer subgroups with very high accuracy (exceeding 90%) [28]. The selection of appropriate machine learning algorithms significantly impacts classification performance, with kernel- and ensemble-based algorithms consistently outperforming other methodologies across diverse gene-expression datasets [29]. The integration of multi-omic data represents a promising approach to potentially enhance classification accuracy beyond what can be achieved with single-omic data sources [27].
Algorithm Performance for Biomarker Discovery
The high-dimensional nature of genomic data, where the number of features (p) far exceeds the number of samples (n), creates unique computational challenges collectively known as the "n << p" problem [28] [30]. Feature selection and machine learning algorithm selection are critical components in addressing this challenge and deriving robust biomarkers from complex molecular data.
Table 2: Machine Learning Algorithm Performance for Gene-Expression Classification
| Algorithm Type | Performance Characteristics | Best For | Limitations |
|---|---|---|---|
| Kernel-Based Algorithms | Consistently high performance across datasets [29] | Complex pattern recognition | Computational intensity |
| Ensemble Methods | Top-performing category [29] | High-dimensional data | Model interpretability |
| Logistic Regression | Best average rank overall [29] | General-purpose applications | Poor performance in 4.9% of cases [29] |
| PPLasso | Outperforms traditional Lasso for correlated biomarkers [30] | Prognostic and predictive biomarker identification | Continuous endpoints only |
Hyperparameter optimization and feature selection typically improve predictive performance, with univariate feature-selection algorithms often outperforming more sophisticated methods [29]. The PPLasso method represents a significant advancement specifically designed to identify both prognostic and predictive biomarkers in high-dimensional genomic data where biomarkers are highly correlated, simultaneously integrating both effects into a single statistical model [30].
Experimental Protocols and Methodologies
Multi-Omic Data Integration Protocol
Comprehensive cancer subgroup classification requires systematic integration of diverse molecular data types. The following protocol outlines the methodology for such integrated analysis:
Data Acquisition and Preprocessing:
- Source multi-level gene expression data from curated repositories such as The Cancer Genome Atlas (TCGA), which contains pan-genomic data from numerous cancers with multiple omic measurements [28]
- Include transcriptome, miRNA, methylation, and proteome data types for comprehensive coverage
- Address the "n << p" problem through feature selection methods such as Fisher ratio, which assumes Gaussian distribution and selects top features based on means and standard deviations [28]
Model Building and Validation:
- Implement multiple classification algorithms representing diverse machine learning methodologies
- Apply nested cross-validation to evaluate the effects of hyperparameter optimization and feature selection
- Compare performance between models using single-omic data versus integrated multi-omic data
- Validate identified features for biological relevance across different gene expression levels [28]
This experimental approach has demonstrated that sets of genes discriminant in one gene level may not be discriminant in other levels, highlighting the importance of multi-level analysis [28].
Prognostic and Predictive Biomarker Identification
The PPLasso method provides a specialized statistical framework for simultaneous identification of prognostic and predictive biomarkers:
Statistical Modeling:
- Format the identification problem as variable selection in an ANCOVA (Analysis of Covariance) type model
- Include both treatment-specific effects (predictive components) and general biomarker effects (prognostic components)
- Account for potential correlation between biomarkers across different treatments [30]
Correlation Handling:
- Transform the design matrix to remove correlations between biomarkers before applying generalized Lasso
- Overcome limitations of traditional Lasso, which struggles when biomarkers are highly correlated
- Employ Precision Lasso approach that assigns similar weights to correlated variables [30]
Validation Framework:
- Conduct extensive numerical experiments comparing PPLasso to traditional Lasso and extensions
- Evaluate performance metrics including biomarker selection accuracy and model robustness
- Apply to publicly available transcriptomic and proteomic data for real-world validation [30]
This methodology specifically addresses the challenge of identifying both prognostic and predictive biomarkers in high-dimensional settings where traditional methods may fail.
Signaling Pathways and Technical Workflows
Multi-Omic Data Integration Workflow
Diagram 1: Multi-Omic Data Integration Workflow for Cancer Classification. This workflow illustrates the process from sample collection through multi-omic integration for cancer subgroup classification, highlighting the parallel processing of different molecular data types.
Prognostic vs Predictive Biomarker Identification
Diagram 2: Prognostic vs Predictive Biomarker Identification Pathway. This diagram outlines the critical pathway for distinguishing prognostic versus predictive biomarkers, requiring comparison of treatment to control in patients with and without the biomarker.
Key Research Reagent Solutions
Table 3: Essential Research Tools for Biomarker Discovery and Validation
| Resource Category | Specific Tools/Platforms | Function | Application Context |
|---|---|---|---|
| Data Resources | The Cancer Genome Atlas (TCGA) | Provides curated pan-genomic data from multiple cancers | Multi-omic cancer subgroup classification [27] [28] |
| UK Biobank Metabolomic Data | World's largest metabolomic dataset (~250 metabolites in 500,000 volunteers) | Disease risk prediction, drug discovery [31] | |
| Analytical Platforms | Mass Spectrometry (LC-MS/MS, GC-MS) | High-sensitivity metabolite measurement and quantification | Metabolomics, proteomics [32] |
| Nuclear Magnetic Resonance (NMR) | Molecular structure determination and metabolite quantification | Metabolomics with structural insights [32] | |
| Next-Generation Sequencing | High-throughput DNA and RNA sequencing | Genomic and transcriptomic biomarker discovery [33] | |
| Computational Tools | PPLasso R Package | Simultaneous selection of prognostic and predictive biomarkers | High-dimensional genomic data with correlated features [30] |
| ShinyLearner Tool | Benchmark comparison of classification algorithms | Algorithm selection for gene-expression classification [29] | |
| Feature Selection Methods | Fisher Ratio | Selects features based on means and standard deviations | Pre-processing high-dimensional omic data [28] |
The integration of multi-level biomarker data represents a transformative approach in modern precision medicine, enabling more accurate disease classification and patient stratification than single-omic approaches. Through comprehensive performance comparisons, we have demonstrated that while individual molecular levels often achieve high classification accuracy, integrated multi-omic strategies provide a more comprehensive biological understanding. The distinction between prognostic and predictive biomarkers remains clinically essential, with advanced statistical methods like PPLasso offering robust solutions for identifying both biomarker types in high-dimensional data. As metabolomic, proteomic, and genomic datasets continue to expand—exemplified by resources like UK Biobank—and as analytical technologies advance, researchers and drug development professionals are increasingly equipped to develop sophisticated biomarker panels that optimize therapeutic decision-making and patient outcomes.
The Evolving Role of Biomarkers in Precision Medicine and Proactive Health Management
The landscape of modern medicine is undergoing a fundamental transformation, shifting from traditional disease diagnosis and treatment models toward health maintenance approaches based on prediction and prevention [25]. This paradigmatic shift toward proactive health management is grounded in the biopsychosocial medical model, emphasizing early health risk identification and implementation of targeted interventions to prevent disease onset or delay progression [25]. Biomarkers—defined as objectively measurable indicators of biological processes—serve as the cornerstone of this transformation, providing crucial biological signposts that reveal underlying health conditions and enabling more precise medical interventions [34].
The classification of biomarkers extends beyond simple diagnostic applications to include prognostic biomarkers that forecast disease outcomes independent of treatment, and predictive biomarkers that indicate likely benefit from specific therapeutic interventions [20]. Understanding this distinction is critical for researchers and drug development professionals, as it directly influences clinical trial design, patient stratification strategies, and therapeutic development pathways. The rapid expansion of molecular characterization efforts has permitted the development of clinically meaningful biomarkers that help define optimal therapeutic strategies for individual patients, particularly in oncology where biomarkers have transformed treatment protocols for conditions like HER2-positive breast cancer and EGFR-mutated lung cancer [34].
Biomarker Fundamentals: Classification and Clinical Utility
Defining Biomarker Types and Applications
Biomarkers serve as measurable indicators within the body, appearing in blood, tissue, or other biological samples, providing crucial data about normal processes, disease states, and treatment responses [34]. Their role in healthcare continues to evolve, driving innovations in personalized medicine and therapeutic development. The classification system enables healthcare teams to develop targeted, effective treatment strategies.
Table: Biomarker Classification and Clinical Applications
| Biomarker Type | Primary Function | Clinical Utility | Examples |
|---|---|---|---|
| Diagnostic | Identifies or confirms a current disease state | Determines the presence or absence of disease | Beta-amyloid for Alzheimer's disease [34] |
| Prognostic | Provides information on likely disease outcome irrespective of treatment | Informs about natural disease history and overall outcome | HER2 overexpression in breast cancer (originally identified as poor prognosis) [20] |
| Predictive | Indicates likelihood of response to a specific treatment | Guides treatment selection by predicting therapeutic efficacy | Estrogen receptors in breast cancer predicting response to antiestrogen therapy [20] |
| Pharmacodynamic | Measures biological response to therapeutic intervention | Monitors drug activity and helps determine optimal dosing |
The distinction between prognostic and predictive biomarkers carries significant clinical implications. A single factor may serve both functions, as demonstrated by HER2 overexpression in breast cancer, which initially identified patients with poor prognosis but now predicts response to targeted therapies [20]. Similarly, β-HCG and α-fetoprotein in male germ cell tumors provide both prognostic information through early recognition of disease recurrence and predictive value by indicating when to initiate known effective cytotoxic drugs [20].
Establishing Clinically Relevant Biomarkers
Developing reliable biomarkers requires integrating multidisciplinary approaches and multi-level validation [25]. The advancement of big data and artificial intelligence technologies has transformed biomarker research from hypothesis-driven to data-driven approaches, expanding potential marker identification [25]. A systematic biomarker validation process encompasses discovery, validation, and clinical validation phases, ensuring research findings' reliability and clinical applicability.
Multi-omics integration methods serve a crucial role in this process, developing comprehensive molecular disease maps by combining genomics, transcriptomics, proteomics, and metabolomics data [25]. This approach identifies complex marker combinations that traditional methods might overlook. Temporal data holds distinct value in biomarker research, as longitudinal cohort studies capturing markers' dynamic changes over time provide more comprehensive predictive information than single time-point measurements [25].
Methodological Approaches: From Discovery to Clinical Implementation
Biomarker Development Pipeline
Biomarker research follows a structured pipeline to ensure clinical validity and utility. Researchers should understand and explicitly address what stage of biomarker research they are conducting, as each phase has distinct objectives and requirements [8]. The development process can be partitioned into four sequential phases:
- Discovery Phase: Initial identification of biomarkers associated with pathology, assessment of biological plausibility, and measurement reliability [8]
- Translation Phase: Evaluation of how effectively the biomarker separates diseased from normal patients, or different risk categories [8]
- Single-Center Studies: Assessment of clinical utility in practice within a controlled setting [8]
- Multi-Center Studies: Determination of whether clinical utility maintains across multiple centers and assessment of cost-effectiveness [8]
A critical challenge in biomarker development is adequately powering studies to minimize false-positive results. Traditional "rule of 10" guidelines suggest that studies developing multivariable models should examine approximately one biomarker per 10 events of the least frequent outcome [8]. However, many imaging biomarker studies are characterized by "fishing trips" to identify viable biomarkers without prior hypotheses, tested in underpowered studies using incorrect methods [8]. A recent systematic review of radiomics research found an average type-I error rate (false-positive results) of 76%, largely due to inadequate sample size compared to the number of variables studied [8].
Statistical Considerations and Cut-Point Optimization
Selecting optimal cut-points for biomarkers represents a critical methodological challenge in diagnostic medicine. Several methods of cut-point selection have been developed based on ROC curve analysis, with the most prominent being Youden, Euclidean, Product, Index of Union (IU), and diagnostic odds ratio (DOR) methods [35]. Each method employs unique definition criteria in ROC space, and their performance varies depending on underlying distributions and degree of separation between diseased and non-diseased populations.
Simulation studies comparing these methods under different distribution pairs, degrees of overlap, and sample size ratios have revealed important performance characteristics [35]. With high AUC, the Youden method may produce less bias and MSE, but for moderate and low AUC, Euclidean has less bias and MSE than other methods [35]. The IU method yielded more precise findings than Youden for moderate and low AUC in binormal pairs, but its performance was lower with skewed distributions [35]. In contrast, cut-points produced by DOR were extremely high with low sensitivity and high MSE and bias [35].
Innovative Trial Designs for Biomarker Validation
Novel clinical trial designs are emerging to address the challenges of biomarker validation. The Single-arm Lead-In with Multiple Measures (SLIM) design incorporates repeated biomarker assessments over a short follow-up period to address within-subject variability [36]. This approach is particularly valuable for early-phase trials of brief duration where changes in clinical and functional outcomes are unlikely to be observed.
The SLIM design involves repeated biomarker assessments during both placebo lead-in and post-treatment periods, minimizing between-subject variability and improving the precision of within-subject estimates [36]. Simulation studies demonstrate that this design can substantially reduce required sample sizes compared to traditional parallel-group designs, thereby lowering the recruitment burden [36]. This design is well suited for early-phase, short-duration trials but is not suitable for cognitive tests or other outcomes prone to practice or placebo effects [36].
Technological Innovations Driving Biomarker Discovery
AI and Machine Learning Applications
Artificial intelligence is radically transforming pharmaceutical biomarker analysis, revealing hidden biological patterns that improve target discovery, patient selection, and trial design [37]. After decades of relying on traditional biomarkers and statistical models to inform early-stage research, AI is beginning to reshape how we discover targets, stratify patients, and design clinical trials [37]. AI-driven pathology tools and biomarker analysis provide deeper biological insights and help clinical decision-making in fields as diverse as oncology, where the lack of reliable biomarkers to personalize treatment remains a major challenge [37].
The application of AI for biomarker discovery is particularly evident in digital pathology. Research demonstrates that AI can uncover prognostic and predictive signals in standard histology slides that outperform established molecular and morphological markers [37]. For instance, at DoMore Diagnostics, AI-based digital biomarkers for colorectal cancer prognosis have been developed that can stratify patients according to their risk profiles, potentially avoiding unnecessary adjuvant chemotherapy for low-risk patients [37].
Multi-Omics Integration and Advanced Analytics
Modern biomarker development leverages sophisticated technological platforms that enhance detection accuracy and reliability. The integration of advanced analytics with traditional clinical expertise creates a powerful framework for personalized medicine [34]. Multi-omics approaches are emerging as powerful tools, synthesizing insights from genomics, proteomics, and related fields to enhance diagnostic precision [34]. The genomic biomarker sector shows particular promise, with projections indicating growth to $14.09 billion by 2028, driven by advancements in personalized medicine [34].
Table: Advanced Biomarker Detection Technologies
| Technology Platform | Primary Applications | Key Advantages | Limitations |
|---|---|---|---|
| Next-Generation Sequencing | Genomic biomarker discovery, mutational analysis | Comprehensive genomic assessment, decreasing costs | Data interpretation challenges, storage requirements |
| Mass Spectrometry-Based Proteomics | Protein biomarker identification and validation | High specificity and sensitivity, quantitative analysis | Complex sample preparation, technical expertise needed |
| Liquid Biopsy Platforms | Non-invasive monitoring, treatment response assessment | Minimal invasiveness, serial monitoring capability | Sensitivity limitations for early detection |
| Digital Pathology with AI | Tumor microenvironment analysis, predictive signal detection | Uncovers patterns beyond human perception, uses existing samples | Validation requirements, regulatory considerations |
The integration of multi-omics data with advanced analytical methods has improved early Alzheimer's disease diagnosis specificity by 32%, providing a crucial intervention window [25]. Similarly, in oncology, AI-driven analysis of whole-slide images has demonstrated utility in predicting clinical benefit from immunotherapy in colorectal cancer [38].
Comparative Analysis of Biomarker Performance in Clinical Applications
Oncology Applications
Oncology represents the most significant disease indication category for biomarkers, accounting for 35.1% of the genomic biomarkers market [33]. Biomarkers have transformed cancer care by enabling more precise patient stratification and treatment selection. The comparative performance of different biomarker approaches in oncology reveals distinct advantages and limitations across technologies.
Table: Biomarker Performance in Oncology Applications
| Cancer Type | Biomarker Class | Clinical Application | Performance Metrics | Comparative Advantages |
|---|---|---|---|---|
| Colorectal Cancer | AI-based digital pathology | Predict benefit from atezolizumab + FOLFOXIRI-bevacizumab | Biomarker-high pts: mPFS 13.3 vs 11.5 mos; mOS 46.9 vs 24.7 mos [38] | Identifies patients likely to benefit from immunotherapy combinations |
| ALK+ NSCLC | AI-based imaging biomarkers | Predict PFS based on early brain metastasis response | Low- vs high-risk: 33.3 mo vs 7.8 mo PFS (HR 0.34) [38] | Earlier prediction than RECIST assessments |
| Resectable NSCLC | Radiomics + ctDNA | Predict complete pathological response | AUC 0.82 (radiomics alone); AUC 0.84 (with ctDNA) [38] | Non-invasive predictive tool for treatment response |
| Mesothelioma | AI-based imaging + genomic ITH | Predict response to niraparib | PFS HR 0.19 in high ITH vs 1.40 in low ITH [38] | Combines structural and genomic information for prediction |
The integration of multiple biomarker modalities demonstrates enhanced predictive power compared to single-platform approaches. In mesothelioma, the combination of AI-derived tumor volume assessment from CT scans with genomic intratumoral heterogeneity measures created a dual AI-genomic approach with multiple applications for predicting prognosis and selecting patients likely to benefit from specific treatments [38].
Neurological and Chronic Disease Applications
Beyond oncology, biomarkers are transforming management of neurological disorders, cardiovascular diseases, and other chronic conditions. Neurological biomarker research is gaining momentum, particularly in North America, with expanding applications for improved diagnostic accuracy and treatment optimization [34]. In Alzheimer's disease and related dementias, plasma biomarkers are increasingly used as surrogate outcomes in clinical trials due to their non-invasive nature [36].
The treatment selection segment represents 50.2% of the personalized medicine biomarker market share, demonstrating the growing confidence in biomarker-guided decision-making across therapeutic areas [34]. The global personalized medicine biomarker market is projected to reach USD 72.7 billion by 2033, reflecting expanding applications beyond oncology into neurological, cardiovascular, and autoimmune conditions [34].
Implementation Challenges and Solution Frameworks
Analytical and Validation Challenges
Despite promising technological advances, significant challenges persist in effectively integrating biomarker data, developing reliable predictive models, and implementing these in clinical practice [25]. The biomarker development pipeline faces multiple hurdles, with a 2014 review identifying a "major disconnect between the several hundred thousand published candidate biomarkers and the less than one-hundred US FDA-approved companion diagnostics" [8]. Very few biomarkers undergo any assessment beyond the articles first proposing them, with a recent systematic review finding that most multivariable models incorporating novel imaging biomarkers are never evaluated by other researchers [8].
Common analytical challenges include:
- High-dimensional data: Investigating numerous biomarker candidates with limited sample sizes increases false discovery rates [8]
- Within-subject variability: Biological and measurement error can obscure true treatment effects [36]
- Standardization limitations: Testing methods vary significantly across laboratories, creating inconsistency in results [33]
- Data heterogeneity: Multimodal data integration requires sophisticated analytical approaches [25]
Clinical Translation Barriers
Translating biomarker research into clinical practice faces substantial implementation barriers:
- Regulatory complexity: Approval processes for genomic biomarker tests are lengthy, with each region having its own regulatory framework [33]
- Clinical adoption hurdles: Pathologists, clinicians, and trial sponsors need to trust that AI-generated biomarkers are reproducible, interpretable, and clinically actionable [37]
- Workforce limitations: There is a limited supply of trained geneticists and bioinformaticians, slowing clinical adoption [33]
- Cost constraints: The expense of genomic testing remains high due to advanced sequencing tools and skilled personnel requirements [33]
To address these challenges, researchers have proposed integrated frameworks prioritizing three pillars: multi-modal data fusion, standardized governance protocols, and interpretability enhancement [25]. This systematic approach addresses implementation barriers from data heterogeneity to clinical adoption, enhancing early disease screening accuracy while supporting risk stratification and precision diagnosis.
The Scientist's Toolkit: Essential Research Reagent Solutions
Core Laboratory Materials and Platforms
Successful biomarker research requires specialized reagents and platforms that ensure reproducible, high-quality results. The following table outlines essential research reagent solutions for biomarker development and validation.
Table: Essential Research Reagent Solutions for Biomarker Development
| Reagent/Platform | Primary Function | Key Applications | Considerations for Selection |
|---|---|---|---|
| Next-Generation Sequencing Kits | Comprehensive genomic profiling | Genetic biomarker discovery, mutational analysis, tumor sequencing | Coverage depth, error rates, input DNA requirements |
| Multi-Omics Sample Preparation Kits | Standardized nucleic acid and protein extraction | Integrated genomic, transcriptomic, and proteomic analysis | Compatibility across platforms, yield, purity |
| Automated Homogenization Systems | Standardized sample processing | Consistent biomarker extraction from diverse sample types | Throughput, cross-contamination prevention, sample volume range |
| High-Sensitivity Immunoassay Reagents | Low-abundance protein detection | Pharmacodynamic biomarkers, inflammatory markers | Dynamic range, specificity, multiplexing capability |
| Liquid Biopsy Collection Tubes | Stabilization of circulating biomarkers | ctDNA, exosome, and circulating cell preservation | Stability duration, compatibility with downstream assays |
| Digital Pathology Slide Preparation Kits | Tissue processing for AI-based analysis | Tumor microenvironment characterization, morphology quantification | Stain consistency, image clarity, compatibility with scanners |
Analytical and Computational Tools
Beyond wet laboratory reagents, biomarker research requires sophisticated analytical and computational solutions:
- Bioinformatic Pipelines: Specialized software for processing next-generation sequencing data, including alignment, variant calling, and annotation tools [25]
- AI and Machine Learning Platforms: Computational frameworks for developing predictive models from complex biomarker data, including deep learning algorithms for image analysis [37] [38]
- Statistical Analysis Packages: Software solutions for cut-point optimization, including implementations of Youden, Euclidean, Product, IU, and DOR methods [35]
- Multi-Omics Integration Tools: Computational platforms that enable synthesis of genomic, proteomic, and metabolomic data for comprehensive biomarker discovery [25]
Visualizing Biomarker Development Workflows
Biomarker Development Pipeline
AI-Enhanced Biomarker Analysis Workflow
The field of biomarker research continues to evolve rapidly, with several emerging trends shaping future development. The global genomic biomarkers market is projected to reach USD 17 billion by 2033, rising from USD 7.1 billion in 2023, with a CAGR of 9.1% expected during 2024-2033 [33]. This growth is supported by the shift toward precision medicine, with genomic biomarkers increasingly used to classify patients, forecast disease progression, and optimize therapy decisions [33].
Future directions in biomarker research include:
- Expansion to rare diseases: Applying predictive models to conditions with unmet diagnostic needs [25]
- Dynamic health monitoring: Incorporating continuous physiological data from wearable devices and other digital health technologies [25]
- Strengthened multi-omics approaches: Enhancing integrative analysis across biological layers [25]
- Longitudinal cohort studies: Capturing biomarker trajectories over extended periods [25]
- Edge computing solutions: Leveraging decentralized data handling for low-resource settings [25]
In conclusion, biomarkers represent a transformative framework in modern healthcare, offering powerful insights into human biology and disease. The distinction between prognostic and predictive biomarkers carries significant implications for clinical trial design and therapeutic development. While technological innovations like AI and multi-omics integration are accelerating biomarker discovery, implementation challenges remain. Researchers and drug development professionals must navigate these complexities while advancing the field toward more precise, personalized healthcare solutions.
Biomarker Development and Implementation: Technical Pathways and Clinical Applications
Methodological Frameworks for Biomarker Discovery and Validation
Biological markers, or biomarkers, are defined characteristics measured as indicators of normal biological processes, pathogenic processes, or responses to an exposure or intervention [39]. In modern oncology, biomarkers have become indispensable tools that enable a shift from one-size-fits-all treatments to precision medicine, where prevention, screening, and treatment strategies are customized to patients with similar molecular characteristics [39]. The clinical utility of biomarkers spans their application as prognostic indicators, which provide information about overall expected clinical outcomes regardless of therapy, and as predictive indicators, which inform the likely response to a specific treatment [39] [40]. This distinction forms the cornerstone of biomarker clinical utility assessment research, guiding therapeutic decision-making and clinical trial design.
The journey of a biomarker from discovery to clinical implementation is long and arduous, with only approximately 0.1% of potentially clinically relevant cancer biomarkers described in literature progressing to routine clinical use [41]. This high attrition rate underscores the critical importance of rigorous methodological frameworks that can systematically address challenges at each development stage. The evolving landscape of biomarker science now integrates cutting-edge technologies including liquid biopsies, multi-omics platforms, artificial intelligence, and advanced validation techniques that collectively enhance the reliability and clinical applicability of novel biomarkers [14] [42] [43].
Foundational Concepts: Prognostic versus Predictive Biomarkers
Understanding the fundamental distinction between prognostic and predictive biomarkers is essential for proper clinical utility assessment. These biomarker types differ in their clinical applications, methodological requirements for identification, and statistical validation approaches.
A prognostic biomarker provides information about the natural history of the disease and overall expected clinical outcomes independent of therapy [39]. For example, in non-squamous non-small cell lung cancer (NSCLC), STK11 mutation is associated with poorer outcomes regardless of treatment selection [39]. Prognostic biomarkers help stratify patients into different risk groups, which can inform disease monitoring intensity and patient counseling about expected disease course.
A predictive biomarker informs the likely response to a specific therapeutic intervention [39] [40]. The most important predictive biomarkers found for NSCLC include mutations in the epidermal growth factor receptor (EGFR) gene [39]. The IPASS study demonstrated that patients with EGFR mutated tumors had significantly longer progression-free survival when receiving gefitinib compared to carboplatin plus paclitaxel, while patients with EGFR wildtype tumors had significantly shorter progression-free survival when receiving gefitinib [39]. This treatment-by-biomarker interaction is the hallmark of predictive biomarkers.
Table 1: Key Differences Between Prognostic and Predictive Biomarkers
| Characteristic | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Clinical Question | What is the likely disease course regardless of treatment? | Will this specific treatment benefit the patient? |
| Study Design Requirement | Can be identified in properly conducted retrospective studies | Must be identified using data from randomized clinical trials |
| Statistical Test | Main effect test of association between biomarker and outcome | Interaction test between treatment and biomarker |
| Clinical Application | Patient stratification by risk, intensity of monitoring | Treatment selection, therapy personalization |
| Example | STK11 mutation in NSCLC [39] | EGFR mutation for gefitinib response in NSCLC [39] |
| Regulatory Considerations | Demonstrates association with clinical outcomes | Demonstrates ability to predict response to specific intervention |
Methodological Frameworks for Biomarker Discovery
Biomarker Discovery Workflow and Technologies
The biomarker discovery process follows a multi-stage approach designed to systematically identify, test, and implement biological markers for enhanced disease diagnosis, prognosis, and treatment strategies [42]. The initial stage involves sample collection and preparation from relevant patient groups using proper handling and storage protocols to maintain sample integrity [42]. This is followed by high-throughput screening and data generation using technologies such as genomics, proteomics, and metabolomics to analyze large volumes of biological data and reveal patterns across numerous samples [42]. The subsequent data analysis and candidate selection phase employs bioinformatics and statistical tools to identify promising biomarker candidates that distinguish between diseased and healthy samples or indicate specific disease characteristics [42].
Diagram 1: Biomarker Discovery and Validation Workflow
Several advanced technological platforms have revolutionized biomarker discovery. Next-generation sequencing (NGS) enables high-throughput DNA sequencing, allowing researchers to rapidly analyze entire genomes and identify genetic mutations linked to disease progression and treatment responses [14] [42]. In colorectal cancer, NGS has been used to profile mutations across cancer-related genes, revealing that patients with wild-type profiles in these genes experienced longer progression-free survival when treated with cetuximab [42]. Mass spectrometry-based proteomics advances biomarker discovery by enabling precise identification and quantification of proteins linked to diseases, analyzing proteins in body fluids to pinpoint biomarkers for early diagnosis and monitoring of conditions like cancer and cardiovascular diseases [42]. Microarray technologies allow simultaneous measurement of thousands of gene expressions, enabling identification of disease-related biomarkers, particularly in cancer research where they help detect specific genetic changes associated with various cancer stages and types [42].
Key Considerations for Robust Discovery Studies
Several methodological considerations are critical during the discovery phase to ensure biomarker validity. The intended use of the biomarker (e.g., risk stratification, screening, diagnosis, prognosis, prediction of response to intervention, or disease monitoring) and the target population must be defined early in the development process [39]. The patients and specimens should directly reflect the target population and intended use, with careful attention to patient selection, specimen collection, specimen analysis, and patient evaluation to minimize bias [39].
Bias control represents one of the most crucial aspects of biomarker discovery. Bias can enter a study during patient selection, specimen collection, specimen analysis, and patient evaluation, potentially leading to failure in subsequent validation studies [39]. Randomization and blinding are two of the most important tools for avoiding bias. Randomization in biomarker discovery should control for non-biological experimental effects due to changes in reagents, technicians, machine drift, and other factors that can result in batch effects [39]. Specimens from controls and cases should be assigned to testing platforms by random assignment, ensuring equal distribution of cases, controls, and specimen age [39]. Blinding prevents bias induced by unequal assessment of biomarker results by keeping individuals who generate the biomarker data from knowing the clinical outcomes [39].
The analytical approach must be carefully planned to address study-specific goals and hypotheses. The analytical plan should be written and agreed upon by all research team members before data access to prevent data from influencing the analysis [39]. This includes pre-defining outcomes of interest, hypotheses to be tested, and criteria for success. When multiple biomarkers are evaluated, control of multiple comparisons should be implemented; measures of false discovery rate (FDR) are especially useful when using large-scale genomic or other high-dimensional data for biomarker discovery [39].
Methodological Frameworks for Biomarker Validation
Validation Pathways and Performance Metrics
Biomarker validation progresses through structured phases that establish analytical validity, clinical validity, and ultimately clinical utility. Analytical validation ensures the biomarker test accurately and reliably measures the intended analyte across specified sample matrices, assessing parameters including accuracy, precision, sensitivity, specificity, and reproducibility [41] [43]. The clinical validation phase demonstrates that the biomarker consistently correlates with or predicts clinical outcomes of interest [41] [43]. Finally, clinical utility establishes that using the biomarker in clinical decision-making improves patient outcomes or provides beneficial information for patient management [39] [40].
Table 2: Biomarker Validation Metrics and Their Interpretations
| Validation Metric | Definition | Interpretation | Common Assessment Methods |
|---|---|---|---|
| Sensitivity | Proportion of true cases that test positive | Ability to correctly identify individuals with the condition | ROC analysis, comparison to gold standard [39] |
| Specificity | Proportion of true controls that test negative | Ability to correctly identify individuals without the condition | ROC analysis, comparison to gold standard [39] |
| Positive Predictive Value (PPV) | Proportion of test positive patients who actually have the disease | Probability that a positive test result truly indicates disease | Clinical follow-up, outcome assessment [39] |
| Negative Predictive Value (NPV) | Proportion of test negative patients who truly do not have the disease | Probability that a negative test result truly excludes disease | Clinical follow-up, outcome assessment [39] |
| Area Under Curve (AUC) | Overall measure of how well the marker distinguishes cases from controls | Ranges from 0.5 (no discrimination) to 1.0 (perfect discrimination) | Receiver Operating Characteristic (ROC) curve [39] |
| Calibration | How well a marker estimates the risk of disease or of the event of interest | Agreement between predicted probabilities and observed outcomes | Calibration plots, goodness-of-fit tests [39] |
Regulatory agencies including the FDA and EMA advocate for a tailored approach to biomarker validation, emphasizing alignment with the specific intended use rather than a one-size-fits-all method [41]. These agencies now demand more comprehensive validation data, including enhanced analytical validity such as accuracy and precision of assays, often requiring independent sample sets and cross-validation techniques to strengthen evidence supporting biomarker effectiveness [41]. A review of the EMA biomarker qualification procedure revealed that 77% of biomarker challenges were linked to assay validity, with frequent issues including problems with specificity, sensitivity, detection thresholds, and reproducibility [41].
Advanced Validation Technologies Beyond Traditional Methods
While enzyme-linked immunosorbent assay (ELISA) has long been the gold standard for biomarker validation, advanced technologies now offer superior precision, sensitivity, and efficiency [41]. Liquid chromatography tandem mass spectrometry (LC-MS/MS) provides enhanced sensitivity and specificity compared to traditional ELISA, making it particularly useful for detecting low-abundance species and enabling analysis of hundreds to thousands of proteins in a single run [41]. Meso Scale Discovery (MSD) platforms, utilizing electrochemiluminescence (ECL) detection, offer up to 100 times greater sensitivity than traditional ELISA and a broader dynamic range [41].
These advanced technologies also provide significant economic and operational advantages. For example, measuring four inflammatory biomarkers (IL-1β, IL-6, TNF-α, and IFN-γ) using individual ELISAs costs approximately $61.53 per sample, while using MSD's multiplex assay reduces the cost to $19.20 per sample—representing a saving of $42.33 per sample [41]. MSD's U-PLEX multiplexed immunoassay platform allows researchers to design custom biomarker panels and measure multiple analytes simultaneously within a single sample, enhancing efficiency in biomarker research, especially when dealing with complex diseases or therapeutic responses [41].
Comparative Analysis of Biomarker Selection Techniques
Feature Selection Methods in High-Dimensional Data
Biomarker discovery from high-dimensional genomics data is typically modeled as a feature selection problem, where the aim is to identify the most discriminating features (e.g., genes) for a given classification task, such as distinguishing between healthy and tumor tissues or between different tumor stages [44]. These selection techniques can be broadly categorized as univariate methods, which evaluate the relevance of each feature independently from the others, and multivariate methods, which take into account interdependencies among features [44]. Different feature selection techniques may result in different sets of biomarkers, raising questions about biological significance and necessitating systematic comparison approaches [44].
A comparative methodology for evaluating biomarker selection techniques should address two key dimensions: (1) measuring the similarity/dissimilarity of selected gene sets, and (2) evaluating the implications of these differences in terms of both predictive performance and stability of selected gene sets [44]. Similarity analysis should incorporate both gene overlapping similarity (measuring the number of genes present in both sets) and functional similarity (evaluating whether different gene sets capture similar biological functions despite limited gene overlap) [44].
Diagram 2: Biomarker Selection Technique Comparison Framework
Stability and Performance Evaluation
The stability of a biomarker selection algorithm—its robustness with respect to sample variation—represents a critical but often overlooked aspect of biomarker validation [44]. Small changes in the original dataset should not significantly affect the outcome of the selection process. Evaluation protocols should jointly assess both stability and predictive performance through experimental procedures that involve creating multiple reduced datasets from the original data, applying selection techniques to each reduced dataset, and comparing the resulting biomarker subsets in terms of overlapping and classification performance [44].
Predictive performance evaluation should be incorporated into this stability assessment protocol by building classification models on each reduced dataset using the selected gene subsets and estimating model performance on test sets containing instances not included in the reduced datasets [44]. The Area Under the Curve (AUC) serves as an appropriate performance metric as it synthesizes sensitivity and specificity information and provides more reliable estimates with unbalanced class distributions [44]. This approach minimizes selection bias since test instances are not used in the gene selection stage [44].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Biomarker Research
| Tool Category | Specific Solutions | Primary Applications | Key Advantages |
|---|---|---|---|
| Sample Preparation | Protein arrays [42], Liquid biopsy kits [14] | Protein profiling, non-invasive cancer detection | High-throughput capabilities, precise detection, minimal patient burden |
| Analysis Platforms | Next-generation sequencing [14] [42], Mass spectrometry [42] [41] | Genomic mutation profiling, protein identification and quantification | Comprehensive coverage, high sensitivity and specificity |
| Validation Technologies | Meso Scale Discovery (MSD) [41], LC-MS/MS [41] | Biomarker verification, multiplex analysis | Superior sensitivity, broad dynamic range, cost efficiency |
| Data Analysis | Bioinformatics tools [42], Machine learning algorithms [14] [42] | Pattern recognition, biomarker signature identification | Ability to identify complex patterns in large datasets |
| Electronic Lab Notebooks | Labguru [45], SciNote [45] | Experimental documentation, data management | Reproducibility, data integrity, regulatory compliance |
Methodological frameworks for biomarker discovery and validation continue to evolve with technological advancements, yet fundamental principles remain critical for success. The distinction between prognostic and predictive biomarkers dictates distinct pathways for clinical utility assessment, with prognostic biomarkers requiring demonstration of association with clinical outcomes and predictive biomarkers necessitating evidence of treatment interaction effects. Robust study design incorporating randomization, blinding, pre-specified analytical plans, and appropriate control of multiple comparisons provides essential safeguards against bias, particularly crucial in high-dimensional data environments.
The emerging era of biomarker science increasingly leverages multiplex technologies, artificial intelligence, and multi-omics integration to enhance biomarker discovery efficiency and validation robustness. Advanced validation technologies including MSD and LC-MS/MS offer superior sensitivity and cost-effectiveness compared to traditional methods, while electronic laboratory notebooks and data management systems ensure reproducibility and regulatory compliance. As these methodologies continue to mature, they promise to accelerate the translation of biomarker research from bench to bedside, ultimately advancing personalized medicine and improving patient outcomes across diverse disease areas, particularly in oncology where biomarker-driven treatment strategies have demonstrated profound clinical impact.
Biomarkers have transformed oncology and drug development by enabling a shift from a one-size-fits-all treatment approach to personalized therapeutic strategies. This paradigm shift relies on two distinct but complementary types of biomarkers: prognostic and predictive. Prognostic biomarkers provide information about a patient's likely disease course or outcome regardless of therapy, serving as indicators of inherent disease aggressiveness [6]. In contrast, predictive biomarkers identify patients who are more likely to respond to a specific treatment, illuminating the biological interaction between a therapy and its target [6] [23]. The clinical utility of these biomarkers must be established through carefully designed validation trials that account for their distinct purposes and methodological requirements.
The fundamental difference between these biomarker types lies in their application and validation requirements. Prognostic biomarkers can often be validated through observational studies of patients receiving standard care or no treatment, as they reflect the natural history of the disease. Predictive biomarkers, however, require comparison of treatment effects between biomarker-defined subgroups, typically within the context of randomized controlled trials (RCTs), to determine if biomarker status modifies treatment response [6] [46]. This distinction forms the foundation for selecting appropriate clinical trial designs to establish biomarker utility.
Core Concepts: Prognostic Enrichment versus Predictive Stratification
Defining Key Strategies
Prognostic enrichment and predictive stratification represent two methodological approaches that leverage biomarkers to optimize clinical trial design and interpretation. Prognostic enrichment refers to the selection of patients with a higher likelihood of experiencing a disease-related outcome of interest, such as mortality or disease progression [47]. This strategy is particularly valuable when studying therapies with significant risk, as it focuses on patients who stand to benefit most and improves trial efficiency by increasing event rates. A classic example is the CONSENSUS trial, which demonstrated mortality benefit from enalapril in patients with severe heart failure using a relatively small sample size by selectively enrolling high-risk patients [47].
Predictive stratification, meanwhile, involves categorizing patients based on biological characteristics that anticipate differential response to specific therapies [47]. This approach enables truly personalized treatment by matching therapeutic mechanisms to patient biomarkers. The development of trastuzumab for HER2-positive breast cancer exemplifies successful predictive stratification, where treatment benefit was concentrated in a biologically defined subgroup [46] [47]. The following diagram illustrates how these strategies function within a precision medicine framework:
Statistical Interactions and Clinical Decision-Making
Understanding the nature of biomarker-treatment interactions is crucial for clinical application. Statistical interactions between biomarkers and treatments can be quantitative or qualitative. A quantitative interaction occurs when treatment effects differ in magnitude but not direction across biomarker subgroups [6]. In such cases, the experimental therapy may be superior for both biomarker-positive and negative patients, though to varying degrees. A qualitative interaction, in contrast, occurs when treatment effects differ in direction across biomarker subgroups - the experimental therapy is beneficial for one subgroup but ineffective or harmful for another [6]. This latter scenario represents the ideal predictive biomarker, as it enables clear treatment decisions based on biomarker status.
Distinguishing truly predictive biomarkers from merely prognostic ones requires careful analysis. A biomarker that appears associated with treatment response in a single-arm study may actually be prognostic rather than predictive. This determination requires comparison with a control group, as the same survival differences according to biomarker status may exist regardless of treatment [6]. The following diagram illustrates this critical analytical distinction:
Clinical Trial Designs for Biomarker Validation
Classification of Trial Designs
Multiple clinical trial designs have been developed to validate predictive biomarkers, each with distinct strengths, limitations, and applications. These designs can be broadly categorized as retrospective or prospective approaches, with prospective designs further classified into several specific types [46]. The selection of an appropriate design depends on the strength of preliminary evidence for the biomarker, assay reliability, prevalence of the biomarker, and ethical considerations regarding treatment allocation.
Table 1: Clinical Trial Designs for Predictive Biomarker Validation
| Design Type | Key Features | When to Use | Examples | Limitations |
|---|---|---|---|---|
| Retrospective Analysis of RCTs [46] | Uses archived specimens from previously conducted RCTs; prospectively specified analysis plan | When high-quality RCT specimens exist; strong biological rationale | KRAS validation for anti-EGFR antibodies in colorectal cancer [46] | Potential selection bias if specimens incomplete; limited by original trial design |
| Enrichment/Targeted Design [46] [48] | Enrollment restricted to biomarker-positive patients only | Strong preliminary evidence that treatment only benefits biomarker-positive patients | HER2-positive breast cancer trials for trastuzumab [46] | Cannot detect benefit in biomarker-negative patients; may leave questions about assay reproducibility |
| Unselected/All-Comers Design [46] [48] | Enrolls all patients regardless of biomarker status; includes pre-planned subgroup analysis | Preliminary evidence uncertain; want to evaluate biomarker in broad population | EGFR markers in lung cancer [46] | Larger sample size needed; potential diluted treatment effect in unselected population |
| Stratified Design [48] | All patients enrolled; randomization stratified by biomarker status | Biomarker is prognostic; want to ensure balance across arms | PD-L1 in NSCLC trials [48] | Does not specifically test treatment-biomarker interaction |
| Adaptive Design [49] | Allows modification of trial based on interim results (e.g., dropping biomarker subgroups) | Multiple biomarker-defined subgroups with uncertain treatment effects | BATTLE trial in lung cancer [49] | Operational complexity; potential statistical inflation |
Biomarker-Driven Trial Designs in Practice
The practical implementation of biomarker-driven trial designs requires careful consideration of operational and statistical factors. Enrichment designs offer efficiency when compelling evidence suggests treatment benefit is restricted to a biomarker-defined subgroup [46]. For example, the development of vemurafenib specifically for BRAF V600E-mutant melanoma followed this paradigm, as preclinical evidence strongly indicated the drug would be ineffective in BRAF wild-type tumors [6]. However, enrichment designs risk missing potential benefits in excluded populations and depend on highly accurate and reproducible biomarker assays [46].
All-comers designs (also called biomarker-stratified designs) provide the most comprehensive approach for validating predictive biomarkers [6] [48]. In this design, all eligible patients are enrolled and randomized to treatment options, with biomarker status determined either before or after randomization. This allows direct comparison of treatment effects across biomarker-defined subgroups and can detect both qualitative and quantitative interactions [6]. While this design requires larger sample sizes, it provides the most complete evidence about a biomarker's predictive utility and can evaluate whether the biomarker identifies patients who should receive the experimental therapy, avoid it, or be treated regardless of biomarker status.
Adaptive biomarker designs represent a more flexible approach, allowing modification of the trial based on interim results [49]. The BATTLE trial in non-small cell lung cancer exemplified this approach, using adaptive randomization to assign patients to treatments based on continuously updated probabilities of treatment success given their biomarker profile [49]. Such designs can more efficiently allocate patients to promising treatments but require sophisticated statistical methods and careful implementation to maintain trial integrity [49].
Experimental Protocols and Methodologies
Biomarker Assay Validation Framework
Before implementing any biomarker-driven trial design, rigorous analytical validation of the biomarker assay is essential. The validation process encompasses three critical components: analytical validity, clinical validity, and clinical utility [23]. Analytical validity refers to the assay's accuracy, reliability, and reproducibility when measuring the biomarker [23]. Clinical validity establishes that the test result correlates with the clinical endpoint of interest [23]. Clinical utility demonstrates that using the test to guide treatment decisions actually improves patient outcomes [23].
For gene-expression-based classifiers, particular methodological care is required during development. The key principle is that data used for evaluation must be distinct from data used for developing the classifier [23]. When datasets are sufficiently large, separate test sets should be used; with smaller datasets, complete cross-validation provides a more efficient approach [23]. Proper validation avoids the common pitfall of overoptimistic performance estimates that can occur when the same data is used for both classifier development and performance assessment.
Table 2: Essential Research Reagents and Platforms for Biomarker Validation
| Reagent/Platform Category | Specific Examples | Primary Function in Biomarker Research | Key Considerations |
|---|---|---|---|
| Genomic Analysis Platforms [25] | Whole genome sequencing, PCR, SNP arrays | Detection of DNA sequence variants and genetic alterations | Coverage depth, variant calling accuracy, turnaround time |
| Transcriptomic Profiling Technologies [25] | RNA-seq, microarrays, real-time qPCR | Gene expression analysis and signature development | RNA quality requirements, normalization methods, platform comparability |
| Proteomic Analysis Tools [25] | Mass spectrometry, ELISA, protein arrays | Protein expression and post-translational modification measurement | Antibody specificity, quantitative range, multiplexing capability |
| Multiplex Immunoassay Platforms | Multiplex IHC, phospho-flow cytometry | Simultaneous measurement of multiple protein biomarkers | Validation of antibody performance in multiplex setting, signal unmixing |
| Single-Cell Analysis Technologies [50] | Single-cell RNA-seq, CYTOF | Resolution of cellular heterogeneity in tumor microenvironments | Cell viability requirements, data integration challenges, cost considerations |
| Liquid Biopsy Platforms [50] | ctDNA analysis, exosome profiling | Non-invasive biomarker assessment and monitoring | Sensitivity for rare variants, standardization of pre-analytical variables |
Statistical Analysis Plan for Predictive Biomarker Validation
A prespecified statistical analysis plan is critical for robust validation of predictive biomarkers. The plan should clearly define the primary biomarker analysis, including the specific statistical test for treatment-biomarker interaction [46]. For time-to-event endpoints, such as overall survival or progression-free survival, Cox regression models with an interaction term between treatment and biomarker status are commonly used [6]. The analysis should be intent-to-treat, including all randomized patients in the groups to which they were randomly assigned.
The sample size calculation must account for the testing of interaction effects, which typically requires larger sample sizes than overall treatment effect comparisons [46]. For binary biomarkers, the required sample size is approximately four times larger than that needed to detect a main effect of the same magnitude [46]. When multiple biomarker subgroups are evaluated, consideration should be given to adjustment for multiple comparisons to control the overall type I error rate [46].
Case Studies in Prognostic Enrichment and Predictive Stratification
Oncology Applications
The development of trastuzumab for HER2-positive breast cancer represents a landmark example of successful predictive stratification [46]. The initial clinical trials used an enrichment design, enrolling only patients with HER2-positive breast cancer [46]. This approach efficiently demonstrated significant improvement in disease-free survival with trastuzumab combined with chemotherapy [46]. However, subsequent analyses raised questions about whether a broader patient population might benefit, highlighting a limitation of enrichment designs when biomarker biology is incompletely understood [46].
The validation of KRAS mutation status as a predictive biomarker for anti-EGFR antibodies in colorectal cancer demonstrates the power of well-designed retrospective analysis [46]. Using archived specimens from previously conducted randomized controlled trials, researchers showed that patients with wild-type KRAS tumors benefited from panitumumab or cetuximab, while those with KRAS mutations derived no benefit [46]. This retrospective validation approach allowed rapid translation of this biomarker into clinical practice without requiring new prospective trials [46].
Non-Oncology Applications: Sepsis
The application of prognostic and predictive enrichment strategies extends beyond oncology to complex heterogeneous conditions like sepsis [47]. The PERSEVERE (Paediatric Sepsis Biomarker Risk Model) platform exemplifies prognostic enrichment, incorporating biomarkers including CCL3, IL-8, and granzyme B to stratify children with septic shock by mortality risk [47]. This model enables selection of high-risk patients who might derive the greatest benefit from novel therapies and provides a foundation for predictive enrichment by identifying biologically homogeneous subgroups [47].
Sepsis research has also utilized discovery-based approaches to identify predictive biomarkers. For example, a coding variant in the IL-1 receptor antagonist gene was associated with improved survival and faster shock resolution in the Vasopressin and Septic Shock Trial [47]. This variant was linked to higher IL-1 receptor antagonist levels, suggesting a potential predictive biomarker for therapies targeting this pathway [47]. These approaches demonstrate how prognostic and predictive stratification can be applied to non-malignant diseases with substantial biological heterogeneity.
Future Directions and Emerging Methodologies
The field of biomarker-driven clinical trials continues to evolve with several emerging trends. Multi-omics approaches that integrate genomic, proteomic, metabolomic, and transcriptomic data are expected to provide more comprehensive biomarker signatures that better reflect disease complexity [50] [25]. The rise of artificial intelligence and machine learning enables more sophisticated analysis of complex biomarker datasets, potentially identifying novel patterns and interactions not apparent through traditional statistical methods [50] [25].
Liquid biopsy technologies are advancing rapidly, with improvements in sensitivity and specificity for circulating tumor DNA analysis expected to make liquid biopsies a standard tool in clinical trials by 2025 [50]. These technologies facilitate real-time monitoring of biomarker changes and treatment response, enabling more dynamic adaptive trial designs [50]. Additionally, single-cell analysis technologies provide unprecedented resolution of tumor heterogeneity, potentially identifying rare cell populations that drive treatment resistance [50].
Regulatory science is also advancing to keep pace with these technological innovations. Regulatory agencies are developing more streamlined approval processes for biomarkers validated through large-scale studies and real-world evidence [50]. There is increasing emphasis on standardization initiatives to enhance reproducibility and reliability across studies [50]. These developments will support more efficient co-development of therapeutics and companion diagnostics, accelerating the implementation of precision medicine approaches across diverse disease areas.
In the pursuit of precision medicine, biomarkers have become indispensable tools for optimizing clinical trial design and therapeutic decision-making. Within this context, a critical distinction exists between two primary classes of biomarkers: prognostic and predictive. A prognostic biomarker provides information about the likely natural course of a patient's disease, irrespective of the specific therapy administered. It identifies patients at higher risk of experiencing a clinical event, enabling stratification based on disease aggressiveness or outcome probability [20]. In contrast, a predictive biomarker offers insights into the differential efficacy of a particular treatment, helping to identify patient subgroups more likely to benefit from a specific therapeutic intervention [10] [20]. Understanding this distinction is fundamental, as it directly influences how biomarkers are integrated into clinical trial design, ultimately shaping patient eligibility criteria, sample size requirements, and the interpretation of trial results.
The strategic use of these biomarkers has given rise to distinct enrichment strategies in clinical trials. Prognostic enrichment involves selectively enrolling patients at higher risk for a clinical endpoint into a trial. This approach increases the event rate in the study population, which can enhance statistical power and potentially reduce the required sample size [51] [52]. A classic example is the CONSENSUS trial for enalapril, which enrolled only very high-risk heart failure patients (with a 6-month mortality of 44%) and demonstrated efficacy with only 253 participants [52] [53]. Conversely, predictive enrichment focuses on selecting patients based on their anticipated response to a specific treatment, as seen in oncology trials where therapies are often targeted to tumors expressing specific proteins like HER2 or PD-L1 [51] [10]. This guide focuses primarily on tools for prognostic enrichment, a strategy that, while well-established in cardiology and nephrology, has received less methodological attention than predictive biomarkers until recently [51] [52].
The Biomarker Prognostic Enrichment Tool (BioPET) Framework
BioPET for Binary Outcomes
The Biomarker Prognostic Enrichment Tool (BioPET) represents a significant methodological advancement for planning clinical trials with binary endpoints. Developed to address the gap in quantitative methods for evaluating prognostic enrichment biomarkers, BioPET provides a structured framework to assess whether a biomarker can improve trial efficiency without presuming it predicts treatment response [51].
The methodology requires investigators to specify several key parameters: the event rate in the non-intervention group without enrichment, the treatment effect size the trial should be powered to detect, statistical testing parameters (α-level, power, one-sided or two-sided testing), and the prognostic capacity of the biomarker summarized by the area under the ROC curve (AUC) and the shape of the curve [51]. BioPET then calculates three crucial efficiency metrics across varying enrichment levels (i.e., different biomarker thresholds for trial eligibility): (1) Clinical trial sample size - which typically decreases with more stringent enrichment as higher-risk populations have more events; (2) Calendar time to enroll the trial - which depends on both the sample size and the proportion of patients who meet the enrichment threshold; and (3) Total trial costs - incorporating both per-patient trial costs and biomarker screening costs [51].
A key insight from the BioPET methodology is that even modestly prognostic biomarkers can meaningfully improve trial efficiency when strategically implemented. The tool is available as both an R package and a user-friendly webtool (http://prognosticenrichment.com), making this methodology accessible to clinical investigators [51] [54].
BioPETsurv for Time-to-Event Outcomes
BioPETsurv extends the BioPET framework to accommodate time-to-event endpoints, such as overall survival or progression-free survival, which are common in oncology and other medical specialties. This extension is methodologically significant because time-to-event analyses incorporate more information from the data, including censored observations, and require different statistical approaches [52] [53].
The software supports two common trial designs: fixed-duration trials, where all participants have the same observation period, and accrual plus follow-up designs, where participants are enrolled over an accrual period and then followed for an additional fixed period [52]. For a fixed-duration trial, the number of required events is calculated using the formula N0 = 4(z₁₋α/₂ + z₁₋β)² / log²(HR), where HR is the treatment hazard ratio. The total sample size N is then derived as N = 2N0 / (p̂C + p̂T), where p̂C and p̂T are the estimated event rates in the control and treatment arms, respectively, based on the survival function estimates in the enriched population [52].
For the accrual plus follow-up design, BioPETsurv uses Simpson's rule to estimate event rates, accounting for varying follow-up times: p̂C = 1 - ⅙[Ŝ(f) + 4Ŝ(f + 0.5a) + Ŝ(f + a)], where a is the accrual time and f is the follow-up time [52]. Like its predecessor, BioPETsurv is available as an R package and through a webtool, enabling investigators to explore enrichment strategies for survival outcomes using their own data or simulated datasets matching their clinical context [52] [54] [53].
Table 1: Comparison of BioPET and BioPETsurv Tools
| Feature | BioPET | BioPETsurv |
|---|---|---|
| Endpoint Type | Binary outcomes | Time-to-event outcomes |
| Supported Designs | Single assessment | Fixed-duration; Accrual + follow-up |
| Key Inputs | Event rate, treatment effect, AUC | Hazard ratio, follow-up duration, AUC |
| Analysis Methods | ROC analysis | Kaplan-Meier, nearest neighbor estimation |
| Cost Modeling | Fixed per-patient costs | Time-dependent or fixed costs |
| Output Metrics | Sample size, screening numbers, costs | Sample size, screening numbers, costs |
| Availability | R package, webtool | R package, webtool |
Sample Size Considerations in Biomarker-Enabled Trials
Fundamental Principles and Formulas
Determining appropriate sample size is a critical aspect of clinical trial design that becomes more complex when incorporating biomarkers. For prognostically enriched trials, the sample size depends heavily on the event rate in the enriched population, which is influenced by both the prognostic strength of the biomarker and the chosen enrichment threshold [51] [52].
For trials with time-to-event endpoints, the number of events needed can be calculated using the formula: N0 = 4(z₁₋α/₂ + z₁₋β)² / log²(HR), where z₁₋α/₂ and z₁₋β are quantiles of the standard normal distribution corresponding to the type I error and power, and HR is the target hazard ratio [52]. The total sample size required is then determined by the expected event rates in the enriched population. This relationship means that as prognostic enrichment increases the event rate, the required sample size decreases correspondingly [51].
For predictive biomarker evaluation in treatment selection contexts, sample size determination may focus on different parameters. One approach targets a precision-based criterion, such as estimating a confidence interval for Θ (the expected benefit of biomarker-guided therapy) with a specified width [55]. This method uses Monte Carlo simulation and regression (the "SWIRL" procedure) to determine the sample size needed to achieve the desired precision in estimating the improvement in survival probability under optimal biomarker-guided treatment compared to a standard approach [55].
Sample Size Estimation for Predictive Models
When developing clinical prediction models that incorporate biomarkers, sample size estimation must account for the number of predictor variables and the expected model performance. Traditional "rules of thumb," such as requiring 10 events per predictor variable (EPP), have been widely used but are increasingly questioned for their context-insensitive nature [56].
More sophisticated approaches, such as Riley's method, consider multiple factors including the disease prevalence, number of predictor variables, and expected model fit (as measured by R² values) [56]. This method performs multiple calculations to ensure the model meets four criteria: precise estimation of overall risk, precise estimation of predictor effects, accurate estimation of the model's residual variance, and minimizing overfitting. The largest sample size from these four calculations is selected to ensure robust model development [56].
For model validation, a minimum of 100 events is often recommended to ensure reliable performance assessment [56]. These sample size considerations are particularly relevant for complex biomarker signatures that combine multiple variables, such as radiomic features or genomic expression profiles, where the risk of overfitting is substantial without adequate sample sizes.
Table 2: Sample Size Guidance for Different Biomarker Trial Contexts
| Trial Context | Key Determining Factors | Common Approaches | Considerations |
|---|---|---|---|
| Prognostic Enrichment | Event rate in enriched population, treatment effect size | Event-based calculation | Trade-off between higher event rate and increased screening |
| Predictive Biomarker Evaluation | Expected benefit of biomarker-guided therapy, desired precision | Monte Carlo simulation (SWIRL) | Accounts for qualitative treatment-biomarker interactions |
| Prediction Model Development | Number of predictors, outcome prevalence, expected model fit | Riley's method, EPP rules | More flexible than fixed EPP rules; addresses multiple objectives |
| Model Validation | Required precision for performance metrics | Minimum 100 events | Ensures reliable estimate of model performance in new data |
Experimental Protocols and Applications
Protocol for Evaluating a Prognostic Enrichment Biomarker
The evaluation of a candidate prognostic enrichment biomarker follows a systematic protocol. First, researchers must specify the clinical context, including the expected event rate in the unenriched population and the clinical meaningfulness of the endpoint [51]. Next, they define the statistical parameters for the trial: type I error rate (α), power (1-β), and the target treatment effect size (e.g., relative risk reduction or hazard ratio) [51] [52].
The biomarker performance characteristics must then be quantified, typically using the AUC, with values of 0.7, 0.8, and 0.9 representing modest, good, and excellent prognostic performance, respectively [51]. If preliminary biomarker data are available, BioPET or BioPETsurv can analyze them directly; otherwise, the tools can simulate data matching the specified parameters [52] [53].
The core analysis involves varying the enrichment threshold (the percentile cut-point of the biomarker distribution above which patients are eligible) and calculating how trial efficiency metrics change. Investigators examine how sample size, number needed to screen, and total costs vary across different threshold levels [51] [52]. Finally, optimal threshold selection involves balancing these quantitative metrics with qualitative considerations about trial feasibility, generalizability, and ethical implications of excluding lower-risk patients [51].
Case Study Applications
The practical utility of prognostic enrichment is illustrated by several real-world applications. In autosomal dominant polycystic kidney disease (ADPKD), Total Kidney Volume (TKV) was qualified by the FDA as a prognostic biomarker for clinical trials. Without enrichment, 13 patients needed screening to enroll 11 patients and observe one event. Using TKV for prognostic enrichment, 25 patients needed screening to enroll 9 patients and observe one event—a favorable trade-off that made the trial feasible despite increased screening [52].
In the PRIORITY trial for patients with type 2 diabetes, prognostic enrichment identified patients at high risk for developing confirmed microalbuminuria. The event rate was 28% in the high-risk group versus only 9% in low-risk patients. Without this enrichment strategy, the sample size would have needed to be 3-4 times larger, exposing many more patients to a therapy with potential side effects [52].
In oncology, the UK NCRI RAPID trial incorporated gene expression biomarkers (CD22, BID, IL15RA) alongside interim PET imaging to enhance prediction of event-free survival in classical Hodgkin lymphoma. The combined model demonstrated independent predictive value beyond traditional clinical risk scores, showing the potential for biomarkers to refine prognostic stratification in cancer trials [57].
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools
| Reagent/Tool | Function | Application Context |
|---|---|---|
| BioPET R Package | Evaluates biomarkers for prognostic enrichment | Clinical trials with binary endpoints |
| BioPETsurv R Package | Extends BioPET functionality to survival outcomes | Trials with time-to-event endpoints |
| BioPET Webtools | User-friendly interface for enrichment analysis | Exploratory analysis without programming |
| pmsampsize R Package | Sample size calculation for prediction models | Development of clinical prediction models |
| Quantigene Plex Assay | Multiplex gene expression quantification | Biomarker discovery and validation [57] |
| Tumor Tissue Biobanks | Source of biomaterial for biomarker studies | Retrospective biomarker evaluation [57] |
Integrated Workflow for Biomarker Evaluation
The following diagram illustrates the key decision points and methodological approaches in the quantitative assessment of biomarkers for clinical trials:
The quantitative assessment of biomarkers for clinical trial design has been significantly advanced by methodological frameworks like BioPET and BioPETsurv. These tools enable researchers to systematically evaluate how prognostic biomarkers can optimize trial efficiency through enrichment strategies, providing concrete metrics on sample size, screening requirements, and costs across different enrichment thresholds [51] [52]. For predictive biomarker evaluation, specialized sample size methods address the distinct challenge of quantifying expected benefit from biomarker-guided treatment strategies [55].
Beyond the quantitative considerations, successful biomarker integration requires careful attention to broader implications. Ethical considerations may favor prognostic enrichment when treatments have significant toxicities, as it limits exposure to patients most likely to experience the outcomes the treatment aims to prevent [51]. Generalizability concerns necessitate planning for how trial results from an enriched population might extend to broader patient groups, potentially requiring subsequent trials in lower-risk populations if efficacy is demonstrated [51].
As precision medicine advances, the strategic use of both prognostic and predictive biomarkers will continue to transform clinical trial design. The tools and methodologies described in this guide provide a foundation for making evidence-based decisions about biomarker implementation, ultimately supporting more efficient and informative clinical development programs.
In the evolving landscape of precision medicine, the ability to accurately distinguish between predictive and prognostic biomarkers has become a cornerstone of effective therapeutic development. A prognostic biomarker provides information about a patient's likely disease outcome, such as recurrence or overall survival, irrespective of the treatment received. In contrast, a predictive biomarker offers insight into the likely benefit a patient will derive from a specific therapeutic intervention [58] [26]. This distinction is not merely academic; it carries significant clinical, financial, and ethical consequences. Misclassifying a predominantly prognostic biomarker as predictive may result in withholding a potentially beneficial treatment from patients who could benefit, while incorrectly labeling a predictive biomarker as prognostic may lead to uniform treatment application without regard for differential therapeutic effects across patient subpopulations [58].
The integration of genomics and proteomics through advanced artificial intelligence (AI) methodologies represents a transformative approach to biomarker discovery and validation. These multi-modal data integration strategies leverage complementary biological information: genomics provides a blueprint of potential disease risk, while proteomics reflects the dynamic functional expression of physiological and pathological processes [59] [60]. The convergence of these data modalities with AI creates unprecedented opportunities to unravel complex biomarker signatures that can accurately predict treatment responses and disease trajectories, ultimately enhancing drug development pipelines and clinical decision-making.
Methodological Framework: AI Approaches for Multi-Omics Integration
Deep Learning Architectures for Data Integration
The integration of genomics and proteomics data presents significant computational challenges due to high dimensionality, heterogeneity, and biological complexity. Deep learning approaches have emerged as powerful tools to address these challenges through several specialized architectures:
Non-generative Methods: These include feedforward neural networks (FNNs), graph convolutional neural networks (GCNs), and autoencoders, which learn mappings from input data to outcomes without explicitly modeling the underlying data distribution. For instance, MOLI employs a late integration approach using modality-specific encoding FNNs to learn features separately for each data type before concatenation for final prediction [61]. Autoencoders are particularly valuable for creating shared latent representations that capture complementary information across genomic and proteomic modalities.
Generative Methods: This category includes variational autoencoders, generative adversarial networks (GANs), and generative pretrained transformers (GPTs). These methods explicitly model the joint probability distribution of input data and labels, offering advantages such as the ability to handle missing data, impose biological constraints on learned representations, and generate synthetic samples for data augmentation [61].
Integration Strategies and Workflows
The workflow for multi-modal data integration typically follows one of three principal strategies, each with distinct advantages for specific research contexts, as visualized below:
Table 1: Comparison of Multi-Modal Data Integration Strategies
| Integration Strategy | Technical Approach | Advantages | Limitations | Best-Suited Applications |
|---|---|---|---|---|
| Early Integration | Concatenation of raw features from all modalities before model input | Simplicity of implementation; Captures cross-modal correlations at input level | Prone to overfitting with high-dimensional data; Amplifies curse of dimensionality | Small-scale datasets with low dimensionality; Preliminary exploratory analysis |
| Intermediate Integration | Learning shared representations through specialized architectures (e.g., autoencoders) | Balances modality-specific and cross-modal learning; Flexible representation learning | Complex model architecture; Computationally intensive | Most multi-omics applications; Handling missing data; Large-scale biomarker discovery |
| Late Integration | Training separate models per modality with subsequent prediction combination | Preserves modality-specific patterns; Enables parallel processing | May miss important cross-modal interactions; Requires separate validation per modality | Distinct data modalities with independent relevance; Ensemble modeling approaches |
Experimental Comparisons: Platform Performance and Analytical Validation
Proteomics Platform Performance Metrics
The selection of appropriate proteomic profiling platforms is critical for generating high-quality data for multi-modal integration. Recent large-scale comparisons between the two major high-throughput proteomics platforms—SomaScan and Olink—reveal important performance characteristics that directly impact biomarker discovery efforts, as summarized in the table below.
Table 2: Comparative Analysis of High-Throughput Proteomics Platforms [60]
| Performance Metric | SomaScan v4 Platform | Olink Explore 3072 Platform | Experimental Methodology | Implications for Biomarker Studies |
|---|---|---|---|---|
| Median Coefficient of Variation (Precision) | 9.9% (all assays)9.5% (shared proteins) | 16.5% (all assays)14.7% (shared proteins) | Calculated using duplicate measurements of 1,474 samples (UKB dataset for Olink) and 227 samples (Icelandic dataset for SomaScan) | SomaScan demonstrates superior technical precision, potentially offering more consistent measurements for longitudinal studies |
| Median Spearman Correlation (Platform Concordance) | 0.33 (with SMP normalization)0.39 (without SMP normalization) | Same correlation values observed with matching assays | Analysis of 1,514 Icelandic individuals with data from both platforms; 1,848 proteins with matching assays | Moderate correlation suggests platform-specific biases; caution needed when comparing studies using different platforms |
| Assays with cis-pQTL Support | 2,120 assays (43% of platform) | 2,101 assays (72% of platform) | Genome-wide association studies stratified by ancestry in UK Biobank (46,218 BI, 953 SA, 1,513 AF) and Icelandic (35,892) cohorts | Olink shows higher proportion of assays with genetic validation, potentially indicating better target specificity |
| Dilution Group Performance | Lowest correlation in low dilution group; CV higher in highest dilution group | Lowest correlation and highest CV in undiluted group (lowest abundance proteins) | Stratified analysis by dilution groups reflecting protein abundance in plasma | Both platforms struggle with low-abundance proteins; careful interpretation needed for biomarkers in these categories |
Methodologies for Biomarker Classification
Distinguishing between predictive and prognostic biomarkers requires specialized experimental designs and analytical approaches. The INFO+ framework represents a novel methodology that leverages information theory to quantitatively separate predictive from prognostic biomarker signals [58].
The experimental protocol for biomarker classification typically involves:
- Dataset Requirements: Randomized clinical trial data with treatment assignment indicators, candidate biomarker measurements, and clinical outcomes
- Information-Theoretic Formulation: Quantifying the joint effect of patient characteristics and treatment on outcome as the sum of prognostic effect and predictive effect: Joint effect = Prognostic effect + Predictive effect
- Computational Implementation: Using mutual information and conditional mutual information to measure biomarker-outcome associations under different treatment conditions
- Validation: Resampling techniques and comparison with established methods like Virtual Twins, SIDES, and Interaction Trees
This approach enables ranking biomarkers by their predictive strength (measured in bits of information) while accounting for potential synergistic effects of multiple biomarkers through higher-order interaction detection [58].
Clinical Applications: Biomarker Utility in Oncology
The integration of genomic and proteomic data has yielded significant advances in cancer biomarker development, with important implications for both predictive and prognostic assessment.
Table 3: Clinically Validated Biomarkers in Oncology [10] [26]
| Biomarker | Cancer Type | Biomarker Type | Clinical Utility | Evidence Level |
|---|---|---|---|---|
| PD-L1 Expression | Non-small cell lung cancer (NSCLC) | Predictive | Identifies patients likely to respond to PD-1/PD-L1 inhibitors; KEYNOTE-024 showed median OS of 30 months vs 14.2 months with chemotherapy (HR: 0.63) in PD-L1 ≥50% patients | Level I evidence from prospective randomized trials |
| MSI-H/dMMR | Multiple cancers (tissue-agnostic) | Predictive | FDA-approved for pembrolizumab with 39.6% overall response rate and durable responses in 78% of cases; reflects defects in DNA repair pathways | Level I evidence from multiple cohort studies |
| HER2/neu Amplification | Breast cancer | Both prognostic and predictive | Prognostic: indicates more aggressive disease in node-positive patients; Predictive: guides HER2-targeted therapies (trastuzumab) reducing recurrence by ~50% | Level II evidence for prognostic value; Level I for predictive utility |
| Tumor Mutational Burden (TMB) | Multiple solid tumors | Predictive | ≥10 mutations/Mb associated with 29% ORR vs 6% in low-TMB tumors (KEYNOTE-158); ≥20 mutations/Mb associated with improved survival (HR: 0.52) | Level II evidence from basket trials and retrospective analyses |
| Lactate Dehydrogenase (LDH) | Melanoma | Prognostic | Included in AJCC staging; elevated levels correlate with poor prognosis but do not predict response to specific therapies | Level II evidence from multivariate analyses |
Implementation Challenges and Technical Considerations
Analytical Validation and Translational Gaps
Despite promising technological advances, significant challenges remain in translating multi-modal biomarker signatures from discovery to clinical application. The translational gap between preclinical promise and clinical utility represents a major roadblock, with less than 1% of published cancer biomarkers ultimately entering clinical practice [62].
Key challenges include:
- Model Biological Relevance: Traditional animal models often demonstrate poor correlation with human disease biology, limiting their predictive value for biomarker validation
- Analytical Standardization: Lack of robust validation frameworks and standardized protocols across laboratories, resulting in irreproducible findings
- Tumor Heterogeneity: Controlled preclinical conditions fail to fully capture the genetic diversity and evolving nature of human tumors, including variations in tumor microenvironments
- Platform Discrepancies: As highlighted in Table 2, different proteomic platforms show only moderate correlation, complicating cross-study comparisons and meta-analyses
Integration of Functional Assays and Longitudinal Sampling
Advanced validation strategies are emerging to address these translational challenges:
- Longitudinal Sampling: Repeated biomarker measurements over time provide dynamic assessment of disease progression and treatment response, offering more robust information than single time-point measurements [62]
- Functional Validation: Moving beyond correlative associations to demonstrate biological relevance through functional assays that confirm a biomarker's role in disease processes or therapeutic mechanisms [62]
- Multi-Omic Cross-Species Integration: Approaches such as cross-species transcriptomic analysis integrate data from multiple models to provide more comprehensive biomarker validation [62]
Table 4: Research Reagent Solutions for Multi-Modal Biomarker Studies
| Research Tool | Function | Application Context | Considerations for Implementation |
|---|---|---|---|
| Olink Explore 3072 | High-throughput proteomics using proximity extension assay technology | Simultaneous measurement of 2,941 proteins with minimal sample volume; ideal for large cohort studies | Higher CV than SomaScan but greater proportion of assays with cis-pQTL support; uses dual antibody recognition for potentially better specificity |
| SomaScan v4 | Aptamer-based proteomic profiling platform | Measurement of 4,719 proteins via 4,907 assays; recommended SMP normalization affects inter-platform correlations | Superior precision metrics (lower CV) but smaller percentage of assays supported by genetic evidence; uses single aptamer per protein |
| Patient-Derived Xenografts (PDX) | In vivo models using human tumor tissues implanted in immunodeficient mice | Biomarker validation in context that better recapitulates human tumor biology; used successfully for HER2 and BRAF biomarkers | More accurate than cell line-based models for therapy response prediction; retains tumor heterogeneity and characteristics |
| Organoids and 3D Co-culture Systems | 3D structures recapitulating organ or tissue identity | Prediction of therapeutic responses and identification of diagnostic biomarkers; retains biomarker expression better than 2D models | Incorporates multiple cell types (immune, stromal, endothelial) for comprehensive microenvironment modeling |
| INFO+ Computational Framework | Information-theoretic biomarker classification | R-based tool for distinguishing predictive versus prognostic biomarker strength; handles higher-order interactions | Available via GitHub; outperforms complex methods in noisy data scenarios; enables quantitative ranking of biomarker utility |
The integration of genomics, proteomics, and artificial intelligence represents a paradigm shift in biomarker discovery and validation. The distinction between predictive and prognostic biomarkers remains clinically essential, guiding therapeutic decisions and clinical trial design. As multi-modal data integration methodologies continue to evolve, emphasis must be placed on robust analytical validation, standardization across platforms, and demonstration of clinical utility. The future of biomarker development lies in effectively leveraging complementary data modalities through sophisticated AI approaches that can capture the complex, non-linear relationships between molecular signatures and clinical outcomes, ultimately advancing the goals of precision medicine and personalized therapeutic strategies.
In the evolving landscape of precision medicine, the distinction between predictive and prognostic biomarkers is fundamental to optimizing patient care and guiding therapeutic development. A prognostic biomarker provides information on the likely course of a disease in an untreated individual, identifying patients with a higher risk of disease recurrence or progression [6]. In contrast, a predictive biomarker identifies individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a specific medical product [6]. Some biomarkers can be both prognostic and predictive. This distinction is critical for clinical trial design and treatment decisions, as it enables drug developers to target the right patient populations and maximize therapeutic benefit [63].
Concurrently, Real-World Evidence (RWE) derived from real-world data (RWD) such as electronic health records (EHRs), and patient registries has emerged as a powerful tool to complement findings from traditional Randomized Controlled Trials (RCTs) [64]. RWE is particularly valuable for understanding a treatment's effectiveness (performance in routine clinical practice) versus its efficacy (performance under ideal conditions), studying patient populations typically excluded from RCTs, and generating insights in areas where conducting traditional trials is challenging [65] [64]. This article explores the convergence of these two fields through comparative case studies across major disease areas, highlighting how RWE is being used to assess and validate the clinical utility of biomarkers in real-world settings.
Biomarker Fundamentals: Prognostic vs. Predictive
Conceptual Framework and Definitions
The FDA-NIH Biomarker Working Group's BEST (Biomarkers, EndpointS, and other Tools) Resource provides formal definitions that are central to modern drug development [6] [63].
- Prognostic Biomarkers are used to identify the likelihood of a clinical event, disease recurrence, or progression in patients who have the disease or medical condition of interest. They inform about the natural history of the disease irrespective of treatment [6].
- Predictive Biomarkers are used to identify individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a medical product or an environmental agent. They help select patients for specific therapies [6].
Table 1: Key Categories of Biomarkers in Drug Development [63]
| Biomarker Category | Primary Use in Drug Development | Example |
|---|---|---|
| Susceptibility/Risk | Identify individuals with an increased risk of developing a disease | BRCA1/2 mutations for breast/ovarian cancer |
| Diagnostic | Accurately detect or confirm the presence of a disease | Hemoglobin A1c for diabetes mellitus |
| Monitoring | Monitor disease status or response to a therapy | HCV RNA viral load for Hepatitis C infection |
| Prognostic | Identify patients with higher-risk disease to enhance trial efficiency | Total kidney volume for polycystic kidney disease |
| Predictive | Predict response to a specific therapy | EGFR mutation status in non-small cell lung cancer |
| Pharmacodynamic/Response | Show that a biological response has occurred in a patient who has received a therapeutic intervention | HIV RNA (viral load) in HIV treatment |
| Safety | Monitor the potential for organ damage or adverse effects during treatment | Serum creatinine for acute kidney injury |
Statistical and Clinical Distinctions
Distinguishing between prognostic and predictive biomarkers requires careful study design. A biomarker's status as predictive can generally only be established by comparing a treatment to a control in patients with and without the biomarker [6]. The following diagram illustrates the key statistical interactions that differentiate a purely prognostic biomarker from a predictive one.
Diagram 1: Biomarker Clinical Utility Decision Framework. This workflow outlines the analytical pathway for determining whether a biomarker is prognostic, predictive, or both. A purely prognostic biomarker shows consistent outcome differences between positive and negative groups across different treatments. A predictive biomarker demonstrates a qualitative interaction, where the treatment effect differs significantly based on biomarker status [6].
Case Studies in Oncology
Oncology remains at the forefront of biomarker-driven drug development, with RWE playing an increasingly critical role in validating biomarkers and understanding their performance in heterogeneous real-world populations.
Case Study: Mantle Cell Lymphoma (Prognostic Biomarker & Drug Approval)
Background & Unmet Need: Following initial treatment with a covalent BTK inhibitor (cBTKi), there was little guidance on appropriate patient care for Mantle Cell Lymphoma (MCL), creating a significant unmet need [65].
Experimental Protocol & RWE Methodology:
- Data Source: A retrospective study used de-identified Electronic Health Record (EHR)-derived data from Flatiron Health [65].
- Patient Cohort: 1,150 eligible patients who had received a cBTKi treatment. The cohort's demographic makeup and care sites (77% community practices) were consistent with the typical MCL population [65].
- Outcomes Measured: Duration of therapy, time to next treatment (TTNT), and overall survival (OS) were analyzed [65].
- Statistical Analysis: Real-world outcomes were quantified to demonstrate the prognosis of this patient population post-cBTKi [65].
Key Findings & Clinical Utility: The study revealed considerable heterogeneity in treatments immediately following cBTKi therapy. The median TTNT was 3.0 months, and the median OS from the start of the next therapy was only 13.2 months [65]. These poor outcomes quantified a significant unmet need and served as a prognostic benchmark. This RWE was subsequently submitted to the FDA and successfully supported the accelerated approval of pirtobrutinib for patients with relapsed/refractory MCL after two lines of therapy, including a cBTKi [65].
Case Study: Ovarian Cancer (Predictive Biomarker & Comparative Effectiveness)
Background & Unmet Need: The NOVA Phase 3 clinical trial established the efficacy of niraparib, a PARP inhibitor, as a maintenance therapy for recurrent ovarian cancer. However, its performance in broader, more diverse real-world populations, particularly regarding overall survival (OS), needed further investigation [65].
Experimental Protocol & RWE Methodology:
- Study Design: A comparative effectiveness study analyzing real-world OS [65].
- Data Source: Flatiron Health RWD was used to identify 1,172 eligible patients with BRCA wild-type (wt) recurrent ovarian cancer [65].
- Cohorts: Patients treated with second-line maintenance niraparib monotherapy were compared to those under active surveillance. A subgroup analysis created a "NOVA study-like" cohort with characteristics similar to the clinical trial population [65].
- Methodology: Robust statistical methods were employed to minimize potential differences in patient characteristics between the groups (e.g., propensity score matching or adjustment) [65].
Key Findings & Clinical Utility: The analysis demonstrated a statistically significant survival benefit for niraparib compared to active surveillance.
Table 2: Real-World Overall Survival with Niraparib in BRCAwt Ovarian Cancer [65]
| Patient Cohort | Treatment Arm | Median Real-World Overall Survival (Months) |
|---|---|---|
| Overall Cohort | Niraparib | 24.1 |
| Active Surveillance | 18.4 | |
| NOVA Study-like Cohort | Niraparib | 28.1 |
| Active Surveillance | 21.5 |
The results confirmed the predictive value of the clinical context (platinum-sensitive recurrence) for benefit from niraparib in a real-world setting and complemented the initial trial data by providing evidence of effectiveness in a more demographically diverse population [65].
RWE Limitations in Oncology
While powerful, RWE analyses in oncology have inherent limitations. Patients treated in real-world practice often have a worse prognosis than clinical trial participants due to poorer performance status, more comorbidities, and older age [64]. For example, analyses of sorafenib in hepatocellular carcinoma and docetaxel in prostate cancer showed significantly shorter survival in real-world populations compared to RCTs [64]. This highlights that effectiveness in practice can be lower than efficacy in trials. Therefore, comparative RWE studies require sophisticated methodologies to control for confounding factors, and the absence of randomization remains a key limitation when estimating causal treatment benefits [64].
Case Studies in Cardiovascular Disease
Cardiovascular disease management heavily utilizes risk assessment tools, which often function as prognostic biomarkers, and RWE provides insights into their application and patient communication.
Case Study: QRISK2 vs. JBS3 Risk Calculators in NHS Health Checks
Background & Unmet Need: The UK's NHS Health Check programme uses risk calculators like QRISK2 (which provides a 10-year CVD risk percentage) and JBS3 (which incorporates additional features like "heart age" and risk manipulation) to communicate risk and motivate behavioral change [66].
Experimental Protocol & RWE Methodology:
- Study Design: A qualitative and quantitative study (the RICO study) analyzing audio-video recordings of health checks and conducting patient interviews [66].
- Data Source: Within-case analysis of 10 patients selected based on evidence of positive intentions/behaviors post-check, balanced across risk calculator groups [66].
- Methodology: In-depth case study analysis of patient-practitioner interactions, including consultation duration, communication style, and patient understanding [66].
Key Findings & Clinical Utility:
- Visual Aids & Manipulation: Features like JBS3's "heart age" and risk manipulation were powerful tools for patient engagement. One patient, "Abbie," found the visual heart age "an understandable way of presenting it" and immediately implemented dietary changes after seeing how modifying risk factors altered her results [66].
- Communication is Key: A common area for improvement was practitioners failing to check patient understanding. Patient "Barry" could not recall his 10-year risk score, stating, "I didn't remember it no, I don't understand it" [66]. In another case, a practitioner misunderstood and miscommunicated the "event-free survival age" metric, leading to patient confusion [66].
- Prognostic Utility: Both tools served as prognostic biomarkers, identifying patients at elevated risk. However, their effectiveness in motivating change was highly dependent on the practitioner's ability to communicate the information clearly and tailor the discussion to the individual patient [66].
Case Studies in Chronic Condition Management
The management of chronic diseases is being transformed by digital health technologies, which generate novel RWD and create new paradigms for predictive monitoring.
Case Study: Remote Monitoring and AI in Chronic Disease Management
Background & Unmet Need: Chronic diseases like diabetes, cardiac conditions, and COPD require continuous monitoring, which is often challenging due to geographical barriers, resource limitations, and the high cost of frequent hospital visits [67].
Experimental Protocol & RWE Methodology: Multiple real-world telemedicine implementations have been studied globally [67]:
- Remote Diabetes Monitoring (India): A mobile app-based system synced with smart glucose meters, allowing doctors to remotely track blood sugar levels [67].
- AI-Powered Cardiac Care (USA): AI-powered wearable heart monitors detected irregular rhythms and alerted doctors in real-time, supplemented by virtual consultations [67].
- Virtual COPD Management (Canada): A home-based program used smart inhalers connected to an app to track breathing patterns, with remote monitoring by pulmonologists and physiotherapists [67].
Key Findings & Clinical Utility: These digital tools function as monitoring and predictive biomarkers, identifying early signs of deterioration before they become critical.
Table 3: Real-World Outcomes of Telemedicine in Chronic Disease Management [67]
| Disease Area | Intervention | Key Real-World Outcome |
|---|---|---|
| Diabetes | Mobile app-based remote monitoring | 40% reduction in hospital visits |
| Cardiac Disease | AI-powered wearable heart monitors | 25% decrease in emergency heart-related admissions |
| COPD | Smart inhalers & virtual rehabilitation | 50% decrease in COPD-related hospital admissions |
The predictive capability of continuous data streams enables early intervention, preventing complications and hospitalizations. This demonstrates a shift from traditional, episodic care to a proactive, predictive model driven by RWD [67].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents, technologies, and methodologies essential for conducting RWE and biomarker studies as highlighted in the featured case studies.
Table 4: Essential Research Tools for RWE and Biomarker Studies
| Tool / Solution | Function / Application | Example Use Case in Case Studies |
|---|---|---|
| De-identified EHR-derived Datasets | Provides longitudinal, real-world patient data from routine clinical practice for outcomes research. | Flatiron Health data was used to study treatment patterns in MCL and ovarian cancer [65]. |
| Biomarker Assay Platforms | Analytically validated tests to measure specific biomarkers (e.g., NGS for mutations, IHC for protein expression). | Used to determine biomarker status (e.g., BRCAwt) for patient stratification in the ovarian cancer study [65]. |
| Statistical Analysis Software (e.g., R, SAS) | Performs advanced statistical analyses, including propensity score matching, survival analysis, and regression modeling, to mitigate confounding in RWE. | Employed robust methodologies to minimize differences in patient characteristics between niraparib and surveillance cohorts [65]. |
| Patient Risk Calculators (e.g., JBS3, QRISK2) | Software tools that integrate patient data to generate prognostic risk estimates (e.g., 10-year CVD risk, heart age). | Used in NHS Health Checks to communicate prognostic risk and motivate lifestyle changes [66]. |
| Digital Remote Monitoring Platforms | Collects real-time physiological data from patients in their home environment via connected devices (e.g., smart glucose meters, wearables). | Enabled remote monitoring of blood sugar, heart rhythms, and inhaler use in chronic disease management [67]. |
Integrated Workflow: From Data to Decision
The process of generating and applying RWE for biomarker validation involves a multi-stage workflow, integrating data from diverse real-world sources to inform clinical and regulatory decisions. The following diagram illustrates this complex pipeline.
Diagram 2: RWE and Biomarker Validation Workflow. This pipeline shows the transformation of raw data from sources like EHRs and wearables into actionable evidence. The process involves careful data curation, rigorous statistical analysis to characterize the biomarker and control for confounding, and culminates in evidence generation that supports regulatory and clinical decisions. This cycle is iterative, as new data from clinical application feeds back into the system, continuously refining the evidence base [65] [63] [64].
The integration of sophisticated biomarker classification and real-world evidence is fundamentally enhancing drug development and patient care across oncology, cardiovascular, and chronic diseases. The case studies presented demonstrate that:
- RWE is pivotal for contextualizing prognostic biomarkers, as seen in the MCL study, where it quantified an unmet need and directly supported a new drug's regulatory approval [65].
- RWE can validate the predictive utility of biomarkers in broader, more diverse populations, strengthening the evidence for therapies like niraparib in ovarian cancer beyond the controlled trial environment [65].
- The communication of prognostic risk, even with validated tools, is a critical determinant of clinical utility, requiring clear, visual, and patient-centered approaches to motivate behavioral change [66].
- Digital health technologies are creating new classes of dynamic, monitoring, and predictive biomarkers that enable proactive chronic disease management and demonstrate significant positive impact on real-world outcomes like hospital admissions [67].
As the field evolves, a fit-for-purpose approach to biomarker validation—tailoring the evidentiary requirements to the specific context of use—will be essential [63]. Furthermore, the strategic shift of biopharma companies toward using RWE earlier in the development lifecycle and the practical application of AI to analyze complex, multimodal data streams promise to further accelerate the delivery of precision medicines to the patients most likely to benefit [68].
Navigating Implementation Challenges: Barriers and Strategic Solutions
The journey of a biomarker from initial discovery to routine clinical practice is a complex and arduous process, marked by a significant translational gap. Despite remarkable advances in biomarker discovery, less than 1% of published cancer biomarkers actually enter clinical practice, creating substantial roadblocks in drug development and personalized medicine [62]. This guide systematically compares the performance of various biomarker translation strategies by examining critical barriers and the experimental data supporting potential solutions, framed within the crucial context of distinguishing predictive from prognostic biomarker clinical utility.
Predictive biomarkers identify individuals who are more likely to experience a favorable or unfavorable effect from a specific medical product, while prognostic biomarkers identify the likelihood of clinical events, disease recurrence, or progression in patients who already have the disease of interest [6]. This distinction is fundamental to clinical utility assessment, as it determines whether a biomarker can guide treatment selection or merely provides information about disease course independent of therapy. The differentiation requires comparison of treatment to control in patients with and without the biomarker, without which a biomarker's true predictive value cannot be established [6].
Comparative Analysis of Biomarker Translation Barriers and Solutions
Table 1: Critical Barriers in Biomarker Translation and Validated Solutions
| Translation Barrier | Experimental Evidence & Impact | Proven Solutions | Data Supporting Efficacy |
|---|---|---|---|
| Preclinical Model Limitations | Syngeneic mouse models show poor human clinical correlation; Only 1% of published cancer biomarkers enter clinical practice [62] | Patient-derived xenografts (PDX), organoids, 3D co-culture systems | KRAS mutant PDX models correctly predicted cetuximab resistance; Organoids retain characteristic biomarker expression better than 2D models [62] |
| Data Heterogeneity & Standardization | Inconsistent protocols cause result variability between labs; Multi-omics integration improves Alzheimer's diagnosis specificity by 32% [69] [25] | FAIR Data Principles, standardized governance protocols, multi-modal data fusion | NIH PhenX Toolkit provides standardized protocols; NIA Translational Geroscience Network develops shared outcome measures [70] |
| Clinical Validation Challenges | Disease heterogeneity in human populations vs. controlled preclinical conditions; Genetic diversity affects biomarker performance [62] | Longitudinal sampling, functional validation assays, cross-species transcriptomic analysis | Serial transcriptome profiling with cross-species integration identified novel neuroblastoma therapeutic targets [62] |
| Regulatory and Analytical Hurdles | Regulatory frameworks struggle with novel biomarkers; Lack of clear guidelines for data sharing across legal systems [70] | FDA Biomarker Qualification Program, EMA novel methodologies procedure, real-world evidence incorporation | FDA/EMA qualified 7 preclinical kidney toxicity biomarkers through Predictive Safety Testing Consortium [71] |
| Technical & Logistical Issues | Sample quality degradation during global shipping; Need for fresh biosamples increases complexity [72] | Sample stabilization technologies, integrated logistics solutions, clear processing procedures | Investment in worldwide lab network and global infrastructure improves sample quality [72] |
Experimental Protocols for Biomarker Validation
Protocol for Predictive vs. Prognostic Biomarker Differentiation
Objective: To experimentally distinguish predictive from prognostic biomarkers using clinical trial data.
Methodology:
- Study Design: Randomized controlled trial comparing experimental therapy to standard therapy
- Patient Population: Patients with the disease of interest, stratified by biomarker status (positive vs. negative)
- Data Collection:
- Collect biomarker measurements at baseline
- Record clinical outcomes (e.g., survival, disease progression) for all treatment groups
- Ensure balanced follow-up across all subgroups
- Statistical Analysis:
- Generate survival curves for all four combinations: biomarker-positive/negative patients receiving experimental/standard therapy
- Test for treatment-by-biomarker interaction using appropriate statistical methods
- For qualitative interactions (ideal predictive biomarkers), experimental treatment should benefit one biomarker subgroup while showing lack of benefit or harm in the other [6]
Interpretation: A biomarker is considered predictive if there is a significant interaction between treatment and biomarker status on clinical outcomes. A biomarker is prognostic if it shows consistent outcome associations across treatment groups but does not modify treatment effect [6].
Protocol for Longitudinal Biomarker Validation
Objective: To capture temporal biomarker dynamics for enhanced clinical predictability.
Methodology:
- Sample Collection: Repeated biomarker measurements over time rather than single time-point assessments
- Time Points: Baseline, during treatment, at suspected disease progression, and post-treatment
- Sample Processing: Standardized collection, processing, and storage protocols across all sites
- Analysis Platform: Multi-omics integration (genomics, transcriptomics, proteomics) to identify context-specific biomarkers
- Functional Assays: Complement quantitative measurements with biological activity assessments
Data Interpretation: Pattern analysis of biomarker trajectories rather than absolute values at single time points; correlation with clinical outcomes to establish predictive validity [62].
Visualization of Biomarker Translation Pathways
Diagram 1: Biomarker translation pathway showing key stages and critical barriers
Visualization of Predictive vs. Prognostic Biomarker Differentiation
Diagram 2: Experimental differentiation between predictive and prognostic biomarkers
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagent Solutions for Biomarker Translation
| Research Tool | Function in Biomarker Translation | Experimental Application | Performance Data |
|---|---|---|---|
| Patient-Derived Xenografts (PDX) | Maintain tumor heterogeneity and molecular characteristics of original tumors | Predictive biomarker validation; Drug response profiling | More accurate than cell line-based models; Crucial for HER2 and BRAF biomarker investigation [62] |
| Organoids & 3D Co-culture Systems | Recapitulate human tissue architecture and cell-cell interactions | Biomarker-informed patient selection; Therapeutic response prediction | Retain characteristic biomarker expression better than 2D models; Identify chromatin biomarkers for treatment resistance [62] |
| Liquid Biopsy Platforms | Non-invasive serial monitoring of biomarker dynamics | Real-time treatment response assessment; Early disease detection | ctDNA and exosome profiling enable monitoring; Expanding beyond oncology to infectious diseases [50] |
| Multi-Omics Integration Platforms | Comprehensive molecular profiling across biological layers | Identification of complex biomarker signatures; Systems biology understanding | Improves early Alzheimer's disease diagnosis specificity by 32%; Identifies circulating diagnostic biomarkers in gastric cancer [69] [62] |
| AI/ML Analytical Tools | Pattern recognition in large, complex datasets | Predictive analytics; Automated data interpretation | AI-driven genomic profiling improves targeted therapy responses; Identifies patterns traditional methods miss [69] [62] |
| Single-Cell Analysis Technologies | Resolution of cellular heterogeneity within tissues | Rare cell population identification; Tumor microenvironment mapping | Reveals tumor heterogeneity; Identifies rare cells driving disease progression [50] |
The translation of biomarkers from discovery to clinical practice remains challenging, with success dependent on addressing multiple critical barriers simultaneously. The distinction between predictive and prognostic biomarkers is fundamental to clinical utility assessment and requires rigorous experimental designs that include appropriate control groups and test for treatment-by-biomarker interactions [6]. Current evidence indicates that strategies incorporating human-relevant models, longitudinal validation, multi-omics integration, and standardized data protocols demonstrate superior performance in overcoming translational hurdles.
Moving forward, the field requires enhanced collaboration between stakeholders, including researchers, clinicians, regulatory bodies, and patients. The adoption of FAIR data principles, development of more sophisticated model systems, and implementation of robust validation frameworks will be critical to improving the less than 1% success rate of biomarker translation [62] [70]. Furthermore, the increasing incorporation of real-world evidence and artificial intelligence methodologies promises to enhance the predictive validity and clinical utility of biomarkers across diverse patient populations, ultimately advancing the goal of precision medicine and improved patient outcomes.
Addressing Data Heterogeneity and Standardization Protocols
The efficacy of biomarker-driven precision medicine hinges on robust data analysis and standardized methodologies. Within clinical utility assessment, a fundamental distinction exists between prognostic and predictive biomarkers. Prognostic biomarkers provide information on the likely patient health outcome irrespective of the treatment administered, offering insights into the natural course of the disease. In contrast, predictive biomarkers indicate the likely benefit to the patient from a specific treatment compared to their condition at baseline, thereby guiding therapeutic selection [20]. Some biomarkers, such as HER2 overexpression in breast cancer, can serve both prognostic and predictive functions, highlighting the complexity of their clinical application [20]. The accurate interpretation of both biomarker types is critically dependent on overcoming significant challenges in data heterogeneity and implementing rigorous standardization protocols across the research and clinical continuum.
Comparative Analysis of Biomarker Types and Data Challenges
Table 1: Comparative Analysis of Prognostic versus Predictive Biomarkers
| Characteristic | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Core Definition | Indicates likely disease outcome regardless of therapy [20] | Predicts response to a specific therapeutic intervention [20] |
| Clinical Utility | Informs about disease aggressiveness, recurrence risk, and overall survival probability [20] | Guides treatment selection by identifying patients most likely to benefit from a particular drug [20] |
| Representative Examples | Cancer stage, tumor grade, HER2 overexpression (initially) [20] | Estrogen receptor in breast cancer, KRAS mutations in colorectal cancer, PD-L1 expression [20] |
| Primary Data Source | Tumor tissue, clinical records, traditional serum tests (e.g., β-HCG) [20] | Multi-omics platforms (genomics, proteomics), liquid biopsies (ctDNA), immunohistochemistry [25] [14] |
| Key Heterogeneity Challenges | Population variability in disease progression, sample timing inconsistencies [25] | Tumor heterogeneity, temporal evolution under treatment pressure, platform variability [25] [14] |
Table 2: Data Heterogeneity Challenges Across the Biomarker Development Workflow
| Development Stage | Sources of Heterogeneity | Impact on Clinical Utility |
|---|---|---|
| Sample Acquisition & Biobanking | Pre-analytical variables (ischemia time, fixation protocols), sample provenance differences [25] | Introduces analytical noise, reduces reproducibility, and compromises biomarker validity [25] |
| Analytical Platforms & Assays | Inconsistent standardization protocols across labs, reagent lot variations, different technology platforms [25] [50] | Limits model generalizability, creates interoperability barriers, and hinders multi-center validation [25] |
| Data Processing & Bioinformatics | Non-standardized computational pipelines, diverse genomic aligners, variant callers, and data normalization methods [25] | Impedes data fusion, causes inconsistent biomarker calls, and affects prognostic/predictive accuracy [25] [73] |
| Clinical Data Integration | Heterogeneous electronic health record systems, unstructured clinical notes, missing data patterns [25] | Restricts phenotypic correlation, complicates outcome analysis, and biases utility assessment [25] |
Experimental Protocols for Biomarker Validation
Multi-Omics Integration Workflow for Biomarker Discovery
The following protocol outlines a standardized approach for discovering and validating biomarkers using multi-omics data integration, designed to address heterogeneity challenges:
- Sample Collection and Preparation: Collect matched tissue and liquid biopsy samples (blood for ctDNA, serum for proteomics) from well-characterized patient cohorts. Use standardized SOPs for sample processing, including fixed ischemia times, uniform anticoagulants for blood, and controlled storage conditions to minimize pre-analytical variation [25] [14].
- Multi-Modal Data Generation:
- Perform whole genome/exome sequencing (tissue/ctDNA) to identify somatic mutations and copy number alterations [14].
- Conduct RNA sequencing (tissue) to define gene expression subtypes and fusion transcripts.
- Utilize high-throughput proteomics (mass spectrometry) or multiplex immunoassays (e.g., Olink) to quantify protein biomarker levels [25].
- Generate DNA methylation arrays (e.g., EPIC) to assess epigenetic regulation [25].
- Data Processing and Normalization: Process each data type through standardized, version-controlled bioinformatic pipelines. Employ batch effect correction algorithms (e.g., ComBat) to mitigate technical variation. Normalize data to appropriate reference standards for cross-platform comparability [25].
- Integrative Computational Analysis: Implement multi-omics factor analysis (MOFA) or similar tools to identify latent factors that explain variation across data layers. Train machine learning models (e.g., random forest, neural networks) on integrated features to build prognostic (overall survival) and predictive (treatment response) classifiers [25] [50].
- Independent Validation: Validate the final biomarker signature in a hold-out validation cohort or independent patient dataset, ensuring representation of diverse demographics and clinical characteristics to assess generalizability [25].
Liquid Biopsy Assay Validation for Predictive Biomarker Application
This protocol details the analytical and clinical validation of liquid biopsy-based predictive biomarkers, such as for monitoring therapy response:
- Pre-analytical Controls: Standardize blood collection tubes (e.g., Streck cfDNA), plasma processing protocols (centrifugation speed/time), and cfDNA extraction kits across all collection sites. Implement a QC system for cfDNA yield, fragmentation, and purity [50] [14].
- Assay Analytical Validation:
- Determine limit of detection (LOD) for variant allele fractions (VAFs) using synthetic controls or cell line-derived reference materials.
- Assess assay precision (repeatability/reproducibility) across multiple operators, instruments, and days.
- Establish linearity and quantitative accuracy for allele frequency quantification across the assay's dynamic range [50].
- Clinical Concordance Study: Perform a method comparison study against an established orthogonal method (e.g., tissue-based NGS) to determine positive/negative percent agreement for targetable alterations (e.g., EGFR T790M) [14].
- Longitudinal Monitoring Study: In patients receiving targeted therapy, serially collect plasma at baseline, early on-treatment (e.g., 2-4 weeks), and at progression. Measure ctDNA variant allele frequency of the drug target (predictive biomarker) and correlate with radiographic tumor response (RECIST criteria) and progression-free survival [20] [50].
Diagram 1: Biomarker discovery and validation workflow.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Biomarker Analysis
| Reagent / Solution | Primary Function | Application in Biomarker Studies |
|---|---|---|
| ctDNA Reference Standards | Provide standardized materials with known mutation VAFs for assay calibration and validation [50] | Enables analytical validation of liquid biopsy assays; ensures inter-laboratory reproducibility and accurate quantification of predictive biomarkers [50] [14] |
| Multiplex Immunoassay Panels | Simultaneously quantify dozens to hundreds of protein biomarkers from minimal sample volume [25] [14] | Facilitates high-throughput serum protein profiling for prognostic signature discovery and therapy response monitoring [25] |
| Single-Cell RNA-Seq Kits | Enable transcriptomic profiling at individual cell level to resolve tumor heterogeneity [50] | Identifies rare resistant cell populations and characterizes tumor microenvironment, informing both prognostic and predictive models [50] |
| Automated Nucleic Acid Extractors | Standardize and streamline DNA/RNA isolation from diverse sample types (tissue, blood) [25] | Reduces pre-analytical variability, a major source of data heterogeneity in multi-center biomarker studies [25] |
| Targeted NGS Panels | Focused sequencing of clinically relevant genes for efficient variant detection [14] | Supports routine clinical screening for predictive biomarkers (e.g., EGFR, KRAS, BRAF mutations) in solid tumors [20] [14] |
Standardization Frameworks and Visualizing the Solution
To systematically address data heterogeneity, an integrated framework prioritizing three pillars is essential: multi-modal data fusion, standardized governance protocols, and interpretability enhancement [25]. This framework systematically tackles implementation barriers from data acquisition to clinical adoption.
Diagram 2: Framework for data heterogeneity and standardization.
Ensuring Model Generalizability Across Diverse Populations
Model generalizability remains a critical challenge in translational biomarker research, directly impacting the clinical utility of predictive and prognostic biomarkers. Predictive biomarkers guide treatment selection by indicating likely response to specific therapies, whereas prognostic biomarkers provide information on overall disease outcomes irrespective of treatment [26] [20]. This distinction fundamentally influences generalizability requirements; predictive biomarkers must demonstrate consistent performance across diverse populations and treatment contexts, while prognostic biomarkers require stability across heterogeneous patient groups with varying baseline risks [58]. The limited generalizability of biomarker-driven models compromises their real-world clinical application, particularly for underrepresented populations who often experience different disease manifestations and treatment responses [74] [75].
The convergence of artificial intelligence with multi-omics technologies has intensified both the challenges and opportunities in achieving generalizability. While digital technology and artificial intelligence have revolutionized predictive models based on clinical data, creating opportunities for proactive health management, significant challenges persist in effectively integrating biomarker data and developing reliable predictive models that perform consistently across populations [25]. Contemporary detection platforms generate comprehensive molecular profiles including metabolomic, proteomic, and epigenetic features, offering unprecedented insights into disease mechanisms, yet these technological advances have not fully addressed the fundamental generalizability gap [25]. This comparison guide examines systematic approaches to enhance generalizability, providing researchers with methodological frameworks validated across diverse clinical contexts.
Comparative Analysis of Generalizability Strategies
Table 1: Strategic Approaches to Enhance Model Generalizability
| Strategy | Implementation Methodology | Performance Evidence | Key Limitations |
|---|---|---|---|
| Multi-Center Cohort Design | Recruitment across geographically diverse medical centers with standardized protocols [76] | RA metabolomic classifiers maintained AUC 0.734-0.928 across 3 regions [76] | High implementation costs and operational complexity |
| Machine Learning Risk Stratification | Gradient boosting models to stratify patients into prognostic phenotypes [75] | High-risk phenotypes showed significantly lower survival benefits vs. RCT results (HR: 1.21-2.38) [75] | Requires large, well-curated EHR datasets with complete follow-up |
| Demographic Benchmarking | Real-world data comparison to disease-specific demographic estimates [74] | Improved representativeness of trial populations for rheumatoid arthritis and stroke [74] | Limited to demographic variables without clinical or biomarker data |
| Feature Selection Optimization | Boruta algorithm with random forest-based wrapper method [77] | XGBoost achieved consistent training-testing performance (AUC 0.75 vs 0.72) in CVD-T2DM prediction [77] | Computational intensity with high-dimensional data |
Table 2: Quantitative Performance Across Validation Settings
| Model Context | Initial Performance | External Validation Performance | Performance Retention |
|---|---|---|---|
| RA Metabolite Classifier | AUC 0.928 (primary cohort) [76] | AUC 0.837-0.928 (3 geographic cohorts) [76] | 90-97% performance maintenance |
| Frailty Assessment (XGBoost) | AUC 0.963 (training) [78] | AUC 0.850 (external validation) [78] | 88% performance maintenance |
| CVD Risk in T2DM | AUC 0.75 (training) [77] | AUC 0.72 (testing) [77] | 96% performance maintenance |
| Oncology Trial Emulation | Variable by cancer type [75] | High-risk phenotypes showed 25-60% reduced treatment benefit [75] | Significant effect modification by risk stratum |
Experimental Protocols for Generalizability Assessment
Multi-Center Validation Framework
The metabolomic classifier development for rheumatoid arthritis (RA) diagnosis exemplifies a comprehensive generalizability assessment protocol [76]. This research employed a structured framework comprising seven cohorts (2,863 total samples) across three geographically distinct regions in China. The experimental workflow initiated with untargeted metabolomic profiling on an exploratory cohort (n=90) to identify candidate biomarkers, followed by targeted validation using absolute quantification with stable isotope-labeled internal standards. Machine learning classifiers were developed using six identified metabolites (imidazoleacetic acid, ergothioneine, N-acetyl-L-methionine, 2-keto-3-deoxy-D-gluconic acid, 1-methylnicotinamide, and dehydroepiandrosterone sulfate) and validated across five independent cohorts from different medical centers [76]. Critical methodological considerations included standardized sample collection (EDTA plasma processed promptly and stored at -80°C), consistent LC-MS/MS analysis across sites, and harmonized clinical data collection including anti-CCP, RF, CRP, and ESR. This protocol confirmed classifier independence from serological status, demonstrating particular value for seronegative RA diagnosis where conventional biomarkers fail [76].
Prognostic Phenotyping for Trial Generalizability Assessment
The TrialTranslator framework addresses oncology trial generalizability through machine learning-based prognostic phenotyping [75]. This method employs gradient boosting survival models (GBM) trained on real-world electronic health record data to stratify patients into low, medium, and high-risk phenotypes based on mortality risk scores. The implementation protocol first develops cancer-specific prognostic models optimized for predictive performance at clinically relevant timepoints (1-year survival for NSCLC, 2-year for other solid tumors). Model features include age, weight loss, ECOG performance status, cancer biomarkers, and serum markers of frailty such as albumin and hemoglobin. After identifying real-world patients meeting key trial eligibility criteria, the framework calculates mortality risk scores and stratifies patients into risk tertiles. Inverse probability of treatment weighting balances features between treatment arms within each phenotype, enabling comparison of treatment effects across risk groups [75]. This approach revealed that high-risk phenotypes (characterized by older age, ECOG>1, and adverse laboratory values) derive significantly reduced survival benefits from therapies compared to RCT populations, quantifying the generalizability gap across 11 landmark oncology trials [75].
Technical Implementation and Reagent Solutions
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for Generalizable Biomarker Development
| Reagent/Platform | Specific Function | Implementation Example |
|---|---|---|
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Quantitative metabolite profiling with high sensitivity and dynamic range [76] | Absolute quantification of RA diagnostic metabolites using stable isotope-labeled internal standards [76] |
| Stable Isotope-Labeled Internal Standards | Normalization for precise absolute quantification in targeted metabolomics [76] | Implementation in RA metabolomic classifier validation across multiple centers [76] |
| UHPLC Systems (e.g., Vanquish) | High-resolution separation of polar metabolites [76] | Separation with Waters ACQUITY BEH Amide column for metabolomic profiling [76] |
| Orbitrap Mass Spectrometers | High-mass-accuracy detection for untargeted metabolomics [76] | Identification of novel metabolite biomarkers in discovery phase [76] |
| Electronic Health Record (EHR) Systems | Real-world data extraction for prognostic model development [75] | Flatiron Health database analysis for oncology trial emulation [75] |
| Gradient Boosting Machines (GBM) | Prognostic risk prediction with complex clinical data [75] | Mortality risk stratification in TrialTranslator framework [75] |
Methodological Considerations for Enhanced Generalizability
The frailty assessment tool development exemplifies optimal feature selection methodology for generalizable models [78]. Researchers applied five complementary feature selection algorithms (LASSO regression, VSURF, Boruta, varSelRF, and Recursive Feature Elimination) to 75 potential variables, identifying a minimal set of eight clinically accessible parameters. This approach balanced predictive accuracy with implementation feasibility across diverse clinical settings [78]. Similarly, the cardiovascular risk prediction model for diabetic patients demonstrated the utility of the Boruta algorithm for identifying robust predictors in high-dimensional clinical data [77]. These methodologies address critical barriers to generalizability by minimizing domain-specific technical requirements while maintaining performance across heterogeneous populations.
Achieving robust model generalizability requires systematic approaches addressing population diversity, analytical standardization, and clinical context variability. The comparative evidence indicates that multi-center designs with standardized protocols, machine learning-based risk stratification, and rigorous feature selection optimize performance consistency across diverse populations. The distinction between predictive and prognostic biomarkers remains fundamental, as predictive biomarkers require demonstration of consistent treatment interaction effects across populations, while prognostic biomarkers demand stable performance across heterogeneous baseline risks [58] [26]. Researchers should prioritize prospective validation across geographically and demographically distinct populations, implement computational methods to quantify and address generalizability gaps, and balance model complexity with implementation feasibility across diverse clinical settings. These strategies collectively enhance the translational potential of biomarker-based models, supporting more equitable and effective healthcare applications across diverse patient populations.
Strategies for Cost Optimization and Resource-Limited Settings
In the pursuit of robust biomarker validation, research institutions and drug development professionals increasingly operate within constrained budgets that demand strategic financial management. The ability to distinguish between prognostic and predictive biomarkers represents not merely a scientific challenge but also a significant resource allocation problem. As the National Institutes of Health resource notes, this distinction requires specific comparison study designs that directly impact trial costs and research efficiency [6]. Within resource-limited settings, understanding these financial implications becomes as critical as the scientific methodology itself.
The complex landscape of biomarker development necessitates sophisticated cost optimization strategies similar to those employed in technology sectors, where organizations reportedly waste 27-32% of cloud budgets through inefficient practices [79]. Similarly, research institutions often allocate substantial resources to biomarker studies without clear financial governance, leading to redundant experiments, underutilized equipment, and inefficient reagent procurement. This guide examines proven cost optimization frameworks adapted for biomedical research settings, enabling teams to maintain scientific rigor while maximizing resource utilization.
Biomarker Clinical Utility Assessment: Core Concepts and Economic Impact
Defining Prognostic and Predictive Biomarkers
Understanding the fundamental distinction between prognostic and predictive biomarkers is essential for appropriate trial design and resource allocation in drug development. According to FDA-NIH Biomarker Working Group resources, a prognostic biomarker provides information about the natural history of the disease in untreated individuals or those receiving standard treatment, independently of any specific therapy [6]. In contrast, a predictive biomarker identifies individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a specific medical product or environmental agent [6] [20].
The clinical utility of these biomarkers differs significantly. Prognostic biomarkers help stratify patients based on disease aggressiveness or natural history, potentially sparing low-risk patients from unnecessary treatments [23]. Predictive biomarkers directly inform treatment selection by identifying patients likely to respond to specific therapeutics, thereby optimizing therapy and reducing exposure to ineffective treatments [20]. As Maurie Markman explains, "A prognostic factor has been evident since the first descriptions of cancer as a clinical entity," while predictive biomarkers represent a more recent advancement enabling personalized treatment approaches [20].
Financial Implications of Biomarker Misclassification
Incorrectly classifying biomarkers or implementing them without proper validation carries significant financial consequences for drug development:
Development Costs: Misguided clinical trials that fail to properly account for the prognostic/predictive distinction lead to failed trials and wasted resources, with Deloitte noting that poor contract management alone costs organizations nearly $2 trillion annually in global economic value [80].
Treatment Efficiency: Without validated predictive biomarkers, healthcare systems incur substantial costs from treating patients with ineffective drugs. Research indicates that diagnostics not reliably evaluated can detract from proper patient management and increase medical care costs [23].
Trial Design Efficiency: Proper biomarker classification enables more efficient trial designs, such as enrichment strategies where only biomarker-positive patients are enrolled, potentially reducing required sample sizes and development costs [6] [23].
Cost Optimization Framework for Biomarker Research
Adapting principles from IT and business cost optimization, biomedical research institutions can implement structured approaches to maximize resource utilization while maintaining scientific integrity.
Strategic Resource Allocation
The fundamental principle of strategic resource allocation involves directing resources toward investments with the highest potential scientific return, mirroring the approach Deloitte describes as "prioritizing long-term investments" rather than simple cost-cutting [81]. This requires:
Portfolio Rationalization: Systematically evaluating research projects to identify and terminate those with limited potential, focusing resources on promising biomarkers with clear clinical utility pathways [82].
Zero-Based Budgeting: Establishing a "minimum viable" spend and redirecting savings to invest in structural changes for a "strategic optimum" spend baseline, particularly relevant for core laboratory operations [82].
Dynamic Investment Planning: Implementing quarterly and monthly monitoring and decision-making rather than annual budget cycles alone, enabling rapid reallocation based on emerging data [82].
Operational Efficiency in Laboratory Research
Laboratory operations present multiple opportunities for cost optimization through process improvement and waste elimination:
Reagent Management: Consolidating vendor relationships for research reagents to leverage volume discounts while maintaining quality, potentially achieving 10-30% savings through strategic partnerships [80] [83].
Equipment Utilization: Implementing shared equipment facilities with scheduling systems to maximize usage of high-cost instrumentation, similar to the cloud resource optimization approaches that identify 15-25% of resources as idle [84].
Process Automation: Automating repetitive laboratory processes such as liquid handling, DNA extraction, and data processing to reduce manual errors and increase throughput, with 88% of IT decision-makers increasing investment in automation [80].
Table: Common Resource Waste Patterns in Research Laboratories
| Waste Category | Examples in Research Settings | Potential Impact |
|---|---|---|
| Unused Capacity | Idle sequencing instruments, underutilized core facilities | 15-25% of resources typically idle [84] |
| Redundant Services | Multiple vendors for similar reagents, overlapping software licenses | 30% waste typical in software spending [83] |
| Process Inefficiency | Manual data entry, non-standardized protocols | 20-35% savings potential through automation [79] |
| Suboptimal Procurement | Lack of volume discounts, emergency ordering | 10-20% savings through vendor consolidation [79] |
Cross-Functional Collaboration
Breaking down silos between research teams, core facilities, and administrative functions enables significant cost optimization opportunities:
Shared Knowledge Management: Creating systems for sharing optimized protocols, failed experiments, and reagent performance data to prevent redundant experimentation across teams [82].
Strategic Partnerships: Developing deeper relationships with fewer vendors and research partners rather than transactional relationships, enabling joint incentives and reward mechanisms [81] [82].
Demand Management: Rationalizing research requests across departments, prioritizing projects based on strategic alignment and potential impact rather than first-come-first-served approaches [82].
Experimental Design Considerations for Resource-Limited Settings
Well-designed experiments represent both a scientific and economic imperative in biomarker research, with careful planning significantly reducing required resources while maintaining statistical validity.
Biomarker Validation Methodologies
The validation of prognostic and predictive biomarkers requires distinct approaches with different resource implications:
Analytical Validation: Establishing that the biomarker test is accurate, reproducible, and robust regarding assay performance and tissue handling [23]. This foundation prevents wasted resources on clinically invalid assays.
Clinical Validation: Demonstrating that the test result correlates with clinical endpoints, which for predictive biomarkers generally requires comparison of treatment to control in patients with and without the biomarker [6] [23].
Clinical Utility Assessment: Proving that using the test results in improved patient outcomes, typically requiring prospective trials showing that test-guided therapy decisions yield better results than standard approaches [23].
Table: Key Differences in Validation Requirements for Biomarker Types
| Validation Aspect | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Minimum Evidence | Correlation with outcome in patients receiving standard care or no treatment [23] | Treatment-by-biomarker interaction in randomized trials [6] |
| Study Design | Can often be established retrospectively using archived specimens [23] | Generally requires prospective or retrospective analysis of randomized controlled trial [6] |
| Statistical Approach | Time-to-event analysis with stratification by marker status [23] | Test for interaction between treatment and marker status [6] |
| Resource Implications | Lower cost; can utilize existing datasets and biobanks | Higher cost; typically requires controlled trial data |
Efficient Trial Designs for Biomarker Development
Several trial designs optimize resources while rigorously evaluating biomarker utility:
Adaptive Enrichment Designs: Beginning with a broadly eligible population, then using interim analyses to restrict enrollment to biomarker-positive subgroups if initial data suggests differential benefit [23].
Hybrid Prognostic-Predictive Designs: Developing biomarkers that serve dual purposes, such as HER2 in breast cancer, which initially provided prognostic information and later guided targeted therapy selection [20].
Case-Control Designs Within Cohorts: Using nested case-control approaches within larger observational studies to reduce laboratory testing costs while maintaining statistical power [23].
The following diagram illustrates the strategic decision pathway for biomarker development in resource-constrained environments:
Research Reagent Solutions for Cost-Effective Biomarker Studies
Strategic selection and management of research reagents significantly impact both experimental quality and resource utilization in biomarker development.
Table: Essential Research Reagents and Cost Optimization Strategies
| Reagent Category | Primary Function | Cost Optimization Approaches |
|---|---|---|
| Antibodies | Protein detection and quantification via IHC, Western blot | Consolidate vendors for volume discounts; implement shared antibody banks; validate reusable aliquots |
| PCR Reagents | Gene expression analysis, mutation detection | Bulk purchasing of master mixes; implement reagent sharing systems; optimize reaction volumes |
| Sequencing Kits | Nucleic acid sequencing for genomic biomarkers | Coordinate runs to maximize capacity; evaluate different platform economics; utilize core facilities |
| Cell Culture Media | Maintaining cell lines for functional studies | Prepare in-house when feasible; implement media sharing protocols; optimize serum concentrations |
| ELISA Kits | Protein quantification in patient samples | Centralize procurement; batch testing; validate in-house alternatives for high-volume assays |
Effective cost optimization in biomarker research extends beyond specific techniques to encompass an organizational culture that values resource efficiency while maintaining scientific excellence. This requires embedding cost awareness into research planning, laboratory processes, and strategic decision-making. Institutions that successfully implement these approaches can achieve 20-30% savings in operational costs while accelerating biomarker development [79] [82].
The distinction between prognostic and predictive biomarkers continues to evolve, with some biomarkers serving both functions depending on clinical context. As Markman notes, "Although based on currently available data we should appropriately conclude a particular biomarker is a reasonable prognostic factor... it is possible future therapeutic developments and research efforts may clinically meaningfully alter this scenario" [20]. This dynamic landscape necessitates both scientific and financial flexibility, enabling research institutions to adapt quickly to new discoveries while responsibly managing limited resources.
By implementing structured cost optimization frameworks alongside rigorous scientific methodologies, research organizations can maximize their impact in advancing personalized medicine while operating sustainably within resource constraints.
The evolution of precision medicine hinges on the ability to accurately distinguish and validate biomarkers that can reliably predict treatment response or forecast disease course. The clinical utility of a biomarker is determined by its capacity to inform decisions that ultimately improve patient outcomes. Within this realm, a critical distinction exists between predictive and prognostic biomarkers [85]. A predictive biomarker identifies patients who are most likely to benefit from a specific therapeutic intervention. For example, HER2 overexpression predicts response to trastuzumab in breast cancer, and EGFR mutations predict response to tyrosine kinase inhibitors in lung cancer [85]. In contrast, a prognostic biomarker provides information about the likely natural history of the disease, including recurrence risk or overall disease aggressiveness, irrespective of a specific treatment. Examples include the Ki67 proliferation marker in breast cancer or the 21-gene Oncotype DX Recurrence Score, which helps assess the risk of cancer recurrence [85].
Accurately assessing the clinical utility of these biomarkers, particularly within complex modern datasets, presents significant challenges. The integration of multi-omics data, the heterogeneity of data sources, and the "black box" nature of advanced AI models create substantial barriers to clinical adoption and regulatory approval [86] [37]. This guide objectively compares an integrated framework, built on three core pillars—multi-modal data fusion, standardized governance protocols, and interpretability enhancement—against traditional and alternative contemporary approaches [86] [25]. We present supporting experimental data and detailed methodologies to provide researchers, scientists, and drug development professionals with a clear comparison of performance and implementation requirements.
Framework Performance Comparison
The following tables provide a quantitative and qualitative comparison of the integrated three-pillar framework against traditional and other modern approaches for biomarker discovery and validation.
Table 1: Comparative Analysis of Framework Performance in Biomarker Clinical Utility Assessment
| Evaluation Metric | Traditional Single-Omics Approach | AI-Driven Multi-Omics without Standardized Governance | Integrated Three-Pillar Framework (Data Fusion, Governance, Interpretability) |
|---|---|---|---|
| Early Disease Screening Accuracy | Moderate (e.g., 60-75% specificity for single markers) [85] | Improved (e.g., 5-15% increase over traditional) [85] | High (e.g., 32% improvement in early Alzheimer's diagnosis specificity) [25] |
| Patient Stratification for Clinical Trials | Limited to 1-2 biomarkers (e.g., PD-L1 IHC, EGFR mutation) | Good, but risk of bias from non-standardized data [37] | Superior; enables identification of clinically actionable subgroups missed by single-omics [87] |
| Treatment Response Prediction (Predictive Biomarker Power) | Variable; high for some targets (e.g., HER2), low for others (e.g., immunotherapy) | Good for complex patterns, but limited trust from clinicians [37] | High; 15% improvement in survival risk stratification in Phase 3 trials [85] |
| Model Generalizability Across Populations | Poor to moderate, often population-specific | Often limited due to data heterogeneity and batch effects [86] | Enhanced through standardized governance and diverse data protocols [86] |
| Clinical Translation & Adoption Speed | Slow, years to decades for novel markers | Slow, hindered by regulatory and trust barriers [37] | Accelerated via interpretable results and IVDR/regulatory-ready frameworks [87] [50] |
Table 2: Comparison of Implementation Requirements and Experimental Outcomes
| Aspect | Traditional Single-Omics Approach | AI-Driven Multi-Omics without Standardized Governance | Integrated Three-Pillar Framework |
|---|---|---|---|
| Key Experimental Workflow | Hypothesis-driven; targeted assays (e.g., PCR, IHC) | Data-driven discovery on multi-omics datasets (RNA-Seq, Proteomics) | End-to-end pipeline from fused data ingestion to validated, interpretable models [85] |
| Data Integration Capability | Low (single data modality) | High, but often results in "data spaghetti" | Systematic multi-modal data fusion [86] [25] |
| Governance & Standardization | Lab-specific SOPs | Ad-hoc or minimal data management | Full standardized governance protocols (e.g., based on DMBOK, ISO/IEC 38505) [86] [88] |
| Model Interpretability | Inherently high (simple models) | Low ("black box" models) | High; uses Explainable AI (XAI) for transparent, clinician-trustworthy results [85] |
| Infrastructure & Cost | Lower initial cost, high long-term marginal cost | Very high compute and data storage cost | High initial setup, lower long-term cost due to efficiency and reduced trial failure [86] |
Detailed Experimental Protocols and Methodologies
Protocol for Multi-Modal Data Fusion in Predictive Biomarker Discovery
This protocol is designed to identify composite biomarker signatures from diverse data sources, enhancing the discovery of both predictive and prognostic biomarkers.
1. Data Ingestion and Collection:
- Multi-omics Data: Collect paired samples for Whole Genome Sequencing (WGS), bulk and single-cell RNA-Seq, proteomics (e.g., mass spectrometry), and metabolomics. For retrospective studies, leverage large-scale biobanks [85].
- Clinical and Real-World Data (RWD): Integate structured Electronic Health Record (EHR) data (e.g., treatments, lab values) and unstructured clinical notes. Link with real-world evidence from cancer registries and outcome databases [37].
- Digital Pathology & Radiomics: Digitize histopathology slides at 40x magnification. Extract quantitative features (morphological, topological) using deep learning-based image analysis [37] [85].
2. Preprocessing and Data Harmonization:
- Quality Control: Apply technology-specific QC filters. For genomics, use FastQC and Trimmomatic; for proteomics, use peptide-level abundance thresholds.
- Batch Effect Correction: Utilize Combat or Harmony algorithms to remove technical artifacts from different processing batches or sites [85].
- Data Transformation and Normalization: Employ log-transformation for RNA-Seq data (e.g., TPM counts), quantile normalization for proteomics, and Z-score normalization for radiomic features to render datasets comparable.
3. Multi-Modal Data Integration and Fusion:
- Early Fusion: Concatenate features from different omics layers into a unified input matrix for model training.
- Intermediate Fusion: Use multi-modal deep learning architectures (e.g., Multi-Layer Perceptrons with separate input branches) to learn joint representations from different data types [85].
- Late Fusion: Train separate models on each data modality (genomics, pathomics, clinical) and combine their predictions using a meta-learner (e.g., a stacking classifier).
4. Biomarker Signature Validation:
- Analytical Validation: Assess repeatability and reproducibility using CLIA-certified laboratory protocols [50].
- Biological Validation: Conduct in vitro or in vivo perturbation experiments (e.g., CRISPR knock-out) to confirm the functional role of identified biomarker candidates.
- Clinical Validation: Validate the composite biomarker signature in independent, held-out clinical cohorts. For predictive biomarkers, this must involve a cohort where patients received the specific drug in question [85].
Protocol for Implementing Standardized Data Governance
A robust data governance framework is essential for ensuring the quality, security, and reproducibility of biomarker data, which is a prerequisite for regulatory approval.
1. Establish Governance Structure and Policies:
- Define Roles: Appoint a Chief Data Officer (CDO), data stewards from scientific domains, and data custodians from IT [88] [89]. A Data Management Office (DMO) may oversee the program.
- Develop Policies: Create clear, documented policies for data access, sharing, ownership, and lifecycle management (retention, archiving, secure disposal) [90] [89].
- Select a Governance Framework: Adopt an established framework like DAMA-DMBOK or ISO/IEC 38505 to structure the program [88].
2. Implement Data Quality and Lifecycle Management:
- Data Quality Rules: Implement automated checks for accuracy, completeness, and consistency at the point of data entry and ingestion. Define standardized formats for critical data elements.
- Metadata Management & Cataloging: Create a centralized data catalog with rich metadata, including data lineage (sources, transformations), protocols, and versioning [90]. This is critical for audit trails.
- Lifecycle Management: Automate data retention and archiving policies based on regulatory and business requirements. For clinical trial data, this aligns with ICH and GCP guidelines.
3. Ensure Security, Privacy, and Compliance:
- Data Security: Apply encryption for data at rest and in transit. Implement strict, role-based access controls (RBAC) to sensitive datasets.
- Privacy Protection: Anonymize or pseudonymize patient data in compliance with GDPR, HIPAA, and other regional regulations [90].
- Regulatory Readiness: For IVDR compliance in Europe, maintain extensive documentation on assay performance, clinical validity, and quality management systems [87] [50].
The following diagram illustrates the logical relationships and workflow between the core components of this standardized governance framework.
Governance Framework Implementation Workflow
Protocol for Interpretability Enhancement using Explainable AI (XAI)
This protocol ensures that complex AI model predictions are transparent and actionable for clinicians and researchers.
1. Integrate XAI Techniques into Model Training:
- Model Selection: Prioritize inherently interpretable models (e.g., Random Forests, Generalized Linear Models) where performance allows. For complex deep learning models, integrate XAI methods post-hoc [85].
- Feature Importance Analysis: Use TreeSHAP for tree-based models and Integrated Gradients or Layer-wise Relevance Propagation (LRP) for deep neural networks to quantify the contribution of each input feature to a prediction [85].
2. Generate and Visualize Explanations:
- Local Explanations: For a single patient's prediction, generate a report highlighting the top 5-10 biomarkers (e.g., gene mutations, protein expression levels) that most strongly influenced the model's output, indicating whether they increased or decreased the predicted risk or response probability.
- Global Explanations: Analyze the model at a population level to identify the features that are consistently most important across all predictions, helping to validate known biology and uncover new insights.
3. Clinical Validation of Explanations:
- Domain Expert Review: Present model predictions alongside XAI-generated explanations to clinical pathologists and oncologists in an interactive dashboard. Gather qualitative feedback on the biological and clinical plausibility of the explanations.
- Correlation with Known Biology: Quantitatively assess whether the top features identified by XAI align with known pathways and established biomarkers for the disease (e.g., PD-L1 for immunotherapy, EGFR for TKIs) [85].
The workflow for incorporating interpretability throughout the AI model lifecycle is shown below.
Explainable AI (XAI) Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents, software, and platforms essential for implementing the integrated framework described in this guide.
Table 3: Key Research Reagent Solutions for Integrated Biomarker Discovery
| Item Name/Category | Function/Brief Explanation | Example Vendor/Platform |
|---|---|---|
| AVITI24 System | Combines sequencing with cell profiling to capture RNA, protein, and morphological data simultaneously in one workflow, enabling spatial biology. | Element Biosciences [87] |
| Single-Cell RNA-Seq Kit | Enables analysis of gene expression in individual cells, uncovering heterogeneity in tumor microenvironments and identifying rare cell populations. | 10x Genomics [87] |
| High-Throughput Proteomics Panel | Platforms capable of profiling thousands of proteins from a single sample, scaling to thousands of samples daily for biomarker discovery. | Sapient Biosciences [87] |
| Federated Learning Platform | Enables secure, collaborative AI model training across distributed datasets (e.g., multiple hospitals) without moving sensitive patient data. | Lifebit [85] |
| Liquid Biopsy ctDNA Assay | A non-invasive tool for real-time monitoring of disease progression and treatment response via analysis of circulating tumor DNA. | Multiple (e.g., Galleri test) [50] [85] |
| Data Catalog & Lineage Tool | Software for creating a centralized inventory of data assets, tracking data lineage, and managing metadata to ensure reproducibility and governance. | Atlan, Collibra [90] |
| AI/ML Modeling Suite | Integrated software environment supporting model training, hyperparameter optimization, and the application of Explainable AI (XAI) techniques. | Python (scikit-learn, PyTorch, SHAP) [85] |
Validation Frameworks and Comparative Utility Assessment
In the rigorous field of biomarker development, the journey from a promising discovery to a clinically adopted tool is governed by a structured evaluation framework often visualized as a three-tier pyramid: Analytical Validity, Clinical Validity, and Clinical Utility. This hierarchical model provides the foundational criteria used by regulators, health technology assessors, and payers to evaluate diagnostic tools [91]. For researchers and drug development professionals, navigating this validation pathway is critical for translating scientific discoveries into tools that genuinely impact patient care. It is estimated that fewer than 1 in 100 biomarker candidates undergo sufficient validation to be implemented in clinical practice, with most failing not due to flawed biology, but insufficient evidence for adoption [91]. This guide objectively compares the performance criteria and experimental methodologies across these three essential validation tiers, providing a structured approach for evidence generation within predictive and prognostic biomarker research.
The following diagram illustrates the hierarchical relationship between the three tiers and their key questions:
Decoding the Three Tiers: Definitions and Performance Metrics
Core Definitions and Hierarchical Dependence
Each tier of the validation pyramid addresses a distinct and fundamental question about the biomarker, with each level building upon the evidence gathered from the tier below.
- Analytical Validity: This foundation asks, "Does the test accurately and reliably measure the biomarker?" It assesses the technical performance of the assay itself, focusing on its ability to detect the analyte of interest consistently within a laboratory setting [92]. A test must first prove its analytical mettle before its clinical relevance can be meaningfully investigated.
- Clinical Validity: Building upon a solid analytical foundation, this tier asks, "Does the test result correlate with the clinical condition or outcome of interest?" It evaluates the strength of the association between the biomarker result and the patient's clinical status, whether for diagnosis, prognosis, or prediction [92] [91].
- Clinical Utility: The apex of the pyramid addresses the most consequential question: "Does the use of the test lead to improved patient outcomes, clinical decisions, or cost-effective care?" [91] [92] Clinical utility shifts the focus from correlation to consequence, demanding evidence that integrating the test into clinical pathways results in a net benefit for patients and the healthcare system.
Quantitative Performance Standards
The performance of a biomarker at each validation tier is quantified using specific, standardized metrics. The table below summarizes the key parameters and the thresholds often considered acceptable for clinical use.
Table 1: Key Performance Metrics Across the Validation Tiers
| Validation Tier | Key Performance Metrics | Typical Benchmark for Clinical Adoption | Primary Evidence Generated |
|---|---|---|---|
| Analytical Validity [92] | Accuracy, Precision, Sensitivity, Specificity, Limit of Detection, Robustness | >99% specificity and sensitivity for analytical detection [92] | Evidence of a reliable and reproducible measurement. |
| Clinical Validity [92] [91] | Clinical Sensitivity, Clinical Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV) | High PPV/NPV (e.g., >95%); varies with disease prevalence and clinical context [92] | Evidence of a statistical association between the biomarker and a clinical endpoint. |
| Clinical Utility [91] | Impact on clinical decision-making, Improvement in patient outcomes (e.g., survival, quality of life), Cost-effectiveness, Risk-benefit ratio | Demonstration of a net improvement in health outcomes and/or a favorable cost-effectiveness profile. | Evidence that using the test improves patient management and health. |
Experimental Protocols for Tiered Validation
Generating robust evidence for each tier requires carefully designed experiments and protocols. The following workflows and methodologies are central to building a compelling validation dossier.
Experimental Workflow for Multi-Omics Biomarker Discovery and Validation
The contemporary approach to biomarker development often involves high-throughput technologies and a multi-step process from discovery to clinical application, as detailed in studies on prostate cancer biomarkers [93]. The following diagram visualizes a generalized experimental workflow that integrates multi-omics data and machine learning for biomarker development.
Key Methodologies for Each Validation Tier
Analytical Validity Protocols
The focus here is on characterizing the assay's technical performance. Key experiments include [92]:
- Accuracy and Precision Studies: Repeatedly testing well-characterized samples (e.g., reference standards, patient samples with known biomarker status) to determine how close the measurements are to the true value (accuracy) and how reproducible the results are over multiple runs (precision).
- Limit of Detection (LoD) and Quantification (LoQ): Establishing the lowest amount of the biomarker that can be reliably detected and the lowest level that can be precisely measured.
- Robustness and Ruggedness Testing: Assessing the assay's performance under deliberate, small variations in pre-analytical and analytical conditions (e.g., different operators, reagent lots, instruments) to ensure consistency across real-world laboratory settings.
Clinical Validity Protocols
This tier establishes the statistical link between the biomarker and clinical endpoints. Core study designs include [91] [93]:
- Case-Control and Cohort Studies: Using samples from retrospective biobanks or prospective collections to determine the biomarker's ability to distinguish between patients with and without a disease (diagnostic), or between those with different clinical outcomes (prognostic). For example, the clinical validity of a prostate cancer biomarker signature can be established by analyzing its association with biochemical recurrence in a cohort like TCGA-PRAD [93].
- Blinded Validation: The biomarker assay is performed and interpreted without knowledge of the patient's clinical outcome to prevent bias.
- Multivariate Analysis: Statistical models are used to confirm that the biomarker provides independent predictive information beyond standard clinical or pathological variables.
Clinical Utility Protocols
Demonstrating utility requires evidence that using the test changes management for the better. This is the most demanding tier and relies on [91]:
- Randomized Controlled Trials (RCTs): The gold standard, where patients are randomized to have their treatment guided by the biomarker or by standard care. The ATOMIC phase 3 trial, which showed that adding atezolizumab to chemotherapy significantly improved disease-free survival in a specific genetic subtype of colon cancer, is a prime example of high-level evidence for clinical utility [94].
- Clinical Impact Studies: These studies measure how often test results lead to a change in treatment plans (e.g., choice of drug, dose modification) in a real-world clinical setting.
- Health Economic Analyses: Formal cost-effectiveness analyses that weigh the benefits of biomarker-guided care against the costs of testing and subsequent management.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successfully navigating the validation pyramid requires a suite of reliable reagents, platforms, and computational tools. The following table details key solutions used in modern biomarker development pipelines, as referenced in the multi-omics prostate cancer study [93].
Table 2: Key Research Reagent Solutions for Biomarker Development
| Tool Category | Specific Solution / Platform | Primary Function in Validation |
|---|---|---|
| Data Generation & Analysis | Seurat R Package [93] | A comprehensive toolkit for single-cell RNA-seq data quality control, analysis, and visualization. |
| Data Generation & Analysis | DESeq2 / EdgeR [93] | Statistical software for identifying differentially expressed genes from bulk RNA-seq data. |
| Data Generation & Analysis | Weighted Gene Co-expression Network Analysis (WGCNA) [93] | An R package for constructing co-expression networks and identifying modules of highly correlated genes linked to clinical traits. |
| Computational & Modeling | Random Survival Forest (RSF), Lasso-Cox [93] | Machine learning algorithms used for feature selection and building robust prognostic models from high-dimensional data. |
| Computational & Modeling | Gene Set Variation Analysis (GSVA) / ssGSEA [93] | Methods for assessing pathway-level activity in individual samples, providing functional context for biomarker signatures. |
| Functional Validation | Cell Line Models (e.g., LNCaP, PC-3) [93] | In vitro models for experimentally validating the function of candidate biomarkers (e.g., via gene knockdown/overexpression). |
| Functional Validation | Immunohistochemistry (IHC) / Western Blot [93] | Standard techniques for confirming protein-level expression and cellular localization of biomarkers in patient tissues. |
The three-tier validation pyramid of Analytical Validity, Clinical Validity, and Clinical Utility provides an indispensable, hierarchical framework for transitioning biomarkers from promising discoveries to proven clinical tools. This structured approach demands a sequential and rigorous evidence-generation process, beginning with technical robustness and culminating in demonstrated patient benefit. For researchers and drug developers, a deep understanding of the distinct requirements, performance metrics, and experimental protocols at each tier is paramount. Successfully scaling this pyramid requires strategic planning from the outset, leveraging advanced multi-omics technologies, sophisticated computational models, and ultimately, validation through well-designed clinical trials. Adherence to this framework not only strengthens scientific rigor but also maximizes the likelihood that transformative biomarkers will be adopted into clinical practice, ultimately fulfilling their potential to improve patient care and outcomes.
The path from identifying a statistical association to demonstrating a clear impact on patient outcomes is a complex but critical journey in modern medicine, particularly in oncology. This process forms the bedrock of precision medicine, ensuring that biological discoveries translate into tangible clinical benefits. Central to this pathway is the crucial distinction between prognostic and predictive biomarkers—a distinction that fundamentally shapes their clinical utility and application in drug development and patient care [20]. A prognostic biomarker provides information on the likely course of a disease irrespective of treatment, offering insights into natural history, while a predictive biomarker indicates the likelihood of benefit from a specific therapeutic intervention [63] [20]. This guide provides a structured comparison of these biomarker classes, detailing their validation pathways, clinical applications, and integration into patient care, framed within the context of their ultimate impact on health outcomes.
Biomarker Classification and Clinical Utility
Comparative Framework: Prognostic vs. Predictive Biomarkers
Table 1: Diagnostic, Prognostic, and Predictive Biomarker Comparison
| Biomarker Category | Clinical Function | Representative Example | Impact on Clinical Decision-Making |
|---|---|---|---|
| Diagnostic | Identifies the presence or type of a disease [63]. | Hemoglobin A1c for diagnosing diabetes mellitus [63]. | Confirms disease status, enabling initial treatment planning. |
| Prognostic | Provides information on the likely disease course or outcome independent of specific treatment [63] [20]. | Cancer stage (e.g., metastatic disease indicating poor short-term outcome) [20]. | Informs patients about disease outlook and identifies high-risk patients who may need more aggressive management, though not tied to a specific therapy. |
| Predictive | Indicates the likelihood of patient benefit from a specific treatment compared to their baseline condition [63] [20]. | EGFR mutation status predicting response to EGFR tyrosine kinase inhibitors in non-small cell lung cancer [63]. | Directly guides therapy selection, enabling clinicians to choose treatments with a higher probability of success for a specific patient. |
| Monitoring | Tracks disease status or response to therapy over time [63]. | HCV RNA viral load for monitoring response to antiviral therapy in chronic Hepatitis C [63]. | Allows for real-time assessment of treatment effectiveness and necessary adjustments. |
| Safety | Monitors for potential adverse effects or toxicity during treatment [63]. | Serum creatinine for monitoring renal function and potential nephrotoxicity [63]. | Helps in managing treatment risks and preventing serious adverse events. |
The Distinction in Clinical Practice
The clinical utility of a biomarker is determined by its ability to change management decisions and improve patient outcomes. A classic illustration of this distinction, and sometimes the convergence, is seen with the HER2 biomarker in breast cancer. Historically, HER2 overexpression was identified as a strong prognostic biomarker, indicating a more aggressive disease course and diminished survival [20]. However, with the development of targeted therapies like trastuzumab, HER2 status evolved into a crucial predictive biomarker, identifying patients who are highly likely to benefit from this specific treatment [20]. This dual utility highlights how a biomarker's role can expand with therapeutic advancements.
In contrast, some biomarkers retain a purely prognostic role. For years, the serum CA-125 level in ovarian cancer was studied as a potential predictive tool for initiating early treatment upon rise during remission. However, a major randomized trial demonstrated that initiating treatment based solely on a rising CA-125, in the absence of other symptoms, failed to improve overall survival [20]. This underscores that a statistically significant association with disease (prognostic ability) does not automatically translate into utility for guiding a specific treatment (predictive ability).
Quantitative Data and Validation Metrics
The validation of biomarkers requires rigorous assessment using standardized metrics that evaluate both their analytical performance and their clinical value.
Table 2: Key Validation Metrics for Biomarker Performance
| Validation Phase | Key Performance Metrics | Interpretation and Clinical Implication |
|---|---|---|
| Analytical Validation | Accuracy & Precision: Closeness to true value and reproducibility of results [63]. | Ensures the test reliably measures the biomarker, forming the foundation for all subsequent clinical claims. |
| Analytical Sensitivity & Specificity: Ability to correctly detect the biomarker and distinguish it from similar molecules [63]. | Minimizes false positives and false negatives at the analytical level. | |
| Reportable Range: The range of biomarker concentrations the test can accurately measure [63]. | Defines the clinical scenarios where the test is applicable. | |
| Clinical Validation | Clinical Sensitivity & Specificity: Ability to correctly identify patients with or without the clinical outcome of interest [63]. | Directly measures how well the biomarker identifies the target patient population or predicts the clinical endpoint. |
| Positive/Negative Predictive Value (PPV/NPV): Probability that a positive/negative test result truly reflects the clinical state [63]. | Provides the most clinically relevant information for a physician interpreting a test result for an individual patient. | |
| Hazard Ratio (HR) & Concordance Index (C-index): Strength of association with a time-to-event outcome (e.g., survival) and model's predictive accuracy [95]. | Quantifies the biomarker's prognostic power (e.g., a HR of 2.15 indicates a significantly worse survival). The c-index evaluates prediction model discrimination [95]. |
Advanced machine learning frameworks are now being deployed to enhance biomarker discovery and validation. For instance, the Graph-Encoded Mixture Survival (GEMS) model, applied to advanced non-small cell lung cancer (aNSCLC), achieved a c-index of 0.665 for predicting overall survival, outperforming traditional statistical models [95]. This demonstrates how AI can identify complex "predictive subphenotypes" from electronic health records, grouping patients with similar baseline characteristics and coherent survival outcomes [95].
Experimental Protocols for Biomarker Assessment
The Fit-for-Purpose Validation Framework
Biomarker validation is not a one-size-fits-all process; it follows a "fit-for-purpose" principle, where the required level of evidence is determined by the specific Context of Use (COU) [63]. The COU is a precise description of how the biomarker will be used in drug development or clinical practice [63]. The pathway involves three core stages:
- Analytical Validation: This establishes that the test itself is reliable. It involves a series of experiments to determine the performance characteristics of the biomarker assay, including its accuracy, precision, sensitivity, specificity, and reportable range [63]. The protocol requires testing the assay across multiple replicates, operators, and days to ensure reproducibility under defined conditions.
- Clinical Validation: This step moves from the lab to the clinic, demonstrating that the biomarker is consistently and reproducibly associated with the clinical outcome or endpoint of interest [63]. This typically involves retrospective analyses of well-characterized clinical cohorts or biobanks. The protocol includes defining the patient population, collecting and processing samples uniformly, and performing blinded biomarker analysis to prevent bias. Statistical analysis then correlates biomarker status with clinical endpoints like overall survival or objective response rate.
- Clinical Utility / Qualification: This final stage proves that using the biomarker in the proposed COU actually improves patient care or drug development decision-making compared to the standard of care. The highest level of evidence comes from prospective clinical trials or from prospectively-retrospective analyses of large, randomized controlled trials [63]. For regulatory qualification for broad use, developers can submit evidence to the FDA's Biomarker Qualification Program (BQP), which provides a structured framework for review and acceptance [63] [96].
Protocol for a Predictive Biomarker Clinical Trial
A standard protocol for validating a predictive biomarker in a Phase III oncology trial involves:
- Objective: To confirm that patients selected based on the biomarker status derive greater benefit from the investigational drug versus standard therapy.
- Design: A randomized, controlled trial. The key design element is whether to use an all-comers design with biomarker stratification or an enrichment design that only enrolls biomarker-positive patients.
- Methodology:
- Patient Screening: Obtain informed consent and collect tumor tissue or blood for biomarker testing from all potential participants.
- Biomarker Testing: Analyze samples in a Central Laboratory using a analytically validated assay.
- Randomization & Stratification: Patients are randomized to the experimental or control arm. Biomarker status (positive/negative) is used as a stratification factor to ensure balance between treatment arms.
- Blinding: The study can be double-blinded (if possible) or open-label, but the biomarker analysis is often performed blinded to the clinical outcome data until the pre-specified analysis time.
- Endpoint Analysis: The primary endpoint (e.g., Overall Survival) is compared between treatment arms within the biomarker-positive subgroup and the biomarker-negative subgroup. A significant interaction test confirms the biomarker's predictive nature.
Visualizing Biomarker Pathways and Utility
The following diagrams map the conceptual pathways and validation workflows for prognostic and predictive biomarkers, illustrating their distinct roles in clinical decision-making.
Biomarker Clinical Utility Pathway
Biomarker Validation and Integration Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Reagents and Platforms for Biomarker Research and Development
| Tool Category | Specific Examples | Function in Biomarker Workflow |
|---|---|---|
| Omics Technologies | Next-Generation Sequencing (NGS) panels, Mass Spectrometry (LC-MS/MS), Microarrays [25] [14]. | Enables comprehensive profiling of biomarkers across genomic, transcriptomic, proteomic, and metabolomic layers for discovery and validation [25] [50]. |
| Single-Cell Analysis | Single-cell RNA sequencing (scRNA-seq) platforms [50]. | Provides deep insights into tumor microenvironments and identifies rare cell populations driving disease heterogeneity and therapy resistance [50]. |
| Liquid Biopsy Technologies | Circulating tumor DNA (ctDNA) assays, Circulating Tumor Cell (CTC) capture systems [50] [14]. | Facilitates non-invasive, real-time monitoring of disease progression and treatment response through blood-based biomarker analysis [50]. |
| Immunoassays & Biosensors | ELISA, Multiplex Immunoassays, Electrochemical Biosensors, Surface Plasmon Resonance (SPR) [14]. | Quantifies specific protein biomarkers with high sensitivity and specificity; biosensors offer potential for point-of-care applications. |
| Digital Pathology & AI | AI-based image analysis algorithms (e.g., for histopathology slides) [37]. | Identifies complex prognostic and predictive patterns in tissue images that surpass human observational capacity, creating digital biomarkers [37]. |
| Data Integration & AI Platforms | Graph Neural Networks (GNNs), Machine Learning (ML) frameworks for multi-modal data fusion [25] [95]. | Integrates diverse data types (EHR, omics, imaging) to identify novel biomarker signatures and predictive subphenotypes [25] [95]. |
The journey from a statistical association to a validated biomarker that improves patient outcomes is rigorous and complex, demanding a clear understanding of the fundamental distinction between prognostic and predictive utility. While prognostic markers inform the natural history of disease, predictive biomarkers are indispensable tools for therapy selection, directly enabling personalized medicine. The future of biomarker development lies in embracing multi-omics integration, leveraging artificial intelligence to uncover complex patterns, and adopting fit-for-purpose validation strategies within clear regulatory pathways. As these technologies and frameworks evolve, the systematic assessment of clinical utility will ensure that biomarkers continue to bridge the gap between statistical discovery and meaningful patient impact.
In the evolving landscape of precision medicine, the clinical utility of biomarkers is rigorously assessed through specific performance metrics that determine their value in research and clinical practice. Predictive biomarkers identify patients likely to respond to a specific treatment, while prognostic biomarkers provide information about a patient's overall disease outcome regardless of therapy [10] [40]. This distinction fundamentally shapes how biomarkers are applied in drug development and clinical decision-making. The evaluation of both biomarker types relies critically on a core set of statistical measures: sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) [63]. These metrics provide a standardized framework for quantifying a biomarker's ability to correctly classify patients, enabling objective comparison across different biomarker candidates and technologies.
The U.S. Food and Drug Administration (FDA) emphasizes that biomarker validation is a "fit-for-purpose" process, where the required level of evidence depends on the specific context of use (COU) [63] [97]. For predictive biomarkers that guide therapeutic choices, accurate classification is paramount, as misclassification can lead to ineffective treatments or unnecessary side effects. Similarly, prognostic biomarkers used for patient stratification in clinical trials must reliably identify disease trajectories to demonstrate true clinical utility. Within this framework, sensitivity, specificity, PPV, and NPV serve as fundamental tools for developers and regulators to assess biomarker performance, guide strategic decisions in drug development, and ultimately ensure that biomarkers provide meaningful improvements to patient care.
Core Metric Definitions and Clinical Interpretation
Fundamental Definitions and Calculations
The performance of a diagnostic or classification test, including biomarker assays, is characterized by four interdependent metrics. These metrics are derived from a 2x2 contingency table that cross-tabulates the test results with the true disease status, as determined by a gold standard reference [98] [99].
Sensitivity (True Positive Rate) measures the test's ability to correctly identify individuals who have the condition. It is the probability of a positive test result given that the individual truly has the disease [98] [99]. Calculated as: Sensitivity = True Positives / (True Positives + False Negatives)
Specificity (True Negative Rate) measures the test's ability to correctly identify individuals who do not have the condition. It is the probability of a negative test result given that the individual is truly disease-free [98] [99]. Calculated as: Specificity = True Negatives / (True Negatives + False Positives)
Positive Predictive Value (PPV) is the probability that an individual with a positive test result truly has the disease. Unlike sensitivity and specificity, PPV is directly influenced by the prevalence of the disease in the population [98] [100]. Calculated as: PPV = True Positives / (True Positives + False Positives)
Negative Predictive Value (NPV) is the probability that an individual with a negative test result truly does not have the disease. Like PPV, NPV varies with disease prevalence [98] [100]. Calculated as: NPV = True Negatives / (True Negatives + False Negatives)
Clinical Application and Rule-In/Rule-Out Value
The clinical utility of these metrics is often summarized by the mnemonics "SNOUT" and "SPIN." A highly SeNsitive test, when Negative, helps to rule OUT disease. This is crucial when the consequences of missing a diagnosis are severe, such as in screening for infectious diseases or life-threatening conditions [100] [101]. Conversely, a highly SPecific test, when Positive, helps to rule IN disease. High specificity is desirable for confirmatory testing after a positive screening result, as it minimizes false positives and the associated anxiety, cost, and risk of unnecessary follow-up procedures [100] [101].
PPV and NPV are particularly valuable to clinicians at the point of care, as they answer the question: "Given this test result, what is the chance my patient does or does not have the disease?" [101]. However, it is critical to remember that these values are not intrinsic to the test alone; they depend heavily on the disease prevalence in the tested population. A test will have a higher PPV and a lower NPV when used in a high-prevalence setting compared to a low-prevalence setting, even though its sensitivity and specificity remain unchanged [100].
Comparative Analysis of Biomarker Types Using Performance Metrics
Performance Metrics in Action: A Prostate Cancer Case Study
A recent study on prostate-specific antigen density (PSAD) for detecting clinically significant prostate cancer provides a concrete example of these metrics in practice [98]. Using a PSAD cutoff of ≥0.08 ng/mL/cc as an indicator for recommending biopsy, and considering prostate biopsy as the gold standard, the study yielded the following results:
- True Positives (TP): 489
- False Positives (FP): 1400
- True Negatives (TN): 263
- False Negatives (FN): 10
From this data, the performance metrics were calculated [98]:
- Sensitivity = 489 / (489 + 10) = 98%
- Specificity = 263 / (263 + 1400) = 16%
- PPV = 489 / (489 + 1400) = 26%
- NPV = 263 / (263 + 10) = 96%
This case highlights the intrinsic trade-off between sensitivity and specificity. The chosen PSAD cutoff achieved a very high sensitivity (98%), meaning it missed very few actual cancer cases (only 10 false negatives). However, this came at the cost of low specificity (16%), resulting in a large number of false positives (1400 men without cancer who would have undergone an unnecessary biopsy). The high NPV (96%) indicates that a negative test result reliably excludes disease, which was the study's stated goal [98].
Comparative Performance of Validated Cancer Biomarkers
Different biomarkers exhibit varying profiles of these metrics based on their underlying biology and clinical application. The table below summarizes the reported performance of several established and emerging biomarkers in oncology.
Table 1: Comparative Performance of Selected Cancer Biomarkers
| Biomarker | Cancer Type | Reported Sensitivity | Reported Specificity | Clinical Role & Notes |
|---|---|---|---|---|
| PD-L1 [10] | NSCLC | Varies by assay & cutoff | Varies by assay & cutoff | Predictive: Guides anti-PD-1/PD-L1 therapy. Performance is context-dependent. |
| MSI-H/dMMR [10] | Pan-cancer (e.g., Colorectal) | Not explicitly stated | Not explicitly stated | Predictive: Tissue-agnostic biomarker for immunotherapy. High response rate (ORR: 39.6%). |
| Tumor Mutational Burden (TMB) [10] | Pan-cancer | Not explicitly stated | Not explicitly stated | Predictive: TMB ≥10 mut/Mb associated with 29% ORR vs. 6% in low-TMB. |
| Circulating Tumor DNA (ctDNA) [10] | Multiple (e.g., Colon) | >90% (metastatic setting) | High | Monitoring/Prognostic: Detects molecular residual disease; ≥50% reduction post-therapy correlates with improved PFS/OS. |
| PSAD [98] | Prostate | 98% (at 0.08 cutoff) | 16% (at 0.08 cutoff) | Diagnostic/Risk-stratification: High NPV used to avoid unnecessary biopsy. |
Impact of Prevalence on Predictive Values
A critical concept in applying these metrics is that PPV and NPV are profoundly influenced by the prevalence of the disease in the population being tested, while sensitivity and specificity are considered intrinsic properties of the test [100] [101]. The same test will perform very differently in a high-risk population compared to a general screening population.
Table 2: Effect of Disease Prevalence on PPV and NPV for a Hypothetical Test with 90% Sensitivity and 90% Specificity
| Prevalence | Positive Predictive Value (PPV) | Negative Predictive Value (NPV) |
|---|---|---|
| 1% | 8% | >99% |
| 10% | 50% | 99% |
| 20% | 69% | 97% |
| 50% | 90% | 90% |
This relationship demonstrates why a screening test with seemingly high performance characteristics can still yield a large number of false positives when applied to a low-prevalence population. For developers, this underscores the necessity of validating biomarkers in populations that reflect their intended clinical use setting.
Threshold Optimization and the Sensitivity-Specificity Trade-Off
The Inverse Relationship
A fundamental principle in biomarker science is the inverse relationship between sensitivity and specificity. Adjusting the threshold or cutoff point for a positive test result inherently involves a trade-off: increasing the sensitivity typically decreases the specificity, and vice versa [98] [99]. This trade-off is visualized in the DOT diagram below, which shows how moving the classification threshold changes the balance between correctly identifying true positives and true negatives.
Case Study: Threshold Optimization in PSAD Testing
The PSAD study again provides a clear illustration. When the researchers lowered the PSAD cutoff from 0.08 to 0.05 ng/mL/cc, the sensitivity increased from 98% to 99.6%, meaning even fewer cancers were missed. However, this further reduced the specificity from 16% to 3%, dramatically increasing the number of false positives [98]. Conversely, raising the cutoff would be expected to improve specificity but at the expense of missing more true cases (lower sensitivity). The optimal threshold is therefore not a fixed statistical value but must be determined based on the clinical context and the relative consequences of false negatives versus false positives.
Experimental Protocols for Metric Validation
Standardized Workflow for Biomarker Validation
The path from biomarker discovery to clinical validation requires a structured, multi-phase approach to ensure that performance metrics are reliable and reproducible. The following workflow outlines the key stages, integrating both analytical and clinical validation components as emphasized by regulatory agencies [63] [43].
The Scientist's Toolkit: Essential Reagents and Materials
The successful validation of biomarker performance metrics relies on a suite of critical reagents and technological platforms. The following table details key components of the "research reagent solutions" required for robust biomarker evaluation.
Table 3: Essential Research Reagents and Platforms for Biomarker Validation
| Tool Category | Specific Examples | Primary Function in Validation |
|---|---|---|
| Preclinical Models [43] | Patient-Derived Organoids (PDOs), Patient-Derived Xenografts (PDX), Genetically Engineered Mouse Models (GEMMs) | Provide physiologically relevant systems for initial biomarker discovery and functional assessment of candidate biomarkers. |
| Advanced Assay Platforms [10] [43] | Immunohistochemistry (IHC) for PD-L1, Next-Generation Sequencing (NGS) for TMB/MSI, PCR/digital PCR for ctDNA, Liquid Biopsy platforms | Enable precise detection and quantification of the biomarker signal in complex biological samples. |
| Analytical Reagents [43] | Validated Antibodies, CRISPR-Based Functional Genomics kits, Single-Cell RNA Sequencing kits, Multi-omics Reagent Kits | Facilitate the specific measurement of biomarker targets and exploration of biological mechanisms. |
| Gold Standard Reference Materials [98] [63] | Certified Reference Standards, Control Cell Lines, Characterized Biobank Samples (e.g., tumor tissue with confirmed pathology) | Serve as benchmarks for analytical validation, ensuring assay accuracy, precision, and reproducibility across sites. |
| Data Analysis Suites [68] [43] | AI/Machine Learning Algorithms, Bioinformatic Pipelines, Statistical Software (e.g., R, Python with scikit-learn) | Support the calculation of performance metrics, manage multi-omics data integration, and identify complex biomarker signatures. |
The objective comparison of biomarkers through standardized performance metrics is indispensable for advancing predictive and prognostic biomarker research. Sensitivity, specificity, PPV, and NPV provide a foundational framework for this assessment, each offering unique and complementary insights. The case studies presented, particularly on PSAD and immuno-oncology biomarkers, demonstrate that there is no single "best" metric; their utility is contextual and must be interpreted in light of the biomarker's intended clinical use, the target population's disease prevalence, and the clinical consequences of misclassification [98] [10] [100].
Future developments in biomarker science will increasingly rely on integrated multi-omics approaches and artificial intelligence to identify complex biomarker signatures that outperform single-analyte tests [10] [68] [43]. Furthermore, the regulatory landscape continues to evolve, with programs like the FDA's Biomarker Qualification Program encouraging the development of publicly available, well-validated biomarkers for specific contexts of use [63] [97]. As these trends progress, the rigorous application of comparative performance metrics will remain the cornerstone of translating promising biomarkers from the research laboratory into tools that genuinely enhance drug development and patient care.
In the modern era of precision oncology, biomarkers have transitioned from research tools to essential components of clinical decision-making. Biomarkers are defined as measurable biological indicators of normal biological processes, pathogenic processes, or biological responses to an exposure or intervention [39]. Within drug development, biomarkers are broadly classified as either prognostic or predictive, each with distinct clinical applications. Prognostic biomarkers provide information about a patient's likely disease course and overall outcome regardless of specific therapy. In contrast, predictive biomarkers identify patients who are more or less likely to benefit from a particular therapeutic intervention [46] [23]. This fundamental distinction is crucial for clinical utility assessment, as prognostic markers inform disease trajectory while predictive markers guide treatment selection.
The validation pathway for biomarkers spans multiple stages, from initial discovery to clinical implementation. Analytical validation ensures the test accurately and reliably measures the biomarker, while clinical validation establishes that the biomarker correlates with clinical endpoints. The ultimate goal is demonstrating clinical utility, where using the biomarker actually improves patient outcomes [23]. The complex journey from biomarker discovery to clinical application requires specifically designed clinical trials that can adequately address the unique challenges of biomarker validation, particularly for predictive biomarkers that require demonstration of a treatment-by-biomarker interaction effect [39].
Classifying Biomarker Clinical Trial Designs
Retrospective versus Prospective Validation Approaches
Clinical trial designs for biomarker validation are broadly categorized into retrospective and prospective approaches, each with distinct advantages and limitations.
Retrospective validation utilizes archived specimens and data from previously conducted randomized controlled trials (RCTs) to evaluate biomarker utility. This approach offers significant efficiencies in time and resources compared to prospective studies. The successful validation of KRAS mutation status as a predictive biomarker for anti-EGFR therapies in colorectal cancer exemplifies the power of well-designed retrospective analysis. In this case, retrospective analysis of phase III trial data demonstrated that patients with wild-type KRAS tumors benefited from panitumumab or cetuximab (hazard ratio [HR] for progression-free survival = 0.45), while those with mutant KRAS tumors derived no benefit (HR = 0.99), with a significant treatment-by-biomarker interaction (P < .0001) [46].
For retrospective validation to yield reliable results, several requirements must be met: availability of specimens from a well-conducted RCT, samples from a large majority of patients to avoid selection bias, prospectively stated analysis plans, predefined assay methods, and appropriate sample size justification [46]. While retrospective analysis can bring effective treatments to biomarker-defined subgroups more rapidly, it remains susceptible to biases related to specimen availability and unmeasured confounding factors.
Prospective validation represents the gold standard for establishing biomarker utility, with several specialized designs available depending on the strength of preliminary evidence and the specific research questions [46].
Prospective Clinical Trial Designs for Biomarker Validation
Table 1: Comparison of Prospective Clinical Trial Designs for Biomarker Validation
| Design Type | Key Features | Best-Suited Scenarios | Advantages | Limitations | Real-World Examples |
|---|---|---|---|---|---|
| Enrichment (Targeted) Design | Only patients with specific biomarker status are enrolled | Strong preliminary evidence that treatment benefit is restricted to biomarker-defined subgroup | Reduced sample size; focused recruitment; ethical allocation | May leave questions about utility in excluded populations; requires validated assay | HER2-positive breast cancer trials for trastuzumab [46] |
| Unselected (All-Comers) Design | All eligible patients enrolled regardless of biomarker status | Uncertain preliminary evidence about treatment benefit; assay reproducibility concerns | Evaluates utility in broad population; can assess prevalence | Larger sample size; more expensive | IPASS study of gefitinib in lung cancer [39] |
| Hybrid Design | Combines elements of enrichment and unselected designs | Strong evidence for efficacy in one subgroup but uncertainty in others | Ethical allocation in known subgroups; learns about uncertain subgroups | Complex statistical analysis; larger than pure enrichment | Multigene assay trials in breast cancer [46] |
| Biomarker-Strategy Design | Patients randomized to biomarker-guided therapy vs. standard care | Evaluating clinical utility of biomarker-based treatment strategy | Tests overall strategy effectiveness; clinician-friendly | Less efficient than targeted designs for treatment effect | OPTIMA trial in breast cancer [102] |
| Adaptive Signature Design | Integrates biomarker development and validation in single trial | No fully validated biomarker available before phase III | Efficiently identifies predictive biomarkers; flexible | Complex statistical adjustment; multiple testing issues | Emerging designs for targeted therapies [103] |
Methodological Considerations and Experimental Protocols
Statistical Framework for Biomarker Validation
The statistical validation of predictive biomarkers requires demonstration of a significant treatment-by-biomarker interaction – where the treatment effect differs meaningfully between biomarker-defined subgroups [39]. This is typically evaluated using multivariate regression models containing terms for treatment, biomarker status, and their interaction. For time-to-event outcomes, the Cox proportional hazards model is commonly employed:
logit(pit) = boi + b2it + b3i(x∗t) + eit
Where b3i represents the interaction effect between the biomarker (x) and treatment (t) [103].
In the IPASS study validating EGFR mutation as a predictive biomarker for gefitinib in lung cancer, the highly significant interaction (P < .001) demonstrated opposite effects: patients with EGFR mutated tumors had significantly longer progression-free survival with gefitinib versus chemotherapy (HR = 0.48), while those with wild-type tumors had significantly shorter PFS (HR = 2.85) [39].
For biomarker discovery using high-dimensional data (e.g., genomics), strict control of false discovery rates is essential, with cross-validation approaches critical for unbiased performance estimation [23] [39].
Biomarker Assay Validation Protocols
Table 2: Essential Research Reagent Solutions for Biomarker Validation
| Reagent Category | Specific Examples | Primary Function in Biomarker Validation | Key Considerations |
|---|---|---|---|
| Nucleic Acid Analysis Platforms | RT-PCR, qPCR, Next-Generation Sequencing | Detect genetic variants, expression levels; gold standard for mutation detection | Sensitivity, throughput, cost, automation capability [104] |
| Protein Detection Systems | ELISA, Meso Scale Discovery (MSD), Western Blot, Immunohistochemistry | Measure protein expression, modification, localization | Multiplexing capability, dynamic range, spatial information [104] |
| Cellular Analysis Tools | Flow Cytometry, Single-Cell RNA Sequencing | Characterize cell populations, functional states | Single-cell resolution, parameter number, viability requirements [104] |
| Spatial Biology Platforms | CODEX, Spatial Transcriptomics, Imaging Mass Cytometry | Preserve tissue architecture while mapping molecular features | Resolution, multiplexing capacity, tissue requirements [104] |
| Automation & Integration Systems | Automated liquid handlers, robotic sample processors | Improve reproducibility, throughput, and standardization | Integration with existing platforms, customization options [104] |
Regardless of the specific technology platform, analytical validation must establish precision (reproducibility), accuracy (deviation from true value), sensitivity (detection limit), and specificity (discrimination from related analytes) following regulatory guidelines [104]. For clinical implementation, clinical validity (correlation with clinical endpoints) and clinical utility (improvement in patient outcomes) must be demonstrated [23].
Advanced Adaptive Designs for Biomarker Development
Biomarker Adaptive Signature Designs
When a fully validated biomarker is unavailable before initiating phase III trials, adaptive signature designs provide a framework for simultaneously developing and validating predictive biomarkers. These designs address the challenge that "completely phase II validated biomarkers for uses in the phase III trial are often unavailable" [103].
The adaptive signature approach typically involves:
- Biomarker identification through analysis of treatment-by-biomarker interactions
- Classifier development using machine learning algorithms (e.g., random forests, support vector machines)
- Performance assessment with strict control of type I error rates [103]
These designs incorporate pre-specified analysis plans for identifying biomarker signatures and testing treatment effects within identified subgroups, with statistical adjustments for the data-driven nature of the biomarker development process.
Multi-Biomarker Adaptive Selection Designs
When multiple biomarker candidates exist, adaptive designs can efficiently select the most promising biomarker for the validation phase of a trial. The OPTIMA trial in breast cancer exemplifies this approach, where multiple biomarker tests were evaluated in an initial stage, with the most promising test selected for the remainder of the trial based on pre-specified criteria [102].
This design incorporates:
- An initial stage where patients are evaluated with multiple biomarkers
- An interim analysis comparing biomarker performance and concordance
- A selection rule for choosing the primary biomarker for subsequent stages
- Incorporation of early patients into the final analysis when appropriate [102]
Such designs can substantially reduce trial costs when alternative biomarkers differ significantly in expense, with only minimal power loss when biomarkers are highly concordant.
Visualization of Key Concepts and Workflows
Biomarker Classification and Clinical Utility
Diagram Title: Biomarker Classification and Examples
Clinical Trial Design Workflow for Biomarker Validation
Diagram Title: Biomarker Validation Pathway
The strategic implementation of appropriate clinical trial designs is fundamental to translating biomarker discoveries into clinically useful tools that advance personalized medicine. The choice between retrospective and prospective approaches, and among various prospective designs, depends on multiple factors including the strength of preliminary evidence, assay maturity, prevalence of the biomarker, and practical considerations of cost and timeline.
As biomarker science continues to evolve, adaptive designs offer promising approaches for efficiently addressing multiple questions within single trial frameworks, potentially accelerating the development of biomarker-guided therapies. Regardless of the specific design, rigorous attention to statistical principles, assay validation, and regulatory requirements remains essential for generating reliable evidence that can transform patient care through precision medicine approaches.
The successful integration of biomarkers into clinical practice requires close collaboration among clinicians, statisticians, laboratory scientists, and regulatory specialists throughout the validation process. Only through such multidisciplinary approaches can we fully realize the potential of biomarkers to guide therapeutic decisions and improve outcomes for patients.
Economic and Ethical Considerations in Biomarker Implementation
The integration of biomarkers into oncology has fundamentally transformed therapeutic landscapes, shifting the paradigm from a one-size-fits-all approach to precision medicine. This evolution hinges on accurately distinguishing between two distinct biomarker classes: predictive biomarkers, which identify patients likely to benefit from a specific treatment, and prognostic biomarkers, which provide information on the likely course of the disease irrespective of the therapy received [20]. The clinical utility of any biomarker is critically dependent on this distinction, as mistakenly assuming a biomarker is predictive when it is largely prognostic can have significant personal, financial, and ethical consequences [58]. Such errors may lead to withholding effective treatments from some patients or administering costly and potentially toxic therapies to those unlikely to benefit. This guide objectively compares the implementation of these biomarker classes, framing the analysis within a broader assessment of their clinical utility and providing a detailed examination of the associated economic and ethical considerations that are paramount for researchers, scientists, and drug development professionals.
Biomarker Classification and Direct Clinical Utility Comparison
The foundational step in biomarker implementation is understanding their core functions. A prognostic biomarker is "a clinical or biological characteristic that provides information on the likely patient health outcome irrespective of the treatment," while a predictive biomarker "indicates the likely benefit to the patient from the treatment, compared with their condition at baseline" [20]. For example, the serum CA-125 level in ovarian cancer historically served a prognostic role, indicating disease recurrence, but clinical trials demonstrated it was not predictive of benefit from early therapeutic intervention based solely on its elevation [20]. In contrast, HER2 overexpression in breast cancer serves a dual role; it is a negative prognostic factor and a predictive biomarker for the efficacy of HER2-targeted therapies [20].
The table below summarizes key validated and emerging biomarkers, categorizing their primary utility and clinical role.
Table 1: Comparison of Key Validated and Emerging Biomarkers
| Biomarker | Primary Classification | Associated Therapy/Cancer Type | Key Clinical Utility & Limitation |
|---|---|---|---|
| PD-L1 | Predictive | PD-1/PD-L1 inhibitors (e.g., Pembrolizumab) in NSCLC [10] | Guides first-line therapy in NSCLC with high expression (≥50%); limited by assay variability and tumor heterogeneity [10]. |
| MSI-H/dMMR | Predictive | Immune Checkpoint Inhibitors (e.g., Pembrolizumab) across multiple cancers [10] | Tissue-agnostic biomarker with high response rates (39.6% ORR); utility limited to a subset of patients [10]. |
| Tumor Mutational Burden (TMB) | Predictive | Immune Checkpoint Inhibitors [10] | Reflects neoantigen load; TMB ≥10 mutations/Mb associated with improved response; requires further standardization [10]. |
| HER2 | Predictive & Prognostic | HER2-targeted therapies (e.g., Trastuzumab) in breast cancer [10] [20] | Predictive for targeted therapy response; also a negative prognostic factor in the absence of targeted treatment [20]. |
| Lactate Dehydrogenase (LDH) | Prognostic | Included in AJCC staging for melanoma [10] | Elevated levels indicate high tumor burden and poor prognosis; lacks predictive value for specific therapies [10]. |
| Circulating Tumor DNA (ctDNA) | Predictive & Prognostic | Monitoring response to ICIs; guiding adjuvant chemotherapy in colon cancer [10] | ≥50% reduction post-ICI correlates with better PFS/OS; can detect molecular residual disease and predict recurrence [10]. |
| Tumor-Infiltrating Lymphocytes (TILs) | Predictive & Prognostic | Immunotherapy in TNBC and HER2+ breast cancer [10] | High levels associated with improved response and prognosis; low-cost and reproducible but lacks universal scoring standards [10]. |
Experimental Protocols for Biomarker Assessment
Robust experimental methodologies are essential for validating biomarkers and distinguishing their predictive strength from prognostic effects. The following sections detail key approaches.
The PPLasso Model for High-Dimensional Genomic Data
In the context of high-dimensional genomic data, where the number of candidate biomarkers (p) far exceeds the number of patients (n), traditional statistical methods struggle. The PPLasso (Prognostic Predictive Lasso) method was developed to simultaneously select prognostic and predictive biomarkers while accounting for correlations between biomarkers that can alter selection accuracy [30].
Detailed Methodology:
- Statistical Modeling: The approach uses an ANCOVA-type model. Let
X₁andX₂be the design matrices for patients in treatment groups 1 and 2, respectively. The model is specified as:y = Xα + Xβ + εwhereyis the continuous response vector,αrepresents the treatment effects,βrepresents the biomarker effects, andεis the error term [30]. - Data Integration: The design matrix
Xis structured to include all patient data from both treatment groups, with separate columns for the biomarkers' effects under each treatment. - Correlation Handling: A key innovation of PPLasso is transforming the design matrix to remove correlations between biomarkers before applying a generalized Lasso penalty, which improves selection accuracy when biomarkers are highly correlated [30].
- Variable Selection: The model applies a penalized regression framework that automatically performs variable selection, identifying which biomarkers have significant prognostic effects (main effects) and/or predictive effects (interaction effects with the treatment) [30].
Information-Theoretic Framework for Biomarker Ranking
The INFO+ procedure offers a data-driven method for ranking biomarkers based on their prognostic and predictive strength using an information-theoretic approach, which is particularly useful when the underlying model is not linear [58].
Detailed Methodology:
- Objective Formalization: The method formalizes the problem using information theory. The joint effect of patient characteristics and treatment on outcome is decomposed into a prognostic effect and a predictive effect [58].
- Quantification: INFO+ quantifies the predictiveness and prognosticness of each biomarker in "bits" of information, providing a separate, self-consistent ranking for each type of effect [58].
- Higher-Order Interactions: The method can capture second-order biomarker interactions, helping to identify synergistic effects between multiple biomarkers [58].
- Visualization: The approach introduces a graphical representation that plots each biomarker based on its quantified predictive and prognostic strength, offering intuitive insight into its primary clinical utility [58].
Visualization of Biomarker Pathways and Decision Frameworks
Biomarker Clinical Utility Decision Pathway
The following diagram illustrates the logical pathway for classifying a biomarker and assessing its clinical utility, incorporating economic and ethical considerations.
Predictive Biomarker Mechanism of Action
This diagram outlines the signaling pathway and mechanism by which a predictive biomarker, such as PD-L1, enables a specific therapy to exert its effect.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and computational tools essential for conducting research in biomarker discovery and validation.
Table 2: Essential Research Reagents and Tools for Biomarker Studies
| Research Tool / Reagent | Primary Function | Example Application in Biomarker Research |
|---|---|---|
| Anti-PD-L1 Antibodies | Immunohistochemistry (IHC) detection of PD-L1 protein expression. | Quantifying PD-L1 expression levels on tumor cells to determine patient eligibility for anti-PD-1/PD-L1 therapies [10]. |
| Next-Generation Sequencing (NGS) Panels | High-throughput sequencing of genomic DNA to identify mutations. | Calculating Tumor Mutational Burden (TMB) and detecting Microsatellite Instability (MSI) status from tumor tissue [10]. |
| ctDNA Extraction Kits | Isolation of cell-free circulating tumor DNA from blood plasma. | Enabling non-invasive "liquid biopsy" for treatment response monitoring and relapse detection via ctDNA analysis [10]. |
| INFO+ Software (R package) | Information-theoretic ranking of biomarkers by predictive/prognostic strength. | Distinguishing and quantifying whether a biomarker's primary signal is predictive or prognostic in a clinical trial dataset [58]. |
| PPLasso Algorithm | Simultaneous selection of prognostic and predictive biomarkers in high-dimensional data. | Identifying key genomic biomarkers from transcriptomic or proteomic datasets where variables are highly correlated [30]. |
Conclusion
The successful integration of prognostic and predictive biomarkers into clinical practice requires a systematic, phased approach that spans from foundational definition to robust validation. While significant challenges remain in standardization, generalizability, and clinical translation, emerging frameworks that leverage multi-modal data integration, artificial intelligence, and innovative trial designs offer promising pathways forward. Future progress will depend on strengthening multi-omics approaches, conducting longitudinal cohort studies, developing edge computing solutions for low-resource settings, and establishing clearer regulatory pathways. By adopting comprehensive assessment strategies that balance analytical rigor with practical clinical utility, researchers and drug developers can more effectively advance personalized medicine and improve patient outcomes across diverse disease areas.
References
- 1. Prognostic Biomarker - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK402289/]
- 2. Predictive Biomarker - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK402283/]
- 3. Evaluating the Clinical Utility of a Biomarker - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3138723/]
- 4. Methods for determining clinical utility [https://www.sciencedirect.com/science/article/abs/pii/S0009912023002023]
- 5. Prognostic versus predictive value of biomarkers in oncology [https://pubmed.ncbi.nlm.nih.gov/18396036/]
- 6. Understanding Prognostic versus Predictive Biomarkers [https://www.ncbi.nlm.nih.gov/books/NBK402284/]
- 7. Predictive Biomarkers and Companion Diagnostics. The ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4215952/]
- 8. The current state of imaging biomarker development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187508/]
- 9. an analysis based on population-level parametric distributions ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02656-5]
- 10. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 11. Generalizability of Treatment Outcome Prediction Across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11926635/]
- 12. Development of the treatment prediction model in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185704/]
- 13. Unveiling prognostic biomarkers and immunotherapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599034/]
- 14. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 15. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 16. About Biomarkers and Qualification [https://www.fda.gov/drugs/biomarker-qualification-program/about-biomarkers-and-qualification]
- 17. Biomarkers and surrogate endpoints - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1884846/]
- 18. Simple Methods for Evaluating 4 Types of Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412628/]
- 19. Biomarkers and Surrogate Endpoints In Clinical Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3551627/]
- 20. Prognostic vs Predictive Factors in Oncology Carry ... [https://www.onclive.com/view/prognostic-vs-predictive-factors-in-oncology-carry-differing-intent-but-may-have-complementary-clinical-utility]
- 21. FDA Facts: Biomarkers and Surrogate Endpoints [https://www.fda.gov/about-fda/innovation-fda/fda-facts-biomarkers-and-surrogate-endpoints]
- 22. Biomarkers as Surrogate Endpoints in Drug Development [https://www.sciencedirect.com/science/article/abs/pii/S0149291825002693]
- 23. Clinical trial designs for evaluating the medical utility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2851173/]
- 24. Bayesian hierarchical meta‐analytic methods for modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7065251/]
- 25. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 26. Prognostic versus predictive value of biomarkers in oncology [https://www.sciencedirect.com/science/article/abs/pii/S0959804908002335]
- 27. Performance comparison between multi-level gene ... [https://pubmed.ncbi.nlm.nih.gov/38955118/]
- 28. Performance comparison between multi-level gene ... [https://www.sciencedirect.com/science/article/abs/pii/S0344033824003303]
- 29. The ability to classify patients based on gene-expression data ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1009926]
- 30. Identification of prognostic and predictive biomarkers in high ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05143-0]
- 31. World's largest metabolomic study completed, paving way ... [https://www.ukbiobank.ac.uk/news/worlds-largest-metabolomic-study-completed-paving-way-for-predictive-medicine/]
- 32. Metabolomics in drug research and development: The recent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10465962/]
- 33. Genomic Biomarkers Market Surges Toward USD 17B by ... [https://media.market.us/genomic-biomarkers-market-news-2025/]
- 34. What Are Biomarkers? Definition, Applications and ... [https://blog.omni-inc.com/blog/what-are-biomarkers-and-whats-new-in-2025]
- 35. Comparison of methods of optimal cut-point selection for ... [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-025-07245-9]
- 36. Seeking optimal repeated fluid biomarker assessments to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541280/]
- 37. AI and the future of biomarker analysis in early R&D [https://www.drugtargetreview.com/article/190428/ai-and-the-future-of-biomarker-analysis-in-early-rd/]
- 38. New AI-based biomarkers offer insight into treatment ... [https://dailyreporter.esmo.org/esmo-congress-2025/ai-digital-oncology/new-artificial-intelligence-based-biomarkers-offer-early-insight-into-treatment-response]
- 39. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 40. Diagnostics Evaluation Branch (DEB) - NCI [https://dctd.cancer.gov/programs/cdp/organization/deb]
- 41. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 42. Biomarker discovery and validation: Bridging research and ... [https://www.abcam.com/en-us/knowledge-center/immunology-and-infectious-disease/biomarker-discovery-and-validation]
- 43. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 44. A Comparative Analysis of Biomarker Selection Techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC3842054/]
- 45. Best ELN Software for 2025: Key Features Of The Top [https://research.com/software/best-eln-software]
- 46. Clinical Trial Designs for Predictive Biomarker Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2734400/]
- 47. Prognostic and predictive enrichment in sepsis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7097452/]
- 48. Biomarker-Driven Clinical Trials in Oncology [https://www.precisionformedicine.com/blog/biomarker-driven-clinical-trials-in-oncology-enrichment-stratification-all-comers-basket-when-to-use-what-and-why]
- 49. Clinical trial designs for testing biomarker-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4296980/]
- 50. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 51. Evaluating biomarkers for prognostic enrichment of clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5714681/]
- 52. BioPETsurv: Methodology and open source software to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7500596/]
- 53. BioPETsurv: Methodology and open source software to ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0239486]
- 54. Kathleen F. Kerr - Software [http://faculty.washington.edu/katiek/software.html]
- 55. Sample size methods for evaluation of predictive biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC9233020/]
- 56. A practical solution to estimate the sample size required for ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-022-00276-y]
- 57. A Sub-Analysis of the UK NCRI RAPID Trial [https://www.sciencedirect.com/science/article/pii/S0006497118720624]
- 58. Distinguishing prognostic and predictive biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC6157098/]
- 59. AI applications in functional genomics - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8566780/]
- 60. Large-scale plasma proteomics comparisons through ... [https://www.nature.com/articles/s41586-023-06563-x]
- 61. Deep learning-based approaches for multi-omics data integration and analysis | BioData Mining | Full Text [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-024-00391-z]
- 62. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 63. Use of Biomarkers in Drug Development for Regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489174/]
- 64. Real‐World Evidence in Oncology: Opportunities and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7216461/]
- 65. Oncology case studies: How two life sciences companies ... [https://resources.flatiron.com/real-world-evidence/oncology-case-studies-real-world-evidence]
- 66. Results 5: case studies - Cardiovascular disease risk ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK573185/]
- 67. Real-World Case Studies & Applications of Telemedicine ... [https://imjhealth.org/real-world-case-studies-and-applications-of-telemedicine-in-chronic-disease-management]
- 68. How AI & Biomarkers Are Reshaping the Next Frontier in ... [https://www.precisionformedicine.com/blog/how-ai-biomarkers-are-reshaping-the-next-frontier-in-drug-development]
- 69. Frontiers | Applications and challenges of biomarker-based predictive models in proactive health management [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1633487/full]
- 70. Challenges and recommendations for the translation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12262637/]
- 71. Translational Biomarkers: from Preclinical to Clinical a Report ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3085704/]
- 72. Strategies to Support Successful Translation of Preclinical ... [https://www.precisionformedicine.com/blog/preclinical-biomarker-assays-translation-strategies/]
- 73. Biomarker data visualisation for decision making in clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S1386505619307270]
- 74. Demographic clinical trial diversity assessment methods [https://www.sciencedirect.com/science/article/pii/S2451865425000067]
- 75. Evaluating generalizability of oncology trial results to real- ... [https://www.nature.com/articles/s41591-024-03352-5]
- 76. Development and multi-center validation of machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604152/]
- 77. Development and validation of a machine learning model ... [https://www.nature.com/articles/s41598-025-18443-7]
- 78. Development and multi-cohort validation of a machine ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06728-4]
- 79. Cloud Cost Optimization 2025: 5 Proven Strategies to Save [https://www.ilink-digital.com/insights/blog/cloud-cost-optimization-strategies-2025/]
- 80. Mastering IT Cost Optimization: 14 Strategies for Long ... [https://www.prosperops.com/blog/it-cost-optimization/]
- 81. Unlocking the promise of cost optimization [https://www.deloitte.com/us/en/insights/topics/operations/cost-optimization-operations-strategy.html]
- 82. Five areas of focus for IT cost optimization [https://www.ey.com/en_us/insights/financial-services/five-areas-of-focus-for-it-cost-optimization]
- 83. 11 IT Cost Optimization Strategies for Scalable Savings in ... [https://www.digitalocean.com/resources/articles/it-cost-optimization-strategies]
- 84. 10 cloud cost optimization strategies and best practices in ... [https://northflank.com/blog/cloud-cost-optimization]
- 85. AI-Powered Biomarker Discovery: 7 ... [https://lifebit.ai/blog/ai-powered-biomarker-discovery/]
- 86. Applications and challenges of biomarker-based predictive models in... [https://pubmed.ncbi.nlm.nih.gov/40900695/]
- 87. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 88. Top 10 Data in Governance - Carmatec Frameworks 2025 [https://www.carmatec.com/nl/blog/top-10-data-governance-frameworks/]
- 89. Top Data in Governance Frameworks 2025 [https://www.kellton.com/kellton-tech-blog/popular-data-governance-frameworks]
- 90. Pillars: Essential Data for Governance Frameworks 2025 [https://atlan.com/data-governance-pillars/]
- 91. From Promising to Proven: Lessons from the Validation ... [https://www.linkedin.com/pulse/from-promising-proven-lessons-validation-trenches-jose-pereira-leal-jh2ff]
- 92. Genetic Tests:Clinical Validity and Clinical Utility - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4084965/]
- 93. Unveiling prognostic biomarkers and immunotherapeutic ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03363-z]
- 94. ASCO 2025 Highlights [https://www.diaceutics.com/articles/asco-2025-highlights]
- 95. Identification of predictive subphenotypes for clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12069721/]
- 96. New Study Shows Future Biomarker Development Needs ... [https://friendsofcancerresearch.org/news/new-study-shows-future-biomarker-development-needs-enhancements/]
- 97. How Biomarkers Can Improve the Drug Development ... [https://www.fda.gov/drugs/biomarker-qualification-program/biomarker-qualification-program-educational-module-series-module-2-how-biomarkers-can-improve-drug]
- 98. Sensitivity, Specificity, Positive Predictive Value, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8156826/]
- 99. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 100. Statistics | Sensitivity, Specificity, PPV and NPV [https://geekymedics.com/sensitivity-specificity-ppv-and-npv/]
- 101. Statistics - Sensitivity Specificity PPV NPV - GP Exams [https://gpexams.com/statistics-sensitivity-specificity-ppv-npv/]
- 102. Adaptive designs for clinical trials assessing biomarker ... [https://www.nature.com/articles/bjc2014156]
- 103. Biomarker adaptive designs in clinical trials - Chen [https://tcr.amegroups.org/article/view/2551/html]
- 104. Precision-Driven Biomarker Validation: A Biotech ... [https://www.criver.com/eureka/precision-driven-biomarker-validation-biotech-perspective-part-i]