Validating Cancer Stem Cell Biomarkers: From Bench to Bedside in Precision Oncology
The validation of reliable cancer stem cell (CSC) biomarkers is a critical frontier in oncology, holding the potential to revolutionize cancer diagnosis, prognosis, and therapeutic development.
Validating Cancer Stem Cell Biomarkers: From Bench to Bedside in Precision Oncology
Abstract
The validation of reliable cancer stem cell (CSC) biomarkers is a critical frontier in oncology, holding the potential to revolutionize cancer diagnosis, prognosis, and therapeutic development. This article provides a comprehensive analysis for researchers and drug development professionals, exploring the foundational biology of CSCs and the significant challenge posed by their heterogeneity and the lack of universal markers. It delves into advanced methodological frameworks for biomarker identification and validation, from single-cell omics to functional assays. The content further addresses major troubleshooting areas, including overcoming technological limitations and CSC plasticity, and culminates in a comparative evaluation of validation strategies and their translation into targeted therapies and clinical trials. By synthesizing current knowledge and emerging trends, this article serves as a roadmap for advancing robust CSC biomarker validation to eradicate therapy-resistant cell populations and improve patient outcomes.
The CSC Biomarker Landscape: Understanding Heterogeneity, Key Markers, and Biological Challenges
Defining the Cancer Stem Cell Niche and Its Role in Therapy Resistance and Metastasis
The cancer stem cell (CSC) niche is a specialized tumor microenvironment that plays a pivotal role in maintaining stemness, driving therapy resistance, and promoting metastatic spread. This structured guide compares the cellular components, molecular features, and therapeutic targeting strategies of CSC niches across different cancer types, supported by experimental data and methodologies. We summarize key biomarkers and niche characteristics in clearly organized tables, provide detailed experimental protocols for studying CSC-niche interactions, and visualize critical signaling pathways. Within the broader context of validating CSC biomarkers across cancer types, this analysis reveals both conserved and tumor-specific niche mechanisms that represent promising therapeutic targets for overcoming treatment resistance.
Cancer stem cells (CSCs) constitute a minor subpopulation within tumors characterized by self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies [1] [2]. These cells are situated in specialized microenvironments termed "CSC niches" that provide critical signals for maintaining stemness and regulating CSC fate decisions [1] [3]. The niche concept was originally proposed by Schofield in 1978 for hematopoietic stem cells and has since been extended to solid tumors, where these specialized microterritories maintain self-renewal, guide differentiation, and respond to microenvironmental cues such as oxygenation, mechanical stresses, and soluble factors [4].
CSC niches demonstrate remarkable spatial organization, with recent research using ultra-wide field microscopy revealing that CSCs cluster together and are spatially separated from differentiated cancer cells, forming patterns resembling niches even in unperturbed conditions [5]. The bidirectional crosstalk between CSCs and their niche creates a dynamic ecosystem that supports tumor progression, metastatic dissemination, and therapy resistance through both intrinsic CSC properties and extrinsic microenvironmental factors [6] [3]. Understanding this complex interplay is essential for developing effective strategies to target CSCs and overcome treatment failure.
Composition and Characteristics of the CSC Niche
The CSC niche comprises diverse cellular and acellular components that collectively create a protective microenvironment sustaining CSC function. Table 1 summarizes the major niche constituents and their functional roles across different cancer types.
Table 1: Cellular and Molecular Components of the CSC Niche
| Component Type | Specific Elements | Functional Role in CSC Niche | Cancer Types Where Documented |
|---|---|---|---|
| Cellular Components | Cancer-Associated Fibroblasts (CAFs) | Secrete stemness-maintaining factors (e.g., CLCF1); induce therapy resistance [3] | Gastric, pancreatic, breast cancer |
| Tumor-Associated Macrophages (TAMs) | Promote immune evasion; support stemness through cytokine secretion [6] [3] | Glioblastoma, breast cancer | |
| Mesenchymal Stem Cells (MSCs) | Enhance self-renewal through direct contact and paracrine signaling [3] | Multiple solid tumors | |
| Endothelial Cells & Pericytes | Form vascular niches; regulate CSC quiescence and activation [7] [8] | Glioblastoma, colorectal cancer | |
| Extracellular Matrix | Type I Collagen, Fibronectin | Increase matrix stiffness; promote CSC proliferation and inhibit apoptosis [3] | Breast cancer, hepatocellular carcinoma |
| Hyaluronan | Maintains multipotent state; supports CSC marker expression [3] | Liver cancer | |
| Physiological Conditions | Hypoxia | Activates HIF signaling; upregulates CSC markers (CD133, CD44); promotes quiescence [8] | Multiple solid tumors |
| Inflammation | Creates pro-tumorigenic signaling environment; enhances plasticity [3] | Colorectal, pancreatic cancer | |
| Acidic pH | Contributes to therapy resistance; alters CSC metabolism [3] | Multiple solid tumors |
Spatial analysis of CSC distribution reveals that niches are not randomly organized within tumors. CSCs with high clonal formation and invasion capabilities predominantly localize at the invasive frontier of tumors, where extracellular matrix (ECM) stiffness is significantly higher compared to the tumor core [3]. This spatial organization is functionally important, as mechanical factors like matrix stiffness can trigger stemness in non-stem cancer cells and regulate CSC marker expression [3]. The biomechanical properties of the niche, therefore, represent a crucial regulatory element in CSC biology.
Experimental Models and Methodologies for Studying CSC Niches
Key Experimental Protocols
Research into CSC-niche interactions employs specialized methodologies to isolate CSCs, model their microenvironment, and track dynamic behaviors:
CSC Isolation and Identification: The gold standard for CSC identification combines sphere colony formation assays with in vivo xeno transplantation of tumor cells into immunodeficient mice [8]. Fluorescence-Activated Cell Sorting (FACS) and Magnetic-Activated Cell Sorting (MACS) are routinely used to isolate CSCs based on surface markers such as CD44, CD133, EpCAM, and ALDH activity [9]. For instance, as few as 100 CD44+/CD24- cells can initiate tumors in immunocompromised mice, demonstrating their tumor-initiating capacity [1] [9].
Spatiotemporal Imaging of CSC Niches: Ultra-wide field microscopy enables tracking of thousands of individual cells over several days using stemness reporters such as pALDH1A1:mNeptune [5]. This approach allows for single-cell tracking and analysis of phenotypic transitions, revealing that CSC reprogramming is influenced by the phenotypic state of neighboring cells—promoted by CSCs and inhibited by differentiated cancer cells in the immediate vicinity [5].
3D Organoid and Co-culture Models: 3D organoid systems recapitulate the tumor microenvironment by incorporating stromal components such as CAFs and immune cells alongside CSCs [2]. These models permit the investigation of niche-mediated therapy resistance and metabolic symbiosis in conditions that mimic in vivo settings.
The following diagram illustrates a representative experimental workflow for analyzing CSC-niche interactions:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Research Reagents for CSC Niche Studies
| Reagent/Category | Specific Examples | Experimental Function | Key Applications |
|---|---|---|---|
| CSC Markers | CD44, CD133, ALDH, EpCAM | Isolation and identification of CSC populations | FACS/MACS sorting; immunohistochemistry |
| Stemness Reporters | pALDH1A1:mNeptune | Visualization of stem-like phenotypes in live cells | Real-time tracking of phenotypic transitions [5] |
| Niche Modeling Components | Type I Collagen, Laminin, Fibronectin | Recapitulation of ECM stiffness and composition | 3D organoid cultures; invasion assays [3] |
| Signaling Pathway Modulators | Wnt/β-catenin antagonists (sFRP4), Notch inhibitors | Dissection of niche signaling mechanisms | Functional studies of stemness pathways [1] |
| Cytokine/Chemokine Assays | IL-6, BDNF, NGF, CCL5 detection kits | Analysis of niche-derived paracrine signals | Evaluation of CSC-stroma crosstalk [5] [3] |
Signaling Pathways in CSC Niche Maintenance
Several evolutionarily conserved signaling pathways play critical roles in mediating niche signals that regulate CSC self-renewal, plasticity, and therapy resistance. The following diagram illustrates the key pathways and their interconnections:
The Wnt/β-catenin pathway demonstrates particular importance in niche signaling. Upregulation of Wnt/β-catenin promotes expression of stemness markers (CD44, ALDH) and drug resistance transporters (ABCG2, ABCC4) in head and neck squamous cell carcinoma [1]. This pathway can be counteracted using sFRP4, a Wnt antagonist that reverses both drug resistance and epithelial-to-mesenchymal transition (EMT) markers [1].
Hypoxia-inducible factors (HIFs), especially HIF-1α, serve as master regulators of the niche response to low oxygen tension. HIF activation promotes CSC proliferation, self-renewal, and tumorigenicity while upregulating surface markers like CD133 and CD44 [8]. The hypoxic niche protects CSCs from DNA damage caused by oxidative stress and contributes to therapy resistance, as radiation has been shown to double HIF-1 activity within 24-48 hours post-exposure [8].
Notch and Hedgehog signaling pathways additionally contribute to niche-mediated CSC maintenance. In breast CSCs and oral squamous cell carcinoma, Notch signaling promotes self-renewal and controls expression of EMT regulators like SLUG and TWIST [1]. Hedgehog pathway overexpression maintains self-renewal in lung squamous cell carcinoma, glioma, colon, and breast cancers through regulation of pluripotency factors OCT4, SOX2, and BMI1 [1].
Role of the CSC Niche in Therapy Resistance and Metastasis
Therapy Resistance Mechanisms
CSC niches contribute to treatment failure through multiple interconnected mechanisms:
Physical Protection: The ECM in CSC niches physically shelters CSCs from therapeutic agents [1]. Increased matrix stiffness from collagen and laminin deposition enhances this protective effect [3].
Metabolic Adaptations: Hypoxic conditions within niches shift CSCs toward anaerobic glycolysis, reducing dependence on mitochondrial function and decreasing susceptibility to oxidative stress-induced damage [8].
Enhanced DNA Repair: CSCs in specialized niches exhibit preferential activation of DNA damage response pathways. Following radiation treatment in glioblastoma, CSC populations increased 2-4-fold due to enhanced DNA repair capabilities [1].
Immune Evasion: Niches create immune-privileged sites through multiple strategies, including upregulated immune checkpoint proteins (PD-L1, B7-H4), recruitment of immunosuppressive cells (Tregs, MDSCs), and reduced MHC class I expression [6].
Cellular Plasticity: Under therapeutic pressure, non-CSCs can dedifferentiate into CSC-like states through niche-mediated signals. This plasticity represents a major mechanism of acquired resistance [6].
Metastatic Dissemination
The CSC niche plays a critical role in metastatic progression by regulating the behavior of metastatic stem cells (MetSCs)—disseminated cancer cells capable of reinitiating tumor growth in distant tissues [7]. Key niche functions in metastasis include:
Dormancy Regulation: Niches maintain disseminated tumor cells (DTCs) in a quiescent, non-proliferative state that is resistant to conventional antimitotic therapies [7]. Bone marrow niches particularly excel at maintaining this dormant state.
Pre-metastatic Niche Formation: CSCs prime future metastatic sites by secreting factors that create a supportive microenvironment before arrival of disseminated cells [7] [3].
Stemness Maintenance at Secondary Sites: Successful metastases require maintenance of CSC properties in foreign microenvironments. CD44+ gastric CSCs demonstrate self-renewal and differentiation capacity that enables establishment of secondary tumors [9].
Table 3: Biomarker Validation Across Cancer Types and Clinical Implications
| Biomarker | Cancer Types | Role in Therapy Resistance | Association with Metastasis |
|---|---|---|---|
| CD44 | Breast, colorectal, pancreatic, gastric, ovarian [9] | High expression associated with chemoresistance; CD44v isoforms increase tumor initiation frequency in gastric cancer [9] | CD44+ populations show enhanced metastatic potential in xenograft models [9] |
| CD133 | Glioblastoma, hepatocellular carcinoma, colon, ovarian [9] | CD133+ cells exhibit increased chemo- and radioresistance in glioblastoma [1] [9] | CD133+CD44+ population in HCC produces intrahepatic and lung metastases [9] |
| ALDH | Head and neck SCC, breast, ovarian [9] | ALDH activity confers resistance to chemotherapeutic agents through detoxification [9] | ALDHhighCD44+ cells mediate metastatic capability in breast cancer [9] |
| EpCAM | Breast, colon, HCC, pancreatic [9] | EpCAM+ CSCs contribute to therapy resistance and recurrence | EpCAM+/CD133+ HCC cells demonstrate metastatic stem cell properties [9] |
Concluding Perspectives and Future Directions
The CSC niche represents a compelling therapeutic target for overcoming treatment resistance and preventing metastatic spread across cancer types. Future research directions should focus on:
Therapeutic Targeting of Niche Components: Strategies including niche-disrupting agents, immune checkpoint modulators specific to CSCs, and metabolic reprogramming approaches hold promise for clinical translation [2] [6].
Biomarker Validation: While markers like CD44, CD133, and ALDH have been established across multiple cancers, further validation is needed to address tumor-type specificities and functional heterogeneity [10] [9].
Advanced Modeling Techniques: Integrating single-cell sequencing, spatial transcriptomics, and AI-driven multiomics analysis will provide unprecedented resolution of niche architecture and function [2].
Dual-Targeting Approaches: Combining CSC-directed therapies with conventional treatments may prevent the repopulation of tumors from therapy-resistant CSCs, addressing the fundamental challenge of relapse [9].
Understanding the complex heterogeneity of CSC niches remains a prerequisite for designing superior therapeutic strategies that target both CSCs and their supportive microenvironments. As research continues to unravel the dynamic interplay between CSCs and their niches, new opportunities will emerge for developing more effective combination therapies aimed at eliminating the root causes of treatment failure and metastasis.
The cancer stem cell (CSC) paradigm has revolutionized our understanding of tumor development, progression, and therapeutic resistance. CSCs constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [2] [11]. Despite substantial progress in characterizing CSC biology, the field faces a fundamental obstacle: the lack of universally reliable CSC biomarkers and significant tissue-specific variation in marker expression [2]. This dual challenge impedes consistent identification, isolation, and targeting of CSCs across different cancer types, presenting a critical bottleneck in both basic research and clinical translation.
The absence of universal biomarkers stems from the profound molecular heterogeneity of CSCs and their dynamic nature. CSCs represent reversible states along developmental and treatment-induced trajectories rather than a fixed, intrinsic phenotype [12]. Their identity is shaped by both intrinsic genetic programs and extrinsic cues from the tumor microenvironment [2]. Furthermore, stem-like features can be acquired de novo by non-CSCs in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure, indicating that CSCs may represent a dynamic functional state rather than a static subpopulation [2]. This plasticity fundamentally challenges the notion of a fixed CSC hierarchy and highlights the necessity for context-specific, function-based approaches in CSC research and therapy development.
Current Landscape of CSC Biomarkers: A Comparative Analysis
Established Markers and Their Limitations
The quest for reliable CSC biomarkers has predominantly focused on cell surface proteins, enzymatic activity, and functional characteristics. The table below summarizes the most widely utilized CSC markers across different cancer types, highlighting their tissue-specific expression patterns and limitations.
Table 1: Established CSC Biomarkers Across Different Cancer Types
| Biomarker | Cancer Types with Reported Expression | Key Limitations | Functional Role |
|---|---|---|---|
| CD44 | Breast, pancreatic, prostate, colorectal, head and neck | Also expressed on normal stem cells and activated lymphocytes [2] | Cell adhesion, hyaluronan receptor, activates pro-survival signaling [13] |
| CD133 | Glioblastoma, colon, pancreatic, liver | Expression varies with tumor stage and hypoxia; not cancer-specific [2] [14] | Membrane glycoprotein, modulates autophagy and stemness maintenance |
| ALDH1 | Breast, lung, colon, ovarian, pancreatic | Multiple isoforms with tissue-specific expression patterns [13] | Detoxifying enzyme, retinoic acid metabolism, drug resistance [11] |
| EpCAM | Colorectal, pancreatic, prostate, ovarian | Expression influenced by epithelial-mesenchymal transition (EMT) [2] | Epithelial cell adhesion, Wnt signaling modulation |
| LGR5 | Colorectal, gastric, intestinal cancers | Limited to specific tissue types; marks normal stem cells [2] | Wnt pathway receptor, maintains stem cell identity |
| CD44v6 | Colorectal, pancreatic, gastric | Specific isoform requiring specialized detection methods | Metastasis promotion, growth factor receptor signaling |
The fundamental limitation of these markers is their lack of exclusivity to CSCs. As noted in recent research, "although surface proteins such as CD44 and CD133 have been widely used to isolate CSC populations, these markers are not exclusive to CSCs and are often expressed in normal stem cells (NSCs) or non-tumorigenic cancer cells" [2]. This creates significant challenges in distinguishing CSCs from normal tissue stem cells during therapeutic interventions, raising concerns about potential on-target, off-tumor toxicity.
Tissue-Specific Variation in CSC Marker Expression
The expression of CSC markers demonstrates remarkable variation across different tissue types and cancer lineages, reflecting the influence of tissue origin and microenvironmental context on CSC phenotypes. The table below illustrates this tissue-specific variation, emphasizing how marker utility depends heavily on cancer type.
Table 2: Tissue-Specific Variation in CSC Marker Expression Patterns
| Cancer Type | Primary CSC Markers | Secondary/Context-Dependent Markers | Notes on Heterogeneity |
|---|---|---|---|
| Breast Cancer | CD44+/CD24-/low, ALDH1+ [2] | EpCAM, SOX2 | CD44+/CD24- and ALDH1+ populations partially overlap |
| Glioblastoma | CD133+, Nestin+, SOX2+ [2] | SSEA-1, L1CAM, A2B5 | Marker expression influenced by hypoxia and vascular niches |
| Colorectal Cancer | LGR5+, CD133+, CD44+ [2] | CD166, EpCAM, ALDH1 | Spatial heterogeneity along crypt-axis and tumor regions |
| Pancreatic Cancer | CD133+, CD44+, CXCR4+ | c-Met, ALDH1, ESA | Markers associated with metastatic potential and therapy resistance |
| Prostate Cancer | CD44+, CD133+, ITGA2+ | ALDH1, Trop2 | Marker expression changes with disease progression to castration resistance |
| Lung Cancer | CD133+, CD44+, ALDH1+ | SOX2, Oct-4 | Lineage-specific variations between NSCLC and SCLC |
| Melanoma | ABCB5+, CD271+ | ALDH1, JARID1B | Dynamic marker expression influenced by microenvironment |
This tissue-specific variation presents substantial challenges for developing pan-cancer CSC targeting strategies. For instance, glioblastoma CSCs frequently express neural lineage markers such as Nestin and SOX2, whereas gastrointestinal cancers may harbor CSCs characterized by LGR5 or CD166 expression [2]. This diversity suggests that CSC identity is shaped by both cell-of-origin signatures and adaptation to local microenvironmental niches.
Methodological Approaches for CSC Identification and Validation
Standard Experimental Protocols
Overcoming the challenges of CSC biomarker validation requires rigorous methodological approaches that combine surface marker analysis with functional validation. The following experimental protocols represent the current gold standards in the field.
Table 3: Core Methodologies for CSC Identification and Validation
| Method Category | Specific Protocol | Key Output Measures | Technical Considerations |
|---|---|---|---|
| Surface Marker-Based Isolation | Flow cytometry with antibody conjugates (e.g., CD44-APC/CD24-PE) | Percentage of marker-positive population, intensity of expression | Requires appropriate isotype controls and compensation panels [13] |
| Functional Assays | Sphere formation in serum-free, non-adherent conditions [13] | Number and size of primary and secondary spheres | Passage number affects stemness properties; matrix composition influences results |
| Enzymatic Activity Assays | Aldefluor assay for ALDH activity [13] | ALDH-high population percentage, inhibition by DEAB | Enzyme activity varies with cell cycle and metabolic state |
| In Vivo Validation | Limiting dilution transplantation in immunocompromised mice [11] [13] | Tumor-initiating cell frequency, tumor latency, histology | Strain selection (NSG > NOD/SCID > SCID) significantly impacts engraftment rates |
| Clonal Lineage Tracing | Lentiviral barcoding and sequencing | Phylogenetic trees of tumor evolution, stem cell dynamics | Requires single-cell sequencing and bioinformatic reconstruction |
The integration of these complementary approaches is essential for comprehensive CSC characterization. As emphasized in recent methodological reviews, "the gold standard for CSC validation remains in vivo tumorigenicity assays, wherein sorted cells are injected into immunocompromised mice to evaluate their tumor-initiating potential" [13]. This functional validation is particularly crucial given the limitations of surface markers alone.
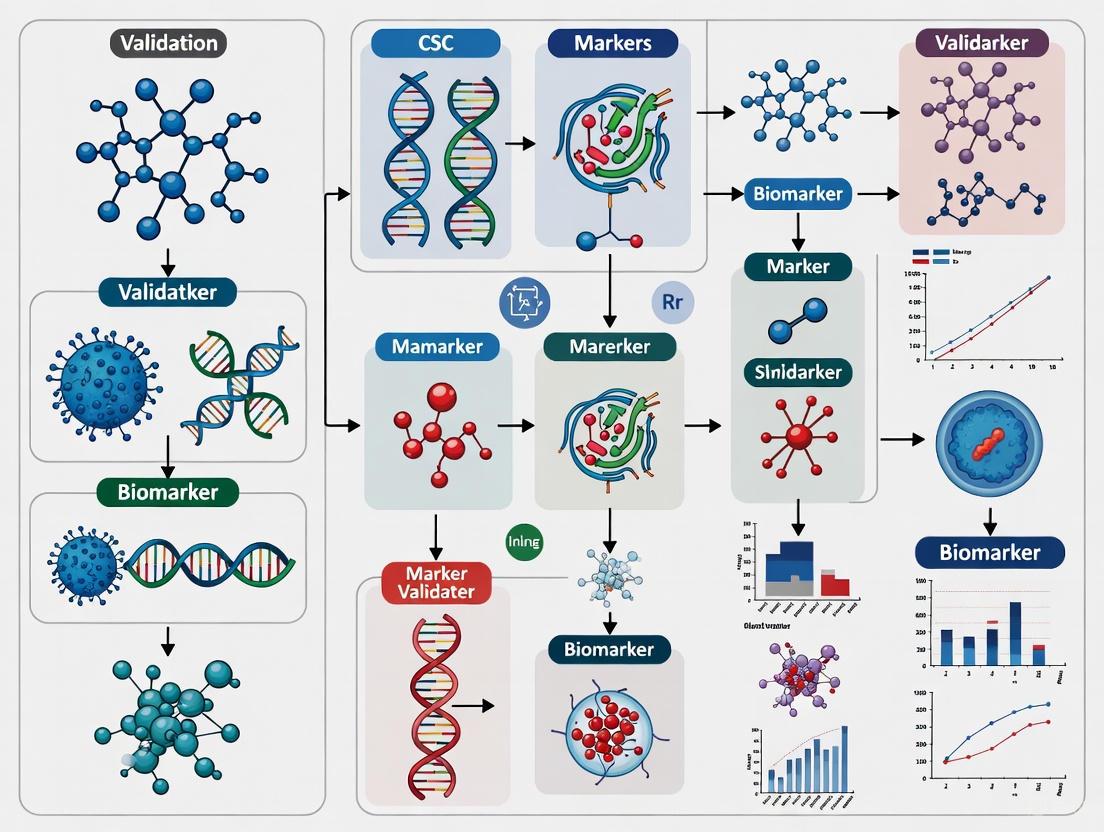
CSC Validation Workflow
The diagram below illustrates the integrated experimental workflow for CSC identification and validation, combining multiple methodological approaches to overcome the limitations of individual techniques.
Emerging Technologies and Future Directions
Advanced Approaches for CSC Characterization
Novel technological platforms are increasingly enabling researchers to move beyond traditional surface markers and embrace a more dynamic, functional definition of CSCs. Single-cell RNA sequencing (scRNA-seq) has transformed our understanding of tumor biology by enabling high-resolution profiling of rare subpopulations (<5%) and revealing the functional heterogeneity that contributes to treatment failure [12]. Supported by advanced bioinformatics tools, these approaches now enable the dynamic characterization of CSC potential at unprecedented resolution.
Table 4: Computational Tools for CSC Stemness Assessment
| Tool Name | Algorithm Basis | Application Context | Key Advantages |
|---|---|---|---|
| CytoTRACE | Gene counts and expression | Developmental potential inference | Marker-free approach, web server available [12] |
| StemID | Shannon entropy | Stemness quantification from scRNA-seq | Identifies intermediate cell states [12] |
| SCENT | Signaling entropy | Cell potency and differentiation potential | Uses protein-protein interaction networks [12] |
| mRNAsi | Machine learning | Stemness index based on transcriptome | Pan-cancer application, TCGA-compatible [12] |
| StemSC | Relative expression orderings | Stemness comparison across samples | Robust to batch effects and normalization [12] |
| scEpath | Energy landscape modeling | Inference of transition probabilities | Models epigenetic barriers between states [12] |
These computational approaches are particularly valuable because they "enable the dynamic characterization of CSC potential at unprecedented resolution" and challenge the traditional view of CSCs as "rare but static entities," suggesting instead that "stemness might be a rather dynamic, context-dependent state" [12].
Research Reagent Solutions for CSC Studies
The table below outlines essential research tools and reagents critical for advancing CSC biomarker discovery and validation efforts.
Table 5: Essential Research Reagent Solutions for CSC Studies
| Reagent Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| Validated Antibody Panels | CD44-PE, CD24-FITC, CD133/1-APC | Flow cytometry, immunofluorescence | Clone validation across species, titration for specific applications |
| ALDH Activity Detection | Aldefluor Kit, DEAB inhibitor | Functional CSC identification | Optimization for different cell types, viability controls |
| 3D Culture Matrices | Matrigel, synthetic hydrogels | Sphere formation assays, organoid culture | Batch-to-batch variability, growth factor composition |
| CSC Functional Assay Kits | SphereCulture Medium, Extreme Limiting Dilution Analysis software | Self-renewal quantification | Serum-free formulation, growth factor supplementation |
| Single-Cell Multi-omics Kits | 10x Genomics Chromium, Parse Biosciences | High-resolution CSC profiling | Cell viability requirements, sequencing depth requirements |
| In Vivo Validation Models | NSG mice, patient-derived xenografts | Tumor-initiating cell assessment | Ethical considerations, engraftment timeframes |
The fundamental challenge of universal CSC biomarkers persists due to the dynamic nature of CSCs, their phenotypic plasticity, and extensive tissue-specific variation. No single marker or methodology currently suffices for comprehensive CSC identification across cancer types. The most promising path forward involves integrated approaches that combine multiple surface markers with functional assays and in vivo validation, while leveraging emerging single-cell technologies and computational tools.
Future efforts should focus on developing tissue-specific biomarker panels validated through multi-institutional consortia, establishing standardized protocols for CSC assessment, and creating reference databases that capture the dynamic spectrum of CSC states across different cancer types. As the field moves toward these goals, acknowledging and systematically addressing the core challenge of biomarker variability remains essential for advancing both basic CSC biology and the development of effective CSC-targeted therapies.
Established and Emerging CSC Surface Markers (CD44, CD133, ALDH1, EpCAM)
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [2]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies [2]. The clinical detection and targeting of CSCs represent a major challenge in oncology, primarily due to the lack of specific and reliable biomarkers [15].
The identification of CSCs largely relies on specific surface markers that enable their isolation and characterization. Among the most widely studied are CD44, CD133, ALDH1, and EpCAM [13]. However, these markers are not universal across cancer types, and their expression varies significantly depending on tissue origin and microenvironmental context [2]. This comparative guide provides an objective analysis of these four established and emerging CSC surface markers, presenting experimental data and methodologies to aid researchers in selecting appropriate markers for specific cancer types and research applications.
Marker Comparison Tables
Table 1: Key Characteristics of Established and Emerging CSC Markers
| Marker | Full Name | Primary Function | Common Cancers | Cellular Localization |
|---|---|---|---|---|
| CD44 | Cluster of Differentiation 44 | Cell surface glycoprotein receptor for hyaluronic acid; involved in cell adhesion, migration, metastasis [16] | Breast, HNSCC, Prostate, Pancreatic [16] | Cell membrane [16] |
| CD133 | Prominin-1 | Pentaspan transmembrane glycoprotein; function not fully understood, associated with stem cell maintenance [15] | NSCLC, Colon, Glioblastoma [15] | Cell membrane protrusions [15] |
| ALDH1 | Aldehyde Dehydrogenase 1 | Cytosolic enzyme; oxidizes retinol to retinoic acid in early stem cell differentiation [16] | Breast, HNSCC, Lung, Pancreatic [16] [17] | Cytoplasm [16] |
| EpCAM | Epithelial Cell Adhesion Molecule | Calcium-independent epithelial cell adhesion molecule [2] | Prostate, Colorectal, Pancreatic [2] | Cell membrane [2] |
Table 2: Prognostic Value and Experimental Detection Methods
| Marker | Prognostic Value | Key Experimental Assays | Detection Reagents |
|---|---|---|---|
| CD44 | Independent prognostic factor for PFS and OS in breast cancer; higher expression in triple-negative vs luminal subtypes [18] | Flow cytometry, IHC, serum ELISA [16] [18] | Anti-CD44 antibodies (Biogenex DF1485) [16] |
| CD133 | Limited prognostic value in NSCLC; glycosylation-specific epitopes (AC133) may be more relevant [15] | Flow cytometry, IHC, lectin-based glycosylation detection [15] | Anti-CD133-APC antibodies (Beckman Coulter C15190) [15] |
| ALDH1 | Correlates with poor prognosis in HNSCC; higher expression in dysplastic OPMDs and OSCC [16] | Aldefluor assay, IHC, flow cytometry [16] [13] | Anti-ALDH1A1 antibodies (Bio SB Clone EP168) [16] |
| EpCAM | Target for CAR-T therapy in prostate cancer; demonstrated effectiveness in preclinical models [2] | Flow cytometry, IHC, CAR-T functional assays [2] | Anti-EpCAM-APC antibodies (Miltenyi 130-109-764) [15] |
Table 3: Functional Roles in Cancer Progression
| Marker | Role in Tumorigenesis | Role in Metastasis | Therapeutic Resistance Mechanisms |
|---|---|---|---|
| CD44 | High CD44/CD24 ratio correlates with strong proliferative capacity and tumorigenicity [17] | CD44 staining index higher in OSCC without lymph node metastasis [16] | Enhances drug efflux, DNA repair capacity, and interaction with tumor microenvironment [11] |
| CD133 | Putative role in tumor initiation; expression associated with tumorigenic capacity [15] | Contributes to metastatic potential through glycosylation patterns [15] | Associated with resistance to conventional chemotherapy in NSCLC [15] |
| ALDH1 | ALDH1+ population indicates malignancy but less directly linked to tumorigenesis than CD44 [17] | Stronger indicator for cell migration and metastasis than CD44 [17] | Detoxifies chemotherapeutic agents; mediates resistance via ALDH1 activity [11] |
| EpCAM | Contributes to tumor initiation through cell adhesion and signaling pathways [2] | Facilitates metastatic spread through epithelial cell adhesion mechanisms [2] | Not well-characterized for therapeutic resistance specifically |
Experimental Protocols for CSC Marker Analysis
Flow Cytometry and Cell Sorting
Protocol Purpose: Isolation and quantification of CSC subpopulations based on surface marker expression.
Workflow Description: The process begins with creating a single-cell suspension from cultured cells or dissociated tumor tissue. Cells are then incubated with fluorescently-conjugated antibodies targeting specific CSC markers (e.g., anti-CD44-APC, anti-CD133-APC). For ALDH1 detection, the Aldefluor assay is employed, where cells are incubated with a fluorescent ALDH substrate. Viable cells are selected by excluding dead cells with propidium iodide staining. Finally, analysis and sorting are performed using instruments like BD FACSAria III cell sorters, with data analysis conducted using specialized software such as Kaluza [15] [13].
Immunohistochemical Staining
Protocol Purpose: Detection of CSC markers in formalin-fixed paraffin-embedded (FFPE) tissue sections.
Detailed Methodology:
- Sectioning: Cut 3-4 μm sections from FFPE tissue blocks and mount on silane-coated slides.
- Deparaffinization: Bake slides at 56°C for 2 hours, followed by dewaxing in xylene and rehydration through graded alcohol series.
- Antigen Retrieval: Perform heat-induced epitope retrieval using 10 mM citrate buffer (pH 6) in an autoclave at 121°C for 30 minutes.
- Blocking: Block endogenous peroxidase activity with 3% hydrogen peroxide for 10 minutes.
- Primary Antibody Incubation: Apply prediluted primary antibodies (CD44, ALDH1A1, etc.) for 60 minutes in a humidifying chamber.
- Detection: Incubate with appropriate secondary antibodies followed by 3,3'-diaminobenzidine-tetrahydrochloride (DAB) chromogen substrate.
- Counterstaining: Counterstain with Mayer's hematoxylin for 3 minutes, then mount and evaluate under microscopy [16].
Functional Assessment: Clonogenic Assay
Protocol Purpose: Evaluation of self-renewal capacity of sorted CSC populations.
Method Details: After sorting based on marker expression, seed cells in ultra-low attachment 96-well plates at decreasing cell densities (1000, 100, 10, and 1 cell per well) in defined serum-free medium. Culture for 4-8 weeks, adding 50 μL of fresh medium weekly. Quantify sphere formation per well using optical microscopy, imaging spheroids every 7 days. Measure spheroid size using ImageJ software to assess self-renewal capacity [15].
CSC Marker Signaling Pathways
Research Reagent Solutions
Table 4: Essential Research Reagents for CSC Marker Studies
| Reagent Type | Specific Examples | Application | Experimental Function |
|---|---|---|---|
| Antibodies | Anti-CD44 (Biogenex DF1485), Anti-ALDH1A1 (Bio SB Clone EP168), Anti-CD133-APC (Beckman Coulter C15190), Anti-EpCAM-APC (Miltenyi 130-109-764) [15] [16] | IHC, Flow Cytometry | Specific detection and isolation of CSC subpopulations |
| Cell Sorting Kits | CELLection Biotin Binder Kit (Invitrogen-ThermoFisher) [15] | Magnetic Cell Sorting | Isolation of marker-specific cell populations using magnetic separation |
| Detection Assays | Aldefluor Kit (StemCell Technologies) [13] | ALDH Activity Detection | Functional assessment of ALDH enzyme activity in live cells |
| Cell Culture Supplies | Ultra-low attachment plates (Falcon Corning), Defined serum-free medium [15] | Spheroid Formation Assays | Assessment of self-renewal capacity under non-adherent conditions |
Discussion
Comparative Analysis of Marker Utility
The established and emerging CSC markers present distinct advantages and limitations across different cancer types. CD44 demonstrates significant prognostic value, particularly in breast cancer, where high serum levels correlate with aggressive subtypes and poorer outcomes [18]. Its role in tumorigenesis appears more pronounced than in metastasis, as evidenced by higher CD44 staining indices in OSCC without lymph node metastasis [16].
CD133, while historically important in CSC research, shows limitations in prognostic value for NSCLC, prompting investigations into glycosylation-specific epitopes that may offer greater clinical relevance [15]. The AC133 epitope, selectively expressed in CSCs but masked in differentiated tumor cells, represents a promising direction for improved detection specificity [15].
ALDH1 serves as a functional marker with particular strength in identifying metastatic potential. Research indicates it may be a stronger indicator for cell migration and metastasis than CD44, though its role in tumorigenesis appears less direct [17]. In head and neck cancers, ALDH1 shows promise as a specific marker for dysplasia and malignant progression [16].
EpCAM has emerged as a valuable target for therapeutic applications, particularly in CAR-T cell approaches for prostate cancer [2]. Its role in cell adhesion mechanisms makes it particularly relevant for understanding metastatic spread.
Emerging Approaches and Research Directions
Current challenges in CSC marker research include the lack of universal biomarkers, dynamic plasticity of CSCs, and context-dependent expression patterns [2]. Emerging technologies are addressing these limitations through several innovative approaches:
Glycosylation-Based Detection: Novel methodologies using lectin combinations (UEA-1 and GSL-I) that recognize specific CSC glycan patterns show promise for improved specificity over conventional markers like CD133. This approach has demonstrated prognostic value for overall survival in early-stage NSCLC patients [15].
Multi-Marker Strategies: Research indicates that combining markers (e.g., high CD44/CD24 ratio with ALDH1+) provides more reliable CSC characterization than single markers alone [17]. This approach accounts for the heterogeneity and plasticity of CSC populations.
Advanced Detection Platforms: Cutting-edge technologies including single-cell sequencing, spatial transcriptomics, and AI-driven multiomics analysis are refining CSC characterization and enabling precision medicine applications [2] [13]. Circulating tumor cell analysis and liquid biopsy approaches are also being explored for non-invasive CSC monitoring [18].
The continued refinement of CSC surface markers and detection methodologies remains crucial for advancing our understanding of cancer biology and developing targeted therapeutic strategies to overcome treatment resistance and improve patient outcomes.
The Impact of CSC Plasticity and Dynamic Phenotypic States on Biomarker Stability
The cancer stem cell (CSC) hypothesis has revolutionized our understanding of tumorigenesis, positioning a small subpopulation of cells with self-renewal capacity as the primary drivers of tumor initiation, progression, metastasis, and therapeutic resistance [2] [19]. The reliable identification and targeting of CSCs have consequently emerged as paramount goals in oncology research. This pursuit heavily depends on CSC biomarkers—specific surface proteins, enzymatic activities, and molecular signatures that enable the isolation and study of these cells [20] [13].
However, a fundamental complication arises from the intrinsic plasticity of CSCs—their ability to dynamically switch between phenotypic states in response to environmental cues, therapeutic pressure, and interactions with the tumor microenvironment (TME) [21] [12]. This plasticity challenges the very concept of a stable biomarker, as the molecular identity of CSCs is not fixed but is instead a fluid and context-dependent property [2] [22]. This review objectively compares the stability and reliability of established and emerging CSC biomarkers across different cancer types, framing this analysis within the broader thesis of validating CSC biomarkers for clinical application. We synthesize experimental data to elucidate how phenotypic plasticity directly impacts biomarker expression, with critical implications for diagnostic accuracy, therapeutic targeting, and drug development.
Comparative Analysis of Established CSC Biomarker Stability
The stability of traditional CSC biomarkers is not absolute but varies significantly across cancer types and under different selective pressures. The table below summarizes the stability profiles of key biomarkers based on current experimental evidence.
Table 1: Stability Profile of Established CSC Biomarkers Across Cancer Types
| Biomarker | Primary Cancer Types | Reported Stability | Key Influencing Factors | Functional Role |
|---|---|---|---|---|
| CD44 | Breast, Pancreatic, Prostate, Colorectal, HNSCC [20] [13] | Moderate-High (but functionally heterogeneous) | Hypoxia, TGF-β signaling, HA-rich niche [13] | Cell adhesion, migration, hyaluronan binding, pro-survival signaling [20] |
| CD133 (Prominin-1) | Glioblastoma, Colon, Pancreatic, Breast [20] | Low-Moderate (highly dynamic) | Chemotherapy, tumor dissociation, metabolic stress [12] [20] | Membrane protrusion organization, cholesterol interaction [20] |
| ALDH1 | Breast, Lung, Ovarian, Bladder [13] | Moderate (functional activity) | Retinoic acid signaling, oxidative stress, chemotherapy [13] [19] | Detoxifying enzyme, retinoic acid metabolism, oxidative stress response [13] |
| EpCAM | Prostate, Colorectal, Pancreatic [2] [13] | High (but subject to cleavage) | EMT, inflammatory cytokines [2] | Cell adhesion, proliferation, and migration signaling [2] |
| CD90 (Thy-1) | Liver, Brain, Colorectal, TNBC [20] | Moderate | β3 integrin, AMPK/mTOR signaling [20] | Cell-cell and cell-matrix interactions, potential immune modulatory role [20] |
The data reveals a core dilemma: while biomarkers like CD44 and EpCAM show relatively stable expression, their presence does not always correlate with a functional CSC state due to heterogeneity within the positive population. Conversely, markers like CD133 exhibit significant dynamism, where their expression can be rapidly induced or lost, making them unreliable for tracking CSCs over time or after therapy [12] [20].
Experimental Dissection of Biomarker Dynamics: Methodologies and Data
Understanding the factors that govern biomarker stability requires sophisticated experimental models that can capture cellular dynamics. The following protocols and resulting data highlight how plasticity directly impacts biomarker readouts.
Experimental Protocol 1: Inducing Plasticity via Therapy Exposure
Objective: To quantify changes in canonical CSC biomarker expression in response to conventional chemotherapy. Methodology:
- Cell Model: Patient-derived organoids (PDOs) from triple-negative breast cancer (TNBC) or pancreatic ductal adenocarcinoma (PDAC) [12] [13].
- Treatment Regimen: Organoids are treated with a clinically relevant dose of gemcitabine (for PDAC) or paclitaxel (for TNBC) for 72 hours. A control group is maintained in parallel with vehicle treatment [21].
- Analysis:
- Flow Cytometry: Pre- and post-treatment cells are stained for CD44, CD24, CD133, and ALDH1 (via Aldefluor assay). The frequency of marker-positive populations (e.g., CD44+CD24–, CD133+, ALDH1high) is quantified [13].
- Functional Validation: Sorted populations pre- and post-therapy are subjected to in vivo limiting dilution assays in immunocompromised mice to measure tumor-initiating cell (TIC) frequency [13].
- Single-Cell RNA Sequencing (scRNA-seq): A subset of cells is processed for scRNA-seq to profile transcriptomic changes associated with therapy resistance and state transitions [12].
Hypothetical Data & Interpretation: Table 2: Biomarker Flux in PDAC Organoids Post-Gemcitabine Treatment
| Cell Population | Pre-Treatment Frequency (%) | Post-Treatment Frequency (%) | Fold Change in TIC Frequency |
|---|---|---|---|
| CD133+ | 2.1 ± 0.5 | 8.5 ± 1.2 | 4.8x |
| ALDH1high | 3.5 ± 0.7 | 12.3 ± 2.1 | 6.2x |
| CD44+CD24– | 1.8 ± 0.4 | 4.2 ± 0.9 | 3.5x |
| Double Negative (CD133–ALDH1low) | 92.6 ± 3.1 | 74.9 ± 5.4 | 1.0x (reference) |
This data would demonstrate that conventional therapy enriches for populations with high CSC biomarker expression and, more importantly, a functionally validated increase in tumor-initiating capacity. It indicates that biomarker expression can be induced in previously negative or low-expressing cells, a direct result of cellular plasticity [21] [12].
Experimental Protocol 2: Tracking State Transitions via EMT Induction
Objective: To map the relationship between epithelial-mesenchymal transition (EMT), a key plasticity program, and the stability of CSC biomarkers. Methodology:
- Induction System: Use a TGF-β-based in vitro model to induce EMT in a panel of epithelial cancer cell lines (e.g., from breast, lung) [21].
- Longitudinal Monitoring: Employ live-cell imaging of reporters for EMT transcription factors (e.g., Twist, Snail) and surface biomarkers (e.g., CD44-GFP, CD133-RFP) [21] [22].
- Multi-Omic Analysis: Perform scRNA-seq and ATAC-seq (Assay for Transposase-Accessible Chromatin with high-throughput sequencing) on cells at different stages of EMT to correlate chromatin accessibility with gene expression of CSC biomarkers [12].
- Functional Assays: At each time point, cells are assessed for sphere-forming capacity in vitro and tumorigenicity in vivo.
Hypothetical Data & Interpretation: The data would likely show a heterogeneous and transient response to TGF-β. A subset of cells would successfully undergo a full EMT, characterized by downregulation of epithelial markers (E-cadherin) and upregulation of mesenchymal markers (vimentin, N-cadherin). This transition would be temporally correlated with a gradual upregulation of CD44 and induction of CD133, while other markers like EpCAM may be downregulated. scRNA-seq would reveal distinct clusters along the EMT spectrum, with the "partial EMT" or "hybrid E/M" state showing the highest expression of a core stemness signature and the greatest sphere-forming efficiency, supporting the model that plasticity, not a fixed state, underpins the CSC phenotype [21] [12].
Molecular Mechanisms Linking Plasticity to Biomarker Instability
The experimental data on biomarker dynamism can be explained by several underlying molecular mechanisms. The following diagram synthesizes these pathways into a unified model of regulation.
Diagram 1: Mechanisms of biomarker instability. Extrinsic drivers rewire intrinsic molecular pathways, leading to unstable biomarker output and functional adaptation. TME: Tumor Microenvironment.
Epigenetic Reprogramming
CSCs exhibit extensive epigenetic plasticity that allows for rapid, reversible changes in gene expression without altering the DNA sequence. Hypoxia, a common feature of the TME, induces DNA methylation and histone modification changes that promote the expression of stemness genes like OCT4, SOX2, and NANOG, while simultaneously influencing the expression of surface markers like CD44 and CD133 [21] [19]. This reprogramming enables CSCs to adapt their molecular phenotype to survive stress, directly contributing to the transient nature of biomarker-based identification.
Alternative Splicing
Alternative splicing (AS) is a potent and rapid mechanism for proteome diversification. Dysregulation of splicing factors (e.g., SRSF1, SRSF3, hnRNPA1) is a common feature in cancer that drives plasticity [22]. For instance, splicing switches can generate isoforms of receptors and signaling molecules that promote a stem-like state. The expression of these splicing factors themselves is often altered by therapeutic stress or microenvironmental cues, creating a direct link between external pressures and the internal generation of CSC-associated protein variants, thereby destabilizing the definition of a "marker" [22].
Signaling Pathway Crosstalk
The core stemness-associated pathways—Wnt/β-catenin, Notch, and Hedgehog—are not isolated but engage in extensive crosstalk with each other and with pathways activated by the TME (e.g., TGF-β, JAK/STAT) [13] [19]. This integrated signaling network regulates the expression of CSC biomarkers. For example, Wnt signaling can directly transcriptionally activate CD44 expression, while Notch signaling can modulate the expression of CD133. The dynamic activity of these pathways in response to fluctuating signals ensures that biomarker expression remains a fluid readout of cellular state [2] [13].
The Scientist's Toolkit: Essential Reagents for Studying CSC Plasticity
Investigating the unstable nature of CSC biomarkers requires a specific set of research tools designed to capture dynamic cellular processes.
Table 3: Key Research Reagent Solutions for CSC Plasticity and Biomarker Studies
| Reagent / Solution | Function & Utility | Key Applications |
|---|---|---|
| Patient-Derived Organoids (PDOs) | 3D ex vivo models that preserve tumor heterogeneity, TME components, and patient-specific drug responses better than 2D cultures [2] [13]. | Modeling therapy-induced plasticity, longitudinal biomarker tracking, functional validation of TIC frequency. |
| Aldefluor Assay Kit | Fluorescent-based functional assay to detect cells with high aldehyde dehydrogenase (ALDH) enzyme activity, a CSC characteristic in many cancers [13]. | Isolation and analysis of ALDHhigh CSCs, tracking of ALDH1 activity shifts after perturbations. |
| CRISPR/dCas9 Epigenetic Editor Systems | Tools for targeted epigenetic manipulation (e.g., DNA methylation/demethylation, histone acetylation/deacetylation) at specific gene loci [12]. | Causally linking epigenetic changes at biomarker gene promoters to their expression stability and functional stemness. |
| Splicing Factor Inhibitors | Small-molecule inhibitors targeting dysregulated splicing factors (e.g., compounds against SRSF1) [22]. | Probing the role of specific AS events in driving biomarker variability and CSC plasticity. |
| CSC Pathway Modulators | Recombinant proteins (e.g., Wnt3a, Dll4) and small-molecule inhibitors (e.g., LGK974 for Wnt, GANT61 for Hedgehog) for manipulating core stemness pathways [13] [19]. | Experimentally controlling signaling pathways to observe resultant changes in biomarker expression and functional stemness. |
| Single-Cell Multi-Omic Kits | Commercial kits for parallel scRNA-seq and scATAC-seq from the same single cell, enabling coupled analysis of gene expression and chromatin accessibility [12]. | Deconvoluting heterogeneity, mapping trajectories of state transitions, and identifying regulators of biomarker instability. |
The compelling body of evidence synthesized in this review underscores a paradigm shift: CSC biomarkers are not static identifiers but dynamic outputs of a plastic cellular state. This inherent instability, driven by epigenetic, splicing, and signaling dynamics, poses a significant challenge for the validation of CSC biomarkers across cancer types. Relying on a single, fixed marker for diagnostic or therapeutic purposes is likely to fail, as it captures only a transient snapshot of a highly adaptable system.
The future of CSC research and drug development lies in embracing this complexity. This involves:
- Moving beyond static markers to functional signatures that integrate multiple omics layers (transcriptomic, epigenetic, proteomic) to define the CSC state.
- Utilizing computational tools and AI to analyze single-cell data and predict state transitions, identifying critical windows of vulnerability during phenotypic flipping [23] [12].
- Developing therapeutic combinations that simultaneously target the CSC state itself (e.g., via signaling pathway inhibition) and block the plasticity mechanisms that allow for escape (e.g., epigenetic modulators) [2] [19].
For researchers and drug development professionals, this implies that the next generation of biomarkers and targeted therapies must be designed against a backdrop of cellular dynamism. Success in eradicating CSCs and preventing relapse will depend not on finding a stable target, but on understanding and controlling the very processes that make these cells so notoriously evasive.
CSC-Immune System Crosstalk and Its Implications for Biomarker-Driven Immunotherapy
Cancer stem cells (CSCs) represent a specialized subpopulation of tumor cells with capabilities for self-renewal, differentiation, and tumor initiation, playing crucial roles in driving tumor recurrence, metastasis, and resistance to therapies [24] [25]. The interaction between CSCs and the immune system creates a dynamic microenvironment that profoundly influences therapeutic outcomes. CSCs actively shape an immunosuppressive tumor microenvironment (TME) through various mechanisms, including secretion of soluble factors, exosome-mediated communication, and metabolic reprogramming [24] [26]. Conversely, immune cells such as tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs) reciprocally support CSC stemness and maintenance [27] [6]. Understanding these complex interactions is paramount for developing effective biomarker-driven immunotherapies that can overcome CSC-mediated resistance and achieve durable therapeutic responses.
CSC Biomarkers: Landscape and Validation Across Cancer Types
The reliable identification of CSCs through specific biomarkers forms the foundation for targeted therapeutic approaches. However, the CSC biomarker landscape is marked by significant heterogeneity and contextual specificity.
Table 1: Established CSC Biomarkers Across Different Cancer Types
| Biomarker | Cancer Types | Cellular Localization | Functional Role | Specificity Challenges |
|---|---|---|---|---|
| CD44 | Breast, Colon, Glioblastoma, Prostate, Gastric, HNSCC | Cell Surface | Adhesion receptor, stemness maintenance | Expressed on non-stem cancer cells and healthy cells [25] [28] |
| CD133 | Breast, Liver, Lung, Ovarian, Glioblastoma, Sarcomas | Cell Surface Glycoprotein | Cholesterol binding, tumor initiation | Conserved but not universal across cancers [25] [27] |
| ALDH1 | Breast, Prostate, Colon, Lung, Ovarian | Intracellular Enzyme | Aldehyde dehydrogenase, detoxification | Activity-based marker, shared with normal stem cells [25] |
| ABCB5 | Melanoma | Cell Surface Transporter | Drug efflux, chemoresistance | Melanoma-specific [25] |
| ABCG2 | Lung, Pancreatic, Liver, Breast, Ovarian | Cell Surface Transporter | Multidrug resistance | Shared across multiple CSC types [25] |
| CD34 | Leukemia | Cell Surface | Hematopoietic stem cell marker | Limited to hematopoietic malignancies [25] |
| EpCAM | Prostate, Various Carcinomas | Cell Surface | Epithelial cell adhesion | CSC-specific CAR-T target [2] |
The Biomarker of Cancer Stem Cell Database (BCSCdb) serves as a comprehensive repository that systematically categorizes CSC biomarkers identified through both high-throughput and low-throughput methods [29]. This resource has compiled 171 low-throughput biomarkers validated in primary tissues (clinical biomarkers), 283 high-throughput markers validated by low-throughput methods, and 8,307 high-throughput markers, providing a valuable platform for biomarker validation across different cancer types [29]. Each biomarker in BCSCdb is assigned a confidence score based on experimental validation methods and a global score identifying CSC biomarkers across ten different cancer types, enabling researchers to prioritize targets with the strongest evidence [29].
A significant challenge in CSC biomarker development is the lack of universal specificity. Most identified surface markers are also expressed by non-stem cancer cells or healthy cells, albeit at different abundances [25] [2]. Furthermore, CSC markers exhibit considerable plasticity, with expression patterns shifting in response to environmental cues and therapeutic pressures [6] [12]. This dynamic nature necessitates multimodal biomarker approaches that combine surface markers with functional assays for reliable CSC identification across different cancer contexts.
Mechanisms of CSC-Immune Cell Crosstalk in the Tumor Microenvironment
The bidirectional communication between CSCs and immune cells creates a self-reinforcing immunosuppressive niche that protects CSCs from immune elimination and facilitates tumor progression.
CSC-Mediated Immunosuppression
CSCs employ multiple strategies to actively suppress antitumor immunity. They secrete soluble factors including immunosuppressive cytokines (TGF-β, IL-10), chemokines (CCL2, CCL5), and exosomes carrying bioactive molecules that recruit and reprogram immune cells toward immunosuppressive phenotypes [24] [26]. CSCs also modulate immune checkpoint expression, with elevated levels of PD-L1, B7-H4, B7-H3, CD47, and CD24 being reported across various CSC populations [6]. These checkpoints interact with corresponding receptors on immune cells to directly inhibit cytotoxic functions. Additionally, CSCs downregulate antigen-presentation machinery, particularly MHC class I molecules, reducing their visibility to CD8+ cytotoxic T cells [24] [6].
Immune Cell Regulation of CSC Stemness
Reciprocally, immune cells in the TME provide supportive signals that enhance CSC properties. TAMs promote CSC stemness through secretion of growth factors and cytokines such as IL-6, IL-10, and TGF-β, which activate STAT3 and NF-κB signaling pathways within CSCs [24] [26]. MDSCs contribute to CSC survival by secreting immunosuppressive cytokines (IL-10, TGF-β) and exosomes containing microRNAs (miR-21, miR-210) that enhance CSC self-renewal and chemoresistance [24]. Tregs further promote CSC-mediated tumor progression through cytokine secretion and cell-contact-dependent mechanisms, while CSC-secreted chemokines (CCL1, CCL5) specifically attract Tregs, creating a self-amplifying immunosuppressive loop [24] [28].
Figure 1: Bidirectional Crosstalk Between CSCs and Immune Cells. CSCs and immune cells engage in reciprocal communication through cytokines, chemokines, exosomes, and cell-surface interactions, creating an immunosuppressive niche that supports CSC maintenance and immune evasion.
Signaling Pathways Mediating CSC-Immune Interactions
The interplay between CSCs and immune cells is orchestrated by several critical signaling cascades. Wnt/β-catenin, Notch, Hedgehog, and PI3K/Akt/mTOR pathways have been identified as pivotal regulators of CSC-immune crosstalk [24] [27]. These pathways not only maintain CSC stemness but also influence immune cell function and polarization. For instance, the Wnt/β-catenin pathway in CSCs has been linked to T cell exclusion and resistance to checkpoint inhibitors, while Notch signaling regulates both CSC self-renewal and immune cell differentiation [27]. The plasticity of these interactions is further enhanced by epigenetic reprogramming that allows CSCs to dynamically adapt to immune pressure and therapeutic interventions [6].
Experimental Models and Methodologies for Studying CSC-Immune Interactions
Core Experimental Protocols
Research into CSC-immune interactions employs specialized methodologies that enable functional characterization of these rare cell populations and their immunological properties.
CSC Isolation and Enrichment: CSCs are typically isolated using fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) with surface marker combinations (e.g., CD44+/CD24− for breast CSCs, CD133+ for glioblastoma CSCs) [25] [28]. The Aldefluor assay is commonly employed to identify CSCs with high aldehyde dehydrogenase (ALDH) activity [25]. Functional enrichment through sphere-forming assays under non-adherent, serum-free conditions allows for the propagation of CSCs as tumorspheres that maintain stemness properties [30].
In Vitro Co-culture Systems: Direct and indirect co-culture systems enable the investigation of CSC-immune cell interactions. In direct co-cultures, CSCs and immune cells are cultured together, allowing cell-cell contact, while transwell systems permit the study of paracrine signaling without direct contact [28]. These systems are used to assess immune cell migration, polarization, and cytotoxic activity against CSCs, as well as the effects of immune cells on CSC stemness and proliferation.
In Vivo Tumor Models: Immunocompromised mouse models (e.g., NOD/SCID/IL2Rγnull or NSG mice) support the engraftment of human CSCs and enable the study of tumor initiation and growth [30]. Syngeneic immunocompetent models allow for the investigation of interactions between CSCs and a fully functional immune system. Patient-derived xenograft (PDX) models maintain the original tumor heterogeneity and stromal components, providing a more physiologically relevant context for studying CSC-immune interactions [30].
Single-Cell Multi-Omics Approaches: Advanced single-cell technologies, including scRNA-seq, enable high-resolution profiling of rare CSC populations and their transcriptional states within the TME [12]. Computational methods such as CytoTRACE and StemID leverage single-cell data to infer stemness dynamics and cellular differentiation trajectories, moving beyond static marker-based definitions [12].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Studying CSC-Immune Interactions
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| CSC Surface Markers | Anti-CD44, Anti-CD133, Anti-EPCAM Antibodies | CSC isolation and identification | Flow cytometry, cell sorting, immunohistochemistry |
| Intracellular CSC Markers | ALDH1 Assays (Aldefluor) | CSC functional identification | Detection of ALDH enzyme activity |
| Immune Cell Markers | Anti-CD3, CD11b, CD68, FOXP3 Antibodies | Immune cell profiling | Characterization of tumor-infiltrating immune cells |
| Immune Checkpoint Reagents | Anti-PD-1, PD-L1, CD47 Antibodies | Blockade of immune evasion pathways | Immune checkpoint inhibition studies |
| Cytokine/Chemokine Detection | TGF-β, IL-6, IL-10 ELISA Kits | Soluble factor measurement | Quantification of immunosuppressive mediators |
| Exosome Isolation Kits | Ultracentrifugation, Precipitation Kits | Extracellular vesicle studies | Isolation of CSC-derived exosomes |
| Signaling Pathway Inhibitors | LGK974 (Wnt), DAPT (Notch) | Pathway targeting | Dissection of specific signaling mechanisms |
Emerging Therapeutic Strategies and Clinical Translation
Targeting the interface between CSCs and the immune system represents a promising approach to overcome therapy resistance. Several strategy classes have emerged, with varying degrees of clinical validation.
Table 3: Emerging Therapeutic Strategies Targeting CSC-Immune Crosstalk
| Therapeutic Strategy | Molecular Targets | Mechanism of Action | Clinical Development Status | Representative Agents/Trials |
|---|---|---|---|---|
| TAM-targeted Therapies | CSF-1R, CCL2 | Reprogram TAMs to anti-tumor phenotype; reduce CSC niche support | Phase I/II | Pexidartinib (NCT02777710), Emactuzumab [24] |
| MDSC-targeted Strategies | CXCR1/2, STAT3 | Block MDSC recruitment and function; restore T cell activity | Phase I | SX-682 + Pembrolizumab (NCT03161431) [24] |
| Treg Depletion | CCR4, CD25 (IL-2Rα) | Deplete Tregs to relieve immune suppression | Phase II | Mogamulizumab (NCT02946671), Basiliximab [24] |
| CSC-specific Immunotherapies | CD133, EpCAM, ALDH | Target CSC antigens for immune-mediated killing | Phase I | CD133-CAR-T cells (NCT03423992, NCT02541370) [24] [2] |
| CSC Signaling Pathway Inhibitors | Wnt, Notch, Hedgehog pathways | Inhibit CSC self-renewal and reduce immunosuppressive cytokines | Phase I | LGK974 (Wnt inhibitor) + anti-PD-1 (NCT01351103) [24] |
| Metabolic Modulation | Glutaminase, fatty acid metabolism | Disrupt CSC and immune cell metabolic crosstalk | Phase I/II | CB-839 (NCT02771626), CPI-613 (NCT03399396) [24] |
| Epigenetic Therapy Combinations | DNMT, HDAC | Reverse CSC-driven immune suppression and resistance | Phase I | Guadecitabine + Atezolizumab (NCT03250273) [24] |
Figure 2: Multimodal Therapeutic Approach to Target CSC-Immune Crosstalk. Effective strategies combine immunotherapy enhancement, direct CSC targeting, and microenvironment modulation to overcome therapeutic resistance.
The clinical translation of CSC-targeted immunotherapies faces several challenges, including the dynamic plasticity of CSCs, which enables them to adapt to therapeutic pressure by altering biomarker expression and metabolic states [6] [12]. Additionally, the lack of universal CSC-specific biomarkers complicates the precise targeting of CSCs without affecting normal stem cells [25] [2]. The immunosuppressive TME further limits the efficacy of immunotherapies by creating physical and molecular barriers that prevent immune cell infiltration and function [24] [6].
Future directions include the development of integrated therapeutic approaches that simultaneously target multiple aspects of CSC-immune crosstalk. Combination strategies incorporating CSC-directed agents with immune checkpoint blockade, adoptive cell therapies, and microenvironment modulators hold promise for achieving more durable responses [24] [6]. Advances in single-cell technologies, spatial transcriptomics, and computational modeling are enabling more precise characterization of CSC states and their interactions with immune cells, paving the way for personalized biomarker-driven immunotherapy approaches [12].
The intricate crosstalk between CSCs and the immune system represents a critical determinant of therapeutic outcomes in cancer treatment. CSCs employ multiple strategies to evade immune surveillance and create an immunosuppressive niche, while immune cells reciprocally support CSC maintenance and stemness. This bidirectional interaction contributes significantly to therapy resistance and tumor recurrence. Comprehensive understanding of CSC-immune dynamics, coupled with validated biomarkers across cancer types, provides the foundation for developing innovative immunotherapeutic strategies. Future research should focus on leveraging advanced technologies to dissect the spatial and temporal dynamics of these interactions, enabling the design of multimodal therapies that can effectively target CSCs and overcome immunosuppression. The integration of CSC biomarkers into clinical trial designs will be essential for advancing biomarker-driven immunotherapy and achieving lasting therapeutic responses for cancer patients.
Advanced Methodologies for CSC Biomarker Discovery and Functional Validation
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with self-renewal capacity and the ability to drive tumor growth, metastasis, and therapeutic resistance [12] [2]. Their elusive nature and dynamic plasticity have made them a primary focus of cancer research, necessitating advanced technologies for their comprehensive characterization. High-throughput omics technologies have revolutionized our ability to profile CSCs across multiple molecular layers, moving beyond static, marker-based definitions to a dynamic and functional perspective [12]. These approaches enable researchers to dissect CSC heterogeneity, identify novel biomarkers, and uncover therapeutic vulnerabilities that could lead to more effective cancer treatments.
The integration of genomics, transcriptomics, and proteomics provides complementary insights into CSC biology. Genomics identifies hereditary and acquired mutations that confer stem-like properties; transcriptomics reveals gene expression patterns and regulatory networks that maintain stemness; and proteomics characterizes the functional effectors that execute CSC programs including surface markers, signaling molecules, and drug efflux pumps [31] [32]. When applied at single-cell resolution, these technologies can capture the rare and heterogeneous nature of CSC populations that are often obscured in bulk analyses [12] [33]. This guide provides a comprehensive comparison of current high-throughput omics approaches, their performance characteristics, and experimental protocols for profiling CSCs across different cancer types.
Comparative Performance of Omics Technologies
Table 1: Comparison of High-Throughput Omics Technologies for CSC Profiling
| Technology Type | Molecular Target | Key Platforms | Resolution | Throughput | Primary Applications in CSC Research |
|---|---|---|---|---|---|
| Genomics | DNA sequences and variations | NGS, DNBSEQ | Single-nucleotide | High | Identifying mutations in stemness genes (BRCA1/2), clonal evolution [32] |
| Transcriptomics | RNA expression patterns | RNA-Seq, scRNA-seq, Stereo-seq | Single-cell (10-500 nm) | High | CSC subpopulation identification, trajectory inference, stemness scoring [12] [34] |
| Proteomics | Protein abundance and modifications | Mass spectrometry, CITE-seq, RPPA | Single-cell to bulk | Moderate-High | Surface marker validation (CD44, CD133), signaling pathway activity, drug targets [31] [33] |
| Multi-Omics Integration | Multiple molecular layers | CITE-seq, ECCITE-seq, Abseq | Single-cell | High | Comprehensive CSC profiling, biomarker validation, network analysis [33] [35] |
Performance Metrics of Single-Cell Clustering Algorithms Across Omics Types
The computational analysis of omics data, particularly clustering algorithms for cell type identification, shows significant performance variation across different omics modalities. A recent comprehensive benchmark evaluation of 28 clustering algorithms across 10 paired transcriptomic and proteomic datasets revealed distinct performance characteristics.
Table 2: Performance Comparison of Top Single-Cell Clustering Algorithms Across Omics Types
| Clustering Algorithm | Transcriptomics Performance (ARI) | Proteomics Performance (ARI) | Computational Efficiency | Robustness to Noise | Recommended Application |
|---|---|---|---|---|---|
| scAIDE | High (Ranked 2nd) | Highest (Ranked 1st) | Moderate | High | Cross-omics applications, large datasets [33] |
| scDCC | Highest (Ranked 1st) | High (Ranked 2nd) | Memory-efficient | High | Proteomics-focused studies with limited resources [33] |
| FlowSOM | High (Ranked 3rd) | High (Ranked 3rd) | Fast | Excellent | Rapid screening, quality control [33] |
| CarDEC | High (Ranked 4th) | Moderate (Ranked 16th) | Moderate | Moderate | Transcriptomics-specific analyses [33] |
| PARC | High (Ranked 5th) | Low (Ranked 18th) | Fast | Moderate | Transcriptomics-specific analyses [33] |
The benchmarking study demonstrated that top-performing methods like scAIDE, scDCC, and FlowSOM show consistent performance across both transcriptomic and proteomic data, indicating strong generalization capabilities [33]. However, several algorithms exhibited significant performance disparities between omics types. For instance, CarDEC and PARC ranked highly for transcriptomics but dropped significantly in proteomics performance, highlighting the importance of selecting modality-appropriate computational tools [33].
Experimental Protocols for CSC Omics Profiling
Integrated Multi-Omics Workflow for CSC Biomarker Discovery
Diagram 1: Multi-omics workflow for CSC biomarker discovery
Single-Cell RNA Sequencing Protocol for CSC Identification
Protocol Title: Single-Cell RNA Sequencing for CSC Subpopulation Identification
Sample Preparation:
- Obtain fresh tumor tissues or liquid biopsies and process within 1 hour of collection
- Prepare single-cell suspensions using appropriate dissociation protocols (enzymatic/mechanical)
- Assess cell viability (>90%) using trypan blue or automated cell counters
- For CITE-seq: Stain cells with oligonucleotide-tagged antibodies against surface proteins (CD44, CD133, EpCAM) following manufacturer's recommendations [33]
Library Preparation and Sequencing:
- Use droplet-based single-cell platforms (10X Genomics, DNBelab C) according to manufacturer's protocols
- Target cell recovery: 5,000-10,000 cells per sample for adequate CSC capture (CSCs typically <5% of population) [12]
- For full-length transcriptome analysis: Use platforms like scCYCLONE-seq that integrate microfluidics with nanopore chemistry [34]
- Sequence on high-throughput platforms (DNBSEQ, Illumina) with recommended read depth (50,000 reads/cell)
Computational Analysis:
- Process raw data using standardized pipelines (Cell Ranger, Seurat)
- Perform quality control: Remove cells with <200 genes, >10% mitochondrial reads, or high hemoglobin genes
- Normalize data using SCTransform or similar methods
- Identify highly variable genes (HVGs) - typically 2,000-5,000 genes
- Perform dimensionality reduction (PCA, UMAP) and clustering using high-performing algorithms (scDCC, scAIDE) [33]
- Calculate stemness scores using computational tools (CytoTRACE, StemID, mRNAsi) [12]
- Validate CSC populations through trajectory inference and RNA velocity analysis
Chemical Proteomics Protocol for CSC Surface Marker Validation
Protocol Title: Affinity-Based Chemical Proteomics for CSC Surface Marker Identification
Sample Preparation:
- Culture CSC-enriched populations (via tumorsphere assays or FACS sorting)
- Harvest cells at logarithmic growth phase
- Prepare cell lysates using RIPA buffer with protease and phosphatase inhibitors
- Determine protein concentration using BCA assay
Affinity Enrichment and Target Identification:
- For affinity-based approaches: Immobilize small molecule probes (e.g., CSC-targeting compounds) on sepharose beads
- Incubate cell lysates with immobilized compounds (4°C for 4 hours with gentle rotation)
- Wash beads extensively to remove non-specific binders
- Elute bound proteins using competitive elution or SDS-PAGE loading buffer
- For DARTS (Drug Affinity Responsive Target Stability) approach: Incubate protein extracts with compounds of interest, then digest with pronase at room temperature for 30 minutes [31]
Mass Spectrometry Analysis:
- Digest proteins with trypsin overnight at 37°C
- Desalt peptides using C18 stage tips
- Analyze by LC-ESI-MS/MS using high-resolution mass spectrometers
- Identify proteins using database search engines (MaxQuant, Proteome Discoverer) against human protein databases
- Validate targets through orthogonal methods (western blot, functional assays)
Signaling Pathways in CSC Biology
Diagram 2: Core signaling pathways regulating CSC properties
The molecular pathways governing CSC function represent promising therapeutic targets. Multi-omics approaches have been particularly valuable in mapping these complex networks and identifying key regulatory nodes. Central stemness signaling pathways include JAK/STAT, Wnt/β-catenin, Hedgehog, Notch, and TGF-β, which are aberrantly regulated in CSCs compared to normal stem cells [31]. Topology-based pathway analysis tools like Signaling Pathway Impact Analysis (SPIA) and Drug Efficiency Index (DEI) enable quantitative assessment of pathway activation levels from multi-omics data, facilitating personalized drug ranking [35].
Multi-omics integration has revealed that CSCs exhibit significant metabolic plasticity, allowing them to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids [2]. This adaptability contributes to therapy resistance and is regulated by complex interactions between transcriptional networks, protein signaling, and metabolic enzymes. The integration of DNA methylation data with transcriptomic and proteomic profiles has further illuminated the epigenetic mechanisms that stabilize the CSC state, revealing opportunities for epigenetic therapies [35].
Research Reagent Solutions for CSC Omics Studies
Table 3: Essential Research Reagents for High-Throughput CSC Omics Studies
| Reagent Category | Specific Products/Platforms | Application in CSC Research | Key Features |
|---|---|---|---|
| Single-Cell Sequencing Kits | 10X Genomics Chromium, DNBelab C | Single-cell transcriptomics and multi-omics | High cell throughput, compatibility with multiple readouts [34] |
| CSC Surface Marker Antibodies | CD44, CD133, EpCAM, CD24 | FACS sorting and CITE-seq | Validated for specific cancer types, conjugated with oligonucleotides [33] [36] |
| Spatial Transcriptomics | Stereo-seq, Nanostring GeoMx | Spatial mapping of CSC niches | Nanoscale resolution (500nm), large field of view (>160cm²) [34] |
| Pathway Analysis Software | Oncobox, SPIA, DEI | Pathway activation assessment | Topology-based analysis, drug efficiency prediction [35] |
| Multi-Omics Integration Tools | MOFA+, OmicsNet, NetworkAnalyst | Integrated analysis of multiple omics layers | User-friendly interfaces, comprehensive visualization [37] [35] |
High-throughput omics technologies have fundamentally transformed our approach to CSC research, enabling the transition from static marker-based definitions to dynamic, functional characterization of these critical cell populations. The integration of genomics, transcriptomics, and proteomics—particularly at single-cell resolution—provides unprecedented insights into CSC heterogeneity, plasticity, and therapeutic vulnerabilities. As benchmarking studies have revealed, careful selection of computational methods tailored to specific omics modalities is essential for optimal performance in CSC identification and characterization [33].
The continuing evolution of multi-omics technologies, including spatial transcriptomics, chemical proteomics, and artificial intelligence-driven analysis, promises to further accelerate CSC research. These advances are paving the way for novel therapeutic strategies that target CSC plasticity, niche adaptation, and immune evasion mechanisms. Moving forward, the integration of metabolic profiling and functional genomics with established omics approaches will provide a more comprehensive understanding of CSC biology, ultimately leading to more effective therapies that prevent tumor recurrence and improve patient outcomes across diverse cancer types.
Single-Cell RNA Sequencing and Spatial Transcriptomics to Decipher CSC Heterogeneity
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [2]. Their ability to evade conventional treatments and adapt to metabolic stress makes them critical targets for innovative therapeutic strategies. However, CSC research faces major challenges, including significant heterogeneity and the lack of universally reliable CSC biomarkers that vary across tumor types [2]. Traditional bulk sequencing methods, which average gene expression across cell populations, fall short in capturing this cellular diversity, potentially masking critical CSC subpopulations [38].
Single-cell RNA sequencing (scRNA-seq) has revolutionized our ability to dissect cellular heterogeneity by providing gene expression profiles of individual cells, enabling the identification and characterization of rare cell subtypes that would otherwise be overlooked [38]. However, a key limitation of scRNA-seq is its inability to preserve spatial information about the RNA transcriptome, as the process requires tissue dissociation and cell isolation [38]. Spatial transcriptomics (ST) has emerged as a pivotal advancement, facilitating the identification of RNA molecules in their original spatial context within tissue sections, thereby offering substantial advantages over traditional single-cell sequencing techniques [39] [40]. This integrated approach provides unprecedented insights into CSC biology, including their spatial localization, niche interactions, and molecular signatures driving therapy resistance.
Technological Platforms and Performance Comparisons
Sequencing-Based Spatial Transcriptomic Platforms
Sequencing-based spatial transcriptomics (sST) enables unbiased whole-transcriptome analysis by capturing poly(A)-tailed transcripts with poly(dT) oligos on spatially barcoded arrays [41]. These platforms vary significantly in capture efficiency, transcript diffusion control, and spatial resolution. A systematic comparison of 11 sST methods revealed substantial variability across technologies, with molecular diffusion identified as a critical parameter significantly affecting effective resolutions [39].
Table 1: Performance Comparison of Sequencing-Based Spatial Transcriptomics Platforms
| Platform | Spatial Resolution | Capture Efficiency | Key Strengths | Limitations |
|---|---|---|---|---|
| Stereo-seq | 0.5 μm sequencing spots | Highest capturing capability; regular array size 1 cm (up to 13.2 cm) | Highest sensitivity; minimal molecular diffusion | Requires extensive sequencing (up to 4 billion reads) [39] |
| Visium HD | 2 μm features; 8 μm binned analysis | High sensitivity with probe-based method | Compatible with FFPE samples; reduced off-target binding (0.70%) | - |
| Slide-seq V2 | 10 μm resolution | High sensitivity in downsampled data | Bead-based approach | Limited capture area [39] |
| DBiT-seq | Variable depending on microfluidic channel width | Moderate sensitivity | Microfluidics approach; combines with protein detection | Variable capture size [39] |
| Visium (probe-based) | 55 μm with 100 μm center-center distance | High summed total counts; better read-capturing efficiency | Potentially reduced UMI quantification issues | Lower resolution than newer platforms [39] |
The performance evaluation of these platforms using reference tissues including mouse embryonic eyes, hippocampal regions, and olfactory bulbs demonstrated that technologies with smaller distances between spot centers (e.g., Stereo-seq, BMKMANU S1000, and Salus with <10 μm) achieved higher physical resolution [39]. However, capture efficiency varied independently of resolution, with Visium (probe-based) demonstrating remarkable efficiency in specific tissue contexts despite its lower spatial resolution [39].
Imaging-Based Spatial Transcriptomic Platforms
Imaging-based spatial transcriptomics (iST) utilizes iterative hybridization of fluorescently labeled probes followed by sequential imaging to profile gene expression in situ at single-molecule resolution [41]. Recent commercial platforms have dramatically expanded their gene panels while maintaining single-cell resolution.
Table 2: Performance Comparison of Imaging-Based Spatial Transcriptomics Platforms
| Platform | Genes Profiled | Resolution | Sensitivity | Tissue Compatibility |
|---|---|---|---|---|
| Xenium 5K | 5,001 genes | Single-molecule | Superior sensitivity for multiple marker genes | FFPE, fresh frozen [41] |
| CosMx 6K | 6,175 genes | Single-molecule | Higher total transcript count than Xenium but lower correlation with scRNA-seq | FFPE, fresh frozen [41] |
| MERFISH | ~1,000 genes | Single-molecule | High sensitivity for targeted genes | Fresh frozen [41] |
| STARmap | 1,020 genes | Single-molecule | High spatial accuracy | Fresh frozen [41] |
A systematic benchmarking of four high-throughput platforms with subcellular resolution demonstrated that Xenium 5K consistently outperformed other platforms in detection sensitivity for multiple marker genes, while maintaining high correlation with matched scRNA-seq profiles [41]. CosMx 6K, despite detecting a higher total number of transcripts than Xenium 5K, showed substantial deviation from matched scRNA-seq reference data, indicating potential technical artifacts [41].
Single-Cell RNA Sequencing Platforms
Single-cell RNA sequencing technologies have established themselves as key tools for dissecting genetic sequences at the level of single cells, revealing cellular diversity and allowing for the exploration of cell states and transformations with exceptional resolution [38].
Table 3: Performance Comparison of Single-Cell RNA Sequencing Platforms
| Platform | Throughput | Gene Sensitivity | Cell Type Representation | Ambient RNA Control |
|---|---|---|---|---|
| 10× Chromium | High | High gene sensitivity | Lower sensitivity for granulocytes | Different noise source than plate-based [42] |
| BD Rhapsody | High | Similar gene sensitivity to 10× Chromium | Lower proportion of endothelial and myofibroblast cells | Different noise source than droplet-based [42] |
A systematic comparison between 10× Chromium and BD Rhapsody platforms demonstrated similar gene sensitivity, but revealed distinct cell type detection biases, suggesting that platform selection should consider the specific cell populations of interest in CSC research [42].
Experimental Design and Methodologies for CSC Studies
Reference Tissue Selection and Sample Preparation
Well-designed benchmarking studies have established robust protocols for spatial transcriptomics that are directly applicable to CSC research. The selection of appropriate reference tissues with well-defined histological architectures is crucial for meaningful comparisons. Established reference tissues include:
- Adult mouse brain hippocampus: Exhibits consistent thickness and comprises regions such as cornu ammonis (CA)1, CA2, CA3, and dentate gyrus, each with distinct expression profiles [39].
- E12.5 mouse embryo eyes: Feature known structure with a lens surrounded by neuronal retina cells [39].
- Mouse olfactory bulbs: Contain clear layer separation with various neuron types [39].
- Human tumor samples: Clinical samples from colon adenocarcinoma, hepatocellular carcinoma, and ovarian cancer provide biologically relevant benchmarks [41].
For spatial transcriptomics, sample preparation varies by platform requirement. Tissues can be processed into formalin-fixed paraffin-embedded (FFPE) blocks, fresh-frozen (FF) blocks embedded in optimal cutting temperature (OCT) compound, or dissociated into single-cell suspensions for scRNA-seq [41]. Serial tissue sections are essential for parallel profiling across multiple omics platforms and validation studies.
Establishing Ground Truth Data
Rigorous CSC studies require multiple layers of validation to establish reliable ground truth data:
- Single-cell RNA sequencing: Provides a reference for cell type identification and validation of transcriptional profiles [41].
- Protein profiling: Technologies such as CODEX (co-detection by indexing) applied to tissue sections adjacent to those used for ST enable protein-level validation of transcriptional findings [41].
- Immunohistochemistry and fluorescence in situ hybridization: Offer orthogonal validation of marker expression and spatial localization [40].
- Manual annotation and nuclear segmentation: Essential for accurate cell type identification and spatial mapping [41].
Data Processing and Analysis Framework
Standardized data processing pipelines are critical for cross-platform comparisons. The established workflow includes:
- Spatial barcode processing: Generation of spatial barcodes and their corresponding locations with expression profiles per spatial location [39].
- Region of interest selection: Selective retention of reads within regions with known morphology based on spatial distribution of total counts and morphological information from H&E images [39].
- Downsampling analysis: Normalization of different methods to the same total number of sequencing reads to control for sequencing depth variations [39].
- Cell type annotation: Integration with single-cell reference datasets for cell type identification [40].
- Spatial clustering: Identification of spatially resolved cell communities and niches [41].
Figure 1: Experimental workflow for integrated single-cell and spatial transcriptomic analysis of CSCs
Signaling Pathways in CSC Biology Revealed by Transcriptomic Approaches
Advanced transcriptomic technologies have identified several key signaling pathways and molecular mechanisms that govern CSC heterogeneity, plasticity, and therapy resistance. These pathways represent potential therapeutic targets for eradicating CSCs and preventing cancer recurrence.
Figure 2: Key signaling pathways in cancer stem cell biology and therapy resistance
The PI3K/mTOR pathway has been identified as a crucial regulator of CSC survival under stress conditions. Studies integrating scRNA-seq and spatial transcriptomics in disease models have revealed that early upregulation of PI3K/mTOR in oligodendrocytes mitigates Rps29-bax-mediated ribosomal stress and oxidative phosphorylation, promoting survival, while prolonged stress suppresses PI3K/mTOR, triggering apoptosis/autophagy [43]. This pathway dynamic may have parallels in CSC biology, particularly in understanding how CSCs survive therapy-induced stress.
Spatial transcriptomic analyses have also revealed enhanced Tnfrsf21-App interactions between specific cell types that exacerbate neuroinflammation and functional decline [43], suggesting similar interaction networks may operate in CSC-microenvironment cross-talk. The metabolic plasticity of CSCs, allowing them to switch between glycolysis, oxidative phosphorylation, and alternative fuel sources such as glutamine and fatty acids, represents another key pathway that enables survival under diverse environmental conditions [2].
Biomarker Validation Across Cancer Types
The integration of single-cell and spatial transcriptomics has accelerated the discovery and validation of CSC biomarkers across different cancer types. Biomarker validation follows a multi-step process involving computational prediction and experimental confirmation.
Table 4: Validated CSC Biomarkers Across Cancer Types
| Cancer Type | Validated CSC Biomarkers | Validation Method | Confidence Score |
|---|---|---|---|
| Bladder Cancer | AURKA, BUB1B, CDCA5, CDCA8, KIF11, KIF18B, KIF2C, KIFC1, KPNA2, NCAPG, NEK2, NUSAP1, RACGAP1 | WGCNA, mRNAsi analysis, molecular subtyping | High confidence (0.6-1.0) [44] |
| Multiple Cancers | CD44, CD133, EpCAM, SOX2, NANOG, POU5F1 | Literature curation, BCSCdb database | Variable confidence [45] |
| Glioblastoma | Nestin, SOX2 | Functional studies, single-cell analysis | High confidence [2] |
| Gastrointestinal Cancers | LGR5, CD166 | Lineage tracing, functional assays | Moderate to high confidence [2] |
The Biomarkers of Cancer Stem Cells database (BCSCdb) provides a comprehensive resource of CSC biomarkers, categorizing them as high-throughput markers (HTM-8,307), high-throughput markers validated by low-throughput methods (283), and low-throughput markers (LTM-525) [45]. A total of 171 low-throughput biomarkers were identified in primary tissue and referred to as clinical biomarkers [45]. Each biomarker is assigned a confidence score based on the experimental method of detection, with western blotting receiving the highest score (0.7 for cell lines, 0.9 for primary tissues) and transcriptomics receiving the lowest score (0.1 for cell lines, 0.3 for primary tissues) [45].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 5: Essential Research Reagents for CSC Transcriptomics Studies
| Reagent Category | Specific Products/Platforms | Application in CSC Research |
|---|---|---|
| Spatial Transcriptomics Platforms | Visium HD, Stereo-seq, Xenium, CosMx | Whole-transcriptome or targeted spatial mapping of CSCs in tissue context |
| Single-Cell RNA Sequencing Platforms | 10× Chromium, BD Rhapsody | Dissection of CSC heterogeneity at single-cell resolution |
| Cell Isolation Kits | FACS antibodies for CSC surface markers (CD44, CD133, EpCAM) | Isolation of pure CSC populations for downstream analysis |
| Spatial Barcoding Reagents | Visium HD Gene Expression Slide, Stereo-seq chips | Spatial indexing of transcriptomic data |
| Tissue Preservation Media | RNAlater, Optimal Cutting Temperature (OCT) compound | Preservation of RNA integrity for spatial transcriptomics |
| Nucleic Acid Amplification Kits | SMART-seq kits, MDA kits | Amplification of minute RNA quantities from single cells |
| Library Preparation Kits | Nextera XT, Illumina RNA Prep | Preparation of sequencing libraries from amplified material |
| Bioinformatics Tools | Seurat, Scanpy, Giotto, Space Ranger | Analysis of single-cell and spatial transcriptomic data |
The integration of single-cell RNA sequencing and spatial transcriptomics has fundamentally transformed our approach to deciphering CSC heterogeneity. These technologies have revealed the remarkable plasticity of CSCs, their metabolic adaptability, and their complex interactions with the tumor microenvironment. Performance benchmarking across platforms provides researchers with critical guidance for selecting appropriate technologies based on their specific research questions, whether prioritizing spatial resolution, transcriptome-wide coverage, or sample compatibility.
The future of CSC research will likely be shaped by several emerging trends. Multi-omics integration combining transcriptomic, epigenomic, and proteomic data at single-cell resolution will provide more comprehensive views of CSC states [2]. The development of 3D spatial transcriptomics will enable better understanding of CSC organization within tumors [2]. Additionally, computational methods leveraging artificial intelligence and machine learning are poised to extract deeper insights from the complex datasets generated by these technologies, potentially identifying novel therapeutic vulnerabilities in CSCs [2].
As these technologies continue to evolve, they will undoubtedly uncover new aspects of CSC biology and provide innovative approaches for targeting these critical drivers of tumor progression and therapy resistance. The ongoing standardization of benchmarking efforts and experimental protocols will ensure that data generated across different platforms and laboratories can be effectively compared and integrated, accelerating progress in overcoming the clinical challenges posed by cancer stem cells.
Within the hierarchy of tumor cells, cancer stem cells (CSCs) represent a subpopulation with self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies. These cells are functionally defined by their ability to drive tumor initiation, progression, and metastasis [13] [2]. The validation of putative CSC biomarkers—such as CD44, CD133, and ALDH1—extends beyond mere detection to rigorous functional characterization. Two assays have emerged as the cornerstone methodologies for this purpose: the sphere formation assay and the in vivo tumorigenicity assay [13] [46]. This guide provides an objective comparison of these gold-standard methods, detailing their protocols, applications, and performance in validating CSC biomarkers across different cancer types.
Core Assay Principles and Methodologies
Sphere Formation Assay
The sphere formation assay is an in vitro functional test that leverages the principle that CSCs can survive and proliferate under anchorage-independent, serum-free conditions, whereas differentiated cancer cells typically undergo anoikis [46] [47]. This enriches a population with stem-like properties, and its output—the sphere-forming efficiency (SFE)—serves as a quantitative measure of self-renewal potential [46].
Detailed Experimental Protocol [46]:
- Culture Conditions: Single-cell suspensions are plated at low density (e.g., 1000 cells/mL) in serum-free medium supplemented with growth factors (e.g., EGF, bFGF, and B-27 supplement).
- Matrix and Environment: Cells are cultured in ultra-low attachment plates or embedded in a semi-solid, growth factor-reduced Matrigel to prevent adhesion and force suspension growth.
- Incubation and Monitoring: Cultures are maintained for 1-2 weeks, with fresh medium added periodically. The formation of 3D multicellular spheres is monitored.
- Quantification: The primary readout is the number and size of spheres formed, often measured manually or with automated algorithms like the Automatic Quantification of Spheres Algorithm (AQSA) [47]. A high SFE indicates enrichment of CSCs.
In Vivo Tumorigenicity Assay
The in vivo tumorigenicity assay, particularly the Limiting Dilution Assay (LDA), is the in vivo gold standard for validating the tumor-initiating capacity of CSCs [13] [48]. It tests the defining functional property of a CSC: the ability to form a new tumor in vivo that recapitulates the heterogeneity of the original malignancy.
Detailed Experimental Protocol [13] [48]:
- Cell Preparation and Inoculation: Putative CSCs, isolated via surface markers (e.g., CD44+/CD24- for breast cancer) or functional properties, are serially diluted. These dilutions are then injected into immunocompromised mice (e.g., NOD/SCID mice) via a relevant site (subcutaneous, mammary fat pad, etc.).
- Tumor Monitoring: Mice are monitored over several weeks for tumor formation. The frequency of tumor-initiating cells is calculated using statistical models (e.g., LDA analysis) that determine the dilution at which 37% of the injections fail to form a tumor.
- Validation: The resulting tumors can be analyzed histologically to confirm they mirror the original tumor's structure and biomarker expression.
The following diagram illustrates the workflow that integrates both assays for the functional validation of Cancer Stem Cells (CSCs).
Comparative Performance Analysis
The following table provides a detailed, data-driven comparison of the two gold-standard assays, summarizing their key characteristics and performance metrics.
Table 1: Functional Assay Comparison for CSC Validation
| Parameter | Sphere Formation Assay | In Vivo Tumorigenicity Assay |
|---|---|---|
| Core Principle | Anchorage-independent growth in 3D serum-free culture enriches self-renewing cells [46] [47]. | Serial dilution of cells in immunocompromised hosts measures tumor-initiation capacity [13] [48]. |
| Primary Readout | Sphere-Forming Efficiency (SFE): Number and size of spheres formed [46]. | Tumor-Initiating Cell Frequency: Calculated using limiting dilution analysis [48]. |
| Key Strengths | • Rapid, cost-effective in vitro screen [46]. • Amenable to high-throughput drug screening [46]. • Avoids ethical constraints of animal models. | • Confirms the definitive gold-standard property of CSCs: in vivo tumorigenicity [13]. • Preserves tumor heterogeneity and microenvironment interactions [49]. |
| Key Limitations | • Remains an in vitro model that may not fully recapitulate the in vivo TME [46]. • Sphere formation may not exclusively measure "stemness" (e.g., influenced by cell aggregation) [50]. | • Expensive, time-consuming, and requires specialized animal facilities [48]. • Ethical considerations and regulatory oversight. • Species-specific host factors may influence engraftment. |
| Typical Duration | 1-3 weeks [46] | 1-6 months [48] |
| Quantitative Data from Research | In breast cancer, organotropic metastatic cell lines (e.g., 231.BoM) showed a significant increase in MFE compared to parental lines [48]. Automated algorithms like AQSA can analyze images in ~0.3 seconds per image [47]. | The chick embryo CAM-LDA model demonstrated a correlation between inoculated cell number and tumor size, reproducing mouse xenograft growth patterns [48]. |
The Scientist's Toolkit: Essential Research Reagents
Successful execution of these functional assays relies on a specific set of reagents and tools. The table below details essential materials and their functions.
Table 2: Essential Research Reagents and Tools
| Category | Specific Examples | Function in Assay |
|---|---|---|
| Culture Media & Supplements | Serum-free DMEM/F12 medium; B-27 supplement; recombinant human EGF (rhEGF); recombinant human FGF (rhFGF) [46] [47] | Creates defined, non-differentiating conditions that selectively support CSC survival and proliferation. |
| Specialized Matrices & Plates | Growth factor-reduced Matrigel; Ultra-low attachment (ULA) multiwell plates [46] | Prevents cellular adhesion, forcing anchorage-independent growth and 3D sphere formation. |
| Enzymes & Dissociation Agents | Collagenase Type II; Dispase; Trypsin/EDTA [46] | Dissociates tumor tissues or spheres into single-cell suspensions for plating and passaging. |
| In Vivo Model Systems | NOD/SCID mice; Chick Embryo Chorioallantoic Membrane (CAM) [48] | Provides an in vivo environment for testing tumor initiation and growth. The CAM model is a lower-cost, rapid alternative. |
| Analysis & Quantification Tools | Flow cytometer (FACS); Automatic Quantification of Spheres Algorithm (AQSA); SpheroidJ software [51] [47] | Enables precise cell sorting based on biomarkers and automated, objective quantification of sphere number and area. |
Both the sphere formation and in vivo tumorigenicity assays are indispensable, yet complementary, tools in the functional validation of CSC biomarkers. The sphere assay serves as an efficient, high-throughput gateway to assess self-renewal potential in vitro, while the tumorigenicity assay provides the definitive, gold-standard confirmation of a cell's capacity to initiate tumors in vivo [13] [46] [48]. For robust biomarker validation, a sequential approach is recommended: initial enrichment and screening via sphere formation followed by ultimate validation through a limiting dilution tumorigenicity assay. As the field advances, the integration of these classical methods with emerging technologies—such as automated quantification, patient-derived organoids, and advanced in vivo models—will continue to refine our ability to identify and target therapeutically resistant cancer stem cells [49] [47].
Leveraging Patient-Derived Organoids (PDOs) for Biomarker Validation in a Clinically Relevant Model
The validation of predictive biomarkers represents a critical bottleneck in the translation of cancer biology to clinical practice. This challenge is particularly acute in the realm of cancer stem cell (CSC) research, where cellular plasticity and tumor heterogeneity complicate the identification of robust, clinically actionable biomarkers. While transcriptomic classifications and genomic profiling have provided foundational insights, they often fall short in predicting therapeutic response, especially in complex malignancies like pancreatic ductal adenocarcinoma (PDAC) [52]. The emergence of patient-derived organoids (PDOs) offers a transformative platform for biomarker validation. As three-dimensional ex vivo models that recapitulate the histological, genetic, and functional features of parental tumors, PDOs enable a functional reframing of biomarker discovery, moving beyond static molecular descriptions to dynamic assessment of drug response phenotypes within a clinically relevant context [53] [52].
PDOs as a Bridge Between Discovery and Clinical Application
Key Advantages of PDOs in Biomarker Research
Patient-derived organoids have emerged as powerful tools for biomarker validation due to several unique properties. They closely mirror the tissue of origin by preserving patient-specific genetic mutations, tumor heterogeneity, and the stem-cell hierarchy, including the crucial CSC subpopulations [53] [2]. This preservation is vital for studying CSC biomarkers, as PDOs maintain the cellular plasticity and differentiation potential that define stem-like cells. Unlike traditional 2D cell lines, PDOs retain key physiological characteristics such as cell-cell and cell-matrix interactions, creating physiological gradients of oxygen, nutrients, and growth factors that more accurately mimic the in vivo tumor microenvironment [53]. This fidelity makes them particularly suited for validating biomarkers of therapeutic response, as they functionally recapitulate the drug resistance mechanisms often driven by CSCs.
Establishing Living Biobanks for Systematic Validation
The development of living PDO biobanks has significantly advanced systematic biomarker discovery and validation. These biobanks, comprising organoids derived from a wide range of tumor types and patient populations, serve as essential platforms for drug screening, biomarker discovery, and functional genomics [53]. The classification and global distribution of these biobanks reflect a growing international effort to standardize protocols and broaden accessibility. For instance, substantial PDO biobanks have been established for colorectal cancer (with sample numbers ranging from 22 to 151), breast cancer (up to 168 samples), pancreatic cancer, and other malignancies, often with matched healthy control organoids [53]. These repositories provide the statistical power needed to correlate molecular features with functional drug responses, thereby enabling the validation of candidate biomarkers across diverse genetic backgrounds and tumor types.
Experimental Workflows for Biomarker Validation Using PDOs
Core Methodologies for PDO Establishment and Screening
The validation of CSC biomarkers using PDOs follows a structured workflow that integrates clinical sampling, ex vivo culture, functional testing, and multi-omic analysis. The foundational protocol begins with the collection of patient tumor specimens, which are dissociated and embedded in a specialized extracellular matrix such as Matrigel [54]. The cells are then cultured in a tailored medium containing specific growth factors and signaling pathway agonists/antagonists essential for maintaining stemness and promoting organoid formation. Key components typically include Wnt3A to activate Wnt signaling, Noggin to suppress BMP signaling, and other tissue-specific factors [53] [55] [54].
Following establishment and expansion, PDOs undergo high-throughput drug screening where they are exposed to a panel of therapeutic agents at varying concentrations. The subsequent readout of drug response phenotypes—typically measured through cell viability, apoptosis assays, and morphological changes—forms the functional data layer against which molecular biomarkers can be correlated [54]. This integrated approach allows researchers to distinguish between PDOs that are sensitive or resistant to specific therapies and to identify the molecular features underlying these differential responses.
Figure 1: Experimental workflow for biomarker validation using patient-derived organoids, illustrating the integration of model establishment, functional profiling, and biomarker discovery phases.
Advanced Co-Culture Systems for Immunotherapy Biomarkers
A significant advancement in PDO technology is the development of immune-organoid co-culture systems, which enable the validation of biomarkers for immunotherapy response. These systems can be broadly categorized into two types: innate immune microenvironment models and reconstituted immune microenvironment models [55]. The innate approach utilizes tumor tissue-derived organoids that naturally retain autologous tumor-infiltrating lymphocytes (TILs), preserving the original immune contexture of the tumor. For example, Neal et al. developed a tumor tissue-derived organoid model that maintained functional TILs and replicated PD-1/PD-L1 immune checkpoint interactions, providing a platform for validating biomarkers of immune checkpoint inhibitor response [55].
In contrast, reconstituted models involve co-culturing established PDOs with peripheral blood mononuclear cells (PBMCs) or engineered immune cells such as chimeric antigen receptor (CAR)-T cells or CAR-macrophages (CAR-M) [55] [54]. These systems allow for the controlled investigation of specific immune-tumor interactions and the identification of biomarkers predicting response to adoptive cell therapies. For instance, a recent study established a PDO-PBMC co-culture system that demonstrated specific immune cell cytotoxicity toward organoids, highlighting its potential for validating biomarkers of immunotherapy efficacy [54].
Key Signaling Pathways and CSC Biomarkers Accessible in PDO Models
Modeling CSC-Specific Signaling Networks
PDOs provide a unique platform for studying the altered signaling pathways that characterize cancer stem cells and serve as potential biomarker sources. CSCs display distinct activation patterns in key developmental and survival pathways compared to non-stem cancer cells [2] [25]. These include the Wnt/β-catenin pathway, which promotes self-renewal; the Notch pathway, which regulates asymmetric cell division; the Hedgehog pathway, which supports stem cell maintenance; and growth factor signaling pathways such as PI3K/Akt and JAK/STAT [25]. The 3D architecture of PDOs preserves the gradient of signaling molecules and cell-cell contact-mediated signaling that is crucial for maintaining these pathways in their physiological state, enabling more accurate biomarker identification than possible in 2D cultures.
Figure 2: Key signaling pathways in cancer stem cells that can be modeled using PDOs, showing their relationship to hallmark CSC functionalities.
Established and Emerging CSC Biomarkers
Research using PDO models has helped validate numerous CSC-associated biomarkers across different cancer types. These biomarkers can be broadly categorized into cell surface markers and intracellular markers, each with distinct applications in diagnostic and therapeutic development [25]. Cell surface markers, such as transporters and signaling receptors, are particularly valuable as they enable direct targeting of CSCs. Commonly validated surface markers include CD44, which is widely expressed across multiple cancer types; CD133, a glycoprotein conserved in breast, liver, lung, and ovarian CSCs; and ABC transporters like ABCB5 (melanoma) and ABCG2 (lung, pancreatic, liver, breast, and ovarian cancers) [25].
Among intracellular markers, aldehyde dehydrogenase 1 (ALDH1) has emerged as a consistently validated biomarker across breast, prostate, colon, lung, and ovarian CSCs [25]. Transcription factors such as BMI-1, c-MYC, OCT3/4, and SOX2, which maintain tumorigenicity and stemness, have also been confirmed as functional intracellular biomarkers in PDO-based studies. However, a significant challenge remains the lack of universal CSC-specific markers, as most identified biomarkers are also expressed in normal stem cells or non-stem cancer cells, albeit at different levels [2] [25]. This highlights the importance of using PDOs to validate biomarker expression in context-specific models that preserve cellular heterogeneity.
Table 1: Experimentally Validated CSC Biomarkers Accessible in PDO Models
| Biomarker Category | Specific Markers | Associated Cancer Types | Experimental Validation in PDOs |
|---|---|---|---|
| Cell Surface Markers | CD44 | Breast cancer, colon cancer, glioblastoma | Drug response correlation in breast cancer PDO biobanks [53] [25] |
| CD133 | Breast cancer, liver cancer, lung cancer, ovarian cancer | Maintenance of stem-cell hierarchy in colorectal PDOs [53] [25] | |
| ABCB5 | Melanoma | Functional characterization in melanoma PDOs [25] | |
| ABCG2 | Lung cancer, pancreatic cancer, liver cancer, breast cancer, ovarian cancer | Chemoresistance profiling in pancreatic PDOs [25] | |
| LGR5 | Gastrointestinal cancers | Growth potential in intestinal and gastric PDOs [53] [2] | |
| Intracellular Markers | ALDH1 | Breast cancer, prostate cancer, colon cancer, lung cancer, ovarian cancer | Activity-based sorting and drug screening [25] |
| BMI-1 | Multiple solid tumors | Expression correlation with therapy resistance [25] | |
| OCT3/4, SOX2 | Multiple solid tumors | Maintenance of tumorigenicity in expanded PDOs [25] |
Quantitative Data from PDO-Based Biomarker Studies
Correlation Between PDO Drug Response and Clinical Outcomes
The predictive validity of PDO-based biomarker validation is demonstrated by the strong correlation between PDO drug responses and patient clinical outcomes across multiple cancer types. In a comprehensive study of pancreatic cancer PDOs, researchers established five PDO lines and four matched patient-derived organoid xenograft (PDOX) models that retained the morphological, biological, and genomic characteristics of the primary tumors [54]. High-throughput screening with 111 FDA-approved drugs revealed significant variability in drug sensitivity across different organoids, yet PDOs and PDOX models derived from the same patient showed a high degree of concordance in their response to clinical chemotherapy agents, validating their predictive capacity.
Similar concordance has been demonstrated in other malignancies. Colorectal cancer PDO biobanks have shown remarkable success in predicting patient responses, with one study of 22 PDOs demonstrating 100% sensitivity, 93% specificity, 88% positive predictive value, and 100% negative predictive value in forecasting patient responses to irinotecan-based chemotherapy [53]. This high predictive accuracy underscores the utility of PDOs as avatars for therapy response and as platforms for validating predictive biomarkers that can guide treatment selection.
Table 2: Representative PDO-Based Biomarker Validation Studies Across Cancer Types
| Cancer Type | PDO Biobank Scale | Key Validated Biomarkers | Clinical Correlation |
|---|---|---|---|
| Colorectal Cancer | 55-151 PDO lines [53] | LGR5, CD44, CD133 [53] [25] | Drug response prediction (100% sensitivity, 93% specificity for irinotecan) [53] |
| Pancreatic Cancer | 13-77 PDO lines [53] | ABCG2, ALDH1, UGT1A10 [25] [54] | High concordance between PDO/PDOX and patient responses [54] |
| Breast Cancer | 33-168 PDO lines [53] | CD44, CD133, ALDH1 [53] [25] | Drug response prediction in subtypes (TNBC, ER+/PR+, Her2+) [53] |
| Ovarian Cancer | 76 PDO lines [53] | CD133, ABCG2, ALDH1 [25] | Disease modeling and drug response prediction [53] |
Functional Validation of Biomarker-Drug Relationships
Beyond correlative observations, PDOs enable direct functional validation of biomarker-therapeutic relationships through genetic manipulation in an otherwise native context. In the aforementioned pancreatic cancer PDO study, integration of next-generation sequencing analysis with drug sensitivity profiling identified the drug metabolism gene UGT1A10 as a crucial regulator of chemotherapy response [54]. Subsequent knockdown of UGT1A10 in PDOs significantly increased drug sensitivity, functionally validating its role as a predictive biomarker for treatment response. This approach exemplifies how PDO models can bridge the gap between observational biomarker discovery and functional validation, providing mechanistic insights that strengthen biomarker candidacy.
Similar functional approaches have been applied to CSC-specific biomarkers. For instance, PDO models have been used to test therapies targeting EpCAM, a CSC surface marker in prostate cancer, demonstrating the effectiveness of EpCAM-targeted CAR-T cell therapy in eliminating CSCs and improving treatment outcomes [2]. These functional validations provide compelling evidence for the clinical translation of CSC biomarkers identified through PDO-based screening.
Essential Research Reagent Solutions for PDO-Based Biomarker Validation
The successful establishment and application of PDO models for biomarker validation relies on a standardized set of research reagents and culture components. These materials support the growth and maintenance of organoids while preserving the stem cell populations and signaling pathways essential for accurate biomarker studies.
Table 3: Essential Research Reagent Solutions for PDO-Based Biomarker Validation
| Reagent Category | Specific Components | Function in PDO Culture |
|---|---|---|
| Basal Medium | Advanced DMEM/F12 [54] | Foundation for culture medium, providing essential nutrients and salts |
| Growth Supplements | B27 supplement, N-acetylcysteine, Nicotinamide [54] | Provide essential vitamins, antioxidants, and cofactors for cell growth |
| Signaling Pathway Modulators | Wnt3A (Wnt pathway activator), Noggin (BMP signaling inhibitor), A8301 (TGF-β inhibitor) [53] [54] | Maintain stemness and support organoid growth by regulating key developmental pathways |
| Extracellular Matrix | Matrigel, synthetic hydrogels (e.g., GelMA) [55] | Provide 3D structural support and biochemical cues for organoid formation |
| Cell Survival Enhancers | Y27632 (ROCK inhibitor), Forskolin [54] | Enhance cell survival after passage and support organoid growth |
| Tissue-Specific Factors | FGF10 (for pancreatic PDOs), EGF, R-spondin [53] [55] [54] | Support growth of specific tissue types through targeted pathway activation |
Integration with Real-World Data and Advanced Analytics
The power of PDO-based biomarker validation is greatly enhanced when integrated with real-world data (RWD) and advanced computational approaches. This integration creates a virtuous cycle where PDO functional data informs biomarker discovery, which is then validated against clinical outcomes at scale. As noted in recent research, "By analyzing longitudinal, multi-omic de-identified data from individual patients and combining it with insights from broader patient populations, we can subtype patients based on their molecular, immune, and clinical features" [56]. This approach allows researchers to identify which patient cohorts are most likely to benefit from specific treatments based on their biomarker profiles.
A compelling example of this integrated approach comes from a project that combined PDO screening with RWD analysis. Researchers began by screening standard-of-care antibody-drug conjugates against a PDO repository, leading to the discovery of a unique RNA-based, pan-cancer gene signature of response to enfortumab vedotin (a Nectin-4-targeting ADC) [56]. This signature was subsequently validated in a real-world cohort of bladder cancer patients, where it significantly correlated with real-world progression-free survival. Such integrated workflows demonstrate how PDO-derived biomarkers can be rapidly translated into clinically applicable tools for patient stratification.
Current Challenges and Future Perspectives
Despite their considerable promise, PDO-based biomarker validation faces several technical and methodological challenges. The standardization of culture protocols across different laboratories remains problematic, with variations in extracellular matrix composition, growth factor concentrations, and medium formulations potentially affecting biomarker expression and drug response phenotypes [53] [55]. The incomplete recapitulation of the tumor microenvironment, particularly the immune compartment, in conventional PDO models has prompted the development of more complex co-culture systems, but these add technical complexity and cost [55]. Additionally, the time required to establish and expand PDOs from patient samples (typically 2-4 weeks) may limit their utility in clinical decision-making for rapidly progressive diseases [53] [55].
Future advances are likely to focus on addressing these limitations through technological innovation. The integration of artificial intelligence and machine learning with PDO screening data holds particular promise for identifying complex biomarker signatures that predict therapeutic response [55] [56]. As one expert noted, "Ultimately, I envision a future where foundation models can integrate clinical data alongside DNA, RNA, and spatial context from a patient's H&E slide" [56]. Additionally, developments in microfluidic organoid culture, 3D bioprinting, and automated high-content imaging are expected to improve the scalability, reproducibility, and analytical depth of PDO-based biomarker studies [55]. These advances will further solidify the position of PDOs as indispensable tools for validating clinically relevant biomarkers in a functionally relevant context.
Cancer stem cells (CSCs) are a subpopulation of tumor cells with self-renewal capacity and the ability to drive tumor growth, metastasis, and relapse, widely recognized as major contributors to therapeutic resistance [12] [2]. Despite extensive efforts to characterize and target CSCs, their elusive nature continues to drive therapeutic resistance and relapse in epithelial malignancies [12]. The complex pathophysiology of cancer is shaped by diverse genetic, environmental, and molecular factors, leading to considerable variability in patient outcomes even within the same cancer types, which complicates treatment strategies [57]. This heterogeneity fosters the emergence of resistant subclones that survive therapy and contribute to recurrence, with CSCs commonly representing <5% of the total cancer cell pool yet driving tumor progression through self-renewal and plasticity [12].
In recent years, high-throughput molecular profiling technologies have become fundamental in precision medicine, enabling comprehensive analysis of DNA, RNA, and proteins to discover biomarkers [57]. However, relying on single omics data provides only partial insights into the intricate mechanisms of cancer, potentially missing critical biomarkers and therapeutic opportunities [57]. The integration of multiple omics data types is crucial for gaining a holistic understanding of cancer biology and enabling personalized treatment strategies [57]. Multi-omics integration can reveal new cell subtypes, cell interactions, and interactions between different omic layers leading to gene regulatory and phenotypic outcomes [58]. Since each omic layer is causally tied to the next, multi-omics integration serves to disentangle this relationship to properly capture cell phenotype [58].
This guide objectively compares the current methodologies, computational frameworks, and experimental protocols for building robust prognostic signatures from multi-omics data, with particular emphasis on their application in validating CSC biomarkers across different cancer types. We present comprehensive performance comparisons, detailed experimental workflows, and essential research tools to assist researchers, scientists, and drug development professionals in navigating this complex landscape.
Multi-Omics Integration Strategies: A Comparative Analysis
Integration of multi-omics data represents a considerable challenge to researchers due to the large, complex, multimodal nature of the data [58]. The principal distinction between computational strategies is whether the tool is designed for multi-omics data that is matched (recorded from the same cell) or unmatched (recorded from different cells) [58]. Furthermore, integration can be categorized as horizontal, vertical, or diagonal, each with distinct technical requirements and applications [58].
Table 1: Comparison of Multi-Omics Integration Strategies and Tools
| Integration Type | Data Relationship | Key Tools | Best Use Cases | Limitations |
|---|---|---|---|---|
| Matched (Vertical) | Different omics from same cells | Seurat v4, MOFA+, totalVI, SCENIC+ | Single-cell multi-omics (RNA+ATAC, RNA+protein) | Requires simultaneous measurement; technical noise alignment |
| Unmatched (Diagonal) | Different omics from different cells | GLUE, Pamona, UnionCom, LIGER | Integrating separate omics experiments; large cohort studies | Relies on computational alignment; potential misprojection |
| Mosaic | Various omic combinations across samples | COBOLT, MultiVI, StabMap | Studies with partial overlap in omics profiling | Requires sufficient overlapping features across datasets |
| Horizontal | Same omic across multiple datasets | Standard single-omic integration | Batch correction; meta-analysis | Not true multi-omics integration |
The challenges in multi-omics integration are substantial. Drawing insights from two specific omics requires unique strategies since each omic has a unique data scale, noise ratio, and hence its own preprocessing steps [58]. For example, actively transcribed genes should have greater open chromatin accessibility, but for other modalities, such as RNA-seq and protein data, the most abundant protein may not correlate with high gene expression [58]. This disconnect makes integration very difficult. Moreover, sensitivity remains an issue—a gene detected at the RNA level may simply be missing in the protein dataset [58].
Emerging Approaches for CSC-Focused Integration
For CSC research specifically, single-cell multi-omics has transformed our understanding of tumor biology by enabling high-resolution profiling of rare subpopulations (<5%) and revealing the functional heterogeneity that contributes to treatment failure [12]. New bioinformatics tools enable researchers to infer cellular differentiation potential, state transition rates, and even fate decisions without relying on traditional surface markers [12]. Among them, methods such as transcriptional entropy and RNA velocity are free of external cell-type labels, while some stemness scoring tools (e.g., mRNAsi, StemSC) rely on training with stem cell reference samples [12].
Supported by these advances, CSCs are increasingly understood as representing reversible states along developmental and treatment-induced trajectories rather than a fixed, intrinsic phenotype [12]. The most promising therapeutic strategies may not target static CSC markers but instead exploit transient, high-entropy states during cell state transitions—periods of instability that may represent therapeutic opportunities [12].
Performance Benchmarking: Framework Comparison
To objectively evaluate the performance of different multi-omics prognostic frameworks, we have compiled experimental data from recent studies implementing these approaches across various cancer types. The benchmarking focuses on prognostic accuracy, clinical feasibility, and computational efficiency.
Table 2: Performance Benchmarking of Multi-Omics Prognostic Frameworks
| Framework | Cancer Types Validated | Prognostic Accuracy (C-index) | Feature Reduction Efficiency | Clinical Feasibility |
|---|---|---|---|---|
| PRISM [57] | BRCA (0.698), CESC (0.754), OV (0.618), UCEC (0.754) | 0.618-0.754 | High (minimal biomarker panels) | Excellent (cost-effective signatures) |
| 9-Gene Peroxisome Signature [59] | ccRCC | 1-year AUC: 0.739, 2-year: 0.709, 3-year: 0.712 | Moderate (9 genes) | Good (qPCR compatible) |
| 16-Gene Inflammatory Signature [60] | Cervical Cancer | HR: 0.48 (95% CI: 0.275-0.85) | Moderate (16 genes) | Good (targets immune response) |
| 4-Gene ESCC Signature [61] | ESCC | Significant stratification (p<0.05) | High (4 genes) | Excellent (minimalist panel) |
| MCMLS [62] | Colorectal Cancer | Superior to existing models (p<0.05) | Variable (ML-based) | Moderate (requires full omics) |
| SurvivalML [63] | 21 solid tumors | Cross-cohort validation | High (identifies robust biomarkers) | Excellent (platform for discovery) |
Key Performance Insights
The PRISM framework demonstrates that cancer types benefit from unique combinations of omics modalities reflecting their molecular heterogeneity [57]. Notably, miRNA expression consistently provided complementary prognostic information across all cancers, enhancing integrated model performance [57]. This framework advances cancer prognosis by delivering scalable, interpretable multi-omics integration and identifying concise biomarker signatures with performance comparable to full-feature models, promoting clinical feasibility and precision oncology [57].
For CSC-focused applications, the ability to capture dynamic cellular states is crucial. Single-cell entropy methods such as StemID, SCENT, and SLICE enable quantification of the degree of "disorder" or "uncertainty" in a cell's transcriptome, serving as an indicator of its differentiation potential or phenotypic plasticity [12]. Meanwhile, CytoTRACE uses gene counts and expression to infer differentiation state, while RNA velocity predicts immediate future states from unspliced/spliced mRNA ratios [12].
Experimental Protocols for Robust Signature Development
The PRISM Framework Methodology
The PRISM framework employs a comprehensive multi-omics integration approach with the following detailed protocol [57]:
Data Acquisition and Preprocessing: Multi-omics data including gene expression, DNA methylation, miRNA expression, and copy number variations are obtained from TCGA. Only samples with complete data across all categories are included. For gene expression features with more than 20% missing values are removed, and the top 10% most variable genes are selected using a 90th percentile variance threshold.
Feature Selection: Employ multiple feature selection methods including univariate/multivariate Cox filtering and Random Forest importance. Apply rigorous filtering to identify survival-associated features from each omics modality independently.
Multi-Stage Integration: Selected features from single-omics analyses are integrated via feature-level fusion. The framework employs recursive feature elimination to enhance robustness and minimize signature panel size without compromising performance.
Survival Modeling: Benchmark multiple survival models including CoxPH, ElasticNet, GLMBoost, and Random Survival Forest. Perform cross-validation and bootstrapping to ensure model robustness.
Validation: Validate the final model on independent datasets using concordance index (C-index) and time-dependent ROC curves to assess prognostic performance.
CSC-Specific Stemness Assessment Protocols
For CSC-focused prognostic signature development, additional specialized protocols are required:
Stemness Quantification: Calculate stemness indices using tools such as CytoTRACE, which infers differentiation state based on gene counts and expression diversity, or mRNAsi, a machine learning-based stemness index [12].
Single-Cell Entropy Analysis: Apply transcriptional entropy algorithms to quantify cellular plasticity using tools such as StemID or SLICE, which compute entropy of the transcriptome as an indicator of differentiation potential [12].
Trajectory Inference: Utilize RNA velocity or pseudotime analysis to reconstruct developmental trajectories and identify transitional stem-like states using tools such as scEpath or MultiVelo [12].
Functional Validation: Implement CRISPR-based functional screens to validate CSC vulnerabilities identified through multi-omics analysis [12].
The following workflow diagram illustrates the complete experimental process for developing and validating multi-omics prognostic signatures with emphasis on CSC applications:
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of multi-omics prognostic signature development requires specific research reagents and computational tools. The following table details essential solutions for conducting this research:
Table 3: Essential Research Reagent Solutions for Multi-Omics Prognostic Signature Development
| Category | Specific Tools/Reagents | Function | Considerations |
|---|---|---|---|
| Single-cell Multi-omics Platforms | 10X Genomics Multiome, CITE-seq | Simultaneous measurement of transcriptome + epigenome/proteome | Enables matched integration; higher technical complexity |
| Stemness Assessment Tools | CytoTRACE, mRNAsi, StemSC, StemID | Quantify stemness and plasticity | CSC-focused applications; reference-based vs unsupervised |
| Bulk Omics Technologies | RNA-seq, ATAC-seq, Methylation arrays | Comprehensive molecular profiling | Cost-effective for large cohorts; loses single-cell resolution |
| Computational Integration Tools | Seurat, MOFA+, GLUE, LIGER | Integrate across omics modalities | Matched vs unmatched capacity; scalability considerations |
| Survival Modeling Packages | SurvivalML, PRISM, MOVICS | Develop and validate prognostic models | Clinical endpoint handling; censoring data management |
| Functional Validation Systems | CRISPR screens, Organoid models | Experimental validation of signatures | CSC maintenance; translational relevance |
Based on comprehensive performance comparisons and experimental data, the optimal approach for building prognostic signatures from multi-omics data depends on the specific research context and available resources. For most CSC-focused applications, we recommend:
Prioritize clinical feasibility by developing minimal gene signatures that maintain prognostic power, as demonstrated by the 4-gene ESCC signature and PRISM framework [57] [61].
Incorporate CSC-specific assessments including stemness indices and plasticity metrics to capture the dynamic nature of cancer stem cells [12].
Implement cross-cohort validation using platforms such as SurvivalML to ensure robustness and reproducibility across diverse patient populations [63].
Leverage multi-omics integration strategically, noting that miRNA expression consistently provides complementary prognostic information across cancer types [57].
The rapid advancement of single-cell technologies, artificial intelligence-driven predictive modeling, and multi-omics integration is paving the way for more effective precision medicine strategies for disrupting CSC plasticity, niche adaptation, and immune evasion [12]. By implementing the rigorous comparative frameworks and experimental protocols outlined in this guide, researchers can accelerate the development of robust prognostic signatures that ultimately improve patient outcomes across diverse cancer types.
Overcoming Technical Hurdles and Optimizing Biomarker Assays for Clinical Translation
Addressing Sensitivity and Specificity Issues in CSC Biomarker Detection
Cancer stem cells (CSCs) constitute a highly plastic and therapy-resistant cell subpopulation within tumors that drives tumor initiation, progression, metastasis, and relapse [2]. Their ability to evade conventional treatments and adapt to metabolic stress makes them critical targets for innovative therapeutic strategies. A significant challenge in CSC research lies in the accurate identification and isolation of these cells, which is hampered by the lack of universal CSC biomarkers and substantial heterogeneity across cancer types [2]. While surface proteins such as CD44, CD133, ALDH, LGR5, and EpCAM have been used to isolate CSC populations, these markers are not exclusive to CSCs and are often expressed in normal stem cells or non-tumorigenic cancer cells [2]. This limitation directly impacts the sensitivity and specificity of CSC detection methods, potentially leading to false positives and negatives in both research and clinical settings. The dynamic nature of CSCs, which can transition between states in response to environmental stimuli, further complicates detection efforts [2]. This guide systematically compares current CSC biomarker detection platforms, analyzes their performance limitations, and provides detailed experimental methodologies to enhance detection fidelity for researchers and drug development professionals.
Comparative Analysis of CSC Biomarker Detection Platforms
The evaluation of CSC biomarker detection technologies requires careful consideration of multiple performance parameters across different methodological approaches. The table below summarizes the key characteristics of major detection platforms used in CSC research:
Table 1: Performance Comparison of CSC Biomarker Detection Platforms
| Detection Platform | Theoretical Sensitivity | Practical Specificity Challenges | Sample Requirements | Key Applications in CSC Research |
|---|---|---|---|---|
| Immunohistochemistry (IHC) | High for protein localization | Limited by marker specificity; cross-reactivity with normal stem cells [2] [64] | Tissue sections | Spatial distribution of CSCs in tumor microenvironments |
| Flow Cytometry | Can detect rare populations (0.1-1%) | False positives from non-specific antibody binding [2] | Single-cell suspensions | Live cell sorting for functional assays |
| Single-Cell RNA Sequencing | Transcriptome-wide detection | Limited by transcript capture efficiency; may miss low-abundance targets [2] | Viable single cells | Heterogeneity mapping and novel biomarker discovery |
| Liquid Biopsy (ctDNA) | Varies by mutation allele frequency | Cannot distinguish cellular origin without enrichment [65] | Plasma/Serum | Non-invasive monitoring of therapy-resistant clones |
| AI-Based Histopathology | AUC 0.847-0.890 for EGFR in LUAD [66] | Requires extensive validation across cancer types | Digital H&E slides | Tissue-preserving computational biomarker detection |
The sensitivity limitations in CSC detection primarily stem from the rare frequency of CSCs within bulk tumor populations and their dynamic phenotypic states [2]. Specificity challenges largely arise from the overlap between CSC markers and normal stem cell programs, as well as technical artifacts in detection methodologies [2] [64]. For instance, the EAGLE model for EGFR mutation detection in lung adenocarcinoma demonstrates how computational approaches can achieve high sensitivity (AUC 0.847-0.890) while preserving tissue for additional analyses [66].
Experimental Protocols for Enhanced CSC Biomarker Validation
Multiparametric Flow Cytometry Protocol for CSC Isolation
Objective: To isolate viable CSCs with high purity while minimizing false positives from non-specific marker expression.
Materials and Reagents:
- Single-cell suspension from dissociated tumor tissue
- Fluorescently conjugated antibodies against CSC markers (CD44-APC, CD133-PE, EpCAM-FITC)
- ALDEFLUOR kit for ALDH activity detection
- Viability dye (e.g., 7-AAD or DAPI)
- Cell sorting buffer (PBS with 2% FBS and 1mM EDTA)
- FACS sorter with multiple laser capabilities
Procedure:
- Prepare single-cell suspension from tumor tissue using enzymatic digestion (collagenase/hyaluronidase) and mechanical dissociation.
- Filter cells through 40μm strainer to obtain single-cell suspension.
- Divide cells into aliquots for individual staining controls and multiparametric panel.
- Incubate cells with antibody cocktail for 30 minutes at 4°C in the dark.
- Process ALDEFLUOR staining according to manufacturer's protocol, including DEAB control.
- Add viability dye to exclude dead cells.
- Resuspend cells in sorting buffer at concentration of 5-10×10^6 cells/mL.
- Perform compensation using single-stained controls and fluorescence minus one (FMO) controls.
- Set sorting gates using appropriate negative controls and isotype controls.
- Sort cells using a high-purity mode (4-way purity) into collection tubes containing complete media.
Validation: Assess sorted population functionality through limiting dilution transplantation assays to confirm tumor-initiating capacity [2].
Super-ARMS ctDNA Detection Protocol for CSC-Derived Mutations
Objective: To detect CSC-associated mutations in circulating tumor DNA with enhanced sensitivity.
Materials and Reagents:
- Blood collection tubes (cfDNA-specific tubes recommended)
- Plasma separation reagents
- DNA extraction kit (cfDNA-specific)
- Super-ARMS EGFR Mutation Detection Kit
- Real-time PCR system
- Carcinoembryonic antigen (CEA) ELISA kit for correlation studies
Procedure:
- Collect 8-10mL blood in cfDNA preservation tubes, invert gently 8-10 times.
- Centrifuge at 1600-2000×g for 10 minutes at room temperature within 2 hours of collection.
- Transfer supernatant to fresh tubes and centrifuge at 16,000×g for 10 minutes to remove residual cells.
- Extract cfDNA using silica-membrane columns according to manufacturer's protocol.
- Quantify cfDNA using fluorometric methods.
- Prepare Super-ARMS reaction mix according to kit specifications.
- Add 10-20ng cfDNA per reaction.
- Run real-time PCR with following conditions: 95°C for 5 minutes, 45 cycles of 95°C for 15 seconds and 60°C for 45 seconds.
- Include positive and negative controls in each run.
- Correlate ctDNA findings with serum CEA levels (AUC 0.828 for EGFR mutation prediction) [65].
Troubleshooting: For samples with low ctDNA yield, consider increasing input volume or using digital PCR platforms for improved sensitivity.
Signaling Pathways in CSC Biomarker Regulation
The expression of CSC biomarkers is regulated through complex signaling networks that influence both their detection and functional properties. The diagram below illustrates key pathways associated with common CSC markers:
Figure 1: CSC Biomarker Signaling Network. This diagram illustrates the core signaling pathways regulating common cancer stem cell (CSC) biomarkers, highlighting the interconnected nature of these networks.
The signaling pathways depicted demonstrate how surface biomarkers connect to fundamental oncogenic drivers. For instance, KRAS activates both MAPK and PI3K-AKT-mTOR pathways, which in turn modulate CD133 and ALDH expression [67]. This interconnection explains why multiple biomarkers often need to be assessed simultaneously for accurate CSC identification and why pathway activity assays can complement surface marker detection.
Research Reagent Solutions for CSC Biomarker Studies
Table 2: Essential Research Reagents for CSC Biomarker Detection
| Reagent Category | Specific Examples | Research Application | Considerations for Specificity |
|---|---|---|---|
| Validated Antibodies | Anti-CD44 (clone IM7), Anti-CD133 (clone AC133), Anti-EpCAM (clone VU-1D9) | Flow cytometry, IHC, immunofluorescence | Clone validation for specific applications; species cross-reactivity |
| Enzyme Activity Assays | ALDEFLUOR kit, SP dye efflux assays | Functional CSC identification | Background fluorescence; inhibitor controls required |
| ctDNA Detection Kits | Super-ARMS EGFR mutation test, digital PCR assays | Liquid biopsy approaches | Optimal blood collection tubes; rapid processing to prevent lysis |
| Cell Separation Reagents | Magnetic bead conjugates, FACS sorting buffers | CSC isolation for functional studies | Viability maintenance; appropriate isotype controls |
| Primary CSC Cultures | Organoid media, low-attachment plates, growth factor cocktails | Functional validation of isolated CSCs | Serum-free conditions; oxygenation levels |
The selection of appropriate research reagents is critical for overcoming sensitivity and specificity challenges in CSC detection. For example, the ALDEFLUOR system detects aldehyde dehydrogenase activity, a functional marker that complements surface protein expression [2]. Similarly, the Super-ARMS technology demonstrates improved sensitivity for ctDNA-based detection, with clinical studies showing 68.1% positivity rate for EGFR mutations in NSCLC compared to tissue testing [65].
Emerging Technologies and Future Directions
Innovative approaches are rapidly evolving to address persistent limitations in CSC biomarker detection. Artificial intelligence applications, such as the EAGLE model for EGFR mutation prediction from H&E slides, demonstrate how computational methods can achieve clinical-grade accuracy (AUC 0.847-0.890) while preserving tissue for additional analyses [66]. This approach reduced the need for rapid molecular tests by up to 43% while maintaining clinical standard performance [66]. Similarly, radiomics-based biomarkers are showing promise for non-invasive assessment of PD-1 status in hepatocellular carcinoma, with models achieving AUCs of 0.897 in training cohorts [68].
Advanced multi-omics integration represents another frontier in CSC biomarker development. Integrative profiling of lung cancer biomarkers (EGFR, ALK, KRAS, and PD-1) using structural modeling, molecular docking, and transcriptomic validation provides a blueprint for comprehensive biomarker characterization [69] [70]. Such approaches confirmed significant overexpression of these biomarkers in NSCLC tissues (EGFR: 2.8-fold, KRAS: 2.3-fold) while providing structural insights into drug-binding interfaces [69]. Population-scale studies integrating multiple biomarkers (54 blood-derived biomarkers with epidemiological factors) have demonstrated robust risk stratification capabilities (AUROC 0.767) for multiple cancer types [71], suggesting similar frameworks could be adapted for CSC detection.
The experimental workflows below illustrate how these advanced technologies can be integrated into comprehensive CSC biomarker detection pipelines:
Figure 2: Integrated CSC Biomarker Detection Workflow. This diagram outlines a comprehensive experimental pipeline combining traditional and emerging technologies for enhanced CSC biomarker detection and validation.
As CSC biomarker research advances, the integration of these sophisticated technologies with traditional detection methods will be essential for overcoming current sensitivity and specificity limitations. The development of standardized validation frameworks, similar to the Comprehensive Oncological Biomarker Framework that integrates genetic testing, imaging, histopathology, and multi-omics data [64], will be crucial for establishing reliable CSC detection protocols across different cancer types and research settings.
Cancer stem cells (CSCs) are a subpopulation of tumor cells with self-renewal capacity, therapy resistance, and metastatic potential that drive tumor initiation, progression, and recurrence across diverse cancer types [30] [2] [72]. The identification and validation of reliable CSC biomarkers represent a critical frontier in precision oncology, with potential applications in diagnosis, prognosis, therapeutic targeting, and treatment response monitoring [10] [72]. Despite two decades of research and the identification of numerous candidate markers including CD133, CD44, ALDH1, OCT4, and SOX2, the field faces significant challenges in standardizing detection methods and ensuring reproducible results across different laboratories and patient populations [2] [73].
The clinical implications of these challenges are substantial. Studies have demonstrated that CSC marker expression correlates with aggressive disease phenotypes and poor patient outcomes. For example, in ovarian cancer, high ALDH1A1 expression functions as an independent prognostic indicator for shorter overall survival, while in breast cancer, CD44+/CD24- or ALDH-high populations display more aggressive clinical trajectories with increased metastatic potential and chemotherapy resistance [72]. Similarly, in non-small cell lung cancer (NSCLC), combined detection of CD133 and OCT4 provides superior diagnostic accuracy (AUC=0.893) compared to single markers and correlates with poor differentiation, lymph node metastasis, and reduced 2-year overall survival [74]. Without standardized approaches, these promising findings struggle to transition from research settings to validated clinical applications.
This guide examines the fundamental hurdles confronting multi-center CSC biomarker validation, compares experimental methodologies and their impact on result variability, and outlines strategic frameworks for enhancing reproducibility through standardized protocols, reagent validation, and multi-omics integration.
Biological and Technical Challenges
The validation of CSC biomarkers across multiple centers is confounded by several interconnected sources of variability that affect both reliability and clinical translatability. CSC plasticity represents a fundamental biological challenge, as these cells can dynamically alter their phenotypic and functional characteristics in response to microenvironmental cues, therapeutic pressure, and metabolic stress [10] [2]. This plasticity manifests as fluctuations in marker expression that complicate consistent identification and isolation across different experimental conditions and patient populations.
Technical variability introduces additional complexity through multiple dimensions:
- Marker heterogeneity: There is no universal CSC marker, and expression patterns vary significantly across cancer types. For instance, glioblastoma CSCs frequently express neural lineage markers like Nestin and SOX2, while gastrointestinal cancers may harbor CSCs characterized by LGR5 or CD166 expression [2].
- Detection method inconsistencies: Variations in sample processing, antibody specificity, staining protocols, and analytical pipelines create substantial inter-laboratory variability [74] [72].
- Threshold determination: The definition of "high expression" varies significantly across studies, often relying on semi-quantitative scoring systems with limited standardization [74].
The regulatory landscape presents further complications, particularly in Europe where IVDR (In Vitro Diagnostic Regulation) implementation has created uncertainty through poorly defined requirements, inconsistencies between jurisdictions, and lack of centralized transparency compared to the US FDA system [75]. This regulatory heterogeneity impedes the development of harmonized biomarker assays across different geographic regions.
Analytical Challenges in Multi-Center Studies
The table below summarizes key analytical challenges specific to multi-center CSC biomarker research:
Table 1: Analytical Challenges in Multi-Center CSC Biomarker Studies
| Challenge Category | Specific Issues | Impact on Reproducibility |
|---|---|---|
| Sample Processing | Variation in collection methods, preservation techniques, storage conditions, and processing timelines | Affects biomarker stability and detection reliability [74] [76] |
| Analytical Protocols | Differences in antibody clones, dilution factors, antigen retrieval methods, and detection systems | Introduces substantial inter-laboratory variability [74] [72] |
| Data Interpretation | Subjective scoring systems, varying threshold definitions, and different gating strategies | Limits comparability across studies and institutions [74] |
| Platform Diversity | Use of different sequencing platforms, imaging systems, and analytical instruments | Creates technical bias that is difficult to quantify [75] [76] |
Comparative Analysis of Experimental Approaches
Methodological Variations and Their Impact
Direct comparison of experimental approaches reveals how methodological choices significantly impact CSC biomarker detection and validation. The table below summarizes key methodologies used in CSC biomarker research, along with their specific standardization challenges and performance characteristics:
Table 2: Comparison of Experimental Methodologies in CSC Biomarker Research
| Method | Applications | Standardization Challenges | Inter-Lab Concordance | References |
|---|---|---|---|---|
| Immunohistochemistry (IHC) | Protein localization and expression in tissue sections | Antibody validation, antigen retrieval variability, subjective scoring | Moderate (70-85% with strict protocols) | [74] [72] |
| Flow Cytometry | Cell surface marker quantification and cell sorting | Gating strategies, instrument calibration, sample preparation | Variable (60-90% depending on marker) | [2] [72] |
| Next-Generation Sequencing (NGS) | Mutation profiling, gene expression, multi-omics | Library prep, platform differences, bioinformatics pipelines | High (>95% for DNA variants) | [75] [76] |
| Functional Assays | Tumor sphere formation, drug resistance, in vivo tumorigenicity | Culture conditions, timeframe, endpoint determination | Low to moderate (highly context-dependent) | [30] [2] |
A multi-institutional study implementing in-house NGS testing for NSCLC samples demonstrated that rigorous standardization could achieve 99.2% sequencing success rates for DNA and 98% for RNA, with high interlaboratory concordance (95.2%) and a strong correlation (R² = 0.94) between observed and expected variant allele fractions [76]. This highlights the potential for achieving reproducibility when implementing strict technical controls.
Case Study: CD133 and OCT4 Detection in NSCLC
A recent retrospective study of 80 early-stage NSCLC patients and 40 healthy controls exemplifies both the promise and challenges of CSC biomarker detection [74]. The research employed both IHC and qRT-PCR to assess CD133 and OCT4 expression, revealing significant upregulation in NSCLC tissues compared with adjacent normal tissues. However, the study also illustrated several methodological challenges:
- Sample processing variation: Tissue collection methods, fixation times, and RNA extraction protocols introduced pre-analytical variability.
- Detection method inconsistencies: IHC employed semi-quantitative scoring (0-9 based on intensity and percentage of positive cells), while qRT-PCR required normalization to reference genes, creating different expression thresholds.
- Threshold determination: "High expression" was defined as a total score ≥6 for IHC, an arbitrary cutoff that may not translate directly across laboratories.
Despite these challenges, the combined detection of CD133 and OCT4 demonstrated superior diagnostic accuracy (AUC=0.893) compared to single markers, with combined sensitivity of 88.7% and specificity of 82.5% [74]. This suggests that multi-marker approaches may partially compensate for methodological variability.
Strategies for Enhancing Standardization and Reproducibility
Integrated Workflows for CSC Biomarker Validation
The following diagram illustrates a standardized workflow for CSC biomarker validation that incorporates quality control checkpoints at critical stages to enhance multi-center reproducibility:
Experimental Protocols for Reproducible CSC Biomarker Detection
Standardized Immunohistochemistry Protocol
Based on methodologies from multiple studies [74] [72], a standardized IHC protocol for CSC marker detection should include:
- Tissue Processing: Uniform fixation in 10% neutral buffered formalin for 24-48 hours, followed by paraffin embedding with standardized processing conditions.
- Antigen Retrieval: Use of 0.01 mol/L citrate buffer (pH 6.0) heated in a microwave at medium-high power for 10 minutes, with consistent cooling procedures.
- Antibody Incubation: Primary antibodies (e.g., anti-CD133 at 1:200 dilution, anti-OCT4 at 1:150) incubated in a humid chamber at 4°C overnight with strict temperature control.
- Detection and Visualization: HRP-conjugated secondary antibody incubation at room temperature for 30 minutes, DAB development for 3-8 minutes monitored microscopically.
- Scoring System: Semi-quantitative assessment incorporating staining intensity (0-3) and percentage of positive cells (0-4), with total scores of 0-12 rather than 0-9 to provide finer granularity.
Next-Generation Sequencing Quality Framework
For molecular CSC biomarker detection, NGS protocols require rigorous standardization [75] [76]:
- Sample QC: DNA/RNA quality assessment through fluorometric quantification and integrity number (e.g., RIN >7 for RNA).
- Library Preparation: Use of identical kits and protocols across centers with standardized input amounts.
- Sequencing Parameters: Uniform sequencing depth (e.g., 500x for DNA, 50M reads for RNA) and platform calibration.
- Bioinformatic Analysis: Centralized pipeline for variant calling, expression quantification, and fusion detection to minimize computational variability.
The Scientist's Toolkit: Essential Research Reagents
The table below details key research reagents and their critical functions in CSC biomarker studies, emphasizing validation requirements for reproducible results:
Table 3: Essential Research Reagents for CSC Biomarker Studies
| Reagent Category | Specific Examples | Function | Validation Requirements |
|---|---|---|---|
| Validated Antibodies | Anti-CD133, Anti-OCT4, Anti-CD44, Anti-ALDH1A1 | Specific detection of CSC markers via IHC, flow cytometry | Application-specific validation; lot-to-lot consistency testing [74] [72] |
| Enzymatic Assay Kits | ALDEFLUOR kit, sphere formation assays | Functional identification of CSCs based on ALDH activity | Standardized positive controls; established gating protocols [72] |
| NGS Library Prep Kits | Hybridization capture panels, amplicon kits | Molecular profiling of CSC-associated mutations and expression | Input quantity standardization; cross-lot performance verification [75] [76] |
| Cell Culture Reagents | Defined serum-free media, growth factors | Maintenance of CSC phenotype in vitro | Lot-to-lot consistency testing; contamination screening [30] [2] |
Emerging Technologies and Future Directions
Multi-Omics Integration and AI-Based Approaches
The integration of multi-omics approaches represents a promising strategy to overcome current limitations in CSC biomarker validation [77] [75]. By combining genomic, transcriptomic, proteomic, and metabolomic data, researchers can develop composite biomarker signatures that are more robust than single-marker approaches. Recent studies demonstrate that multi-omics data fusion models can provide predictions with F1 scores of 0.63-0.85 across external testing sets, outperforming single-domain approaches [75] [78].
Spatial biology technologies enable precise mapping of CSC markers within tissue architecture, providing critical context for biomarker expression patterns. As noted in recent research, "protein profiling revealed a tumor region expressing a poor-prognosis biomarker with a known therapeutic target: a signal that standard RNA analysis had entirely missed" [75]. This highlights how multi-modal approaches can uncover clinically actionable subgroups that traditional single-method assays overlook.
Artificial intelligence and machine learning approaches are increasingly being applied to standardize biomarker analysis and reduce subjective interpretation variability. AI-driven image analysis platforms can provide consistent quantification of IHC staining across multiple centers, while machine learning algorithms can integrate complex multi-omics data to identify reproducible CSC signatures [75] [78].
Conceptual Framework for CSC Biomarker Validation
The following diagram outlines a comprehensive framework for validating CSC biomarkers across multiple centers, incorporating technological and analytical standardization approaches:
The journey toward standardized, reproducible CSC biomarker validation across multiple centers remains challenging yet increasingly feasible through integrated approaches. The persistent issues of biological plasticity, technical variability, and analytical heterogeneity require coordinated solutions including standardized protocols, validated reagents, multi-omics integration, and AI-enhanced analysis. Promisingly, studies demonstrate that rigorous standardization can achieve high inter-laboratory concordance (>95%) for molecular biomarkers [76], while multi-marker approaches improve diagnostic accuracy beyond single markers [74].
As the field advances, success will depend on collaborative frameworks that prioritize reproducibility from initial discovery through clinical validation. This will require commitment to shared protocols, centralized bioinformatic pipelines, and transparent reporting standards. By addressing these standardization challenges systematically, the research community can unlock the full potential of CSC biomarkers to guide precision oncology and improve patient outcomes across diverse cancer types.
The Role of AI and Machine Learning in Mining Complex Datasets for Novel Biomarker Patterns
Cancer Stem Cells (CSCs) represent a critical therapeutic target in oncology due to their role in tumor initiation, metastasis, and therapy resistance [20]. The validation of reliable CSC biomarkers across different cancer types remains a fundamental challenge in precision oncology. CSCs are characterized by specific biomarkers and surface proteins—such as CD44, CD133, and EpCAM—that differ from those on non-CSC tumor cells [45] [20]. The ability to accurately identify and target CSCs hinges on discovering and validating these molecular patterns across diverse tumor types and datasets. Traditional biomarker discovery approaches have struggled with the complexity and heterogeneity of CSC populations, creating an pressing need for advanced computational methods.
Artificial intelligence (AI) and machine learning (ML) are revolutionizing this field by mining complex, high-dimensional datasets to uncover novel biomarker patterns that elude conventional statistical methods [79] [80]. These technologies can systematically explore massive molecular datasets to identify both established and novel CSC biomarkers, significantly accelerating the validation pipeline. The integration of AI in CSC biomarker research enables more comprehensive characterization of these elusive cell populations, potentially unlocking new therapeutic strategies that specifically target the root causes of cancer recurrence and treatment resistance.
Performance Comparison: AI Models in Biomarker Discovery
Multiple AI and ML approaches have been developed and applied to CSC biomarker discovery and validation, each with distinct strengths and performance characteristics. The table below summarizes the quantitative performance metrics of various computational methods reported in recent studies:
Table 1: Performance comparison of AI/ML models in biomarker discovery and validation
| AI/ML Model | Application Context | Key Performance Metrics | Reference Dataset | Advantages |
|---|---|---|---|---|
| ABF-CatBoost Integration | Multi-targeted drug discovery in colon cancer using biomarker signatures | Accuracy: 98.6%, Specificity: 0.984, Sensitivity: 0.979, F1-score: 0.978 | Colon cancer molecular profiles [81] | Addresses drug resistance by analyzing mutation patterns and conserved binding sites |
| Random Forest & XGBoost | Identification of hub genes in lung cancer pathogenesis | Effective identification of common genes; MLP algorithm achieved highest accuracy with complete gene set | Lung cancer samples [79] | Robust performance in identifying pivotal hub genes for CSC characterization |
| AI-Powered Biomarker Discovery Pipeline | General biomarker discovery across cancer types | Reduces discovery timeline from years to months or days; 15% improvement in survival risk prediction in phase 3 trials | Multi-omics datasets [80] | Systematic exploration of massive datasets; identifies patterns traditional methods miss |
| Confidence Scoring System (BCSCdb) | CSC biomarker validation across 10 cancer types | Normalized confidence scores (0.04-1.0); biomarkers categorized as high-confidence (>0.6), moderate (0.4-0.6), low (<0.4) | 1,962 scientific works on CSC biomarkers [45] | Provides standardized validation metrics based on experimental methods |
The performance advantage of integrated AI approaches like ABF-CatBoost is particularly evident in their ability to handle high-dimensional molecular data while maintaining exceptional accuracy and specificity [81]. These systems excel at identifying subtle biomarker patterns that correlate with therapeutic response and resistance mechanisms—critical factors in CSC-targeted therapies. The confidence scoring system implemented in BCSCdb (Biomarkers of Cancer Stem Cells database) further provides a standardized framework for evaluating CSC biomarkers across different cancer types, with weighting based on detection methods from transcriptomics (lowest score) to Western blotting (highest score) [45].
Experimental Protocols and Methodologies
High-Confidence CSC Biomarker Validation Framework
The validation of CSC biomarkers requires rigorous experimental protocols that leverage both computational and laboratory methods. The BCSCdb database employs a meticulous framework for scoring biomarker confidence levels based on experimental validation methods [45]:
Data Collection and Curation: Manually curated from 1,962 scientific publications until May 2022 using PubMed advanced search with targeted queries for different cancer types. The curation excluded animal cell line-specific papers, review papers, and non-English publications, focusing exclusively on human primary tissues and human cell lines [45].
Biomarker Classification System: Categorization into three distinct classes: (1) High-throughput markers (HTM-8,307) from transcriptomic and proteomic studies; (2) High-throughput markers validated by low-throughput methods (283); and (3) Low-throughput markers (LTM-525) from detection methods including RT-PCR, Western blotting, immunohistochemistry staining, and fluorescence-activated cell sorting. A subset of 171 low-throughput biomarkers were identified in primary tissue and classified as clinical biomarkers [45].
Confidence Scoring Algorithm: Implementation of a weighted scoring system based on detection methodology. For cell line studies: Western blotting (0.7), immunohistochemistry (0.5), immunofluorescence (0.5), RT-PCR (0.3), flow cytometry (0.3), and transcriptomics (0.1). For primary tissue studies, an additional 0.2 score was added to each method. Normalization to a 0.04-1 scale using the formula: Normalized Confidence Score = (Raw Score ÷ 2.5) × 1, where 2.5 represents the highest combinatorial method score observed [45].
Global Scoring System: Calculation of biomarker frequency across 10 different cancer types using the formula: GSA = NA ÷ NT, where NA is the number of unique papers reporting the gene, and NT is the number of unique papers. Normalization to a 0.001-1 scale to identify universal CSC biomarkers versus cancer-type specific markers [45].
AI-Driven Biomarker Discovery Pipeline
Advanced AI platforms follow a systematic pipeline for biomarker discovery that can be adapted specifically for CSC biomarker validation:
Data Ingestion and Harmonization: Collection of multi-modal datasets from diverse sources including genomic sequencing data, medical imaging, electronic health records, and laboratory results. Implementation of data lakes and cloud-based platforms for managing massive, heterogeneous datasets with rigorous quality control measures [80].
Preprocessing and Feature Engineering: Quality control, normalization, and feature engineering to handle missing data imputation and outlier detection. Correction of batch effects from different sequencing platforms or imaging equipment. Creation of derived variables such as gene expression ratios or radiomic texture features that capture biologically relevant patterns [80].
Model Training and Optimization: Employing various machine learning approaches including random forests, support vector machines, deep neural networks, convolutional neural networks, autoencoders, and graph neural networks depending on data type and clinical question. Implementation of cross-validation and holdout test sets with hyperparameter optimization through grid search or Bayesian optimization [81] [80].
Validation and Clinical Translation: Independent validation across multiple cohorts and biological experiments encompassing analytical validation (test reliability), clinical validation (outcome prediction), and clinical utility assessment (patient care improvement). Deployment through clinical decision support systems with ongoing performance monitoring [80].
Diagram 1: AI-powered biomarker discovery workflow
Visualization of Methodologies and Relationships
Multi-Omics Data Integration for CSC Biomarker Discovery
The integration of multi-omics data represents a cornerstone of modern CSC biomarker discovery, enabling comprehensive characterization of these complex cell populations across molecular dimensions:
Diagram 2: Multi-omics data integration for CSC biomarker discovery
This integrated approach enables the identification of CSC-specific patterns across different molecular layers, enhancing both the sensitivity and specificity of biomarker validation. AI algorithms excel at detecting non-linear relationships between these data types that would escape conventional analysis methods [79] [80]. For example, the integration of transcriptomic data with proteomic profiles can reveal post-transcriptional regulation patterns specific to CSCs, while epigenomic data can identify methylation signatures that maintain stemness properties [20].
Successful validation of CSC biomarkers across cancer types requires specialized research reagents and computational resources. The following table details essential solutions for this field:
Table 2: Key research reagent solutions for CSC biomarker validation
| Resource Category | Specific Examples | Function in CSC Biomarker Research | Application Notes |
|---|---|---|---|
| CSC Surface Marker Antibodies | Anti-CD44, Anti-CD133, Anti-CD87, Anti-CD90, Anti-EpCAM | Identification and isolation of CSC populations via flow cytometry, immunohistochemistry, and immunocytochemistry | CD44 variants (especially CD44v) show differential expression in metastatic cells; CD133 enrichment increases tumorigenicity [20] |
| CSC Biomarker Databases | BCSCdb, CSCdb, CSCTT, Human miRNA Disease Database (HMDD), CoReCG | Repository of validated CSC biomarkers with confidence scores, therapeutic targets, and interaction data | BCSCdb contains 8307 high-throughput markers, 283 validated markers, and 525 low-throughput markers with confidence scoring [45] |
| Multi-omics Platforms | RNA sequencing (mRNA, miRNA, circRNA, lncRNA), proteomic arrays, epigenetic profiling | Comprehensive molecular profiling of CSC populations across transcriptomic, proteomic, and epigenomic dimensions | Extracellular RNAs (exRNAs) in bodily fluids show promise as non-invasive CSC biomarkers [79] |
| AI/ML Toolkits | Random Forest, XGBoost, CatBoost, Deep Neural Networks, Convolutional Neural Networks | Analysis of high-dimensional data to identify novel biomarker patterns and predict therapeutic responses | CatBoost efficiently classifies patients based on molecular profiles and predicts drug responses [81] |
| Validation Assays | Western blotting, IHC, IF, FACS, RT-PCR, organoid models | Experimental validation of computationally-predicted biomarkers across model systems | Primary tissue validation adds 0.2 to confidence scores in the BCSCdb scoring system [45] |
These research reagents form an integrated ecosystem for CSC biomarker discovery and validation. The combination of high-quality molecular profiling tools, comprehensive databases, and advanced AI analytics enables researchers to move from initial biomarker identification to functional validation across multiple cancer types. Particularly valuable are the curated CSC biomarker databases like BCSCdb that provide standardized confidence metrics, helping researchers prioritize biomarkers for therapeutic development [45].
The integration of AI and machine learning with multi-omics data represents a paradigm shift in CSC biomarker validation across different cancer types. These computational approaches dramatically accelerate the discovery timeline while improving the accuracy and clinical relevance of identified biomarkers. The rigorous validation frameworks, such as the confidence scoring system in BCSCdb, provide standardized metrics for evaluating biomarker utility across diverse cancer contexts.
As AI technologies continue to evolve, their ability to identify subtle patterns in increasingly complex datasets will further enhance our understanding of Cancer Stem Cell biology. This promises not only more reliable biomarkers for diagnosis and prognosis but also novel therapeutic targets for overcoming treatment resistance. The future of CSC research lies in the continued integration of computational and experimental approaches, creating a virtuous cycle of discovery and validation that ultimately improves patient outcomes across the spectrum of malignant diseases.
Navigating CSC Metabolic Plasticity as a Confounding Factor in Biomarker Validation
Cancer stem cells (CSCs) represent a dynamic subpopulation within tumors that demonstrate remarkable metabolic adaptability, enabling them to transition between glycolysis and oxidative phosphorylation (OXPHOS) in response to microenvironmental cues. This metabolic plasticity constitutes a significant confounding factor in the validation of reliable CSC biomarkers, as expression patterns fluctuate with metabolic state transitions. This review systematically examines how metabolic reprogramming influences canonical CSC markers across different cancer types, presents experimental methodologies to account for metabolic context in biomarker validation, and provides a comparative analysis of biomarker stability under varying metabolic conditions. By integrating recent advances in single-cell technologies and spatial transcriptomics, we offer a framework for developing metabolically-informed biomarker validation protocols that enhance reproducibility and clinical translatability in CSC-targeted therapeutic development.
The cancer stem cell (CSC) paradigm posits that a small subpopulation of cells with self-renewal and differentiation capacities drives tumor initiation, progression, and therapy resistance [2] [25]. A defining characteristic of CSCs is their enhanced metabolic plasticity—the ability to dynamically switch between different metabolic programs in response to therapeutic pressure, nutrient availability, and hypoxic conditions within the tumor microenvironment [82] [83]. While this plasticity confers survival advantages to CSCs, it introduces substantial variability in biomarker expression patterns, thereby complicating validation efforts aimed at consistent CSC identification and targeting [10] [25].
The validation of CSC-specific biomarkers represents a critical step in translating basic research findings into clinical applications for tailored therapies. However, conventional validation approaches often fail to account for metabolic context, potentially explaining why promising biomarkers demonstrate inconsistent performance across different experimental conditions and patient populations [84] [25]. As metabolic plasticity has been recognized as an emerging hallmark of cancer [85], there is growing recognition that biomarker validation protocols must incorporate metabolic parameters to achieve reliable, reproducible results. This review addresses this methodological gap by providing a comprehensive analysis of how metabolic states influence biomarker expression and offering practical strategies to navigate this confounding variable in validation pipelines.
Metabolic Basis of CSC Plasticity
The Glycolysis-OXPHOS Spectrum in CSCs
CSCs demonstrate remarkable metabolic flexibility, occupying various positions along the glycolysis-OXPHOS spectrum depending on cancer type, microenvironmental conditions, and therapeutic exposure [82]. Unlike the traditional Warburg effect observed in bulk tumor cells, where aerobic glycolysis predominates even in oxygen-rich conditions, CSCs dynamically reprogram their metabolism to optimize survival under stress [82] [83].
Glycolytic Dependency: Some CSC populations predominantly utilize glycolysis for energy production, supporting rapid proliferation and biomass generation. These cells typically exhibit upregulated glucose transporters (GLUT1, GLUT3), hexokinase 2 (HK2), and lactate dehydrogenase A (LDHA) [83]. This metabolic state is frequently associated with hypoxic regions within tumors where hypoxia-inducible factors (HIF-1α) drive glycolytic gene expression while suppressing mitochondrial oxidative metabolism [82].
OXPHOS Preference: Conversely, certain CSC subpopulations rely heavily on oxidative phosphorylation, particularly in contexts of therapy resistance and metastatic dissemination [82] [86]. These CSCs maintain enhanced mitochondrial function and demonstrate dependencies on fatty acid oxidation (FAO) and glutaminolysis to fuel electron transport chain activity [82] [83]. Quiescent CSCs often reside in this metabolic state, utilizing OXPHOS to maintain stemness while minimizing proliferative activity that might render them vulnerable to conventional therapies [82].
Plasticity Mechanisms: The molecular machinery enabling metabolic switching involves multifaceted regulation at genetic, epigenetic, and post-translational levels. Key regulators include MYC oncogenes, which coordinate glucose and glutamine metabolism; p53 mutations, which remove constraints on glycolytic flux; and mitochondrial dynamics, where fission and fusion events rapidly adapt to energy demands [82]. Recent research has highlighted the role of mitochondrial RNA modifications, particularly NSUN3-mediated m5C and f5C modifications in mitochondrial tRNAMet, in shaping translational efficiency of OXPHOS components and enabling metabolic adaptation in metastatic CSCs [86].
Metabolic Symbiosis in the Tumor Microenvironment
CSCs do not exist in metabolic isolation but engage in cross-talk with stromal components including cancer-associated fibroblasts (CAFs), immune cells, and vascular endothelial cells [85] [2]. This metabolic symbiosis further complicates biomarker validation, as CSC metabolic states—and consequently biomarker expression—may be influenced by paracrine signaling and nutrient exchange within specific niche microenvironments [85] [83]. For instance, CSCs can utilize lactate produced by glycolytic cancer cells through monocarboxylate transporters, effectively employing a " metabolic coupling" strategy that obfuscates biomarker expression patterns when analyzed outside the contextual tissue architecture [83].
Impact of Metabolic Plasticity on Established CSC Biomarkers
Variable Expression of Surface Markers Across Metabolic States
The expression of commonly utilized CSC surface biomarkers demonstrates significant heterogeneity across different metabolic conditions. The table below summarizes how metabolic context influences established CSC markers:
Table 1: Influence of Metabolic State on CSC Biomarker Expression
| Biomarker | Glycolytic Conditions | OXPHOS Conditions | Cancer Types Affected | Mechanistic Insights |
|---|---|---|---|---|
| CD44 | Upregulated [25] [83] | Downregulated/Variable [25] | Breast, colon, glioblastoma [25] [83] | HIF-1α mediated enhancement under hypoxia; OXPHOS promotes differentiation [83] |
| CD133 | Generally stable [25] | Generally stable [25] | Glioblastoma, liver, lung, ovarian [25] | Cholesterol binding function less metabolically sensitive [25] |
| ALDH1 | Upregulated [25] | Downregulated [25] | Breast, prostate, colon, lung, ovarian [25] | Retinoic acid signaling and differentiation state influenced by metabolism [25] |
| ABCB5 | Upregulated [25] | Downregulated [25] | Melanoma [25] | ATP-binding function directly coupled to metabolic state [25] |
| EpCAM | Variable [2] | Variable [2] | Prostate, gastrointestinal [2] | Context-dependent regulation through cell adhesion signaling [2] |
Intracellular Markers and Metabolic Regulation
Intracellular CSC markers, particularly transcription factors governing stemness, exhibit metabolic sensitivity that further complicates validation efforts:
Table 2: Metabolic Regulation of Intracellular CSC Markers
| Marker | Function | Metabolic Regulation | Impact on Biomarker Validation |
|---|---|---|---|
| OCT4 | Pluripotency maintenance [10] | Glycolysis promotes stability; OXPHOS promotes degradation [10] | Protein levels fluctuate with metabolic state; mRNA may not correlate with functional protein [10] |
| SOX2 | Stemness regulation [85] [10] | Hypoxia and HIF-1α enhance expression [85] | Expression varies with oxygen tension in tumor regions [85] |
| NANOG | Self-renewal control [10] | Glycolytic intermediates stabilize protein [10] | Nutrient availability directly impacts detection reliability [10] |
| c-MYC | Metabolic reprogramming [10] [82] | Reciprocal regulation with metabolic state [82] | Creates feedback loops that amplify expression variability [82] |
| KLF4 | Reprogramming factor [10] | Context-dependent (oncogenic/tumor suppressor) [10] | Dual functions lead to inconsistent correlation with stemness [10] |
The experimental data summarized in these tables highlight a critical consideration for biomarker validation: the metabolic context during sample acquisition and analysis significantly influences marker detection and interpretation. For example, analyses performed on CSCs under glycolytic conditions may yield markedly different results compared to those conducted on OXPHOS-dependent CSCs, even within the same tumor type [25] [83].
Experimental Approaches to Account for Metabolic Plasticity in Biomarker Validation
Metabolic Context Reporting Standards
To enhance reproducibility in CSC biomarker studies, researchers should implement comprehensive metabolic reporting alongside traditional experimental parameters. The following diagram illustrates key metabolic parameters that should be documented during biomarker validation studies:
Methodologies for Metabolic State-Specific Biomarker Validation
Advanced experimental approaches enable more accurate biomarker validation by accounting for metabolic heterogeneity:
Single-Cell Multi-Omics Profiling
The integration of single-cell RNA sequencing with metabolic gene signatures allows simultaneous assessment of CSC marker expression and metabolic state in individual cells [85] [2]. This approach reveals subpopulations that might be overlooked in bulk analyses and identifies markers that remain stable across metabolic transitions versus those that fluctuate significantly.
Protocol:
- Cell Preparation: Dissociate tumor tissue to single-cell suspension using gentle enzymatic digestion to preserve surface markers
- Viability Assessment: Confirm >90% viability via trypan blue exclusion or fluorescent viability dyes
- Library Preparation: Utilize 10X Genomics platform for single-cell RNA sequencing with extended read coverage for metabolic genes
- Metabolic Signature Analysis: Apply predefined metabolic gene sets (Glycolysis, OXPHOS, FAO) to classify individual cells
- Correlation Analysis: Determine correlation coefficients between metabolic programs and putative CSC markers
Metabolic Locking Strategies
Employing pharmacological or genetic interventions to "lock" CSCs in specific metabolic states during validation studies enhances reproducibility:
Glycolytic Locking:
- Intervention: 2-Deoxy-D-glucose (2-DG, 10mM) or HIF-1α stabilizers (DMOG, 1mM)
- Duration: 24-hour pretreatment before analysis
- Validation: Confirm glycolytic state via extracellular acidification rate (ECAR) measurement
OXPHOS Locking:
- Intervention: Oligomycin (1μM) or complex I inhibitors (rotenone, 100nM)
- Duration: 12-hour pretreatment before analysis
- Validation: Confirm OXPHOS state via oxygen consumption rate (OCR) measurement
Spatial Metabolomics and Marker Correlation
Integrating matrix-assisted laser desorption/ionization (MALDI) mass spectrometry imaging with immunohistochemistry enables direct correlation of metabolite distributions with biomarker expression in tissue sections [85]. This approach preserves architectural context that is often lost in dissociated cell analyses.
Research Reagent Solutions for Metabolic Plasticity Studies
The following toolkit provides essential reagents for conducting biomarker validation studies that account for metabolic plasticity:
Table 3: Essential Research Reagents for CSC Metabolic Plasticity Studies
| Reagent Category | Specific Examples | Function in Experimental Design | Considerations for Biomarker Validation |
|---|---|---|---|
| Metabolic Phenotyping Assays | Seahorse XF Glycolysis Stress Test, Seahorse XF Mito Stress Test [82] | Quantitatively measure glycolytic flux and mitochondrial function | Establish baseline metabolic state before biomarker analysis; correlate marker expression with metabolic parameters |
| Metabolic Inhibitors | 2-DG (glycolysis inhibitor), Oligomycin (ATP synthase inhibitor), Etomoxir (CPT1 inhibitor) [82] [83] | Experimentally manipulate metabolic pathways | Use for metabolic locking strategies; validate specificity with rescue experiments |
| Hypoxia Modeling Systems | Hypoxic chambers (1% O2), Cobalt chloride, DMOG (HIF stabilizers) [83] | Reproduce physiological oxygen tensions encountered in tumor microenvironments | Essential for evaluating hypoxia-sensitive markers like CAIX and GLUT1 |
| Mitochondrial Dyes | MitoTracker Red CMXRos, TMRM, JC-1 [82] | Assess mitochondrial mass, membrane potential, and activity | Correlate mitochondrial function with stem marker expression at single-cell level |
| CSC Surface Marker Antibodies | CD44-APC, CD133-PE, ALDEFLUOR Kit [25] [83] | Identify and isolate CSC populations | Validate antibody specificity with knockdown controls; compare expression across metabolic conditions |
| Pluripotency Transcription Factor Antibodies | OCT4, SOX2, NANOG [10] [25] | Intracellular staining for stemness factors | Optimize fixation/permeabilization protocols; account for metabolic-dependent expression changes |
Comparative Analysis of Biomarker Stability Across Metabolic Conditions
To guide selection of appropriate biomarkers for validation studies, we conducted a comparative analysis of commonly used CSC markers based on their stability across metabolic transitions:
The metabolic plasticity of CSCs represents a fundamental confounding factor in biomarker validation that demands systematic addressing in experimental design. Rather than dismissing variable biomarkers as unreliable, researchers should document metabolic context as an essential parameter in validation studies. The approaches outlined in this review—including metabolic state reporting standards, single-cell multi-omics integration, and metabolic locking strategies—provide a framework for developing more robust, reproducible biomarker panels that account for this plasticity.
Looking forward, emerging technologies such as CRISPR-based functional screens conducted under different metabolic conditions and AI-driven analysis of multi-omics datasets will further refine our understanding of how metabolism influences CSC identity [2]. Additionally, the development of dual metabolic inhibitors that target both glycolytic and OXPHOS pathways may reveal biomarkers that remain stable across metabolic transitions by preventing state switching [82] [2]. By embracing metabolic complexity rather than attempting to control it, the research community can develop validation protocols that ultimately yield more reliable biomarkers for clinical application in CSC-targeted therapies.
The integration of metabolic parameters into CSC biomarker validation represents not merely a technical adjustment but a paradigm shift in how we define and target this plastic population. As the field advances, acknowledging and designing around metabolic confounding factors will be essential for translating CSC biology into effective clinical interventions that address the root causes of therapeutic resistance and tumor recurrence.
Strategies for Distinguishing CSCs from Normal Stem Cells to Minimize On-Target Toxicity
A cornerstone of modern oncology is the cancer stem cell (CSC) hypothesis, which posits that a small subpopulation of cells with stem-like properties drives tumor initiation, progression, metastasis, and therapeutic resistance [2] [11]. The development of therapies that specifically target these CSCs holds immense promise for achieving durable cancer remissions and preventing relapse. However, a significant and persistent challenge lies in the shared biological properties between CSCs and normal stem cells (NSCs), which can lead to severe on-target toxicity when CSC-directed therapies inadvertently damage vital normal stem cell populations [2]. This comparison guide objectively evaluates current and emerging strategies to differentiate CSCs from NSCs, framing the discussion within the broader thesis of validating CSC biomarkers across diverse cancer types. We synthesize experimental data and methodologies to provide researchers and drug development professionals with a clear framework for designing safer, more precise therapeutic interventions.
Comparative Analysis of Core Biomarkers and Functional Properties
A multi-faceted approach is essential for reliably distinguishing CSCs from NSCs. The following sections provide a detailed comparison of surface markers, functional assays, and signaling pathway activities that define these cell populations.
Surface Marker Expression Profiles
The identification of CSC-specific surface antigens is a primary strategy for their isolation and targeting. However, as illustrated in Table 1, many proposed CSC markers are not exclusive and are also expressed on NSCs or other cell types, necessitating careful validation [2].
Table 1: Comparison of Putative CSC Markers and Their Expression in Normal Stem Cells
| Marker | Common Cancer Types | Reported Expression in Normal Stem/Progenitor Cells | Key Challenges for Specific Targeting |
|---|---|---|---|
| CD44 | Breast, HNSCC, Pancreatic, CRC [2] [11] [87] | Hematopoietic stem cells, mesenchymal stem cells [2] | Broad expression on immune cells and other stromal cells; high heterogeneity [2] |
| CD133 (PROM1) | Glioblastoma, Colon, Liver [2] [11] | Hematopoietic stem cells, neural stem cells, epithelial progenitors [11] | Expression varies with tumor stage and hypoxia; functional role in CSCs not fully defined [2] |
| ALDH1 (High ALDH activity) | Breast, Lung, HNSCC, Bladder [11] [87] | Hematopoietic stem cells, various tissue-specific progenitor cells [11] | A functional marker of enzyme activity, not a direct surface target; expressed in normal detoxifying cells [87] |
| EpCAM | Prostate, Colorectal, Pancreatic [2] | Various epithelial cells and progenitors [2] | Widespread expression on normal epithelial tissues risks off-target damage [2] |
| LGR5 | Colorectal, Gastrointestinal Cancers [2] | Intestinal stem cells [2] | Direct overlap with critical normal stem cell population in the same tissue [2] |
Functional and Metabolic Characteristics
Beyond surface markers, CSCs exhibit distinct functional behaviors and metabolic adaptations that can be exploited for differentiation. Table 2 compares these properties, which form the basis for many functional assays in CSC research.
Table 2: Functional and Metabolic Properties of CSCs vs. NSCs
| Property | Cancer Stem Cells (CSCs) | Normal Stem Cells (NSCs) | Potential for Exploitation |
|---|---|---|---|
| Tumor Initiation | Capable of initiating tumors in immunodeficient mice (e.g., as few as 100 CD44+/CD24- cells in breast cancer) [11] | Non-tumorigenic; support tissue homeostasis | Gold-standard functional assay, but requires in vivo models [11] |
| Therapy Resistance | High resistance to chemo/radiotherapy via ABC transporters, DNA repair, quiescence [2] [11] [87] | Generally sensitive to genotoxic stress, but protected in niches | Targeting resistance mechanisms (e.g., ABC inhibitors) must be carefully timed to spare NSCs [87] |
| Metabolic Plasticity | Flexible utilization of glycolysis, OXPHOS, glutamine, and fatty acid oxidation; adapts to hypoxia [2] | Primarily rely on oxidative phosphorylation; niche-dependent metabolism | Dual metabolic inhibition may target CSC adaptability while NSCs can rely on stable OXPHOS [2] |
| Proliferation State | Often quiescent/slow-cycling in established tumors, but can rapidly proliferate [11] [87] | Careful balance of quiescence and proliferation regulated by niche signals | Targeting quiescent cells is challenging; may require differentiation therapy first [87] |
| DNA Methylation-based Stemness Index (mDNAsi) | Higher mDNAsi correlates with poor prognosis in TCGA cohorts (e.g., COAD, READ) [88] | Lower mDNAsi in differentiated tissues | Computational tool for prognosis, but not a direct therapeutic target [88] |
Experimental Protocols for CSC Identification and Validation
Core Methodological Workflow
A combination of in vitro and in vivo techniques is required to definitively identify and characterize CSCs. The diagram below outlines a standard experimental workflow for their isolation and validation.
Detailed Protocol for Key Assays
1. Fluorescence-Activated Cell Sorting (FACS) for CSC Enrichment
- Objective: Isolate a live cell population based on a specific combination of surface and intracellular markers.
- Procedure:
- Single-Cell Suspension: Generate a single-cell suspension from fresh tumor tissue or cultured cell lines using enzymatic digestion (e.g., collagenase/hyaluronidase).
- Antibody Staining: Incubate cells with fluorochrome-conjugated antibodies against target markers (e.g., anti-CD44-APC, anti-CD24-FITC) and a viability dye (e.g., DAPI) to exclude dead cells. Include isotype controls for gating.
- ALDEFLUOR Assay: To measure ALDH activity, incubate cells with the BODIPY-aminoacetate substrate. A specific inhibitor (DEAB) serves as a negative control. The ALDH⁺ population is identified by high fluorescence.
- Cell Sorting: Use a high-speed cell sorter (e.g., BD FACS Aria) to collect the target population (e.g., CD44⁺CD24⁻ALDH⁺) into a collection tube containing culture medium.
- Data Interpretation: The frequency of the putative CSC population can be correlated with clinical parameters like tumor stage or grade.
2. In Vivo Limiting Dilution Transplantation Assay (LDA)
- Objective: Quantitatively assess the bona fide tumor-initiating capacity of a cell population, which is the definitive functional test for CSCs.
- Procedure:
- Cell Preparation: Serially dilute the sorted putative CSCs and control populations (e.g., 10,000, 1,000, 100, 10 cells).
- Transplantation: Mix each cell dose with Matrigel and orthotopically inject into immunocompromised mice (e.g., NOD/SCID/IL2Rγ⁻/⁻ or NSG mice). A minimum of 8-10 mice per group is recommended for statistical power.
- Monitoring: Monitor mice for tumor formation over several months. Tumor formation is confirmed by palpation and/or bioluminescent imaging if cells are luciferase-tagged.
- Analysis: Calculate the frequency of tumor-initiating cells using extreme limiting dilution analysis (ELDA) software, which compares the number of tumor-positive mice per injection to the number of cells injected.
- Data Interpretation: A population is considered enriched for CSCs if it has a significantly higher tumor-initiating frequency (e.g., 1 in 100 cells) compared to the non-CSC population (e.g., 1 in 100,000 cells) [11].
Signaling Pathways as a Source of Differential Vulnerability
The nuanced differences in the activity and context of core stemness pathways between CSCs and NSCs provide a promising avenue for therapeutic discrimination. The following diagram and analysis detail these critical pathways.
Comparative Pathway Analysis:
Wnt/β-catenin Pathway: In NSCs, Wnt signaling is tightly regulated by extracellular antagonists (e.g., DKK1) and niche cells to maintain homeostasis. In contrast, CSCs often exhibit constitutive activation of Wnt signaling due to mutations (e.g., APC in CRC) or aberrant microenvironmental cues [11] [89]. Therapeutic inhibitors like LGK974 (targeting Porcupine) are in clinical trials (NCT01351103) and may have a wider therapeutic window in cancers with hyperactive Wnt signaling [24] [26].
Notch Pathway: Notch signaling in NSCs is typically paracrine, requiring contact with neighboring ligand-expressing cells. CSCs, however, can exploit autocrine Jagged-1/Notch signaling loops to sustain their self-renewal independently of the niche [11]. Furthermore, γ-secretase inhibitors (GSIs) can differentially affect CSCs and NSCs based on the dependency of the specific tissue, offering a potential window for intervention.
Hedgehog (Hh) Pathway: While Hh signaling is crucial for embryonic development and some adult NSCs, its activity in many adult tissues is low. CSCs in malignancies like pancreatic cancer and glioblastoma often re-activate the Hh pathway in a tumor-autonomous manner, making them more susceptible to Smoothened (SMO) inhibitors like vismodegib than most quiescent adult NSCs [89].
Advanced Therapeutic Strategies and Research Tools
Emerging Therapeutic Approaches to Minimize Toxicity
Moving beyond monotherapies, combination strategies that leverage the unique CSC microenvironment and plasticity are showing promise in improving specificity.
Metabolic Targeting: CSCs display remarkable metabolic plasticity, shifting between glycolysis and oxidative phosphorylation (OXPHOS) [2]. Simultaneous inhibition of both pathways (e.g., using a glycolysis inhibitor like 2-DG with an OXPHOS inhibitor like metformin) may synergistically target CSCs while sparing NSCs that rely on a more stable metabolic program. Glutaminase inhibitors (e.g., CB-839) are also under investigation in clinical trials (NCT02771626) [24].
Immunotherapy-Based Targeting: The development of CAR-T cells targeting CSC-associated antigens (e.g., CD133, EpCAM) is a promising frontier [2] [24]. Clinical trials such as NCT03423992 and NCT02541370 are evaluating CD133-CAR-T cells. A key strategy to avoid on-target/off-tumor toxicity is the use of "logic-gated" CARs that require the presence of two CSC-specific antigens to fully activate, thereby increasing specificity.
Differentiation Therapy: Forcing CSCs to differentiate into non-tumorigenic, therapy-sensitive cells is a powerful way to circumvent their inherent resistance. This can be achieved using epigenetic modulators like DNA methyltransferase inhibitors (e.g., Guadecitabine) or retinoids. By eroding the CSC state, these agents can sensitize tumors to subsequent conventional chemotherapy [24] [87].
Nanoparticle-Mediated Precision Targeting: Third-generation photosensitizers and drug carriers use nanoparticles functionalized with CSC-targeting ligands (e.g., anti-CD44 or anti-EGFR antibodies) [90]. This allows for the spatial and temporal control of cytotoxic agent delivery, concentrating the therapeutic effect within the tumor and minimizing systemic exposure to normal stem cell compartments.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for CSC Research
| Reagent / Tool | Function in CSC Research | Example Application |
|---|---|---|
| Fluorochrome-Conjugated Antibodies (e.g., anti-CD44, CD133, EpCAM) | Identification and isolation of putative CSCs via FACS or MACS. | Sorting CD44+/CD24- population from breast cancer cell lines for subsequent functional assays [2] [11]. |
| ALDEFLUOR Kit | Measures aldehyde dehydrogenase (ALDH) enzyme activity, a functional CSC marker. | Identifying and isolating the ALDH-bright cell population from dissociated HNSCC tumors [11] [87]. |
| Ultra-Low Attachment Plates | Prevents cell adhesion, enabling the growth of non-adherent 3D spheres that enrich for stem/progenitor cells. | Performing sphere-forming assays to assess the self-renewal capacity of sorted cells in vitro [11]. |
| Pathway-Specific Small Molecule Inhibitors (e.g., LGK974 (Wnt), DAPT (Notch), Vismodegib (Hh)) | Probing the functional importance of stemness signaling pathways in CSCs. | Treating patient-derived organoids to determine if pathway inhibition reduces CSC frequency and tumorigenicity [24] [89]. |
| Cytokine/Chemokine Arrays | Profiling the secretome of CSCs to understand their crosstalk with immune cells in the TME. | Analyzing conditioned media from CSC vs. non-CSC cultures to identify key factors like IL-6, TGF-β, CCL5 that recruit immunosuppressive cells [24] [26]. |
The strategic distinction of CSCs from NSCs is not a hurdle to be overcome by a single "magic bullet," but a continuous process of refining diagnostic and therapeutic precision. A successful clinical strategy will inevitably involve multi-parametric profiling that integrates specific surface markers, metabolic dependencies, and pathway activation states within the context of the tumor microenvironment. The ongoing validation of CSC biomarkers across different cancer types, supported by advanced single-cell omics and bioinformatics, is steadily revealing the critical nuances that separate malignant stemness from normal tissue maintenance. By leveraging these differences through intelligent drug design, combination therapies, and sophisticated delivery systems, the field moves closer to the ultimate goal of eradicating cancer at its root while preserving the regenerative capacity of the patient.
Cross-Cancer Validation and Clinical Application of CSC Biomarkers
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies, driving tumor initiation, progression, metastasis, and recurrence [2] [25]. The identification and targeting of CSCs are crucial for improving cancer treatment outcomes, yet their elusive nature and dynamic properties present significant challenges. A cornerstone of CSC research involves the discovery and validation of biomarkers that enable their isolation, characterization, and targeting. However, the field grapples with a fundamental dichotomy: the quest for universal, conserved biomarkers across cancer types versus the reality of context-dependent markers that vary by tissue of origin, tumor microenvironment, and disease stage [2] [12].
This pan-cancer analysis systematically compares conserved and context-dependent CSC biomarkers, integrating latest findings from single-cell multi-omics, spatial transcriptomics, and functional validation studies. We dissect the molecular signatures that define CSC populations across diverse carcinomas, providing a structured framework for researchers and drug development professionals to navigate the complexity of CSC biomarker discovery and its applications in precision medicine.
Conserved CSC Biomarkers: Universal Stemness Signatures
Conserved CSC biomarkers are molecules, pathways, or functional attributes consistently present across multiple cancer types, often reflecting core stemness properties. These biomarkers represent the closest approximation to universal CSC identifiers and provide common therapeutic targets.
Table 1: Conserved CSC Biomarkers Across Cancer Types
| Biomarker | Molecular Function | Cancer Types with Documented Expression | Conservation Level |
|---|---|---|---|
| CD44 | Cell surface adhesion receptor, hyaluronan binding [13] | Breast Cancer, Colon Cancer, Glioblastoma, Head and Neck SCC [25] [91] | High |
| CD133 (PROM1) | Transmembrane glycoprotein, cholesterol binding [25] | Breast Cancer, Liver Cancer, Lung Cancer, Ovarian Cancer, Glioblastoma [2] [25] | High |
| ALDH1 | Intracellular enzyme, aldehyde oxidation [25] | Breast, Prostate, Colon, Lung, and Ovarian Cancers [25] | High |
| ABCG2 | Cell surface transporter, drug efflux [25] | Lung, Pancreatic, Liver, Breast, and Ovarian Cancers [25] | Medium |
| EpCAM | Cell surface adhesion molecule [2] | Prostate Cancer, Gastrointestinal Cancers [2] | Medium (mainly epithelial) |
The conservation of these biomarkers underscores fundamental biological processes essential for CSC maintenance. For instance, CD44 and CD133 facilitate interactions with the niche microenvironment, while ALDH1 activity and ABCG2 expression contribute directly to therapy resistance mechanisms [25] [13]. Despite their widespread utility, a critical limitation remains: none are entirely specific to CSCs, as they are also expressed, albeit often at lower levels, in normal stem cells or non-malignant cells, posing a challenge for targeted therapies to achieve a favorable therapeutic window [2] [25].
Context-Dependent CSC Biomarkers: Tissue-Specific Identities
Context-dependent biomarkers highlight the influence of tissue origin and mutational background on CSC phenotypes. Their expression is often restricted to specific cancer types or lineages.
Table 2: Context-Dependent CSC Biomarkers
| Biomarker | Molecular Function | Cancer Types | Notes on Specificity |
|---|---|---|---|
| LGR5 | Wnt receptor, stem cell marker [2] | Gastrointestinal Cancers [2] | Marks normal and cancerous intestinal stem cells |
| Nestin | Intermediate filament protein [2] | Glioblastoma (GBM) [2] | Neural lineage marker |
| CD34 | Cell surface glycoprotein, adhesion [25] | Acute Myeloid Leukemia (AML) [25] | Not a reliable marker for solid tumor CSCs |
| ABCB5 | Cell surface transporter, drug efflux [25] | Melanoma [25] | Specific to melanoma CSCs |
| Notch2 | Transmembrane receptor, cell signaling [92] | Pancreatic Ductal Adenocarcinoma (PDAC) [92] | Increased in PDAC vs. normal pancreas |
The presence of context-dependent biomarkers like LGR5 and Nestin demonstrates how CSC identity is shaped by the developmental pathways of their tissue of origin [2]. Furthermore, comparative studies reveal that even putative conserved markers can exhibit context-dependent behavior. For example, in pancreatic ductal adenocarcinoma (PDAC), the expression of CD133 and Notch2 was found to be inversely correlated with tumor grade, a pattern not universally observed for these markers in other cancers [92]. This highlights the necessity of validating biomarker function and clinical relevance within specific tumor contexts.
Signaling Pathways as Functional Biomarkers
Beyond surface proteins, conserved intracellular signaling pathways act as functional biomarkers and regulators of CSC stemness. Targeting these pathways presents an alternative strategy to overcome the limitations of surface marker heterogeneity.
Pathways such as Wnt/β-catenin, Hedgehog, and Notch are evolutionarily conserved regulators of stem cell fate and are frequently dysregulated in CSCs across diverse cancer types [24] [13]. Their activation promotes fundamental CSC properties like self-renewal, epithelial-mesenchymal transition (EMT), and therapy resistance [13]. Furthermore, these pathways are not isolated; they engage in extensive crosstalk with the tumor immune microenvironment. For instance, CSC-derived cytokines activate STAT3 and NF-κB signaling in immune cells like myeloid-derived suppressor cells (MDSCs) and tumor-associated macrophages (TAMs), which in turn release factors that reinforce CSC stemness, creating a resilient feedback loop [24]. This intricate network positions these pathways as high-priority targets for combination therapies.
Experimental Protocols for Biomarker Validation
The validation of CSC biomarkers relies on a multidisciplinary toolkit that combines phenotypic isolation with functional assessment. The following established protocols are considered the gold standard in the field.
Surface Marker-Based Isolation and Analysis
This protocol utilizes flow cytometry to isolate putative CSCs based on cell surface antigen expression.
- Key Reagents: Fluorescently conjugated antibodies against targets like CD44, CD133, and EpCAM [13].
- Procedure: Single-cell suspensions from tumor tissues or dissociated xenografts are stained with antibody panels. Cells are then sorted using a Fluorescence-Activated Cell Sorter (FACS) into marker-positive and marker-negative populations for downstream functional assays [13].
- Validation: The tumor-initiating capacity of sorted populations is tested in vivo, often in immunocompromised mice. A significantly higher frequency of tumor formation from the marker-positive population validates its functional enrichment for CSCs [2] [13].
Functional Assay for Self-Renewal: Sphere Formation
The sphere formation assay evaluates the self-renewal and clonogenic potential of CSCs in vitro.
- Key Reagents: Serum-free medium supplemented with growth factors (EGF, bFGF), and B27 supplement, on low-attachment plates [13].
- Procedure: Single cells are plated at low density in non-adherent conditions. The formation of non-adherent, spherical colonies (tumorspheres) over 1-2 weeks is monitored.
- Validation: Self-renewal is confirmed by serially passaging dissociated spheres, with the capacity to form new spheres over multiple generations indicating the presence of CSCs [13]. This assay is a functional correlate of stemness independent of specific surface markers.
Aldefluor Assay for ALDH Enzymatic Activity
The Aldefluor assay identifies CSCs based on high levels of intracellular aldehyde dehydrogenase (ALDH) activity.
- Key Reagents: The Aldefluor substrate (BODIPY-aminoacetaldehyde) and the specific ALDH inhibitor diethylaminobenzaldehyde (DEAB) as a control [13].
- Procedure: Live cells are incubated with the substrate, which is converted into a fluorescent product retained inside cells with high ALDH activity. The DEAB control tube inhibits this reaction, establishing a baseline for fluorescence. Cells with fluorescence intensity above the control (ALDH-high) are isolated via FACS.
- Validation: The ALDH-high population is tested for enhanced tumorigenicity in vivo and resistance to chemotherapeutics, confirming its association with the CSC phenotype [25] [13].
The Scientist's Toolkit: Essential Research Reagents
Successful dissection of CSC biomarkers requires a suite of specialized reagents and tools. The following table details essential solutions for researchers in this field.
Table 3: Key Research Reagent Solutions for CSC Biomarker Studies
| Research Reagent | Specific Function | Application Example |
|---|---|---|
| Fluorochrome-Conjugated Antibodies | Bind specifically to cell surface antigens (e.g., CD44, CD133) for detection and isolation. | Isolation of CD44+/CD24- breast CSCs via Flow Cytometry [25] [13]. |
| Aldefluor Assay Kit | Measures intracellular ALDH enzyme activity to identify a functional CSC population. | Identification and sorting of ALDH-high CSCs from lung cancer cell lines [25] [13]. |
| Pathway-Specific Inhibitors | Small molecules that selectively inhibit key signaling pathways (e.g., Wnt, Notch, Hedgehog). | Functional validation of pathway necessity using LGK974 (Wnt inhibitor) [24]. |
| Low-Attachment Plates | Provide a non-adherent surface for cell culture, preventing differentiation and enabling sphere growth. | Tumorsphere formation assay to assess self-renewal capability [13]. |
| CRISPR/Cas9 Systems | Enable targeted gene knockout or editing to assess gene function in stemness and tumorigenicity. | Functional genomic screens to identify novel CSC-specific vulnerabilities [2] [12]. |
| Single-Cell RNA-Seq Kits | Allow for barcoding, reverse transcription, and library preparation from individual cells. | Profiling tumor heterogeneity and identifying novel CSC subpopulations [12]. |
Emerging Paradigms and Technologies
The field of CSC biomarker research is rapidly evolving, moving beyond static marker definitions. Key emerging trends include:
- Dynamic State Transitions: Single-cell multi-omics and trajectory inference tools challenge the static CSC model, revealing that stemness is a transient, reversible state influenced by the microenvironment and therapy [12]. This plasticity allows non-CSCs to acquire stem-like properties, complicating biomarker-based targeting.
- AI and Computational Tools: Machine learning algorithms analyze high-dimensional data to derive stemness indices (e.g., mRNAsi, CytoTRACE) that predict CSC potential from transcriptomic data without pre-defined markers, offering a powerful complementary approach [2] [12].
- Spatial Context: Spatial transcriptomics and proteomics map the location of cells with CSC signatures within the tumor architecture, revealing how specific niches maintain stemness and drive conserved transcriptional programs across cancer types [2] [93].
This pan-cancer analysis delineates a complex landscape of CSC biomarkers, characterized by a core set of conserved signaling pathways and surface molecules co-existing with a plethora of context-dependent markers shaped by tissue-specific biology. The functional validation of these biomarkers through rigorous experimental protocols remains paramount. The future of CSC targeting lies in combinatorial strategies that integrate pathway inhibitors with immunotherapy, leveraging our growing understanding of conserved CSC-immune cell crosstalk [24]. Furthermore, the adoption of advanced computational and single-cell technologies is refining the very definition of CSCs, steering the field toward a more dynamic, state-based understanding that will ultimately inform the development of more effective therapeutic interventions to eradicate these drivers of tumor recurrence and therapy resistance.
The validation of robust biomarkers is a critical cornerstone of modern precision oncology, enabling early detection, accurate prognosis, and prediction of treatment response. Biomarkers provide valuable information about the molecular characteristics of individual tumors, allowing clinicians to tailor treatment strategies to each patient's unique profile [94]. The clinical success of several immunotherapies has further underscored the need for reliable biomarkers to evaluate which patients are most likely to benefit from specific treatments [94]. However, the validation pathway from discovery to clinical application remains challenging, with less than 1% of published cancer biomarkers ultimately entering clinical practice [95]. This comparative analysis examines the validation landscapes of biomarkers across three major cancer categories—breast, lung, and gastrointestinal cancers—to identify common challenges, distinctive considerations, and emerging solutions in translational biomarker research.
The validation process requires demonstrating clinical utility across diverse patient populations and standardized testing conditions. Despite increasing interest and publication output in cancer biomarker research, significant hurdles persist in clinical translation [77]. These challenges include the inherent heterogeneity of human cancers, biological differences between preclinical models and human physiology, and a lack of robust validation frameworks with standardized protocols [95]. This review synthesizes current validation methodologies, performance metrics, and emerging trends across different cancer types to provide researchers and drug development professionals with a comprehensive comparative framework for biomarker evaluation.
Comparative Analysis of Biomarker Validation Across Cancer Types
Breast Cancer Biomarkers
Table 1: Validation Status of Key Breast Cancer Biomarkers
| Biomarker Category | Specific Biomarkers | Clinical Validation Status | Primary Applications | Key Challenges |
|---|---|---|---|---|
| Multigene Assays | Oncotype DX, MammaPrint, uPA/PAI-1 | Routinely employed in clinical practice [96] | Prognostication in early-stage HR+/HER2- breast cancer [96] | Cost, accessibility in resource-limited settings |
| Hormone Receptors | ER, PR | Cornerstone predictive biomarkers [96] | Predicting response to endocrine therapy [96] | Temporal heterogeneity in metastatic setting |
| Circulating Biomarkers | ctDNA (ESR1 mutations) | Emerging validation for clinical use [96] | Monitoring treatment response and resistance [96] | Standardization of detection methods |
| Immunotherapy Biomarkers | PD-L1, TMB, TILs | Variable predictive value across subtypes [97] | Identifying responders to immune checkpoint inhibitors [97] | Discrepancies between primary and metastatic sites |
Breast cancer exemplifies successful biomarker validation with well-established multigene assays and receptor status guiding therapeutic decisions. The validation of biomarkers such as hormone receptors (ER, PR) and HER2 has transformed treatment paradigms, enabling targeted therapies that significantly improve patient outcomes [96]. These traditional biomarkers are now complemented by validated multigene assays including Oncotype DX and MammaPrint, which are routinely employed to inform adjuvant treatment decisions in hormone receptor-positive, HER2-negative subtypes [96]. The robust validation of these biomarkers across large, prospective randomized trials has solidified their role in clinical practice.
Emerging biomarkers in breast cancer include circulating tumor DNA (ctDNA) and immunotherapy biomarkers such as tumor mutational burden (TMB) and tumor-infiltrating lymphocytes (TILs). Notably, ESR1 mutations detected in ctDNA have emerged as potential indicators of resistance to aromatase inhibitors [96]. Validation studies have revealed distinctive mutational features between primary and recurrent/metastatic tumors in breast cancer patients, with enrichment of PD-L1 amplification in metastatic triple-negative breast cancer (TNBC), highlighting the necessity to re-biopsy metastatic tumors for accurate biomarker assessment [97]. Current challenges in breast cancer biomarker validation include identifying robust biomarkers to predict response to chemotherapy and radiotherapy, which remains a critical unmet need [96].
Lung Cancer Biomarkers
Table 2: Lung Cancer Biomarker Validation Approaches and Metrics
| Validation Approach | Study Examples | Sample Characteristics | Key Validation Metrics | Limitations |
|---|---|---|---|---|
| Large-scale Screening Cohorts | LEAP Study (n=2,841) [98] | Longitudinal biospecimens with LDCT imaging | Correlation with imaging findings and LC diagnosis [98] | Limited diversity in participant demographics |
| Blood-based Biomarker Panels | Multiple combined biomarkers | Pre-diagnostic samples within 5 years of diagnosis [98] | Improved risk stratification accuracy [98] | False positive rates in high-risk populations |
| Metabolic Biomarkers | Glycolytic enzymes (LDHA, PKM2) [99] | Tissue and liquid biopsy samples | Diagnostic and prognostic correlation [99] | Early translational stage for most biomarkers |
Lung cancer biomarker validation has been advanced through large, well-characterized cohort studies with longitudinal biospecimen collection. The LEAP study, an international prospective cohort, established a comprehensive resource with 2,841 participants undergoing low-dose computed tomography (LDCT) screening with matched blood specimens collected at baseline and annual intervals [98]. This study design provides a robust framework for validating promising biomarkers in the context of lung cancer screening, with aims to improve risk stratification and nodule malignancy assessment. The cohort includes 126 pre-diagnostic lung cancer samples collected within five years of diagnosis, offering valuable material for validation studies [98].
Blood-based biomarkers represent a promising approach for enhancing the effectiveness of lung cancer screening programs. Metabolic biomarkers have shown particular promise, with consistent upregulation of glycolytic enzymes such as LDHA and PKM2 across multiple cancer types, including lung cancer [99]. These enzymes contribute to cancer progression, metastasis, and therapy resistance, offering potential as diagnostic, prognostic, and predictive biomarkers [99]. While several metabolic proteins show strong potential for clinical translation, only a few, such as tumor M2-pyruvate kinase (TuM2-PK) and serum LDH measurement, have progressed into clinical use or trials [99]. The integration of multi-omics approaches, including genomics, transcriptomics, and proteomics, is paving the way for more sensitive and specific biomarkers for early lung cancer detection [94].
Gastrointestinal Cancer Biomarkers
Table 3: GI Cancer Biomarker Performance Characteristics
| Biomarker | Cancer Type | Sensitivity (%) | Specificity (%) | Clinical Applications | Limitations |
|---|---|---|---|---|---|
| CEA | Colorectal | 18.8-52.2 (early-stage) [100] | Variable | Monitoring treatment response, detecting metastases [100] | High false-positive rate for early detection |
| CEA Panel | Colorectal | 85.3 (with other markers) [100] | 95 (with other markers) [100] | Early-stage detection when combined with other markers [100] | Requires multiple assays |
| SEPT9 | Colorectal | 76.6 [100] | 95.9 [100] | FDA-approved for non-invasive CRC detection [100] | Cost, technological requirements |
| CA19-9 | Gastric | Variable | Variable | Monitoring disease progression [100] | Limited diagnostic utility alone |
Gastrointestinal cancers, particularly colorectal and gastric cancers, present distinct biomarker validation challenges due to their anatomical location and frequently late-stage diagnosis. Conventional biomarkers for colorectal cancer such as carcinoembryonic antigen (CEA) demonstrate limitations as standalone diagnostic tools, with sensitivity for early-stage detection ranging from only 18.8% to 52.2% [100]. However, when CEA is combined with other glycoproteins (CA19-9, CA242, CA72-4, and CA125) in a panel, sensitivity significantly increases to 85.3% with 95% specificity for early-stage CRC detection [100]. This validation approach demonstrates how combining multiple biomarkers can overcome the limitations of individual markers.
Emerging non-invasive biomarkers for gastrointestinal cancers include circulating tumor DNA (ctDNA) and methylation markers such as SEPT9. The SEPT9 DNA methylation test has been validated as an FDA-approved diagnostic biomarker for colorectal cancer, with demonstrated sensitivity of 76.6% and specificity of 95.9% [100]. This biomarker has been commercialized as CRC screening tools under names such as Epi proColon 2.0 and ColoVantage [100]. Liquid biopsy approaches that analyze circulating tumor cells (CTCs), exosomes, and ctDNA from body fluids offer promising alternatives to traditional tissue biopsy, addressing limitations such as invasiveness and tissue sampling variability [100]. However, CTCs currently demonstrate limited utility for early detection of colorectal cancer due to low sensitivity and specificity [100].
Experimental Methodologies in Biomarker Validation
Analytical Validation Techniques
Figure 1: Biomarker Analytical Validation Workflow. This diagram outlines the standardized workflow for genomic biomarker validation, from sample processing through sequencing and bioinformatic analysis to functional confirmation.
Robust biomarker validation requires standardized analytical methodologies across different technology platforms. Next-generation sequencing (NGS) has emerged as a fundamental technology for biomarker assessment, with nearly 100 novel cancer biomarker solutions currently available in the market utilizing this technology [94]. The analytical workflow typically begins with sample processing and DNA extraction from formalin-fixed, paraffin-embedded (FFPE) tumor tissue specimens or peripheral blood lymphocytes using standardized kits such as the ReliaPrep FFPE gDNA Miniprep System or QIAamp DNA Blood Mini Kit [97]. Following DNA fragmentation, indexed NGS libraries are prepared using kits such as the NEBNext Ultra DNA Library Prep Kit for Illumina [97].
Hybridization capture with customized gene panels represents a targeted approach for biomarker validation. Studies have employed panels covering approximately 1.5 Mbp of the genome and 1,021 cancer-related genes for comprehensive biomarker assessment [97]. Following target enrichment, indexed libraries are sequenced on platforms such as the Gene+Seq-2000 sequencing system [97]. Bioinformatic analysis includes read mapping to reference genomes, local realignment around single nucleotide variants and small insertions/deletions, and sophisticated variant calling algorithms to distinguish true biomarkers from technical artifacts [97]. This standardized approach enables consistent biomarker validation across different cancer types and research institutions.
Functional Validation Approaches
Functional validation strategies are essential to confirm the biological relevance of candidate biomarkers and their therapeutic implications. While traditional biomarker analysis primarily focuses on the presence or quantity of specific biomarkers, functional assays provide critical evidence about biomarker activity and functional impact on disease processes or treatment responses [95]. These approaches represent a shift from correlative to functional evidence, strengthening the case for real-world clinical utility.
In the context of cancer stem cell (CSC) biomarkers, functional validation often includes sphere-forming assays, in vivo tumor initiation experiments, and treatment resistance assessments. The validation of stromal cell sialylation as a biomarker for immune suppression in colorectal cancer exemplifies a comprehensive functional validation approach [101]. Researchers used genetic knockdown of the sialyltransferase ST6GALNAC6 to demonstrate reduced expression of Siglec-10 ligands in mesenchymal stromal cells [101]. Functional co-culture assays then confirmed that hypersialylated stromal cells induced Siglec-10 on macrophages and NK cells, impairing macrophage phagocytosis and NK cell cytotoxicity [101]. Sialidase treatment reversed this immunosuppression, restoring antitumor immune functions—a finding validated in immunocompetent mouse models [101]. This multifaceted functional validation approach provides compelling evidence for the biological and therapeutic relevance of stromal sialylation as a biomarker in colorectal cancer.
Technological Platforms and Research Models
Advanced Preclinical Models
Figure 2: Advanced Preclinical Models for Biomarker Validation. This diagram illustrates how advanced model systems better replicate human tumor biology and integrate with multi-omics technologies to improve biomarker prediction.
Advanced preclinical models have significantly enhanced the predictive validity of biomarker studies by better replicating human tumor biology. Traditional animal models frequently fail to correlate with human clinical disease, resulting in poor prediction of treatment responses [95]. Patient-derived xenograft (PDX) models, developed by implanting human tumor tissue into immunodeficient mice, more accurately recapitulate cancer characteristics, tumor progression, and evolution observed in human patients [95]. These models have played crucial roles in validating key biomarkers including HER2 and BRAF, as well as predictive, metabolic, and imaging biomarkers [95]. The demonstrated accuracy of PDX models for biomarker validation is highlighted by studies showing that KRAS mutant PDX models do not respond to cetuximab, potentially expediting biomarker validation if utilized earlier in drug development [95].
Three-dimensional organoid cultures and co-culture systems provide complementary platforms for biomarker validation. Organoids retain expression of characteristic biomarkers more effectively than two-dimensional culture models and have been used to predict therapeutic responses and guide personalized treatment selection [95]. Three-dimensional co-culture systems that incorporate multiple cell types (including immune, stromal, and endothelial cells) offer comprehensive models of the human tissue microenvironment, enabling more physiologically accurate cellular interactions for biomarker validation [95]. These advanced models become particularly powerful when integrated with multi-omics strategies that leverage genomics, transcriptomics, and proteomics to identify context-specific, clinically actionable biomarkers that might be missed with single-platform approaches [95].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Biomarker Validation Studies
| Research Reagent Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| Nucleic Acid Extraction Kits | ReliaPrep FFPE gDNA Miniprep System, QIAamp DNA Blood Mini Kit [97] | DNA isolation from FFPE tissue and blood samples [97] | DNA quality and fragment length critical for NGS |
| Library Preparation Kits | NEBNext Ultra DNA Library Prep Kit for Illumina [97] | NGS library construction from fragmented DNA | Compatibility with sequencing platform |
| Target Enrichment Panels | Custom panels (1,021 cancer-related genes) [97] | Hybridization capture of genomic regions of interest | Coverage uniformity, off-target rates |
| Cell Culture Media | Defined media for organoid cultures [95] | Maintenance of 3D culture systems | Batch-to-batch consistency |
| Immunoassay Reagents | Antibodies for CD44, CD133, CD44, LGR5 [2] | Identification and isolation of cancer stem cells | Specificity validation across models |
| Enzyme Inhibitors | Sialyltransferase inhibitors (3FAX) [101] | Functional validation of glycosylation biomarkers | Concentration optimization required |
The biomarker validation pipeline relies on specialized research reagents that ensure reproducibility and accuracy across experiments. Nucleic acid extraction kits form the foundation of genomic biomarker studies, with systems such as the ReliaPrep FFPE gDNA Miniprep System optimized for challenging sample types like formalin-fixed, paraffin-embedded tissues [97]. The quality and integrity of extracted DNA significantly impact downstream sequencing applications, making selection of appropriate extraction methodologies crucial for validation studies. For liquid biopsy approaches, kits such as the QIAamp DNA Blood Mini Kit enable efficient isolation of circulating tumor DNA from blood samples [97].
Library preparation reagents, including the NEBNext Ultra DNA Library Prep Kit for Illumina, facilitate the construction of sequencing-ready libraries from fragmented DNA [97]. Custom target enrichment panels covering cancer-related genes enable focused investigation of genomic regions relevant to specific cancer types [97]. For functional validation studies, specialized reagents such as sialyltransferase inhibitors (3FAX) and sialidases (E610) enable mechanistic investigation of biomarker function, as demonstrated in studies of stromal cell sialylation in colorectal cancer [101]. Antibodies targeting putative cancer stem cell markers such as CD44, CD133, and LGR5 facilitate the isolation and characterization of these therapy-resistant cell populations [2]. Consistent quality and performance of these research reagents across experiments and laboratories is essential for robust biomarker validation.
Emerging Trends and Future Perspectives
The field of cancer biomarker validation is rapidly evolving with several emerging trends shaping future research directions. Multi-omics integration represents a paradigm shift from single-platform biomarker discovery to comprehensive molecular profiling. Rather than focusing on single targets, multi-omic approaches leverage multiple technologies including genomics, transcriptomics, and proteomics to identify context-specific, clinically actionable biomarkers [95]. The depth of information obtained through these integrated approaches enables identification of potential biomarkers for early detection, prognosis, and treatment response across different cancer types [95]. Recent studies have demonstrated that multi-omic approaches have helped identify circulating diagnostic biomarkers in gastric cancer and discover prognostic biomarkers across multiple cancers [95].
Artificial intelligence and machine learning are revolutionizing biomarker discovery and validation by identifying patterns in large datasets that cannot be detected using traditional methods [95]. AI-driven genomic profiling has already demonstrated improved responses to targeted therapies and immune checkpoint inhibitors, resulting in better response rates and survival outcomes for patients with various cancer types [95]. The full potential of these computational approaches relies on access to large, high-quality datasets that include comprehensive characterization from multiple sources [95]. This necessitates collaboration between AI researchers, oncologists, and regulatory agencies to establish standards for AI-derived biomarker validation.
Longitudinal biomarker assessment represents another emerging trend, moving beyond single timepoint measurements to dynamic monitoring of biomarker changes throughout disease progression and treatment. Repeatedly measuring biomarkers over time provides a more comprehensive view, revealing subtle changes that may indicate cancer development or recurrence before clinical symptoms appear [95]. This approach is particularly valuable for monitoring treatment resistance, as demonstrated by the emergence of ESR1 mutations in ctDNA during aromatase inhibitor therapy in breast cancer [96]. The integration of longitudinal sampling into clinical trial designs and routine practice will enhance our understanding of biomarker dynamics and enable more responsive treatment adaptations.
The global research landscape for cancer biomarkers continues to expand, with investigations demonstrating consistent growth in publications between 2015 and 2023, followed by a significant surge from 2023 to 2024 [77]. China has emerged as the country with the highest number of publications, followed by the United States, the United Kingdom, Japan, and Italy [77]. This global research interest underscores the recognized potential of biomarkers to transform cancer diagnosis and treatment. However, despite these promising trends, challenges remain in clinical translation, including the need for large-scale, multi-center validation studies and standardized analytical frameworks [77]. Addressing these challenges will require continued international collaboration and data sharing to accelerate the translation of promising biomarkers from bench to bedside.
{ARTICLE CONTENT STARTS HERE}
Liquid Biopsies and Circulating CSC Markers: A Minimally Invasive Tool for Monitoring
Liquid biopsy has emerged as a transformative, non-invasive approach for cancer diagnosis and monitoring. This review objectively compares the performance of circulating biomarkers, with a focused analysis on circulating tumor cells (CTCs) and their utility in profiling cancer stem cells (CSCs). We detail the experimental protocols for isolating and characterizing these cells, provide structured comparisons of key CSC markers, and outline essential research reagents. Supported by current data and visualization, this guide underscores the significant potential of liquid biopsies in validating CSC biomarkers across diverse cancer types, offering researchers and drug development professionals a critical resource for advancing metastatic cancer research and therapeutic development.
The global liquid biopsy market is projected to grow from USD 6.39 billion in 2025 to USD 25.43 billion by 2035, reflecting its escalating importance in oncology [102]. This growth is fueled by the critical need to overcome the limitations of traditional tissue biopsies, which are invasive, cannot be performed repeatedly, and fail to capture the full heterogeneity of a tumor [103] [104] [105]. Liquid biopsies address these challenges by enabling minimally invasive, serial sampling of tumor-derived components from blood and other bodily fluids, thus providing a dynamic window into tumor evolution [106].
For researchers focused on cancer metastasis and therapeutic resistance, circulating tumor cells (CTCs) represent a particularly valuable analyte. As viable tumor cells shed into the vasculature, CTCs are the principal agents of metastasis and are the only liquid biopsy component that allows for functional characterization [107]. A crucial subpopulation of CTCs exhibits properties of cancer stem cells (CSCs)—a small group of cells with capabilities of self-renewal, differentiation, and tumorigenicity that are implicated in tumor initiation, progression, and therapy resistance [108]. The convergence of liquid biopsy technology and CSC marker analysis offers an unprecedented opportunity to monitor these critical drivers of cancer progression in real-time, providing insights that are foundational to the development of more effective, targeted therapies.
Comparative Analysis of Liquid Biopsy Biomarkers
Liquid biopsies encompass a range of tumor-derived components, each with distinct advantages and technical challenges. The primary biomarkers include circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and extracellular vesicles (EVs), such as exosomes [103] [104] [105]. The following table provides a structured, objective comparison of their performance characteristics for researchers evaluating the most suitable analyte for specific applications.
Table 1: Performance Comparison of Key Liquid Biopsy Biomarkers
| Biomarker | Composition / Origin | Key Strengths | Major Limitations | Primary Research Applications |
|---|---|---|---|---|
| Circulating Tumor Cells (CTCs) | Viable intact cells shed from primary or metastatic tumors [109]. | - Enables functional studies & drug screens [107].- Provides whole genome/transcriptome data [109].- Capable of ex vivo culture and xenografting [105]. | - Extreme rarity (~1-10 CTCs/mL of blood among billions of blood cells) [105] [109].- Short half-life (1-2.5 hours) [103].- Lacks a universal, specific marker for all CTC types [108]. | - Studying metastatic biology [109].- Monitoring therapy response [105].- Prognostic assessment [103]. |
| Circulating Tumor DNA (ctDNA) | Short fragments of DNA released by tumor cells via apoptosis or necrosis [103] [104]. | - Short half-life (~2 hours) allows for real-time monitoring of tumor dynamics [105].- High specificity for tumor-associated mutations [103].- Technologically mature detection methods (e.g., ddPCR, NGS) [104]. | - Can be difficult to detect in early-stage disease or low-shedding tumors [102].- Does not provide information on viable cell functionality [107].- Susceptible to noise from clonal hematopoiesis (CHIP) [104]. | - Detecting minimal residual disease (MRD) [105].- Identifying targetable mutations [103].- Tracking tumor clonal evolution [104]. |
| Extracellular Vesicles (EVs)/ Exosomes | Lipid-bilayer vesicles secreted by cells, carrying proteins, RNA, and DNA [103] [104]. | - Protect molecular cargo from degradation [104].- Abundant in biofluids [105].- Reflect cell of origin, including surface proteins. | - Complex isolation and standardization [104].- Heterogeneous in size and content.- Challenging to specifically isolate tumor-derived EVs. | - Investigating cell-cell communication [105].- Discovering novel protein and RNA biomarkers [104]. |
Among these, the CTC segment is projected to account for over 70% of the global liquid biopsy market revenue by biomarker type in 2025, underscoring its central role in cancer diagnostics and research [102]. While ctDNA excels in tracking specific genomic alterations, CTCs are the only analyte that provides a viable, functional snapshot of the tumor, making them indispensable for researching CSCs and the metastatic cascade [107].
Isolation and Characterization of CTCs and Circulating CSCs
Experimental Protocols for CTC Enrichment and Detection
The extreme rarity and heterogeneity of CTCs necessitate sophisticated and highly sensitive methods for their isolation. The protocols can be broadly categorized into label-dependent (affinity-based) and label-independent (biophysics-based) techniques [109].
1. Immunomagnetic Enrichment (Label-Dependent):
- Principle: This method uses magnetic beads conjugated with antibodies against surface antigens expressed on CTCs. The most common target is the epithelial cell adhesion molecule (EpCAM) [109].
- Protocol Details:
- Blood Collection: Collect 7.5-10 mL of peripheral blood in specialized CellSave or EDTA tubes to preserve cell integrity.
- Enrichment: Incubate the blood sample with anti-EpCAM coated magnetic beads. The CellSearch system, the only FDA-cleared method for CTC enumeration, is a prime example of this technology [103] [109]. It performs an immunomagnetic enrichment step followed by automated staining.
- Staining & Identification: After enrichment, cells are stained with fluorescently labeled antibodies against cytokeratins (CK, epithelial markers), a leukocyte marker (CD45), and a viability dye (DAPI). CTCs are typically defined as nucleated (DAPI+), CK+, and CD45- [109].
- Advantages & Limitations: High specificity for epithelial cancers. A key limitation is the potential to miss CTCs that have undergone Epithelial-Mesenchymal Transition (EMT) and downregulated EpCAM [109].
2. Microfluidic Enrichment (Label-Dependent/Independent):
- Principle: Microfluidic chips (e.g., CTC-Chip, Cluster-Chip) use precise fluid control and miniature architectures to isolate CTCs. This can be based on antibody capture (e.g., anti-EpCAM coated microposts) or on biophysical properties like cell size and deformability [105] [109].
- Protocol Details:
- Sample Preparation: Blood is processed to remove red blood cells via lysis or density gradient centrifugation.
- Microfluidic Processing: The prepared sample is pumped through the microfluidic device at optimized flow rates. CTCs are captured based on affinity or size, while blood cells are washed away.
- Recovery: Captured CTCs can be released for downstream molecular analysis (e.g., single-cell sequencing) or cultured [109].
- Advantages & Limitations: Allows for high-purity recovery and the potential to capture both epithelial and EMT-like CTCs. Throughput and chip fouling can be challenges [109].
3. Size-Based Filtration (Label-Independent):
- Principle: Technologies like ISET (Isolation by Size of Epithelial Tumor Cells) use porous membranes to separate larger CTCs from smaller hematological cells [109].
- Protocol Details:
- Filtration: Whole blood is passed through a membrane with pores of a defined diameter (e.g., 7-8 µm).
- Analysis: CTCs, which are generally larger, are retained on the membrane and can be identified by immunofluorescence or other staining techniques.
- Advantages & Limitations: It is marker-agnostic, making it suitable for capturing CTCs independent of EpCAM expression. It may miss smaller CTCs or be clogged by large numbers of white blood cells [109].
Workflow for Circulating CSC Marker Analysis
The following diagram illustrates a generalized, integrated workflow for isolating CTCs and subsequently identifying and characterizing the circulating CSC subpopulation.
Validation of CSC Markers Across Cancer Types
CSCs constitute only 0.05–1% of the total tumor cell population, making their identification and validation a significant challenge [108]. The isolation and study of this subpopulation from CTCs rely on a combination of cell surface markers and functional assays. The table below summarizes key CSC markers, their utility across different cancers, and associated signaling pathways, providing a comparative guide for researchers.
Table 2: Comparative Analysis of Key Cancer Stem Cell (CSC) Markers
| Marker | Cancer Type(s) with Demonstrated Utility | Molecular Function & Pathway Association | Experimental Notes & Co-expression |
|---|---|---|---|
| CD44 | Breast, Lung, Prostate, Colorectal [108] [73] | Hyaluronic acid receptor; regulates EMT, self-renewal via interaction with RAS and Wnt pathways [73]. | Often used in combination (e.g., CD44+/CD24- in breast cancer). A study identified EpCAM+/CD166+/CD44+ triple-positive NSCLC cells with CSC properties [108]. |
| CD133 (PROM1) | Brain, Colon, Liver, Lung [108] [73] | Transmembrane glycoprotein; function not fully defined, but linked to PI3K/AKT, NF-κB, and Wnt/β-catenin signaling pathways promoting self-renewal [73]. | A common marker for isolating CSCs from various solid tumors. Its expression alone may not be sufficient, requiring functional validation [108]. |
| ALDH (ALDH1A1) | Breast, Lung, Ovarian, Pancreatic [108] | Intracellular enzyme; confers chemoresistance by detoxifying agents; active in retinoic acid signaling, regulating cell proliferation and differentiation [108]. | Measured by ALDEFLUOR assay (functional activity). Often combined with surface markers (e.g., ALDHhigh + CD44+ in lung cancer) to define a highly tumorigenic subpopulation [108]. |
| EpCAM | Colorectal, Pancreatic, Hepatocellular, Breast [109] | Epithelial cell adhesion molecule; modulates cell-cell adhesion, proliferation, and Wnt signaling [109]. | While a primary marker for CTC capture, its expression may be lost in EMT. Its role as a CSC marker is often in combination with others [109]. |
| LGR5 | Colorectal, Gastric [73] | Receptor for R-spondins; potentiates Wnt/β-catenin signaling, a critical pathway for stem cell maintenance [73]. | A key marker for intestinal stem cells and associated CSCs. |
The selection of markers is critical, as no single marker is universally specific for CSCs. Research indicates that using a combination of markers (e.g., EpCAM+/CD166+/CD44+ or ALDHhigh + CD44+) significantly improves the identification and isolation of a highly tumorigenic CTC subpopulation with stem-like properties [108]. Furthermore, the expression of these markers on CTCs is dynamic and can be influenced by therapy, highlighting the need for serial monitoring via liquid biopsy.
The Researcher's Toolkit: Essential Reagents and Solutions
The effective isolation and analysis of CTCs and circulating CSCs depend on a suite of specialized research reagents and platforms. The following table details essential materials and their functions for designing robust experimental workflows.
Table 3: Essential Research Reagents and Platforms for CTC/CSC Analysis
| Reagent / Solution / Platform | Primary Function in Workflow | Key Considerations for Researchers |
|---|---|---|
| Anti-EpCAM Magnetic Beads | Immunomagnetic positive selection and enrichment of epithelial CTCs from whole blood [109]. | Core component of the FDA-cleared CellSearch system. Efficiency depends on EpCAM expression levels on target CTCs [109]. |
| CellSearch System | Automated, FDA-cleared platform for CTC enumeration. Integrates immunomagnetic enrichment and immunofluorescence staining [103] [109]. | Considered a gold standard for clinical CTC counts. Provides high standardization but is limited to enumeration and fixed-cell analysis. |
| ALDEFLUOR Assay Kit | Functional assay to measure ALDH enzymatic activity in viable cells to identify the ALDHhigh CSC subpopulation [108]. | Requires flow cytometry for analysis. Often used in combination with surface marker staining (e.g., CD44) to define CSCs. |
| Fluorochrome-Conjugated Antibodies | Immunophenotyping for detection of CSC surface markers (e.g., CD44, CD133) and for defining CTCs (anti-CK, anti-CD45) [109]. | Panel design is critical. Requires validation for compatibility and minimal spectral overlap in flow cytometry or immunofluorescence. |
| Microfluidic Chips (e.g., CTC-Chip) | Label-independent or antibody-based capture of CTCs from whole blood, enabling high-purity recovery [105] [109]. | Ideal for subsequent molecular or functional analysis due to gentle processing and viable cell retrieval. |
| Single-Cell RNA Sequencing Reagents | Genome-wide transcriptomic profiling of individual CTCs to uncover heterogeneity, EMT status, and stem-like signatures [109]. | Reveals the molecular landscape of CTCs and circulating CSCs without predefined marker biases. |
Liquid biopsy, particularly the analysis of CTCs for CSC markers, represents a paradigm shift in how researchers and clinicians can monitor cancer. This minimally invasive tool provides dynamic insights into the biology of metastasis and therapy resistance that are simply unattainable through static tissue biopsies. The validation of CSC biomarkers like CD44, CD133, and ALDH across different cancer types, as facilitated by advanced CTC isolation protocols, is paving the way for a deeper understanding of tumor hierarchy and evolution.
Future research will be geared toward standardizing isolation and analysis methods to improve reproducibility across labs [105]. Furthermore, the integration of artificial intelligence with multi-omics data from CTCs and ctDNA holds the promise of deciphering complex, real-time tumor dynamics [102]. As these technologies mature, the routine clinical application of liquid biopsies for early detection, monitoring minimal residual disease, and guiding personalized therapy based on a patient's evolving CSC profile will become a tangible reality, ultimately improving outcomes for cancer patients.
{ARTICLE CONTENT ENDS HERE}
Cancer Stem Cells (CSCs) represent a subpopulation of tumor cells with capabilities of self-renewal, differentiation, and tumorigenicity, playing a critical role in driving tumor heterogeneity and resistance to conventional therapies [25]. These cells, often comprising less than 1% of tumor cells, demonstrate remarkable resistance to chemotherapy and radiation therapy, largely due to their quiescent nature, enhanced DNA repair mechanisms, and expression of drug efflux pumps [25] [2]. The surviving CSCs can rebuild aggressive, treatment-resistant tumors, leading to disease recurrence and metastasis [25]. This biological understanding has catalyzed the development of therapies specifically targeting CSCs, with CAR-T-cell therapies and antibody-drug conjugates (ADCs) emerging as two promising modalities. The clinical advancement of these therapies depends significantly on the successful identification and validation of CSC-specific biomarkers that can serve as reliable therapeutic targets [25] [12].
The transition from biomarker discovery to targeted therapy requires navigating considerable challenges. CSC identity is increasingly recognized as a dynamic state rather than a fixed cellular phenotype, influenced by both intrinsic genetic programs and extrinsic microenvironmental cues [2] [12]. This plasticity complicates the identification of universally reliable surface markers. Furthermore, the lack of exclusivity of many CSC biomarkers, which are often shared with normal stem cells or non-stem cancer cells, poses significant hurdles for achieving therapeutic specificity and minimizing off-target toxicity [25] [2]. Despite these challenges, ongoing research continues to validate novel targets and refine therapeutic approaches, bringing CSC-directed precision medicine closer to clinical reality.
Established CSC Biomarkers and Associated Targeted Therapies
The development of CSC-directed therapies relies on targeting specific cell surface and intracellular biomarkers. These biomarkers facilitate the precise identification and targeting of CSCs while providing insight into their functional biology.
Table 1: Established CSC Biomarkers and Their Therapeutic Applications
| Biomarker | Cancer Types | Therapeutic Modality | Therapeutic Agent/Approach | Development Status |
|---|---|---|---|---|
| CD44 | Breast, Colon, Glioblastoma, Pancreas, Prostate [25] [20] | Antibody-drug conjugates, Targeted liposomes | Hyaluronic acid-based drug delivery; Silibinin/Cabazitaxel liposomes [20] | Preclinical; Clinical trials |
| CD133 (Prominin-1) | Glioblastoma, Colon, Pancreatic, Breast Cancer [25] [20] | Not specified | Sorafenib (reduces CD133+ population); Nifuroxazide (STAT3 inhibitor) [20] | Experimental/Preclinical |
| ALDH1 | Breast, Prostate, Colon, Lung, Ovarian Cancer [25] | Prodrug therapy | CSC-activatable prodrugs [25] | Experimental/Preclinical |
| EpCAM | Prostate Cancer [2] | CAR-T-cell Therapy | EpCAM-targeted CAR-T cells [2] | Preclinical |
| BCMA | Multiple Myeloma [110] | CAR-T-cell Therapy | Ide-cel, Cilta-cel [110] | FDA Approved |
| ABCB5 | Melanoma [25] | Not specified | Not specified | Research |
| CD87 (uPAR) | Lung Cancer [20] | Not specified | 64Cu-DOTA-AE105 (diagnostic) [20] | Phase I Clinical Trial |
The biomarkers in Table 1 represent promising yet imperfect targets. For instance, CD44 is a transmembrane glycoprotein involved in cell adhesion and migration, and influences key signaling pathways like Wnt, Notch, and Hedgehog that maintain CSC properties [20]. Similarly, CD133, a cell-surface glycoprotein that binds cholesterol, is conserved across multiple cancer types and is associated with increased tumorigenicity and chemotherapy resistance [25] [20]. A significant challenge is that these surface markers are rarely exclusive to CSCs and are often expressed by non-stem cancer cells or healthy cells, albeit at different abundances, creating a risk of on-target, off-tumor effects [25]. This underscores the necessity for robust biomarker validation across different cancer types and patient populations.
CAR T-Cell Therapies: Targeting CSC Surface Antigens
Chimeric Antigen Receptor (CAR) T-cell therapy involves engineering a patient's own T-cells to express synthetic receptors that recognize specific tumor surface antigens, redirecting immune cells to kill cancerous cells. This approach holds significant potential for eradicating CSCs by directly targeting their unique surface markers.
Clinical Evidence and Trial Data
Clinical trials have demonstrated the viability of targeting CSC antigens. In multiple myeloma, B-cell maturation antigen (BCMA)-directed CAR T-cells have shown remarkable efficacy. The ide-cel (idecabtagene vicleucel) therapy achieved a 73% overall response rate with a 33% complete response rate or better in triple-refractory patients, while cilta-cel (ciltacabtagene autoleucel) demonstrated an unprecedented 97% overall response rate in the CARTITUDE-1 trial [110]. A cost-effectiveness analysis predicted that despite high upfront costs, these CAR-T therapies provide significantly greater quality-adjusted life years (QALYs) gained compared to conventional therapies like belantamab mafodotin [110].
Beyond hematologic malignancies, preclinical studies support targeting solid tumor CSCs. For prostate cancer, CAR T-cells engineered to target EpCAM (epithelial cell adhesion molecule), a CSC-specific marker, demonstrated effectiveness in eliminating CSCs and improving outcomes in preclinical models [2]. These findings validate the principle that CSC surface antigens can be successfully targeted by engineered immune cells.
Experimental Workflow for CAR T-Cell Development
The standard methodology for developing CSC-targeted CAR T-cells involves a multi-step process:
- Target Identification: CSC-specific surface antigens (e.g., EpCAM, CD133, CD44) are identified through single-cell RNA sequencing, proteomic analyses, and functional assays [2] [12].
- CAR Design: A synthetic gene is constructed encoding an extracellular single-chain variable fragment (scFv) derived from a monoclonal antibody specific for the target antigen. This is fused to intracellular T-cell signaling domains (commonly CD3ζ) plus one or more co-stimulatory domains (e.g., CD28, 4-1BB).
- T-Cell Engineering: Patient T-cells are activated and transduced with the CAR gene using viral vectors (e.g., lentivirus, retrovirus) or non-viral methods (e.g., transposons, CRISPR/Cas9).
- Expansion and Validation: Engineered CAR T-cells are expanded ex vivo to therapeutic doses. The product is validated for CAR expression, sterility, potency, and specificity.
- Preclinical Testing: CAR T-cell efficacy and safety are evaluated in vitro using CSC-rich cell cultures and in vivo using immunocompromised mouse models xenotransplanted with human CSCs [2].
- Clinical Trials: Following preclinical success, CAR T-cell products are administered to patients in phased clinical trials to assess safety, dosing, and antitumor activity.
Antibody-Drug Conjugates (ADCs): Precision Payload Delivery to CSCs
Antibody-Drug Conjugates (ADCs) are a class of biotherapeutics that combine the specificity of monoclonal antibodies with the potent cytotoxicity of small-molecule payloads. They are designed to selectively deliver chemotherapeutic agents to cancer cells expressing specific surface antigens, minimizing systemic exposure and off-target toxicity.
ADC Technology and Payloads for CSC Targeting
ADCs target cell surface antigens overexpressed on CSCs, internalize upon binding, and release their cytotoxic payload within the target cell [111]. The therapeutic success of ADCs hinges on the stability of the linker connecting the antibody to the payload and the potency of the payload itself. Current ADC payloads relevant to CSC targeting include:
- Microtubule-disrupting agents (e.g., auristatins like MMAE, maytansinoids like DM1/DM4) which inhibit tubulin polymerization, triggering mitotic arrest and apoptosis [111].
- Topoisomerase I inhibitors (e.g., camptothecin derivatives like deruxtecan) which cause DNA single-strand breaks during replication. These are particularly relevant for tumors with homologous recombination deficiency (e.g., BRCA1/2 mutations) and may also suppress HIF-1α, a protein involved in CSC maintenance [111].
- DNA alkylating agents (e.g., pyrrolobenzodiazepines) which cause irreversible DNA cross-linking [111].
CSC-Targeting ADC Strategies and Clinical Outlook
While no ADC is yet approved specifically for a CSC indication, several are in development that target known CSC markers. The strategy often involves targeting antigens like CD44, CD133, or CD87 with antibodies conjugated to highly potent payloads. For example, CD44-targeting using hyaluronic acid as a natural ligand is being explored for the delivery of toxins or chemotherapeutics directly to CSCs [20]. Similarly, the CD87 (uPAR) receptor is a promising therapeutic target for lung CSCs, with a diagnostic agent (64Cu-DOTA-AE105) already in Phase I trials [20].
A key advantage of ADCs in targeting CSCs is the "bystander effect" exhibited by some payloads, where the released cytotoxic agent can diffuse into and kill adjacent cancer cells within a heterogeneous tumor, even if they do not express the target antigen. This is crucial for eradicating both CSCs and the bulk tumor population they generate [111].
Diagram 1: Mechanism of Action of an Antibody-Drug Conjugate (ADC) Targeting a Cancer Stem Cell (CSC). The ADC binds a specific surface antigen, is internalized, and releases its cytotoxic payload, leading to CSC death.
Emerging Technologies and Future Directions
The field of CSC-targeted therapy is rapidly evolving, driven by technological advancements that provide deeper insights into CSC biology.
Single-Cell Multi-Omics and Artificial Intelligence
Advanced analytical platforms are redefining our understanding of CSCs. Single-cell RNA sequencing (scRNA-seq) enables high-resolution profiling of rare CSC subpopulations and reveals their functional heterogeneity [12]. This technology has challenged the traditional view of CSCs as static entities, suggesting instead that stemness is a dynamic, context-dependent state that non-CSCs can acquire under environmental pressures like hypoxia or therapy [12].
Computational tools leveraging Artificial Intelligence (AI) and Machine Learning (ML) are now essential for analyzing complex single-cell data. These include:
- CytoTRACE/CytoTRACE2: Predicts cellular differentiation states and stemness potential based on gene counts and expression patterns [12].
- RNA Velocity: Predicts immediate future cell states from ratios of unspliced to spliced mRNA [12].
- StemID & SCENT: Calculate transcriptional or signaling entropy to quantify a cell's differentiation potential or phenotypic plasticity [12].
These tools allow for the dynamic characterization of CSC potential without relying solely on traditional surface markers, opening new avenues for identifying therapeutic vulnerabilities during state transitions [12].
The Scientist's Toolkit: Key Reagents for CSC Therapy Research
Table 2: Essential Research Reagents for Developing CSC-Directed Therapies
| Reagent / Solution | Function in Research | Specific Application Example |
|---|---|---|
| Single-Cell RNA-seq Kits | High-resolution transcriptomic profiling of rare CSC populations | Identifying novel CSC biomarkers and dynamic state transitions [12] |
| CRISPR/Cas9 Libraries | Functional genomic screens to identify essential genes and vulnerabilities in CSCs | In vitro and in vivo dropout screens to discover new ADC or CAR-T targets [2] [12] |
| Recombinant Antibodies (scFv) | Generation of targeting moieties for CAR-T and ADC platforms | Creating the antigen-binding domain for a CAR targeting EpCAM or CD133 [2] |
| Cytotoxic Payloads (e.g., MMAE, Deruxtecan) | Potent cell-killing agents for ADC construction | Conjugating to anti-CD44 antibody for selective killing of CD44+ CSCs [111] |
| Cytokines (IL-2, IL-7, IL-15) | Ex vivo expansion and maintenance of engineered T-cells | Culturing and enhancing the persistence of CD133-targeting CAR T-cells [110] |
| 3D Organoid Culture Systems | Modeling tumor heterogeneity and CSC-TME interactions ex vivo | Preclinical testing of ADC/CAR-T efficacy against patient-derived CSCs [2] |
The translation of CSC biomarkers into effective therapies via CAR-T cells and ADCs represents a frontier in oncology. While significant challenges remain—including tumor heterogeneity, CSC plasticity, and on-target/off-tumor toxicity—the progress to date is substantial. The validation of targets like BCMA in multiple myeloma and the preclinical success against markers like EpCAM and CD44 provide a strong foundation.
Future success will depend on an integrative approach. This includes leveraging single-cell multi-omics to define CSC states with greater precision, employing AI-driven bioinformatics to nominate the most promising targets, and developing combination therapies that simultaneously target CSCs and the bulk tumor. The ongoing clinical trials and technological innovations provide a compelling outlook for ultimately overcoming therapeutic resistance and relapse driven by this resilient cell population.
Regulatory Pathways and Frameworks for Approving CSC Biomarker-Based Companion Diagnostics
Companion diagnostics (CDx) represent a critical bridge between therapeutic products and patient selection, serving as essential tools in precision oncology. For biomarkers related to cancer stem cells (CSCs)—a small subpopulation of tumor cells with self-renewal and differentiation capabilities—the development and regulatory approval of CDx tests present unique challenges and opportunities [10]. These biomarkers are crucial because CSCs contribute significantly to therapy resistance, metastasis, and cancer recurrence, making them attractive targets for novel cancer therapeutics [45] [10]. The regulatory pathways for these advanced diagnostics are evolving rapidly, particularly with the integration of artificial intelligence and digital pathology, which are reshaping the validation and implementation landscape [112] [113].
The development of CDx for CSC biomarkers must account for several inherent complexities, including the plasticity of CSCs, their interaction with microenvironments, and their heterogeneous expression patterns across different cancer types [10]. Currently, over 60 FDA-approved companion diagnostic tests exist in hematology and oncology, with numerous others in development pipelines, including those targeting emerging CSC-related biomarkers [113]. This guide examines the current regulatory frameworks, validation methodologies, and comparative performance data for CSC biomarker-based companion diagnostics, providing researchers and drug development professionals with essential insights for navigating the approval process.
Current Regulatory Landscape for Companion Diagnostics
Established Regulatory Pathways and Emerging Trends
Regulatory frameworks for companion diagnostics continue to evolve as biomarker technologies advance. The U.S. Food and Drug Administration (FDA) and other regulatory bodies have established pathways for CDx approval, with recent adaptations to address innovative technologies such as AI-enabled digital pathology and liquid biopsy platforms [112] [113]. The transition from traditional glass slide interpretation to digital image analysis, accelerated by recent FDA clearances for digital pathology systems, represents a significant shift in diagnostic validation paradigms [113].
A key development in the regulatory landscape is the growing acceptance of biomarker-driven trial designs, including basket trials, adaptive designs, and umbrella studies, all of which rely on biomarkers to match patients to therapies more effectively [114]. These trial designs are particularly relevant for CSC biomarkers, which often target rare biomarker expressions or specific glycan patterns that require sophisticated detection methods [15]. Regulatory agencies are increasingly emphasizing the need for diverse and representative datasets during biomarker validation to ensure accuracy across different patient populations and prevent the reinforcement of health disparities [112].
The integration of AI-based diagnostic algorithms into regulatory frameworks presents both opportunities and challenges. While AI can enhance pattern recognition, reduce scoring subjectivity, and automate routine tasks, it also requires new validation approaches to ensure reproducibility and clinical utility [113] [114]. Regulatory alignment for these technologies continues to evolve within frameworks such as the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), with emphasis on clinical validation in real-world settings using large, diverse datasets [114].
Table 1: Key Regulatory Considerations for CSC Biomarker-Based Companion Diagnostics
| Regulatory Aspect | Current Status | Emerging Trends |
|---|---|---|
| Digital Pathology Integration | FDA clearances for digital pathology systems obtained [113] | Development of CDx that can only be scored with digital pathology [113] |
| AI Algorithm Validation | Evolving regulatory frameworks [114] | Emphasis on diverse datasets to avoid bias and ensure generalizability [112] [114] |
| Trial Design | Acceptance of biomarker-driven designs (basket, umbrella, adaptive trials) [114] | Enriched study designs that adapt based on emerging biomarker insights [114] |
| Biomarker Specificity | Focus on detection methods for rare biomarkers [112] [15] | Glycosylation-based detection surpassing traditional protein markers [15] |
| Multi-Omics Approaches | Increasing incorporation of genomic, proteomic, and transcriptomic data [114] | Integration of histopathology with molecular data for improved predictive accuracy [114] |
Validation Frameworks for CSC Biomarkers
Analytical Validation Requirements
The analytical validation of CSC biomarker-based companion diagnostics requires rigorous assessment of performance characteristics, including sensitivity, specificity, reproducibility, and reliability. For CSC biomarkers, which often target rare cell populations within heterogeneous tumors, validation presents unique challenges. Trial enrollment often depletes available samples, limiting material available for diagnostic validation studies, which can delay companion diagnostic development and approval [112]. This challenge is particularly acute for rare CSC biomarkers, where obtaining sufficient clinical samples for validation remains a significant bottleneck.
The detection method selected for CSC biomarkers significantly impacts validation requirements. Traditional approaches have relied on surface markers such as CD133, CD44, EpCAM, and ALDH1A1 [15] [10]. However, newer methods targeting specific glycan patterns or glycosylation changes have demonstrated superior specificity in some cancer types. For instance, in non-small cell lung cancer (NSCLC), a lectin-based detection method (MIX) recognizing specific glycosylation patterns outperformed CD133 in prognostic value and CSCs detection efficiency [15]. This method enabled better stratification of early-stage patients at high risk of relapse, suggesting its potential for clinical implementation.
Algorithm validation represents another critical component for AI-enabled CSC biomarker tests. As Katie Robertson, Ph.D., oncology network lead at Roche Diagnostics, notes: "There will also be some CDx that will only be used to score with digital pathology because the slide can't be evaluated with the naked eye" [113]. This trend underscores the growing importance of robust computational validation frameworks alongside traditional biological validation. The Roche open environment, which allows seamless access to algorithms developed both internally and by third parties, exemplifies the collaborative approach needed for comprehensive validation [113].
Clinical Validation Standards
Clinical validation of CSC biomarker-based companion diagnostics must establish a clear relationship between the test result and relevant clinical outcomes, such as treatment response, progression-free survival, or overall survival. The validation cohorts must be sufficiently large and diverse to ensure generalizability across different patient populations. As noted in recent research, "without representative data, these technologies risk misclassifying biomarker status, limiting patient access to appropriate treatments and reinforcing existing disparities" [112].
For CSC biomarkers, clinical validation often involves demonstrating utility in predicting therapy resistance or tumor aggressiveness. In bladder cancer, an 8-gene CSC prognostic signature (ALDH1A1, CBX7, CSPG4, DCN, FASN, INHBB, MYC, NCAM1) demonstrated strong predictive power for overall survival in both TCGA and GEO cohorts [36]. Similarly, in NSCLC, the lectin-based MIX detection method showed significant prognostic value for overall survival, suggesting its potential for detecting CSCs directly linked to tumor aggressiveness [15].
Retrospective validation using existing datasets represents an important step in clinical validation. For example, the BCSCdb database contains information on 710 biomarkers of cancer stem cells, including 171 low-throughput biomarkers identified in primary tissue referred to as clinical biomarkers [45] [36]. These resources enable researchers to conduct initial clinical validations before proceeding to prospective trials. However, ultimately, prospective clinical trials remain the gold standard for establishing clinical utility, particularly for regulatory approval.
Table 2: Key Experimental Protocols for CSC Biomarker Validation
| Validation Method | Protocol Description | Application in CSC Biomarkers |
|---|---|---|
| Flow Cytometry with CSC Markers | Cell sorting based on surface markers (CD133, EpCAM) or lectin binding (MIX) [15] | Isolation and quantification of CSCs from heterogeneous tumor populations [15] |
| Clonogenic Assay | Sorted cells seeded in ultra-low attachment plates with defined medium; sphere formation quantified over 4-8 weeks [15] | Assessment of self-renewal capability and stemness properties [15] |
| In Vivo Tumorigenicity | Sorted cells transplanted into immunodeficient mice at limiting dilutions [15] [10] | Evaluation of tumor-initiating capacity, a defining feature of CSCs [15] [10] |
| Drug Sensitivity Testing | Treatment of sorted CSCs with increasing drug doses; IC50 determination after 72 hours [15] | Assessment of therapy resistance mechanisms in CSCs [15] |
| Digital Pathology Analysis | AI-based analysis of histopathology images for prognostic and predictive signals [114] | Identification of CSC-related patterns in standard histology slides [114] |
Comparative Analysis of CSC Biomarker Detection Platforms
Traditional vs. Emerging Detection Methodologies
The landscape of CSC biomarker detection encompasses both traditional protein-based markers and emerging approaches targeting functional characteristics or specific post-translational modifications. Traditional markers such as CD133, CD44, EpCAM, and ALDH1A1 have been widely used for CSC identification and isolation across multiple cancer types [10]. However, these markers often lack specificity, as they may be expressed in both CSCs and differentiated tumor cells [15]. For example, while CD133 protein is present in both CSCs and differentiated tumor cells, the AC133 epitope is selectively masked and expressed only in CSCs [15].
Emerging detection methodologies offer promising alternatives with potentially superior specificity. The lectin-based MIX approach, which recognizes specific glycan patterns exclusively expressed by CSCs, has demonstrated enhanced prognostic value compared to CD133 in both colorectal and lung cancers [15]. In NSCLC, this method detected CSCs with higher tumorigenic capacity than CD133+ cells and provided significant prognostic value for overall survival in early-stage patients [15]. Similarly, chromosomal instability (CIN) signature biomarkers represent another innovative approach, capable of predicting resistance to key chemotherapy classes across multiple cancer types using a single genomic assay [115].
Multi-omics approaches that integrate genomic, proteomic, transcriptomic, and histopathology data are increasingly important for comprehensive CSC characterization [114]. AI-driven analysis of these complex datasets can reveal hidden patterns and relationships between biomarkers and disease pathways, potentially exceeding human observational capacity and improving reproducibility [114]. For instance, at DoMore Diagnostics, AI-based digital biomarkers derived from standard histopathology slides have demonstrated the ability to outperform established molecular and morphological markers in predicting colorectal cancer outcomes [114].
Performance Metrics Across Platforms
When comparing different platforms for CSC biomarker detection, several performance metrics must be considered, including sensitivity, specificity, prognostic value, and predictive utility for treatment response. The lectin-based MIX method demonstrated significant enrichment of CSCs compared to CD133+ cells in NSCLC, with sorted MIX+ cells exhibiting higher tumorigenic capacity in vivo [15]. Clinically, this method showed prognostic value for overall survival in early-stage NSCLC patients, suggesting its potential for identifying patients at high risk of relapse who might benefit from more aggressive therapy [15].
For genomic approaches, CIN signature biomarkers have shown impressive predictive value for chemotherapy resistance across multiple cancer types. In ovarian cancer, patients classified as resistant to platinum therapy had approximately 1.5x higher risk of treatment failure, while those resistant to taxane therapy had ~7x higher risk of failure compared to alternative treatments [115]. Similarly strong predictive performance was observed in metastatic prostate, breast, and sarcoma cases [115].
Multi-gene signatures derived from CSC-related genes also demonstrate robust prognostic performance. In bladder cancer, an 8-gene prognostic signature (ALDH1A1, CBX7, CSPG4, DCN, FASN, INHBB, MYC, NCAM1) effectively stratified patients into risk categories with significant differences in overall survival in both TCGA and independent GEO validation cohorts [36]. The nomogram incorporating this signature with clinical parameters like age and tumor stage demonstrated high predictive accuracy for 1-, 3-, and 5-year survival rates [36].
Diagram Title: CSC Biomarker Validation Workflow
Case Studies: CSC Biomarkers in Development Pipelines
Emerging CSC-Related Biomarkers and Their Diagnostic Potential
Several promising CSC-related biomarkers are currently advancing through development pipelines, targeting various cancer types with significant unmet needs. In non-small cell lung cancer (NSCLC), researchers are addressing the lack of approved therapies for patients with overexpression of c-MET protein, which occurs in 35% to 72% of NSCLC tumors [113]. Companion diagnostics for c-MET protein overexpression are in development, targeting different patient populations [113]. Similarly, in gastric cancer, where 61% of patients present with advanced disease at diagnosis, a companion diagnostic for FGFR2b—expressed in 20% to 30% of gastric cancers—represents a promising approach for a cancer with a 5-year survival rate of only 7% for metastatic disease [113].
The PTEN biomarker in prostate cancer illustrates another compelling case study. PTEN loss or deficiency fuels cancer cell growth through dysregulation of the PI3K/AKT pathway and is associated with poor outcomes in prostate cancer patients [113]. As a CSC-related biomarker, PTEN represents both a diagnostic challenge and therapeutic opportunity currently under investigation in diagnostic development pipelines [113].
For bladder cancer, the integrative analysis of CSC biomarkers has identified several promising therapeutic targets. The 8-gene signature not only provided prognostic value but also revealed varying drug sensitivities across patient risk groups when analyzed using the 'oncoPredict' algorithm based on the GDSC2 dataset [36]. This approach highlights the potential for CSC biomarker signatures to guide both prognosis and treatment selection, moving beyond traditional histopathological classification.
Implementation Challenges and Solutions
The implementation of CSC biomarker-based companion diagnostics faces several significant challenges, ranging from technical limitations to regulatory and reimbursement hurdles. Sample availability remains a persistent issue, as trial enrollment often depletes available samples, limiting material for diagnostic validation studies [112]. Potential alternative approaches, such as using post-mortem samples, present logistical and ethical considerations due to rapid tissue degradation and challenges obtaining informed consent [112].
Technology standardization across different healthcare institutions represents another implementation challenge. Hospitals use varied genetic testing equipment and methods, creating barriers to consistent biomarker testing implementation [115]. For blood-based tests, limitations persist, as evidenced by CIN signature biomarkers that could only classify approximately 31% of ovarian cancer cases using blood samples alone, with the remainder still requiring tissue biopsies [115].
To address these challenges, several solutions are emerging. Collaborative development models between diagnostic companies, pharmaceutical partners, and academic institutions help align diagnostic and therapeutic development [113]. The integration of digital pathology and AI facilitates more standardized analysis across institutions, potentially reducing inter-observer variability [113] [114]. Additionally, regulatory science advancements are creating more efficient pathways for biomarker qualification, with evolving frameworks from both the FDA and EMA addressing the unique challenges of novel biomarker classes [114].
Diagram Title: CSC Biomarkers and Clinical Outcomes
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for CSC Biomarker Research
| Reagent/Platform | Function | Application Example |
|---|---|---|
| Lectin MIX (UEA-1 + GSL-I) | Detection of CSC-specific glycan patterns [15] | Isolation of lung CSCs with higher specificity than CD133 [15] |
| Anti-CD133/AC133 Antibodies | Recognition of CSC surface marker [15] | Traditional isolation of CSCs from various cancer types [15] |
| ALDH1A1 Detection Reagents | Identification of aldehyde dehydrogenase activity [36] | Functional assessment of CSC populations [36] |
| Digital Pathology Systems | Digitization and AI-based analysis of histopathology slides [113] [114] | Identification of CSC-related patterns in standard H&E stains [114] |
| CIN Signature Analysis Tools | Quantification of chromosomal instability from genomic data [115] | Prediction of chemotherapy resistance across cancer types [115] |
| BCSCdb Database | Repository of experimentally validated CSC biomarkers [45] | Reference for CSC biomarker selection and validation [36] |
| Single-cell RNA Sequencing | Characterization of heterogeneity within CSC populations [36] | Identification of novel CSC subpopulations and biomarkers [36] |
| Sphere Formation Assay Reagents | Assessment of self-renewal capability in ultra-low attachment conditions [15] | Functional validation of CSC properties [15] |
The regulatory pathways and frameworks for approving CSC biomarker-based companion diagnostics are evolving rapidly, driven by advancements in detection technologies, computational analysis, and our understanding of cancer stem cell biology. The integration of digital pathology, AI algorithms, and multi-omics approaches is creating new opportunities for developing more precise and predictive diagnostics that can better identify patients who will benefit from targeted therapies [113] [114].
Despite these advancements, significant challenges remain, including the need for standardized validation protocols, diverse and representative datasets, and regulatory frameworks that can accommodate innovative technologies while ensuring patient safety [112] [114]. The successful development and implementation of CSC biomarker-based companion diagnostics will require continued collaboration among researchers, diagnostic companies, pharmaceutical partners, regulatory agencies, and clinical stakeholders [112] [113].
As the field progresses, CSC biomarker tests are poised to play an increasingly important role in precision oncology, potentially enabling clinicians to shift from a "one-size-fits-all" approach to a biomarker-driven, patient-specific strategy [115]. This evolution promises to improve patient outcomes while reducing treatment-related morbidity, ultimately fulfilling the promise of precision medicine in oncology.
Conclusion
The successful validation of CSC biomarkers across cancer types is paramount for shifting the paradigm of cancer treatment towards eliminating the root cause of recurrence and metastasis. This synthesis of knowledge confirms that while the field faces significant challenges—primarily CSC heterogeneity, plasticity, and a lack of universal markers—the integration of advanced technologies like single-cell multi-omics, AI-driven analysis, and patient-derived organoids is rapidly accelerating progress. Future efforts must focus on standardizing validation protocols, fostering collaborative open-access databases, and designing innovative clinical trials that combine conventional therapies with CSC-targeted agents. By continuing to unravel the complexities of CSC biology and refining our validation strategies, the oncology community can unlock powerful new biomarkers that predict therapeutic response, guide personalized treatment regimens, and ultimately, lead to lasting cures for cancer patients.
References
- 1. Drug Resistance Driven by Cancer Stem Cells and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5751177/]
- 2. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 3. Cancer stem cells and their niche in cancer progression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10693166/]
- 4. Stem Cell Niche Concept: Search for Current Expert ... [https://www.mdpi.com/1422-0067/26/17/8422]
- 5. Spatial self-organization of cancer stem cell niches revealed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560515/]
- 6. Cancer stem cells and niches: challenges in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02265-2]
- 7. Metastatic Stem Cells: Sources, Niches, and Vital Pathways [https://pmc.ncbi.nlm.nih.gov/articles/PMC3998185/]
- 8. Characteristics of the cancer stem cell niche and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9166529/]
- 9. Targeting cancer stem cells for reversing therapy resistance [https://www.nature.com/articles/s41392-020-00430-1]
- 10. Biomarkers of Cancer Stem Cells for Experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9147761/]
- 11. Cancer stem cells: Bridging microenvironmental interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264091/]
- 12. Single-cell multi-omics and machine learning for dissecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570030/]
- 13. Cancer stem cells in personalized therapy [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1619597/full]
- 14. Cancer stem cells: landscape, challenges and emerging therapeutic... [https://pubmed.ncbi.nlm.nih.gov/40759634/]
- 15. Comparison of methods for cancer stem cell detection in ... [https://www.nature.com/articles/s41416-024-02839-9]
- 16. Cancer Stem Cell Markers, CD44 and ALDH1, for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9187836/]
- 17. Unraveling the roles of CD44/CD24 and ALDH1 as cancer ... [https://www.nature.com/articles/s41598-017-14364-2]
- 18. Breast cancer stem cell markers CD44 and ALDH1A1 in ... [https://www.jcancer.org/v09p3728.htm]
- 19. Biology of stem cell paradox: a double-edged sword ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03981-x]
- 20. Cancer stem cells as a biomarker – A mini review [https://www.probiologists.com/article/cancer-stem-cells-as-a-biomarker-a-mini-review]
- 21. Cancer cell plasticity and therapeutic resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465352/]
- 22. The Evolving Role of Alternative Splicing in Cancer Stem ... [https://www.sciencedirect.com/science/article/abs/pii/S1040842825004081]
- 23. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 24. Targeting CSC-immune cell crosstalk to overcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325370/]
- 25. Biomarkers and Targeted Therapy for Cancer Stem Cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842814/]
- 26. Targeting CSC-immune cell crosstalk to overcome ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1620807/full]
- 27. Cross-talk between cancer stem cells and immune cells [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01748-4]
- 28. Bidirectional Crosstalk Between Cancer Stem Cells and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.00140/full]
- 29. BCSCdb - Database Commons [https://ngdc.cncb.ac.cn/databasecommons/database/id/8429]
- 30. Cancer stem cells and post-therapy tumour recurrence [https://ecancer.org/en/journal/article/2016-cancer-stem-cells-and-post-therapy-tumour-recurrence-a-systematic-review-of-mechanistic-pathways-and-translational-gaps]
- 31. Chemical Proteomic Approaches Targeting Cancer Stem Cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC5611518/]
- 32. Advancing Breast Cancer Heterogeneity Analysis: Insights ... [https://www.mdpi.com/2072-6694/15/16/4164]
- 33. Comparative benchmarking of single-cell clustering ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03719-y]
- 34. Future Of Omics 2025 - MGI Tech [https://global-mgitech.com/fo2025/]
- 35. Multi-omics data integration for topology-based pathway ... [https://pubs.rsc.org/en/content/articlehtml/2025/mo/d5mo00151j]
- 36. Integrative Analysis of Biomarkers for Cancer Stem Cells in ... [https://www.mdpi.com/2073-4425/16/10/1146]
- 37. The Power of High-Throughput Omics Integration [https://www.mdpi.com/2227-7382/12/3/25]
- 38. Advancements in single-cell RNA sequencing and spatial ... [https://www.frontierspartnerships.org/journals/acta-biochimica-polonica/articles/10.3389/abp.2025.13922/full]
- 39. Systematic comparison of sequencing-based spatial ... [https://www.nature.com/articles/s41592-024-02325-3]
- 40. High-definition spatial transcriptomic profiling of immune ... [https://www.nature.com/articles/s41588-025-02193-3]
- 41. Systematic benchmarking of high-throughput subcellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534522/]
- 42. Performance comparison of high throughput single-cell ... [https://www.sciencedirect.com/science/article/pii/S2405844024132161]
- 43. Single‐Cell RNA Sequencing and Spatial Transcriptomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183525/]
- 44. Identification of Biomarkers for Controlling Cancer Stem ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2019.00613/full]
- 45. BCSCdb: a database of biomarkers of cancer stem cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC9517164/]
- 46. Sphere-Formation Assay: Three-Dimensional in vitro ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2018.00347/full]
- 47. AQSA—Algorithm for Automatic Quantification of Spheres ... [https://www.mdpi.com/2313-433X/10/11/295]
- 48. A New In Vivo Tool to Evaluate Breast Cancer Stem Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7795925/]
- 49. Ex vivo 3D micro-tumour testing platform for predicting ... [https://www.nature.com/articles/s41698-025-01080-8]
- 50. Cell morphology best predicts tumorigenicity and metastasis ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-024-01796-8]
- 51. Comparison of methods for cancer stem cell detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11519646/]
- 52. Functional Precision in Pancreatic Cancer: Redefining ... [https://www.mdpi.com/1422-0067/26/18/9083]
- 53. Patient-Derived Organoid Biobanks for Translational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12387782/]
- 54. Combining molecular characteristics and therapeutic analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11863571/]
- 55. Breakthroughs and challenges of organoid models for ... [https://www.nature.com/articles/s41420-025-02505-w]
- 56. Q&A: Using RWD to bridge discovery and development in ... [https://www.tempus.com/resources/content/articles/qa-using-rwd-to-bridge-discovery-and-development-in-translational-research/?srsltid=AfmBOopTixLpk_s_rqGYOQJo9JNQzLNitRHbYYtZ0AbSlREzdWpJQwlA]
- 57. Multi-omics prognostic marker discovery and survival ... [https://www.nature.com/articles/s41598-025-20572-y]
- 58. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 59. Identification and Experimental Validation of Prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109615/]
- 60. Multi-omics analyses construct an inflammatory response ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1563593/full]
- 61. Multi-omics analysis unveils a four-gene prognostic signature ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14150-8]
- 62. Integrative analysis of multi-omics data and gut microbiota ... [https://www.nature.com/articles/s41598-025-08915-1]
- 63. Efficient discovery of robust prognostic biomarkers and ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525000667]
- 64. A Comprehensive Oncological Biomarker Framework Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466961/]
- 65. Biomarker and Prognostic Value of Super-ARMS Detection ... [https://pubmed.ncbi.nlm.nih.gov/40655938/]
- 66. Real-world deployment of a fine-tuned pathology ... [https://www.nature.com/articles/s41591-025-03780-x]
- 67. Advances in biomarkers of resistance to KRAS mutation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508421/]
- 68. Radiomics-based biomarker for PD-1 status and prognosis ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1435668/full]
- 69. Integrative profiling of lung cancer biomarkers EGFR, ALK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12414981/]
- 70. Integrative Profiling of Lung Cancer Biomarkers EGFR, ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1649445/abstract]
- 71. Development and validation of an integrative 54 biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341305/]
- 72. Cancer Stem Cell Markers [https://www.atlasantibodies.com/knowledge-hub/white-papers/cancer-stem-cell-markers/]
- 73. Cancer Stem Cell markers: Symphonic masters of ... [https://www.sciencedirect.com/science/article/pii/S0024320524006052]
- 74. Combined Detection of Tumor Stem Cell Markers CD133 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12456660/]
- 75. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 76. Impact and Reproducibility of In-House Targeted Next ... [https://www.sciencedirect.com/science/article/pii/S152515782500042X]
- 77. Global research dynamics in metabolic biomarkers and cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589725/]
- 78. Interpretable Multiomics Models for Predicting Surgical ... [https://www.nature.com/articles/s41746-025-02072-5]
- 79. Integrating AI and RNA biomarkers in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512311/]
- 80. AI-Powered Biomarker Discovery: 7 ... [https://lifebit.ai/blog/ai-powered-biomarker-discovery/]
- 81. Machine learning-driven multi-targeted drug discovery in ... [https://www.nature.com/articles/s41698-025-01058-6]
- 82. Metabolic Plasticity and Cancer Stem Cell Metabolism [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504402/]
- 83. The Metabolic Landscape of Cancer Stem Cells [https://www.mdpi.com/2073-4409/14/10/717]
- 84. Clinical Biomarkers 2025 [https://biomarkers.cancersummit.org/events-list/biomarkers-validation-and-verification]
- 85. Advancing Cancer Biology: Highlights from the 2025 FASEB ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599846/]
- 86. Mitochondrial RNA modifications shape metabolic plasticity ... [https://www.nature.com/articles/s41586-022-04898-5]
- 87. Cancer stem cell mechanisms and targeted therapeutic ... [https://www.sciencedirect.com/science/article/pii/S0304383525005853]
- 88. Construction of a Prognostic Model based on CSC-related ... [https://www.jcancer.org/v16p2375.htm]
- 89. Pharmacological modulation of stem cells signaling pathway ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04438-8]
- 90. Overcoming colorectal cancer and cancer stem cell resistance ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra07380d]
- 91. Cancer stem cell biomarkers in locally advanced head and ... [https://www.sciencedirect.com/science/article/pii/S1808869425001338]
- 92. Comparative Evaluation of Cancer Stem Cell Markers in ... [https://pubmed.ncbi.nlm.nih.gov/21922151/]
- 93. Pan-cancer spatial characterization of key immune ... [https://www.sciencedirect.com/science/article/pii/S2666379125004914]
- 94. Cancer Biomarkers Market Forecast Report 2025-2035 [https://finance.yahoo.com/news/cancer-biomarkers-market-forecast-report-082300982.html]
- 95. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 96. Advances in prognostic and predictive biomarkers for ... [https://pubmed.ncbi.nlm.nih.gov/40716694/]
- 97. The evolving landscape of genetic biomarkers for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1522262/full]
- 98. The LEAP Study: A Multicenter Biospecimen and Imaging ... [https://pubmed.ncbi.nlm.nih.gov/41191414/]
- 99. Insights from Lung, Breast, Colorectal, Liver, and Gastric ... [https://pubmed.ncbi.nlm.nih.gov/41154605/]
- 100. Beyond Detection: Conventional and Emerging Biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427498/]
- 101. Stromal cells modulate innate immune cell phenotype and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542748/]
- 102. Liquid Biopsy Market Trends & Growth Outlook 2025-2035 [https://www.futuremarketinsights.com/reports/liquid-biopsy-market]
- 103. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 104. Novel markers for liquid biopsies in cancer management [https://pmc.ncbi.nlm.nih.gov/articles/PMC10314793/]
- 105. Liquid biopsies in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923355/]
- 106. Liquid Biopsies: A Revolution in Early Cancer Detection ... [https://www.aicr.org/resources/blog/liquid-biopsies-a-revolution-in-early-cancer-detection-and-monitoring/]
- 107. Circulating tumor cells as liquid biopsy markers in cancer ... [https://www.sciencedirect.com/science/article/pii/S0098299724000177]
- 108. Cancer Stem Cells (CSCs), Circulating Tumor Cells (CTCs) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9139858/]
- 109. Circulating tumor cells: biology and clinical significance [https://www.nature.com/articles/s41392-021-00817-8]
- 110. Cost-Effectiveness Analysis of CAR T-Cell Therapies vs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9869188/]
- 111. The evolving landscape of antibody-drug conjugates ... [https://www.nature.com/articles/s41698-025-01131-0]
- 112. Meeting Recap | 2025 Diagnostics and Regulatory ... [https://friendsofcancerresearch.org/blog/meeting-recap-advancing-the-future-of-diagnostics-and-regulatory-innovations-meeting-recap-sharing-next-steps-and-opportunities-with-advocates/]
- 113. 2025: The future of cancer diagnostics in the pathology lab [https://diagnostics.roche.com/us/en/article-listing/2025-the-future-of-cancer-diagnostics-in-the-pathology-lab.html]
- 114. AI and the future of biomarker analysis in early R&D [https://www.drugtargetreview.com/article/190428/ai-and-the-future-of-biomarker-analysis-in-early-rd/]
- 115. New Biomarkers Predict Chemotherapy Resistance Across ... [https://binaytara.org/cancernews/article/new-biomarkers-predict-chemotherapy-resistance-across-multiple-cancer-types]