Beyond Accuracy: A Comprehensive Framework for Validating Machine Learning Models in Cancer Detection
This article provides a comprehensive guide for researchers and drug development professionals on the critical process of validating machine learning (ML) models for cancer detection.
Beyond Accuracy: A Comprehensive Framework for Validating Machine Learning Models in Cancer Detection
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the critical process of validating machine learning (ML) models for cancer detection. It addresses the journey from foundational principles and data challenges to advanced methodological applications, optimization strategies for robust performance, and rigorous comparative validation. The content synthesizes current research and clinical insights to outline a pathway for transitioning ML models from experimental settings to reliable, real-world clinical tools, emphasizing the importance of generalizability, interpretability, and clinical integration for advancing precision oncology.
The Imperative for Rigorous Validation: Foundations and Challenges in Oncology AI
In oncology, the validation of machine learning (ML) models transcends mere technical performance, representing a rigorous, multi-stage process to ensure models are reliable, equitable, and useful in real-world clinical settings. Clinical prediction models, which provide individualised risk estimates to aid diagnosis and prognosis, are widely developed in oncology [1]. The journey from model development to clinical implementation is fraught with methodological challenges, and a robust validation framework is critical for bridging this gap. This guide defines this framework, comparing key validation metrics and methodologies to equip researchers and drug development professionals with the tools for rigorous model assessment.
The fundamental question precedes development: is a new model necessary? The field often suffers from duplication, with over 900 models for breast cancer decision-making and over 100 for predicting overall survival in gastric cancer [1]. Therefore, the first step in any validation-centric workflow is a systematic review of existing models to critically appraise them and, if appropriate, evaluate and update them before embarking on new development [1].
Core Technical Metrics for Model Validation
Technical validation metrics provide the foundational evidence of a model's predictive accuracy. These metrics are typically evaluated during internal validation and are prerequisites for assessing clinical utility. The table below summarizes the core metrics used in clinical prediction models.
Table 1: Key Technical Validation Metrics for Clinical ML Models
| Metric Category | Specific Metric | Definition and Interpretation | Common Use Cases |
|---|---|---|---|
| Discrimination | C-statistic (AUC) | Measures the model's ability to distinguish between patients with and without the outcome. Values range from 0.5 (no discrimination) to 1.0 (perfect discrimination). | Overall assessment of a diagnostic or prognostic model's performance. |
| Calibration | Calibration Slope | Assesses the agreement between predicted probabilities and observed outcomes. A slope of 1 indicates perfect calibration. | Critical for risk stratification; often visualized with calibration plots. |
| Overall Performance | Brier Score | The mean squared difference between predicted probabilities and actual outcomes. Lower scores indicate better accuracy. | Provides a single value to evaluate probabilistic predictions. |
Beyond these standard metrics, comprehensive internal validation using bootstrapping or cross-validation is essential to avoid overfitting and obtain reliable performance estimates [1]. Furthermore, validation must address data-specific complexities such as censored observations, competing risks, or clustering effects, which, if ignored, can produce misleading inferences and limit clinical utility [1].
Beyond Technical Metrics: Assessing Clinical Utility
A model with excellent technical metrics may still fail in clinical practice if it does not improve decision-making. Clinical utility assessment determines whether using the model leads to better patient outcomes or more efficient care compared to standard practice.
The primary method for evaluating clinical utility is decision curve analysis, which calculates the "net benefit" of the model across a range of probability thresholds [1]. This analysis weighs the true positive rate against the false positive rate, quantifying the model's value for making clinical decisions. Engaging end-users—including clinicians, patients, and the public—early in the development process is critical to ensure the model addresses a genuine clinical need, selects meaningful predictors, and aligns with real-world workflows [1]. Their involvement ensures the model's outputs are actionable and relevant to those it is intended to serve.
Experimental Protocols for Model Validation
A standardized experimental protocol is mandatory for trustworthy validation. This begins with protocol development and public registration to reduce transparency risks and methodological inconsistencies [1].
Internal and External Validation Workflow
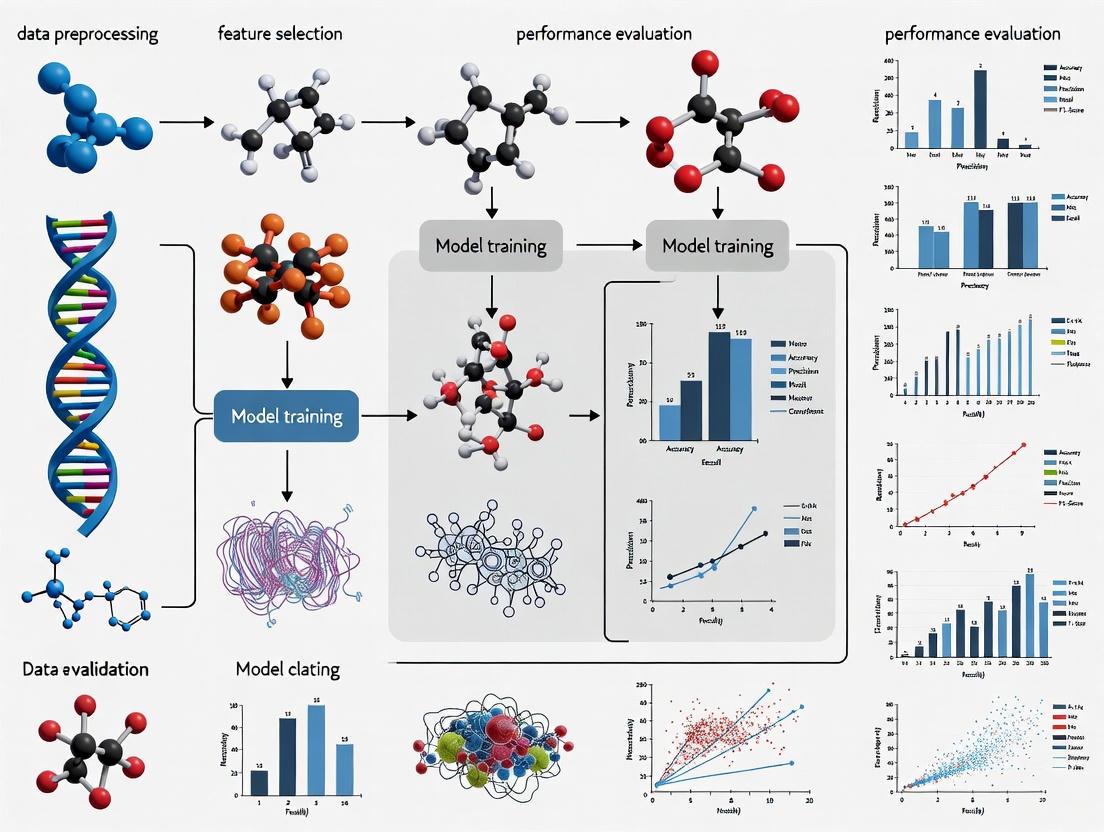
The following diagram illustrates the critical stages of model validation, from initial internal checks to assessing real-world generalizability.
Comparison of Methods Experiment
For validating a new model or test against an existing benchmark, a comparison of methods experiment is standard practice. The protocol involves analyzing a minimum of 40 different patient specimens by both the new (test) method and a established comparative method [2]. These specimens should cover the entire working range of the method and represent the spectrum of diseases expected in routine use. The experiment should be conducted over a minimum of 5 days to capture day-to-day variability, and specimens should be analyzed within two hours of each other to ensure stability [2].
Data analysis should include:
- Graphical Analysis: Creating difference plots (test result minus comparative result) or comparison plots to visually inspect for systematic errors and outliers [2].
- Statistical Calculations: For data covering a wide analytical range, use linear regression to estimate the slope, y-intercept, and standard error about the line (S~y/x~). The systematic error (SE) at a critical medical decision concentration (X~c~) is calculated as SE = Y~c~ - X~c~, where Y~c~ = a + bX~c~ [2].
Quantitative Validation Metrics
Moving beyond graphical comparisons, quantitative validation metrics that incorporate uncertainty are essential. A confidence interval-based approach provides a rigorous statistical method [3]. The core idea is to compute the difference between the computational result (e.g., the model's prediction, S) and the experimentally observed mean (μ~exp~) at a given validation point. The validation metric (ν) is then defined with an associated confidence interval.
The equation for the validation metric is: ν = |S - μ~exp~| ± U~ν~
Where U~ν~ is the uncertainty in the metric, which combines the experimental uncertainty (often a confidence interval based on the t-distribution) and the numerical error in the simulation. This provides a quantitative, probabilistic measure of the agreement between model and reality [3].
A Case Study in AI Agent Validation
A 2025 study in Nature Cancer on an autonomous AI agent for oncology decision-making provides a contemporary template for comprehensive validation [4]. The study developed an AI agent that integrated GPT-4 with specialized precision oncology tools, including vision transformers for detecting genetic alterations from histopathology slides, MedSAM for radiological image segmentation, and search tools like OncoKB and PubMed [4].
Experimental Protocol and Benchmarking
The researchers devised a benchmark of 20 realistic, multimodal patient cases focused on gastrointestinal oncology [4]. For each case, the AI agent autonomously selected and applied relevant tools to derive insights and then used a retrieval-augmented generation (RAG) step to base its responses on medical evidence. Performance was evaluated through a blinded manual review by four human experts, focusing on three areas [4]:
- Tool Use: Accuracy in recognizing and successfully using required tools.
- Output Quality: Completeness and correctness of clinical conclusions and treatment plans.
- Citation Precision: Accuracy in citing relevant oncology guidelines.
Table 2: Quantitative Performance Results of the AI Agent [4]
| Evaluation Dimension | Performance Metric | Result | Comparison: GPT-4 Alone |
|---|---|---|---|
| Tool Use | Overall Success Rate | 87.5% (56/64 required tools) | Not Applicable |
| Clinical Conclusions | Correct Treatment Plans | 91.0% of cases | 30.3% |
| Evidence Integration | Accurate Guideline Citations | 75.5% of the time | Not Reported |
| Overall Completeness | Coverage of Expected Statements | 87.2% (95/109 statements) | 30.3% |
This multi-faceted protocol demonstrates a robust framework for validating complex clinical AI systems, moving beyond simple accuracy to assess practical functionality and integration of evidence.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key resources and tools used in advanced clinical ML validation, as exemplified by the featured case study and general practice.
Table 3: Key Research Reagent Solutions for Clinical ML Validation
| Tool or Resource Name | Type | Primary Function in Validation |
|---|---|---|
| OncoKB [4] | Precision Oncology Database | Provides evidence-based information on the clinical implications of genetic variants, used to validate model conclusions against known biomarkers. |
| Vision Transformers [4] | Specialized Deep Learning Model | Detects genetic alterations (e.g., MSI, KRAS, BRAF mutations) directly from histopathology slides, serving as a validated tool for feature extraction. |
| MedSAM [4] | Medical Image Segmentation Model | Segments regions of interest in radiological images (MRI, CT), enabling quantitative measurement of tumor size and growth for response assessment. |
| PubMed / Google Scholar [4] | Scientific Literature Database | Provides access to peer-reviewed literature and clinical guidelines for evidence-based reasoning and citation, grounding model outputs in established science. |
| Retrieval-Augmented Generation (RAG) [4] | AI Technique | Enhances LLM responses by grounding them in a curated repository of medical documents, improving accuracy and providing citable sources. |
| TRIPOD+AI Guideline [1] | Reporting Standard | Ensures transparent and complete reporting of all aspects of model development and validation, facilitating critical appraisal and reproducibility. |
True validation in the clinical context is a continuous journey, not a single event. It begins with robust technical assessment using standardized metrics, extends through rigorous external validation to prove generalizability, and culminates in the demonstration of tangible clinical utility. As the case study shows, even advanced AI systems require integration with specialized tools and evidence bases to achieve clinical-grade accuracy. Finally, overcoming implementation barriers—such as limited stakeholder engagement, workflow integration challenges, and the absence of post-deployment monitoring plans—is essential [1]. Successful clinical translation demands that researchers adopt this comprehensive view of validation, ensuring that models are not only statistically sound but also trustworthy, equitable, and capable of improving patient care.
The integration of artificial intelligence (AI) and machine learning (ML) into oncology represents a paradigm shift with transformative potential for cancer diagnosis, treatment selection, and drug development. These technologies demonstrate remarkable capabilities, from classifying cancer types with over 97% accuracy to accelerating drug discovery timelines [5] [6]. However, the deployment of inadequately validated models carries significant risks that extend beyond algorithmic performance metrics to direct patient harm and resource misallocation. Recent evidence indicates substantial deficiencies in methodological and reporting quality within ML studies for cancer applications, with approximately 98% failing to report sample size calculations and 69% neglecting data quality issues [7]. This analysis examines the critical consequences of poor model validation through comparative performance assessment, detailed experimental methodologies, and standardized reporting frameworks essential for researchers and drug development professionals navigating this evolving landscape.
Comparative Performance of Validated Versus Non-Validated Models
Diagnostic and Detection Performance
Table 1: Performance Comparison of AI Models in Cancer Detection and Diagnosis
| Cancer Type | Modality | Task | Model Type | Performance Metrics | Validation Status |
|---|---|---|---|---|---|
| Colorectal Cancer | Colonoscopy | Malignancy detection | CRCNet (Deep Learning) | Sensitivity: 91.3% vs Human: 83.8% (p<0.001); AUC: 0.882 [8] | External validation across three independent cohorts |
| Osteosarcoma | Histopathological & Clinical Data | Detection and classification | Extra Trees Algorithm | 97.8% AUC; 10ms classification time [5] | Stratified 10-fold cross-validation with hyperparameter optimization |
| Breast Cancer | 2D Mammography | Screening detection | Ensemble of 3 DL models | AUC: 0.889 (UK), 0.810 (US); +9.4% improvement vs radiologists (p<0.001) [8] | External validation on different population datasets |
| Various Cancers | Electronic Health Records | Diagnosis categorization | GPT-4o | Free-text accuracy: 81.9%; F1-score: 71.8 [9] | Expert oncology review with benchmark against specialized BioBERT |
| Cancer Survival | Real-world Data | Survival prediction | Random Survival Forest | C-index performance similar to Cox models (SMD: 0.01, 95% CI: -0.01 to 0.03) [10] | Meta-analysis of 21 studies showing limited validation advantage |
The performance differential between rigorously validated and poorly validated models manifests most significantly in real-world clinical settings. Externally validated models such as CRCNet demonstrate robust performance across diverse patient populations, maintaining sensitivity above 90% when tested across three independent hospital systems [8]. In contrast, models lacking rigorous validation frequently exhibit performance degradation when applied to new populations, as evidenced by the performance drop in breast cancer detection models transitioning from UK to US datasets (AUC decrease from 0.889 to 0.810) [8]. This pattern underscores the critical importance of external validation across diverse demographic and clinical populations.
For survival prediction, a comprehensive meta-analysis of 21 studies revealed that machine learning models showed no superior performance over traditional Cox proportional hazards regression (standardized mean difference in C-index: 0.01, 95% CI: -0.01 to 0.03) [10]. This finding challenges claims of ML superiority in time-to-event prediction and highlights the validation gap between theoretical model performance and clinical application, particularly for high-stakes prognostic assessments that guide treatment intensification or palliative care transitions.
Model Performance in Drug Discovery and Development
Table 2: AI Model Performance in Oncology Drug Discovery Applications
| Application Area | Model/Platform | Key Performance Metrics | Validation Level | Reported Outcomes |
|---|---|---|---|---|
| Target Identification | BenevolentAI | Novel target prediction in glioblastoma [6] | Limited clinical validation | Identification of promising leads for further validation |
| Molecular Design | Insilico Medicine | 18-month preclinical candidate development (vs. 3-6 years traditional) [6] | Early-stage clinical trials | QPCTL inhibitors advancing to oncology pipelines |
| Drug Sensitivity Prediction | DREAM Challenge Multimodal AI | Superior prediction vs. unimodal approaches [11] | Benchmarking on standardized datasets | Consistent outperformance in therapeutic outcome prediction |
| Treatment Response | Pathomic Fusion | Outperformed WHO 2021 classification for risk stratification [11] | Glioma and renal cell carcinoma datasets | Improved risk stratification for treatment planning |
| Clinical Trial Optimization | TRIDENT Model | HR reduction: 0.88-0.56 in non-squamous NSCLC [11] | Phase 3 POSEIDON study data | Identified >50% population obtaining optimal treatment benefit |
AI-driven drug discovery platforms demonstrate accelerated timelines, with companies like Exscientia and Insilico Medicine reporting compound development in 12-18 months compared to traditional 4-5 year timelines [6]. However, the ultimate validation metric—regulatory approval and clinical adoption—remains limited. Early reviews suggest an 80-90% success rate for AI-designed molecules in Phase 1 trials, substantially higher than the industry standard, though the sample size remains limited [11]. This discrepancy between accelerated development and regulatory approval highlights the validation gap between computational prediction and clinical efficacy.
Multimodal AI approaches integrating histology and genomics, such as Pathomic Fusion, demonstrate validated performance superior to World Health Organization 2021 classifications for risk stratification in glioma and clear-cell renal-cell carcinoma [11]. Similarly, the TRIDENT machine learning model, which integrates radiomics, digital pathology, and genomics from the Phase 3 POSEIDON study, identified patient subgroups with significant hazard ratio reductions (0.88-0.56 in non-squamous populations) for metastatic non-small cell lung cancer [11]. These exemplars demonstrate the validation rigor required for clinical implementation in precision oncology.
Experimental Protocols and Methodologies
Protocol for Diagnostic Model Validation
A comprehensive validation framework for cancer diagnostic models requires multiple assessment phases. The following protocol synthesizes methodologies from rigorously validated studies analyzed in this review:
Phase 1: Data Curation and Preprocessing
- Apply data denoising techniques including principal component analysis, mutual information gain, and analysis of variance to address data quality issues [5]
- Implement class balancing through random oversampling and address multicollinearity via principal component analysis [5]
- Establish standardized data formats (HL7 for clinical results, FASTQ for omics data) with detailed metadata annotations covering data provenance, collection methods, and quality metrics [12]
Phase 2: Model Training with Robust Internal Validation
- Utilize repeated stratified 10-fold cross-validation to assess model stability [5]
- Optimize hyperparameters using grid search methodologies with appropriate performance metrics (AUC, sensitivity, specificity) [5]
- Implement ensemble methods such as Cascade Deep Forest models to reduce overfitting and maintain generalizability in data-sparse scenarios [13]
Phase 3: External Validation and Performance Assessment
- Validate model performance on completely independent datasets from different institutions or demographic populations [8]
- Compare model performance against clinical expert benchmarks using predefined statistical superiority or non-inferiority margins [8]
- Assess real-world clinical utility through impact studies measuring changes in diagnostic accuracy, time to diagnosis, or clinical decision-making [7]
Phase 4: Reporting and Transparency Documentation
- Adhere to CONSORT, TRIPOD-AI, and CREMLS reporting guidelines with specific attention to sample size justification, data quality issues, and handling of outliers [7]
- Document model architecture, training parameters, and potential limitations for regulatory review and clinical implementation [13]
Protocol for Predictive Model Validation in Drug Discovery
The validation of AI models for oncology drug discovery requires specialized methodologies to address unique challenges in target identification, compound screening, and clinical trial optimization:
Target Identification and Compound Screening
- Integrate multi-omics data (genomics, transcriptomics, proteomics) using deep learning architectures such as DeepDTA for drug-target interaction prediction [13]
- Employ graph-based neural networks including GraphDTA and Mol2Vec to encode chemical structures as graph embeddings for bioactivity prediction [13]
- Utilize generative adversarial networks (GANs) and variational autoencoders trained on large chemical libraries (ZINC, ChEMBL) for de novo molecular design with optimized ADMET properties [13]
Clinical Trial Optimization and Predictive Biomarker Development
- Implement multimodal AI frameworks such as AstraZeneca's ABACO platform that integrate real-world evidence with explainable AI to identify predictive biomarkers [11]
- Apply natural language processing tools (PubTator, LitCovid) to mine biomedical literature and clinical trial data for hidden associations between drugs, genes, and diseases [13]
- Validate predictive signatures through retrospective analysis of Phase 3 trial data (e.g., TRIDENT analysis of POSEIDON study) before prospective implementation [11]
Transversal Validation Considerations
- Address model interpretability through explainable AI techniques, particularly for "black box" deep learning models requiring regulatory approval [6] [13]
- Assess potential algorithmic bias by evaluating model performance across demographic subgroups and cancer subtypes [7]
- Establish continuous monitoring systems for model performance drift in real-world clinical settings [11]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Oncology AI Validation
| Tool/Category | Specific Examples | Primary Function | Validation Role |
|---|---|---|---|
| Specialized AI Models | BioBERT, DeepDTA, Cascade Deep Forest | Domain-specific model architectures | Enhanced performance on biomedical data through specialized training |
| Data Processing Frameworks | Principal Component Analysis, Mutual Information Gain, Analysis of Variance | Data denoising and feature selection | Address data quality issues and reduce dimensionality for improved generalizability |
| Model Training Platforms | MONAI, PyTorch, TensorFlow | Deep learning framework with medical imaging focus | Standardized implementation and reproducibility of model architectures |
| Validation Datasets | The Cancer Genome Atlas, SEER Database, OMI-DB | Large-scale standardized oncology datasets | External validation benchmark across diverse patient populations |
| Explainability Tools | SHAP, LIME, Attention Mechanisms | Model interpretability and feature importance | Regulatory compliance and clinical trust through transparent decision-making |
| Federated Learning Infrastructure | NVIDIA FLARE, OpenFL | Privacy-preserving collaborative learning | Multi-institutional validation without data sharing constraints |
The selection of appropriate research reagents and computational tools fundamentally influences validation outcomes. Specialized domain-specific models such as BioBERT, which is pretrained on biomedical corpora, demonstrate superior performance in categorizing cancer diagnoses from electronic health records compared to general-purpose large language models, achieving weighted macro F1-scores of 84.2 for structured ICD code classification [9]. This performance advantage highlights the importance of domain-adapted architectures for clinically relevant tasks.
Federated learning infrastructure represents a critical advancement for validation across institutions while addressing data privacy constraints. This approach enables model training and validation across multiple healthcare systems without sharing raw patient data, enhancing the diversity and representativeness of validation cohorts while maintaining compliance with regulations such as HIPAA and GDPR [12]. Similarly, standardized medical imaging frameworks like MONAI provide pre-trained models and specialized processing layers for consistent evaluation across different imaging modalities and devices [11].
Consequences of Inadequate Validation
Direct Patient Harms
Poorly validated models precipitate cascading failures throughout the clinical oncology pathway. In diagnostic applications, validation deficiencies manifest as differential performance across demographic groups, potentially exacerbating healthcare disparities. For instance, breast cancer screening models demonstrating strong performance in UK populations (AUC: 0.889) showed significantly reduced accuracy when applied to US datasets (AUC: 0.810), highlighting the potential for systematic diagnostic errors in different healthcare contexts [8]. Such performance variations risk both false negatives delaying critical interventions and false positives leading to unnecessary invasive procedures, psychological distress, and radiation exposure from follow-up imaging.
In treatment selection, inadequately validated predictive models for therapy response can direct patients toward ineffective treatments while delaying more appropriate alternatives. For example, models predicting immunotherapy response without proper validation across different cancer subtypes may fail to identify nuanced biomarkers of resistance, resulting in treatment failure and unnecessary toxicity [6] [11]. The integration of AI-derived biomarkers into clinical decision-making necessitates validation rigor comparable to traditional laboratory-developed tests, particularly for high-stakes treatment decisions in advanced malignancies.
Resource and Economic Impacts
The resource implications of poorly validated oncology AI models extend across the healthcare ecosystem. At the institutional level, implementation of under-validated systems incurs substantial infrastructure costs without demonstrating clear clinical benefit, potentially diverting resources from proven interventions. In drug development, AI-platforms claiming accelerated discovery timelines require validation against the ultimate endpoint of regulatory approval and clinical adoption. Early analyses suggest promising trends, with AI-designed molecules potentially progressing to clinical trials at twice the rate of traditionally developed compounds [11]. However, the validation gap between in silico prediction and clinical efficacy remains substantial, with an estimated 90% of oncology drugs still failing during clinical development [6].
The opportunity cost of pursuing AI-derived therapeutic targets without robust validation includes both direct financial expenditure and the diversion of scientific resources from potentially more productive avenues. Conversely, properly validated AI models in clinical trial optimization, such as those enabling synthetic control arms or predictive enrichment strategies, demonstrate potential to reduce trial costs and accelerate approvals [11]. This dichotomy underscores the economic imperative for rigorous validation frameworks that distinguish clinically viable AI applications from those with only theoretical promise.
Regulatory and Reputational Consequences
The regulatory landscape for AI in oncology remains evolving, with frameworks such as the FDA's Software as a Medical Device (SaMD) classification requiring demonstration of clinical validity and utility [13]. Poorly validated models face increasing regulatory scrutiny, particularly as real-world performance discrepancies emerge post-implementation. The absence of standardized validation methodologies contributes to regulatory uncertainty, potentially delaying beneficial innovations while allowing problematic applications to reach clinical use.
Transparent reporting of model limitations, training data characteristics, and performance boundaries represents a critical component of responsible validation. Current analyses indicate significant deficiencies in ML study reporting, with fewer than 40% adequately describing strategies for handling outliers or data quality issues [7]. These reporting failures impede regulatory evaluation, scientific reproducibility, and clinical trust, ultimately undermining the broader integration of AI methodologies into oncology research and practice.
The integration of AI and ML into oncology presents unprecedented opportunities to address complex challenges in cancer diagnosis, treatment optimization, and therapeutic development. However, the substantial consequences of inadequate validation—including direct patient harm, resource misallocation, and erosion of clinical trust—demand rigorous methodological standards exceeding traditional software validation frameworks. The comparative analyses presented demonstrate that properly validated models maintain performance across diverse populations and clinical settings, while those lacking robust validation frequently fail in translation from development to implementation.
Future advances in oncology AI will require sustained focus on validation methodologies, including standardized protocols for external testing, prospective clinical impact studies, and transparent reporting of limitations and failures. The scientist's toolkit must evolve to include specialized domain-adapted models, privacy-preserving validation infrastructures, and explainability frameworks that bridge the gap between algorithmic prediction and clinical decision-making. Only through this comprehensive validation paradigm can the oncology community fully harness AI's potential while mitigating the substantial risks of premature or inappropriate clinical implementation.
The advancement of machine learning (ML) in oncology presents a critical paradox: models require vast, diverse datasets to achieve high performance and generalizability, yet medical data is often scarce, fragmented across institutions, and governed by stringent privacy regulations. This "data trilemma" creates significant barriers to developing robust models for cancer detection. The scarcity challenge is particularly acute in rare cancers and specific disease subtypes, where limited patient numbers restrict the statistical power of studies [14]. Furthermore, data heterogeneity—variations in collection protocols, equipment, and patient demographics across institutions—hinders the development of models that perform consistently across diverse populations [15] [16]. Compounding these issues, privacy regulations like HIPAA and GDPR rightly restrict data sharing, creating additional friction for collaborative research that could overcome scarcity and heterogeneity [14] [17]. This guide objectively compares emerging technological solutions designed to navigate these challenges, evaluating their experimental performance and methodologies within the context of validating ML models for cancer detection.
Comparative Analysis of Technological Solutions
The following table summarizes three primary technological approaches being developed to address the core challenges in medical data for oncology research.
Table 1: Comparison of Technological Solutions for Medical Data Challenges
| Solution | Primary Addressed Challenge | Core Mechanism | Reported Performance | Key Limitations |
|---|---|---|---|---|
| Federated Learning (FL) [15] [16] | Data Privacy, Heterogeneity | Decentralized model training; data remains at source | FednnU-Net outperformed local training in multi-institutional segmentation tasks [16] | Complex coordination; sensitive to data heterogeneity |
| Synthetic Data Generation [18] [14] | Data Scarcity, Privacy | AI generates artificial datasets mimicking real data | KNN model achieved 97+% accuracy on synthetic breast cancer data [18] | Risk of capturing or amplifying real-data biases |
| Explainable AI (XAI) & Ensemble Models [18] [19] | Model Validation, Trust | Provides model interpretability; combines multiple models | Random Forest ensemble achieved 84% F1-score in breast cancer prediction [19] | Adds computational overhead; does not solve data access |
Experimental Protocols and Performance Data
Federated Learning in Action: The FednnU-Net Framework
Federated learning has emerged as a leading privacy-preserving approach for multi-institutional collaboration. The FednnU-Net framework provides a specific implementation for medical image segmentation, a critical task in oncology. Its experimental protocol involves a decentralized setup where multiple institutions (clients) collaborate to train a model without sharing their raw data.
- Core Methodology: The framework introduces two key methods to handle dataset heterogeneity across institutions. Federated Fingerprint Extraction (FFE) allows the system to analyze dataset characteristics (like image spacing and voxel size) from all clients to determine a unified training strategy. Asymmetric Federated Averaging (AsymFedAvg) enables the aggregation of model updates from clients even when their model architectures differ slightly, a common occurrence in real-world federated settings [16].
- Experimental Workflow: The process is cyclic: (1) A central server sends a global model to all client institutions. (2) Each client trains the model locally on its own data. (3) Clients send only the model updates (weights) back to the server. (4) The server aggregates these updates using AsymFedAvg to create an improved global model. This cycle repeats, refining the model without data ever leaving the original hospital [16].
- Performance Data: In experiments across six datasets from 18 institutions for breast, cardiac, and fetal segmentation, FednnU-Net consistently outperformed models trained locally at single institutions, demonstrating successful knowledge integration while preserving privacy [16].
The following diagram illustrates the operational workflow and the two novel protocols of the FednnU-Net framework.
Synthetic Data Generation for Augmenting Rare Datasets
Synthetic data generation creates artificial datasets that mimic the statistical properties of real patient data, directly addressing data scarcity and privacy.
- Core Methodology: Several techniques are employed, ranging from statistical models like Gaussian Copula to advanced deep learning models like Generative Adversarial Networks (GANs) and Variational Autoencoders (VAEs). For tabular medical data (e.g., patient records), architectures like Conditional Tabular GANs (CTGANs) and Tabular VAEs (TVAE) are particularly relevant [14]. These models learn the underlying distribution, correlations, and patterns from the original dataset and generate new, synthetic samples.
- Experimental Workflow: A typical protocol involves: (1) Using an original, often small, clinical dataset. (2) Training a generative model (e.g., TVAE) on this data. (3) Using the trained model to produce a larger synthetic dataset. (4) Training a downstream ML model (e.g., a classifier) on the synthetic data and evaluating its performance on a held-out set of real data to validate utility [18] [14].
- Performance Data: A 2025 study on breast cancer prediction compared models trained on original versus synthetic data. The K-Nearest Neighbors (KNN) model achieved high accuracy on the original dataset, while an AutoML approach (H2OXGBoost) trained on synthetic data generated by Gaussian Copula and TVAE also showed competitively high accuracy, demonstrating synthetic data's potential [18].
Table 2: Breast Cancer Prediction Model Performance on Original vs. Synthetic Data [18]
| Machine Learning Model | Dataset Type | Key Performance Metric | Reported Result |
|---|---|---|---|
| K-Nearest Neighbors (KNN) | Original Data | Accuracy | High (Precise figure not stated, "outperformed others") |
| H2O AutoML (XGBoost) | Synthetic Data (Gaussian Copula, TVAE) | Accuracy | High |
| Stacked Ensemble Model | Original Data | F1-Score | 83% |
| Random Forest | Original Data | F1-Score | 84% |
Explainable AI and Ensemble Models for Robust Validation
Beyond data access, ensuring model reliability and trust is crucial for clinical validation. Explainable AI (XAI) and ensemble models address this.
- Core Methodology: Ensemble models, such as stacking multiple algorithms (e.g., SVM, Random Forest, XGBoost), combine the strengths of individual models to improve overall prediction accuracy and stability [18] [19]. Explainable AI (XAI) techniques, including SHAP and LIME, are then used to interpret the model's predictions, identifying which features (e.g., tumor size, involved nodes) were most influential [19].
- Experimental Workflow: Researchers first preprocess data and handle missing values. They then train multiple base classifiers. For an ensemble, a meta-learner is trained on the outputs of these base models. Finally, XAI methods are applied to the final model to interpret its decision-making process, validating that it relies on clinically relevant features [19].
- Performance Data: A 2025 study on breast cancer detection using the UCTH Breast Cancer Dataset found that a Random Forest model achieved an F1-score of 84%, while a custom Stacked Ensemble model achieved 83%. The study used SHAP analysis to validate that features like "Involved nodes," "Tumor size," and "Metastasis" were the top contributors to the model's predictions, aligning with clinical knowledge [19].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table catalogs key computational tools and frameworks cited in the featured experiments, essential for replicating and advancing this research.
Table 3: Key Research Reagents and Computational Solutions
| Tool / Solution | Type | Primary Function | Application Context |
|---|---|---|---|
| FednnU-Net [16] | Software Framework | Privacy-preserving, decentralized medical image segmentation | Multi-institutional collaboration without sharing raw data |
| nnU-Net [16] | Software Framework | Automated configuration of segmentation pipelines | Gold-standard baseline for medical image segmentation tasks |
| Generative Adversarial Networks (GANs) [14] | AI Model Architecture | Generates synthetic data (images, tabular, genomic) | Data augmentation for rare diseases; creating privacy-safe datasets |
| Variational Autoencoders (VAEs) [14] | AI Model Architecture | Generates synthetic data with probabilistic modeling | Often used with smaller datasets; can be combined with GANs (VAE-GANs) |
| SHAP / LIME [19] | Explainable AI Library | Interprets model predictions to build trust and identify key features | Validating that ML models use clinically relevant features for cancer detection |
| H2O AutoML [18] | Automated ML Platform | Automates the process of training and tuning multiple ML models | Benchmarking and efficiently finding top-performing models for a given dataset |
| Synthetic Data Generators (Gaussian Copula, TVAE) [18] [14] | Data Generation Tool | Creates artificial tabular datasets that mimic real data | Overcoming data scarcity for training and testing ML models |
The validation of machine learning models in cancer detection research is inherently constrained by the available data landscape. No single solution perfectly resolves the tensions between scarcity, heterogeneity, and privacy. Federated learning offers a robust path for privacy-preserving collaboration but requires sophisticated infrastructure. Synthetic data generation effectively mitigates scarcity and privacy concerns but demands rigorous validation to ensure fidelity and fairness. Finally, Explainable AI and ensemble models are indispensable for building reliable, interpretable, and high-performing systems that clinicians can trust. The future of robust oncology AI likely lies in the strategic combination of these approaches, leveraging their complementary strengths to navigate the complex medical data landscape and deliver equitable, impactful tools for cancer care.
The integration of artificial intelligence (AI) into clinical oncology offers transformative potential for improving cancer diagnostics, treatment planning, and patient outcomes [20]. However, the proliferation of complex machine learning (ML) and deep learning (DL) models has brought to the forefront the critical challenge of the "black box" problem—where model decisions are made in an opaque manner that is not easily understood by human experts [21]. This opacity represents a significant barrier to clinical adoption, as healthcare professionals require trust and verifiability when making high-stakes decisions that affect patient lives [22]. The lack of transparency and accountability in predictive models can have severe consequences, including incorrect treatment recommendations and the perpetuation of biases present in training data [22] [23].
Within oncology, where models are increasingly used for early cancer detection, risk stratification, and treatment personalization, the demand for interpretability is not merely academic but ethical and practical [20]. Interpretability serves as a bridge between predictive performance and clinical utility, enabling researchers and clinicians to validate model reasoning, identify potential failures, and ultimately build the trust necessary for integration into healthcare workflows [23]. This review examines the critical role of model interpretability as a foundational prerequisite for clinical trust and adoption, comparing approaches for explaining black-box models with inherently interpretable alternatives within the context of cancer detection research.
Explaining Black Boxes vs. Inherently Interpretable Models: A Fundamental Divide
A fundamental dichotomy exists in approaches to model transparency: creating post-hoc explanations for black-box models versus designing models that are inherently interpretable from their inception [22]. This distinction carries significant implications for clinical validation and trust.
Black-box models, such as deep neural networks and complex ensemble methods, operate as opaque systems where internal workings are not easily accessible or interpretable [21]. While these models can achieve high predictive performance, their decision-making process remains hidden, requiring secondary "explainable AI" (XAI) techniques to generate post-hoc rationales for their predictions [22] [21]. In contrast, inherently interpretable models are constrained in their form to be transparent by design, providing explanations that are faithful to what the model actually computes [22]. These include sparse linear models, decision lists, and models that obey structural domain knowledge such as monotonicity constraints (e.g., ensuring that the risk of cancer increases with age, all else being equal) [22].
A critical misconception in the field is the presumed necessity of a trade-off between accuracy and interpretability [22]. In many applications with structured data and meaningful features, there is often no significant difference in performance between complex black-box classifiers and much simpler interpretable models [22]. The ability to interpret results can actually lead to better overall accuracy through improved data processing and feature engineering in subsequent iterations of the knowledge discovery process [22].
Table 1: Comparison of Interpretability Approaches in Machine Learning
| Characteristic | Post-hoc Explainable AI (XAI) | Inherently Interpretable Models |
|---|---|---|
| Explanation Fidelity | Approximate; may not perfectly represent the black box's true reasoning [22] | Exact and faithful to the model's actual computations [22] |
| Model Examples | LIME, SHAP, attention mechanisms [21] | Sparse linear models, decision lists, generalized additive models [22] |
| Clinical Trust | Limited by potential explanation inaccuracies in critical regions of feature space [22] | Higher potential due to transparent reasoning process [22] |
| Typical Use Cases | Explaining pre-existing complex models (DNNs, random forests) [21] | New model development for high-stakes decision domains [22] |
| Regulatory Considerations | Challenging to validate due to separation of model and explanation [22] | Potentially simpler validation pathway due to integrated transparency [22] |
Interpretability Frameworks and Methodologies
The field of explainable AI has developed numerous technical approaches to address the black box problem, which can be broadly categorized into model-specific and model-agnostic methods, as well as global and local explanation techniques [21].
Model-Agnostic Interpretation Methods
Model-agnostic methods can be applied to any machine learning model after it has been trained, making them particularly valuable for explaining complex black-box models already in use in clinical settings. One prominent example is SHapley Additive exPlanations (SHAP), which connects game theory with local explanations to quantify the contribution of each feature to a individual prediction [21] [24]. For example, in a study predicting delays in seeking medical care among breast cancer patients, researchers used SHAP to provide model visualization and interpretation, identifying key factors influencing predictions [24]. Similarly, LIME (Local Interpretable Model-agnostic Explanations) approximates black-box models locally with interpretable models to create explanations for individual instances [21].
inherently Interpretable Model Architectures
Inherently interpretable models avoid the fidelity issues of post-hoc explanations by design. These models include:
- Sparse linear models: These constrain the number of features used, making it easier for humans to comprehend the relationships since people can handle at most 7±2 cognitive entities at once [22].
- Decision lists and rules: These provide explicit, logical conditions that lead to specific predictions, mirroring clinical decision-making processes.
- Monotonic models: These enforce directional constraints (e.g., risk increases with age) that align with clinical domain knowledge [22].
- Generalized additive models (GAMs): These provide transparent structure while capturing nonlinear relationships [22].
Table 2: Experimental Metrics for Evaluating Interpretability Methods in Cancer Prediction
| Evaluation Metric | Description | Application in Cancer Research |
|---|---|---|
| Prediction Accuracy | Standard measures of model predictive performance (AUC, F1-score, etc.) | CatBoost achieved 98.75% accuracy in cancer risk prediction [25]; RF showed AUC of 0.86 in predicting care delays [24] |
| Explanation Faithfulness | Degree to which explanations accurately represent the model's actual reasoning process [22] | Critical for clinical validation; post-hoc explanations necessarily have imperfect fidelity [22] |
| Human Interpretability | Assessment of how easily domain experts can understand the explanation | Sparse models allow view of how variables interact jointly rather than individually [22] |
| Robustness | Consistency of explanations for similar inputs | Essential for clinical reliability; small changes in input shouldn't cause large explanation changes [23] |
| Bias Detection | Ability to identify discriminatory patterns or unfair treatment of subgroups | Interpretable models can be audited to ensure they don't discriminate based on demographics [23] |
Experimental Protocols for Interpretability Validation in Cancer Detection
Validating interpretability methods requires rigorous experimental protocols that assess both explanatory power and predictive performance. The following methodologies represent current approaches in cancer detection research.
Model Development and Interpretation Workflow
The experimental workflow for developing and interpreting machine learning models in cancer research typically follows a structured pipeline that integrates both performance optimization and explanation generation, as exemplified by recent studies in cancer risk prediction [25] and care delay prediction [24].
Case Study: Predicting Delays in Breast Cancer Care
A 2025 study on predicting delays in seeking medical care among breast cancer patients in China provides a representative experimental protocol for interpretable machine learning in oncology [24]:
Dataset and Preprocessing: The study utilized a cross-sectional methodology collecting demographic and clinical characteristics from 540 patients with breast cancer. Of these, 212 patients (39.26%) experienced a delay in seeking care, creating a balanced classification scenario [24].
Feature Selection: Feature selection was performed using a Lasso algorithm, which identified eight variables most predictive of care delays. This sparse feature selection enhances interpretability by focusing on the most clinically relevant factors [24].
Model Training and Comparison: Six machine learning algorithms were applied for model construction: XGBoost (XGB), Logistic Regression (LR), Random Forest (RF), Complement Naive Bayes (CNB), Support Vector Machines (SVM), and K-Nearest Neighbors (KNN). The k-fold cross-validation method was used for internal verification [24].
Model Evaluation: Multiple evaluation approaches were employed:
- ROC curves assessed discrimination capability
- Calibration curves evaluated prediction accuracy
- Decision Curve Analysis (DCA) quantified clinical utility
- External validation tested generalizability [24]
Interpretation and Visualization: The SHAP (SHapley Additive exPlanations) method was used for model interpretation and visualization, providing both global and local explanations of model behavior [24].
Results: The Random Forest model demonstrated superior performance with AUC values of 1.00, 0.86, and 0.76 in the training set, validation set, and external verification respectively. The calibration curves closely resembled ideal curves, and DCA showed net clinical benefit [24].
Case Study: Cancer Risk Prediction Using Lifestyle and Genetic Data
A 2025 study on cancer risk prediction provides another exemplar of interpretable ML protocols in oncology research [25]:
Dataset: The study used a structured dataset of 1,200 patient records with features including age, gender, BMI, smoking status, alcohol intake, physical activity, genetic risk level, and personal history of cancer [25].
Model Comparison: Nine supervised learning algorithms were evaluated and compared: Logistic Regression, Decision Tree, Random Forest, Support Vector Machines, and several ensemble methods [25].
Performance Assessment: The models were evaluated using stratified cross-validation and a separate test set. Categorical Boosting (CatBoost) achieved the highest predictive performance with a test accuracy of 98.75% and an F1-score of 0.9820 [25].
Feature Importance Analysis: The study conducted feature importance analysis, which confirmed the strong influence of cancer history, genetic risk, and smoking status on prediction outcomes, providing clinical face validity to the model [25].
The Scientist's Toolkit: Essential Research Reagents for Interpretable AI in Cancer Research
The implementation and validation of interpretable machine learning models in cancer detection requires a suite of methodological tools and software frameworks.
Table 3: Essential Research Reagents for Interpretable AI in Cancer Research
| Tool/Reagent | Type | Function in Interpretable AI Research |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | Software Library | Explains output of any ML model by quantifying feature importance for individual predictions [21] [24] |
| LIME (Local Interpretable Model-agnostic Explanations) | Software Library | Creates local surrogate models to explain individual predictions of black box models [21] |
| Lasso Regression | Algorithm | Performs feature selection for sparse, interpretable models by penalizing non-essential coefficients [24] |
| Random Forest | Algorithm | Provides inherent feature importance metrics while maintaining high performance in medical applications [24] [25] |
| CatBoost | Algorithm | Gradient boosting implementation with built-in feature importance analysis and high predictive accuracy [25] |
| Stratified Cross-Validation | Methodological Protocol | Ensures reliable performance estimation across data subsets, critical for clinical validation [24] [25] |
| Decision Curve Analysis (DCA) | Statistical Method | Evaluates clinical utility of models by quantifying net benefit across threshold probabilities [24] |
| ROC/AUC Analysis | Evaluation Metric | Measures discriminatory capability of models using receiver operating characteristic curves and area under curve [24] [25] |
The black box problem in machine learning represents a critical challenge for clinical adoption in oncology, where decisions directly impact patient outcomes and require rigorous validation [22] [20]. While post-hoc explanation methods like SHAP and LIME provide valuable tools for interpreting existing complex models, inherently interpretable models offer distinct advantages for high-stakes medical applications through their guaranteed explanation fidelity and alignment with clinical reasoning patterns [22].
The experimental protocols and case studies presented demonstrate that interpretability need not come at the cost of performance, with many studies achieving high predictive accuracy while maintaining model transparency [24] [25]. As AI continues to transform cancer diagnostics and treatment, the research community must prioritize the development and validation of interpretable models that enable clinical experts to understand, trust, and effectively utilize these powerful tools in patient care [22] [20]. Future work should focus on standardizing evaluation metrics for interpretability, developing domain-specific interpretable model architectures, and establishing regulatory frameworks that ensure transparency and accountability in clinical AI systems [20].
The integration of machine learning (ML) models into clinical practice for cancer detection represents a paradigm shift in oncology. However, their path from research validation to clinical deployment is fraught with complex regulatory and ethical challenges. The validation of these models extends beyond mere algorithmic accuracy; it necessitates rigorous adherence to data protection laws like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in the EU, as well as medical device regulations enforced by the U.S. Food and Drug Administration (FDA) [26] [6]. These frameworks collectively aim to ensure that innovative technologies are not only effective but also safe, ethical, and respectful of patient privacy. For researchers and drug development professionals, understanding the nuances and intersections of these regulations is crucial for designing robust validation protocols and facilitating the successful translation of ML models from the bench to the bedside. This guide provides a comparative analysis of these key regulatory hurdles, supported by experimental data and structured to inform the validation process within cancer detection research.
Comparative Analysis of Key Regulatory Frameworks
HIPAA vs. GDPR: A Privacy-Centric Comparison
For any ML model handling patient data, compliance with data privacy regulations is the first critical hurdle. HIPAA and GDPR are the two most influential frameworks, but they approach data protection with distinct philosophies and requirements.
Table 1: Core Differences Between HIPAA and GDPR in Clinical Research
| Feature | HIPAA (U.S. Focus) | GDPR (EU Focus) |
|---|---|---|
| Scope & Application | Applies to "covered entities" (healthcare providers, plans, clearinghouses) and their "business associates" [27] [28]. | Applies to any organization processing personal data of EU individuals, regardless of location [27] [28]. |
| Data Definition | Protects "Protected Health Information (PHI)" [27]. | Protects "personal data," defined much more broadly to include any information relating to an identified or identifiable person [28]. |
| Legal Basis for Processing | Primarily relies on patient authorization for use/disclosure of PHI [28]. | Offers multiple bases, including explicit consent, legitimate interest, or performance of a task in the public interest [29] [28]. |
| Data Subject Rights | Rights to access, amend, and receive an accounting of disclosures [28]. | Extensive rights including access, rectification, erasure ("right to be forgotten"), and data portability [27] [28]. |
| Data Breach Notification | Required within 60 days of discovery for breaches affecting 500+ individuals [27]. | Mandatory reporting to authorities within 72 hours of becoming aware of the breach [27] [28]. |
| Anonymization | De-identified data (per Safe Harbor or Expert Determination methods) is no longer considered PHI and is exempt [30] [28]. | Pseudonymized data is still considered personal data and remains under GDPR protection [28]. |
| Cross-Border Data Transfer | No specific provisions for international transfers [28]. | Strict rules requiring adequacy decisions or safeguards like Standard Contractual Clauses (SCCs) [28]. |
The implications for ML validation are profound. Under HIPAA, once data is de-identified, it can be used more freely for model training and testing [28]. In contrast, the GDPR's stricter view of pseudonymization means that most data used in ML workflows for cancer research likely remains subject to its requirements, including the principles of data minimization and purpose limitation [29]. This means researchers must justify the amount of data collected and specify its use at the outset, challenging practices where data is repurposed for new ML projects without a fresh legal basis.
FDA Regulatory Pathways for AI/ML-Enabled Medical Devices
In the U.S., ML models intended for clinical use in cancer detection, diagnosis, or treatment planning are typically regulated by the FDA as software as a medical device (SaMD). The FDA has authorized over 1,000 AI/ML-enabled medical devices, with the vast majority (76%) focused on radiology, a key area for cancer detection [31] [32].
Table 2: FDA Regulatory Pathways and AI/ML-Specific Considerations
| Pathway | Description | Relevance to AI/ML Cancer Detection Models |
|---|---|---|
| 510(k) Clearance | For devices "substantially equivalent" to a legally marketed predicate device [31]. | The most common pathway (96.4% of devices); suitable for incremental innovations in established domains like radiology AI [31]. |
| De Novo Classification | For novel devices with no predicate, but with low to moderate risk [31]. | Used for first-of-their-kind AI diagnostics (3.2% of devices); establishes a new predicate for future devices [31]. |
| Premarket Approval (PMA) | The most stringent pathway for high-risk (Class III) devices [31]. | Required for AI models guiding critical, irreversible treatment decisions (0.4% of devices) [31]. |
| Predetermined Change Control Plan (PCCP) | A proposed framework to allow safe and iterative modification of AI/ML models after deployment [31]. | Critical for "locked" and "adaptive" algorithms; enables continuous learning and improvement while maintaining oversight. Only 1.5% of approved devices reported a PCCP as of 2024 [31]. |
A significant challenge in this domain is transparency. A 2025 study evaluating FDA-reviewed AI/ML devices found that the average transparency score was low (3.3 out of 17), with over half of the devices not reporting any performance metric like sensitivity or specificity in their public summaries [31]. This highlights a gap between regulatory review and the information available to the scientific community for independent assessment.
Experimental Data and Validation Protocols
Performance Metrics for Regulatory Evaluation
To gain regulatory approval, ML models for cancer detection must demonstrate robust performance through rigorously designed clinical studies. The following table summarizes reported performance metrics for a range of FDA-cleared AI/ML devices, providing a benchmark for researchers.
Table 3: Reported Performance Metrics of FDA-Cleared AI/ML Medical Devices (Adapted from [31])
| Performance Metric | Reported Median (IQR) (%) | Frequency of Reporting in FDA Summaries (n=1012 devices) |
|---|---|---|
| Sensitivity | 91.2 (85 - 94.6) | 23.9% |
| Specificity | 91.4 (86 - 95) | 21.7% |
| Area Under the ROC (AUROC) | 96.1 (89.4 - 97.4) | 10.9% |
| Positive Predictive Value (PPV) | 59.9 (34.6 - 76.1) | 6.5% |
| Negative Predictive Value (NPV) | 98.9 (96.1 - 99.3) | 5.3% |
| Accuracy | 91.7 (86.4 - 95.3) | 6.4% |
It is critical to note that nearly half (46.9%) of authorized devices did not report a clinical study at all, and 51.6% did not report any performance metric in their public summaries [31]. This underscores the importance of comprehensive and transparent reporting in model validation research.
Detailed Experimental Protocol for Model Validation
A protocol designed to satisfy both scientific and regulatory requirements should include the following key methodologies, drawn from successful regulatory submissions and best practices:
- Retrospective and Prospective Data Collection: While most studies (32.1%) are retrospective, prospective data collection (7.4%) provides stronger evidence for real-world performance [31]. A hybrid approach (1.1%) can balance speed and robustness.
- Dataset Characterization and Curation: Researchers must meticulously document dataset sources, sizes, and demographics. Only 23.7% of FDA-approved devices reported dataset demographics, a major transparency gap [31]. For GDPR compliance, the provenance and legal basis for all data must be documented.
- Clinical Validation Study: A key step is conducting a clinical study to evaluate the model's performance against the standard of care. The median sample size for such studies in FDA submissions is 306 patients (IQR 142-650) [31]. The study should be designed to test the model's intended use and its impact on clinical workflow and patient outcomes.
- Bias and Fairness Assessment: Models must be evaluated for performance across appropriate subgroups (e.g., age, sex, ethnicity). This is not only an ethical imperative but also a requirement under FDA's Good Machine Learning Practice (GMLP) principles and the EU AI Act for high-risk systems [26] [31].
- Privacy-Preserving Validation Techniques: To comply with data minimization principles, techniques like federated learning (training models across decentralized data without sharing it) and the use of synthetic data should be explored. Recent research, such as the DP-TimeGAN model, demonstrates the generation of realistic, longitudinal electronic health records with quantifiable privacy protections aligned with both HIPAA and GDPR [33].
Visualization of Regulatory Workflows
FDA Pathway for AI/ML Medical Devices
The following diagram illustrates the key decision points and pathways for bringing an AI/ML-based cancer detection model to market in the U.S.
FDA AI/ML Device Pathway
Integrated Data Governance for Clinical ML Research
This workflow outlines the integrated data governance considerations when managing patient data for model training under both HIPAA and GDPR.
Data Governance Workflow
The Scientist's Toolkit: Research Reagent Solutions
Navigating the regulatory landscape requires both methodological and technical tools. The following table details essential "research reagents" for validating ML models in a compliant manner.
Table 4: Essential Tools for Compliant ML Model Validation in Cancer Detection
| Tool / Solution | Function | Relevance to GDPR/HIPAA/FDA |
|---|---|---|
| Privacy-Preserving Synthetic Data (e.g., DP-TimeGAN) | Generates realistic, synthetic patient datasets with mathematical privacy guarantees (e.g., Differential Privacy) [33]. | Enables model development and testing without using real PHI/personal data, addressing data minimization and utility for research. |
| Federated Learning Platforms | A distributed ML approach where the model is trained across multiple decentralized data sources without moving or sharing the raw data [29]. | Mitigates cross-border data transfer issues under GDPR and reduces centralization of sensitive data, aiding compliance with both GDPR and HIPAA. |
| De-identification & Pseudonymization Tools | Software that automatically identifies and removes (de-identification) or replaces with a reversible token (pseudonymization) personal identifiers in datasets [30]. | Core to creating HIPAA-compliant de-identified datasets. Pseudonymization is a key security measure under GDPR, though it does not exempt data from the regulation. |
| Data Protection Impact Assessment (DPIA) Template | A structured tool to systematically identify and minimize the data protection risks of a project [29]. | A mandatory requirement under GDPR for high-risk processing, such as large-scale use of health data for ML. |
| Predetermined Change Control Plan (PCCP) Framework | A documented protocol outlining the planned modifications to an AI/ML model and the validation methods used to ensure those changes are safe and effective [31]. | A proposed framework by the FDA to manage the lifecycle of AI/ML devices, allowing for continuous improvement post-deployment. |
Methodologies in Action: Building and Applying Validated ML Models for Cancer Detection
The validation of machine learning models has become a cornerstone of modern cancer detection research, providing the rigorous methodology required to translate computational predictions into clinical insights. Among the diverse artificial intelligence architectures, Convolutional Neural Networks (CNNs), Recurrent Neural Networks (RNNs)—including their variant Long Short-Term Memory networks (LSTMs)—and hybrid models have emerged as particularly transformative. Each architecture offers distinct advantages aligned with the data modalities prevalent in oncology: CNNs excel at parsing spatial hierarchies in imaging data, RNNs/LSTMs capture temporal and sequential dependencies in genomic information, and hybrid models integrate multiple data types and algorithms to create more robust predictive systems. This guide provides a systematic comparison of these architectures, detailing their performance, experimental protocols, and implementation requirements to inform researchers, scientists, and drug development professionals in selecting and validating appropriate models for specific oncological applications. The objective analysis presented herein is framed within the critical context of model validation, emphasizing reproducibility, performance metrics, and clinical applicability across various cancer types.
Convolutional Neural Networks (CNNs) for Medical Imaging
Performance and Experimental Data
CNNs have demonstrated exceptional performance in analyzing medical images for cancer detection, classification, and segmentation. Their capacity to automatically learn hierarchical spatial features from pixel data makes them particularly suited for modalities like mammography, MRI, and histopathology. Recent studies validate their high accuracy across multiple imaging types and cancer domains.
Table 1: CNN Performance Across Cancer Imaging Modalities
| Cancer Type | Imaging Modality | Dataset(s) | Model Architecture | Key Performance Metrics | Reference |
|---|---|---|---|---|---|
| Breast Cancer | Mammography | DDSM, MIAS, INbreast | Custom CNN | Accuracy: 99.2% (DDSM), 98.97% (MIAS), 99.43% (INbreast) | [34] |
| Breast Cancer | Ultrasound, MRI, Histopathology | Ultrasound, MRI, BreaKHis | Custom CNN | Accuracy: 98.00% (Ultrasound), 98.43% (MRI), 86.42% (BreaKHis) | [34] |
| Brain Tumors | MRI | Custom dataset (3,000+ images) | VGG, ResNet, EfficientNet, ConvNeXt, MobileNet | Best accuracy: 98.7%; MobileNet: 23.7 sec/epoch training time | [35] |
| Brain Tumors | MRI | Custom dataset (7,023 images) | CNN-TumorNet | Accuracy: 99.9% for tumor vs. non-tumor classification | [36] |
Detailed Experimental Protocols
Multimodal Breast Cancer Detection Framework [34]: This study developed a unified CNN framework capable of processing multiple imaging modalities within a single model. The methodology involved: (1) Data Acquisition and Preprocessing: Collecting images from several benchmark datasets (DDSM, MIAS, INbreast for mammography; additional datasets for ultrasound, MRI, and histopathology). Standardized preprocessing procedures were applied across all datasets, including resizing, normalization, and augmentation to ensure consistency. (2) Model Architecture and Training: Implementing a CNN architecture optimized to minimize overfitting through strategic design choices like dropout layers and batch normalization. The model was trained to perform binary classification (cancerous vs. non-cancerous) across all modalities. (3) Validation and Comparison: Evaluating the model on held-out test sets for each modality and comparing performance against leading state-of-the-art techniques using accuracy as the primary metric.
Brain Tumor Classification Study [35]: This research comprehensively analyzed CNN performance for brain tumor classification using MRI. The experimental protocol included: (1) Dataset Curation: Utilizing over 3,000 MRI images spanning three tumor types (gliomas, meningiomas, pituitary tumors) and non-tumorous images. (2) Architecture Comparison: Exploring recent deep architectures (VGG, ResNet, EfficientNet, ConvNeXt) alongside a custom CNN with convolutional layers, batch normalization, and max-pooling. (3) Training Methodologies: Assessing different approaches including training from scratch, data augmentation, transfer learning, and fine-tuning. Hyperparameters were optimized using separate validation sets. (4) Performance Evaluation: Measuring accuracy and computational efficiency (training time, image throughput) on independent test sets.
Research Reagent Solutions
Table 2: Essential Research Materials for CNN Experiments in Oncology Imaging
| Reagent/Resource | Function in Experimental Protocol | Example Specifications |
|---|---|---|
| Curated Medical Image Datasets | Model training and validation | DDSM, MIAS, INbreast (mammography); TCIA (MRI); BreaKHis (histopathology) |
| Deep Learning Frameworks | Model implementation and training | TensorFlow, Keras, PyTorch with GPU acceleration |
| Data Augmentation Tools | Dataset expansion and regularization | Rotation, flipping, scaling, contrast adjustment transforms |
| Transfer Learning Models | Pre-trained feature extractors | VGG, ResNet, EfficientNet weights pre-trained on ImageNet |
| GPU Computing Resources | Accelerated model training | NVIDIA Tesla V100, A100, or RTX series with CUDA support |
| Medical Image Preprocessing Libraries | Standardization of input data | SimpleITK, OpenCV, scikit-image for resizing, normalization |
RNNs/LSTMs for Genomic Sequences
Performance and Experimental Data
RNNs and their more sophisticated variants, particularly LSTMs and Gated Recurrent Units (GRUs), have shown significant promise in analyzing genomic sequences for cancer mutation prediction, transcription factor binding site identification, and oncogenic progression forecasting. Their ability to capture long-range dependencies in sequential data makes them naturally suited for genomic applications.
Table 3: RNN/LSTM Performance in Genomic Cancer Applications
| Application Domain | Data Source | Model Architecture | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Oncogenic Mutation Progression | TCGA Database | RNN with LSTM units | Accuracy: >60%, ROC curves comparable to existing diagnostics | [37] |
| Transcription Factor Binding Site Prediction | ENCODE ChIP-seq data | Bidirectional GRU with k-mer embedding (KEGRU) | Superior AUC and APS compared to gkmSVM, DeepBind, CNN_ZH | [38] |
| Cancer Classification from Exome Sequences | Twenty exome datasets | Ensemble with MLPs | Weighted average accuracy: 82.91% | [39] |
Detailed Experimental Protocols
RNN Framework for Mutation Progression [37]: This study developed an end-to-end framework for predicting cancer severity and mutation progression using RNNs. The methodology comprised: (1) Data Processing: Isolation of mutation sequences from The Cancer Genome Atlas (TCGA) database. Implementation of a novel preprocessing algorithm to filter key mutations by mutation frequency, identifying a few hundred key driver mutations per cancer stage. (2) Network Module: Construction of an RNN with LSTM architectures to process mutation sequences and predict cancer severity. The model incorporated embeddings similar to language models but applied to cancer mutation sequences. (3) Result Processing and Treatment Recommendation: Using RNN predictions combined with information from preprocessing algorithms and drug-target databases to predict future mutations and recommend possible treatments.
KEGRU for TF Binding Site Prediction [38]: This research introduced KEGRU, a model combining Bidirectional GRU with k-mer embedding for predicting transcription factor binding sites. The experimental protocol included: (1) Sequence Representation: DNA sequences were divided into k-mer sequences with specified length and stride window, treating each k-mer as a word in a sentence. (2) Embedding Training: Pre-training word representation models using the word2vec algorithm on k-mer sequences. (3) Model Architecture: Constructing a deep bidirectional GRU model for feature learning and classification, using 125 TF binding sites ChIP-seq experiments from the ENCODE project. (4) Performance Validation: Comparing model performance against state-of-the-art methods (gkmSVM, DeepBind, CNN_ZH) using AUC and average precision score as metrics.
Research Reagent Solutions
Table 4: Essential Research Materials for RNN/LSTM Experiments in Genomics
| Reagent/Resource | Function in Experimental Protocol | Example Specifications |
|---|---|---|
| Genomic Databases | Source of sequence and mutation data | TCGA, ENCODE, SEER, NCBI SRA |
| Sequence Preprocessing Tools | K-mer segmentation and data cleaning | Biopython, custom Python scripts for k-mer generation |
| Embedding Algorithms | Sequence vectorization | word2vec, GloVe, specialized biological embedding methods |
| Specialized RNN Frameworks | Model implementation | TensorFlow, PyTorch with LSTM/GRU cell support |
| High-Performance Computing | Handling large genomic datasets | CPU cluster with high RAM for sequence processing |
| Genomic Annotation Databases | Functional interpretation of results | ENSEMBL, UCSC Genome Browser, dbSNP |
Hybrid Models for Comprehensive Cancer Analysis
Performance and Experimental Data
Hybrid models that integrate multiple algorithmic approaches or data modalities have emerged as powerful tools for addressing the multifaceted nature of cancer biology. These models combine the strengths of different architectures to overcome individual limitations and enhance predictive performance, particularly for complex tasks like survival prediction and multi-modal data integration.
Table 5: Hybrid Model Performance in Oncology Applications
| Application Domain | Cancer Type | Hybrid Architecture | Key Performance Metrics | Reference |
|---|---|---|---|---|
| Survival Prediction | Cervical Cancer | CoxPH with Elastic Net + Random Survival Forest | C-index: 0.82, IBS: 0.13, AUC-ROC: 0.84 | [40] [41] |
| Early Mortality Prediction | Hepatocellular Carcinoma | Ensemble of ANN, GBDT, XGBoost, DT, SVM | AUROC: 0.779 (internal), 0.764 (external), Brier score: 0.191 | [42] |
| Cancer Classification | Multiple Cancers | Ensemble with KNN, SVM, MLPs | Accuracy: 82.91% (increased to 92% with GAN/TVAE) | [39] |
Detailed Experimental Protocols
Hybrid Survival Model for Cervical Cancer [40] [41]: This research developed a hybrid survival model integrating traditional statistical approaches with machine learning for cervical cancer survival prediction. The methodology included: (1) Data Source and Preprocessing: Extraction of cervical cancer patient data from the SEER database (2013-2015) with preprocessing involving normalization, encoding, and handling missing values through multiple imputation. (2) Model Components: Implementation of two complementary models: Random Survival Forest (RSF) to capture non-linear interactions between covariates, and Cox Proportional Hazards (CoxPH) model with Elastic Net regularization for linear interpretability and feature selection. (3) Hybridization Strategy: Combination of predictions from both models using a weighted averaging approach based on linear regression weighting coefficients determined through cross-validation. (4) Validation: Assessment of model performance on an independent test set using concordance index (C-index), Integrated Brier Score (IBS), and AUC-ROC metrics.
Ensemble Model for Early Mortality Prediction [42]: This study constructed an ensemble machine learning model to predict early mortality among hepatocellular carcinoma (HCC) patients with bone metastases. The experimental protocol involved: (1) Data Extraction and Cohort Definition: Identifying HCC patients with bone metastases from the SEER database (2000-2019), with early mortality defined as survival ≤3 months. (2) Feature Selection and Model Training: Selecting significant clinical variables through subgroup analysis and training five machine learning models (artificial neural network, gradient boosting decision tree, eXGBoosting machine, decision tree, and support vector machine). (3) Ensemble Construction: Implementing soft voting to combine predictions from all models, with hyperparameter optimization through grid and random searches. (4) Validation: Conducting both internal validation (80:20 split) and external validation on patients from two tertiary hospitals, evaluating discrimination (AUROC) and calibration (Brier score, calibration plots).
Research Reagent Solutions
Table 6: Essential Research Materials for Hybrid Model Experiments
| Reagent/Resource | Function in Experimental Protocol | Example Specifications |
|---|---|---|
| Multi-modal Data Repositories | Integrated clinical, genomic, and imaging data | SEER database, TCGA, custom institutional datasets |
| Survival Analysis Packages | Implementation of specialized survival models | R survival package, scikit-survival, lifelines |
| Ensemble Learning Frameworks | Model combination and weighting | Scikit-learn VotingClassifiers, custom ensemble code |
| Hyperparameter Optimization Tools | Model tuning and performance enhancement | GridSearchCV, RandomizedSearchCV, Optuna, Hyperopt |
| Model Interpretation Libraries | Explainability and feature importance | SHAP, LIME, partial dependence plots |
| Validation Frameworks | Robust internal and external validation | Scikit-learn cross-validation, calibration curve tools |
Comparative Analysis and Clinical Implementation
Architecture Selection Guidelines
The optimal architecture selection depends on the specific data modalities, clinical question, and implementation constraints. CNNs consistently demonstrate superior performance for image-based detection tasks, with recent models achieving exceptional accuracy (>98%) in classifying tumors across multiple imaging modalities [34] [35] [36]. RNNs/LSTMs provide specialized capability for sequential genomic data, with architectures like bidirectional GRUs showing particular promise for tasks such as transcription factor binding site prediction [38]. Hybrid models offer the most flexible framework for integrating diverse data types and addressing complex clinical questions like survival prediction, with ensemble approaches demonstrating robust performance across multiple cancer types [40] [42] [41].
Validation Considerations
Robust validation remains paramount across all architectures, with particular considerations for each approach. CNN validation requires careful attention to dataset diversity across imaging devices and protocols to ensure generalizability [34] [35]. RNN/LSTM validation must address genomic heterogeneity and population-specific mutation patterns through external validation cohorts [37] [39]. Hybrid model validation necessitates both statistical rigor in evaluating survival predictions and clinical relevance in risk stratification [40] [42]. Explainability techniques like LIME have emerged as crucial components for clinical adoption, particularly for complex models where interpretability is challenging [36].
Implementation Challenges and Solutions
Clinical implementation faces several common challenges across architectures. Class imbalance frequently affects cancer datasets, with techniques like SMOTE oversampling and appropriate metric selection (e.g., AUC-ROC, F1-score) providing mitigation [39]. Computational resource requirements vary significantly, with CNNs demanding substantial GPU memory for high-resolution images [35], while RNNs benefit from high RAM capacity for genomic sequence processing [37] [38]. Data privacy and regulatory compliance present additional considerations, particularly for models integrating multiple data sources [42] [41]. Prospective validation in clinical workflows remains the critical final step for translating these architectures from research tools to clinical decision support systems.
Data Preprocessing and Augmentation Techniques for Robust Feature Extraction in Medical Data
The validation of machine learning models in cancer detection research hinges on the quality and robustness of the features extracted from medical data. In clinical settings, data is often scarce, noisy, and heterogeneous, which can lead to models that overfit and fail to generalize in real-world scenarios. Data preprocessing and augmentation are therefore not merely preliminary steps but foundational techniques for building reliable, robust models. This guide objectively compares the performance of various preprocessing and augmentation methodologies, framing them within the critical context of developing validated machine learning applications for oncology.
Core Techniques and Comparative Analysis
Fundamental Preprocessing Techniques
Preprocessing aims to standardize data and enhance image quality, which is crucial for consistent feature extraction. The following techniques form the backbone of most medical image analysis pipelines [43].
- Background Removal: This process isolates the Region of Interest (ROI) from the background, improving computational efficiency and model accuracy by removing irrelevant data. A common application is skull stripping in brain MRI scans.
- Denoising: Medical images often contain noise from acquisition processes. Denoising techniques, such as Gaussian filtering, median filtering, or more advanced wavelet-based and deep learning methods, reduce this noise while striving to preserve critical structural details.
- Resampling: This technique changes the pixel or voxel size of an image to standardize resolution across a dataset acquired from different scanners or protocols, ensuring consistent input dimensions for models.
- Intensity Normalization: Standardizing the range of pixel intensity values across a dataset is vital. It ensures that models learn from structural information rather than being biased by variations in contrast or brightness.
Data Augmentation: Classic vs. Generative Approaches
Data augmentation expands the size and diversity of training datasets. The two primary paradigms are classic and generative augmentation.
- Classic Data Augmentation: This involves applying simple, label-preserving transformations to existing images, such as rotation, flipping, scaling, and elastic deformations. These methods are computationally efficient and widely used to teach models invariance to these transformations [44].
- Generative Data Augmentation: With advances in deep learning, synthetic data generation using Generative Adversarial Networks (GANs) and Diffusion Models has emerged. These methods can generate entirely new, realistic images, which is particularly valuable for creating examples of rare conditions or complex variations [45] [46].
The table below summarizes a performance comparison between these approaches based on studies in medical imaging.
Table 1: Comparison of Classic vs. Generative Augmentation Techniques
| Augmentation Type | Key Methods | Reported Performance Improvement | Computational Cost | Key Advantages | Primary Challenges |
|---|---|---|---|---|---|
| Classic Augmentation | Rotation, Flipping, Scaling, Elastic Deform. | Ubiquitous use; essential for baseline performance. | Low | Simple, efficient, well-understood. | Limited diversity; may not cover all real-world variations. |
| Generative (GAN-based) | GliGAN [46], DCGAN [44] | Ranked 1st in BraTS 2025 challenge; significantly improved Dice scores for small lesions. | High | Can generate highly realistic and diverse synthetic data. | Computationally intensive; requires expertise to train. |
| Generative (LLM-based) | Llama3 for text paraphrasing [47] | Increased F1-score by 2.3 to 3.9 points for metastases detection in radiology reports. | High | Effective for non-image data; requires minimal seed data. | Quality of generation depends on model and prompt design. |
An Alternative Approach: Feature Extraction Without Augmentation
Some methodologies aim to bypass the need for data augmentation altogether by developing more powerful feature extraction techniques. The Feature Extraction Based on Region of Mines (FE_mines) approach is one such method, which derives multiple formulas from each image using signal and image processing [48]. It then uses data distribution skew to calculate statistical measurements that reveal hidden features, thereby increasing discrimination among classes. In experiments on diabetic retinopathy, brain tumor, and COVID-19 chest X-ray datasets, this approach achieved accuracy gains of 1% to 13% compared to traditional methods like RGB and ASPS, without requiring data augmentation [48].
Experimental Protocols and Workflows
Workflow for Robust Model Development
The following diagram illustrates a comprehensive workflow for developing and validating robust machine learning models in cancer detection, integrating the techniques discussed.
Protocol: On-the-Fly Generative Augmentation for Brain Tumor Segmentation
A state-of-the-art protocol from the winning solution of the BraTS 2025 Challenge demonstrates the effective integration of generative augmentation [46].
- Objective: To improve the robustness and accuracy of a deep learning model in segmenting brain tumor subregions from MRI scans, particularly for small and underrepresented lesions.
- Model Architecture: The base model was a 3D nnU-Net, a self-configuring framework known for its performance in medical segmentation. The input was random patches of shape 128×160×112.
- Augmentation Strategy - On-the-Fly GliGAN:
- Synthetic Tumor Insertion: Instead of pre-generating and storing thousands of synthetic images, a pre-trained GliGAN (a GAN for glioma MRI) was integrated into the training loop. For each batch, images were dynamically modified with a probability
pto insert a synthetic tumor. - Targeted Class Balancing: To address class imbalance, the input label masks to the GAN were strategically modified. For instance, the "Surrounding non-enhancing FLAIR hyperintensity" (SNFH) class was replaced with "Enhancing Tumor" (ET), and ET was then replaced with "Non-enhancing tumor core" (NETC) with a probability of 0.7. This increased the prevalence of these underrepresented classes in the training stream.
- Small Lesion Synthesis: A scale parameter was used to deliberately generate smaller versions of real tumor labels, forcing the model to learn features of small lesions that are often missed due to their low contribution to the overall loss function.
- Synthetic Tumor Insertion: Instead of pre-generating and storing thousands of synthetic images, a pre-trained GliGAN (a GAN for glioma MRI) was integrated into the training loop. For each batch, images were dynamically modified with a probability
- Evaluation: The model was evaluated on the BraTS validation set using lesion-wise Dice scores. An ensemble of a baseline model and models trained with different on-the-fly augmentation strategies achieved top performance, with Dice scores of 0.79 (ET), 0.749 (NETC), and 0.872 (RC) [46].
Protocol: Diagnostic Framework for Temporal Validation
Beyond image analysis, ensuring model robustness over time is critical. A diagnostic framework for validating clinical machine learning models on time-stamped data, such as Electronic Health Records (EHR), involves the following steps [49]:
- 1. Performance Evaluation with Temporal Splitting: Instead of a simple random split, data is partitioned by year. Models are trained on data from one period and validated on data from subsequent years to test temporal robustness.
- 2. Characterize Temporal Evolution: The framework analyzes how patient characteristics (features) and outcomes (labels) evolve. This helps identify potential data drift, such as changes in medical practices or coding systems.
- 3. Explore Model Longevity: Different training schedules are tested, such as using only the most recent data versus all historical data, to find the optimal trade-off between data quantity and recency.
- 4. Feature and Data Valuation: Feature importance analysis and data valuation algorithms are applied to reduce dimensionality and assess the quality and relevance of data points over time.
- Application: When applied to predict Acute Care Utilization (ACU) in cancer patients, this framework highlighted moderate signs of drift, underscoring the need for temporal considerations in model deployment [49].
The Scientist's Toolkit
The table below lists key resources and tools used in the experiments cited in this guide, providing a practical starting point for researchers.
Table 2: Essential Research Reagents and Tools for Medical Data Preprocessing & Augmentation
| Item Name | Type | Primary Function | Example Use Case |
|---|---|---|---|
| nnU-Net [46] | Software Framework | Self-configuring pipeline for medical image segmentation. | Baseline and advanced segmentation models (e.g., Brain Tumor in BraTS challenges). |
| GliGAN [46] | Pre-trained Model | Generative Adversarial Network for inserting realistic synthetic tumors into brain MRIs. | On-the-fly data augmentation to increase tumor diversity and address class imbalance. |
| TorchIO [43] | Python Library | Efficient loading, preprocessing, and augmentation of 3D medical images in PyTorch. | Building reproducible preprocessing pipelines (resampling, normalization, etc.). |
| FE_mines [48] | Algorithm | Novel feature extraction method based on region statistics and data distribution skew. | Building classifiers without data augmentation on limited medical image data. |
| SimpleITK / ITK [43] | Software Library | Comprehensive toolkit for image registration and segmentation. | Advanced preprocessing tasks like aligning images from different modalities (registration). |
| Llama3 / BERT [47] | Large Language Model | Generating synthetic training data and fine-tuning for NLP tasks on clinical text. | Data augmentation for extracting metastasis information from free-text radiology reports. |
The choice of data preprocessing and augmentation strategy has a profound impact on the robustness of feature extraction and the subsequent validation of machine learning models in cancer detection. While classic augmentation remains a reliable and efficient baseline, generative methods offer powerful capabilities for tackling data scarcity and class imbalance, as evidenced by their leading performance in competitive challenges. Simultaneously, innovative feature extraction methods can sometimes circumvent the need for augmentation. A critical emerging theme is the necessity for temporal validation frameworks, especially when working with real-world clinical data, to ensure that models remain relevant and accurate in the face of evolving medical practice. Ultimately, a carefully designed and experimentally validated pipeline combining these techniques is indispensable for building trustworthy AI tools in oncology.
In the field of oncology, the development of robust machine learning models for cancer detection is often hampered by a critical constraint: the scarcity of large, meticulously labeled datasets. Acquiring such data is expensive, time-consuming, and fraught with privacy concerns. Transfer learning (TL) has emerged as a powerful training paradigm to overcome this fundamental limitation. This technique involves taking a pre-trained model—a neural network already trained on a large, general-purpose dataset like ImageNet—and adapting or fine-tuning it for a specific, related task, such as classifying lung nodules from CT scans. By leveraging the generic feature representations the model has already learned, transfer learning enables the development of high-performance models even with limited labeled medical data, reducing both the data and computational resources required.
Framed within the broader thesis of validating machine learning models in cancer detection research, this guide provides an objective comparison of transfer learning performance against other approaches and across different model architectures. It synthesizes recent experimental data and detailed methodologies to offer researchers, scientists, and drug development professionals a clear, evidence-based overview of the current state of the art.
Performance Comparison of Transfer Learning Models in Oncology
Empirical evidence consistently demonstrates that transfer learning not only mitigates data scarcity but also achieves diagnostic accuracy comparable to, and often surpassing, models trained from scratch. The following tables summarize the quantitative performance of various TL models across different cancer types, providing a basis for objective comparison.
Table 1: Performance of Transfer Learning Models in Classifying Different Cancers
| Cancer Type | Imaging Modality | Top-Performing Model(s) | Reported Accuracy | Key Metric(s) | Source |
|---|---|---|---|---|---|
| Lung Cancer | CT Scan | ILN-TL-DM (Hybrid) | 96.2% | Accuracy: 0.962, Specificity: 0.955, NPV: 0.964 | [50] |
| Breast Cancer | Ultrasound | ResNet50 (Fine-tuned) | 95.5% | Accuracy | [51] |
| InceptionV3 | 92.5% | Accuracy | [51] | ||
| VGG16 | 86.5% | Accuracy | [51] | ||
| Skin Cancer | Dermoscopic | Xception + Self-Attention | 94.11% | Accuracy | [52] |
| Xception (Baseline) | 91.05% | Accuracy | [52] | ||
| Lung & Colon Cancer | Histopathological | EfficientNetB3 | High Performance* | Accuracy | [53] |
Note: The specific accuracy value for EfficientNetB3 was not provided in the available excerpt, but the source highlights its "robust" performance [53].
Table 2: Comparison of TL Model Performance on a Common Task (Chest X-Ray Classification)
| Model | Reported Accuracy | Key Strengths | Key Weaknesses | Source |
|---|---|---|---|---|
| ResNet50 | Highest | High accuracy, robust feature learning | Higher computational complexity | [54] |
| MobileNetV2 | Acceptable | Suitable for real-time apps, faster, smaller volume | Lower accuracy than ResNet50 | [54] |
| VGG16 | Lower | Simple, well-understood architecture | Older structure, lower complexity, lower accuracy | [54] |
Detailed Experimental Protocols and Methodologies
To ensure the validity and reproducibility of results, understanding the underlying experimental protocols is crucial. The following section details the methodologies from several key studies cited in this guide.
Lung Cancer Classification from CT Scans
The study proposing the ILN-TL-DM model for lung cancer classification employed a comprehensive, multi-stage pipeline [50]:
- Pre-processing: An Adaptive Gaussian filtering method was applied to eliminate noise and enhance the quality of the input CT images.
- Segmentation: An Improved Attention-based ResU-Net (P-ResU-Net) model was used to accurately isolate the lung and tumor regions from the background. This model incorporated a Residual Dual Channel Attention Block to adaptively focus on important features.
- Feature Extraction: A diverse set of features was derived from the segmented images, including handcrafted features like Local Gabor Transitional Pattern (LGTrP) and Pyramid of Histograms of Oriented Gradients (PHOG), alongside deep features and improved entropy-based features designed to better represent tumor regions.
- Classification: A hybrid architecture combining an improved LeNet structure with Transfer Learning (ILN-TL) and a DeepMaxout (DM) network was used. The outputs of these two models were merged using a soft voting strategy to produce the final classification (cancerous vs. non-cancerous).
Breast Cancer Detection from Ultrasound Images
The research comparing deep learning models for breast cancer detection utilized the publicly available BUSI dataset and followed this protocol [51]:
- Model Selection & Adaptation: Four pre-trained models—MobileNetV2, InceptionV3, ResNet50, and VGG16—were employed. The top layers of these models were frozen, and additional custom layers were added for the specific classification task. A
GlobalAveragePooling2Dlayer was used to reduce the spatial dimensions of the feature maps. - Training for Comparison: The models were trained and tested on the breast ultrasound image dataset. The primary metric for evaluation and comparison was classification accuracy.
Skin Cancer Detection with Attention Mechanisms
The investigation into skin cancer diagnosis explored the effect of augmenting a TL model with attention mechanisms [52]:
- Dataset: The experiments were conducted on the HAM10000 dataset, a large collection of dermoscopic images.
- Experimental Design: Four distinct experiments were run:
- Experiment 1: The standard Xception model (without any attention mechanism) was used as a baseline.
- Experiments 2-4: The Xception architecture was integrated with three different types of attention mechanisms: Self-Attention (SL), Hard Attention (HD), and Soft Attention (SF). Each mechanism allowed the model to focus on diagnostically relevant parts of the image in a unique way.
- Evaluation: The performance of all four models was compared based on accuracy and recall, with the latter being particularly critical for ensuring malignant cases are not missed.
Workflow Visualization of a Transfer Learning Pipeline
The following diagram illustrates a generalized experimental workflow for applying transfer learning to medical image classification, synthesizing the common elements from the cited methodologies.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers aiming to replicate or build upon these studies, the following table details key computational "reagents" and tools referenced in the literature.
Table 3: Key Research Reagents and Computational Tools for Transfer Learning in Cancer Detection
| Item Name | Type | Function in Experiment | Example Use Case |
|---|---|---|---|
| Pre-trained Models (ResNet50, Xception, etc.) | Software Model | Serves as the foundational feature extractor, providing a robust starting point for the target task. | Feature extraction and fine-tuning for breast ultrasound classification [51] [54]. |
| Attention Mechanisms | Algorithmic Module | Allows the model to dynamically focus on the most salient regions of a medical image, improving interpretability and accuracy. | Enhancing Xception for skin lesion classification [52]. |
| Public Datasets (e.g., BUSI, HAM10000) | Dataset | Provides a standardized, annotated set of medical images for training, validation, and benchmarking model performance. | Served as the primary data source for breast cancer [51] and skin cancer [52] studies. |
| ImageDataGenerator / Augmentation Tools | Software Library | Artificially expands the training dataset by creating modified versions of images, combating overfitting. | Used in chest X-ray studies for image normalization and augmentation [54]. |
| OncoKB | Knowledge Base | A precision oncology database used to ground model decisions in evidence-based, actionable cancer mutations. | Integrated into an AI agent for clinical decision-making in oncology [4]. |
| MedSAM | Software Model | A foundation model for segmenting various medical images, used to isolate and measure regions of interest. | Deployed by an AI agent to segment tumors from radiological images [4]. |
Multimodal data fusion represents a transformative approach in oncology, leveraging advances in artificial intelligence (AI) and machine learning (ML) to integrate diverse data types such as medical imaging, genomic sequencing, and clinical electronic health records (EHR). This integration aims to overcome the limitations of single-modality analysis, creating predictive models that more accurately reflect the complex, multifactorial nature of cancer [55] [56]. The practice mirrors clinical decision-making, where physicians naturally synthesize information from multiple sources—including imaging findings, laboratory values, and patient history—to form diagnostic conclusions and treatment plans [56] [57]. Technological advancements in high-throughput sequencing and medical imaging have generated unprecedented volumes of patient data, creating both opportunities and challenges for comprehensive analysis [58] [59].
In cancer detection and prognosis, different data modalities provide complementary biological insights. Genomic data reveals molecular alterations and inherited predispositions, medical imaging captures structural and functional phenotypes of tumors, and EHRs provide contextual clinical information including patient history, symptoms, and laboratory results [59] [56]. By fusing these disparate data streams, researchers hope to achieve more personalized risk assessment, accurate diagnosis, and prediction of treatment response than any single modality can provide alone [55] [58]. However, the integration of multimodal data presents significant computational and methodological challenges, including data heterogeneity, varying dimensionalities, missing values, and the need for specialized analytical approaches [58] [56]. This guide systematically compares the predominant fusion strategies, their performance characteristics, and implementation considerations to inform researchers developing validated ML models for cancer detection.
Comparative Analysis of Fusion Strategies
Multimodal data fusion strategies are broadly categorized into three architectural frameworks based on the stage at which data integration occurs: early, joint, and late fusion. Each approach presents distinct advantages, limitations, and optimal use cases, with performance heavily dependent on data characteristics and the specific clinical question [56] [57].
Table 1: Comparison of Multimodal Data Fusion Strategies
| Fusion Strategy | Description | Best Use Cases | Advantages | Limitations |
|---|---|---|---|---|
| Early Fusion (Feature-level) | Raw features or extracted features from multiple modalities are concatenated into a single feature vector before model input [56]. | Modalities with similar dimensionalities; Strong inter-modality correlations; Availability of powerful feature selection methods [58]. | Preserves potential correlations between modalities during feature learning; Single model simplifies training pipeline [56]. | Susceptible to overfitting with high-dimensional data (e.g., genomics); Requires alignment and normalization of heterogeneous features [58]. |
| Joint Fusion (Intermediate) | Learned feature representations from intermediate layers of separate neural networks are integrated and fed to a final model with loss propagation to all networks [56]. | Complex relationships between modalities; When modalities require specialized feature extraction networks [56] [57]. | Allows modality-specific feature learning while capturing cross-modal interactions; More flexible than early fusion [56]. | Increased model complexity; Requires careful training procedures; More computationally intensive [56]. |
| Late Fusion (Decision-level) | Separate models are trained for each modality, and their predictions are combined using aggregation functions (averaging, voting, meta-classifier) [56]. | Modalities with highly divergent dimensionalities; Heterogeneous data types; Settings requiring model interpretability [58]. | Resistant to overfitting; Handles data heterogeneity effectively; Allows natural weighting of modalities based on informativeness [58]. | Cannot model cross-modal interactions at the feature level; Requires training multiple models [56]. |
Table 2: Performance Comparison of Fusion Strategies in Cancer Research
| Study | Cancer Type | Modalities Integrated | Fusion Strategy | Performance | Key Finding |
|---|---|---|---|---|---|
| npj Precision Oncology (2025) [58] | Lung, Breast, Pan-cancer | Transcripts, proteins, metabolites, clinical factors | Late Fusion | Consistently outperformed single-modality approaches | Late fusion showed higher accuracy and robustness particularly with high-dimensional omics data |
| Systematic Review (2020) [56] | Various (from 17 studies) | Medical imaging + EHR | Early Fusion (11/17 studies) | 6 of 7 studies showed improvement over single modality | Early fusion improved performance or reduced standard deviation |
| AstraZeneca Multimodal Pipeline [58] | Multiple cancer types | Multi-omics data (transcriptomic, proteomic, metabolomic) | Varies by data structure | Dependent on data characteristics | Early fusion worked best with 2-3 modalities and 10²-10³ features; Late fusion superior with 4-7 modalities and 10³-10⁵ features |
Experimental Protocols and Methodologies
Data Preprocessing and Feature Extraction
Robust preprocessing pipelines are fundamental to successful multimodal integration. Experimental protocols typically begin with modality-specific processing to extract meaningful features while addressing challenges of high dimensionality and data heterogeneity.
Imaging Data Processing: Medical images (CT, MRI, PET) undergo preprocessing including normalization, resampling, and registration. Subsequently, features are extracted through: (1) Radiomics: Automated extraction of quantitative features (texture, shape, intensity) from regions of interest using software platforms like PyRadiomics [56]; (2) Deep Learning Features: Convolutional Neural Networks (CNNs) or Vision Transformers (ViTs) automatically learn relevant feature representations from images [60] [57]. For example, ResNet architectures with skip connections effectively detect subtle abnormalities in complex imaging data like Digital Breast Tomosynthesis [60].
Genomic Data Processing: Genomic sequencing data requires specialized preprocessing pipelines: (1) Variant Calling: Identification of single nucleotide polymorphisms (SNPs) and other genetic variants from sequencing data; (2) Polygenic Risk Scores: Aggregation of multiple genetic variants into composite risk scores [55] [59]; (3) Gene Signature Development: Machine learning frameworks identifying optimal gene combinations predictive of outcomes, as demonstrated in breast cancer research where 117 ML combinations were evaluated to develop a post-translational modification gene signature [61].
Clinical Data Processing: EHR data contains both structured (laboratory values, demographics) and unstructured (clinical notes) information: (1) Structured Data Normalization: Continuous variables are scaled, categorical variables encoded; (2) Temporal Modeling: Sequential clinical data modeled using transformer architectures to capture dynamic risk trajectories [55] [57]; (3) Feature Selection: Techniques like mutual information, univariate analysis, or genetic algorithms identify clinically relevant predictors [56].
Machine Learning Approaches and Validation
The selection of ML architectures depends on data characteristics and fusion strategies, with rigorous validation essential for clinical translation.
Algorithm Selection: Studies employ diverse ML approaches: (1) Traditional ML: Random Forests, XGBoost, and SVM effectively handle tabular data from fused features [19] [18]; (2) Deep Learning: CNNs process imaging data, while transformers capture temporal dependencies in EHR data [60] [57]; (3) Ensemble Methods: Stacking multiple models or using AutoML frameworks often achieves superior performance, as demonstrated in breast cancer prediction where ensemble models reached 99.99% accuracy [18].
Validation Frameworks: Robust validation is critical for model credibility: (1) Internal Validation: Train-test splits with bootstrapping or k-fold cross-validation assess performance stability [58]; (2) External Validation: Testing on completely independent datasets from different institutions evaluates generalizability [62] [56]; (3) Performance Metrics: Area under the receiver operating characteristic curve (AUC/AUROC), C-index for survival models, calibration metrics, and reclassification statistics (NRI, IDI) provide comprehensive performance assessment [55] [62].
Recent studies highlight the importance of multi-site external validation. For example, an ML system predicting cancer-related symptoms demonstrated significant performance heterogeneity across 82 cancer centers (I² 46.4%-66.9%), underscoring the necessity of broad validation before clinical deployment [62].
Multimodal Data Fusion Experimental Workflow
Advanced Architectures and Emerging Approaches
Beyond conventional fusion techniques, several advanced AI architectures show significant promise for handling complex multimodal data in oncology research.
Transformer Networks
Originally developed for natural language processing, transformer architectures have been adapted for multimodal biomedical data due to their ability to process sequential information and capture long-range dependencies through self-attention mechanisms [57]. Transformers assign weighted importance to different components of input data, making them particularly effective for integrating free-text clinical notes, genomic sequences, and time-series EHR data [55] [57]. For example, in Alzheimer's disease diagnosis, a transformer framework integrating imaging, clinical, and genetic information achieved an exceptional AUC of 0.993 [57]. Transformers also enable temporal modeling of EHR data, capturing dynamic risk trajectories that static models cannot represent [55].
Graph Neural Networks (GNNs)
GNNs represent a groundbreaking approach for modeling non-Euclidean relationships inherent in multimodal healthcare data [57]. Unlike grid-based architectures, GNNs operate on graph-structured data where nodes represent entities (e.g., imaging features, genetic markers, clinical parameters) and edges represent their relationships [57]. This architecture explicitly models complex interactions between modalities rather than artificially appending features in tabular format. In oncologic applications, GNNs have been used to predict lymph node metastasis in esophageal squamous cell carcinoma by mapping learned embeddings across image features and clinical parameters into a graphical feature space [57]. Similarly, GNNs have demonstrated utility in predicting cancer patient survival using gene expression data [57].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Tools for Multimodal Data Fusion
| Tool/Category | Specific Examples | Function | Application Context |
|---|---|---|---|
| Data Processing Frameworks | Python Pandas, NumPy, Scikit-learn | Data cleaning, normalization, feature scaling | Foundation for all preprocessing pipelines |
| Radiomics Platforms | PyRadiomics, IBEX | Automated extraction of quantitative imaging features | Converting medical images to analyzable feature sets |
| Genomic Analysis Suites | GATK, PLINK, Polygenic Risk Score calculators | Variant calling, quality control, risk score calculation | Processing raw sequencing data into meaningful genetic features |
| Deep Learning Frameworks | TensorFlow, PyTorch, MONAI | Building CNN, transformer, and GNN architectures | Implementing complex fusion models and feature extraction |
| Multimodal Pipeline Libraries | AstraZeneca-AI Multimodal Pipeline [58] | Comprehensive framework for fusion experiments | Standardizing comparison of fusion strategies across modalities |
| Explainable AI Tools | SHAP, LIME, ELI5 | Interpreting model predictions and feature contributions | Validating model logic and establishing clinical trust |
| AutoML Platforms | H2O.ai, TPOT, Auto-SKlearn | Automated model selection and hyperparameter tuning | Streamlining optimization of complex multimodal pipelines |
Multimodal data fusion represents a paradigm shift in cancer detection research, moving beyond single-modality analysis to integrated approaches that more comprehensively capture disease complexity. The optimal fusion strategy depends critically on data characteristics: late fusion generally outperforms with high-dimensional omics data, while early and joint fusion excel when modalities have complementary features and similar dimensionalities [58] [56]. Emerging architectures like transformers and graph neural networks offer promising avenues for modeling complex cross-modal interactions that conventional approaches cannot capture [57].
Successful implementation requires rigorous validation across diverse patient cohorts to ensure generalizability and mitigate algorithmic bias [62]. As the field advances, the translation of these approaches to clinical practice will depend not only on technical performance but also on interpretability, robustness, and seamless integration into clinical workflows [55] [60]. By strategically selecting fusion approaches matched to data characteristics and clinical questions, researchers can develop more accurate, validated ML models that ultimately enhance cancer detection, prognosis, and treatment personalization.
In the high-stakes field of oncology, where diagnostic decisions directly impact patient survival and treatment outcomes, robust validation of machine learning (ML) models is not merely an academic exercise but a clinical imperative. The integration of artificial intelligence into cancer detection pipelines has demonstrated transformative potential, with deep learning applications revolutionizing diagnostic accuracy, speed, and accessibility across imaging modalities including mammography, digital breast tomosynthesis, ultrasound, and MRI [60]. However, this promise can only be realized through rigorous performance benchmarking that establishes transparent, comparable baselines using standardized evaluation metrics. Within cancer prediction research, where datasets often exhibit significant class imbalance—with actual positive cases (malignant findings) substantially outnumbered by negative cases (benign findings)—understanding the nuanced interpretation of accuracy, precision, recall, F1-score, and AUC-ROC becomes paramount [19] [63]. This comparison guide provides an objective framework for researchers, scientists, and drug development professionals to evaluate ML model performance within the specific context of cancer detection, enabling informed model selection and supporting the translational pathway from algorithmic development to clinical implementation.
Core Metric Definitions and Mathematical Foundations
The performance of binary classification models in cancer detection is quantified through metrics derived from four fundamental outcomes in a confusion matrix: True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN). Each evaluation metric emphasizes different aspects of model performance, with optimal metric selection dependent on the specific clinical context and relative costs of different error types [64].
Table 1: Fundamental Definitions for Binary Classification in Cancer Detection
| Term | Definition | Clinical Example in Cancer Detection |
|---|---|---|
| True Positive (TP) | Malignant cases correctly identified as malignant | A biopsy-confirmed malignant tumor correctly flagged by the model |
| False Positive (FP) | Benign cases incorrectly identified as malignant | A benign lesion mistakenly flagged as malignant, potentially leading to unnecessary biopsy |
| True Negative (TN) | Benign cases correctly identified as benign | A healthy patient correctly classified as cancer-free |
| False Negative (FN) | Malignant cases incorrectly identified as benign | A malignant tumor missed by the model, potentially delaying critical treatment |
Based on these fundamental outcomes, the primary metrics for model evaluation are calculated as follows [64] [65]:
- Accuracy = (TP + TN) / (TP + TN + FP + FN)
- Precision = TP / (TP + FP)
- Recall (Sensitivity) = TP / (TP + FN)
- F1-Score = 2 × (Precision × Recall) / (Precision + Recall)
The AUC-ROC (Area Under the Receiver Operating Characteristic Curve) represents the probability that a randomly chosen positive instance (malignant case) is ranked higher than a randomly chosen negative instance (benign case) [63]. The ROC curve itself plots the True Positive Rate (recall) against the False Positive Rate at various classification thresholds, providing a comprehensive view of model performance across all possible threshold choices [66].
Comparative Analysis of Evaluation Metrics
Metric Strengths, Weaknesses, and Clinical Applications
Each evaluation metric provides a distinct perspective on model performance, with trade-offs that must be carefully balanced against clinical requirements and the consequences of different error types in cancer detection.
Table 2: Metric Comparison for Cancer Detection Applications
| Metric | Optimal Use Case | Strengths | Weaknesses | Clinical Scenario |
|---|---|---|---|---|
| Accuracy | Balanced datasets where all error types have equal cost [64] | Intuitive interpretation; provides overall correctness measure [66] | Misleading with class imbalance; high accuracy possible with useless models [63] | Initial model assessment with balanced benign/malignant cases |
| Precision | When false positives are costly (e.g., avoiding unnecessary invasive procedures) [64] | Measures reliability of positive predictions; minimizes patient anxiety from false alarms | Does not account for false negatives; can be gamed by predicting few positives | Triage systems determining which patients require biopsy |
| Recall (Sensitivity) | When false negatives are dangerous (e.g., early cancer screening) [64] | Captures ability to identify all positive cases; critical for life-threatening conditions | Does not penalize false positives; can be gamed by predicting many positives | Population screening programs where missing cancer is unacceptable |
| F1-Score | Imbalanced datasets requiring balance between precision and recall [63] [65] | Harmonic mean balances both concerns; more informative than accuracy for imbalanced data | Obscures which metric (precision or recall) is weaker; single threshold | General cancer detection models where both false positives and false negatives matter |
| AUC-ROC | Comparing overall model performance across all thresholds [63] [66] | Threshold-independent; measures ranking capability rather than classification | Over-optimistic with imbalanced data; less interpretable for clinicians | Model selection phase comparing multiple algorithms |
Strategic Metric Selection Guidance
The choice of primary optimization metric should be driven by the specific clinical context and the relative consequences of different error types. For cancer detection applications, recall (sensitivity) often takes priority in initial screening contexts where missing a malignant case (false negative) could have fatal consequences [64]. As an example, in a study detecting breast cancer using machine learning, researchers prioritized recall because failing to identify malignant cases presents greater risk than false alarms, which could be resolved through further testing [19]. Conversely, in confirmation testing or triage systems where unnecessary invasive procedures (false positives) cause patient harm and increase healthcare costs, precision may become the primary metric of interest [64]. The F1-score provides a balanced perspective when both concerns are substantial, particularly valuable for imbalanced datasets common in cancer prediction [63]. While accuracy offers intuitive appeal for communicating with non-technical stakeholders, it should never be the sole metric for imbalanced cancer detection datasets, where a model that always predicts "benign" could achieve high accuracy while being clinically useless [64] [63].
Experimental Performance Benchmarking in Cancer Research
Performance Metrics in Recent Cancer Detection Studies
Recent research demonstrates the application of these metrics across various cancer types, with model performance varying significantly based on dataset characteristics, feature selection, and algorithm choice.
Table 3: Metric Performance in Recent Cancer Detection Research
| Study & Cancer Type | Best Performing Model | Accuracy | Precision | Recall | F1-Score | AUC-ROC |
|---|---|---|---|---|---|---|
| Breast Cancer Detection [19] | Random Forest | Not Reported | Not Reported | Not Reported | 84% | Not Reported |
| Breast Cancer Detection [19] | Stacked Ensemble | Not Reported | Not Reported | Not Reported | 83% | Not Reported |
| Cancer Risk Prediction [25] | CatBoost | 98.75% | Not Reported | Not Reported | 98.20% | Not Reported |
| Vision Transformers (ViTs) in Breast Cancer Imaging [60] | ViT (Histopathology) | 99.99% | Not Reported | Not Reported | Not Reported | Not Reported |
| Vision Transformers (ViTs) in Breast Cancer Imaging [60] | ViT (Medical Image Retrieval) | 98.9% (MAP) | Not Reported | Not Reported | Not Reported | Not Reported |
| Vision Transformers (ViTs) in Breast Cancer Imaging [60] | Wavelet-based ViT | Not Reported | Not Reported | Not Reported | Not Reported | High (Specific value not reported) |
Experimental Protocols and Methodologies
The performance benchmarks presented in Table 3 derive from rigorous experimental methodologies standardized across cancer detection research. For instance, the breast cancer detection study employing Random Forest and stacked ensemble models utilized the UCTH Breast Cancer Dataset from the University of Calabar Teaching Hospital, Nigeria, containing nine clinical features from 213 patients [19]. The experimental protocol involved comprehensive data preprocessing including handling of missing values, label encoding for categorical variables, and max-abs scaling to normalize features between -1 and 1 [19]. Feature selection employed both mutual information and Pearson's correlation to identify the most predictive variables, with involved nodes, tumor size, metastasis, and age emerging as highest correlated with diagnosis results [19].
Similarly, the cancer risk prediction study implementing CatBoost employed a structured dataset of 1,200 patient records with features including age, gender, BMI, smoking status, alcohol intake, physical activity, genetic risk level, and personal history of cancer [25]. The experimental methodology featured a complete ML pipeline with data exploration, preprocessing, feature scaling, and model evaluation using stratified cross-validation with a separate test set to ensure robust performance estimation [25]. This study compared nine supervised learning algorithms, with CatBoost achieving superior performance potentially due to its effective handling of categorical features and sophisticated gradient boosting implementation [25].
Visualization of Model Evaluation Workflows
Performance Benchmarking Workflow for Cancer Detection
The following diagram illustrates the standardized workflow for evaluating machine learning models in cancer detection research, from dataset preparation through metric selection and clinical interpretation:
Trade-offs in Metric Selection for Cancer Detection
This visualization illustrates the fundamental relationship between precision and recall and how the F1-score balances these competing objectives across different classification thresholds:
Implementation of robust performance benchmarking requires specific computational tools and methodological approaches. The following table details essential components of the experimental pipeline for validating ML models in cancer detection research.
Table 4: Essential Research Tools for Cancer Detection Model Validation
| Tool Category | Specific Examples | Function in Validation Pipeline |
|---|---|---|
| Programming Frameworks | Python, scikit-learn, TensorFlow, PyTorch [63] [66] | Provide metric calculation functions (accuracyscore, precisionscore, recallscore, f1score, rocaucscore) and model implementation |
| Validation Methodologies | Stratified k-fold Cross-Validation, Hold-out Test Sets [25] | Ensure reliable performance estimation, particularly crucial with imbalanced medical datasets |
| Explainability Tools | SHAP, LIME, ELI5, Anchor, QLattice [19] | Provide model interpretability and feature importance analysis, critical for clinical adoption and trust |
| Data Preprocessing Libraries | Scikit-learn preprocessing, Pandas, NumPy [19] [25] | Handle missing values, feature encoding, and data scaling to optimize model performance |
| Visualization Tools | Matplotlib, Seaborn, Graphviz [63] | Generate ROC curves, precision-recall curves, and other diagnostic plots for model evaluation |
| Statistical Analysis Tools | Jamovi, Scipy [19] | Conduct descriptive statistics, t-tests, and chi-square tests to validate feature significance |
Performance benchmarking using accuracy, precision, recall, F1-score, and AUC-ROC provides the foundational framework for validating machine learning models in cancer detection research. As demonstrated across recent studies, the selection of appropriate metrics must be driven by clinical context, with recall prioritized when false negatives present grave risks, precision emphasized when minimizing unnecessary procedures is critical, and F1-score providing a balanced perspective for imbalanced datasets [64] [19] [63]. The increasing integration of explainable AI (XAI) techniques, including SHAP, LIME, and ELI5, represents a crucial advancement for clinical translation, enabling researchers to interpret model predictions and validate feature importance against domain knowledge [19]. Future directions in the field point toward multimodal data integration, combining imaging, genomic, and clinical features for enhanced predictive accuracy, and the development of standardized benchmarking protocols that facilitate direct comparison across studies and institutions [60]. As deep learning architectures continue to evolve, with Vision Transformers and sophisticated ensemble methods demonstrating remarkable performance, rigorous metric-driven validation remains essential to ensure these technologies deliver safe, effective, and equitable cancer detection capabilities in clinical practice.
Overcoming Real-World Hurdles: Strategies for Optimizing Model Robustness and Generalizability
In the high-stakes field of oncology, the accuracy of machine learning (ML) models can directly impact patient survival rates. A model that performs flawlessly during training but fails in real-world clinical deployment represents more than a technical failure—it could lead to misdiagnosis and delayed treatment. This critical challenge, known as overfitting, occurs when models learn patterns specific to their training data rather than generalizable features that apply to new patient data [67]. The combat against overfitting is particularly crucial in cancer detection, where datasets are often limited, imbalanced, and heterogeneous [67] [68] [69].
The clinical implications of overfitting are profound. In breast cancer metastasis prediction, for instance, overfitting can obscure critical indicators that determine treatment plans, potentially leading to under- or over-treatment [67]. Similarly, in lung cancer detection from CT scans, where early diagnosis significantly improves survival rates, overfitting can reduce a model's ability to identify subtle malignant features [68]. This article provides a comprehensive comparison of two primary defensive strategies—K-fold cross-validation and data augmentation—evaluating their effectiveness across various cancer types and imaging modalities, with supporting experimental data to guide research implementation.
Understanding Overfitting in Cancer Detection
The Fundamental Challenge
Overfitting represents a fundamental paradox in medical machine learning: as models become more complex and capable, they also become more susceptible to learning dataset-specific noise rather than clinically relevant patterns [67]. In cancer diagnostics, this manifests when a model achieves high accuracy on its training data but demonstrates significantly reduced performance on unseen patient data, imaging from different institutions, or diverse demographic groups.
The consequences are particularly severe in oncology, where a model's generalization capability directly impacts diagnostic reliability. One empirical study on breast cancer metastasis prediction found that overfitting substantially weakened model generalization, ultimately reducing predictive accuracy on real-world clinical data [67]. This performance degradation directly affects clinical decision-making, potentially missing critical metastases or generating false positives that lead to unnecessary interventions.
Root Causes in Medical Imaging
Several factors unique to medical data contribute to overfitting in cancer detection:
- Limited dataset sizes: Curated, labeled medical imaging datasets are often small due to the expertise required for annotation and privacy concerns [68]. For rare cancers, this problem intensifies, forcing models to learn from few examples.
- Class imbalance: In many cancer detection scenarios, positive cases (malignant findings) are significantly outnumbered by negative cases (benign findings) [69]. This imbalance biases models toward the majority class.
- Dataset bias: Images collected from single institutions may share technical artifacts (scanning protocols, equipment) or demographic biases that models can exploit rather than learning true pathological features [70].
- High-dimensional data: Medical images contain thousands or millions of pixels, creating a high-dimensional feature space where models can easily find spurious correlations [67].
Table 1: Impact of Various Hyperparameters on Overfitting in Cancer Prediction Models
| Hyperparameter | Impact on Overfitting | Relationship with Performance | Recommendations for Cancer Data |
|---|---|---|---|
| Learning Rate | Higher values tend to reduce overfitting [67] | Moderate values optimal; too high harms both training and generalization [67] | Use moderate learning rates (0.01-0.1) with decay schedules [67] |
| Batch Size | Smaller batches increase overfitting [67] | Smaller batches often show better final performance despite overfitting risk [67] | Balance with computational resources; consider 32-128 for medical images [67] |
| L1/L2 Regularization | Both designed to reduce overfitting [67] | Excessive regularization harms performance; L2 generally more stable [67] | Use moderate L2 values; L1 for feature selection [67] |
| Dropout Rate | Higher rates reduce overfitting [67] | Too high degrades training performance [67] | 0.2-0.5 for convolutional layers; 0.5-0.8 for dense layers [67] |
| Number of Epochs | More epochs increase overfitting [67] | Performance peaks then declines on validation data [67] | Use early stopping with validation monitoring [67] |
K-Fold Cross-Validation: Methodology and Comparative Performance
Technical Foundations
K-fold cross-validation provides a robust framework for evaluating model generalization while mitigating the overfitting caused by limited data. The technique partitions available data into K complementary subsets (folds), performing K rounds of training and validation where each fold serves once as validation data and K-1 times as training data [70]. This process generates K performance estimates that better reflect true generalization error compared to single train-test splits.
For medical applications, this approach offers critical advantages. It maximizes utility of small datasets—a common challenge in cancer imaging—by ensuring every sample contributes to both training and validation. Additionally, the variance of performance estimates decreases as K increases, providing more reliable metrics for model selection [70]. The stability of these estimates is particularly valuable in clinical translation, where performance consistency directly impacts regulatory approval and clinical adoption.
Implementation Protocols
The standard implementation protocol for K-fold cross-validation in medical imaging involves:
- Stratification: Maintaining consistent class distributions across folds, preserving the proportion of malignant versus benign cases in each subset [70]. This is particularly crucial for imbalanced cancer datasets.
- Institutional separation: When multiple medical centers contribute data, keeping images from the same institution within the same fold prevents artificially inflated performance from learning institutional artifacts [70].
- Patient-level separation: Ensuring all images from the same patient reside in the same fold prevents data leakage that would overestimate performance [71].
A recent innovation combines K-fold cross-validation with Bayesian hyperparameter optimization, creating a more powerful approach for model development. In this enhanced protocol, the hyperparameter optimization process occurs within each fold, exploring different combinations of learning rates, dropout rates, and other regularization parameters specific to each training-validation split [70]. The final hyperparameters are selected based on best average performance across all folds.
Performance Comparison in Cancer Detection
Table 2: Performance Comparison of K-Fold Cross-Validation in Cancer Detection Studies
| Cancer Type | Imaging Modality | Base Model Accuracy | With K-fold CV | Additional Techniques | Reference |
|---|---|---|---|---|---|
| Land Cover/Land Use Classification | Remote Sensing | 94.19% | 96.33% | Bayesian Hyperparameter Optimization [70] | [70] |
| Canine Malignancies | Serum Biomarkers | Not Reported | AUC: 0.98, Sensitivity: 90%, Specificity: 97% | Gradient Boosting Model [71] | [71] |
| Breast Cancer Metastasis | Electronic Health Records | Varies with hyperparameters | Improved AUC with optimized hyperparameters | Feedforward Neural Networks [67] | [67] |
The performance improvements demonstrated in Table 2 highlight several important patterns. First, the combination of K-fold cross-validation with Bayesian optimization consistently enhances model accuracy across domains, from remote sensing to direct medical applications [70]. Second, the technique proves valuable across data types, from medical imagery to serum biomarkers [71]. Finally, the approach shows particular value with complex deep learning architectures where hyperparameter optimization is especially challenging [67].
Diagram 1: K-fold cross-validation workflow with hyperparameter optimization. This process ensures robust performance estimation while optimizing model parameters.
Data Augmentation: Techniques and Comparative Efficacy
Theoretical Basis
Data augmentation addresses overfitting at its root by artificially expanding training datasets, forcing models to learn invariant features rather than memorizing specific examples. For medical images, this involves creating plausible variations that maintain pathological truth while introducing diversity in appearance, orientation, and context [68]. Effective augmentation teaches models that a malignant lung nodule remains malignant regardless of its position, orientation, or minor appearance variations.
The mathematical foundation of data augmentation rests on the concept of invariance learning. By exposing models to transformed versions of training samples, the learning algorithm regularizes itself to develop decision boundaries that remain stable under these transformations [68]. This approach proves particularly valuable for deep learning architectures, which contain sufficient parameters to memorize training sets without seeing sufficient examples to generalize.
Advanced Augmentation Techniques for Medical Imaging
While basic transformations (rotation, flipping, scaling) provide value, medical imaging demands more sophisticated approaches:
Random Pixel Swap (RPS): A novel technique specifically designed for medical images that randomly swaps pixel regions within CT scans while maintaining pathological integrity [68]. Unlike methods that erase or alter critical regions, RPS preserves all diagnostic information by rearranging rather than removing content. The method operates across multiple directions—horizontal (RPSH), vertical (RPSW), and diagonal (RPSU, RPSD)—creating diverse transformations from single images [68].
Traditional transformations: Standard approaches including rotation (typically ±20°), width and height shifting (±20%), shearing (±20°), zooming (±20%), and horizontal flipping effectively expand dataset size [72]. These transformations mimic natural variations in imaging while preserving malignant characteristics.
Advanced alternatives: Methods like Cutout, Random Erasing, MixUp, and CutMix have shown promise in natural images but present limitations for medical contexts [68]. These techniques may remove critical diagnostic regions or blend features across patients, potentially confusing learning models with subtle pathological features [68].
Performance Comparison in Cancer Detection
Table 3: Performance Comparison of Data Augmentation Techniques in Cancer Detection
| Cancer Type | Model Architecture | Baseline Accuracy | With Augmentation | Augmentation Technique | Reference |
|---|---|---|---|---|---|
| Lung Cancer | ResNet, MobileNet, ViT, Swin Transformer | Not Reported | 97.56-97.78% | Random Pixel Swap (RPS) [68] | [68] |
| Lung Cancer | Multiple CNNs and Transformers | Lower than RPS results | 98.61% AUROC (IQ-OTH/NCCD) 99.46% AUROC (Chest CT) | Random Pixel Swap (RPS) [68] | [68] |
| Skin Cancer | MobileNetV2 | Imbalanced baseline | 98.48% Accuracy, 97.67% Precision, 100% Recall | Rotation, Shearing, Zooming, Flipping [72] | [72] |
| Multiple Cancers | DenseNet121 | Not Reported | 99.94% Validation Accuracy | Traditional Transformations [73] | [73] |
The performance gains in Table 3 demonstrate several important principles. First, specialized augmentation techniques like RPS outperform generic approaches for medical imagery, achieving exceptional accuracy and AUROC scores across multiple architectures [68]. Second, augmentation proves critical for addressing class imbalance, as demonstrated in skin cancer detection where balancing through augmentation enabled 100% recall for malignant cases [72]. Finally, the combination of augmentation with modern architectures (DenseNet, MobileNetV2) produces state-of-the-art results across cancer types [73] [72].
Diagram 2: Decision framework for selecting augmentation techniques in cancer detection. Medical imaging requires methods that preserve pathological truth.
Integrated Approaches: Combining K-Fold CV and Data Augmentation
Synergistic Implementation
The most effective defense against overfitting emerges from combining K-fold cross-validation with data augmentation in a coordinated framework. This integrated approach addresses both evaluation bias (through cross-validation) and training data limitations (through augmentation). The synergy occurs because augmentation expands the effective training size within each fold, while cross-validation ensures the augmented models undergo rigorous validation.
The implementation protocol follows this sequence:
- Initial data partitioning: Split data into K folds, maintaining stratification and institutional/patient separation [70].
- Fold-specific augmentation: For each training fold, apply appropriate augmentation techniques before model training [68] [72].
- Hyperparameter optimization: Conduct Bayesian optimization within each augmented training fold to identify optimal parameters [70].
- Validation: Evaluate each model on its corresponding non-augmented validation fold.
- Performance aggregation: Combine results across all folds for robust performance estimation [70].
This approach ensures that augmented images never leak into validation folds, maintaining the integrity of performance evaluation while maximizing training diversity.
Performance Gains in Cancer Research
Studies implementing combined approaches report superior performance compared to either technique alone. In land cover classification (a proxy for medical imaging challenges), the combination of K-fold cross-validation with Bayesian hyperparameter optimization achieved 96.33% accuracy, substantially outperforming models without cross-validation (94.19%) [70]. Similarly, in skin cancer detection, the integration of comprehensive augmentation with hyperparameter optimization via memetic algorithms produced 98.48% accuracy with perfectly balanced precision and recall [72].
These combined approaches prove particularly valuable for multi-cancer detection systems. Research evaluating seven cancer types (brain, oral, breast, kidney, leukemia, lung/colon, cervical) found that integrated regularization approaches enabled DenseNet121 to achieve 99.94% validation accuracy—near-perfect performance across diverse cancer types and imaging modalities [73].
Table 4: Essential Research Reagents and Computational Resources for Combatting Overfitting
| Resource Category | Specific Tools/Solutions | Function in Overfitting Prevention | Application Context |
|---|---|---|---|
| Cross-Validation Frameworks | Scikit-learn (Python), CARET (R) | Implements stratified K-fold validation with patient grouping | General model evaluation [70] |
| Data Augmentation Libraries | TensorFlow ImageDataGenerator, PyTorch Transforms | Applies transformations to expand training diversity | Medical image preprocessing [68] [72] |
| Hyperparameter Optimization | Bayesian Optimization, Memetic Algorithms | Finds optimal regularization parameters to balance fit and complexity | Model tuning [70] [72] |
| Specialized Augmentation | Random Pixel Swap (RPS) | Medical-specific augmentation preserving diagnostic regions | CT scan analysis [68] |
| Biomarker Assays | Canine TK1 ELISA, CRP ELISA | Provides serum biomarkers for multimodal validation | Veterinary cancer diagnostics [71] |
| Deep Learning Architectures | DenseNet121, MobileNetV2, ResNet | Modern architectures with built-in regularization properties | Multi-cancer detection [73] [72] |
The validation of machine learning models for cancer detection demands rigorous defenses against overfitting, with K-fold cross-validation and data augmentation representing two essential, complementary strategies. Cross-validation provides the methodological framework for reliable performance estimation, while data augmentation actively expands model generalization during training. The experimental evidence across multiple cancer types consistently demonstrates that integrated approaches—combining these techniques with appropriate hyperparameter optimization—deliver superior performance capable of clinical translation.
As cancer detection increasingly leverages artificial intelligence, the systematic implementation of these anti-overfitting strategies will determine whether research models successfully transition to clinical deployment. The techniques compared herein provide researchers with evidence-based approaches to build more reliable, generalizable models that maintain diagnostic accuracy across diverse patient populations and clinical settings—ultimately fulfilling AI's promise to enhance early cancer detection and improve patient outcomes.
In the field of cancer detection research, the phenomenon of class imbalance presents a significant challenge to the development of reliable machine learning models. Class imbalance occurs when the distribution of classes in a dataset is highly skewed, with one class (typically the "normal" or "non-cancerous" class) significantly outnumbering the other (the "cancerous" or "minority" class). This imbalance is particularly prevalent in medical diagnostics, where the number of healthy individuals vastly exceeds those with a specific disease [74]. For instance, in cancer detection datasets, the ratio of non-cancerous to cancerous samples can be extremely disproportionate, leading to models that exhibit high overall accuracy but fail to identify the critical minority class—the very cases that are of primary interest in medical diagnostics [74] [75].
The consequences of ignoring class imbalance in cancer detection are far-reaching and clinically significant. Conventional machine learning algorithms, when trained on imbalanced datasets, tend to develop a bias toward the majority class. In practice, this means that a model might achieve 95% accuracy by simply classifying all instances as "non-cancerous," while completely failing to identify actual cancer cases—a potentially catastrophic outcome in clinical settings [74] [76]. The gravity of this problem is underscored by the fact that the cost of misclassifying a diseased patient (false negative) in oncology far exceeds the cost of misclassifying a healthy individual (false positive), as the former can lead to delayed treatment and significantly worsened prognosis [74].
Addressing class imbalance is therefore not merely a technical exercise in model optimization but a crucial step toward developing clinically viable diagnostic systems. This guide provides a comprehensive comparison of contemporary methods for handling imbalanced datasets, with particular emphasis on their application, efficacy, and implementation in cancer detection research.
Understanding the Class Imbalance Problem in Medical Data
In medical datasets, particularly in oncology, class imbalance arises from multiple inherent characteristics of healthcare data and disease populations:
- Natural Disease Prevalence: Many cancers are inherently rare conditions, with incidence rates often as low as 1 per 100,000 in the population, creating a fundamental imbalance between positive (cancer) and negative (non-cancer) cases [74].
- Data Collection Biases: Certain demographic groups may be underrepresented in research datasets due to disparities in healthcare access, leading to sampling biases that exacerbate class imbalance [74].
- Longitudinal Study Limitations: Medical studies conducted over time often experience patient attrition (lost to follow-up), which can disproportionately affect certain classes and increase imbalance in the dataset [74].
- Data Privacy and Ethical Constraints: The sensitive nature of certain medical conditions can limit researcher access to positive cases, particularly for rare diseases, further contributing to imbalance [74].
The degree of imbalance is typically quantified using the Imbalance Ratio (IR), calculated as IR = Nmaj/Nmin, where Nmaj and Nmin represent the number of instances in the majority and minority classes, respectively. In medical datasets, this ratio can range from moderate (e.g., 4:1) to extreme (e.g., 100:1 or higher), posing significant challenges for model development [74].
Performance Metrics for Imbalanced Datasets
Traditional accuracy metrics are particularly misleading when evaluating models on imbalanced medical datasets, as they can mask poor performance on the critical minority class. The research community has established more informative evaluation metrics that prioritize minority class performance [77] [76]:
Table 1: Evaluation Metrics for Imbalanced Classification in Medical Diagnostics
| Metric | Formula | Clinical Interpretation |
|---|---|---|
| Precision | TP/(TP+FP) | Measures how many of the predicted cancer cases are actually cancerous (avoiding unnecessary procedures) |
| Recall (Sensitivity) | TP/(TP+FN) | Measures how many actual cancer cases are correctly identified (critical for early detection) |
| F1-Score | 2×(Precision×Recall)/(Precision+Recall) | Harmonic mean of precision and recall, balancing both concerns |
| AUC-PR | Area under Precision-Recall curve | More informative than ROC-AUC for imbalanced data; focuses on positive class performance |
| MCC (Matthews Correlation Coefficient) | (TP×TN - FP×FN)/√((TP+FP)(TP+FN)(TN+FP)(TN+FN)) | Comprehensive metric that considers all confusion matrix categories |
For cancer detection, recall (sensitivity) is often prioritized during early screening stages, as false negatives (missed cancer cases) have more severe consequences than false positives [78] [74]. However, the optimal balance between precision and recall depends on the specific clinical context and the relative costs of different error types.
Comprehensive Comparison of Methods for Imbalanced Data
Data-Level Approaches: Resampling Techniques
Data-level methods address class imbalance by altering the composition of the training dataset through various resampling strategies before model training [77] [74].
Oversampling Techniques increase the representation of the minority class by generating new instances:
- Random Oversampling: Duplicates existing minority class instances randomly until classes are balanced. While simple to implement, it can lead to overfitting as it replicates existing samples without adding new information [77].
- SMOTE (Synthetic Minority Oversampling Technique): Generates synthetic minority class samples by interpolating between existing minority instances in feature space. It selects a minority instance and its k-nearest neighbors (typically k=5), then creates new points along the line segments connecting them [78] [79].
- Advanced SMOTE Variants:
- Borderline-SMOTE: Focuses synthetic sample generation on minority instances near the class decision boundary, where misclassification is most likely [76].
- ADASYN (Adaptive Synthetic Sampling): Generates synthetic samples adaptively, with more samples created for minority examples that are harder to learn [76].
- SMOTE-ENC: An extension that handles both nominal and continuous features by encoding categorical variables based on their association with the minority class [79].
Undersampling Techniques reduce the number of majority class instances:
- Random Undersampling: Randomly removes majority class instances until balance is achieved. While computationally efficient, it risks discarding potentially valuable majority class information [78] [77].
- Tomek Links: Identifies and removes majority class instances that form "Tomek Links"—pairs of instances from different classes that are each other's nearest neighbors. This helps clean the decision boundary between classes [77] [76].
- Edited Nearest Neighbors (ENN): Removes majority class samples that are misclassified by their k-nearest neighbors, effectively eliminating noisy and borderline majority instances [77].
Hybrid Approaches combine both oversampling and undersampling:
- SMOTE-Tomek: Applies SMOTE to generate synthetic minority samples, then uses Tomek Links to remove ambiguous instances from both classes [80].
- SMOTE-ENN: Combines SMOTE oversampling with ENN cleaning to generate a balanced dataset with well-defined class clusters [77] [81].
Algorithm-Level Approaches: Model-Centric Solutions
Algorithm-level methods modify the learning process itself to make models more sensitive to minority classes without altering the training data distribution [77] [74].
Cost-Sensitive Learning incorporates misclassification costs directly into the model training process:
- Class Weights: Assigns higher weights to minority class instances in the loss function, increasing the penalty for misclassifying minority samples. This approach is widely supported in machine learning libraries like scikit-learn, XGBoost, and LightGBM [76].
- Cost Matrix: Uses a predefined cost matrix that specifies different misclassification costs for different types of errors, typically assigning higher costs to false negatives (missed cancer cases) [74].
Specialized Loss Functions modify the optimization objective to focus on hard-to-classify examples:
- Focal Loss: Adapts standard cross-entropy loss by down-weighting easy examples and focusing training on hard negatives. The loss function is defined as FL(pt) = -αt(1-pt)^γ log(pt), where pt is the model's estimated probability, αt balances class importance, and γ focuses learning on hard examples [77] [81] [82].
- Label-Distribution-Aware Margin (LDAM) Loss: Encourages larger classification margins for minority classes by incorporating class-frequency information directly into the loss function [81].
Ensemble Methods combine multiple models to improve overall performance on imbalanced data:
- Balanced Random Forest: Adapts the Random Forest algorithm to use balanced bootstrap samples for each tree, ensuring better minority class representation [83] [76].
- EasyEnsemble: Trains multiple classifiers on different balanced subsets of the data (created via undersampling) and aggregates their predictions [83] [76].
- RUSBoost: Combines random undersampling with boosting algorithms, sequentially training models that focus on previously misclassified examples [77].
- Routine Implementation in Cancer Research: Studies have successfully implemented these techniques, with one analysis of five cancer datasets finding that Balanced Random Forest and XGBoost showed particularly strong performance [75].
Emerging Adaptive and Hybrid Methods
Recent research has introduced more dynamic approaches that adapt to changing class difficulties during training:
- ART (Adaptive Resampling-based Training): Periodically updates the training data distribution based on class-wise performance metrics (e.g., macro F1-score), allowing the model to incrementally shift attention toward underperforming classes [81].
- HSMOTE-EDDCM (Hybrid SMOTE with Ensemble Deep Dynamic Classifier Model): Combines density-aware synthetic sample generation with dynamic ensemble strategies that adapt to evolving data distributions, particularly effective for big data analytics in healthcare [80].
- IADASYN-FLCatBoost: Integrates improved ADASYN oversampling (with outlier detection) with Focal Loss-enhanced CatBoost, demonstrating strong performance in handling complex imbalanced scenarios [82].
Experimental Comparison and Performance Analysis
Experimental Protocols and Dataset Characteristics
To objectively compare the performance of various imbalance handling methods, researchers have conducted extensive experiments across multiple cancer datasets. The following table summarizes key datasets and their imbalance characteristics used in these comparative studies:
Table 2: Cancer Dataset Characteristics in Imbalance Learning Studies
| Dataset | Cancer Type | Total Samples | Minority Class | Imbalance Ratio | Features |
|---|---|---|---|---|---|
| TCGA-LIHC [78] | Liver Cancer | 403 | 39 normal samples | 9.3:1 | RNA seq, CNV, DNA methylation |
| TCGA-BRCA [78] | Breast Cancer | 841 | 65 normal samples | 11.9:1 | RNA seq, CNV, DNA methylation |
| TCGA-COAD [78] | Colon Adenocarcinoma | 295 | 19 normal samples | 14.5:1 | RNA seq, CNV, DNA methylation |
| WBCD [75] | Breast Cancer | 699 | 241 malignant tumors | 1.9:1 | Clinical and cytological features |
| Lung Cancer Detection [75] | Lung Cancer | 309 | 39 non-cancer cases | 6.9:1 | Demographic and clinical variables |
A typical experimental protocol for comparing imbalance handling methods includes the following steps [78] [75]:
- Data Preprocessing: Handling missing values, normalization, and feature scaling as appropriate for the specific dataset.
- Dimensionality Reduction: Applying techniques like Principal Component Analysis (PCA) to address the curse of dimensionality common in omics data (e.g., reducing from ~54,000 features to a few hundred principal components) [78].
- Resampling Implementation: Applying various resampling techniques exclusively to the training set to prevent data leakage.
- Model Training: Training multiple classifier types using cross-validation (typically 10-fold) to ensure robust performance estimation.
- Performance Evaluation: Assessing models using multiple metrics (precision, recall, F1-score, AUC-PR) with particular emphasis on minority class performance.
Comparative Performance Analysis
Comprehensive experimental studies provide valuable insights into the relative performance of different imbalance handling methods across various cancer datasets:
Table 3: Performance Comparison of Resampling Methods on Cancer Datasets
| Method | Average Performance | Best Performing Context | Key Limitations |
|---|---|---|---|
| SMOTEENN [75] | 98.19% (Accuracy) | Multiple cancer diagnosis datasets | Computational complexity with large datasets |
| IHT (Instance Hardness Threshold) [75] | 97.20% (Accuracy) | Prognostic cancer datasets | May remove informative majority samples |
| RENN [75] | 96.48% (Accuracy) | Breast cancer detection | Sensitive to noise in data |
| SMOTE-Tomek [75] | 95.92% (Accuracy) | Mixed-type feature datasets | May not handle severe imbalance effectively |
| Random Undersampling [78] | 94.10% (Accuracy) | High-dimensional omics data | Loss of potentially useful majority information |
| SMOTE [78] | 96.50% (Accuracy) | Liver and breast cancer omics data | Can generate noisy samples in high-dimension spaces |
| No Resampling (Baseline) [75] | 91.33% (Accuracy) | (Reference only) | Severe bias toward majority class |
When examining classifier performance in conjunction with resampling techniques, studies have found:
Table 4: Classifier Performance with Resampling on Cancer Data
| Classifier | Best Performing With | Reported Performance | Dataset |
|---|---|---|---|
| Random Forest [75] | SMOTEENN | 94.69% (Mean Accuracy) | Multiple cancer datasets |
| Balanced Random Forest [75] | (Built-in balancing) | 93.84% (Mean Accuracy) | Multiple cancer datasets |
| XGBoost [75] | SMOTE-Tomek | 93.22% (Mean Accuracy) | Multiple cancer datasets |
| SVM with SGD [78] | SMOTE | >99% Accuracy, AUC ≥0.999 | Liver and breast cancer |
| CatBoost with Focal Loss [82] | IADASYN | 0.912 (F1-Score) | Credit card churn (method applicable to medical data) |
Recent evidence suggests that the effectiveness of resampling methods varies significantly based on the classifier type and dataset characteristics. One systematic study found that while SMOTE and random oversampling showed improvements for "weak" learners (e.g., decision trees, SVM), they provided minimal benefits for "strong" classifiers like XGBoost and CatBoost when combined with appropriate probability threshold tuning [83].
Workflow Visualization
The following diagram illustrates a comprehensive workflow for addressing class imbalance in cancer detection research, integrating both data-level and algorithm-level approaches:
Imbalance Handling Methods Workflow
The Scientist's Toolkit: Research Reagent Solutions
Implementing effective solutions for class imbalance requires both conceptual understanding and practical tools. The following table summarizes key resources and their applications in addressing imbalance in cancer detection research:
Table 5: Essential Tools for Handling Class Imbalance in Cancer Research
| Tool/Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| Imbalanced-Learn [83] | Python Library | Provides implementation of oversampling, undersampling, and hybrid methods | Data preprocessing for scikit-learn compatible workflows |
| Class Weight Parameters [76] | Algorithm Parameter | Built-in class balancing in classifiers like SVM, Random Forest | Quick implementation of cost-sensitive learning without data modification |
| Focal Loss Implementation [82] | Custom Loss Function | Focuses training on hard examples in neural networks | Deep learning applications with extreme class imbalance |
| XGBoost/LightGBM [83] | Ensemble Algorithm | Advanced gradient boosting with scaleposweight parameter | Handling imbalance while maintaining high performance on tabular medical data |
| TCGA Data Portal [78] | Data Repository | Source of multi-omics cancer datasets with inherent imbalance | Access to real-world imbalanced cancer datasets for method validation |
| SHAP/LIME | Interpretability Tools | Explains model predictions and identifies feature importance | Understanding how imbalance handling affects model decision processes |
The validation of machine learning models in cancer detection research necessitates robust strategies for addressing class imbalance. Through comparative analysis, several key insights emerge:
First, the performance of different imbalance handling methods is highly context-dependent. No single approach universally outperforms others across all cancer types, datasets, and model architectures. However, hybrid methods like SMOTEENN have demonstrated consistently strong performance across multiple cancer domains, achieving the highest mean accuracy (98.19%) in comprehensive evaluations [75].
Second, the choice between data-level and algorithm-level approaches should be informed by dataset characteristics and clinical requirements. For high-dimensional omics data, algorithm-level methods like cost-sensitive learning often provide more practical solutions, while for smaller clinical datasets with moderate imbalance, resampling techniques can yield significant improvements [78] [83].
Third, proper evaluation metrics are crucial for meaningful model comparison in cancer detection contexts. Metrics like AUC-PR, F1-score, and recall provide more clinically relevant performance measures than traditional accuracy, particularly for the early detection scenarios where identifying true positives (cancer cases) is paramount [74] [76].
Future research directions should focus on developing more adaptive methods like ART that dynamically adjust to class-wise performance during training [81], integrating domain knowledge into synthetic sample generation for medical data, and establishing standardized benchmarking protocols specific to medical applications. As machine learning continues to transform cancer detection, addressing the fundamental challenge of class imbalance will remain essential for developing clinically viable, equitable, and reliable diagnostic systems.
The integration of artificial intelligence (AI) into oncology represents a paradigm shift in cancer detection and diagnosis. However, the transition from experimental algorithms to clinically viable tools is fraught with a fundamental challenge: ensuring that models performing excellently on development data maintain their accuracy in diverse, real-world clinical settings. This discrepancy often stems from domain shift, where models encounter data in practice that differs from their training data in aspects such as patient populations, imaging devices, and acquisition protocols [84]. Consequently, a model's performance can significantly degrade when faced with this variability, leading to unreliable predictions and potential clinical risks.
Robust validation strategies, particularly through multi-center studies and external validation, have emerged as the scientific community's response to this challenge. These methodologies rigorously test a model's ability to generalize beyond the narrow confines of its training data. This guide objectively compares the performance of AI models developed and validated using these critical approaches, providing researchers and drug development professionals with the experimental data and methodological frameworks necessary to evaluate and build trustworthy AI tools for oncology.
Performance Comparison: Single-Center vs. Multi-Center External Validation
The following tables synthesize quantitative evidence from recent studies, comparing model performance on internal versus external datasets and highlighting the consistency of multi-center, externally validated models.
Table 1: Performance Comparison of AI Models in Internal vs. External Validation Sets
| Cancer Type / Application | Model Architecture | Internal Validation Performance | External Validation Performance | Key Metric |
|---|---|---|---|---|
| Clear Cell Renal Cell Carcinoma (ccRCC) Staging [85] | 3D Transformer-ResNet (TR-Net) | Training set: AUC 0.939 (micro) | External Set 1: AUC 0.939 (micro); External Set 2: AUC 0.954 (micro) | Micro-AUC |
| Multi-Cancer Early Detection (OncoSeek) [86] | AI-empowered protein marker analysis | Previously published cohorts: AUCs 0.826, 0.744, 0.819 | Four new cohorts: AUCs 0.883, 0.912, 0.822, 0.825 | AUC |
| Ovarian Cancer Detection from Ultrasound [84] | Transformer-based Neural Network | Leave-one-center-out cross-validation | Performance consistently superior to human experts across 19 centers | F1 Score: 83.50% |
Table 2: Detailed Performance Metrics of Externally Validated Models
| Study Description | Sensitivity | Specificity | Accuracy / Other Metrics | Notes |
|---|---|---|---|---|
| OncoSeek (All Cohorts, n=15,122) [86] | 58.4% (56.6-60.1%) | 92.0% (91.5-92.5%) | Overall Accuracy: 70.6% | Detects 14 cancer types; TOO prediction accuracy: 70.6% for true positives. |
| ccRCC T-Staging Model [85] | - | - | External Set 1 ACC: 0.843; External Set 2 ACC: 0.869 | Performance was moderate for advanced subclasses (T3+T4). |
| AI vs. Human Experts in Ovarian Cancer [84] | 89.31% (vs. Expert 82.40%) | 88.83% (vs. Expert 82.67%) | F1 Score: 83.50% (vs. Expert 79.50%) | AI reduced false negative rates by 39.27% and false positive rates by 35.53% versus experts. |
The data consistently demonstrates that models subjected to multi-center external validation not only maintain robust performance but also establish a verifiable and trustworthy profile of their strengths and limitations across diverse clinical environments.
Experimental Protocols for Rigorous External Validation
Multi-Center Data Collection and Preprocessing
A foundational protocol for ensuring generalizability involves collecting data from multiple, independent clinical centers. The study on clear cell renal cell carcinoma (ccRCC) provides a exemplary methodology [85].
- Patient Cohort and Inclusion Criteria: Data was retrospectively collected from 1,148 ccRCC patients across five medical centers. Inclusion criteria comprised surgical treatment, postoperative pathological confirmation of ccRCC, and contrast-enhanced CT scans conducted within thirty days prior to surgery. This ensures data relevance and clinical applicability.
- Data Partitioning Strategy: Data from two centers were merged and randomly split into a training set (80%) and an internal testing set (20%). Data from two additional centers formed External Validation Set 1, and data from a fifth, independent center constituted External Validation Set 2. This tiered approach tests generalizability across progressively distant data distributions.
- Image Preprocessing and Standardization: To handle variability from multiple centers, tumor Regions of Interest (ROIs) were manually delineated on corticomedullary phase CT images slice-by-slice by junior radiologists, with a senior radiologist resolving discrepancies. Data blocks of size 128x128x64 were extracted from the center of the tumor ROI outward to preserve morphological and textural information without resizing distortion [85].
Leave-One-Center-Out Cross-Validation
For international studies with numerous centers, Leave-One-Center-Out Cross-Validation (LOCO-CV) provides a robust validation protocol, as utilized in the international ovarian cancer study [84].
- Model Training and Testing Cycle: The dataset comprised 17,119 ultrasound images from 3,652 patients across 20 centers in eight countries. In this scheme, iteratively, each center is isolated as the test set once, while the model is trained on the combined data from the remaining 19 centers.
- Performance Aggregation: This process is repeated until every center has served as the independent test set. The performance metrics (e.g., F1 score, sensitivity, specificity) from all these iterations are aggregated to produce a final estimate of the model's ability to generalize to completely unseen clinical environments [84].
- Benchmarking Against Human Performance: The study collected 51,179 assessments from 66 expert and non-expert examiners on the same cases, providing a direct, clinically meaningful benchmark for the AI's performance [84].
Clinical Utility Assessment: Human-Machine Collaboration
The ultimate test of a model's value is its ability to positively impact clinical workflows. A critical protocol involves human-machine collaboration experiments [85] [87].
- Experimental Setup: Clinicians, typically radiologists or oncologists, first assess cases without AI assistance, providing their diagnostic decisions and confidence levels.
- AI-Assisted Assessment: In a subsequent session, the same clinicians re-evaluate the cases with the predictions and supporting evidence (e.g., Grad-CAM heatmaps) from the AI model.
- Outcome Measurement: The primary outcome is the improvement in diagnostic accuracy, sensitivity, and specificity with AI assistance compared to the unaided baseline. The ccRCC staging study reported that such collaboration "demonstrated improved diagnostic accuracy with model assistance," highlighting its practical utility [85]. A scoping review of oncology AI algorithms further confirmed that these tools "improved clinician performance with AI assistance" [87].
Visualization of Validation Workflows and Concepts
Multi-Center Validation Data Flow
The following diagram illustrates the flow of data from multiple independent clinical centers through the model development and validation process, which is crucial for assessing generalizability.
LOCO-CV Process for Generalizability
Leave-One-Center-Out Cross-Validation (LOCO-CV) is a powerful technique for maximizing the use of multi-center data while rigorously testing generalizability.
Building and validating generalizable AI models for cancer detection requires a suite of methodological tools and resources. The following table details key solutions and their functions based on successful implementations in the cited research.
Table 3: Research Reagent Solutions for Robust AI Validation
| Category / Solution | Specific Examples from Research | Function & Role in Validation |
|---|---|---|
| Deep Learning Architectures | 3D Transformer-ResNet (TR-Net) [85], Transformer-based CNNs [84] | Combines local feature extraction (CNN) with global context understanding (Transformer) for analyzing complex medical images like CT scans and ultrasounds. |
| Interpretability & Explainability Tools | Gradient-weighted Class Activation Mapping (Grad-CAM) [85] | Generates visual "heatmaps" highlighting image regions most influential in the model's decision, building clinical trust and enabling error analysis. |
| Model Validation Frameworks & Libraries | Scikit-learn, TensorFlow, PyTorch [88] [89] | Provide standardized implementations of critical validation techniques like cross-validation, bootstrapping, and performance metric calculation. |
| Data Sourcing & Curation | Multi-center, international collaborations [85] [86] [84] | Provides diverse, clinically representative datasets essential for rigorous external validation and testing model generalizability across populations and equipment. |
| Performance Benchmarking | Comparisons against human expert performance [84] | Establishes a clinically relevant benchmark, demonstrating whether AI can meet or exceed the current standard of care and defining its practical utility. |
The evidence from recent, large-scale studies in oncology AI is unequivocal: rigorous validation through multi-center datasets and external testing is not merely an academic exercise but a critical prerequisite for clinical applicability. Models developed in this paradigm, such as those for renal cell carcinoma staging, multi-cancer early detection, and ovarian cancer diagnosis, demonstrate robust performance across diverse populations and clinical settings, outperforming single-center models in generalizability and clinical readiness.
For researchers and drug development professionals, the path forward is clear. Adopting the structured experimental protocols, visualization workflows, and research toolkit outlined in this guide is essential. By prioritizing generalizability from the outset, the field can accelerate the transition of promising AI research from the laboratory to the clinic, ultimately fulfilling the promise of precision oncology and improving patient outcomes worldwide.
The integration of Artificial Intelligence (AI) into oncology has marked a transformative era in cancer care, enhancing capabilities from early detection to personalized treatment planning. However, the "black-box" nature of complex AI models, particularly deep learning systems, remains a significant barrier to their widespread clinical adoption [90] [91]. Explainable AI (XAI) has emerged as a critical field addressing this transparency gap by developing methods that make AI decision-making processes understandable and trustworthy to human users [90]. In high-stakes domains like oncology, where decisions directly impact patient survival and quality of life, clinicians require more than just predictive outputs—they need insights into the reasoning behind these predictions to verify their validity, align them with clinical knowledge, and integrate them safely into patient care pathways [92] [93]. This review systematically compares leading XAI methodologies, their performance characteristics across various oncology applications, and implementation frameworks designed to bridge the gap between algorithmic performance and clinical interpretability.
Comparative Analysis of XAI Techniques in Oncology
XAI techniques can be broadly categorized into model-specific and model-agnostic approaches, each with distinct operational characteristics, advantages, and limitations for oncology applications.
Table 1: Comparison of Major XAI Techniques in Oncology Applications
| XAI Technique | Category | Mechanism | Common Oncology Applications | Strengths | Limitations |
|---|---|---|---|---|---|
| SHAP | Model-agnostic, post-hoc | Computes feature importance using cooperative game theory | Risk stratification, biomarker discovery [90] [94] | Provides unified, consistent feature attribution; handles complex feature interactions | Computationally intensive for large datasets; approximate versions may be needed |
| LIME | Model-agnostic, post-hoc | Creates local surrogate models to explain individual predictions | Treatment outcome prediction [90] | Intuitive local explanations; model-agnostic flexibility | Instability across different samples; surrogate model fidelity issues |
| Grad-CAM | Model-specific, post-hoc | Generates heatmaps using gradient information from CNN layers | Medical imaging (radiology, histopathology) [90] [95] | Visual, intuitive localization; requires no architectural changes | Limited to CNN architectures; lower resolution than original image |
| Attention Mechanisms | Model-specific, intrinsic | Learns to weight important regions or features during prediction | Genomic sequencing, report analysis [90] | Built-in interpretability; no separate explanation model needed | May not reflect true reasoning process; "fake explainability" risk |
| Decision Trees | Intrinsically interpretable | Creates hierarchical decision rules based on feature thresholds | Clinical decision support systems [94] | Fully transparent reasoning; clinically aligned decision pathways | Limited complexity; potential overfitting without careful tuning |
| Prototype-based | Model-specific, intrinsic | Compares input to learned prototypical cases [96] | Medical imaging (e.g., gestational age estimation) [96] | Case-based reasoning mirrors clinical thinking; intuitive similarities | Limited to training data coverage; prototype learning challenges |
The selection of appropriate XAI methods depends heavily on the specific clinical context, data modality, and user needs. For imaging-intensive specialties like radiology and pathology, visual explanation methods such as Grad-CAM and attention mechanisms have demonstrated particular utility by highlighting anatomically relevant regions corresponding to model predictions [90] [95]. Conversely, for clinical decision support systems leveraging electronic health record data, feature attribution methods like SHAP and intrinsically interpretable models like decision trees provide transparent reasoning that aligns with clinical thought processes [90] [94].
Performance Comparison of XAI-Enabled Systems in Oncology
Rigorous evaluation of XAI systems requires assessing both predictive performance and explanation quality across diverse oncology domains.
Table 2: Performance Metrics of XAI Systems in Cancer Detection and Diagnosis
| Application Domain | XAI Technique | Dataset | Key Performance Metrics | Comparative Performance |
|---|---|---|---|---|
| Melanoma Detection | Grad-CAM with DenseNet121 (SmartSkin-XAI) [95] | ISIC, Kaggle dataset | Accuracy: 97-98%Precision: HighRecall: HighF1-Score: High | Outperformed benchmark models (DenseNet121, InceptionV3, ResNet50) |
| Breast Cancer Malignancy Classification | Decision Tree with SHAP analysis [94] | Kaggle breast cancer dataset (213 patients) | Accuracy: 91.7%Sensitivity: 90.1-92.8%F1-Score: 90.1-92.8%MCC: 83.1% | Matched ensemble method performance with higher interpretability |
| Gestational Age Estimation | Prototype-based XAI [96] | Fetus ultrasound dataset | MAE: 14.3 days (with explanations) vs 15.7 days (predictions only) vs 23.5 days (baseline) | Explanations provided non-significant additional improvement over predictions alone |
| Radiomics for Cancer Imaging | SHAP, LIME, Grad-CAM [90] [97] | Multimodal imaging datasets | Variable across studies; some show improved clinician performance with explanations | Dependent on clinical context and user characteristics; no consistent superiority |
Beyond quantitative metrics, human factor evaluations reveal crucial insights into XAI effectiveness. A reader study on gestational age estimation demonstrated that while model predictions significantly reduced clinician mean absolute error (from 23.5 to 15.7 days), the addition of explanations produced variable effects across participants, with some clinicians performing worse with explanations than without them [96]. This highlights the importance of considering individual differences in clinician interaction with XAI systems and the potential need for personalized explanation formats.
Experimental Protocols and Methodologies
Protocol for Imaging-Based Cancer Detection with XAI
The experimental protocol for developing and validating the SmartSkin-XAI system for melanoma detection exemplifies a rigorous approach for imaging applications [95]:
Data Preprocessing and Augmentation: The ISIC and Kaggle dermatoscopy image datasets underwent rigorous preprocessing, including resizing to uniform dimensions, normalization of pixel values, and data augmentation techniques (rotation, flipping, scaling) to enhance model robustness and address class imbalance.
Model Architecture and Training: A DenseNet121 architecture was fine-tuned using transfer learning. The model was trained with a categorical cross-entropy loss function and optimized using adaptive moment estimation (Adam) with a carefully tuned learning rate schedule. Ten-fold cross-validation was employed to ensure generalizability.
XAI Integration and Visualization: Gradient-weighted Class Activation Mapping (Grad-CAM) was implemented to generate visual explanations. This technique utilizes the gradients of the target concept flowing into the final convolutional layer to produce a coarse localization map highlighting important regions in the image for predicting the specific class.
Validation and Evaluation: The model was evaluated on a held-out test set using multiple metrics (accuracy, precision, recall, F1-score). Explanations were qualitatively assessed by domain experts for clinical plausibility and alignment with known dermatological features.
Protocol for Clinical Decision Support with XAI
For non-imaging applications using clinical and demographic features, the breast cancer malignancy detection study demonstrates a structured protocol [94]:
Feature Engineering and Selection: Clinical variables (tumor size, lymph node status, metastasis, age, menopausal status) were carefully selected based on clinical relevance. Categorical variables were encoded using label encoding (for ordinal variables) or one-hot encoding (for nominal variables).
Model Selection and Training: Eight machine learning algorithms (decision trees, discriminant analysis, logistic regression, SVM, Naive Bayes, K-NN, ensemble methods, ANN) were systematically compared using ten-fold cross-validation. Hyperparameter optimization was performed via Bayesian optimization to enhance performance while avoiding overfitting.
Explainability Implementation: Two complementary explainability approaches were implemented: (1) visualization of the decision tree structure to present transparent decision rules, and (2) SHAP analysis to quantitatively evaluate each variable's contribution to model predictions.
Performance Assessment and Validation: Models were evaluated using comprehensive metrics including accuracy, sensitivity, specificity, F1 score, AUC, and Matthews Correlation Coefficient (MCC). The hold-out test set (10% of data) provided final performance evaluation.
Visualization of XAI Logical Frameworks
Understanding the logical relationships between different XAI approaches and their clinical integration pathways is essential for effective implementation.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing and evaluating XAI systems in oncology requires specialized computational tools, frameworks, and datasets.
Table 3: Essential Research Toolkit for XAI in Oncology
| Tool/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| XAI Python Libraries | Captum [93], Alibi Explain [93], Quantus [93] | Model interpretation and explanation generation | General XAI implementation for various model architectures |
| Model Development Frameworks | TensorFlow, PyTorch, scikit-learn | Building and training machine learning models | Developing base models requiring explanation |
| Medical Imaging Datasets | ISIC (skin lesions) [95], institutional radiology/pathology repositories | Benchmarking and validation | Training and testing XAI systems for image-based diagnosis |
| Clinical Data Repositories | Public cancer registries, EHR datasets (e.g., Kaggle breast cancer dataset) [94] | Model development with clinical variables | Non-imaging decision support system development |
| Visualization Tools | Matplotlib, Seaborn, Plotly | Explanation visualization and result reporting | Creating clinician-friendly explanation interfaces |
| Evaluation Metrics | Faithfulness, sparsity, simulatability [96] | Quantitative assessment of explanation quality | Systematic evaluation of XAI method performance |
The selection of appropriate tools depends on the specific research objectives and clinical context. For medical imaging applications, frameworks with built-in visualization capabilities like Grad-CAM implementation in TensorFlow or PyTorch are particularly valuable [95]. For clinical decision support systems leveraging electronic health record data, libraries like SHAP and LIME that provide feature importance rankings offer more relevant insights [90] [94].
The implementation of Explainable AI in oncology represents a critical pathway toward clinically trustworthy and deployable AI systems. Current evidence demonstrates that XAI techniques can provide meaningful explanations without necessarily compromising predictive performance, as shown by systems achieving 91-98% accuracy while maintaining interpretability [95] [94]. However, significant challenges remain, including the development of standardized evaluation frameworks, creation of context- and user-dependent explanations, and validation of clinical utility through human-in-the-loop studies [96] [93].
Future progress in XAI for oncology will likely focus on three key areas: (1) advancing multimodal XAI approaches that integrate imaging, clinical, and genomic data into unified explanations [93] [97]; (2) developing interactive explanation systems that support genuine dialogue between clinicians and AI systems [93]; and (3) establishing rigorous validation protocols that assess both technical adequacy and clinical usefulness across diverse healthcare settings [90] [96]. As these developments mature, XAI-powered systems have the potential to transform oncology practice by augmenting clinical expertise with transparent, evidence-based AI insights tailored to individual patient characteristics and needs.
Federated Learning (FL) represents a paradigm shift in machine learning, moving away from traditional centralized data collection towards a decentralized, privacy-preserving model. In classical machine learning, data is aggregated from various sources—such as phones, cars, laptops, and medical devices—onto a central server for model training [98]. While effective, this approach raises significant privacy concerns, as sensitive data must be shared and stored centrally, creating risks of leakage or misuse [99].
FL addresses this fundamental privacy challenge by reversing the data-flow logic. Instead of bringing data to the model, FL brings the model to the data [98]. The core process involves a central server that initializes a global model and distributes it to participating client devices or institutions. Each client trains the model locally using its own private data. Only the model updates (e.g., weights or gradients) are sent back to the server, where they are aggregated to create an improved global model. This process repeats iteratively until the model converges [98]. By keeping raw data localized, FL enables collaborative model development without direct data sharing, making it particularly valuable for sensitive domains like healthcare, where patient data is governed by strict privacy regulations [100] [101].
Federated Learning in Cancer Detection: Performance Evaluation
The application of FL in cancer detection has demonstrated remarkable performance across various imaging modalities, often rivaling or even exceeding traditional centralized learning approaches while maintaining strict data privacy. The following table summarizes key quantitative results from recent studies applying FL to different cancer diagnostic tasks.
Table 1: Performance of Federated Learning Models in Cancer Detection Applications
| Cancer Type | Imaging Modality | FL Framework | Model Architecture | Performance Metrics | Centralized Comparison |
|---|---|---|---|---|---|
| Breast Cancer [102] | 3D Mammography | FedAvg | CNN | Accuracy: 97.37% | Centralized CNN: 97.30% |
| Breast Cancer [102] | 3D Mammography | FedAvg | Transfer Learning (VGG16, VGG19, ResNet50) | Accuracy: 48.83%-89.24% | Lower than centralized |
| Skin Cancer [100] | Dermoscopic Images | FedAvg | VGG19 | Accuracy: High classification performance (specific metrics not provided) | Comparable to centralized training |
| General Cancer [103] | Medical Imaging | FL with LightGBM & SHAP | LightGBM | Accuracy: 98.3%, Precision: 97.8%, Recall: 97.2%, F1-Score: 95% | Not provided |
| Brain Tumor [101] | MRI | FedHG with VAT | 3D U-Net | Dice Score: Improvement of 2.2% over FL baseline | Within 3% of centralized training |
These results demonstrate that FL can achieve diagnostic accuracy comparable to centralized approaches while preserving data privacy. The CNN-based FL framework for 3D breast cancer detection is particularly notable, achieving marginally higher accuracy (97.37%) than its centralized counterpart (97.30%) [102]. The integration of Explainable AI (XAI) techniques with FL, as shown in the LightGBM-SHAP framework, further enhances the practical utility of these models by providing interpretable insights for healthcare professionals [103].
Experimental Protocols and Methodologies
Standard Federated Learning Workflow
The foundational workflow for FL follows a structured, iterative process that maintains data decentralization while enabling collaborative learning. The following diagram illustrates this standard FL workflow.
Standard FL Workflow Diagram
The methodology follows these key phases [98] [99]:
Global Model Initialization: A central server creates and initializes a baseline machine learning model with random or pre-trained parameters.
Model Distribution: The server distributes the current global model parameters to a selected subset of participating clients (devices or institutions).
Local Training: Each client trains the model on its local dataset for a predetermined number of epochs or steps. The data never leaves the client's device or institutional boundary.
Update Transmission: Clients send their updated model parameters (weights or gradients) back to the server. Only model updates are shared, not raw training data.
Secure Aggregation: The server aggregates the received model updates, typically using a weighted averaging approach like Federated Averaging (FedAvg), to create a refined global model.
Iterative Refinement: Steps 2-5 repeat for multiple communication rounds until the model converges to a satisfactory performance level.
Advanced Methodologies for Medical Imaging
In cancer detection applications, researchers have developed specialized FL methodologies to address domain-specific challenges:
Data Heterogeneity Mitigation: The FedHG algorithm addresses non-IID (non-independent and identically distributed) data across medical institutions by incorporating Virtual Adversarial Training (VAT) into a 3D U-Net architecture and using a public validation dataset to derive improved aggregation weights [101].
Multimodal Integration: For skin cancer diagnosis, researchers have implemented FL with Deep Transfer Learning, using pre-trained VGG19 architectures fine-tuned on local dermatology datasets and incorporating Gradient-weighted Class Activation Mapping (Grad-CAM) for explainability [100].
3D Image Processing: For breast cancer detection with 3D mammograms, specialized preprocessing techniques transform DICOM volumes into standardized 2D representations suitable for FL, while maintaining the rich diagnostic information from the original 3D data [102].
Privacy and Security Analysis
While FL provides inherent privacy benefits by keeping raw data decentralized, model updates can still potentially leak sensitive information. Several privacy-preserving techniques have been developed to enhance FL's security guarantees. The following table compares their effectiveness against various attacks based on recent research.
Table 2: Security Analysis of Privacy-Preserving Techniques in Federated Learning [104]
| Privacy Technique | Backdoor Attack Success Rate | Untargeted Poisoning Success Rate | Targeted Poisoning Success Rate | Model Inversion Attack MSE | Man-in-the-Middle Accuracy Degradation |
|---|---|---|---|---|---|
| Base FL | Baseline | Baseline | Baseline | Baseline | Baseline |
| FL with SMPC | Improved | 0.0010 | 0.0020 | Improved | Improved |
| FL with HE (CKKS) | Improved | Improved | 0.0020 | Improved | Improved |
| FL with PATE | Improved | Improved | Improved | 19.267 | Improved |
| FL with CKKS & SMPC | Improved | 0.0010 | 0.0020 | Improved | Lowest degradation |
| FL with PATE, CKKS & SMPC | 0.0920 | Improved | Improved | Improved | 1.68% |
Technique Explanations:
- Homomorphic Encryption (HE): A cryptographic technique that permits computations on encrypted data without decryption [104].
- Secure Multi-Party Computation (SMPC): Enables collaborative computation of functions over private inputs without disclosing the raw data [104].
- Private Aggregation of Teacher Ensembles (PATE): A differential privacy technique that combines multiple teacher models trained on separate data subsets and adds noise to aggregated results [104].
The research demonstrates that combining multiple privacy techniques significantly enhances security. FL with PATE, CKKS, and SMPC achieved the lowest backdoor attack success rate (0.0920), while FL with CKKS and SMPC provided the strongest defense against poisoning attacks [104].
The Scientist's Toolkit: Research Reagent Solutions
Implementing effective federated learning systems for cancer detection requires both computational frameworks and domain-specific components. The following table catalogues essential "research reagents" for developing FL solutions in medical imaging.
Table 3: Essential Research Reagents for Federated Learning in Cancer Detection
| Reagent Category | Specific Tool/Solution | Function in FL Experimentation |
|---|---|---|
| FL Frameworks | Flower [98] | Provides the foundational infrastructure for implementing FL systems and managing client-server communication. |
| Model Architectures | CNN [102], 3D U-Net [101], VGG16/VGG19 [100], LightGBM [103] | Core learning models adapted for local training on distributed medical imaging data. |
| Aggregation Algorithms | Federated Averaging (FedAvg) [100], FedHG [101], FedProx, FedBN | Algorithms for combining local model updates into an improved global model while handling data heterogeneity. |
| Privacy Enhancements | Homomorphic Encryption [104], SMPC [104], PATE [104], Differential Privacy | Cryptographic and statistical techniques for protecting against information leakage from model updates. |
| Explainability Tools | SHAP [103], Grad-CAM [100] | Provide interpretability and transparency for model predictions, crucial for clinical adoption. |
| Medical Imaging Datasets | ISIC (Skin Lesions) [100], 3D DBT (Breast Cancer) [102], Brain Tumor MRI [101] | Benchmark datasets for training and evaluating FL models in cancer detection applications. |
| Validation Metrics | Dice Similarity Coefficient [101], Accuracy/Precision/Recall [103], F1-Score | Specialized metrics for evaluating model performance on medical segmentation and classification tasks. |
Federated Learning represents a transformative approach to collaborative model development in cancer detection, effectively balancing the dual imperatives of data privacy and diagnostic performance. The experimental evidence demonstrates that FL can achieve accuracy comparable to centralized learning—reaching 97-98% in various cancer detection tasks—while maintaining patient data within institutional boundaries [103] [102]. The integration of privacy-enhancing technologies like homomorphic encryption and secure multi-party computation further strengthens FL's security guarantees against sophisticated attacks [104].
For researchers and drug development professionals, FL offers a viable pathway to leverage diverse, multi-institutional datasets without violating privacy regulations or intellectual property concerns. The emerging methodologies for handling data heterogeneity, incorporating explainable AI, and processing 3D medical images continue to enhance FL's practical utility in clinical settings [100] [101]. As these technologies mature, federated learning is poised to become an indispensable tool for validating machine learning models in cancer detection research, enabling broader collaboration while upholding the highest standards of data privacy and security.
The Proof is in the Performance: Comparative Frameworks and Clinical Validation Pathways
The integration of machine learning (ML) into cancer detection and prognostication represents a paradigm shift in biomedical research. However, the transition from a high-performing predictive model to a clinically validated tool that can reliably inform patient care requires robust validation strategies. The foundation of determining whether a biometric monitoring tool is fit-for-purpose lies in a rigorous, multi-stage evaluation process often summarized as Verification, Analytical Validation, and Clinical Validation (V3) [105]. This framework, adapted from established software engineering and biomarker development practices, ensures that ML models are not only computationally sound but also clinically useful and reliable within their specific context of use. This guide objectively compares the methodologies and performance of various validation approaches, from initial hold-out sets to full-scale prospective trials, providing researchers with a structured pathway for translating computational models into clinical tools.
The V3 Framework: Foundation for Model Validation
A comprehensive validation strategy for ML models in healthcare should be structured around the three-component V3 framework, which combines established practices from both software engineering and clinical development [105].
Core Components of the V3 Framework
Verification: A systematic evaluation conducted by hardware manufacturers or engineers to ensure that the system components meet their specified requirements. This stage involves assessing sample-level sensor outputs and occurs computationally in silico and at the bench in vitro. Verification answers the question "Did we build the system right?" according to technical specifications [105].
Analytical Validation: This phase occurs at the intersection of engineering and clinical expertise and translates the evaluation procedure from the bench to in vivo settings. Analytical validation focuses on evaluating the data processing algorithms that convert sample-level sensor measurements into physiological or clinical metrics. This step is typically performed by the entity that created the algorithm, either the vendor or the clinical trial sponsor, and assesses whether the tool measures what it claims to measure accurately and reliably [105].
Clinical Validation: The final component demonstrates that the ML tool acceptably identifies, measures, or predicts the clinical, biological, physical, functional state, or experience in the defined context of use, which includes specific population definitions. This step is generally performed on cohorts of patients with and without the phenotype of interest and is typically conducted by clinical trial sponsors to facilitate the development of new medical products [105].
The diagram below illustrates the sequential flow and key objectives of the V3 framework:
Experimental Validation Methodologies: A Comparative Analysis
Hold-Out Sets and Cross-Validation
The use of hold-out sets represents a fundamental approach for initial model validation, serving to estimate model performance on unseen data and mitigate overfitting. Recent research has highlighted both the methodological value and ethical considerations of hold-out sets in clinical prediction models [106].
Table 1: Comparison of Hold-Set Implementation Strategies
| Strategy | Key Methodology | Primary Application | Ethical Considerations | Statistical Limitations |
|---|---|---|---|---|
| Random Hold-Out | Random sampling without replacement from overall population | Initial model development and performance estimation | Potential deprivation of beneficial interventions from control group | May not adequately capture population heterogeneity |
| Stratified Hold-Out | Sampling preserves distribution of key clinical variables | Ensuring representative samples across subpopulations | Similar to random hold-out but with better subgroup representation | Requires careful selection of stratification variables |
| Temporal Hold-Out | Data from most recent time period held out | Assessing model performance over time and temporal drift | Historical controls may not reflect current standard of care | Confounds temporal trends with model performance |
| Ethical Hold-Out | Prioritizes patients where intervention uncertainty is highest | Balancing model updating needs with patient welfare | Minimizes harm by restricting hold-out to clinical equipoise situations | Complex implementation requiring continuous monitoring |
In practice, hold-out sets create two mutually exclusive patient groups: the intervention set (X^I, Y^I) that receives model-derived risk scores and subsequent interventions, and the hold-out set (X^H, Y^H) that receives standard medical care without model influence [106]. This separation enables researchers to retrain models on data unaffected by performative prediction effects—where the model's predictions subsequently influence the outcomes they were designed to predict.
Prospective Clinical Trials
Prospective clinical trials represent the gold standard for establishing clinical utility and obtaining regulatory approval for ML-based tools. The fundamental workflow progresses from initial discovery to full clinical validation, as illustrated below:
Recent studies in cancer research demonstrate the application of this rigorous approach. For example, in developing a post-translational modification gene signature for breast cancer prognosis, researchers created 117 different machine learning models and evaluated their predictive performance using the C-index and AUC values across multiple datasets before selecting the optimal combination of RSF + Ridge algorithm [61]. Similarly, in hepatocellular carcinoma (HCC) prediction, researchers implemented five ML models (logistic regression, K-nearest neighbour, support vector machine, random forest, and artificial neural network) and conducted internal validation with a 70:30 train-test split [107].
Performance Comparison Across Validation Settings
Quantitative Performance Metrics
Table 2: Performance Comparison of ML Models Across Validation Types in Cancer Detection
| Cancer Type | Model Type | Hold-Set Performance (AUC) | Prospective Performance (AUC) | Key Predictive Features | Reference |
|---|---|---|---|---|---|
| Breast Cancer | PTMRS (RSF + Ridge) | 0.722 (1-year) | Not Reported | SLC27A2, TNFRSF17, PEX5L, FUT3, COL17A1 | [61] |
| Hepatocellular Carcinoma | Random Forest | 0.996 (Training) | 0.993 (Validation) | Age, BLR, D-Dimer, AST/ALT, GGT, AFP | [107] |
| Hepatocellular Carcinoma | Support Vector Machine | 0.801 (Internal Val) | Not Reported | Laboratory parameters, demographics, comorbidities | [107] |
| Hepatocellular Carcinoma | Artificial Neural Network | 0.812 (Internal Val) | Not Reported | Laboratory parameters, demographics, comorbidities | [107] |
The performance differential between hold-out set validation and prospective clinical validation highlights the phenomenon of model decay or drift that occurs when models transition from controlled development environments to real-world clinical settings. This drift can result from multiple factors including changes in patient populations, clinical practices, measurement techniques, or the performative effects of the model itself [106].
Research Reagent Solutions for Validation Studies
Successful implementation of validation frameworks requires specific methodological tools and approaches. The table below details essential "research reagents" for constructing robust validation studies.
Table 3: Essential Research Reagents for ML Model Validation in Cancer Research
| Reagent Category | Specific Tools/Methods | Function in Validation | Application Context |
|---|---|---|---|
| Data Processing | LASSO Regression | Feature selection and dimensionality reduction | Identifying most predictive variables from high-dimensional data [107] |
| Model Training | Random Forest, SVM, ANN, KNN | Developing predictive algorithms with different characteristics | Comparing model performance across architectures [107] |
| Performance Metrics | AUC, C-index, Calibration Plots, Brier Score | Quantifying discrimination, calibration, and overall performance | Objective model evaluation and comparison [61] [107] |
| Interpretability | SHAP (SHapley Additive exPlanations) | Explaining model predictions and feature importance | Enhancing clinical trust and understanding of ML models [107] |
| Validation Frameworks | V3 Framework (Verification, Analytical, Clinical) | Structured approach to comprehensive validation | Ensuring fit-for-purpose from technical to clinical utility [105] |
Integration of Validation Approaches: A Strategic Pathway
The most effective validation strategy employs a sequential approach that integrates multiple methodologies, beginning with hold-out sets and progressing to prospective trials. This pathway ensures both statistical rigor and clinical relevance.
Initial internal validation using techniques such as k-fold cross-validation and bootstrapping provides the first assessment of model performance [108]. Subsequent temporal validation assesses model stability over time, while external validation across different healthcare settings evaluates generalizability [106]. The final step involves prospective clinical trials that measure not just analytical performance but also clinical utility and impact on patient outcomes [105].
Each step in this pathway addresses different aspects of model validation: hold-out sets primarily address model performance and overfitting, while prospective trials evaluate clinical impact and practical implementation. The convergence of evidence across these methodologies provides the strongest foundation for clinical adoption of ML tools in cancer detection and prognostication.
Robust validation of machine learning models in cancer research requires a systematic, multi-stage approach that progresses from internal validation using hold-out sets to comprehensive prospective clinical trials. The V3 framework provides a structured foundation for this process, emphasizing the distinct but interconnected goals of verification, analytical validation, and clinical validation. Performance comparisons consistently demonstrate that while models may achieve exceptional metrics in initial hold-out validation, their real-world clinical utility must be established through prospective evaluation in diverse patient populations. As the field advances, the integration of methodological rigor with ethical considerations—particularly regarding hold-out set implementations—will be essential for translating computational promise into clinical reality that benefits cancer patients.
The integration of machine learning (ML) into oncology represents a paradigm shift in cancer detection and risk stratification. This guide provides a comparative analysis of ML model performance across three major cancers—breast, lung, and liver—focusing on validation methodologies and practical implementation for research and clinical applications. As these technologies transition from research to clinical settings, understanding their comparative strengths, limitations, and validation requirements becomes crucial for researchers, scientists, and drug development professionals working to implement robust, clinically viable solutions.
Performance Comparison of ML Models Across Cancer Types
The following tables summarize key performance metrics and architectural approaches for ML models applied to breast, lung, and liver cancer detection and risk prediction, based on recent validation studies.
Table 1: Comparative Performance Metrics of ML Models in Cancer Detection
| Cancer Type | Best-Performing Model(s) | Reported Accuracy | AUC | Sensitivity/Specificity | Key Dataset(s) | Citation |
|---|---|---|---|---|---|---|
| Breast Cancer | Vision Transformer (ViT) | Up to 99.99% (histopathology) | 0.722 (5-year prediction) | Sensitivity: 80.8% (RF model) | BreakHis, TCGA, hospital datasets | [60] [19] [18] |
| Random Forest | 84% F1-score | - | - | UCTH Breast Cancer Dataset | [19] | |
| K-Nearest Neighbors | Highest on original dataset | - | - | Wisconsin Breast Cancer | [18] | |
| Lung Cancer | XGBoost, Logistic Regression | ~100% (staging) | 0.83 (BU model) | Specificity: 55% at 95% sensitivity | National Lung Screening Trial | [109] [110] |
| Brock University (BU) Model | - | 0.83 | Specificity: 55% at 95% sensitivity | National Lung Screening Trial | [109] | |
| Liver Cancer | Random Forest | 97.7% accuracy | 0.993 | Sensitivity: 80.8%, Specificity: 99.1% | HBV patient cohorts | [111] [107] |
| Support Vector Machine | - | 0.979 | - | HBV-related cACLD cohort | [111] |
Table 2: Model Architectures and Implementation Considerations
| Cancer Type | Model Architecture | Key Features | Validation Approach | Clinical Readiness |
|---|---|---|---|---|
| Breast Cancer | CNNs, ViTs, GANs, Ensemble models | Multi-modal data integration, synthetic data generation | Multi-site retrospective validation, cross-dataset testing | Advanced research stage with interpretability focus |
| Lung Cancer | Mathematical prediction models (MPMs), XGBoost, Logistic Regression | Standardized sensitivity calibration, clinical feature integration | Large-scale screening cohort (NLST) with calibrated thresholds | Clinical implementation with specificity limitations |
| Liver Cancer | Random Forest, SVM, Logistic Regression, Neural Networks | Clinical biomarkers (LSM, age, platelet), SHAP interpretability | Internal validation with temporal split, calibration curves | High predictive performance with need for external validation |
Experimental Protocols and Methodologies
Breast Cancer Detection with Vision Transformers and Ensemble Methods
Dataset Preparation: Models were trained on multi-institutional datasets comprising mammography, digital breast tomosynthesis, ultrasound, and histopathological images. The BreakHis dataset was utilized for histopathology analysis, while clinical data from the UCTH Breast Cancer Dataset (213 patients, 9 features) supported clinical parameter-based models [60] [19]. Data preprocessing included handling missing values, label encoding for categorical variables, and max-absolute scaling for normalization.
Feature Selection: Mutual information and Pearson's correlation identified key predictive features including tumor size, involved nodes, metastasis status, and age. For ViT models, images were divided into patches and treated as sequences to capture both local and global contextual information [60] [19].
Model Training: Vision Transformers employed self-attention mechanisms without convolutional operations, pre-trained on large unlabeled medical image datasets before fine-tuning on annotated data. Ensemble methods combined multiple algorithms (SVM, RF, KNN) through stacking methodologies, with AutoML frameworks (H2OXGBoost) optimizing hyperparameters [60] [18]. Synthetic data generation using Gaussian Copula and Tabular Variational Autoencoders addressed data scarcity.
Validation: Stratified k-fold cross-validation assessed performance across multiple institutions to evaluate generalizability. Explainable AI techniques (SHAP, LIME, ELI5) provided model interpretability by identifying feature contributions to predictions [19].
Lung Cancer Nodule Malignancy Prediction with Mathematical Models
Dataset: The National Lung Screening Trial (NLST) dataset with 1,353 patients (122 malignant) was utilized. Nodules ≥4 mm were included, with calcified nodules excluded. The cohort was split 20:80 for calibration and testing while maintaining class balance [109].
Model Implementation: Four established mathematical prediction models (Mayo Clinic, Veterans Affairs, Peking University, Brock University) were implemented. These are post-imaging models using multivariate logistic regression on clinical risk factors and imaging features to generate continuous risk scores (0-1) [109].
Calibration Approach: A sub-cohort (n=270) calibrated decision thresholds for each model targeting 95% sensitivity for lung cancer detection. This standardized sensitivity enabled cross-model comparison at equivalent clinical operating points [109].
Performance Evaluation: Area under the receiver-operating-characteristic curve (AUC-ROC), area under the precision-recall curve (AUC-PR), sensitivity, and specificity were calculated. Performance stability was assessed by applying calibrated thresholds to the remaining cohort (n=1,083) [109].
Hepatocellular Carcinoma Risk Prediction in Hepatitis B Patients
Study Population: Patients with HBV-related compensated advanced chronic liver disease (cACLD) were retrospectively enrolled (n=1,051). Inclusion required LSM ≥10 kPa, no decompensation signs, and complete clinical/Follow-up data. The cohort was randomly split 7:3 into training (n=736) and validation (n=315) sets [111].
Feature Selection: Three machine learning approaches—least absolute shrinkage and selection operator (LASSO) regression, random forest, and support vector machine—identified key predictors from 63 clinical indicators. Intersection analysis determined final feature set [111] [107].
Model Development: Five ML algorithms (SVM, RF, logistic regression, XGBoost, Naive Bayes) were constructed using selected features. The RF model configured 100 decision trees with bootstrap aggregation to reduce overfitting. Hyperparameters were optimized through grid search [111].
Validation and Interpretation: Performance was evaluated using AUC, accuracy, sensitivity, specificity, and F1 score. The SHapley Additive exPlanations (SHAP) method provided model interpretability, quantifying feature importance and interaction effects [111] [107].
Workflow Visualization
ML Model Validation Workflow for Cancer Detection
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for ML Implementation in Cancer Research
| Resource Category | Specific Tools/Components | Function in Research | Application Examples |
|---|---|---|---|
| Computational Frameworks | Python, Scikit-learn, TensorFlow, PyTorch | Model development and training | Implementing RF, XGBoost, ViTs, CNNs |
| Explainability Tools | SHAP, LIME, ELI5, Anchor | Model interpretation and validation | Feature importance analysis, prediction explanation |
| Data Resources | NLST, TCGA, BreakHis, UCTH Dataset | Model training and benchmarking | Multi-site validation, synthetic data generation |
| Clinical Parameters | Liver stiffness measurement, platelet count, age, tumor size | Feature engineering and selection | HCC risk prediction, nodule malignancy assessment |
| Validation Metrics | AUC-ROC, AUC-PR, calibration curves, decision curve analysis | Performance evaluation and clinical utility assessment | Model comparison, net benefit calculation |
This comparative analysis demonstrates that while high-performing ML models exist across all three cancer types, their validation frameworks and clinical readiness vary substantially. Breast cancer models, particularly Vision Transformers and ensemble methods, show exceptional accuracy but require more extensive external validation. Lung cancer models provide standardized sensitivity but face specificity limitations that restrict clinical utility. Liver cancer risk prediction with Random Forest achieves outstanding performance but needs validation across diverse populations. Across all domains, explainable AI techniques and rigorous calibration emerge as critical components for clinical translation, enabling researchers and drug development professionals to implement these tools with appropriate understanding of their capabilities and limitations.
The integration of artificial intelligence (AI) into oncology represents a paradigm shift in cancer detection, offering the potential to enhance the accuracy, efficiency, and consistency of diagnostic imaging and pathology. As AI systems, particularly deep learning models, become more sophisticated, rigorous benchmarking against the established gold standard—expert human interpreters—is essential for clinical validation. This guide provides a systematic comparison of AI and human performance in cancer detection, synthesizing quantitative evidence from recent meta-analyses and multicentric studies. It further delineates standard experimental protocols for validation, visualizes core workflows, and catalogues essential research reagents, thereby offering a comprehensive resource for researchers and drug development professionals working at the intersection of computational oncology and clinical translation.
Performance Comparison Tables
The following tables synthesize diagnostic performance metrics for AI and human experts across multiple cancer types, as reported in recent systematic reviews and meta-analyses.
Table 1: Performance Comparison in Cancer Detection and Diagnosis
| Cancer Type | Modality | Task | AI Model | Sensitivity (AI vs. Human) | Specificity (AI vs. Human) | AUC (AI) | Evidence Level |
|---|---|---|---|---|---|---|---|
| Breast Cancer [8] | 2D Mammography | Screening detection | Ensemble DL | +9.4% (US) / +2.7% (UK) | +5.7% (US) / +1.2% (UK) | 0.81 - 0.89 | Diagnostic case-control |
| Colorectal Cancer [112] | Histopathology | Predicting LNM in T1/T2 CRC | DL/ML Models | 0.87 (95% CI: 0.76–0.93) | 0.69 (95% CI: 0.52–0.82) | 0.88 (95% CI: 0.84–0.90) | Meta-analysis (9 studies) |
| Early Gastric Cancer [113] | Endoscopy | Diagnosis | DCNN | 0.94 (95% CI: 0.87-0.93) | 0.91 (95% CI: 0.87-0.95) | 0.96 (95% CI: 0.94-0.98) | Meta-analysis (26 studies) |
| Prostate Cancer [114] | Multimodal Data | Predicting Biochemical Recurrence | ML Models | - | - | 0.82 (95% CI: 0.81–0.84) | Meta-analysis (16 studies) |
Table 2: Performance of RSNA AI Challenge Models in Breast Cancer Detection (n=1,537 algorithms) [115]
| Model Type | Sensitivity | Specificity | Recall Rate | Notes |
|---|---|---|---|---|
| Median of All Algorithms | 27.6% | 98.7% | 1.7% | Thresholds optimized for high specificity. |
| Ensemble of Top 3 | 60.7% | - | - | Different algorithms identified different cancers. |
| Ensemble of Top 10 | 67.8% | - | - | Performance close to an average screening radiologist in Europe/Australia. |
Detailed Experimental Protocols for AI Validation
To ensure the robustness and generalizability of AI models, studies employ rigorous experimental protocols. The following methodologies are commonly cited in the literature.
Multi-Cohort Diagnostic Studies with External Validation
This design is considered a high standard for evaluating diagnostic accuracy.
- Objective: To assess the real-world performance and generalizability of an AI system.
- Patient Cohorts: Studies typically involve a Training Cohort from one or multiple institutions. Performance is then tested on separate Internal Validation and External Validation Cohorts from different clinical sites to ensure the model is not over-fitted to the training data [8].
- Gold-Standard Labels: Expert consensus among multiple skilled specialists (e.g., five endoscopists) or histopathological confirmation by board-certified pathologists is used as the reference standard [8] [112].
- Blinding: The clinicians establishing the gold standard are blinded to the AI system's predictions to prevent bias.
- Statistical Analysis: Performance metrics (Sensitivity, Specificity, AUC) are calculated for each cohort and compared against human expert performance using statistical tests for non-inferiority or superiority [8].
Systematic Review and Meta-Analysis
This methodology provides the highest level of evidence by synthesizing all available research.
- Protocol Registration: The study protocol is registered a priori with platforms like PROSPERO (e.g., CRD42024607756) [112].
- Literature Search: A comprehensive search is conducted across multiple databases (e.g., PubMed, Embase, Web of Science) using predefined MeSH and free-text terms related to the cancer type and AI [112] [114] [113].
- Study Selection: Following PRISMA guidelines, identified records are screened for eligibility based on strict inclusion/exclusion criteria (e.g., population, intervention, outcomes) [112] [116].
- Data Extraction and Quality Assessment: Two reviewers independently extract data (e.g., TP, FP, FN, TN) and assess the risk of bias using tools like QUADAS-2 [112] [113].
- Statistical Synthesis: A bivariate random-effects model is often used to pool sensitivity and specificity. The area under the summary receiver operating characteristic (SROC) curve (AUC) is the primary metric for overall performance. Heterogeneity is explored using the I² statistic [112] [113].
Multicentric Model Development and External Validation
This protocol tests an AI model's ability to generalize across diverse patient populations and clinical settings.
- Objective: To develop a model that is robust to variations in clinical practice and patient demographics.
- Cohort Designation: Data from multiple centers are split into an Investigational Cohort (IC) for model training and internal validation (e.g., using leave-one-out cross-validation) and a completely separate External Validation Cohort (EVC) from different institutions for final testing [117].
- Handling Data Imbalance: Techniques like resampling and ensemble methods are implemented to address class imbalance, which is common in medical datasets (e.g., a small number of cancer cases versus controls) [117].
- Explainability Analysis: eXplainable AI (XAI) techniques such as SHAP or LIME are applied to interpret model predictions and identify key clinical risk factors, ensuring alignment with clinical knowledge [117] [118].
Workflow Visualization
The following diagram illustrates a standardized workflow for the development and validation of AI models in cancer diagnostics, integrating elements from the described experimental protocols.
AI Validation Workflow - This flowchart outlines the key stages in the rigorous validation of AI models for cancer diagnosis, from data collection to final assessment of clinical utility.
The Scientist's Toolkit: Research Reagent Solutions
The table below details key resources and their functions as derived from the experimental setups in the cited literature. These are essential for replicating studies and advancing research in this field.
Table 3: Essential Research Reagents and Resources for AI Validation in Cancer Diagnostics
| Research Reagent / Resource | Function in AI Validation | Example Use Case |
|---|---|---|
| Curated Public Datasets | Serves as benchmark data for training and initial validation of algorithms, ensuring reproducibility and comparison against other models. | DDTI dataset for thyroid cancer [118]; RSNA Challenge dataset for breast cancer [115]. |
| High-Resolution Digital Whole Slide Images (WSI) | Provides the raw input data for developing AI models in digital pathology; enables analysis of microscopic cellular architecture. | Used in studies for detecting lymph node metastasis in colorectal cancer [112] and for ovarian cancer risk assessment [117]. |
| Explainable AI (XAI) Tools (e.g., SHAP, LIME, Grad-CAM) | Provides post-hoc interpretations of model predictions, highlighting which image features or clinical variables drove the decision, crucial for clinical trust and adoption. | Identifying significant risk factors in BRCA-mutated patients [117] and highlighting suspicious regions in thyroid ultrasound [118]. |
| Cloud-Based Computing Platforms & Centralized Imaging Portals | Enables scalable storage, sharing, and analysis of large multi-institutional datasets, facilitating collaborative research and external validation. | Discussed as a solution for data standardization and AI validation in cancer research and clinical trials [119]. |
| Quality Assessment Tools (e.g., QUADAS-2) | A critical methodological reagent used to assess the risk of bias and applicability of primary studies included in systematic reviews and meta-analyses. | Employed in meta-analyses to ensure the quality and reliability of the synthesized evidence [112] [114] [113]. |
| Ensemble Modeling Techniques | A software-based reagent that combines predictions from multiple AI models to improve overall accuracy, sensitivity, and robustness. | Combining top algorithms from the RSNA AI Challenge significantly boosted sensitivity for breast cancer detection [115]. |
The validation of machine learning (ML) models in cancer detection research has traditionally prioritized computational accuracy metrics, such as area under the curve (AUC) and F1-scores. However, for these advanced algorithms to transition from research novelties to clinical assets, they must demonstrate excellence beyond statistical performance. They must achieve seamless clinical workflow integration, a multidimensional concept encompassing how well a technology incorporates into the work system elements—people, tasks, tools, physical environment, and organization—and their interactions over time [120] [121]. Poorly integrated health information technology (IT) contributes significantly to clinician burnout, with approximately 50% of clinicians affected, and introduces patient safety risks [120] [121]. In oncology, where diagnostic and treatment pathways are complex, the stakes for integration are particularly high. This guide provides a structured approach to assessing workflow integration, usability, and computational efficiency, offering a comparative analysis of methodologies and tools relevant to researchers, scientists, and drug development professionals working to validate ML models in real-world clinical settings.
Theoretical Framework: Defining and Deconstructing Workflow Integration
A Systems-Based Definition
Workflow integration is not merely a sequence of tasks but a complex system. Grounded in human factors (HF) principles, it can be defined as the extent to which a technology is seamlessly incorporated within the work system elements and their interactions over time [120] [121]. This involves fitting within the sequence and flow of tasks, people, information, and tools across individual, team, and organizational levels, and throughout the patient journey [120] [121]. When a new technology like an ML-based decision support system is introduced, it alters the entire work system, leading to the emergence of a new workflow. Successful integration means these new system interactions fit harmoniously within the temporal flow of clinical work.
Core Dimensions of Workflow Integration
The concept of workflow integration can be operationalized through four key dimensions, which provide a scaffold for assessment [120] [121]:
Table: Dimensions of Workflow Integration
| Dimension | Description | Key Considerations for Oncology AI |
|---|---|---|
| Time | The temporal nature of work execution. | Sequential, parallel, or discontinuous tasks; model inference speed relative to clinical decision points. |
| Flow | The movement of core elements within the system. | Flow of tasks, people, information, and tools; how AI outputs are channeled to relevant personnel. |
| Scope of Patient Journey | The care continuum across which integration occurs. | Intra-visit, intra-organizational, or inter-organizational; integration from screening through treatment follow-up. |
| Level | The organizational hierarchy affected. | Individual clinician, multidisciplinary team, or organizational processes; how AI affects team dynamics. |
Methodologies for Assessing Workflow Integration and Usability
Qualitative and Mixed-Methods Approaches
A scoping review on EHR usability highlights the value of qualitative and mixed-method approaches, including interviews, focus groups, and time-motion studies, for identifying deep-seated workflow disruptions [122]. These methodologies can uncover specific integration barriers such as task-switching, excessive screen navigation, and information fragmentation that necessitate workarounds like duplicate documentation or use of external tools [122]. For instance, interviews with emergency department physicians identified 134 distinct excerpts detailing barriers and facilitators to the workflow integration of a clinical decision support (CDS) system, which were then mapped onto the four dimensions of workflow integration [120]. This granular data is invaluable for understanding the real-world impact of ML tools on clinical workflows.
Structured Evaluation Frameworks
Structured frameworks enable the systematic evaluation of usability and integration. One such framework, developed to assess AI scribes in primary care, organizes evaluation across three domains [123]:
- Usability: Measures user interface quality, EMR compatibility/integration, and process flow (e.g., steps and time to launch the tool).
- Effectiveness and Technical Performance: Assesses metrics like average documentation time and performance under challenging conditions (e.g., background noise, multiple speakers).
- Accuracy and Quality: Evaluates the quality of generated outputs, such as medical notes, against benchmarked standards [123].
This framework employs a 3-point Likert scale (Poor, Good, Excellent) for rating applicable items, providing a standardized method for comparative analysis [123].
Standardized Surveys and Quantitative Metrics
Surveys offer a scalable way to gather quantitative data on user perceptions. The System Usability and Risk Evaluation (SURE) scale is a 25-item instrument with excellent internal consistency (McDonald’s omega = 0.96) that assesses key usability domains [124]. Nationally, physicians rate their EMRs at an average of just 52.2% of the maximum possible score on the SURE scale, with low scores particularly in collaborating with external colleagues, prioritizing daily tasks, and preventing data entry errors [124]. The System Usability Scale (SUS) is also widely used; U.S. physicians rate their EHRs with a median SUS score of 45.9, placing them in the bottom 9% of all software systems [122]. Each one-point drop in the SUS score is associated with a 3% increase in burnout risk, underscoring the critical link between usability, workflow integration, and clinician well-being [122].
The diagram below illustrates the interconnected relationship between the work system, the process of care, and the outcomes achieved, which forms the conceptual basis for workflow integration analysis.
Comparative Performance of ML Models in Cancer Detection
Performance Metrics Across Cancer Types
The following table summarizes the performance of various machine learning models as reported in recent research, providing a benchmark for computational efficiency and accuracy in cancer detection and classification.
Table: Comparative Performance of Machine Learning Models in Cancer Detection
| Cancer Type / Focus | Data Modality | ML Model | Key Performance Metrics | Source/Study |
|---|---|---|---|---|
| Pan-Cancer Classification | RNA-seq Gene Expression | Support Vector Machine (SVM) | Accuracy: 99.87% (5-fold cross-validation) | [125] |
| Cancer Risk Prediction | Lifestyle & Genetic Data | Categorical Boosting (CatBoost) | Accuracy: 98.75%, F1-score: 0.9820 | [25] |
| Ovarian Cancer Detection | Multi-omic Blood Test | Proprietary ML Platform | AUC: 0.92 (all stages), AUC: 0.89 (early-stage) | [126] |
| Symptom Deterioration Prediction | EHR Data from Treatments | Best-Performing ML System | AUROC: 0.73 (for drowsiness), AUROC: 0.66 (for dyspnea) | [62] |
| Autonomous AI for Oncology | Multimodal Patient Data | GPT-4 with Tool Integration | Clinical Conclusion Accuracy: 91.0%, Tool Use Accuracy: 87.5% | [4] |
Experimental Protocols for Model Validation
1. Protocol for RNA-seq Pan-Cancer Classification [125]:
- Data: PANCAN RNA-seq dataset from UCI Machine Learning Repository (801 samples, 20,531 genes, 5 cancer types).
- Preprocessing: Check for missing values and outliers. Employ feature selection algorithms (Lasso and Ridge Regression) to identify dominant genes and mitigate the "large p, small n" problem and multicollinearity.
- Model Training & Evaluation: Assess eight classifiers (SVM, K-Nearest Neighbors, AdaBoost, Random Forest, Decision Tree, Quadratic Discriminant Analysis, Naïve Bayes, Artificial Neural Networks). Validate model performance using a 70/30 train-test split and 5-fold cross-validation. Use accuracy, precision, recall, and F1 score as evaluation metrics.
2. Protocol for AI Scribe Evaluation [123]:
- Design: Systematic competitive analysis using an evaluation framework based on expert usability and human factors engineering principles.
- Data Generation: Use audio files from standardized patient encounters to generate transcripts and SOAP-format medical notes via multiple AI scribes.
- Benchmarking: Compare AI-generated outputs against a verbatim transcript, detailed case notes, and a physician-written medical note.
- Rating: Rate items across usability, effectiveness/technical performance, and accuracy/quality domains on a predefined 3-point Likert scale. Gather supplementary qualitative insights from clinical experts.
3. Protocol for Autonomous Oncology AI Agent [4]:
- System Design: Integrate GPT-4 with specialized tools: vision transformers for detecting MSI and KRAS/BRAF mutations from histopathology slides, MedSAM for radiological image segmentation, and web-based search tools (OncoKB, PubMed, Google), augmented with a Retrieval-Augmented Generation (RAG) system of ~6,800 medical documents.
- Evaluation Benchmark: Develop 20 realistic, multimodal patient cases focusing on gastrointestinal oncology.
- Assessment: The agent autonomously selects and uses tools in a multi-step process. Four human experts perform a blinded manual evaluation of three areas: appropriateness of tool use, quality/completeness of textual outputs, and precision of citations from the RAG system.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key resources and their functions as utilized in the experimental protocols cited in this guide.
Table: Key Research Reagent Solutions and Materials
| Item | Function in Research/Validation | Example Use Case |
|---|---|---|
| PANCAN RNA-seq Dataset | Provides standardized gene expression data for training and benchmarking pan-cancer classification models. | Served as the primary data source for comparing eight ML classifiers [125]. |
| The Cancer Genome Atlas (TCGA) | A comprehensive public repository of cancer genomics data, often used as a data source for model development. | Basis for the RNA-seq data in the UCI PANCAN dataset [125]. |
| Standardized Patient Encounter Audio | Provides a consistent, benchmarkable input for fairly comparing the performance of different AI scribes. | Used to generate and compare SOAP notes from multiple AI scribe vendors [123]. |
| OncoKB Database | A precision oncology knowledge base detailing the clinical implications of genetic variants, used to ground AI decisions in evidence. | Integrated as a tool for the autonomous AI agent to query therapeutic implications of mutations [4]. |
| Vision Transformers (for Histopathology) | Specialized deep learning models trained to analyze histopathology slides and predict genetic alterations directly from tissue images. | Used by the autonomous AI agent to predict MSI status and KRAS/BRAF mutations from slide images [4]. |
| MedSAM | A foundation model for segmenting various anatomical structures from medical images, enabling quantitative analysis. | Used by the autonomous AI agent to segment tumors from MRI and CT scans for measurement [4]. |
The workflow for developing and validating a clinical AI tool, from data preparation to integration assessment, involves a multi-stage process that ensures both computational and clinical viability.
The journey from a high-accuracy ML model to a clinically valuable tool is incomplete without rigorous assessment of its integration into the healthcare workflow. As the data shows, even models with near-perfect accuracy in silico must be evaluated on their ability to fit seamlessly into the temporal, sequential, and organizational flow of clinical work without contributing to cognitive load or necessitating workarounds. A comprehensive validation strategy for ML in cancer detection must therefore synthesize three core pillars: computational performance (e.g., AUC, accuracy), clinical efficacy (impact on care decisions and patient outcomes), and workflow integration (usability, efficiency, and user satisfaction). For researchers and drug development professionals, adopting the structured frameworks, methodologies, and comparative metrics outlined in this guide is essential for developing oncology AI solutions that are not only intelligent but also indispensable and harmonious components of modern clinical practice.
The integration of machine learning (ML) into clinical oncology represents a paradigm shift in cancer detection and diagnosis. However, the dynamic nature of real-world medical environments—characterized by evolving clinical practices, changing patient demographics, and emerging technologies—poses a significant challenge to the longevity and reliability of static ML models [49]. Model drift, the degradation of model performance over time due to shifts in data distributions, is a critical concern that can compromise patient safety and diagnostic accuracy [127]. Consequently, a single validation at deployment is insufficient; a framework for continuous validation is essential to ensure models remain safe, effective, and reliable throughout their operational lifecycle. This guide explores and compares the leading methodologies and frameworks for achieving this continuous oversight, with a specific focus on applications in cancer detection research.
Comparative Analysis of Continuous Validation Frameworks
The approach to continuous validation varies from established MLOps maturity models to specialized diagnostic frameworks. The table below provides a high-level comparison of these strategic frameworks.
Table 1: Comparison of Continuous Validation and Monitoring Frameworks
| Framework Name | Core Focus | Proposed Maturity Levels | Key Strengths | Primary Context |
|---|---|---|---|---|
| Healthcare MLOps Maturity Model [128] | Operationalizing the end-to-end ML lifecycle | 1. Low Maturity2. Partial Maturity3. Full Maturity | Provides a holistic view of automation from data to deployment; tailored to healthcare barriers. | General Healthcare ML |
| Temporal Diagnostic Framework [49] | Pre-deployment temporal validation & longevity assessment | A four-stage diagnostic process: 1. Performance Evaluation2. Temporal Evolution Analysis3. Longevity & Recency Trade-offs4. Feature & Data Valuation | Model-agnostic; easy-to-implement; proactively vets future applicability. | Clinical ML (Oncology) |
| Continuous AI Assurance [129] | Diagnostic testing and verification of AI components | Four technical pillars: 1. Diagnostics2. Uncertainty Estimation3. Robustness Verification4. Safety Verification | High focus on explainability and model introspection for "black box" models. | Safety-Critical AI Systems |
The Healthcare MLOps Maturity Model
This model, synthesized from a scoping review, conceptualizes continuous validation as a journey through increasing levels of automation in the ML pipeline [128]. The workflow spans data extraction, preparation, model training, evaluation, deployment, and—crucially—continuous monitoring (CM) and continual learning (CL) [128]. Its maturity levels are defined as:
- Low Maturity: The complete absence of CM and CL processes. Models are deployed statically without systematic tracking or retraining.
- Partial Maturity: The presence of continuous monitoring, where model performance and data are tracked, but any model retraining is manually triggered by an engineering team.
- Full Maturity: The presence of both CM and fully automated CL, where the system automatically retrains and redeploys models when performance decay is detected [128].
Temporal Diagnostic Framework for Prospective Validation
This model-agnostic framework is designed for rigorous, pre-deployment validation using time-stamped data to simulate future performance and uncover drift [49]. Its four-stage protocol is ideal for oncology contexts where data evolves rapidly. The stages are:
- Temporal Performance Evaluation: Partitioning data from multiple years into training and temporally distinct validation cohorts to assess performance over time.
- Temporal Evolution Analysis: Characterizing how patient outcomes (labels) and characteristics (features) fluctuate over the study period.
- Longevity and Recency Trade-offs: Exploring how the quantity versus the recentness of training data impacts model performance and longevity.
- Feature Reduction and Data Valuation: Applying feature importance and data valuation algorithms to refine the model's input and assess data quality [49].
Continuous AI Assurance with Diagnostic Tools
This framework emphasizes the technical tools required for the diagnostic pillar of AI assurance, which is vital for interpreting and trusting model decisions in a clinical setting [129]. It categorizes tools as:
- Decision Explainability Tools: Such as Layer-wise Relevance Propagation (LRP) and SHapley Additive exPlanations (SHAP), which visualize the parts of an input (e.g., a region in a medical image) that were most influential to a model's prediction [129].
- Model Diagnosis Tools: Such as WeightWatcher (WW), which analyzes the internal state of a deep neural network (DNN) to assess training effectiveness and layer-level performance without needing access to the original data [129].
Experimental Protocols for Continuous Validation
Implementing the frameworks above requires specific, actionable experimental protocols. The following section details key methodologies cited in recent literature.
Protocol: Evaluating Model Longevity with Sliding Windows
This protocol is central to the Temporal Diagnostic Framework and is used to determine the optimal trade-off between using more historical data for stability versus more recent data for relevance [49].
Methodology:
- Cohort Construction: Define a cohort with data spanning multiple years. For example, a cohort of cancer patients initiating systemic therapy from 2010 to 2022 [49].
- Sliding Window Training: Train multiple models using different training "windows" of data.
- Incremental Windows: Use an expanding window of data (e.g., 2010-2015, then 2010-2016, etc.) to assess the benefit of more data.
- Rolling Windows: Use a fixed-length, sliding window of data (e.g., 2015-2017, then 2016-2018, etc.) to assess the benefit of recent data.
- Temporal Validation: Evaluate all trained models on a fixed, held-out test set from the most recent time period (e.g., 2021-2022). This simulates a prospective validation and measures how well a model trained on past data predicts future outcomes.
Visualization of Training Schedules: The following diagram illustrates the incremental and rolling window approaches for training model cohorts to assess longevity.
Protocol: Implementing a Basic MLOps Workflow
This protocol outlines the core steps for moving from a static model to a partially or fully mature MLOps system, as defined in the MLOps Maturity Model [128].
Methodology:
- Data Extraction & Preparation: Implement automated pipelines for data extraction and feature engineering [128].
- Model Training & Validation: Automate model training and validate performance against a set of predefined metrics on a hold-out set.
- Model Deployment: Serve the validated model via an API or within a clinical application for real-time or batch inference [128].
- Continuous Monitoring (CM): The critical step for continuous validation. This involves:
- Continual Learning (CL): Establish a feedback loop where model performance decay or significant data drift triggers model retraining, either manually (Partial Maturity) or automatically (Full Maturity) [128].
Visualization of the MLOps Workflow: The following diagram maps the automated pipeline and feedback loops that characterize a mature MLOps system.
The Scientist's Toolkit: Key Software & Research Reagents
Successful continuous validation relies on a suite of software tools and libraries that implement the theoretical frameworks.
Table 2: Essential Software Tools for Continuous Validation in Clinical ML
| Tool Category | Specific Tool / Library | Primary Function | Application in Clinical Validation |
|---|---|---|---|
| Explainability (XAI) | SHAP (SHapley Additive exPlanations) [129] | Explains any ML model's output by quantifying each feature's contribution. | Verifies that a cancer detection model bases its prediction on medically relevant image regions or features, not spurious correlations. |
| Explainability (XAI) | LRP (Layer-wise Relevance Propagation) [129] | Generates heatmaps for deep learning models, showing pixel-level relevance for computer vision tasks. | Audits image-based classifiers (e.g., histopathology or radiology) to ensure decisions are based on pathologically relevant areas. |
| Model Diagnosis | WeightWatcher [129] | Diagnoses the health and training quality of deep neural networks without requiring data. | Assesses if a pre-trained model for genomic analysis is over-trained or under-trained, predicting its generalization potential. |
| Drift Detection | Open-source libraries (e.g., Evidently AI, Alibi Detect) | Statistically compares data distributions and monitors model performance metrics over time. | Integrated into a monitoring dashboard to automatically alert researchers to performance degradation or data shift in a live model. |
| MLOps Orchestration | Open-source platforms (e.g., MLflow, Kubeflow) | Automates and manages the end-to-end ML lifecycle, from pipelines to deployment and monitoring. | Provides the infrastructural backbone for implementing the automated retraining and deployment required for full MLOps maturity. |
The transition from static to dynamic, continuous validation is a critical evolution for the safe and effective deployment of ML in clinical oncology. As detailed in this guide, researchers have multiple frameworks at their disposal, from the comprehensive Healthcare MLOps Maturity Model to the targeted Temporal Diagnostic Framework. The experimental protocols for temporal validation and MLOps implementation provide a actionable roadmap, while the growing toolkit of explainability and diagnostic software empowers scientists to look inside the "black box" and maintain trust. By adopting these rigorous, continuous validation practices, the research community can ensure that machine learning models for cancer detection remain robust, reliable, and responsive to the ever-changing clinical landscape.
Conclusion
The successful validation of machine learning models in cancer detection is a multifaceted endeavor that extends far beyond achieving high accuracy on a static dataset. It requires a holistic framework that addresses foundational data challenges, employs rigorous methodological applications, proactively troubleshoots for robustness, and commits to thorough comparative and clinical validation. Future progress hinges on fostering interdisciplinary collaboration among data scientists, clinicians, and regulators. Key directions include the widespread adoption of explainable AI (XAI) to build trust, the use of federated learning to access diverse data while preserving privacy, and the execution of large-scale, prospective clinical trials to firmly establish the efficacy and reliability of these tools. By adhering to this comprehensive validation pathway, ML models can truly fulfill their transformative potential, enabling earlier detection, personalized treatment strategies, and improved outcomes in the global fight against cancer.
References
- 1. Clinical prediction models using machine learning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506039/]
- 2. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 3. Measures of agreement between computation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0021999106001860]
- 4. Development and validation of an autonomous artificial ... [https://www.nature.com/articles/s43018-025-00991-6]
- 5. A comparative assessment of machine learning models ... [https://www.sciencedirect.com/science/article/pii/S2772442524000820]
- 6. Artificial Intelligence in Cancer Drug Discovery in 2025 [https://oncodaily.com/oncolibrary/artificial-intelligence-in-cancer-drug-discovery]
- 7. Methodological and reporting quality of machine learning ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1555247/full]
- 8. Artificial intelligence in cancer: applications, challenges, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574039/]
- 9. Cancer Diagnosis Categorization in Electronic Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490771/]
- 10. a systematic literature review and meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570641/]
- 11. The AI revolution: how multimodal intelligence will reshape ... [https://www.nature.com/articles/s44387-025-00044-4]
- 12. Medical laboratory data-based models [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06802-x]
- 13. Advancing cancer care through artificial intelligence [https://link.springer.com/article/10.1007/s44272-025-00052-0]
- 14. Synthetic data generation: a privacy-preserving approach ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958975/]
- 15. A Triple-Embedding Model Selector Approach [https://ojs.aaai.org/index.php/AAAI/article/view/32807]
- 16. Federated nnU-Net for privacy-preserving medical image ... [https://www.nature.com/articles/s41598-025-22239-0]
- 17. The Genetic Data Market: Institutional Governance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12520235/]
- 18. Advancing breast cancer prediction: Comparative analysis of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326221]
- 19. Detection of breast cancer using machine learning and ... [https://www.nature.com/articles/s41598-025-12644-w]
- 20. Current AI technologies in cancer diagnostics and treatment [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02369-9]
- 21. Interpreting Black-Box Models: A Review on Explainable ... [https://link.springer.com/article/10.1007/s12559-023-10179-8]
- 22. Stop Explaining Black Box Machine Learning Models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9122117/]
- 23. 2 Interpretability – Interpretable Machine Learning [https://christophm.github.io/interpretable-ml-book/interpretability.html]
- 24. Development and validation of a machine learning model ... [https://pubmed.ncbi.nlm.nih.gov/41029530/]
- 25. Predicting cancer risk using machine learning on lifestyle ... [https://www.nature.com/articles/s41598-025-15656-8]
- 26. Artificial Intelligence in healthcare - Public Health - European ... [https://health.ec.europa.eu/ehealth-digital-health-and-care/artificial-intelligence-healthcare_en]
- 27. HIPAA vs. GDPR Compliance: What's the Difference? | Blog [https://www.onetrust.com/blog/hipaa-vs-gdpr-compliance/]
- 28. Top 10 Privacy Compliance Differences: US vs. EU Trials [https://www.clinicaltrialvanguard.com/article/top-10-privacy-compliance-differences-us-vs-eu-trials/]
- 29. GDPR for Machine Learning: Data Protection in AI ... [https://gdprlocal.com/gdpr-machine-learning/]
- 30. HIPAA Compliance AI in 2025: Critical Security ... [https://www.sprypt.com/blog/hipaa-compliance-ai-in-2025-critical-security-requirements]
- 31. Evaluating transparency in AI/ML model characteristics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12624113/]
- 32. Artificial Intelligence-Enabled Medical Devices [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-enabled-medical-devices]
- 33. Vironix Health Accepted to ML4H 2025 & NeurIPS TS4H ... [https://www.cbs42.com/business/press-releases/ein-presswire/867312755/vironix-health-accepted-to-ml4h-2025-neurips-ts4h-for-privacy-preserving-generative-health-data-modeling]
- 34. Enhancing Automated Breast Cancer Detection: A CNN ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565606/]
- 35. Performance of convolutional neural networks for the ... [https://pubmed.ncbi.nlm.nih.gov/38352765/]
- 36. CNN-TumorNet: leveraging explainability in deep learning ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1554559/full]
- 37. A Novel Recurrent Neural Network Framework for ... [https://arxiv.org/html/2509.12732v1]
- 38. Recurrent Neural Network for Predicting Transcription ... [https://www.nature.com/articles/s41598-018-33321-1]
- 39. Implementation of ensemble machine learning algorithms on ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-05050-w]
- 40. Development and validation of hybrid machine learning ... [https://pubmed.ncbi.nlm.nih.gov/40606977/]
- 41. Development and validation of hybrid machine learning ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1605378/full]
- 42. Development and validation of an ensemble machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9986604/]
- 43. Medical Image Preprocessing: Key Techniques & Best Practices [https://collectiveminds.health/articles/the-ultimate-guide-to-preprocessing-medical-images-techniques-tools-and-best-practices-for-enhanced-diagnosis]
- 44. Medical image data augmentation: techniques, ... [https://link.springer.com/article/10.1007/s10462-023-10453-z]
- 45. Impacts on Breast Ultrasound Image Classification [https://pubmed.ncbi.nlm.nih.gov/40310743/]
- 46. On-the-Fly Data Augmentation for Brain Tumor Segmentation [https://arxiv.org/html/2509.24973v1]
- 47. Targeted generative data augmentation for automatic ... [https://pubmed.ncbi.nlm.nih.gov/39981192/]
- 48. A new feature extraction approach of medical image based ... [https://www.sciencedirect.com/science/article/pii/S2772528622000590]
- 49. Diagnostic framework to validate clinical machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12219301/]
- 50. Transfer learning based deep architecture for lung cancer ... [https://www.nature.com/articles/s41598-025-13755-0]
- 51. Employing transfer learning for breast cancer detection using ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000907]
- 52. Skin Cancer Detection Using Transfer Learning and Deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11720014/]
- 53. A robust transfer learning approach with histopathological ... [https://www.sciencedirect.com/science/article/pii/S2772442525000103]
- 54. Performance Evaluation and Comparison of Transfer ... [https://msesj.com/index.php/mses/article/view/220]
- 55. A Narrative Review of Multimodal Data Fusion Strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12591514/]
- 56. Fusion of medical imaging and electronic health records ... [https://www.nature.com/articles/s41746-020-00341-z]
- 57. The future of multimodal artificial intelligence models for ... [https://dirjournal.org/articles/the-future-of-multimodal-artificial-intelligence-models-for-integrating-imaging-and-clinical-metadata-a-narrative-review/dir.2024.242631]
- 58. A machine learning approach for multimodal data fusion ... [https://www.nature.com/articles/s41698-025-00917-6]
- 59. Recent advances in data-driven fusion of multi-modal ... [https://www.sciencedirect.com/science/article/pii/S1566253524005165?dgcid=rss_sd_all]
- 60. Exploring AI Approaches for Breast Cancer Detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553387/]
- 61. Integrating machine learning and experimental validation ... [https://www.nature.com/articles/s41598-025-23772-8]
- 62. Development of Machine Learning Systems to Predict ... [https://pubmed.ncbi.nlm.nih.gov/40997295/?utm_source=SimplePie&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1bAXfGTh08tVk-e1kpwuqxoVfiUn_5olMN9ewCML2bdAMGPEOD&fc=20220524054416&ff=20250925205146&v=2.18.0.post9+e462414]
- 63. F1 Score vs ROC AUC vs Accuracy vs PR AUC [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 64. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 65. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 66. Understanding F1 Score, Accuracy, ROC-AUC & PR- ... [https://www.deepchecks.com/f1-score-accuracy-roc-auc-and-pr-auc-metrics-for-models/]
- 67. Empirical Study of Overfitting in Deep Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10093528/]
- 68. Lung Cancer Diagnosis From Computed Tomography Images ... [https://bioinform.jmir.org/2025/1/e68848]
- 69. Comparison of Deep Transfer Learning Against ... [https://pubmed.ncbi.nlm.nih.gov/40431843/]
- 70. Combining K-fold cross validation with bayesian ... [https://www.nature.com/articles/s41598-025-23336-w]
- 71. A novel cross-validated machine learning based Alertix- ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1570106/full]
- 72. Advanced skin cancer prediction with medical image data ... [https://www.nature.com/articles/s41598-025-14963-4]
- 73. Automating cancer diagnosis using advanced deep ... [https://www.nature.com/articles/s41598-024-75876-2]
- 74. Handling imbalanced medical datasets: review of a decade ... [https://link.springer.com/article/10.1007/s10462-024-10884-2]
- 75. Learning from Imbalanced Data: Integration of Advanced ... [https://www.mdpi.com/2072-6694/16/19/3417]
- 76. Imbalanced Dataset: Strategies to Fix Skewed Class ... [https://labelyourdata.com/articles/imbalanced-dataset]
- 77. Imbalanced Data | Peter Lorenz - GitHub Pages [https://lorenz-peter.github.io/blog/2025/imbalanced-data/]
- 78. Performance analysis of data resampling on class imbalance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10903850/]
- 79. A Novel SMOTE-Based Method to Generate Synthetic Data ... [https://www.mdpi.com/2571-5577/4/1/18]
- 80. Hybrid Synthetic Minority Over-sampling Technique ... [https://www.nature.com/articles/s41598-025-23062-3]
- 81. ART: Adaptive Resampling-based Training for Imbalanced ... [https://arxiv.org/html/2509.00955v1]
- 82. Imbalanced customer churn classification using a new ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417424001167]
- 83. Should You Use Imbalanced-Learn in 2025? [https://www.blog.trainindata.com/should-you-use-imbalanced-learn-in-2025/]
- 84. International multicenter validation of AI-driven ultrasound ... [https://www.nature.com/articles/s41591-024-03329-4]
- 85. Multicenter study of CT-based deep learning for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535075/]
- 86. A large-scale, multi-centre validation study of an AI ... [https://www.nature.com/articles/s41698-025-01105-2]
- 87. Externally validated and clinically useful machine learning ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02463-y]
- 88. AI Model Validation: Best Practices for Accuracy & Reliability [https://galileo.ai/blog/best-practices-for-ai-model-validation-in-machine-learning]
- 89. Model Evaluation and Validation in Machine Learning [https://medium.com/ai-disruption/model-evaluation-and-validation-in-machine-learning-709fc0e411d0]
- 90. Explainable AI in Clinical Decision Support Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427955/]
- 91. Interpretable and Explainable Machine Learning Models in ... [https://www.frontiersin.org/research-topics/31441/interpretable-and-explainable-machine-learning-models-in-oncology/magazine]
- 92. Editorial: Interpretable and explainable machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10075249/]
- 93. Explainable AI in medicine: challenges of integrating XAI ... [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1627169/full]
- 94. A simple and fast explainable artificial intelligence-based ... [https://www.nature.com/articles/s41598-025-16842-4]
- 95. SmartSkin-XAI: An Interpretable Deep Learning Approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11720047/]
- 96. The human factor in explainable artificial intelligence [https://www.nature.com/articles/s41746-025-02023-0]
- 97. Innovations in Cancer Imaging and Radiomics through ... [https://www.frontiersin.org/research-topics/69141/innovations-in-cancer-imaging-and-radiomics-through-explainable-artificial-intelligence]
- 98. Federated Learning Vs Classical Machine Learning [https://medium.com/@jamsherbhanbhro/federated-learning-vs-classical-machine-learning-6b8592eb02b4]
- 99. The UK-US Blog Series on Privacy-Preserving Federated ... [https://www.nist.gov/blogs/cybersecurity-insights/uk-us-blog-series-privacy-preserving-federated-learning-introduction]
- 100. Privacy preserving skin cancer diagnosis through ... [https://www.nature.com/articles/s41598-025-19905-8]
- 101. A highly generalized federated learning algorithm for brain ... [https://www.nature.com/articles/s41598-025-05297-2]
- 102. Federated Learning Architecture for 3D Breast Cancer Image ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609610/]
- 103. Enhancing cancer detection in medical imaging through ... [https://www.sciencedirect.com/science/article/pii/S1110866525001446]
- 104. A Comparative Study of Privacy-Preserving Techniques in ... [https://www.mdpi.com/2078-2489/16/3/244]
- 105. Verification, analytical validation, and clinical validation (V3) [https://www.nature.com/articles/s41746-020-0260-4]
- 106. Ethical considerations of use of hold-out sets in clinical ... [https://link.springer.com/article/10.1007/s43681-024-00561-z]
- 107. Development and validation of an interpretable machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899164/]
- 108. Applications of machine learning in drug discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6552674/]
- 109. Performance comparison of four published lung cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541660/]
- 110. A Comprehensive Analysis on Machine Learning based ... [https://www.sciencedirect.com/science/article/pii/S2666521225001139]
- 111. Machine learning-based hepatocellular carcinoma risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504168/]
- 112. The diagnostic accuracy of deep learning-based AI models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599673/]
- 113. Comparative diagnostic accuracy of different artificial ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1670843/full]
- 114. Diagnostic systematic review and meta-analysis of ... [https://www.nature.com/articles/s41598-025-11445-5]
- 115. AI Challenge Models Performance [https://www.rsna.org/news/2025/august/ai-challenge-models-performance]
- 116. Machine learning in colorectal cancer prediction and ... [https://pubmed.ncbi.nlm.nih.gov/41175842/]
- 117. a multicentric study on BRCA-mutated patients undergoing ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1574037/full]
- 118. A novel hybrid deep learning and chaotic dynamics ... [https://www.nature.com/articles/s41598-025-24334-8]
- 119. Digital pathology imaging artificial intelligence in cancer ... [https://www.sciencedirect.com/science/article/pii/S2153353925001178]
- 120. Workflow Integration Analysis of a Human Factors-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8474147/]
- 121. Workflow integration analysis of a human factors-based ... [https://www.sciencedirect.com/science/article/abs/pii/S0003687021001459]
- 122. Usability Challenges in Electronic Health Records: Impact on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206486/]
- 123. Evaluating the Usability, Technical Performance, and ... [https://humanfactors.jmir.org/2025/1/e71434]
- 124. EMR usability and patient safety: a national survey of ... [https://www.nature.com/articles/s41746-025-01657-4]
- 125. Machine learning approach to identify significant genes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547461/]
- 126. AOA Dx Demonstrates High Accuracy in AI-Powered Blood ... [https://aoadx.com/aacr2025/]
- 127. Evaluating AI-enabled Medical Device Performance in ... [https://www.fda.gov/medical-devices/digital-health-center-excellence/request-public-comment-measuring-and-evaluating-artificial-intelligence-enabled-medical-device]
- 128. Maturity Framework for Operationalizing Machine Learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448258/]
- 129. Continuous AI Assurance Framework – Diagnostic Tools [https://applydata.io/continuous-ai-assurance-diagnostic-tools/]